Abstract
Objective
To evaluate visual field abnormalities after an episode of optic neuritis among participants in the Optic Neuritis Treatment Trial.
Methods
Three readers independently evaluated 10 443 visual fields from 454 patients and classified visual field abnormalities into 21 different monocular categories representing 3 general types of visual loss: diffuse, localized, and artifactual. Classification frequency was determined and reader agreement was evaluated. The association of visual field abnormality classifications with mean deviation, pattern standard deviation, visual acuity, and foveal threshold was assessed.
Results
At baseline, diffuse loss accounted for 66.2% of the abnormalities in the affected eyes but only 6.2% of the abnormalities in the fellow eyes. During years 1 through 15, the affected and fellow eyes exhibited predominantly localized loss in the nerve fiber bundle region (partial arcuate, paracentral, and arcuate defects). At year 1, 35.7% of the abnormalities in the affected eyes and 34.4% in the fellow eyes consisted of localized defects. At year 15, 39.5% of abnormalities in the affected eyes and 26.3% in the fellow eyes consisted of localized defects. Foveal threshold was highly correlated with visual acuity and contrast sensitivity in the affected eye at baseline (−0.82 vs 0.79, respectively), 6 months (−0.84 vs 0.81), and 1 year (−0.84 vs 0.79).
Conclusions
Diffuse and central loss were more predominant in the affected eye at baseline, and nerve fiber bundle defects (partial arcuate, paracentral, and arcuate) were the most predominant localized abnormalities in both the affected and fellow eyes during the study.
The final reports from the Optic Neuritis Treatment Trial (ONTT) on visual function and risk of multiple sclerosis were recently published.1–4 The baseline5 and 1-year follow-up6 visual field results for the ONTT were previously published. This article examines visual fields from baseline through the 15-year follow-up in ONTT participants and presents an overview of the longitudinal visual field data. The main objectives were (1) to classify visual field abnormalities using updated methods, (2) to examine foveal threshold (FT) values in the affected eye and correlate those values with visual acuity (VA) and contrast sensitivity for the first year of the study, and (3) to correlate visual field abnormality classifications with visual field mean deviation (MD), mean pattern standard deviation (PSD), mean VA, and mean FT.
METHODS
ABNORMAL VISUAL FIELD CLASSIFICATION
In 1987, Keltner and Johnson began characterizing the types and severity of visual field defects in the ONTT.5–8 We have refined the methods previously reported in the 1993 baseline5 and 1994 1-year follow-up6 articles. For the purpose of identifying visual field abnormalities in patients with optic neuritis, we developed the current methods based on a visual field classification system developed in 1999 for the Ocular Hypertension Treatment Study (OHTS).9–14 These methods have allowed us to more carefully define visual field characteristics and classifications for the ONTT. We have now characterized the entire cohort of visual field abnormalities in the ONTT from baseline through 15 years (10 443 visual fields). Reliable and unreliable visual fields were evaluated in this study. Visual fields were considered unreliable if the false-positives, false-negatives, and fixation loss indices exceeded 33%. Given the nature of optic neuritis, we decided not to exclude visual fields from the classification process based on reliability indices.
The 21 abnormal visual field classification categories developed for the ONTT included patterns of visual field loss divided into 3 broad groups: localized, diffuse, and artifactual. These visual field patterns of loss appear to be characteristic of the visual field loss associated with optic neuritis and patterns associated with testing artifacts. An abnormal field in the ONTT was defined as meeting any of the following criteria: (1) a Glaucoma Hemifield Test result outside normal limits; (2) a corrected PSD or PSD at P < 5%; (3) a single point worse than the 0.5% probability level on the total and/or pattern deviation probability plots; (4) 2 adjacent points (cluster) beyond normal limits (P < 5%) and at least 1 point worse than the P < 1% on the total and/or pattern deviation probability plot (a cluster is defined as ≥2 horizontally or vertically, not diagonally, contiguous abnormal points at P < 5%); or (5) 3 or more clustered points worse than the P < 5% level on the total and/or pattern deviation probability plot. For all classification evaluations (criteria 3–5), the pattern of loss had to be consistent with ocular abnormalities. The predominant visual field pattern of loss was used to determine the abnormality classification defined in the Box. The most frequent types of ONTT visual field classifications are shown in Figure 1. The complete set of ONTT visual field classification examples is shown in eFigures 1–4 (http://www.archophthalmol.com).
Box. Classification of Visual Field Abnormalities.
A visual field is definitely normal if all locations are within normal limits on the total deviation plot.
-
A visual field is definitely abnormal if any of the conditions below are met:
The Glaucoma Hemifield Test visual field index is abnormal (outside the reference range or general reduction of sensitivity); and/or
The corrected pattern standard deviation visual field index is abnormal (P < 5%); and/or
A single point is worse than the 0.5% probability level on the total and/or pattern deviation plot; and/or
Two clustered points are beyond the reference range (P < 5%), and at least 1 point worse than the P < 1% on the total and/or pattern deviation plot (a cluster is defined as ≥2 horizontally or vertically, not diagonally, contiguous abnormal points with P < 5%); and/or
Three or more clustered points worse than P < 5% on the total and/or pattern deviation plot and the pattern of loss is consistent with ocular abnormalities.
The most predominant visual field defect will be used to determine the abnormality classification for the entire visual field.
In general, the pattern of abnormal points on the deviation plot (total or pattern) showing the greater number of abnormal points should be used to determine the appropriate classification for an abnormality. However, the other deviation plot as well as the gray scale should be evaluated to confirm the appropriateness of the classification. Abnormal points that are extraneous to the salient pattern should be ignored.
