Abstract
Hyperestrogenicity is a risk factor for endometrial cancer. 17β-estradiol (E2) is known to stimulate both genomic and nongenomic estrogen receptor-α (ERα) actions in a number of reproductive tissues. However, the contributions of transcription-independent ERα signaling on normal and malignant endometrium are not fully understood. Phosphatase and tensin homolog (PTEN) is a tumor suppressor that decreases cellular mitosis primarily through negative regulation of the phosphoinositide 3-kinase/AKT signaling axis. PTEN levels are elevated during the E2 dominated, mitotically active, proliferative phase of the menstrual cycle, indicating possible hormonal regulation of PTEN in the uterus. In order to determine if rapid E2 signaling regulates PTEN, we used ERα-positive, PTEN-positive, endometrial cells. We show that cytosolic E2/ERα signaling leads to increased phosphorylation of PTEN at key regulatory residues. Importantly, E2 stimulation decreased PTEN lipid phosphatase activity and caused consequent increases in phospho-AKT. We further demonstrate that cytosolic ERα forms a complex with PTEN in an E2-dependent manner, and that ERα constitutively complexes with protein kinase2-α (CK2α), a kinase previously shown to phosphorylate the C-terminal tail of PTEN. These results provide mechanistic support for an E2-dependent, ERα cytosolic signaling complex that negatively regulates PTEN activity through carboxy terminus phosphorylation. Using an animal model, we show that sustained E2 signaling results in increased phospho-PTEN (S380, T382, and T383), total PTEN, and phospho-AKT (S473). Taken together, we provide a novel mechanism in which transcription-independent E2/ERα signaling may promote a pro-tumorigenic environment in the endometrium.
Electronic supplementary material
The online version of this article (doi:10.1007/s12672-014-0184-z) contains supplementary material, which is available to authorized users.
Keywords: Endometrial Cancer, Endometrial Cancer Cell, Uterine Gland, Regulatory Residue, PTEN Activity
Introduction
Endometrial cancer (EC) is the most common gynecologic cancer and the fourth most common cancer in women in the USA [55]. The American Cancer Society estimates that 52,630 new cases will be diagnosed in 2014 and 8,590 women will die from this disease [4]. Eighty percent of EC are type I and are characterized by expression of estrogen receptor (ER) [12, 18, 35, 46]. There are three main forms of estrogen, estrone (E1), 17β-estradiol (E2), and estriol (E3). In the nonpregnant uterus, E2 is the dominant regulatory estrogen. Unopposed, chronic or excess exposure to estrogens, including E2 and the adipocyte produced E1, are the main risk factors for type I EC [25].
E2 acting through ERα provides the primary proliferative signal in the uterine epithelium, and hyperestrogenicity is a major risk factor for EC [21, 23]. Traditionally, ERα has been thought of as ligand-dependent transcription factor that influences gene regulation. However, increasing evidence implicates transcription-independent actions of ERα in both normal and pathological processes [8, 36, 43, 48]. Transcription-independent ERα signaling is involved in regulation of proliferation [60] and cytoskeletal remodeling [2]. Additionally, non-nuclear ERα signaling has been implicated in invasion, migration, and metastasis in hormone sensitive breast cancer cells [7, 14, 15, 66]. Emerging data highlight the importance of rapid actions of estrogens; however, the role of transcription-independent E2 signaling in the endometrium and in EC is poorly understood.
During the normal menstrual cycle, phosphatase and tensin homolog (PTEN) levels fluctuate, suggesting that tumor suppressor PTEN is regulated by hormones in the endometrium [37]. PTEN regulates growth in normal cells via its lipid phosphatase activity. Specifically, PTEN antagonizes the phosphoinositide 3-kinase (PI3K)/Akt survival and growth pathway by converting phosphatidylinositol (3,4,5)-trisphosphate (PIP3) to phosphatidylinositol 4,5-bisphosphate (PIP2) to decrease available PIP3 for downstream signaling [28, 32, 50, 51].
PTEN phosphatase activity is regulated through oxidation [27], acetylation [39], ubiquitination [31], and phosphorylation [38, 56]. Phosphorylation at three key regulatory sites on the C terminus of PTEN (S380, T382, and T383) has been shown to decrease lipid phosphatase activity [56]. Decreased PTEN activity and consequent increased AKT signaling result in increased proliferation, inhibition of apoptosis, and resistance to progestin therapy [49]. Stimuli that induce phosphorylation of PTEN may therefore confer shifts in PTEN activity, which have been shown to cause endometrial hyperplasia and uterine dysplasia in vivo [3].
The normal endometrium cycles between periods of dramatic proliferation and differentiation in response to changing hormone levels. Unexpectedly, work from two different labs shows that PTEN protein levels are the highest in uterine epithelial cells during the pro-growth, E2-dominated, proliferative phase of the menstrual cycle [1, 37]. However, in these studies PTEN phosphorylation status and correlative activity was not assessed. Additionally, direct hormonal regulation of PTEN activity in the endometrium has not been investigated.
In normal cycling endometrial tissues, high levels of PTEN may be protective against potential aberrant proliferation, while low PTEN activity allows growth of the uterine lining. We hypothesize that E2 rapidly signals to key negative regulatory residues in the carboxy terminus of PTEN to suppress PTEN activity. We anticipate that risk factors for uterine cancer, which result in increased, chronic, or unopposed E2 exposure, cause an abnormal reduction in PTEN activity. Reduced PTEN activity and associated upregulation of AKT signaling promote cellular processes that contribute to a pro-cancer environment. As normal endometrial cell models are not available [26], we initially conducted molecular and biochemical studies using engineered EC cell models to determine if E2 signaling impacts PTEN phosphorylation and activity.
Materials and Methods
Cell Culture
Ishikawa EC cells and 293TN cells were obtained from American Type Culture Collection (Manassas, VA). Cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM; Fisher Scientific, Pittsburgh, PA) supplemented with 10 % (v/v) fetal calf serum (Thermo Scientific, Rockford, IL) and 50 μg/mL penicillin and streptomycin (Mediatech Inc., Manassas, VA). Cells were maintained at 37 °C in 5 % CO2.
Antibodies and 17β-estradiol
Rabbit anti-PTEN, phospho-PTEN (S380, T382, and T383), AKT, β-actin, and GAPDH as well as mouse anti-phospho-AKT (S473) were purchased from Cell Signaling Technologies (Danvers, MA). Mouse anti-protein kinase CK2α was purchased from Millipore (Billerica, MA). Mouse anti-ERα, rabbit anti-ERα and rabbit anti-ERβ were purchased from Santa Cruz Biotechnology, Inc. (Dallas, TX). Rabbit anti-GPER antibody was supplied by GenScript USA Inc. (Piscataway, NJ). IRDye conjugated secondary antibodies used in Western immunoblotting are from LI-COR Biosciences (Lincoln, NE) while HRP-conjugated secondary antibodies used in Western immunoblotting are from Cell Signaling Technologies (Danvers, MA). E2 was diluted in 200 proof ethanol (Fisher Scientific, Pittsburgh, PA) and used at a final concentration of 10 nM (Sigma-Aldrich, St. Louis, MO).
17β-Estradiol Treatment
Cells at 80 % confluence were starved for 24 h in serum free media (phenol red free DMEM, Thermo Scientific, Rockford, IL) supplemented with 50 μg/mL penicillin and streptomycin (Mediatech Inc., Manassas, VA). Cells were then treated with either 10 nM E2 (Sigma-Aldrich, St. Louis, MO) or vehicle (100 % ethanol; Fisher Scientific, Pittsburgh, PA) for 0, 10, 30, or 50 min. Unless otherwise noted, all experiments were conducted as described here.
Western Immunoblotting
Cells were harvested in Laemmli’s SDS sample buffer (Bio-Rad, Hercules, CA) for Western blot analysis. Protein concentration was assessed using the bicinchoninic acid (BCA) assay following the manufacturer’s instructions (Thermo Scientific, Rockford, IL). Proteins were resolved by 10 % SDS polyacrylamide gel electrophoresis and transferred to nitrocellulose membrane (Bio-Rad, Hercules, CA). Western blotting was preformed as per standard protocols provided by the antibody manufacturer. When IRDye conjugated secondary antibodies were used, resultant membranes were scanned by Odyssey CLx (LI-COR Biosciences, Lincoln, NE). Quantification was completed using Odyssey CLx software (LI-COR Biosciences, Lincoln, NE). When HRP-conjugated secondary antibodies were used, densitometry was used to quantify developed X-ray films (ISC BioExpress, Kaysville, UT) using Bio-Rad Analyzer Quantity One software (Bio-Rad, Hercules, CA).
Cellular Fractionation
One million cells were fractionated with NE-PER Nuclear and Cytoplasmic extraction kit following the manufacturer’s instructions (Thermo Scientific, Rockford, IL).
PTEN Immunoprecipitation and Lipid Phosphatase Assay
Cells were harvested in phosphate free nondenaturing buffer (20 mM Tris base, pH 7.4, 150 mM NaCL, 1 mM EGTA, 1 % v/v Triton X-100). Protein G sepharose beads (GE Healthcare Life Sciences, Piscataway, NJ) were pre-incubated with 3 % bovine serum albumin (Fisher Scientific, Pittsburgh, PA) for 1 h and washed in phosphate free nondenaturing buffer. After pre-incubation, 2.5 μg of antibody and cell lysates were added to beads and incubated end-over-end for 1 h at 4 °C. Cells were washed in phosphate free nondenaturing buffer and centrifuged at 8,000×g for 5 min at 4 °C followed by PTEN phosphatase assay. PTEN lipid phosphatase activity was assessed using the PTEN Malachite Green Assay (Echelon Biosciences Inc., Salt Lake City, UT). Briefly, immunoprecipitated PTEN was incubated with PtdIns(3,4,5)P3 substrate for 15 min at 37 °C in a buffer containing malachite green molybdate (Echelon Biosciences Inc., Salt Lake City, UT). Free phosphate was observed via formation of green molybdophosphoric acid complex and absorbance at 620 nm was measured. Free phosphate (pmol) was determined by interpolation from a standard curve.
