Abstract
Purpose of review
Hand hygiene and isolation are basic, but very effective, means of preventing the spread of pathogens in healthcare. Although the principle may be straightforward, this review highlights some of the controversies regarding the implementation and efficacy of these interventions.
Recent findings
Hand hygiene compliance is an accepted measure of quality and safety in many countries. The evidence for the efficacy of hand hygiene in directly reducing rates of hospital-acquired infections has strengthened in recent years, particularly in terms of reduced rates of staphylococcal sepsis. Defining the key components of effective implementation strategies and the ideal method(s) of assessing hand hygiene compliance are dependent on a range of factors associated with the healthcare system. Although patient isolation continues to be an important strategy, particularly in outbreaks, it also has some limitations and can be associated with negative effects. Recent detailed molecular epidemiology studies of key healthcare-acquired pathogens have questioned the true efficacy of isolation, alone as an effective method for the routine prevention of disease transmission.
Summary
Hand hygiene and isolation are key components of basic infection control. Recent insights into the benefits, limitations and even adverse effects of these interventions are important for their optimal implementation.
Keywords: alcohol-based hand rub, hand hygiene, hospital acquired infections, isolation, WHO
INTRODUCTION
Hand hygiene and patient isolation are two basic principles that have long been recognized as effective methods of reducing hospital-acquired infections. However, the optimal methods for implementation and monitoring of such programmes are not straightforward.
The WHO Global Patient Safety Challenge: ‘Clean Care is Safer Care’ campaign was launched in 2005 with the aim of reducing healthcare-associated infections worldwide [1]. Consensus guidelines on hand hygiene in healthcare were subsequently published in 2009 [2,3] after the early success of the WHO hand hygiene multimodal implementation strategy and toolkit [4,5▪▪,6]. Ongoing research and experience from other programmes worldwide is helping in guiding the optimal implementation of these interventions.
Recent experience with emerging infectious diseases has highlighted the role of isolation in outbreak settings. However, new studies have also emphasized the limitations, and even negative effects, of isolation under certain circumstances.
THE CLINICAL IMPACT OF HAND HYGIENE PROGRAMMES
Since the early initiatives by the WHO, hand hygiene campaigns have been initiated worldwide [7,8,9▪]. The countries participating in the WHO CleanHandsNet [10], a global network of coordinators or leaders involved in the promotion of hand hygiene in healthcare, are shown in Fig. 1. In many countries, hand hygiene has been incorporated as a measure of quality of care at the national or subnational level [11▪,12▪].
FIGURE 1.

Map of current participants of the WHO CleanHandsNet.
Box 1.
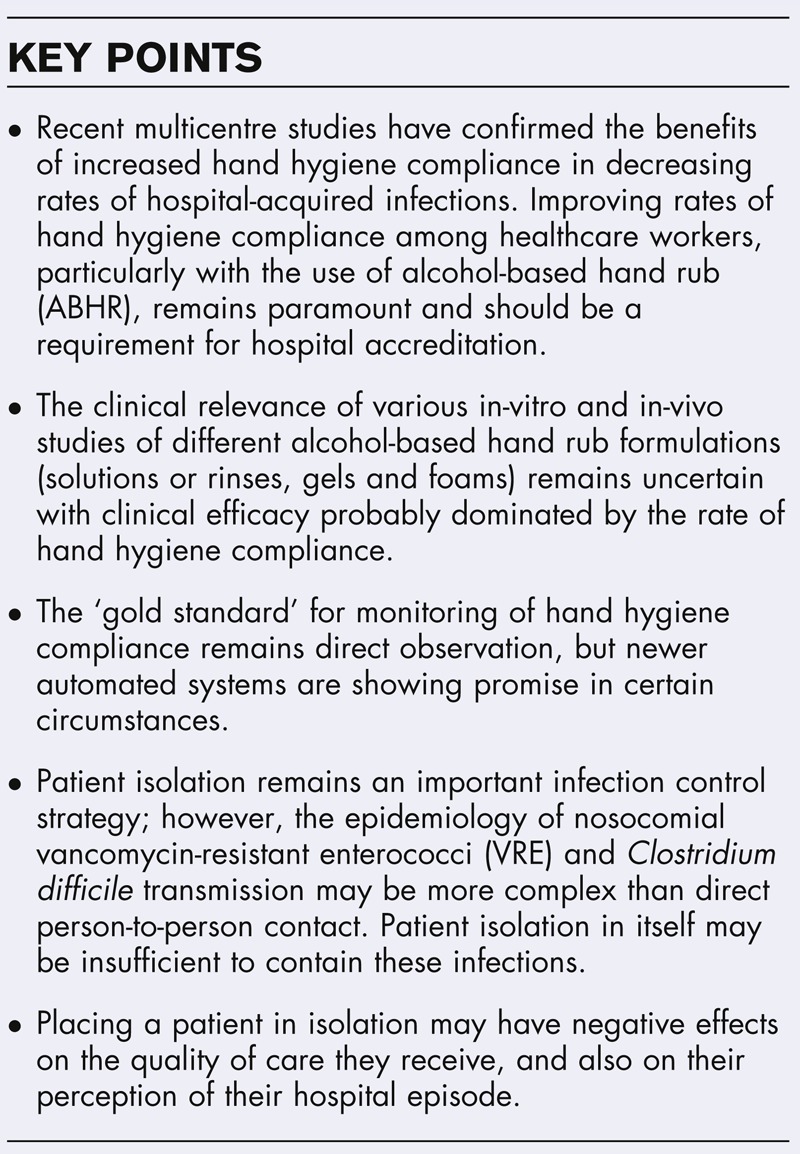
no caption available
Until recently, the preponderance of data demonstrating the clinical benefits of improved hand hygiene compliance came from single-centre or multicentre before-and-after studies [13–15], including the landmark study from Pittet et al.[16]. In the last few years, the clinical evidence for hand hygiene has strengthened in two ways. First, the outcomes of several major national and subnational programmes have been reported [17–20]. Second, a number of recent studies have incorporated more advanced study designs in their assessment of hand hygiene efficacy.
The Cleanyourhands campaign was instituted in all acute National Health Service (NHS) hospital trusts in England and Wales commencing in 2004. In the first 4 years of this initiative, rates of Clostridium difficile and methicillin-resistant Staphylococcus aureus (MRSA) bacteraemia declined significantly [18]. In addition, when consumption of hand hygiene products by individual trust was reviewed, procurement of soap was independently associated with reduction in C. difficile rates, and alcohol-based hand rub (ABHR) was independently associated with reduction in MRSA bacteraemia, although only in the last four quarters of the study period. Notably (and somewhat disappointingly), formal surveillance of hand hygiene compliance rates was not assessed, with consumption data used as a surrogate for compliance.
The Australian National Hand Hygiene Initiative (NHHI) commenced in 2009, following a number of successful state-based programmes, which were associated with reductions in rates of MRSA bacteraemia [13,21,22]. The aim was to implement a standardized hand hygiene culture change programme on the basis of the WHO multimodal hand hygiene improvement strategy throughout all Australian public and private hospitals. Hand hygiene compliance increased from 63.6 to 68.3% in the first 2 years of this programme [17]. The NHHI now involves data submission from more than 740 hospitals three times annually, with the national hand hygiene compliance rate improving to 79% in late 2013 [12▪]. Public reporting of hand hygiene compliance and healthcare-associated S. aureus bacteraemia (SAB) rates for individual hospitals is a mandatory component of Federal Government hospital accreditation [12▪,23]. Subsequently, the national rates of healthcare-associated SAB have continued to decrease [24].
