Abstract
Objectives:
Thoracic manipulation is widely used in physical therapy and has been shown to be effective at addressing mechanical neck pain. However, thoracic mobilization may produce similar effects. The purpose of this systematic review was to evaluate the current literature regarding the effectiveness of thoracic manipulation versus mobilization in patients with mechanical neck pain.
Methods:
ProQuest, NCBI-PubMed, APTA's Hooked on Evidence, Cochrane Library, CINAHL and SPORTDiscus were searched to identify relevant studies. Fourteen studies meeting the inclusion criteria were analyzed using the Physiotherapy Evidence Database (PEDro) scale and the GRADE approach.
Results:
The literature as assessed by the PEDro scale was fair and the GRADE method showed overall quality ranging from very low to moderate quality. The 14 included studies showed positive outcomes on cervical pain levels, range of motion, and/or disability with the use of thoracic manipulation or mobilization. There was a paucity of literature directly comparing thoracic manipulation and mobilization.
Discussion:
Current limitations in the body of research, specifically regarding the use of thoracic mobilization, limit the recommendation of its use compared to thoracic manipulation for patients with mechanical neck pain. There is, however, a significant amount of evidence, although of varied quality, for the short-term benefits of thoracic manipulation in treating patients with this condition. Further high quality research is necessary to determine which technique is more effective in treating patients with mechanical neck pain.
Keywords: Manipulation, Mechanical neck pain, Mobilization, Systematic review, Thoracic
Introduction
Neck pain is a common occurrence within the general population, estimated to affect 10% of the adult population at any given time.1 It is thought that approximately 50–70% of individuals will experience neck pain at least once during their lifetime and up to 60% of patients continue to report chronic pain 5 years after onset of symptoms.1–3 There is a tremendous economic burden associated with neck pain, resulting in increased visits to health care providers, missed work, and loss of productivity, and it is responsible for the second highest annual workers’ compensation costs in the United States.1,4–6
A common classification of neck pain is mechanical neck pain.7 Although the definition varies among different research studies, mechanical neck pain is most commonly defined as pain located in the cervical spine or cervicothoracic junction that is elicited and/or exacerbated by cervical motion and/or palpation of cervical musculature.7–12
Neck pain may be accompanied by neurological deficits and/or referred or radiating pain into the upper extremities, or headaches with a cervical origin (termed ‘cervicogenic headaches’);12,13 however, these signs/symptoms are often excluded when referring to mechanical neck pain.7 The current physical therapy clinical practice guidelines for neck pain have separated the clinical findings of patients presenting with neck pain into categories, with headaches and referred or radiating pain into the upper extremities having their own individual categories.13 Patients presenting with headaches and/or radiating pain may respond to physical therapy interventions, specifically thoracic manipulation and mobilization, differently than those with mechanical neck pain. Thus, the focus of this systematic review is mechanical neck pain, with the exclusion of radiculopathy and cervicogenic headaches.
Mechanical neck pain is commonly treated conservatively with physical therapy.2 In fact, approximately one-quarter of all patients visiting an outpatient physical therapy clinic have neck pain as their chief complaint.14 A common intervention utilized by physical therapists to address mechanical neck pain is manual therapy, which is intended to increase tissue extensibility and range of motion, mobilize or manipulate soft tissue and joints, and to decrease pain.15 Specific manual therapy techniques such as mobilization/manipulation are skilled passive movements to joints and/or related soft tissues which are applied at varying speeds and amplitudes.15
In recent years, clinicians and researchers have begun to investigate manual therapy techniques applied to the thoracic spine for the treatment of mechanical neck pain.
Although the exact mechanisms by which this approach garners positive results are not completely understood, it is widely thought that the conceptual model of regional interdependence is involved.2,16–18 This model theorizes that restrictions or dysfunction in a body region may be treated by mobilization of adjacent body segments.2 This has led to an increased focus in clinical research on treatment of biomechanically linked segments, such as treating the thoracic spine for neck pain. Neurophysiological effects may also be involved.11,16 Bialosky et al.19 proposed a model in which a mechanical stimulus (provided by a manual therapy technique) may induce neurophysiologic effects such as hypoalgesia, neuromuscular responses, endocrine responses and more via peripheral, spinal, and supraspinal mechanisms.19 Bialosky et al.19 also discuss the possibility of a combined effect of both biomechanical and neurophysiological mechanisms rather than independent effects.
There is a growing body of evidence that manual therapy directed to the thoracic spine, particularly thoracic manipulation, is effective at improving patient outcomes such as reducing pain and disability and increasing range of motion, in patients with neck pain, regardless of the number or location of cavitations achieved.3,3,7,9,16,17,20 Recent evidence seems to favor the use of thoracic high-velocity low-amplitude thrust (HVLA) manipulation over non-thrust mobilization; however, based on current evidence it is difficult to make the determination as to which is superior, as only one study, to our knowledge, has made a direct comparison between the two techniques.14
Three systematic reviews7,12,16 have been published comparing thoracic manipulation versus other controls in the treatment of mechanical neck pain. However, one of these reviews12 included cervical mobilizations and manipulations and did not exclude patients with cervicogenic headache and/or radicular symptoms. Only one systematic review12 compared thoracic manipulation to thoracic mobilization, but notably the only published study14 to directly compare the two treatments was not included in any of these reviews. No review has been published that specifically examined patient outcomes for thoracic manipulations versus thoracic mobilizations in patients with mechanical neck pain (without cervicogenic headache and/or radicular symptoms). The objective of this systematic review is to determine the effectiveness of thoracic manipulation versus thoracic mobilization in improving outcomes in patients with mechanical neck pain.
Methods
Data sources and searches
A review of six databases was conducted by four individuals (KD, NH, SS, DW) from June to September of 2012. Included databases were ProQuest, NCBI-PubMed, American Physical Therapy Association’s (APTA) Hooked on Evidence, Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and SPORTDiscus. There was no limitation in the date ranges for the search so all relevant research was included in this review. Due to the variability of the terms ‘thrust’, ‘non-thrust’, ‘mobilization’, and ‘manipulation’ used in the literature, the Boolean operator ‘OR’ was used to return all possible search results. The search terms used in all six of the databases for thoracic manipulation included: ‘(thrust OR manipulation) AND (neck OR cervical) AND thoracic’; the search terms used for mobilization included ‘(non-thrust OR mobilization) AND (neck OR cervical) AND thoracic’.
