Abstract
Signaling through the B cell receptor (BCR) can drive B cell activation and contribute to B cell differentiation into antibody-secreting plasma cells. The positive BCR signal is counterbalanced by a number of membrane-localized inhibitory receptors that limit B cell activation and plasma cell differentiation. Deficiencies in these negative signaling pathways may cause autoantibody generation and autoimmune disease in both animal models and human patients. We have previously shown that the transcription factor Ets1 can restrain B cell differentiation into plasma cells. Here, we tested the roles of the BCR and inhibitory receptors in controlling the expression of Ets1 in mouse B cells. We found that Ets1 is down regulated in B cells by BCR or TLR signaling through a pathway dependent on PI3 kinase, Btk, IKK2 and JNK. Deficiencies in inhibitory pathways, such as a loss of the tyrosine kinase Lyn, the phosphatase SHP1 or membrane receptors CD22 and/or Siglec-G, result in enhanced BCR signaling and decreased Ets1 expression. Restoring Ets1 expression in Lyn- or SHP1-deficient B cells inhibits their enhanced plasma cell differentiation. Our findings indicate that downregulation of Ets1 occurs in response to B cell activation via either BCR or TLR signaling thereby allowing B cell differentiation and that the maintenance of Ets1 expression is an important function of the inhibitory Lyn → CD22/SiglecG → SHP1 pathway in B cells.
Introduction
B cells differentiate to antibody-secreting plasma cells to mediate the humoral arm of the immune response. Normally this process is under tight control to allow useful antibodies to be produced, while inhibiting the production of pathogenic, autoreactive antibodies. However, in autoimmune diseases in humans and mouse models, B cell differentiation to plasma cells fails to be regulated correctly resulting in autoantibody production. This can arise either through B cell-intrinsic deficiencies or by B cell-extrinsic factors such as aberrant T cell activation.
Activation of B cells can be achieved by antigen binding to the B cell antigen receptor (BCR) and by other pathways such as triggering of Toll-like receptors (TLRs). Antigen binding to the BCR triggers activation of Src family kinases such as Lyn and Fyn leading to phosphorylation of Igα (CD79a) and Igβ (CD79b), recruitment of Syk kinase and subsequent recruitment and phosphorylation of BLNK, Btk and PLCγ (1). These events activate the Ras pathway, PKC pathway and calcium flux, eventually triggering the activation of NF-κB, Erk and JNK. These positive signals are normally counterbalanced by negative signals that limit B cell activation and prevent spontaneous B cell proliferation and differentiation to plasma cells (2). Negative signals are generated by a series of membrane receptors (CD22, CD72, FcγRIIb, PIR-B, Siglec-G, etc.) that are phosphorylated by Lyn. This allows them to recruit phosphatases such as SHP1 and SHIP1 that reverse phosphorylation of signaling molecules in the BCR pathway and dampen BCR signaling (3-5).
Loss of negative signaling leads to increased BCR-dependent B cell activation and can result in autoimmune disease. For instance, Lyn−/− mice, which have defective negative signaling, develop severe autoimmunity (6-9). Reduced Lyn expression has been observed in PBMCs from human autoimmune patients (10, 11). Similarly, loss of SHP1, one of the main phosphatases downstream of Lyn, also results in severe autoimmunity in mice (12, 13). In contrast, loss of membrane receptors such as CD22, CD72, FcγRIIb or Siglec-G alone leads to more modest autoreactive B cell activation, probably due to functional redundancy among these receptors (14-17). Indeed functional redundancy exists since combined deletion of both CD22 and Siglec-G leads to a more severe autoimmune phenotype than loss of either single receptor alone (18). Interestingly, autoimmune disease in Lyn−/− mice can be ameliorated by reducing the levels of Btk, an important BCR effector kinase (19-21). This supports the idea that there is a careful balance between the positive and negative pathways.
Although much is known about the positive and negative signaling pathways that control B cell activation, less is understood about the downstream targets of these pathways or how they regulate B cell differentiation into antibody-secreting plasma cells. However, B cell differentiation is under the control of a network of transcription factors (22). Plasma cell differentiation requires the transcription factor Blimp1 as well as Irf4 and Xbp1. On the other hand the transcription factors Pax5, Bach2 and Ets1 are thought to block plasma cell differentiation.
We observed several phenotypes of mice lacking Ets1 that are common with those of mice lacking Lyn. These include increased B cell activation, decreases in marginal zone B cells, early accumulation of IgM-secreting plasma cells, production of IgG autoAbs with specificities classically-associated with SLE, and immune complex deposition in the kidney (6-8, 23, 24). We theorized therefore that Ets1 might be an important downstream target of the negative signaling pathway regulated by Lyn. In this study, we explored a relationship between Ets1 expression and positive (BCR) and negative signaling in B cells.
Materials and Methods
Mice Used
The following mouse strains were used in this report: C57BL/6, Ets1−/− (23), Lyn−/− (8), Btk−/− (25), Btklo (26), Lyn−/−Btklo mice (27), MD4 BCR transgenic (28), CD19-Cre mice (29), Rosa26 Stop-flox IKK2ca mice (30), B6.Cg-Gpi1a Thy1a Igha/J (congenic IgMa+ C57BL/6), Rag2−/− (31), motheaten viable (mev) (12), FcγRIIb−/− (32), Pten floxed (33), SHP1 floxed (13), SHIP1 floxed (34), mb-1 Cre (CD79a-Cre knockin) (35), CD22−/− mice (14, 36, 37), SiglecG−/−mice (16), CD22−/−SiglecG−/− mice (18), CD72−/− mice (15) and PIR-B−/− (38). All mouse strains were crossed multiple generations onto a C57BL/6 background with the exception of adult Ets1−/− mice (described in (23)) and their littermate controls, since the loss of Ets1 results in perinatal lethality on a C57BL/6 background (39). Adult Ets1−/− mice were instead derived from a C57BL/6 × 129Sv mixed genetic background strain.
Lyn-deficient chimeras were generated by reconstituting lethally-irradiated congenic IgMa+ C57BL/6 hosts with a 50:50 mixture of bone marrow from IgMa+ C57BL/6 and either Lyn+/+ or Lyn−/− (IgMb+). Ets1-deficient chimeras were generated by reconstituting lethallyirradiated Rag2−/− hosts with a 50:50 mixture of fetal liver derived from E16.5 day congenic IgMa+ C57BL/6 embryos and either Ets1+/+ or Ets1−/− (C57BL/6 background, IgMb+) embryos.
Cell lines and reagents
A20 and M12 B cell lymphoma cells were maintained RPMI-1640 medium supplemented with FBS, antibiotics, glutamine and 50 μM β-mercaptoethanol. The retroviral packaging cell line Platinum-E (Plat-E) was maintained in DMEM supplemented with FBS, antibiotics, glutamine, blasticidin and puromycin. Plat-E cells were switched to medium lacking blasticidin and puromycin a day before transfection.
B cell purification and stimulation
B cells were purified from mouse spleens and lymph nodes either by negative selection with CD43 microbeads or by positive selection with B220 or CD19 microbeads (Miltenyi Biotec). Most samples were purified using positive selection with B220 microbeads to obtain better purity, except for the samples listed below.
CD43 microbeads: Wild-type B cells used in signaling experiments, Pten−/− B cells and B cells from Ets1−/− mice and littermate controls (all experiments except Supplemental Figure 1C)
CD19 microbeads: CD22−/−, SiglecG−/−, CD22−/−SiglecG−/− and littermate controls
For in vitro stimulation, purified splenic B cells were allowed to rest in a tissue culture incubator at 37°C for 30 minutes either in media alone or for some experiments in media with specific inhibitors and then stimulated with one or more of the following reagents: anti-IgM F(ab’)2 (Jackson ImmunoResearch) various doses as described in the Figure Legends, 5μg/ml LPS (Sigma Aldrich), 0.5 or 5 μg/ml CpG ODN 1826 (Invivogen), 50 ng/ml PMA (Sigma), 500 ng/ml ionomycin (Calbiochem), 10 μg/ml anti-CD40 (clone3/23 Biolegend), 10 ng/ml IL-4 (R&D Systems) or 100 ng/ml IL-21 (R&D Systems) for the indicated times. For inhibitor experiments, a PI3K kinase inhibitor (LY294002, Cell Signaling), a Btk inhibitor (PCI-32765, Selleckchem), an IKKβ inhititor (Inhibitor IV, Calbiochem), a MEK1 inhibitor (PD98059, Cell Signaling), two JNK inhibitors (SP600125 and JNK-In-8, EMD Millipore) and a p38 inhibitor (SB203580, EMD Millipore) were used. B cells were pretreated with inhibitors for one hour prior to stimulation.
Plasmids and transient transfections
Mouse Ets1 with a C-terminal HA tag was cloned into the retroviral plasmid MIGR1. Plasmids harboring constitutively-active IKK2 (IKK2-CA) (40), kinase inactive IKK2 (IKK2-KI) (40) and constitutively-active JNK (JNK-CA) (41) were purchased from Addgene and the kinase inserts were subcloned into MIGR1 and pCDNA3.1. A retroviral plasmid harboring a constitutively-active form of Akt kinase (myr-Akt) was a kind gift of Dr Kira Gritsman at Brigham and Women’s Hospital, Boston, MA. Myr-Akt was also subcloned from this plamid into pCDNA3.1. pCDNA3.1 plasmids were transfected into A20 B cells by nucleofection and analyzed 8 hours post transfection.
Protein and mRNA stability
To measure protein and RNA stability, purified splenic B cells were treated for 0 to 6 hours with either cycloheximide (200 μM) to inhibit new protein synthesis or with actinomycin D (4 μM) to inhibit RNA transcription. Ets1 levels were assessed by Western blot or RT-qPCR analysis as described below.
Immunoprecipitation Assay
Purified splenic B cells were lysed in a 1% NP-40 lysis buffer with protease and phosphatase inhibitors. Lysates were immunoprecipitated with either a rabbit polyclonal anti-Lyn antibody (Santa Cruz) or a control rabbit IgG antibody. Immunoprecipitates were Western blotted using anti-phosphotyrosine antibody (clone 4G10, Millipore).
ELISPOT assay
ELISPOT analysis was performed as described previously (23, 42). Sorted virally-infected splenic B cells were plated at 500, 1,000, 2,500, 5,000 cells per well. ELISPOT plates were counted with an automated reader (Zellnet Consulting).
Retroviral Production and Transduction
Retrovirus production transductions were performed as previously described (42, 43). Purified splenic B cells were stimulated with 10 μg/ml LPS for 24 hours prior to infection with virus. Two days after infection, GFP-positive populations were sorted using FACsAria Cell Sorter and plated out for ELISPOT assay. Virally-infected cells were also analyzed for B220 and CD138 staining in the GFP+ population.
Western Blot Analysis
Whole B cell lysates were prepared by boiling in Laemmli sample buffer. The following antibodies were used in Western blotting: rabbit monoclonal anti-mouse Ets1 antibody (clone EPR546, Epitomics), mouse monoclonal anti-GAPDH (clone 6C5, Millipore), mouse monoclonal anti-Lyn (clone LYN-01, Biolegend), rabbit monoclonal anti-phospho-Y507 Lyn (EP504Y, Epitomics), rabbit monoclonal anti-phospho-Y396 Lyn (EP503Y, Epitomics), rabbit monoclonal anti-phospho-S473 Akt (clone EP2109Y, Epitomics), rabbit monoclonal anti-IKKβ (clone D30C6, Cell Signaling), rabbit monoclonal anti-phospho-S63-c-Jun (clone 54B3, Cell Signaling) or mouse monoclonal anti-Flag (clone M2, Stratagene). Signals were quantitated by ImageJ software. Loading was normalized by GAPDH levels.
