Abstract
The need to provide invasive mechanical ventilatory support to patients with myocardial infarction and acute left heart failure is common. Despite the large number of patients requiring mechanical ventilation in this setting, there are remarkably few data addressing the ideal mode of respiratory support in such patients. Although there is near universal acceptance regarding the use of non-invasive positive pressure ventilation in patients with acute pulmonary oedema, there is more concern with invasive positive pressure ventilation owing to its more significant haemodynamic impact. Positive end-expiratory pressure (PEEP) is almost universally applied in mechanically ventilated patients due to benefits in gas exchange, recruitment of alveolar units, counterbalance of hydrostatic forces leading to pulmonary oedema and maintenance of airway patency. The limited available clinical data suggest that a moderate level of PEEP is safe to use in severe left ventricular (LV) dysfunction and cardiogenic shock, and may provide haemodynamic benefits as well in LV failure which exhibits afterload-sensitive physiology.
INTRODUCTION
Acute left heart failure is a well-documented complication of acute myocardial infarction (MI).1 Acute MI is complicated by cardiogenic shock in 5%–10% of the cases2,3 and by pulmonary oedema in up to 40% of the patients admitted to the intensive care unit (ICU).2 The need to provide non-invasive or invasive mechanical ventilatory support to patients in acute left heart failure is common due to acute hypoxemic respiratory failure, increased work of breathing, electrical instability and the need to perform percutaneous or surgical interventions.1 The requirement for mechanical ventilation in acute MI is independently associated with high mortality, as are the degree of ventilatory support and severity of hypoxaemia.2,4 The mortality in patients with acute MI who require mechanical ventilation is consistently reported at or above 50%2–4 compared with the overall mortality of 10%–25% in subjects with acute MI admitted to the ICU.5
Despite the large number of patients requiring mechanical ventilation in the setting of acute MI, there are remarkably few data addressing the ideal mode of respiratory support in such patients. This is especially surprising given the well-recognised haemodynamic effects of positive pressure ventilation (PPV); in these individuals with tenuous haemodynamic status, inappropriate ventilation settings could have severe deleterious effects. Moreover, recent reviews on the subject tended to focus on theoretical and physiological investigations rather than clinical studies.6,7 This paper will summarize the available clinical evidence on mechanical ventilation with positive end-expiratory pressure (PEEP) in patients with acute MI complicated by haemodynamic instability and cardiogenic shock. We hope to be able to recommend guidelines for safe and effective practice.
PEEP IN MECHANICAL VENTILATION
PEEP refers to an adjunct to PPV in which the alveolar pressure is maintained above atmospheric pressure (usually by 5–15 cm H2O) at the conclusion of expiration. PEEP is almost universally applied in mechanically ventilated patients due to benefits in gas exchange, recruitment of alveolar units, counterbalance of hydrostatic forces leading to pulmonary oedema and maintenance of airway patency.8–12 However, there are exceptions to this general rule of using PEEP, particularly in a tenuous patient where there is concern that increased intrathoracic pressure will worsen a patient’s haemodynamic stability or where the risk of pulmonary barotrauma is high.13,14
The past two decades have produced a plethora of research clarifying the utility and safety of PEEP. Prospective randomised controlled trials have shown that high, yet controlled, levels of PEEP can be safely used in patients with acute respiratory distress syndrome (ARDS).15 The general consensus maintains that complications of PEEP, particularly barotrauma, dynamic hyperinflation and auto (intrinsic) PEEP, can be avoided by carefully monitoring the tidal volumes, peak and plateau pressures and transthoracic pressure gradients.13 Thus, maintaining at least a small degree of PEEP remains a consensus recommendation for most mechanically ventilated patients.13
While a small amount of PEEP (3–5 cm H2O) is beneficial in the majority of cases, higher levels of PEEP may be necessary in specific subsets of mechanically ventilated patients, such as those with ARDS, in whom pulmonary compliance is reduced and, thus, recruitment of collapsed alveoli and reversal of atelectasis are critical. In addition, early studies on patients with pulmonary oedema established that PEEP can shift fluid from alveoli and the interstitial space back into the circulation, thereby reducing the degree of intrapulmonary shunting and improving oxygenation.10,16
HAEMODYNAMIC EFFECTS OF PPV
Although PEEP can have varied haemodynamic effects in all patients requiring mechanical ventilation, it is of great concern in patients with acute MI or acute left heart failure due to potentially deleterious effect on cardiac output (CO) and systemic perfusion. In fact, the most frequent objection to using PEEP is due to fear that it will worsen CO and haemodynamic stability.17
Early investigations of the effects of invasive PPV in animals and in patients with other underlying pathologies, such as the ARDS, found that PEEP exerted unfavourable haemodynamic effects such as diminishing venous blood return,18–20 increasing right ventricular (RV) afterload,21 decreasing left ventricular (LV) filling and depressing CO and overall organ perfusion (See figure 1).22–27 These data were extrapolated to patients with cardiogenic shock, and avoidance of mechanical ventilation and/or early extubation was initially recommended in that patient subset.17
Figure 1.
