Abstract
Back pain in the pediatric population is a common complaint presenting to sports medicine clinic. There is a wide differential that should be considered, including mechanical, infectious, neoplastic, inflammatory, and amplified musculoskeletal pain. The history, pain quality, and examination are key components to help distinguish the etiologies of the pain and direct further evaluation. Laboratory investigations, including blood counts and inflammatory markers, can provide insight into the diagnosis. The HLA-B27 antigen can be helpful if a spondyloarthropathy is suspected. Imaging as clinically indicated typically begins with radiographs, and the use of MRI, CT, or bone scan can provide additional information. Proper diagnosis of back pain is important because prognosis and treatments are significantly different. This paper will review the pertinent evaluation, differential diagnoses, and treatment of low back pain in the pediatric population.
Keywords: back pain, pyogenic sacroiliitis, chronic recurrent multifocal osteomyelitis, spondyloarthropathy, amplified musculoskeletal pain, youth
INTRODUCTION
Low back pain is the most common type of back pain, often begins in childhood, has high recurrence, and can return more intense than previously.1 Low back pain is limited to the regions below the lower margins of the 12th rib and the gluteal fold2 and occurs in 60–80% of people during their lifetime.3 Prevalence ranges widely from 9% to 66% in the pediatric population depending on the source population and definition of pain.1 Similarly, back pain occurs in 10–25% of athletes and is more common in football players and gymnasts.4 Prevalence of back pain in children increases with age and is more common in females.1
There are many etiologies of low back pain in the pediatric population. The majority of children with low back pain presenting to the sports medicine clinic have an underlying musculoskeletal or biomechanical cause;5 however, additional causes including an infectious, oncologic, or rheumatologic etiology should be considered. This paper will review the pertinent evaluation, differential diagnoses, and treatment of low back pain in the pediatric population.
HISTORY
A through history is important to help inform the workup of pediatric low back pain. Knowing the sport and position, degree of conditioning, training regimen, any associated mechanism of injury, and description of pain should be obtained during the history.6 Acute onset pain is often indicative of trauma or infection while insidious onset pain may herald an inflammatory etiology or longstanding altered biomechanics.6 Non-localizable back pain is often secondary to muscular or inflammatory etiologies while focal back pain may indicate a stress fracture or bony lesion. Sharp or burning pain is characteristic of a neurologic etiology. Inflammatory back pain is defined in adults as lower back pain that starts insidiously, improves with exercise, is associated with more than 30 minutes of morning stiffness, and alternating buttock pain.7, 8 Findings that should trigger a more in-depth investigation include fever, weight loss, nighttime pain or pain that awakens the child from sleep, neurologic deficits, worsening pain over time, or inflammatory back pain.6 Appropriate evaluation of back pain starts with a thorough history and physical exam.9
EVALUATION
Survey instruments such as the Modified Oswestry Low Back Pain Disability Questionnaire and the Roland Morris Disability Questionnaire have been validated to evaluate adult low back pain and the Micheli Functional Scale is validated to evaluate low back pain in pediatric athletes.10 Examination of the lower back includes palpation of bony landmarks such as the spinous and transverse processes, paraspinal muscles, iliac crests, and sacroiliac joints.6 Evaluation of range of motion includes back flexion and extension, lateral bending, rotation, and symmetric movement of the sacroiliac joints. Loss of the normal lumbar lordosis during forward flexion is abnormal and suggests a spondyloarthropathy.11 A positive stork test, which is low back pain with a one-legged stance during hyperextension, or pain at L4-L5 with hyperextension may indicate spondylolysis or spondylolisthesis.6 A positive Trendelenburg, which is downward pelvic tilt to the unaffected side with single-leg stance, indicates weak core muscles12 or neurologic deficit that can be seen be seen in a variety of conditions as discussed in sections below. To perform a modified Schober test, the Dimples of Venus are identified while standing and marks are made at 10 cm proximal and 5 cm distal; the marks are re-measured after the patient forward flexes with knees extended.11 A modified Schober less than 21 cm suggests restriction of lumbar flexion and can be indicative of a spondyloarthropathy13 or altered biomechanics including tight hamstrings.14 Back pain with the hip placed in flexion, abduction, and external rotation (FABER) or pain with Gaenslen maneuver can also suggest sacroiliac joint pathology.15 Relevant neurologic testing includes muscle strength, reflexes, straight leg raise, and gait evaluation.6 It is also important to evaluate the hip, including hip hyperextension and hamstring tightness, as these can cause referred pain to the back.6
Imaging usually starts with radiographs, which can identify fractures, spondylolysis, spondylolisthesis, Scheuermann disease, and some bony lesions. The use of diagnostic radiographs is controversial and there is no universal imaging screening protocol.16, 17 Some authors recommend radiographic imaging routinely after three months of non-traumatic back pain and then proceeding to bone scan or MRI only if suspicion of pathology remains highbased on the history and physical exam.9 Others recommend every patient have diagnostic radiographs after trauma.6 Recent literature shows there is no difference in the sensitivity and specificity between the two-view anteroposterior and lateral views and the four-view anteroposterior, lateral, right, and left oblique views, and thus only two views should be obtained for evaluation of spondylolysis,18 but this is not a universally accepted practice and needs further investigation. One case series in pediatric patients without constitutional symptoms or night pain reports that a combined hyperextension test and radiograph has a negative predictive value of 0.81 and sensitivity of 0.90, and addition of bone scan has excellent negative predictive value and sensitivity if pain is less than 6 weeks duration.17 Many algorithms for additional workup have been suggested, but there is not a universally accepted protocol outside of a through history and physical exam.17
Magnetic resonance imaging (MRI) is a useful modality to evaluate soft tissues, joint inflammation, and detailed anatomy without radiation. MRI is necessary to detect early sacroiliitis in juvenile arthritis and has detected abnormalities in 60% of cases whereas radiographs only show long-standing and permanent damage.19 Computed tomography (CT) is fast to obtain and is thus a preferred modality for emergency room evaluations. CT provides detailed bony anatomy but is not as good as MRI for soft tissue pathology and has significant radiation exposure. Children less than 8 years often require sedation for MRI but not for CT. Bone scan is helpful to perform a full body evaluation, particularly when multiple sites of pathology are suspected. Bone scan also involves radiation, and sites of inflammation near the open physis can be difficult to interpret in a child and may require additional imaging.
Laboratory evaluation is useful in a patient with inflammatory back pain or other red flags on history or examination and includes a complete blood count, sedimentation rate, C-reactive protein, blood culture, and testing for sexually transmitted infections (STI). Lactic dehydrogenase and uric acid are helpful if malignancy is suspected. A complete metabolic panel including albumin and liver function tests should be checked if inflammatory bowel disease (IBD) is suspected. The HLA-B27 antigen is positive in approximately 10% of Caucasians, of which approximately 3% will have a spondyloarthropathy;20 this test should only be obtained if there is a high suspicion for a spondyloarthropathy.
DIFFERENTIAL DIAGNOSIS
Keeping a broad differential diagnosis is important when evaluating low back pain. One case series shows the majority (88%) of back pain presenting to an emergency department is acute in onset with direct trauma, muscle strain, idiopathic, urinary tract infection, and viral syndrome as common etiologies.21 However, another case series shows that half of pediatric patients evaluated in orthopedic clinic for back pain had serious underlying spinal pathology. In this case series the most common diagnoses were osteomyelitis, discitis, spondylolisthesis, Scheuermann disease, and tumors.22
MECHANICAL CAUSES
Spondylolysis is a unilateral fracture of the pars interarticularis and commonly results from back hyperextension and can be seen in up to 47% of athletes presenting with back pain.23 It is most prevalent in athletes who participate in football, gymnastics, swimming, and diving.24 Spondylolysis can also occur in congenital spinal abnormalities25, 26 presenting with gradual rather than acute onset pain.26 Spondylolisthesis is a bilateral fracture of the pars interarticularis with anterior displacement of the vertebral body or sacrum. These patients have pain with back hyperextension and may have neurologic findings if spondylolisthesis is present. Imaging starts with radiographs. If radiographs are normal and clinical suspicion is high, MRI, CT, or bone scan should be obtained as they have greater sensitivity. Treatment includes rest and a formal course of physical therapy focusing on core strength. More than 80% heal within a year and the use of bracing is not likely to influence healing.27 Surgical intervention is rarely indicated.