Although these longitudinal studies demonstrate a temporal relationship between increases in hand hygiene compliance and reductions in hospital acquired infection rates, few controlled, prospective studies have been performed until recently. Two multicentre cluster-randomized trials conducted in long-term care facilities in Hong Kong demonstrated the efficacy of multimodal interventions in both improving hand hygiene compliance, and reducing infection rates (respiratory outbreaks or infections requiring hospitalization) [25,26].
In comparison, a single-centre cluster-randomized trial (RCT) in Canada failed to demonstrate a reduction in hospital-acquired MRSA colonization in their hand hygiene intervention arm compared with the control arm [27]. However, this was not unexpected, as hand hygiene adherence improved in both the intervention arm (15.9–48.2%) and the control arm (15.9–42.6%) during the intervention. This ‘contamination’ of the control group demonstrates one of the challenges of implementing a randomized controlled study involving behaviour change within a single institution. To improve on the simple before-and-after study design, Kirkland et al.[28] performed an interrupted time-series study in which interventions were introduced sequentially at a rural hospital in New Hampshire to provide insights into the temporal associations between interventions, hand hygiene performance and clinical outcomes. Notably, they observed that although improvement in hand hygiene was temporally associated with a significant decline in healthcare-associated infections, there was an increase in (nonclonal) S. aureus infections attributable to the operating room (where improvements in routine hand hygiene would not be expected to impact).
Lee et al.[29▪▪] recently published an ambitious prospective, multicentre, interventional cohort study comparing interventions aimed at reducing rates of MRSA clinical isolates across 10 hospitals in Europe. Hospitals were assigned to enhanced hand hygiene (using the WHO multimodal hand hygiene promotion programme), screening for colonization with contact precautions and decolonization (if needed), or both. The individual interventions were not effective in reducing MRSA rates during the study period. However, the combination of hand hygiene promotion and target screening resulted in a reduction of MRSA isolates of 12% per month. Importantly, these hospitals had relatively low baseline rates of MRSA infection – thus, whether these findings can be generalized to other settings with high MRSA rates is less clear. Furthermore, the brief intervention period of only 12 months may have contributed to the failure of enhanced hygiene to reduce MRSA rates, as a number of studies have demonstrated a time lag between hand hygiene improvement and changes in infection rates [16,18,28].
WHAT IS THE OPTIMAL APPROACH TO IMPROVING HAND HYGIENE COMPLIANCE?
Allegranzi et al.[5▪▪] recently reported a quasiexperimental study to assess the effect of the WHO multimodal hand hygiene promotion programme on hand hygiene compliance and healthcare worker knowledge at six sites in Costa Rica, Italy, Mali, Pakistan and Saudi Arabia. Implementation of the WHO strategy led to an improvement in hand hygiene compliance from 51% to 67.2%, with healthcare worker knowledge about hand hygiene and infection prevention also improving. After adjustment for key confounders, the intervention was significantly associated with improved hand hygiene compliance (adjusted odds ratio 2.15, 95% confidence interval 1.99–2.32). This study represents an important proof of concept for the WHO multimodal strategy, demonstrating that it can be successfully implemented in a diverse range of clinical and socio-economic settings.
Which components of the WHO multimodal strategy are the most important and how they should be combined for optimal impact remains uncertain. Schweizer et al.[30▪▪] addressed this issue in a recent meta-analysis of hand hygiene promotion interventions. Importantly, this meta-analysis differed from the earlier Cochrane review [31] by including quasiexperimental studies – a pragmatic decision that has particular importance in the field of infection control and quality improvement in which randomized controlled studies are particularly challenging, and often unfeasible. Thus, 46 studies (including six randomized controlled trials) were included [30▪▪]. This analysis suggested that two bundled interventions were associated with an increase in hand hygiene compliance – namely, the WHO bundle comprising feedback, education, reminders, access to ABHR and administrative support [3], and a bundle that only included feedback, education and reminders (although, healthcare settings using the later approach almost certainly had preexisting access to ABHR). Pooled effect measures for these two interventions were calculated, further supporting the impact of the WHO multimodal strategy.
The Feedback Intervention Trial (FIT) [32] used a stepped wedge cluster randomized controlled trial design conducted across 16 trusts in the United Kingdom to evaluate the impact of feedback at group and individual levels. The intervention was designed using goal setting, control and operant learning theories. In the intention to treat analysis, hand hygiene compliance rose postrandomization (odds ratio 1.44; 95% CI 1.18, 1.76; P < 0.001) in the intensive therapy units, but not aged care wards.
The use of personality profiling techniques, similar to those routinely used in advertising to better determine and target the most effective hand hygiene education strategies for various healthcare workers, has undergone preliminary assessment in Australia [33] and will be used in a forthcoming multicentre trial to improve hand hygiene compliance.
ASSESSING THE ACCURACY OF VARIOUS APPROACHES TO HAND HYGIENE SURVEILLANCE
Approaches to the monitoring of hand hygiene include direct observation, self-reporting, measurement of product consumption and use of various automated devices; each approach has strengths and weaknesses [34]. Although no method is ideal, direct monitoring is generally considered the gold standard, although limitations include resource intensity, observer bias and the potential of a Hawthorne effect [35,36]. In fact, multiple factors can affect results (Table 1), including the type of hand hygiene compliance audit tool used. Use of a standardized tool, such as the WHO 5 Moments tool, allows valid comparability between sites, although standardization of assessors and wards surveyed requires careful attention [37]. For example, approximately 80% of the current Hand Hygiene Australia (HHA) budget is required solely to maintain appropriate auditor (and therefore data) standardization to allow valid interhospital comparisons (Grayson ML, personal communication). Standardized hand hygiene auditing tools for nonacute settings, such as long-term care facilities, day surgical centres and psychiatry units, need to be defined and validated. When various surveillance methodologies have been directly compared [38–40], there has not always been a strong correlation. Table 2 summarizes the monitoring methods used in recent publications on hand hygiene programmes [41,42▪,43–45].
Table 1.
Factors affecting the validity and comparability of hand hygiene compliance rates in healthcare
| Variables | Options | Comments | |
| Strengths | Weaknesses | ||
| Hand hygiene audit tool | WHO 5 Moment | Validated | Specific auditor training required |
| Risk-stratifies hand hygiene contacts (in terms of whether a procedure is being performed or there is body-fluid contact) | Developed for routine ward use; may not be ideal for ICU | ||
| Allows national and international comparisons | |||
| Before and after patient room entry | Easy to teach | Nonvalidated | |
| Auditors are not required to enter patient rooms | Does not risk stratify hand hygiene contacts | ||
| Is the basis of many automated compliance audit systems | Limited interhospital comparisons | ||
| Locally developed tools | Associated with local engagement | Nonvalidated | |
| Tool can be tailored to local practices | Usually no risk stratification | ||
| Interhospital comparisons invalid | |||
| Auditing of hand hygiene ‘Opportunities’ vs. ‘Moments’ | ‘Opportunities’ are clinically logical compared with ‘Moments’, but auditing ‘Moments’ is easier to teach for a national programme and more easily validated | ||
| Ward selection | Multibed wards vs. single rooms | Difficult to audit hand hygiene compliance in single-bed wards without high risk of Hawthorne effect | |
| General ward vs. ICU | Most audit tools are not specifically designed for ICU and may under-estimate the true hand hygiene compliance | ||
| Glove use | Glove use often recommended in many isolation protocols | High rates of glove use often associated with lower rates of hand hygiene compliance and cross-transmission in multibed wards | |
| Auditing in acute vs. subacute healthcare facilities | Acute-care facilities | Consequences of pathogen cross-transmission is high – thus improved hand hygiene compliance likely to have a large beneficial impact | |
| Subacute facilities (e.g., long-term care facilities) | Since high rates of cross-transmission likely, infection control interventions may assist | Role of poor hand hygiene compliance in cross-transmission uncertain | |
| Most hand hygiene audit tools are not designed for subacute settings | |||
Table 2.
