Abstract
Background
Individuals with borderline personality disorder frequently display comorbid mental disorders. These disorders include “internalizing” disorders (such as major depressive disorder and anxiety disorders) and “externalizing” disorders (such as substance use disorders and antisocial personality disorder). It is hypothesized that these disorders may arise from latent “internalizing” and “externalizing” liability factors. Factor analytic studies suggest that internalizing and externalizing factors both contribute to borderline personality disorder, but the extent to which such contributions are familial is unknown.
Methods
Participants were 368 probands (132 with borderline personality disorder; 134 without borderline personality disorder; and 102 with major depressive disorder) and 885 siblings and parents of probands. Participants were administered the Diagnostic Interview for DSM-IV Personality Disorders; the Revised Diagnostic Interview for Borderlines; and the Structured Clinical Interview for DSM-IV.
Results
On confirmatory factor analysis of within-person associations of disorders, borderline personality disorder loaded moderately on internalizing (factor loading .53, SE .10; p<.001) and externalizing latent variables (.48, SE .10; p<.001). Within-family associations were assessed using structural equation models of familial and non-familial factors for borderline personality disorder, internalizing disorders, and externalizing disorders. In a Cholesky decomposition model, 84% (SE 17%; p<.001) of the association of borderline personality disorder with internalizing and externalizing factors was accounted for by familial contributions.
Conclusions
Familial internalizing and externalizing liability factors are both associated with, and therefore may mutually contribute to BPD. These familial contributions account largely for the pattern of comorbidity between BPD and internalizing and externalizing disorders.
Different mental disorders frequently co-occur within individuals, and explaining this phenomenon of “comorbidity” is a major challenge of psychiatric nosology. One approach to this problem has been to examine the extent to which comorbid disorders may reflect shared underlying dimensions of psychopathology or latent liability factors. Several studies (Kessler et al., 2011, Kotov et al., 2011, Krueger, 1999, Krueger et al., 1998, Roysamb et al., 2011, Vollebergh et al., 2001) using large datasets have found that patterns of comorbidity are well explained by models with only a few such factors. The most consistent of these factors have been those labeled as “internalizing” and “externalizing” – although finer-grained patterns, involving internalizing subfactors (Krueger, 1999, Vollebergh et al., 2001) or additional factors beyond internalizing and externalizing (Roysamb et al. 2011, Kotov et al., 2011, Kendler et al., 2011a), have been proposed. Family (Kendler et al., 1997) and twin studies (Kendler et al., 2003) have suggested that both internalizing and externalizing factors exhibit a familial/genetic basis.
Individuals with borderline personality disorder (BPD) exhibit a very broad range of comorbid mental disorders, including disorders characterized as internalizing, such as mood and anxiety disorders, and externalizing, including substance use disorders and other personality disorders (James and Taylor, 2008, Ruocco, 2005, Slade, 2007, Zanarini et al., 2004a, Zanarini et al., 2004b). Moreover, these same types of disorders also associate with BPD within families. Specifically, relatives of probands with BPD show an elevated risk for both internalizing disorders – including major depressive disorder (Baron et al., 1985, Links et al., 1988, Silverman et al., 1991, Zanarini et al., 2009, Zanarini et al., 1988) and anxiety disorders (Zanarini et al., 2009) – and externalizing disorders, including substance use disorders (Loranger and Tulis, 1985, Pope et al., 1983, Silverman et al., 1991, Zanarini et al., 2009, Zanarini et al., 1988) as well as antisocial personality disorder (Links et al., 1988, Pope et al., 1983, Silverman et al., 1991, Zanarini et al., 2009, Zanarini et al., 1988). However, almost all of the family studies (with notable exceptions (Klein et al., 1995, Riso et al., 2000)) contain methodologic limitations that compromise interpretation of their results, including biased sampling, reliance on information from probands to determine a diagnosis in relatives rather than direct interviews of relatives, and small sample sizes (White et al., 2003; Gunderson et al., 2011). Furthermore, no family study has examined the relationship of BPD with internalizing and externalizing disorders in a multivariate manner.
Importantly, the relationship of BPD to internalizing and externalizing factors appears to be more complex than that of most mental disorders. Clinically, BPD is characterized by prominent internalizing features, such as affective instability, as well as prominent externalizing features, such as impulsivity and unstable relationships. In factor analytic studies, most psychiatric disorders load primarily on (i.e., are strongly correlated with) just one of these 2 factors, whereas BPD, almost uniquely among psychiatric disorders, loads consistently on both (Eaton et al., 2011, James and Taylor, 2008, Kotov et al., 2011, Roysamb et al., 2011).
However, despite great interest in the internalizing and externalizing aspects of BPD and thereby in the potential association with internalizing and externalizing latent factors, the familial contributions to these patterns have not been investigated in any previous study. Thus it is important to further explore the familial relationship of BPD to internalizing and externalizing disorders. Accordingly, we sought to test the hypothesis – replicating and extending findings of previous studies – that familial contributions to internalizing and externalizing factors both also contribute to BPD.
METHOD
DESIGN AND PARTICIPANTS
The design was a family study with direct interviews of probands and their parents and siblings. Three groups of female probands aged 18–35 were recruited: 1) individuals with BPD by criteria of both the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM5-IV) and the Revised Diagnostic Interview for Borderlines (DIB-R) (Zanarini et al., 1989) criteria; 2) individuals with a lifetime diagnosis of major depressive disorder, regardless of the presence or absence of lifetime BPD; 3) individuals without lifetime BPD, regardless of the presence or absence of lifetime major depressive disorder. For groups 1 and 2, we recruited from the inpatient units and partial hospital program of McLean Hospital, and for all groups we recruited from the community using advertisements. Further details of recruitment are presented elsewhere (Gunderson et al., 2011). All potential probands were also required to not have a lifetime diagnosis of schizophrenia, schizoaffective disorder, bipolar I disorder, any organic condition that could cause serious psychiatric symptoms, or mental retardation. Probands supplied contact information on their parents and siblings, and these individuals were asked to participate in the study.
This study was approved by the McLean Hospital Institutional Review Board. After complete description of the study to the participants, written informed consent was obtained.