Co-immunoprecipitation
Ten million cells were harvested and lysates were prepared in nondenaturing buffer (50 mM Tris–HCl pH 7.4, 1 % (v/v) NP-40, 0.5 % (v/v) Na-deoxycholate, 150 mM NaCL, 1 mM EDTA, and 50 mM NaF). Lysates were pre-cleared by 1 h incubation with protein G sepharose beads (GE Healthcare Life Sciences, Piscataway, NJ). Lysates were incubated with 2.5 μg of antibody at 4 °C overnight. Blocked (3 % BSA × 1 h) protein G sepharose beads (GE Healthcare Life Sciences, Piscataway, NJ) were added to the lysate + antibody mixture and incubated for 1 h at 4 °C. Beads were washed in nondenaturing buffer and centrifuged at 8,000×g for 5 min at 4 °C. Laemmli’s SDS sample buffer (Bio-Rad, Hercules, CA) was then added to the samples for Western blot analysis.
Transfections
One million EC cells were transfected with Lipofectamine 2000 following manufacturer’s instructions (Life Technologies, Grand Island, NY). A 1:4 ratio of DNA to Lipofectamine 2000 transfection reagent was used. For transient transfections, pGZ21-GFP-PTEN expression plasmid or empty PGZ21-GFP control plasmid was used. pGZ21 contains a CMV promoter and a GFP coding sequence with three amino acid residue substitutions (S65A, V68L, and S72A) to increase its fluorescence in mammalian cells [9]. Cells incubated in transfection mix for 6 h. Eight million 293TN cells were transfected with Lipofectamine 2000 following manufacturer’s instructions. A 1:1:10 ratio of DNA to pPACKH1 lentiviral packaging DNA to Lipofectamine 2000 was used (Systems Biosciences, Mountain View, CA). Cells were incubated in transfection mix for 48 h.
Lentiviral Constructs
PTEN sequence was removed from pIND/hygro plasmid (Life Technologies, Grand Island, NY) via digest with BamHI and NotI and cloned into the lentiviral expression vector pCDH-CMV-MCS-EF1-copGFP (System Biosciences, Mountain View, CA). Lentiviral particles were produced in 293TN packaging cells. Media containing packaged virus were collected 48 and 72 h after transfection. Ten million EC cells were incubated with 20 mL of DMEM media containing viral particles. After 72 h, puromycin selection was initiated (5 μg/mL). Puro selection was carried out for 3 days, and cells were diluted into 96-well cell culture dishes at an estimated frequency of 1 cell/well (Thermo Scientific, Rockford, IL). GFP-positive single clones were identified and expanded. Clones were screened for PTEN expression via Western blot.
Experimental Animals
Mouse experiments were conducted as previously described [17, 44]. Briefly, ovariectomized (ovx) female athymic nu/nu mice were obtained from Harlan Sprague–Dawley (Indianapolis, IN) at 5 to 6 weeks of age. All animals were implanted with silastic pellets containing E2 (2 mg 17 h-estradiol + 8 mg cellulose) or placebo (10 mg cellulose) [45]. Pellets resulted in 145 ± 47 pg/mL circulating estradiol. At 8 weeks mice were euthanized by CO2 asphyxiation, and uteri were excised and prepared for immunohistochemistry (IHC).
Immunohistochemistry
Formalin fixed paraffin embedded tissues were sectioned at 5 μm and mounted onto positively charged slides (Fisher Scientific, Pittsburgh, PA). Samples were de-paraffinized and rehydrated through descending series of ethanol/water baths. Tissues were antigen retrieved in citrate buffer, pH 6 (16 mM sodium citrate trisodium salt dihydrate and 4 mM citrate acid monohydrate). Samples were blocked with 5 % bovine serum albumin (w/v) in SuperBlock (Fisher Scientific, Pittsburgh, PA) followed by overnight incubation at 4 °C with primary antibody specific to phospho-PTEN (S380, T382, and T383; Abcam, Cambridge, MA), total PTEN, or phospho-AKT (S473; Cell Signaling, Danver, MA). Primary antibodies were diluted 1:100, 1:100, and 1:50, respectively, in Signal Stain Antibody Diluent (Cell Signaling, Danvers, MA). Negative control slides were performed by omitting the primary antibody. Slides were rinsed in IHC wash buffer (50 mM Tris–Cl, pH 7.5, 150 mM NaCl, 0.1 % Tween-20 (v/v)) and incubated with HRP-conjugated Rabbit Signal Boost (Cell Signaling, Danvers, MA) for 30 min. Immunopositive cells were visualized by addition of a 3,3-diaminobenzidine substrate (Vector Labs, Burlingame, CA), rinsed with IHC wash buffer and counterstained with hematoxylin (Sigma-Aldrich, St. Louis, MO). Samples were dehydrated through ascending series of water/ethanol baths followed by incubation in xylene (Sigma-Aldrich, St. Louis, MO). Slides were mounted with permount mounting media (Sigma-Aldrich, St. Louis, MO).
Quantification of IHC
Quantification of phospho-PTEN, total PTEN, and phospho-AKT IHC was preformed using NIS-Elements Imaging Software (Nikon Microscopes, Melville, NY). Uteri from a minimum of six ovx mice and nine E2-treated mice were analyzed. At least three uterine glands per mouse uterus were analyzed. Uterine glands were manually outlined and identified as regions of interest (ROI) for NIS-Elements Imaging Software analysis. Threshold measurements of immunopositive staining were applied to each ROI to measure protein abundance. The sum intensity measurement (SI) of positive staining in each identified gland (ROI) was divided by gland area in order to measure SI per unit area (SI/mm2).
Statistical Analysis
Data are expressed as change ± standard deviation (SD). Data were analyzed with Student’s t test between two groups of analysis of variance (ANOVA) coupled with Dunnett’s multiple comparison test for multiple pairwise comparisons. Probability values of P < 0.05 were considered to be statistically significant.
Results
E2 Regulates PTEN Phosphorylation, Protein Stability, and Lipid Phosphatase Activity
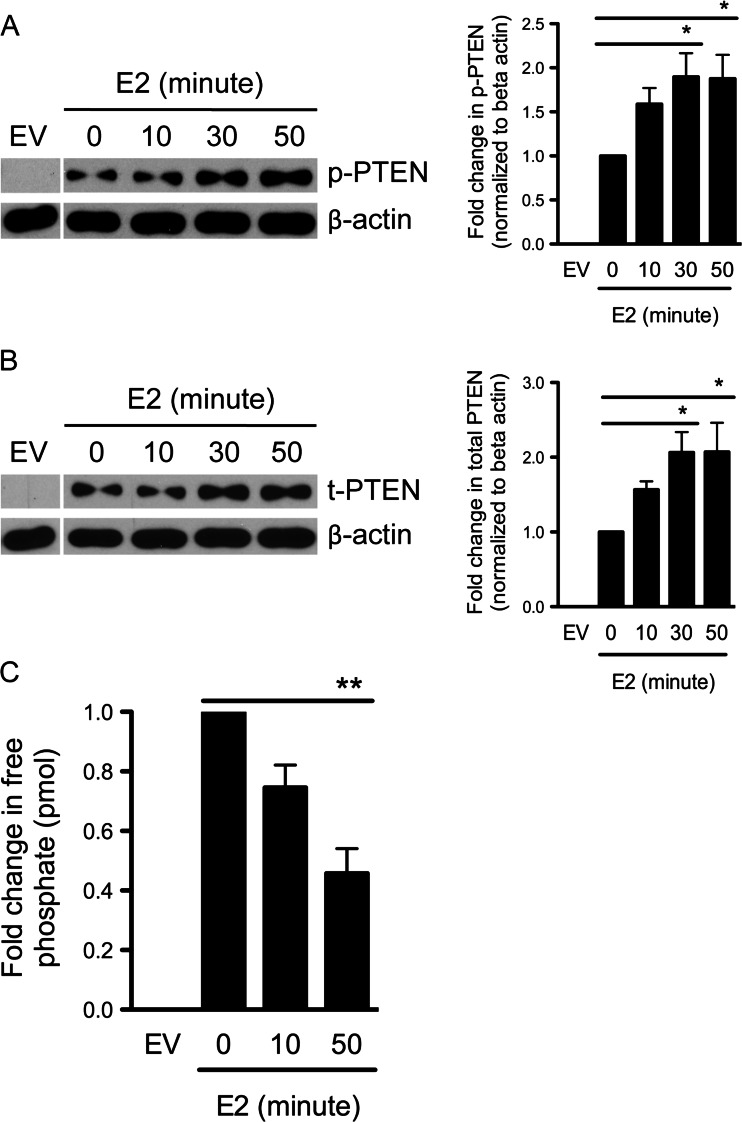
Seminal studies conducted by Vazquez et al. identified S380, T382, and T383 as key negative regulatory residues in the PTEN carboxy tail [56]. Phosphorylation of these residues resulted in decreased PTEN lipid phosphatase activity and increased protein stability [56]. However, specific stimuli that induce PTEN phosphorylation in vivo were not investigated. In order to determine if E2 signaling induced phosphorylation of PTEN carboxy terminal regulatory residues, we utilized ERα wild-type, type 1 Ishikawa endometrial cells (ISH-ERαWT). As ISH-ERαWT cells are PTEN null, we first transiently transfected cells with either an empty GFP-fusion vector or a GFP-PTEN expression construct. The transfected cells were starved in serum free media for 24 h, stimulated with 10-nM E2, and harvested over a 50-min time course for Western blot analysis. The Western blot in Fig. 1a shows that E2 induced phosphorylation of S380, T382, and T383 over the time course, as assayed by a phospho-specific PTEN antibody. The corresponding graph shows the average of phospho-PTEN normalized to the β-actin loading control in three independent experiments. E2 treatment induced a 2-fold, statistically significant increase in PTEN phosphorylation at 30 and 50 min. Using a pan-PTEN antibody, we also observed a concurrent increase in total PTEN protein levels, indicating increased PTEN stability (Fig. 1b). These data are consistent with the original phospho-PTEN mapping studies conducted by Vazquez et al., which demonstrated that PTEN stability is governed by phosphorylation at S380, T382, and T383 [56]. We have further observed that inhibiting PTEN phosphorylation blocks E2-induced PTEN protein stability (Supplemental Fig. 1). Therefore, increased PTEN stability requires E2-induced PTEN phosphorylation. Similar experiments were conducted in MCF7 breast cancer cells. E2 treatment also leads to increased PTEN phosphorylation and PTEN protein stability in MCF7 cells, suggesting that E2 regulation of PTEN may occur in a variety of hormonally responsive tissues (Supplemental Fig. 2).
Fig. 1.