A normal visual field is designated as NL.
-
An abnormal visual field is given a designation from the list below:
-
Neurologic abnormalities: Chiasmal, retrochiasmal, optic nerve chiasm
Vertical step (VS): Limited visual field loss that respects the vertical meridian and that includes at least 2 abnormal points at or outside 15° along the vertical meridian.
Quadrant (Q): Significant visual field loss throughout an entire quadrant that respects the vertical midline. Essentially all points must have a P < 5% value on the total deviation plot.
Partial hemianopia (PH): A visual field defect that respects the vertical meridian and that is greater than 1 quadrant but less than a complete vertical hemifield.
Hemianopia (H): A visual field defect that respects the vertical meridian and that involves essentially all points in a vertical hemifield.
Three quadrants (3Q): Significant visual field loss throughout 3 quadrants; essentially all points must have a P < 5% value on the total deviation plot.
-
Optic nerve abnormalities
-
Nerve fiber bundle abnormalities
Temporal wedge (TW): A small visual field defect that is temporal to the blind spot.
Enlarged blind spot (EBS): A visual field abnormality in the nerve fiber bundle region that involves at least 2 points and is contiguous with the blind spot.
Nasal step (NS)mild/severe: Limited field loss adjacent to the nasal horizontal meridian with at least 1 abnormal point at or outside 15° on the meridian. Cannot include more than 1 significant point (on either plot) in the nerve fiber bundle region on the temporal side.
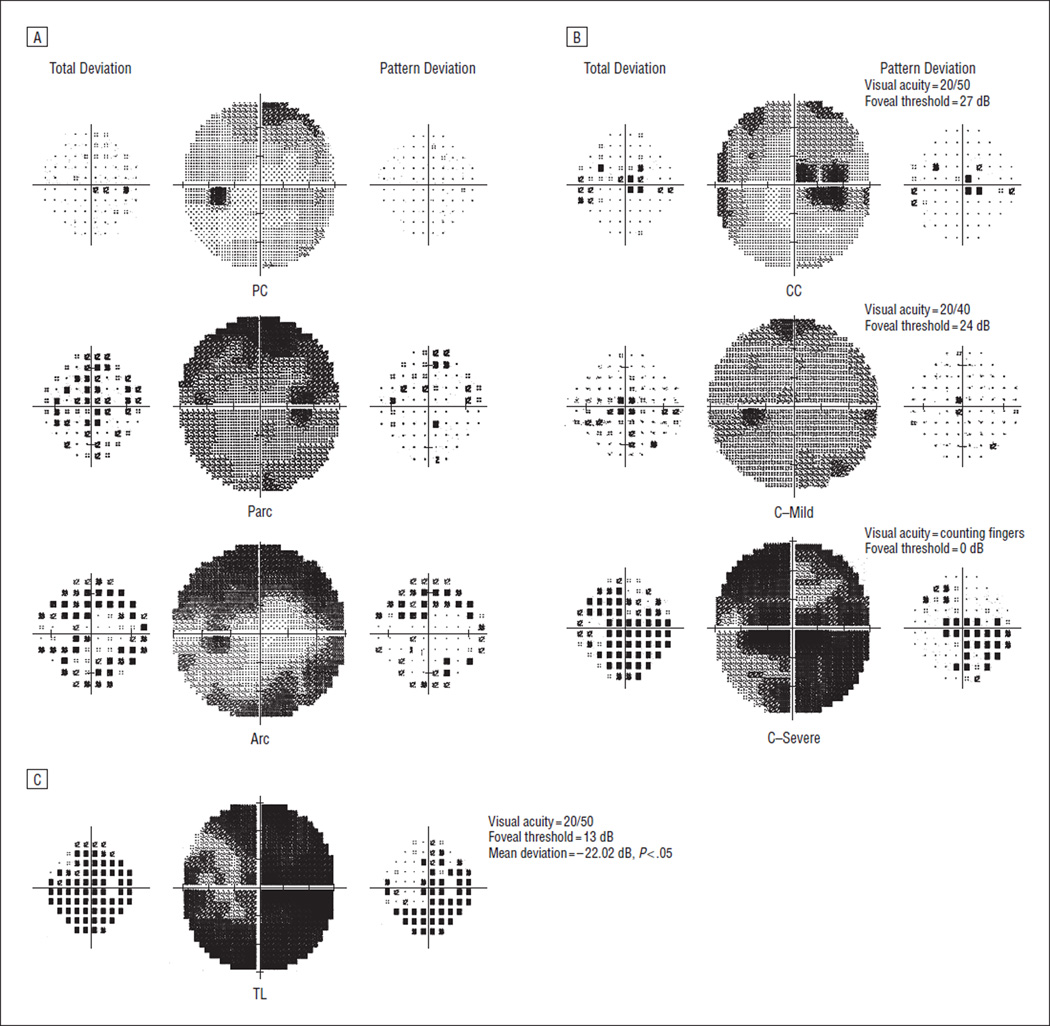
Paracentral (PC): A relatively small visual field abnormality in the nerve fiber bundle region that is generally not contiguous with the blind spot or the nasal meridian. In particular, it does not involve points outside 15° that are adjacent to the nasal meridian (Figure 1).
Partial arcuate (PArc): Visual field loss in the nerve fiber bundle region that extends incompletely from the blind spot to the nasal meridian. The defect is generally contiguous with either the blind spot or the nasal meridian and must include at least 1 abnormal location in the temporal visual field (Figure 1).
