Abstract
Theories of borderline personality disorder (BPD) postulate that high-risk transactions between caregiver and child are important for the development and maintenance of the disorder. Little empirical evidence exists regarding the reciprocal effects of parenting on the development of BPD symptoms in adolescence. The impact of child and caregiver characteristics on this reciprocal relationship is also unknown. Thus, the current study examines bidirectional effects of parenting, specifically harsh punishment practices and caregiver low warmth, and BPD symptoms in girls aged 14–17 years based on annual, longitudinal data from the Pittsburgh Girls Study (N = 2,451) in the context of child and caregiver characteristics. We examined these associations through the use of autoregressive latent trajectory models to differentiate time-specific variations in BPD symptoms and parenting from the stable processes that steadily influence repeated measures within an individual. The developmental trajectories of BPD symptoms and parenting were moderately associated, suggesting a reciprocal relationship. There was some support for time-specific elevations in BPD symptoms predicting subsequent increases in harsh punishment and caregiver low warmth. There was little support for increases in harsh punishment and caregiver low warmth predicting subsequent elevations in BPD symptoms. Child impulsivity and negative affectivity, and caregiver psychopathology were related to parenting trajectories, while only child characteristics predicted BPD trajectories. The results highlight the stability of the reciprocal associations between parenting and BPD trajectories in adolescent girls and add to our understanding of the longitudinal course of BPD in youth.
Borderline personality disorder (BPD) is a severe psychological disorder that emerges by adolescence or early adulthood. It is characterized by dysfunction across emotions, behaviors, relationships, and sense of self (American Psychiatric Association, 2000). BPD is challenging for clinicians to treat and is associated with considerable impairment, including social stigma; elevated risk for suicide; and poor social, occupational, and academic outcomes (Bagge et al., 2004; Bagge, Stepp, & Trull, 2005; Bender et al., 2001; Skodol et al., 2005; Soloff, Lynch, & Kelly, 2002; Trull, Useda, Conforti, & Doan, 1997; Zweig-Frank & Paris, 2002). With suicide rates almost 50 times higher in those with BPD than in the general population (Holm & Severinsson, 2011), BPD and related impairments are a major public health concern.
Converging evidence suggests that symptoms of BPD are recognizable by adolescence, if not earlier in childhood (Beauchaine, Klein, Crowell, Derbidge, & Gatzke-Kopp, 2009; Chanen & Kaess, 2011; Ludolph et al., 1990; Miller, Muehlenkamp, & Jacobson, 2008). Although the diagnosis of BPD in adolescents has been somewhat controversial, studies indicate that BPD is highly prevalent among juvenile delinquent and inpatient adolescent populations (Miller et al., 2008). There is also evidence that adolescent BPD features resemble those in adult BPD samples, are related to concurrent distress and dysfunction, and are predictive of receiving a diagnosis of BPD in adulthood (Becker, 2000; Dell'Osso, Berlin, Serati, & Altamura, 2010; Grant et al., 2008; Grilo et al., 1995; Johnson et al., 2001; Zanarini et al., 1998). In addition, substantial temporal stability has been demonstrated among children and adolescents for dimensional measures of BPD features or underlying traits (Beauchaine et al., 2009; Bornovalova, Hicks, Iacono, & McGue, 2009; Crick, Murray-Close, & Woods, 2005; de Clercq, van Leeuwen, van den Noortgate, de Bolle, & de Fruyt, 2009; Goodman et al., 2010; Stepp, Pilkonis, Hipwell, Loeber, & Stouthamer-Loeber, 2010). Among adolescents, Bornovalova, Hicks, Patrick, Iacono, and McGue (2011) reported moderate rank-order stability in BPD features from ages 14 to 24. However, the sample showed the highest mean levels of BPD symptoms and highest mean-level stability during the period from 14 to 17 years old, with a significant decline in mean-level symptoms from ages 17 to 24, suggesting that ages 14 to 17 represents an especially high-risk period for BPD characteristics.
Adolescent girls appear to be at particularly high risk for BPD features and their detrimental consequences. Although BPD is equally prevalent among males and females in community samples (Grant et al., 2008), significantly higher rates of BPD are consistently observed among females as compared to males in both clinical and forensic populations of adolescents and adults (American Psychological Association, 2000; Sansone & Sansone, 2009a; Skodol & Bender, 2003). An estimated 31% to 61% of female conduct disordered and hospitalized adolescents meet criteria for the disorder, in contrast to 0% to 39% of their male counterparts (Eppright, Kashani, Robinson, & Reid, 1993; Grilo et al., 1995; Myers, Burkett, & Otto, 1993; for a review, see Miller et al., 2008). Evidence also shows that BPD is associated with greater distress and disability among women than among men (Grant et al., 2008), suggesting that girls may be in greatest need of prevention and treatment efforts.
Despite the prevalence and severity of BPD and its developmental course in childhood and adolescence, the development of BPD has been the focus of little empirical work. Prominent theories propose that the disorder results from a combination of temperamental factors and early experiences, particularly transactions between the child and caregivers (e.g., Bateman & Fonagy, 2003; Kernberg, 1984; Linehan, 1993). For example, the biosocial theory (Linehan, 1993) suggests that the environment and individual continuously affect one another to influence the development of BPD, emphasizing the mutually interactive, reciprocal, and interdependent nature of the individual–environment system (Linehan, 1993). According to this theory, an emotionally and behaviorally dysregulated child might challenge parents and evoke dysfunctional responses that in turn promote further dysregulation in the child. However, these theories have rarely been explored prospectively. Most research has focused on cross-sectional associations between parenting practices and BPD, with the view that parenting is a cause, but not an effect, of BPD in youth. Thus, child-driven effects on specific parenting practices have largely been ignored in this population. In addition, there has been limited longitudinal work that has tested the bidirectional relationships between these constructs and how they may change across developmental periods, such as adolescence. Therefore, we sought to extend current knowledge on the development of BPD by investigating the bidirectional associations between developmental trajectories of BPD symptoms during adolescence and specific parenting behaviors in a longitudinal study of girls. We also simultaneously tested the year-to-year variations in BPD symptoms and parenting behaviors to determine temporal precedence. That is, we examined whether time-specific elevations in BPD symptoms drive parenting behaviors or vice versa during this developmental period. We explored these bidirectional associations within the context of specific child and caregiver factors, including child temperament and parental psychopathology. We will first provide a review of evidence regarding the putative developmental antecedents (i.e., precursors and risk factors) to the development of BPD.
Developmental Antecedents to BPD
Antecedents is a broad term used here to refer to both precursors and risk factors. Precursors are early signs and symptoms that precede onset of a disorder (Eaton, Badawi, & Melton, 1995; Keenan, Loeber, & Green, 1999), and may bear resemblance to symptoms as manifested in adult disorders. However, precursors are developmentally appropriate manifestations, and as such they are often not identical to the features of the disorder in later developmental stages. In contrast, risk factors are experiential or environmental factors (i.e., poverty, parental psychopathology, and trauma) that increase the probability of developing psychopathology (Cicchetti & Rogosch, 1999). Research has only just begun to identify developmental antecedents of BPD (Cohen, Crawford, Johnson, & Kasen, 2005; Crawford, Cohen, Chen, Anglin, & Ehrensaft, 2009; Johnson, Smailes, Cohen, Brown, & Bernstein, 2000; Lenzenweger & Cicchetti, 2005; Winograd, Cohen, & Chen, 2008; Yen et al., 2004). So far, studies suggest several putative antecedents to the later development of BPD, including difficult child temperament (Zanarini et al., 2006), childhood externalizing disorders (Burke & Stepp, 2012; Stepp, Burke, Hipwell, & Loeber, 2012), child maltreatment (e.g., Battle et al., 2004), child's experience of separation and loss (e.g., Crawford et al., 2009), parent temperament (Fassino et al., 2009), parent psychiatric disorders (White, Gunderson, Zanarini, & Hudson, 2003), dysfunctional family environments (Afifi et al., 2011; Fruzzetti, Shenk, & Hoffman, 2005; Zanarini et al., 1997), and poor parenting practices (Johnson, Cohen, Chen, Kasen, & Brook, 2006). In the current study, we focus on characteristics of child temperament and psychopathology, parent psychopathology, and parenting practices.
Child temperament
Temperamental characteristics such as negative emotionality and poor impulse control are widely recognized in virtually all etiological theories as early markers or precursors of BPD traits. Temperament is defined as the physiological basis for individual differences in reactivity and self-regulation and is heritable and relatively stable (Rothbart & Bates, 2006). Studies with children and adolescents have generally found a link among negative emotionality, impulsivity, and BPD (Belsky et al., 2012; Crowell, Beauchaine, & Linehan, 2009; Crowell et al., 2005, 2012). However, infant activity and emotionality, but not impulsivity, were related to BPD symptoms at age 28 (Carlson, Egeland, & Sroufe, 2009). These inconsistencies may reflect methodological differences in the measurement of impulsivity across these developmental periods. Furthermore, evidence suggests that externalizing problems, such as conduct disorder (CD) and oppositional defiant disorder (ODD), during childhood and early adolescence are prospectively associated with BPD symptoms in adolescent girls (Stepp et al., 2012) and young men (Burke & Stepp, 2012), which is likely because these problems share underlying features of impulsivity and negative affectivity. Such temperamental characteristics in a child may evoke more negative parenting behaviors over time, further increasing risk for BPD. Bidirectional relations have been found between child temperament and parenting in healthy samples, such that inconsistent discipline increased negative emotionality in middle childhood, and child irritability led to more inconsistent discipline by parents (Lengua & Kovacs, 2005). These bidirectional associations have yet to be investigated for BPD in youth.
Parental psychopathology
Several studies suggest that parental psychopathology serves as a risk factor for BPD in offspring (e.g., Belsky et al., 2012; Bradley, Jenei, & Westen, 2005; Helgeland & Torgersen, 2004; White et al., 2003). In particular, first-degree relatives of individuals with BPD have a much greater risk of developing the disorder than does the general population (for a review, see White et al., 2003). There is a genetic component to BPD that also puts offspring at risk (Lis, Greenfield, Henry, Guilé, & Dougherty, 2007; Skodol et al., 2002). There is also evidence that retrospectively reported parental antisocial problems and mood disorders are associated with BPD features in young adult offspring (Trull, 2001). Antisocial features and mood disorders in parents have also been shown to predict children's internalizing and externalizing problems at various stages of development (Zahn-Waxler, Duggal, Gruber, & Bornstein, 2002). Hence, parental psychopathology, especially BPD, antisocial behaviors, or depressed mood, likely increases the risk for BPD features during adolescence. In the current study, we focus on parental antisocial behavior and depressed mood because parental BPD symptoms were not measured.
Parenting practices
Developmental models of BPD posit that invalidating parenting experiences transact with a child's genetic vulnerabilities to put them at risk for the emergence of BPD (Fruzzetti et al., 2005; Linehan, 1993). The specific characteristics that constitute “invalidating parenting” have yet to be reliably defined and measured. Using Linehan's (1993) definition as a guide, empirical work suggests that invalidating parenting is characterized by emotional and/or physical neglect, dysfunctional parenting practices (including parents' emotional and behavioral responses to their children), and poor parent–child relationship quality (Eisenberg, Cumberland, & Spinrad, 1998; Eisenberg et al., 1999; Gottman, Katz, & Hooven, 1997). Specific parenting practices or behaviors defined by both content and socialization goals (Morris, Silk, Steinberg, Myers, & Robinson, 2007) can contribute to invalidation in the family environments in those at risk for the development of BPD. In normative samples, negative, invalidating parenting behaviors have been associated with social and emotional difficulties throughout childhood (Eisenberg et al., 1999; Kiff, Lengua, & Zalewski, 2011; Silk et al., 2009) and psychological distress in adulthood (Krause, Mendelson, & Lynch, 2003).
Prospective evidence from the Children in the Community Study (Cohen et al., 2005) has found maternal inconsistency and emotional over involvement (Bezirganian, Cohen, & Brook, 1993), and low warmth and harsh punishment (Johnson, Cohen, Kasen, & Brook, 2006) to predict BPD symptoms in adolescence and adulthood, respectively. Winsper, Zanarini, and Wolke (2012) also found a prospective relationship between harsh punishment and risk for BPD in children. Maternal hostility, boundary dissolution, and family life stress have been linked to BPD symptoms in adulthood (Carlson et al., 2009). However, these studies did not examine the reciprocal influences of parenting and BPD symptoms.
Most research has asked patients with BPD to retrospectively report on the parental care that they received as children. In such studies, BPD patients portray the parenting that they received as children quite unfavorably (Sansone & Sansone, 2009b), often describing their parents as neglectful, invalidating, overinvolved, and indifferent (Gunderson & Lyoo, 1997; Weaver & Clum, 1993; Zweig-Frank & Paris, 1991). These individuals also describe relationships with caregivers and the ambience in their households as conflictual and inconsistent (Zanarini et al., 2000). Several independent lines of research have also confirmed an association between parental emotional unavailability and neglect, and BPD features, such as self-injury (Bureau et al., 2009; Gratz, 2006; Gratz, Conrad, & Roemer, 2002; Gratz, Hepworth, et al., 2011; Gratz, Latzman, Tull, Reynolds, & Lejuez, 2011; Helgeland & Torgersen, 2004; Lyons-Ruth, Choi-Kain, Pechtel, Bertha, & Gunderson, 2011).