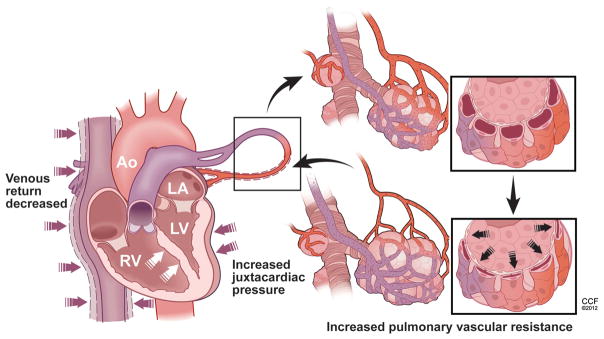
Mechanical effects of positive pressure ventilation on cardiopulmonary circulation. The detrimental mechanical effects of positive pressure ventilation on cardiac haemodynamics include: (1) decreased venous return due to external pressure on the inferior vena cava with resultant decrease in its caliber; (2) increased right ventricular dilatation with septal shift (white arrows) as a result of the elevation on the right ventricular afterload and (3) decreased left ventricular filling and cardiac output. Access the article online to view this figure in colour.
However, these data were by no means conclusive in cardiogenic shock, as other studies did not indicate that PPV had detrimental effects on LV function28–30 and showed that, conversely, PEEP decreased LV oxygen demand and improved oxygen delivery to the ischaemic myocardium, as evidenced by a decreased intracardiac lactate production.31 Thus, the theoretical concerns that emerged from earlier physiological studies were not consistently reproduced in the clinical setting.32 This is likely due to the varied models, conditions and measured variables found in the laboratory compared with observations in vivo.
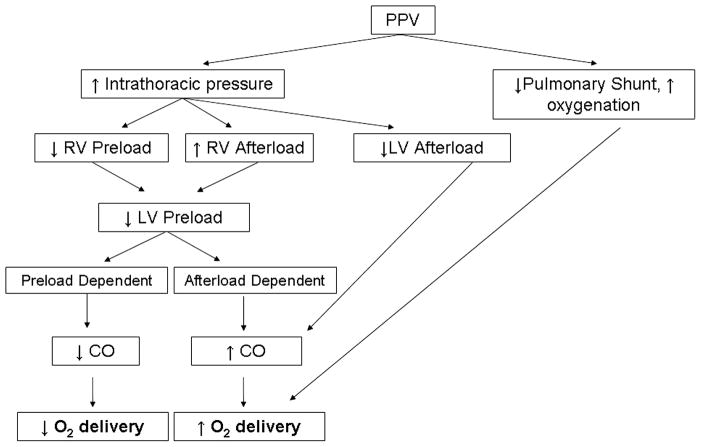
A number of mechanisms for the haemodynamic improvement observed with positive pressure mechanical ventilation and PEEP include reduced LV afterload due to decreased transmural (or transthoracic) pulmonary pressure;33–37 reduced LV preload thereby unloading the congested heart38; decreased work of breathing and overall metabolic demand;39,40 reversal of hypoxia-related pulmonary vasoconstriction; and improved oxygenation that may optimise oxygen supply to the stressed myocardium (See figure 2).41,42 These haemodynamic effects are of great advantage to the dysfunctional LV that is both extremely sensitive to changes in afterload and subject to oxygen delivery that is below its metabolic demand. In contrast, the normal LV is predominantly preload-dependent. Therefore, the reduction in preload via decreased venous return with PPV may have a more prominent effect in the normal heart than afterload reduction thereby decreasing CO (see table 1).14,43–45
Figure 2.
Cardiopulmonary effects of invasive positive pressure ventilation (PPV). CO, cardiac output; LV, left ventricular; RV, right ventricular.
Table 1.