Study selection
In an effort to be as thorough as possible, databases were searched for published research of any study design and methodological quality. To be included in this systematic review, studies must have been published in English from a peer-reviewed journal. Titles and abstracts were screened for inclusion of: (1) mechanical neck pain, (2) intervention to the thoracic spine, or (3) an outcome for the neck/cervical spine. Remaining studies were excluded if they: (1) examined non-mechanical neck pain (radiculopathy, whiplash, etc), (2) utilized only non-thoracic mobilization or manipulation, (3) did not have at least one intervention in which manipulation or mobilization was directed to the thoracic spine only, or were: (4) a book review, (5) an evidence summary, (6) non-published research, (7) a systematic review of thoracic manipulation or mobilization in the treatment of mechanical neck pain, or (8) an incomplete study.
Data extraction
Studies that met eligibility criteria were screened for relevant demographic information, including sample size, age, gender, duration of symptoms, interventions, outcome measures, treatment frequency, follow-up, and controls used. As the intent of this review was to compare general outcomes, all possible outcome measures were examined. Outcome measures from all 14 studies were enumerated by two authors (KD, SS) for assessment. All relevant statistical analyses for these outcome measures were aggregated for further analysis by four individuals (KD, NH, SS, DW).
Quality assessment
To assess the quality of studies in this review, the Physiotherapy Evidence Database (PEDro) Scale was used. The PEDro scale was developed by a group of clinical trial experts in an effort to support and advance research quality of trials within Physiotherapy/Physical Therapy.21,22 It is comprised of 11 criteria designed to reflect both internal and external validity while assessing quality of clinical trials and lower level evidence.21,23 Of these 11 criteria, 10 evaluate internal validity while only one evaluates external validity. The first item of the PEDro scale is related to external validity, but as the intent of the PEDro score in its use for this review was to address the studies’ internal validity, it was not calculated in the scoring.21 If a reviewer answers ‘yes’ to a particular criterion, a score of one is given. If a reviewer answers ‘no’, a score of zero is given. Refer to Table 1 for individual criterion. After scoring the criteria in the PEDro scale, the final score is added up for that specific study, which can range from zero to 10 points.23
Table 1. PEDro scoring of included studies.
| Reference | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total score | Study quality |
| Fernández-de-las-Peñas et al.9 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9 | High |
| González-Iglesias et al.10 | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9 | High |
| Cleland et al.8 | Y | Y | Y | Y | N | Y | Y | N | Y | Y | 8 | High |
| Lau et al.20 | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 | High |
| Cleland et al.4 | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 | High |
| Cleland et al.14 | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7 | High |
| González-Iglesias et al.24 | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 | High |
| Martínez-Segura et al.11 | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 | High |
| Puentedura et al.2 | Y | Y | Y | N | N | Y | N | Y | Y | Y | 7 | High |
| Krauss et al.17 | Y | Y | Y | N | N | Y | N | N | Y | Y | 6 | Fair |
| Fernández-de-las-Peñas et al.25 | N | N | N | N | N | N | Y | Y | Y | Y | 4 | Poor |
| Savolainen et al.26 | Y | N | Y | N | N | N | N | N | Y | Y | 4 | Poor |
| Cleland et al.3 | N | N | N | N | N | N | Y | N | Y | Y | 3 | Poor |
| Ko et al.27 | N | N | Y | N | N | N | N | N | Y | Y | 3 | Poor |
| Total of ‘yes’ scores | 11 | 10 | 12 | 3 | 0 | 8 | 10 | 7 | 14 | 14 | ||
| % of ‘yes’ per criterion | 79% | 71% | 86% | 21% | 0% | 57% | 71% | 50% | 100% | 100% | ||
| Score Average | 6.36 | Fair | ||||||||||
| Standard Deviation | 2.06 | |||||||||||
Y = Criterion satisfied; N = Criterion not satisfied.
2. Subjects were randomly allocated to groups (in a crossover study, subjects were randomly allocated an order in which treatments were received).
3. Allocation was concealed.
4. The groups were similar at baseline regarding the most important prognostic indicators.
5. There was blinding of all subjects.
6. There was blinding of all therapists who administered the therapy.
7. There was blinding of all assessors who measured at least one key outcome.
8. Measurements of at least one key outcome were obtained from more than 85% of the subjects initially allocated to groups.
9. All subjects for whom outcome measurements were available received the treatment or control condition as allocated, or where this was not the case, data for at least one key outcome were analyzed by ‘intention to treat’.
10. The results of between-group statistical comparisons are reported for at least one key outcome.
11. The study provides both point measurements and measurements of variability for at least one key outcome.
Of the 14 studies selected for this systematic review, nine2,4,8,11,14,17,20,24,25 had already received a published and peer-reviewed PEDro score, with which all the current authors agreed upon individual review of the published scores.21 According to Maher23 the reliability of the PEDro scale is considered ‘fair to good’ when studies were rated by a committee. Therefore, four individuals (KD, NH, SS, DW) individually rated the remaining five studies3,9,10,26,27, and discrepancies in the scoring of four studies3,9,26,27 were resolved by discussion until a consensus was met. The trials included in this review were assigned methodological quality ratings proposed by Walser et al.16 A study was considered to be of ‘high’ quality if it received a PEDro score of seven or above.16 Similarly, a study was found to be of ‘fair’ quality if it received a score of five to six, and of ‘poor’ quality if the score was four or below.16
To assess the overall body of evidence, the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach28 was also utilized on all included studies. There are five domains used in the GRADE system, including limitations in study design, inconsistency of results, indirectness of evidence, imprecision, and reporting bias.28,29 After appraising the evidence, each outcome is classified as one of the following:28,29
High quality evidence – Further research is very unlikely to change our confidence in the estimate of effect, all domains are met
Moderate quality evidence – Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate, one of the domains is not met
Low quality evidence – Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate, two of the domains are not met
Very low quality evidence – Any estimate of effect is very uncertain, three of the domains are not met
Randomized controlled trials begin with a high quality evidence classification, but may be downgraded if one or more of the above described domains is present.28 Observational studies, on the other hand, start with a low quality evidence classification, and may be upgraded if a dose response relation is found or if the treatment effect is very large.28 Hence, although some studies may score high on the PEDro scale, it is possible that their quality rating via the GRADE approach may be low because the GRADE approach accounts for some different methodological qualities. After assessing the studies, an overall strength of recommendation for the included studies was made.