Scheuermann disease presents in late childhood and early adolescence and is characterized by increasing thoracic or thoracolumbar kyphosis with tightness of the hamstrings and iliopsoas.28 Diagnosis is made when radiographs demonstrate anterior wedging more than 5 degrees of three or more consecutive vertebrae.28 Treatment includes physical therapy with a focus on hamstring stretching. Additional considerations include bracing but might not provide long-term benefits.28 Severe cases may require surgical treatment.28
Sacroiliac dysfunction can be seen after mild trauma and is caused by altered biomechanics that normally allow the ilium to glide backwards and downward during hip flexion.29, 30 This is best detected on physical exam with unequal movement of the pelvis with forward flexion, leg length discrepancy, radicular pain, and focal sacroiliac tenderness,30 but no specific test has been validated to clearly establish this diagnosis.31 Treatment includes realignment of the sacroiliac joint with physical therapy and strengthening exercises.30
Mechanical causes of low back pain include tight hamstrings and paraspinal muscle spasm,6 but the associations between decreased mobility and pain are controversial.32 These are associated with poor posture and heavy backpack load.33 Hamstring tightness is associated with stiffness but not usually pain.34 The diagnosis is made by physical examination and treatment can focus on correcting biomechanical deficits and decreasing the backpack weight.
Apophysitis, or growth plate irritation from chronic repetitive stress, is pain localized to the iliac crests or ischial tuberosity. This entity is particularly common in the adolescent population.5 Radiographs show widening of the physis and sometimes an associated fracture. Initial evaluation includes radiographs. Additional workup includes MRI if clinical suspicion is high or if further characterization of the involved physis is warranted.35 Treatment includes rest and non-weight bearing until the physis widening and pain have resolved.
INFECTIOUS CAUSES
There are many structures in the low back that are susceptible to infection, including the vertebrae, the fibrocartilagenous disc, and the sacroiliac joints.
Mycobacterium tuberculosis causing spinal tuberculosis (“Potts disease”) can involve the bony vertebral bodies but may also involve the spinal cord, disc, and surrounding tissues and is thought to spread hematogenously. It most commonly involves the lower thoracic and lumbar spine in children.36 It can be difficult to diagnose unless there is a high index of suspicion. Recent travel or immigration from an area with high tuberculosis prevalence, or personal or family history of tuberculosis should raise suspicion.36 It often presents with neurologic symptoms, back pain, and fever.36 Imaging may demonstrate bone destruction of the involved vertebra or sacrum; there may also be accompanying abscess formation extending into the epidural space or surrounding soft tissue (Figure 1A and 1B). Optimum treatment is controversial but involves antibiotics and possible surgery.36
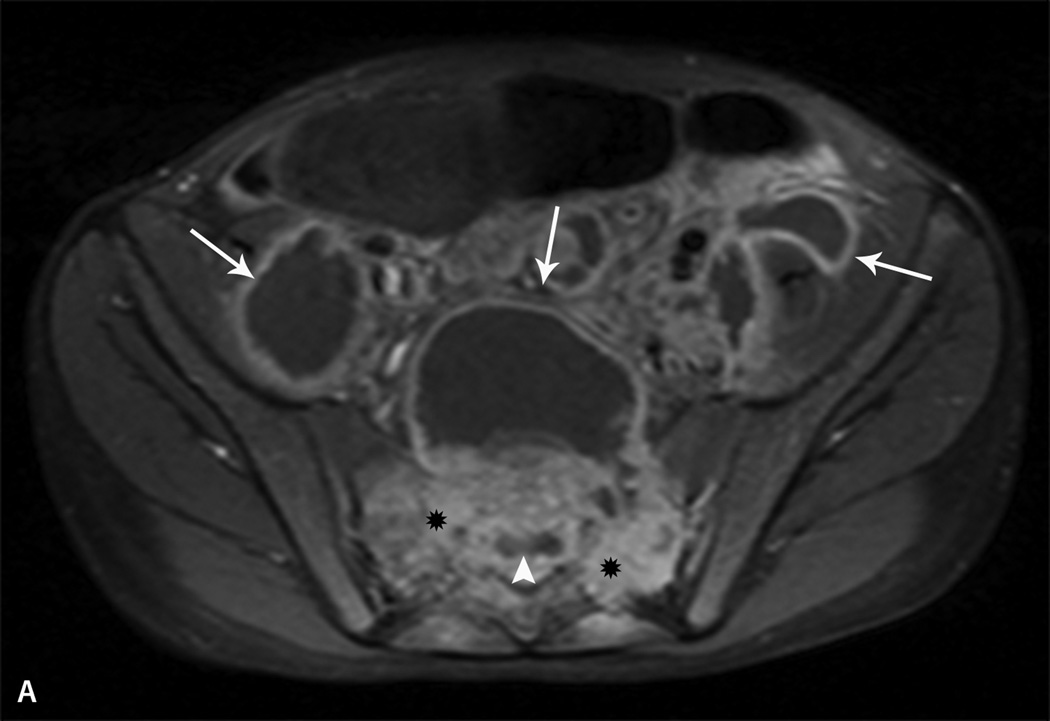
Figure 1.
Tuberculosis. Axial (A) and sagittal (B) T1 fat-saturated post contrast images of the sacrum in a 10 year-old boy with lower back and abdominal pain demonstrate a large region of abnormal bone marrow enhancement (*) with bone destruction within the sacrum consistent with osteomyelitis. There is a large, multiseptated presacral abscess extending into the paraspinal and pelvic muscles (arrows) as well as an associated epidural abscess (arrowheads).
Pyogenic sacroiliitis is more common in adolescents than young children37 and accounts for 1–2% of pediatric joint infections.38 One case series suggests pyogenic sacroiliitis accounts for 2.5/10,000 admissions a pediatric institution and the incidence is increasing.39 Predisposing factors include history of trauma, break in skin integrity, severe atopic dermatitis, acne38, 40 and intravenous drug use. Patients may have limp, and back pain that worsens with hip flexion, abduction, and external rotation (FABER position). They may have a positive straight leg raise, decreased hip range of motion, abdominal, hip or buttock pain. Only 40% have fever at presentation. Most children, but not all, seek care within a week of symptom onset38, 40 and 82% will have normal radiographs at presentation.41 In adults, the diagnosis is often delayed by an average of 43 days and 40% of affected individuals have normal radiographs at presentation.42 MRI is preferred over plain films or bone scan as it demonstrates joint effusions, marrow changes, abscess formation, as well as the extent of soft tissue involvement.38 The arthritis characteristically involves the lower one-half to one-third of the joint and is unilateral.40 Thirty percent of adults develop an associated psoas abscess42. White blood cell count may be normal but inflammatory markers are typically elevated.38, 40 Staphylococcus aureus, including methicillin resistant Staphylococcus aureus, is the most common organism in children. The infection responds well to a course of antibiotics and rest.38, 40