Bidirectional parent–child influences
Unfortunately, research on developmental antecedents reviewed above has not assessed the impact that the child's early BPD features and symptoms may have on parenting behaviors. BPD symptoms are often viewed as a consequence, rather than as a driving force, of these associations. Both parent- and child-driven effects create change in behaviors and symptoms across development (Sameroff, 1975). In normative samples, there is evidence for reciprocal influences when both the adolescent and the parent are engaged in negative behaviors during problem-solving interactions (Rueter & Conger, 1998). Using a large, longitudinal sample, Rueter and Conger (1998) found evidence for the bidirectional nature of parent–adolescent interactions, particularly when behavior was negative. For example, if both the parent and the adolescent displayed ineffective or coercive behavior, the interactions between them grew more negative over time. It is interesting that the authors also found evidence for declines in nurturing parenting over time when the adolescent alone was disruptive and inflexible. Finally, harsh and inconsistent parenting related negatively to flexible, involved adolescent behavior, indicating that this parenting strategy discouraged the development of effective adolescent problem-solving skills. In addition, supportive parenting behaviors declined over time when the adolescent behaved consistently negative and inflexible.
There is ample evidence for bidirectional influences between parenting practices and child internalizing and externalizing problems (Pardini, 2008). Huh, Tristan, Wade, and Stice (2006) found that externalizing problems predicted a decreased perception of parental support and parental control in adolescent girls, but they did not find support for the converse. Bidirectional influences have also been shown between parenting practices, and children's behavior problems and callous–unemotional traits (Hawes, Dadds, Frost, & Hasking, 2011; Larsson, Viding, Rijsdijk, & Plomin, 2007). Related research has shown that parental hostility is both a response to adolescent antisocial behaviors and a contributing factor to the development of these behaviors (Scaramella, Conger, Spoth, & Simons, 2003). Depressive symptoms in adolescence have also been shown to negatively predict the quality of the parent–adolescent relationship (Branje, Hale, Frijns, & Meeus, 2010) and to elicit more hostile parenting responses and decreases in warm parenting techniques, which may relate to further adolescent withdrawal and depression (Kim, Conger, Lorenz, & Elder, 2001; Slesnick & Waldron, 1997).
Having a child with BPD symptoms may be perceived by parents as a burden (Goodman, 2011), and this may negatively impact the way parents respond to their child. In turn, these negative effects on parenting responsiveness may further increase the child's maladaptive behaviors. In addition, many parents report difficulties adjusting to their adolescent's individuation and autonomy striving (Silverberg & Steinberg, 1990). Parents of adolescents with BPD symptoms may have an even harder time coping with this developmental change, especially if the adolescent engages in risky and problematic behaviors that parents perceive as worthy of discipline. In response to such behaviors, parents may increase the amount of control and discipline they exercise. If the adolescent is engaging in risky and dangerous behaviors, these are not likely to evoke parental warmth. Thus, adolescence represents an ideal time to study the dynamic and reciprocal nature of relations between parenting and the development of BPD.
Summary
Taken together, the findings reviewed above suggest that (a) BPD symptoms, measured dimensionally, are prevalent, functionally impairing, and stable in adolescents; (b) aspects of childhood temperament, particularly those related to negative affectivity and impulsivity, may be biologically determined precursors to BPD; and (c) facets of parenting and parental psychopathology may also contribute to the development of BPD. However, most previous research on the development of BPD has relied on the retrospective reports of adults, and few longitudinal studies are able to prospectively examine links between childhood experiences and BPD. Furthermore, previous work is limited by the use of univariate models of risk factors to predict BPD, which fail to account for the bidirectional and transactional nature of the relations between these interdependent developmental processes. BPD symptoms and parenting may influence each other via two processes: first, the traitlike, stable components of BPD symptoms and parenting behaviors may be associated over time; and second, statelike, year-to-year variations in BPD symptoms and parenting behaviors may also be linked. Linehan's (1993) biosocial theory and other prominent theoretical models (Crowell et al., 2009; Fruzzetti et al., 2005) emphasize the transactional nature of the development of BPD, with child characteristics (e.g., temperament) and characteristics of the environment (e.g., caregivers' responses) interacting with each other over time, with both the trait components and state components of these processes influencing one another. Although none of the identified developmental antecedents are, taken in isolation, unique to the development of BPD, the use of multivariate longitudinal models incorporating several putative risk factors creates a more robust model of prospective risk that may include unique pathways to BPD.
Current Study
In order to address these limitations to the understanding of developmental pathways to BPD, we explored the bidirectional nature of adolescent BPD symptoms and parenting practices, namely, harsh punishment and low warmth, in a large, longitudinal community sample of girls. The current study examined the associations between BPD symptoms and parenting through statistical methods that differentiate time-specific variations in BPD symptoms and parenting behaviors from the stable processes that steadily influence repeated measures within an individual. This method can help establish temporal precedence of BPD symptoms and parenting practices during adolescence. We expected to see two processes unfolding over time: one process representing the stable, traitlike nature of BPD symptoms and parenting behaviors; and the other process reflecting time-specific (yearly) variations in these constructs. The stable component represents, for example, the average level of BPD symptoms across ages 14–17. This component reflects individual differences in the trajectory of BPD symptoms during adolescence. The time-specific process reveals, for example, increases or decreases in BPD symptoms relative to one's own trajectory. For instance, an individual may have a general propensity for elevated BPD symptoms during adolescence; however, one particular year these symptoms may be even more extreme owing to changes in parenting that occurred the previous year. These time-specific deviations may also influence one another (e.g., relative increases in age 14 symptoms predict relative increases in symptoms at age 15) and may also predict time-specific variations in subsequent parenting behaviors (e.g., relative increases in BPD symptoms at age 14 predict relative increases in harsh punishment at age 15).
Our overall aim was to examine the reciprocal and bidirectional relationship between BPD symptoms and parenting behaviors during adolescence. We list the specific aims and hypotheses:
Aim 1
Our first aim was to examine the nature of BPD symptoms and parenting practices during adolescence. Hypothesis 1a: We expected to find evidence suggesting that BPD symptoms and parenting practices reflect two processes: a stable, traitlike component as well as a more variable, statelike component, indicating year-to-year variations in BPD symptoms and parenting practices. Hypothesis 1b: Based on previous research on both normative and disordered personality development during adolescence, we expected that BPD symptoms would demonstrate moderate levels of stability during this timeframe. Hypothesis 1c: Because adolescence is a time of increasing autonomy, we expected decreases in parenting practices of harsh punishment and caregiver low warmth during this developmental period.
Aim 2
Our second aim was to examine the bidirectional influences between BPD symptoms and both harsh punishment and caregiver low warmth. Hypothesis 2a: Based on prominent theories of BPD development (e.g., Linehan, 1993; Kernberg, 1984; Bateman & Fonagy, 2003), we expected that trajectories of parenting practices and BPD symptoms would reciprocally influence each other, such that both forms of parenting practices would predict BPD symptoms just as BPD symptoms would also predict parenting practices. Hypothesis 2b: We also predicted that year-to-year fluctuations in BPD symptoms predicted changes in parenting practices 1 year later and vice versa.
Aim 3
Our third aim was to determine the impact of child and caregiver characteristics on these developmental trajectories. We examined associations among child characteristics (impulsivity and negative affectivity), parental psychopathology (depression severity and antisocial behavior), BPD symptoms, and parenting trajectories during adolescence. Given that externalizing problems have been shown to be an important predictor of BPD symptoms in a previous study using this sample (Stepp et al., 2012), we also include ODD/CD severity as a predictor. Hypothesis 3: We expected to find that child impulsivity, negative affectivity, and ODD/CD severity as well as parental depression severity and antisocial behavior would be related to increased levels of BPD symptoms, harsh punishment, and caregiver low warmth during this developmental period.
Method
Sample description
The Pittsburgh Girls Study (N = 2,451) involves an urban community sample of four cohorts of girls, ages 5–8 at the first assessment, and their primary caretakers, followed annually according to an accelerated longitudinal design. To identify the study sample, low-income neighborhoods were oversampled, such that neighborhoods in which at least 25% of families were living at or below poverty level were fully enumerated and a random selection of 50% of households in all other neighborhoods were enumerated (see Hipwell et al., 2002, for details on study design and recruitment). The primary analyses presented here use four consecutive waves of data collected (Waves 7–10), covering ages 14 to 17 years. In addition, we used Wave 4 data (when girls were aged 8–11 years) to measure caregiver antisocial behavior and age 11 data (Waves 4–7) to assess child temperament. See Table 1 for the timing and informant used for each study variable. Participants who contributed to at least one assessment during this time period were retained for analyses (n = 2,212; 90.25% of original sample). Attrition analyses showed that girls who were retained did not differ from attritors on minority race, family poverty, or single parenthood at baseline.
Table 1. Descriptive statistics and correlations for all study variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Age 14 harsh punishment (C) | 1 | ||||||||||||||||||||||
| 2. | Age 15 harsh punishment (C) | .61 | 1 | |||||||||||||||||||||
| 3. | Age 16 harsh punishment (C) | .58 | .63 | 1 | ||||||||||||||||||||
| 4. | Age 17 harsh punishment (C) | .55 | .53 | .57 | 1 | |||||||||||||||||||
| 5. | Age 14 harsh punishment (P) | .42 | .36 | .36 | .34 | 1 | ||||||||||||||||||
| 6. | Age 15 harsh punishment (P) | .41 | .42 | .34 | .35 | .69 | 1 | |||||||||||||||||
| 7. | Age 16 harsh punishment (P) | .39 | .40 | .43 | .44 | .65 | .71 | 1 | ||||||||||||||||
| 8. | Age 17 harsh punishment (P) | .41 | .38 | .36 | .46 | .61 | .66 | .68 | 1 | |||||||||||||||
| 9. | Age 14 low warmth (P) | .27 | .21 | .20 | .16 | .49 | .39 | .37 | .37 | 1 | ||||||||||||||
| 10. | Age 15 low warmth (P) | .28 | .25 | .22 | .19 | .43 | .51 | .42 | .37 | .68 | 1 | |||||||||||||
| 11. | Age 16 low warmth (P) | .24 | .25 | .24 | .24 | .42 | .43 | .51 | .37 | .64 | .73 | 1 | ||||||||||||
| 12. | Age 17 low warmth (P) | .29 | .18 | .21 | .25 | .40 | .45 | .47 | .49 | .66 | .69 | .75 | 1 | |||||||||||
| 13. | Age 14 BPD symptoms (C) | .31 | .26 | .24 | .17 | .17 | .18 | .13 | .12 | .21 | .23 | .24 | .22 | 1 | ||||||||||
| 14. | Age 15 BPD symptoms (C) | .31 | .30 | .24 | .22 | .17 | .21 | .17 | .15 | .22 | .28 | .26 | .19 | .55 | 1 | |||||||||
| 15. | Age 16 BPD symptoms (C) | .29 | .28 | .30 | .24 | .17 | .18 | .18 | .13 | .19 | .21 | .22 | .14 | .48 | .59 | 1 | ||||||||
| 16. | Age 17 BPD symptoms (C) | .28 | .17 | .21 | .28 | .11 | .15 | .15 | .12 | .17 | .17 | .19 | .18 | .42 | .52 | .58 | 1 | |||||||
| 17. | Minority race | .24 | .22 | .24 | .15 | .25 | .25 | .24 | .19 | .06 | .08 | .10 | .07 | .09 | .13 | .13 | .05 | 1 | ||||||
| 18. | Age 14 public assistance | .13 | .13 | .15 | .16 | .19 | .20 | .18 | .16 | .11 | .09 | .15 | .08 | .11 | .12 | .08 | .09 | .34 | 1 | |||||
| 19. | Age 14 impulsivity (P) | .25 | .13 | .16 | .11 | .25 | .19 | .18 | .19 | .29 | .21 | .27 | .30 | .26 | .17 | .12 | .12 | .14 | .15 | 1 | ||||
| 20. | ODD/CD severity (C) | .41 | .23 | .26 | .24 | .22 | .21 | .19 | .17 | .22 | .26 | .26 | .23 | .53 | .35 | .31 | .28 | .13 | .08 | .31 | 1 | |||
| 21. | Age 11 negative affect (P) | .23 | .13 | .15 | .12 | .33 | .27 | .27 | .22 | .52 | .46 | .45 | .50 | .21 | .18 | .16 | .17 | −.01 | .11 | .34 | .24 | 1 | ||
| 22. | Age 14 parent depression severity (P) | .14 | .13 | .12 | .04 | .20 | .22 | .23 | .15 | .24 | .24 | .25 | .21 | .13 | .13 | .13 | .17 | .04 | .19 | .11 | .25 | .07 | 1 | |
| 23. | Wave 4 parent antisocial behavior (P) | .12 | .08 | .10 | .00 | .20 | .19 | .14 | .15 | .17 | .17 | .13 | .08 | .09 | .06 | .11 | −.01 | .08 | .11 | .07 | .21 | .16 | .10 | 1 |
| Mean/proportion (%) | 8.9 | 8.8 | 8.5 | 8.2 | 8.9 | 8.8 | 8.7 | 8.3 | 8.5 | 8.5 | 8.6 | 8.4 | 2.4 | 2.5 | 2.4 | 2.3 | 59 | 39 | 1.7 | 6.8 | 1.7 | 6.8 | 3 | |
| SD | 2.4 | 2.5 | 2.3 | 2.1 | 2.1 | 2.2 | 2.2 | 2.1 | 2.3 | 2.4 | 2.5 | 2.3 | 1.9 | 1.9 | 1.9 | 1.9 | — | — | 1.8 | 5.5 | 1.6 | 8.1 | 3.4 | |
Note: C, girl (child) report; P, parent report; BPD symptoms, borderline personality disorder symptoms; ODD/CD severity, oppositional defiant disorder/conduct disorder severity. p ≤ .05 for rs ≥ |.05|.
African American girls made up slightly more than half of the sample (53%), while 41.2% were Caucasian. Most of the remaining 5.8% of girls were described as multiracial. At the Wave 4 assessment, the vast majority of caretakers were biological mothers, accounting for 86% of the sample. Biological fathers were the next largest category of caretakers, with 5.8% of the sample; followed by grandmothers, consisting of 3.1%; and adoptive mothers comprising 2.6% of the sample. Less frequent relationships among caretakers and girls included aunts and uncles or other relatives (1.1%), stepmothers (0.6%), foster parents (0.4%), and stepfathers (0.1%). Given that the overwhelming majority of the caretakers were parents, we refer to caretakers as “caregivers.” Most caregivers (57%) were cohabiting with a spouse or domestic partner, and 50% completed more than 12 years of education. Caregivers' ages at Wave 1 ranged from 21 to 83 years (M = 37.76, SD = 8.57).
