Abstract
Japanese encephalitis virus (JEV) is a leading cause of viral encephalitis worldwide and vaccination is one of the most effective ways to prevent disease. A suitable live-attenuated JEV vaccine could be formulated with a live-attenuated tetravalent dengue vaccine for the control of these viruses in endemic areas. Toward this goal, we generated chimeric virus vaccine candidates by replacing the precursor membrane (prM) and envelope (E) protein structural genes of recombinant dengue virus type 4 (rDEN4) or attenuated vaccine candidate rDEN4Δ30 with those of wild-type JEV strain India/78. Mutations were engineered in E, NS3 and NS4B protein genes to improve replication in Vero cells. The chimeric viruses were attenuated in mice and some elicited modest but protective levels of immunity after a single dose. One particular chimeric virus, bearing E protein mutation Q264H, replicated to higher titer in tissue culture and was significantly more immunogenic in mice. The results are compared with live-attenuated JEV vaccine strain SA14-14-2.
Keywords: Japanese encephalitis virus, Chimeric virus, Live-attenuated vaccine
1. Introduction
Japanese encephalitis virus (JEV), a member of the genus flavivirus, is a major cause of viral encephalitis in Asia. The virus has a single-strand, plus-sense, RNA genome of approximately 11 kb in length and a single ORF codes for a polyprotein that is processed by viral and host cellular proteases into 3 structural proteins (capsid [C], precursor-membrane [prM] and envelope [E]) and at least 7 non-structural proteins (NS1, NS2A, NS2B, NS3, NS4A, NS4B and NS5) [1]. The E protein is responsible for cell binding and entry and is the major target of virus neutralizing antibodies that mediate protection from disease [2,3]. Although there exist five recognizable JEV genotypes, there is only a single JEV serotype [4]. Studies have demonstrated significant cross-neutralization and cross-protection between virus strains from different JEV genotypes [5–7], supporting the conclusion that immunity to one JEV strain would be sufficient to protect against strains of the other four genotypes [8,9].
Three billion people live in regions with endemic JEV transmission resulting in approximately 60,000 cases annually [10]. However, only a small proportion of human JEV infections lead to clinical disease, which ranges from a mild febrile illness to acute and potentially lethal meningoencephalomyelitis [11]. Typically, 20–40% of human cases are fatal and 45–70% of survivors have neurologic sequelae [12]. Thus, Japanese encephalitis continues to be a significant public health burden even though it is a vaccine preventable disease.
Inactivated JEV vaccines have been available for human use since the mid 1950s [8,13,14]. Vero cell culture-derived, inactivated vaccines have gradually replaced mouse brain and primary cell culture-derived vaccines and have proven to be safe and immunogenic [13,15]. The limitations of inactivated vaccines include a high production cost and the requirement for multiple doses, often making them impractical for mass vaccination in most JEV endemic areas. The only live-attenuated vaccine in widespread use is JEV SA14-14-2 (Chengdu Institute of Biological Products), which was licensed in China in 1988 and more recently in Nepal, Korea, and Sri Lanka [13] and is produced in primary hamster kidney cells. This vaccine recently gained WHO prequalification in October of 2013. Attempts to adapt JEV SA14-14-2 to other cell substrates, such as primary dog kidney (PDK) cells, have resulted in mutations in the virus and reduced vaccine efficacy [16,17]. This has led to alternative approaches to develop live-attenuated JEV vaccines such as IMOJEV (Acambis/Sanofi-Aventis), which incorporates the prM and E structural genes of JEV SA14-14-2 into the yellow fever virus (YFV) 17D vaccine strain, and has recently been licensed for use in Australia and Thailand [14].
JEV co-circulates with dengue virus (DENV) serotypes 1–4 in Asia, causing a significant amount of morbidity and mortality, especially in children [18]. There are currently no licensed DENV vaccines, although several are in various stages of clinical development [19,20]. The live-attenuated tetravalent DENV vaccine developed at NIH is safe and immunogenic in humans, and a single dose induces a trivalent or better neutralizing antibody response in the majority of vaccines [21]. This prompted us to design a compatible, live-attenuated JEV vaccine candidate for incorporation into the NIH tetravalent DENV vaccine, thus creating a pentavalent vaccine for use in Asia. To that end, we generated JEV vaccine candidates by replacing the structural genes of a recombinant DENV-4 (rDEN4) and vaccine candidate rDEN4Δ30 with those of JEV genotype III strain India/78. A similar strategy has been used to generate vaccine candidates for DENV-2, West Nile virus (WNV), St. Louis encephalitis virus (SLEV), and tick-borne encephalitis virus (TBEV) [22–25]. Here we report the construction, in vitro characterization, and evaluation in mice of these JEV chimeric virus vaccine candidates.
2. Materials and methods
2.1. Cells and viruses
Vero (African green monkey kidney) cells were maintained at 37 °C in OptiPRO- SFM (Gibco) supplemented with 4 mM L-glutamine (Gibco). C6/36 (Aedes albopictus mosquito) cells were maintained at 32 °C in EMEM (Lonza) supplemented with 10% FBS (HyClone), 2 mM L-glutamine, and 0.1 mM NEAA (Gibco). Raji (human B-cell lymphoblast) cells were maintained at 37 °C in RPMI 1640 medium (Gibco) supplemented with 10% FBS, 2 mM L-glutamine, and 100 U/mL penicillin-streptomycin (Gibco). HEK-293T (human kidney) cells were maintained at 37 °C in EMEM supplemented with 10% FBS, 2 mM L-glutamine, and 100 U/mL penicillin-streptomycin.
JEV genotype III strain 7812474, designated “India/78” (Gen-Bank accession nos. EF688633 and U70387) [26,27] was obtained from the World Reference Center for Emerging Viruses and Arboviruses (UTMB, Galveston, TX), biologically cloned by terminal end-point dilution in Vero cells and sequenced. JEV strain SA14-14-2 was obtained from our laboratory archive and passaged once in Vero cells and sequenced. Although the previous passage history of our JEV strain SA14-14-2 was undocumented, the sequence matches that of Genbank accession no. JN604986 [28]. The rDEN4 and rDEN4Δ30 viruses were derived previously from cDNA clones [29].