E2 stimulation increases phospho-PTEN and total PTEN levels but decreases lipid phosphatase activity. a ISH-ERαWT cells were transiently transfected with a GFP-PTEN expression construct or empty vector (EV) followed by starvation for 24 h in serum-free media. Starved cells were treated with E2 for 0, 10, 30, or 50 min. Cells were harvested and analyzed via Western blotting with an antibody specific to phospho-PTEN (S380, T382, and T383) or b total PTEN. Corresponding graphs to the right represent quantification of fold change ± SD (n = 3) of a phospho-PTEN or b total PTEN normalized to β-actin (*P < 0.05 by ANOVA). c ISH-ERαWT cells were transiently transfected with a GFP-PTEN expression construct or EV followed by E2 treatment for 0, 10, or 50 min. Cells were lysed in nondenaturing lysis buffer followed by IP of exogenous PTEN. Immunoprecipitated PTEN was then exposed to PtdIns(3,4,5)P3 substrate. Resulting phosphatase activity was then measured via malachite colorimetric assay to calculate picomoles of free phosphate. Graph represent quantification of fold change ± SD (n = 3) of free phosphate (pmol) (**P < 0.01 by ANOVA)
In order to determine if changes in PTEN phosphorylation affected activity, we performed an immunoprecipitation (IP) lipid phosphatase activity assay in ISH-ERαWT cells expressing exogenous PTEN. In Fig. 1c, it can be seen that PTEN activity significantly decreased concurrently with increased phosphorylation at S380, T382, and T383. Taken together, these results indicate that E2 induces PTEN phosphorylation, increases PTEN protein stability and decreases PTEN lipid phosphatase activity. Furthermore, the timing of these actions (30–50 min) suggests that rapid, nongenomic signaling mediates these effects.
E2-Induced Phosphorylation and Regulation of PTEN Activity Is ERα-Dependent
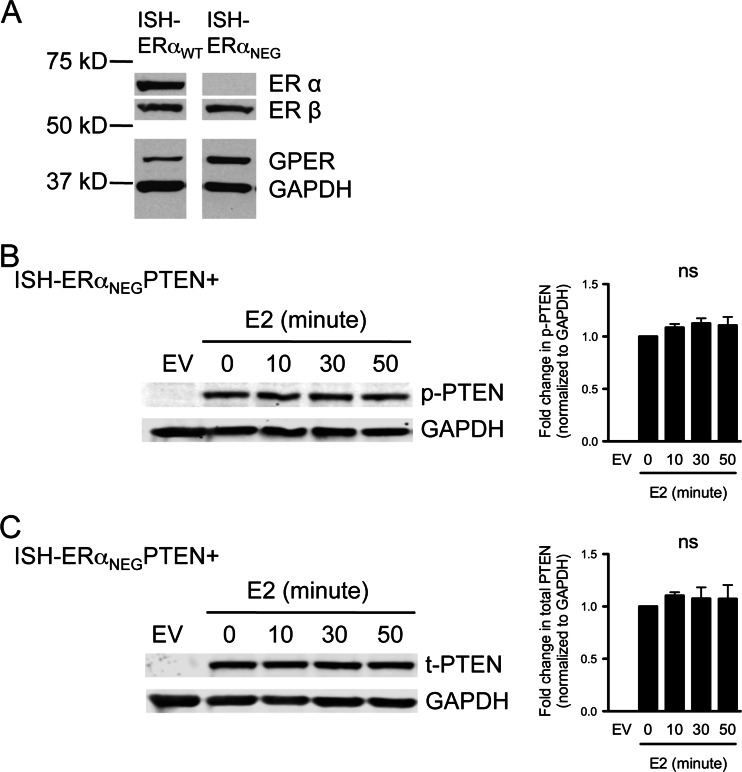
E2 has been shown to rapidly signal through ERα [36], estrogen receptor-β (ERβ) [65] and an alternate ER, G protein-coupled estrogen receptor 1 (GPER) [5, 13]. In order to determine if E2 signals through classical nuclear ERα to regulate PTEN activity, we utilized an ERα negative subclone of Ishikawa cells, the ISH-ERαNEG cells. ISH-ERαNEG cells lack detectable ERα, but express ERβ and GPER (Fig. 2a). Our pilot studies (Fig. 1) utilized transient transfection of PTEN, as Ishikawa endometrial cells are PTEN null due to a stop codon mutation in exon 8 [59]. To facilitate further studies, cell lines that stably express PTEN were developed and these cell lines are used in the remainder of the experiments presented in this manuscript unless otherwise stated (described and characterized in Supplemental Fig. 3). ISH-ERαNEG PTEN+ cells were starved for 24 h in serum-free media followed by E2 treatment over the indicated time course. Cells were harvested and analyzed for phospho and total PTEN expression via Western blotting. Lane 1 of Fig. 2b shows lysates prepared from ISH-ERαNEG parental cells transduced with viral particles expressing an empty pCDH vector (EV). In the ISH-ERαNEG PTEN+ cells, basal PTEN phosphorylation was observed (0 min time point), however E2 stimulation did not induce additional phosphorylation of PTEN at residues S380, T382, and T383 (10–50 min time points). The corresponding graph shows the average of phospho-PTEN normalized to the GAPDH loading control from five independent experiments. Additionally, using a total PTEN antibody we show that PTEN protein levels did not increase in ISH-ERαNEG PTEN+ cells upon E2 stimulation (Fig. 2c). As a control, similar experiments were conducted concurrently using the ISH-ERαWT PTEN+ cells. In the control experiments increased PTEN C-terminal phosphorylation and increased total PTEN protein were observed with E2 stimulation (Supplemental Fig. 3). These data show that E2 signals through ERα, but not ERβ or GPER, to modulate PTEN phosphorylation and protein stability.
Fig. 2.
E2 regulation of PTEN is ERα-dependent. a Western blot analysis of whole cell lysates from ISH-ERαWT and ISH-ERαNEG cells with antibodies specific to ERα, ERβ, GPER, and GAPDH. b ISH-ERαNEG PTEN+ cells were starved in serum free media for 24 h followed by E2 treatment for 0, 10, 30, or 50 min. ISH-ERαNEG PTEN+ cells and ISH-ERαNEG empty vector control cells (EV) were harvested and analyzed via Western blotting with an antibody specific to phospho-PTEN (S380, T382, and T383) or c total PTEN. Corresponding graphs to the right represent quantification of fold change ± SD (n = 5) of a phospho-PTEN or b total PTEN normalized to GAPDH (P = ns, by ANOVA)
Cytosolic ERα Signaling Is Sufficient to Mediate PTEN Regulation
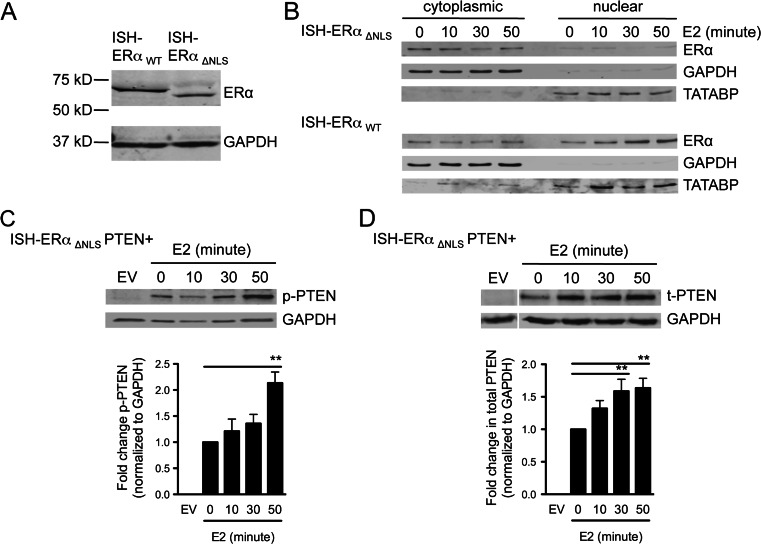
To directly test whether E2 regulates PTEN phosphorylation and activity exclusively through cytosolic signaling mechanisms, we developed a PTEN positive Ishikawa cell line that stably expresses an exogenous ERα mutant, lacking the nuclear localization sequence (ISH-ERαΔNLS PTEN+). Characterization of this cell line is shown in Fig. 3a, b. Figure 3a shows the results of a Western blot using whole cell lysates. ERαΔNLS migrates approximately 5 kDa lower than ERαWT due to the nuclear localization sequence deletion (amino acids 252 through 303) [63]. Figure 3b shows the results of cellular fractionation followed by Western blotting of the cytosolic and nuclear lysates of ISH-ERαΔNLS PTEN+ and ISH-ERαWT PTEN+ cells. GAPDH and TATA binding protein were used as markers to assess cytosolic and nuclear fraction purity. It can be seen that stimulation with E2 does not lead to ERαΔNLS nuclear accumulation (Fig. 3b, top panel). As a control, ISH-ERαWT PTEN+ cells were also fractionated, and E2 induced the expected nuclear accumulation of ERαWT (Fig. 3b, lower panel). Additionally, in transcription assays using an ER element-luciferase reporter construct, we observed no E2-stimulated transcription activity in the ISH-ERαΔNLS PTEN+ cells when compared with ISH-ERαWT PTEN+ cells (not shown). Taken together, these data demonstrate that ISH-ERαΔNLS PTEN+ cells express transcriptionally incompetent ERα that do not translocate to the nucleus with E2 treatment. As such, they provide a useful model for studying cytosolic ERα signaling.
Fig. 3.