RNA isolation and RT-qPCR
Total RNA was isolated using Direct-zol RNA Purification Kit (Zymo Research). Equal amounts of RNA were reverse-transcribed to cDNA using QuantiTect Reverse Transcription Kit (Qiagen). Quantitative real-time PCR was performed using SYBR Green Supermix (Bio-Rad). Gene expression was normalized to HPRT as reference gene and further normalized to control groups, which were arbitrarily set to a value of 1. The following primers were used:
Ets1: Forward: 5′-AGTCTTGTCAGTCCTTTATCAGC-3′, Reverse: 5′-TTTTCCTCTTTCCCCATCTCC-3′,
Lyn: Forward: 5′-TCCTCGCATCACTTTTCCC3-3′, Reverse: 5′-GATCTCCCAGGCATCTTTATCC-3′,
HPRT: Forward: 5′-CCTCATGGACTGATTATGGACAG-3′, Reverse: 5′-TCAGCAAAGAACTTATAGCCCC-3′,
Statistical analysis
Statistical analysis was performed with the Prism software (GraphPad Software). P-values were determined using unpaired Student’s t-tests (two-tailed) or ANOVA with multiple comparisons test. For half-life experiments, non-linear curve fitting was used and curves were compared with the extra sum-of-squares F test. Differences between groups were considered significant for p-values <0.05.
Results
Both Lyn and Ets1 regulate plasma cell differentiation in a B cell-intrinsic fashion
Both Lyn and Ets1 are highly expressed in B cells (44, 45) and there are B cell abnormalities in mice lacking Lyn or Ets1 including a prominent increase in IgM- and IgG-secreting plasma cells (7, 42). However, Lyn expression is also high in myeloid cells (44), while Ets1 is found at high levels in T cells and NK cells (46, 47). To determine whether Lyn and Ets1 regulate B cell differentiation in a B cell-intrinsic manner, we generated mixed chimeras in which Lyn-deficient or Ets1-deficient B cells develop in the same environment as wild-type B cells (Figure 1A). We transferred bone marrow from Lyn+/+ or Lyn−/− mice on a C57BL/6 genetic background (and hence carrying the IgHb immunoglobulin allotype) along with wild-type congenic bone marrow carrying the IgHa allotype into irradiated congenic C57BL/6 IgMa+ recipients. We made similar chimeras with Ets1−/− mice. However, since virtually all Ets1−/− mice on a C57BL/6 genetic background die at birth (39), we transferred C57BL/6 background Ets1+/+ or Ets1−/− fetal liver cells from E16.5 day embryos (IgHb) along with wild-type IgHa E16.5 day fetal liver cells into irradiated Rag2−/− recipients. All chimeras were allowed to reconstitute for 6-8 weeks prior to analysis.
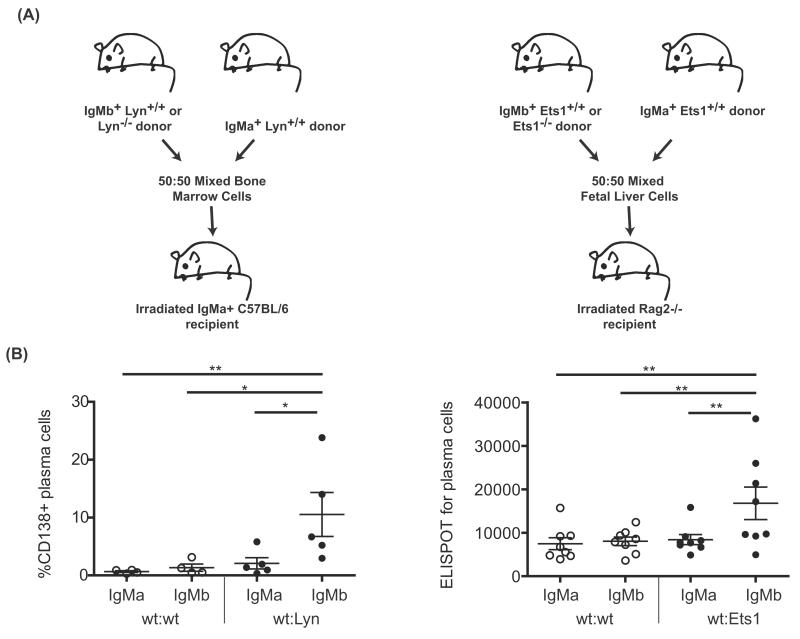
Figure 1. Both Lyn and Ets1 regulate plasma cell differentiation in a B cell-intrinsic fashion.
(A) Lyn-deficient bone marrow chimeras were generated by mixing wild-type congenic B6.IgMa bone marrow with IgMb+ C57BL/6 genetic background Lyn+/+ or Lyn−/− bone marrow and transferring into irradiated B6.IgMa recipients. Ets1-deficient bone marrow chimeras were generated by mixing wild-type congenic B6.IgMa fetal liver cells from E16.5 day embryos with C57BL/6 IgMb+ Ets1+/+ or Ets1−/− fetal liver cells (also from E16.5 day embryos) and transferring into irradiated Rag2−/− recipients. (B) Six to eight weeks later, the frequency of B220loCD138hi plasma cells among IgMa (wild-type) and IgMb (wild-type or Lyn−/−) expressing cells was determined by flow cytometry. In Ets1-deficient chimeras, IgMa (wild-type) and IgMb (wild-type or Ets1−/−) plasma cells were enumerated with allotype-specific ELISPOT. Two separate groups of 3-4 chimeric mice of each genotype were generated and analyzed independently. *p<0.05, **p<0.01.
After reconstitution, allotype-specific plasma cells were enumerated in Lyn+/+ and Lyn−/− chimeras using flow cytometry. Because Lyn−/− B cells compete poorly with wild-type cells in mixed chimeras (data not shown), we used flow cytometry to determine the frequency of B220loCD138hi cells among IgMa and IgMb expressing cells. As shown in Figure 1B, Lyn−/− B cells differentiate more readily to plasma cells than do wild-type B cells developing in the same environment. Because similar numbers of Ets1+/+ and Ets1−/− derived B cells develop in chimeric mice, we quantitated allotype-specific plasma cells using ELISPOT assays. Like Lyn−/− B cells, Ets1−/− B cells showed an intrinsic propensity to differentiate to plasma cells.
Ets1 deficiency does not change expression or phosphorylation of Lyn in B cells
As both Ets1 and Lyn regulate B cell differentiation in a B cell-intrinsic fashion and control B cell secretion of autoantibodies, we hypothesized that they may act in the same signaling pathway. We first asked whether Ets1 can regulate Lyn expression or phosphorylation. Lyn expression was normal at both the protein and mRNA level in B cells from Ets1−/− mice (Supplemental Figure 1A-B). Phosphorylation of Y508 inhibits Lyn activity, whereas phosphorylation of Y397 stimulates Lyn activity (48). Neither of these phosphorylation events was altered in resting Ets1−/− B cells (Supplemental Figure 1A), nor was total tyrosine phosphorylation of Lyn (Supplemental Figure 1D). Unexpectedly, Lyn Y397 phosphorylation was not significantly induced by BCR crosslinking in either wild-type or Ets1−/− B cells (Supplemental Figure 1C), but rather showed high levels prior to stimulation. High basal levels of Y397 phosphorylation of Lyn in hematopoietic cells have also been observed in other studies (49-51). This may be relevant to its role in signaling through inhibitory pathways. Therefore, it appears that Ets1 does not regulate the expression of the Lyn gene nor other genes that control the activity of kinases or phosphatases that regulate Lyn.
Ets1 levels are downregulated in Lyn−/− B cells
Since Ets1 did not appear to be upstream of Lyn, we asked if Lyn might instead regulate levels of Ets1. Ets1 protein levels were downregulated in Lyn−/− B cells compared to B cells from wild-type mice (Figure 2A). As Lyn−/− mice age, they develop severe autoimmunity accompanied by increased levels of inflammatory cytokines such as IL-6 (21, 52, 53). To determine whether downregulation of Ets1 in Lyn−/− B cells was due to the inflammatory environment that develops in these mice as they age, we compared Ets1 protein levels in B cells isolated from young pre-diseased mice (Figure 2B). Ets1 was downregulated in B cells even in Lyn−/− mice as young as 1 month old, suggesting that this is a primary defect and not a secondary effect of the autoimmune disease. Quantification of Western blots showed that on average Ets1 protein was expressed in Lyn−/− B cells at levels ~27 ± 5% of the levels in wild-type B cells (p<0.0001). We also examined Ets1 mRNA levels in Lyn−/− B cells and found that these were also decreased (Figure 2C). In most experiments the protein levels of Ets1 seemed to show a somewhat stronger decrease than the mRNA levels in Lyn−/− B cells, indicating that Lyn might regulate not only Ets1 mRNA expression, but also Ets1 protein synthesis or stability.
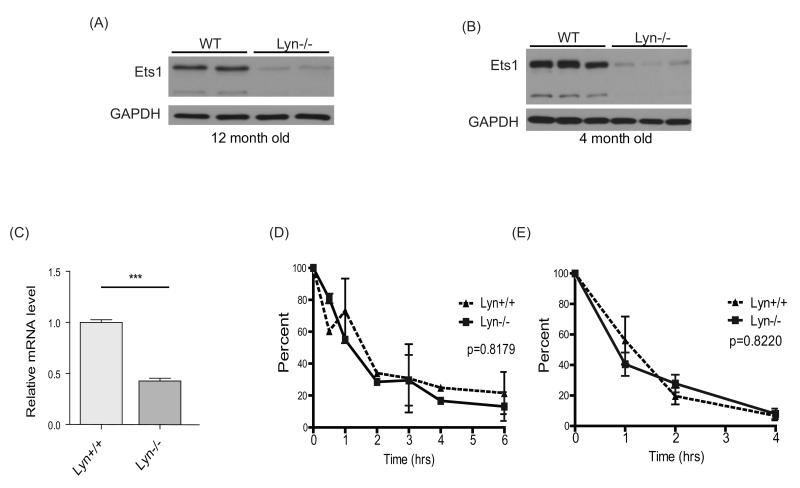
Figure 2. Lyn regulates Ets1 levels in B cells.
(A) Western blot analysis of splenic B cell lysates from two wild-type and two Lyn-deficient mice at (A) 12 months of age or (B) 4 months of age shows downregulation of the two most predominant isoforms of Ets1, the p54 and p42 isoforms, in Lyn−/− cells. Nine separate Western blots for Ets1 were done and included 18 wild-type and 15 Lyn−/− mice analyzed at ages between 1-12 months. (C) RT-qPCR analysis of Ets1 mRNA in B cells from wild-type (Lyn+/+, n=7) and Lyn−/− (n=6) mice. ***p< 0.001 (D) Wild-type (WT) or Lyn−/− splenic B cells were treated with cycloheximide for various times to inhibit protein synthesis and Western blot was performed to measure the levels of Ets1 protein. GAPDH was used as loading control, as it has been reported to have a long half-life (85), and its levels were not changed during the treatment time. Average values of three independent experiments are shown as the quantified ratio of the major p54 isoform of Ets1 to the levels of GAPDH, normalized to the levels at time 0. (E) Equal numbers of B cells from each genotype were treated with actinomycin D for various times to suppress mRNA transcription. Ets1 mRNA levels were measured by RT-qPCR and normalized by the level at time 0. Data represent quantitation of both major RNA isoforms of Ets1 (encoding the p54 and p42 variants of the protein) from three independent experiments. No differences were observed when independently calculating the half-life of each separate isoform.
To better define the mechanisms that regulate Ets1 protein and mRNA levels in Lyn−/− B cells, we measured the half-life of Ets1 protein and mRNA by treating B cells with cycloheximide or actinomycin D to inhibit protein or mRNA synthesis, respectively. The half-life of Ets1 protein was short, about ~1.1 hours in wild-type B cells (Figure 2D), and was unchanged in Lyn-deficient B cells. The half-life of Ets1 mRNA was also short (~ 1 hour) in wild-type B cells (Figure 2E) and slightly shorter (~45 minutes) in Lyn−/− B cells, but this difference was not statistically-significant. Since the absence of Lyn appears to result in very minor or no changes to the stability of Ets1 mRNA and protein, downregulation of Ets1 mRNA in Lyn−/− B cells may instead result from decreased transcription of the Ets1 gene. Downregulation of Ets1 protein may be a combined effect of decreased mRNA levels and inhibition of mRNA translation into protein.
Ets1 can be downregulated by BCR and TLR signaling
One major function of Lyn in B cells is to inhibit BCR signaling via its ability to phosphorylate inhibitory receptors. Thus, BCR signaling is hyper-active in Lyn−/− B cells. Ets1 levels can be downregulated by activation of the antigen receptors in B cells and T cells (54, 55). We theorized that enhanced BCR signaling in Lyn−/− B cells might cause downregulation of Ets1 in these cells, leading to enhanced plasma cell formation.