Results
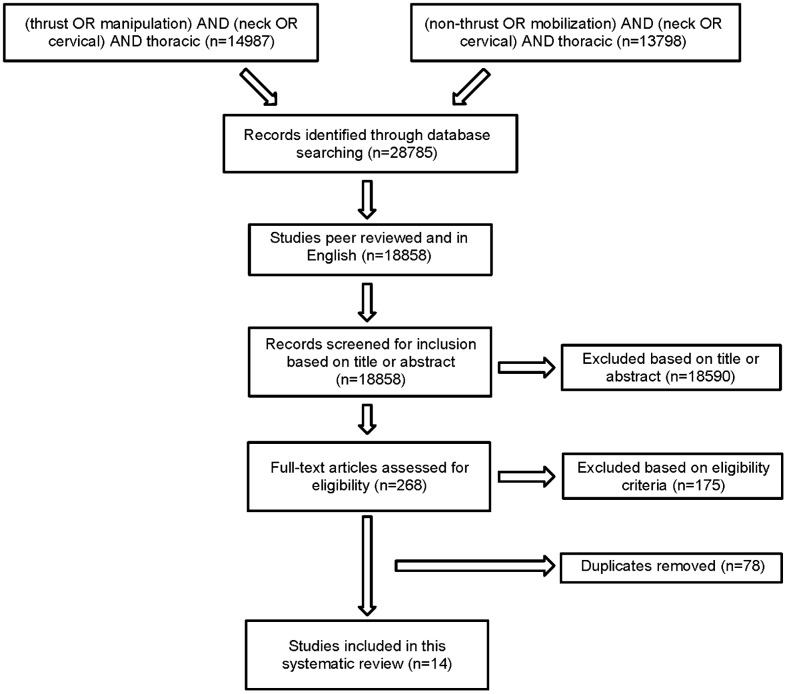
A total of 29 studies were identified for potential inclusion. After review of the abstracts, only 14 met the inclusion criteria (Fig. 1). Ten of the included studies were randomized controlled trials.2,4,8,10,11,14,17,20,24,25 The remaining four studies included one quasi-experimental study lacking randomization27, one prospective cohort study3, one case series26, and one secondary analysis of a randomized controlled trial.9 The 14 included studies had a mixed population of men and women. All of the patients were diagnosed with mechanical neck pain. Each of the patients had varying symptom duration and ages ranging from 18 to 60 years old. Thirteen different outcome measures were used across the 14 studies reviewed. The two most commonly used outcome measures in the included studies were the NPRS2–4,10,11,14,20,26 and the NDI.2–4,14,27 The physical impairment of cervical ROM was measured post-intervention in six of the studies.9–11,17,20,24,26 All of these have been shown to be reliable as measures of improvement in the clinic.30–33 Follow-up times ranged from immediately post-intervention to 6 months or longer. (Table 2)
Figure 1.
Flow diagram for study selection.
Table 2. Study characteristics.
| Article | Control group | Experimental group | Intervention | Frequency | Assessment Post-Intervention | Follow-Up | Results |
| Cleland et al.8 | n = 17 | n = 19 | Experimental: supine thoracic manipulation | One time treatment | VAS | Immediate | Manipulation: immediate reduction in pain over placebo. Experimental group averaged 15.5 mm change in VAS, placebo group averaged 4.2 mm change. |
| Control: placebo thoracic manipulation | |||||||
| Cleland et al.3 | None | n = 78 | Six thoracic manipulations per session via three different techniques and CROM exercise | 1–2 sessions maximum | GROC, NPRS, NDI | 2–4 days | Established six predictor variables. If patient = 4/6, post-test probability of success = 93%. If 3/6, post-test probability = 86% |
| Cleland et al.14 | n = 30 | n = 30 | Thoracic manipulation vs thoracic mobilization with both groups performing CROM exercise | One time treatment | NDI, NPRS | 2–4 days | Manipulation: clinically and statistically significant reductions in disability and pain and statistically significant improvement in GROC scores. |
| Cleland et al.4 | n = 70 | n = 70 | Experimental: thoracic manipulation and exercise | Experimental: two sessions of manipulation and CROM followed by three sessions of exercise | NDI, NPRS, GROC | 1 week, 4 weeks, 6 months | Manipulation: clinically significant short and long-term reduction in disability, short-term (1 week) reduction in pain and improved perceived recovery at 4 weeks and 6 months |
| Control: exercise only | Control: five sessions over 4 weeks | ||||||
| Fernández-de-las-Peñas et al.26 | None | n = 7 | Thoracic manipulation | One time treatment | NPRS, CROM | Immediate, 2 days | Manipulation: clinically and statistically significant decrease in pain immediately, which was sustained at 2-day follow-up. CROM: improvement in all motions but none were statistically significant at either follow-up. |
| Fernández-de-las-Peñas et al.9 | n = 22 | n = 23 | Experimental: thoracic manipulation once per week (1st, 3rd, and 5th sessions)+control interventions | Five sessions over 3 weeks | VAS, CROM | Immediate | Manipulation: clinically meaningful and statistically significant reduction in pain, as well as significant improved CROM (all motions) |
| Control: electrotherapy and thermotherapy program | |||||||
| González-Iglesias et al.10 | n = 22 | n = 23 | Experimental: thoracic manipulation once per week for 3 weeks+control intervention | six sessions over three consecutive weeks | NPRS, CROM, NPQ | 1 week | Manipulation: statistically significant and clinically meaningful reduction in pain and statistically significant decreased disability and improved CROM (all motions) |
| Control: electrotherapy, superficial thermotherapy+STM | |||||||
| González-Iglesias et al.24 | n = 22 | n = 23 | Experimental: thoracic manipulation once per week (1st, 3rd, and 5th session)+control intervention | five sessions over 3 weeks | VAS, CROM, NPQ | Immediate, 2 weeks, 4 weeks | Manipulation: statistically significant and clinically meaningful decrease in pain immediately and at 2 and 4 weeks. Also statistically significant improvement in CROM and disability immediately and at 2 weeks. |
| Control: electro and thermotherapy program | |||||||
| Ko et al.27 | n = 26 | n = 27 | Experimental: thoracic mobilizations+control intervention | Three times per week for 6 weeks | VAS, NDI, muscular endurance of deep cranio-cervical flexors | Immediate | Mobilization: statistically significant reduction in disability and pain as well as increased cervical muscle endurance |
| Control: cranio-cervical flexor exercises | |||||||
| Krauss et al.17 | n = 10 | n = 22 | Experimental: thoracic manipulation | One time treatment after initial evaluation | FPS, CROM | Immediate | Manipulation: statistically significant increase in bilateral cervical rotation and statistically significant improvement in pain |
| Control: no intervention | |||||||
| Lau et al.20 | n = 60 | n = 60 | Experimental: thoracic manipulation+control interventions | Two times per week for eight sessions | CV angle, NPRS, NPQ, SF36Q, CROM | Immediate, 3 months, 6 months | Manipulation: statistically significant and clinically meaningful decrease in pain immediately and up to 6 months. Statistically significant improvements in disability, CV angle and CROM at all follow-ups. |