Arcuate (Arc): Significant visual field loss in the nerve fiber bundle region, extending across contiguous abnormal points from the blind spot to at least 1 point outside 15° adjacent to the nasal meridian (Figure 1).
Altitudinal (Alt): Severe visual field loss throughout the entire superior or inferior hemifield that respects the horizontal midline, with most points in the hemifield having a P < 5% value on the total deviation plot and the entire horizontal midline demonstrating abnormality.
-
Diffuse abnormalities
Multiple foci (MF): Visual field loss that includes 2 or more clusters of abnormal points (P < 5%) located in different areas of the visual field that do not correspond to a particular abnormality pattern. The loss must be present in both the total and pattern deviation plots.
Widespread (Wsp): Diffuse visual field loss that includes all 4 quadrants. The Glaucoma Hemifield Test may show a general reduction of sensitivity or the MD must have a P level < 5%. The corrected pattern standard deviation must not have a P level < 5%. Most abnormal points on the total deviation plot are not abnormal on the pattern deviation plot.
-
Central abnormalities
Centrocecal (CC): Visual field loss that is in the macular region and contiguous with the blind spot. The foveal threshold must have a P < 5% value. The loss must be symmetrical above and below the midline (Figure 1).
Central (C) mild/severe: Visual field loss that is predominantly in the macular region. The foveal threshold must have a P < 5% value, and the visual acuity must be impaired. Can be associated with a single hemifield and paired with another defect (Figure 1).
-
Severe abnormalities:
Total loss of vision (TL): Severe widespread visual field loss (MD ≤ −20.00 dB) with visual acuity not totally impaired (Figure 1).
-
-
Artifactual abnormalities
Superior depression (SD): Two or more abnormal points in the very superior region.
Inferior depression (ID): Two or more abnormal points in the very inferior region.
Partial peripheral rim (PPR): Generally continuous field loss outside 15°, but not in all quadrants; must have some curvature.
Peripheral rim (PR): Generally continuous visual field loss outside 15° in all 4 quadrants, usually with no visual field loss inside 15° on either deviation plot. There must be visual field loss temporal to the blind spot.
-
Figure 1.
Classifications for optic nerve visual field abnormalities. A, Nerve fiber bundle abnormalities: paracentral (PC), partial arcuate (Parc), and arcuate (Arc). B, Central abnormalities: centrocecal (CC), central (C)—Mild, and C —Severe. C, Severe abnormalities: total loss (TL) of vision. The total deviation plot is on the left and the pattern deviation plot is on the right of each gray scale for all visual fields.
READER AGREEMENT
Three certified readers (J.L.K., C.A.J., and K.E.C.) independently classified 10 443 full-threshold 30–2 visual fields (5840 from affected eyes and 4603 from fellow eyes) from 454 patients with available data over 15 visits (visits 1–8 [within the first year] and single visits for years 1–5, 10, and 15). The abnormal visual fields were graded using the classification system described in the Box. The readers reviewed the visual fields in a random masked fashion unrelated to the order of the patient visits. Thirty-one of the 454 affected eyes (6.8%)were not tested at baseline (visit 1) because VA was determined to be either no light perception or light perception only. Readers assigned classifications to the entire visual field using primarily the total and pattern deviation probability plots showing the greater number of abnormal points. However, the numeric deviation plots, as well as the gray scale, were evaluated to confirm the appropriateness of the classification. Extraneous abnormal points separate from the salient pattern were given lower consideration. The final classification was determined by unanimous agreement among all 3 readers, 2 of the 3 readers, or by consensus when there was no initial agreement. If 2 of 3 readers agreed on a classification, then a final classification was determined for that visual field. If the 3 readers did not agree, then the visual fields were adjudicated by group consensus. After a final classification was made for each visual field, the mean reader agreement and the frequency of classifications for affected and fellow eyes were calculated. Test-retest reader agreement was determined by re-reading a 10% sample from the abnormal visual fields from visits 1 through 8. The sample reflected a distribution of the 21 abnormality classifications. The visual field classification criteria have been described in previous publications.9–14
We obtained reader agreement (at least 2 of the 3 readers) of 94.9% for the 10 443 visual fields. The remaining cases required adjudication. The retest reader assessment resulted in unanimous agreement in 59.8% of cases and agreement among 2 of 3 readers in an additional 34.8% of cases (94.6% total). In 5.4% of cases, there was complete disagreement (eTable 1).
CORRELATION OF ABNORMAL VISUAL FIELDS WITH OTHER MEASURES OF VISUAL FUNCTION
Summary statistics were provided for visual function measurements and visual field classifications. Pearson coefficients were calculated to assess the correlation at different follow-up times between FT values and the following visual measurements: VA (logMAR [logarithm of the minimum angle of resolution] values), contrast sensitivity (log units), and MD of visual field (decibels [dB]). Statistical analyses were conducted using SAS statistical software, version 9.1 (SAS Institute Inc, Cary, North Carolina).
RESULTS
ABNORMAL VISUAL FIELD CLASSIFICATION
At baseline, 100.0% of the visual fields from the affected eyes and 74.7% of the visual fields from the fellow eyes were abnormal. After year 1, the frequencies of abnormal and normal visual fields for the affected eye were evenly distributed at approximately 50.0% each, whereas the abnormal visual field frequency in the fellow eye ranged between 34.3% and 39.7% (eTable 2).
