Abstract
Objectives
Body image is a critical issue for cancer patients undergoing reconstructive surgery, as they can experience disfigurement and functional impairment. Distress related to appearance changes can lead to various psychosocial difficulties, and patients are often reluctant to discuss these issues with their healthcare team. Our goals were to design and evaluate a screening tool to aid providers in identifying patients who may benefit from referral for specialized psychosocial care to treat body image concerns.
Methods
We designed a brief 4-item instrument and administered it at a single time point to cancer patients who were undergoing reconstructive treatment. We used simple and multinomial regression models to evaluate whether survey responses, demographic, or clinical variables predicted interest and enrollment in counseling.
Results
Over 95% of the sample (n = 248) endorsed some concerns, preoccupation, or avoidance due to appearance changes. Approximately one-third of patients were interested in obtaining counseling or additional information to assist with body image distress. Each survey item significantly predicted interest and enrollment in counseling. Concern about future appearance changes was the single best predictor of counseling enrollment. Sex, age, and cancer type were not predictive of counseling interest or enrollment.
Conclusions
We present initial data supporting use of the Body Image Screener for Cancer Reconstruction. Our findings suggest benefits of administering this tool to patients presenting for reconstructive surgery. It is argued that screening and treatment for body image distress should be provided to this patient population at the earliest possible time point.
Keywords: body image, distress screening, breast cancer, head and neck cancer, reconstructive surgery
Body image is a multidimensional construct involving perceptions, thoughts, and feelings about the entire body and its functioning.1 It is recognized as a critical psychosocial issue for cancer patients undergoing reconstructive surgery because they are at high risk of experiencing disfigurement and functional impairment. The process of adjusting to bodily changes during reconstructive treatment is ongoing, as multi-staged procedures are often required. Interim outcomes may be particularly bothersome to patients when cosmetic form and function have not been fully restored. Among the adverse psychosocial difficulties linked with body image disturbance in cancer patients include depression and anxiety2–6, sexual functioning difficulties7–10, and impairments in overall quality of life11–13.
High rates of body image concerns have been documented for head and neck and breast cancer patients, two groups who most often undergo reconstructive surgery. Body image disturbance is among the most common psychosocial concern reported by women with breast cancer.14 Moreover, up to 75% of patients with head and neck cancer have been found to endorse concerns or embarrassment about bodily changes following diagnosis.15,16 It is difficult to estimate rates of body image concerns among cancer patients undergoing reconstructive surgery as most research on body image and cancer has either been conducted with disease-specific samples or with a particular subgroup receiving reconstruction (i.e., breast reconstruction). The vast literature reviewing patient-reported outcomes in breast reconstruction identifies various demographic (e.g., age, marital status)17 psychological (e.g., depression, anxiety)5,18, medical (e.g., body mass index)19 and disease/treatment related factors (e.g., cancer type, type and timing of reconstruction, complications)20–22 associated with body image and quality of life.
Increasing attention is being given to delivering psychosocial care to cancer patients which specifically targets body image difficulties. Much of this work is based on cognitive-behavioral models of body image disturbance which highlight the importance of addressing maladaptive thoughts, behaviors, and emotions related to one’s appearance.23–25 For a patient struggling with body image concerns, emphasis is placed on acceptance of body image changes and increasing self-confidence in social situations. Key treatment strategies for mental health specialists to manage body image issues in the oncology setting have been described elsewhere,26–29 and it is recognized that treatment should be tailored based upon the distinct phase of the cancer journey.
A significant source of distress for cancer patients undergoing reconstructive surgery is related to body image changes they experience during treatment. Unfortunately, much research suggests that physicians are not adept or comfortable with evaluating or managing patient distress. Lack of time is the most frequently reported barrier for medical professionals in being able to identify and manage patient distress.30 Moreover, patients are reluctant to bring up their distress with their oncologists31,32 and this may especially be true for those experiencing body image concerns. It is not uncommon for a cancer patient to worry about being seen as “vain” and experience shame and embarrassment about having body image concerns.26 For these reasons, it is critical to develop a useful screening tool that will facilitate the identification and treatment of patients with body image difficulties in the oncology setting.
Validated tools assessing body image in cancer patients are lacking, and we are not aware of any tools developed for the purpose of screening patients for body image. A systematic review by Annunziata et al., found only six questionnaires dedicated to body image assessment for cancer patients. Only one tool was applicable to patients with diverse disease sites, while remaining tools were specific to breast or gastrointestinal cancer.33 None of these tools were identified as offering a gold standard for evaluating body image in the oncology setting, nor were any specifically developed as a screening tool. More recent advancements have been made with the development of assessment tools for breast cancer patients undergoing reconstructive surgery, focused on satisfaction with outcomes and quality of life. Tools such as the Breast Reconstruction Satisfaction Questionnaire (BRECON-31)34 and Breast-Q35 have gained more widespread use, and have undergone extensive validation. However, these tools focus on a specific subset of patients undergoing reconstruction, and again are not intended for use as a screening measure of body image distress.
Our goals were to design and evaluate a brief body image screening tool for cancer patients undergoing reconstructive surgery that has the potential to be used as part of routine clinical practice. This tool is needed to assist medical professionals in identifying patients with body image distress who may benefit from a referral for specialized psychosocial care.