PROCEDURES
Clinically experienced raters administered 4 semi-structured interviews to all participants (probands and relatives): 1) the Background Information Schedule (Zanarini et al., 2001); 2) the Structured Clinical Interview for DSM-IV (First et al., 1996); 3) the Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) (Zanarini et al., 1996); and 4) the Revised Diagnostic Interview for Borderlines (DIB-R) (Zanarini et al., 1989). Further details of these procedures are presented elsewhere (Gunderson et al., 2011). The kappa statistic for interrater reliability for the diagnosis of BPD, assessed on the basis of 18 interviews, was 1.0 for both the DIPD-R and DIB-R.
STATISTICAL ANALYSIS
To compare demographic characteristics of probands and relatives between the proband groups, we used linear regression for continuous variables and Fisher’s exact test for categorical variables.
For all analyses (i.e., confirmatory factor analysis and Cholesky decomposition models) except for characteristics of the sample, we corrected for the effects of over-sampling probands with BPD and MDD compared with their representation in the source population by weighting participants proportionally to the inverse probability of their selection. Calculation of the selection probabilities requires knowing the prevalence of BPD from the source population from which our sample was drawn. To calculate the prevalence of BPD, we used a method developed for estimating prevalence from relatives of case and control probands (Javaras et al., 2010b), and used previously (Arnold et al., 2006, Gunderson et al., 2011, Hudson et al., 2008, Javaras et al., 2008a, Javaras et al., 2008b). To calculate the prevalence of MDD, we used the prevalence of MDD from the weighted sample of probands and relatives from the BPD and non-BPD proband groups. The effect of these procedures was to create a pseudo-sample that is representative of families from the underlying source population.
To examine the within-person association of BPD with internalizing and externalizing disorders, we performed confirmatory factor analysis to examine the within-person association of BPD with internalizing and externalizing disorders. We based the selection of disorders that loaded on internalizing and externalizing factors on previous work (Kendler et al., 2003, Kessler et al., 2011, Krueger, 1999). The internalizing disorders were generalized anxiety disorder, major depressive disorder, obsessive-compulsive disorders, panic disorder with or without agoraphobia, posttraumatic stress disorder, social anxiety disorder, and specific phobia. The externalizing disorders were alcohol abuse or dependence, drug abuse or dependence (non-alcohol substance use disorders), and antisocial personality disorder. Note that we considered only a rather basic confirmatory model of one internalizing and one externalizing factor, rather than more elaborated models, such as those incorporating internalizing sub-factors or other factors. The reason is that it was not possible to run more complicated models for the corresponding analysis of familial factors, since our dataset only barely supported the fitting of internalizing and externalizing latent factors.
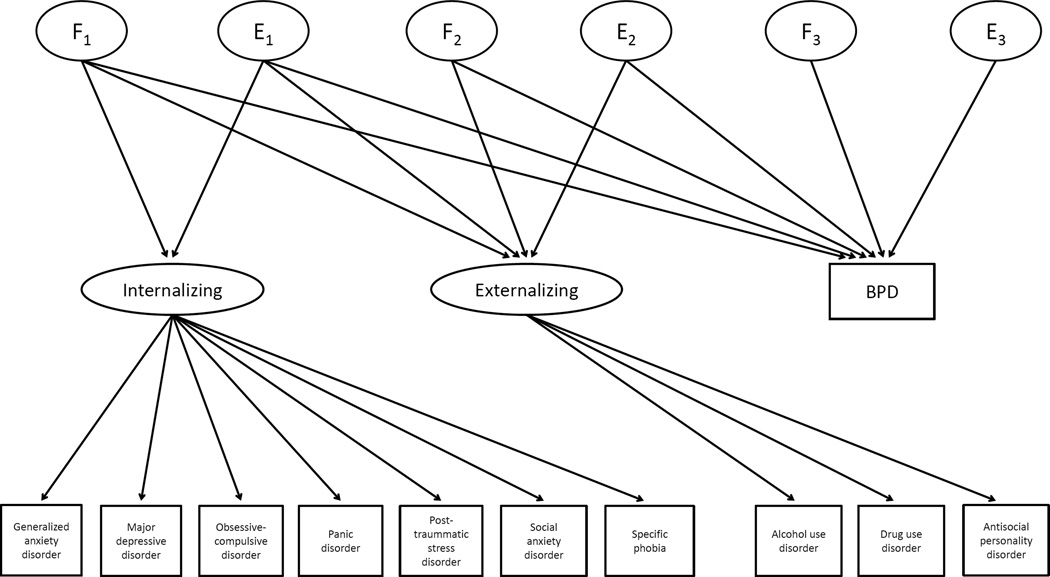
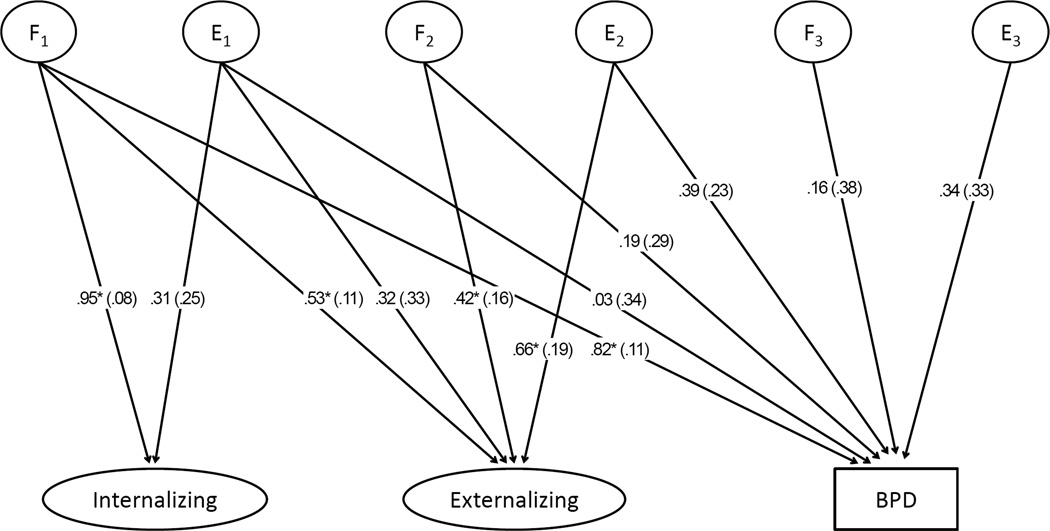
To examine the within-family association of BPD with internalizing and externalizing factors (which in turn, mediate the association of BPD with internalizing and externalizing disorders), we fitted Cholesky decomposition models, which partition the variance of BPD and the covariance between BPD and internalizing and/or externalizing factors into components reflecting familial and unique environmental causal factors. Stated differently, these models partition the variance into components that are familial and non-familial, and also whether these components are shared or not shared with other disorders. Note that we did not attempt to compare the relative fit of these saturated models with potentially more parsimonious reduced models, since the moderate amount of data available only barely allowed fitting full models and thus would be vulnerable to falsely accepting reduced models due to an inability to detect lack of relative fit. We first fit models for the association of BPD with internalizing and externalizing factors separately, and then fit a combined model for the association of BPD with both internalizing and externalizing factors (Figure 1). Proportions of variance, e.g., the amount of variance in BPD due to familial factors, were calculated by squaring a given standardized path coefficient or summing multiple squared path coefficients and multiplying by 100. The percentage of the correlation of one variable with another variable that was accounted for by a given path (or set of paths) was calculated by dividing the squared path (or sum of paths) by the total covariance of the two variables and then multiplying by 100.
