Abstract
Frailty is a clinical state in which there is an increase in an individual’s vulnerability for developing increased dependency and/or mortality when exposed to a stressor. Frailty can occur as the result of a range of diseases and medical conditions. A consensus group consisting of delegates from 6 major international, European, and US societies created 4 major consensus points on a specific form of frailty: physical frailty.
Physical frailty is an important medical syndrome. The group defined physical frailty as “a medical syndrome with multiple causes and contributors that is characterized by diminished strength, endurance, and reduced physiologic function that increases an individual’s vulnerability for developing increased dependency and/or death.”
Physical frailty can potentially be prevented or treated with specific modalities, such as exercise, protein-calorie supplementation, vitamin D, and reduction of polypharmacy.
Simple, rapid screening tests have been developed and validated, such as the simple FRAIL scale, to allow physicians to objectively recognize frail persons.
For the purposes of optimally managing individuals with physical frailty, all persons older than 70 years and all individuals with significant weight loss (≥5%) due to chronic disease should be screened for frailty.
Keywords: Frailty, physical frailty, rapid screening tests, weight loss, comorbidities
Frailty is a condition in which the individual is in a vulnerable state at increased risk of adverse health outcomes and/or dying when exposed to a stressor.1 The European Union has placed specific importance on defining frailty, as frail persons are high users of community resources, hospitalization, and nursing homes. It is assumed that early intervention with frail persons will improve quality of life and reduce costs of care.2,3
Frailty is either physical or psychological or a combination of the 2 components, and is a dynamic condition that can improve or worsen over time. Two approaches to defining physical frailty have become popular. The deficit model consists of adding together an individual’s number of impairments and conditions to create a Frailty Index.4 The second model originally defined a specific physical phenotype consisting of a constellation of 5 possible components (weight loss, exhaustion, weakness, slowness, and reduced physical activity), which marked an underlying physiologic state of multisystem and energy dysregulation.5 Both of these definitions are currently used to define a frail and a prefrail state, a condition between frail and nonfrail. Frailty domains appear to belong to a common construct, with physical strength being one of the discriminating characteristics. 6 Numerous other frailty definitions have been developed, for the most part based on one or the other of these 2 basic approaches.
A recent systematic review incorporating 31 studies of frailty in persons 65 years or older found a prevalence of from 4.0% to 17.0% (mean 9.9%) of physical frailty, with a higher prevalence when psychosocial frailty was also included.7 Women (9.6%) were almost twice as likely as men (5.2%) to be frail. The prevalence of frailty is markedly increased in persons older than 80.
A previous consensus conference on frailty agreed “on the usefulness of defining frailty in clinical settings” and that there was a need for a clear conceptual framework.8 Other areas in which they had more than 80% agreement included that frailty is
A clinical syndrome
Not disability
Increased vulnerability in which minimal stress can cause functional impairment
Might be reversible or attenuated by interventions
Mandatory for health workers to detect as soon as possible
Useful in primary and community care
However, the conference failed to recommend a clear course forward because of an inability to agree on a “single operational definition of frailty that can satisfy all experts.” The heterogeneity of that consensus group may have contributed to the inability to come to a firm conclusion.
Rockwood9 previously suggested criteria for a successful definition of frailty. These are content validity (ie, is dynamic, includes multiple determinants, and is useful in different situations), construct validity (ie, more common in women and advancing age and related to disability), and criterion validity (ie, predicts adverse outcomes including mortality). Numerous models are available that meet most of these criteria (Table 1).10–26
Table 1.
Examples of Well-Validated Frailty Models
Because of the uncertainty created by the previous consensus conference on frailty and a need to determine whether there is sufficient information available to advocate screening by all physicians for frailty, a consensus conference was convened in Orlando, Florida, on December 7, 2012. The conference was based on the International Association of Gerontology and Geriatrics and World Health Organization white paper, recognizing the need to improve the “ability of older persons to age in place” rather than to be institutionalized.19 The aim of this consensus conference was to define an operational definition of frailty and to frame aspects for screening and treatment and identify an appropriate population to screen. A major finding of this group was a recognition and agreement on the distinction between the broader definition of frailty, which is a general state or condition of an individual, and a more specific medical syndrome: physical frailty. This communication provides the consensus opinions of experts involved in the Frailty Consensus Conference.
Methods
Six major international (International Association of Gerontology and Geriatrics; Society on Sarcopenia, Cachexia, and Wasting Diseases; and the International Academy of Nutrition and Aging), European (European Union Geriatric Medicine Society), and US societies (American Medical Directors Association and American Federation for Aging Research) provided delegates to attend this consensus meeting. In addition, 7 other experts in the area of frailty were invited by the conveners (Bruno Vellas and John Morley) to enrich the content knowledge base. Separate areas were discussed and a broad consensus was reached on a variety of recommendations. During the discussion, it became apparent that a major reason that prior attempts at a consensus around frailty were not successful is that they did not resolve distinctions between broad definitions of frailty and more specific subsets. In this meeting, a full consensus was developed and agreement attained around physical frailty being a specific medical syndrome within the broader context of frailty.