Recent publications on hand hygiene (HH) programmes and reported methods of monitoring of HH compliance
| Reference | Involved sites | Method of hand hygiene compliance surveillance or other outcome measures | Direct observation method (if used) |
| Allegranzi et al. [5▪▪] | Six pilot sites across Costa Rica, Italy, Mali, Pakistan and Saudi Arabia | Direct observation | 5 Moments |
| Questionnaire on knowledge of health care workers | |||
| Allegranzi et al. [9▪] | 168 facilities across the USA | 76.1% direct observation at least every 3 months | Primarily room entry and exit although numbers not specified |
| 39.8% ABHR consumption | |||
| 34.1% soap consumption | |||
| Fuller et al. [32] | 16 acute hospitals in England and Wales | Direct observation | Hand Hygiene Observation Tool (HHOT) [41] |
| Consumption of hand hygiene products | |||
| Grayson et al. [17] | National programme in Australia | Direct observation | 5 Moments |
| Jarlier et al. [19] | 38 teaching hospitals in France | Consumption of hand hygiene products | |
| Kirkland et al. [28] | Single centre in the USA | Direct observation | ‘Before-and-after contact with patients or their immediate environments’ |
| Latham et al. [11▪] | Evaluations of 18 hand hygiene campaigns across the European Union and European Economic Area Member States | 70% direct observation | Not specified |
| 33% consumption of HH products | |||
| 10% availability of ABHR | |||
| 10% questionnaire | |||
| 20% self assessment survey | |||
| Reichardt et al. [42▪] | German national programme | Direct observation in 180 of >700 hospitals | 5 Moments |
| Consumption of hand hygiene products | |||
| Reisinger et al. [43] | Veterans Health Administration encompassing 141 medical centres in the USA | 98.6% direct observation | A variety of moments observed, most often room entry and exit |
| 22.7% consumption of hand hygiene products | 41.4% reported monitoring ‘5 Moments’ in addition to other opportunities | ||
| 2.8% automated monitoring systems | |||
| Salmon et al. [44] | Single centre in Vietnam | Direct observation | |
| Consumption of hand hygiene products | |||
| Stone et al. [18] | 187 acute trusts in England and Wales | Consumption of hand hygiene products | |
| Schweizer et al. [30▪▪] | Meta analysis of 45 hand hygiene intervention bundles worldwide | 86.6% direct observation | Variety of methods utilized most commonly ‘5 Moments’, room entry and exit, before and after patient contact, or unspecified |
| 13.3% consumption of hand hygiene products | |||
| 4.4 % video surveillance | |||
| 11.1% automated monitoring systems | |||
| Szilagyi et al. [45] | Single centre in Singapore | Evaluation of HH technique |
ABHR, alcohol-based hand rub.
Measuring consumption of ABHR as a surrogate for hand hygiene behaviour has been used widely across Europe [46], including Germany [42▪] and Britain [18]. The benefits of this approach are objectivity, the availability of quantitative data and in some cases, an indication of daily use. However, this measure does not take into account variability in the amount of product used by an individual or differential use by family members and staff. More importantly, consumption data does not take into account the frequency of occasions when hand hygiene should have been performed, nor the appropriateness of ABHR usage. Similar limitations occur when using automated ABHR dispenser counters.
Automated wireless systems for monitoring hand hygiene behaviour are an emerging area of interest [47,48▪▪]. These systems generally involve the healthcare worker carrying an electronic identifying badge or tag, with sensors installed at various locations in the healthcare setting to record use of ABHR by individual healthcare workers. Several recent studies have evaluated these systems, reporting varying levels of accuracy [49–51]. Nevertheless, some systems provide an automated mechanism for performance feedback, which may assist individuals in improving compliance. Second, they may be useful in single rooms in which direct unobtrusive observation may be impractical. Unfortunately, current systems are unable to detect all WHO 5 Moments, and significant financial investment is generally required if an institution commits to one of these systems.
HAND HYGIENE PREPARATIONS AND THEIR COMPARABLE EFFICACY
Current guidelines recommend the use of ABHR when hands are not visibly soiled, but recommendations vary in terms of the concentration of required alcohol (60–95%), the type of alcohol and the formulation (solution or rinse vs. gel vs. foam) [3,52]. The WHO has created simple formulations for ABHR solutions for use in settings in which commercial products may not be readily available [3].
Factors that can affect results include in-vitro vs. in-vivo testing methodology (e.g., European Norm 1500 vs. ASTM E1174 vs. glove juice techniques), the species and inoculum of pathogens tested, the volume of ABHR utilized and the time between ABHR application and assessment of pathogen kill. Overall, the optimum ABHR formulation has not been clearly established [53–58]. Edmonds et al.[55] evaluated 12 different ABHR formulations and did not find that alcohol content (within the WHO recommended range) influenced efficacy. Contrary to previous reports, gel or foam ABHR preparations were not shown to be inferior to solutions or rinses, although design flaws have subsequently been highlighted with this study [56]. A key issue with all these studies is that they utilize in-vivo models to extrapolate to clinical effectiveness, whereas multiple other factors, including healthcare worker product preference, ease or accuracy of various dispensers and hand hygiene compliance, are also critical factors in this equation. Gels and foams appeared to be equally acceptable to healthcare workers in one study [59], whereas solutions were preferred in others [13,14,16,17].
Novel approaches to hand hygiene, such as nonalcohol-based products [60], cold plasma systems [61] and photodynamic therapy [62], have recently been investigated, but there is insufficient efficacy or safety data to recommend their use.
ALCOHOL-BASED HAND RUB EFFICACY AGAINST SPECIFIC PATHOGENS
A number of ABHR preparations have demonstrated virucidal and bactericidal activity [63,64]. The effectiveness of ABHR against norovirus remains controversial [65]. Although the WHO favours the use of ABHR during norovirus outbreaks [66], the Centre for Disease Control (CDC) continues to recommend handwashing with soap and water [67]. Paulmann et al.[68] recently demonstrated that two WHO ABHR solutions were effective against murine norovirus (a surrogate for human norovirus) both in vitro and in vivo, although the efficacy of other formulations remains unclear. Further research is required in this area. A variety of ABHR formulations appeared to have equivalent efficacy to soap and water handwashing in reducing hand contamination with H1N1 influenza [63]. A study from Taiwan [69▪] demonstrated poor activity of existing ABHR formulations against human enterovirus 71, a nonenveloped virus of public health significance in the Asia-Pacific region.