| Control: infrared radiation therapy and a standard set of education materials | |||||||
| Martínez-Segura et al.11 | None | Cervical n = 57; Thoracic n = 33 | Cervical: midcervical, midrange manipulation; Thoracic: AP end range upper thoracic manipulation | One time treatment | PPTs, CROM, NPRS | Immediate | Thoracic group: statistically significant and clinically meaningful decrease in pain. Improvements in PPT and CROM were shown, but were not significant. |
| Puentedura et al.2 | None | Cervical n = 14; Thoracic n = 10 | Cervical: cervical manipulation; Thoracic: thoracic manipulation; | five sessions over 2 weeks | NDI, NPRS, FABQ, GROC | 1 week, 4 weeks, 6 months | Thoracic manipulation: 10% of patients met or exceeded the MDC/MCID at 4 weeks and 6 months for NDI. 40% of patients met or exceeded MDC/MCID for pain at 4 weeks whereas only 20% did so at 6 months. 20% of patients reported GROC scores equal to/greater than +5 at all follow-ups. |
| Both groups: standard exercise program | |||||||
| Savolainen et al.25 | None | Exercise group n = 32; Manipulation group n = 43 | Exercise group: program instructed by a PT; Manipulation group: four thoracic manipulations by a physiatrist | Exercise group: not stated; | VAS | 6 months, 12 months | Manipulation: statistically significant lower level of perceived worst pain at 12-month follow-up. Both groups demonstrated statistically significant decreases in muscular tenderness and tender thoracic levels at all follow-ups. |
| Manipulation group: 1 week intervals |
Note: NDI, Neck Disability Index; NPRS, Numeric Pain Rating Scale; FABQ, Fear Avoidance Beliefs Questionnaire; FABQPA, Fear Avoidance Beliefs Questionnaire physical activity subscale; GROC, Global Rating of Change; FPS, Faces Pain Scale; CROM, Cervical Range of Motion; VAS, Visual Analog Scale; NPQ, Northwick Park Neck Disability Questionnaire; CV Angle, Craniovertebral Angle; SF36Q, SF-36 Health Questionnaire; PPTs, Pressure Pain Thresholds.
Methodological quality assessment
PEDro scores for each study are presented in Table 1. The scores of the included studies ranged from two to nine with a mean score of 6.36 (SD 2.06), indicating that the average quality of the included research is ‘fair’. Nine2,4,8–11,14,20,24 studies were found to be of ‘high’ quality, one17 of ‘fair’ quality, and four3,25–27 of ‘poor’ quality. Two PEDro criteria were seen in all of the included studies: comparing between groups and reporting of point measures and variability.2–4,8–11,14,17,20,24–27 None of the studies blinded the treating clinicians and only three met criterion five5,9,10 regarding blinding of subjects. Blinding of the treating clinicians, of course, is not feasible in studies involving manual therapy.
The quality assessment also included classifying the evidence according to the GRADE approach.28,29 The literature is sparse for direct comparisons between thoracic manipulation and mobilization, as well as for the use of thoracic mobilization. There are several studies that utilize thoracic manipulation, but most are in conjunction with another intervention.2–4,8–11,17,20,24–26
The lone study14 we found that directly compared thoracic manipulation to mobilization was of moderate quality via the GRADE assessment, and the one study that included thoracic mobilization27 was very low quality evidence according to the GRADE criteria. All of the other included studies2–4,8–11,17,20,24–26 incorporating manipulation compared it to another intervention, and their quality ranged from very low to moderate.
From the GRADE assessment, an overall strength of recommendation for the included studies was determined, which ranged from very low to high. Although the quality of five studies9,10,14,20,24 was moderate, the recommendation is high because four10,14,20,24 of the five studies were randomized controlled trials, all were without serious limitations, and all had significant findings in their assessed outcomes. Conversely, three studies3,17,26 were of low quality evidence as per the GRADE method, but the strength of recommendation is very low because the evidence is from a prospective cohort study3, a case series26, and only one randomized controlled trial17, all with low PEDro scores and study limitations. See Table 3 for the GRADE classification of evidence and strength of recommendation for all included studies.
Table 3. GRADE scoring of included studies.
| Intervention | Outcomesassessed | Trial limitations | Inconsistency | Indirectness | Imprecision | Publication bias | GRADE quality of evidence | Strength of recommendation |
| Thoracic manipulation versus mobilization14 | Disability pain | None | N/A | No indirectness | -1# | None | Moderate | High |
| Manipulation with modality versus modality9,10,20,24 | CV Angle pain CROM | None | No inconsistency | −1 ˆ | No imprecision | None | Moderate | High |
| Thoracic manipulation versus cervical manipulation11 | Pain | None | N/A | No indirectness | −1# | None | Moderate | Moderate |
| Thoracic manipulation with exercise2,4 | Disability pain | None | −1x | −1 ˆ</noteref> | No imprecision | None | Low | Low |
| Thoracic manipulation versus placebo thoracic manipulation8 | Pain | None | N/A | −1 ˆ | −1# | None | Low | Low |
| Thoracic manipulation only3,17,26 | Disability pain CROM | −1* | No inconsistency | −1 ˆ | No imprecision | None | Low | Very low |
| Thoracic manipulation versus exercise25 | Pain CROM | −1* | N/A | −1 ˆ | −1# | None | Very low | Very low |
| Thoracic mobilization with exercise27 | Disability pain | −1* | N/A | −1 ˆ | −1# | None | Very low | Very low |
CROM, Cervical Range of Motion; CV Angle, Craniovertebral Angle; N/A, Not Applicable.