Methods
Development of the Screening Tool
Survey items were developed based on knowledge gleaned from the body image literature and clinical expertise of a multidisciplinary research team. The lead and second authors have considerable experience providing psychological care treating body image difficulties for an array of patients, including those with cancer. The final three authors have expertise as reconstructive surgeons working within a large comprehensive cancer center, highly familiar with the types of body image difficulties of cancer patients report during reconstructive treatment. Key areas of content included distress, preoccupation, and behavioral avoidance. These domains encompass emotional, cognitive, and behavioral aspects of body image disturbance which are consistently represented in body image assessment tools. Moreover, they reflect core aspects of cognitive-behavioral models of body image disturbance as discussed above. We generated four items related to concerns about recent changes to appearance, worry about future appearance changes from reconstructive surgery, time spent thinking about appearance, and time spent avoiding activities due to appearance concerns (see Table 1). We underwent an iterative process as each member of the team reviewed item content and offered feedback. Language and wording was also reviewed by our institution’s Patient Education Office to ensure an 8th grade reading level. We refer to the instrument as the Body Image Screener for Cancer Reconstruction (BICR).
Table 1.
Body Image Screener for Cancer Reconstruction Survey
| Body Image Screener for Cancer Reconstruction (BICR) | ||||
| Many patients have concerns about how cancer treatment will change the way they look. Both men and women worry about changes to their appearance before and after reconstructive surgery. | ||||
Body image specialists are available to help you cope with appearance concerns. Our specialists can help you:
| ||||
| Please read each question and circle the number that describes your feelings. | ||||
| Not at all | A little | Quite a bit | Very much | |
| 1. How concerned are you about recent changes to your appearance and body? | 0 | 1 | 2 | 3 |
| 2. How much do you worry about future changes to your appearance from reconstructive surgery? | 0 | 1 | 2 | 3 |
| None of the time | A little of the time | Some of the time | Most of the time | |
| 3. How often do you think about your appearance? | 0 | 1 | 2 | 3 |
| 4. How often do you avoid certain activities because of concerns about your appearance? | 0 | 1 | 2 | 3 |
The BICR was administered as a paper-pencil measure and included a brief introductory paragraph designed to normalize concerns about appearance changes for patients undergoing reconstructive surgery (see Table 1). Patients were informed that body image specialists were available to help them cope with appearance concerns. As part of the study, patients were also asked via paper and pencil if they would like to meet with a specialist or would like more information about these services.
This study was approved by our institutional review board. Since information obtained as part of this study was used for clinical purposes (i.e., directing patients to available psychosocial services), a waiver of informed consent was granted.
Evaluation of the Screening Tool
BICR surveys were administered over a 3-month period (6/2011 – 9/2011) to all patients seen by three reconstructive surgeons at The University of Texas MD Anderson Cancer Center. Patients were given the BICR while waiting to see their treating physician. This study employed a cross-sectional design with analyses focused only on the first time point the survey was completed by a given patient. Any patient expressing interest in speaking with a specialist about his or her concerns (regardless of their scores on the BICR) was contacted and offered additional information and a counseling appointment. Those requesting further information received a brief introductory call about available psychosocial services or a letter providing these details if they could not be reached.
We recorded demographic and clinical characteristics of each participant from a review of medical records, and conducted descriptive analyses on these variables and on survey responses. Simple and multinomial logistic regression models were used to evaluate whether demographic, clinical variables and survey items predicted counseling interest as well as counseling enrollment. We first conducted simple logistic regression analyses to predict interest in body image counseling where we considered each survey item separately and used the full range of response options. Individual survey items were also analyzed as binary variables reflecting little or no concerns (values < 2) versus moderate or extreme concerns (values ≥ 2). Further analyses summarized survey scores into a single value. We assigned a value of 0 if responses for all 4 questions were 2 or less and a value of 1 if the score on any question was a 3.
Multiple logistic regression models were used to evaluate all predictor variables in determining counseling outcomes. We conducted simple stepwise variable selection procedures (forward and backward) and report the best model based on maximization of the goodness of fit estimate using the Nagelkerke R square index.
Results
Table 2 presents demographic and clinical characteristics of our sample, which included 248 patients. The majority of participants were female (87%) and had breast cancer (71%). However, 16% were patients with head and neck and 13% had other cancers. The other category included patients with various cancers affecting the extremities, abdomen, pelvic, or groin regions. These types of cancers included but were not limited to ovarian, rectal, renal cell, melanoma, sarcoma, and chordoma. Patients were either being seen at an initial stage of reconstruction (consult/preop) or were seen for follow-up and/or discussion of revision surgery.
Table 2.
Patient Demographic and Clinical Characteristics (N = 248)
| Characteristics | No. of Patients/Values |
|---|---|
| Age, years | Mean = 51.86, sd = 13.15 (range, 13–85) |
| Sex | 87% female |
| 13% male | |
| Race | 70% white |
| 30% non-white | |
| Marital status | 73% married |
| 15% single | |
| 9% divorced/separated | |
| 3% widowed | |
| Cancer type | 71% breast |
| 16% head and neck | |
| 13% other | |
| BMI | Mean = 27.40, sd = 5.75 (range, 15.70–46.00) |
| Clinic visit type | 29% consult/preop |
| 71% revision/follow-up | |
| Time since initial reconstructive surgery |
Mean = 10.48 months, sd = 1.28 years (range, 0–6.77 years) |
Note. BMI = body mass index; sd = standard deviation; preop = preoperative.
