Abstract
Imatinib is considered standard therapy for patients with chronic myelogenous leukemia (CML), inducing a high rate of hematologic and cytogenetic responses. Despite these excellent results, several patients develop resistance to imatinib. Mechanisms of resistance are varied and include BCR-ABL1 kinase domain mutations, decreased entry of imatinib into cells, acquisition of secondary genetic changes and activation of alternate signaling pathways. Second-generation tyrosine kinase inhibitors (TKI) (dasatinib, nilotinib) were developed as an alternative for patients that develop resistance or are intolerant to imatinib. Dasatinib is a dual Abl/Src kinase TKI that is structurally unrelated to imatinib and is approved for therapy of all phases of CML in patients who are resistant or intolerant to imatinib. Nilotinib is a compound related to imatinib that has greater specificity and improved binding characteristics, and has clinical activity in the setting of imatinib failure. Resistance to multiple TKIs does occur, particularly in patients with the T315I mutation. Several new agents are in development including new TKIs, aurora kinase inhibitors and homoharringtonine.
Keywords: Chronic myelogenous leukemia, imatinib, dasatinib, nilotinib, therapy
Introduction
Chronic myelogenous leukemia (CML) is a myelo-proliferative disorder (MPD) defined by the presence of the Philadelphia (Ph) chromosome (product of translocation t(9;22)(q34;q11)) and/or the chimeric gene BCR-ABL1 [1–3]. The Ph chromosome is present in 95% of cases of CML and it gives rise to the BCR-ABL1 gene, with the remaining 5% of cases having an alternative or occult translocation [2,4]. The translocation occurs in a primitive hematopoietic stem cell and the BCR-ABL1 gene encodes a fusion protein (Bcr-Abl) that has deregulated tyrosine kinase (TK) activity and activates intracellular pathways that lead to increased cellular proliferation, resistance to apoptosis and genetic instability [1,3].
The clinical course of CML typically goes through three phases [4]. Most patients (90%) are diagnosed in chronic phase (CP), characterized by an increase in white blood cell counts with immature granulocytes in the peripheral blood, and up to 40% are asymptomatic at time of diagnosis. Left untreated the disease inexorably progresses to blastic phase (BP), defined by the presence of 30% or more blasts in the bone marrow and a clinical picture indistinguishable from acute leukemia. In most patients, the transition between CP and BP is gradual and manifested by an accelerated phase (AP) characterized by the development of a progressive increase in blast counts, cytopenias and acquisition of new chromosomal abnormalities [4].
Historically, patients with CML were treated with conventional chemotherapeutic agents, such as bu-sulfan and hydroxyurea. However, these drugs did not prevent progression and the disease was considered uniformly fatal [5]. The appearance of interferon-α was a great advance, as the drug could induce hematologic and cytogenetic remissions and improvements in survival, but it was poorly tolerated due to frequent side effects [6]. Hematopoietic stem cell transplantation (HSCT) is the only proven curative treatment for CML, but it is applicable in only a fraction of patients, mainly younger patients with a matched donor [7]. Therapy with tyrosine kinase inhibitors (TKIs) has changed the natural history of CML, which has gone from a potentially fatal disorder to one that can be easily controlled [8]. Nevertheless, not all patients respond equally to TKIs and there is a potential for development of resistance. Both newer TKIs and other non-ATP-competitive agents are being evaluated in patients with CML in particular those resistant to imatinib. This review focuses on the most recent clinical results of therapy in CML with the 2nd-generation TKIs (dasatinib, nilotinib) and on newer compounds currently under development.
Imatinib
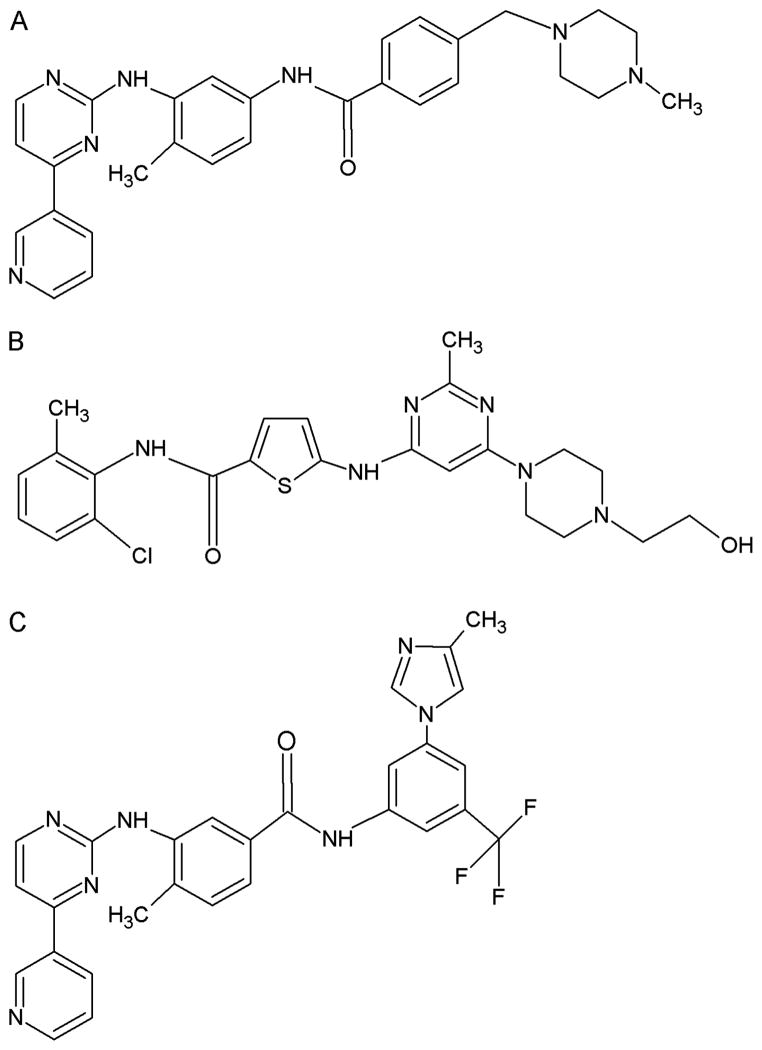
Imatinib (STI-571; Glivec, Gleevec; Novartis, Basel, Switzerland) is a 2-phenylamino-pyrimidine compound which has activity as a TKI [Figure 1(A)] [9]. Imatinib binds to the inactive conformation of the Bcr-Abl TK, occluding its ATP-binding pocket and preventing its switch to the active conformation [10]. In vitro studies showed that imatinib inhibited the proliferation of BCR-ABL1-positive cells (concentration at which 50% of the enzyme is inhibited [IC50] is 250–280 nM) [11–13]. It was discovered later that imatinib is not selective for Bcr-Abl, also inhibiting other TKs including platelet derived growth factor receptor-α and -β (PDGFR-α/β) and C-Kit [14].
Figure 1.
Tyrosine kinase inhibitors currently available for the treatment of CML. Imatinib (A), Dasatinib (B), Nilotinib (C).
Clinical results with imatinib
The early clinical studies with imatinib evaluated its efficacy in the treatment of patients with CML in CP that had failed prior therapy with interferon-α and in patients with advanced stages of the disease (AP and BP) [15–19]. These studies demonstrated the remarkable clinical activity of imatinib in CML in all phases, in particular in CP. These encouraging results were followed by a phase III trial, the IRIS (International Randomized Study of Interferon and STI571) study, which randomized 1106 patients with untreated CP CML to receive imatinib (400 mg daily) or interferon-α plus low-dose cytarabine [20]. After a median follow-up of 19 months, the rate of major cytogenetic response (MCyR, defined as 0–35% Ph+-metaphases in a conventional cytogenetic evaluation) was 87% in the imatinib arm versus 35% in the interferon arm (p <0.001). Similarly, the rate of complete cytogenetic response (CCyR, 0% Ph+-metaphases) was 76% versus 15% (p <0.001). At 18 months, the transformation free survival (TFS) was 97% vs. 91.5% (p <0.001). Therapy with imatinib was generally well tolerated. Most common side effects were superficial edema, nausea, diarrhea, rash and muscle cramps, and were usually mild or moderate in severity. Grade 3–4 cytopenias included neutropenia (17%) and thrombocytopenia (9%).