*Quality point deducted for high risk of bias (PEDro score<6/10).29
xQuality point deducted for conflicting results between studies, leading to inconsistency.29
ˆQuality point deducted for indirectness from comparison/control group receiving intervention that is expected to be less effective than standard treatment and/or inclusion of a co-intervention (i.e. exercise, modality).
#Quality point deducted for imprecision due to only one study reporting data.29
Thoracic manipulation vs thoracic mobilization
Cleland et al.14 (PEDro score = 7) was the only study we found that directly compared thoracic manipulation to thoracic mobilization, with each group having 30 subjects. The results demonstrated clinically and statistically significant reductions in disability (P<0.001) and pain (P<0.001), as well as statistically significantly increased perceived recovery (P<0.01) at 2–4-day follow-up for the manipulation group. In addition, no significant differences were observed in the number of side effects experienced by the manipulation or mobilization groups. The reported side effects included aggravation of symptoms, muscle spasm, neck stiffness, headache, and radiating symptoms.14
Thoracic manipulation
Four studies9,10,20,24 utilized thoracic manipulation with modalities compared to a modality only or a modality and education group. The sample sizes ranged from 459,10,24 to 120 patients.20 González-Iglesias et al.10 (PEDro score = 9) and Lau et al.20 (PEDro score = 8) demonstrated that the thoracic manipulation groups experienced significant and clinically meaningful decreases in pain at 1 week10 (P<0.001) and up to 6 months20 follow-up (P<0.05), whereas Fernández-de-las-Peñas et al.9 (PEDro score = 9) and González-Iglesias et al.24 (PEDro score = 7) demonstrated a significant and clinically meaningful improvement in pain immediately9,24 (P<0.001) and at 2- and 4-week follow-ups (P<0.001).24 Three of the studies10,20,24 also demonstrated statistically significant improvements in disability at follow-ups ranging from immediately post-intervention (P<0.00124, P = 0.01820), one week (P<0.001)10 and up to 6 months duration (P = 0.007).20 Lau et al.20 demonstrated statistically significant improvements in the cranio-vertebral angle up to 6 months post-treatment and in health-related quality of life throughout the study. All four of the studies9,10,20,24 demonstrated statistically significant increases in cervical range of motion (P<0.001,9,10 P<0.05).20,24
Cleland et al.8 (PEDro score = 8) compared thoracic manipulation to a placebo intervention in 36 patients. The study demonstrated a significant and clinically meaningful improvement in pain immediately post-intervention for the 19 patients in the thoracic manipulation group (P<0.001).
Cleland et al.4 (PEDro score = 7) and Puentedura et al.2 (PEDro score = 7) examined the use of thoracic manipulation along with an exercise regimen. Puentedura et al.2 also included a cervical manipulation group, but for the purpose of this review, only the thoracic manipulation data were extracted. Cleland et al.4 found that the 70 patients receiving manipulation experienced clinically and statistically greater short and long-term reduction in disability (P = 0.003 at 1 week, P = 0.001 at 4 weeks, P<0.001 at 6 months) and short-term reduction in pain (P<0.001 at 1 week) than the 70 patients given the exercise regimen. In addition, although there was no significant difference in perceived recovery between groups at 1-week follow-up, the manipulation group demonstrated clinically and statistically significant improvement at both 4-week (P = 0.01) and 6-month follow-ups (P value not reported). Puentedura et al.2 found that only one of the 10 patients in the thoracic manipulation and exercise group experienced statistically significant and clinically meaningful reductions in disability upon follow-up at 4 weeks and 6 months (P value not reported). Forty percent of patients experienced clinically and statistically significant reductions in pain at the 4-week follow-up but this decreased to 20% by 6 months (P value not reported). In addition, only 20% of the patients in the thoracic manipulation group demonstrated a clinically and statistically significant improvement in perceived recovery at all follow-up intervals (P value not reported).
Martínez-Segura et al.11 (PEDro score = 7) compared the short-term effects of thoracic manipulation to cervical spine manipulation on patients’ pressure pain threshold (cervical spine, lateral epicondyle, and tibialis anterior), pain levels, and cervical range of motion in 90 patients. For the purpose of this review, only the thoracic manipulation data were extracted. The 33 patients in the thoracic manipulation group demonstrated a statistically significant and clinically meaningful decrease in pain (P<0.001) immediately post intervention. Although this study demonstrated improvements in pressure pain thresholds and active cervical range of motion, these improvements were not statistically significant.
Two studies, a randomized clinical trial by Krauss et al.17 (PEDro score = 6) and a case series by Fernandez et al.26 (PEDro score = 4), utilized a single thoracic manipulation without any supplemental exercise program. Fernandez et al.26 included seven patients in their study and demonstrated increases in all cervical ranges of motion, but none of these were statistically significant (P<0.05). The 22 patients in the experimental group in the Krauss et al.17 study demonstrated statistically significant increases in bilateral cervical rotation immediately post intervention (P<0.05). In addition, Krauss et al.17 exhibited statistically significantly decreased pain immediately post intervention (P<0.05), while the Fernandez et al.26 patients demonstrated both clinically and statistically significant decrease in pain immediately post intervention (P<0.001). The Fernandez et al.26 subjects maintained this significant decrease in pain two days post intervention.
Savolainen et al.25 (PEDro score = 4) compared a thoracic manipulation group of 43 patients to an exercise only group of 32 patients. Patients in the manipulation group demonstrated statistically significantly lower pain levels at 12-month follow-up (P<0.05). Additionally, both the thoracic manipulation and exercise groups demonstrated statistically significant decreases in muscular tenderness and tender thoracic levels at 6 and 12-month follow-ups (P<0.001). However, 34 drop-out subjects who attended the 12-month follow-up demonstrated similar improvements as well, with no significant differences noted between all three groups.
