Abstract
Skin lesions in atopic dermatitis (AD) are characterized by hypertrophy of the dermis and epidermis, infiltration by T cells and eosinophils, and expression of the cytokines IL-4, IL-5, and IFN-γ. The role of these cytokines in the pathogenesis of AD is not known. We took advantage of a recently described murine model of AD elicited by epicutaneous sensitization with ovalbumin (OVA) (1) and of the availability of mice with targeted deletions of the IL-4, IL-5, and IFN-γ cytokine genes to assess the role of these cytokines in this model.OVA-sensitized skin from IL-5–/– mice had no detectable eosinophils and exhibited decreased epidermal and dermal thickening. Sensitized skin from IL-4–/– mice displayed normal thickening of the skin layers but had a drastic reduction in eosinophils and a significant increase in infiltrating T cells. These findings were associated with a reduction in eotaxin mRNA and an increase in mRNA for the T-cell chemokines macrophage inflammatory protein-2 (MIP-2), MIP-1β, and RANTES. Sensitized skin from IFN-γ–/– mice was characterized by reduced dermal thickening.These results suggest that both the TH2 cytokines IL-4 and IL-5 and the TH1 cytokine IFN-γ play important roles in the inflammation and hypertrophy of the skin in AD.
Introduction
Atopic dermatitis (AD) is a chronically relapsing inflammatory disease of the skin. T cells and eosinophils are thought to play a major role in the pathogenesis of the disease (1). Affected skin lesions in AD reveal a mononuclear cell infiltrate, predominantly in the dermis, consisting of macrophages and activated memory CD4+ T cells bearing HLA-DR+ and CD45RO+ (2). The presence of eosinophil-derived major basic protein and eosinophil cationic protein in the dermis, along with eosinophil degeneration, are indicative of eosinophil involvement in AD (3, 4).
In acute lesions of AD, there is a significant increase in the number of cells expressing IL-4, IL-5, and IL-13 mRNA and protein, suggesting preferential accumulation of TH2 cells. Additionally, PBMCs show increased IL-4 and IL-5 expression in CD4+ and CD8+ cells in patients with AD (5, 6). Recent studies have revealed that expression of the TH1 cytokine IFN-γ is predominant in the chronic eczematous AD skin lesions (7, 8). Furthermore, biopsies of skin lesions elicited by patch testing of AD patients with dust-mite antigens reveal that a majority of T cells in the lesions express IFN-γ mRNA and protein, alone or in combination with IL-4 (7, 9–11). These results indicate that both TH1 and TH2 cytokines may contribute to the lesions in AD (12).
The TH1 cytokines (IL-2 and IFN-γ) play an important role in cell-mediated immunity and chronic inflammation. IL-2 is important for T-cell growth and activation. IFN-γ induces expression of MHC class I and II molecules, activates monocytes and macrophages, and favors the development of TH1 cells (13). The TH2 cytokines have a critical role in the initiation of the allergic response. IL-4 is important for IgE isotype switching, development of TH2 cells, and induction of adhesion molecules on endothelial cells that recruit eosinophils (1, 14). IL-5 is important for eosinophil development and differentiation (15). Additional evidence for the role of TH2 cytokines in allergic diseases comes from the study of mice with targeted gene deletions. For example, murine models of asthma show decreased tissue and bronchoalveolar lavage eosinophilia in both IL-4–/– and IL-5–/– mice, as well as decreased hyperresponsiveness to methacholine following allergen exposure (16–20).
Recently, we described a murine model of AD elicited by repeated epicutaneous sensitization with ovalbumin (OVA). This model operates in both BALB/c and C57BL/6 mouse strains (21). The skin lesions exhibit significant dermal and epidermal thickening, a cellular infiltrate consisting of T cells and eosinophils, and elevated levels of IL-4, IL-5, and IFN-γ mRNA. We have taken advantage of our model and the availability of mice with a targeted deletion of cytokine genes to explore the role of IL-4, IL-5, and IFN-γ in the pathogenesis of AD. The results obtained suggest that all three cytokines contribute to the lesions in AD. IL-4 and IL-5 are important for eosinophil infiltration, and IL-5 and IFN-γ are important for skin hypertrophy. In addition, IL-4 may play an anti-inflammatory role in AD by virtue of its ability to modulate the expression of T-cell chemokines and its subsequent recruitment of T cells in the skin lesion.
Methods
Mice sensitization.
IL-4–/– and IFN-γ–/– mice on BALB/c background were obtained from The Jackson Laboratory (Bar Harbor, Maine, USA), and IL-5–/– mice on a C57BL/6 background were donated by M. Kopf (Freiburg, Germany). IgE–/– mice were generated as described previously (22). Wild-type (WT) BALB/c, C57BL/6, and 129Sv mice were purchased from Taconic Farms (Germantown, New York, USA). All mice were kept in a pathogen-free environment. All procedures performed on the mice were in accordance with the Animal Care and Use Committee of the Children’s Hospital.
Epicutaneous sensitization of four- to six-week-old female mice was performed as described previously (21). Briefly, mice were anesthetized with methoxyflurane (Metofane; Schering-Plough Animal Health Corp., Union,New Jersey, USA) and then shaved with an electric razor. One hundred micrograms of OVA (Grade V; Sigma Chemical Co., St. Louis, Missouri, USA) in 100 μl of normal saline or placebo (100 μl of normal saline) was placed on a patch of sterile gauze (1 × 1 cm), which was secured to the skin with a transparent bioocclusive dressing (Johnson & Johnson Medical Inc., Arlington, Texas, USA). The patches were placed for a one-week period and then removed. Two weeks later, an identical patch was reapplied to the same skin site. Each mouse had a total of three one-week exposures to the patch separated from each other by two-week intervals.
Antibodies.
Rat and hamster mAb’s were used for immunohistochemical analysis and were directed against mouse CD3ε (145-2C11), CD4 (H129.19), CD8α (53-6.7), CD45 (30F11.1), and CD106-VCAM (429/MVCAM.A). The mAb’s used in OVA-specific ELISA were biotin-conjugated rat anti-mouse IgG2a clone R19-15 and IgE clone R35-92, rat anti-mouse IgE mAb clone R35-72, rat anti-mouse IgG2a mAb clone R11-89, and mouse IgG2a mAb 5.7. All antibodies were purchased from PharMingen (San Diego, California, USA).
ELISA.