Figure 1.
Cholesky decomposition model for relationship of borderline personality disorder (BPD) to internalizing and externalizing factors. “F” variables represent familial factors; “E” variables represent non-familial environmental factors
We fitted the structural equation models under the assumption that associations between family members were attributable to genetic factors alone, based on evidence from previous studies that the effect of common family environment is negligible for BPD (Distel et al., 2010, Jang et al., 1996, Livesley and Jang, 2008) and most internalizing and externalizing disorders (Hettema et al., 2001, Hicks et al., 2004, Kendler and Eaves, 2005, Kendler et al., 2003, Sullivan et al., 2000). Thus, we set the correlation of familial factors between all pairs of first-degree relatives at 0.5.
We used Stata 12.0 software (StataCorp LP, College Station, Texas) for the statistical analyses except for the factor analyses and structural equation models, for which we used Mplus, version 6.0 (Muthén and Muthén, 1998–2010). The standard errors for all analyses except for sample characteristics were corrected for the correlation of observations within families. We set alpha at 0.05, 2-tailed.
The analyses reported here used data from interviewed relatives only because information about non-interviewed relatives provided by the interviewed relatives or probands is likely to be of poorer quality than information obtained from direct interviews, may depend on the informants’ outcome and thus may introduce bias (Kendler et al., 1991, Roy et al., 1996), and may differ between diagnoses in terms of quality and degree of bias (Hudson et al., 2003).
RESULTS
CHARACTERISTICS OF PARTICIPANTS
We collected data between August 2005 and July 2009. We interviewed 368 probands: BPD group, N=132 (of which 61 were patients and 71 were from the community); MDD group, N=102 (of which 6 were patients and 96 were from the community); and non-BPD group N=134 (all from the community). We interviewed 885 parents and siblings of the probands. The demographic characteristics of the probands and relatives are presented in Table 1 (and more detail on characteristics is presented elsewhere (Gunderson et al., 2011)).
Table 1.
Demographic Characteristics of Probands and Relatives
| Proband Group | |||
|---|---|---|---|
| Characteristic | Borderline Personality Disorder |
Non-Borderline Personality Disorder |
Major Depressive Disorder |
| Probands | |||
| Total No. | 132 | 134 | 102 |
| Age, y, mean (SD) | 23.9 (4.6) | 25.7 (4.7) | 27.0 (5.1) |
| Female, No. (%) | 132 (100) | 134 (100) | 102 (100) |
| Relatives | |||
| Total No. | 314 | 337 | 234 |
| Age, y, mean (SD) | 41.5 (14.8) | 40.5 (15.5) | 41.4 (16.1) |
| Relationship to proband, No. (%) | |||
| Mother | 113 (36.0) | 109 (32.3) | 84 (35.9) |
| Father | 73 (23.2) | 56 (16.6) | 38 (16.2) |
| Sister | 78 (24.8) | 110 (32.6) | 73 (31.2) |
| Brother | 50 (15.9) | 62 (18.4) | 39 (16.7) |
FACTOR ANALYSIS
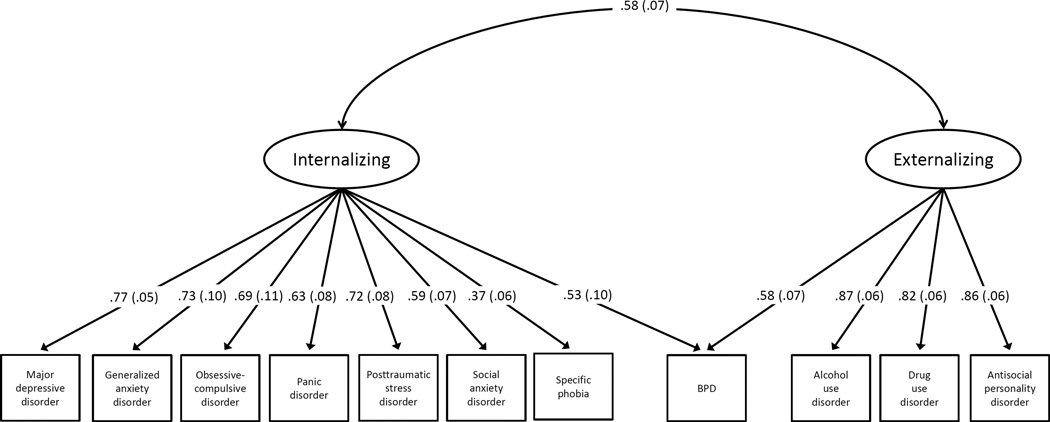
Results of confirmatory factor analysis of the association of BPD with internalizing and externalizing factors (Figure 2) revealed that BPD loaded moderately, significantly, and approximately equally on both factors (estimate .53, SE .10 [p<.001] for internalizing and .48, SE .10 [p<.001] for externalizing); there was also a moderate correlation (r = .58, SE .07; p<.001) between internalizing and externalizing factors themselves. All of the internalizing disorders loaded at least moderately (>.50) on the internalizing factor, with the exception of specific phobia (.37); the 3 externalizing disorders loaded strongly (>.75) on the externalizing factor. The fit indices showed evidence of good model fit: χ2 = 54.4, df = 42, p = 0.09; Comparative Fit Index = 0.98; Root Mean Squared Error of Approximation = 0.015 (90% confidence interval: 0, 0.026).
Figure 2.
Estimated loadings (SE) of borderline personality disorder (BPD) and other psychiatric disorders on internalizing and externalizing latent variables from confirmatory factor analysis (p<.05 for all loadings).