To clarify signaling cascades in the downregulation of Ets1, we treated wild-type B cells with BCR-crosslinking agents and other types of stimuli. As expected, BCR crosslinking downregulated Ets1 protein and mRNA levels within a few hours after stimulation (Figure 3AB). BCR activation induces mobilization of intracellular calcium and activation of Ras and PKC enzymes. PMA can induce Ras and PKC activation, while ionomycin can transport calcium across the plasma membrane resulting in elevated intracellular calcium. Hence, PMA and ionomycin mimic many aspects of BCR signaling. Stimulation of splenic B cells with either ionomycin or PMA alone (Figure 3A) or both together (not shown) downregulated Ets1 protein within 4 hours, whereas treatment with vehicle (DMSO) alone had no effect. Although both PMA and ionomycin were equally effective in down-regulating the protein levels of Ets1, PMA was more effective in down-regulating the Ets1 message than was ionomycin (Figure 3B), suggesting they may modify Ets1 expression by somewhat different mechanisms.
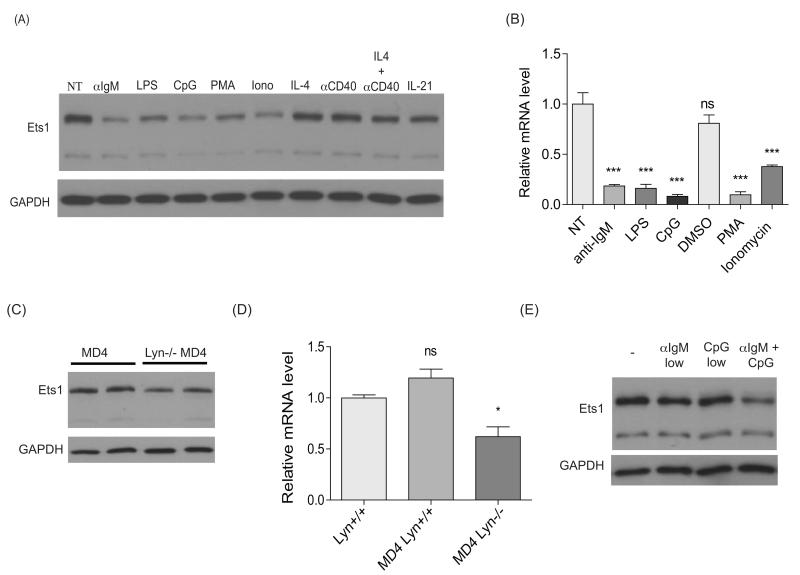
Figure 3. Ets1 is downregulated by BCR or TLR activation as well as PMA or Ca2+ flux.
(A) Purified wild-type splenic B cells were rested at 37°C for 30 minutes in a tissue-culture incubator and then left untreated (NT) or treated with the stimuli indicated for 4 hours, followed by Western blotting for Ets1 and GAPDH. Western blots with each type of stimulus were repeated a minimum of 3 separate times. (B) mRNA was purified from B cells stimulated for 2 hours with stimuli that downregulate Ets1 protein levels as shown in part A and analyzed by RT-qPCR. Shown is the average of 3 separate experiments. (C) Western blot for Ets1 and GAPDH with lysates of B cells purified from MD4 Lyn+/+ or MD4 Lyn−/− mice. Shown is representative data from 1 of 3 independent experiments (total of 5 MD4 Lyn+/+ and 6 MD4 Lyn−/− mice analyzed) (D) RT-qPCR analysis of Ets1 mRNA in B cells from wild-type (WT, n=3), MD4 Lyn+/+ (n=6) or MD4 Lyn−/− mice (n=6). (E) B cells isolated from wild-type mice were stimulated with either 1 μg/ml of anti-IgM or 0.5 μg/ml of CpG ODN or a combination of both stimuli for 3.5 hours. Representative data from one of two similar experiments is shown. *p< 0.05, ***p<0.001.
To test whether BCR signaling was required for the downregulation of Ets1 levels in vivo, we generated MD4 BCR transgenic Lyn−/− mice. The MD4 transgene encodes heavy and light immunoglobulin chains that confer specificity to the foreign antigen hen egg lysozyme (HEL) (28). B cells from MD4 transgenic mice are thus naïve since they do not encounter antigen. MD4+ Lyn−/− B cells exhibited a less dramatic reduction of Ets1 levels than non-transgenic Lyn−/−B cells (Figure 3C-D, compare to Figure 2A, 2B, 3A). Quantification indicated that MD4+ Lyn−/− B cells express ~54 ± 7% as much Ets1 as do non-transgenic or MD4+ wild-type B cells (p<0.0001). This suggests that BCR signaling in response to antigen binding plays a role in the downregulation of Ets1 in Lyn−/− B cells. However, fixing the BCR to a non-self antigen did not fully restore Ets1 expression to wild-type levels.
B cells can also be activated and induced to differentiate by certain TLR ligands, such as LPS and unmethylated CpG containing DNA sequences (CpG DNA). As shown in Figure 3A, both LPS and CpG DNA can downregulate Ets1 levels shortly after stimulation. Furthermore, low levels of anti-IgM cooperate with low levels of CpG DNA to induce downregulation of Ets1 (Figure 3E). We also tested a variety of other stimuli that activate B cells including IL-4, anti-CD40, IL-21, IL-6 and TGF-β, none of which significantly affected the expression of Ets1 protein (Figure 3A and data not shown). Based on these results, either BCR or TLR signaling can down regulate Ets1 levels in B cells.
PI3 kinase and Btk, but not Akt, are required for Ets1 downregulation during B cell activation
The BCR signaling component Btk is a target of several Lyn-dependent inhibitory signaling pathways (56, 57). To determine the role of Btk in the downregulation of Ets1, we examined Ets1 levels in Lyn−/−Btklo mice, which express low levels of Btk in B cells and do not accumulate plasma cells (21, 26). Interestingly, reduced Btk signaling led to a restoration of Ets1 protein expression in Lyn−/− B cells (Figure 4A). Quantification indicated that Lyn−/−Btklo B cells express on average 118 ± 4% as much Ets1 as wild-type B cells (p = not significant). Ets1 mRNA levels were also partially restored in Lyn-deficient B cells by reducing Btk signaling (Figure 4B). This suggests that Lyn regulates Ets1 expression by inhibiting positive BCR signaling which requires Btk activity. We further analyzed the role of Btk signaling in down-regulating Ets1 by stimulating wild-type, Btklo or Btk−/− B cells wild-type for Lyn with anti-IgM. Although the Btk-deficient B cells responded to IgM-crosslinking by induction of Akt phosphorylation similar to wild-type B cells, they failed to downregulate Ets1 (Figure 4C).
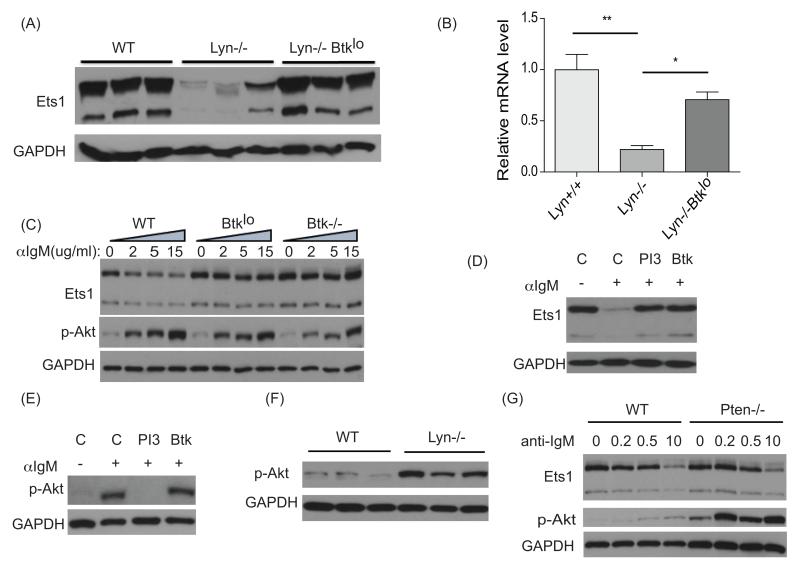
Figure 4. Ets1 downregulation in Lyn−/− B cells is dependent on signaling via Btk.
(A) Western blot for Ets1 and GAPDH with B cell lysates from wild-type (WT), Lyn−/− or Lyn−/−Btklo B cell mice (shown is a representative example of 3 independent experiments, n=4-5 mice of each genotype analyzed in total) (B) RT-qPCR analysis of Ets1 mRNA in B cells from wild-type, Lyn−/− or Lyn−/−Btklo mice (n=3 for each genotype). (C) Purified splenic B cells from wild-type (WT), Btklo or Btk−/− mice were rested at 37°C for 30 min before treatment with the indicated dose (μg/ml) of anti-IgM for 3.5 hours. Western blot for Ets1, p-Akt and GAPDH levels was performed with cell lysates. One of two similar experiments is shown. (D) Wild-type splenic B cells were rested at 37°C and pretreated with either DMSO vehicle control (labeled C), 5 μg/ml of a PI3K inhibitor Ly294002 (labeled PI3), 100 ng/ml of a Btk inhibitor PCI32765 (labeled Btk) for 1 hour, then stimulated with 10 μg/ml anti-IgM for 3.5 hours. Cell lysates were analyzed for Ets1 and GAPDH levels by Western blot. One of two similar experiments is shown. (E) To test the specificity of the inhibitors used in part D, cells were stimulated for 5 minutes and levels of phospho-S473 of Akt (activated Akt) were measured. One of two similar experiments is shown. (F) Western blot with lysates from wild-type (WT) or Lyn−/− B cells to show constitutive activation of the Akt pathway in the absence of Lyn. One of three similar experiments is shown. (G) Splenic B cells from wild-type (WT) or Pten−/− mice were rested at 37°C for 30 minutes followed by treatment with the indicated dose (μg/ml) of anti-IgM for 3.5 hours. Cell lysates were analyzed by Western blot. Shown is the data from one of two similar experiments. *p< 0.05, **p<0.01.
Btk binds to phosphatidyl inositol (3,4,5) trisphosphate (PIP3) produced by the activity of PI3 kinase. Binding of Btk to PIP3 is required for its maximal activation (58, 59), suggesting that PI3 kinase activity may be required for downregulation of Ets1. To further validate the involvement of PI3 kinase and Btk signaling pathways in regulating Ets1 expression, we pretreated B cells with DMSO (Control), a PI3K inhibitor (LY294002) or a Btk inhibitor (PCI-32765) followed by stimulation with anti-IgM crosslinking antibody (Figure 4D). Inhibiting either PI3 kinase or Btk was sufficient to prevent Ets1 downregulation in response to BCR crosslinking. To test specificity of the inhibitors used above, we confirmed that the PI3 kinase inhibitor, but not the Btk inhibitor, could block activation of Akt (Figure 4E).
Because PI3 kinase activity is essential for downregulating Ets1, we sought to determine whether PI3 kinase induced activation of Akt was also important. Akt is constitutively-phosphorylated in Lyn−/− B cells (Figure 4F), likely due to hyper-active BCR signaling. However, Akt activation did not correlate with the levels of Ets1. Akt was normally activated in BCR-stimulated Btk-deficient B cells or when Btk inhibitor was used, but Ets1 levels were not downregulated. To further study the involvement of the PI3→Akt kinase pathway in the regulation of Ets1 levels, Pten−/− B cells (derived from CD19-Cre PtenloxP/loxP mice) were used (Figure 4F). Pten−/− B cells produce increased PIP3 upon BCR crosslinking, resulting in increased activation of Akt and presumably other PIP3-dependent enzymes (33). In keeping with this, we detected robust Akt phosphorylation with a low dose of anti-IgM stimulation in Pten-deficient B cells, but not in wild-type cells (Figure 4G). However, Ets1 downregulation was not enhanced in Pten−/− B cells indicating that supra-physiological levels of PIP3 are not required for the downregulation of Ets1. This data also supports the idea that Akt activation does not regulate Ets1 levels, as Akt is hyper-activated upon BCR crosslinking in Pten−/− B cells, yet Ets1 levels are similar to those found in wild-type B cells under the same conditions. Taken together, these results suggested that PI3 kinase and Btk signaling, but not Akt signaling, are involved in regulating Ets1 expression during B cell activation.