Data collection
Separate in-home interviews for both the girl and the caregiver were conducted annually by trained interviewers using a laptop computer. All study procedures were approved by the University of Pittsburgh Institutional Review Board. Families were compensated for their participation.
Measures
Parenting practices
Harsh punishment was assessed using caregiver and child reports on the Conflict Tactics Scale: Parent–Child version (Straus, Hamby, Finkelhor, Moore, & Runyan, 1998). Items referring to the primary caregiver were used and were scored on a 3-point scale (1 = never, 2 = sometimes, 3 = often). Five items from the psychological aggression subscale (e.g., from parent report, “In the past year, if your daughter did something that she is not allowed to do or something that you didn't like, how often did you shout, yell, or scream at her?”) were combined with a single item on spanking to produce the harsh punishment construct. Satisfactory discriminant and construct validity has been previously reported for the psychological aggression scale (Straus et al., 1998). In the current sample, the average internal consistency for child report was α = 0.76, with values ranging from α = 0.74 (age 17) to α = 0.78 (age 16). For caregiver report the average internal consistency was α = 0.77, with values ranging from α = 0.76 (age 14) to α = 0.78 (ages 16 and 17).
Low parental warmth was measured by caregiver report using six items of the Parent–Child Rating Scale (Loeber, Farrington, Stouthamer-Loeber, & Van Kammen, 1998). Child report was not obtained for this construct. Items (e.g., “How often have you wished she would just leave you alone?”) were scored on a 3-point scale (1 = almost never, 2 = sometimes, 3 = often). The average internal consistency was α = 0.80, with values ranging from α = 0.78 (age 14) to α = 0.82 (age 16).
BPD symptoms
BPD symptoms were assessed with girls' reports when they were 14 to 17 years old using the questions from the screening questionnaire of the International Personality Disorders Examination (IPDE-BOR; Loranger et al., 1994). The Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV; American Psychological Association, 2000) version of the IPDE was used. Caregiver report was not obtained. The IPDE-BOR consists of nine items (e.g., “I get into very intense relationships that don't last”) scored either true or false. The IPDE was originally developed for adults. However, adequate concurrent validity, and sensitivity and specificity of BPD symptom scores to clinicians' diagnosis have been demonstrated for the IPDE-BOR in a sample of youth, and a score of 4.0 or greater may be considered in the clinically significant range, experiencing distress and/or impairment (Smith, Muir, & Blackwood, 2005). To demonstrate the level of severity in this sample, the upper quartile had an average score of 5.1 at ages 14–15, 5.0 at age 16, and 4.4 at age 17. Thus, level of severity in one quarter of our sample is well within the clinically significant range. The average internal consistency for BPD symptoms was adequate, α = 0.64, with values ranging from α = 0.62 (age 15) to α = 0.66 (age 17) but relatively lower when compared to other scales used in this study, which may reflect the small number of binary items used to create this construct or that the items underlying this score may be less unidimensional comparatively (Kuder & Richardson, 1937).1 In a sub-sample of the Pittsburgh Girls Survey (n = 65), we have demonstrated convergent validity of the IPDE-BOR with BPD symptom severity scores from a semistructured clinical interview, the Structured Interview for DSM-IV Personality Disorders (Pfohl, Blum, & Zimmerman, 1997; r = .71, p < .001).
Finally, we inspected the content of BPD symptoms, negative affectivity, impulsivity, and ODD/CD items for overlap. This was our preliminary check to ensure that our measures could be considered distinct constructs. Three negative affectivity items and two ODD items were similar to the wording of BPD items. Specifically, the negative affectivity items of “cries easily,” “often fusses and cries,” and “gets easily upset” appeared similar to three BPD symptom items: “temper tantrums or angry outbursts,” “very moody,” and “shows feelings easily.” In addition, the ODD items of “temper tantrums” and “angry and resentful” appeared similar to two BPD items: “temper tantrums or angry outbursts” and “very moody.” There were no impulsivity items that appeared similar to the BPD items.
Caregiver psychopathology
Caregiver self-report on the Beck Depression Inventory (BDI-II; Beck, Steer, & Brown, 1996) was used to assess depression severity over the past 2 weeks. The assessment point from when girls were aged 14 was used. The BDI-II consists of 21 items (e.g., feelings of guilt or sadness) scored on a 4-point scale (0 = absent, 3 = severe). The internal consistency was α = 0.93.
Caregiver self-report on 26 items from the Antisocial Behavior Checklist (Zucker & Noll, 1980) was used to assess the frequency of antisocial acts committed during one's lifetime (e.g., being fired or resisting arrest). Items are scored on a 4-point scale (0 = never, 3 = often). This was only administered at the Wave 4 assessment. The internal consistency coefficient was α = 0.70.
Child characteristics
Child impulsivity was assessed by caregiver report on the Adolescent Symptom Inventory, Fourth Edition (ASI-4; Gadow & Sprafkin, 1997) when girls were 14 years old. The ASI-4 impulsivity scale includes three items assessing the impulsivity dimension of attention-deficit/ hyperactivity disorder: “difficulty waiting turn,” “blurting out answers,” and “interrupting others,” scored on a 4-point scale (0 = never, 3 = very often). In the present study, the internal consistency coefficient was α = 0.82.
Child negative affectivity was measured by caregiver report at age 11 using the Emotionality, Activity, and Sociability Temperament Survey (Buss & Plomin, 1984). The negative affectivity subscale consists of five items (e.g., “She cries easily”) scored using a 5-point scale (1 = a little, 5 = a lot). This subscale has demonstrated construct validity in comparisons of girls with and without depression in a community sample (Goodyer, Ashby, Altham, Vize, & Cooper, 1993). In our study, the internal consistency coefficient for the emotionality scale was α = 0.81.
To create a parsimonious measure of externalizing problems, the CD and ODD scales from the ASI-4 were combined to create a measure of ODD/CD severity that was assessed by child report when girls were 14 years old. The CD scale contains 15 items and the ODD scale contains 8 items, reflecting DSM-IV diagnostic criteria, scored on a 4-point scale (0 = never, 3 = very often). In the present study, the internal consistency coefficient was α = 0.87.
Covariates
We included minority race (0 = Caucasian, 1 = minority race), cohort, and family poverty at age 14 (0 = no receipt of public assistance, 1 = receipt of public assistance).
Data analytic plan
In order to test our hypotheses regarding the traitlike and statelike nature of BPD symptoms and parenting practices, and how these processes reciprocally influenced one another, we needed to employ a series of models. Autoregressive models are a series of regressions, each variable regressed on an earlier value (e.g., harsh punishment at age 15 predicted by harsh punishment at age 14), and represent the statelike deviations from year to year. In contrast, the latent growth curve model allows for trajectories over time for repeated measures (e.g., trajectory of harsh punishment across adolescence) and represents the traitlike portion of BPD symptoms and parenting. Each person would have her own trajectory, indicated by different intercept and slope values over time. However, the autoregressive latent trajectory (ALT) model is a hybrid of the autoregressive and latent growth curve models, and allows for the examination of both processes simultaneously, one process representing the stable, traitlike nature of BPD symptoms and parenting (the latent growth curve part of the ALT model) and the other process reflecting time-specific variations in these constructs (the autoregressive part of the ALT model). In order to test that these processes have both a statelike and a traitlike nature, and that these processes reciprocally influence one another, we had to test if the ALT model was the best-fitting model, which required us to compare the fit of a more complicated model against the base model. If the ALT model provided the best fit to our data, it points to both statelike and traitlike influences for BPD symptoms and parenting practices during this developmental window. Once we determine the best-fitting model, we are then able to examine coefficients to determine the relationships among the variables as well as introduce predictor variables.
Models were estimated with Mplus 6.1 (Muthén & Muthén, 2010) using a maximum likelihood estimator. Maximum likelihood estimation was provided under the assumption that missing data were missing at random (Little & Rubin, 2002). Missing data are not allowed for the observed covariates because outcomes are modeled conditionally on the covariates and the covariates have no distributional assumption. Model fit was evaluated using the χ2 likelihood ratio test, Akaike information criterion, Tucker-Lewis index, root mean square error of approximation, and the standardized root mean square residual. For the Tucker-Lewis index, we used the conventional cutoff ≥0.90 for acceptable fit and ≥0.95 for good fit. Root mean square error of approximation values <0.08 represent acceptable fit, while values <0.05 indicate good fit. Standardized root mean square residual values <0.10 support acceptable fit, while values <0.08 support good fit (Hu & Bentler, 1999; McDonald & Ho, 2002). Lower Akaike information criterion values indicate better fit. Nested models were compared using the χ2 difference test (Δχ2; Bollen, 1989).
Bollen and Curran's (2004, 2006) data analytic recommendations for building and testing ALT models were followed as well as the technical report provided by Morin, Maïano, Marsh, Janosz, and Nagengast (2011). First, univariate latent growth curve models (LCMs), autoregressive (AR) models, and ALT models were estimated for one growth process (child-reported harsh parenting, caregiver-reported harsh parenting, caregiver-reported caregiver low warmth, and child-reported BPD symptoms) at a time. Because these models revealed similar results to the multivariate models, they are not presented here but are available by request from the corresponding author. Second, multivariate LCM, AR, and ALT models (i.e., three multivariate models: each parenting construct with BPD symptoms) were estimated and compared to determine which model provided the most complete and parsimonious picture of the data. Figure 1 illustrates an unconditional ALT model with no constraints. In order to achieve identification, the first time point was treated as endogenous. Although ALT and LCM models are not nested, it is possible to specify an ALT model in which the autoregressive and cross-lagged parameters are fixed to zero, which is equivalent to a LCM and nested within the ALT. The multivariate AR and ALT models included cross-lagged regression parameters going from each construct (parenting and BPD symptoms) to the other. In the multivariate LCM, correlations were added between the intercept and slope factors of both growth processes. Next, additional constraints were progressively added to the ALT to ensure that the final model was the most parsimonious: (a) fixed the slope factor's variance to zero, (b) excluded the slope factor, (c) excluded time-specific uniqueness correlations, (d) constrained the time-specific uniqueness correlations to equality, (e) constrained the autoregressive parameters to equality across time points, and (f) imposed equality constraints on the cross-lagged parameters. The first three were added to one construct at a time.
Figure 1.
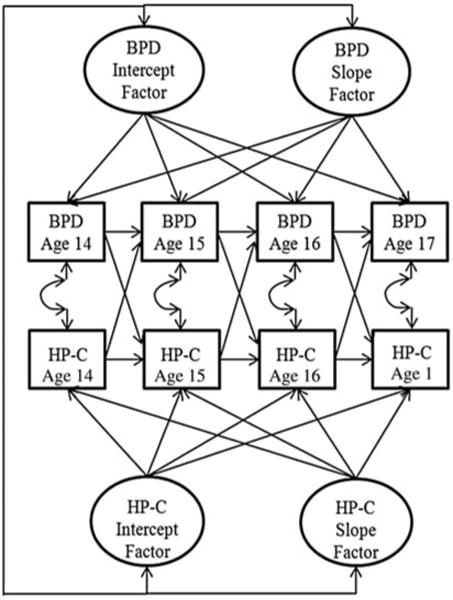
The unconditional multivariate autoregressive latent trajectory (ALT) model. Three multivariate ALT models were examined, one for each parenting practice. Constraints were added to this model to ensure that the most parsimonious ALT model was retained (e.g., no slope factor). BPD, borderline personality disorder symptoms; HP-C, harsh punishment child report.
Finally, the predictors were added to the final model. Specifically, the intercept and slope factors of both processes were regressed on each predictor. Interactions between all study covariates were also tested.
Results
Descriptive statistics
The descriptive statistics and correlations of all study variables are reported in Table 1. The correlation coefficients within each construct across time are moderately correlated and stable. Parenting practices are also moderately related to BPD symptoms, with caregiver-reported parenting practices showing a somewhat lower degree of association compared to child-reported harsh parenting practices. Minority race and receipt of public assistance have a small degree of association with parenting practices and BPD symptoms. The individual-level characteristics of impulsivity, negative affectivity, and ODD/CD severity are moderately related to both parenting practices and BPD symptoms over time. This moderate degree of association suggests that while the constructs are related, each one remains unique. Finally, caregiver psychopathology is only modestly related to some of the measurement points of BPD symptoms and somewhat more strongly associated with parenting practices as reported by the caregiver.
Unconditional multivariate models
The results from the three sets of unconditional multivariate models are reported in Table 2. These results revealed that the ALT models provided a significant improvement in model fit over both the nested ALT-LCM and the AR mode based on the Δχ2 statistics. The parameter estimates for the final ALT models are reported in Table 3. This finding supported Hypothesis 1a, suggesting that BPD symptoms and parenting behaviors are composed of two processes: a stable, traitlike component, as well as a time-specific, statelike component.