Spondylodiscitis, or inflammation of the intervertebral disc space or end-plate, is seen in all ages and is usually preceded by an illness within the past month.43 One author reports 12 cases of spondylodiscitis out of 520 pediatric patients with back pain.44 It typically affects the thoracic and lumbar discs, and L5-S1 is the most commonly affected level.43 Symptoms are often non-specific and include fatigue, irritability, limp, or refusal to sit or walk. Most children lack localizing symptoms and fever.45 Tenderness to palpation is infrequent. Leukocytosis is usually absent and inflammatory markers are elevated.43 Staphylococcus and Streptococcus species are the most commonly isolated bacteria, but the majority of blood cultures are negative. Radiographs demonstrate disc space narrowing after two to four weeks but can also be normal.45, 46 MRI shows irregularities and destruction of the end plates47 and is also useful for the evaluation of the spinal canal contents and for epidural abscesses. Bone scans are helpful to localize pathology but often need to be followed by additional imaging.43 Most cases are self-limited and resolve without antibiotics but not treating with antibiotics is controversial.43, 46 Bracing reduces pain and allows healing. It is important to continue to follow these children as long-term studies show decreased spine motion and fusion years after diagnosis that usually does not result in functional deficits.43, 48
BONY AND SPINAL NEOPLASMS
Vertebral and spinal neoplasms are rare in children and typically present with persistent and localized back pain that is worse at night.49 Benign neoplasms include osteoid osteoma, osteoblastoma, and aneurismal bone cyst. Malignancies include Ewing’s sarcoma, lymphoma, neuroblastoma, Langerhans cell histiocytosis, and metastatic disease.49
Osteoid osteomas and osteoblastomas usually present in long bones but can present in the spine in 10–20% of cases.50 Osteoid osteomas are characteristically less than 2 cm while osteoblastomas are typically larger than 2 cm. While non-steroidal anti-inflammatory drugs (NSAIDs) can alleviate the pain,51 definitive treatment is radiofrequency ablation or surgical resection to remove the nidus.52 Osteoblastomas may become malignant.51 CT is the preferred imaging modality to help characterize the lesions and to look for the bony nidus. MRI can also demonstrate an inflammatory response and may be useful to differentiate these lesions from other malignancies.51
Langerhans cell histiocytosis (LCH) is an eosinophilic granuloma that can affect the vertebral body53 and spinal disease accounts for 6–25% of all LCH cases.54 Common symptoms include focal and dull back pain that steadily increases over time, decreased flexibility, radiculopathy, and back stiffness.53 The underlying etiology is unknown. Open or needle biopsy is often necessary for diagnosis. These lytic lesions have high risk of vertebral collapse and are often initially discovered on radiographs but are best visualized on MRI or CT (Figure 2A and 2B).53 When disease is severe or involves extraskeletal manifestations, methotrexate, prednisone, vinblastine, and radiation are therapeutic options.55
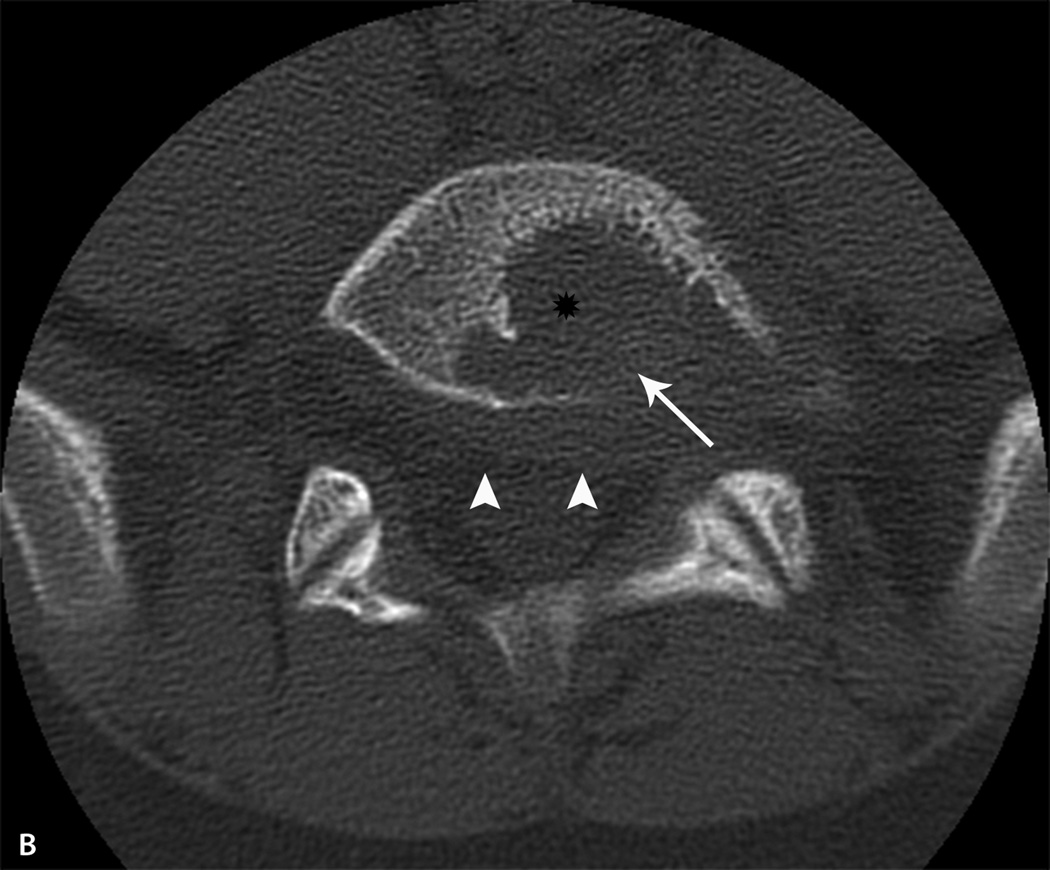
Fig. 2.
Langerhans Cell Histiocytosis. A. Sagittal fluid-sensitive MR image of the lumbar spine in a 12 yearold boy with back pain demonstrates edema within the L5 vertebral body (thick arrow) with bone destruction of the inferior aspect of the vertebra (thin arrow). B. Non-contrast CT axial image in bone algorithm shows a lytic lesion (*) with destruction of the cortex along the posterior aspect of the L5 vertebral body (arrow). There is abnormal soft tissue extending into the epidural space (arrowheads).
Lesions within the spinal cord account for 0.5–1% of all central nervous system neoplasms.56, 57 Glial tumors, including astrocytomas and ependymomas are the most common spinal tumors in children.56, 57 These occur at any age but are more common in late childhood and early adolescence.56, 57 Spinal cord tumors typically present with a long history of non-specific, waxing and waning symptoms that progress to motor weakness, gait alterations, or muscle rigidity.57 Pain is present in 25–60%, can be dull, achy, or sharp in quality.56, 57 It is therefore important to complete a through history and physical including a detailed neurologic exam. MRI is helpful to determine the extent of soft tissue involvement and may show characteristic scalloping of the vertebral body.57 Treatment is surgical.57