IKK and JNK signaling downstream of BCR and TLR receptors regulate Ets1 levels
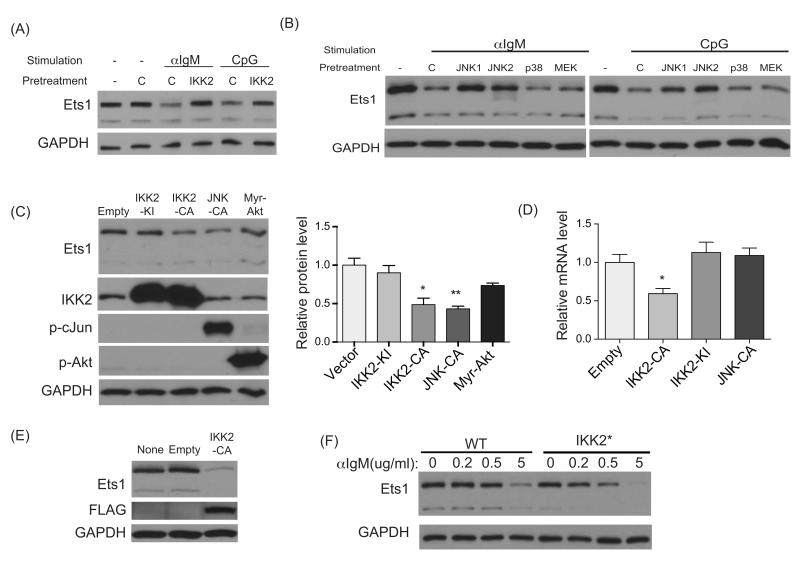
Btk signaling is crucial for activating the NF-κB pathway in B cells (60, 61). NF-κB signaling is also triggered by TLR ligation and by treatment of B cells with PMA, stimuli that we have shown above to result in downregulation of Ets1 expression. We hypothesized that NF-κB may inhibit the expression of the Ets1 gene, either directly or indirectly. To test this, we pre-treated primary B cells with an inhibitor of the IKK2 subunit of the NF-κB activating IKK complex followed by crosslinking the BCR with anti-IgM or activating TLR signaling with CpG DNA. The IKK2 inhibitor was able to prevent downregulation of Ets1 by either anti-IgM or TLR agonists (Figure 5A), confirming a role for the NF-κB signaling pathway in Ets1 regulation.
Figure 5. IKK2 and JNK both contribute to downregulating Ets1.
For experiments shown in parts A-B, wild-type splenic B cells were rested at 37°C and then pretreated with either DMSO vehicle control (labeled C) or with the inhibitors indicated below for 1 hour. Cells were then stimulated for 3.5 hours with anti-IgM (10 μg/ml) or CpG (5 μg/ml) for 3.5 hours followed by Western blotting for Ets1 and GAPDH. (A) Cells treated with 5 μg/ml IKK2 inhibitor IV (labeled Ikk2). Shown is data from one of 3 similar experiments. (B) Cells were treated with 25 μg/ml of one of two JNK inhibitors (SP600215 labeled JNK1 or JNK-In-8 labeled JNK2), 25 μg/ml of a p38 inhibitor (labeled p38) or 30 μg/ml of a MEK inhibitor (labeled MEK). One of two similar experiments is shown. (C) A20 B lymphoma cells were nucleofected with an empty vector or vectors carrying kinase inactive IKK2 (IKK2-KI), constitutively-active IKK2 (IKK2-CA), constitutively active JNK (JNK-CA) or constitutively-active Akt (Myr-Akt). Eight hours post-nucleofection, cells were harvested and processed for Western blot to detect the levels of Ets1, IKK2, phospho-cJun, phospho-Akt and GAPDH. Shown are the results of one of three similar independent experiments. Also shown is a quantification of the 3 Western blots with statistical analysis. (D) Cells transfected as in (C) were used to prepare RNA and measure Ets1 and HPRT by RT-qPCR. Shown is the average value of 3 independent experiments. (E) M12 B cell lymphoma cells were infected with an empty virus or a virus carrying a constitutively-active form of IKK2 (IKK2-CA). Infected cells (GFP+) were sorted by FACS 48 hours later. The sorted cells were returned to culture for another 24-72 hours before being analyzed by Western blot for Ets1, GAPDH and FLAG (the epitope tag on IKK2-CA). Shown are the results of one representative experiment of 3 replicates done (experiment shown was harvested at 72 hours post-sort). (F) Splenic B cells were isolated from wild-type (WT) or CD19-Cre x Rosa26 Stop-flox IKK2ca mice (labeled IKK2*) and then stimulated with indicated doses of anti-IgM for 3.5 hours before being analyzed by Western blot. Shown are representative results from one of two independent experiments. *p< 0.05, **p<0.01.
Btk has also been implicated in the activation of JNK MAP kinase and in some, but not all, studies in the activation of Erk MAP kinase (20, 62-65). We tested whether inhibition of MAP kinase pathways could prevent downregulation of Ets1. We pre-treated primary B cells with either an inhibitor of MEK kinases (the upstream activators of Erk), with two different JNK inhibitors or with a p38 inhibitor. After pre-treatment for 1 hour, B cells were stimulated by crosslinking the BCR with anti-IgM or activating TLR signaling with CpG DNA (Figure 5B). Both of the JNK inhibitors were able to prevent downregulation of Ets1 by either anti-IgM or CpG DNA. However, neither the MEK inhibitor nor the p38 inhibitor prevented Ets1 downregulation.
To further explore potential roles for IKK2, JNK and Akt in regulating Ets1 levels, we transfected A20 B lymphoma cells with plasmids encoding a constitutively-active version of IKK2 (IKK2-CA), a kinase-dead form of IKK2 (IKK2-KI), a constitutively-active version of JNK1 (JNK-CA) or a constitutively-active version of Akt (Myr-Akt). BCR crosslinking downregulates Ets1 expression in A20 B cells in a similar fashion to that seen in primary splenic B cells (data not shown), suggesting that A20 cells are a suitable model for studying pathways regulating Ets1. The constitutively-active form of IKK2 was capable of downregulating Ets1, while the kinase-inactive form failed to do so (Figure 5C-D). Similarly, transfection of the constitutively-active JNK plasmid (denoted JNK-CA) in A20 cells also resulted in downregulation of Ets1 protein (Figure 5C), although not Ets1 mRNA (Figure 5D). Transfection of constitutively-active Akt resulted in a modest downregulation of Ets1 (to about ~75% of the levels in vector-transfected cells), but this was not statistically-significant. We also attempted to generate stable cell lines using viruses containing constitutively-active IKK2 and JNK. We were unable to obtain long-term, stable expression of IKK2-CA in A20 B cells, but we did obtain such expression in another B cell line, M12 B lymphoma cells, using retroviral transduction (Figure 5E). In these cells, stable expression of IKK2-CA leads to a dramatic downregulation of Ets1. Stable expression of JNK-CA was not obtained in either B cell line, likely due to its effects on cellular apoptosis.
We also examined primary B cells purified from mice expressing constitutively-active IKK2 under the control of a CD19-Cre-responsive locus (designated IKK2* mice) (30). B cells from IKK2* mice had normal levels of Ets1 in the resting state, but low doses of anti-IgM that failed to induce downregulation of Ets1 in wild-type B cells were able to do so in IKK2* B cells (Figure 5F). Together the data suggest that both IKK2 and JNK are important downstream effectors of BCR and TLR signaling that modulate Ets1 levels, but that Akt plays only a minor role.
Ets1 levels are maintained in B cells by phosphatases that inhibit BCR signaling
Lyn is crucially-important for negative signaling pathways that limit B cell activation, while other Src family kinases can substitute for Lyn in positive signaling via the BCR (8, 9). We hypothesized that loss of negative signaling in Lyn-deficient B cells, which results in enhanced positive activation signals, triggers the downregulation of Ets1. When phosphorylated by Lyn, inhibitory receptors such as CD22, CD72, PIR-B, Siglec-G, FcγRIIb and others recruit phosphatases (SHP1 or SHIP1) to reverse the positive phosphorylation events triggered by BCR signaling (4). Loss of SHP1, SHIP1 or the inhibitory receptors results in autoantibody secretion to varying degrees (4, 13, 18, 66, 67).
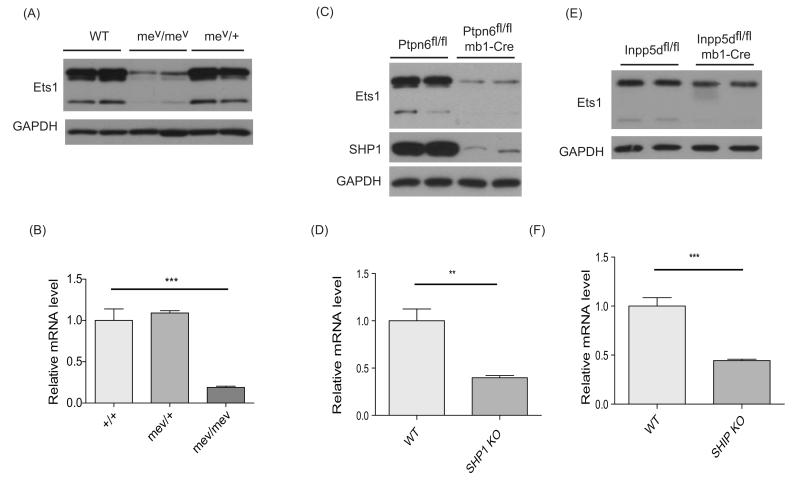
We first examined the role of SHP1 in regulating Ets1 because the majority of negative receptors phosphorylated by Lyn recruit SHP1 rather than SHIP1. We purified B cells from motheaten viable mice (mev mice), which harbor a loss of function mutation in the Ptpn6 gene (encoding SHP1) (12). Ets1 levels were dramatically reduced in B cells from mev mice compared to wild-type or heterozygous mice (Figure 6A-B). Quantification indicated that mev B cells express ~9 ± 4% as much Ets1 as do wild-type B cells (p<0.0001). mev mice develop severe inflammatory disease within weeks of birth that results in a greatly altered immune cell environment that could influence B cell differentiation (68). We therefore examined Ets1 expression in B cells from mice with a B cell-specific deletion of SHP1 (mb1-cre Ptpn6f/f mice, hereafter referred to as SHP1−/−), in which B cells develop in a more normal environment. Ets1 was also very much downregulated in these B cells to an average of 12 ± 3% the levels in wild-type B cells (p<0.0001) (Figure 6C-D). The downregulation of Ets1 in B cells lacking SHP1 was stronger than is its downregulation in B cells lacking Lyn, indicating that SHP1 may function via both Lyn-dependent and Lyn-independent mechanisms to control Ets1 levels.
Figure 6. SHP1 is the major phosphatase regulating Ets1 levels in B cells.
(A) Western blot for Ets1 and GAPDH with B cell lysates from wild-type or motheaten viable mice with heterozygous (mev/me+) or homozyogous (mev/mev) mutations in the SHP1 phosphatase (shown are representative results from one of 3 separate experiments, n=4 mice of each genotype in total analyzed) (B) RT-qPCR analysis of Ets1 mRNA in B cells from mev mice (n=3 for each genotype). (C) Western blot for Ets1 and GAPDH with B cell lysates from wild-type, Ptpn6fl/fl (SHP1 floxed) and Ptpn6fl/fl mb1-Cre (SHP1 knockout) mice. Shown are the results of one of three independent experiments (with a total of 6 mice of each genotype analyzed). (D) RT-qPCR analysis of Ets1 mRNA in B cells from SHP1fl/fl and SHP1fl/fl mb1-Cre mice (n=4 mice of each genotype). (E) Western blot for Ets1 and GAPDH with B cell lysates from wild-type mice, Inpp5dfl/fl (SHIP1 floxed) or CD19-Cre Inpp5dfl/fl (SHIP1 knockout) mice. Shown are the results of one of two independent experiments (with a total of 4 mice of each genotype analyzed). (F) RT-qPCR analysis of Ets1 mRNA in B cells from Inpp5dfl/fl or Inpp5dfl/fl mb1-Cre mice (n=4 for each genotype). **p< 0.01, ***p<0.001.