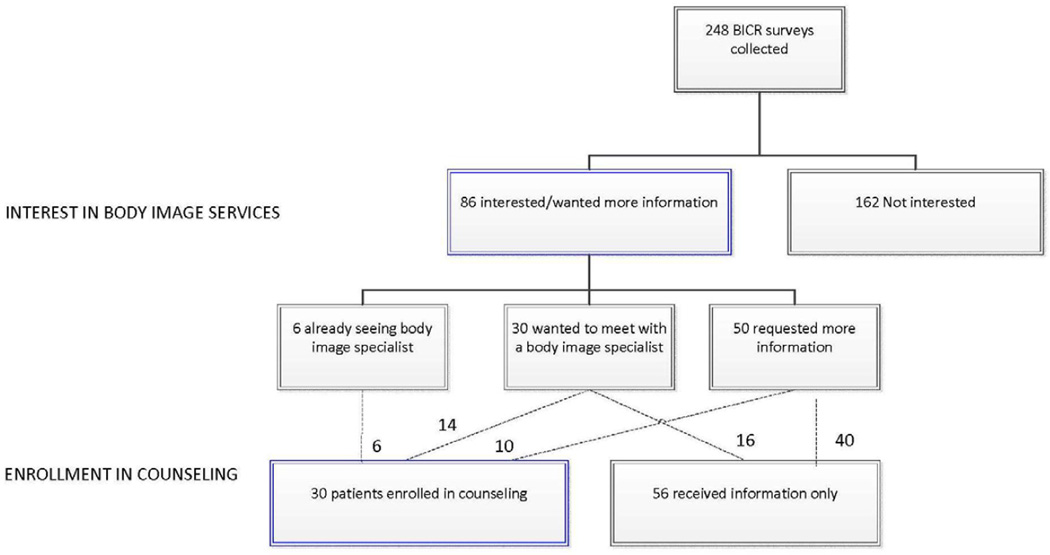
Survey responses revealed that 95% of participants had some degree of concern, preoccupation, or avoidance due to appearance changes. That is, they endorsed at least one item on the BICR at a value other than “not at all” or “none of the time”. Table 3 presents information on rate of endorsement of each survey item, and shows that depending on the item approximately 10–24% of the sample endorsed an extreme response (“very much” or “most of the time”.) A total of 35% expressed an interest in counseling or wanted more information related to counseling. Among those interested in speaking with a body image specialist, 35% were seen in person for counseling. Figure 1 presents further data on patient interest and subsequent enrollment in body image counseling following completion of the BICR.
Table 3.
Rate of Endorsement on Individual Items of the BICR
| Not at all | A Little | Quite A bit | Very Much | |
|---|---|---|---|---|
| Q1: current concerns | 51 (20.6%) | 98 (39.5%) | 55 (22.2%) | 44 (17.7%) |
| Q2: future concerns | 60 (24.2%) | 79 (31.9%) | 62 (25.0%) | 47 (19.0%) |
| None of the time | A little of the time | Some of the time | Most of the time | |
| Q3: thoughts | 19 (7.7%) | 71 (28.6%) | 99 (39.9%) | 59 (23.8%) |
| Q4: avoidance | 104 (41.9%) | 52 (21.0%) | 67 (27.0%) | 25 (10.1%) |
Note. BICR = Body Image Screener for Cancer Reconstruction. Q1 refers to Question 1, Q2 refers to Question 2, Q3 refers to Question 3, Q4 refers to Question 4
Figure 1.
Patient Interest and Enrollment in Body Image Counseling Following Completion of BICR
Note. BICR = Body Image Screener for Cancer Reconstruction, *represents surveys that were completed by patients at repeat visits
Interest in Body Image Counseling
We conducted simple logistic regressions predicting counseling interest based on responses to each survey item. Interest in counseling was defined as requesting more information, requesting to meet with a specialist, or stating that one had already seen a specialist. When considering the full range of response options on the BICR, the odds of being interested in counseling significantly increased with extreme (“very much”) concerns about recent appearance changes (OR = 4.39; p = 0.04, 95% CI 1.06-18.14) and with moderate (“quite a bit”) and extreme (“very much”) concerns about future appearance changes (OR = 3.33; p = 0.04, 95% CI 1.06-10.49 and OR = 4.67, p = 0.02, 95% CI 1.31-6.64, respectively). When considering survey items as binary variables, we found that each survey item significantly predicted counseling interest (Table 4). Age, race, marital status, sex, cancer type, and time since initial reconstructive surgery were not found to significantly predict counseling interest. Type of clinic visit (p = .06) and BMI (p = .07) were associated with marginally significant findings.
Table 4.