AUTOINFLAMMATORY AND AUTOIMMUNE CAUSES
Chronic recurrent multifocal osteomyelitis (CRMO) is a childhood autoinflammatory disease that is often confused with bacterial osteomyelitis; however unlike bacterial osteomyelitis, CRMO lesions are sterile and do not resolve with antibiotic therapy.58 The incidence and prevalence is unknown.59 Symptoms can be present for days to years before diagnosis.58 Contrary to bacterial osteomyelitis, CRMO does not have an associated abscess or fistula formation. The distribution of lesions is usually symmetric and involves sites not commonly seen with bacterial osteomyelitis such as the mandible, sternum, and clavicle.58 As the name suggests, these lesions are multifocal that can recur at the same or additional sites.60 29% of patients with CRMO have vertebral involvement.61 Spinal involvement indicates a high risk of vertebral collapse. Laboratory findings are nonspecific and include normal or slightly elevated inflammatory markers with normal cell counts.58 Very elevated inflammatory markers, anemia, and hypoalbuminemia should raise suspicion of co-existing inflammatory bowel disease (IBD). Radiographs are often the initial imaging study and reveal lytic lesions. Bone scan and whole body MRI are helpful to assess the full extent of lesions and to assess for vertebral involvement (Figure 3A and 3B).62–64 Biopsy is a key component to exclude infection and oncologic conditions that may be difficult to differentiate from CRMO by imaging alone.58 Treatment primarily consists of NSAIDs, such as naproxen and indomethacin, which are effective in up to 80% of cases.58 Although not FDA-approved for CRMO, the use of bisphosphonates may be helpful to prevent vertebral collapse and other complications.65 Additional therapies such as glucocorticoids, disease-modifying anti-rheumatic drugs (DMARDs), and biologics have been reported with varied success.58, 64 Physical therapy can improve range of motion, improve strength, and should be used alongside pharmacologic therapy.64
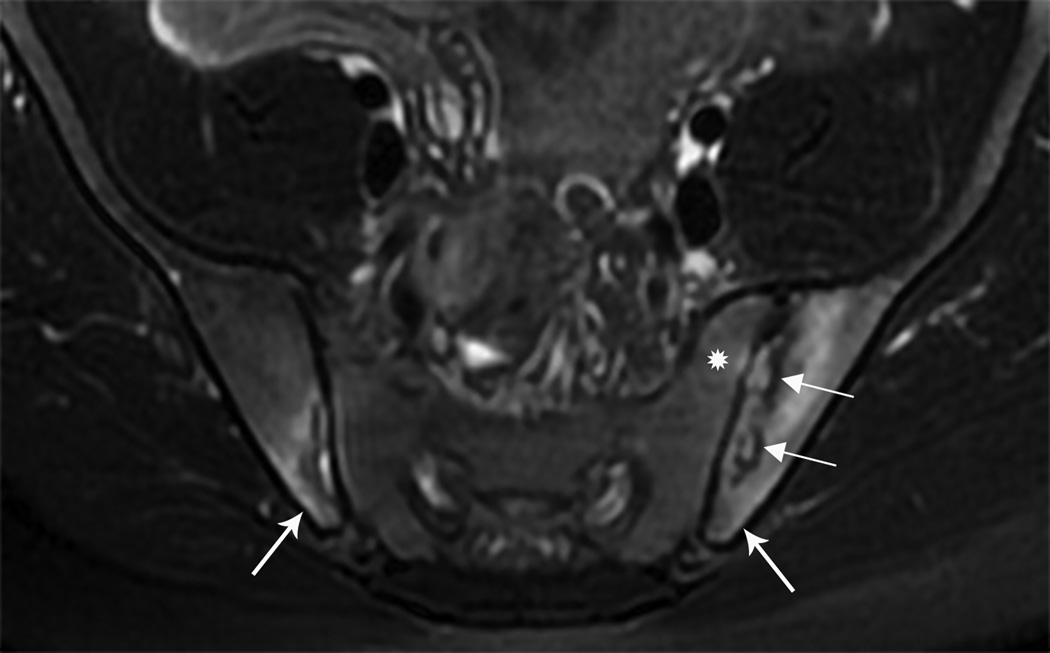
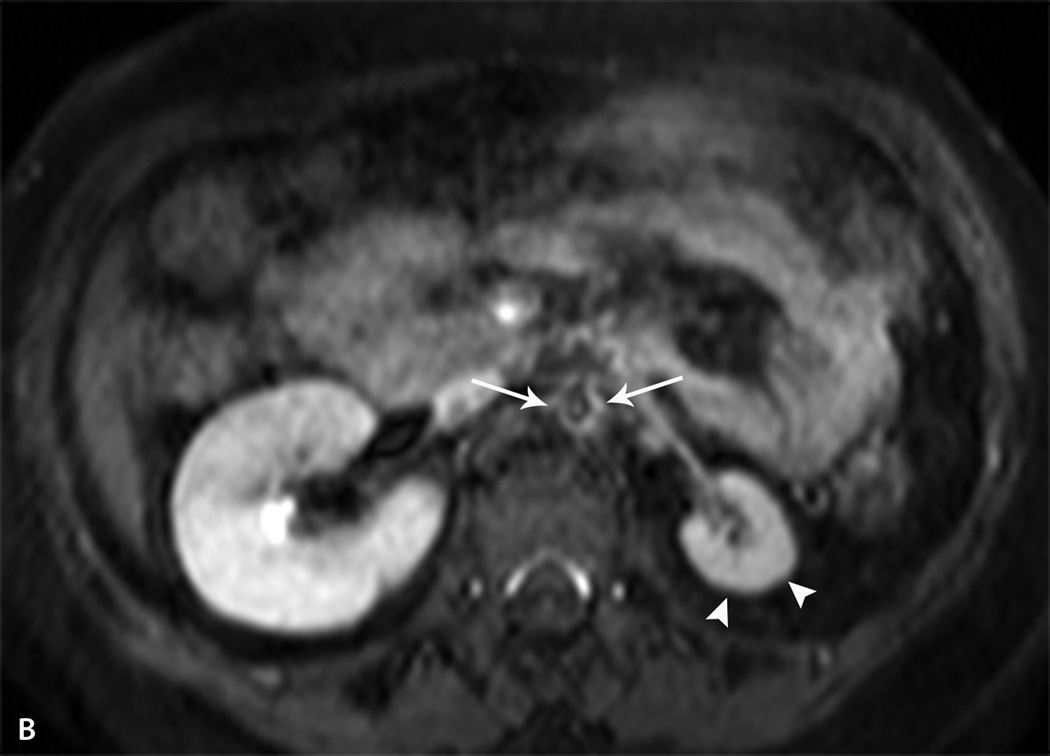
Fig. 3.
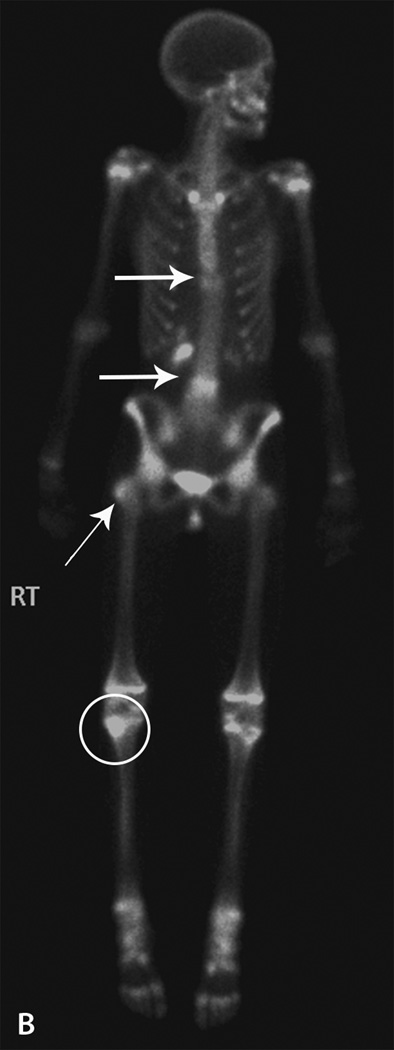
Chronic recurrent multifocal osteomyelitis. A. Sagittal fluid-sensitive MR image of the thoracolumbar spine in a 15 year-old girl with back pain demonstrates edema within the T10 and L4 vertebral bodies (thick arrows) with loss of vertebral body height. There is endplate irregularity of the T10 and L4 vertebral bodies with disc space narrowing above and below. Nuclear medicine bone scan was obtained to evaluate for additional lesions B. Tc -99m MDP 3- hour delayed whole body bone scan image in the anterior projection shows increased radiotracer activity within the T10 and L4 vertebral bodies. Abnormal radiotracer activity was also seen within the right greater trochanter (thin arrow) and within the right proximal tibia (circle) consistent with additional sites of inflammation. Normal, expected radiotracer activity is seen within the open physes.
SPONDYLOARTHROPATHIES
The spondyloarthropathies include reactive arthritis, enthesitis-related arthritis, psoriatic arthritis, and IBD-related arthritis. Although there are many similarities and all can present with sacroiliitis, there are many distinguishing features and identifying the underlying diagnosis can affect treatment.66 Common features of spondyloarthropathies include inflammatory low back pain, enthesitis, sacroiliitis, HLA-B27 positivity, and HLA-B27-related diseases in first-degree relatives.67
Reactive arthritis, formerly Reiter syndrome is characterized by painful asymmetric arthritis that occurs after enteropathoic or urogenital infections which include Yersinia, Salmonella, Shigella, Campylobacter, and Chlamydia trachomatis.68 The classic triad of arthritis, acute and symptomatic uveitis, and urethritis is uncommon is children. The typical onset is 2–4 weeks after diagnosis but it may also occur within days of the infection. The arthritis can involve the lower extremities as well as the sacroiliac joints. The course of arthritis is variable and may progress to a chronic spondyloarthropathy, including ankylosing spondylitis. Pertinent findings on examination may include erythema over affected joints, enthesitis, keratoderma blenorrhagicum, nail changes, circinate balanitis, and oral ulcers. Reactive arthritis is characteristically very painful and often raises suspicion for septic arthritis. Evaluation includes stool studies, STI testing, and imaging. If only 1 joint is affected, evaluation for septic arthritis is often required. Treatment includes NSAIDs such as indomethacin or naproxen; glucocorticoids are seldom required.