Despite these in-vivo studies, the clinical utility of ABHR for preventing respiratory virus infections in the community remains less certain. Turner et al.[70] conducted a randomized trial in young adult volunteers on the ability of ABHR to prevent rhinovirus infection or rhinovirus-associated illness. Despite the earlier promise in experimental models [71], they were not able to demonstrate a benefit. Wong et al.[72▪▪] performed a meta-analysis on the efficacy of hand hygiene interventions in preventing influenza virus transmission in the community. Although subgroup analysis from developed countries suggested that a combined intervention of hand hygiene with facemasks is a beneficial strategy, the efficacy of hand hygiene alone was not demonstrated.
It has previously been demonstrated that washing with soap and water is more effective than ABHR in removing C. difficile spores from the hands of healthcare workers [73]. Edmonds et al.[74] evaluated 10 different test products in their ability to remove C. difficile spores from the hands of test subjects. The only substances that were able to achieve significantly higher log10 reductions than tap water were not suitable for routine use in healthcare environments. This reinforces the current recommendation of handwashing with soap and water and contact precautions for care of patients with C. difficile.
One formulation of ABHR (70% isopropanol and 0.5% chlorhexidine) effectively reduced the density of vancomycin-resistant enterococci (VRE) contamination by approximately 104 in a detailed assessment of 20 healthcare workers who had their hands heavily contaminated (108 cfu/ml) with two strains of VRE [75].
CURRENT GUIDELINES ON ISOLATION AND RECENT EXPERIENCES
Guidelines for isolation precautions were published by the Healthcare Infection Control Practices Advisory Committee (HICPAC) in 2007 [76]. Recently, guidelines on the control of multidrug-resistant Gram-negative infections have been published by the European Society of Clinical Microbiology and Infectious Diseases (ESCMID) [77▪▪], the CDC [78] and the Australian Commission on Safety and Quality in Healthcare [79]; all recommend isolation.
Recent experience with emerging pathogens has highlighted the importance of isolation precautions in preventing the spread of various infections during outbreaks. During the severe acute respiratory syndrome (SARS) outbreak in Hong Kong [80], overcrowding of medical wards, suboptimal air processing and inadequate isolation facilities were some of the key factors associated with transmission. Similarly, the description of nosocomial transmission of the Middle East respiratory syndrome (MERS) coronavirus highlighted the importance of isolation precautions in the outbreak setting [81].
During the 2009 influenza A (H1N1) pandemic, Lee et al.[82] conducted a prospective, observational study to evaluate the impact of public health measures in the control of pandemic influenza among military personnel in Singapore. Healthcare workers and military units considered ‘essential’ were subject to additional public health measures, including enhanced surveillance, isolation via home medical leave and segregation. This intervention bundle was effective in decreasing H1N1 pandemic influenza infection with 17% in the ‘essential’ worker cohort developing serologically confirmed infection compared with 44% in the standard cohort.
Finally, the worldwide dissemination of carbapenem-resistant enterobacteriaceae (CRE) has provided some insights into effective infection control strategies. These strategies, usually instituted as bundles, include patient isolation, active surveillance, geographic cohorting, standards for detection and reporting, monitoring of adherence and environmental control initiatives. These bundles have proven to be successful in multiple settings worldwide [83▪,84▪,85,86], with early identification and isolation of asymptomatic carriers appearing to be a key component of successful interventions [85,87].
IS ISOLATION ALWAYS NEEDED OR EFFECTIVE? WHAT ARE THE LIMITATIONS?
Recent progress into the molecular epidemiology of infections due to VRE and C. difficile has provided new insights into modes of pathogen acquisition and the limitations of patient isolation in preventing new infections.
Eyre et al.[88▪▪] performed whole genome sequencing of all C. difficile isolates from symptomatic patients over a 3-year period in Oxfordshire, in the United Kingdom. They found that 45% of the cases were due to transmission from either environmental reservoirs, or transmission from asymptomatic carriers, rather than previous symptomatic hospital cases. Asymptomatic carriage (and presumably shedding) is known to be relatively common [89,90]. These findings support a greater emphasis on improved antimicrobial stewardship to minimize emergence of clinical disease, in addition to prevention of cross-transmission [88▪▪].
The epidemiology of VRE transmission may not be dissimilar. Using large-scale comparative genomics, Howden et al.[91▪] demonstrated that the epidemiology of hospital vanB VRE was more complex than previously thought. They and others [92,93] have proposed a model in which silent circulation of closely related vancomycin-susceptible Enterococcus faecium isolates acquires the vanB operon via lateral gene transfer from anaerobic bacteria in the gastrointestinal tract. Hence, hospital-acquired vanB VRE may also be driven by de-novo generation rather than solely nosocomial transmission via direct contact. This is in keeping with previous work by Johnson et al.[94], in which it was observed within an institution that each time a new vancomycin-resistant E. faecium (VREfm) sequence type appeared, it was observed first as vancomycin-sensitive E. faecium (VSEfm). This may explain why the incidence of VRE has continued to rise in many countries despite strict patient isolation, effective infection control measures and significant reduction rates of nonenteric pathogens, such as MRSA [94,95].
NEGATIVE EFFECTS OF ISOLATION
The potential adverse outcomes of contact precautions have been recently reviewed [96]. In addition, a single-centre retrospective cohort study by Karki et al.[97] compared the incidence rate of documented adverse events in patients before and after initiation of contact precautions for VRE. They found that the overall rate of adverse events was not significantly different, but that there was an increase in medication administration errors and nonpressure-related injuries. The same group also observed that the waiting time for patients to obtain a CT scan, whereas under contact precautions for VRE colonization, was 46% longer than those who were not isolated [98].
In a prospective cohort study by Mehrotra et al.[99], patients who were managed under contact precautions perceived problems with care twice as frequently as those not under precautions. Although this difference may be attributable to bias, it appears that patient perception of care is negatively impacted by isolation.
Dhar et al.[100▪▪] conducted a multicentre, prospective cohort study that evaluated whether the proportion of patients in isolation is a determinant of compliance with contact isolation precautions. They observed a stepwise increase in noncompliance as the overall proportion of patients in isolation in a unit increased, with an apparent ‘tipping point’ when 40% of patients was reached. They hypothesized that at this point ‘compliance fatigue’ became more common, particularly for hand hygiene prior to gloving.
The evidence to support isolation in the intensive care unit is limited. In a 2011 cluster randomized controlled trial involving 10 intensive care units [101], surveillance for MRSA and VRE and expanded barrier precautions for colonized patients was not effective in reducing transmission rates. In a recent post-hoc analysis of a large cohort encompassing three intensive care units, a number of medical errors and adverse events were observed more frequently in the patients under contact isolation [102▪]. This occurred despite the higher staffing ratios in the ICU compared with other wards. Despite these issues, isolation in ICU is still recommended.
CONCLUSION
Hand hygiene and isolation remain key components of the infection control ‘toolkit’ to reduce cross-transmission of key viral and multiresistant bacterial pathogens. Future research should focus on the optimal methods for implementation and monitoring of these strategies as well as ways to mitigate any potential negative effects.
Acknowledgements
None.