Recently, a 5 years update of the IRIS trial showed continued improvement in clinical results in patients receiving imatinib [8]. Overall, 382 patients remained on therapy with imatinib. The complete hematologic response (CHR), MCyR, and CCyR rates were 98, 92, and 87%, respectively. The event-free survival (EFS) was 83%, and TFS was 93% at 5 years. The rate of progression to AP/BP seemed to decrease with time, being 1.5% in the first year, 2.8% in the second year, 1.6% in the third year, 0.9% in the fourth year, and 0.6% in the fifth year. Importantly, cytogenetic and molecular responses had significant association with long-term outcomes. For patients achieving a CCyR within 12 months, the event-free survival at 5 years was 97%, versus 93% for patients with a partial cytogenetic response (PCyR, 1–35% Ph+ metaphases) and 81% for those without a MCyR (p <0.001). Patients who had a CCyR and a major molecular response (MMR, defined as a 3-log reduction in BCR-ABL1 transcripts by real-time quantitative polymerase chain reaction) at 18 months of therapy had a 5-year overall survival (OS) of 100%. The estimated OS at 5 years for all patients in the imatinib arm was 87%, and was 95% considering CML-only deaths. The design of the study allowed crossover between arms and there was no difference in OS between imatinib and interferon-α with cytarabine cohorts. However, historical comparisons between imatinib and interferon-α based therapy have clearly shown an improvement in survival with the use of imatinib [21–23].
Resistance to imatinib
Despite these excellent results, several patients develop resistance to imatinib. In the latest update of the IRIS study at 7 years, 60% of patients who started on therapy with imatinib remain on the study [24]. The most common reason for discontinuation of imatinib was lack of efficacy and progression in 15% of patients. Resistance to imatinib can be classified into primary (never had a response to frontline therapy with imatinib) or secondary (achieved a response but then lost it) [25]. The incidence of resistance to imatinib in untreated CP CML is ~4% per year [8]. Patients with advanced stage have a much higher incidence of resistance, around 40% in AP and 90% in BP [26]. Consensus criteria for defining resistance to imatinib have been recently defined [27].
Mechanisms of resistance to imatinib are considered to be Bcr-Abl dependent or Bcr-Abl independent [25]. Bcr-Abl dependent resistance can be the result of Bcr-Abl protein overexpression or mutations in the kinase domain. Bcr-Abl overexpression is secondary to BCR-ABL1 gene amplification and was identified both in vitro and in vivo [28]. Bcr-Abl overexpression is responsible for resistance in a small percentage of patients. BCR-ABL1 mutations are the most frequent mechanism of resistance to imatinib and other TKIs. They occur in 30–50% of patients, and are more common in patients who progress to AP and BP at time of resistance [28–32]. Mutations associated with imatinib resistance disrupt critical contact points between imatinib and the Bcr-Abl protein (e.g. Y253, T315) or induce a change in conformation from inactive to active, to which imatinib is unable to bind (e.g. H396) [28,33]. Some mutations induce mild to moderate resistance to imatinib while others are associated with a high degree of resistance. The P-loop mutations (in the phosphate binding loop, amino acids 244 to 255) and the gatekeeper T315I mutation are associated with a high level of resistance to imatinib [28,31,34].
Several other mechanisms of resistance to imatinib have been described in patients who do not have BCR-ABL1 mutations. There is interpatient variability in imatinib concentrations [35,36]. Measuring the plasma concentrations of imatinib has been demonstrated to be useful by some investigators, showing a better outcome in patients who achieve higher plasma levels of imatinib [37,38]. Other reports have not found such a correlation, however [39]. Imatinib is transported into cells via the human organic cationic transporter-1 (OCT-1) [40]. Polymorphisms may affect the expression of OCT-1. There is in vitro and in vivo data suggesting that low OCT-1 expression is a potential mechanism of imatinib resistance by leading to decreased intracellular drug concentrations [41,42]. Clonal evolution and acquisition of secondary genetic changes may also be associated with resistance to imatinib, such as loss of p53 [43].
Some recent reports have focused on the role of other TK in mediating resistance to imatinib, in particular members of the Src family of kinases (SFK) [44–46]. Activation of Src kinases may promote cell growth and survival and lead to Bcr-Abl independence [45–47]. Overexpression of the SFK Lyn has been demonstrated in K562 cells resistant to imatinib, and lysate of blood cells of patients with BP CML resistant to imatinib were found to contain high levels of Lyn and Hck proteins [45].
Dasatinib
Dasatinib (formerly known as BMS-354825; Sprycel; Bristol-Myers Squibb, New York, NY) [Figure 1(B)] is an orally available, multi-targeted TKI structurally unrelated to imatinib [48]. Dasatinib binds to the ATP binding pocket of Bcr-Abl, and is capable of binding Bcr-Abl both in the active and inactive conformation [48,49].
Dasatinib is 325-fold more potent than imatinib in vitro against wild-type Bcr-Abl [50,51]. In cellular assays, dasatinib inhibited the proliferation of BCR-ABL1 transfected BaF3 cells with IC50 values of 0.8 nM [51]. Dasatinib has activity against most imatinib-resistant BCR-ABL1 mutants [50,51]. However, the T315I mutation is still highly resistant to dasatinib [50,51]. Similar to imatinib, dasatinib has activity against PDGFR-β (IC50 28 nM) and C-Kit (IC50 13 nM) [52,53]. In addition dasatinib also inhibits several members of the SFK, including Src (IC50 0.55 nM), Lck (IC50 1.1 nM), Fyn (IC50 0.2 nM), and Yes (IC50 0.41 nM) [52]. The activity of dasatinib in vivo was confirmed in mouse models of Ph+-leukemias with expression of different genotypes of BCR-ABL1 [50]. Recently, dasatinib was approved by the FDA for use as a single agent for the treatment of patients with CML (all phases) and Ph+-acute lymphoblastic leukemia (ALL) who have developed resistance or intolerance to imatinib.
Clinical results with dasatinib
Phase I study
Dasatinib was first evaluated in a phase I dose escalation study in patients with CML and Ph+-ALL that were resistant- or intolerant to imatinib [54] (Table I). A total of 84 patients (CP = 40, AP = 11, myeloid BP [MBP] = 23, lymphoid BP [LBP]/Ph+-ALL = 10) were treated with dasatinib with doses ranging from 15 to 240 mg daily, administered on a once daily or twice daily schedule.
Table I.
| Study | Disease stage | N | % Response
|
||
|---|---|---|---|---|---|
| CHR | Cytogenetic response
|
||||
| Major | Complete | ||||
| Phase I | CP | 40 | 92 | 45 | 35 |
| AP | 11 | 45 | 27 | 18 | |
| MBP | 23 | 35 | 35 | 26 | |
| LBP/Ph+ ALL | 10 | 70 | 80 | 30 | |
| START-C | CP | 387 | 91 | 59 | 49 |
| START-A | AP | 174 | 45 | 39 | 32 |
| START-B | MBP | 109 | 25 | 33 | 26 |
| START-L | LBP | 48 | 29 | 52 | 46 |
AP, accelerated phase; CHR, complete hematological response; CP, chronic phase; LBP, lymphoid blast phase; MBP, myeloid blast phase; Ph+-ALL, Philadelphia-positive acute lymphoblastic leukemia.
Clinical results confirmed the activity of dasatinib as Bcr-Abl inhibitor. For patients in CP, a CHR was obtained in 92%, and a MCyR in 45% (35% CCyR). Similarly, patients in AP also had a high rate of CHR (45%) and MCyR (27%; 18% CCyR). Responses were durable, with 95% of patients in CP and 82% of patients in AP maintaining their response after a median follow-up of 12 and 5 months, respectively. Responses were also observed in patients with MBP with CHR in 35% and MCyR in 35% (26% CCyR). In patients with LBP/Ph+-ALL, the CHR rate was 70% and the MCyR rate was 80% (30% CCyR). Responses were of short duration in BP, with only one patient (10%) with LBP/Ph+-ALL still maintaining response after a median follow-up of 4 months, and only six patients with MBP still receiving the drug with a follow-up of 5 to 12 months. Sixty patients (71%) had BCR-ABL1 mutations at the beginning of study, and clinical responses to dasatinib were observed among all BCR-ABL1 mutations, with the exception of the T315I mutation. Pharmacokinetic and pharmacodynamic data supported a twice daily dosing schedule to achieve consistent TK inhibition over a period of 24 h, and the dose of 70 mg twice daily was chosen as the ideal dose to be pursued for further studies.
Phase II studies
A series of phase II studies (START studies; Src-Abl Tyrosine kinase inhibition Activity Research Trials) evaluated the efficacy of single agent dasatinib in patients with CML in CP (START-C), AP (START-A), MBP (START-B), and LBP/Ph+-ALL (START-L) that were resistant or intolerant to imatinib. Patients were treated with dasatinib at a dose of 70 mg twice daily, with dose escalation and reduction allowed for lack of response and toxicity, respectively. The results are summarized in Table I.