A clinical prediction rule derivation study including 78 patients by Cleland et al.3 (PEDro score = 3) aimed to identify patients with mechanical neck pain most likely to benefit from thoracic manipulation. This study demonstrated that if subjects met three out of six specific criteria, the post-manipulation probability of perceived recovery increased from 54 to 86%. The probability of perceived recovery increased even higher to 93% if subjects met four out of the six criteria.
Thoracic mobilization
One of the lowest quality studies utilized in this review investigated thoracic mobilization. Ko et al.27 (PEDro score = 3) examined the use of thoracic mobilization. Ko et al.27 compared thoracic spine mobilization and cranio-cervical flexor exercises to exercise alone in 53 patients. The mobilization with exercise group demonstrated a clinically and statistically significant reduction in neck disability, statistically significant reduced pain and increased cervical muscle endurance compared to the exercise only group (P<0.05).
Discussion
Due to the noticeable paucity of high level research addressing thoracic mobilization to treat mechanical neck pain, the quality of the evidence included in this review is considered to be ‘fair’ with the use of the PEDro scale. The GRADE method was also used to examine the quality of evidence and then determine an overall recommendation of the strength of intervention for the included studies. The quality of evidence ranged from very low to moderate, but the strength of recommendations regarding the studies ranged from very low to high.
There were various issues with blinding in many of the included studies.2,4,8–11,17,20,24 The absence of blinding in these studies introduces the potential for multiple biases, including cointervention and expectation biases and could result in an exaggerated or diminished treatment effect.34–36
The studies in this review included follow-ups ranging from immediately post-intervention to 12 months duration. However, only four of the studies2,4,20,25 reported follow up data after 1 month, significantly limiting the evidence for long-term outcomes. Additionally, multiple issues related to limited sampling were evident in the included studies. Only four of the studies2,4,14,17 collected data at more than one clinical location, and one27 used a sample of women exclusively, thus limiting the application of the studies’ findings to a wider population.
In manual therapy, there are multiple techniques used to achieve the desired treatment effect. This was evident in the studies included in this review, as the differences seen in technique in the application of manipulation were either an anterior to posterior (AP) thoracic manipulation in supine2–4,8,11,14,17,20,26 or a seated distraction manipulation.2–4,9,10,24 One study25 did not indicate the manipulative technique utilized. At this time, the authors of this review are unaware of any published study to date that examines the effectiveness of one thoracic manipulation technique over the other. In an effort to be as inclusive as possible and in the absence of a clearly superior technique, this review included all techniques utilized. In terms of specific mobilization techniques, only two studies14,27 included mobilization. These studies utilized different techniques including central posterior to anterior (PA) mobilizations (grades III and IV) in prone14 and central anterior to posterior (AP) mobilizations (grades II and III) in supine.27
Only one study14 in this review directly compared thoracic manipulation to thoracic mobilization, demonstrating superior short-term outcomes for the manipulation group. Cleland et al.14 included 60 patients randomly assigned to either a manipulation or mobilization group. The manipulation group received one upper thoracic and one middle thoracic spine manipulation, and the mobilization group received a 3-minute treatment session of prone grade III–IV joint mobilizations from T1–T6. Both groups received a cervical AROM exercise for use at home. All patients had follow-up visits 2–4 days after intervention to complete outcome measures and a questionnaire regarding side effects from treatment. While the authors improved the generalizability of their findings by utilizing a standardized treatment program that did not target a specific segmental restriction, their failure to blind subjects, therapists, and assessors, along with the failure to collect long-term follow-up data, are significant limitations and worthwhile considerations for future studies.
When thoracic manipulation was examined along with modalities,9,10,20,24 significant short-term (up to 1 week) improvements in pain, range of motion9,10,20,24 and disability10,20,24 were shown. However, only two studies20,24 examined follow-up beyond 1 week and only one20 demonstrated long-term benefits (up to 6 months) with regards to pain, disability, range of motion, and neck posture. While three studies9,10,24 only utilized patients with acute mechanical neck pain, Lau et al.20 examined patients with chronic mechanical neck pain. In addition, three of the four studies9,10,24 excluded patients older than 45 years of age. While potential biases are present in all of the studies, particularly concerning is the timing bias evident in Lau et al.,20 as the manipulation group received more treatment time. However, all of these studies blinded the assessors and two9,10 blinded the subjects, helping to mitigate some of the potential biases.
Compared to placebo intervention, Cleland et al.8 showed that thoracic manipulation resulted in immediate improvements in pain. However, the failure to collect long-term follow-up data is a significant limitation and the utilization of subjects from only one clinic presents a significant sampling bias. In addition, the utilization of segmental mobility testing via palpation to guide the level of thoracic manipulation is problematic due to the lack of reliability in identifying segmental motion restrictions.8 Although this is common for a clinical setting and occurred in quite a few of this review’s studies, this subjects the study to measurement and proficiency biases and is a consideration for future studies.
Positive, yet conflicting, results were demonstrated when thoracic manipulation was examined along with exercise in two studies.2,4 The conflicting results may be due to different exercise regimens utilized in the studies including a lack of manual stretching in Puentedura et al.,2 as well as a difference in patients’ mean duration of symptoms (18.8 days for Puentedura et al.2 versus 63.5 days for Cleland et al.4). In addition, although Puetendura et al.2 blinded the assessors, it had a small sample size from two locations and involved treatment by only one practitioner. A study from Savolainen et al.25 included exercise, and it was rife with potential biases and thus should be interpreted judiciously. No details are provided on the manipulative techniques or exercises utilized. Particularly problematic is the fact that 34 subjects dropped out with no further information provided, introducing probable withdrawal bias. No intent to treat analysis was performed. Furthermore, in addition to a lack of blinding, no duration of symptoms was provided for the subjects.