2.2. Construction and recovery of chimeric viruses and rJEV
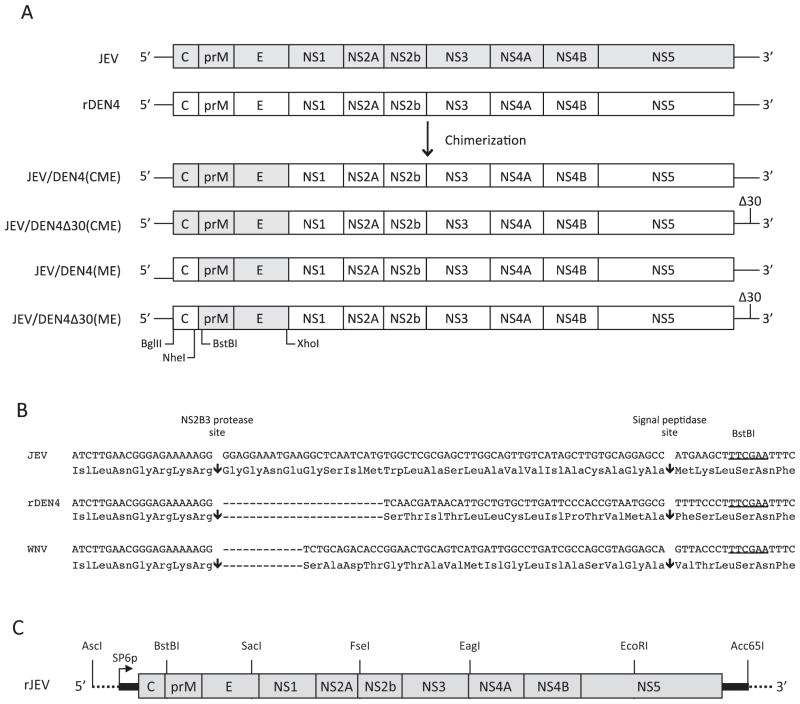
The cDNA clones of rDEN4 (p4) and rDEN4Δ30 (p4Δ30) were constructed previously [29]. A JEV-CME AscI-XhoI fragment containing the C, prM and E genes was synthesized and cloned into p4 and p4Δ30 to generate p4-JEV-CME and p4Δ30-JEV-CME (Fig. 1A). The JEV C gene sequence was exchanged for rDEN4 with a BglII-BstBI fragment, which generated p4-JEV-ME and p4Δ30-JEV-ME (Fig. 1A). The C-prM junction sequence was replaced using NheI-BstBI cDNA fragments (Fig. 1A and B). The cDNA gene segments encoding point mutations (Table 1) were cloned as BsiWI-XhoI, StuI-XmaI, and PmlI-XmaI cDNA fragments. Stability of chimeric virus cDNA constructs was improved by inserting a DNA stop codon linker (forward sequence 5′-TCGAGTGAGTTAACTTAGTCTAC-3′ and reverse sequence 5′-TCGAGTAGACTAAGTTAACTCAC-3′) into the XhoI restriction site.
Fig. 1.
Construction of recombinant chimeric virus and wild-type JEV cDNA clones. (A) For chimeric viruses, the C, prM and E genes, or just the prM and E genes of rDEN4 and rDEN4Δ30 cDNA clones (p4 and p4Δ30, respectively) were replaced with those of JEV strain India/78. The locations of restriction enzyme recognition sites used for cloning are indicated. (B) Three C-prM junction sequences, corresponding to JEV, rDEN4 and WNV, were used for constructing the JEV/DEN4 (ME) clones. The nucleotide and amino acid sequences surrounding the NS2B3 protease and signal peptidase cleavages sites (arrows) at the C-prM junction are shown. The BstBI restriction enzyme recognition site used for cloning is underlined. The other restriction enzyme site used for cloning (NheI) is located further upstream and not depicted in this figure. (C) Construction of a recombinant JEV India/78 cDNA clone. Restriction enzyme recognition sites used for cloning of the six, synthesized cDNA segments are indicated. UTR sequence is indicated in black and flanking vector sequence is indicated by a dotted line. The SP6 polymerase start site (SP6p) for generation of infectious transcripts is shown.
Table 1.
Properties of chimeric viruses.
| Virusa (clone) | C-prM junction | Geneb | Nucleotide change (chimeric virus numbering)b | Amino acid change (individual protein numbering)b | Phenotype in vero cells | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Mean peak titer (log10 PFU/mL) | Plaque size prior to adaptationc,d | Plaque size after adaptationc | |||||
| First-generation | |||||||
| JEV/DEN4 (CF-ME-0-13) | JEV | E | T1465C | F167S | 6.0 | Small | Large |
| E | A1900G | K312R | |||||
| E | T2254C | I430T | |||||
| NS4B | C7171T | P101L | |||||
| JEV/DEN4 (GG-ME-1-17) | DENV-4 | E | G1733C | Q264H | 6.6 | Small | Large |
| E | T2230C | I430T | |||||
| NS4B | C7147T | P101L | |||||
| 3′UTR | 10,485 A insert | N/A | |||||
| JEV/DEN4 (GG-ME-2-21) | WNV | E | A1671C | M240L | 6.1 | Small | Medium |
| E | A2391G | M480V | |||||
| NS3 | C5026T | S158L | |||||
| NS4B | C7171T | T105I | |||||
| JEV/DEN4Δ30 (CF-ME-0-14) | JEV | E | G1722T | V253F | 5.5 | Small | Small |
| NS2A | A4023G | M168V | |||||
| NS3 | G5170T | R202I | |||||
| NS4B | T7195C | V109A | |||||
| NS4B | C7588T | A240V | |||||
| JEV/DEN4Δ30 (GG-ME-1-24) | DENV-4 | NS3 | C5014T | S158L | 5.6 | Small | Small |
| NS4B | C7159T | T105I | |||||
| JEV/DEN4Δ30 (CF-ME-2-18) | WNV | E | T2043C | S364P | 5.3 | Small | Small |
| E | G2190A | G413R | |||||
| NS4B | T7192C | L112S | |||||
| Second-generation | |||||||
| JEV/DEN4 (B-1a) | DENV-4 | prM | G765A | E109K | 5.8 | Small | Small |
| NS3 | C5014T | S158L | |||||
| NS4B | C7159T | T105I | |||||
| JEV/DEN4 (C-14) | DENV-4 | E | T2230C | I430T | 6.0 | Small | Large |
| NS4B | C7147T | P101L | |||||
| JEV/DEN4 (AC-7a) | DENV-4 | E | G1733C | Q264H | 6.6 | Large | Large |
| E | T2230C | I430T | |||||
| NS4B | C7147T | P101L | |||||
| JEV/DEN4 (D-5a) | DENV-4 | E | A1567G | K209R | 6.0 | Small | Medium |
| NS4B | T7180C | L112S | |||||
| JEV/DEN4Δ30 (B-2a) | DENV-4 | prM | T936C | Y166H | 5.0 | Small | Small |
| NS3 | C5014T | S158L | |||||
| NS4B | C7159T | T105I | |||||
| JEV/DEN4Δ30 (D-6a) | DENV-4 | NS3 | G4667T | M42I | 3.9 | Small | Small |
| NS4B | T7180C | L112S | |||||
All viruses are ME chimeric viruses (CME chimeric viruses were not viable). ME has been omitted from the virus names.