Mice were bled and sera were collected one day after the end of the series of three epicutaneous sensitizations. The standard PharMingen protocol for sandwich ELISA was used to quantify the total amount of IgE and IgG2a in serum. For IgE measurements, rat anti-mouse IgE mAb clone R35-72 was used for coating the plates, and rat anti-mouse IgE mAb clone R35-92 was used for detection. For IgG2a measurements in sera of BALB/c and C57BL6 mice, coating antibodies were rat R12-14 mAb and mouse 5.7 mAb, respectively, and detection antibodies were rat R19-15 mAb and mouse 5.7 mAb, respectively. IgG2a and IgE OVA-specific antibodies were measured as described previously using the mAb’s listed above (21).
Histological analysis.
For histological examination, specimens were obtained from patched areas on the skin 24 h after the patch from the third sensitization was removed. Specimens were fixed in 10% buffered formalin and embedded in paraffin. Multiple 4-μm sections were stained with hematoxylin and eosin (H&E) or Giemsa. Individual inflammatory cell types were counted in 10–20 high-power fields (HPFs) at ×1,000 and expressed as cells per HPF, with mean and SEM calculated.
Immunohistological analysis.
Skin sections were embedded in Tissue-Tek oxacalcitriol (OCT) compound (Miles Inc., Elkhart, Indiana, USA) on dry ice. Sections of 4 μm were prepared and stored at –80°C. Sections were stained by an avidin-biotin method as described previously (21, 23). Stained cells were counted in 10–20 HPFs at ×400.
Serum IL-5 levels.
IL-5 levels were determined in serum using a commercial sandwich ELISA assay from Amersham Pharmacia Biotech (Buckinghamshire, England). The sensitivity for the assay was 5 pg/ml.
Analysis of eosinophils in peripheral blood.
Blood was collected 24 h after the third sensitization. The absolute eosinophil count was determined by counting heparinized blood on a hemocytometer after staining with Discombe’s fluid (24).
RNA preparation.
Skin biopsies were obtained 24 h after the third patch was removed and immediately frozen in dry ice. To extract the RNA, the samples were homogenized in Trizol (GIBCO BRL, Grand Island, New York, USA) using a Polytron RT-3000 (Kinematica AG, Littau, Switzerland). RNA quantity was determined by measuring OD at 260 nm.
cDNA synthesis and PCR amplification of reverse-transcribed cDNA.
cDNA was synthesized from 10 μg of total RNA in a 50-μl reaction mix using Superscript II (GIBCO BRL) for 90 min at 37°C. The primers used to amplify cDNA for β2-microglobulin, IL-2, IL-4, IL-5, IFN-γ, and DNA amplification were as described previously (21). To quantify mRNA, a fixed amount of reverse-transcribed cellular mRNA was coamplified in the presence of serial dilutions of a multispecific internal plasmid control (pMUS) that contains nucleotide sequences from multiple cytokines (25). The results were expressed as a ratio of cytokine cDNA to cDNA of the constitutively expressed β2-microglobulin gene.
RNase protection assay.
Multiprobe template mCK-5 containing DNA templates for the chemokines LTN, RANTES, eotaxin, macrophage inflammatory protein-1α (MIP-1α), MIP-2, MIP-1β, IFN-γ–inducible protein-10 (IP-10), monocyte chemoattractant protein-1 (MCP-1), and TCA-3, and for the housekeeping genes L32 (ribosomal RNA) and GAPDH (all from PharMingen). The assay was performed according to the manufacturer’s protocol. Briefly, the DNA templates were used to synthesize probes, labeled with α-[32P]UTP (3,000 Ci/mmol, 10 μCi/μl; Du Pont NEN Research Products, Boston, Massachusetts, USA), in the presence of a GACU pool using a T7 polymerase according to manufacturer’s protocol. The probe was hybridized overnight with 10 μg of total RNA, followed by digestion with RNase A and T1. The samples were then treated with proteinase K-SDS mixture, extracted with phenol-chloroform (Roche Molecular Biochemicals, Indianapolis, Indiana, USA), and precipitated in the presence of ammonium acetate. The samples were loaded on an acrylamide-urea sequencing gel next to undigested label probes and run at 50 W with 0.5× Tris-borate/EDTA electrophoresis buffer (TBE). The gel was dried on filter paper under vacuum, exposed to XAR film (Eastman Kodak Co., Rochester, New York, USA) with intensifying screens, and developed at –70°C. For quantification, gels were scanned with a QuantiScan densitometer, and analysis of integration peaks was done with ImageQuant software. Each band was normalized to L32 and GAPDH and expressed as a percentage of GAPDH + L32. We analyzed duplicate skin biopsies from 10 mice in each group.
Results
Eosinophils are virtually absent in OVA-sensitized skin sites of IL-5–/– mice.
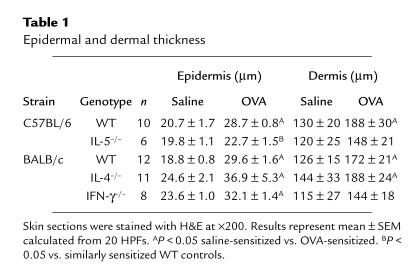
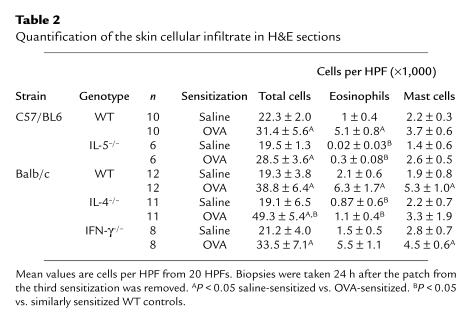
We have shown previously that epicutaneous sensitization with OVA induced significant thickening of dermis, epidermis, and a cellular infiltrate in the dermis (Table 1) that contained T cells, eosinophils, and mast cells (Tables 2 and 3). Importantly, equivalent skin lesions were elicited in C57BL/6 mice, a strain with a propensity for TH1 responses, as in BALB/c mice, a strain with a propensity for TH2 responses (Ref. 21; Figure 1, Tables 1 and 2).
Table 1.
Epidermal and dermal thickness
Table 2.
Quantification of the skin cellular infiltrate in H&E sections
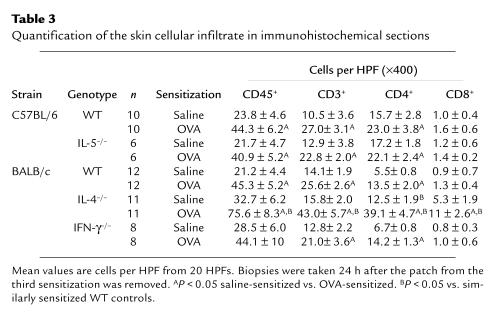
Table 3.