Enthesitis-related arthritis (ERA) is enthesitis plus arthritis and is a category of juvenile idiopathic arthritis (JIA). Approximately 60% are males, 45% are HLA-B27 positive,69 and most cases present during adolescence.70 The presence of enthesitis, or tenderness at the sites of tendon, ligament, or joint capsule insertions should raise suspicion of the diagnosis. Axial involvement may be characterized by pain, decreased forward flexion, loss of lumbar lordosis on forward flexion, and tenderness of the sacroiliac joints. However, children may not develop back pain until the disease has been present for many years.71 Approximately 35–45% of children with ERA have clinical or radiographic evidence of sacroiliitis.69, 72 Untreated sacroiliitis may progress to spondylitis which is a condition characterized by radiographic findings of squaring, erosions, syndesmophytes, diskitis, and ankylosis or fusion of the axial joints. Radiographs are not able to distinguish between acute and chronic disease and are typically normal at diagnosis.71 MRI without or without contrast is the preferred modality to evaluate for acute sacroiliitis;71 the most common finding is bone edema (Figure 4). NSAIDs may help reduce structural damage, new bone growth, and syndesmophyte formation, if used continuously. Biologics including anti-tumor necrosis factor agents such as etanercept and adalimumab can be helpful to improve symptoms and function.70 DMARDs such as methotrexate and sulfasalazine may be helpful for peripheral arthritis but have not been shown to improve axial disease in adults.
Fig. 4.
Enthesitis related arthritis. Axial fluid-sensitive MR image of a 16 year-old boy with lower back pain. Bone marrow edema is seen within the medial aspect of both iliac (thick arrows) and to a lesser extent, the left sacral ala (*). A small amount of fluid is seen within the right sacroiliac joint. There are erosive changes seen on the left (thin arrows). Follow-up laboratory studies revealed that the boy was HLA-B27 positive.
Psoriatic arthritis, like ERA, is a category of JIA and is characterized by the presence of arthritis and psoriasis.66, 73 ERA and psoriatic arthritis combined have a prevalence of 0.28–88 cases per 100,000 children.74 The diagnosis of arthritis can precede or follow the diagnosis of psoriasis.73 Nail pits, distal interphalangeal arthritis, and dactylitis (sausage digit) should raise suspicion of the diagnosis.73 10–30% of children with psoriatic arthritis have clinical or radiographic evidence of clinical or radiographic sacroiliitis.75–77 Spondylitis develops in as many as 20% of adults with psoriatic arthritis.78 As with ERA, treatment involves immunosuppressive medications including DMARDs and biologic agents.
Extraintestinal manifestations of IBD, including IBD-associated arthritis, are most common in ulcerative colitis but can also occur with Crohn’s disease.79 Arthritis may be the initial presenting symptom and arthritis affects 1/3 of patients.80 As many as 45% develop sacroiliitis.81 Although the link between IBD and sacroiliitis is well established, the mechanism of IBD-associated arthritis is unknown.80, 82 In addition to sacroiliitis, it is also common for patients with IBD to have asymmetrical arthritis in peripheral joints as well as enthesitis.82, 83 MRI is the preferred imaging modality as it can show acute inflammatory changes including effusions, synovitis, and subchondral marrow edema that are not visible on radiographs.79, 84 Axial arthritis typically improves once the underlying gut inflammation is controlled.79, 83 Biologic therapies, such as anti-tumor necrosis factor medications including infliximab and adalimumab, have been efficacious in the treatment of IBD; additionally, they may also address any additional underlying peripheral or axial arthritis. The use of NSAIDs is not recommended as these can precipitate a flare or worsening of IBD; however COX-2 inhibitors such as celecoxib may have a lower risk of flare in this population.79, 83 Physical therapy can be effective in increasing range of motion and flexibility.79, 83
VASCULITIS
Referred low back pain from vasculitis is rare but a very important diagnosis not to miss.
Vasculitis is systemic inflammation of blood vessels that can affect any size vessel and thus can affect multiple organs and have a variety of presentations.85 Takayasu arteritis, a large vessel vasculitis, presents in early adolescence, and is more common in females.85 It typically affects the aorta but also can affect other large vessels including renal, subclavian, and carotid arteries.86 When the mid-aorta is involved there may be referred back pain. It can be difficult to diagnose because symptoms are non-specific and include weight loss, back pain, abdominal pain, fever, claudication, and headache; hypertension is usually present and can be a key clue as to the presence of this vasculitis.86 Angiography is the gold standard, but MR-angiogram and CT imaging can also detect changes in vessel wall to assist with the diagnosis (Figure 5A and 5B.) Treatment typically includes a combination of immunosuppressants, glucocorticoids, anti-hypertensives, and anti-coagulants.
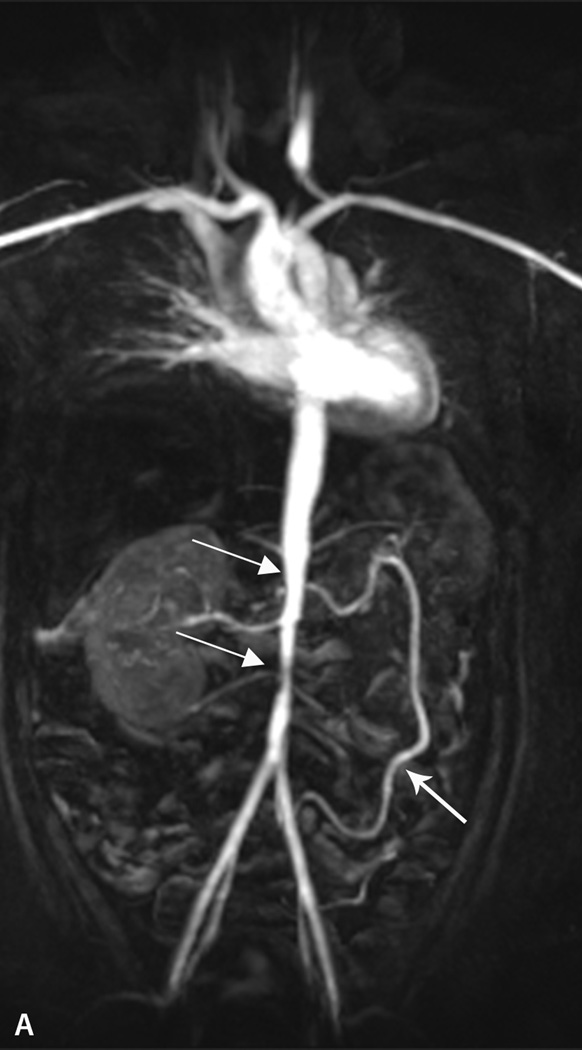
Fig. 5.
Takayasu arteritis. A. Coronal post contrast Maximum Intensity Projection (MIP) MR angiogram in the arterial phase of the chest, abdomen and pelvis in a 13 year-old girl demonstrates narrowing and irregularity of the mid to distal abdominal aorta (thin arrows). There is enlargement of the Arc of Rioland (thick arrow) due to severe stenosis of the celiac and superior mesenteric arteries (not shown). B. Axial post contrast T1 fat-saturated image shows severe narrowing of the abdominal aorta with a thick, enhancing wall (arrows). There is atrophy of the left kidney (arrowheads) due to severe stenosis of the left renal artery.
REFLEX NEUROVASCULAR DYSTROPHY
Reflex neurovascular dystrophy, also known as complex regional pain syndrome and amplified musculoskeletal pain, is a common condition in teenage females87 and frequently manifests as back pain. Musculoskeletal pain accounts for 4–40% of pediatric patients with chronic pain.88 Pain can be intermittent or constant, and can involve a single site, multiple sites, or the entire body. This condition is related to injury, illness, and psychological stress. Keys to diagnosis is the presence of allodynia, which is sensitivity to non-painful stimuli such as a breeze or light touch, la belle indifference regarding the pain and dysfunction caused by pain, and incongruent affect.87 These patients are usually high achievers in sports and school.87 Exam shows non-dermatomal allodynia and varying borders with repeated examination; skin can be cool to touch and discolored.87 Imaging is typically done during the workup to exclude other conditions but is not usually necessary; MRI can show disuse atrophy and bony demineralization, and bone scan can show increased activity.89 NSAIDs do not improve pain. Treatment should be multidisciplinary and include both psychological counseling, intense physical therapy focusing on desensitization of the painful areas combined with aerobic activity.87, 90
CONCLUSION
Pediatric low back pain is a common complaint presenting to the sports medicine clinic. Although the majority have an underlying musculoskeletal or biomechanical origin, infectious, neoplastic, inflammatory or amplified pain etiologies should be considered. Key elements in the history that should raise index of suspicion for more concerning diagnoses include antecedent trauma or infection, neurologic complaints such burning pain, numbness or tingling, as well as systemic complaints including fever, weight loss, night pain, diarrhea. Red flags on physical examination include hypertension, extreme pain, focal tenderness, weakness, radiculopathy, or restricted range of motion. The history and physical examination should direct the additional laboratory and imaging evaluation. Treatment typically involves physical therapy but the underlying infectious, neoplastic, inflammatory, or amplified pain process must be addressed. It is important for the sports medicine clinician to consider these conditions, especially if the pain is refractory or atypical.