Based on this consensus, a preliminary manuscript was developed and a modified Delphi process was used in which the manuscript was circulated to all the delegates until agreement was obtained on the content, leading to the development of this consensus report.27
Recommendations
1. Physical Frailty Is an Important Medical Syndrome
The group defined frailty as
“A medical syndrome with multiple causes and contributors that is characterized by diminished strength, endurance, and reduced physiologic function that increases an individual’s vulnerability for developing increased dependency and/or death.”
In addition to the definition, the group made 4 key points:
Although recognizing that frail individuals could be disabled and that not all disabled persons are frail, the group agreed that the emphasis on case finding should target the pre-disabled not the dependent (defined here as persons with 1 or more deficits in basic activities of daily living). Targeting those who are frail and pre-disabled in this manner, case finding becomes of major importance, as it allows interventions that could prevent dependency.
Although sarcopenia may be a component of frailty, it was agreed that frailty is more multifaceted than sarcopenia alone.27–31
The group agreed that a number of well-validated models of frailty existed and that the definitive diagnosis of frailty should be done by a geriatrician using the basic criteria of these well-defined models. It is accepted that these models predict increased vulnerability to adverse health outcomes and mortality.32–39
As conceived in this document, physical frailty differs from multimorbidity. Both are common, but multimorbidity is more pervasive, being present in 3 of 4 persons older than 65 years and 1 of 4 in those younger than 65.40 Physical frailty focuses on specific areas for which a general treatment approach can be developed, whereas multimorbidity moves the focus to the management of each condition separately, although both require multidimensional assessment and management. A larger construct of frailty, as proposed by Rockwood et al,41 as a state of increased vulnerability due to impairments in many systems that may give rise to diminished ability to respond to even mild stresses, incorporates multimorbidity and central nervous system impairments that can be recognized in relation to cognitive and affective disorders.
2. Simple Screening Tests Are Available to Be Used by Physicians to Recognize Frail Persons and Identify Persons With Physical Frailty or at Risk of Frailty
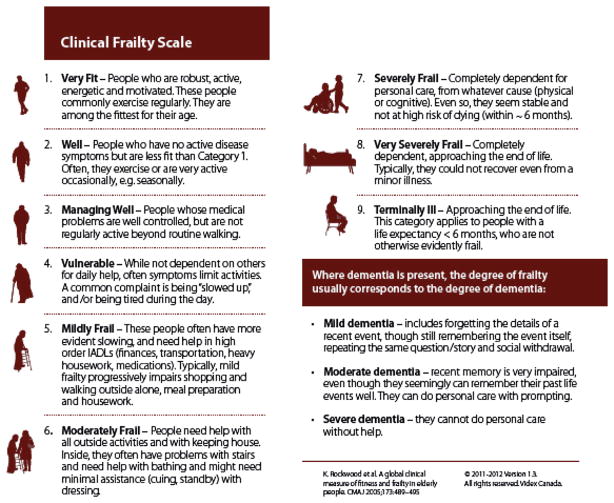
The Royal College of Physicians and the French Society of Geriatrics and Gerontology advocated screening for frailty in older persons.42,43 Simple rapid screening tests have been developed and validated to allow physicians to rapidly recognize frail persons. Examples of some commonly used and validated frailty tools include the FRAIL (Table 2),44–47 the Cardiovascular Health Study Frailty Screening Measure (Table 3),10,11 the Clinical Frailty Scale (Figure 1),41 and the Gérontopôle Frailty Screening Tool (Table 4).48 The group agreed that such instruments can be used to identify persons with the physical frailty syndrome who are in need of a more in-depth assessment. All persons aged 70 years and older, as well as any person with significant weight loss (≥5% over the past year) due to chronic illnesses should be screened for frailty.
Table 2.
The Simple “FRAIL” Questionnaire Screening Tool
| 3 or greater = frailty; 1 or 2 = prefrail |
| Fatigue: Are you fatigued? |
| Resistance: Cannot walk up 1 flight of stairs? |
| Aerobic: Cannot walk 1 block? |
| Illnesses: Do you have more than 5 illnesses? |
| Loss of weight: Have you lost more than 5% of your weight in the past 6 months? |
Table 3.
Prefrail, 1 or 2; Frail, ≥3
|
Data for older women (lowest 20th percentile).
Fig. 1.
Clinical Frailty Scale. Scoring is based on clinical judgment. Reprinted with permission from Rockwood et al.41
Table 4.