Simple Logistic Regressions Predicting Interest in Body Image Counseling
| 95% CI | |||||
|---|---|---|---|---|---|
| OR | Lower | Upper | p value | ||
| BICR survey responses1 | |||||
| BICR 1: current concerns | 4.47 | 2.56 | 7.81 | <.01 | |
| BICR 2: future concerns | 6.14 | 3.42 | 10.95 | <.01 | |
| BICR 3: preoccupation | 3.68 | 1.99 | 6.79 | <.01 | |
| BICR 4: avoidance | 3.75 | 2.16 | 6.52 | <.01 | |
| Demographic variables | |||||
| Age | 0.99 | .098 | 1.01 | 0.50 | |
| Sex | 1.49 | 0.66 | 3.37 | 0.34 | |
| Race | 1.44 | 0.82 | 2.52 | 0.21 | |
| Marital status2 | 0.62 | ||||
| Clinical variables | |||||
| Cancer type3 | 0.28 | ||||
| BMI | 1.04 | 0.98 | 1.09 | .07 | |
| Clinic visit type4 | 0.06 | ||||
| Time since initial surgery | 1.00 | 0.99 | 1.00 | 0.32 | |
CI = confidence interval; OR = odds ratio; BICR = Body Image Screener for Cancer Reconstruction.
Response options for each survey item were dichotomized to reflect none/minimal or moderate/high levels.
Marital status comprised the following categories: married, single, divorced, separated, widowed. Each was not significant; p values > .05.
Cancer type comprised the categories or breast, head and neck, and other. Each was not significant; p values >.05.
For clinic visit type, we defined two types of consult visits (initial consult and follow-up consult), two types of preoperative visits (preop prior to initial surgery, preop prior to revision surgery), and follow-up visits. Significant findings emerged only when comparing follow-up visits to initial consults (OR = −1.02, 95% CI 0.18-.071, p <01).
Multinomial logistic regression analyses revealed that the odds of requesting more information, with respect to no interest, were 3.26 times higher (p = 0.05, 95% CI 1.44-7.38) when a person had extreme concern (value = 3) in at least one area. Similarly, the odds of requesting to meet with a specialist were 16.08 times higher (p < .001, 95% CI 2.13-121.22) when a person had extreme concern in at least one area versus when a person had no concerns.
Multivariate regression analyses evaluating interest in counseling included survey responses (binary variables) and demographic and clinical variables as predictors. The best model included the following significant predictors: BMI, Q1 (current concerns), and Q2 (future concerns), with a Nagelkerke R Square index of 0.26. There was a small but significantly greater interest in counseling for those with a higher BMI (p = 0.03, OR = 1.06, 95% CI 1.01-1.12). In addition, greater interest in counseling was found to be related to higher levels of concern about recent changes in appearance (p = 0.03, OR = 2.17, 95% CI 1.12-4.21) and future changes in appearance (p < .001, OR = 4.45, 95% CI 2.26-8.75) due to reconstructive surgery.
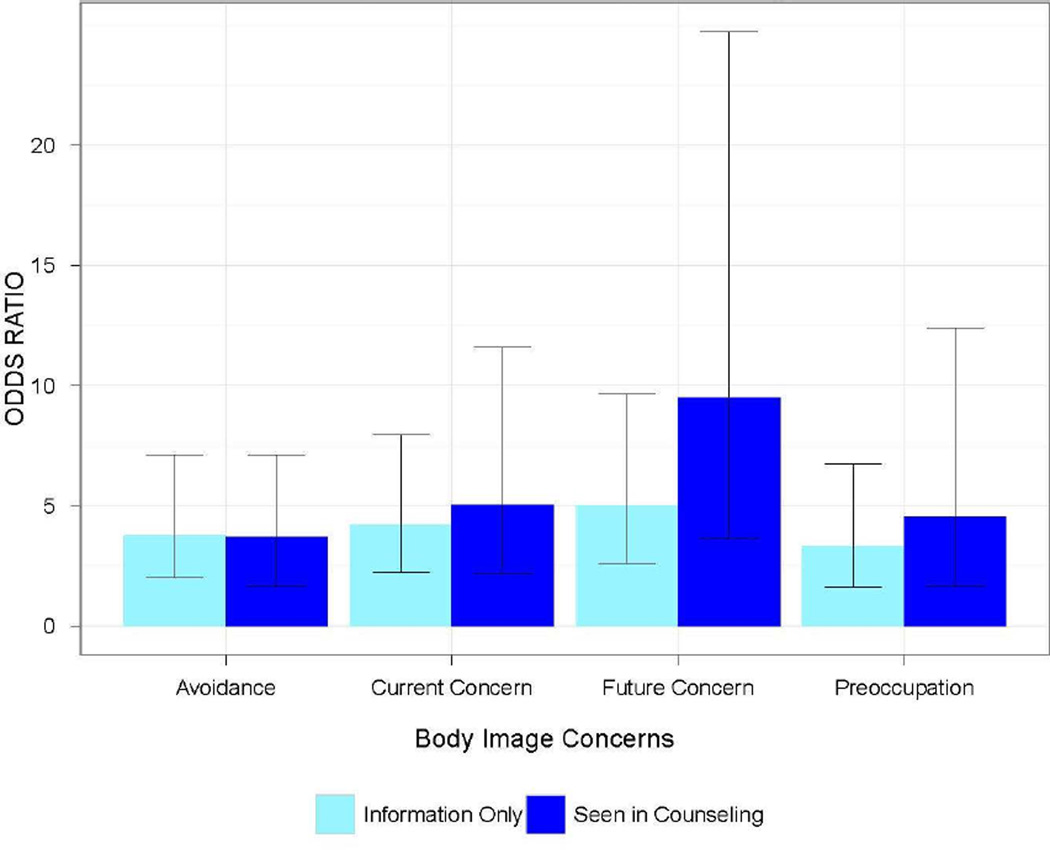
Enrollment in Counseling
Participants were categorized according to whether they were actually seen in counseling, received information only, or expressed no interest in counseling. Results of multinomial regressions predicting enrollment in counseling based on survey responses (binary variable) are presented in Figure 2. The odds of enrolling in counseling and seeking information significantly increased with greater concerns on each survey item. Specifically, the probability of enrolling in counseling increased 9-fold whenever the patient was quite a bit or very much concerned about future appearance changes (OR = 9.5, 95% CI 3.66-24.72, p < .001), whereas the probability of seeking information about these services increased 5-fold (OR = 5.02, 95% CI 2.61-9.65, p < .001).