E2/ERα cytosolic actions are sufficient to regulate PTEN phosphorylation and protein stability. a Western blot analysis of whole cell lysates from ISH-ERαWT and ISH-ERαΔNLS cells with antibodies specific to ERα and GAPDH. b ISH-ERαΔNLS cells (top) and ISH-ERαWT cells (bottom) were starved in serum-free media for 24 h followed by E2 treatment for 0, 10, or 50 min. Cell lysates were collected for biochemical subcellular fractionation. Cytoplasmic (left) and nuclear (right) fractions were analyzed via Western blotting. Compartmentalization of ERα over E2 treatment times was assessed by immunoblotting with an antibody specific to ERα. Fractionation purity was determined using antibodies specific to nuclear protein, TATABP, and cytosolic protein, GAPDH. c ISH-ERαΔNLS PTEN+ cells were starved in serum free media for 24 h followed by E2 treatment for 0, 10, 30, or 50 min. ISH-ERαΔNLS PTEN+ cells and ISH-ERαΔNLS empty vector control cells (EV) were harvested and analyzed via Western blotting with an antibody specific to phospho-PTEN (S380, T382, and T383) or d total PTEN. Corresponding graphs below Western blot image represent quantification of fold change ± SD of c phospho-PTEN or d total PTEN normalized to GAPDH (n = 5 and 9, respectively. **P < 0.01 by ANOVA)
We used the ISH-ERαΔNLS PTEN+ cells to exclude potential nuclear contributions of E2/ERα signaling to the PTEN regulatory residues S380, T382, and T383. ISH-ERαΔNLS PTEN+ cells were starved in serum- free media for 24 h, treated with E2, and harvested at 0, 10, 30, and 50 min, followed by Western blotting for PTEN regulatory phospho-residues. Figure 3c shows a representative Western blot of phospho-PTEN (S380, T382, and T383) in cells expressing the cytosolic only ERαΔNLS mutant. We observed a 2-fold increase in phospho-PTEN levels, indicating that nuclear ERα is not necessary for E2/ERα signaling to PTEN carboxy tail regulatory residues. The corresponding graph shows the fold change in phospho-PTEN levels normalized to the GAPDH loading control from five independent experiments. In order to determine if the ERαΔNLS mutant also conferred increased PTEN protein stability, the same lysates were probed with an antibody against total PTEN (Fig. 3d). We observed increased protein stability with E2 stimulation. The graph in Fig. 3d shows the fold change in total PTEN normalized to the GAPDH loading control from nine independent experiments. Taken together, the results in Fig. 3c, d demonstrate that rapid, non-nuclear E2/ERα signaling mediates PTEN phosphorylation at key negative regulatory residues, and increases PTEN stability.
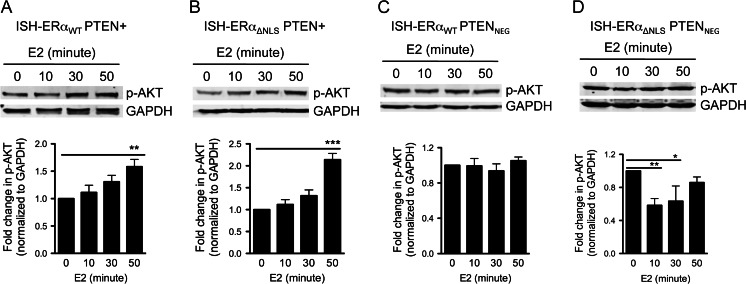
E2-Induced Activation of AKT Requires PTEN
PTEN lipid phosphatase activity antagonizes the PI3K/AKT signaling axis [32, 50, 57]. Therefore, negative regulation of PTEN by E2 is predicted to lead to increased AKT activity. In order to determine if E2/ERα-dependent negative regulation of PTEN causes increased AKT activity, we treated ISH-ERαWT PTEN+ cells and ISH-ERαΔNLS PTEN+ cells with E2, harvested lysates at 0, 10, 30, and 50 min and probed for phospho-AKT (S473) and total AKT. Figure 4a shows a representative Western blot. The graph below shows the average fold change in phospho-AKT normalized to GAPDH from four independent experiments. E2 treatment in ISH-ERαWT PTEN+ cells lead to an average 1.5-fold increase in AKT phosphorylation at serine 473, a phospho-residue associated with AKT activation. However, no change was observed in total AKT levels (not shown).
Fig. 4.
E2 stimulation increases phospho-AKT in a PTEN-dependent manner. a ISH-ERαWT PTEN+ and b ISH-ERαΔNLS PTEN+ were starved in serum free media for 24 h followed by E2 treatment for 0, 10, 30, or 50 min. Cells were harvested and analyzed via Western blotting with an antibody specific to phospho-AKT (473) and total AKT. Corresponding graphs below Western blot image represent quantification of fold change ± SD of phospho-AKT normalized to GAPDH (ISH-ERαWT PTEN+ cells, n = 4 (*P < 0.05 by ANOVA) and ISH-ERαΔNLS PTEN+ cells, n = 6 (***P < 0.001 by ANOVA)). c ISH-ERαWT PTENNEG and d ISH-ERαΔNLS PTENNEG cells were starved in serum-free media for 24 h followed by E2 treatment for 0, 10, 30, or 50 min. Cells were harvested and analyzed via Western blotting with an antibody specific to phospho-AKT (473) and total AKT. Corresponding graphs below Western blot image represent quantification of fold change ± SD (n = 3) of phospho-AKT normalized to GAPDH (ISH-ERαWT PTENNEG cells, P = ns by ANOVA and ISH-ERαΔNLS PTENNEG cells, **P < 0.01 by ANOVA). Quantification of fold change ± SD (n = 3) of total AKT normalized to GAPDH resulted in P = ns, by ANOVA, in all cell lines (data not shown)
In order to confirm that non-nuclear actions of ERα are responsible for increased AKT phosphorylation, we performed similar experiments using the ISH-ERαΔNLS PTEN+ cells. Figure 4b shows a representative Western blot for phospho-AKT. The corresponding graph shows the average fold change in phospho-AKT normalized to GAPDH from six independent experiments. We observed an average 2-fold increase in AKT phosphorylation in response to E2 stimulation in our cell line expressing the cytosolic only, deleted NLS ERα mutant. Total AKT levels did not change with E2 stimulation (not shown). These data indicate that the cytosolic actions of ERα are sufficient to promote E2-stimulated AKT phosphorylation.
Our data show that E2/ERα directly modulates PTEN activity, and we observed rapid increases in AKT phosphorylation with E2 treatment. However, rapid E2/ERα signaling has been shown to activate AKT directly by interacting with the p85 regulatory subunit of PI3K [6, 33, 48]. In order to show that E2-induced AKT phosphorylation in EC cells is due to ERα acting on PTEN, and not PI3K, we examined the effect of E2 on AKT phosphorylation status in PTEN null cells. ISH-ERαWT PTENNEG cells were treated with E2, harvested, and phospho-AKT status, as well as total AKT levels, were analyzed using Western blotting (Fig. 4c). In the representative Western blot, it can be seen that E2 treatment does not increase phoshorylation of AKT above baseline in ERα wild-type cells lacking PTEN. Total AKT levels also did not change upon E2 treatment (not shown). The corresponding graph shows the average fold change in phospho-AKT normalized to GAPDH from three independent experiments. In order to determine if cytosolic-only ERα signaling impacted AKT phosphorylation in the absence of PTEN, identical experiments were performed using the PTEN negative, ERαΔNLS mutant cell line (Fig. 4d). In these experiments, it is unclear whether the PTEN-independent decrease in phospho-AKT (10 and 30 min) is biologically relevant or is a result of enhanced cytosolic ERα signaling. Total AKT levels did not significantly increase above baseline or decrease below baseline (data not shown). Taken together, the results in Fig. 4 show that E2/ERα signaling increases AKT phosphorylation via negative regulatory actions on PTEN and requires only cytosolic ERα mechanisms.
ERα Forms a Complex with Protein Kinase CK2 and PTEN in Endometrial Cancer Cells
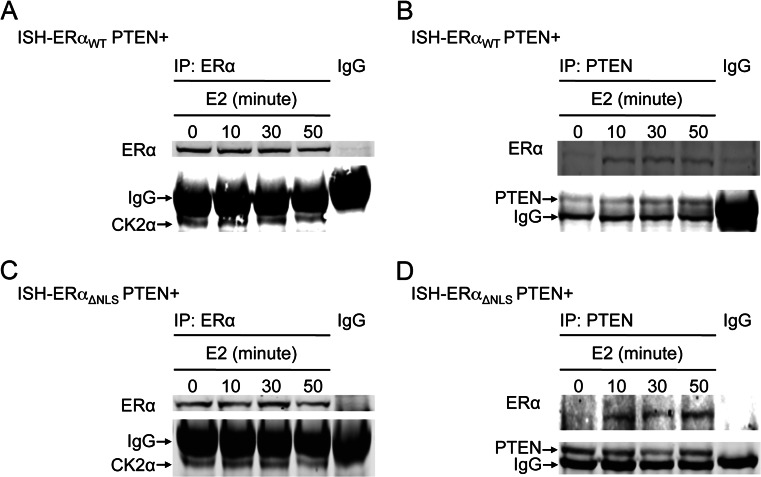
The C-terminal tail of PTEN contains protein kinase CK2 (formerly termed “casein kinase 2”) consensus sequences that encompass the regulatory residues S380, T382, and T383 [53]. Additionally, in vitro studies indicate that this region of PTEN can be phosphorylated by CK2 [53]. We observed that the CK2 inhibitor, (E)-3-(2,3,4,5-tetrabromophenyl) acrylic acid (TBCA), blocked E2-induced PTEN phosphorylation of S380, T382, and T383 and E2-induced increases in total PTEN (Supplemental Fig. 1). As ERα is thought to promote rapid signaling through interactions with cytosolic kinases, we sought to determine if ERα and CK2α (the catalytic subunit of the CK2 holoenzyme) form a complex in EC cells using co-immunoprecipitation (co-IP). ISH-ERαWT PTEN+ cells were serum starved for 24 h and treated with E2 for 0, 10, 30, or 50 min, followed by IP with an antibody specific to ERα. Normal IgG was used as a control to show antibody specificity. Lysates were analyzed via Western blot using an antibody against CK2α. In ISH-ERαWT PTEN+ cells CK2α co-immunoprecipitated with ERα in both the absence and presence of E2 (Fig. 5a). To determine if ERα and PTEN form a complex, we performed co-IP experiments using an antibody against PTEN, and probed the resultant Western blots with an antibody against ERα. Figure 5b shows that ERα and PTEN form a complex only in the presence of E2. Our co-IP experiments show that ERα and CK2α exist in a complex in both the presence and absence of E2 and that E2 promotes the formation of a complex that contains both ERα and PTEN.
Fig. 5.