In the START-C trial, a total of 387 patients (288 = imatinib resistant; 99 = imatinib intolerant) in CP were treated with dasatinib [55]. A CHR was obtained or maintained in 91% of patients. Median duration of response was not reached after 18 months of follow-up. A MCyR was obtained or maintained in 59% of patients, with 49% achieving a CCyR. Only seven patients who achieved a MCyR progressed, and three of them had developed BCR-ABL1 mutations (V299L, T315I, E459K). BCR-ABL1 mutations were present at baseline in 40% of patients, and there was no difference in response rate between patients with and without mutations. Median daily dose was 101 mg, and dose reductions were required in 73% of patients and treatment interruption in 87%. At 15 months, the progression-free survival (PFS) was 90% and the OS was 96%.
A total of 174 patients with CML in AP were treated in the START-A trial [56]. After a median follow-up of 14.1 months, a CHR was obtained in 45% of patients, with MCyR and CCyR seen in 39% and 32%, respectively. The PFS and OS at 12 months were 66% and 82%, respectively. Dose reductions were required in 65% of patients and dose interruptions in 85%. The START-B trial treated 109 patients with MBP and the START-L trial treated 48 patients with LBP. The final results of both trials were recently combined in one report [57]. Most patients (90%) were resistant to imatinib. A major hematologic response (MaHR, defined as CHR plus no evidence of leukemia [NEL]) was obtained in 31% of patients with MBP (25% CHR) and 35% of patients with LBP (29% CHR). The median duration of MaHR was not reached in patients with MBP and was 4.9 months in patients with LBP. A MCyR was achieved in 33% of patients with MBP (26% CCyR) and 52% of patients with LBP (46% CCyR). The median PFS was 6.7 months in patients with MBP and 3.0 months in patients with LBP. The median OS was 11.8 months and 5.3 months in patients with MBP and LBP, respectively.
Overall, all these studies defined dasatinib as a very active agent in patients with CML in all phases who had failed or were intolerant to previous therapy with imatinib.
Dasatinib versus high dose imatinib
Dasatinib was also compared head-to-head with imatinib in a study of patients with CML in CP that failed therapy with imatinib (400–600 mg daily) (START-R trial) [58]. Patients were randomized 2:1 between dasatinib (70 mg twice daily) and high-dose imatinib (800 mg daily). A total of 150 patients were enrolled (dasatinib = 101; imatinib = 49). Approximately two-thirds of them had received imatinib at a dose of 600 mg daily. Overall, CHR rates were higher with dasatinib (93% vs. 82%, p = 0.034). There was also a higher rate of MCyR (52% vs. 33%, p = 0.023) and CCyR (40% vs. 16%, p = 0.004). There was no difference in the MCyR rate between imatinib and dasatinib in the subgroup of patients that had only received 400 mg of imatinib before being considered resistant (58% vs. 53%, p = non significant). Major molecular responses were also improved by switching to dasatinib (16% vs. 4%, p = 0.038). The survival outcomes favored dasatinib, and the hazard ratio for PFS was 0.14 (p <0.001). Dasatinib lead to more episodes of pleural effusion (all grades) (17% vs. 0%) and grade 3–4 cytopenias (neutropenia: 61% vs. 39%; thrombocytopenia: 56% vs. 14%).
Dasatinib dose optimization study
Based on the results of the START-C trial, where the median daily dose administered was 101 mg, but responses were still seen in the majority of patients, a randomized phase III study was conducted to evaluate what would be the optimal dose and schedule of dasatinib in patients with CML in CP [59]. A total of 670 patients with imatinib-resistant or –intolerant CML in CP were randomized between one of four dasatinib treatments: 100 mg once daily, 50 mg twice daily, 140 mg once daily, and 70 mg twice daily. With median treatment duration of 8 months, there was no difference in outcomes, with similar rates of CHR, MCyR, and CCyR. There was no difference in time to achieve a CyR and in PFS. Importantly, compared to the approved dose of 70 mg twice daily, the dose of 100 mg once daily lead to lower rates of pleural effusion (7% vs. 16%, p = 0.024), grade 3–4 thrombocytopenia (22% vs. 37%, p = 0.004), and fewer patients requiring treatment interruptions (51% vs. 68%) and dose reductions (30% vs. 55%). These results reflect in vitro data demonstrating that intermittent, but potent inhibition of Bcr-Abl is sufficient to lead to apoptosis in CML cell lines [60]. As a consequence the approved dose of dasatinib for therapy of patients with CML in CP has changed to 100 mg once daily.
Managing toxicity of dasatinib
Therapy with dasatinib is relatively well tolerated. The most common side effects are cytopenias, specially neutropenia and thrombocytopenia. Cytopenias are more common in patients with advanced stages of CML (AP/BP) (grade 3–4: 80–90%) than in CP (grade 3–4: 50%) [55–57]. Besides the fact that many of the patients in AP/BP already have cytopenias at baseline, this high incidence may be a reflection of the rapid elimination of the malignant clone with few normal residual hematopoietic cells present to reconstitute hematopoiesis [57]. In general, most cytopenias are managed with treatment interruptions and dose reductions. Growth factor support (such as G-CSF and interleukin-11) can be used in this setting to decrease treatment interruptions [61].
Other side effects of dasatinib that deserve mention include pleural effusions and bleeding episodes. Pleural effusions occur more commonly in patients receiving higher doses (>140 mg daily) and on a twice daily schedule [62]. The incidence of grade 1–4 pleural effusion can range from 10 to 30% [55–57,62]. The precise mechanism is not known, but it may involve dasatinib inhibition of PDGFRβ. It has been shown that PDGFRβ regulates interstitial fluid homeostasis by the phosphatidylinositol-3-kinase (PI3K) pathway [63]. Dasatinib induced pleural effusions are more common in patients with a previous history of cardiac disease and hypertension. In most cases (80%), pleural effusions are exudates. The management of pleural effusions induced by dasatinib includes treatment interruption, diuretics, corticosteroids, and thoracocentesis [62].
Dasatinib has also been shown to be associated with bleeding diathesis, in particular gastrointestinal (GI) bleeding [64]. The overall incidence is in the range of 23%, with grade 3 episodes occurring in 7% of patients [64]. Most episodes (69%) occur in the first 3 months of therapy and the GI tract is involved in 81% of cases [64]. In more than half of cases, platelets are above 30 ×109/L [64]. Laboratory analysis has revealed that dasatinib induces platelet dysfunction with an aspirin-like effect, inhibiting platelet aggregation in response to arachidonic acid and epinephrine [65]. Patients on dasatinib are at an increased risk of bleeding even with normal platelet counts, and the use of concomitant platelet inhibitors should be avoided if possible.
Nilotinib
Nilotinib (formerly known as AMN107; Tasigna; Novartis, Basel, Switzerland) is a TKI structurally similar to imatinib [Figure 1(C)] [66]. Nilotinib was developed by modifying the methylpiperazinyl group of imatinib and improving its binding characteristics [66]. Nilotinib has a higher binding affinity and selectivity for the Bcr-Abl kinase than imatinib. It is more potent than imatinib in inhibiting TK activity of Bcr-Abl and 10–30 times more potent in inhibiting the proliferation of BaF3 cells transfected with the BCR-ABL1 oncogene (IC50 25 nM) [66]. Nilotinib also showed efficacy in inhibiting CML cell lines expressing imatinib-resistant mutant Bcr-Abl kinases [51,67]. Mouse models of Bcr-Abl positive leukemias confirmed in vivo activity of nilotinib [66]. Nilotinib also inhibits, albeit with less potency than imatinib, the TK PDGFRβ (IC50 57 nM), and C-Kit (IC50 160 nM) [66]. Nilotinib has no activity against SFK. Nilotinib is approved by the FDA for the treatment of patients with CML in CP and AP who are resistant or intolerant to imatinib.
Clinical results with nilotinib
Phase I study
A phase I dose escalation study in patients with CML and Ph+-ALL that were imatinib-resistant evaluated the safety and tolerability of nilotinib [68]. A total of 119 patients (CP = 17, AP = 56, BP = 33, Ph+-ALL = 13) were treated with doses of nilotinib ranging from 50 to 1200 mg once daily and 400 to 600 mg twice daily. Mutations of the BCR-ABL1 gene were present in 37 of 91 patients who had a mutation analysis at baseline.