Table 2. Results from the unconditional multivariate latent curve, autoregressive and autoregressive latent curve models.
| χ2 (df) | CM | Δχ2 (df) | AIC | TLI | RMSEA | SRMR | ||
|---|---|---|---|---|---|---|---|---|
| BPD Symptoms (Child Report) and Harsh Punishment (Child Report) | ||||||||
|
| ||||||||
| 1. | LCM, full model | 74.07 (21)* | — | — | 42962.70 | 0.98 | 0.03 | 0.03 |
| 2. | Autoregressive, full model | 249.18 (12)* | — | — | 43155.81 | 0.82 | 0.10 | 0.08 |
| 3. | ALT, full model | 5.52 (5) | — | — | 42962.16 | 1 | 0.01 | 0.01 |
| 4. | ALT, nested LCM model | 48.12 (17) | 3 | 42.60 (12)* | 42944.75 | 0.98 | 0.03 | 0.03 |
| 5. | ALT + no slope variance on BPD | 12.74 (9) | 3 | 7.22 (4) | 42925.37 | 1 | 0.01 | 0.02 |
| 6. | ALT + no slope on BPD | 14.81 (11) | 5 | 2.07 (2) | 42923.45 | 1 | 0.01 | 0.01 |
| 7. | ALT-6 + no slope variance on HP-C | 37.75 (14)* | 6 | 22.94 (3)*a | 42940.38 | 0.99 | 0.03 | 0.05 |
| 8. | ALT-6 + no slope on HP-C | 39.59 (15)* | 6 | 24.78 (4)* | 42940.22 | 0.99 | 0.03 | 0.05 |
| 9. | ALT-7 + no time-specific uniqueness correlations | 50.72 (17)* | 7 | 12.97 (3)* | 42947.36 | 0.98 | 0.03 | 0.05 |
| 10. | ALT-7 + fixed time-specific uniqueness correlations | 41.79 (16)* | 7 | 4.04 (2) | 42940.42 | 0.99 | 0.03 | 0.05 |
| 11. | ALT-10 + fixed autoregressions for BPD | 41.98 (18)* | 10 | 0.19 (2) | 42936.61 | 0.99 | 0.03 | 0.05 |
| 12. | ALT-11 + fixed autoregressions for HP-C | 44.86 (20)* | 11 | 2.88 (2) | 42935.49 | 0.99 | 0.02 | 0.06 |
| 13. | ALT-12 + fixed HP-C → BPD regressions | 75.05 (22)* | 12 | 30.19 (2)* | 42961.68 | 0.98 | 0.03 | 0.06 |
| 14. | ALT-12 + fixed BPD → HP-C regressions | 47.26 (22)* | 12 | 2.40 (2) | 42933.9 | 0.99 | 0.02 | 0.06 |
|
| ||||||||
| BPD Symptoms (Child Report) and Harsh Punishment (Parent Report) | ||||||||
|
| ||||||||
| 1. | LCM, full model | 66.25 (21)* | — | — | 41739.19 | 0.98 | 0.03 | 0.03 |
| 2. | Autoregressive, full model | 301.88 (12)* | — | — | 41992.81 | 0.87 | 0.9 | 0.1 |
| 3. | ALT, full model | 7.97 (5) | — | — | 41712.91 | 1 | 0.02 | 0.03 |
| 4. | ALT, nested LCM model | 56.72 (17)* | 3 | 48.75 (12)* | 41737.66 | 0.98 | 0.03 | 0.03 |
| 5. | ALT + no slope variance on BPD | 9.68 (9) | 3 | 1.71 (4) | 41706.62 | 1 | 0.01 | 0.02 |
| 6. | ALT + no slope on BPD | 15.73 (11) | 5 | 6.05 (2) | 41708.67 | 1 | 0.01 | 0.03 |
| 7. | ALT-6 + no slope variance on HP-P | 23.44 (14) | 6 | 7.71 (3) | 41710.38 | 1 | 0.02 | 0.04 |
| 8. | ALT-6 + no slope on HP-P | 37.37 (15)* | 6 | 21.64 (4)* | 41722.31 | 0.99 | 0.03 | 0.03 |
| 9. | ALT-7 + no time-specific uniqueness correlations | 26.58 (16) | 7 | 3.14 (3) | 41707.51 | 0.99 | 0.02 | 0.03 |
| 10. | ALT-7 + fixed autoregressions for BPD | 28.67 (19) | 7 | 5.23 (5) | 41705.60 | 0.99 | 0.02 | 0.03 |
| 11. | ALT-10 + fixed autoregressions for HP-P | 31.07 (21) | 9 | 2.40 (2) | 41704.00 | 1 | 0.02 | 0.04 |
| 12. | ALT-10 + fixed HP-P → BPD regressions | 56.66 (23)* | 10 | 25.59 (2)* | 41722.60 | 0.99 | 0.03 | 0.04 |
| 13. | ALT-10 + fixed BPD → HP-P regressions | 33.00 (23) | 11 | 1.93 (2) | 41701.94 | 1.00 | 0.01 | 0.04 |
|
| ||||||||
| BPD Symptoms (Child Report) and Low Warmth (Parent Report) | ||||||||
|
| ||||||||
| 1. | LCM, full model | 64.20 (21)* | — | — | 42639.51 | 0.99 | 0.03 | 0.03 |
| 2. | Autoregressive, full model | 280.65 (12)* | — | — | 23631.56 | 0.85 | 0.1 | 0.08 |
| 3. | ALT, full model | 4.42 (5) | — | — | 42611.74 | 1 | 0 | 0.02 |
| 4. | ALT, nested LCM model | 54.29 (17)* | 3 | 49.87 (12)* | 42637.61 | 0.98 | 0.03 | 0.03 |
| 5. | ALT + no slope variance on BPD | 8.01 (9) | 3 | 3.59 (4) | 42607.00 | 1 | 0 | 0.02 |
| 6. | ALT + no slope on BPD | 9.98 (11) | 5 | 1.97 (2) | 42605.29 | 1 | 0 | 0.02 |
| 7. | ALT-6 + no slope variance on LW | 14.01 (14) | 6 | 4.03 (3) | 42603.33 | 1 | 0 | 0.03 |
| 8. | ALT-6 + no slope on LW | 45.86 (15)* | 6 | 31.85 (4)* | 42633.18 | 0.99 | 0.03 | 0.04 |
| 9. | ALT-7 + no time-specific uniqueness correlations | 52.41 (18)* | 7 | 38.40 (2)* | 42633.73 | 0.99 | 0.03 | 0.04 |
| 10. | ALT-7 + fixed time-specific uniqueness correlations | 50.45 (17)* | 7 | 36.44 (2)* | 42979.20 | 0.99 | 0.03 | 0.04 |
| 11. | ALT-7 + fixed autoregressions for BPD | 46.42 (17)* | 7 | 32.41 (2)* | 42629.73 | 0.99 | 0.03 | 0.04 |
| 12. | ALT-7 + fixed autoregressions for LW | 47.28 (17)* | 7 | 33.27 (2)* | 42630.59 | 0.99 | 0.03 | 0.04 |
| 13. | ALT-7 + fixed LW → BPD regressions | 51.52 (17)* | 7 | 37.51 (2)* | 42634.84 | 0.99 | 0.03 | 0.05 |
| 14. | ALT-7 + fixed BPD → LW regressions | 55.32 (17)* | 7 | 41.31 (2)* | 42638.64 | 0.98 | 0.03 | 0.05 |
Note: The bold type indicates the final model. BPD, borderline personality disorder symptoms; HP-C, harsh punishment, child report; HP-P, harsh punishment, parent report; LW, low warmth; χ2, chi-square test of model fit; df, degrees of freedom; Δχ2, chi-square difference test; CM, comparison model in the Δχ2; AIC, Akaike information criterion; TLI, Tucker-Lewis index; RMSEA, root mean square error of approximation; SRMR, standardized root mean square residual.
Estimation problem (negative variance) occurred in the previous model, so this model was retained.
p ≤ .01
Table 3. Variances, covariances, and correlations between the estimated parameters and the final unconditional multivariate autoregressive latent curves.
| Intercept Factor | Intercept Factor | |||
|---|---|---|---|---|
|
| ||||
| BPD | HP-C | HP-P | LW | |
| BPD | 1.71 (0.16) | 0.70 (0.18) | 0.70 (0.12) | 0.85 (0.16) |
| HP-C | 0.35 (0.07) | 2.40 (0.31) | — | — |
| HP-P | 0.30 (0.05) | — | 3.12 (0.16) | — |
| LW | 0.32 (0.05) | — | — | 3.82 (0.23) |
Note: Variances are reported on the diagonal, covariances over the diagonal, correlations under the diagonal, and standard errors in parentheses. The BPD variance reported was for the HP-C multivariate model; the BPD variances in the HP-P (1.79, SE = 0.15) and LW (1.82, SE = 0.21) models were similar. All estimates are significant (p ≤ .001). BPD, borderline personality disorder symptoms; HP-C, harsh punishment, child report; HP-P, harsh punishment, parent report; LW, low warmth.
BPD symptoms and child-reported harsh punishment
Because all three multivariate models presented similar parameter estimates for BPD symptoms, estimates concerning BPD symptoms from the multivariate child-reported harsh punishment model are discussed. These results demonstrated that the slope factor for BPD symptoms can be removed without significantly changing the overall fit of the model (Model 6), suggesting intraindividual stability in BPD symptoms from ages 14 to 17 years and supporting Hypothesis 1b. Adolescent girls' average levels of BPD symptoms have an initial mean value of 2.45 (SE = 0.04, p < .001), and there was significant interindividual variability in levels of BPD symptoms (Table 3). Concerning child-reported harsh punishment, it was necessary to model the slope factor, but the variance of the slope parameter was set to zero in the following analyses owing to a small negative variance parameter (Models 7 and 8). The estimated parameters revealed that the average levels of child-reported harsh punishment had an initial mean value of 8.93 (SE = 0.05, p < .001), had significant interindividual variability, and decreased slightly over time (Ms = −0.23, SE = 0.02, p < .001). The rate of intraindividual decline was common to all adolescent girls (i.e., the slope variance was set to zero). These findings supported Hypothesis 1c. The correlation between the intercept factors was significant (r = .35, p < .001), indicating a moderate degree of association between BPD symptoms and child-reported harsh punishment trajectories, supporting Hypothesis 2a. In addition, the inclusion of time-specific uniqueness covariances between BPD symptoms and child-reported harsh punishment was necessary (Model 9) and the covariances were constrained to equality over time (τ̂ = 0.43, p < .001; r = .21 p < .001; Model 10), suggesting a moderate degree of association between child-reported harsh punishment and BPD symptoms that remains stable during adolescence.
The results also demonstrated that the BPD symptom and child-reported harsh punishment autoregressions as well as the child-reported harsh punishment on BPD symptom cross-lagged regressions could be constrained to equality (Models 11, 12, and 14), but the BPD symptom on child-reported harsh punishment cross-lagged regressions could not (Model 13). These findings demonstrated that (a) statelike deviations in BPD symptoms predicted later levels of BPD symptoms moderately and did so consistently over time (b = 0.18, SE = 0.04, p < .001); (b) statelike deviations in child-reported harsh punishment predicted later levels of this parenting practice and were stable over time (b = 0.20, SE = 0.05, p < .001); (c) statelike deviations in child-reported harsh punishment only predicted BPD symptoms at age 15 (b = 0.08, SE = 0.04, p < .05), and all other time points were nonsignificant; and (d) predictions of child-reported harsh punishment from statelike deviations in BPD symptoms were significant, stable, and small at all time points (b = 0.08, SE = 0.04, p < .05). These findings suggest that during the adolescent period, year-to-year changes in BPD symptoms predict later harsh punishment practices rather than year-to-year changes in harsh punishment predicting later BPD symptoms. The final model (Model 14) maintained a satisfactory fit to the data. This finding partially supported Hypothesis 2b. Specifically, year-to-year fluctuations in BPD symptoms predicted changes in child-reported harsh punishment but not vice versa.
BPD symptoms and caregiver-reported harsh punishment
Similar to the multivariate model that included child-reported harsh punishment, these findings showed that it was necessary to model the slope factor for caregiver-reported harsh punishment (Model 8), but the variance of the slope parameter was not necessary to include. These findings indicated that the average levels of caregiver-reported harsh punishment had an initial mean value of 8.91 (SE = 0.04, p < .001), had significant interindividual variability, and decreased slightly over time (Ms = −0.16, SE = 0.02, p < .001), again supporting Hypothesis 1c. The rate of decline was similar for all participants (i.e., slope variance was set to zero). There was a moderate degree of association between the trajectories of BPD symptoms and caregiver-reported harsh punishment (r = .30, p < .001), supporting Hypothesis 2a. It was not necessary to model time-specific uniqueness covariances, suggesting a nonsignificant association between statelike deviations in BPD symptoms and caregiver-reported harsh punishment over this time period.
The autoregressions were able to be constrained to equality (Models 10 and 11), indicating a moderate ability of statelike deviations in BPD symptoms to predict later levels of BPD symptoms (b = 0.18, SE = 0.04, p < .001) and a small ability of statelike deviations in caregiver-reported harsh punishment to predict later levels of harsh punishment (b = 0.11, SE = 0.04, p < .01). In addition, the caregiver-reported cross-lagged regressions on BPD symptoms can be constrained to equality (Model 12), but the BPD symptoms cross-lagged regressions on caregiver-reported harsh punishment could not be constrained to equality (Model 13). However, the cross-lagged predictive ability of BPD symptoms to caregiver-reported harsh punishment as well as caregiver-reported harsh punishment to BPD symptoms was small and nonsignificant at all time points. These findings suggest that year-to-year perturbations in BPD symptoms and caregiver-reported harsh punishment do not predict later caregiver-reported harsh punishment and BPD symptoms, respectively. This finding did not support Hypothesis 2b.
BPD symptoms and caregiver low warmth
Concerning the parenting practice of low warmth, it was necessary to model the slope factor (Model 6) but not the variance of the slope factor. The average levels of caregiver low warmth had an initial mean value of 8.50 (SE = 0.05, p < .001), with significant individual variability in the average levels across time with a small and nonsignificant decline that was common across all participants (Ms = −0.02, SE = 0.02, p > .05). These findings supported Hypothesis 1c. The correlation between the intercept factors was significant (r = .32, p < .001), demonstrating a moderate degree of association between the BPD symptoms and caregiver low-warmth trajectories, which supported Hypothesis 2a. In addition, the inclusion of time-specific uniqueness covariances between BPD symptoms and caregiver low warmth was necessary, indicating an association between BPD symptoms and caregiver low warmth that was strongest at age 15 (τ̂ = 0.37, p < .001; r = .20 p < .001; Model 10).