Quantification of the skin cellular infiltrate in immunohistochemical sections
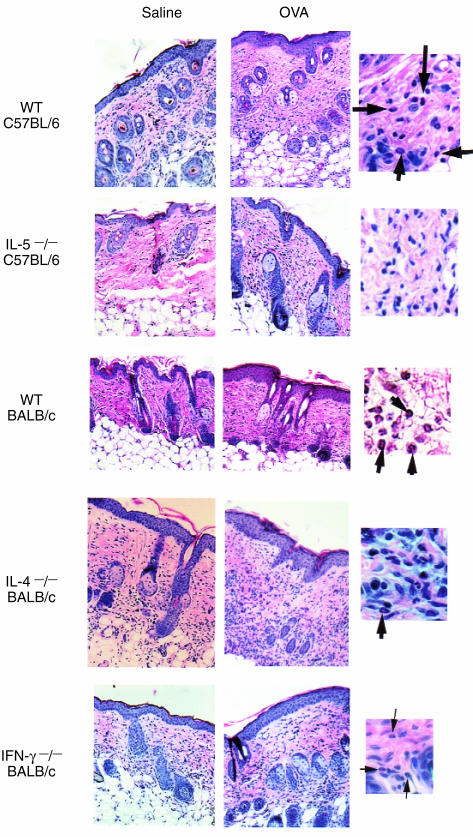
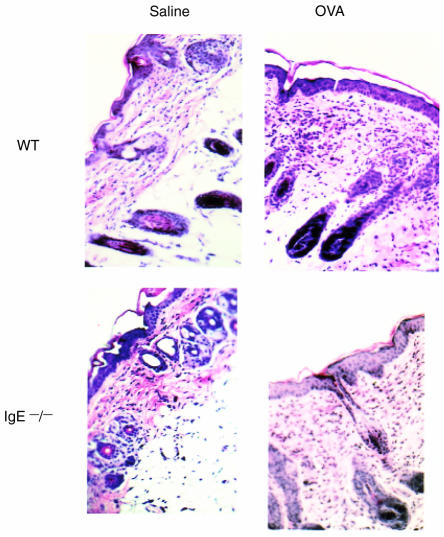
Figure 1.
Histological features of OVA-sensitized and saline-sensitized skin sites. Skin sections were stained with H&E. Magnification for large panels: ×200 ; small panels: ×800. Arrowheads point to eosinophils. The epidermal layer of IL-5 –/– mice does not contain as many cell layers as its WT control, and there is less thickening of the dermal layer. IL-4–/– mice have an increased cellular infiltrate and decreased eosinophils compared with WT mice. The IFN-γ–/– mice have decreased thickness of dermal layer.
Table 1 shows that in contrast to WT mice of the same C57BL/6 genetic background, IL-5–/– mice had no significant increase in the thickness of the epidermal or dermal layers following OVA sensitization. However, the number per HPF of infiltrating cells — including CD45+, CD3+, CD4+, and CD8+ cells — in sensitized skin of IL-5–/– mice was equivalent to that in similarly sensitized WT controls (Figure 1, Tables 2 and 3). IL-5–/– mice had virtually no eosinophils in either saline-sensitized skin or in OVA-sensitized skin (Table 2). There were no significant differences in the expression of chemokines in OVA-sensitized skin sites between IL-5–/– mice and WT controls (data not shown).
OVA-sensitized skin sites of IL-4 –/– mice have increased inflammatory cells but decreased eosinophils.
The thickness of epidermis and dermis was equivalent in the OVA-sensitized skin sites of IL-4–/– mice and WT mice (Table 1). Saline-sensitized skin sites from IL-4–/– mice had a higher total number of cells per HPF in the dermis compared with WT controls but had significantly reduced numbers of eosinophils (Table 2). More importantly, OVA-sensitized skin from IL-4–/– mice had significantly more infiltrating cells but significantly less eosinophils in the dermis than OVA-sensitized skin from WT controls (Figure 1, Tables 2 and 3). The number of eosinophils in OVA-sensitized skin was no different than that in saline-treated skin of IL-4–/– mice. This is in contrast to WT mice, where eosinophils increased by threefold in OVA-sensitized skin sites (Table 2). Also in contrast to WT mice, the numbers of dermal mast cells in IL-4–/– mice did not show a significant increase following OVA sensitization.
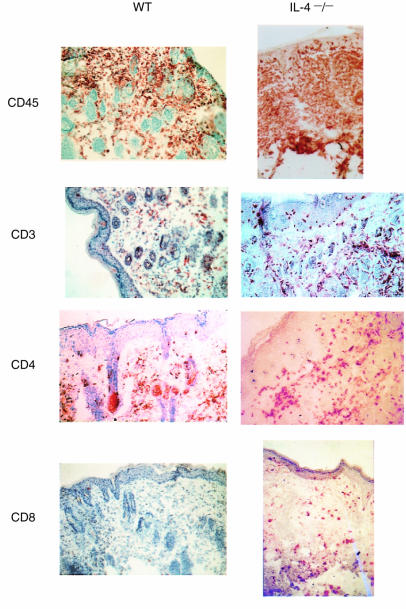
Detailed immunohistochemical analysis revealed that saline-sensitized skin sites of IL-4–/– mice had increased numbers of CD45+, CD4+, and CD8+ cells compared with WT controls, with only the increase in CD4+ cells reaching a significant level (Table 3). Following OVA sensitization, there was a significant increase (P < 0.05) in CD45+, CD3+, CD4+, and CD8+ cells in both IL-4–/– mice and WT controls. More importantly, OVA-sensitized skin sites in IL-4–/– mice had significantly increased numbers of cells bearing CD45, CD3, CD4, and CD8, compared with OVA-sensitized skin sites in WT controls (Figure 2 and Table 3). These results suggest that T-cell infiltration into OVA-sensitized skin is increased in the absence of IL-4.
Figure 2.
Immunohistochemical staining of OVA-sensitized skin sites in WT BALB/c and IL-4–/– mice. IL-4–/– mice show an increase in the number of CD45+, CD3+, CD4+, and CD8+ cells. Magnification: ×200. Positive cells stain brown.