ERα and CK2α exist in a complex in both absence and presence of E2, while ERα and PTEN form a complex in an E2-dependent manner. a ISH-ERαWT PTEN+ and c ISH-ERαΔNLS PTEN+ cells were starved in serum free media for 24 h followed by E2 treatment for 0, 10, 30, or 50 min. Cells were harvested in nondenaturing buffer followed by immunoprecipitation (IP) with an antibody specific to ERα or IgG control antibody. Immunoprecipitates were analyzed via Western blotting with an antibody specific to ERα. Co-immunoprecipitation (co-IP) of CK2α was assessed with an antibody specific to CK2α. IgG arrow shows heavy chain IgG from ERα IP antibody (50 kDa). Representative Western blot images for a ISH-ERαWT PTEN+ cells and c ISH-ERαΔNLS PTEN+ cells shown (n = 3). b ISH-ERαWT PTEN+ and d ISH-ERαΔNLS PTEN+ cells were starved in serum free media for 24 h followed by E2 treatment and IP with an antibody specific to PTEN or IgG control antibody. Immunoprecipitates were analyzed via Western blotting with an antibody specific to PTEN and co-IP of ERα was assessed with an antibody specific to ERα. IgG arrow shows heavy chain IgG from PTEN IP antibody (50 kDa). Representative Western blot images for b ISH-ERαWT PTEN+ cells and d ISH-ERαΔNLS PTEN+ cells shown (n = 3)
As the ERα nuclear localization sequence mutant promoted phosphorylation of PTEN on regulatory residues in response to E2, we repeated the co-IP experiments described in Fig. 5a, b using the ISH-ERαΔNLS PTEN+ cell line. The ERαΔNLS deletion mutant also constitutively complexes with CK2α and forms a complex with PTEN in an E2-dependent manner (Fig. 5c, d, respectively). These data provide evidence that deletion of amino acids 252 through 303 does not abolish the ability of ERαΔNLS to complex with both CK2α and PTEN. We propose that E2 exposure recruits PTEN to the ERα:CK2α complex, thereby providing a potential mechanism by which rapid E2/ERα actions lead to phosphorylation and negative regulation of PTEN activity. However, further molecular studies are required to confirm this pathway.
Long-Term E2 Exposure Correlates with Increased Phospho-PTEN, Total PTEN, and Phospho-AKT in Normal Murine Endometrial Cells
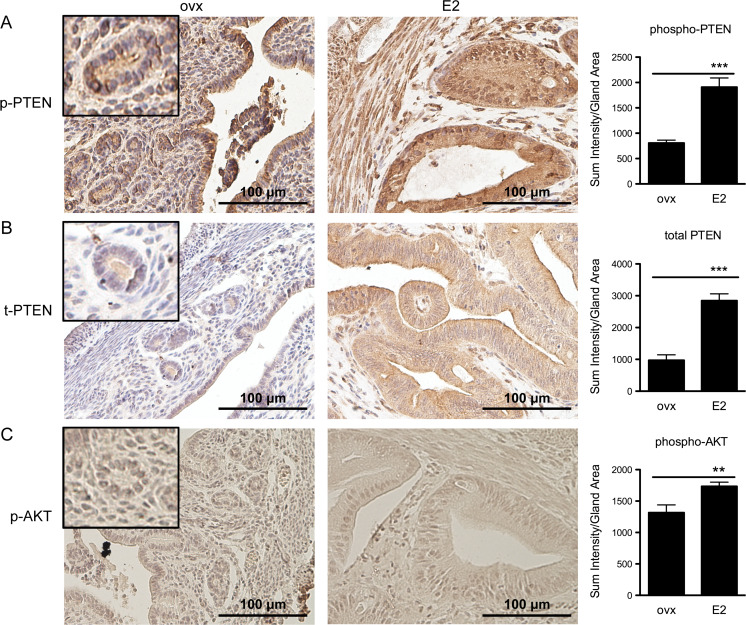
The data in Figs. 1, 2, 3, 4, and 5 utilize EC cell culture models to show that rapid E2 actions can regulate PTEN phosphorylation, stability and activity. Additionally, these data show that ERα (and not ERβ or GPER) is necessary for E2 regulation of PTEN phoshorylation and that only cytosolic actions of ERα are required. Using these models, we show that E2-stimulated reduction in PTEN lipid phosphatase activity results in increased AKT phosphorylation at the S473 activation site. To determine a potential role for E2 regulation of PTEN in vivo, we used IHC to examine phospho-PTEN (S380, T382, and T383), total PTEN and phospho-AKT (S473) status in mice uteri exposed to long-term E2 treatment as described [17, 44]. Figure 6a shows representative images of uterine glands stained for phospho-PTEN from ovx mice (Fig. 6a, ovx) or from mice exposed to sustained E2 for 8 weeks (Fig. 6a, E2). It can be seen that the columnar endometrial cells lining the glands exhibit increased phospho-PTEN staining in the uteri exposed to E2 when compared with uteri from ovx mice. As endometrial cells in ovx mice are smaller than endometrial cells of mice exposed to E2, the insert shows a ×2.5 magnification to allow comparison at the individual cell level. The corresponding graph shows the average SI per gland area of nine ovx or E2-treated mice. The phospho-PTEN SI/gland area was 2.3 times greater in the uteri of mice exposed to 8 weeks of E2 treatment as compared with the ovx control mice. Figure 6b shows the results of IHC staining of mouse uteri with an antibody against total PTEN. As shown in the representative images and corresponding graph, uterine glands from mice exposed to E2 for 8 weeks showed an increase in total PTEN when compared with the ovx control mice.
Fig. 6.
Unopposed E2 treatment leads to increased phospho-PTEN, total PTEN and phospho-AKT in murine endometrium. Mice were ovariectomized (ovx) or ovariectomized and treated with E2 (E2) for 8 weeks. Uteri from ovx and E2 mice were formalin fixed and paraffin embedded. Sections (5 μm) were stained with antibodies specific for a phospho-PTEN (S380, T382, and T383), b total PTEN, and c phospho-AKT (S473) and counterstained with hematoxylin. Corresponding graphs to the right represent quantification of SI/gland area ± SD (phospho-PTEN, n = 9 ovx, n = 9 E2 mice (***P < 0.001 by Student’s t test); total PTEN, n = 6 ovx, n = 10 E2 mice (***P < 0.001 by Student’s t test); and phospho-AKT, n = 6 ovx n = 9 E2 mice (**P < 0.01 by Student’s t test)). Representative fields were taken at ×40 magnification. ovx inset gland magnified an additional ×2.5. Scale bar, 100 μm
We next sought to determine if phospho-PTEN observed in endometrial glands from mice exposed to sustained levels of E2, correlated with the predicted increase in AKT activity. To this end, we stained uteri from ovx and E2 exposed mice with an antibody directed against phospho-AKT (S473). Quantification of representative glands yielded a 1.3-fold increase in phospho-AKT in E2 exposed endometrial glands when compared with ovx controls (Fig. 6c).
Taken together, the data in Fig. 6 show that sustained E2 exposure leads to increased phospho-PTEN, total PTEN and phospho-AKT in the context of a normal mouse uterus. While the IHC data are correlative, they extend the molecular signaling data obtained from our cell lines and suggest that E2 may regulate PTEN and AKT in vivo.
Discussion
Our discovery that rapid E2 signaling decreases PTEN tumor suppressive activity is an extraordinarily relevant finding within the context of the endometrium, as hyperestrogenicity, or unopposed E2 stimulation, is thought to cause type 1 EC [23, 25, 34]. It has long been known that E2 activates ER transcriptional activity to promote proliferation in normal uterine epithelial cells and that type 1 EC is dependent on E2 signaling [21, 25]. However, the effects of transcription-independent E2 signaling on the endometrium or endometrial carcinoma have not been fully investigated. Our data in human EC cells demonstrate that rapid E2 action leads to decreased PTEN activity. Additionally we show that sustained E2 treatment in a mouse model correlates with increased phospho-PTEN and decreased PTEN activity as assessed by phospho/active AKT status. While the majority of our studies focus on endometrial cancer, we have observed similar results in MCF7 breast cancer cells (Supplemental Fig. 2). These data provide a second pathway by which E2 exposure may increase the risk of steroid-dependent cancers, including breast and endometrial.
E2 treatment also leads to the predicted increase in PTEN protein stability. In the context of the normal endometrium, high levels of PTEN protein may be protective against potential aberrant proliferation. Our mice data support the conclusion that E2 exposure corresponds with PTEN phosphorylation and decreased function as assessed by activity of the downstream target, AKT. Essentially, the function of high levels of low activity PTEN observed during the proliferative phase of the normal menstrual cycle may function as a “brake” in the event of aberrant proliferative signals. Hyperestrogenicity may shift the amount of inactive PTEN beyond the normal protective range, causing activation of AKT signaling, thereby increasing and risk for hyperplasia and endometrial cancer.
We show that E2 negatively regulates PTEN activity solely through ERα cytosolic mechanisms in EC cells. Jakacka et al. have shown that mice expressing mutant ERα, which are unable to bind estrogen response elements (NERKI+/− mouse), show significantly increased uterine weight as well as cystic endometrial hyperplasia, a precursor to endometrial cancer [22]. Furthermore, microarray data from NERKI+/− mice uteri, show E2-dependent regulation of the Wnt/β-catenin signaling pathway, a pathway highly misregulated in many cancers [10, 19, 61]. The impact of rapid E2 signaling in the uterus may be an underappreciated, yet significant, contributor to endometrial cancer initiation and progression.
By contrast, in a mouse model expressing membrane only ERα (MOER mouse) only atrophic uteri were observed [41]. Additionally, when mice expressing wild-type ERα were treated with an estrogen-dendrimer conjugate, which sequesters ERα in the cytosol, no uterine proliferation was noted [8]. Therefore, our understanding of the role of rapid, nongenomic E2 signaling and how it contributes to normal uterine development as well as uterine carcinogenesis is only beginning to be understood.
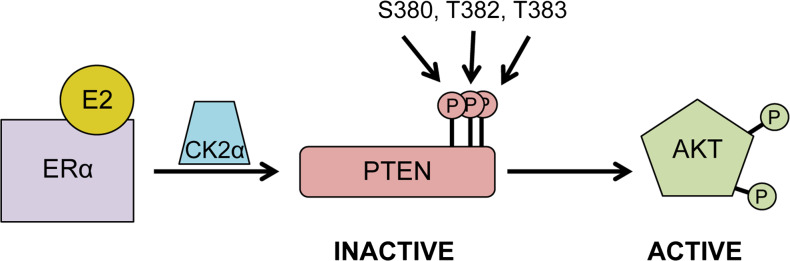
Our data show that E2 stimulates increased PTEN phosphorylation at S380, T382, and T383, leading to decreased activity and consequent activation of AKT in endometrial cancer cells (Fig. 7). Additionally, our IHC data show significant increases in phospho-PTEN (inactive) and phospho-AKT (active) in mice exposed to sustained circulating E2 for 8 weeks [17, 44]. Hyperactivation of AKT promotes cancer through several pathways [24, 47]. AKT enacts its proliferative effects through inhibition of p27, resulting in a loss of G1 arrest in breast cancer cells, and promotes VEGF production and angiogenesis in prostate cancer cell [29, 67]. Upregulated phospho-AKT is also positively correlated with increased survivin expression in endometrial tumors, causing further decreases in apoptosis through inhibition of caspase activation [40, 52]. Overall, increased AKT signaling, a result of E2-induced PTEN inactivation, may contribute to increased endometrial cancer risk through a number of signaling pathways.