We next examined B cells from mice with a B cell specific deletion of the SHIP1 phosphatase (mb1-cre Inpp5df/f mice, hereafter referred to as SHIP1−/−). Ets1 expression was lower in SHIP1-deficient B cells than in wild-type B cells, but the difference was not as striking as in B cells lacking SHP1 (Figure 6E-F). Indeed, SHIP1−/− B cells express ~61 ± 5% as much Ets1 as do wild-type B cells (p<0.001). These observations suggest that SHP1 is the major phosphatase that controls Ets1 expression, but that SHIP1 may also contribute in a smaller way.
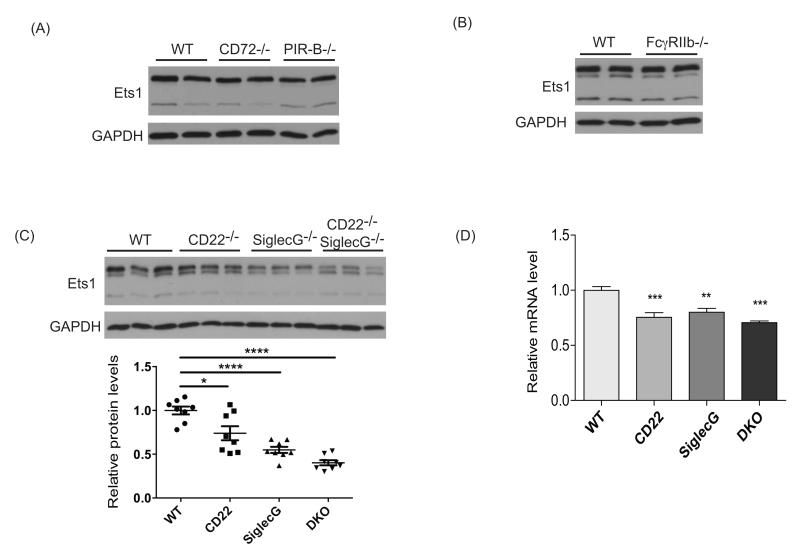
To test the role of cell surface receptors that are phosphorylated by Lyn and that recruit phosphatases, we purified B cells from several different mouse strains lacking individual inhibitory receptors. Ets1 levels were largely normal in B cells lacking FcγRIIb (92 ± 10% of wild-type levels), PIR-B (90 ± 8% of wild-type levels) or CD72 (98 ± 8% of wild-type levels) (Figure 7A-B). In contrast, loss of CD22 or SiglecG resulted in lower expression of Ets1 (Figure 7C), although the effect was modest when compared to loss of either Lyn or SHP1 (levels in CD22−/− were 74 ± 8% of wild-type (p<0.01) and levels in SiglecG−/− were 55 ± 4% of wild-type levels (p<0.0001)). Because CD22 and SiglecG are functionally redundant in regulating B cell responses (18), we also examined Ets1 expression in B cells lacking both CD22 and SiglecG. Ets1 expression in these cells was less than in either CD22−/− or SiglecG−/− B cells (levels in CD22−/−SiglecG−/− B cells were 40 ± 3% of levels in wild-type B cells (p<0.0001)) (Figure 7C), but still not as low as the levels Lyn−/− or SHP1−/− B cells. These results suggest that CD22 and SiglecG are both involved in control of Ets1 expression, but that other Lyn- and SHP1-dependent receptors likely also play a role.
Figure 7. CD22 and SiglecG both contribute to maintaining Ets1 expression in B cells.
(A) Western blot for Ets1 and GAPDH with B cell lysates from wild-type (WT), CD72−/− or PIR-B−/−mice. Shown are results of one of two independent experiments with a total of 4 mice of each genotype being analyzed. (B) Western blot for Ets1 and GAPDH with B cell lysates from wild-type (WT) or FcγRIIb−/− mice. Shown are results of one of two independent experiments with a total of 3 mice of each genotype. (C) Western blot for Ets1 and GAPDH with B cell lysates from wild-type (WT), CD22−/−, SiglecG−/− or CD22−/−SiglecG−/− mice. Shown are the results of one of two independent experiments (n = 8 mice of each genotype). Below is a quantification of multiple Western blots. **p< 0.01, ***p<0.001 (D) RT-qPCR analysis of Ets1 mRNA in B cells from wild-type (WT), CD22−/−, SiglecG−/− or CD22−/−SiglecG−/− B cells (n= 5 for each genotype) ***p< 0.001, ****p<0.0001.
Restoration of Ets1 limits the differentiation of Lyn or SHP1 deficient B cells into plasma cells in vitro
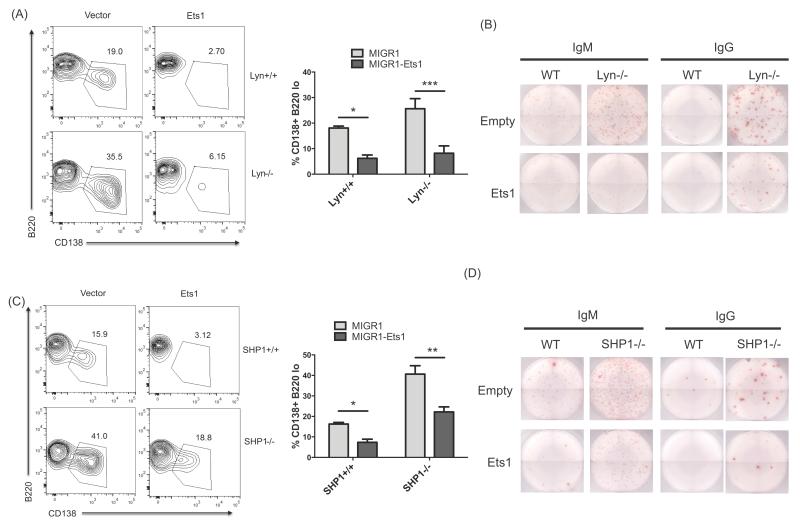
B cells lacking Lyn or SHP1 show a major defect in expression of Ets1, which is known to control plasma cell differentiation. However, Lyn and SHP1 likely also control other pathways that influence B cell differentiation. To determine whether the downregulation of Ets1 in Lyn−/− or SHP1−/− B cells was important for their increased propensity to differentiate to plasma cells, we restored Ets1 expression in these cells using a retroviral construct and measured their differentiation in response to LPS. Both Lyn−/− and SHP1−/− B cells showed increased differentiation to plasmablasts as compared to wild-type B cells. Enforced expression of Ets1 could limit plasmablast differentiation in wild-type as well as Lyn−/− and SHP1−/− B cells. This was evident both in flow cytometry (as measured by a B220low CD138+ phenotype, Figure 8A & C) as well as in ELISPOT assays to measure IgM- and IgG-secreting cells among retrovirally transduced cells (Figure 8B & D). Although loss of Lyn or SHP1 presumably alters the expression of a large number of genes, our results suggest that maintenance of Ets1 is a key event under the control of a Lyn → CD22/SiglecG → SHP1 pathway that is crucial for limiting B cell differentiation in response to TLR stimulation.
Figure 8. Ets1 prevents excess differentiation of Lyn−/− or SHP1−/− B cells.
Total splenocytes from Lyn deficient (A-B) or B220+ splenic B cells from SHP1 deficient mice (C-D) were stimulated overnight with LPS to induce cell cycle progression. Cells were infected with an empty retrovirus (Empty) or with a virus-containing mouse Ets1 (Ets1). (A and C) Flow cytometry was performed after 2 additional days in culture with LPS to determine the frequency of B220lowCD138high plasma cells (plasmablasts) among GFP+ virally-infected cells. Shown is a representative flow plot as well as quantification of four (Lyn−/−) or five (SHP1−/−) separate experiments in the bar graphs. (B and D) GFP+ cells were also sorted out and replated in LPS-containing medium for an additional day on ELISPOT plates for enumeration of IgM- and IgG-secreting plasma cells. Three independent experiments were performed with similar results. **p< 0.01, ***p<0.001.
Discussion
B cells can be triggered to differentiate into plasma cells that secrete antibodies, a process relevant to both normal immune responses and autoimmune diseases. BCR signaling pathways can promote B cell differentiation to antibody-secreting plasma cells (69, 70) and are normally counterbalanced by inhibitory signaling pathways such that B cell differentiation is limited (4). The crucial targets whose expression is regulated by the BCR pathway and inhibitory signaling pathways have remained ill-defined. In this report, we have determined that the transcription factor Ets1 and the tyrosine kinase Lyn both play B cell-intrinsic roles in regulating plasma cell formation. Consistent with these findings, B cell-specific deletion of Lyn results in increased plasma cells and autoantibody secretion (71). We have further demonstrated that Ets1 is downregulated by the BCR signaling cascade and that its expression is maintained in naïve B cells by Lyn-dependent inhibitory signaling pathways. We also found that PMA or ionomycin, which mimic some aspects of BCR signaling, or TLR ligands (LPS or CpG DNA) can also downregulate Ets1 expression in B cells. Interestingly, low levels of anti-IgM stimulation cooperated with low levels of CpG stimulation to downregulate Ets1. This may be relevant to autoimmune disease where combined BCR/TLR ligation can drive autoantibody production (72). In contrast to BCR and TLR signaling, signaling via CD40 or a number of different cytokine receptors that activate Stat1, Stat3 or Stat6 failed to alter Ets1 levels in B cells.
Ets1 inhibits B cell differentiation to antibody-secreting plasma cells by both stimulating the expression of Pax5 and by blocking Blimp1 DNA binding (42, 43). Thus, downregulation of Ets1 can explain the ability of the BCR and TLRs to promote B cell differentiation. It is likely that the inhibitory Lyn → CD22/SiglecG → SHP1 pathway that normally counterbalances B cell activation regulates a number of different transcriptional programs to control B cell differentiation. However, the key role of Ets1 as an important down-stream target of this pathway is demonstrated by the ability of virally-expressed Ets1 to suppress the excessive plasma cell formation characteristic of both Lyn−/− and SHP1−/− B cells in response to LPS stimulation.
Ets1−/− B cells expressed normal levels of Lyn and showed normal phosphorylation of Lyn in basal and stimulated states. However, both Ets1 protein and mRNA levels were downregulated in B cells from Lyn-deficient mice. Ets1 levels are low in B cells from both young and aged Lyn−/− mice, indicating that development of frank autoimmune disease or of an inflammatory environment is not necessary for the down-modulation of Ets1.
Analysis of Ets1 protein levels in Lyn−/− B cells showed that they were dramatically downregulated (~25-30% of the level in wild-type B cells). The level of Ets1 mRNA was also reduced in Lyn−/− B cells, but not by as much (~50% of the level of wild-type B cells). Yet, the half-lives of Ets1 protein and mRNA were not significantly altered in Lyn−/− B cells. The most likely explanation for these observations is that Lyn promotes both the transcription of the Ets1 gene and also the translation of Ets1 mRNA into protein. Lyn may control translation of Ets1 mRNA by altering levels of microRNAs that bind to long and well-conserved 3′UTR of the major Ets1 mRNA species (73).
Lyn is a crucial mediator of inhibitory signaling pathways in B cells, but is redundant with other Src family kinases in mediating positive BCR signaling (6, 8, 9). Therefore, Lyn-deficient B cells have alterations in BCR signaling with some downstream proteins showing impaired phosphorylation, but with an overall increased Ca2+ flux and MAP kinase activation (6, 8, 9). Our data suggest that the downregulation of Ets1 in Lyn−/− B cells is due to enhanced BCR signaling in these cells. This is supported by the fact that crossing Lyn−/− mice to mice with low levels of Btk (Lyn−/−Btklo) largely restores Ets1 expression. In addition, fixing the specificity of the BCR on Lyn-deficient B cells to a foreign antigen (HEL) also partially restores Ets1 expression, although it does not reach the levels of Lyn+/+ B cells. Two different models can explain the fact that fixing the BCR fails to completely restore Ets1 expression in Lyn−/− B cells. First, it is possible that tonic low level and antigen-independent signaling via the BCR also controls Ets1 expression. Second, Ets1 may be downregulated in Lyn−/− mice not only because of enhanced BCR signaling, but also because of enhanced signaling via other pathways. TLR-mediated signaling pathways can also be negatively regulated by Lyn (74) and are potential contributors to the downregulation of Ets1 in the second model.