Gérontopôle Frailty Screening Tool48
| Frailty Screening
| |||
|---|---|---|---|
| Older patients, 65 y and older, not dependent (activities of daily living ≥5/6)
| |||
| Yes | No | Unknown | |
| Is your patient living alone? | □ | □ | □ |
| Involuntary weight loss in the past 3 months? | □ | □ | □ |
| Fatigability from the past 3 months? | □ | □ | □ |
| Have some mobility difficulties for the past 3 months? | □ | □ | □ |
| Memory complaints? | □ | □ | □ |
| Slow gait speed (+4 s for 4 meters)? | □ | □ | □ |
If yes to at least one of these questions:
Do you feel in your own clinical opinion that your patient is frail and at an increased risk for further disabilities?
□ Yes □ No
If yes, propose to the patient an evaluation of the causes of frailty and prevention of disabilities in a day hospital.
Reprinted with permission from Subra et al.48
3. Physical Frailty Is a Manageable Condition
The committee recognized there are numerous potential causes of physical frailty, and many of these could be targeted in future intervention development. However, they agreed that at this time at least some evidence supported 4 possible treatments that appeared to have some efficacy in the treatment of frailty.
Exercise (resistance and aerobic)
Caloric and protein support
Vitamin D
Reduction of polypharmacy
Singh et al49 demonstrated that a year of resistance exercise in frail persons following hip fracture decreased hospitalizations and nursing home placement. Yamada et al,50 in a community-based exercise program involving 610 frail persons, found that exercise was cost effective in preventing frailty progression and disability. Theou et al,51 in a systematic review, found that 45 to 60 minutes of exercise 3 times a week seemed to have positive effects on frail older adults and may be used for the management of frailty. Exercise in frail individuals increases functional performance, walking speed, chair stand, stair climbing, and balance, and decreased depression and fear of falling. Group and home-based exercise programs reduce falls.52
Weight loss is a major component of the frailty syndrome.53–55 Calorie supplement enhanced weight gain and reduced mortality in undernourished older individuals and reduced complications according to the Cochrane Collaboration.56 Protein-calorie supplementation improved outcomes in persons with chronic obstructive pulmonary disease.57 Nutritional supplementation is effective in the treatment of weight loss.58,59 Protein supplementation increases muscle mass,60–65 reduces complications,66 improves grip strength,66 produces weight gain,66 and may act synergistically with resistance exercise in older persons.62,63 Frailty can also be seen in persons who are morbidly obese.67
In older persons who are 25(OH) vitamin D deficient, there is evidence that vitamin D supplementation will reduce falls,68 hip fractures,69 and mortality.70 It may also improve muscle function.71 Although there are no large-scale clinical trials that show that frailty can be prevented or treated by vitamin D alone, there is sufficient evidence of efficacy in frailty-appearing populations to suggest that vitamin D in frail persons who are vitamin D deficient would be useful.
It was agreed that interventions against sarcopenia could be clinically beneficial in cases of frailty.72,73 Polypharmacy is recognized as a possible major contributor to the pathogenesis of frailty.74–78 Hence, reduction in inappropriate medicines can clearly decrease costs79 and medication side effects in frail populations.80–83 The Beers criteria84 and STOPP and START criteria85,86 can be helpful guidelines to reduce inappropriate medicine use in this population.
Other potential causes for frailty can be found in some specific individuals. These include depression, visual and hearing problems, diabetes mellitus, congestive heart failure, and cognitive decline, as examples. The intervention plan in frail older adults must include the management of reversible diseases.
4. All Persons Older Than 70 Years Should Be Screened for Frailty
It was agreed that sufficient evidence exists for the implementation of frailty screening by health care providers in persons 70 years and older. Although finite evidence is not yet available, there are compelling reasons to screen, as it is noninvasive and may uncover remedial conditions. Based on available data, screening tests for frailty meet the major criteria for screening, viz. they are sensitive. Effective treatments are available for components of the syndrome and simple screening tests produce more beneficial than harmful outcomes.87 In the presence of a positive screen, the physician can institute management for frailty or refer the patient to a geriatrician. 88 A similar approach has been successfully instituted by the Gérontopôle in Toulouse.48,89 A screening approach is being carried out widely in Japan, with interventions as suggested by the consensus group proving successful.90–92 Both primary care physicians and specialists need to screen for frailty. Evidence suggests that persons with heart failure,93 cancer,94 renal failure,95 HIV,96 or diabetes,97 as well as those undergoing surgery,98 are more likely to be frail and have more adverse outcomes than those who are not frail. Hence, a focus on the treatment of frail persons in this group may improve overall outcomes. The frailty diagnosis can be implemented to judge the appropriateness of a number of invasive management strategies, such as radiotherapy, chemotherapy, surgery, and cardiology procedures.
To successfully combat frailty, our medical practice must be targeted, strong, and sustained. With the aging of our population, we cannot wait and must implement the screening and management of frailty into clinical practice worldwide.
Acknowledgments
Supported by unrestricted educational grants from Sanofi and Nutricia Advanced Medical Nutrition (group Danone).
Footnotes
The authors declare no conflicts of interest.