At baseline, 66.2% of the abnormalities in the affected eyes consisted of diffuse loss, which includes total loss, central, centrocecal, and widespread loss; 33.6% of abnormalities were localized loss (Table 1). Visual field abnormality in the affected eye showed a relatively stable decrease in diffuse loss from 66.2% at baseline to approximately 8% to 10% for years 1 through 15. Localized loss remained stable at approximately 39% for years 1, 5, 10, and 15 with paracentral, partial arcuate, and arcuate visual field defects as the most predominant patterns of visual field loss.
Table 1.
Frequency Distribution of Visual Field Classifications in the Affected Eyea
| No. (%) of Visual Fields |
|||||
|---|---|---|---|---|---|
| Year |
|||||
| Visual Field Classification |
Baseline (n=423)b |
1 (n=420) |
5 (n=388) |
10 (n=262) |
15 (n=233) |
| Normal | 0 | 219 (52.1) | 191 (49.2) | 133 (50.8) | 115 (49.4) |
| Diffuse | 280 (66.2) | 44 (10.5) | 38 (9.8) | 26 (9.9) | 20 (8.6) |
| Total loss of vision | 156 (36.9) | 15 (3.6) | 11 (2.8) | 9 (3.4) | 6 (2.6) |
| Central | 113 (26.7) | 7 (1.7) | 6 (1.5) | 6 (2.3) | 5 (2.1) |
| Centrocecal | 9 (2.1) | 5 (1.2) | 2 (0.5) | 2 (0.8) | 2 (0.9) |
| Widespread | 2 (0.5) | 17 (4.0) | 19 (4.9) | 9 (3.4) | 7 (3.0) |
| Localized | 142 (33.6) | 150 (35.7) | 155 (39.9) | 101 (38.5) | 92 (39.5) |
| Arcuate | 66 (15.6) | 16 (3.8) | 24 (6.2) | 15 (5.7) | 13 (5.6) |
| Altitudinal | 34 (8.0) | 3 (0.7) | 5 (1.3) | 1 (0.4) | 0 |
| Partial arcuate | 21 (5.0) | 49 (11.7) | 42 (10.8) | 29 (11.1) | 22 (9.4) |
| Enlarged blind spot | 5 (1.2) | 6 (1.4) | 4 (1.0) | 8 (3.1) | 1 (0.4) |
| Vertical step | 3 (0.7) | 9 (2.1) | 9 (2.3) | 3 (1.1) | 3 (1.3) |
| Hemianopia | 3 (0.7) | 1 (0.2) | 3 (0.8) | 0 | 0 |
| Three quadrants | 3 (0.7) | 1 (0.2) | 0 | 0 | 0 |
| Paracentral | 2 (0.5) | 38 (9.0) | 44 (11.3) | 29 (11.1) | 44 (18.9) |
| Multiple foci | 2 (0.5) | 15 (3.6) | 8 (2.1) | 7 (2.7) | 4 (1.7) |
| Partial hemianopia | 2 (0.5) | 3 (0.7) | 0 | 0 | 1 (0.4) |
| Nasal step | 1 (0.2) | 4 (1.0) | 8 (2.1) | 5 (1.9) | 1 (0.4) |
| Temporal wedge | 0 | 2 (0.5) | 3 (0.8) | 1 (0.4) | 2 (0.9) |
| Quadrant | 0 | 3 (0.7) | 5 (1.3) | 3 (1.1) | 1 (0.4) |
| Double arcuate | 0 | 0 | 0 | 0 | 0 |
| Artifactual | 1 (0.2) | 7 (1.7) | 4 (1.0) | 2 (0.8) | 6 (2.6) |
| Peripheral rim | 1 (0.2) | 1 (0.2) | 0 | 0 | 0 |
| Partial peripheral rim | 0 | 5 (1.2) | 1 (0.3) | 2 (0.8) | 5 (2.1) |
| Superior depression | 0 | 1 (0.2) | 3 (0.8) | 0 | 1 (0.4) |
| Inferior depression | 0 | 0 | 0 | 0 | 0 |
Four visual fields were omitted owing to low patient reliability.
Thirty-one of the 454 affected eyes (6.8%) were not tested at baseline (visit 1) because visual acuity was determined to be either no light perception or light perception only.
In contrast, 74.7% of the visual fields in the fellow eye at baseline were classified as being abnormal. A total of 6.2% of the abnormal visual fields were classified as having diffuse loss, whereas 65.6% were classified as having localized loss (Table 2). At year 1, localized loss decreased to 34.4% and remained stable through year 15 with paracentral, partial arcuate, and arcuate visual field defects as the most predominant pattern of visual field loss.
Table 2.