The results also demonstrated that none of the autoregressions or cross-lagged regressions could be constrained to equality (Models 11, 12, 13, and 14). These findings showed that the ability of statelike deviations of BPD symptoms to predict later levels of BPD symptoms decreased over time (b = 0.21, SE = 0.05, p < .001; b = 0.17, SE = 0.08, p < .05; b = 0.13, SE = 0.10, p > .05; for ages 14, 15, and 16, respectively), while the ability of statelike deviations in caregiver low warmth to predict later levels of caregiver low warmth increased during this time (b = 0.08, SE = 0.07, p > .05; b = 0.16, SE = 0.08, p < .05; b = 0.24, SE = 0.08, p < .01; for ages 14, 15, and 16, respectively). While the cross-lagged regressions were necessary to model, only BPD symptoms at age 15 predicted caregiver low warmth at age 16 (b = 0.19, SE = 0.07, p < .01), and caregiver low warmth did not significantly predict later BPD symptoms at any age. These findings provide some support for BPD symptoms predicting later caregiver low warmth during adolescence but not for caregiver low warmth predicting later BPD symptoms, which provided partial support for Hypothesis 2b.
Effect of caregiver psychopathology and child characteristics on BPD symptom and parenting trajectories
To test Aim 3, the intercept and slope factors in the final ALT models were regressed onto predictors of interest, including caregiver depression severity and antisocial behavior as well as child characteristics of impulsivity, negative affectivity, and externalizing problems (ODD/CD severity). Table 4 presents the regression coefficients from all models. These models were adjusted for key demographic variables, including age, race, and family poverty. The pattern of results for the BPD symptom trajectory was the same in all models, so only the BPD symptom results from the child-reported harsh punishment multivariate model are reported here. The results showed that child characteristics influenced the BPD symptom trajectory, with impulsivity, negative affectivity, and ODD/CD severity predicting higher levels of BPD symptoms throughout adolescence. Neither marker of caregiver psychopathology (depression or antisocial behavior) predicted the BPD symptom trajectory during adolescence. In addition, race and family poverty were predictive of the BPD symptom trajectory, such that, on average, African American girls and girls living in poverty had higher levels of BPD symptoms during adolescence. As for child-reported harsh punishment, child characteristics and caregiver psychopathology predicted this trajectory. Specifically, impulsivity, negative affectivity, and ODD/CD severity had a moderate predictive effect, while caregiver antisocial behavior had a small predictive effect on the child-reported harsh punishment trajectory. Race and age also significantly predicted the child-reported harsh punishment trajectory, such that African American and older girls reported higher average levels of harsh punishment. Only family poverty predicted a faster rate of increase in the trajectory of child-reported harsh punishment. ODD/CD severity had a small negative effect on the rate of increase in child-reported harsh punishment. Concerning caregiver-reported harsh punishment, child impulsivity, negative affectivity, and ODD/CD severity as well as caregiver depression and antisocial behavior significantly predicted this trajectory. African American girls and girls living in poverty reported higher levels of caregiver-reported harsh punishment. None of the predictors significantly impacted the slope factor of caregiver-reported harsh punishment.
Table 4. Regresssion coefficients from the final multivariate conditional autoregressive latent curve models.
| Factors | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||||
| Intercept BPD | Intercept HP-C | Slope HP-C | Intercept HP-P | Slope HP-P | Intercept LW | Slope LW | ||||||||
|
|
|
|
|
|
|
|
||||||||
| b | SE | b | SE | b | SE | b | SE | b | SE | b | SE | b | SE | |
| Demographics | ||||||||||||||
| Age | 0.04 | 0.03 | 0.13** | 0.04 | −0.04 | 0.04 | 0.01 | 0.04 | −0.06 | 0.03 | 0.08* | 0.04 | −0.08* | 0.04 |
| Race | 0.22** | 0.08 | 0.98*** | 0.11 | −0.02 | 0.06 | 0.91*** | 0.09 | −0.02 | 0.05 | 0.11 | 0.09 | 0.12* | 0.05 |
| Family Poverty, age 14 | 0.16* | 0.08 | 0.10 | 0.11 | 0.10* | 0.05 | 0.25** | 0.09 | 0.03 | 0.04 | 0.07 | 0.09 | 0.00 | 0.05 |
| Parental psychopathology | ||||||||||||||
| Depression Severity, age 14 | 0.01 | 0.00 | 0.01 | 0.01 | 0.00 | 0.00 | 0.02*** | 0.01 | 0.00 | 0.00 | 0.03*** | 0.01 | 0.00 | 0.01 |
| Antisocial behavoir, Year 3 | 0.01 | 0.01 | 0.03* | 0.02 | −0.01 | 0.01 | 0.06*** | 0.01 | −0.01 | 0.01 | 0.03* | 0.01 | −0.01 | 0.01 |
| Child characteristics | ||||||||||||||
| Impulsivity, age 14 | 0.18*** | 0.02 | 0.22*** | 0.03 | −0.02 | 0.02 | 0.13*** | 0.03 | −0.01 | 0.01 | 0.22*** | 0.03 | −0.06 | 0.03 |
| ODD/CD severity, age 14 | 0.15*** | 0.01 | 0.14*** | 0.01 | −0.02* | 0.01 | 0.04*** | 0.01 | 0.00 | 0.00 | 0.04*** | 0.01 | 0.01 | 0.01 |
| Negative affectivity, age 11 | 0.14*** | 0.02 | 0.22*** | 0.03 | −0.02 | 0.02 | 0.32*** | 0.03 | −0.02 | 0.02 | 0.58*** | 0.03 | −0.01 | 0.08 |
Note: The BPD regression coefficients are from the HP-C multivariate model, and the pattern of results was similar across all models. BPD, borderline personality disorder symptoms; HP-C, harsh punishment, child report; HP-P, harsh punishment, parent report; LW, low warmth; ODD/CD severity, oppositional defiant disorder/conduct disorder severity.
p < .05.
p < .01.
p < .001.
The multivariate model including caregiver low warmth showed that child characteristics of impulsivity, negative affectivity, and ODD/CD severity as well as caregiver depression and antisocial behavior significantly predicted this parenting trajectory. Age predicted higher average levels of caregiver low warmth, such that older girls reported higher levels of caregiver low warmth. Only race significantly predicted the slope factor of caregiver low warmth, suggesting that the rate of increase in caregiver low warmth is higher for African American girls. Thus, many of these covariates were significant predictors of BPD symptoms, harsh punishment and caregiver low warmth, which supports Hypothesis 3.
As a final step, we tested the impact of interactions between child characteristics and caregiver psychopathology in predicting BPD symptom and parenting trajectories. None of these interactions were significant.
Discussion
These analyses provide a comprehensive examination of the putative reciprocal nature between parenting practices, specifically harsh punishment and caregiver low warmth, and BPD symptoms during adolescence in a large, prospective study of girls' development. The use of the ALT model revealed both traitlike and statelike reciprocal relationships among BPD symptoms and parenting practices during adolescence, supporting Hypothesis 1a. Although postulated as a critical high-risk transaction in the development of BPD, these relationships have not been addressed in prior research. The influence of child impulsivity, negative affectivity, and ODD/CD severity as well as caregiver depression and antisocial behavior on these developmental trajectories was also examined.
As we anticipated, BPD symptoms were stable across ages 14 to 17. Given that a BPD symptom slope factor was not necessary to model, the average level of BPD symptoms within each adolescent girl did not significantly change during this period of development. These findings supported Hypothesis 1b. This is similar to previous findings on the stability of BPD symptoms during adolescence (Beauchaine et al., 2009; Bornovalova et al., 2009; Crick et al., 2005; de Clercq et al., 2009; Goodman et al., 2010; Stepp et al., 2010). Two recent reviews have also reviewed the prevalence, stability and features of BPD in adolescence (Chanen, Jovev, McCutcheon, Jackson, & McGorry, 2008; Miller et al., 2008). The statelike elevations in BPD symptoms were also predictive of subsequent elevations in symptoms, suggesting that an increase in BPD symptoms one year will predict an increase in BPD symptoms the following year.
In addition, as we expected, the overall levels of harsh punishment and caregiver low warmth declined across adolescence, supporting Hypothesis 1c. The decline in caregiver low warmth suggests that parents may become less emotionally cold and distant during adolescence and may even increase warmth and responsivity during this developmental period. This is not surprising, given that adolescence is a time of increasing independence, and roles between parents and adolescents must be redefined and renegotiated from childhood (Youniss & Smollar, 1985). During adolescence there is a strong drive for autonomy and independence from parents (Collins & Laursen, 2004; Steinberg, 1990). Throughout this time, parents and adolescents renegotiate their roles by distributing some of the parental power to the adolescent (Collins & Steinberg, 1997; Smetana, Campione-Barr, & Metzger, 2006). The relationship becomes less hierarchical and more parallel, possibly resulting in fewer opportunities for overt discipline. Statelike deviations in parenting practices also predicted subsequent deviations in parenting behaviors during adolescence. For example, elevations in child-reported harsh punishment at age 14 predicted elevations in child-reported harsh punishment at age 15.
Supporting Hypothesis 2a, the trajectories of BPD symptoms and parenting practices demonstrated a moderate degree of association, suggesting that these two processes are reciprocally related in adolescent girls. Not only are the underlying traitlike processes related, but the time-specific variations in BPD symptoms and child-reported harsh punishment and caregiver low warmth are also moderately associated (as revealed by the time-specific uniqueness covariances), which supports Hypothesis 2a. Taken together, these findings reflect the reciprocal nature between BPD symptoms and child-reported harsh punishment and caregiver low warmth in adolescent girls, such that elevations in BPD symptoms at one year are also related to elevations in these parenting practices during the same year. Across childhood and adolescence, conduct problems have also been shown to be as strong of an influence on parenting behaviors as parenting behaviors are on conduct problems (Pardini, Fite, & Burke, 2008), suggesting strong bidirectional relationships between child psychopathology and parenting practices. Here, we have demonstrated that specific high-risk parenting practices and BPD symptoms exert bidirectional influences on one another in adolescent girls, which provides some support for the biosocial theory of BPD (Crowell et al., 2009; Linehan, 1993). It may be that BPD symptoms and harsh, caregiver low-warmth parenting practices maintain each other during this developmental period. This finding is intriguing, given that there is an overall decline for these parenting practices during adolescence in this sample. It is possible that BPD maintains more coercive caregiver–child interactions that extend through the adolescent period. Future research is needed to examine the extent to which this transaction impacts the relationship between the caregiver and the child during the transition to young adulthood.
We found it interesting that the year-to-year fluctuations in parenting practices did not systematically predict subsequent elevations in BPD symptoms. Only child-reported harsh punishment at age 14 predicted elevations in BPD symptoms at age 15. All other time-specific parenting practices predicting time-specific BPD elevations were nonsignificant. There was more support for time-specific elevations in BPD symptoms predicting subsequent elevations in harsh punishment or caregiver low warmth. These findings provide partial support for Hypothesis 2b. However, these effects were small and were only significant for child-reported harsh punishment and caregiver-reported caregiver low warmth, not caregiver-reported harsh punishment. Time-specific elevation in BPD symptoms during adolescence may be more likely to influence harsh punishment parenting practices rather than the other way around because, by this developmental stage, BPD symptoms may be impervious to parenting practices. Perhaps the erratic nature of BPD symptoms continues to evoke changes in this deleterious parenting practice. Future studies should examine the reciprocal relationship between parenting and BPD features during childhood to determine if time-specific elevations in BPD symptoms earlier in development are more reactive to parenting practices. Other types of child psychopathology have also been shown to influence subsequent parenting practices, including adolescent depression and antisocial behaviors (Florsheim, Tolan, & Gorman-Smith, 1998; Kim et al., 2001; Scaramella et al., 2003; Slesnick & Waldron, 1997). Similar findings have been reported for child temperament in younger, shy, or emotionally dysregulated children (Coplan, Reichel, & Rowan, 2009; Rubin, Nelson, Hastings, & Asendorpf, 1999). Child irritability has also been shown to predict inconsistent use of discipline by parents from ages 8 to 11, whereas child positive emotionality and fearfulness predict future maternal acceptance (Lengua & Kovacs, 2005).
Including child characteristics (negative affectivity, impulsivity, and ODD/CD severity), caregiver psychopathology (depression and antisocial behavior), and demographic (age and race) variables in our final model enabled us to examine the influence that these factors have on trajectories of BPD symptoms and parenting practices. It is important that after including these predictors in our final model, the relationship between BPD and parenting practices remained the same. Thus, the relationship between BPD and parenting practices could not be accounted for by these child characteristics, caregiver psychophathology, and demographic variables.
We found mixed support for Hypothesis 3. Consistent with previous work on the relation between childhood temperament and BPD in adulthood (Carlson et al., 2009), our findings demonstrated that childhood negative affectivity, impulsivity, and ODD/CD severity were associated with higher levels of BPD symptoms throughout adolescence. In addition, consistent with the Children in the Community study (Cohen et al., 2008), family poverty was also associated with higher levels of BPD symptoms. However, we did not find an association between caregiver psychopathology and BPD symptom trajectories. This finding is surprising, given the genetic overlap, and is inconsistent with previous studies (Bandelow et al., 2005). When examining the zero-order correlations between caregiver depression and adolescent BPD, there were modest associations. However, this was not true for caregiver antisocial behavior, which was measured at a much earlier time point and could be too distant of a predictor. The insignificant findings could reflect the multivariate nature of our study, such that caregiver psychopathology is not associated once child temperament and parenting practices are taken into account.