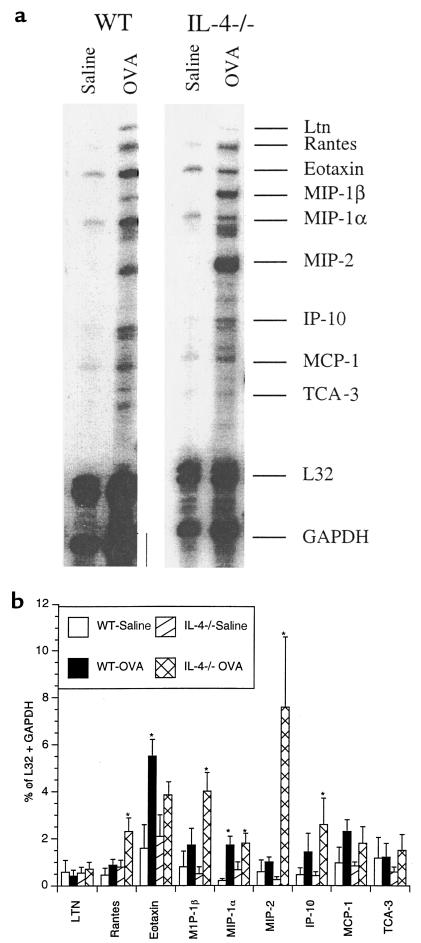
Chemokines are 8- to 10-kDa proteins that are key components of the leukocyte recruitment process. Chemokines and their receptors have specific tissue and cellular distribution leading to a selective inflammatory process in response to different stimuli (26). For example, eotaxin, MCP-3, and MCP-4 are chemoattractants for eosinophils and TH2 cells, while MIP-1β, MIP-2, RANTES, and IP-10 are chemoattractants for TH1 cells (27–31). To explore the cause of the increased numbers of infiltrating T cells and the decreased numbers of eosinophils in OVA-sensitized skin of IL-4–/– mice, we examined chemokine expression in sensitized skin sites. For this purpose, we performed an RNase protection assay that detects mRNA for nine chemokines: LTN, RANTES, eotaxin, MIP-1α, MIP-2, MIP-1β, IP-10, MCP-1, and TCA-3. Figure 3a depicts a representative experiment. Each band represents a radiolabeled, protected probe specific for each chemokine. In the experiment shown, there was general increased expression of chemokine genes in OVA-sensitized skin compared with saline-sensitized skin in both WT and IL-4–/– mice. To quantify the results, we analyzed duplicate skin biopsies from 10 mice in each group. The bands were scanned using a densitometer, and the intensity of each chemokine signal was expressed as a percentage of the combined signals for the two housekeeping genes, L32 and GAPDH. There was a significant increase in the expression of MIP-1α in OVA-sensitized sites in both WT and IL-4–/– mice, whereas MIP-2, MIP-1β, IP-10, and RANTES increased significantly only in IL-4–/– mice (Figure 3b). More importantly, MIP-2, MIP-1β, and RANTES expression was significantly increased in IL-4–/– mice compared with WT controls following OVA sensitization. Increased expression of MIP-1β, MIP-2, and RANTES chemokines may underlie the increased accumulation of T cells in the skin of OVA-sensitized IL-4–/– mice.
Figure 3.
RNase protection assay for chemokine expression. (a) The OVA-sensitized IL-4 –/– mice have a strong signal for MIP-1β and MIP-2 and a less-intense signal for eotaxin compared with OVA-sensitized WT controls. Undigested labeled 32P probes were used as markers, and bands were matched to chemokines based on the predicted digested length. The samples were run on acrylamide (30:2) and exposed to Kodak X-AR film. (b) Pooled results of experiments using 10 OVA-sensitized mice and 10 saline-sensitized controls with duplicate biopsies. Intensity was determined by using a QuantiScan densitometer, and analysis of integration peaks were done with ImageQuant software. Samples were normalized to the combined L32 and GAPDH intensity. Columns represent mean ± SE. *P = 0.05 compared with saline.
Figure 3b shows that following OVA sensitization, eotaxin expression increased significantly (3.5-fold) only in WT mice. Furthermore, eotaxin expression was significantly decreased in IL-4–/– mice compared with WT controls following OVA sensitization. The decreased eotaxin expression in IL-4–/– mice may contribute to reduced eosinophil infiltration.
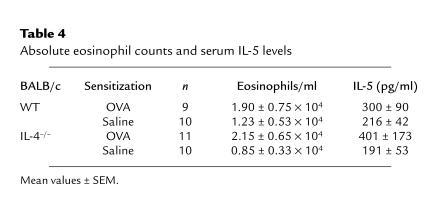
Given the role of IL-5 in eosinophil differentiation and survival, we investigated whether reduced serum IL-5 levels and diminished blood eosinophilia are additional causes of decreased eosinophilic infiltration in the skin of IL-4–/– mice. There were no significant differences in either absolute blood eosinophil count or in serum IL-5 level between IL-4–/– and WT mice sensitized with saline or between IL-4–/– and WT mice sensitized with OVA (WT-saline 1.23 ± 0.53 × 104 eosinophils/ml; WT-OVA 1.90 ± 0.75 × 104 eosinophils/ml; IL-4–/–-saline 0.85 ± 0.33 × 104 eosinophils/ml; IL-4–/–-OVA 2.15 ± 0.65 × 104 eosinophils/ml). In both IL-4–/– and WT mice, serum IL-5 levels increased following OVA sensitization; however, the increase was not statistically significant (WT-saline 216 ± 42 pg/ml; WT-OVA 300 ± 90 pg/ml; IL-4–/–-saline 191 ± 53 pg/ml; IL-4–/–-OVA 401 ± 173 pg/ml). These results suggest that the decrease in skin infiltration with eosinophils is not due to inefficient IL-5–driven differentiation of eosinophils.
Vascular cell adhesion molecule-1 (VCAM-1) is the counter-ligand to very late activation-4 antigen (VLA-4), which is expressed on eosinophils. VCAM-1 is essential for efficient adhesion of eosinophils to endothelium and their subsequent migration into tissue. We showed previously that VCAM-1 expression is increased in OVA-sensitized skin sites. IL-4 has been shown to upregulate the expression of VCAM-1 on endothelial cells (32). We investigated the possibility that lack of upregulation of VCAM-1 in sensitized skin of IL-4–/– mice underlies the decrease in tissue eosinophilia. Immunohistochemical analysis using an mAb to VCAM-1 showed that VCAM-1 expression was similar in IL-4–/– and WT mice sensitized with saline and in IL-4–/– and WT mice sensitized with OVA (data not shown). Possibly this is because other cytokines, such as TNF-α, also upregulate VCAM-1 expression (32).
OVA-sensitized skin sites of IFN-γ –/– mice have decreased thickening of the dermal layer.
Although the dermis in IFN-γ–/– mice thickened after OVA sensitization, the increase in thickness was not significant — in contrast to WT controls (Table 1). The number of cells per HPF and the distribution of infiltrating cells (e.g., CD45, CD3, CD4, CD8), eosinophils, and mast cells were equivalent in IFN-γ–/– mice and WT controls (Figure 1, Tables 2 and 3). There were no significant differences in the expression of chemokines in OVA-sensitized skin sites between IFN-γ–/– mice and WT controls (data not shown).