Frequency Distribution of Visual Field Classifications in the Fellow Eyea
| No. (%) of Visual Fields |
|||||
|---|---|---|---|---|---|
| Year |
|||||
| Visual Field Classification |
Baseline (n=454) |
1 (n=418) |
5 (n=390) |
10 (n=264) |
15 (n=236) |
| Normal | 115 (25.3) | 252 (60.3) | 238 (61.0) | 174 (65.9) | 152 (64.4) |
| Diffuse | 28 (6.2) | 9 (2.2) | 18 (4.6) | 11 (4.2) | 12 (5.1) |
| Widespread | 22 (4.8) | 8 (1.9) | 10 (2.6) | 7 (2.7) | 7 (3.0) |
| Central | 4 (0.9) | 1 (0.2) | 3 (0.8) | 0 | 2 (0.8) |
| Centrocecal | 1 (0.2) | 0 | 1 (0.3) | 0 | 0 |
| Total loss of vision | 1 (0.2) | 0 | 4 (1.0) | 4 (1.5) | 3 (1.3) |
| Localized | 298 (65.6) | 144 (34.4) | 124 (31.8) | 77 (29.2) | 62 (26.3) |
| Partial arcuate | 116 (25.6) | 27 (6.5) | 37 (9.5) | 19 (7.2) | 18 (7.6) |
| Paracentral | 81 (17.8) | 52 (12.4) | 43 (11.0) | 28 (10.6) | 26 (11.0) |
| Arcuate | 42 (9.3) | 16 (3.8) | 14 (3.6) | 10 (3.8) | 8 (3.4) |
| Multiple foci | 28 (6.2) | 19 (4.5) | 6 (1.5) | 3 (1.1) | 2 (0.8) |
| Nasal step | 19 (4.2) | 8 (1.9) | 8 (2.1) | 6 (2.3) | 5 (2.1) |
| Vertical step | 5 (1.1) | 9 (2.2) | 7 (1.8) | 3 (1.1) | 1 (0.4) |
| Temporal wedge | 3 (0.7) | 3 (0.7) | 2 (0.5) | 1 (0.4) | 0 |
| Quadrant | 2 (0.4) | 1 (0.2) | 1 (0.3) | 1 (0.4) | 1 (0.4) |
| Altitudinal | 1 (0.2) | 0 | 2 (0.5) | 0 | 0 |
| Enlarged blind spot | 1 (0.2) | 6 (1.4) | 3 (0.8) | 3 (1.1) | 1 (0.4) |
| Partial hemianopia | 0 | 3 (0.7) | 0 | 0 | 0 |
| Hemianopia | 0 | 0 | 1 (0.3) | 3 (1.1) | 0 |
| Three quadrants | 0 | 0 | 0 | 0 | 0 |
| Double arcuate | 0 | 0 | 0 | 0 | 0 |
| Artifactual | 13 (2.9) | 13 (3.1) | 10 (2.6) | 2 (0.8) | 10 (4.2) |
| Partial peripheral rim | 6 (1.3) | 10 (2.4) | 5 (1.3) | 1 (0.4) | 7 (3.0) |
| Peripheral rim | 4 (0.9) | 2 (0.5) | 0 | 0 | 1 (0.4) |
| Inferior depression | 2 (0.4) | 1 (0.2) | 3 (0.8) | 1 (0.4) | 1 (0.4) |
| Superior depression | 1 (0.2) | 0 | 2 (0.5) | 0 | 1 (0.4) |
Three visual fields were omitted owing to low patient reliability.
CORRELATION OF ABNORMAL VISUAL FIELDS WITH OTHER MEASURES OF VISUAL FUNCTION
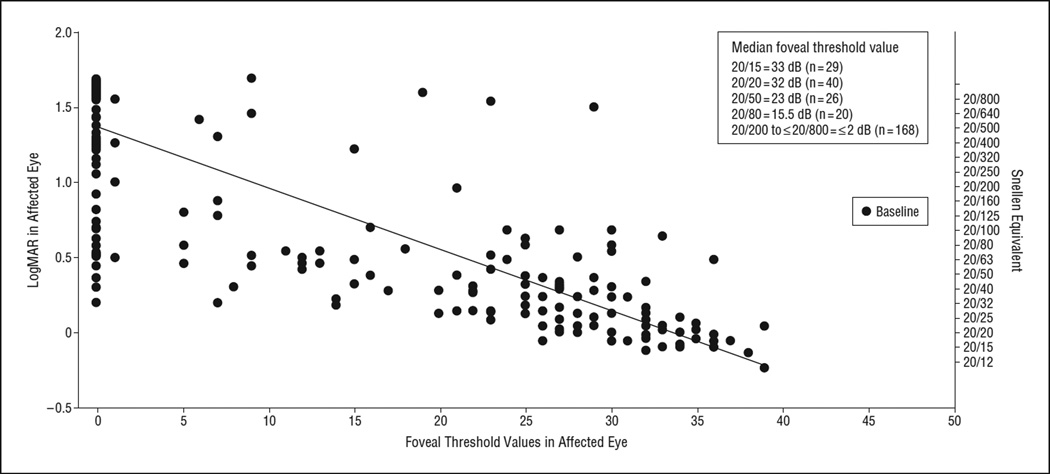
Foveal threshold was highly correlated with Snellen and logMAR VA and contrast sensitivity in the affected eye during the first year of the study. At baseline, FT was correlated with VA (−0.82) and contrast sensitivity (0.79) (Figure 2). At 6 months, FT was correlated with VA (−0.84) and contrast sensitivity (0.81). At year 1, FT was correlated with VA (−0.84) and contrast sensitivity (0.79). For visits 1 through 8 and years 1 through 5, 10, and 15, we also compared the percentage of abnormal visual fields in the affected and fellow eyes with mean visual field MD, FT, VA, and PSD (years 10 and 15 only). The MD for visual field classifications with large numbers was fairly similar in the affected and fellow eyes. (eTables 3 and 4 and eFigures 5 and 6 present frequency of visual field abnormalities and association of visual field classifications with mean MD, mean PSD, mean logMAR VA, and mean FT).
Figure 2.
Foveal threshold vs Snellen and logMAR (logarithm of the minimum angle of resolution) visual acuity and contrast sensitivity in the affected eye at baseline. Pearson correlation for foveal threshold and logMar values, r = −0.82; and for foveal threshold and contrast sensitivity, r=0.79.