Conflicts of interest
None declared.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Pittet D, Donaldson L. Clean Care is Safer Care: a worldwide priority. Lancet 2005; 366:1246–1247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pittet D, Allegranzi B, Boyce J. The World Health Organization guidelines on hand hygiene in healthcare and their consensus recommendations. Infect Control Hosp Epidemiol 2009; 30:611–622 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. WHO guidelines on hand hygiene in healthcare: World Health Organization; 2009; Available from: https://extranet.who.int/iris/restricted/bitstream/10665/44102/1/9789241597906_eng.pdf [Accessed 17 March 2014] [Google Scholar]
- 4.Pittet D, Allegranzi B, Storr J. The WHO Clean Care is Safer Care programme: field-testing to enhance sustainability and spread of hand hygiene improvements. J Infect Public Health 2008; 1:4–10 [DOI] [PubMed] [Google Scholar]
- 5▪▪.Allegranzi B, Gayet-Ageron A, Damani N, et al. Global implementation of WHO's multimodal strategy for improvement of hand hygiene: a quasi-experimental study. Lancet Infect Dis 2013; 13:843–851 [DOI] [PubMed] [Google Scholar]; This quasiexperimental study evaluated the implementation of WHOs multimodal strategy at six pilot sites worlwide. They found the strategy to be feasible, effective and sustainable across a range of diverse settings.
- 6.Stewardson A, Allegranzi B, Perneger T, et al. Testing the WHO hand hygiene self-assessment framework for usability and reliability. J Hosp Infect 2013; 83:30–35 [DOI] [PubMed] [Google Scholar]
- 7.Magiorakos AP, Suetens C, Boyd L, et al. National hand hygiene campaigns in Europe, 2000–2009. Euro Surveill 2009; 14:493–497 [PubMed] [Google Scholar]
- 8.Mathai E, Allegranzi B, Kilpatrick C, et al. Promoting hand hygiene in healthcare through national/subnational campaigns. J Hosp Infect 2011; 77:294–298 [DOI] [PubMed] [Google Scholar]
- 9▪.Allegranzi B, Conway L, Larson E, Pittet D. Status of the implementation of the World Health Organization multimodal hand hygiene strategy in United States of America healthcare facilities. Am J Infect Control 2014; 42:224–230 [DOI] [PMC free article] [PubMed] [Google Scholar]; This study reviewed the results of United States healthcare facilities who completed the hand hygeine self-assessment framework from the WHO. Although only 7.5% of invited facilites responded to the survey, the level of progress was promising, although this may reflect reporting bias.
- 10.World Health Organization. WHO CleanHandsNet – a network of campaigning countries: World Health Organization; 2014; Available from: http://www.who.int/gpsc/national_campaigns/en/ [Accessed 17 March 2014] [Google Scholar]
- 11▪.Latham JR, Magiorakos AP, Monnet DL, et al. The role and utilisation of public health evaluations in Europe: a case study of national hand hygiene campaigns. BMC Public Health 2014; 14:131. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study aimed to assess the proportion of European hand hygiene programmes that had undergone evaluation and the characteristics of those evaluations. Among 36 programmes, 50% had undergone evaluation and they utilized a variety of methologies and indicators pre- and postintervention.
- 12▪.Hand Hygiene Australia. Hand Hygiene Australia: National Data Period Three, 2013: Hand Hygiene Australia; 2013; Available from: http://www.hha.org.au/LatestNationalData.aspx [Accessed 17 March 2014] [Google Scholar]; This website summarizes the key hand hygiene compliance rates for more than 740 Australian acute-care hospitals (95% of all public hospitals and 50% of private hospitals) following the successful implementation of the hand hygiene Australia programme.
- 13.Grayson ML, Jarvie LJ, Martin R, et al. Significant reductions in methicillin-resistant Staphylococcus aureus bacteraemia and clinical isolates associated with a multisite, hand hygiene culture-change program and subsequent successful statewide roll-out. Med J Aust 2008; 188:633–640 [DOI] [PubMed] [Google Scholar]
- 14.Johnson PD, Martin R, Burrell LJ, et al. Efficacy of an alcohol/chlorhexidine hand hygiene program in a hospital with high rates of nosocomial methicillin-resistant Staphylococcus aureus (MRSA) infection. Med J Aust 2005; 183:509–514 [DOI] [PubMed] [Google Scholar]
- 15.Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect 2009; 73:305–315 [DOI] [PubMed] [Google Scholar]
- 16.Pittet D, Hugonnet S, Harbarth S, et al. Effectiveness of a hospital-wide programme to improve compliance with hand hygiene. Lancet 2000; 356:1307–1312 [DOI] [PubMed] [Google Scholar]
- 17.Grayson ML, Russo PL, Cruickshank M, et al. Outcomes from the first 2 years of the Australian National Hand Hygiene Initiative. Med J Aust 2011; 195:615–619 [DOI] [PubMed] [Google Scholar]
- 18.Stone SP, Fuller C, Savage J, et al. Evaluation of the national Cleanyourhands campaign to reduce Staphylococcus aureus bacteraemia and Clostridium difficile infection in hospitals in England and Wales by improved hand hygiene: four year, prospective, ecological, interrupted time series study. BMJ 2012; 344:e3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jarlier V, Trystram D, Brun-Buisson C, et al. Curbing methicillin-resistant Staphylococcus aureus in 38 French hospitals through a 15-year institutional control program. Arch Intern Med 2010; 170:552–559 [DOI] [PubMed] [Google Scholar]
- 20.Roberts S, Sieczkowski C, Campbell T, et al. Implementing and sustaining a hand hygiene culture change programme at Auckland District Health Board. N Z Med J 2012; 125:75–85 [PubMed] [Google Scholar]
- 21.McLaws ML, Pantle AC, Fitzpatrick KR, Hughes CF. Improvements in hand hygiene across New South Wales public hospitals: clean hands save lives, part III. Med J Aust 2009; 191:S18–S24 [DOI] [PubMed] [Google Scholar]
- 22.McLaws ML, Pantle AC, Fitzpatrick KR, Hughes CF. More than hand hygiene is needed to affect methicillin-resistant Staphylococcus aureus clinical indicator rates: clean hands save lives, part IV. Med J Aust 2009; 191:S26–S31 [DOI] [PubMed] [Google Scholar]
- 23.Australian Comission on Safety and Quality in Healthcare 2014; Available from: http://www.safetyandquality.gov.au [Accessed 19 March 2014] [Google Scholar]
- 24.National Health Performance Authority. Healthcare-associated Staphylococcus aureus bloodstream infections in 2012-2013: National Health Performance Authority; Available from: http://www.myhospitals.gov.au/Content/Reports/sab/2014-03/pdf/HospitalPerformance_SAB_Infocus_2012_13.pdf [Accessed 19 March 2014] [Google Scholar]
- 25.Ho ML, Seto WH, Wong LC, Wong TY. Effectiveness of multifaceted hand hygiene interventions in long-term care facilities in Hong Kong: a cluster-randomized controlled trial. Infect Control Hosp Epidemiol 2012; 33:761–767 [DOI] [PubMed] [Google Scholar]
- 26.Yeung WK, Tam WSW, Wong TW. Clustered randomized controlled trial of a hand hygiene intervention involving pocket sized containers of alcohol based hand rub for the control of infections in long term care facilities. Infect Control Hosp Epidemiol 2011; 32:67–76 [DOI] [PubMed] [Google Scholar]
- 27.Mertz D, Dafoe N, Walter SD, et al. Effect of a multifaceted intervention on adherence to hand hygiene among healthcare workers: a cluster randomized trial. Infect Control Hosp Epidemiol 2010; 31:1170–1176 [DOI] [PubMed] [Google Scholar]
- 28.Kirkland KB, Homa KA, Lasky RA, et al. Impact of a hospital-wide hand hygiene initiative on healthcare-associated infections: results of an interrupted time series. BMJ Qual Saf 2012; 21:1019–1026 [DOI] [PubMed] [Google Scholar]
- 29▪▪.Lee AS, Cooper BS, Malhotra-Kumar S, et al. Comparison of strategies to reduce meticillin-resistant Staphylococcus aureus rates in surgical patients: a controlled multicentre intervention trial. BMJ Open 2013; 3:e003126. [DOI] [PMC free article] [PubMed] [Google Scholar]; In this prospective, multicentre, interventional cohort study, investigators evaluated the efficacy of enhanced hand hygiene vs screening, contact precautions and decolonization vs. both interventions in their ability to reduce MRSA rates. Baseline MRSA rates were low in the study population, and only the combination of the two interventions resulted in a reduction in MRSA rates.