Cytokine expression in skin of cytokine deletion mice.
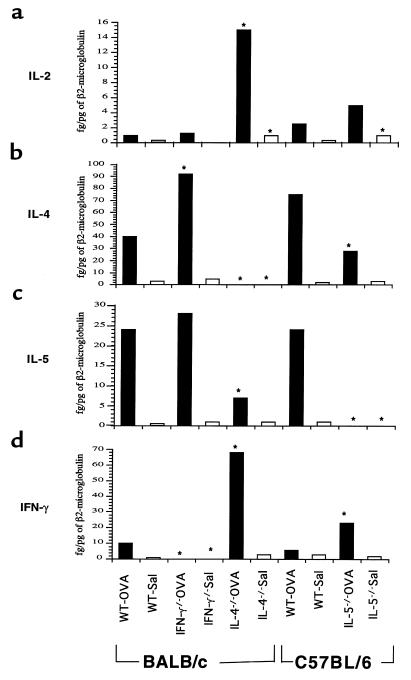
We have shown previously, using a semiquantitative RT-PCR, that epicutaneous sensitization with OVA increased local expression of mRNA for IL-4, IL-5, and IFN-γ (21). We used the same strategy to examine cytokine mRNA expression in sensitized skin sites of cytokine-deficient mice. OVA-sensitized skin sites from IL-4–/– mice demonstrated skewing to TH1 cytokines, with a 15-fold increase in IL-2 expression and a 6.8-fold increase in IFN-γ expression compared with WT control (Figure 4). In contrast, OVA-sensitized skin sites from IFN-γ–/– mice demonstrated skewing to IL-4 expression, with a significant twofold increase in IL-4 expression compared with WT control. OVA-sensitized skin from IL-5–/– mice had a significant twofold decrease in IL-4 expression and a significant threefold increase in IFN-γ expression.
Figure 4.
RT-PCR analysis of IL-2, IL-4, IL-5, IFN-γ, and β2-microglobulin mRNA levels in the skin biopsies from skin sites of mice sensitized with OVA or saline. Levels were normalized to β2-microglobulin. The filled bars represent the OVA-sensitized mice, and open bars represent the saline-sensitized mice. Pooled results of experiments using four OVA-sensitized mice and four saline-sensitized controls in duplicate for each strain of mice. IL-4–/– and IFN-γ–/– mice are in BALB/c background, and IL-5 –/– mice are in C57BL/6 background. (a) IL-2 levels. (b) IL-4 levels. (c) IL-5 levels. (d) IFN-γ levels. Bars represent mean ± SE. *P < 0.05 compared with WT controls.
Skewing of antibody isotypes in mice with targeted deletion of cytokine genes following epicutaneous sensitization with OVA.
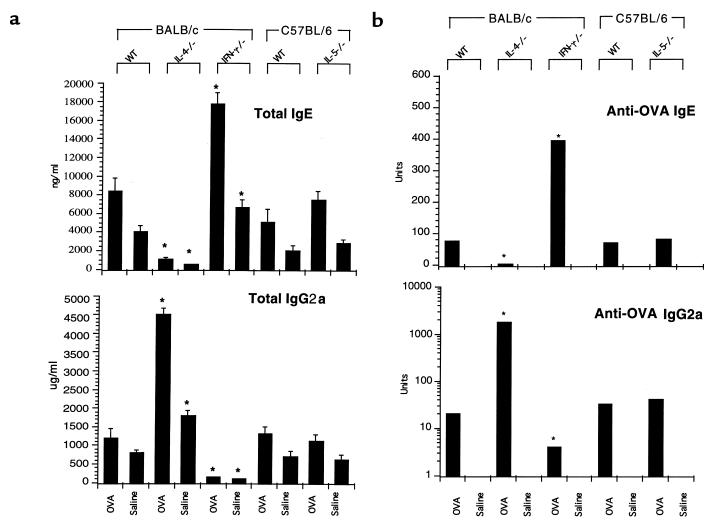
We showed previously that epicutaneous sensitization with OVA induces a rise in total serum IgE, as well as in OVA-specific IgE, IgG1, IgG2a, and IgG2b antibodies. Cytokines are known to affect immunoglobulin isotype switching. IL-4 plays an important role in switching to IgE, and IFN-γ plays an important role in switching to IgG2a (33, 34). This is demonstrated by the failure of IL-4–/– mice to mount an IgE antibody response and of IFN-γ–/– mice to make an IgG2a response (35, 36). These principles held true in our epicutaneous OVA-sensitization model. IL-4–/– mice had drastically less total and OVA-specific IgE and significantly more total and OVA-specific IgG2a in serum than did WT controls (Figure 5). Conversely, total and OVA-specific IgE were increased in IFN-γ–/– mice, whereas total and OVA-specific IgG2a were significantly decreased (Figure 5). Total and OVA-specific IgE and IgG2a in IL-5 –/– mice were equivalent to those in WT C57BL/6 controls (Figure 5).
Figure 5.
Serum immunoglobulin and OVA-specific antibody levels. (a) Total IgE and IgG2a were determined by ELISA (four mice per group). (b) OVA-specific IgE and IgG2a antigen-specific antibodies were determined by ELISA (four mice per group). The columns and error bar represent mean ± SE. *P < 0.05 compared with WT controls.
IgE antibody is not essential for the induction of skin inflammation by epicutaneous sensitization with OVA.
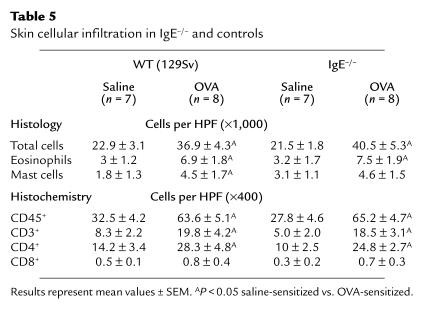
Serum IgE levels are elevated in the majority of patients with AD. Epicutaneous sensitization with OVA induces a vigorous increase in total and OVA-specific serum IgE (21). To assess the role of IgE antibody in the skin inflammation induced by epicutaneous sensitization with OVA, we studied IgE–/– mice. Figure 6 and Table 5 show that the cellular infiltrate in OVA-sensitized skin sites of IgE–/– mice was similar to that in OVA-sensitized skin sites of WT 129Sv controls. Histochemical analysis revealed a similar profile of cells bearing CD45, CD3, CD4, and CD8 in OVA-sensitized skin sites of IgE–/– mice and WT controls (Table 5). Furthermore, IL-2, IL-4, IL-5, and IFN-γ mRNA expression in OVA-sensitized skin sites of IgE–/– mice and WT controls was comparable (data not shown).