Fig. 7.
Model of ERα regulation of PTEN. E2-bound ERα induces phosphorylation of PTEN at C terminus regulatory residues S380, T382, and T383 via CK2α. Phosphorylation of PTEN at these residues decreases PTEN lipid phosphatase activity, which leads to downstream activation of AKT signaling
E2 treatment resulted in reduced PTEN activity in endometrial cancer cells. However, PTEN activity was not fully abolished. While complete loss of PTEN is seen in many human cancers, it is becoming clear that incremental changes in PTEN activity may significantly impact susceptibility to a variety of cancers, including endometrial cancer [3, 54]. Pten +/− haploinsufficient mice, which express 50 % of normal PTEN levels and show high levels of active AKT staining, show increased incidence of endometrial neoplasia [11, 24, 42, 58]. Furthermore, endometrial tumors from the Pten +/− haploinsufficient mice show elevated phospho-AKT levels as well as phosphorylation of the Bcl-2-associated death promoter (Bad) protein, a known target of AKT that allows for evasion of apoptosis through binding of 14-3-3 proteins [24, 64]. Genetically engineered Pten hyper (Ptenhy/+) mice, which express 80 % PTEN mRNA and protein when compared with wild-type mice, develop endometrial atypical complex hyperplasia, a precursor to endometrial cancer [3]. Mammory glands from Pten hyper mice displayed an increase in proliferative index, and the majority of female mice developed mammory tumors [3]. Additionally, Pten hypo (Ptenhy/−) mice (20 % PTEN expression) develop prostate hyperplasia and invasive prostate cancer [54]. Therefore, growing evidence demonstrates that even slight alterations in PTEN activity levels have significant biological consequences in the uterine environment as well as in other reproductive tissues.
We observed that inhibition of CK2 with TBCA abolished E2 induced phosphorylation of PTEN, and PTEN is a known substrate of CK2. A recent report by Hagan et al. shows that progesterone receptor indirectly interacts with CK2 via a common docking domain on the N terminus of progesterone receptor-B [16]. Furthermore, CK2 has been shown to phosphorylate ERα on S282 and S559 in vivo and in vitro [62]. We have shown that CK2 phosphorylates PTEN in our cells; however, it is possible that CK2 also acts on ERα S282 and S559 to modulate rapid ERα signaling to PTEN. Additionally, Lin et al. have shown that the androgen receptor and PTEN directly interact through the androgen receptor DBD and N terminus phosphotase domain of PTEN (amino acids 110–163) [30]. As nuclear receptors are highly conserved, we sought to determine if similar interactions may provide a potential mechanism by which rapid E2/ERα interactions regulate PTEN. We observed a constitutive cystosolic complex containing ERα and CK2, and an E2-dependent complex formation between ERα and PTEN. Our data suggest that E2 exposure recruits PTEN to a cystolic complex containing ERα and CK2α and provide a potential mechanism by which rapid E2 signaling regulates PTEN.
While our studies focus on endometrial cancer cells, we have observed similar results in MCF7 breast cancer cells (Supplemental Fig. 2). These data support observations in the Pten hyper mice as a reduction in PTEN correlated with an increase in phospho-AKT (S473) and Ki-67 in mammory tumors [3]. Additionally, pilot studies using microdissected epithelial cells from random periareolar fine needle aspiration samples have shown that women at risk for breast cancer, have elevated levels of phosphorylated PTEN (S380), total PTEN and active phospho-AKT (S473) [20]. These studies suggest that E2 regulation of PTEN may be an important mechanism in a number of steroid responsive tissues. Furthermore, other steroids and steroid analogs may also regulate PTEN.
E2 has been thought to be a risk factor for uterine cancer solely through proliferative mechanisms. Our data demonstrate that cytosolic E2/ERα actions decrease PTEN tumor suppressive activity, thereby providing an alternate mechanism by which hyperestrogenicity may increase the risk for EC. Current treatment of EC involves hysterectomy, which is costly and associated with high morbidity and mortality. Our research suggests that expanding studies focused on transcription-independent signaling of E2 may broaden our understanding of E2/ER interaction with pathways involved in cancer initiation and progression. Therefore, elucidating the role(s) of rapid E2/ERα signaling may uncover new prognostic markers, reveal targetable pathways, and allow for individualized treatment of women with uterine cancer.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
CK2 inhibitor blocks E2-induced PTEN phosphorylation and protein stability. a ISH-ERαWT cells were transiently transfected with a GFP-PTEN expression construct or empty vector (EV) followed by starvation for 24 h in serum free media. Cells were pretreated for 45 min with vehicle or CK2 inhibitor, tetrabromocinnamic acid (TBCA), at the concentrations indicated in the figure. Cells were then treated with vehicle or E2 for 50 min. Cells were harvested and analyzed via Western blotting with an antibody specific to phospho-PTEN (S380, T382, and T383) or b total PTEN and quantified via Odyssey CLx software. Graphs represent quantification normalized to GAPDH (n = 1) (PDF 70 kb)
E2 stimulation increases phospho-PTEN and total PTEN levels in MCF7 cells a MCF7 cells were starved for 24 h in serum free media. Starved cells were treated with E2 for 0, 5, 10, 20, or 30 min. Cells were harvested and analyzed via Western blotting with an antibody specific to phospho-PTEN (S380, T382, and T383), total PTEN and GAPDH. Corresponding graph right represents quantification of a phospho-PTEN or b total PTEN normalized to GAPDH (n = 1) (PDF 50 kb)
E2 increases PTEN phosphorylation and protein stability in cells stably expressing PTEN. a ISH-ERαWT, ISH-ERαΔNLS, and ISH-ERαNEG cells were transduced with either pCDH-PTEN or empty pCDH vector followed by selection with puromycin. Whole cell lysates were analyzed by Western blot to verify stable expression of PTEN. ERα expression of each cell line is also shown (ERα WT = 66 kDa and ERαΔNLS = 61 kDa). ISH-ERαWT PTEN+ cells were starved in serum free media for 24 h followed by E2 treatment for 0, 10, 30, or 50 min. ISH-ERαWT PTEN+ cells and ISH-ERαWT empty vector control cells (EV) were harvested and analyzed via Western blotting with an antibody specific to b phospho-PTEN (S380, T382, and T383) or c total PTEN. Corresponding graphs to the right represent quantification of fold change ± SD of b phospho-PTEN or c total PTEN normalized to GAPDH. (n = 9 and n = 6, respectively. **P < 0.01 by ANOVA) (PDF 133 kb)
Acknowledgments
We thank Dr. Jennifer Richer for providing uterine samples and Nicole Spoelstra from the University of Colorado Cancer Center Tissue Biobanking and Processing Core. We would like to thank Dr. Joanne Masterson for training and guidance in using the Nikon Microscope and NIS-Elements Imaging Software. We would like to thank Dr. Louise Glover for assistance in generating pCDH-PTEN plasmids and general advice in molecular technologies. We thank Dr. Eric Campbell for his assistance and thoughtful discussions. We thank Dr. Pierre Chambon (Institute de Chimie Biologique, France) for providing the pSG5-HE241G vector (ERαΔNLS). This work was supported by the National Institutes of Health/National Cancer Institute (R01 CA125427), the University of Colorado Obstetrics and Gynocology department Academic Enrichment Fund, and the National Institutes of Health/National Center for Advancing Translational Sciences Colorado Clinical and Translational Sciences Institute (TL1 TR001081).
Conflict of Interest
The authors declare that they have no conflict of interest.