References
- 1.Walston J, Hadley EC, Ferrucci L, et al. Research agenda for frailty in older adults: Toward a better understanding of physiology and etiology: Summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54:991–1001. doi: 10.1111/j.1532-5415.2006.00745.x. [DOI] [PubMed] [Google Scholar]
- 2.Cerreta F, Eichler HG, Rasi G. Drug policy for an aging population—the European Medicines Agency’s geriatric medicines strategy. N Engl J Med. 2012;367:1972–1974. doi: 10.1056/NEJMp1209034. [DOI] [PubMed] [Google Scholar]
- 3. [Accessed April 22, 2013]; Available at: http://ec.europa.eu/economy_finance/publications/european_economy/2012/pdf/ee-2012-2_en.pdf.
- 4.Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med. 2011;27:17–26. doi: 10.1016/j.cger.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 5.Fried LP, Ferrucci L, Darer J, et al. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59:255–263. doi: 10.1093/gerona/59.3.m255. [DOI] [PubMed] [Google Scholar]
- 6.Sourial N, Bergman H, Karunananthan S, et al. Contribution of frailty markers in explaining differences among individuals in five samples of older persons. J Gerontol A Biol Sci Med Sci. 2012;67:1197–1204. doi: 10.1093/gerona/gls084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: A systematic review. J Am Geriatr Soc. 2012;60:1487–1492. doi: 10.1111/j.1532-5415.2012.04054.x. [DOI] [PubMed] [Google Scholar]
- 8.Rodríguez-Mañas L, Féart C, Mann G, et al. on behalf of the FOD-CC group. Searching for an operational definition of frailty: A Delphi method based consensus statement. The Frailty Operative Definition-Consensus Conference Project. J Gerontol A Biol Sci Med Sci. 2013;68:62–67. doi: 10.1093/gerona/gls119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rockwood K. What would make a definition of frailty successful? Age Ageing. 2005;34:432–434. doi: 10.1093/ageing/afi146. [DOI] [PubMed] [Google Scholar]
- 10.Fried LP, Tangen CM, Walston J, et al. Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 11.Bandeen-Roche K, Xue QL, Ferrucci L, et al. Phenotype of frailty: Characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci. 2006;61:262–266. doi: 10.1093/gerona/61.3.262. [DOI] [PubMed] [Google Scholar]
- 12.Ensrud KE, Ewing SK, Taylor BC, et al. Comparison of 2 frailty indexes for prediction of falls, disability, fractures, and death in older women. Arch Intern Med. 2008;168:382–389. doi: 10.1001/archinternmed.2007.113. [DOI] [PubMed] [Google Scholar]
- 13.Kiely DK, Cupples LA, Lipsitz LA. Validation and comparison of two frailty indexes: The MOBILIZE Boston Study. J Am Geriatr Soc. 2009;57:1532–1539. doi: 10.1111/j.1532-5415.2009.02394.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rockwood K, Abeysundera MJ, Mitnitski A. How should we grade frailty in nursing home patients? J Am Med Dir Assoc. 2007;8:595–603. doi: 10.1016/j.jamda.2007.07.012. [DOI] [PubMed] [Google Scholar]
- 15.Rockwood K, Mitnitski A, Song X, et al. Long-term risks of death and institutionalization of elderly people in relation to deficit accumulation at age 70. J Am Geriatr Soc. 2006;54:975–979. doi: 10.1111/j.1532-5415.2006.00738.x. [DOI] [PubMed] [Google Scholar]
- 16.Abellan van Kan G, Rolland YM, Morley JE, Vellas B. Frailty: Toward a clinical definition. J Am Med Dir Assoc. 2008;9:71–72. doi: 10.1016/j.jamda.2007.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Abellan van Kan G, Rolland Y, Bergman H, et al. The I.A.N.A. Task Force on Frailty assessment of older people in clinical practice. J Nutr Health Aging. 2008;12:29–37. doi: 10.1007/BF02982161. [DOI] [PubMed] [Google Scholar]
- 18.Romero-Ortuno R. The Frailty Instrument of the Survey of Health, Ageing and Retirement in Europe (SHARE-FI) predicts mortality beyond age, comorbidities, disability, self-rated health, education and depression. Eur Geriatr Med. 2011;2:323–326. doi: 10.1016/j.eurger.2011.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Romero-Ortuno R, Walsh CD, Lawlor BA, Kenny RA. A frailty instrument for primary care: Findings from the Survey of Health, Ageing and Retirement in Europe (SHARE) BMC Geriatr. 2010;10:57. doi: 10.1186/1471-2318-10-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Min LC, Elliott MN, Wenger NS, Saliba D. Higher vulnerable elders survey scores predict death and functional decline in vulnerable older people. J Am Geriatr Soc. 2006;54:507–511. doi: 10.1111/j.1532-5415.2005.00615.x. [DOI] [PubMed] [Google Scholar]