STRUCTURAL EQUATION MODELS
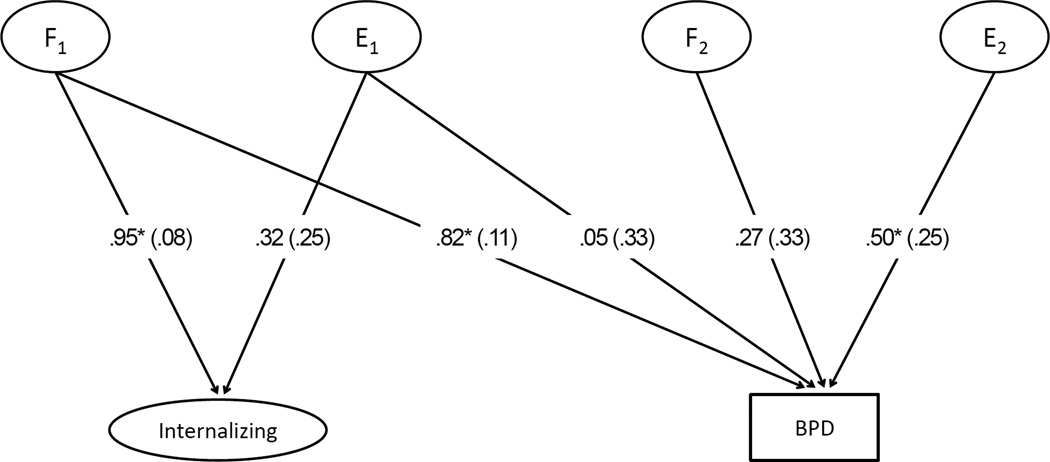
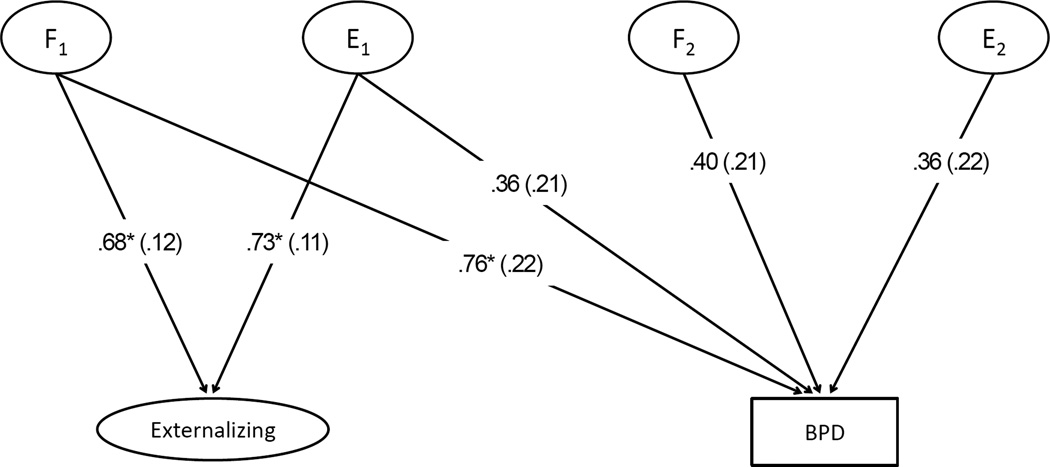
The results of Cholesky decompositions for the association of BPD with internalizing and the association of BPD with externalizing are presented in Figures 3 and 4. The correlation of BPD and internalizing was almost exclusively due to familial influences (estimate 99%; SE .2%; p<.001). Similarly, 82% (SE 25%; p<.001) of the correlation between BPD and externalizing was due to familial influences, with the remainder due to the non-familial environment.
Figure 3.
Estimated path coefficients (SE) for model with borderline personality (BPD) and internalizing latent variable; *p<.05. “F” variables represent familial factors; “E” variables represent non-familial environmental factors.
Figure 4.
Estimated path coefficients (SE) for model with borderline personality (BPD) and externalizing latent variable; *p<.05). “F” variables represent familial factors; “E” variables represent non-familial environmental factors.
In the full Cholesky decomposition with internalizing and externalizing factors (Figure 5), 84% (SE 17%; p<.001) of the association of BPD with internalizing and externalizing factors was accounted for by familial influences; specifically, (((F1−BPD)2 + (F2−BPD)2)/((F1−BPD)2 + (F2−BPD)2 + (E1−BPD)2 + (E2−BPD)2)) × 100% = 84%. Furthermore, the total variance of BPD could be decomposed as follows: 71% (SE 25%; p=.006) due to familial influences shared with internalizing or externalizing; 2% (SE 19%; p=.91) due to familial influences not shared with internalizing or externalizing; 14% (SE 13%; p=.30) due to non-familial environmental influences shared with internalizing or externalizing factors; and 14% (SE 13%; p=.29) due to non-familial environmental influences not shared with internalizing or externalizing factors. A corollary of the second element of this decomposition is that 98% (SE 19%; p<.001) of the familial aggregation of BPD (i.e., the correlation of BPD between family members) was accounted for by familial influences shared with internalizing or externalizing factors.
Figure 5.
Estimated path coefficients (SE) for model with borderline personality (BPD), internalizing latent variable, and externalizing latent variable; *p.05. “F” variables represent familial factors; “E” variables represent non-familial environmental factors.
Note that changing the order of the variables entered into the Cholesky decomposition models had a negligible effect on the results.
DISCUSSION
We used data from a family interview study of BPD, involving 368 probands and 885 of their siblings and parents, to analyze the relationship of BPD with internalizing and externalizing disorders. The main finding was that familial contributions to internalizing and externalizing liability factors also mutually contributed to BPD. Moreover, these familial contributions accounted largely for the pattern of comorbidity between BPD and the various internalizing and externalizing disorders examined in our study and explained almost all of the familiality of BPD.
Examining our results in more detail, and looking first at the within-person associations of BPD with comorbid disorders, our finding on confirmatory factor analysis that BPD loaded substantially on internalizing and externalizing factors is broadly consistent with previous exploratory factor analytic studies (Eaton et al., 2011, James and Taylor, 2008, Kotov et al., 2011, Roysamb et al., 2011). For example, James and Taylor (James and Taylor, 2008) found that BPD loaded on the externalizing factor and the distress or anxious-misery sub-factor of the internalizing factor. In models with a larger number of separate factors, Roysamb et al. (2011) found loading on internalizing, externalizing, and an additional factor of cognitive-relational disturbance; and Kotov et al. 2011 found loading on internalizing and antagonism (but not externalizing).