Downregulation of Ets1 in B cells is dependent on the BCR signaling components PI3 kinase, Btk, IKK2 and JNK. PI3 kinase generates PIP3 that recruits Btk to the membrane. Btk then triggers a pathway that eventually activates the IKK complex and JNK. Another effector of PI3K signaling, Akt, does not appear to contribute. This is shown by (1) the fact that Akt activation is normal in both Btk-deficient B cells and in wild-type B cells treated with a Btk-specific inhibitor, yet Ets1 downregulation is blocked, (2) that Pten−/− B cells, which have hyperactive Akt, do not show enhanced downregulation of Ets1 upon BCR crosslinking and (3) that transfection of constitutively-active Akt into A20 B lymphoma cells results in only a very modest downregulation of Ets1.
Downstream of Btk, both JNK and IKK2 appear to regulate Ets1 levels. Studies with an inhibitor that blocks IKK2 activity showed that IKK2 signaling is essential in down-regulating Ets1 in response to BCR ligation. However, activation of IKK2 alone (as found in IKK2* mice) was not sufficient to downregulate Ets1 in primary B cells, but rather cooperated with low levels of BCR ligation to inhibit Ets1 expression. In contrast, activation of IKK2 alone was sufficient to downregulate Ets1 in A20 and M12 B lymphoma cells. One or more signaling pathways that cooperate with IKK2 activation to downregulate Ets1 may have become activated in the B lymphoma cells during their oncogenic conversion. Similarly, JNK kinases also appear to be involved in regulation of Ets1 expression. Two separate inhibitors of JNK kinases that function by different mechanisms blocked the downregulation of Ets1 in stimulated primary B cells. Furthermore, expression of a constitutively-active form of JNK1 downregulated Ets1 in A20 B lymphoma cells, although a caveat to this result is that the A20 cells may have activated other pathways that cooperate with JNK to downregulate Ets1 as we determined for IKK2. The targets of the IKK2 and JNK pathways that regulate Ets1 expression remain to be defined.
A series of inhibitory signaling pathways counterbalance the BCR signaling pathway to limit B cell activation. Lyn-mediated phosphorylation of inhibitory membrane receptors results in the recruitment of phosphatases to these receptors, either SHP1 to CD22, CD72, Siglec-G, PIR-B and FcγRIIb or SHIP1 to FcγRIIb. SHP1 suppresses BCR signaling by dephosphorylating key substrates such as Igα, Igβ, Syk and Lyn (75, 76), whereas SHIP1 functions to convert PIP3 to PI(3,4)P2 thereby suppressing PI3 kinase-dependent signaling pathways. The absence of SHP1 or SHIP1 leads to autoimmune symptoms, presumably due in part to increased BCR signaling (12, 13, 17, 66). Ets1 is dramatically downregulated in B cells lacking SHP1, but only modestly downregulated in B cells lacking SHIP1. Restoration of Ets1 to SHP1-deficient B cells by retroviral transduction reversed their enhanced differentiation into plasma cells in response to LPS stimulation. This indicates the SHP1 is the primary Lyn-dependent phosphatase controlling Ets1 levels in B cells.
Mice lacking any one of the inhibitory receptors showed relatively weak (CD22 and Siglec-G single knockouts) or no (FcγRIIB, CD72 and PIR-B single knockouts) downregulation of Ets1. The strongest downregulation of Ets1 was obtained in mice doubly-deficient in both CD22 and Siglec-G, although the level of Ets1 in B cells from these mice is still higher than that found in B cells lacking Lyn or SHP1. This suggests that multiple inhibitory receptors on the B cell surface, including CD22 and Siglec-G, cooperate to maintain Ets1 expression under physiological conditions.
Disease-associated SNPs in the LYN and ETS1 gene loci have been identified in human autoimmune patients (77-81). Furthermore, both Lyn and Ets1 levels have been shown to be downregulated in PBMCs and B cells of autoimmune disease patients (10, 11, 82-84). These studies support the involvement of LYN and ETS1 in human autoimmune disease processes. We propose that in human B cells, like in mouse B cells, Lyn is an upstream regulator of Ets1 expression and that mutations in either gene can promote susceptibility to autoimmune disease. Thus, the Lyn-Ets1 axis could be a fruitful target for new therapeutics for autoimmune diseases.
Supplementary Material
Acknowledgements
We thank Dr. Toshiyuki Takai at Tohoku University for providing PIR-B knockout samples via an arrangement with Dr. Shu-hsia Chen at Mount Sinai Medical School. We thank Dr. Satrajit Sinha for helpful comments and Kirsten Smalley and Hansaa Abbasi for technical assistance. We thank Dr Kira Gritsman at Brigham and Women’s Hospital, Boston for myr-Akt plasmid.
2) Abbreviations Used
Footnotes
These studies were supported by research grants from the Alliance for Lupus Research, the National Institutes of Health (AI085127, AI099422, AI41649, AI039824, AI005284, AI56363 and GM076982) and the Deutsche Forschungsgemeinschaft (SFB643 and TRR130).
References
- 1.Packard TA, Cambier JC. B lymphocyte antigen receptor signaling: initiation, amplification, and regulation. 2013. p. 40. F1000prime reports 5. [DOI] [PMC free article] [PubMed]
- 2.Nitschke L. The role of CD22 and other inhibitory co-receptors in B-cell activation. Curr Opin Immunol. 2005;17:290–297. doi: 10.1016/j.coi.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 3.Poe JC, Tedder TF. CD22 and Siglec-G in B cell function and tolerance. Trends Immunol. 2012;33:413–420. doi: 10.1016/j.it.2012.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tsubata T. Role of inhibitory BCR co-receptors in immunity. Infectious disorders drug targets. 2012;12:181–190. doi: 10.2174/187152612800564455. [DOI] [PubMed] [Google Scholar]
- 5.Vang T, Miletic AV, Arimura Y, Tautz L, Rickert RC, Mustelin T. Protein tyrosine phosphatases in autoimmunity. Annu Rev Immunol. 2008;26:29–55. doi: 10.1146/annurev.immunol.26.021607.090418. [DOI] [PubMed] [Google Scholar]
- 6.Nishizumi H, Taniuchi I, Yamanashi Y, Kitamura D, Ilic D, Mori S, Watanabe T, Yamamoto T. Impaired proliferation of peripheral B cells and indication of autoimmune disease in lyn-deficient mice. Immunity. 1995;3:549–560. doi: 10.1016/1074-7613(95)90126-4. [DOI] [PubMed] [Google Scholar]
- 7.Hibbs ML, Tarlinton DM, Armes J, Grail D, Hodgson G, Maglitto R, Stacker SA, Dunn AR. Multiple defects in the immune system of Lyn-deficient mice, culminating in autoimmune disease. Cell. 1995;83:301–311. doi: 10.1016/0092-8674(95)90171-x. [DOI] [PubMed] [Google Scholar]
- 8.Chan VW, Meng F, Soriano P, DeFranco AL, Lowell CA. Characterization of the B lymphocyte populations in Lyn-deficient mice and the role of Lyn in signal initiation and down-regulation. Immunity. 1997;7:69–81. doi: 10.1016/s1074-7613(00)80511-7. [DOI] [PubMed] [Google Scholar]
- 9.Chan VW, Lowell CA, DeFranco AL. Defective negative regulation of antigen receptor signaling in Lyn-deficient B lymphocytes. Curr Biol. 1998;8:545–553. doi: 10.1016/s0960-9822(98)70223-4. [DOI] [PubMed] [Google Scholar]
- 10.Liossis SN, Solomou EE, Dimopoulos MA, Panayiotidis P, Mavrikakis MM, Sfikakis PP. B-cell kinase lyn deficiency in patients with systemic lupus erythematosus. J Investig Med. 2001;49:157–165. doi: 10.2310/6650.2001.34042. [DOI] [PubMed] [Google Scholar]
- 11.Flores-Borja F, Kabouridis PS, Jury EC, Isenberg DA, Mageed RA. Decreased Lyn expression and translocation to lipid raft signaling domains in B lymphocytes from patients with systemic lupus erythematosus. Arthritis Rheum. 2005;52:3955–3965. doi: 10.1002/art.21416. [DOI] [PubMed] [Google Scholar]
- 12.Tsui HW, Siminovitch KA, de Souza L, Tsui FW. Motheaten and viable motheaten mice have mutations in the haematopoietic cell phosphatase gene. Nat Genet. 1993;4:124–129. doi: 10.1038/ng0693-124. [DOI] [PubMed] [Google Scholar]
- 13.Pao LI, Lam KP, Henderson JM, Kutok JL, Alimzhanov M, Nitschke L, Thomas ML, Neel BG, Rajewsky K. B cell-specific deletion of protein-tyrosine phosphatase Shp1 promotes B-1a cell development and causes systemic autoimmunity. Immunity. 2007;27:35–48. doi: 10.1016/j.immuni.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 14.Nitschke L, Carsetti R, Ocker B, Kohler G, Lamers MC. CD22 is a negative regulator of B-cell receptor signalling. Curr Biol. 1997;7:133–143. doi: 10.1016/s0960-9822(06)00057-1. [DOI] [PubMed] [Google Scholar]
- 15.Pan C, Baumgarth N, Parnes JR. CD72-deficient mice reveal nonredundant roles of CD72 in B cell development and activation. Immunity. 1999;11:495–506. doi: 10.1016/s1074-7613(00)80124-7. [DOI] [PubMed] [Google Scholar]
- 16.Hoffmann A, Kerr S, Jellusova J, Zhang J, Weisel F, Wellmann U, Winkler TH, Kneitz B, Crocker PR, Nitschke L. Siglec-G is a B1 cell-inhibitory receptor that controls expansion and calcium signaling of the B1 cell population. Nat Immunol. 2007;8:695–704. doi: 10.1038/ni1480. [DOI] [PubMed] [Google Scholar]
- 17.Bolland S, Ravetch JV. Spontaneous autoimmune disease in Fc(gamma)RIIB-deficient mice results from strain-specific epistasis. Immunity. 2000;13:277–285. doi: 10.1016/s1074-7613(00)00027-3. [DOI] [PubMed] [Google Scholar]
- 18.Jellusova J, Wellmann U, Amann K, Winkler TH, Nitschke L. CD22 × Siglec-G double-deficient mice have massively increased B1 cell numbers and develop systemic autoimmunity. J Immunol. 2010;184:3618–3627. doi: 10.4049/jimmunol.0902711. [DOI] [PubMed] [Google Scholar]
- 19.Satterthwaite AB, Lowell CA, Khan WN, Sideras P, Alt FW, Witte ON. Independent and opposing roles for Btk and lyn in B and myeloid signaling pathways. J Exp Med. 1998;188:833–844. doi: 10.1084/jem.188.5.833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whyburn LR, Halcomb KE, Contreras CM, Lowell CA, Witte ON, Satterthwaite AB. Reduced dosage of Bruton’s tyrosine kinase uncouples B cell hyperresponsiveness from autoimmunity in lyn−/− mice. J Immunol. 2003;171:1850–1858. doi: 10.4049/jimmunol.171.4.1850. [DOI] [PubMed] [Google Scholar]