COMMENT
The University of California, Davis, Visual Field Reading Center (UCDVFRC) has monitored the ONTT visual field parameters during the past 15 years, and, as a result, now has a unique cohort of 454 patients with 10 443 visual fields. The classification system has evolved during the past 15 years based on the UCDVFRC’s previous experience with the OHTS.9–14 We have refined the methods previously reported in our ONTT 1993 baseline5 and 1994 one-year follow-up6 studies. The evolution of our Visual Field Classification System involved developing specific parameters and definitions of the OHTS visual field patterns of loss.11 These definitions were then adapted for the visual field patterns of loss in the ONTT. In the OHTS, we classified the superior and inferior hemifields of the abnormal visual fields because glaucomatous visual fields tend to exhibit more nerve fiber bundle types of visual field defects (arcuate loss).However, in the ONTT, we classified the entire visual field because visual fields in patients with optic neuritis exhibit central and nerve fiber bundle defects (arcuate loss).
We have also tried to establish the parameters for abnormal visual field classifications with MD and FT values because it may be useful in future clinical trials or in other studies when comparing classification methods. In addition, this classification system could possibly serve as a basis for an automated algorithm to classify abnormal visual fields in patients with optic neuritis or other optic neuropathies.
Classifying the ONTT visual fields for 15 years has allowed us to provide mean VA and MD parameters (a comparative guide) for each of the 21 classifications. There are some differences between the affected and fellow eyes; however, the parameters appear to be similar in the visual fields with the largest number of abnormal classifications. Therefore, physicians can use these tables as rough guides to determine whether the VA and MD values are in the appropriate ranges for a given type of visual field abnormality classification (Figure 2, eFigures 5 and 6, and eTables 3 and 4).
This study also yielded important clinical information. Results from all visual field examinations performed on the affected eye at baseline were abnormal, per the inclusion criteria. However, what has not been well appreciated is the fact that results of 75% of the visual field examinations in the fellow eyes at baseline were also abnormal, and close to 40% were abnormal at year 15. Therefore, these findings appear to show that optic neuritis is not typically a unilateral disease. Reasonable evidence suggests there is bilateral involvement among many patients early in the disease course, when the fellow eye frequently remains involved. We know that, during the study, there were recurrent attacks of optic neuritis in both eyes of the current cohort of patients. However, we do not have adequate information about the frequency of such attacks. Because abnormalities in the fellow eye were present at baseline, these outcomes are not explained by recurrent attacks of optic neuritis.
The classification type of a visual field defect is another important piece of clinical information. Most results of visual field examinations in the affected eye at baseline consisted of central visual field loss. We have found that diffuse loss, representing a large central-type scotoma for the 30–2 test pattern, which includes total loss, central, centrocecal, and widespread loss, represented 66.2% of the visual field abnormalities in the affected eye at baseline, whereas only 6.2% of the abnormalities in the fellow eye at baseline consisted of diffuse and central loss. However, throughout the first year of the study, central visual field loss in the affected eye changed to amore localized loss in the form of nerve fiber bundle defects (ie, partial arcuate, paracentral, and arcuate defects).Most results from the visual field examinations in the fellow eyes at baseline exhibited localized visual field loss, and the defects remained localized during the next 15 years. At year 1, 35.7% of the abnormalities in the affected eyes and 34.4% in the fellow eyes consisted of localized defects. At year 15, 39.5% of abnormalities in the affected eyes and 26.3% in the fellow eyes consisted of localized defects. In addition, these defects were predominantly in the nerve fiber bundle region (partial arcuate, paracentral, and arcuate loss). Thus, over time, the affected and fellow eyes show similar patterns of loss in the nerve fiber bundle, with the affected eye being more severely involved.
Comparison of the 2 methods for the ONTT Visual Field Classification System revealed that, in the 1993 baseline study,5 visual field abnormalities in the affected eyes consisted of 56.5% diffuse loss (combined with central and centrocecal loss) vs 66.2% in the present study. In the fellow eye, diffuse loss (combined with central and centrocecal loss) accounted for 19.7% of abnormalities compared with 6.2% in the present study. Although these numbers are similar, the difference can likely be explained by our more rigorous definitions of the ONTT Visual Field Classification System and improved reader classification methods.
In recent studies published by Nevalainen et al15 and Fang et al,16 a similar visual field pattern was demonstrated. Central scotomas and nerve fiber bundle defects were reported as the most common, with a slight “condensation” of visual loss between the center and the blind spot of the visual field. The higher proportion of central scotomas was owing to higher spatial resolution of their testing strategy. The present study demonstrates similar findings.
Patients with optic neuropathies frequently have VA and contrast sensitivity loss. We have attempted to evaluate patients with optic neuritis by correlating VA with FT and contrast sensitivity measurements. As shown in Figure 2, the FT at baseline appears to correlate well with VA and contrast sensitivity. This is a useful piece of clinical information because, occasionally, there are patients with exceptionally good FT measurements but very reduced vision, which suggests that there may be other factors involved rather than an optic neuropathy causing central visual loss. We have found the FT measurement to be a very valuable clinical tool.
In this report, we correlated types of visual field abnormalities with VA and MD. As recently reported by Kupersmith et al,17 moderate to severe loss in the threshold perimetry, along with VA and contrast testing at 1 month, can help to predict abnormal visual function at 6 months. However, no single parameter is a good predictor.1 We did not examine binocular visual field loss or chiasmal or retrochiasmal defects, which had been adequately addressed in the 1-year follow-up report.6
One potential reason for the increase in fellow-eye abnormalities compared with previous reports is the change in definition of abnormal results on visual field examinations. As can be seen in Table 3, there were a greater percentage of abnormal results on visual field examinations in the affected and fellow eyes at year 15 than in the most recent ONTT report.1 Different MD criteria were used for visual field abnormalities in this study. The standard measure used was an MD of 2 SDs beyond the reference value (≤3.00 dB). However, in our present report, we used a more generous criterion for abnormality to reflect axonal loss as evidenced by recent publications using optical coherence tomography to demonstrate optic nerve damage following acute optic neuritis.18–23 Several investigators have discovered axonal loss in the nerve fiber bundle in patients with multiple sclerosis.24–28 Further correlation with optical coherence tomography will help to define the structure-function relationship of visual field loss implications. From these studies it has become apparent that a patient can have loss of nerve fiber bundles in the optic nerve with a normal or nearly normal visual field after an attack of optic neuritis or multiple sclerosis. The reason for normal visual fields when there is obvious nerve fiber layer damage appears to be redundancy in the optic nerve visual system.