Our sample size was not large enough to perform an informative exploratory factor analysis of the loading of BPD on other potential factors or sub-factors. Furthermore, even if we were to specify more potential factors on the basis of either exploratory or confirmatory factor analysis of within-person associations, it would not have been possible to run more complicated models for familial factors, since our dataset only barely supported the fitting of internalizing and externalizing latent factors. Nevertheless, even though a more fine-grained analysis with respect to internalizing sub-factors and potentially other factors would be desirable, as a “first approximation,” our data are consistent with and thereby buttress the findings of prior studies. For future work using larger samples, of particular interest would be the potential loading on sub-factors related to internalizing disorders (Eaton et al., 2010; James and Taylor 2008, Kendler et al., 2011b) or the relationship of BPD to potential latent factors associated with axis I and axis II psychopathology when also taking internalizing and externalizing factors into account (Kendler et al., 2011a).
Turning to our analysis of associations between family members, 3 conclusions emerge. First, we found that the association of externalizing and internalizing factors with BPD was largely familial in nature, since additional shared non-familial (that is, shared unique environmental) influences were small. This result is not surprising, given that internalizing and externalizing factors themselves have been shown to have genetic bases specific for each factor and to some extent also shared across both factors (Kendler et al., 2003).
Second, our findings extend the results of prior studies, including our own, showing that BPD is highly familial (discussed further elsewhere (Gunderson et al., 2011)). The present analysis demonstrates further that the familial contributions to BPD are almost exclusively those shared with internalizing or externalizing factors. Thus, there is little evidence for familial influences specific to BPD or shared with another spectrum of psychopathology (for example, another cluster of disorders, such as one involving other personality disorders, that has a shared familial liability factor).
Family study data, unlike twin study data, cannot generate estimates of the proportion of familial influences caused by genetic factors and those caused by common family environment without strong additional assumptions (Javaras et al., 2010a). However, it is likely that the great preponderance of familial influences identified in our study are genetic, because twin studies of BPD (Bornovalova et al., 2009, Distel et al., 2008, Kendler et al., 2008, Torgersen et al., 2000) and of several of the comorbid disorders assessed in our present study (Hettema et al., 2001, Hicks et al., 2004, Kendler and Eaves, 2005, Kendler et al., 2003, Sullivan et al., 2000) have found little evidence for a significant contribution of common family environment.
The finding that both internalizing and externalizing factors were associated with, and therefore may contribute to, BPD suggests that BPD is, in the terminology of Roysamb et al. (2011), “interspectral in nature.” As discussed by others (Eaton et al., 2011, Paris, 2007, Roysamb et al., 2011), several possibilities might account for this interspectrality. The first, which we refer to as “clinical and causal heterogeneity,” is that BPD might embrace in its clinical manifestations a mixture of primarily internalizing and primarily externalizing subtypes caused by underlying largely independent internalizing and externalizing factors. The second, “clinical homogeneity, causal heterogeneity,” is that BPD might be homogeneous at the level of its clinical manifestations, but heterogeneous in its causality – that is, caused by different degrees of underlying internalizing and externalizing factors in different individuals. To give an oversimplified medical analogy, diabetes has a fairly homogeneous clinical presentation, but is heterogeneous in causality, with one form caused by destruction of pancreatic islet cells and the other form by insulin resistance. In favor of this second hypothesis, factor analytic studies (Aggen et al., 2009, Eaton et al., 2011, Johansen et al., 2004, Sanislow et al., 2002) show that the diagnostic criteria for BPD load on a unitary factor. Also supportive are previously published findings from the present family study database (Gunderson et al., 2011) and from twin studies (Distel et al., 2010, Kendler et al., 2011b) showing that a model with a unitary familial/heritable liability to BPD better explains the familiality of BPD than a model with multiple familial/heritable liabilities reflecting the individual sectors of BPD psychopathology (e.g., affective, interpersonal, behavioral, and cognitive).
A third possible hypothesis, “clinical and causal homogeneity,” is that the internalizing and externalizing factors are not truly independent in the first place, and that BPD effectively arises from a single joint internalizing/externalizing factor. Lending some support for the plausibility of this “joint-factor” hypothesis, Kendler and colleagues (Kendler et al., 2003) in a twin study found that “the internalizing general genetic factor consistently loads modestly on the externalizing disorders and vice versa,” and noted that a strict division between internalizing and externalizing factors may be an oversimplification. In the present study we found a substantial correlation between internalizing and externalizing factors in the within-person analyses and also strong evidence for shared familial basis for internalizing and externalizing disorders. Thus, BPD might be roughly as causally homogeneous as any of the individual internalizing or externalizing disorders, but give only the appearance of greater causal heterogeneity.
The inability of our analysis to discriminate among the above 3 competing hypotheses reflects to some extent the inherent limitations of using phenomenology alone to understand the causal structure of mental disorders such as BPD. Thus, further progress will likely require integration of phenomenology with a better understanding of underlying psychopathological, developmental, and neurobiological processes (Insel et al., 2010, Kendler, 2012). This progress will likely include identification of relevant endophenotypes (Siever et al., 2002). An example of this type of work is a recent study (Ruocco et al., 2012) which found that a subgroup of relatives of individuals with BPD had clinically meaningful deficits of response inhibition despite not having BPD themselves. In addition, future research should explore the developmental trajectory of BPD, following the lines of recent work that attempts to integrate the internalizing and externalizing features of BPD into a developmental framework (Chaen and Kaess, 2012, Crowell et al., 2009, Stepp et al., 2012).