Contributor Information
Melanie M. Scully, Email: melanie.scully@UCDenver.edu
Leslie K. Palacios-Helgeson, Email: leslie.palacios-helgeson@UCDenver.edu
Lah S. Wah, Email: lah.wah@UCDenver.edu
Twila A. Jackson, Phone: 303-724-3508, Email: twila.jackson@UCDenver.edu
References
- 1.Abd El-Maqsoud NM, El-Gelany S. Differential expression patterns of PTEN in cyclic, hyperplastic and malignant endometrium: its relation with ER, PR and clinicopathological parameters. J Egypt Natl Canc Inst. 2009;21(4):323–331. [PubMed] [Google Scholar]
- 2.Acconcia F, Barnes CJ, Kumar R. Estrogen and tamoxifen induce cytoskeletal remodeling and migration in endometrial cancer cells. Endocrinology. 2006;147(3):1203–1212. doi: 10.1210/en.2005-1293. [DOI] [PubMed] [Google Scholar]
- 3.Alimonti A, Carracedo A, Clohessy JG, Trotman LC, Nardella C, Egia A, Salmena L, et al. Subtle variations in PTEN dose determine cancer susceptibility. Nat Genet. 2010;42(5):454–458. doi: 10.1038/ng.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.American Cancer Society (2014) What are the key statistics about endometrial cancer? http://www.cancer.org/cancer/endometrialcancer/detailedguide/endometrial-uterine-cancer-key-statistics. Accessed 10 March 2014
- 5.Carmeci C, Thompson DA, Ring HZ, Francke U, Weigel RJ. Identification of a gene (GPR30) with homology to the G-protein-coupled receptor superfamily associated with estrogen receptor expression in breast cancer. Genomics. 1997;45(3):607–617. doi: 10.1006/geno.1997.4972. [DOI] [PubMed] [Google Scholar]
- 6.Castoria G, Migliaccio A, Bilancio A, Di Domenico M, de Falco A, Lombardi M, Fiorentino R, Varricchio L, Barone MV, Auricchio F. PI3-kinase in concert with Src promotes the S-phase entry of oestradiol-stimulated MCF-7 cells. EMBO J. 2001;20(21):6050–6059. doi: 10.1093/emboj/20.21.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chakravarty D, Nair SS, Santhamma B, Nair BC, Wang L, Bandyopadhyay A, Agyin JK, et al. Extranuclear functions of ER impact invasive migration and metastasis by breast cancer cells. Cancer Res. 2010;70(10):4092–4101. doi: 10.1158/0008-5472.CAN-09-3834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chambliss KL, Wu Q, Oltmann S, Konaniah ES, Umetani M, Korach KS, Thomas GD, et al. Non-nuclear estrogen receptor alpha signaling promotes cardiovascular protection but not uterine or breast cancer growth in mice. J Clin Invest. 2010;120(7):2319–2330. doi: 10.1172/JCI38291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cormack BP, Valdivia RH, Falkow S. FACS-optimized mutants of the green fluorescent protein (GFP) Gene. 1996;173(1 Spec No):33–38. doi: 10.1016/0378-1119(95)00685-0. [DOI] [PubMed] [Google Scholar]
- 10.Dey N, Barwick BG, Moreno CS, Ordanic-Kodani M, Chen Z, Oprea-Ilies G, Tang W, et al. Wnt signaling in triple negative breast cancer is associated with metastasis. BMC Cancer. 2013;13(1):537. doi: 10.1186/1471-2407-13-537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Di Cristofano A, Pesce B, Cordon-Cardo C, Pandolfi PP. Pten is essential for embryonic development and tumour suppression. Nat Genet. 1998;19(4):348–355. doi: 10.1038/1235. [DOI] [PubMed] [Google Scholar]
- 12.Emons G, Fleckenstein G, Hinney B, Huschmand A, Heyl W. Hormonal interactions in endometrial cancer. Endocr Relat Cancer. 2000;7(4):227–242. doi: 10.1677/erc.0.0070227. [DOI] [PubMed] [Google Scholar]
- 13.Filardo EJ, Quinn JA, Frackelton AR, Jr, Bland KI. Estrogen action via the G protein-coupled receptor, GPR30: stimulation of adenylyl cyclase and cAMP-mediated attenuation of the epidermal growth factor receptor-to-MAPK signaling axis. Mol Endocrinol. 2002;16(1):70–84. doi: 10.1210/mend.16.1.0758. [DOI] [PubMed] [Google Scholar]
- 14.Ganapathy V, Banach-Petrosky W, Xie W, Kareddula A, Nienhuis H, Miles G, Reiss M. Luminal breast cancer metastasis is dependent on estrogen signaling. Clin Exp Metastasis. 2012;29(5):493–509. doi: 10.1007/s10585-012-9466-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giretti MS, Fu XD, De Rosa G, Sarotto I, Baldacci C, Garibaldi S, Mannella P, et al. Extra-nuclear signalling of estrogen receptor to breast cancer cytoskeletal remodelling, migration and invasion. PLoS One. 2008;3(5):e2238. doi: 10.1371/journal.pone.0002238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hagan CR, Knutson TP, Lange CA. A common docking domain in progesterone receptor-B links DUSP6 and CK2 signaling to proliferative transcriptional programs in breast cancer cells. Nucleic Acids Res. 2013;41(19):8926–8942. doi: 10.1093/nar/gkt706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harvell DM, Richer JK, Allred DC, Sartorius CA, Horwitz KB. Estradiol regulates different genes in human breast tumor xenografts compared with the identical cells in culture. Endocrinology. 2006;147(2):700–713. doi: 10.1210/en.2005-0617. [DOI] [PubMed] [Google Scholar]
- 18.Hecht JL, Mutter GL. Molecular and pathologic aspects of endometrial carcinogenesis. J Clin Oncol. 2006;24(29):4783–4791. doi: 10.1200/JCO.2006.06.7173. [DOI] [PubMed] [Google Scholar]
- 19.Hewitt SC, O’Brien JE, Jameson JL, Kissling GE, Korach KS. Selective disruption of ER{alpha} DNA-binding activity alters uterine responsiveness to estradiol. Mol Endocrinol. 2009;23(12):2111–2116. doi: 10.1210/me.2009-0356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ibarra-Drendall C, Troch MM, Barry WT, Broadwater G, Petricoin EF, 3rd, Wulfkuhle J, Liotta LA, et al. Pilot and feasibility study: prospective proteomic profiling of mammary epithelial cells from high-risk women provides evidence of activation of pro-survival pathways. Breast Cancer Res Treat. 2012;132(2):487–498. doi: 10.1007/s10549-011-1609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ishiwata I, Nozawa S, Okumura H. Effects of 17beta-estradiol and progesterone on growth and morphology of human endometrial carcinoma cells in vitro. Cancer Res. 1977;37(12):4246–4249. [PubMed] [Google Scholar]
- 22.Jakacka M, Ito M, Martinson F, Ishikawa T, Lee EJ, Jameson JL. An estrogen receptor (ER)alpha deoxyribonucleic acid-binding domain knock-in mutation provides evidence for nonclassical ER pathway signaling in vivo. Mol Endocrinol. 2002;16(10):2188–2201. doi: 10.1210/me.2001-0174. [DOI] [PubMed] [Google Scholar]
- 23.Kaaks R, Lukanova A, Kurzer MS. Obesity, endogenous hormones, and endometrial cancer risk: a synthetic review. Cancer Epidemiol Biomarkers Prev. 2002;11(12):1531–1543. [PubMed] [Google Scholar]
- 24.Kanamori Y, Kigawa J, Itamochi H, Shimada M, Takahashi M, Kamazawa S, Sato S, Akeshima R, Terakawa N. Correlation between loss of PTEN expression and Akt phosphorylation in endometrial carcinoma. Clin Cancer Res Off J Am Assoc Cancer Res. 2001;7(4):892–895. [PubMed] [Google Scholar]
- 25.Key TJ, Pike MC. The dose–effect relationship between ‘unopposed’ oestrogens and endometrial mitotic rate: its central role in explaining and predicting endometrial cancer risk. Br J Cancer. 1988;57(2):205–212. doi: 10.1038/bjc.1988.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Korch C, Spillman MA, Jackson TA, Jacobsen BM, Murphy SK, Lessey BA, Jordan VC, Bradford AP. DNA profiling analysis of endometrial and ovarian cell lines reveals misidentification, redundancy and contamination. Gynecol Oncol. 2012;127(1):241–248. doi: 10.1016/j.ygyno.2012.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kwon J, Lee SR, Yang KS, Ahn Y, Kim YJ, Stadtman ER, Rhee SG. Reversible oxidation and inactivation of the tumor suppressor PTEN in cells stimulated with peptide growth factors. Proc Natl Acad Sci U S A. 2004;101(47):16419–16424. doi: 10.1073/pnas.0407396101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee JO, Yang H, Georgescu MM, Di Cristofano A, Maehama T, Shi Y, Dixon JE, Pandolfi P, Pavletich NP. Crystal structure of the PTEN tumor suppressor: implications for its phosphoinositide phosphatase activity and membrane association. Cell. 1999;99(3):323–334. doi: 10.1016/S0092-8674(00)81663-3. [DOI] [PubMed] [Google Scholar]
- 29.Liang J, Zubovitz J, Petrocelli T, Kotchetkov R, Connor MK, Han K, Lee JH, et al. PKB/Akt phosphorylates p27, impairs nuclear import of p27 and opposes p27-mediated G1 arrest. Nat Med. 2002;8(10):1153–1160. doi: 10.1038/nm761. [DOI] [PubMed] [Google Scholar]
- 30.Lin HK, Hu YC, Lee DK, Chang C. Regulation of androgen receptor signaling by PTEN (phosphatase and tensin homolog deleted on chromosome 10) tumor suppressor through distinct mechanisms in prostate cancer cells. Mol Endocrinol. 2004;18(10):2409–2423. doi: 10.1210/me.2004-0117. [DOI] [PubMed] [Google Scholar]
- 31.Maccario H, Perera NM, Gray A, Downes CP, Leslie NR. Ubiquitination of PTEN (phosphatase and tensin homolog) inhibits phosphatase activity and is enhanced by membrane targeting and hyperosmotic stress. J Biol Chem. 2010;285(17):12620–12628. doi: 10.1074/jbc.M109.072280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maehama T, Dixon JE. The tumor suppressor, PTEN/MMAC1, dephosphorylates the lipid second messenger, phosphatidylinositol 3,4,5-trisphosphate. J Biol Chem. 1998;273(22):13375–13378. doi: 10.1074/jbc.273.22.13375. [DOI] [PubMed] [Google Scholar]
- 33.Mannella P, Brinton RD. Estrogen receptor protein interaction with phosphatidylinositol 3-kinase leads to activation of phosphorylated Akt and extracellular signal-regulated kinase 1/2 in the same population of cortical neurons: a unified mechanism of estrogen action. J Neurosci Off J Soc Neurosci. 2006;26(37):9439–9447. doi: 10.1523/JNEUROSCI.1443-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McPherson CP, Sellers TA, Potter JD, Bostick RM, Folsom AR. Reproductive factors and risk of endometrial cancer. The Iowa Women’s Health Study. Am J Epidemiol. 1996;143(12):1195–1202. doi: 10.1093/oxfordjournals.aje.a008707. [DOI] [PubMed] [Google Scholar]
- 35.Merritt MA, Cramer DW. Molecular pathogenesis of endometrial and ovarian cancer. Cancer Biomark. 2010;9(1–6):287–305. doi: 10.3233/CBM-2011-0167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Migliaccio A, Di Domenico M, Castoria G, de Falco A, Bontempo P, Nola E, Auricchio F. Tyrosine kinase/p21ras/MAP-kinase pathway activation by estradiol-receptor complex in MCF-7 cells. EMBO J. 1996;15(6):1292–1300. [PMC free article] [PubMed] [Google Scholar]