Table 3.
Abnormal VFs vs Abnormal MD at 15 Yearsa
| Eye | Abnormal VF Using Current Methods |
MD <3.00 dB Using Current Methods |
MD <3.00 dB Using ONTT Criteria Only |
|---|---|---|---|
| AE | 51 | 28 | 27 |
| FE | 36 | 19 | 19 |
Abbreviations: AE, affected eye; FE, fellow eye; MD, mean deviation; ONTT, Optic Neuritis Treatment Trial; VF, visual field.
Data are given as the percentage of eyes unless otherwise indicated.
In summary, at baseline, 100% of the visual fields from the affected eyes and 74.7% from the fellow eyes were classified as being abnormal. At baseline and early in the study, the affected eyes mainly exhibited central diffuse loss. Eventually, localized nerve fiber bundle loss (paracentral, partial arcuate, and arcuate defects) predominated. In the fellow eyes, the same pattern of localized nerve fiber bundle loss was seen at baseline and throughout the 15 years of follow-up. The classification parameters defined in this article, including the correlation of VA with FT and contrast sensitivity, may help physicians evaluate the characteristics of optic neuritis and other optic neuropathies in the future.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by cooperative agreement EY09435 from the National Eye Institute, National Institutes of Health and Research to Prevent Blindness.
Footnotes
Optic Neuritis Study Group: Available at http://aaojournal.org (see “Appendix”).
Financial Disclosure: None reported.
Online-Only Material: The eTables and eFigures are available at http://www.archophthalmol.com.
REFERENCES
- 1.Optic Neuritis Study Group. Visual function 15 years after optic neuritis: a final follow-up report from the Optic Neuritis Treatment Trial [published online November 5, 2007] Ophthalmology. 2008;115(6):1079.e5–1082.e5. doi: 10.1016/j.ophtha.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Optic Neuritis Study Group. Multiple sclerosis risk after optic neuritis: final Optic Neuritis Treatment Trial follow-up. Arch Neurol. 2008;65(6):727–732. doi: 10.1001/archneur.65.6.727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beck RW, Gal RL. Treatment of acute optic neuritis: a summary of findings from the Optic Neuritis Treatment Trial. Arch Ophthalmol. 2008;126(7):994–995. doi: 10.1001/archopht.126.7.994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Volpe NJ. The Optic Neuritis Treatment Trial: a definitive answer and profound impact with unexpected results. Arch Ophthalmol. 2008;126(7):996–999. doi: 10.1001/archopht.126.7.996. [DOI] [PubMed] [Google Scholar]
- 5.Keltner JL, Johnson CA, Spurr JO, Beck RW Optic Neuritis Study Group. Baseline visual field profile of optic neuritis: the experience of the optic neuritis treatment trial. Arch Ophthalmol. 1993;111(2):231–234. doi: 10.1001/archopht.1993.01090020085029. [DOI] [PubMed] [Google Scholar]
- 6.Keltner JL, Johnson CA, Spurr JO, Beck RW Optic Neuritis Study Group. Visual field profile of optic neuritis: 1-year follow-up in the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1994;112(7):946–953. doi: 10.1001/archopht.1994.01090190094027. [DOI] [PubMed] [Google Scholar]
- 7.Keltner JL, Johnson CA, Beck RW, Cleary PA, Spurr JO Optic Neuritis Study Group. Quality control functions of the Visual Field Reading Center (VFRC) for the Optic Neuritis Treatment Trial (ONTT) Control Clin Trials. 1993;14(2):143–159. doi: 10.1016/0197-2456(93)90016-7. [DOI] [PubMed] [Google Scholar]
- 8.Keltner JL, Johnson CA, Spurr JO, Beck RW Optic Neuritis Study Group. Comparison of central and peripheral visual field properties in the Optic Neuritis Treatment Trial. Am J Ophthalmol. 1999;128(5):543–553. doi: 10.1016/s0002-9394(99)00304-9. [DOI] [PubMed] [Google Scholar]
- 9.Keltner JL, Johnson CA, Quigg JM, Cello KE, Kass MA, Gordon MO Ocular Hypertension Treatment Study Group. Confirmation of visual field abnormalities in the Ocular Hypertension Treatment Study. Arch Ophthalmol. 2000;118(9):1187–1194. doi: 10.1001/archopht.118.9.1187. [DOI] [PubMed] [Google Scholar]
- 10.Johnson CA, Keltner JL, Cello KE, et al Ocular Hypertension Study Group. Baseline visual field characteristics in the Ocular Hypertension Treatment Study. Ophthalmology. 2002;109(3):432–437. doi: 10.1016/s0161-6420(01)00948-4. [DOI] [PubMed] [Google Scholar]
- 11.Keltner JL, Johnson CA, Cello KE, et al Ocular Hypertension Treatment Study Group. Classification of visual field abnormalities in the Ocular Hypertension Treatment Study. Arch Ophthalmol. 2003;121(5):643–650. doi: 10.1001/archopht.121.5.643. [DOI] [PubMed] [Google Scholar]