Figure 6.
Histological features of OVA-sensitized and saline-sensitized skin sites of IgE–/– and WT 129Sv controls.
Table 5.
Skin cellular infiltration in IgE–/– and controls
Discussion
The results of the present study suggest that the TH2 cytokines IL-4 and IL-5 contribute to skin inflammation and that the TH1 cytokine IFN-γ contributes to dermal thickening in a murine model of AD.
Eosinophils were absent from the skin of IL-5–/– mice. These findings are consistent with the nonredundant role of IL-5 in the differentiation of eosinophils from bone marrow precursors (37–39). More importantly, absence of eosinophils in OVA-sensitized skin sites of IL-5–/– mice was associated with a lack of increase in the thickness of the epidermal and dermal skin layers, a common feature of the skin lesion in AD (2). These results suggest that eosinophils play an important role in the hypertrophy of the skin in AD. Eosinophil major basic protein and eosinophil cationic protein are known to have cytotoxic effects (38). This may lead to tissue hypertrophy during the repair process, resulting in dermal thickening.
The role of IL-4 in our murine model of AD appears to be complex. Our data indicate that IL-4 is important for eosinophil recruitment into the skin. This is consistent with the previously established role of IL-4 in tissue eosinophilia in the allergic model of airway inflammation mice (19, 20, 40). OVA-sensitized skin sites from IL-4–/– mice did not exhibit the increased expression of eotaxin mRNA that we observed in WT controls. This observation agrees with previous observations that IL-4 increases eotaxin gene expression in skin and in dermal fibroblasts (41, 42). Taken together with the observation that serum IL-5 levels, blood eosinophil counts, and VCAM-1 expression at sensitized skin sites are equivalent in IL-4–/– mice and WT controls, our results suggest that IL-4 induction of eotaxin expression plays an important role in the eosinophilic infiltration into the skin lesions in AD. Expression of RANTES, another chemokine with chemotactic activity on eosinophils, remained increased in IL-4–/– mice, suggesting that it does not play a major role in recruiting eosinophils to the skin in our model. We cannot, however, rule out a role for additional chemokines such as MCP-3 and MCP-4, neither of which we have studied. An additional factor in the drastic reduction of eosinophils in the inflamed skin lesions of IL-4–/– mice may be the decreased local expression of mRNA for IL-5, a cytokine that plays a critical role in eosinophil survival. Whether the decrease in IL-5 mRNA and eotaxin expression in the skin of IL-4–/– mice following OVA sensitization can be detected at the induction phase of sensitization is a subject for future experiments.
In contrast to its role in promoting eosinophil infiltration, our results suggest that IL-4 modulates skin infiltration by T cells. OVA-sensitized skin sites in IL-4–/– mice had significantly higher numbers of infiltrating CD3+ cells than did WT controls. This was associated with a significantly increased expression of MIP-1β, MIP-2, and RANTES, chemokines that recruit TH1 cells (29–31, 43–45). These results suggest that IL-4 normally downregulates the expression of T-cell chemokines and the subsequent infiltration and expansion of T cells into the skin lesion. The persistence of a T-cell infiltrate in the OVA-sensitized skin of IL-4–/– mice does not rule out a role for TH2 cells in our model of AD. Indeed, IL-5 expression was still increased in OVA-sensitized skin sites of IL-4–/– mice. Similarly, there was no change in the size of the TH2 granuloma or in IL-5 expression in IL-4–/– mice sensitized with Schistosoma mansoni (31).
The thickness of the epidermal and dermal layers of OVA-sensitized skin sites of IL-4–/– mice did not differ from that of similar sites in WT controls. This may reflect the balance between the dual activities of IL-4 in AD. IL-4 may function as a proinflammatory cytokine by virtue of its ability to recruit eosinophils and to enhance collagen synthesis (46). IL-4 may also function as an anti-inflammatory cytokine, by virtue of its ability to suppress the infiltration of T cells, including TH1 cells that secrete IFN-γ, a cytokine that appears to play a role in enhancing dermal thickening.
We found significantly less thickening of the dermal layer in IFN-γ–/– mice than in WT mice following sensitization with OVA. These findings suggest that IFN-γ plays a role in the skin hypertrophy of AD. This is consistent with the predominant expression of IFN-γ in the hypertrophic skin lesions of patients with chronic AD and may be related to the ability of IFN-γ to activate tissue macrophages (47), which play an important role in the skin hypertrophy of delayed hypersensitivity reactions.
OVA-sensitized IL-4–/– mice had drastically reduced levels of IgE (Figure 5). Residual IgE probably is due to the effect of IL-13, a cytokine that has been shown recently to drive IgE isotype switching in murine B cells (48). The observation that skin infiltration with T cells was at least as intense in IL-4–/– mice as in WT controls strongly suggests that IgE is not important for the T-cell accumulation in our AD model. This is consistent with the observation that OVA-sensitized skin sites in IgE–/– mice and WT controls are similar (Figure 6 and Table 5); it is also consistent with the finding that antigen-induced airway inflammation and hyperresponsiveness can be elicited in IgE–/– mice (49). It should also be noted that serum IgE is not elevated in a small subgroup of patients with AD (50).
Our results are important because they establish a role for both the TH2 cytokines IL-4 and IL-5 and the TH1 cytokine IFN-γ in a murine model of AD. IL-4 and IL-5 are important for eosinophil infiltration, and IL-5 and IFN-γ are important for skin hypertrophy. In addition, IL-4 plays an anti-inflammatory role in AD by virtue of its ability to downmodulate T-cell infiltration into the skin. These findings have important implications for designing therapeutic strategies aimed at modulating cytokines and chemokines in AD.
Table 4.
Absolute eosinophil counts and serum IL-5 levels
Acknowledgments
The authors thank Amy Woodward for assistance in preparation of the manuscript. J.M. Spergel was supported by Glaxo Wellcome Allergy Training Award and Child Health Research Center grant NICHD P30HD27805. This work was also supported by National Institutes of Health (NIH) grants DK-47677 and DK-43551 (to A.K. Bhan) and NIH grants AI-31541, AI-31136T, 32AI-07512 (to R.S. Geha). R.S. Geha acknowledges the support of the Baxter, Olsten, and Alpha Therapeutics corporations.