- 21.Min L, Yoon W, Mariano J, et al. The vulnerable elders-13 survey predicts 5-year functional decline and mortality outcomes in older ambulatory care patients. J Am Geriatr Soc. 2009;57:2070–2076. doi: 10.1111/j.1532-5415.2009.02497.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Biganzoli L, Boni L, Becheri D, et al. Evaluation of the cardiovascular health study (CHS) instrument and the Vulnerable Elders Survey-13 (VES-13) in elderly cancer patients. Are we still missing the right screening tool? Ann Oncol. 2013;24:494–500. doi: 10.1093/annonc/mds331. [DOI] [PubMed] [Google Scholar]
- 23.Gobbens RJ, van Assen MA, Luijkx KG, et al. The Tilberg Frailty Indicator: Psychometric properties. J Am Med Dir Assoc. 2010;11:344–355. doi: 10.1016/j.jamda.2009.11.003. [DOI] [PubMed] [Google Scholar]
- 24.Gobbens RJ, van Assen MA, Luijkx KG, et al. Determinants of frailty. J Am Med Dir Assoc. 2010;11:356–364. doi: 10.1016/j.jamda.2009.11.008. [DOI] [PubMed] [Google Scholar]
- 25.Peters LL, Boter H, Buskens E, Slaets JP. Measurement properties of the Groningen Frailty Indicator in home-dwelling and institutionalized elderly people. J Am Med Dir Assoc. 2012;13:546–551. doi: 10.1016/j.jamda.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 26.Hoogendijk EO, van Hout HP. Investigating measurement properties of the Groningen Frailty Indicator: A more systematic approach is needed. J Am Med Dir Assoc. 2012;13:757. doi: 10.1016/j.jamda.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 27.Morley JE, Abbatecola AM, Argiles JM, et al. Sarcopenia with limited mobility: An international consensus. J Am Med Dir Assoc. 2011;12:403–409. doi: 10.1016/j.jamda.2011.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fielding RA, Vellas B, Evans WJ, et al. Sarcopenia: An undiagnosed condition in older adults. Current consensus definition: Prevalence, etiology, and consequences. International Working Group on Sarcopenia. J Am Med Dir Assoc. 2011;12:249–256. doi: 10.1016/j.jamda.2011.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Muscaritoli M, Anker SD, Argiles J, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: Joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting disease” and “nutrition in Geriatrics. Clin Nutr. 2010;29:154–159. doi: 10.1016/j.clnu.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing. 2010;39:412–423. doi: 10.1093/ageing/afq034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Von Haehling S, Morley JE, Anker SD. From muscle wasting to sarcopenia and myopenia: Update 2012. J Cachexia Sarcopenia Muscle. 2012;3:213–217. doi: 10.1007/s13539-012-0089-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Morley JE. Developing novel therapeutic approaches to frailty. Curr Pharm Des. 2009;15:3384–3395. doi: 10.2174/138161209789105045. [DOI] [PubMed] [Google Scholar]
- 33.Lacas A, Rockwood K. Frailty in primary care: A review of its conceptualization and implications for practice. BMC Med. 2012;10:4. doi: 10.1186/1741-7015-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pialoux T, Goyard J, Lesourd B. Screening tools for frailty in primary health care: A systematic review. Geriatr Gerontol Int. 2012;12:189–197. doi: 10.1111/j.1447-0594.2011.00797.x. [DOI] [PubMed] [Google Scholar]
- 35.Sternberg SA, Wershof Schwartz A, Karunananthan S, et al. The identification of frailty: A systematic literature review. J Am Geriatr Soc. 2011;59:2129–2138. doi: 10.1111/j.1532-5415.2011.03597.x. [DOI] [PubMed] [Google Scholar]
- 36.Hubbard RE, Rockwood K. Frailty in older women. Maturitas. 2011;69:203–207. doi: 10.1016/j.maturitas.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 37.Pijpers E, Ferreira I, Stehouwer CD, et al. The frailty dilemma. Review of the predictive accuracy of major frailty scores. Eur J Intern Med. 2012;23:118–123. doi: 10.1016/j.ejim.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 38.Morley JE. Frailty: Diagnosis and management. J Nutr Health Aging. 2011;15:667–670. doi: 10.1007/s12603-011-0338-4. [DOI] [PubMed] [Google Scholar]
- 39.Shamliyan T, Talley KM, Ramakrishnan R, Kane RL. Association of frailty with survival: A systematic literature review. Ageing Res Rev. 2012 Mar 12; doi: 10.1016/j.arr.2012.03.001. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 40.Tinetti ME, Fried TR, Boyd CM. Designing health care for the most common chronic condition—multimorbidity. JAMA. 2012;307:2493–2494. doi: 10.1001/jama.2012.5265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–495. doi: 10.1503/cmaj.050051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Royal College of Physicians. [Accessed December 20, 2012];Acute Care Toolkit 3: Acute Medical Care for Frail Older people. 2012 Mar; Available at: http://www.rcplondon.ac.uk/sites/default/files/acute-care-toolkit-3.pdf.