- 30▪▪.Schweizer ML, Reisinger HS, Ohl M, et al. Searching for an optimal hand hygiene bundle: a meta-analysis. Clin Infect Dis 2014; 58:248–259 [DOI] [PubMed] [Google Scholar]; The authors performed a systematic review on all studies on interventions to improve hand hygiene compliance. They included quasiexperimental studies as well as randomized controlled trials. Two bundled interventions were associated with an increase in compliance: the WHO bundle, and a bundle comprised of feedback, education and reminders.
- 31.Gould DJ, Moralejo D, Drey N, Chudleigh JH. Interventions to improve hand hygiene compliance in patient care. Cochrane Database Syst Rev 2010; 9:CD005186. [DOI] [PubMed] [Google Scholar]
- 32.Fuller C, Michie S, Savage J, et al. The Feedback Intervention Trial (FIT) – improving hand-hygiene compliance in UK healthcare workers: a stepped wedge cluster randomised controlled trial. PLoS One 2012; 7:e41617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Grayson ML.Keynote: ‘Antibiotics are dead: how will we manage?’. European Congress of Clinical Microbiology and Infectious Diseases; Berlin. 2013. Abstract L454. [Google Scholar]
- 34.Haas J, Larson E. Measurement of compliance with hand hygiene. J Hosp Infect 2007; 66:6–14 [DOI] [PubMed] [Google Scholar]
- 35.Eckmanns T, Bessert J, Behnke M, et al. Compliance with antiseptic hand rub use in intensive care units: the Hawthorne effect. Infect Control Hosp Epidemiol 2006; 27:931–934 [DOI] [PubMed] [Google Scholar]
- 36.Kohli E, Ptak J, Smith R, et al. Variability in the Hawthorne effect with regard to hand hygiene performance in high and low performing inpatient care units. Infect Control Hosp Epidemiol 2009; 30:222–225 [DOI] [PubMed] [Google Scholar]
- 37.Hand Hygiene Australia [Homepage] [[Accessed 19 March 2014]]. Available from: http://www.hha.org.au. [Google Scholar]
- 38.Sodré da Costa LS, Neves VM, Marra AR, et al. Measuring hand hygiene compliance in a hematology–oncology unit: a comparative study of methodologies. Am J Infect Control 2013; 41:997–1000 [DOI] [PubMed] [Google Scholar]
- 39.Marra AR, Moura DF, Jr, Paes AT, et al. Measuring rates of hand hygiene adherence in the intensive care setting: a comparative study of direct observation, product usage, and electronic counting devices. Infect Control Hosp Epidemiol 2010; 31:796–801 [DOI] [PubMed] [Google Scholar]
- 40.Morgan DJ, Pineles L, Shardell M, et al. Automated hand hygiene count devices may better measure compliance than human observation. Am J Infect Control 2012; 40:955–959 [DOI] [PubMed] [Google Scholar]
- 41.McAteer J, Stone S, Fuller C, et al. Development of an observational measure of healthcare worker hand-hygiene behaviour: the hand-hygiene observation tool (HHOT). J Hosp Infect 2008; 68:222–229 [DOI] [PubMed] [Google Scholar]
- 42▪.Reichardt C, Königer D, Bunte-Schönberger K, et al. Three years of national hand hygiene campaign in Germany: what are the key conclusions for clinical practice? J Hosp Infect 2013; 83:S11–S16 [DOI] [PubMed] [Google Scholar]; This outlines the successful implementation of the WHO hand hygiene multimodal intervention strategy in Germany.
- 43.Reisinger HS, Yin J, Radonovich L, et al. Comprehensive survey of hand hygiene measurement and improvement practices in the Veterans Health Administration. Am J Infect Control 2013; 41:989–993 [DOI] [PubMed] [Google Scholar]
- 44.Salmon S, Tran HL, Bùi DP, et al. Beginning the journey of hand hygiene compliance monitoring at a 2,100-bed tertiary hospital in Vietnam. Am J Infect Control 2014; 42:71–73 [DOI] [PubMed] [Google Scholar]
- 45.Szilágyi L, Haidegger T, Lehotsky Á, et al. A large-scale assessment of hand hygiene quality and the effectiveness of the ‘WHO 6-steps’. BMC Infect Dis 2013; 13:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Magiorakos AP, Leens E, Drouvot V, et al. Pathways to clean hands: highlights of successful hand hygiene implementation strategies in Europe. Euro Surveill 2010; 15:18. [PubMed] [Google Scholar]
- 47.Boyce JM. Measuring healthcare worker hand hygiene activity: current practices and emerging technologies. Infect Control Hosp Epidemiol 2011; 32:1016–1028 [DOI] [PubMed] [Google Scholar]
- 48▪▪.Marra AR, Edmond MB. New technologies to monitor healthcare worker hand hygiene. Clin Microbiol Infect 2014; 20:29–33 [DOI] [PubMed] [Google Scholar]; This article discusses some of the alternatives to direct observation to monitor hand hygiene compliance. They discuss product utilization, automated counters and some of the newer electronic systems.