Engineered mutations introduced into the second generation viruses are shown in bold.
Plaque size was measured on day 6 post-infection: small is <1 mm, medium is 1–2 mm, and large is >2 mm. Vero-adapted rJEV India/78 (3 days post-infection) and rDEN4 produce large plaques. Vero-adapted rDENΔ30 produces medium plaques. JEV SA14-14-2 (3 days post-infection) produces small plaques.
Plaque size on Vero cells directly after recovery of virus and prior to terminal dilutions on Vero cells.
A recombinant JEV (rJEV) India/78 was constructed from five synthesized cDNA segments and subcloned into an engineered AscI-SacI-FseI-EagI-EcoRI-Acc65I polycloning site within a modified pBR322 vector (Fig. 1C). Stability of the JEV cDNA construct was achieved by inserting a DNA stop codon linker (forward sequence 5′-CTGACTTAACTTAGACTAGAGCT-3′ and reverse sequence 5′-CTAGTCTAAGTTAAGTCAGAGCT-3′) into the SacI restriction site.
Recovery of the chimeric viruses and rJEV was accomplished by removing the stop codon linker sequence with restriction-enzyme digestion, followed by re-ligation and subsequent linearization with Acc65I. Full genome-length capped RNA transcripts were synthesized with the AmpliCap SP6 Message Maker Kit (Epicentre Biotechnologies). Purified transcripts were transfected into Vero or C6/36 cells and cell culture supernatant was harvested after 3–7 days and titered in Vero cells. Recovered viruses were purified by multiple terminal dilutions, amplified in Vero cells to generate biological clones, and sequenced.
2.3. Mouse studies
Studies in mice were performed in accordance with the regulations and guidelines of the NIH (Bethesda, MD) and approved by the Animal Care and Use Committee of NIAID. Viruses were tested for neuroinvasiveness by intraperitoneal (IP) inoculation (0.1 mL) and neurovirulence by intracerebral (IC) inoculation (0.01 mL) of either 3-week-old (weanling) female or 3-day-old (suckling) Swiss Webster (SW) mice (Taconic). Groups of six weanling mice or ten suckling mice were inoculated with each virus dilution and monitored 21 days for signs of encephalitis leading to a moribund state, including tremors, seizure, and paralysis. Moribund mice were humanely euthanized to minimize pain and distress and LD50 values were determined [30].
To assess virus replication in the brain, groups of five weanling SW mice were inoculated IC with 103 PFU of virus. One group per virus was euthanized on day 1 and every other day for up to 11 days. Brains were homogenized individually as a 10% (w/v) suspension in L-15 medium, clarified by low-speed centrifugation, and frozen on dry ice. Virus titers were determined by plaque assay in Vero cells.
Immunogenicity and protection was evaluated in weanling mice. Groups of mice were immunized IP with 104 PFU of chimeric virus, rDEN4, or JEV SA14-14-2. In experiment #1, serum was collected on day 21 from groups of six mice for neutralization assays. To demonstrate protection, groups of ten immunized mice were challenged IP with 104 (experiment #2), 105 (experiment #3), or 106 (experiment #4) PFU of rJEV on day 28 or day 20 (experiment #4). All challenged mice were monitored for 21 days for signs of encephalitis and moribund mice were euthanized.
2.4. Tissue culture replication kinetics
Vero and C6/36 cells were infected at a multiplicity of infection (MOI) of 0.01 PFU/cell, washed three times with PBS and replenished with fresh medium. Infected Vero and C6/36 cells were incubated at 37 and 32 °C, respectively. Samples were taken at time 0 and every 24 h for 7 days and titered in Vero cells.
2.5. Production of JEV reporter virus particles (RVPs)
A cDNA fragment corresponding to the JEV India/78C, prM, and E genes was synthesized and cloned into mammalian expression vector pCMV6-AC (OriGene) to generate pJEV-CprME. A sub-genomic WNV replicon encoding GFP (WNIIrep-GFP) was provided by Dr. Ted Pierson (NIAID). JEV reporter virus particles (RVPs) were produced by co-transfecting HEK-293T cells, as described [31,32]. JEV RVP stocks were titered in Raji cells 2 days post-infection and the percentage of GFP expressing cells determined by flow cytometry.
2.6. JEV RVP serum neutralization assay
JEV RVPs were diluted in the linear range of infectivity and incubated for 1 h at 37 °C with an equal volume of serially diluted mouse serum or JEV hyperimmune mouse positive control ascitic fluid (American Type Culture Collection). RVP-serum mixtures were combined with an equal volume of Raji cells, incubated at 37 °C for two days, fixed with paraformaldehyde, and counted by flow cytometry to determine the percentage of GFP-expressing cells. The data were fit by a dose–response curve (variable slope) to determine the effective concentration of serum where 50% neutralization occurred (EC50) and titers are reported as the reciprocal geometric mean EC50 titer (GMT) of mice that seroconverted (detectable EC50).
2.7. Statistical analysis
Comparisons of virus titer in tissue culture were analyzed using an unpaired t-test with statistical significance (p < 0.05) determined by the Holm-Sidak method. Mouse survival analyses were done using the Log-rank (Mantel-Cox) test, with p < 0.05 required for significance.
3. Results
3.1. Recovery and characterization of first-generation chimeric viruses
Replacing the C, prM and E structural genes of rDEN4 and rDENΔ30 with those of JEV did not produce viable chimeric viruses on multiple attempts and this strategy was abandoned. However, replacing just the prM and E genes generated viable chimeric viruses (Table 1). JEV/DEN4 and JEV/DEN4Δ30 ME chimeric viruses containing three different C-prM junctions (Fig. 1B) were recovered in either C6/36 or Vero cells. The chimeric viruses replicated in Vero cells to titers of 5.3–6.6 log10PFU/mL and initially had small plaque morphologies after recovery while some developed larger plaques following Vero cell adaptation (Table 1). The biologically cloned chimeric viruses were sequenced and all had acquired multiple mutations (Table 1).
The six chimeric viruses, rDEN4, rDEN4Δ30, and JEV SA14-14-2 did not cause mortality in weanling mice by IC or IP routes of inoculation of a dose up to 104 PFU (Table 2). By comparison, wild-type (wt) JEV was neurovirulent and neuroinvasive, having relatively low IC and IP LD50 levels similar to the recombinant-derived rJEV that was recovered in both Vero and C6/36 cells (Table 2).
Table 2.