Pharmacokinetics showed that the half-life of nilotinib was 15 h, and there was saturation of plasma levels at doses of 400 mg or more when given once daily, probably secondary to saturation of GI absortion. A twice daily schedule was evaluated, and exposure at the steady state was higher with 400 mg twice daily than with 800 mg once daily. The mean through level at the steady state with 400 mg twice daily was 1.7 μM, which exceeds the IC50 values for inhibiting the wild-type Bcr-Abl kinase (20–50 nM) and most imatinib resistant mutants (19–709 nM) [67,68].
Nilotinib had meaningful clinical activity in patients with CML resistant to imatinib (Table II). The hematologic response (HR) rate (includes CHR, marrow response and return to CP) to nilotinib was 39% in BP, 74% in AP and 92% in CP. Cytogenetic responses were seen in 27% of patients with BP (MCyR 18%, CCyR 6%), 55% of patients with AP (MCyR 27%, CCyR 14%), and 53% of CP (CCyR 35%). Dose escalations improved the response rate in 13 of 23 patients who initially received doses of 50 to 400 mg daily. There was no difference in response rate among patients with and without BCR-ABL1 mutations, but two patients with the T315I mutation did not respond, as expected.
Table II.
| Study | Disease stage | N | % Response
|
|||
|---|---|---|---|---|---|---|
| Hematologic response
|
Cytogenetic response
|
|||||
| HR | CHR | Major | Complete | |||
| Phase I | CP | 17 | 92 | 92 | 35 | 35 |
| AP | 56 | 74 | 51 | 27 | 14 | |
| BP | 33 | 39 | 6 | 18 | 6 | |
| Ph+-ALL* | 10 | 10 | – | – | – | |
| Phase II | CP | 321 | NR | 76 | 58 | 42 |
| AP | 134 | 56 | 30 | 32 | 19 | |
| BP | 135 | 38 | 25 | – | – | |
| Ph+-ALL | 41 | 27 | 24 | – | – | |
AP, accelerated phase; BP, blastic phase; CHR, complete hematological response; CP, chronic phase; HR, hematological response; NR, not reported; Ph+-ALL, Philadelphia-positive acute lymphoblastic leukemia.
Three patients with Ph+-ALL who had persistent molecular signs of ALL were enrolled.
One of these patients entered a complete molecular remission.
Phase II studies
Following the results of the phase I study, several phase II studies were designed to evaluate the efficacy of nilotinib in patients with CML who were resistant or intolerant to imatinib (Table II). Patients were treated with nilotinib at a dose of 400 mg twice daily with the option of escalating the dose to 600 mg twice daily in case of no response.
The CP study recruited 321 patients (71% imatinib-resistant). After 2 years follow-up, the MCyR was 58% (CCyR 42%) [69,70]. Responses were durable, and 84% of patients who achieved MCyR were maintaining their response at 18 months. Responses were observed in patients with and without BCR-ABL1 mutations. The estimated OS at 18 months was 91%. In the AP study, 138 patients were enrolled; 80% were imatinib resistant [71]. The HR rate was 56%, with a CHR obtained in 30%. At 1 year, 78% of patients maintained their HR. MCyR and CCyR occurred in 32% and 19% of patients, respectively. After 18 months, 69% of patients maintained MCyR. Estimated OS at 1 year was 82%.
The results of the phase II studies conducted in BP and Ph+-ALL were also encouraging, but response rates and duration were lower [72,73]. In the BP study, 135 patients were treated. The HR rate was 38% (CHR 25%). After a median treatment duration of 84 days, only 16 patients (12%) were still on study. In the Ph+-ALL study 41 patients were treated, and the CHR rate was 24%. After a median treatment duration of 53 days, only 2 patients (5%) remained on the study.
Managing toxicity of nilotinib
Therapy with nilotinib is very well tolerated. The most common hematological toxicities include neutropenia (grade 3–4; 30–40%) and thrombocytopenia (grade 3–4; 28–40%) [70,71]. Non-hematological toxicity is usually mild (grade 1–2), with less than 2% of patients experiencing grade 3–4 toxicity, most commonly rash, diarrhea, nausea, fatigue, and headache [70,71]. Grade 3–4 biochemical laboratory abnormalities include elevated lipase (15–16%), elevated total bilirubin levels (3–7%), hypophosphatemia (12–15%), and hyperglycemia (12%) [70,71]. Usually biochemical abnormalities are transient and without associated clinical symptoms. Elevated bilirubin levels are most commonly due to unconjugated bilirubin. The (TA)7 polymorphism of the promoter region of the gene of uridine diphosphate glucuronosyltransferase 1A1 (UGT1A1), the enzyme responsible for glucoronidation of bilirubin in humans, is clinically associated with Gilbert’s syndrome and the development of nilotinib induced hyperbilirubinemia [74]. Most of the time, toxicities induced by nilotinib are managed with temporary interruptions and dose reductions as necessary. Nilotinib has also been shown to increase the corrected QT interval by Fredericia’s formula (QTcF). QTcF prolongation is uncommon, occurring in only 2.5% of patients [70,71]. Sudden deaths have been reported, however, and clinicians should be aware of potential drug interactions that might increase the risk of QTcF prolongation [68]. Key points of dasatinib and nilotinib are summarized in Table III.
Table III.
Summary of key points for dasatinib and nilotinib.
| Dasatinib |
| Approved for |
| CP |
| AP |
| BP |
| Dose |
| CP – 100 mg once daily |
| AP/BP – 70 mg twice daily |
| BCR-ABL1 mutations with decreased sensitivity (other than T315I) |
| F317L |
| V299L |
| E255K/V |
| Q252H |
| Common toxicities |
| Myelosuppression |
| Fluid retention |
| Pleural effusion |
| Platelet dysfunction |
| Bleeding diathesis
|
| Nilotinib
|
| Approved for |
| CP |
| AP |
| Dose |
| CP/AP – 400 mg twice daily |
| BCR-ABL1 mutations with decreased sensitivity (other than T315I) |
| Y253H |
| E255K/V |
| F359C/V |
| Common toxicities |
| Myelosuppression |
| Hyperbilirubinemia |
| Elevations of amylase and lipase |
| Hyperglicemia |
AP, accelerated phase; BP, blastic phase; CP, chronic phase.
Future therapies in chronic myelogenous leukemia
Besides dasatinib and nilotinib, there are other drugs in development for treatment of patients with imatinib-resistant CML, in particular for patients with the T315I mutation (Table IV). For more details, the reader is referred to recent reviews [75,76].
Table IV.
Selected new agents in development for CML.
| Tyrosine kinase inhibitors |
| Bosutinib |
| INNO-406 |
| AP24534 |
| SGX393 |
| Aurora kinase inhibitors |
| PHA-739358 |
| XL228 |
| AT9283 |
| KW-2449 |
| ABL switch pocket inhibitors |
| DCC-2036 |
| DP-2494 |
| Inductor of apoptosis |
| Omacetaxine mepesuccinate (Homoharringtonine) |
| Heat shock protein 90 inhibitor |
| 17,AAG |
| Phosphatase (PP2A) activator |
| FTY720 |
| Farnesyl transferase inhibitors |
| BMS214662 |
| Rac GTPase inhibitors |
| NSC23766 |
| Histone deacetylase inhibitors |
| LAQ824 |
| Panobinostat (also known as LBH589) |
| Depsipeptide (FK228) |
CML, chronic myelogenous leukemia.
New tyrosine kinase inhibitors
There are several new TKIs in pre-clinical and clinical trials for treatment of patients with CML. Bosutinib (also known as SKI-606) is an orally available dual Abl/Src inhibitor which is more potent than imatinib in inhibiting Bcr-Abl (IC50 13 nM) but has no activity against PDGFRβ (IC50 370 nM) and C-Kit (IC50 6,000 nM) [77]. Two phase II trial have demonstrated the efficacy of bosutinib in patients with CP and advanced CML resistant to imatinib, also demonstrating activity against most BCR-ABL1 genotypes resistant to imatinib [78–80]. In patients with CML in CP resistant to imatinib, the CHR rate was 79% and the MCyR rate was 40% (CCyR 29%) [78]. Bosutinib has as excellent toxicity profile, with few patients developing cytopenias (neutropenia grade 3–4; 13%, thrombocytopenia grade 3–4; 23%) and episodes of fluid retention (grades 1–4; 10%) [78]. This is probably secondary to its decreased activity against PDGFRβ and C-Kit. The most common side effects were diarrhea (grade 3–4; 8%), nausea, and vomiting [78,79]. INNO406 is a TKI that targets wild type and most mutant genotypes of BCR-ABL1 and also has specific activity against the SFK Lyn, with no activity against other SFK members [81,82]. INNO-406 is 25 to 55 times more potent than imatinib in vitro (IC50 11–22 nM) [81,82]. In a phase I study, INNO-406 was shown to have clinical activity in patients with imatinib-resistant or -intolerant Ph+-leukemias with a good tolerance profile [83].