Figure 2.
Multinomial Regressions Predicting Counseling Outcome
Note: Odds ratios for individual items ranged from 3.32 to 9.95, and all p values were < 0.001.
Similar to our findings regarding counseling interest, demographic and clinical variables did not significantly predict counseling enrollment. Multinomial logistic regression models were not significant for age, race, marital status, sex, or cancer type. There was a marginally significant effect for visit type such that the odds of enrolling in counseling were lower for those seen at follow-up versus consult (OR = 0.46, 95% CI 0.20-1.04, p = 0.06) The odds of enrolling in counseling also decreased slightly as time passed since initial reconstructive surgery (OR = 0.99, 95% CI 0.99-1.00, p < .01). In contrast to findings regarding counseling interest, higher BMI slightly decreased the probability of counseling enrollment (OR = 0.94, 95% CI 0.93-0.95, p < .01).
Finally, we evaluated counseling enrollment using multiple logistic regression models. We considered a model where survey responses and demographic and clinical variables were included and a model where only the survey responses were considered. The best model had a single predictor, Q2: concerns about future appearance (p ≤ .01, OR = 6.140, CI 2.41-15.637). For this model, Nagelkerke R2 was 0.14
Discussion
We present initial data supporting use of the Body Image Screener for Cancer Reconstruction (BICR). This screening tool was designed to facilitate the identification of patients who may benefit from a referral for specialized psychosocial care to treat body image concerns. Our findings contribute to the literature on body image and oncologic reconstructive surgery in a number of important ways. To our knowledge, we are among the first to actually document rates of appearance concerns and body image issues for cancer patients undergoing reconstructive surgery. Previous research in this area has typically focused on a single disease site or has examined body image issues only for a specific group of cancer patients undergoing reconstructive surgery. Nearly every patient in our study (95%) endorsed some degree of concern about current and future changes to appearance, preoccupation with appearance, or avoidance due to appearance. Body image concerns were found across all stages of reconstructive treatment and were irrespective of cancer type, sex, age, race, marital status, and BMI. These findings are important in that they underscore the need to normalize and validate body image concerns for cancer patients undergoing reconstructive surgery to help reduce shame, stigma, and embarrassment surrounding these issues.26
Participants may have been more comfortable with acknowledging their concerns because we deliberately crafted an opening paragraph educating patients about the common nature of body image concerns for those undergoing reconstructive surgery. Although nearly all participants endorsed some concerns related to appearance, it is clear that not all were interested in seeking counseling and many feel equipped to manage their concerns without professional guidance. However, greater than one third of our sample expressed a desire for counseling or wanted to obtain more information about these services. This reflects interest in counseling or obtaining resources to help cope with body image issues among a substantial portion of this patient population, and is consistent with other published findings. In a cross-sectional survey of patients with head and neck cancer, 34% of patients endorsed wanting assistance with body image issues, with the majority indicating they were very likely or somewhat likely to utilize counseling resources if made available to them.15
Most of our analyses examined the predictive value of individual items on the BICR because we considered each variable to be categorical. We did not assume the values necessarily “sum up” in a quantitatively measurable way. Our findings suggest that a score of 3 on any single item of the BICR could reasonably be used to identify a patient who may benefit from a referral. Participants with these scores were significantly more likely to enroll in body image counseling or desire further resources to assist them in coping with body image concerns. Additional results suggest that a score of 2 or 3 on any single item, but particularly on Q2 (concerns about future appearance changes), could be used as an indicator for a counseling referral.
Although other research has identified age, BMI, and cancer type as potential risk factors for body image distress,25 our study found very few demographic or clinic variables to demonstrate predictive value in identifying patients likely to be interested in or enroll in body image counseling. Contrary to what one might expect, younger age and female sex did not predict interest in counseling and neither did cancer type. Breast cancer, head and neck cancer, and other types of patients undergoing reconstructive surgery were equally likely to seek or be open to learning about body image counseling. We also found no differences based on marital status or race. There were mixed results regarding BMI, with some findings suggesting that a higher BMI is associated with increased odds of being interested in counseling but slightly decreased odds of enrolling in counseling. While these findings are not clinically meaningful due to the low magnitude of the odds ratios, they suggest that patients with a higher BMI may be reluctant to engage in body image counseling despite having an interest in receiving such assistance. Clearly further research is needed to explore this issue.