Virulence in weanling and suckling mice.
| Virus | Clone | C-prM junction | Weanling mice (n = 6/dose)
|
Suckling mice (n = 10/dose)
|
||
|---|---|---|---|---|---|---|
| IP LD50 (PFU) | IC LD50 (PFU) | IC LD50 (PFU) | Median survival time (days)a | |||
| JEV India/78 | Wild-type | – | 40 | 0.6 | 1.5 | 4 |
| rJEV India/78 | Recombinant | – | 10 | 0.4 | 0.3 | 4 |
| JEV SA14-14-2 | Vaccine Strain | – | >10,000b | >10,000 | 0.3 | 7 |
| rDEN4 | Recombinant | – | >10,000 | >10,000 | >100 | >21c,d,e |
| rDEN4Δ30 | Vaccine strain | – | >10,000 | >10,000 | >100 | >21d,e |
| First-generation | ||||||
| JEV/DEN4 | CF-ME-0-13 | JEV | >10,000 | >10,000 | NT | NTg |
| JEV/DEN4 | GG-ME-1-17 | DENV-4 | >10,000 | >10,000 | NT | NT |
| JEV/DEN4 | GG-ME-2-21 | WNV | >10,000 | >10,000 | NT | NT |
| JEV/DEN4Δ30 | CF-ME-0-14 | JEV | >10,000 | >3000 | NT | NT |
| JEV/DEN4Δ30 | GG-ME-1-24 | DENV-4 | >10,000 | >4000 | NT | NT |
| JEV/DEN4Δ30 | CF-ME-2-18 | WNV | >10,000 | >2000 | NT | NT |
| Second-generation | ||||||
| JEV/DEN4 | B-1a | DENV-4 | >10,000 | >3200 | 22 | 10c,d,e |
| JEV/DEN4 | C-14 | DENV-4 | >10,000 | >5000 | 7 | 13d,e |
| JEV/DEN4 | AC-7a | DENV-4 | >10,000 | >10,000 | 0.8 | 8.5d,e,f |
| JEV/DEN4 | D-5a | DENV-4 | >10,000 | >10,000 | ≥1000 | 18.5d,e |
| JEV/DEN4Δ30 | B-2a | DENV-4 | >10,000 | >1000 | >1000 | >21d,e |
| JEV/DEN4Δ30 | D-6a | DENV-4 | >1600 | >160 | 17h | >21d,e |
Reported for the high dose IC (103 PFU).
All values shown with “>” sign indicate the highest dose administered.
>21 days is reported if the majority of mice survived until the end of the study.
Survival time is statistically different from rJEV India/78 by Log-rank (Mantel-Cox) test.
Survival time is statistically different from JEV SA14-14-2 by Log-rank (Mantel-Cox) test.
Survival time is statistically different from JEV/DEN4 C-14 by Log-rank (Mantel-Cox) test.
Not tested (NT).
Mortality did not follow a clear dose response.
3.2. Recovery and characterization of second-generation chimeric viruses
Combinations of mutations that were identified in first-generation chimeric viruses were introduced into second-generation cDNA clones (Table 1). Together the NS4B-P101L and Δ30 UTR deletion mutation produced a virus that replicated to low titer and was not tested further. However, six other chimeric viruses were recovered and replicated to peak titers of 3.9–6.6 log10PFU/mL and had small plaque morphologies after recovery (except JEV/DEN4 AC-7a), and in some cases developed larger plaques following Vero cell adaptation (Table 1). The chimeric viruses were sequenced and most had acquired additional mutations (generally in the structural-protein regions), with the exception of JEV/DEN4 AC-7a, which was genetically stable (Table 1).
3.3. Virulence of second-generation chimeric viruses for mice
The second-generation chimeric viruses along with rDEN4, rDEN4Δ30, and JEV SA14-14-2 were screened for IP or IC virulence in 3-week-old mice at both a high (up to 104 PFU) and low (102 PFU) dose. Mortality was not observed for these viruses, which confirmed their attenuated phenotypes (Table 2). Wild-type JEV and rJEV were tested at a 102 PFU dose IP and IC and caused >50% IP mortality and 100% IC mortality (data not shown).
Virulence of the second-generation chimeric viruses was subsequently tested in the more sensitive suckling mouse model. Both wt JEV and rJEV were highly virulent, having LD50 levels of ~1 PFU and median survival times of 4 days (Table 2). JEV SA14-14-2 and JEV/DEN4 AC-7a had LD50 levels similar to wt JEV, but had significantly longer median survival times (Table 2). JEV/DEN4 clones B-1a, C-14 and JEV/DEN4Δ30 D-6a had significantly higher LD50 levels and longer median survival times (Table 2). JEV/DEN4Δ30 D-6a mortality did not follow a clear dose response, with 60%, 60%, and 40% mortality at 101, 102, and 103 PFU doses, respectively. The remaining chimeric viruses caused little or no mortality in suckling mice, similar to rDEN4 and rDEN4Δ30 (Table 2).
The genomes of JEV/DEN4 clones C-14 and AC-7a differed by a single nucleotide (Q264H amino acid substitution) in the E protein (Table 1). JEV/DEN4 AC-7a, bearing E mutation Q264H, had an ~10-fold lower IC LD50 and a 4-day reduction in median survival time (Table 2 and Fig. 2A), indicating that this mutation significantly increases virulence in suckling mice.
Fig. 2.
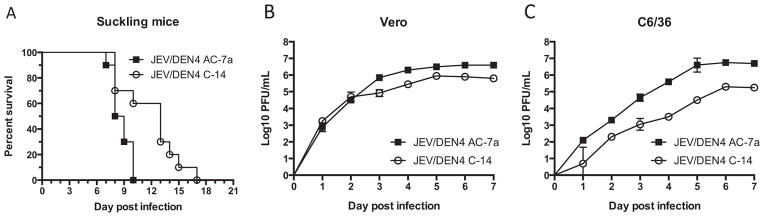
The impact of JEV/DEN4 AC-7a envelope protein mutation Q264H on virulence in suckling mice and replication in tissue culture. (A) Survival curves for suckling mice injected IC with 103 PFU of JEV/DEN4 clones C-14 and AC-7a were significantly different by Log-rank test (p = 0.0076). Replication of JEV/DEN4 clones C-14 and AC-7a in Vero (B) and C6/36 (C) cells infected at an MOI of 0.01 PFU/cell. Samples were taken daily and titered in Vero cells. Error bars represent the standard error of the mean (SEM) from two independent experiments.
3.4. Tissue culture replication of JEV/DEN4 clones C-14 and AC-7a
Tissue culture replication experiments were performed for JEV/DEN4 clones C-14 and AC-7a to determine if the E-Q264H mutation that increased virulence for suckling mice also increased replication. In Vero cells, JEV/DEN4 AC-7a had a modest but significant increase in titer on days 3–7 post-infection and an increase in peak titer of 0.6 log10PFU/mL compared to JEV/DEN4 C-14 (Fig. 2B). The difference in replication between viruses was more pronounced in C6/36 cells, with JEV/DEN4 AC-7a reaching significantly higher titers on days 1–7 post-infection, with an increase in peak titer of 1.5 log10PFU/mL (Fig. 2C) indicating that the E-Q264H mutation enhances replication in mammalian and mosquito cells.