- 43.Rolland Y, Benetos A, Gentric A, et al. Frailty in older population: A brief position paper from the French society of geriatrics and gerontology. Geriatr Psychol Neuropsychiatr Vieil. 2011;9:387–390. doi: 10.1684/pnv.2011.0311. [DOI] [PubMed] [Google Scholar]
- 44.Hyde Z, Flicker L, Almeida OP, et al. Low free testosterone predicts frailty in older men: The Health in Men study. J Clin Endocrinol Metab. 2010;95:3165–3172. doi: 10.1210/jc.2009-2754. [DOI] [PubMed] [Google Scholar]
- 45.Lopez D, Flicker L, Dobson A. Validation of the frail scale in a cohort of older Australian women. J Am Geriatr Soc. 2012;60:171–173. doi: 10.1111/j.1532-5415.2011.03746.x. [DOI] [PubMed] [Google Scholar]
- 46.Morley JE, Malmstrom TK, Miller DK. A simple frailty questionnaire (FRAIL) predicts outcomes in middle aged African Americans. J Nutr Health Aging. 2012;16:601–608. doi: 10.1007/s12603-012-0084-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Woo J, Leung J, Morley JE. Comparison of frailty indicators based on clinical phenotype and the multiple deficit approach in predicting mortality and physical limitation. J Am Geriatr Soc. 2012;60:1478–1486. doi: 10.1111/j.1532-5415.2012.04074.x. [DOI] [PubMed] [Google Scholar]
- 48.Subra J, Gillette-Guyonnet S, Cesari M, et al. The integration of frailty into clinical practice: Preliminary results from the Gérontopôle. J Nutr Health Aging. 2012;16:714–720. doi: 10.1007/s12603-012-0391-7. [DOI] [PubMed] [Google Scholar]
- 49.Singh NA, Quine S, Clemson LM, et al. Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: A randomized controlled trial. J Am Med Dir Assoc. 2012;13:24–30. doi: 10.1016/j.jamda.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 50.Yamada M, Arai H, Sonoda T, Aoyama T. Community-based exercise program is cost-effective by preventing care and disability in Japanese frail older adults. J Am Med Dir Assoc. 2012;13:507–511. doi: 10.1016/j.jamda.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 51.Theou O, Stathokostas L, Roland KP, et al. The effectiveness of exercise interventions for the management of frailty: A systematic review. J Aging Res. 2011;2011:569194. doi: 10.4061/2011/569194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;(9):CD007146. doi: 10.1002/14651858.CD007146.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Landi F, Laviano A, Cruz-Jentoft AJ. The anorexia of aging: Is it a geriatric syndrome? J Am Med Dir Assoc. 2010;11:153–156. doi: 10.1016/j.jamda.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 54.Morley JE. Undernutrition: A major problem in nursing homes. J Am Med Dir Assoc. 2011;12:243–246. doi: 10.1016/j.jamda.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 55.Morley JE. Weight loss in older persons: New therapeutic approaches. Curr Pharm Des. 2007;13:3637–3647. doi: 10.2174/138161207782794149. [DOI] [PubMed] [Google Scholar]
- 56.Milne AC, Potter J, Vivanti A, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev. 2009;(2):CD003288. doi: 10.1002/14651858.CD003288.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.van Wetering CR, Hoogendoorn M, Broekhuizen R, et al. Efficacy and costs of nutritional rehabilitation in muscle-wasted patients with chronic obstructive pulmonary disease in a community-based setting: A prespecified subgroup analysis of the INTERCOM trial. J Am Med Dir Assoc. 2010;11:179–187. doi: 10.1016/j.jamda.2009.12.083. [DOI] [PubMed] [Google Scholar]
- 58.Neelemat F, Bosmans JE, Thijs A, et al. Post-discharge nutritional support in malnourished elderly individuals improves functional limitations. J Am Med Dir Assoc. 2011;12:295–301. doi: 10.1016/j.jamda.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 59.Morley ME, Argiles JM, Evans WJ, et al. Nutritional recommendations for the management of sarcopenia. J Am Med Dir Assoc. 2010;11:391–396. doi: 10.1016/j.jamda.2010.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tieland M, van de Rest O, Dirks ML, et al. Protein supplementation improves physical performance in frail elderly people: A randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2012;13:720–726. doi: 10.1016/j.jamda.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 61.Volpi E, Campbell WW, Dwyer JT, et al. Is the optimal level of protein intake for older adults greater than the recommended dietary allowance? J Gerontol A Biol Sci Med Sci. 2012 Nov 26; doi: 10.1093/gerona/gls229. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Paddon-Jones D. Perspective: Exercise and protein supplementation in frail elders. J Am Med Dir Assoc. 2013;14:73–74. doi: 10.1016/j.jamda.2012.09.028. [DOI] [PubMed] [Google Scholar]