- 49.Boudjema S, Dufour J, Aladro AS, et al. MediHandTrace®: a tool for measuring and understanding hand hygiene adherence. Clin Microbiol Infect 2014; 20:22–28 [DOI] [PubMed] [Google Scholar]
- 50.Pineles LL, Morgan DJ, Limper HM, et al. Accuracy of a radiofrequency identification (RFID) badge system to monitor hand hygiene behavior during routine clinical activities. Am J Infect Control 2013; 42:144–147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fisher DA, Seetoh T, May-Lin HO, et al. Automated measures of hand hygiene compliance among healthcare workers using ultrasound: validation and a randomized controlled trial. Infect Control Hosp Epidemiol 2013; 34:919–928 [DOI] [PubMed] [Google Scholar]
- 52.Boyce JM, Pittet D. Guideline for hand hygiene in health-care settings. Am J Infect Control 2002; 30:1–46 [DOI] [PubMed] [Google Scholar]
- 53.Kramer A, Rudolph P, Kampf G, Pittet D. Limited efficacy of alcohol-based hand gels. Lancet 2002; 359:1489–1490 [DOI] [PubMed] [Google Scholar]
- 54.Kampf G, Marschall S, Eggerstedt S, Ostermeyer C. Efficacy of ethanol-based hand foams using clinically relevant amounts: a cross-over controlled study among healthy volunteers. BMC Infect Dis 2010; 10:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Edmonds SL, Macinga DR, Mays-Suko P, et al. Comparative efficacy of commercially available alcohol-based hand rubs and World Health Organization-recommended hand rubs: formulation matters. Am J Infect Control 2012; 40:521–525 [DOI] [PubMed] [Google Scholar]
- 56.Eggerstedt S. Comparative efficacy of commercially available alcohol-based hand rubs and World Health Organization-recommended hand rubs. Am J Infect Control 2013; 41:472. [DOI] [PubMed] [Google Scholar]
- 57.Larson EL, Cohen B, Baxter KA. Analysis of alcohol-based hand sanitizer delivery systems: efficacy of foam, gel, and wipes against influenza A (H1N1) virus on hands. Am J Infect Control 2012; 40:806–809 [DOI] [PubMed] [Google Scholar]
- 58.Suchomel M, Kundi M, Pittet D, et al. Testing of the World Health Organization recommended formulations in their application as hygienic hand rubs and proposals for increased efficacy. Am J Infect Control 2012; 40:328–331 [DOI] [PubMed] [Google Scholar]
- 59.Marra AR, Camargo TZS, Cardoso VJ, et al. Hand hygiene compliance in the critical care setting: a comparative study of 2 different alcohol handrub formulations. Am J Infect Control 2013; 41:136–139 [DOI] [PubMed] [Google Scholar]
- 60.Biagi M, Giachetti D, Miraldi E, Figura N. New nonalcoholic formulation for hand disinfection. J Chemother 2013; 26:86–91 [DOI] [PubMed] [Google Scholar]
- 61.Daeschlein G, Scholz S, Ahmed R, et al. Skin decontamination by low-temperature atmospheric pressure plasma jet and dielectric barrier discharge plasma. J Hosp Infect 2012; 81:177–183 [DOI] [PubMed] [Google Scholar]
- 62.Eichner A, Gonzales FP, Felgenträger A, et al. Dirty hands: photodynamic killing of human pathogens like EHEC, MRSA and Candida within seconds. Photochem Photobiol Sci 2013; 12:135–147 [DOI] [PubMed] [Google Scholar]
- 63.Grayson ML, Melvani S, Druce J, et al. Efficacy of soap and water and alcohol-based hand-rub preparations against live H1N1 influenza virus on the hands of human volunteers. Clin Infect Dis 2009; 48:285–291 [DOI] [PubMed] [Google Scholar]
- 64.Steinmann J, Paulmann D, Becker B, et al. Comparison of virucidal activity of alcohol-based hand sanitizers versus antimicrobial hand soaps in vitro and in vivo. J Hosp Infect 2012; 82:277–280 [DOI] [PubMed] [Google Scholar]
- 65.Longtin Y, Voss A, Allegranzi B, Pittet D. Norovirus outbreaks and alcohol-based handrub solutions: association does not prove causation. Am J Infect Control 2012; 40:191. [DOI] [PubMed] [Google Scholar]
- 66.World Health Organization. Clean Care is Safer Care: System change – changing hand hygiene behaviour at the point of care: World Health Organization; 2014; Available from: http://www.who.int/gpsc/tools/faqs/system_change/en/ [Accessed 7 May 2014] [Google Scholar]
- 67.Key Infection Control Recommendations for the Control of Norovirus Outbreaks in Healthcare Settings: US Department of Health and Human Services, Centers for Disease Control and Prevention; 2014; Available from: http://www.cdc.gov/hai/pdfs/norovirus/229110A-NorovirusControlRecomm508A.pdf [Accessed 7 May 2014] [Google Scholar]
- 68.Paulmann D, Steinmann J, Becker B, et al. Virucidal activity of different alcohols against murine norovirus, a surrogate of human norovirus. J Hosp Infect 2011; 79:378–379 [DOI] [PubMed] [Google Scholar]
- 69▪.Chang SC, Li WC, Huang KY, et al. Efficacy of alcohols and alcohol-based hand disinfectants against human enterovirus 71. J Hosp Infect 2013; 83:288–293 [DOI] [PubMed] [Google Scholar]; Alcohol-based hand disinfectants had poor efficacy against human enterovirus 71 and should not be relied on alone for preventing the spread of this infection.
- 70.Turner RB, Fuls JL, Rodgers ND, et al. A randomized trial of the efficacy of hand disinfection for prevention of rhinovirus infection. Clin Infect Dis 2012; 54:1–5 [DOI] [PubMed] [Google Scholar]
- 71.Turner RB, Fuls JL, Rodgers ND. Effectiveness of hand sanitizers with and without organic acids for removal of rhinovirus from hands. Antimicrob Agents Chemother 2010; 54:1363–1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72▪▪.Wong VW, Cowling BJ, Aiello AE. Hand hygiene and risk of influenza virus infections in the community: a systematic review and meta-analysis. Epidemiol Infect 2014; 142:922–932 [DOI] [PMC free article] [PubMed] [Google Scholar]; This meta-analysis evaluated studies comparing the effect of hand hygiene interventions in reducing influenza virus transmission in the community. Ten randomized controlled trials met inclusion criteria. The combination of hand hygiene and facemasks was found to be effective whilst hand hygiene alone was not. This is consistent with the known modes of transmission of influenza which includes aerosol transmission which would not be addressed by hand hygiene alone.
- 73.Jabbar U, Leischner J, Kasper D, et al. Effectiveness of alcohol-based hand rubs for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol 2010; 31:565–570 [DOI] [PubMed] [Google Scholar]
- 74.Edmonds SL, Zapka C, Kasper D, et al. Effectiveness of hand hygiene for removal of Clostridium difficile spores from hands. Infect Control Hosp Epidemiol 2013; 34:302–305 [DOI] [PubMed] [Google Scholar]
- 75.Grayson ML, Ballard SA, Gao W, et al. Quantitative efficacy of alcohol-based handrub against vancomycin-resistant enterococci on the hands of human volunteers. Infect Control Hosp Epidemiol 2012; 33:98–100 [DOI] [PubMed] [Google Scholar]
- 76.Siegel JD, Rhinehart E, Jackson M, Chiarello L. 2007 Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. Am J Infect Control 2007; 35:S65–S164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77▪▪.Tacconelli E, Cataldo M, Dancer S, et al. ESCMID guidelines for the management of the infection control measures to reduce transmission of multidrug resistant Gram-negative bacteria in hospitalized patients. Clin Microbiol Infect 2014; 20:1–55 [DOI] [PubMed] [Google Scholar]; The recent ESCMID guidelines make a strong recommendation that in the epidemic setting, contact precautions should be initiated for all patients colonized or infected with extended spectrum B-lactamase producing enterobacteriaceae, multidrug resistant (MDR) Kelbsiella pneumoniae, MDR Acinetobacter baumannii (moderate evidence), and Pseudomonas aeruginosa (low level evidence).