There was consistent evidence that patients in an earlier phase of treatment were more interested in and more likely to enroll in body image counseling. We found that the odds of being interested in counseling and enrolling in counseling were higher for patients seen at consult compared to follow-up. Moreover, concern about future or upcoming appearance changes was clearly the strongest predictor related to counseling. These findings lend support to Cash’s cognitive behavioral model of body image23 wherein he posits that certain types of proximal events can serve as a strong trigger for maladaptive thoughts, behaviors, and emotions tied to appearance. Within this context we consider cancer diagnosis and initiation of reconstructive surgery to be such a trigger.
Our findings suggest a benefit of administering the BICR to patients as early as possible during their treatment, prior to surgical intervention. In previous research, patients with head and neck cancer endorsed the need for services to help them cope with appearance-related and body image changes along the entire treatment continuum. Although many believed that these services would be beneficial before treatment begins, during active treatment, as well as following completion of treatment, a clear majority identified the greatest need for these services prior to treatment.15 Taken together, this fits with a model of care focusing on early recognition and treatment of body image difficulties in order to prevent more serious behavioral and psychological problems from arising.
This study can be placed within the larger context of a nationwide movement promoting distress screening in the oncology setting, which is supported by the Institute of Medicine and Commission on Cancer36–39 as well as by the American Psychosocial Oncology Society, Association of Oncology Social Work, and Oncology Nursing Society.40 The American College of Surgeons now requires that patients undergoing treatment for cancer be screened for distress and appropriate referrals be provided for psychosocial care. These standards clearly delineate identification and management of distress as critical for providing high-quality cancer care. As discussed throughout this manuscript, body image concerns are identified as a significant source of distress for cancer patients undergoing reconstructive treatment. As such, conducting screening for body image distress and providing appropriate referrals for psychosocial care would facilitate compliance with accreditation criteria for cancer centers while addressing a highly relevant clinical issue for cancer patients undergoing reconstructive surgery.
This study was developed based on feedback received from reconstructive surgeons in a comprehensive cancer center requesting a screening tool to help them determine when a referral for specialized psychosocial care treating body image difficulties may be warranted. These providers are aware of the depths to which some of their patients struggle to cope with appearance changes resulting from treatment. This type of care would ideally be delivered by a mental health specialist with expertise in treating body image disturbance of cancer patients. The American Cancer Society, American Psychosocial Oncology Society, or Cancer Support Community can assist in locating such professionals locally as well as directing patients to online resources that may be pertinent.26
Additional consideration could be given to using the BICR as part of clinical query or as a clinical tool for the treatment team to prompt discussion surrounding appearance concerns identified by patients. Further understanding of levels of distress, preoccupation with appearance, and avoidance behaviors tied to appearance are important for the treatment team to be aware of and help to address. Apart from making referrals for body image counseling, this tool could also prompt greater time spent in educating patients about what types of appearance changes to expect from initial reconstruction or revision surgery, or to initiate relevant referrals for other psychosocial resources available in their treating facility.
We acknowledge a number of limitations of this study. This study employed a cross-sectional design, and evaluated patients at only a single time-point. We were unable to consider the influence of body image issues for patients prior to cancer diagnosis. Our findings were limited by our sample size, particularly when evaluating results of regression analyses that divided variables into different categories. While we were able to evaluate which survey items showed greater predictive value in identifying patients who were interested in and ultimately enrolled in counseling, we did not examine whether patients benefitted from treatment. We note that the fit indices for our multiple regression models were low, suggesting there is considerable variance not explained in our model. This could be a result of limited power. Alternatively, we may need to consider expanding our screening tool to include additional items.
Although the BICR shows promise in being able to facilitate enhanced psychosocial care for cancer patients undergoing reconstructive surgery, it is clear that further testing and validation of this tool is needed. While our sample include an array of cancer patients undergoing reconstructive surgery (breast, head and neck, and others), a large proportion of these patients were women with breast cancer. Further testing with a larger sample is needed, and particular attention must be given to evaluating the psychometric properties of this instrument as related to reliability and validity.
Conclusions
To our knowledge, this is the first effort to design and test a body image screening tool for cancer patients undergoing reconstructive surgery. This tool was developed based upon feedback from healthcare providers who identified a strong desire for being able to recognize which patients are in need of referral for specialized psychosocial care to treat body image concerns. This work further demonstrates that helping cancer patients cope with body image concerns is an important component of high-quality cancer care that can ultimately optimize psychosocial well-being during treatment and into survivorship.
Acknowledgments
This research was supported in part by the University of Texas MD Anderson Cancer Support Grant CA016672 and funds received from the Kyte Foundation Research Fund provided to the University of Texas MD Anderson Cancer Center, Department of Plastic Surgery.