- 12.Keltner JL, Johnson CA, Levine RA, et al Ocular Hypertension Treatment Study Group. Normal visual field test results following glaucomatous visual field end points in the Ocular Hypertension Treatment Study. Arch Ophthalmol. 2005;123(9):1201–1206. doi: 10.1001/archopht.123.9.1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Keltner JL, Johnson CA, Anderson DR, et al Ocular Hypertension Treatment Study Group. The association between glaucomatous visual fields and optic nerve head features in the Ocular Hypertension Treatment Study (OHTS) Ophthalmology. 2006;113(9):1603–1612. doi: 10.1016/j.ophtha.2006.05.061. [DOI] [PubMed] [Google Scholar]
- 14.Keltner JL, Johnson CA, Cello KE, et al Ocular Hypertension Treatment Study Group. Visual field quality control in the Ocular Hypertension Treatment Study (OHTS) J Glaucoma. 2007;16(8):665–669. doi: 10.1097/IJG.0b013e318057526d. [DOI] [PubMed] [Google Scholar]
- 15.Nevalainen J, Krapp E, Paetzold J, et al. Visual field defects in acute optic neuritis: distribution of different types of defect pattern, assessed with thresholdrelated supraliminal perimetry, ensuring high spatial resolution [published online February 1, 2008] Graefes Arch Clin Exp Ophthalmol. 2008;246(4):599–607. doi: 10.1007/s00417-007-0722-2. [DOI] [PubMed] [Google Scholar]
- 16.Fang JP, Lin RH, Donahue SP. Recovery of visual field function in the Optic Neuritis Treatment Trial. Am J Ophthalmol. 1999;128(5):566–572. doi: 10.1016/s0002-9394(99)00297-4. [DOI] [PubMed] [Google Scholar]
- 17.Kupersmith MJ, Gal RL, Beck RW, Xing D, Miller N Optic Neuritis Study Group. Visual function at baseline and 1 month in acute optic neuritis. Neurology. 2007;69(6):508–514. doi: 10.1212/01.wnl.0000267272.60714.42. [DOI] [PubMed] [Google Scholar]
- 18.Gundogan FC, Demirkaya S, Sobaci G. Is optical coherence tomography really a new biomarker candidate in multiple sclerosis? a structural and functional evaluation. Invest Ophthalmol Vis Sci. 2007;48(12):5773–5781. doi: 10.1167/iovs.07-0834. [DOI] [PubMed] [Google Scholar]
- 19.Cheng H, Laron M, Schiffman J, Tang R, Frishman L. The relationship between visual field and retinal nerve fiber layer measurements in patients with multiple sclerosis. Invest Ophthalmol Vis Sci. 2007;48(12):5798–5805. doi: 10.1167/iovs.07-0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cettomai D, Pulicken M, Gordon-Lipkin E, et al. Reproducibility of optical coherence tomography in multiple sclerosis. Arch Ophthalmol. 2008;65(9):1218–1222. doi: 10.1001/archneur.65.9.1218. [DOI] [PubMed] [Google Scholar]
- 21.Heijl A, Bengtsson B, Chauhan BC, et al. A comparison of visual field progression criteria of 3major glaucoma trials in EarlyManifest Glaucoma Trial patients. Ophthalmology. 2008;115(9):1557–1565. doi: 10.1016/j.ophtha.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 22.Siger M, Dziegielewski K, Jasek L, et al. Optical coherence tomography in multiple sclerosis: thickness of the retinal nerve fiber layer as a potential measure of axonal loss and brain atrophy. J Neurol. 2008;255(10):1555–1560. doi: 10.1007/s00415-008-0985-5. [DOI] [PubMed] [Google Scholar]
- 23.Watson GM, Keltner JL, Nguyen TG, et al. Comparison of optic nerve and macular thickness among commercially available Fourier-domain and time-domain optical coherence tomography instruments in patients withmultiple sclerosis and/or optic neuritis [e-abstract 1530] Invest Ophthalmol Vis Sci. 2009;50 [Google Scholar]
- 24.Trip SA, Schlottmann PG, Jones SJ, et al. Retinal nerve fiber layer axonal loss and visual dysfunction in optic neuritis. Ann Neurol. 2005;58(3):383–391. doi: 10.1002/ana.20575. [DOI] [PubMed] [Google Scholar]
- 25.Gordon-Lipkin E, Chodkowski B, Reich DS, et al. Retinal nerve fiber layer is associated with brain atrophy in multiple sclerosis. Neurology. 2007;69(16):1603–1609. doi: 10.1212/01.wnl.0000295995.46586.ae. [DOI] [PubMed] [Google Scholar]
- 26.Wu GF, Schwartz ED, Lei T, et al. Relation of vision to global and regional brain MRI in multiple sclerosis. Neurology. 2007;69(23):2128–2135. doi: 10.1212/01.wnl.0000278387.15090.5a. [DOI] [PubMed] [Google Scholar]
- 27.Waxman SG, Black JA. Retinal involvement inmultiple sclerosis. Neurology. 2007;69(16):1562–1563. doi: 10.1212/01.wnl.0000295993.08468.f3. [DOI] [PubMed] [Google Scholar]
- 28.Gerling J, Meyer JH, Kommerell G. Visual field defects in optic neuritis and anterior ischemic optic neuropathy: distinctive features. Graefes Arch Clin Exp Ophthalmol. 1998;236(3):188–192. doi: 10.1007/s004170050062. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.