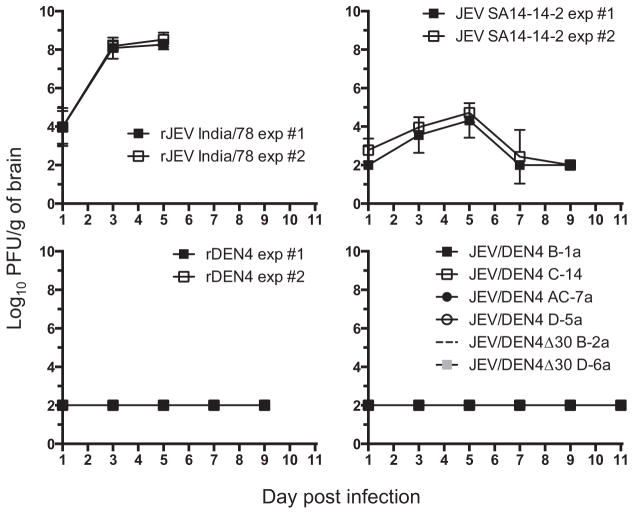
3.5. Replication of chimeric viruses and controls in weanling mouse brain
rJEV replicated in the brain of weanling mice with a mean peak titer greater than 8 log10PFU/g by day 5 post-infection, at which point complete mortality was observed (Fig. 3). JEV SA14-14-2 replicated to greater than 4 log10PFU/g of brain by day 5 post-infection followed by a drop in titer to below the limit of detection and all mice survived with no signs of disease (Fig. 3). All six, second-generation chimeric viruses behaved like rDEN4, having virus titers at or below the limit of detection through day 11 post-infection and showing no signs of disease (Fig. 3).
Fig. 3.
Replication of chimeric viruses and controls in the brain of weanling mice. Groups of five-, three-week-old, SW mice per time-point were infected IC with 103 PFU of virus. Beginning on day 1 post-infection, and then every other day thereafter, groups of animals were euthanized and brains were harvested and homogenized. Virus titers were determined in Vero cells, with a limit of detection of 2 log10 PFU/g of brain. Data for rJEV India/78, JEV SA14-14-2 and rDEN4 are shown for two independent experiments (#1 and #2). The six, second-generation chimeric viruses and rDEN4 had titers at or below the limit of detection. Error bars represent the standard deviation (SD).
3.6. Immunogenicity and protection from wild-type rJEV challenge
Several experiments were performed in weanling mice to determine if the chimeric viruses were immunogenic. In experiment #1, immunization with JEV/DEN4 clones AC-7a, D-5a, and JEV/DEN4Δ30 B-2a resulted in relatively low seroconversion frequencies and mean neutralization titers (GMT) of 10–50 (Table 3). Mice immunized with the other three candidates did not induce detectable JEV neutralizing antibody titers, similar to mock and rDEN4 immunized control mice. In comparison, all mice immunized with JEV SA14-14-2 seroconverted, with a GMT of 267 (Table 3).
Table 3.
Immunogenicity and protection in mice.
| Virus | Clone | Experiment #1 (n = 6) | Experiment #2 (n = 10) | Experiment #3 (n = 10) | Experiment #4 (n = 10) | |||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Seroconversion | GMT (1/EC50 )a | Percent survival (104 PFU rJEV) | Percent survival (105 PFU rJEV) | Seroconversion | GMT (1/EC50 )a | Percent survival (106 PFU rJEV) | ||
| JEV/DEN4 | B-1a | 0/6 | <8 | 80 | –b | 0/10 | <8 | 80 |
| JEV/DEN4 | C-14 | 0/6 | <8 | 80 | – | 1/10 | 8 | 100c |
| JEV/DEN4 | AC-7a | 2/6 | 50 | 100 | – | 6/10 | 80 | 90e |
| JEV/DEN4 | D-5a | 2/6 | 28 | 90 | – | 1/10 | 8 | 60 |
| JEV/DEN4Δ30 | B-2a | 1/6 | 10 | – | 90 | 0/10 | <8 | 50e |
| JEV/DEN4Δ30 | D-6a | 0/6 | <8 | – | 100c,d | 1/10 | 28 | 30e |
| JEV SA14-14-2 | Vaccine strain | 6/6 | 267 | 100 | 100c,d | 6/10 | 41 | 100c |
| rDEN4 | Recombinant | 0/6 | <8 | 70 | 60 | 0/10 | <8 | 70 |
| Mock | Not applicable | 0/6 | <8 | 80 | 60 | 0/10 | <8 | 60 |
Geometric mean reciprocal EC50 titers for mice that seroconverted (limit of detection: <8).
A dash indicates the virus was not tested.
Survival curve is statistically different from mock immunized mice by Log-rank (Mantel-Cox) test.
Survival curve is statistically different from rDEN4 immunized mice by Log-rank (Mantel-Cox) test.
These groups contained mice that were significantly undersized for their reported age (AC-7a = 2/10 mice, B-2a = 9/10 mice, D-6a = 4/10 mice) at the time of immunization and this may have affected the experimental outcomes.
In experiment #2, immunized mice were challenged with 104 PFU of rJEV. Mock and rDEN4 immunized groups of mice only had 20% and 30% mortality, respectively, so statistically significant levels of protection could not be established (Table 3). However, all mice immunized with JEV/DEN4 AC-7a and JEV SA14-14-2 survived, while those immunized with JEV/DEN4 clones D-5a, B-1a and C-14 experienced some mortality (Table 3).
In experiment #3, immunized mice were challenged with a higher, 105 PFU dose of rJEV that resulted in 40% mortality in mock and rDEN4 immunized groups of mice. All of the mice immunized with JEV/DEN4Δ30 D-6a and JEV SA14-14-2 survived challenge, and this was statistically significant (Table 3). JEV/DEN4Δ30 B-2a immunization resulted in 90% survival, but this was not statistically different from mock or rDEN4 immunized mice.
Experiment #4 was designed to correlate the frequency of seroconversion with protection among immunized mice. Immunization with JEV/DEN4 AC-7a and JEV SA14-14-2 resulted in 60% seroconversion and neutralizing GMTs of 80 and 41, respectively. All mice immunized with JEV SA14-14-2 survived challenge, compared to 90% for JEV/DEN4 AC-7a (Table 3). Mice immunized with JEV/DEN4 clones C-14, D-5a or JEV/DEN4Δ30 D-6a each had one mouse seroconvert with relatively low neutralizing antibody titers and only mice immunized with JEV/DEN4C–14 had significant protection from challenge with rJEV (Table 3). Mice immunized with the remaining two chimeric viruses did not induce detectable neutralizing antibody, but JEV/DEN4 B-1a immunization did improve survival (Table 3). Overall, JEV/DEN4 AC-7a was the only candidate to demonstrate protection in conjunction with a substantial level of seroconversion.