Aurora kinase inhibitors
Aurora kinases are serine/threonine kinases that regulate several mitotic processes during cell division [84]. Aurora kinases are overexpressed in several malignancies, and may lead to aneuploidy and carcinogenesis [85]. Aurora kinase inhibitors (AKIs) have been developed for therapy in CML, and their mechanism of action involves simultaneous targeting of both aurora kinases and Bcr-Abl. The first AKI to be developed was MK-0457, and responses were seen in patients with CML with the T315I mutation [86,87]. Most common toxicities included myelosuppression, alopecia, and mucositis [86,87]. More recently, the AKI PHA-739358 and XL-228 are being evaluated in phase I and phase II studies in patients with CML. These drugs have in vitro and in vivo activity against CML cells harboring the BCR-ABL1 T315I mutation [88,89]. Clinical studies are being conducted in patients with CML refractory to other TKIs, and clinical responses have been seen in patients who developed the T315I mutation [90,91]. There is also in vitro data suggesting that these drugs may synergize with imatinib, forming the rationale for future studies with combined therapy [92].
Homoharringtonine
Homoharringtonine (cephalotaxine, HHT) is a natural alkaloid extract from the seeds of the evergreen tree Cephalotaxus harringtonia K. Koch var harringtonia [93]. HHT was first isolated and developed in China and used for treatment of CML and AML in that country [94,95]. Before the development of imatinib, HHT was one of the most efficient agents for salvaging patients that were resistant to interferon-alpha [96]. HHT exerts antitumoral activity by disrupting protein synthesis and inducing apoptosis by down regulating the anti-apoptotic protein myeloid cell leukemia-1 (Mcl-1) [97]. Currently, HHT is being re-evaluated in the treatment of patients with CML who are resistant to imatinib and other TKIs. A single center phase II trial demonstrated activity of subcutaneous HHT in patients with CML in CP that were refractory to previous therapy with TKIs [98]. Patients received an initial i.v. loading dose of 2.5 mg/m2 over 24 h followed by 1.25 mg/m2 s.c. twice daily for 14 days until remission [98]. Six patients were treated, 5 achieved a CHR and 3 had a CyR (CCyR = 1, minor CyR = 2) [98]. A semisynthetic formulation of HHT (omacetaxine mepesuccinate) has been developed [99]. An international phase II trial with omacetaxine is being conducted in patients with CML who harbor the T315I mutation [100]. The outcome for 55 patients has been reported (CP = 32, AP = 14, BP = 9). Sixty-four percent of patients in CP had disappearance of the T315I clones, and 20% had a MCyR. HHT has a different mechanism of action that allows it to exert antitumoral effects in cells that have escaped control from TKIs.
Conclusions
Although it is clear that therapy with imatinib has dramatically changed the outcomes for patients with CML, a fraction of patients will develop resistance. The development of novel TKIs has helped improve treatment outcomes for these patients. However, resistance is still a problem, even with second generation compounds. Further research into the mechanisms of resistance and developing compounds that are able to overcome them will no doubt continue to improve the outcome of patients with this disease.
Footnotes
Declaration of interest: F. Ravandi had research funding from Bristol-Myers-Squibb and had received honoraria from Novartis Pharmaceuticals and Bristol-Myers-Squibb. The authors alone are responsible for the writing of this paper.
References
- 1.Deininger MW, Goldman JM, Melo JV. The molecular biology of chronic myeloid leukemia. Blood. 2000;96:3343–3356. [PubMed] [Google Scholar]
- 2.Faderl S, Talpaz M, Estrov Z, O’Brien S, Kurzrock R, Kantarjian HM. The biology of chronic myeloid leukemia. N Engl J Med. 1999;341:164–172. doi: 10.1056/NEJM199907153410306. [DOI] [PubMed] [Google Scholar]
- 3.Quintas-Cardama A, Cortes J. Molecular biology of bcr-abl1-positive chronic myeloid leukemia. Blood. 2009;113:1619–1630. doi: 10.1182/blood-2008-03-144790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sawyers CL. Chronic myeloid leukemia. N Engl J Med. 1999;340:1330–1340. doi: 10.1056/NEJM199904293401706. [DOI] [PubMed] [Google Scholar]
- 5.Allan NC. Therapeutic options in chronic myeloid leukaemia. Blood Rev. 1989;3:45–52. doi: 10.1016/0268-960x(89)90024-6. [DOI] [PubMed] [Google Scholar]
- 6.Interferon α versus chemotherapy for chronic myeloid leukemia: a meta-analysis of seven randomized trials. Chronic Myeloid Leukemia Trialists’ Collaborative Group. . J Natl Cancer Inst. 1997;89:1616–1620. [PubMed] [Google Scholar]
- 7.Biggs JC, Szer J, Crilley P, et al. Treatment of chronic myeloid leukemia with allogeneic bone marrow transplantation after preparation with BuCy2. Blood. 1992;80:1352–1357. [PubMed] [Google Scholar]
- 8.Druker BJ, Guilhot F, O’Brien SG, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355:2408–2417. doi: 10.1056/NEJMoa062867. [DOI] [PubMed] [Google Scholar]
- 9.Deininger M, Buchdunger E, Druker BJ. The development of imatinib as a therapeutic agent for chronic myeloid leukemia. Blood. 2005;105:2640–2653. doi: 10.1182/blood-2004-08-3097. [DOI] [PubMed] [Google Scholar]
- 10.Nagar B, Bornmann WG, Pellicena P, et al. Crystal structures of the kinase domain of c-Abl in complex with the small molecule inhibitors PD173955 and imatinib (STI-571) Cancer Res. 2002;62:4236–4243. [PubMed] [Google Scholar]
- 11.Buchdunger E, Zimmermann J, Mett H, et al. Inhibition of the Abl protein-tyrosine kinase in vitro and in vivo by a 2-phenylaminopyrimidine derivative. Cancer Res. 1996;56:100–104. [PubMed] [Google Scholar]
- 12.Carroll M, Ohno-Jones S, Tamura S, et al. CGP 57148, a tyrosine kinase inhibitor, inhibits the growth of cells expressing BCR-ABL, TEL-ABL, and TEL-PDGFR fusion proteins. Blood. 1997;90:4947–4952. [PubMed] [Google Scholar]
- 13.Druker BJ, Tamura S, Buchdunger E, et al. Effects of a selective inhibitor of the Abl tyrosine kinase on the growth of Bcr-Abl positive cells. Nat Med. 1996;2:561–566. doi: 10.1038/nm0596-561. [DOI] [PubMed] [Google Scholar]
- 14.Buchdunger E, Cioffi CL, Law N, et al. Abl protein-tyrosine kinase inhibitor STI571 inhibits in vitro signal transduction mediated by c-kit and platelet-derived growth factor receptors. J Pharmacol Exp Ther. 2000;295:139–145. [PubMed] [Google Scholar]
- 15.Druker BJ, Sawyers CL, Kantarjian H, et al. Activity of a specific inhibitor of the BCR-ABL tyrosine kinase in the blast crisis of chronic myeloid leukemia and acute lymphoblastic leukemia with the Philadelphia chromosome. N Engl J Med. 2001;344:1038–1042. doi: 10.1056/NEJM200104053441402. [DOI] [PubMed] [Google Scholar]
- 16.Druker BJ, Talpaz M, Resta DJ, et al. Efficacy and safety of a specific inhibitor of the BCR-ABL tyrosine kinase in chronic myeloid leukemia. N Engl J Med. 2001;344:1031–1037. doi: 10.1056/NEJM200104053441401. [DOI] [PubMed] [Google Scholar]
- 17.Kantarjian H, Sawyers C, Hochhaus A, et al. Hematologic and cytogenetic responses to imatinib mesylate in chronic myelogenous leukemia. N Engl J Med. 2002;346:645–652. doi: 10.1056/NEJMoa011573. [DOI] [PubMed] [Google Scholar]