- 37.Mutter GL, Lin MC, Fitzgerald JT, Kum JB, Eng C. Changes in endometrial PTEN expression throughout the human menstrual cycle. J Clin Endocrinol Metab. 2000;85(6):2334–2338. doi: 10.1210/jcem.85.6.6652. [DOI] [PubMed] [Google Scholar]
- 38.Odriozola L, Singh G, Hoang T, Chan AM. Regulation of PTEN activity by its carboxyl-terminal autoinhibitory domain. J Biol Chem. 2007;282(32):23306–23315. doi: 10.1074/jbc.M611240200. [DOI] [PubMed] [Google Scholar]
- 39.Okumura K, Mendoza M, Bachoo RM, DePinho RA, Cavenee WK, Furnari FB. PCAF modulates PTEN activity. J Biol Chem. 2006;281(36):26562–26568. doi: 10.1074/jbc.M605391200. [DOI] [PubMed] [Google Scholar]
- 40.Pallares J, Martinez-Guitarte JL, Dolcet X, Llobet D, Rue M, Palacios J, Prat J, Matias-Guiu X. Survivin expression in endometrial carcinoma: a tissue microarray study with correlation with PTEN and STAT-3. Int J Gynecol Pathol. 2005;24(3):247–253. doi: 10.1097/01.pgp.0000163849.37129.d4. [DOI] [PubMed] [Google Scholar]
- 41.Pedram A, Razandi M, Kim JK, O’Mahony F, Lee EY, Luderer U, Levin ER. Developmental phenotype of a membrane only estrogen receptor alpha (MOER) mouse. J Biol Chem. 2009;284(6):3488–3495. doi: 10.1074/jbc.M806249200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Podsypanina K, Ellenson LH, Nemes A, Gu J, Tamura M, Yamada KM, Cordon-Cardo C, Catoretti G, Fisher PE, Parsons R. Mutation of PTEN/Mmac1 in mice causes neoplasia in multiple organ systems. Proc Natl Acad Sci U S A. 1999;96(4):1563–1568. doi: 10.1073/pnas.96.4.1563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Razandi M, Pedram A, Levin ER. Estrogen signals to the preservation of endothelial cell form and function. J Biol Chem. 2000;275(49):38540–38546. doi: 10.1074/jbc.M007555200. [DOI] [PubMed] [Google Scholar]
- 44.Sartorius CA, Harvell DM, Shen T, Horwitz KB. Progestins initiate a luminal to myoepithelial switch in estrogen-dependent human breast tumors without altering growth. Cancer Res. 2005;65(21):9779–9788. doi: 10.1158/0008-5472.CAN-05-0505. [DOI] [PubMed] [Google Scholar]
- 45.Sartorius CA, Shen T, Horwitz KB. Progesterone receptors A and B differentially affect the growth of estrogen-dependent human breast tumor xenografts. Breast Cancer Res Treat. 2003;79(3):287–299. doi: 10.1023/A:1024031731269. [DOI] [PubMed] [Google Scholar]
- 46.Sherman ME. Theories of endometrial carcinogenesis: a multidisciplinary approach. Mod Pathol. 2000;13(3):295–308. doi: 10.1038/modpathol.3880051. [DOI] [PubMed] [Google Scholar]
- 47.Shtilbans V, Wu M, Burstein DE. Current overview of the role of Akt in cancer studies via applied immunohistochemistry. Ann Diagn Pathol. 2008;12(2):153–160. doi: 10.1016/j.anndiagpath.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 48.Simoncini T, Hafezi-Moghadam A, Brazil DP, Ley K, Chin WW, Liao JK. Interaction of oestrogen receptor with the regulatory subunit of phosphatidylinositol-3-OH kinase. Nature. 2000;407(6803):538–541. doi: 10.1038/35035131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Slomovitz BM, Coleman RL. The PI3K/AKT/mTOR pathway as a therapeutic target in endometrial cancer. Clin Cancer Res. 2012;18(21):5856–5864. doi: 10.1158/1078-0432.CCR-12-0662. [DOI] [PubMed] [Google Scholar]
- 50.Stambolic V, Suzuki A, de la Pompa JL, Brothers GM, Mirtsos C, Sasaki T, Ruland J, Penninger JM, Siderovski DP, Mak TW. Negative regulation of PKB/Akt-dependent cell survival by the tumor suppressor PTEN. Cell. 1998;95(1):29–39. doi: 10.1016/S0092-8674(00)81780-8. [DOI] [PubMed] [Google Scholar]
- 51.Sun H, Lesche R, Li DM, Liliental J, Zhang H, Gao J, Gavrilova N, Mueller B, Liu X, Wu H. PTEN modulates cell cycle progression and cell survival by regulating phosphatidylinositol 3,4,5,-trisphosphate and Akt/protein kinase B signaling pathway. Proc Natl Acad Sci U S A. 1999;96(11):6199–6204. doi: 10.1073/pnas.96.11.6199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Tamm I, Wang Y, Sausville E, Scudiero DA, Vigna N, Oltersdorf T, Reed JC. IAP-family protein survivin inhibits caspase activity and apoptosis induced by Fas (CD95), Bax, caspases, and anticancer drugs. Cancer Res. 1998;58(23):5315–5320. [PubMed] [Google Scholar]
- 53.Torres J, Pulido R. The tumor suppressor PTEN is phosphorylated by the protein kinase CK2 at its C terminus. Implications for PTEN stability to proteasome-mediated degradation. J Biol Chem. 2001;276(2):993–998. doi: 10.1074/jbc.M009134200. [DOI] [PubMed] [Google Scholar]
- 54.Trotman LC, Niki M, Dotan ZA, Koutcher JA, Di Cristofano A, Xiao A, Khoo AS, et al. PTEN dose dictates cancer progression in the prostate. PLoS Biol. 2003;1(3):E59. doi: 10.1371/journal.pbio.0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.U.S. Cancer statistics working group (2013) United States Cancer Statistics: 1999–2010 incidence and mortality web-based report. Atlanta (GA): Department of Health and Human Services, Centers for Disease Control and Prevention, and National Cancer Institute. http://www.cdc.gov/uscs. Accessed 2013
- 56.Vazquez F, Ramaswamy S, Nakamura N, Sellers WR. Phosphorylation of the PTEN tail regulates protein stability and function. Mol Cell Biol. 2000;20(14):5010–5018. doi: 10.1128/MCB.20.14.5010-5018.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Vazquez F, Sellers WR. The PTEN tumor suppressor protein: an antagonist of phosphoinositide 3-kinase signaling. Biochim Biophys Acta. 2000;1470(1):M21–M35. doi: 10.1016/s0304-419x(99)00032-3. [DOI] [PubMed] [Google Scholar]
- 58.Vilgelm A, Lian Z, Wang H, Beauparlant SL, Klein-Szanto A, Ellenson LH, Di Cristofano A. Akt-mediated phosphorylation and activation of estrogen receptor alpha is required for endometrial neoplastic transformation in Pten+/− mice. Cancer Res. 2006;66(7):3375–3380. doi: 10.1158/0008-5472.CAN-05-4019. [DOI] [PubMed] [Google Scholar]
- 59.Wan X, Yokoyama Y, Shinohara A, Takahashi Y, Tamaya T. PTEN augments staurosporine-induced apoptosis in PTEN-null Ishikawa cells by downregulating PI3K/Akt signaling pathway. Cell Death Differ. 2002;9(4):414–420. doi: 10.1038/sj.cdd.4400982. [DOI] [PubMed] [Google Scholar]
- 60.Watson CS, Jeng YJ, Kochukov MY. Nongenomic actions of estradiol compared with estrone and estriol in pituitary tumor cell signaling and proliferation. FASEB J. 2008;22(9):3328–3336. doi: 10.1096/fj.08-107672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.White BD, Chien AJ, Dawson DW. Dysregulation of Wnt/beta-catenin signaling in gastrointestinal cancers. Gastroenterology. 2012;142(2):219–232. doi: 10.1053/j.gastro.2011.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Williams CC, Basu A, El-Gharbawy A, Carrier LM, Smith CL, Rowan BG. Identification of four novel phosphorylation sites in estrogen receptor alpha: impact on receptor-dependent gene expression and phosphorylation by protein kinase CK2. BMC Biochem. 2009;10:36. doi: 10.1186/1471-2091-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ylikomi T, Bocquel MT, Berry M, Gronemeyer H, Chambon P. Cooperation of proto-signals for nuclear accumulation of estrogen and progesterone receptors. EMBO J. 1992;11(10):3681–3694. doi: 10.1002/j.1460-2075.1992.tb05453.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zha J, Harada H, Yang E, Jockel J, Korsmeyer SJ. Serine phosphorylation of death agonist BAD in response to survival factor results in binding to 14-3-3 not BCL-X(L) Cell. 1996;87(4):619–628. doi: 10.1016/S0092-8674(00)81382-3. [DOI] [PubMed] [Google Scholar]
- 65.Zhang G, Liu X, Farkas AM, Parwani AV, Lathrop KL, Lenzner D, Land SR, Srinivas H. Estrogen receptor beta functions through nongenomic mechanisms in lung cancer cells. Mol Endocrinol. 2009;23(2):146–156. doi: 10.1210/me.2008-0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Zheng S, Huang J, Zhou K, Zhang C, Xiang Q, Tan Z, Wang T, Fu X. 17beta-Estradiol enhances breast cancer cell motility and invasion via extra-nuclear activation of actin-binding protein ezrin. PLoS One. 2011;6(7):e22439. doi: 10.1371/journal.pone.0022439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhong H, Chiles K, Feldser D, Laughner E, Hanrahan C, Georgescu MM, Simons JW, Semenza GL. Modulation of hypoxia-inducible factor 1alpha expression by the epidermal growth factor/phosphatidylinositol 3-kinase/PTEN/AKT/FRAP pathway in human prostate cancer cells: implications for tumor angiogenesis and therapeutics. Cancer Res. 2000;60(6):1541–1545. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CK2 inhibitor blocks E2-induced PTEN phosphorylation and protein stability. a ISH-ERαWT cells were transiently transfected with a GFP-PTEN expression construct or empty vector (EV) followed by starvation for 24 h in serum free media. Cells were pretreated for 45 min with vehicle or CK2 inhibitor, tetrabromocinnamic acid (TBCA), at the concentrations indicated in the figure. Cells were then treated with vehicle or E2 for 50 min. Cells were harvested and analyzed via Western blotting with an antibody specific to phospho-PTEN (S380, T382, and T383) or b total PTEN and quantified via Odyssey CLx software. Graphs represent quantification normalized to GAPDH (n = 1) (PDF 70 kb)
E2 stimulation increases phospho-PTEN and total PTEN levels in MCF7 cells a MCF7 cells were starved for 24 h in serum free media. Starved cells were treated with E2 for 0, 5, 10, 20, or 30 min. Cells were harvested and analyzed via Western blotting with an antibody specific to phospho-PTEN (S380, T382, and T383), total PTEN and GAPDH. Corresponding graph right represents quantification of a phospho-PTEN or b total PTEN normalized to GAPDH (n = 1) (PDF 50 kb)
E2 increases PTEN phosphorylation and protein stability in cells stably expressing PTEN. a ISH-ERαWT, ISH-ERαΔNLS, and ISH-ERαNEG cells were transduced with either pCDH-PTEN or empty pCDH vector followed by selection with puromycin. Whole cell lysates were analyzed by Western blot to verify stable expression of PTEN. ERα expression of each cell line is also shown (ERα WT = 66 kDa and ERαΔNLS = 61 kDa). ISH-ERαWT PTEN+ cells were starved in serum free media for 24 h followed by E2 treatment for 0, 10, 30, or 50 min. ISH-ERαWT PTEN+ cells and ISH-ERαWT empty vector control cells (EV) were harvested and analyzed via Western blotting with an antibody specific to b phospho-PTEN (S380, T382, and T383) or c total PTEN. Corresponding graphs to the right represent quantification of fold change ± SD of b phospho-PTEN or c total PTEN normalized to GAPDH. (n = 9 and n = 6, respectively. **P < 0.01 by ANOVA) (PDF 133 kb)