Haemodynamic effects of positive pressure ventilation on cardiac output
| Haemodynamic effect of positive pressure ventilation | Likely effect on cardiac output
|
|
|---|---|---|
| Preload dependent | Afterload dependent | |
| RV preload ↓ | ↓ | ↑ |
| RV afterload ↑ | ↓ | ↓ |
| LV preload ↓ | ↓ | ↑ |
| LV afterload ↓ | ↑ | ↑ |
The most prominent haemodynamic effects of invasive positive pressure mechanical ventilation include a decrease in right ventricular (RV) preload, an increase in RV afterload, a decrease in left ventricular (LV) preload and a decrease in LV afterload. The theoretical impact of the aforementioned haemodynamic changes on the overall cardiac output (CO) depends on the aetiology of the patient’s underlying physiology. In patients who are ‘preload dependent’, the decrease in RV and LV preload and increase in RV afterload would decrease the CO; the decrease in LV afterload would increase the CO. Overall, the patient would likely experience a net decrease in CO. In patients who are ‘afterload dependent’, the decreased RV and LV preload and decreased LV afterload would increase the CO, whereas the increase in RV afterload would decrease the CO. The patient would likely have an overall improvement in CO.
NON-INVASIVE PPV IN CARDIOGENIC PULMONARY OEDEMA
Non-invasive PPV, either via continuous positive airway pressure or bilevel positive pressure support ventilation (commonly referred to by its trade name BiPAP, Respironics Inc, Murrysville, Pennsylvania, USA) has been shown to improve haemodynamics, respiratory function and oxygenation in patients with acute systolic heart failure and pulmonary oedema compared with oxygen therapy alone.46–51 Moreover, the use of non-invasive ventilation in randomised prospective trials was associated with lower rates of intubation and improved 30-day mortality46,49,51 compared with oxygen therapy alone.48 Results have been similar in patients with systolic heart failure secondary to acute MI47,50 or heart failure with preserved ejection fraction.52,53 Thus, non-invasive PPV has found widespread acceptance in the management of acute symptomatic left heart failure, and would ostensibly have similar haemodynamic effects as its invasive counterpart.
INVASIVE PPV IN SEVERE SYSTOLIC HEART FAILURE
Although there is near-universal use of non-invasive PPV in patients with acute pulmonary oedema, there is more concern in employing invasive PPV with PEEP in this clinical scenario owing to its potentially significant haemodynamic impact. However, a number of reports in patients with severe LV dysfunction and cardiogenic shock suggest that the haemodynamic effects of PEEP may work in favour of the patient with severe left heart failure (see table 2).
Table 2.
Studies showing safety of positive end-expiratory pressure (PEEP) in patients with severe left ventricular (LV) dysfunction
| Study | n | Description of study | Patient groupings | Definition of LV dysfunction | Amount of PEEP (cm H2O) | Cardiopulmonary changes with PEEP |
|---|---|---|---|---|---|---|
| Grace and Greenbaum38 | 21 | Medical ICU; titration of PEEP to maximal CO | Divided by PCWP (≤12, 14–18, ≥19) | AMI, CS or CHF requiring MV | 0–8 | CO increase in 12/13 of patients with PCWP ≥19 |
| Mathru et al,54 | 290 | Surgical ICU, post CABG; MV by CMV, IMV or IMV +PEEP | Divided by EF and LVEDP | EF <60% (mean 34%) and LVEDP >16 Torr (mean 19) | 5 | Improvement in RAP, PCWP, CI, SI |
| Dongelmans, 198610 | 121 | Surgical ICU, post CABG; MV with high versus low PEEP | High (10) versus Low (5) PEEP | None provided | 5–10 | Improved lung compliance, PaO2 and decreased need for supplemental O2 on discharge, but longer duration of MV |
| Malbouisson et al,55 | 10 | Surgical ICU, post CABG; recruitment manoeuvres with high PEEP | – | Requirement of inotropic support for CS (CI <2.5) | Up to 40 | Improved PaO2/FIO2, reduced intrapulmonary shunting, no decrease in MAP or CI |
| Kontoyannis et al,39 | 28 | Medical ICU; patients with myocardial infarction complicated by CS requiring IABP | IABP alone versus IABP plus elective MV+PEEP | Systolic blood pressure <80 mm Hg with end organ damage | 10 | Improved ability to wean mechanical support (90% vs 56%), PCWP, CI, UO and discharge survival (80% vs 28%) |
AMI, acute myocardial infarction; CABG, coronary artery bypass graft; CHF, congestive heart failure; CI, cardiac index; CMV, controlled mechanical ventilation; CO, cardiac output; CS, cardiogenic shock; EF, ejection fraction; IABP, intra-aortic balloon pump; ICU, intensive care unit; IMV, intermittent mechanical ventilation; LVEDP, left ventricular end diastolic pressure; MAP, mean arterial pressure; MV, mechanical ventilation; PCWP, pulmonary capillary blood pressure; RAP, right atrial pressure; SI, stroke index; UO, urine output.