4. Discussion
Since JEV co-circulates with DENV 1–4 in Asia, it would be ideal to produce an inexpensive, live-attenuated, pentavalent vaccine to protect against both diseases. With this goal in mind, we developed a set of chimeric viruses by replacing the structural protein genes of rDEN4 and rDEN4Δ30 with those of wt JEV India/78 to generate vaccine candidates that were compatible with the NIH tetravalent DENV vaccine [21]. Replacing the C, prM and E genes of rDEN4 or rDEN4Δ30 with those of JEV did not result in viable chimeric viruses, similar to results of comparable strategies with other flaviviruses [22,33,34]. However, we were able to recover viable chimeric viruses by exchanging only the prM and E protein genes, inferring that the C protein gene may be incompatible between flaviviruses due to its lack of sequence conservation, which may hinder genome cyclization and encapsidation of viral RNA [35–43].
The first-generation ME chimeric viruses accumulated a number of mutations throughout the genome during passaging and adaptation to Vero cells. All six first-generation candidates contained at least one NS4B mutation (P101L, T105I, V109A, L112S, A240V) known to improve DENV replication in Vero cells [44]. The NS4B-P101L mutation has been shown to decrease replication in mosquitoes or mosquito cell lines and enhance replication in mammalian cell lines [45]. The importance of mutations that were identified outside of the NS4B gene has not been defined. The combinations of mutations E-I430T/NS4B-P101L or NS3-S158L/NS4B-T105I were each found in two separate chimeric viruses, which may indicate that they work well in concert. Additionally, utilization of JEV, rDEN4 and WNV C-prM junctions produced viable chimeric viruses with similar in vitro and in vivo phenotypes, and the lack of mutation within this site indicated that they were genetically stable and interchangeable.
Second-generation ME chimeric viruses were engineered to contain a set of mutations based on observations from the first generation. After recovery and adaptation to Vero cells, only JEV/DEN4 AC-7a bearing the NS4B-P101L/E-I430T/E-Q264H combination was genetically stable. Mutation E-I430T was found in three independently- isolated large-plaque chimeric viruses suggesting that it alleviates an incompatibility created by chimerization and might stabilize the virus genome when combined with NS4B-P101L.
In weanling mice, wt JEV and rJEV were neuroinvasive and highly neurovirulent, replicating to high titer in the brain and causing uniform mortality. The JEV/DEN4 chimeric viruses, by contrast, behaved like the rDEN4 and rDEN4Δ30 parent viruses, which were avirulent and had little or no detectable replication in the brain. In comparison, the JEV SA14-14-2 vaccine strain was also avirulent in this mouse model, but surprisingly replicated to greater than 4 log10PFU/g of brain.
In the more permissive suckling mouse model, wt JEV, rJEV, and JEV SA14-14-2 were highly neurovirulent, whereas rDEN4 and rDEN4Δ30 were avirulent, consistent with their lack of neurovirulence. Various levels of attenuation were observed for the chimeric viruses in these mice. The most attenuated chimeric virus, JEV/DEN4Δ30 B-2a, bearing a 3′ UTR deletion mutation that attenuates rDEN4 [29,46], caused no mortality. The least attenuated chimeric virus in suckling mice, JEV/DEN4 AC-7a, had a virulence phenotype similar to the JEV SA14-14-2 vaccine strain.
JEV/DEN4 clones C-14 and AC-7a differed by a single Q264H amino acid substitution in the E protein that increased replication in mammalian (Vero) and mosquito (C6/36) cells, virulence for suckling mice, and immunogenicity in weanling mice. The ability of mutation NS4B-P101L, which is shared by JEV/DEN4 clones C-14 and AC-7a, to enhance replication in mammalian cells [45] likely masks the true magnitude of the phenotype conferred by E-Q264H. This E protein mutation is rare among wt JEV strains and was one of many mutations that arose during efforts to improve immunogenicity of the JEV SA14-14-2 vaccine strain, which included subcutaneous passage in suckling mice [17]. Our data indicate that E-Q264H might improve immunogenicity by increasing virus replication in vivo, as it does in vitro. It is notable that E-Q264H did not increase replication of JEV/DEN4 AC-7a to detectable levels in weanling mouse brain, indicating that the enhanced replication may only occur in peripheral tissues. E protein residue 264 is located in domain II at the dimer interface, adjacent to histidine (H) 263, which is conserved among JEV serocomplex viruses [47]. Protonation of histidine residues at acidic pH is proposed to drive structural rearrangements of the E protein necessary for flavivirus membrane fusion [48] and the E-Q264H mutation could have an impact on this mechanism.
The rDEN4 and rDEN4Δ30 clones have been used as a platform to generate chimeric virus vaccine candidates for WNV and SLEV, both JEV-serocomplex viruses, with mixed results [23,24]. Like SLEV, chimerization of JEV with rDEN4 or rDEN4Δ30 produced several vaccine candidates that were over-attenuated in mice. However, a single vaccine candidate (JEV/DEN4 AC-7a) bearing the replication enhancing E-Q264H mutation was genetically stable, attenuated, and immunogenic in mice, suggesting it is a suitable candidate for further development. We are currently investigating this possibility along with alternative live-attenuated JEV vaccine options that would be appropriate for combination with the NIH tetravalent DENV vaccine.
Acknowledgments
We would like to thank the NIAID Comparative Medicine Branch for assisting with animal studies, Dr. José Bustos-Arriaga for assisting with flow cytometry, and Drs. Ted Pierson and Kim Dowd for supplying reagents and expertise for the RVP assay. This work was supported by the National Institute of Allergy and Infectious Diseases Intramural Research Program, National Institutes of Health.