Our findings of child characteristics and caregiver psychopathology influencing parenting behaviors are consistent with prior studies (Ge et al., 1996; Pardini et al., 2008; Salihovic, Kerr, Özdemir, & Pakalniskiene, 2012) and are consistent with Hypothesis 3. We found that child negative affectivity, impulsivity, and ODD/CD severity were significantly associated with the average levels of all parenting trajectories. However, these characteristics did not influence the rate of change in these parenting practices across adolescence. African American girls had higher levels of harsh punishment but not caregiver low warmth. Family poverty only predicted increases in child-reported harsh punishment. Caregiver antisocial behavior was associated with higher levels of harsh punishment and caregiver low warmth. Caregiver depression was associated with the caregiver-reported levels of parenting behaviors, not with child-reported harsh punishment. Consistent with child characteristics, caregiver psychopathology did not influence change in these trajectories over time.
The quality of family relationships established during infancy and childhood will influence a child's future development and psychological health as an older child and adolescent (e.g., Jiménez, Musitu, & Murgui, 2005; Sheffield Morris, Silk, Steinberg, Myers, & Robinson, 2007; Stocker, Richmond, & Rhoades, 2007). Although this study finds that BPD symptoms predict subsequent changes in parenting, this may not be the case for earlier periods of development. Throughout development, harsh parenting (including abuse) and caregiver low warmth may be significant etiological factors in the future development of BPD. It is unclear when or if there is a critical window of time when the presence of these parenting behaviors exerts a causal influence on BPD development. Some work has shown evidence for the impact of early parenting practices on the later development of BPD (e.g. Carlson et al., 2009). Our study expands this literature by showing that parenting practices during adolescence remain important. In addition, this study confirms findings from normative samples: caregiver affection and discipline are critical factors for adolescent adjustment and mental health (Fraley & Davis, 1997; Hazan & Zeifman, 1994). Adolescence could be viewed as a turning point for disorders such as BPD. Perhaps the parenting received in early adolescence represents the tipping point for going from asymptomatic to symptomatic, or form symptomatic to disordered. If the BPD symptoms exhibited by adolescents are consistently met with warm, nurturing parenting, the symptoms may abate or remain at their current levels rather than increasing. In contrast, if parents react to the presentation of symptoms with increasingly negative or decreasingly positive parenting practices, disorder may be unavoidable. Overall, parenting influences a child's identity development, attachment, close relationships, and even future parenting (e.g., Belsky, 2005; Bowlby, 1985).
This study was not without limitations. BPD symptoms were not assessed prior to age 14, so relations with parenting practices may be attenuated when earlier personality disturbance is taken into account. However, we did control for childhood negative affectivity and impulsivity, which are early temperamental precursors of BPD. Including these covariates did not weaken the association between parenting and BPD symptoms, suggesting that BPD symptoms during adolescence and parenting practices mutually influence one another even when controlling for prior personality dysfunction. Future research is needed to examine the transactions between parenting practices and BPD symptoms earlier in childhood. In addition, owing to low base rates, we were not able to examine differences between those with a BPD diagnosis and those with clinically impairing symptoms. However, we did have significant variability in BPD symptoms in our sample and the upper quartile of participants had BPD symptoms in the clinically severe range (Smith et al., 2005). We recognize that our items do not explicitly measure physical abuse (e.g., caregiver slapping a child across the face), so it is possible when referring to “spanking” informants may have also reported other types of behavior, such as slapping. Our measure of impulsivity relied on impulsivity symptoms of ADHD as opposed to a trait measure. Several of the items for negative affectivity, ODD/CD, and BPD had content overlap, yet based on the moderate magnitude of the correlation coefficients, these constructs are unique. Finally, because our sample was limited to girls, these findings are not generalizable to understanding the development of BPD in male samples. Although BPD is more common among females than among males in clinical settings, the lack of gender differences in BPD among community samples suggests that similar studies with adolescent boys are warranted. Future studies including both girls and boys may also benefit from examination of potential gender differences in the developmental trajectories and antecedents of BPD.
Our study examined the year-to-year associations between parenting practices and BPD symptoms. It may be that the temporal precedence of parenting practices on subsequent BPD features was masked because the time interval for changes in parenting practices was too long. Future research should examine the relationship between parenting practices and BPD symptoms in “real-time,” with both observational and ecological momentary assessment methods. The transactional nature of BPD symptoms and parenting may occur on several temporal scales, from moment-to-moment to year-to-year, and it is important for our field to determine which scale captures these changes most appropriately.
Strengths of this study included the use of a longitudinal design, a community sample, as well as reports from both caregivers and adolescents. The prospective design allowed us to examine the associations between the developmental trajectories of BPD symptoms and parenting practices, and does not introduce retrospective bias, which has been a major limitation of previous studies relying on adult reports of childhood experiences (Bandelow et al., 2005; Battle et al., 2004; Johnson et al., 2000; Zanarini et al., 1997). The use of community participants rather than clinical patients ensures that the prospective associations observed are more representative of the development of BPD that unfolds in the general population and are less likely to be biased by the effects of treatment or characteristics that are specific to those who seek treatment.
The difference in findings between the child-reported and the caregiver-reported harsh punishment scores raises interesting questions about which informant should be used to report on parenting practices. It is widely accepted that the use of multiple reporters improves validity (Achenbach, 2006; Holmbeck, Li, Schurman, Friedman, & Coakley, 2002); however, caregiver and adolescent reports of adolescent symptoms and behaviors often share both similarities and differences. Frequently, these reports are correlated, but not highly so (Laursen & Collins, 2009). When asked to report on social relationships and interactions, adolescents and caregivers display a moderate level of agreement (Burk & Laursen, 2010; Noller & Callan, 1988), which we also found in regard to reports on harsh punishment. However, lower rates of agreement have been found for adolescent problem behaviors (Achenbach, McConaughy, & Howell, 1987; De Los Reyes & Kazdin, 2005). Furthermore, characteristics of both the caregiver and the adolescent may widen these differences. For example, in a recent study of 11th graders, Ehrlich et al. (2011) found that both adolescent attachment to parents and parental depression depicted differences in self-report measures. Given our findings with child-reported harsh punishment practices, we recommend that investigators include measures of parenting practices from the experience of the child as well as the parent or the caregiver. The children's perceptions of their harsh punishment may be especially useful in predicting psychopathology, especially when asking parents or caregivers to report on practices they may not want to admit. However, emotional sensitivity, a core symptom of BPD, could distort girls' perceptions of their caregiver's behavior to be harsher. Beyond caregiver and child report, observation measures should be used as another source of information regarding parenting practices.
Findings from this study have important implications for future research and clinical practice. Multivariate assessment models, such as the ALT models used in this study, are needed to determine time-specific associations among parenting, parental/caregiver psychopathology, child temperament, and BPD symptoms. This statistical technique can elucidate temporal precedence among risk factors and BPD. Our findings point to parenting practices as one potentially modifiable factor in the treatment of girls at risk for BPD. In addition, this work suggests that alleviating BPD symptoms in the adolescent may also improve parenting. Treatment efforts should include both adolescents and parents or caregivers, given that the transactional nature of the relation between BPD symptoms and high-risk parenting practices is such that they maintain and exacerbate each other. By explaining this bidirectional process to parents/caregivers and adolescents as a key maintaining clinical factor, the blaming of either individual can be reduced. More work elucidating the time course and pattern among parenting behaviors and BPD symptoms can help inform caregiver–child interventions for this population. Finally, this work provides strong evidence that the development of BPD stems from transactional processes occurring through temperamental disposition and environmental factors.
Acknowledgments
This research was supported by grants from the National Institute of Mental Health (MH056630) and the National Institute on Drug Abuse (DA012237), and by funding from the Office of Juvenile Justice and Delinquency Prevention, the FISA Foundation, and the Falk Fund. Further support was provided by K01 MH086713 (to S.D.S.), F31 MH093991 (to D.J.W.), and T32 MH018269 (to L.N.S. and M.Z.).
Footnotes
Because low internal consistency can reduce statistical power and increase Type II errors (i.e., decreasing the likelihood of detecting a significant effect), a power analysis was conducted examining the association between BPD symptoms at age 15 (lowest alpha observed, α = 0.62) and a parenting variable from age 14 with the lowest average reliability (child-reported harsh punishment average α = 0.76). For a sample size of 2,212 and a significance level of .05, these results showed that there was still adequate power (100%) to detect a small effect (r2 = .10).
References
- Achenbach TM. As others see us: Clinical and research implications of cross-informant correlations for psychopathology. Current Directions in Psychological Science. 2006;15:94–98. [Google Scholar]
- Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: Implications of cross-informant correlations for situational specificity. Psychological Bulletin. 1987;101:213–232. [PubMed] [Google Scholar]
- Afifi TO, Mather A, Boman J, Fleisher W, Enns MW, Macmillan H, et al. Childhood adversity and personality disorders: Results from a nationally representative population-based study. Journal of Psychiatric Research. 2011;45:814–822. doi: 10.1016/j.jpsychires.2010.11.008. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th., text revision. Washington DC: Author; 2000. [Google Scholar]
- Bagge CL, Nickell A, Stepp SD, Durrett C, Jackson K, Trull TJ. Borderline personality disorder features predict negative outcomes 2 years later. Journal of Abnormal Psychology. 2004;113:279–288. doi: 10.1037/0021-843X.113.2.279. [DOI] [PubMed] [Google Scholar]
- Bagge CL, Stepp SD, Trull TJ. Borderline personality disorder features and utilization of treatment over two years. Journal of Personality Disorders. 2005;19:420–439. doi: 10.1521/pedi.2005.19.4.420. [DOI] [PubMed] [Google Scholar]
- Bandelow B, Krause J, Wedekind D, Broocks A, Hajak G, Rüther E. Early traumatic life events, parental attitudes, family history, and birth risk factors in patients with borderline personality disorder and healthy controls. Psychiatry Research. 2005;134:169–179. doi: 10.1016/j.psychres.2003.07.008. [DOI] [PubMed] [Google Scholar]
- Bateman AW, Fonagy P. The development of an attachment-based treatment program for borderline personality disorder. Bulletin of the Menninger Clinic. 2003;67:187–211. doi: 10.1521/bumc.67.3.187.23439. [DOI] [PubMed] [Google Scholar]
- Battle CL, Shea MT, Johnson DM, Yen S, Zlotnick C, Zanarini MC, et al. Childhood maltreatment associated with adult personality disorders: Findings from the collaborative longitudinal personality disorders study. Journal of Personality Disorders. 2004;18:193–211. doi: 10.1521/pedi.18.2.193.32777. [DOI] [PubMed] [Google Scholar]
- Beauchaine TP, Klein DN, Crowell SE, Derbidge C, Gatzke-Kopp L. Multifinality in the development of personality disorders: A Biology × Sex × Environment interaction model of antisocial and borderline traits. Development and Psychopathology. 2009;21:735–770. doi: 10.1017/S0954579409000418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory—Second edition (BDI-II) San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Becker DF. Comorbidity of borderline personality disorder with other personality disorders in hospitalized adolescents and adults. American Journal of Psychiatry. 2000;157:2011–2016. doi: 10.1176/appi.ajp.157.12.2011. [DOI] [PubMed] [Google Scholar]
- Belsky DW, Caspi A, Arseneault L, Bleidorn W, Fonagy P, Goodman M, et al. Etiological features of borderline personality related characteristics in a birth cohort of 12-year-old children. Developmental Psychopathology. 2012;24:251–265. doi: 10.1017/S0954579411000812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belsky J. The developmental and evolutionary psychology of intergenerational transmission of attachment. In: Carter CS, Ahnert L, Grossman KE, Hardy SB, Lamb ME, Porges SW, et al., editors. Attachment and bonding: A new synthesis. Cambridge, MA: MIT Press; 2005. pp. 169–198. [Google Scholar]
- Bender DS, Dolan RT, Skodol AE, Sanislow CA, Dyck IR, McGlashan TH, et al. Treatment utilization by patients with personality disorders. American Journal of Psychiatry. 2001;158:295–302. doi: 10.1176/appi.ajp.158.2.295. [DOI] [PubMed] [Google Scholar]
- Bezirganian S, Cohen P, Brook JS. The impact of mother–child interaction on the development of borderline personality disorder. American Journal of Psychiatry. 1993;150:1836–1842. doi: 10.1176/ajp.150.12.1836. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Bollen KA, Curran PJ. Autoregressive latent trajectory (ALT) models: A synthesis of two traditions. Sociological Methods and Research. 2004;32:336–383. [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Hoboken NJ: Wiley; 2006. [Google Scholar]