Footnotes
Financial Disclosures
None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
References
- 1.Pruzinsky T. Social and psychological effects of facial disfigurement: Quality of life, body image and surgical reconstruction. In: Weber RW, Goepfert H, Miller MJ, editors. Basal and Squamous Cell Carcinomas Skin Cancers of the Head and Neck. Philadelphia, PA: Williams & Wilkins; 1996. pp. 357–362. [Google Scholar]
- 2.Lam WW, Li WW, Bonanno GA, et al. Trajectories of body image and sexuality during the first year following diagnosis of breast cancer and their relationship to 6 years psychosocial outcomes. Breast cancer research and treatment. 2012;131:957–67. doi: 10.1007/s10549-011-1798-2. [DOI] [PubMed] [Google Scholar]
- 3.Przezdziecki A, Sherman KA, Baillie A, et al. My changed body: breast cancer, body image, distress and self-compassion. Psycho-Oncology. 2013;22:1872–1879. doi: 10.1002/pon.3230. [DOI] [PubMed] [Google Scholar]
- 4.Bullen TL, Sharpe L, Lawsin C, et al. Body image as a predictor of psychopathology in surgical patients with colorectal disease. Journal of psychosomatic research. 2012;73:459–63. doi: 10.1016/j.jpsychores.2012.08.010. [DOI] [PubMed] [Google Scholar]
- 5.Rosenberg SM, Tamimi RM, Gelber S, et al. Body image in recently diagnosed young women with early breast cancer. Psycho-oncology. 2013;22:1849–55. doi: 10.1002/pon.3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moreira H, Canavarro MC. A longitudinal study about the body image and psychosocial adjustment of breast cancer patients during the course of the disease. European journal of oncology nursing : the official journal of European Oncology Nursing Society. 2010;14:263–70. doi: 10.1016/j.ejon.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 7.Gamba A, Romano M, Grosso IM, et al. Psychosocial adjustment of patients surgically treated for head and neck cancer. Head Neck. 1992;14:218–23. doi: 10.1002/hed.2880140309. [DOI] [PubMed] [Google Scholar]
- 8.Hawighorst-Knapstein S, Fusshoeller C, Franz C, et al. The impact of treatment for genital cancer on quality of life and body image--results of a prospective longitudinal 10-year study. Gynecol Oncol. 2004;94:398–403. doi: 10.1016/j.ygyno.2004.04.025. [DOI] [PubMed] [Google Scholar]
- 9.Sacerdoti RC, Lagana L, Koopman C. Altered Sexuality and Body Image after Gynecological Cancer Treatment: How Can Psychologists Help? Professional psychology, research and practice. 2010;41:533–540. doi: 10.1037/a0021428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rossen P, Pedersen AF, Zachariae R, et al. Sexuality and body image in long-term survivors of testicular cancer. European journal of cancer. 2012;48:571–8. doi: 10.1016/j.ejca.2011.11.029. [DOI] [PubMed] [Google Scholar]
- 11.Falk Dahl CA, Reinertsen KV, Nesvold IL, et al. A study of body image in long-term breast cancer survivors. Cancer. 2010;116:3549–57. doi: 10.1002/cncr.25251. [DOI] [PubMed] [Google Scholar]
- 12.Fingeret MC, Hutcheson KA, Jensen K, et al. Associations among speech, eating, and body image concerns for surgical patients with head and neck cancer. Head & neck. 2013;35:354–60. doi: 10.1002/hed.22980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Taylor-Ford M, Meyerowitz BE, D'Orazio LM, et al. Body image predicts quality of life in men with prostate cancer. Psycho-oncology. 2013;22:756–61. doi: 10.1002/pon.3063. [DOI] [PubMed] [Google Scholar]
- 14.Hewitt M, Herdman R, Holland J, editors. Institute of Medicine: Meeting Psychosocial Needs of Women with Breast Cancer. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- 15.Fingeret MC, Yuan Y, Urbauer D, et al. The nature and extent of body image concerns among surgically treated patients with head and neck cancer. Psychooncology. 2012;21:836–844. doi: 10.1002/pon.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fingeret MC, Vidrine DJ, Reece GP, et al. Multidimensional analysis of body image concerns among newly diagnosed patients with oral cavity cancer. Head & Neck. 2010;32:301–309. doi: 10.1002/hed.21181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fobair P, Stewart SL, Chang SB, et al. Body image and sexual problems in young women with breast cancer. Psycho-Oncology. 2006;15:579–594. doi: 10.1002/pon.991. [DOI] [PubMed] [Google Scholar]
- 18.Harcourt DM, Rumsey NJ, Ambler NR, et al. The psychological effect of mastectomy with or without breast reconstruction: A prospective, multicenter study. Plastic and Reconstructive Surgery. 2003;111:1060–1068. doi: 10.1097/01.PRS.0000046249.33122.76. [DOI] [PubMed] [Google Scholar]
- 19.Atisha DM, Alderman AK, Kuhn LE, et al. The impact of obesity on patient satisfaction with breast reconstruction. Plastic and Reconstructive Surgery. 2008;121:1893–1899. doi: 10.1097/PRS.0b013e3181715198. [DOI] [PubMed] [Google Scholar]