- 18.Sawyers CL, Hochhaus A, Feldman E, et al. Imatinib induces hematologic and cytogenetic responses in patients with chronic myelogenous leukemia in myeloid blast crisis: results of a phase II study. Blood. 2002;99:3530–3539. doi: 10.1182/blood.v99.10.3530. [DOI] [PubMed] [Google Scholar]
- 19.Talpaz M, Silver RT, Druker BJ, et al. Imatinib induces durable hematologic and cytogenetic responses in patients with accelerated phase chronic myeloid leukemia: results of a phase 2 study. Blood. 2002;99:1928–1937. doi: 10.1182/blood.v99.6.1928. [DOI] [PubMed] [Google Scholar]
- 20.O’Brien SG, Guilhot F, Larson RA, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348:994–1004. doi: 10.1056/NEJMoa022457. [DOI] [PubMed] [Google Scholar]
- 21.Kantarjian H, Talpaz M, O’Brien S, et al. Survival benefit with imatinib mesylate therapy in patients with accelerated-phase chronic myelogenous leukemia–comparison with historic experience. Cancer. 2005;103:2099–2108. doi: 10.1002/cncr.21032. [DOI] [PubMed] [Google Scholar]
- 22.Kantarjian HM, Talpaz M, O’Brien S, et al. Survival benefit with imatinib mesylate versus interferon-α-based regimens in newly diagnosed chronic-phase chronic myelogenous leukemia. Blood. 2006;108:1835–1840. doi: 10.1182/blood-2006-02-004325. [DOI] [PubMed] [Google Scholar]
- 23.Kantarjian HM, O’Brien S, Cortes J, et al. Imatinib mesylate therapy improves survival in patients with newly diagnosed Philadelphia chromosome-positive chronic myelogenous leukemia in the chronic phase: comparison with historic data. Cancer. 2003;98:2636–2642. doi: 10.1002/cncr.11831. [DOI] [PubMed] [Google Scholar]
- 24.O’Brien SG, Guilhot F, Goldman JM, et al. International randomized study of interferon versus STI571 (IRIS) 7-year follow-up: sustained survival, low rate of transformation and increased rate of major molecular response (MMR) in patients (pts) with newly diagnosed chronic myeloid leukemia in chronic phase (CMLCP) treated with imatinib (IM) Blood. 2008;112:76. (Abstract 186) [Google Scholar]
- 25.Apperley JF. Part I: mechanisms of resistance to imatinib in chronic myeloid leukaemia. Lancet Oncol. 2007;8:1018–1029. doi: 10.1016/S1470-2045(07)70342-X. [DOI] [PubMed] [Google Scholar]
- 26.Lahaye T, Riehm B, Berger U, et al. Response and resistance in 300 patients with BCR-ABL-positive leukemias treated with imatinib in a single center: a 4. 5-year follow-up. Cancer. 2005;103:1659–1669. doi: 10.1002/cncr.20922. [DOI] [PubMed] [Google Scholar]
- 27.Baccarani M, Saglio G, Goldman J, et al. Evolving concepts in the management of chronic myeloid leukemia: recommendations from an expert panel on behalf of the European LeukemiaNet. Blood. 2006;108:1809–1820. doi: 10.1182/blood-2006-02-005686. [DOI] [PubMed] [Google Scholar]
- 28.Gorre ME, Mohammed M, Ellwood K, et al. Clinical resistance to STI-571 cancer therapy caused by BCR-ABL gene mutation or amplification. Science. 2001;293:876–880. doi: 10.1126/science.1062538. [DOI] [PubMed] [Google Scholar]
- 29.Soverini S, Martinelli G, Rosti G, et al. ABL mutations in late chronic phase chronic myeloid leukemia patients with up-front cytogenetic resistance to imatinib are associated with a greater likelihood of progression to blast crisis and shorter survival: a study by the GIMEMA Working Party on Chronic Myeloid Leukemia. J Clin Oncol. 2005;23:4100–4109. doi: 10.1200/JCO.2005.05.531. [DOI] [PubMed] [Google Scholar]
- 30.Jabbour E, Kantarjian H, Jones D, et al. Frequency and clinical significance of BCR-ABL mutations in patients with chronic myeloid leukemia treated with imatinib mesylate. Leukemia. 2006;20:1767–1773. doi: 10.1038/sj.leu.2404318. [DOI] [PubMed] [Google Scholar]
- 31.Branford S, Rudzki Z, Walsh S, et al. High frequency of point mutations clustered within the adenosine triphosphate-binding region of BCR/ABL in patients with chronic myeloid leukemia or Ph-positive acute lymphoblastic leukemia who develop imatinib (STI571) resistance. Blood. 2002;99:3472–3475. doi: 10.1182/blood.v99.9.3472. [DOI] [PubMed] [Google Scholar]
- 32.Roche-Lestienne C, Soenen-Cornu V, Grardel-Duflos N, et al. Several types of mutations of the Abl gene can be found in chronic myeloid leukemia patients resistant to STI571, and they can pre-exist to the onset of treatment. Blood. 2002;100:1014–1018. doi: 10.1182/blood.v100.3.1014. [DOI] [PubMed] [Google Scholar]
- 33.Shah NP, Nicoll JM, Nagar B, et al. Multiple BCR-ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia. Cancer Cell. 2002;2:117–125. doi: 10.1016/s1535-6108(02)00096-x. [DOI] [PubMed] [Google Scholar]
- 34.O’Hare T, Eide CA, Deininger MW. Bcr-Abl kinase domain mutations, drug resistance, and the road to a cure for chronic myeloid leukemia. Blood. 2007;110:2242–2249. doi: 10.1182/blood-2007-03-066936. [DOI] [PubMed] [Google Scholar]
- 35.le Coutre P, Kreuzer KA, Pursche S, et al. Pharmacokinetics and cellular uptake of imatinib and its main metabolite CGP74588. Cancer Chemother Pharmacol. 2004;53:313–323. doi: 10.1007/s00280-003-0741-6. [DOI] [PubMed] [Google Scholar]
- 36.Peng B, Hayes M, Resta D, et al. Pharmacokinetics and pharmacodynamics of imatinib in a phase I trial with chronic myeloid leukemia patients. J Clin Oncol. 2004;22:935–942. doi: 10.1200/JCO.2004.03.050. [DOI] [PubMed] [Google Scholar]
- 37.Picard S, Titier K, Etienne G, et al. Trough imatinib plasma levels are associated with both cytogenetic and molecular responses to standard-dose imatinib in chronic myeloid leukemia. Blood. 2007;109:3496–3499. doi: 10.1182/blood-2006-07-036012. [DOI] [PubMed] [Google Scholar]
- 38.Larson RA, Druker BJ, Guilhot F, et al. Imatinib pharmacokinetics and its correlation with response and safety in chronic-phase chronic myeloid leukemia: a subanalysis of the IRIS study. Blood. 2008;111:4022–4028. doi: 10.1182/blood-2007-10-116475. [DOI] [PubMed] [Google Scholar]
- 39.Ault P, Kantarjian HM, Bryan J, et al. Clinical use of imatinib plasma levels in patients with chronic myeloid leukemia (CML) Blood. 2008;112:Abstract 4255. [Google Scholar]
- 40.Thomas J, Wang L, Clark RE, Pirmohamed M. Active transport of imatinib into and out of cells: implications for drug resistance. Blood. 2004;104:3739–3745. doi: 10.1182/blood-2003-12-4276. [DOI] [PubMed] [Google Scholar]
- 41.Crossman LC, Druker BJ, Deininger MW, Pirmohamed M, Wang L, Clark RE. hOCT 1 and resistance to imatinib. Blood. 2005;106:1133–1134. doi: 10.1182/blood-2005-02-0694. author reply 1134. [DOI] [PubMed] [Google Scholar]
- 42.White DL, Saunders VA, Dang P, et al. OCT-1-mediated influx is a key determinant of the intracellular uptake of imatinib but not nilotinib (AMN107): reduced OCT-1 activity is the cause of low in vitro sensitivity to imatinib. Blood. 2006;108:697–704. doi: 10.1182/blood-2005-11-4687. [DOI] [PubMed] [Google Scholar]
- 43.Wendel HG, de Stanchina E, Cepero E, et al. Loss of p53 impedes the antileukemic response to BCR-ABL inhibition. Proc Natl Acad Sci USA. 2006;103:7444–7449. doi: 10.1073/pnas.0602402103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lionberger JM, Wilson MB, Smithgall TE. Transformation of myeloid leukemia cells to cytokine independence by Bcr-Abl is suppressed by kinase-defective Hck. J Biol Chem. 2000;275:18581–18585. doi: 10.1074/jbc.C000126200. [DOI] [PubMed] [Google Scholar]