- 78.Guidance for Control of Carbapenem-Resistant Enterobacteriaceae (CRE): National Center for Emerging and Zoonotic Infectious Diseases. Division of Healthcare Quality Promotion. Center for Disease Control; 2012. Available from: http://www.cdc.gov/hai/pdfs/cre/CRE-guidance-508.pdf [Accessed 13 March 2014] [Google Scholar]
- 79.Recommendations for the control of Multidrug resistant Gram-negatives: carbapenem resistant enterobacteriaceae Sydney: Australian Commission on Safety and Quality in Healthcare; 2013; Available from: http://www.safetyandquality.gov.au/wp-content/uploads/2013/12/MRGN-Guide-Enterobacteriaceae-PDF-1.89MB.pdf [Accessed 17 March 2014] [Google Scholar]
- 80.Hui DS. Severe acute respiratory syndrome (SARS): lessons learnt in Hong Kong. J Thorac Dis 2013; 5:S122 –L 126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Assiri A, McGeer A, Perl TM, et al. Hospital outbreak of Middle East respiratory syndrome coronavirus. N Engl J Med 2013; 369:407–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lee VJ, Yap J, Cook AR, et al. Effectiveness of public health measures in mitigating pandemic influenza spread: a prospective sero-epidemiological cohort study. J Infect Dis 2010; 202:1319–1326 [DOI] [PubMed] [Google Scholar]
- 83▪.Schwaber MJ, Carmeli Y. An ongoing national intervention to contain the spread of carbapenem-resistant enterobacteriaceae. Clin Infect Dis 2014; 58:697–703 [DOI] [PubMed] [Google Scholar]; A report on the nationwide intervention in Israel to contain the spread of carbapenem-resistant enterobacteriaceae. The successful intervention involved patient isolation, dedicated staffing, active surveillance and central supervision of adherance to guidelines.
- 84▪.Palmore TN, Henderson DK. Managing transmission of carbapenem-resistant enterobacteriaceae in healthcare settings: a view from the trenches. Clin Infect Dis 2013; 57:1593–1599 [DOI] [PMC free article] [PubMed] [Google Scholar]; This study outlines the approach adopted by the National Institute of Health to control a cluster of carbepenem-resistant Klebsiella pneumoniae in immunocompromised inpatients. The intervention involved rapid detection techniques, active surveillance, strict hand hygiene, enhanced contact precautions, cohorting and source control.
- 85.Munoz-Price LS, Poirel L, Bonomo RA, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis 2013; 13:785–796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Apisarnthanarak A, Pinitchai U, Warachan B, et al. Effectiveness of infection prevention measures featuring advanced source control and environmental cleaning to limit transmission of extremely-drug resistant Acinetobacter baumannii in a Thai intensive care unit: An analysis before and after extensive flooding. Am J Infect Control 2014; 42:116–121 [DOI] [PubMed] [Google Scholar]
- 87.Landman D, Babu E, Shah N, et al. Transmission of carbapenem-resistant pathogens in New York City hospitals: progress and frustration. J Antimicrob Chemother 2012; 67:1427–1431 [DOI] [PubMed] [Google Scholar]
- 88▪▪.Eyre DW, Cule ML, Wilson DJ, et al. Diverse sources of C. difficile infection identified on whole-genome sequencing. N Engl J Med 2013; 369:1195–1205 [DOI] [PMC free article] [PubMed] [Google Scholar]; In this study, whole geonome sequencing was performed on 1223 isolates from symptomatic patients with C. difficile. Notably, 45% of cases of C. difficile were from genetically distinct sources and not transmitted by recent symptomatic carriers in the hospital.
- 89.Eyre DW, Griffiths D, Vaughan A, et al. Asymptomatic Clostridium difficile colonisation and onward transmission. PLoS One 2013; 8:e78445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ozaki E, Kato H, Kita H, et al. Clostridium difficile colonization in healthy adults: transient colonization and correlation with enterococcal colonization. J Med Microbiol 2004; 53:167–172 [DOI] [PubMed] [Google Scholar]
- 91▪.Howden BP, Holt KE, Lam MM, et al. Genomic insights to control the emergence of vancomycin-resistant enterococci. MBio 2013; 4:e00412–e00413 [DOI] [PMC free article] [PubMed] [Google Scholar]; Investigators in this study performed whole-genome sequencing on 61 E. faecium isolates (36 vancomycin resistant) and on 5 vanB positive anaerobic commensals. The results suggest that de-novo generation of VRE was occurring in addition to cross transmission between patients.
- 92.Stinear TP, Olden DC, Johnson PD, et al. Enterococcal vanB resistance locus in anaerobic bacteria in human faeces. Lancet 2001; 357:855–856 [DOI] [PubMed] [Google Scholar]
- 93.Ballard SA, Pertile KK, Lim M, et al. Molecular characterization of vanB elements in naturally occurring gut anaerobes. Antimicrob Agents Chemother 2005; 49:1688–1694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Johnson PD, Ballard SA, Grabsch EA, et al. A sustained hospital outbreak of vancomycin-resistant Enterococcus faecium bacteremia due to emergence of vanB E. faecium sequence type 203. J Infect Dis 2010; 202:1278–1286 [DOI] [PubMed] [Google Scholar]
- 95.Kraker M, Jarlier V, Monen J, et al. The changing epidemiology of bacteraemias in Europe: trends from the European Antimicrobial Resistance Surveillance System. Clin Microbiol Infect 2013; 19:860–868 [DOI] [PubMed] [Google Scholar]
- 96.Morgan DJ, Diekema DJ, Sepkowitz K, Perencevich EN. Adverse outcomes associated with contact precautions: a review of the literature. Am J Infect Control 2009; 37:85–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Karki S, Leder K, Cheng AC. Patients under contact precautions have an increased risk of injuries and medication errors: a retrospective cohort study. Infect Control Hosp Epidemiol 2013; 34:1118–1120 [DOI] [PubMed] [Google Scholar]
- 98.Karki S, Leder K, Cheng AC. Delays in accessing radiology in patients under contact precautions because of colonization with vancomycin-resistant enterococci. Am J Infect Control 2013; 41:1141–1142 [DOI] [PubMed] [Google Scholar]
- 99.Mehrotra P, Croft L, Day HR, et al. Effects of contact precautions on patient perception of care and satisfaction: a prospective cohort study. Infect Control Hosp Epidemiol 2013; 34:1087–1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100▪▪.Dhar S, Marchaim D, Tansek R, et al. Contact precautions: more is not necessarily better. Infect Control Hosp Epidemiol 2014; 35:213–221 [DOI] [PubMed] [Google Scholar]; In this prospective cohort study conducted across 11 sites, investigators found that the proportion of patients in contact isolation increases within an individual unit, compliance with isolation precautions decreased. This was particularly with regards to hand hygiene prior to gloving and gowning.
- 101.Huskins WC, Huckabee CM, O’Grady NP, et al. Intervention to reduce transmission of resistant bacteria in intensive care. N Engl J Med 2011; 364:1407–1418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102▪.Zahar J, Garrouste-Orgeas M, Vesin A, et al. Impact of contact isolation for multidrug-resistant organisms on the occurrence of medical errors and adverse events. Intensive Care Med 2013; 39:2153–2160 [DOI] [PubMed] [Google Scholar]; This post-hoc analysis utilized the Iatroref III study database to evaluate the frequency of medical errors amongst isolated vs. nonisolated patients in the intensive care unit. A number of different medical errors were more frequent in patients who were isolated compared with those who were not suggesting that this may be an issue even in the intensive care setting in which staffing ratios are higher.