- Bornovalova MA, Hicks BM, Iacono WG, McGue M. Stability, change, and heritability of borderline personality disorder traits from adolescence to adulthood: A longitudinal twin study. Development and Psychopathology. 2009;21:1335–1353. doi: 10.1017/S0954579409990186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornovalova MA, Hicks BM, Patrick CJ, Iacono WG, McGue M. Development and validation of the Minnesota Borderline Personality Disorder Scale. Assessment. 2011;18:234–252. doi: 10.1177/1073191111398320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. The role of childhood experience in cognitive disturbance. In: Freeman AM, Mahoney MJ, Devito P, Martin D, editors. Cognition and psychotherapy. 2nd. New York: Springer; 1985. pp. 101–121. [Google Scholar]
- Bradley R, Jenei J, Westen D. Etiology of borderline personality disorder: Disentangling the contributions of intercorrelated antecedents. Journal of Nervous and Mental Disease. 2005;193:24–31. doi: 10.1097/01.nmd.0000149215.88020.7c. [DOI] [PubMed] [Google Scholar]
- Branje SJT, Hale WW, III, Frijns T, Meeus WHJ. Longitudinal associations between perceived parent–child relationship quality and depressive symptoms in adolescence. Journal of Abnormal Child Psychology. 2010;38:751–763. doi: 10.1007/s10802-010-9401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau JF, Martin J, Freynet N, Poirier AA, Lafontaine MF, Cloutier P. Perceived dimensions of parenting and non-suicidal self-injury in young adults. Journal of Youth and Adolescence. 2009;39:484–494. doi: 10.1007/s10964-009-9470-4. [DOI] [PubMed] [Google Scholar]
- Burk W, Laursen B. Mother and adolescent reports of associations between child behavior problems and mother–child relationship qualities: Separating shared variance from individual variance. Journal of Abnormal Child Psychology. 2010;38:657–667. doi: 10.1007/s10802-010-9396-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke JD, Stepp SD. Adolescent disruptive behavior and borderline personality disorder symptoms in young adult men. Journal of Abnormal Child Psychology. 2012;40:35–44. doi: 10.1007/s10802-011-9558-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buss AH, Plomin R. Temperament: Early developing personality traits. Hillsdale, NJ: Erlbaum; 1984. [Google Scholar]
- Carlson EA, Egeland B, Sroufe LA. A prospective investigation of the development of borderline personality symptoms. Development and Psychopathology. 2009;21:1311–1334. doi: 10.1017/S0954579409990174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanen AM, Jovev M, McCutcheon LK, Jackson HJ, McGorry PD. Borderline personality disorder in young people and the prospects for prevention and early intervention. Current Psychiatry Reviews. 2008;4:48–57. [Google Scholar]
- Chanen AM, Kaess M. Developmental pathways to borderline personality disorder. Current Psychiatry Reports. 2011;14:45–53. doi: 10.1007/s11920-011-0242-y. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA. Psychopathology as risk for adolescent substance use disorders: A developmental psychopathology perspective. Journal of Clinical Child Psychology. 1999;28:355–365. doi: 10.1207/S15374424jccp280308. [DOI] [PubMed] [Google Scholar]
- Cohen P, Chen H, Gordon K, Johnson J, Brook J, Kasen S. Socioeconomic background and the developmental course of schizotypal and borderline personality disorder symptoms. Development and Psychopathology. 2008;20:633–650. doi: 10.1017/S095457940800031X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen P, Crawford TN, Johnson JG, Kasen S. The Children in the Community study of developmental course of personality disorder. Journal of Personality Disorders. 2005;19:466–486. doi: 10.1521/pedi.2005.19.5.466. [DOI] [PubMed] [Google Scholar]
- Collins WA, Laursen B. Parent–adolescent relationships and influences. In: Lerner RM, Steinberg L, editors. Handbook of adolescent psychology. 2nd. New York: Wiley; 2004. pp. 331–362. [Google Scholar]
- Collins WA, Steinberg L. Adolescent development in interpersonal context. Social Networks. 1997;3:1003–1067. [Google Scholar]
- Coplan RJ, Reichel M, Rowan K. Exploring the associations between maternal personality, child temperament, and parenting: A focus on emotions. Personality and Individual Differences. 2009;46:241–246. [Google Scholar]
- Crawford TN, Cohen PR, Chen H, Anglin DM, Ehrensaft M. Early maternal separation and the trajectory of borderline personality disorder symptoms. Development and Psychopathology. 2009;21:1013–1030. doi: 10.1017/S0954579409000546. [DOI] [PubMed] [Google Scholar]
- Crick NR, Murray-Close D, Woods K. Borderline personality features in childhood: A short-term longitudinal study. Development and Psychopathology. 2005;17:1051–1070. [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Hsiao RC, Vasilev CA, Yaptangco M, Linehan MM, et al. Differentiating adolescent self-injury from adolescent depression: Possible implications for borderline personality development. Journal of Abnormal Child Psychology. 2012;40:45–57. doi: 10.1007/s10802-011-9578-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Linehan M. A biosocial developmental model of borderline personality: Elaborating and extending Linehan's theory. Psychological Bulletin. 2009;135:495–510. doi: 10.1037/a0015616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Stevens AL, Sylvers P. Psychological, autonomic, and serotonergic correlates of parasuicide among adolescent girls. Development and Psychopathology. 2005;17:1105–1127. doi: 10.1017/s0954579405050522. [DOI] [PubMed] [Google Scholar]
- de Clercq B, van Leeuwen K, van den Noortgate W, de Bolle M, de Fruyt F. Childhood personality pathology: Dimensional stability and change. Development and Psychopathology. 2009;21:853–869. doi: 10.1017/S0954579409000467. [DOI] [PubMed] [Google Scholar]
- Dell'Osso B, Berlin HA, Serati M, Altamura AC. Neuropsychobiological aspects, comorbidity patterns and dimensional models in borderline personality disorder. Neuropsychobiology. 2010;61:169–179. doi: 10.1159/000297734. [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Kazdin AE. Informant discrepancies in the assessment of childhood psychopathology: A critical review, theoretical framework, and recommendations for further study. Psychological Bulletin. 2005;131:483–509. doi: 10.1037/0033-2909.131.4.483. [DOI] [PubMed] [Google Scholar]
- Eaton WW, Badawi M, Melton B. Prodromes and precursors: Epidemiologic data for primary prevention of disorders with slow onset. American Journal of Psychiatry. 1995;152:967–972. doi: 10.1176/ajp.152.7.967. [DOI] [PubMed] [Google Scholar]
- Ehrlich KB, Cassidy J, Dykas MJ, Ehrlich KB, Cassidy J, Dykas MJ. Reporter discrepancies among parents, adolescents, and peers: Adolescent attachment and informant depressive symptoms as explanatory factors. Child Development. 2011;82:999–1012. doi: 10.1111/j.1467-8624.2010.01530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL. Parental socialization of emotion. Psychological Inquiry. 1998;9:241–273. doi: 10.1207/s15327965pli0904_1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg N, Fabes RA, Shepard SA, Guthrie IK, Murphy BC, Reiser M. Parental reactions to children's negative emotions: Longitudinal relations to quality of children's social functioning. Child Development. 1999;70:513–534. doi: 10.1111/1467-8624.00037. [DOI] [PubMed] [Google Scholar]
- Eppright TD, Kashani JH, Robinson BD, Reid JC. Comorbidity of conduct disorder and personality disorders in an incarcerated juvenile population. American Journal of Psychiatry. 1993;150:1233–1236. doi: 10.1176/ajp.150.8.1233. [DOI] [PubMed] [Google Scholar]
- Fassino S, Amianto F, Gastaldi F, Abbate-Daga G, Brambilla F, Leobruni P. Personality trait interactions in parents of patients with borderline personality disorder: A controlled study using the Temperament and Character Inventory. Psychiatry Research. 2009;165:128–136. doi: 10.1016/j.psychres.2007.10.010. [DOI] [PubMed] [Google Scholar]
- Florsheim P, Tolan P, Gorman-Smith D. Family relationships, parenting practices, the availability of male family members, and the behavior of inner-city boys in single-mother and two-parent families. Child Development. 1998;69:1437–1447. [PubMed] [Google Scholar]
- Fraley RC, Davis KE. Attachment formation and transfer in young adults' close friendships and romantic relationships. Personal Relationships. 1997;4:131–144. [Google Scholar]
- Fruzzetti AE, Shenk C, Hoffman PD. Family interaction and the development of borderline personality disorder: A transactional model. Development and Psychopathology. 2005;17:1007–1030. doi: 10.1017/s0954579405050479. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent Symptom Inventory—4 screening manual. Stony Brook, NY: Checkmate Plus; 1997. [Google Scholar]
- Ge X, Conger RD, Cadoret RJ, Neiderhiser JM, Yates W, Troughton E, et al. The developmental interface between nature and nurture: A mutual influence model of child antisocial behavior and parent behaviors. Developmental Psychology. 1996;32:574–589. [Google Scholar]
- Goodman M, Patil U, Triebwasser J, Diamond E, Hiller A, Hoffman P, et al. Parental viewpoints of trajectories to borderline personality disorder in female offspring. Journal of Personality Disorders. 2010;24:204–216. doi: 10.1521/pedi.2010.24.2.204. [DOI] [PubMed] [Google Scholar]
- Goodman M, Patil U, Triebwasser J, Hoffman P, Weinstein ZA, New A. Parental burden associated with borderline personality disorder in female offspring. Journal of Personality Disorders. 2011;25:59–74. doi: 10.1521/pedi.2011.25.1.59. [DOI] [PubMed] [Google Scholar]
- Goodyer IM, Ashby L, Altham PM, Vize C, Cooper PJ. Temperament and major depression in 11- to 16-year-olds. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1993;34:1409–1423. doi: 10.1111/j.1469-7610.1993.tb02099.x. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Katz LF, Hooven C. Meta-emotion: How families communicate emotionally. New York: Psychology Press; 1997. [Google Scholar]
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: Results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2008;69:533–545. doi: 10.4088/jcp.v69n0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL. Risk factors for deliberate self-harm among female college students: The role and interaction of childhood maltreatment, emotional inexpressivity, and affect intensity/reactivity. American Journal of Orthopsychiatry. 2006;76:238–250. doi: 10.1037/0002-9432.76.2.238. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Conrad SD, Roemer L. Risk factors for deliberate self-harm among college students. American Journal of Orthopsychiatry. 2002;72:128–140. doi: 10.1037//0002-9432.72.1.128. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Hepworth C, Tull MT, Paulson A, Clarke S, Remington B, et al. An experimental investigation of emotional willingness and physical pain tolerance in deliberate self-harm: The moderating role of interpersonal distress. Comprehensive Psychiatry. 2011;52:63–74. doi: 10.1016/j.comppsych.2010.04.009. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Latzman RD, Tull MT, Reynolds EK, Lejuez CW. Exploring the association between emotional abuse and childhood borderline personality features: The moderating role of personality traits. Behavior Therapy. 2011;42:493–508. doi: 10.1016/j.beth.2010.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Becker DF, Walker ML, Levy KN, Edell WS, McGlashan TH. Psychiatric comorbidity in adolescent inpatients with substance use disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:1085–1091. doi: 10.1097/00004583-199508000-00019. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Lyoo IK. Family problems and relationships for adults with borderline personality disorder. Harvard Review of Psychiatry. 1997;4:272–278. doi: 10.3109/10673229709030553. [DOI] [PubMed] [Google Scholar]
- Hawes DJ, Dadds MR, Frost ADJ, Hasking PA. Do childhood callous–unemotional traits drive change in parenting practices? Journal of Clinical Child and Adolescent Psychology. 2011;40:507–518. doi: 10.1080/15374416.2011.581624. [DOI] [PubMed] [Google Scholar]
- Hazan C, Zeifman D. Sex and the psychological tether. In: Bartholomew K, Perlman D, editors. Attachment processes in adulthood: Advances in personal relationships. London: Jessica Kingsley; 1994. pp. 151–178. [Google Scholar]
- Helgeland MI, Torgersen S. Developmental antecedents of borderline personality disorder. Comprehensive Psychiatry. 2004;45:138–147. doi: 10.1016/j.comppsych.2003.09.001. [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Loeber R, Stouthamer-Loeber M, Keenan K, White HR, Kroneman L. Characteristics of girls with early onset disruptive and antisocial behaviour. Criminal Behaviour and Mental Health. 2002;12:99–118. doi: 10.1002/cbm.489. [DOI] [PubMed] [Google Scholar]
- Holm AL, Severinsson E. Struggling to recover by changing suicidal behaviour: Narratives from women with borderline personality disorder. International Journal of Mental Health Nursing. 2011;20:165–173. doi: 10.1111/j.1447-0349.2010.00713.x. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN, Li ST, Schurman JV, Friedman D, Coakley RM. Collecting and managing multisource and multimethod data in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:5–18. doi: 10.1093/jpepsy/27.1.5. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Huh D, Tristan J, Wade E, Stice E. Does problem behavior elicit poor parenting? A prospective study of adolescent girls. Journal of Adolescent Research. 2006;21:185–204. doi: 10.1177/0743558405285462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez TI, Musitu G, Murgui S. Family, social support and delinquent behavior in adolescence: Direct and mediating effects. Anuario de Psicologia. 2005;36:181–195. [Google Scholar]
- Johnson JG, Cohen P, Chen H, Kasen S, Brook JS. Parenting behaviors associated with risk for offspring personality disorder during adulthood. Archives of General Psychiatry. 2006;63:579–587. doi: 10.1001/archpsyc.63.5.579. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Brook JS. Personality disorders evident by early adulthood and risk for anxiety disorders during middle adulthood. Journal of Anxiety Disorders. 2006;20:408–426. doi: 10.1016/j.janxdis.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: A community based longitudinal investigation. Acta Psychiatrica Scandinavica. 2001;102:265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Smailes EM, Cohen P, Brown J, Bernstein DP. Associations between four types of childhood neglect and personality disorder symptoms during adolescence and early adulthood: Findings of a community-based longitudinal study. Journal of Personality Disorders. 2000;14:171–187. doi: 10.1521/pedi.2000.14.2.171. [DOI] [PubMed] [Google Scholar]