References
- 1.Calvo-Munoz I, Gomez-Conesa A, Sanchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr. 2013;13:14. doi: 10.1186/1471-2431-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson JA. Problems of classification of low-back pain. Rheumatol Rehabil. 1977 Feb;16(1):34–36. doi: 10.1093/rheumatology/16.1.34. [DOI] [PubMed] [Google Scholar]
- 3.Anderson L. Educational approaches to management of low back pain. Orthop Nurs. 1989 Jan-Feb;8(1):43–46. doi: 10.1097/00006416-198901000-00011. [DOI] [PubMed] [Google Scholar]
- 4.d'Hemecourt PA, Gerbino PG, 2nd, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 2000 Oct;19(4):663–679. doi: 10.1016/s0278-5919(05)70231-3. [DOI] [PubMed] [Google Scholar]
- 5.Stracciolini A, Casciano R, Levey Friedman H, Meehan WP, 3rd, Micheli LJ. Pediatric sports injuries: an age comparison of children versus adolescents. Am J Sports Med. 2013 Aug;41(8):1922–1929. doi: 10.1177/0363546513490644. [DOI] [PubMed] [Google Scholar]
- 6.Haus BM, Micheli LJ. Back pain in the pediatric and adolescent athlete. Clin Sports Med. 2012 Jul;31(3):423–440. doi: 10.1016/j.csm.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 7.Rudwaleit M, van der Heijde D, Landewe R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Annals of the rheumatic diseases. 2009 Jun;68(6):777–783. doi: 10.1136/ard.2009.108233. [DOI] [PubMed] [Google Scholar]
- 8.Rudwaleit M, Metter A, Listing J, Sieper J, Braun J. Inflammatory back pain in ankylosing spondylitis: a reassessment of the clinical history for application as classification and diagnostic criteria. Arthritis and rheumatism. 2006 Feb;54(2):569–578. doi: 10.1002/art.21619. [DOI] [PubMed] [Google Scholar]
- 9.Bhatia NN, Chow G, Timon SJ, Watts HG. Diagnostic modalities for the evaluation of pediatric back pain: a prospective study. J Pediatr Orthop. 2008 Mar;28(2):230–233. doi: 10.1097/BPO.0b013e3181651bc8. [DOI] [PubMed] [Google Scholar]
- 10.d'Hemecourt PA, Zurakowski D, d'Hemecourt CA, et al. Validation of a new instrument for evaluating low back pain in the young athlete. Clin J Sport Med. 2012 May;22(3):244–248. doi: 10.1097/JSM.0b013e318249a3ce. [DOI] [PubMed] [Google Scholar]
- 11.Cassidy JTPR. Textbook of Pediatric Rheumatology. 6th edition ed. Philadelphia: Saunders Company; 2011. [Google Scholar]
- 12.Roussel NA, Nijs J, Truijen S, Smeuninx L, Stassijns G. Low back pain: clinimetric properties of the Trendelenburg test, active straight leg raise test, and breathing pattern during active straight leg raising. J Manipulative Physiol Ther. 2007 May;30(4):270–278. doi: 10.1016/j.jmpt.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Moran HM, Hall MA, Barr A, Ansell BM. Spinal mobility in the adolescent. Rheumatol Rehabil. 1979 Aug;18(3):181–185. doi: 10.1093/rheumatology/18.3.181. [DOI] [PubMed] [Google Scholar]
- 14.Manire JT, Kipp R, Spencer J, Swank AM. Diurnal variation of hamstring and lumbar flexibility. J Strength Cond Res. 2010 Jun;24(6):1464–1471. doi: 10.1519/JSC.0b013e3181d32e8c. [DOI] [PubMed] [Google Scholar]
- 15.Purcell L, Micheli L. Low back pain in young athletes. Sports Health. 2009 May;1(3):212–222. doi: 10.1177/1941738109334212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Feldman DS, Straight JJ, Badra MI, Mohaideen A, Madan SS. Evaluation of an algorithmic approach to pediatric back pain. J Pediatr Orthop. 2006 May-Jun;26(3):353–357. doi: 10.1097/01.bpo.0000214928.25809.f9. [DOI] [PubMed] [Google Scholar]
- 17.Auerbach JD, Ahn J, Zgonis MH, Reddy SC, Ecker ML, Flynn JM. Streamlining the evaluation of low back pain in children. Clin Orthop Relat Res. 2008 Aug;466(8):1971–1977. doi: 10.1007/s11999-008-0296-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beck NA, Miller R, Baldwin K, et al. Do oblique views add value in the diagnosis of spondylolysis in adolescents? J Bone Joint Surg Am. 2013 May 15;95(10):e65. doi: 10.2106/JBJS.L.00824. [DOI] [PubMed] [Google Scholar]
- 19.Bollow M, Braun J, Biedermann T, et al. Use of contrast-enhanced MR imaging to detect sacroiliitis in children. Skeletal Radiol. 1998 Nov;27(11):606–616. doi: 10.1007/s002560050446. [DOI] [PubMed] [Google Scholar]
- 20.van der Linden SM, Valkenburg HA, de Jongh BM, Cats A. The risk of developing ankylosing spondylitis in HLA-B27 positive individuals. A comparison of relatives of spondylitis patients with the general population. Arthritis Rheum. 1984 Mar;27(3):241–249. doi: 10.1002/art.1780270301. [DOI] [PubMed] [Google Scholar]
- 21.Selbst SM, Lavelle JM, Soyupak SK, Markowitz RI. Back pain in children who present to the emergency department. Clin Pediatr (Phila) 1999 Jul;38(7):401–406. doi: 10.1177/000992289903800704. [DOI] [PubMed] [Google Scholar]
- 22.Turner PG, Green JH, Galasko CS. Back pain in childhood. Spine (Phila Pa 1976) 1989 Aug;14(8):812–814. doi: 10.1097/00007632-198908000-00007. [DOI] [PubMed] [Google Scholar]
- 23.Micheli LJ, Wood R. Back pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995 Jan;149(1):15–18. doi: 10.1001/archpedi.1995.02170130017004. [DOI] [PubMed] [Google Scholar]
- 24.Li Y, Hresko MT. Lumbar spine surgery in athletes:: outcomes and return-to-play criteria. Clin Sports Med. 2012 Jul;31(3):487–498. doi: 10.1016/j.csm.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 25.Foreman P, Griessenauer CJ, Watanabe K, et al. L5 spondylolysis/spondylolisthesis: a comprehensive review with an anatomic focus. Childs Nerv Syst. 2013 Feb;29(2):209–216. doi: 10.1007/s00381-012-1942-2. [DOI] [PubMed] [Google Scholar]
- 26.Cavalier R, Herman MJ, Cheung EV, Pizzutillo PD. Spondylolysis and spondylolisthesis in children and adolescents: I. Diagnosis, natural history, and nonsurgical management. J Am Acad Orthop Surg. 2006 Jul;14(7):417–424. doi: 10.5435/00124635-200607000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Klein G, Mehlman CT, McCarty M. Nonoperative treatment of spondylolysis and grade I spondylolisthesis in children and young adults: a meta-analysis of observational studies. J Pediatr Orthop. 2009 Mar;29(2):146–156. doi: 10.1097/BPO.0b013e3181977fc5. [DOI] [PubMed] [Google Scholar]
- 28.Tsirikos AI, Jain AK. Scheuermann's kyphosis; current controversies. J Bone Joint Surg Br. 2011 Jul;93(7):857–864. doi: 10.1302/0301-620X.93B7.26129. [DOI] [PubMed] [Google Scholar]
- 29.Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006 Jan;9(1):61–67. [PubMed] [Google Scholar]
- 30.Stoev I, Powers AK, Puglisi JA, Munro R, Leonard JR. Sacroiliac joint pain in the pediatric population. J Neurosurg Pediatr. 2012 Jun;9(6):602–607. doi: 10.3171/2012.2.PEDS11220. [DOI] [PubMed] [Google Scholar]