- 20.Colakoglu S, Khansa I, Curtis MS, et al. Impact of Complications on Patient Satisfaction in Breast Reconstruction. Plastic and Reconstructive Surgery. 2011;127:1428–1436. doi: 10.1097/PRS.0b013e318208d0d4. [DOI] [PubMed] [Google Scholar]
- 21.Al-Ghazal SK, Sully L, Fallowfield L, et al. The psychological impact of immediate rather than delayed breast reconstruction. European Journal of Surgical Oncology. 2000;26:17–19. doi: 10.1053/ejso.1999.0733. [DOI] [PubMed] [Google Scholar]
- 22.Fingeret MC, Nipomnick SW, Crosby MA, et al. Developing a theoretical framework to illustrate associations among patient satisfaction, body image and quality of life for women undergoing breast reconstruction. Cancer Treatment Reviews. 2013;39:673–681. doi: 10.1016/j.ctrv.2012.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cash TF. Cognitive-behavioral perspectives on body image. In: Cash TF, Smolak L, editors. Body Image: A Handbookd of Science, Practice and Prevention. New York: Guilford Press; 2011. pp. 39–47. [Google Scholar]
- 24.White CA. Body image dimensions and cancer: a heuristic cognitive behavioural model. Psychooncology. 2000;9:183–92. doi: 10.1002/1099-1611(200005/06)9:3<183::aid-pon446>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 25.Fingeret MC, Teo I, Epner DE. Managing body image difficulties of adult cancer patients: Lessons from available research. Cancer. 2013 doi: 10.1002/cncr.28469. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fingeret MC. Body Image and Disfigurement. In: Duffy J, Valentine A, editors. M.D. Anderson Manual of Psychosocial Oncology. Columbus: McGraw-Hill; 2010. pp. 271–288. [Google Scholar]
- 27.Rumsey N, Byron-Daniel J, Charlton R, et al. Identifying the psychosocial factors and processes contributing to successful adjustment to disfiguring conditions. Bristol, England, Appearance Research Collaboration. 2008 [Google Scholar]
- 28.Fadaei S, Janighorban M, Mehrabi T, et al. Effects of cognitive behavioral counseling on body Image following mastectomy. J Res Med Sci. 2011;16:1047–54. [PMC free article] [PubMed] [Google Scholar]
- 29.Bessell A, Brough V, Clarke A, et al. Evaluation of the effectiveness of Face IT, a computer-based psychosocial intervention for disfigurement-related distress. Psychol Health Med. 2012;17:565–577. doi: 10.1080/13548506.2011.647701. [DOI] [PubMed] [Google Scholar]
- 30.Pirl WF, Muriel A, Hwang V, et al. Screening for psychosocial distress: a national survey of oncologists. J Support Oncol. 2007;5:499–504. [PubMed] [Google Scholar]
- 31.Fallowfield L, Ratcliffe D, Jenkins V, et al. Psychiatric morbidity and its recognition by doctors in patients with cancer. Br J Cancer. 2001;84:1011–5. doi: 10.1054/bjoc.2001.1724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maguire P. Improving the detection of psychiatric problems in cancer patients. Soc Sci Med. 1985;20:819–23. doi: 10.1016/0277-9536(85)90336-3. [DOI] [PubMed] [Google Scholar]
- 33.Annunziata MA, Giovannini L, Muzzatti B. Assessing the body image: relevance, application and instruments for oncological settings. Supportive care in cancer : official journal of the Multinational Association of Supportive Care in Cancer. 2012;20:901–7. doi: 10.1007/s00520-011-1339-x. [DOI] [PubMed] [Google Scholar]
- 34.Temple-Oberle CF, Ayeni O, Cook EF, et al. The breast reconstruction satisfaction questionnaire (BRECON-31): an affirmative analysis. J Surg Oncol. 2013;107:451–5. doi: 10.1002/jso.23258. [DOI] [PubMed] [Google Scholar]
- 35.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–53. doi: 10.1097/PRS.0b013e3181aee807. [DOI] [PubMed] [Google Scholar]
- 36.Adler NE, Page AEK, editors. Institute of Medicine: Cancer care for the whole patient: Meeting psychosocial health needs. Washington, DC: The National Academic Press; 2008. [PubMed] [Google Scholar]
- 37.Fashoyin-Aje LA, Martinez KA, Dy SM. New patient-centered care standards from the commission on cancer: opportunities and challenges. J Support Oncol. 2012;10:107–11. doi: 10.1016/j.suponc.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 38.Clark PG, Bolte S, Buzaglo J, et al. From distress guidelines to developing models of psychosocial care: current best practices. J Psychosoc Oncol. 2012;30:694–714. doi: 10.1080/07347332.2012.721488. [DOI] [PubMed] [Google Scholar]
- 39.American College of Surgeons Commission on Cancer. [Accessed May 21, 2013];Understanding standard 3.2 psychosocial distress screening. Available at: http://www.facs.org/cancer/coc/chronicle0212.pdf.
- 40.Pirl WF, Braun IM, Deshields TL, et al. Implementing Screening for Distress: The Joint Position Statement from the American Psychosocial Oncology Society, Association of Oncology Social Work, and Oncology Nursing Society. 2013 www.apos-society.org. [PubMed] [Google Scholar]