- 45.Donato NJ, Wu JY, Stapley J, et al. BCR-ABL independence and LYN kinase overexpression in chronic myelogenous leukemia cells selected for resistance to STI571. Blood. 2003;101:690–698. doi: 10.1182/blood.V101.2.690. [DOI] [PubMed] [Google Scholar]
- 46.Donato NJ, Wu JY, Stapley J, et al. Imatinib mesylate resistance through BCR-ABL independence in chronic myelogenous leukemia. Cancer Res. 2004;64:672–677. doi: 10.1158/0008-5472.can-03-1484. [DOI] [PubMed] [Google Scholar]
- 47.Dai Y, Rahmani M, Corey SJ, Dent P, Grant S. A Bcr/Abl-independent, Lyn-dependent form of imatinib mesylate (STI-571) resistance is associated with altered expression of Bcl-2. J Biol Chem. 2004;279:34227–34239. doi: 10.1074/jbc.M402290200. [DOI] [PubMed] [Google Scholar]
- 48.Lombardo LJ, Lee FY, Chen P, et al. Discovery of N-(2-chloro-6-methyl- phenyl)- 2-(6-(4-(2-hydroxyethyl)-pipera-zin-1-yl)- 2-methylpyrimidin-4- ylamino)thiazole-5-carboxa-mide (BMS-354825), a dual Src/Abl kinase inhibitor with potent antitumor activity in preclinical assays. J Med Chem. 2004;47:6658–6661. doi: 10.1021/jm049486a. [DOI] [PubMed] [Google Scholar]
- 49.Tokarski JS, Newitt JA, Chang CY, et al. The structure of Dasatinib (BMS-354825) bound to activated ABL kinase domain elucidates its inhibitory activity against imatinib-resistant ABL mutants. Cancer Res. 2006;66:5790–5797. doi: 10.1158/0008-5472.CAN-05-4187. [DOI] [PubMed] [Google Scholar]
- 50.Shah NP, Tran C, Lee FY, Chen P, Norris D, Sawyers CL. Overriding imatinib resistance with a novel ABL kinase inhibitor. Science. 2004;305:399–401. doi: 10.1126/science.1099480. [DOI] [PubMed] [Google Scholar]
- 51.O’Hare T, Walters DK, Stoffregen EP, et al. In vitro activity of Bcr-Abl inhibitors AMN107 and BMS-354825 against clinically relevant imatinib-resistant Abl kinase domain mutants. Cancer Res. 2005;65:4500–4505. doi: 10.1158/0008-5472.CAN-05-0259. [DOI] [PubMed] [Google Scholar]
- 52.Lee FY, Lombardo L, Camuso A, et al. BMS-354825 potently inhibits multiple selected oncogenic tyrosine kinases and possesses broad-spectrum antitumor activities in vitro and in vivo. Proc Am Assoc Cancer Res. 2005;46:159. (Abstract 675) [Google Scholar]
- 53.Schittenhelm MM, Shiraga S, Schroeder A, et al. Dasatinib (BMS-354825), a dual SRC/ABL kinase inhibitor, inhibits the kinase activity of wild-type, juxtamembrane, and activation loop mutant KIT isoforms associated with human malignancies. Cancer Res. 2006;66:473–481. doi: 10.1158/0008-5472.CAN-05-2050. [DOI] [PubMed] [Google Scholar]
- 54.Talpaz M, Shah NP, Kantarjian H, et al. Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med. 2006;354:2531–2541. doi: 10.1056/NEJMoa055229. [DOI] [PubMed] [Google Scholar]
- 55.Hochhaus A, Baccarani M, Deininger M, et al. Dasatinib induces durable cytogenetic responses in patients with chronic myelogenous leukemia in chronic phase with resistance or intolerance to imatinib. Leukemia. 2008;22:1200–1206. doi: 10.1038/leu.2008.84. [DOI] [PubMed] [Google Scholar]
- 56.Guilhot F, Apperley JF, Kim D-W, et al. Efficacy of dasatinib in patients with accelerated-phase chronic myelogenous leukemia with resistance or intolerance to imatinib: 2-year follow-up data from START-A (CA180-005) Blood. 2007;110:Abstract 470. [Google Scholar]
- 57.Cortes J, Kim DW, Raffoux E, et al. Efficacy and safety of dasatinib in imatinib-resistant or -intolerant patients with chronic myeloid leukemia in blast phase. Leukemia. 2008;22:2176–2183. doi: 10.1038/leu.2008.221. [DOI] [PubMed] [Google Scholar]
- 58.Kantarjian H, Pasquini R, Hamerschlak N, et al. Dasatinib or high-dose imatinib for chronic-phase chronic myeloid leukemia after failure of first-line imatinib: a randomized phase 2 trial. Blood. 2007;109:5143–5150. doi: 10.1182/blood-2006-11-056028. [DOI] [PubMed] [Google Scholar]
- 59.Shah NP, Kantarjian HM, Kim DW, et al. Intermittent target inhibition with dasatinib 100 mg once daily preserves efficacy and improves tolerability in imatinib-resistant and -intolerant chronic-phase chronic myeloid leukemia. J Clin Oncol. 2008;26:3204–3212. doi: 10.1200/JCO.2007.14.9260. [DOI] [PubMed] [Google Scholar]
- 60.Shah NP, Kasap C, Weier C, et al. Transient potent BCR-ABL inhibition is sufficient to commit chronic myeloid leukemia cells irreversibly to apoptosis. Cancer Cell. 2008;14:485–493. doi: 10.1016/j.ccr.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 61.Quintas-Cardama A, Kantarjian HM, Nicaise C, et al. Cytopenias in patients (pts) with chronic myelogenous leukemia (CML) in chronic phase (CP) treated with dasatinib (SPRYCEL(R)): clinical features and management, including outcome after hematopoietic growth factor therapy. Blood. 2006;108:Abstract 2163. [Google Scholar]
- 62.Quintas-Cardama A, Kantarjian H, O’Brien S, et al. Pleural effusion in patients with chronic myelogenous leukemia treated with dasatinib after imatinib failure. J Clin Oncol. 2007;25:3908–3914. doi: 10.1200/JCO.2007.12.0329. [DOI] [PubMed] [Google Scholar]
- 63.Heuchel R, Berg A, Tallquist M, et al. Platelet-derived growth factor beta receptor regulates interstitial fluid home-ostasis through phosphatidylinositol–3′ kinase signaling. Proc Natl Acad Sci USA. 1999;96:11410–11415. doi: 10.1073/pnas.96.20.11410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Quintas-Cardama A, Kantarjian H, Ravandi F, Burger J, Borthakur G, Cortes J. Bleeding diathesis in patients (pts) with chronic myelogenous leukemia receiving dasatinib therapy. Blood. 2007;110:Abstract 2958. [Google Scholar]
- 65.Quintas-Cardama A, Han X, Kantarjian H, Cortes J. Dasatinib-induced platelet dysfunction. Blood. 2007;110:Abstract 2941. doi: 10.1182/blood-2008-09-180604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Weisberg E, Manley PW, Breitenstein W, et al. Characterization of AMN107, a selective inhibitor of native and mutant Bcr-Abl. Cancer Cell. 2005;7:129–141. doi: 10.1016/j.ccr.2005.01.007. [DOI] [PubMed] [Google Scholar]
- 67.Manley PW, Mestan J, Cowan-Jacob S, et al. AMN107: Inhibitory profile against non-mutated and mutated forms of the Bcr-Abl tyrosine kinase. Proc Am Assoc Cancer Res. 2005;46:1408. (Abstract 5985) [Google Scholar]
- 68.Kantarjian H, Giles F, Wunderle L, et al. Nilotinib in imatinib-resistant CML and Philadelphia chromosome-positive ALL. N Engl J Med. 2006;354:2542–2551. doi: 10.1056/NEJMoa055104. [DOI] [PubMed] [Google Scholar]
- 69.Kantarjian HM, Hochhaus A, Cortes J, et al. Nilotinib is highly active and safe in chronic phase chronic myelogenous leukemia (CML-CP) patients with imatinib-resistance or intolerance. Blood. 2007;110:Abstract 735. [Google Scholar]
- 70.Kantarjian HM, Giles F, Bhalla KN, et al. Nilotinib in chronic myeloid leukemia patients in chronic phase (CMLCP) with imatinib resistance or intolerance: 2-year follow-up results of a phase 2 study. Blood. 2008;112:Abstract 3238. [Google Scholar]
- 71.le Coutre PD, Giles F, Hochhaus A, et al. Nilotinib in chronic myeloid leukemia patients in accelerated phase (CML-AP) with imatinib resistance or intolerance: 2-year follow-up results of a phase 2 study. Blood. 2008;112:Abstract 3229. [Google Scholar]