- 21.Gutierrez T, Halcomb KE, Coughran AJ, Li QZ, Satterthwaite AB. Separate checkpoints regulate splenic plasma cell accumulation and IgG autoantibody production in Lyn-deficient mice. Eur J Immunol. 2010;40:1897–1905. doi: 10.1002/eji.200940043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nutt SL, Taubenheim N, Hasbold J, Corcoran LM, Hodgkin PD. The genetic network controlling plasma cell differentiation. Semin Immunol. 2011;23:341–349. doi: 10.1016/j.smim.2011.08.010. [DOI] [PubMed] [Google Scholar]
- 23.Wang D, John SA, Clements JL, Percy DH, Barton KP, Garrett-Sinha LA. Ets-1 deficiency leads to altered B cell differentiation, hyperresponsiveness to TLR9 and autoimmune disease. Int Immunol. 2005;17:1179–1191. doi: 10.1093/intimm/dxh295. [DOI] [PubMed] [Google Scholar]
- 24.Seo S, Buckler J, Erikson J. Novel roles for Lyn in B cell migration and lipopolysaccharide responsiveness revealed using anti-double-stranded DNA Ig transgenic mice. J Immunol. 2001;166:3710–3716. doi: 10.4049/jimmunol.166.6.3710. [DOI] [PubMed] [Google Scholar]
- 25.Khan WN, Alt FW, Gerstein RM, Malynn BA, Larsson I, Rathbun G, Davidson L, Muller S, Kantor AB, Herzenberg LA, Rosen FS, Sideras P. Defective B cell development and function in Btk-deficient mice. Immunity. 1995;3:283–299. doi: 10.1016/1074-7613(95)90114-0. [DOI] [PubMed] [Google Scholar]
- 26.Satterthwaite AB, Cheroutre H, Khan WN, Sideras P, Witte ON. Btk dosage determines sensitivity to B cell antigen receptor cross-linking. Proc Natl Acad Sci U S A. 1997;94:13152–13157. doi: 10.1073/pnas.94.24.13152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Satterthwaite AB, Willis F, Kanchanastit P, Fruman D, Cantley LC, Helgason CD, Humphries RK, Lowell CA, Simon M, Leitges M, Tarakhovsky A, Tedder TF, Lesche R, Wu H, Witte ON. A sensitized genetic system for the analysis of murine B lymphocyte signal transduction pathways dependent on Bruton’s tyrosine kinase. Proc Natl Acad Sci U S A. 2000;97:6687–6692. doi: 10.1073/pnas.110146697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goodnow CC, Crosbie J, Adelstein S, Lavoie TB, Smith-Gill SJ, Brink RA, Pritchard-Briscoe H, Wotherspoon JS, Loblay RH, Raphael K, et al. Altered immunoglobulin expression and functional silencing of self-reactive B lymphocytes in transgenic mice. Nature. 1988;334:676–682. doi: 10.1038/334676a0. [DOI] [PubMed] [Google Scholar]
- 29.Rickert RC, Roes J, Rajewsky K. B lymphocyte-specific, Cre-mediated mutagenesis in mice. Nucleic Acids Res. 1997;25:1317–1318. doi: 10.1093/nar/25.6.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sasaki Y, Derudder E, Hobeika E, Pelanda R, Reth M, Rajewsky K, Schmidt-Supprian M. Canonical NF-kappaB activity, dispensable for B cell development, replaces BAFF-receptor signals and promotes B cell proliferation upon activation. Immunity. 2006;24:729–739. doi: 10.1016/j.immuni.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 31.Hao Z, Rajewsky K. Homeostasis of peripheral B cells in the absence of B cell influx from the bone marrow. J Exp Med. 2001;194:1151–1164. doi: 10.1084/jem.194.8.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Takai T, Ono M, Hikida M, Ohmori H, Ravetch JV. Augmented humoral and anaphylactic responses in Fc gamma RII-deficient mice. Nature. 1996;379:346–349. doi: 10.1038/379346a0. [DOI] [PubMed] [Google Scholar]
- 33.Anzelon AN, Wu H, Rickert RC. Pten inactivation alters peripheral B lymphocyte fate and reconstitutes CD19 function. Nat Immunol. 2003;4:287–294. doi: 10.1038/ni892. [DOI] [PubMed] [Google Scholar]
- 34.Karlsson MC, Guinamard R, Bolland S, Sankala M, Steinman RM, Ravetch JV. Macrophages control the retention and trafficking of B lymphocytes in the splenic marginal zone. J Exp Med. 2003;198:333–340. doi: 10.1084/jem.20030684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hobeika E, Thiemann S, Storch B, Jumaa H, Nielsen PJ, Pelanda R, Reth M. Testing gene function early in the B cell lineage in mb1-cre mice. Proc Natl Acad Sci U S A. 2006;103:13789–13794. doi: 10.1073/pnas.0605944103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Puel A, Cypowyj S, Bustamante J, Wright JF, Liu L, Lim HK, Migaud M, Israel L, Chrabieh M, Audry M, Gumbleton M, Toulon A, Bodemer C, El-Baghdadi J, Whitters M, Paradis T, Brooks J, Collins M, Wolfman NM, Al-Muhsen S, Galicchio M, Abel L, Picard C, Casanova JL. Chronic mucocutaneous candidiasis in humans with inborn errors of interleukin-17 immunity. Science. 2011;332:65–68. doi: 10.1126/science.1200439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sato S, Miller AS, Inaoki M, Bock CB, Jansen PJ, Tang ML, Tedder TF. CD22 is both a positive and negative regulator of B lymphocyte antigen receptor signal transduction: altered signaling in CD22-deficient mice. Immunity. 1996;5:551–562. doi: 10.1016/s1074-7613(00)80270-8. [DOI] [PubMed] [Google Scholar]
- 38.Ujike A, Takeda K, Nakamura A, Ebihara S, Akiyama K, Takai T. Impaired dendritic cell maturation and increased T(H)2 responses in PIR-B(−/−) mice. Nat Immunol. 2002;3:542–548. doi: 10.1038/ni801. [DOI] [PubMed] [Google Scholar]
- 39.Eyquem S, Chemin K, Fasseu M, Chopin M, Sigaux F, Cumano A, Bories JC. The development of early and mature B cells is impaired in mice deficient for the Ets-1 transcription factor. Eur J Immunol. 2004;34:3187–3196. doi: 10.1002/eji.200425352. [DOI] [PubMed] [Google Scholar]
- 40.Mercurio F, Zhu H, Murray BW, Shevchenko A, Bennett BL, Li J, Young DB, Barbosa M, Mann M, Manning A, Rao A. IKK-1 and IKK-2: cytokine-activated IkappaB kinases essential for NF-kappaB activation. Science. 1997;278:860–866. doi: 10.1126/science.278.5339.860. [DOI] [PubMed] [Google Scholar]
- 41.Lei K, Nimnual A, Zong WX, Kennedy NJ, Flavell RA, Thompson CB, Bar-Sagi D, Davis RJ. The Bax subfamily of Bcl2-related proteins is essential for apoptotic signal transduction by c-Jun NH(2)-terminal kinase. Mol Cell Biol. 2002;22:4929–4942. doi: 10.1128/MCB.22.13.4929-4942.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.John S, Russell L, Chin SS, Luo W, Oshima R, Garrett-Sinha LA. Transcription factor ets1, but not the closely related factor ets2, inhibits antibody-secreting cell differentiation. Mol Cell Biol. 2014;34:522–532. doi: 10.1128/MCB.00612-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.John SA, Clements JL, Russell LM, Garrett-Sinha LA. Ets-1 regulates plasma cell differentiation by interfering with the activity of the transcription factor Blimp-1. J Biol Chem. 2008;283:951–962. doi: 10.1074/jbc.M705262200. [DOI] [PubMed] [Google Scholar]
- 44.Yamanashi Y, Mori S, Yoshida M, Kishimoto T, Inoue K, Yamamoto T, Toyoshima K. Selective expression of a protein-tyrosine kinase, p56lyn, in hematopoietic cells and association with production of human T-cell lymphotropic virus type I. Proc Natl Acad Sci U S A. 1989;86:6538–6542. doi: 10.1073/pnas.86.17.6538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bhattacharya D, Cheah MT, Franco CB, Hosen N, Pin CL, Sha WC, Weissman IL. Transcriptional profiling of antigen-dependent murine B cell differentiation and memory formation. J Immunol. 2007;179:6808–6819. doi: 10.4049/jimmunol.179.10.6808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Barton K, Muthusamy N, Fischer C, Ting CN, Walunas TL, Lanier LL, Leiden JM. The Ets-1 transcription factor is required for the development of natural killer cells in mice. Immunity. 1998;9:555–563. doi: 10.1016/s1074-7613(00)80638-x. [DOI] [PubMed] [Google Scholar]
- 47.Bhat NK, Komschlies KL, Fujiwara S, Fisher RJ, Mathieson BJ, Gregorio TA, Young HA, Kasik JW, Ozato K, Papas TS. Expression of ets genes in mouse thymocyte subsets and T cells. J Immunol. 1989;142:672–678. [PubMed] [Google Scholar]
- 48.Sotirellis N, Johnson TM, Hibbs ML, Stanley IJ, Stanley E, Dunn AR, Cheng HC. Autophosphorylation induces autoactivation and a decrease in the Src homology 2 domain accessibility of the Lyn protein kinase. J Biol Chem. 1995;270:29773–29780. doi: 10.1074/jbc.270.50.29773. [DOI] [PubMed] [Google Scholar]
- 49.McPherson VA, Sharma N, Everingham S, Smith J, Zhu HH, Feng GS, Craig AW. SH2 domain-containing phosphatase-2 protein-tyrosine phosphatase promotes Fc epsilon RI-induced activation of Fyn and Erk pathways leading to TNF alpha release from bone marrow-derived mast cells. J Immunol. 2009;183:4940–4947. doi: 10.4049/jimmunol.0900702. [DOI] [PubMed] [Google Scholar]
- 50.ten Hacken E, Scielzo C, Bertilaccio MT, Scarfo L, Apollonio B, Barbaglio F, Stamatopoulos K, Ponzoni M, Ghia P, Caligaris-Cappio F. Targeting the LYN/HS1 signaling axis in chronic lymphocytic leukemia. Blood. 2013;121:2264–2273. doi: 10.1182/blood-2012-09-457119. [DOI] [PubMed] [Google Scholar]
- 51.Alvarez-Errico D, Yamashita Y, Suzuki R, Odom S, Furumoto Y, Yamashita T, Rivera J. Functional analysis of Lyn kinase A and B isoforms reveals redundant and distinct roles in Fc epsilon RI-dependent mast cell activation. J Immunol. 2010;184:5000–5008. doi: 10.4049/jimmunol.0904064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Silver KL, Crockford TL, Bouriez-Jones T, Milling S, Lambe T, Cornall RJ. MyD88-dependent autoimmune disease in Lyn-deficient mice. Eur J Immunol. 2007;37:2734–2743. doi: 10.1002/eji.200737293. [DOI] [PubMed] [Google Scholar]
- 53.Tsantikos E, Oracki SA, Quilici C, Anderson GP, Tarlinton DM, Hibbs ML. Autoimmune disease in Lyn-deficient mice is dependent on an inflammatory environment established by IL-6. J Immunol. 2010;184:1348–1360. doi: 10.4049/jimmunol.0901878. [DOI] [PubMed] [Google Scholar]
- 54.Hauser J, Verma-Gaur J, Wallenius A, Grundstrom T. Initiation of antigen receptor-dependent differentiation into plasma cells by calmodulin inhibition of E2A. J Immunol. 2009;183:1179–1187. doi: 10.4049/jimmunol.0900455. [DOI] [PubMed] [Google Scholar]
- 55.Raghunandan R, Frissora FW, Muthusamy N. Modulation of Ets-1 expression in B lymphocytes is dependent on the antigen receptor-mediated activation signals and cell cycle status. Scand J Immunol. 2013;77:75–83. doi: 10.1111/sji.12012. [DOI] [PubMed] [Google Scholar]
- 56.Bolland S, Pearse RN, Kurosaki T, Ravetch JV. SHIP modulates immune receptor responses by regulating membrane association of Btk. Immunity. 1998;8:509–516. doi: 10.1016/s1074-7613(00)80555-5. [DOI] [PubMed] [Google Scholar]
- 57.Maeda A, Scharenberg AM, Tsukada S, Bolen JB, Kinet JP, Kurosaki T. Paired immunoglobulin-like receptor B (PIR-B) inhibits BCR-induced activation of Syk and Btk by SHP-1. Oncogene. 1999;18:2291–2297. doi: 10.1038/sj.onc.1202552. [DOI] [PubMed] [Google Scholar]