In a study of 21 mechanically ventilated patients with LV dysfunction of diverse aetiologies (7 had acute MI with CHF, 8 had acute MI with cardiogenic shock and 6 had CHF without acute MI),38 initiation of PEEP led to decreased CO in patients with normal pulmonary capillary wedge pressure (PCWP). However, 4 of 6 patients with a PCWP of 14–18 mm Hg and 12 out of 13 patients with a PCWP ≥19 mm Hg experienced improvement in their CO with the addition of 3–8 cm H2O of PEEP. Similarly, in 12 patients with baseline LV dysfunction who were mechanically ventilated after coronary artery bypass graft surgery, the initiation of 5 cm H2O of PEEP (in either controlled or intermittent mechanical ventilation) was associated with a significant improvement in the PCWP, cardiac index and stroke index compared with spontaneous or intermittent ventilation without PEEP.54 The authors’ conclusion was that PEEP should be used in all the cases of severe LV dysfunction. These results are consistent with the finding that, in mechanically ventilated patients with cardiogenic shock after coronary artery bypass graft surgery, the usage of 10 cm H2O of PEEP can decrease intrapulmonary shunting and improve the lung compliance, and that alveolar recruitment manoeuvres with high levels of PEEP are successful in improving oxygenation and atelectasis without any concomitant detrimental changes in haemodynamics.12,55,56
Mechanical ventilation with PEEP has not only been associated with improved haemodynamic measurements, but also with superior clinical end points as well. A small study of 18 patients with cardiogenic shock necessitating intra-aortic balloon pump placement found that the patients randomised to receive elective mechanical ventilation with 10 cm H2O of PEEP were more likely to be weaned off the intra-aortic balloon pump and survive to discharge than patients who received oxygen supplementation alone.57 In addition, several clinical variables were improved in the mechanically ventilated patients as well, such as urine output, PCWP, cardiac index, ratio of partial pressure of arterial oxygen to the fraction of inspired oxygen (PaO2/FIO2) and usage of vasopressors and inotropes. Of note, this is the only study to measure patient survival, rather than surrogate clinical or haemodynamic end points, in evaluating this query.
While these results are promising and suggest potential benefit for PEEP beyond respiratory support, other studies have not shown haemodynamic improvement with the use of PEEP.58,59 Of note, these authors found that PEEP was not associated with a functional decline in LV function at high levels of PEEP, and it was therefore considered safe in these group of patients.
CONCLUSION
As with any intervention, PEEP has a broad spectrum of haemodynamic consequences, which can be alternatively favourable or unfavourable depending on the clinical scenario in which it is used.
Although the use of PEEP in patients with severe left systolic heart failure, acute MI and cardiogenic shock will always require clinical judgement, based on our review of the literature, we conclude that most patients will benefit from its use. Indeed, the clinical data suggest that, in addition to being safe, moderate levels of PEEP may provide haemodynamic and oxygenation benefits in LV failure exhibiting afterload-dependent physiology. However, in certain scenarios, extra caution must be taken. Specifically, in patients who manifest preload-dependent LV function, particularly those who experience RV infarcts or have hypovolaemia, care must be exercised to ensure that cardiac under-filling does not occur with the decreased venous return which accompanies PEEP (see table 3).6,14 It is not uncommon to observe in clinical practice that patients who are “preload dependent” significantly improve their haemodynamics after the removal of PEEP. If PEEP is used for alveolar recruitment, ventricular preload should be optimised to minimise risk of haemodynamic insult.55 (The ideal measure of preload optimisation has been subject to significant debate in the recent literature, and a number of static and dynamic parameters have been proposed as accurate measures of a patient’s volume status and fluid responsiveness.7,60,61) Similarly, PEEP can have adverse haemodynamic effects when coupled with afterload-induced RV dysfunction.6,14 Thus, the thoughtful clinician should be mindful of the specific clinical scenario and implement PEEP in situations where it has shown clinical benefit, and, conversely, minimise its use in situations where it has proven adverse effects (see figure 3).
Table 3.
Management of positive end-expiratory pressure (PEEP) based on aetiology of shock
| Type of shock | Potential drawback to PEEP | Means of monitoring and compensating |
|---|---|---|
| Hypovolemic | ↓ RV and LV preload can lead to ↓ CO and worsening of hypotension | Ensure adequate volume resuscitation; carefully monitor BP |
| Cardiogenic | Although the ↓ LV afterload will ↑CO, the ↓ RV and LV preload may ↓ CO to a greater degree | Ensure that the patient does not have concomitant hypovolaemia |
| Distributive | ↓ RV and LV preload can lead to ↓ CO and worsening of hypotension | Ensure adequate volume resuscitation; carefully monitor BP |
| Obstructive | ↑ RV afterload may precipitously ↓ CO in light of ↓ RV and LV preload | Vigorous hydration and vasopressor support may be necessary to maintain haemodynamic regulation |
BP, blood pressure; CO, cardiac output; LV, left ventricular; RV, right ventricular.