- 72.Giles FJ, Larson RA, Kantarjian HM, et al. Nilotinib in patients (pts) with Philadelphia chromosome-positive (Ph+) chronic myelogenous leukemia in blast crisis (CML-BC) who are resistant or intolerant to imatinib. Blood. 2007;110:Abstract 1025. [Google Scholar]
- 73.Ottmann OG, Larson RA, Kantarjian HM, et al. Nilotinib in patients (pts) with relapsed/refractory Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ALL) who are resistant or intolerant to imatinib. Blood. 2007;110:Abstract 2815. [Google Scholar]
- 74.Singer JB, Shou Y, Giles F, et al. UGT1A1 promoter polymorphism increases risk of nilotinib-induced hyperbilirubinemia. Leukemia. 2007;21:2311–2315. doi: 10.1038/sj.leu.2404827. [DOI] [PubMed] [Google Scholar]
- 75.Quintas-Cardama A. Experimental non-ATP-competitive therapies for chronic myelogenous leukemia. Leukemia. 2008;22:932–940. doi: 10.1038/leu.2008.47. [DOI] [PubMed] [Google Scholar]
- 76.Quintas-Cardama A, Cortes J. Therapeutic options against BCR-ABL1 T315I-positive chronic myelogenous leukemia. Clin Cancer Res. 2008;14:4392–4399. doi: 10.1158/1078-0432.CCR-08-0117. [DOI] [PubMed] [Google Scholar]
- 77.Puttini M, Coluccia AM, Boschelli F, et al. In vitro and in vivo activity of SKI-606, a novel Src-Abl inhibitor, against imatinib-resistant Bcr-Abl+ neoplastic cells. Cancer Res. 2006;66:11314–11322. doi: 10.1158/0008-5472.CAN-06-1199. [DOI] [PubMed] [Google Scholar]
- 78.Cortes J, Kantarjian HM, Kim D-W, et al. Efficacy and safety of bosutinib (SKI-606) in patients with chronic phase (CP) Ph+ chronic myelogenous leukemia (CML) with resistance or intolerance to imatinib. Blood. 2008;112:Abstract 1098. doi: 10.1182/blood-2011-05-355594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Passerini CG, Pogliani EM, Baccarani M, et al. Bosutinib (SKI-606) demonstrates clinical activity and is well tolerated in patients with AP and BP CML and Ph+ ALL. Blood. 2008;112:Abstract 1101. [Google Scholar]
- 80.Redaelli S, Piazza R, Rostagno R, et al. Activity of bosutinib, dasatinib, and nilotinib against 18 imatinib-resistant BCR/ABL mutants. J Clin Oncol. 2009;27:469–471. doi: 10.1200/JCO.2008.19.8853. [DOI] [PubMed] [Google Scholar]
- 81.Kimura S, Naito H, Segawa H, et al. NS-187, a potent and selective dual Bcr-Abl/Lyn tyrosine kinase inhibitor, is a novel agent for imatinib-resistant leukemia. Blood. 2005;106:3948–3954. doi: 10.1182/blood-2005-06-2209. [DOI] [PubMed] [Google Scholar]
- 82.Yokota A, Kimura S, Masuda S, et al. INNO-406, a novel BCR-ABL/Lyn dual tyrosine kinase inhibitor, suppresses the growth of Ph+ leukemia cells in the central nervous system, and cyclosporine A augments its in vivo activity. Blood. 2007;109:306–314. doi: 10.1182/blood-2006-03-013250. [DOI] [PubMed] [Google Scholar]
- 83.Kantarjian HM, Cortes J, le Coutre P, et al. A phase I study of INNO-406 in patients with advanced Philadelphia (Ph+) chromosome-positive leukemias who are resistant or intolerant to imatinib and second generation tyrosine kinase inhibitors. Blood. 2007;110:Abstract 469. [Google Scholar]
- 84.Carmena M, Earnshaw WC. The cellular geography of aurora kinases. Nat Rev Mol Cell Biol. 2003;4:842–854. doi: 10.1038/nrm1245. [DOI] [PubMed] [Google Scholar]
- 85.Katayama H, Brinkley WR, Sen S. The aurora kinases: role in cell transformation and tumorigenesis. Cancer Metastasis Rev. 2003;22:451–464. doi: 10.1023/a:1023789416385. [DOI] [PubMed] [Google Scholar]
- 86.Giles FJ, Cortes J, Jones D, Bergstrom D, Kantarjian H, Freedman SJ. MK-0457, a novel kinase inhibitor, is active in patients with chronic myeloid leukemia or acute lymphocytic leukemia with the T315I BCR-ABL mutation. Blood. 2007;109:500–502. doi: 10.1182/blood-2006-05-025049. [DOI] [PubMed] [Google Scholar]
- 87.Giles F, Cortes J, Bergstrom DA, et al. MK-0457, a novel aurora kinase and BCR-ABL inhibitor, is active against BCR-ABL T315I mutant chronic myelogenous leukemia (CML) Blood. 2006;108:Abstract 163. [Google Scholar]
- 88.Shah NP, Kasap C, Paquette R, et al. Targeting drug-resistant CML and Ph+-ALL with the spectrum selective protein kinase inhibitor XL228. Blood. 2007;110:Abstract 474. [Google Scholar]
- 89.Gontarewicz A, Balabanov S, Keller G, et al. Simultaneous targeting of aurora kinases and Bcr-Abl kinase by the small molecule inhibitor PHA-739358 is effective against imatinib-resistant BCR-ABL mutations including T315I. Blood. 2008;111:4355–4364. doi: 10.1182/blood-2007-09-113175. [DOI] [PubMed] [Google Scholar]
- 90.Cortes J, Paquette R, Talpaz M, et al. Preliminary clinical activity in a phase I trial of the BCR-ABL/IGF- 1R/aurora kinase inhibitor XL228 in patients with Ph++ leukemias with either failure to multiple TKI therapies or with T315I mutation. Blood. 2008;112:Abstract 3232. [Google Scholar]
- 91.Paquette RL, Shah NP, Sawyers CL, et al. PHA-739358, an aurora kinase inhibitor, induces clinical responses in chronic myeloid leukemia harboring T315I mutations of BCR-ABL. Blood. 2007;110:Abstract 1030. [Google Scholar]
- 92.Balabanov S, Gontarewicz A, Keller G, et al. Combination therapy of small molecule inhibitor PHA-739358 and tyrosine kinase inhibitor imatinib yields synergistic anti-proliferative effects and suppresses emergence of resistance of chronic myeloid leukemia in vitro. Blood. 2008;112:Abstract 3227. [Google Scholar]
- 93.Grem JL, Cheson BD, King SA, Leyland-Jones B, Suffness M. Cephalotaxine esters: antileukemic advance or therapeutic failure? J Natl Cancer Inst. 1988;80:1095–1103. doi: 10.1093/jnci/80.14.1095. [DOI] [PubMed] [Google Scholar]
- 94.Cephalotaxine esters in the treatment of acute leukemia. A preliminary clinical assessment. Chin Med J (Engl) 1976;2:263–272. [PubMed] [Google Scholar]
- 95.Harringtonine in Acute Leukemias. Clinical analysis of 31 cases. Chin Med J (Engl) 1977;3:319–324. [PubMed] [Google Scholar]
- 96.O’Brien S, Kantarjian H, Keating M, et al. Homoharringtonine therapy induces responses in patients with chronic myelogenous leukemia in late chronic phase. Blood. 1995;86:3322–3326. [PubMed] [Google Scholar]
- 97.Tang R, Faussat AM, Majdak P, et al. Semisynthetic homoharringtonine induces apoptosis via inhibition of protein synthesis and triggers rapid myeloid cell leukemia-1 down-regulation in myeloid leukemia cells. Mol Cancer Ther. 2006;5:723–731. doi: 10.1158/1535-7163.MCT-05-0164. [DOI] [PubMed] [Google Scholar]
- 98.Quintas-Cardama A, Kantarjian H, Garcia-Manero G, et al. Phase I/II study of subcutaneous homoharringtonine in patients with chronic myeloid leukemia who have failed prior therapy. Cancer. 2007;109:248–255. doi: 10.1002/cncr.22398. [DOI] [PubMed] [Google Scholar]
- 99.Robin J-P, Dhai R, Dujardin G, Girodier L, Mevellec L, Poutot S. The first semi-synthesis of enantiopure homo-harringtonine via anhydrohomoharringtonine from a pre-formed chiral acyl moiety. Tetrahedron Lett. 1999;40:2931–2934. [Google Scholar]
- 100.Cortes J, Khoury HJ, Corm S, et al. Safety and efficacy of subcutaneous (SC) omacetaxine mepesuccinate in imatinib(IM)-resistant chronic myeloid leukemia (CML) patients (pts) with the T315I mutation – results of an ongoing multicenter phase II study. Blood. 2008;112:Abstract 3239. [Google Scholar]