References
- 1.Lindenbach BD, Rice CM. Molecular biology of flaviviruses. Adv Virus Res. 2003;59:23–61. doi: 10.1016/s0065-3527(03)59002-9. [DOI] [PubMed] [Google Scholar]
- 2.Pierson TC, Fremont DH, Kuhn RJ, Diamond MS. Structural insights into the mechanisms of antibody-mediated neutralization of flavivirus infection: implications for vaccine development. Cell host & microbe. 2008;4:229–38. doi: 10.1016/j.chom.2008.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Markoff L. Points to consider in the development of a surrogate for efficacy of novel Japanese encephalitis virus vaccines. Vaccine. 2000;18(Suppl 2):26–32. doi: 10.1016/s0264-410x(00)00038-4. [DOI] [PubMed] [Google Scholar]
- 4.Solomon T, Ni H, Beasley DW, Ekkelenkamp M, Cardosa MJ, Barrett AD. Origin and evolution of Japanese encephalitis virus in southeast Asia. Journal of virology. 2003;77:3091–8. doi: 10.1128/JVI.77.5.3091-3098.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu X, Yu Y, Li M, Liang G, Wang H, Jia L, et al. Study on the protective efficacy of SA14-14-2 attenuated Japanese encephalitis against different JE virus isolates circulating in China. Vaccine. 2011;29:2127–30. doi: 10.1016/j.vaccine.2010.12.108. [DOI] [PubMed] [Google Scholar]
- 6.Beasley DW, Li L, Suderman MT, Guirakhoo F, Trent DW, Monath TP, et al. Protection against Japanese encephalitis virus strains representing four genotypes by passive transfer of sera raised against ChimeriVax-JE experimental vaccine. Vaccine. 2004;22:3722–6. doi: 10.1016/j.vaccine.2004.03.027. [DOI] [PubMed] [Google Scholar]
- 7.Kurane I, Takasaki T. Immunogenicity and protective efficacy of the current inactivated Japanese encephalitis vaccine against different Japanese encephalitis virus strains. Vaccine. 2000;18(Suppl 2):33–5. doi: 10.1016/s0264-410x(00)00041-4. [DOI] [PubMed] [Google Scholar]
- 8.Beasley DW, Lewthwaite P, Solomon T. Current use and development of vaccines for Japanese encephalitis. Expert Opin Biol Ther. 2008;8(1):95–106. doi: 10.1517/14712598.8.1.95. [DOI] [PubMed] [Google Scholar]
- 9.Tsarev SA, Sanders ML, Vaughn DW, Innis BL. Phylogenetic analysis suggests only one serotype of Japanese encephalitis virus. Vaccine. 2000;18(Suppl 2):36–43. doi: 10.1016/s0264-410x(00)00039-6. [DOI] [PubMed] [Google Scholar]
- 10.Campbell GL, Hills SL, Fischer M, Jacobson JA, Hoke CH, Hombach JM, et al. Estimated global incidence of Japanese encephalitis: a systematic review. Bulletin of the World Health Organization. 2011;89:766–74. 74A–74E. doi: 10.2471/BLT.10.085233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Solomon T, Vaughn DW. Pathogenesis and clinical features of Japanese encephalitis and West Nile virus infections. Curr Top Microbiol Immunol. 2002;267:171–94. doi: 10.1007/978-3-642-59403-8_9. [DOI] [PubMed] [Google Scholar]
- 12.van den Hurk AF, Ritchie SA, Mackenzie JS. Ecology and geographical expansion of Japanese encephalitis virus. Annu Rev Entomol. 2009;54:17–35. doi: 10.1146/annurev.ento.54.110807.090510. [DOI] [PubMed] [Google Scholar]
- 13.Halstead SB, Thomas SJ. New Japanese encephalitis vaccines: alternatives to production in mouse brain. Expert Rev Vaccines. 2011;10(3):355–64. doi: 10.1586/erv.11.7. [DOI] [PubMed] [Google Scholar]
- 14.Appaiahgari MB, Vrati S. Clinical development of IMOJEV (R)—a recombinant Japanese encephalitis chimeric vaccine (JE-CV) Expert Opin Biol Ther. 2012;12(9):1251–63. doi: 10.1517/14712598.2012.704908. [DOI] [PubMed] [Google Scholar]
- 15.McArthur MA, Holbrook MR. Japanese Encephalitis Vaccines. J Bioterror Biodef. 2011;S1:2. doi: 10.4172/2157-2526.S1-002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eckels KH, Yu YX, Dubois DR, Marchette NJ, Trent DW, Johnson AJ. Japanese encephalitis virus live-attenuated vaccine, Chinese strain SA14-14-2; adaptation to primary canine kidney cell cultures and preparation of a vaccine for human use. Vaccine. 1988;6:513–8. doi: 10.1016/0264-410x(88)90103-x. [DOI] [PubMed] [Google Scholar]
- 17.Yu Y. Phenotypic and genotypic characteristics of Japanese encephalitis attenuated live vaccine virus SA14-14-2 and their stabilities. Vaccine. 2010;28(21):3635–41. doi: 10.1016/j.vaccine.2010.02.105. [DOI] [PubMed] [Google Scholar]
- 18.Gould EA, Solomon T. Pathogenic flaviviruses. Lancet. 2008;371(9611):500–9. doi: 10.1016/S0140-6736(08)60238-X. [DOI] [PubMed] [Google Scholar]
- 19.Coller BA, Clements DE. Dengue vaccines: progress and challenges. Curr Opin Immunol. 2011;23(3):391–8. doi: 10.1016/j.coi.2011.03.005. [DOI] [PubMed] [Google Scholar]
- 20.Murphy BR, Whitehead SS. Immune response to dengue virus and prospects for a vaccine. Annu Rev Immunol. 2011;29:587–619. doi: 10.1146/annurev-immunol-031210-101315. [DOI] [PubMed] [Google Scholar]
- 21.Durbin AP, Kirkpatrick BD, Pierce KK, Elwood D, Larsson CJ, Lindow JC, et al. A single dose of any of four different live attenuated tetravalent dengue vaccines is safe and immunogenic in flavivirus-naive adults: a randomized, double-blind clinical trial. The Journal of infectious diseases. 2013;207:957–65. doi: 10.1093/infdis/jis936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pletnev AG, Bray M, Huggins J, Lai CJ. Construction and characterization of chimeric tick-borne encephalitis/dengue type 4 viruses. Proceedings of the National Academy of Sciences of the United States of America. 1992;89:10532–6. doi: 10.1073/pnas.89.21.10532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blaney JE, Jr, Speicher J, Hanson CT, Sathe NS, Whitehead SS, Murphy BR, et al. Evaluation of St. Louis encephalitis virus/dengue virus type 4 antigenic chimeric viruses in mice and rhesus monkeys. Vaccine. 2008;26:4150–9. doi: 10.1016/j.vaccine.2008.05.075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pletnev AG, Putnak R, Speicher J, Wagar EJ, Vaughn DW. West Nile virus/dengue type 4 virus chimeras that are reduced in neurovirulence and peripheral virulence without loss of immunogenicity or protective efficacy. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:3036–41. doi: 10.1073/pnas.022652799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Whitehead SS, Hanley KA, Blaney JE, Jr, Gilmore LE, Elkins WR, Murphy BR. Substitution of the structural genes of dengue virus type 4 with those of type 2 results in chimeric vaccine candidates which are attenuated for mosquitoes, mice, and rhesus monkeys. Vaccine. 2003;21:4307–16. doi: 10.1016/s0264-410x(03)00488-2. [DOI] [PubMed] [Google Scholar]