There are several limitations of the study that should be considered. First, we did not sample probands randomly from a defined source population. Thus, our sampling method may have introduced selection (or ascertainment) bias if the probands were not representative of individuals in the source population in the 3 groups sampled. However, as we have discussed previously (Gunderson et al., 2011) we found no evidence in this dataset for a significant interaction between the source of BPD proband (patient vs. community) and measures of the familial aggregation of BPD, suggesting that these 2 sources were similar, and probands from all groups were recruited without knowledge of whether they had any comorbid mental disorders. Second, we evaluated only a certain set of comorbid disorders, and in particular did not include some disorders of interest with respect to their relationship with BPD such as psychotic disorders and bipolar disorder because presence of these disorders were excluded in probands. However, the exclusion of these disorders is not likely to have affected our findings with respect to the relationship of BPD to internalizing and externalizing disorders. Third, all of the analyses are based on the assumption that, aside from the effects related to the outcome variables, there are no important differences in measures of familial aggregation between pairs of relatives. This assumption is difficult to test, particularly in the setting of the multivariate analyses of the present study, but we found no evidence for such effects in this dataset with respect to the familial aggregation of BPD (Gunderson et al., 2011). Fourth, we used weighting based on the inverse probability of selection using a novel estimator of the prevalence of BPD derived from the data on relatives, rather than a direct assessment of prevalence. Any additional uncertainty attributable to use of this method is not reflected in the confidence intervals, but any such uncertainty would, in any event, be expected to be small relative to other sources. Fifth, not all eligible parents and siblings chose to participate, and thus this missing data could have introduced bias if the characteristics of the non-interviewed relatives were substantially different from those of the interviewed relatives. Sixth, lifetime diagnoses of BPD and other mental disorders are difficult to assess accurately. However, misclassification of this type would be expected to be non-differential and therefore would likely cause bias towards the null. Seventh, as mentioned above, our sample size was not large enough to perform an informative exploratory factor analysis of the loading of BPD on other potential factors or sub-factors. Nor was it large enough to fit more complex confirmatory analyses in a meaningful way, especially since there is less agreement about what factors should be included in such models. However, the present study would seem to represent a reasonable first step in the direction of exploring the latent familial structure of comorbidity with respect to BPD, and hopefully will stimulate further work along these lines using larger and richer datasets. Eighth, our sample size was also not large enough to generate sufficient power to make valid analyses regarding the potential effects of variables such as sex, age, and type of relative pair (e.g., parent-sibling vs. sibling-sibling). However, it is reassuring in this regard that we found no evidence for such effects in an analysis of the familial aggregation of BPD using this same dataset (Gunderson et al., 2011), and that other twin studies have found no evidence of sex effects for the heritability of BPD (Distel et al., 2008). Ninth, due to the small sample size relative to the number of disorders studied, our analysis of familiality was made under the assumption that effects attributable to shared familial environmental were negligible in comparison with those attributable to additive genetic effects. This assumption would appear reasonable on the basis of data from twin studies for the case of BPD alone (Bornovalova et al., 2009, Distel et al., 2008, Kendler et al., 2008, Torgersen et al., 2000) and more generally for the latent structure of the familial comorbidity of mental disorders (Kendler et al., 2003). However, potential effects of shared familial environment would lower the estimates of the magnitude of association. Thus our estimates of the magnitude of the associations may be biased upward, although this bias is likely to be small. We note further that none of the interpretations of the results of this study rest on the assumption that the familial factors identified are entirely genetic, and indeed it is quite plausible that there are not only relevant environmental familial contributions, but also that there are important gene-environment interactions (which are also were assumed solely for modeling purposes to be negligible).
In conclusion, replicating and extending previous work, this study found that familial internalizing and externalizing liability factors are both associated with, and therefore may mutually contribute to BPD, and these familial contributions account largely for the pattern of comorbidity between BPD and internalizing and externalizing disorders.
Acknowledgments
This study was supported by National Institute of Mental Health, grant MH 400130 (R01)
References
- Aggen SH, Neale MC, Roysamb E, Reichborn-Kjennerud T, Kendler KS. A psychometric evaluation of the DSM-IV borderline personality disorder criteria: age and sex moderation of criterion functioning. Psychological Medicine. 2009;39:1967–1978. doi: 10.1017/S0033291709005807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold LM, Hudson JI, Keck PE, Auchenbach MB, Javaras KN, Hess EV. Comorbidity of fibromyalgia and psychiatric disorders. Journal of Clinical Psychiatry. 2006;67:1219–1225. doi: 10.4088/jcp.v67n0807. [DOI] [PubMed] [Google Scholar]
- Baron M, Gruen R, Asnis L, Lord S. Familial transmission of schizotypal and borderline personality disorders. American Journal of Psychiatry. 1985;142:927–934. doi: 10.1176/ajp.142.8.927. [DOI] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: a longitudinal twin study. Developmental Psychopathology. 2009;21:1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanen AM, Kaess M. Developmental Pathways to Borderline Personality Disorder. Current Psychiatry Reports. 2012;14:45–53. doi: 10.1007/s11920-011-0242-y. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan MM. A Biosocial Developmental Model of Borderline Personality: Elaborating and Extending Linehan's Theory. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Distel MA, Trull TJ, Derom CA, Thiery EW, Grimmer MA, Martin NG, Willemsen G, Boomsma DI. Heritability of borderline personality disorder features is similar across three countries. Psychological Medicine. 2008;38:1219–1229. doi: 10.1017/S0033291707002024. [DOI] [PubMed] [Google Scholar]