- Keenan K, Loeber R, Green S. Conduct disorder in girls: A review of the literature. Clinical Child and Family Psychology Review. 1999;2:3–19. doi: 10.1023/a:1021811307364. [DOI] [PubMed] [Google Scholar]
- Kernberg O. Severe personality disorders: Psychotherapeutic strategies. New Haven, CT: Yale University Press; 1984. [Google Scholar]
- Kiff CJ, Lengua LJ, Zalewski M. Nature and nurturing: Parenting in the context of child temperament. Clinical Child and Family Psychology Review. 2011;14:251–301. doi: 10.1007/s10567-011-0093-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim KJ, Conger RD, Lorenz FO, Elder GH., Jr Parent–adolescent reciprocity in negative affect and its relation to early adult social development. Developmental Psychology. 2001;37:775–790. [PubMed] [Google Scholar]
- Krause ED, Mendelson T, Lynch TR. Childhood emotional invalidation and adult psychological distress: The mediating role of emotional inhibition. Child Abuse & Neglect. 2003;27:199–213. doi: 10.1016/s0145-2134(02)00536-7. [DOI] [PubMed] [Google Scholar]
- Kuder GF, Richardson MW. The theory of the estimation of test reliability. Psychometrika. 1937;2:151–160. doi: 10.1007/BF02289147. [DOI] [PubMed] [Google Scholar]
- Larsson H, Viding E, Rijsdijk FV, Plomin R. Relationships between parental negativity and childhood antisocial behavior over time: A bidirectional effects model in a longitudinal genetically informative design. Journal of Abnormal Child Psychology. 2007;36:633–645. doi: 10.1007/s10802-007-9151-2. [DOI] [PubMed] [Google Scholar]
- Laursen B, Collins WA. Parent–child relationships during adolescence Handbook of Adolescent Psychology. Hoboken, NJ: Wiley; 2009. [Google Scholar]
- Lengua LJ, Kovacs EA. Bidirectional associations between temperament and parenting and the prediction of adjustment problems in middle childhood. Journal of Applied Developmental Psychology. 2005;26:21–38. [Google Scholar]
- Lenzenweger MF, Cicchetti D. Toward a developmental psychopathology approach to borderline personality disorder. Development and Psychopathology. 2005;17:893–898. doi: 10.1017/s095457940505042x. [DOI] [PubMed] [Google Scholar]
- Linehan MM. Cognitive behavioral treatment of borderline personality disorder. New York: Guilford Press; 1993. [Google Scholar]
- Lis E, Greenfield B, Henry M, Guilé JM, Dougherty G. Neuroimaging and genetics of borderline personality disorder: A review. Journal of Psychiatry and Neuroscience. 2007;32:162–173. [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. 2nd. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- Loeber R, Farrington DP, Stouthamer-Loeber M, Van Kammen WB. Multiple risk factors for multiproblem boys: Co-occurrence of delinquency, substance use, attention deficit, conduct problems, physical aggression, covert behavior, depressed mood, and shy/withdrawn behavior. In: Jessor R, editor. New perspectives on adolescent risk behavior. Cambridge: Cambridge University Press; 1998. pp. 90–149. [Google Scholar]
- Loranger AW, Sartorius N, Andreoli A, Berger P, Buchheim P, Channabasavanna SM, et al. The international personality disorder examination. Archives of General Psychiatry. 1994;51:215–224. doi: 10.1001/archpsyc.1994.03950030051005. [DOI] [PubMed] [Google Scholar]
- Ludolph PS, Westen D, Misle B, Jackson A, Wixom J, Wiss C. The borderline diagnosis in adolescents: Symptoms and developmental history. American Journal of Psychiatry. 1990;147:470–476. doi: 10.1176/ajp.147.4.470. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Choi-Kain L, Pechtel P, Bertha E, Gunderson J. Perceived parental protection and cortisol responses among young females with borderline personality disorder and controls. Psychiatry Research. 2011;189:426–432. doi: 10.1016/j.psychres.2011.07.038. [DOI] [PubMed] [Google Scholar]
- McDonald RP, Ho MHR. Principles and practice in reporting structural equation analyses. Psychological Methods. 2002;7:64–82. doi: 10.1037/1082-989x.7.1.64. [DOI] [PubMed] [Google Scholar]
- Miller AL, Muehlenkamp JJ, Jacobson CM. Fact or fiction: Diagnosing borderline personality disorder in adolescents. Clinical Psychology Review. 2008;28:969–981. doi: 10.1016/j.cpr.2008.02.004. [DOI] [PubMed] [Google Scholar]
- Morin AJS, Maïano C, Marsh HW, Janosz M, Nagengast B. The longitudinal interplay of adolescents' self-esteem and body image: A conditional autoregressive latent trajectory analysis. Multivariate Behavioral Research. 2011;46:157–201. doi: 10.1080/00273171.2010.546731. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development (Oxford) 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén BO, Muthén LK. Mplus: Version 6.00. Los Angeles: Author; 2010. Computer software. [Google Scholar]
- Myers WC, Burkett RC, Otto TA. Conduct disorder and personality disorders in hospitalized adolescents. Journal of Clinical Psychiatry. 1993;54:21–26. [PubMed] [Google Scholar]
- Noller P, Callan VJ. Understanding parent–adolescent interactions: Perceptions of family members and outsiders. Developmental Psychology. 1988;24:707–714. [Google Scholar]
- Pardini DA. Novel insights into longstanding theories of bidirectional parent–child influences: Introduction to the special section. Journal of Abnormal Child Psychology. 2008;36:627–631. doi: 10.1007/s10802-008-9231-y. [DOI] [PubMed] [Google Scholar]
- Pardini DA, Fite P, Burke J. Bidirectional associations between parenting practices and conduct problems in boys from childhood to adolescence: The moderating effect of age and African-American ethnicity. Journal of Abnormal Child Psychology. 2008;36:647–662. doi: 10.1007/s10802-007-9162-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured interview for DSM-IV personality: SIDP-IV. Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Rothbart MK, Bates JE. Temperament in children's development. In: Damon W, Lerner R, Eisenberg N, editors. Handbook of child psychology: Social, emotional, and personality development. Vol. 3. New York: Wiley; 2006. [Google Scholar]
- Rubin KH, Nelson LJ, Hastings P, Asendorpf J. The transaction between parents' perceptions of their children's shyness and their parenting styles. International Journal of Behavioral Development. 1999;23:937–957. [Google Scholar]
- Rueter MA, Conger RD. Reciprocal influences between parenting and adolescent problem-solving behavior. Developmental Psychology. 1998;34:1470–1482. doi: 10.1037//0012-1649.34.6.1470. [DOI] [PubMed] [Google Scholar]
- Salihovic S, Kerr M, Özdemir M, Pakalniskiene V. Directions of effects between adolescent psychopathic traits and parental behavior. Journal of Abnormal Child Psychology. 2012;40:957–969. doi: 10.1007/s10802-012-9623-x. [DOI] [PubMed] [Google Scholar]
- Sameroff A. Transactional models in early social relations. Human Development. 1975;18:65–79. [Google Scholar]
- Sansone RA, Sansone LA. Borderline personality and criminality. Psychiatry. 2009a;6:16–20. [PMC free article] [PubMed] [Google Scholar]
- Sansone RA, Sansone LA. The families of borderline patients: The psychological environment revisited. Psychiatry. 2009b;6:19–24. [PMC free article] [PubMed] [Google Scholar]
- Scaramella LV, Conger RD, Spoth R, Simons RL. Evaluation of a social contextual model of delinquency: A cross-study replication. Child Development. 2003;73:175–195. doi: 10.1111/1467-8624.00399. [DOI] [PubMed] [Google Scholar]
- Sheffield Morris A, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Social Development. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silk JS, Ziegler ML, Whalen DJ, Dahl RE, Ryan ND, Dietz LJ, et al. Expressed emotion in mothers of currently depressed, remitted, high-risk, and low-risk youth: Links to child depression status and longitudinal course. Journal of Clinical Child and Adolescent Psychology. 2009;38:36–47. doi: 10.1080/15374410802575339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverberg S, Steinberg L. Psychological well-being of parents at mid-life: The impact of early adolescent children. Developmental Psychology. 1990;26:658–666. [Google Scholar]
- Skodol AE, Bender DS. Why are women diagnosed borderline more than men? Psychiatric Quarterly. 2003;74:349–360. doi: 10.1023/a:1026087410516. [DOI] [PubMed] [Google Scholar]
- Skodol AE, Pagano ME, Bender DS, Shea MT, Gunderson JG, Yen S, et al. Stability of functional impairment in patients with schizotypal, borderline, avoidant, or obsessive–compulsive personality disorder over two years. Psychological Medicine. 2005;35:443–451. doi: 10.1017/s003329170400354x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skodol AE, Siever LJ, Livesley WJ, Gunderson JG, Pfohl B, Widiger TA. The borderline diagnosis: II. Biology, genetics, and clinical course. Biological Psychiatry. 2002;51:951–963. doi: 10.1016/s0006-3223(02)01325-2. [DOI] [PubMed] [Google Scholar]
- Slesnick N, Waldron HB. Interpersonal problem-solving interactions of depressed adolescents and their parents. Journal of Family Psychology. 1997;11:234–245. [Google Scholar]
- Smetana JG, Campione-Barr N, Metzger A. Adolescent development in interpersonal and societal contexts. Annual Review of Psychology. 2006;57:255–284. doi: 10.1146/annurev.psych.57.102904.190124. [DOI] [PubMed] [Google Scholar]
- Smith DJ, Muir WJ, Blackwood DHR. Borderline personality disorder characteristics in young adults with recurrent mood disorders: A comparison of bipolar and unipolar depression. Journal of Affective Disorders. 2005;87:17–23. doi: 10.1016/j.jad.2005.02.019. [DOI] [PubMed] [Google Scholar]
- Soloff PH, Lynch KG, Kelly TM. Childhood abuse as a risk factor for suicidal behavior in borderline personality disorder. Journal of Personality Disorders. 2002;16:201–214. doi: 10.1521/pedi.16.3.201.22542. [DOI] [PubMed] [Google Scholar]
- Steinberg L. Autonomy, conflict, and harmony in the family relationship. In: Feldman S, Elliot G, editors. At the threshold: The developing adolescent. Cambridge, MA: Harvard University Press; 1990. pp. 255–276. [Google Scholar]
- Stepp SD, Burke JD, Hipwell AE, Loeber R. Trajectories of attention deficit hyperactivity disorder and oppositional defiant disorder symptoms as precursors of borderline personality disorder symptoms in adolescent girls. Journal of Abnormal Child Psychology. 2012;40:7–20. doi: 10.1007/s10802-011-9530-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepp SD, Pilkonis PA, Hipwell AE, Loeber R, Stouthamer-Loeber M. Stability of borderline personality disorder features in girls. Journal of Personality Disorders. 2010;24:460–472. doi: 10.1521/pedi.2010.24.4.460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stocker CM, Richmond MK, Rhoades GK. Family emotional processes and adolescents' adjustment. Social Development. 2007;16:310–325. [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the parent–child conflict tactics scales: Development and psychometric data for a national sample of American parents. Child Abuse & Neglect. 1998;22:249–270. doi: 10.1016/s0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Trull TJ. Structural relations between borderline personality disorder features and putative etiological correlates. Journal of Abnormal Psychology. 2001;110:471–481. doi: 10.1037//0021-843x.110.3.471. [DOI] [PubMed] [Google Scholar]
- Trull TJ, Useda JD, Conforti K, Doan BT. Borderline personality disorder features in nonclinical young adults: 2. Two-year outcome. Journal of Abnormal Psychology. 1997;106:307–314. doi: 10.1037//0021-843x.106.2.307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver TL, Clum GA. Early family environments and traumatic experiences associated with borderline personality disorder. Journal of Consulting and Clinical Psychology. 1993;61:1068–1075. doi: 10.1037//0022-006x.61.6.1068. [DOI] [PubMed] [Google Scholar]
- White CN, Gunderson JG, Zanarini MC, Hudson JI. Family studies of borderline personality disorder: A review. Harvard Review of Psychiatry. 2003;11:8–19. doi: 10.1080/10673220303937. [DOI] [PubMed] [Google Scholar]
- Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: Prognosis for functioning over 20 years. Journal of Child Psychology and Psychiatry. 2008;49:933–941. doi: 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Winsper C, Zanarini M, Wolke D. Prospective study of family adversity and maladaptive parenting in childhood and borderline personality disorder symptoms in a non-clinical population at 11 years. Psychological Medicine. 2012 doi: 10.1017/S0033291712000542. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Yen S, Shea MT, Sanislow CA, Grilo CM, Skodol AE, Gunderson JG, et al. Borderline personality disorder criteria associated with prospectively observed suicidal behavior. American Journal of Psychiatry. 2004;161:1296–1298. doi: 10.1176/appi.ajp.161.7.1296. [DOI] [PubMed] [Google Scholar]
- Youniss J, Smollar J. Adolescent relations with mothers, fathers, and friends. Chicago: University of Chicago Press; 1985. [Google Scholar]
- Zahn-Waxler C, Duggal S, Gruber R, Bornstein MH. Parental psychopathology. In: Bornstein MH, editor. Handbook of parenting: Social conditions and applied parenting. 2nd. Vol. 4. Mahwah, NJ: Erlbaum; 2002. pp. 295–327. [Google Scholar]
- Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A, et al. Axis I comorbidity of borderline personality disorder. American Journal of Psychiatry. 1998;155:1733–1739. doi: 10.1176/ajp.155.12.1733. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB, Marino MF, Lewis RE, Williams AA, et al. Biparental failure in the childhood experiences of borderline patients. Journal of Personality Disorders. 2000;14:264–273. doi: 10.1521/pedi.2000.14.3.264. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Ridolfi ME, Jager-Hyman S, Hennen J, Gunderson JG. Reported childhood onset of self-mutilation among borderline patients. Journal of Personality Disorders. 2006;20:9–15. doi: 10.1521/pedi.2006.20.1.9. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Williams A, Lewis R, Reich R, Vera S, Marino M, et al. Reported pathological childhood experiences associated with the development of borderline personality disorder. American Journal of Psychiatry. 1997;154:1101–1106. doi: 10.1176/ajp.154.8.1101. [DOI] [PubMed] [Google Scholar]
- Zucker RA, Noll RB. The Antisocial Behavior Checklist. Michigan State University; East Lansing: 1980. Unpublished manuscript. [Google Scholar]
- Zweig-Frank H, Paris J. Parents' emotional neglect and overprotection according to the recollections of patients with borderline personality disorder. American Journal of Psychiatry. 1991;148:648–651. doi: 10.1176/ajp.148.5.648. [DOI] [PubMed] [Google Scholar]
- Zweig-Frank H, Paris J. Predictors of outcome in a 27-year follow-up of patients with borderline personality disorder. Comprehensive Psychiatry. 2002;43:103–107. doi: 10.1053/comp.2002.30804. [DOI] [PubMed] [Google Scholar]