Figure 3.
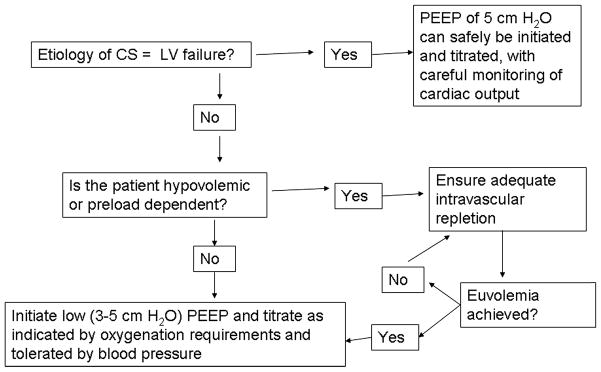
Algorithm for management of PEEP in cardiogenic shock. CS, cardiogenic shock; LV, left ventricle; PEEP, positive end-expiratory pressure.
Acknowledgments
The authors thank Dr Eduardo Mireles-Cabodevila for his thoughtful comments.
Footnotes
Contributors All authors contributed to the planning of the manuscript. JW and MO composed the manuscript, tables and figures, and inserted the relevant editions. ART, VM and RWA edited the manuscript, tables and figures. JW is the guarantor of the manuscript and its content.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
References
- 1.Weir RA, McMurray JJ, Velazquez EJ. Epidemiology of heart failure and left ventricular systolic dysfunction after acute myocardial infarction: prevalence, clinical characteristics, and prognostic importance. Am J Cardiol. 2006;97:13F–25F. doi: 10.1016/j.amjcard.2006.03.005. [DOI] [PubMed] [Google Scholar]
- 2.Kouraki K, Schneider S, Uebis R, et al. Characteristics and clinical outcome of 458 patients with acute myocardial infarction requiring mechanical ventilation. Results of the BEAT registry of the ALKK-study group. Clin Res Cardiol. 2011;100:235–9. doi: 10.1007/s00392-010-0235-6. [DOI] [PubMed] [Google Scholar]
- 3.Drakos SG, Bonios MJ, Anastasiou-Nana MI, et al. Long-term survival and outcomes after hospitalization for acute myocardial infarction complicated by cardiogenic shock. Clin Cardiol. 2009;32:E4–8. doi: 10.1002/clc.20488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lesage A, Ramakers M, Daubin C, et al. Complicated acute myocardial infarction requiring mechanical ventilation in the intensive care unit: prognostic factors of clinical outcome in a series of 157 patients. Crit Care Med. 2004;32:100–5. doi: 10.1097/01.CCM.0000098605.58349.76. [DOI] [PubMed] [Google Scholar]
- 5.Kuch B, Bolte HD, Hoermann A, et al. What is the real hospital mortality from acute myocardial infarction? Epidemiological vs clinical view. Eur Heart J. 2002;23:714–20. doi: 10.1053/euhj.2001.2947. [DOI] [PubMed] [Google Scholar]
- 6.Feihl F, Broccard AF. Interactions between respiration and systemic hemodynamics. Part II: practical implications in critical care. Intensive Care Med. 2009;35:198–205. doi: 10.1007/s00134-008-1298-y. [DOI] [PubMed] [Google Scholar]
- 7.Pinsky MR. Cardiovascular issues in respiratory care. Chest. 2005;128:592S–7S. doi: 10.1378/chest.128.5_suppl_2.592S. [DOI] [PubMed] [Google Scholar]
- 8.Tobin MJ. Mechanical ventilation. N Engl J Med. 1994;330:1056–61. doi: 10.1056/NEJM199404143301507. [DOI] [PubMed] [Google Scholar]
- 9.Manzano F, Fernandez-Mondejar E, Colmenero M, et al. Positive-end expiratory pressure reduces incidence of ventilator-associated pneumonia in nonhypoxemic patients. Crit Care Med. 2008;36:2225–31. doi: 10.1097/CCM.0b013e31817b8a92. [DOI] [PubMed] [Google Scholar]
- 10.Smith TC, Marini JJ. Impact of PEEP on lung mechanics and work of breathing in severe airflow obstruction. J Appl Physiol. 1988;65:1488–99. doi: 10.1152/jappl.1988.65.4.1488. [DOI] [PubMed] [Google Scholar]
- 11.Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA. 2002;287:345–55. doi: 10.1001/jama.287.3.345. [DOI] [PubMed] [Google Scholar]
- 12.Dongelmans DA, Hemmes SN, Kudoga AC, et al. Positive end-expiratory pressure following coronary artery bypass grafting. Minerva Anestesiol. 2012;78:790–800. [PubMed] [Google Scholar]
- 13.Esan A, Hess DR, Raoof S, et al. Severe hypoxemic respiratory failure: part 1—ventilatory strategies. Chest. 2010;137:1203–16. doi: 10.1378/chest.09-2415. [DOI] [PubMed] [Google Scholar]