- Distel MA, Willemsen G, Ligthart L, Derom CA, Martin NG, Neale MC, Trull TJ, Boomsma DI. Genetic covariance structure of the four main features of borderline personality disorder. Journal of Personality Disorders. 2010;24:427–444. doi: 10.1521/pedi.2010.24.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton NR, Krueger RF, Keyes KM, Skodol AE, Markon KE, Grant BF, Hasin DS. Borderline personality disorder co-morbidity: relationship to the internalizing-externalizing structure of common mental disorders. Psychological Medicine. 2011;41:1041–1050. doi: 10.1017/S0033291710001662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbons M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) New York: New York State Psychiatric Institute; 1996. [Google Scholar]
- Gunderson JG, Zanarini MC, Choi-Kain LW, Mitchell KS, Jang KL, Hudson JI. Family study of borderline personality disorder and its sectors of psychopathology. Archives of General Psychiatry. 2011;68:753–762. doi: 10.1001/archgenpsychiatry.2011.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. American Journal of Psychiatry. 2001;158:1568–1578. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- Hicks BM, Krueger RF, Iacono WG, McGue M, Patrick CJ. Family transmission and heritability of externalizing disorders: a twin-family study. Archives of General Psychiatry. 2004;61:922–928. doi: 10.1001/archpsyc.61.9.922. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Javaras KN, Laird NM, VanderWeele TJ, Pope HG, Hernan MA. A structural approach to the familial coaggregation of disorders. Epidemiology. 2008;19:431–439. doi: 10.1097/EDE.0b013e31816a9de7. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Mangweth B, Pope HG, Jr, De Col C, Hausmann A, Gutweniger S, Laird NM, Biebl W, Tsuang MT. Family study of affective spectrum disorder. Archives of General Psychiatry. 2003;60:170–177. doi: 10.1001/archpsyc.60.2.170. [DOI] [PubMed] [Google Scholar]
- Insel T, Cuthbert B, Garvey M, Heinssen R, Pine DS, Quinn K, Sanislow C, Wang P. Research Domain Criteria (RDoC): toward a new classification framework for research on mental disorders. American Journal of Psychiatry. 2010;167:748–751. doi: 10.1176/appi.ajp.2010.09091379. [DOI] [PubMed] [Google Scholar]
- James LM, Taylor J. Revisiting the structure of mental disorders: Borderline personality disorder and the internalizing/externalizing spectra. British Journal of Clinical Psychology. 2008;47:361–380. doi: 10.1348/014466508X299691. [DOI] [PubMed] [Google Scholar]
- Jang KL, Livesley WJ, Vernon PA, Jackson DN. Heritability of personality disorder traits: a twin study. Acta Psychiatrica Scandanavica. 1996;94:438–444. doi: 10.1111/j.1600-0447.1996.tb09887.x. [DOI] [PubMed] [Google Scholar]
- Javaras KN, Hudson JI, Laird NM. Fitting ACE structural equation models to case-control family data. Genetic Epidemiology. 2010a;34:238–245. doi: 10.1002/gepi.20454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javaras KN, Laird NM, Hudson JI, Ripley BD. Estimating disease prevalence using relatives of case and control probands. Biometrics. 2010b;66:214–221. doi: 10.1111/j.1541-0420.2009.01272.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Javaras KN, Laird NM, Reichborn-Kjennerud T, Bulik CM, Pope HG, Jr, Hudson JI. Familiality and heritability of binge eating disorder: results of a case-control family study and a twin study. International Journal of Eating Disorders. 2008a;41:174–179. doi: 10.1002/eat.20484. [DOI] [PubMed] [Google Scholar]
- Javaras KN, Pope HG, Lalonde JK, Roberts JL, Nillni YI, Laird NM, Bulik CM, Crow SJ, McElroy SL, Walsh BT, Tsuang MT, Rosenthal NR, Hudson JI. Co-occurrence of binge eating disorder with psychiatric and medical disorders. Journal of Clinical Psychiatry. 2008b;69:266–273. doi: 10.4088/jcp.v69n0213. [DOI] [PubMed] [Google Scholar]
- Johansen M, Karterud S, Pedersen G, Gude T, Falkum E. An investigation of the prototype validity of the borderline DSM-IV construct. Acta Psychiatrica Scandinavica. 2004;109:289–298. doi: 10.1046/j.1600-0447.2003.00268.x. [DOI] [PubMed] [Google Scholar]
- Kendler KS. Levels of explanation in psychiatric and substance use disorders: implications for the development of an etiologically based nosology. Molecular Psychiatry. 2012;17:11–21. doi: 10.1038/mp.2011.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Czajkowski N, Roysamb E, Tambs K, Torgersen S, Neale MC, Reichborn-Kjennerud T. The structure of genetic and environmental risk factors for DSM-IV personality disorders: a multivariate twin study. Archives of General Psychiatry. 2008;65:1438–1446. doi: 10.1001/archpsyc.65.12.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Aggen SH, Knudsen GP, Roysamb E, Neale MC, Reichborn-Kjennerud T. The Structure of Genetic and Environmental Risk Factors for Syndromal and Subsyndromal Common DSM-IV Axis I and All Axis II Disorders. American Journal of Psychiatry. 2011a;168:29–39. doi: 10.1176/appi.ajp.2010.10030340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: a family history study. British Journal of Psychiatry. 1997;170:541–548. doi: 10.1192/bjp.170.6.541. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Eaves LJ. Psychiatric genetics (Review of Psychiatry) Washington, DC: American Psychiatric Association; 2005. [Google Scholar]
- Kendler KS, Myers J, Reichborn-Kjennerud T. Borderline personality disorder traits and their relationship with dimensions of normative personality: a web-based cohort and twin study. Acta Psychiatrica Scandanavica. 2011b;123:349–359. doi: 10.1111/j.1600-0447.2010.01653.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Silberg JL, Neale MC, Kessler RC, Heath AC, Eaves LJ. The family history method: whose psychiatric history is measured? American Journal of Psychiatry. 1991;148:1501–1504. doi: 10.1176/ajp.148.11.1501. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ormel J, Petukhova M, McLaughlin KA, Green JG, Russo LJ, Stein DJ, Zaslavsky AM, Aguilar-Gaxiola S, Alonso J, Andrade L, Benjet C, de Girolamo G, de Graaf R, Demyttenaere K, Fayyad J, Haro JM, Hu C, Karam A, Lee S, Lepine JP, Matchsinger H, Mihaescu-Pintia C, Posada-Villa J, Sagar R, Ustun TB. Development of lifetime comorbidity in the World Health Organization world mental health surveys. Archives of General Psychiatry. 2011;68:90–100. doi: 10.1001/archgenpsychiatry.2010.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DN, Riso LP, Donaldson SK, Schwartz JE, Anderson RL, Ouimette PC, Lizardi H, Aronson TA. Family study of early-onset dysthymia. Mood and personality disorders in relatives of outpatients with dysthymia and episodic major depression and normal controls. Archives of General Psychiatry. 1995;52:487–496. [PubMed] [Google Scholar]
- Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Archives of General Psychiatry. 2011;68:1003–1011. doi: 10.1001/archgenpsychiatry.2011.107. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56:921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Krueger RF, Caspi A, Moffitt TE, Silva PA. The structure and stability of common mental disorders (DSM-III-R): a longitudinal-epidemiological study. Journal of Abnormal Psychology. 1998;107:216–227. doi: 10.1037//0021-843x.107.2.216. [DOI] [PubMed] [Google Scholar]
- Links PS, Steiner M, Huxley G. The occurrence of borderline personality disorder in the families of borderline patients. Journal of Personality Disorders. 1988;2:14–20. [Google Scholar]
- Livesley WJ, Jang KL. The behavioral genetics of personality disorder. Annual Review of Clinical Psychology. 2008;4:247–274. doi: 10.1146/annurev.clinpsy.4.022007.141203. [DOI] [PubMed] [Google Scholar]
- Loranger AW, Tulis EH. Family history of alcoholism in borderline personality disorder. Archives of General Psychiatry. 1985;42:153–157. doi: 10.1001/archpsyc.1985.01790250047006. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus users guide. Sixth edition. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- Paris J. The nature of borderline personality disorder: Multiple dimensions, multiple symptoms, but one category. Journal of Personality Disorders. 2007;21:457–473. doi: 10.1521/pedi.2007.21.5.457. [DOI] [PubMed] [Google Scholar]
- Pope HG, Jr, Jonas JM, Hudson JI, Cohen BM, Gunderson JG. The validity of DSM-III borderline personality disorder. A phenomenologic, family history, treatment response, and long-term follow-up study. Archives of General Psychiatry. 1983;40:23–30. doi: 10.1001/archpsyc.1983.01790010025003. [DOI] [PubMed] [Google Scholar]
- Riso LP, Klein DN, Anderson RL, Ouimette PC. A family study of outpatients with borderline personality disorder and no history of mood disorder. Journal of Personality Disorders. 2000;14:208–217. doi: 10.1521/pedi.2000.14.3.208. [DOI] [PubMed] [Google Scholar]
- Roy MA, Walsh D, Kendler KS. Accuracies and inaccuracies of the family history method: a multivariate approach. Acta Psychiatrica Scandanavica. 1996;93:224–234. doi: 10.1111/j.1600-0447.1996.tb10639.x. [DOI] [PubMed] [Google Scholar]
- Roysamb E, Kendler KS, Tambs K, Orstavik RE, Neale MC, Aggen SH, Torgersen S, Reichborn-Kjennerud T. The Joint Structure of DSM-IV Axis I and Axis II Disorders. Journal of Abnormal Psychology. 2011;120:198–209. doi: 10.1037/a0021660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruocco AC. Reevaluating the distinction between axis I and axis II disorders: The case of borderline personality disorder. Journal of Clinical Psychology. 2005;61:1509–1523. doi: 10.1002/jclp.20205. [DOI] [PubMed] [Google Scholar]
- Ruocco AC, Laporte L, Russell J, Guttman H, Paris J. Response inhibition deficits in unaffected first-degree relatives of patients with borderline personality disorder. Neuropsychology. 2012;26:473–482. doi: 10.1037/a0028715. [DOI] [PubMed] [Google Scholar]
- Sanislow CA, Grilo CM, Morey LC, Bender DS, Skodol AE, Gunderson JG, Shea MT, Stout RL, Zanarini MC, McGlashan TH. Confirmatory factor analysis of DSM-IV criteria for borderline personality disorder: Findings from the collaborative longitudinal personality disorders study. American Journal of Psychiatry. 2002;159:284–290. doi: 10.1176/appi.ajp.159.2.284. [DOI] [PubMed] [Google Scholar]
- Siever LJ, Torgersen S, Gunderson JG, Livesley WJ, Kendler KS. The borderline diagnosis III: identifying endophenotypes for genetic studies. Biological Psychiatry. 2002;51:964–968. doi: 10.1016/s0006-3223(02)01326-4. [DOI] [PubMed] [Google Scholar]
- Silverman JM, Pinkham L, Horvath TB, Coccaro EF, Klar H, Schear S, Apter S, Davidson M, Mohs RC, Siever LJ. Affective and impulsive personality disorder traits in the relatives of patients with borderline personality disorder. American Journal of Psychiatry. 1991;148:1378–1385. doi: 10.1176/ajp.148.10.1378. [DOI] [PubMed] [Google Scholar]
- Slade T. The descriptive epidemiology of internalizing and externalizing psychiatric dimensions. Social Psychiatry and Psychiatric Epidemiology. 2007;42:554–560. doi: 10.1007/s00127-007-0200-5. [DOI] [PubMed] [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of Attention Deficit Hyperactivity Disorder and Oppositional Defiant Disorder Symptoms as Precursors of Borderline Personality Disorder Symptoms in Adolescent Girls. Journal of Abnormal Child Psychology. 2012;40:7–20. doi: 10.1007/s10802-011-9530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. American Journal of Psychiatry. 2000;157:1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Lygren S, Oien PA, Skre I, Onstad S, Edvardsen J, Tambs K, Kringlen E. A twin study of personality disorders. Comprehensive Psychiatry. 2000;41:416–425. doi: 10.1053/comp.2000.16560. [DOI] [PubMed] [Google Scholar]
- Vollebergh WA, Ledema J, Bijl RV, de Graaf R, Smit F, Ormel J. The structure and stability of common mental disorders: the NEMESIS study. Archives of General Psychiatry. 2001;58:597–603. doi: 10.1001/archpsyc.58.6.597. [DOI] [PubMed] [Google Scholar]
- White CN, Gunderson JG, Zanarini MC, Hudson JI. Family studies of borderline personality disorder: a review. Harvard Review of Psychiatry. 2003;11:8–19. doi: 10.1080/10673220303937. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Barison LK, Frankenburg FR, Reich DB, Hudson JI. Family history study of the familial coaggregation of borderline personality disorder with axis I and nonborderline dramatic cluster axis II disorders. Journal of Personality Disorders. 2009;23:357–369. doi: 10.1521/pedi.2009.23.4.357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J, Reich DB, Silk KR. Axis I comorbidity in patients with borderline personality disorder: 6-year follow-up and prediction of time to remission. American Journal of Psychiatry. 2004a;161:2108–2114. doi: 10.1176/appi.ajp.161.11.2108. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Khera GS, Bleichmar J. Treatment histories of borderline inpatients. Comprehensive Psychiatry. 2001;42:144–150. doi: 10.1053/comp.2001.19749. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Sickel AE, Yong L. The Diagnostic Interview for DSM-IV Personality Disorders (DIPD-IV) Belmont, MA: McLean Hospital; 1996. [Google Scholar]
- Zanarini MC, Frankenburg FR, Vujanovic AA, Hennen J, Reich DB, Silk KR. Axis II comorbidity of borderline personality disorder: description of 6-year course and prediction to time-to-remission. Acta Psychiatrica Scandanavica. 2004b;110:416–420. doi: 10.1111/j.1600-0447.2004.00362.x. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Gunderson JG, Frankenburg FR, Chauncey DL. The Revised Diagnostic Interview for Borderlines: Discriminating BPD from other axis II disorders. Journal of Personality Disorders. 1989;3:10–18. [Google Scholar]
- Zanarini MC, Gunderson JG, Marino MF, Schwartz EO, Frankenburg FR. DSM-III disorders in the families of borderline outpatients. Journal of Personality Disorders. 1988;2:292–302. [Google Scholar]