One study11 compared thoracic manipulation to cervical manipulation with no other interventions involved. While thoracic manipulation demonstrated immediate benefits in pain reduction, no long-term follow-up was performed, only one therapist treated all the patients and no control group was utilized. In addition, only one treatment session occurred, which makes it difficult to extrapolate the results to the multiple sessions typically involved in a plan of care in the clinical setting. However, at this point no suitable dose response rate has been determined, and further research would be helpful in establishing the appropriate quantity of manual therapy that is necessary to produce a positive outcome.
When compared to no intervention at all, a single thoracic manipulation demonstrated short-term improvements in pain17,26 and range of motion;17 however, the results varied amongst the studies. Interpreting and generalizing these results is particularly problematic as Krauss et al.17 did not state the duration of their subjects’ neck pain, and Fernandez et al.26 only included seven patients and one therapist. In addition, Krauss et al.17 directed the manipulation to a thoracic segmental restriction identified through a palpatory technique whereas Fernandez et al.26 utilized a standardized manipulation for all subjects.
Although Cleland et al.3 yielded a poor rating on the PEDro scale due to PEDro’s inherent lack of fit for prospective cohort studies, it helped to identify criteria for classifying neck pain patients most appropriate for thoracic manipulation. However, this is not a validated clinical prediction rule;4 therefore, the results should be interpreted carefully. Despite a subsequent study’s failure to validate the clinical prediction rule, thoracic manipulation was still recommended for patients with mechanical neck pain.4
Significant benefits were demonstrated for thoracic mobilization,27 yet generalizing these results to the clinical setting should be done very circumspectly. Specifically, Ko et al.27 only utilized females with chronic mechanical neck pain in their patient population. In addition, they only examined the immediate effects of intervention with no further follow-up.
Limitations
Several possible limitations have emerged in this review. The lack of high quality evidence examining thoracic mobilization in the treatment of mechanical neck pain made it necessary to include lower level evidence in an attempt to establish a meaningful recommendation for clinic use and future research. The inclusion of these lower quality studies limits the strength of this review and may influence the reader’s interpretation of the information contained within. Also, due to the presence of varying methodology and an equally wide distribution of techniques, follow-up times and outcome measures utilized, it is difficult to make a specific recommendation for clinical use. Another limitation in this review is the exclusion of studies in a language other than English.
Recommendations for Future Research
It is recommended that future research directly compare the use of thoracic manipulation versus mobilization in the treatment of mechanical neck pain. Future studies also need to include long-term follow-up since the preponderance of studies in the current body of literature only examine short-term outcomes. Future study design should also include multicenter trials to help ensure that a representative sample of all mechanical neck pain patients is utilized, incorporate multiple treating clinicians to improve generalizability to the clinical setting and blind the assessor at minimum, to mitigate potential biases including expectation bias. Finally, future research needs to examine the various thoracic manipulation techniques to determine if a specific technique achieves superior patient outcomes.
Conclusion
As a result of methodological concerns associated with the current research on the use of thoracic mobilization in the treatment of mechanical neck pain, there is no definitive evidence to support its clinical efficacy. In contrast, there is a significant amount of evidence, although of varied quality, that exists to support the use of thoracic manipulation in the treatment of mechanical neck pain for short-term improvements in neck pain, range of motion, and disability. Further research will be required to explore the value of thoracic manipulation in long-term relief of mechanical neck pain.
Acknowledgments
The authors would like to thank Nate Hill, PT, DPT for his contributions with writing and research for this systematic review.
References
- 1.Sillevis R, Cleland J, Hellman M, Beekhuizen K. Immediate effects of a thoracic spine thrust manipulation on the autonomic nervous system: a randomized clinical trial. J Man Manip Ther. 2010;18:181–90. doi: 10.1179/106698110X12804993427126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puentedura EJ, Landers MR, Cleland JA, Mintken PE, Huijbregts P, Fernandez-de-Las-Peñas C. Thoracic spine thrust manipulation versus cervical spine thrust manipulation in patients with acute neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2011;41:208–20. doi: 10.2519/jospt.2011.3640. [DOI] [PubMed] [Google Scholar]
- 3.Cleland JA, Childs JD, Fritz JM, Whitman JM, Eberhart SL. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007;87:9–23. doi: 10.2522/ptj.20060155. [DOI] [PubMed] [Google Scholar]
- 4.Cleland JA, Mintken PE, Carpenter K, Fritz JM, Glynn P, Whitman J, et al. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi-center randomized clinical trial. Phys Ther. 2010;90:1239–50. doi: 10.2522/ptj.20100123. [DOI] [PubMed] [Google Scholar]
- 5.Dunning JR, Cleland JA, Waldrop MA, Arnot CF, Young IA, Turner M, et al. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2012;42:5–18. doi: 10.2519/jospt.2012.3894. [DOI] [PubMed] [Google Scholar]
- 6.Saavedra-Hernández M, Castro-Sánchez A, Arroyo-Morales M, Cleland JA, Lara-Palomo IC, Fernández-de-Las-Peñas C. Short-term effects of kinesio taping versus cervical thrust manipulation in patients with mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2012;42:724–30. doi: 10.2519/jospt.2012.4086. [DOI] [PubMed] [Google Scholar]
- 7.Cross KM, Kuenze C, Grindstaff TL, Hertel J. Thoracic spine thrust manipulation improves pain, range of motion, and self-reported function in patients with mechanical neck pain: a systematic review. J Orthop Sports Phys Ther. 2011;41:633–42. doi: 10.2519/jospt.2011.3670. [DOI] [PubMed] [Google Scholar]
- 8.Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of a thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005;10:127–35. doi: 10.1016/j.math.2004.08.005. [DOI] [PubMed] [Google Scholar]