- 58.Li Z, Wahl MI, Eguinoa A, Stephens LR, Hawkins PT, Witte ON. Phosphatidylinositol 3-kinase-gamma activates Bruton’s tyrosine kinase in concert with Src family kinases. Proc Natl Acad Sci U S A. 1997;94:13820–13825. doi: 10.1073/pnas.94.25.13820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Saito K, Scharenberg AM, Kinet JP. Interaction between the Btk PH domain and phosphatidylinositol-3,4,5-trisphosphate directly regulates Btk. J Biol Chem. 2001;276:16201–16206. doi: 10.1074/jbc.M100873200. [DOI] [PubMed] [Google Scholar]
- 60.Petro JB, Rahman SM, Ballard DW, Khan WN. Bruton’s tyrosine kinase is required for activation of IkappaB kinase and nuclear factor kappaB in response to B cell receptor engagement. J Exp Med. 2000;191:1745–1754. doi: 10.1084/jem.191.10.1745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bajpai UD, Zhang K, Teutsch M, Sen R, Wortis HH. Bruton’s tyrosine kinase links the B cell receptor to nuclear factor kappaB activation. J Exp Med. 2000;191:1735–1744. doi: 10.1084/jem.191.10.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Inabe K, Miyawaki T, Longnecker R, Matsukura H, Tsukada S, Kurosaki T. Bruton’s tyrosine kinase regulates B cell antigen receptor-mediated JNK1 response through Rac1 and phospholipase C-gamma2 activation. FEBS Lett. 2002;514:260–262. doi: 10.1016/s0014-5793(02)02375-x. [DOI] [PubMed] [Google Scholar]
- 63.Forssell J, Nilsson A, Sideras P. Reduced formation of phosphatidic acid upon B-cell receptor triggering of mouse B-lymphocytes lacking Bruton’s tyrosine kinase. Scand J Immunol. 2000;52:30–38. doi: 10.1046/j.1365-3083.2000.00747.x. [DOI] [PubMed] [Google Scholar]
- 64.Jiang A, Craxton A, Kurosaki T, Clark EA. Different protein tyrosine kinases are required for B cell antigen receptor-mediated activation of extracellular signal-regulated kinase, c-Jun NH2-terminal kinase 1, and p38 mitogen-activated protein kinase. J Exp Med. 1998;188:1297–1306. doi: 10.1084/jem.188.7.1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Halcomb KE, Contreras CM, Hinman RM, Coursey TG, Wright HL, Satterthwaite AB. Btk and phospholipase C gamma 2 can function independently during B cell development. Eur J Immunol. 2007;37:1033–1042. doi: 10.1002/eji.200636451. [DOI] [PubMed] [Google Scholar]
- 66.O’Neill SK, Getahun A, Gauld SB, Merrell KT, Tamir I, Smith MJ, Porto J. M. Dal, Li QZ, Cambier JC. Monophosphorylation of CD79a and CD79b ITAM motifs initiates a SHIP-1 phosphatase-mediated inhibitory signaling cascade required for B cell anergy. Immunity. 2011;35:746–756. doi: 10.1016/j.immuni.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Xu M, Hou R, Sato-Hayashizaki A, Man R, Zhu C, Wakabayashi C, Hirose S, Adachi T, Tsubata T. Cd72(c) is a modifier gene that regulates Fas(lpr)-induced autoimmune disease. J Immunol. 2013;190:5436–5445. doi: 10.4049/jimmunol.1203576. [DOI] [PubMed] [Google Scholar]
- 68.Shultz LD, Coman DR, Bailey CL, Beamer WG, Sidman CL. “Viable motheaten,” a new allele at the motheaten locus. I. Pathology. Am J Pathol. 1984;116:179–192. [PMC free article] [PubMed] [Google Scholar]
- 69.Kersseboom R, Kil L, Flierman R, van der Zee M, Dingjan GM, Middendorp S, Maas A, Hendriks RW. Constitutive activation of Bruton’s tyrosine kinase induces the formation of autoreactive IgM plasma cells. Eur J Immunol. 2010;40:2643–2654. doi: 10.1002/eji.201040521. [DOI] [PubMed] [Google Scholar]
- 70.Hug E, Hobeika E, Reth M, Jumaa H. Inducible expression of hyperactive Syk in B cells activates Blimp-1-dependent terminal differentiation. Oncogene. 2013 doi: 10.1038/onc.2013.326. In press. [DOI] [PubMed] [Google Scholar]
- 71.Lamagna C, Hu Y, Defranco AL, Lowell CA. B cell-specific loss of lyn kinase leads to autoimmunity. J Immunol. 2014;192:919–928. doi: 10.4049/jimmunol.1301979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Leadbetter EA, Rifkin IR, Hohlbaum AM, Beaudette BC, Shlomchik MJ, Marshak-Rothstein A. Chromatin-IgG complexes activate B cells by dual engagement of IgM and Toll-like receptors. Nature. 2002;416:603–607. doi: 10.1038/416603a. [DOI] [PubMed] [Google Scholar]
- 73.Garrett-Sinha LA. Review of Ets1 structure, function, and roles in immunity. Cell Mol Life Sci. 2013;70:3375–3390. doi: 10.1007/s00018-012-1243-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Keck S, Freudenberg M, Huber M. Activation of murine macrophages via TLR2 and TLR4 is negatively regulated by a Lyn/PI3K module and promoted by SHIP1. J Immunol. 2010;184:5809–5818. doi: 10.4049/jimmunol.0901423. [DOI] [PubMed] [Google Scholar]
- 75.Dustin LB, Plas DR, Wong J, Hu YT, Soto C, Chan AC, Thomas ML. Expression of dominant-negative src-homology domain 2-containing protein tyrosine phosphatase-1 results in increased Syk tyrosine kinase activity and B cell activation. J Immunol. 1999;162:2717–2724. [PubMed] [Google Scholar]
- 76.Somani AK, Yuen K, Xu F, Zhang J, Branch DR, Siminovitch KA. The SH2 domain containing tyrosine phosphatase-1 down-regulates activation of Lyn and Lyn-induced tyrosine phosphorylation of the CD19 receptor in B cells. J Biol Chem. 2001;276:1938–1944. doi: 10.1074/jbc.M006820200. [DOI] [PubMed] [Google Scholar]
- 77.Lu R, Vidal GS, Kelly JA, Delgado-Vega AM, Howard XK, Macwana SR, Dominguez N, Klein W, Burrell C, Harley IT, Kaufman KM, Bruner GR, Moser KL, Gaffney PM, Gilkeson GS, Wakeland EK, Li QZ, Langefeld CD, Marion MC, Divers J, Alarcon GS, Brown EE, Kimberly RP, Edberg JC, Ramsey-Goldman R, Reveille JD, McGwin G, Jr., Vila LM, Petri MA, Bae SC, Cho SK, Bang SY, Kim I, Choi CB, Martin J, Vyse TJ, Merrill JT, Harley JB, Alarcon-Riquelme ME, Nath SK, James JA, Guthridge JM. Genetic associations of LYN with systemic lupus erythematosus. Genes Immun. 2009;10:397–403. doi: 10.1038/gene.2009.19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Harley JB, Alarcon-Riquelme ME, Criswell LA, Jacob CO, Kimberly RP, Moser KL, Tsao BP, Vyse TJ, Langefeld CD, Nath SK, Guthridge JM, Cobb BL, Mirel DB, Marion MC, Williams AH, Divers J, Wang W, Frank SG, Namjou B, Gabriel SB, Lee AT, Gregersen PK, Behrens TW, Taylor KE, Fernando M, Zidovetzki R, Gaffney PM, Edberg JC, Rioux JD, Ojwang JO, James JA, Merrill JT, Gilkeson GS, Seldin MF, Yin H, Baechler EC, Li QZ, Wakeland EK, Bruner GR, Kaufman KM, Kelly JA. Genome-wide association scan in women with systemic lupus erythematosus identifies susceptibility variants in ITGAM, PXK, KIAA1542 and other loci. Nat Genet. 2008;40:204–210. doi: 10.1038/ng.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Han JW, Zheng HF, Cui Y, Sun LD, Ye DQ, Hu Z, Xu JH, Cai ZM, Huang W, Zhao GP, Xie HF, Fang H, Lu QJ, Li XP, Pan YF, Deng DQ, Zeng FQ, Ye ZZ, Zhang XY, Wang QW, Hao F, Ma L, Zuo XB, Zhou FS, Du WH, Cheng YL, Yang JQ, Shen SK, Li J, Sheng YJ, Zuo XX, Zhu WF, Gao F, Zhang PL, Guo Q, Li B, Gao M, Xiao FL, Quan C, Zhang C, Zhang Z, Zhu KJ, Li Y, Hu DY, Lu WS, Huang JL, Liu SX, Li H, Ren YQ, Wang ZX, Yang CJ, Wang PG, Zhou WM, Lv YM, Zhang AP, Zhang SQ, Lin D, Low HQ, Shen M, Zhai ZF, Wang Y, Zhang FY, Yang S, Liu JJ, Zhang XJ. Genome-wide association study in a Chinese Han population identifies nine new susceptibility loci for systemic lupus erythematosus. Nat Genet. 2009;41:1234–1237. doi: 10.1038/ng.472. [DOI] [PubMed] [Google Scholar]
- 80.Okada Y, Terao C, Ikari K, Kochi Y, Ohmura K, Suzuki A, Kawaguchi T, Stahl EA, Kurreeman FA, Nishida N, Ohmiya H, Myouzen K, Takahashi M, Sawada T, Nishioka Y, Yukioka M, Matsubara T, Wakitani S, Teshima R, Tohma S, Takasugi K, Shimada K, Murasawa A, Honjo S, Matsuo K, Tanaka H, Tajima K, Suzuki T, Iwamoto T, Kawamura Y, Tanii H, Okazaki Y, Sasaki T, Gregersen PK, Padyukov L, Worthington J, Siminovitch KA, Lathrop M, Taniguchi A, Takahashi A, Tokunaga K, Kubo M, Nakamura Y, Kamatani N, Mimori T, Plenge RM, Yamanaka H, Momohara S, Yamada R, Matsuda F, Yamamoto K. Meta-analysis identifies nine new loci associated with rheumatoid arthritis in the Japanese population. Nat Genet. 2012;44:511–516. doi: 10.1038/ng.2231. [DOI] [PubMed] [Google Scholar]
- 81.Tsoi LC, Spain SL, Knight J, Ellinghaus E, Stuart PE, Capon F, Ding J, Li Y, Tejasvi T, Gudjonsson JE, Kang HM, Allen MH, McManus R, Novelli G, Samuelsson L, Schalkwijk J, Stahle M, Burden AD, Smith CH, Cork MJ, Estivill X, Bowcock AM, Krueger GG, Weger W, Worthington J, Tazi-Ahnini R, Nestle FO, Hayday A, Hoffmann P, Winkelmann J, Wijmenga C, Langford C, Edkins S, Andrews R, Blackburn H, Strange A, Band G, Pearson RD, Vukcevic D, Spencer CC, Deloukas P, Mrowietz U, Schreiber S, Weidinger S, Koks S, Kingo K, Esko T, Metspalu A, Lim HW, Voorhees JJ, Weichenthal M, Wichmann HE, Chandran V, Rosen CF, Rahman P, Gladman DD, Griffiths CE, Reis A, Kere J, Nair RP, Franke A, Barker JN, Abecasis GR, Elder JT, Trembath RC. Identification of 15 new psoriasis susceptibility loci highlights the role of innate immunity. Nat Genet. 2012;44:1341–1348. doi: 10.1038/ng.2467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Li Y, Sun LD, Lu WS, Hu WL, Gao JP, Cheng YL, Yu ZY, Yao S, He CF, Liu JL, Cui Y, Yang S. Expression analysis of ETS1 gene in peripheral blood mononuclear cells with systemic lupus erythematosus by real-time reverse transcription PCR. Chin Med J (Engl) 2010;123:2287–2288. [PubMed] [Google Scholar]
- 83.Du C, Liu C, Kang J, Zhao G, Ye Z, Huang S, Li Z, Wu Z, Pei G. MicroRNA miR-326 regulates T(H)-17 differentiation and is associated with the pathogenesis of multiple sclerosis. Nat Immunol. 2009;10:1252–1259. doi: 10.1038/ni.1798. [DOI] [PubMed] [Google Scholar]
- 84.Xiang N, Li XP, Li XM, Wang GS, Tao JH, Pan HF, Fang X, Ma Q, Yu N. Expression of Ets-1 and FOXP3 mRNA in CD4CD25 T regulatory cells from patients with systemic lupus erythematosus. Clinical and experimental medicine. 2013 doi: 10.1007/s10238-013-0263-4. In press. [DOI] [PubMed] [Google Scholar]
- 85.Franch HA, Sooparb S, Du J, Brown NS. A mechanism regulating proteolysis of specific proteins during renal tubular cell growth. J Biol Chem. 2001;276:19126–19131. doi: 10.1074/jbc.M101777200. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.