References
- 1.Herz U, Bunikowski R, Renz H. Role of T cells in atopic dermatitis. Int Arch Allergy Immunol. 1998;115:179–190. doi: 10.1159/000023899. [DOI] [PubMed] [Google Scholar]
- 2.Leung DYM. Immunopathology of atopic dermatitis. Springer Semin Immunopathol. 1992;13:427–440. doi: 10.1007/BF00200539. [DOI] [PubMed] [Google Scholar]
- 3.Leiferman KM, et al. Dermal deposition of eosinophil-granule major basic protein in atopic dermatitis: comparison with onchocerciasis. N Engl J Med. 1985;313:282–285. doi: 10.1056/NEJM198508013130502. [DOI] [PubMed] [Google Scholar]
- 4.Cheng J, et al. Dermal eosinophils in atopic dermatitis undergo cytolytic degeneration. J Allergy Clin Immunol. 1997;99:683–692. doi: 10.1016/s0091-6749(97)70031-9. [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto S, Hamasaki Y, Ishii E, Ichimaru T, Miyazaki S. Unbalanced production of interleukin-5 and interleukin-2 in children with atopic dermatitis. Ann Allergy Asthma Immunol. 1997;78:517–523. doi: 10.1016/S1081-1206(10)63241-3. [DOI] [PubMed] [Google Scholar]
- 6.Nakazawa M, et al. Predominance of type cytokines-producing CD4+ and CD8+ cells in patients with atopic dermatitis. J Allergy Clin Immunol. 1997;99:673–682. doi: 10.1016/s0091-6749(97)70030-7. [DOI] [PubMed] [Google Scholar]
- 7.Tsicopoulos A, et al. Kinetics of cell infiltration and cytokine messenger RNA expression after intradermal challenge with allergen and tuberculin in the same atopic individuals. J Allergy Clin Immunol. 1994;94:764–772. doi: 10.1016/0091-6749(94)90185-6. [DOI] [PubMed] [Google Scholar]
- 8.Grewe M, Gyufku K, Schopf K, Krutman J. Lesional expression of interferon-gamma in atopic eczema. Lancet. 1994;343:25–26. doi: 10.1016/s0140-6736(94)90879-6. [DOI] [PubMed] [Google Scholar]
- 9.Werfel T, et al. Allergen specificity of skin-infiltrating T cells is not restricted to type-2 cytokine pattern in chronic skin lesions of atopic dermatitis. J Invest Dermatol. 1996;107:871–876. doi: 10.1111/1523-1747.ep12331164. [DOI] [PubMed] [Google Scholar]
- 10.Thepen T, et al. Biphasic response against aeroallergen in atopic dermatitis showing a switch from an initial Th2 response to a Th1 response in situ: An immunocytochemical study. J Allergy Clin Immunol. 1996;97:828–837. doi: 10.1016/s0091-6749(96)80161-8. [DOI] [PubMed] [Google Scholar]
- 11.Hamid Q, et al. In vivo expression of IL-12 and IL-13 in atopic dermatitis. J Allergy Clin Immunol. 1996;98:225–231. doi: 10.1016/s0091-6749(96)70246-4. [DOI] [PubMed] [Google Scholar]
- 12.Grewe M, et al. A role for Th1 and Th2 in the immunopathogenesis of atopic dermatitis. Immunol Today. 1998;19:359–361. doi: 10.1016/s0167-5699(98)01285-7. [DOI] [PubMed] [Google Scholar]
- 13.O’Garra A. Cytokines induce the development of functionally heterogeneous T helper cell subsets. Immunity. 1998;8:275–283. doi: 10.1016/s1074-7613(00)80533-6. [DOI] [PubMed] [Google Scholar]
- 14.Vercelli D, Geha R. Regulation of isotype switching. Curr Opin Immunol. 1992;4:794–797. doi: 10.1016/0952-7915(92)90064-l. [DOI] [PubMed] [Google Scholar]
- 15.Sanderson CJ. Interleukin-5, eosinophils, and disease. Blood. 1992;79:3101–3109. [PubMed] [Google Scholar]
- 16.Hogan S, Koskinen A, Foster P. Interleukin-5 and eosinophils induce airway damage and bronchial hyperreactivity during allergic airway inflammation in BALB/c mice. Immunol Cell Biol. 1997;75:284–288. doi: 10.1038/icb.1997.43. [DOI] [PubMed] [Google Scholar]
- 17.Hamelmann E, Gelfand E. The role of cytokines in the development of allergen-induced airway hyper-responsiveness. ACI International. 1998;10:59–63. [Google Scholar]
- 18.Foster P, Hogan S, Ramsay A, Matthaei K, Young I. Interleukin 5 deficiency abolishes eosinophilia, airways hyperreactivity and lung damage in a mouse asthma model. J Exp Med. 1996;183:195–201. doi: 10.1084/jem.183.1.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bruselle G, Kips J, Joos G, Bluethmann H, Pauwels R. Allergen-induced airway inflammation and bronchial responsiveness in wild type and interleukin-4 deficient mice. Am J Respir Cell Mol Biol. 1995;12:254–259. doi: 10.1165/ajrcmb.12.3.7873190. [DOI] [PubMed] [Google Scholar]
- 20.Kips JC, et al. Importance of interleukin-4 and interleukin-12in allergen-induced airway changes in mice. Int Arch Allergy Immunol. 1995;107:115–118. doi: 10.1159/000236947. [DOI] [PubMed] [Google Scholar]
- 21.Spergel J, et al. Epicutaneous sensitization with protein antigen induces localized allergic dermatitis and hyperresponsiveness to methacholine after single exposure to aerosolized antigen in mice. J Clin Invest. 1998;101:1614–1622. doi: 10.1172/JCI1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oettgen HC, et al. Active anaphylaxis in IgE-deficient mice. Nature. 1994;370:367–370. doi: 10.1038/370367a0. [DOI] [PubMed] [Google Scholar]
- 23.Mombaerts P, et al. Spontaneous development of inflammatory bowel disease in T cell receptor mutant mice. Cell. 1993;75:275–282. doi: 10.1016/0092-8674(93)80069-q. [DOI] [PubMed] [Google Scholar]
- 24.Colley D. Schistosoma mansoni: eosinophilia and the development of lymphocyte blastogenesis in response to soluble egg antigen in inbred mice. Exp Parasitol. 1972;32:520–526. doi: 10.1016/0014-4894(72)90070-7. [DOI] [PubMed] [Google Scholar]
- 25.Shire D, et al. An invitation to an open exchange of reagents and information useful for the measurements of cytokine mRNA levels by PCR. Eur Cytokine Netw. 1993;4:161–162. [Google Scholar]
- 26.Luster A. Chemokines — chemotactic cytokines that mediate inflammation. N Engl J Med. 1988;338:436–445. doi: 10.1056/NEJM199802123380706. [DOI] [PubMed] [Google Scholar]