- 9.Fernández-De-Las-Peñas C, Cleland JA, Huijbregts P, Palomeque-Del-Cerro L, González-Iglesias J. Repeated applications of thoracic spine thrust manipulation do not lead to tolerance in patients presenting with acute mechanical neck pain: a secondary analysis. J Man Manip Ther. 2009;17:154–62. doi: 10.1179/jmt.2009.17.3.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.González-Iglesias J, Fernández-de-las-Peñas C, Cleland JA, Alburquerque-Sendín F, Palomeque-del-Cerro L, Méndez-Sánchez R. Inclusion of thoracic spine thrust manipulation into an electro-therapy/thermal program for the management of patients with acute mechanical neck pain: a randomized clinical trial. Man Ther. 2009;14:306–13. doi: 10.1016/j.math.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 11.Martínez-Segura R, De-la-Llave-Rincón AI, Ortega-Santiago R, Cleland JA, Fernández-de-Las-Peñas C. Immediate changes in widespread pressure pain sensitivity, neck pain, and cervical range of motion after cervical or thoracic thrust manipulation in patients with bilateral chronic mechanical neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2012;42:806–14. doi: 10.2519/jospt.2012.4151. [DOI] [PubMed] [Google Scholar]
- 12.Gross A, Miller J, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manipulation or mobilisation for neck pain: a Cochrane review. Man Ther. 2010;15:315–33. doi: 10.1016/j.math.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 13.Childs JD, Cleland JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, et al. Neck pain: clinical practice guidelines linked to the International Classification of Functioning, Disability and Health from the Orthopedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008;38:A1–34. doi: 10.2519/jospt.2008.0303. [DOI] [PubMed] [Google Scholar]
- 14.Cleland JA, Glynn P, Whitman JM, Eberhart SL, MacDonald C, Childs JD. Short-term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: a randomized clinical trial. Phys Ther. 2007;87:431–40. doi: 10.2522/ptj.20060217. [DOI] [PubMed] [Google Scholar]
- 15.American Physical Therapy Association. Guide to Physical Therapist Practice. 2nd edn Alexandria: American Physical Therapy Association; 2003. p.110 [Google Scholar]
- 16.Walser RF, Meserve BB, Boucher TR. The effectiveness of thoracic spine manipulation for the management of musculoskeletal conditions: a systematic review and meta-analysis of randomized clinical trials. J Man Manip Ther. 2009;17:237–46. doi: 10.1179/106698109791352085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krauss J, Creighton D, Ely JD, Podlewska-Ely J. The immediate effects of upper thoracic translatoric spinal manipulation on cervical pain and range of motion: a randomized clinical trial. J Man Manip Ther. 2008;16:93–9. doi: 10.1179/106698108790818530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim G, Lee S, Jeong H. Effects of thoracic joint mobilization on dynamic stability of patients with chronic neck pain. J Phys Ther Sci. 2011;23:753–6. [Google Scholar]
- 19.Bialosky J, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14:531–8. doi: 10.1016/j.math.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lau HM, Wing TT, Lam TH. The effectiveness of thoracic manipulation on patients with chronic mechanical neck pain – a randomized controlled trial. Man Ther. 2011;16:141–7. doi: 10.1016/j.math.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 21.Physiotherapy Evidence Database. Pedro Scale. [document on the Internet] The George Institute for Global Health; 2012 [updated 2012 Nov 5; cited 2012 Nov 6]. Available from: http://www.pedro.org.au/english/downloads/pedro-scale [Google Scholar]
- 22.Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro). Aust J Physiother. 2002;48:43–9. doi: 10.1016/s0004-9514(14)60281-6. [DOI] [PubMed] [Google Scholar]
- 23.Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro Scale for rating quality of randomized controlled trials. Phys Ther. 2003;83:713–21. [PubMed] [Google Scholar]
- 24.Gonzalez-Iglesias J, Fernandez-de-las-Penas C, Cleland JA, Gutiérrez-Vega Mdel R. Thoracic spine manipulation for the management of patients with neck pain: a randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:20–7. doi: 10.2519/jospt.2009.2914. [DOI] [PubMed] [Google Scholar]
- 25.Fernández-de-las-Peñas C, Palomeque-del-Cerro L, Rodríguez-Blanco C, Gómez-Conesa A, Miangolarra-Page JC. Changes in neck pain and active range of motion after a single thoracic spine manipulation in subjects presenting with mechanical neck pain: a case series. J Manipulative Physiol Ther. 2007;30:312–20. doi: 10.1016/j.jmpt.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 26.Savolainen A, Ahlberg J, Nummila H, Nissinen M. Active or passive treatment for neck-shoulder pain in occupational health care? a randomized control trial. Occup Med. 2004;54:422–4. doi: 10.1093/occmed/kqh070. [DOI] [PubMed] [Google Scholar]
- 27.Ko T, Jeong U, Lee K. Effects of the inclusion thoracic mobilization into cranio-cervical flexor exercise in patients with chronic neck pain. J Phys Ther Sci. 2010;22:87–91. [Google Scholar]
- 28.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–26. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Furlan AD, Pennick V, Bombardier C, van Tulder M, Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine. 2009341929–41. [DOI] [PubMed] [Google Scholar]
- 30.Rehabilitation Measures Database. Numeric pain rating scale [document on the Internet]. Rehabilitation Institute of Chicago; 2010 [updated 2011 Jan 1; cited 2013 Jan 12]. Available from: http://www.rehabmeasures.org/Lists/RehabMeasures/DispForm.aspx?ID = 891 [Google Scholar]
- 31.Cleland JA, Childs JD, Whitman JM. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch Phys Med Rehabil. 2008;89:69–74. doi: 10.1016/j.apmr.2007.08.126. [DOI] [PubMed] [Google Scholar]
- 32.Audette I, Dumas JP, Côté JN, De Serres SJ. Validity and between-day reliability of the cervical range of motion (CROM) device. J Orthop Sports Phys Ther. 2010;40:318–23. doi: 10.2519/jospt.2010.3180. [DOI] [PubMed] [Google Scholar]
- 33.Pietrobon R, Coeytaux RR, Carey TS, Richardson WJ, DeVellis RF. Standard scales for measurement of functional outcome for cervical pain or dysfunction: a systematic review. Spine. 2002;27:515–22. doi: 10.1097/00007632-200203010-00012. [DOI] [PubMed] [Google Scholar]
- 34.Helewa A, Walker JM. Critical evaluation of research in physical rehabilitation. Philadelphia: Saunders; 2000. [Google Scholar]
- 35.Guyatt G, Rennie D. Users’ guide to the medical literature: a manual for evidence-based clinical practice. Chicago: AMA Press; 2002. [Google Scholar]
- 36.Licciardone JC, Russo DP. Blinding protocols, treatment credibility, and expectancy: methodological issues in clinical trials of osteopathic manipulative treatment. J Am Osteopath Assoc. 2006;106:457–63. [PubMed] [Google Scholar]