- 14.Duke GJ. Cardiovascular effects of mechanical ventilation. Crit Care Resusc. 1999;1:388–99. [PubMed] [Google Scholar]
- 15.Brower RG, Lanken PN, MacIntyre N, et al. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351:327–36. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 16.Malo J, Ali J, Wood LD. How does positive end-expiratory pressure reduce intrapulmonary shunt in canine pulmonary edema? J Appl Physiol. 1984;57:1002–10. doi: 10.1152/jappl.1984.57.4.1002. [DOI] [PubMed] [Google Scholar]
- 17.Gall SA, Jr, Olsen CO, Reves JG, et al. Beneficial effects of endotracheal extubation on ventricular performance. Implications for early extubation after cardiac operations. J Thorac Cardiovasc Surg. 1988;95:819–27. [PubMed] [Google Scholar]
- 18.Guyton AC, Lindsey AW, Abernathy B, et al. Venous return at various right atrial pressures and the normal venous return curve. Am J Physiol. 1957;189:609–15. doi: 10.1152/ajplegacy.1957.189.3.609. [DOI] [PubMed] [Google Scholar]
- 19.Pinsky MR. Determinants of pulmonary arterial flow variation during respiration. J Appl Physiol. 1984;56:1237–45. doi: 10.1152/jappl.1984.56.5.1237. [DOI] [PubMed] [Google Scholar]
- 20.Pinsky MR. Instantaneous venous return curves in an intact canine preparation. J Appl Physiol. 1984;56:765–71. doi: 10.1152/jappl.1984.56.3.765. [DOI] [PubMed] [Google Scholar]
- 21.Rankin JS, Olsen CO, Arentzen CE, et al. The effects of airway pressure on cardiac function in intact dogs and man. Circulation. 1982;66:108–20. doi: 10.1161/01.cir.66.1.108. [DOI] [PubMed] [Google Scholar]
- 22.Cournand A, Motley HL. Physiological studies of the effects of intermittent positive pressure breathing on cardiac output in man. Am J Physiol. 1948;152:162–74. doi: 10.1152/ajplegacy.1947.152.1.162. [DOI] [PubMed] [Google Scholar]
- 23.Beyer J, Beckenlechner P, Messmer K. The influence of PEEP ventilation on organ blood flow and peripheral oxygen delivery. Intensive Care Med. 1982;8:75–80. doi: 10.1007/BF01694870. [DOI] [PubMed] [Google Scholar]
- 24.Cassidy SS, Mitchell JH, Johnson RL., Jr Dimensional analysis of right and left ventricles during positive-pressure ventilation in dogs. Am J Physiol. 1982;242:H549–56. doi: 10.1152/ajpheart.1982.242.4.H549. [DOI] [PubMed] [Google Scholar]
- 25.Jardin F, Farcot JC, Boisante L, et al. Influence of positive end-expiratory pressure on left ventricular performance. N Engl J Med. 1981;304:387–92. doi: 10.1056/NEJM198102123040703. [DOI] [PubMed] [Google Scholar]
- 26.Albert RK. Least PEEP: primum non nocere. Chest. 1985;87:2–4. doi: 10.1378/chest.87.1.2. [DOI] [PubMed] [Google Scholar]
- 27.Suter PM, Fairley B, Isenberg MD. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975;292:284–9. doi: 10.1056/NEJM197502062920604. [DOI] [PubMed] [Google Scholar]
- 28.Calvin JE, Driedger AA, Sibbald WJ. Positive end-expiratory pressure (PEEP) does not depress left ventricular function in patients with pulmonary edema. Am Rev Respir Dis. 1981;124:121–8. doi: 10.1164/arrd.1981.124.2.121. [DOI] [PubMed] [Google Scholar]
- 29.Johnston WE, Vinten-Johansen J, Santamore WP, et al. Mechanism of reduced cardiac output during positive end-expiratory pressure in the dog. Am Rev Respir Dis. 1989;140:1257–64. doi: 10.1164/ajrccm/140.5.1257. [DOI] [PubMed] [Google Scholar]
- 30.Schulman DS, Biondi JW, Zohgbi S, et al. Left ventricular diastolic function during positive end-expiratory pressure. Impact of right ventricular ischemia and ventricular interaction. Am Rev Respir Dis. 1992;145:515–21. doi: 10.1164/ajrccm/145.3.515. [DOI] [PubMed] [Google Scholar]