- 27.Siveke J, Hamann A. T helper 1 and T helper 2 cells respond differentially to chemokines. J Immunol. 1998;160:550–554. [PubMed] [Google Scholar]
- 28.Sallusto F, Lang D, Mackay C, Lanzavecchia A. Flexible programs of chemokine receptor expression on human polarized T helper 1 and 2 lymphocytes. J Exp Med. 1998;187:875–883. doi: 10.1084/jem.187.6.875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bonecchi R, et al. Differential expression of chemokine receptors and chemotactic responsiveness of type 1 helper cells (Th1s) and Th2s. J Exp Med. 1998;187:129–134. doi: 10.1084/jem.187.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Qin S, et al. The chemokine receptors CXCR3 and CCR5 mark subsets of cells associated with certain inflammatory responses. J Clin Invest. 1998;101:746–754. doi: 10.1172/JCI1422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chensue S, Warmington K, Ruth J, Lukacs N, Kunkel S. Mycobacterial and schistosomal antigen-elicited granulomas formation in IFN-gamma and IL-4 knockout mice. J Immunol. 1997;159:3565–3573. [PubMed] [Google Scholar]
- 32.Thornhill M, et al. Tumor necrosis factor combines with IL-4 or IFN-gamma to selectively enhance endothelial cell adhesiveness for T cells, the contribution of vascular cell adhesion molecule-1-dependent and -independent binding mechanisms. J Immunol. 1991;146:592–598. [PubMed] [Google Scholar]
- 33.Bacharier L, Jabara H, Geha R. Molecular mechanisms of immunoglobulin E regulation. Int Arch Allergy Immunol. 1998;115:257–269. doi: 10.1159/000069456. [DOI] [PubMed] [Google Scholar]
- 34.Bossie A, Vitetta E. IFN-gamma enhances secretion of IgG2a from IgG2a-committed LPS–stimulated murine B cells: implications for the role of IFN-gamma in class switching. Cell Immunol. 1991;135:95–104. doi: 10.1016/0008-8749(91)90257-c. [DOI] [PubMed] [Google Scholar]
- 35.Vajdy M, Kosco-Vilboid M, Kopf M, Kohlet G, Lycke N. Impaired mucosal immune response in interleukin-4 targeted mice. J Exp Med. 1995;181:41–53. doi: 10.1084/jem.181.1.41. [DOI] [PubMed] [Google Scholar]
- 36.Graham M, et al. Response to influenza infection in mice with a targeted disruption in the interferon gamma gene. J Exp Med. 1993;178:1725–1732. doi: 10.1084/jem.178.5.1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bagley C, Lopez A, Vadas M. New frontiers for IL-5. J Allergy Clin Immunol. 1997;99:725–728. doi: 10.1016/s0091-6749(97)80002-4. [DOI] [PubMed] [Google Scholar]
- 38.Rothenberg M. Eosinophilia [review] N Engl J Med. 1998;338:1592–1600. doi: 10.1056/NEJM199805283382206. [DOI] [PubMed] [Google Scholar]
- 39.Weller P. Human eosinophils. J Allergy Clin Immunol. 1997;100:283–287. doi: 10.1016/s0091-6749(97)70237-9. [DOI] [PubMed] [Google Scholar]
- 40.Hogan SP, Mould A, Kikutsni H, Ramsay A, Foster P. Aeroallergen-induced eosinophilic inflammation, lung damage, and airway hyperreactivity in mice can occur independently of IL-4 and allergen-specific inflammation. J Clin Invest. 1997;99:1329–1339. doi: 10.1172/JCI119292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sanz M-J, et al. Human eotaxin induces α4 and β2 integrin-dependent eosinophil accumulation in rat skin in vivo: delayed generation of eotaxin in response to IL-4. J Immunol. 1988;160:3569–3576. [PubMed] [Google Scholar]
- 42.Mochizuki M, Bartels J, Mallet A, Christophers E, Schroder J. IL-4 induces eotaxin: a possible mechanism for selective eosinophil recruitment in helminth infection and atopy. J Immunol. 1998;160:60–68. [PubMed] [Google Scholar]
- 43.Boring L, et al. Impaired monocyte migration and reduced type 1 (TH1) cytokine responses in C-C chemokine receptor 2 knockout mice. J Clin Invest. 1997;100:2552–2561. doi: 10.1172/JCI119798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Trumpfheller C, Tenner-Racz K, Racz P, Fleischer B, Frosch S. Expression of macrophage inflammatory protein (MIP)-1alpha, MIP-1beta and RANTES gene in lymph nodes from HIV+ individuals: correlation with Th1-type cytokine response. Clin Exp Immunol. 1998;112:92–99. doi: 10.1046/j.1365-2249.1998.00555.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schrum S, Probst P, Fleischer B, Zipfel P. Synthesis of CC-chemokines MIP-1alpha, MIP-1beta and RANTES is associated with a type 1 immune response. J Immunol. 1996;157:3598–3604. [PubMed] [Google Scholar]
- 46.Sempowski G, Derdak S, Phipps R. Interleukin-4 and interferon-gamma discordantly regulate collagen biosynthesis by functionally distinct lung fibroblast subsets. J Cell Physiol. 1996;167:290–296. doi: 10.1002/(SICI)1097-4652(199605)167:2<290::AID-JCP13>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 47.Boehm U, Klamp T, Groot U, Howard J. Cellular responses to interferon-gamma. Annu Rev Immunol. 1997;15:749–795. doi: 10.1146/annurev.immunol.15.1.749. [DOI] [PubMed] [Google Scholar]
- 48.Emson C, Bell SE, Jones A, Wisden W, McKenzie A. Interleukin (IL)-4-independent induction of immunoglobulin (Ig)E, and perturbation of T cell development in transgenic mice expressing IL-13. J Exp Med. 1998;188:399–404. doi: 10.1084/jem.188.2.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mehlhop PD, et al. Allergen-induced bronchial hyperreactivity and eosinophilic inflammation occur in the absence of IgE in a mouse model of asthma. Proc Natl Acad Sci USA. 1997;94:1344–1349. doi: 10.1073/pnas.94.4.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Leung DYM. Atopic dermatitis: the skin as a window into the pathogenesis of chronic allergic disease. J Allergy Clin Immunol. 1995;96:312–319. doi: 10.1016/s0091-6749(95)70049-8. [DOI] [PubMed] [Google Scholar]