- 31.Hestbaek L, Leboeuf-Yde C. Are chiropractic tests for the lumbo-pelvic spine reliable and valid? A systematic critical literature review. J Manipulative Physiol Ther. 2000 May;23(4):258–275. doi: 10.1067/mmt.2000.106097. [DOI] [PubMed] [Google Scholar]
- 32.Handrakis JP, Friel K, Hoeffner F, et al. Key characteristics of low back pain and disability in college-aged adults: a pilot study. Arch Phys Med Rehabil. 2012 Jul;93(7):1217–1224. doi: 10.1016/j.apmr.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 33.Rodriguez-Oviedo P, Ruano-Ravina A, Perez-Rios M, et al. School children's backpacks, back pain and back pathologies. Arch Dis Child. 2012 Aug;97(8):730–732. doi: 10.1136/archdischild-2011-301253. [DOI] [PubMed] [Google Scholar]
- 34.Marshall PW, Mannion J, Murphy BA. Extensibility of the hamstrings is best explained by mechanical components of muscle contraction, not behavioral measures in individuals with chronic low back pain. PM R. 2009 Aug;1(8):709–718. doi: 10.1016/j.pmrj.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 35.Hebert KJ, Laor T, Divine JG, Emery KH, Wall EJ. MRI appearance of chronic stress injury of the iliac crest apophysis in adolescent athletes. AJR Am J Roentgenol. 2008 Jun;190(6):1487–1491. doi: 10.2214/AJR.07.3399. [DOI] [PubMed] [Google Scholar]
- 36.Eisen S, Honywood L, Shingadia D, Novelli V. Spinal tuberculosis in children. Arch Dis Child. 2012 Aug;97(8):724–729. doi: 10.1136/archdischild-2011-301571. [DOI] [PubMed] [Google Scholar]
- 37.Taylor ZW, Ryan DD, Ross LA. Increased incidence of sacroiliac joint infection at a children's hospital. J Pediatr Orthop. 2010 Dec;30(8):893–898. doi: 10.1097/BPO.0b013e3181fbebe5. [DOI] [PubMed] [Google Scholar]
- 38.Molinos Quintana A, Morillo Gutierrez B, Camacho Lovillo MS, Neth O, Obando Santaella I. Pyogenic sacroiliitis in children-a diagnostic challenge. Clin Rheumatol. 2011 Jan;30(1):107–113. doi: 10.1007/s10067-010-1549-5. [DOI] [PubMed] [Google Scholar]
- 39.Taylor ZW, Ryan DD, Ross LA. Increased incidence of sacroiliac joint infection at a children's hospital. J Pediatr Orthop. 2010 Dec;30(8):893–898. doi: 10.1097/BPO.0b013e3181fbebe5. [DOI] [PubMed] [Google Scholar]
- 40.Wada A, Takamura K, Fujii T, Yanagida H, Surijamorn P. Septic sacroiliitis in children. J Pediatr Orthop. 2008 Jun;28(4):488–492. doi: 10.1097/BPO.0b013e31816d7214. [DOI] [PubMed] [Google Scholar]
- 41.Wu MS, Chang SS, Lee SH, Lee CC. Pyogenic sacroiliitis--a comparison between paediatric and adult patients. Rheumatology. 2007 Nov;46(11):1684–1687. doi: 10.1093/rheumatology/kem201. [DOI] [PubMed] [Google Scholar]
- 42.Hermet M, Minichiello E, Flipo RM, et al. Infectious sacroiliitis: a retrospective, multicentre study of 39 adults. BMC infectious diseases. 2012;12:305. doi: 10.1186/1471-2334-12-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chandrasenan J, Klezl Z, Bommireddy R, Calthorpe D. Spondylodiscitis in children: a retrospective series. J Bone Joint Surg Br. 2011 Aug;93(8):1122–1125. doi: 10.1302/0301-620X.93B8.25588. [DOI] [PubMed] [Google Scholar]
- 44.Spencer SJ, Wilson NI. Childhood discitis in a regional children's hospital. J Pediatr Orthop B. 2012 May;21(3):264–268. doi: 10.1097/BPB.0b013e32834d3e94. [DOI] [PubMed] [Google Scholar]
- 45.Karabouta Z, Bisbinas I, Davidson A, Goldsworthy LL. Discitis in toddlers: a case series and review. Acta Paediatr. 2005 Oct;94(10):1516–1518. doi: 10.1111/j.1651-2227.2005.tb01832.x. [DOI] [PubMed] [Google Scholar]
- 46.Spencer SJ, Wilson NI. Childhood discitis in a regional children's hospital. J Pediatr Orthop B. 2012 May;21(3):264–268. doi: 10.1097/BPB.0b013e32834d3e94. [DOI] [PubMed] [Google Scholar]
- 47.Date AR, Rooke R, Sivashankar S. Lumbar discitis. Arch Dis Child. 2006 Feb;91(2):116. doi: 10.1136/adc.2005.080804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kayser R, Mahlfeld K, Greulich M, Grasshoff H. Spondylodiscitis in childhood: results of a long-term study. Spine (Phila Pa 1976) 2005 Feb 1;30(3):318–323. doi: 10.1097/01.brs.0000152097.57891.98. [DOI] [PubMed] [Google Scholar]
- 49.Haidar R, Saad S, Khoury NJ, Musharrafieh U. Practical approach to the child presenting with back pain. Eur J Pediatr. 2011 Feb;170(2):149–156. doi: 10.1007/s00431-010-1220-9. [DOI] [PubMed] [Google Scholar]
- 50.Erlemann R. Imaging and differential diagnosis of primary bone tumors and tumor-like lesions of the spine. Eur J Radiol. 2006 Apr;58(1):48–67. doi: 10.1016/j.ejrad.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 51.Patel AJ, Fox BD, Fahim DK, et al. A clinicopathologic correlation in osteoblastoma of the spine in a child. J Clin Neurosci. 2011 Dec;18(12):1728–1730. doi: 10.1016/j.jocn.2011.03.017. [DOI] [PubMed] [Google Scholar]
- 52.Gebauer B, Collettini F, Bruger C, et al. Radiofrequency Ablation of Osteoid Osteomas: Analgesia and Patient Satisfaction in Long-term Follow-up. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2013 Aug 23; [PubMed] [Google Scholar]
- 53.Huang WD, Yang XH, Wu ZP, et al. Langerhans cell histiocytosis of spine: a comparative study of clinical, imaging features, and diagnosis in children, adolescents, and adults. Spine J. 2013 Apr 18; doi: 10.1016/j.spinee.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 54.Huang WD, Yang XH, Wu ZP, et al. Langerhans cell histiocytosis of spine: a comparative study of clinical, imaging features, and diagnosis in children, adolescents, and adults. Spine J. 2013 Sep;13(9):1108–1117. doi: 10.1016/j.spinee.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 55.Garg S, Mehta S, Dormans JP. Langerhans cell histiocytosis of the spine in children. Long-term follow-up. J Bone Joint Surg Am. 2004 Aug;86-A(8):1740–1750. doi: 10.2106/00004623-200408000-00019. [DOI] [PubMed] [Google Scholar]
- 56.Huisman TA. Pediatric tumors of the spine. Cancer Imaging. 2009;9(Spec No A):S45–S48. doi: 10.1102/1470-7330.2009.9012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smith AB, Soderlund KA, Rushing EJ, Smirniotopolous JG. Radiologic-pathologic correlation of pediatric and adolescent spinal neoplasms: Part 1, Intramedullary spinal neoplasms. AJR Am J Roentgenol. 2012 Jan;198(1):34–43. doi: 10.2214/AJR.10.7311. [DOI] [PubMed] [Google Scholar]
- 58.Ferguson PJ, El-Shanti HI. Autoinflammatory bone disorders. Curr Opin Rheumatol. 2007 Sep;19(5):492–498. doi: 10.1097/BOR.0b013e32825f5492. [DOI] [PubMed] [Google Scholar]
- 59.Stern SM, Ferguson PJ. Autoinflammatory bone diseases. Rheum Dis Clin North Am. 2013 Nov;39(4):735–749. doi: 10.1016/j.rdc.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Iyer RS, Thapa MM, Chew FS. Chronic recurrent multifocal osteomyelitis: review. AJR Am J Roentgenol. 2011 Jun;196(6 Suppl):S87–S91. doi: 10.2214/AJR.09.7212. [DOI] [PubMed] [Google Scholar]