- 31.Hevroy O, Reikeras O, Grundnes O, et al. Cardiovascular effects of positive end-expiratory pressure during acute left ventricular failure in dogs. Clin Physiol. 1988;8:287–301. doi: 10.1111/j.1475-097x.1988.tb00271.x. [DOI] [PubMed] [Google Scholar]
- 32.Rasanen J, Nikki P, Heikkila J. Acute myocardial infarction complicated by respiratory failure. The effects of mechanical ventilation. Chest. 1984;85:21–8. doi: 10.1378/chest.85.1.21. [DOI] [PubMed] [Google Scholar]
- 33.Fessler HE, Brower RG, Wise RA, et al. Mechanism of reduced LV afterload by systolic and diastolic positive pleural pressure. J Appl Physiol. 1988;65:1244–50. doi: 10.1152/jappl.1988.65.3.1244. [DOI] [PubMed] [Google Scholar]
- 34.Buda AJ, Pinsky MR, Ingels NB, Jr, et al. Effect of intrathoracic pressure on left ventricular performance. N Engl J Med. 1979;301:453–9. doi: 10.1056/NEJM197908303010901. [DOI] [PubMed] [Google Scholar]
- 35.Beyar R, Goldstein Y. Model studies of the effects of the thoracic pressure on the circulation. Ann Biomed Eng. 1987;15:373–83. doi: 10.1007/BF02584291. [DOI] [PubMed] [Google Scholar]
- 36.Peters J, Kindred MK, Robotham JL. Transient analysis of cardiopulmonary interactions. II. Systolic events. J Appl Physiol. 1988;64:1518–26. doi: 10.1152/jappl.1988.64.4.1518. [DOI] [PubMed] [Google Scholar]
- 37.Pinsky MR, Matuschak GM, Bernardi L, et al. Hemodynamic effects of cardiac cycle-specific increases in intrathoracic pressure. J Appl Physiol. 1986;60:604–12. doi: 10.1152/jappl.1986.60.2.604. [DOI] [PubMed] [Google Scholar]
- 38.Grace MP, Greenbaum DM. Cardiac performance in response to PEEP in patients with cardiac dysfunction. Crit Care Med. 1982;10:358–60. doi: 10.1097/00003246-198206000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Aubier M, Lecocguic Y, Murciano D, et al. Function of the respiratory muscles in acute cardiac decompensation. Schweiz Med Wochenschr. 1985;115:190–3. [PubMed] [Google Scholar]
- 40.Mathru M. Mechanical breath. Non-pharmacologic support for a failing heart? Chest. 1984;85:1. doi: 10.1378/chest.85.1.1. [DOI] [PubMed] [Google Scholar]
- 41.Viires N, Sillye G, Aubier M, et al. Regional blood flow distribution in dog during induced hypotension and low cardiac output. Spontaneous breathing versus artificial ventilation. J Clin Invest. 1983;72:935–47. doi: 10.1172/JCI111065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peters J, Ihle P. Coronary and systemic vascular response to inspiratory resistive breathing. J Appl Physiol. 1992;72:905–13. doi: 10.1152/jappl.1992.72.3.905. [DOI] [PubMed] [Google Scholar]
- 43.Peters J. Mechanical ventilation with PEEP—a unique therapy for failing hearts. Intensive Care Med. 1999;25:778–80. doi: 10.1007/s001340050952. [DOI] [PubMed] [Google Scholar]
- 44.Qvist J, Pontoppidan H, Wilson RS, et al. Hemodynamic responses to mechanical ventilation with PEEP: the effect of hypervolemia. Anesthesiology. 1975;42:45–55. doi: 10.1097/00000542-197501000-00009. [DOI] [PubMed] [Google Scholar]
- 45.Harken AH, Brennan MF, Smith B, et al. The hemodynamic response to positive end-expiratory ventilation in hypovolemic patients. Surgery. 1974;76:786–93. [PubMed] [Google Scholar]
- 46.Park M, Sangean MC, de Volpe MS, et al. Randomized, prospective trial of oxygen, continuous positive airway pressure, and bilevel positive airway pressure by face mask in acute cardiogenic pulmonary edema. Crit Care Med. 2004;32:2407–15. doi: 10.1097/01.ccm.0000147770.20400.10. [DOI] [PubMed] [Google Scholar]