- 63.Malafarina V, Uriz-Otano F, Iniesta R, Gil-Guerrero L. Effectiveness of nutritional supplementation on muscle mass in treatment of sarcopenia in old age: A systematic review. J Am Med Dir Assoc. 2013;14:10–17. doi: 10.1016/j.jamda.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 64.Tieland M, Dirks ML, van der Zwaluw N, et al. Protein supplementation increases muscle mass gain during prolonged resistance-type exercise training in frail elderly people: A randomized, double-blind, placebo-controlled trial. J Am Med Dir Assoc. 2012;13:713–719. doi: 10.1016/j.jamda.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 65.Morley JE. Do frail older persons need more protein? J Am Med Dir Assoc. 2012;13:667–668. doi: 10.1016/j.jamda.2012.07.014. [DOI] [PubMed] [Google Scholar]
- 66.Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev. 2012;11:278–296. doi: 10.1016/j.arr.2011.12.008. [DOI] [PubMed] [Google Scholar]
- 67.Waters DL, Vawter R, Qualls C, et al. Long-term maintenance of weight loss after lifestyle intervention in frail, obese older adults. J Nutr Health Aging. 2013;17:3–7. doi: 10.1007/s12603-012-0421-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Murad MH, Elamin KB, Abu Elnour NO, et al. Clinical review: The effect of vitamin D on falls: A systematic review and meta-analysis. J Clin Endocrinol Metab. 2011;96:2997–3006. doi: 10.1210/jc.2011-1193. [DOI] [PubMed] [Google Scholar]
- 69.Bischoff-Ferrari HA, Willett WC, Orav EJ, et al. A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med. 2012;567:40–49. doi: 10.1056/NEJMoa1109617. [DOI] [PubMed] [Google Scholar]
- 70.Rejnmark L, Avenell A, Masud T, et al. Vitamin D with calcium reduces mortality: Patient level pooled analysis of 70,528 patients from eight major vitamin D trials. J Clin Endocrinol Metab. 2012;97:2670–2681. doi: 10.1210/jc.2011-3328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Muir SW, Montero-Odasso M. Effect of vitamin D supplementation on muscle strength, gait and balance in older adults: A systematic review and meta-analysis. J Am Geriatr Soc. 2011;59:2291–2300. doi: 10.1111/j.1532-5415.2011.03733.x. [DOI] [PubMed] [Google Scholar]
- 72.Rolland Y, Onder G, Morley JE, et al. Current and future pharmacologic treatment of sarcopenia. Clin Geriatr Med. 2011;27:423–447. doi: 10.1016/j.cger.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 73.Sukuma K, Yamaguchi A. Molecular mechanisms in aging and current strategies to counteract sarcopenia. Curr Aging Sci. 2010;3:90–101. doi: 10.2174/1874609811003020090. [DOI] [PubMed] [Google Scholar]
- 74.Gnjidic D, Hilmer SN, Blyth FM, et al. Polypharmacy cutoff and outcomes: Five or more medicines were used to identify community-dwelling older men at risk of different adverse outcomes. J Clin Epidemiol. 2012;65:989–995. doi: 10.1016/j.jclinepi.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 75.Flaherty JH, Perry HM, 3rd, Lynchard GS, Morley JE. Polypharmacy and hospitalization among older home care patients. J Gerontol A Biol Sci Med Sci. 2000;55:M554–M559. doi: 10.1093/gerona/55.10.m554. [DOI] [PubMed] [Google Scholar]
- 76.Rockwood K. Medical management of frailty: Confessions of a gnostic. CMAJ. 1997;157:1081–1084. [PMC free article] [PubMed] [Google Scholar]
- 77.Bronskill SE, Gill SS, Paterson JM, et al. Exploring variation in rates of polypharmacy across long term care homes. J Am Med Dir Assoc. 2012;13:309.e15–309.e21. doi: 10.1016/j.jamda.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 78.Gokce Kutsal Y, Barak A, Atalay A, et al. Polypharmacy in the elderly: A multicenter study. J Am Med Dir Assoc. 2009;10:486–490. doi: 10.1016/j.jamda.2009.03.018. [DOI] [PubMed] [Google Scholar]