- 26.Gulati BR, Singha H, Singh BK, Virmani N, Kumar S, Singh RK. Isolation and genetic characterization of Japanese encephalitis virus from equines in India. Journal of veterinary science. 2012;13:111–8. doi: 10.4142/jvs.2012.13.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Uchil PD, Satchidanandam V. Phylogenetic analysis of Japanese encephalitis virus: envelope gene based analysis reveals a fifth genotype, geographic clustering, and multiple introductions of the virus into the Indian subcontinent. Am J Trop Med Hyg. 2001;65(3):242–51. doi: 10.4269/ajtmh.2001.65.242. [DOI] [PubMed] [Google Scholar]
- 28.Song BH, Yun GN, Kim JK, Yun SI, Lee YM. Biological and genetic properties of SA(1)(4)-14-2, a live-attenuated Japanese encephalitis vaccine that is currently available for humans. Journal of microbiology. 2012;50:698–706. doi: 10.1007/s12275-012-2336-6. [DOI] [PubMed] [Google Scholar]
- 29.Durbin AP, Karron RA, Sun W, Vaughn DW, Reynolds MJ, Perreault JR, et al. Attenuation and immunogenicity in humans of a live dengue virus type-4 vaccine candidate with a 30 nucleotide deletion in its 3′-untranslated region. The American journal of tropical medicine and hygiene. 2001;65:405–13. doi: 10.4269/ajtmh.2001.65.405. [DOI] [PubMed] [Google Scholar]
- 30.Reed LJ, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hygiene. 1938;27(3):493–7. [Google Scholar]
- 31.Pierson TC, Sanchez MD, Puffer BA, Ahmed AA, Geiss BJ, Valentine LE, et al. A rapid and quantitative assay for measuring antibody-mediated neutralization of West Nile virus infection. Virology. 2006;346:53–65. doi: 10.1016/j.virol.2005.10.030. [DOI] [PubMed] [Google Scholar]
- 32.Pierson TC, Xu Q, Nelson S, Oliphant T, Nybakken GE, Fremont DH, et al. The stoichiometry of antibody-mediated neutralization and enhancement of West Nile virus infection. Cell host & microbe. 2007;1:135–45. doi: 10.1016/j.chom.2007.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pletnev AG, Men R. Attenuation of the Langat tick-borne flavivirus by chimerization with mosquito-borne flavivirus dengue type 4. Proc Natl Acad Sci USA. 1998;95(4):1746–51. doi: 10.1073/pnas.95.4.1746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chambers TJ, Nestorowicz A, Mason PW, Rice CM. Yellow fever/Japanese encephalitis chimeric viruses: construction and biological properties. Journal of virology. 1999;73:3095–101. doi: 10.1128/jvi.73.4.3095-3101.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Liu ZY, Li XF, Jiang T, Deng YQ, Zhao H, Wang HJ, et al. A novel cis-acting element within the capsid-coding region enhances flavivirus vRNA replication by regulating genome cyclization. Journal of virology. 2013 doi: 10.1128/JVI.00243-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Friebe P, Pena J, Pohl MO, Harris E. Composition of the sequence downstream of the dengue virus 5′ cyclization sequence (dCS) affects viral RNA replication. Virology. 2012;422:346–56. doi: 10.1016/j.virol.2011.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Samsa MM, Mondotte JA, Caramelo JJ, Gamarnik AV. Uncoupling cis-Acting RNA elements from coding sequences revealed a requirement of the N-terminal region of dengue virus capsid protein in virus particle formation. Journal of virology. 2012;86:1046–58. doi: 10.1128/JVI.05431-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khromykh AA, Westaway EG. RNA binding properties of core protein of the flavivirus Kunjin. Arch Virol. 1996;141(3–4):685–99. doi: 10.1007/BF01718326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pong WL, Huang ZS, Teoh PG, Wang CC, Wu HN. RNA binding property and RNA chaperone activity of dengue virus core protein and other viral RNA-interacting proteins. FEBS letters. 2011;585:2575–81. doi: 10.1016/j.febslet.2011.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stocks CE, Lobigs M. Signal peptidase cleavage at the flavivirus C-prM junction: dependence on the viral NS2B-3 protease for efficient processing requires determinants in C, the signal peptide, and prM. J Virol. 1998;72(3):2141–9. doi: 10.1128/jvi.72.3.2141-2149.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lobigs M, Lee E. Inefficient signalase cleavage promotes efficient nucleocapsid incorporation into budding flavivirus membranes. J Virol. 2004;78(1):178–86. doi: 10.1128/JVI.78.1.178-186.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee E, Stocks CE, Amberg SM, Rice CM, Lobigs M. Mutagenesis of the signal sequence of yellow fever virus prM protein: enhancement of signalase cleavage in vitro is lethal for virus production. Journal of virology. 2000;74:24–32. doi: 10.1128/jvi.74.1.24-32.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Amberg SM, Rice CM. Mutagenesis of the NS2B-NS3-mediated cleavage site in the flavivirus capsid protein demonstrates a requirement for coordinated processing. J Virol. 1999;73(10):8083–94. doi: 10.1128/jvi.73.10.8083-8094.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Blaney JE, Jr, Manipon GG, Firestone CY, Johnson DH, Hanson CT, Murphy BR, et al. Mutations which enhance the replication of dengue virus type 4 and an antigenic chimeric dengue virus type 2/4 vaccine candidate in Vero cells. Vaccine. 2003;21:4317–27. doi: 10.1016/s0264-410x(03)00487-0. [DOI] [PubMed] [Google Scholar]
- 45.Hanley KA, Manlucu LR, Gilmore LE, Blaney JE, Jr, Hanson CT, Murphy BR, et al. A trade-off in replication in mosquito versus mammalian systems conferred by a point mutation in the NS4B protein of dengue virus type 4. Virology. 2003;312:222–32. doi: 10.1016/s0042-6822(03)00197-1. [DOI] [PubMed] [Google Scholar]
- 46.Men R, Bray M, Clark D, Chanock RM, Lai CJ. Dengue type 4 virus mutants containing deletions in the 3′ noncoding region of the RNA genome: analysis of growth restriction in cell culture and altered viremia pattern and immunogenicity in rhesus monkeys. Journal of virology. 1996;70:3930–7. doi: 10.1128/jvi.70.6.3930-3937.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luca VC, AbiMansour J, Nelson CA, Fremont DH. Crystal structure of the Japanese encephalitis virus envelope protein. Journal of virology. 2012;86:2337–46. doi: 10.1128/JVI.06072-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fritz R, Stiasny K, Heinz FX. Identification of specific histidines as pH sensors in flavivirus membrane fusion. J Cell Biol. 2008;183(2):353–61. doi: 10.1083/jcb.200806081. [DOI] [PMC free article] [PubMed] [Google Scholar]