- 61.Falip C, Alison M, Boutry N, et al. Chronic recurrent multifocal osteomyelitis (CRMO): a longitudinal case series review. Pediatr Radiol. 2013 Mar;43(3):355–375. doi: 10.1007/s00247-012-2544-6. [DOI] [PubMed] [Google Scholar]
- 62.Khanna G, Sato TS, Ferguson P. Imaging of chronic recurrent multifocal osteomyelitis. Radiographics. 2009 Jul-Aug;29(4):1159–1177. doi: 10.1148/rg.294085244. [DOI] [PubMed] [Google Scholar]
- 63.Guerin-Pfyffer S, Guillaume-Czitrom S, Tammam S, Kone-Paut I. Evaluation of chronic recurrent multifocal osteitis in children by whole-body magnetic resonance imaging. Joint Bone Spine. 2012 Dec;79(6):616–620. doi: 10.1016/j.jbspin.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 64.Twilt M, Laxer RM. Clinical care of children with sterile bone inflammation. Curr Opin Rheumatol. 2011 Sep;23(5):424–431. doi: 10.1097/BOR.0b013e328349c363. [DOI] [PubMed] [Google Scholar]
- 65.Hospach T, Langendoerfer M, von Kalle T, Maier J, Dannecker GE. Spinal involvement in chronic recurrent multifocal osteomyelitis (CRMO) in childhood and effect of pamidronate. Eur J Pediatr. 2010 Sep;169(9):1105–1111. doi: 10.1007/s00431-010-1188-5. [DOI] [PubMed] [Google Scholar]
- 66.Dougados M, Baeten D. Spondyloarthritis. Lancet. 2011 Jun 18;377(9783):2127–2137. doi: 10.1016/S0140-6736(11)60071-8. [DOI] [PubMed] [Google Scholar]
- 67.Rudwaleit M, Landewe R, van der Heijde D, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part I): classification of paper patients by expert opinion including uncertainty appraisal. Ann Rheum Dis. 2009 Jun;68(6):770–776. doi: 10.1136/ard.2009.108217. [DOI] [PubMed] [Google Scholar]
- 68.Carter JD. Reactive arthritis: defined etiologies, emerging pathophysiology, and unresolved treatment. Infect Dis Clin North Am. 2006 Dec;20(4):827–847. doi: 10.1016/j.idc.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 69.Weiss PF, Klink AJ, Behrens EM, et al. Enthesitis in an inception cohort of enthesitis-related arthritis. Arthritis Care Res (Hoboken) 2011 Sep;63(9):1307–1312. doi: 10.1002/acr.20508. [DOI] [PubMed] [Google Scholar]
- 70.Weiss PF. Diagnosis and treatment of enthesitis-related arthritis. Adolesc Health Med Ther. 2012 Jun;2012(3):67–74. doi: 10.2147/AHMT.S25872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pagnini I, Savelli S, Matucci-Cerinic M, Fonda C, Cimaz R, Simonini G. Early predictors of juvenile sacroiliitis in enthesitis-related arthritis. J Rheumatol. 2010 Nov;37(11):2395–2401. doi: 10.3899/jrheum.100090. [DOI] [PubMed] [Google Scholar]
- 72.Flato B, Hoffmann-Vold AM, Reiff A, Forre O, Lien G, Vinje O. Long-term outcome and prognostic factors in enthesitis-related arthritis: a case-control study. Arthritis Rheum. 2006 Nov;54(11):3573–3582. doi: 10.1002/art.22181. [DOI] [PubMed] [Google Scholar]
- 73.Rudwaleit M, Taylor WJ. Classification criteria for psoriatic arthritis and ankylosing spondylitis/axial spondyloarthritis. Best Pract Res Clin Rheumatol. 2010 Oct;24(5):589–604. doi: 10.1016/j.berh.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 74.Colbert RA. Classification of juvenile spondyloarthritis: Enthesitis-related arthritis and beyond. Nat Rev Rheumatol. 2010 Aug;6(8):477–485. doi: 10.1038/nrrheum.2010.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Southwood TR, Petty RE, Malleson PN, et al. Psoriatic arthritis in children. Arthritis Rheum. 1989 Aug;32(8):1007–1013. doi: 10.1002/anr.1780320810. [DOI] [PubMed] [Google Scholar]
- 76.Truckenbrodt H, Hafner R. [Psoriatic arthritis in childhood. A comparison with subgroups of chronic juvenile arthritis] Z Rheumatol. 1990 Mar-Apr;49(2):88–94. [PubMed] [Google Scholar]
- 77.Sills EM. Psoriatic arthritis in childhood. Johns Hopkins Med J. 1980 Feb;146(2):49–53. [PubMed] [Google Scholar]
- 78.Scarpa R, Oriente P, Pucino A, et al. The clinical spectrum of psoriatic spondylitis. Br J Rheumatol. 1988 Apr;27(2):133–137. doi: 10.1093/rheumatology/27.2.133. [DOI] [PubMed] [Google Scholar]
- 79.Van Assche G, Dignass A, Bokemeyer B, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 3: special situations. J Crohns Colitis. 2013 Feb;7(1):1–33. doi: 10.1016/j.crohns.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 80.Brakenhoff LK, van der Heijde DM, Hommes DW, Huizinga TW, Fidder HH. The joint-gut axis in inflammatory bowel diseases. J Crohns Colitis. 2010 Sep;4(3):257–268. doi: 10.1016/j.crohns.2009.11.005. [DOI] [PubMed] [Google Scholar]
- 81.Al-Jarallah K, Shehab D, Al-Azmi W, Al-Fadli A. Rheumatic complications of inflammatory bowel disease among Arabs: a hospital-based study in Kuwait. Int J Rheum Dis. 2013 Apr;16(2):134–138. doi: 10.1111/j.1756-185X.2012.01811.x. [DOI] [PubMed] [Google Scholar]
- 82.Dotson J, Crandall W, Bout-Tabaku S. Exploring the differential diagnosis of joint complaints in pediatric patients with inflammatory bowel disease. Curr Gastroenterol Rep. 2011 Jun;13(3):271–278. doi: 10.1007/s11894-011-0181-0. [DOI] [PubMed] [Google Scholar]
- 83.De Vos M. Review article: joint involvement in inflammatory bowel disease. Aliment Pharmacol Ther. 2004 Oct;20(Suppl 4):36–42. doi: 10.1111/j.1365-2036.2004.02044.x. [DOI] [PubMed] [Google Scholar]
- 84.Smith EA, Dillman JR, Adler J, Dematos-Maillard VL, Strouse PJ. MR enterography of extraluminal manifestations of inflammatory bowel disease in children and adolescents: moving beyond the bowel wall. AJR Am J Roentgenol. 2012 Jan;198(1):W38–W45. doi: 10.2214/AJR.11.6803. [DOI] [PubMed] [Google Scholar]
- 85.Weiss PF. Pediatric vasculitis. Pediatr Clin North Am. 2012 Apr;59(2):407–423. doi: 10.1016/j.pcl.2012.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Cakar N, Yalcinkaya F, Duzova A, et al. Takayasu arteritis in children. J Rheumatol. 2008 May;35(5):913–919. [PubMed] [Google Scholar]
- 87.Sherry DD. Diagnosis and treatment of amplified musculoskeletal pain in children. Clin Exp Rheumatol. 2001 Nov-Dec;19(6):617–620. [PubMed] [Google Scholar]
- 88.Young L, Kemper KJ. Integrative care for pediatric patients with pain. J Altern Complement Med. 2013 Jul;19(7):627–632. doi: 10.1089/acm.2012.0368. [DOI] [PubMed] [Google Scholar]
- 89.Mandell GA. Nuclear Medicine in Pediatric Musculoskeletal Imaging. Semin Musculoskelet Radiol. 1999;3(3):289–316. doi: 10.1055/s-2008-1080073. [DOI] [PubMed] [Google Scholar]
- 90.Cunningham NR, Kashikar-Zuck S. Nonpharmacological treatment of pain in rheumatic diseases and other musculoskeletal pain conditions. Curr Rheumatol Rep. 2013 Feb;15(2):306. doi: 10.1007/s11926-012-0306-y. [DOI] [PMC free article] [PubMed] [Google Scholar]