- 79.Kojima G, Bell C, Tamura B, et al. Reducing cost by reducing polypharmacy: The polypharmacy outcomes project. J Am Med Dir Assoc. 2012;13:818.e11–818. e15. doi: 10.1016/j.jamda.2012.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Fitzgerald SP, Bean NG. An analysis of the interactions between individual comorbidities and their treatments—implications for guidelines and polypharmacy. J Am Med Dir Assoc. 2010;11:475–484. doi: 10.1016/j.jamda.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 81.Tamura BK, Bell CL, Lubimir K, et al. Physician intervention for medication reduction in a nursing home: The polypharmacy outcomes project. J Am Med Dir Assoc. 2011;12:326–330. doi: 10.1016/j.jamda.2010.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Morley JE. Polypharmacy in the nursing home. J Am Med Dir Assoc. 2009;10:289–291. doi: 10.1016/j.jamda.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 83.Merle L, Laroche ML, Dantoine T, Charmes JP. Predicting and preventing adverse drug reactions in the very old. Drugs Aging. 2006;22:375–392. doi: 10.2165/00002512-200522050-00003. [DOI] [PubMed] [Google Scholar]
- 84.Resnick B, Pacala JT. 2012 Beers Criteria. J Am Geriatr Soc. 2012;60:612–613. doi: 10.1111/j.1532-5415.2012.03921.x. [DOI] [PubMed] [Google Scholar]
- 85.Gallagher P, Ryan C, Byrne S, et al. STOPP (Screening Tool of Older Person’s Prescription) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation. Int J Clin Pharmacol Ther. 2008;46:72–83. doi: 10.5414/cpp46072. [DOI] [PubMed] [Google Scholar]
- 86.Pyszka LL, Seys Ranola TM, Milhans SM. Identification of inappropriate prescribing in geriatrics at a Veterans Affairs hospital using STOPP/START screening tools. Consult Pharm. 2010;25:365–373. doi: 10.4140/TCP.n.2010.365. [DOI] [PubMed] [Google Scholar]
- 87.Theou O, Rockwood K. Should frailty status always be considered when treating the elderly patient? Aging Health. 2012;8:261–271. [Google Scholar]
- 88.Espinoza S, Walston JD. Frailty in older adults: Insights and interventions. Cleve Clin J Med. 2005;72:1105–1112. doi: 10.3949/ccjm.72.12.1105. [DOI] [PubMed] [Google Scholar]
- 89.Vellas B, Cestac P, Morley JE. Implementing frailty into clinical practice: We cannot wait. J Nutr Health Aging. 2012;16:599–600. doi: 10.1007/s12603-012-0096-y. [DOI] [PubMed] [Google Scholar]
- 90.Ogawa K, Fujiwara Y, Yoshida H, et al. The validity of the “Kihon Checklist” as an index of frailty and its biomarkers and inflammatory markers in elderly people. Nihon Ronen Igakkai Zasshi. 2011;48:545–552. doi: 10.3143/geriatrics.48.545. Japanese. [DOI] [PubMed] [Google Scholar]
- 91.Tomata Y, Hozawa A, Ohmori-Matsuda K, et al. Validation of the Kihon Checklist for predicting the risk of 1-year incident long term care insurance certification: The Ohsaki Cohort 2006 Study. Nihon Koshu Eisei Zasshi. 2011;58:3–13. Japanese. [PubMed] [Google Scholar]
- 92.Fukutomi E, Okumiya K, Wada T, et al. Importance of cognitive assessment as part of the “Kihon Checklist” developed by the Japanese Ministry of Health, Labor and Welfare for prediction of frailty at a 2-year follow up. Geriatr Gerontol Int. 2012 Nov 22; doi: 10.1111/j.1447-0594.2012.00959.x. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 93.Afilalo J. Frailty in patients with cardiovascular disease: Why, when and how to measure. Curr Cardiovasc Risk Rep. 2011;5:467–472. doi: 10.1007/s12170-011-0186-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ruiz M, Reske T, Cefalu C, Estrada J. Management of elderly and frail elderly patients: The importance of comprehensive geriatrics assessment and the need for guidelines. Am J Med Sci. 2012 Nov 17; doi: 10.1097/MAJ.0b013e31826d59aa. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 95.Shilpak MG, Stehman-Breen C, Fried LF, et al. The presence of frailty in elderly persons with chronic renal insufficiency. Am J Kidney Dis. 2004;43:861–867. doi: 10.1053/j.ajkd.2003.12.049. [DOI] [PubMed] [Google Scholar]
- 96.Desquilbet L, Jacobson LP, Fried LP, et al. HIV-1 infection is associated with an earlier occurrence of a phenotype related to frailty. J Gerontol A Biol Sci Med Sci. 2007;62:1279–1286. doi: 10.1093/gerona/62.11.1279. [DOI] [PubMed] [Google Scholar]
- 97.Sinclair A, Morley JE, Rodriguez-Mañas L, et al. Diabetes mellitus in older people: Position statement on behalf of the International Association of Gerontology and Geriatrics (IAGG), the European Diabetes Working Party for Older People (EDWPOP), and the International Task Force of Experts in Diabetes. J Am Med Dir Assoc. 2012;13:497–502. doi: 10.1016/j.jamda.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 98.Partridge JS, Harari D, Dhesi JK. Frailty in the older surgical patient: A review. Age Ageing. 2012;41:142–147. doi: 10.1093/ageing/afr182. [DOI] [PubMed] [Google Scholar]