- 47.Takeda S, Nejima J, Takano T, et al. Effect of nasal continuous positive airway pressure on pulmonary edema complicating acute myocardial infarction. Jpn Circ J. 1998;62:553–8. doi: 10.1253/jcj.62.553. [DOI] [PubMed] [Google Scholar]
- 48.Pang D, Keenan SP, Cook DJ, et al. The effect of positive pressure airway support on mortality and the need for intubation in cardiogenic pulmonary edema: a systematic review. Chest. 1998;114:1185–92. doi: 10.1378/chest.114.4.1185. [DOI] [PubMed] [Google Scholar]
- 49.Mehta S. Continuous versus bilevel positive airway pressure in acute cardiogenic pulmonary edema? A good question! Crit Care Med. 2004;32:2546–8. doi: 10.1097/01.ccm.0000142946.76136.5c. [DOI] [PubMed] [Google Scholar]
- 50.Rasanen J, Vaisanen IT, Heikkila J, et al. Acute myocardial infarction complicated by left ventricular dysfunction and respiratory failure. The effects of continuous positive airway pressure. Chest. 1985;87:158–62. doi: 10.1378/chest.87.2.158. [DOI] [PubMed] [Google Scholar]
- 51.Masip J. Noninvasive ventilation in acute cardiogenic pulmonary edema. Curr Opin Crit Care. 2008;14:531–5. doi: 10.1097/MCC.0b013e32830c4862. [DOI] [PubMed] [Google Scholar]
- 52.Bendjelid K, Schutz N, Suter PM, et al. Does continuous positive airway pressure by face mask improve patients with acute cardiogenic pulmonary edema due to left ventricular diastolic dysfunction? Chest. 2005;127:1053–8. doi: 10.1378/chest.127.3.1053. [DOI] [PubMed] [Google Scholar]
- 53.Agarwal R, Gupta D. Is the decrease in LVEDV the mechanism of action of continuous positive airway pressure in diastolic heart failure? Chest. 2005;128:1891. doi: 10.1378/chest.128.3.1891. author reply 1891–2. [DOI] [PubMed] [Google Scholar]
- 54.Mathru M, Rao TL, El-Etr AA, et al. Hemodynamic response to changes in ventilatory patterns in patients with normal and poor left ventricular reserve. Crit Care Med. 1982;10:423–6. doi: 10.1097/00003246-198207000-00001. [DOI] [PubMed] [Google Scholar]
- 55.Malbouisson LM, Brito M, Carmona MJ, et al. Hemodynamic impact of alveolar recruitment maneuver in patients evolving with cardiogenic shock in the immediate postoperative period of myocardial revascularization. Rev Bras Anestesiol. 2008;58:112–23. doi: 10.1590/s0034-70942008000200004. [DOI] [PubMed] [Google Scholar]
- 56.Marvel SL, Elliott CG, Tocino I, et al. Positive end-expiratory pressure following coronary artery bypass grafting. Chest. 1986;90:537–41. doi: 10.1378/chest.90.4.537. [DOI] [PubMed] [Google Scholar]
- 57.Kontoyannis DA, Nanas JN, Kontoyannis SA, et al. Mechanical ventilation in conjunction with the intra-aortic balloon pump improves the outcome of patients in profound cardiogenic shock. Intensive Care Med. 1999;25:835–8. doi: 10.1007/s001340050960. [DOI] [PubMed] [Google Scholar]
- 58.Maestroni A, Aliberti S, Amir O, et al. Acute effects of positive end-expiratory pressure on left ventricle diastolic function in healthy subjects. Intern Emerg Med. 2009;4:249–54. doi: 10.1007/s11739-009-0255-2. [DOI] [PubMed] [Google Scholar]
- 59.Fellahi JL, Valtier B, Beauchet A, et al. Does positive end-expiratory pressure ventilation improve left ventricular function? A comparative study by transesophageal echocardiography in cardiac and noncardiac patients. Chest. 1998;114:556–62. doi: 10.1378/chest.114.2.556. [DOI] [PubMed] [Google Scholar]
- 60.Pinsky MR. Hemodynamic evaluation and monitoring in the ICU. Chest. 2007;132:2020–9. doi: 10.1378/chest.07-0073. [DOI] [PubMed] [Google Scholar]
- 61.Durairaj L, Schmidt GA. Fluid therapy in resuscitated sepsis: less is more. Chest. 2008;133:252–63. doi: 10.1378/chest.07-1496. [DOI] [PubMed] [Google Scholar]