Abstract
Molecular mechanisms that generate biological diversity are rewriting ideas about how evolution proceeds, with implications for treating disease.
Molecular biology and evolutionary biology have been separate disciplines and scientific cultures: The former is mechanistic and focused on molecules; the latter is theoretical and focused on populations. However, these domains are beginning to converge in laboratories addressing molecular mechanisms that explain how evolutionary processes work, and bring these processes to bear on medical problems such as cancer and infectious disease. Each discipline can be viewed as a missing link in the other’s description of biology, and in medicine.
Traditional evolutionary biology began in the 1930s with the “modern synthesis,” which fused Darwin’s theses on phenotypic variation and selection with Mendel’s concepts of genetic inheritance to explain the source of biological diversity. This synthesis predated knowledge that genes were made of DNA and of the structure of DNA and how it replicates. Thus, molecular mechanisms could not be integrated into concepts about how phenotypic variation is generated. Instead, assumptions had to be made about the origins of the variation that drives evolution. Among the cornerstone assumptions were that mutations are the sole drivers of evolution; mutations occur randomly, constantly, and gradually; and the transmission of genetic information is vertical from parent to offspring, rather than horizontal (infectious) between individuals and species (as is now apparent throughout the tree of life). But discoveries of molecular mechanisms are modifying these assumptions.
In at least two ways, heritable variation can be generated by proteins, not DNA (1). Spontaneously self-aggregating alternative conformations of some proteins—prions—can flip into their aggregated state and change a cell’s phenotype in an environmentally responsive manner with no change to DNA. The change is transmissible vertically, parent to offspring cell, as well as horizontally, to other cells in which the proteins come in contact. Another mechanism involves chaperones such as heat shock protein 90 (Hsp90), proteins that massage subideal (mutant) proteins into functional conformations but abandon their regular client proteins during heat and other stresses that destabilize proteins. This causes a stress-inducible release of phenotypic diversity, which may drive evolution (with phenotypes ultimately stabilized by subsequent genetic changes). Both of these molecular mechanisms of protein-based inheritance are major departures from the modern synthesis views of solely mutation-directed variation, solely genetic inheritance, and independence of the generation of variation from environmental conditions.
Similarly, transient errors in mRNA synthesis can also cause heritable non–DNA-based phenotypic change. This is observed when low-abundance transcriptional regulators are affected by transcription errors. This disruption can cause a cell to alter its gene expression, resulting in a phenotype that may be heritable (2).
Even the assumption that mutations are random, constant, and gradual has been revised on the basis of molecular mechanisms of mutagenesis. For example, in bacteria, responses to environmental stress can activate mutagenesis mechanisms that increase mutation rate, which can potentially increase the ability of a cell to evolve, specifically when it is poorly adapted to its environment (when stressed). Most of a 93-gene network that promotes mutagenesis in Escherichia coli is devoted to sensing stress and activating stress responses that direct the bacterium to mutate when stressed (3). Stress responses also up-regulate mutagenesis in yeast (4) and human cancer cells (5) and underlie mutations induced by antibiotics that cause resistance to those very drugs, and others (6).
Mutations are also nonrandom in genomic space—for example, forming hot spots at DNA double-strand breaks, as demonstrated in bacteria (7) and suggested by local clusters of mutations in cancer genomes (8, 9). In cancer, the mutations are generated by cytidine deaminases that target single-stranded DNA regions (10), presumably at DNA breaks. Additionally, the structure of the human genome with regard to repetitive DNA (11) and three-dimensional structure (12, 13) predisposes certain regions to copy number variation because of recombination between repeats (11) or proximity in the nucleus of nonrepeated sequences (12, 13). The long-standing assumption of random, constant, and gradual mutagenesis is refuted by observations that mutations occur more frequently when cells are maladapted to their environments, together with the discoveries of mechanisms by which mutations are targeted to specific genomic structures. These modifications of the modern synthesis assumptions could not have been predicted or found without exploration of molecular mechanisms.
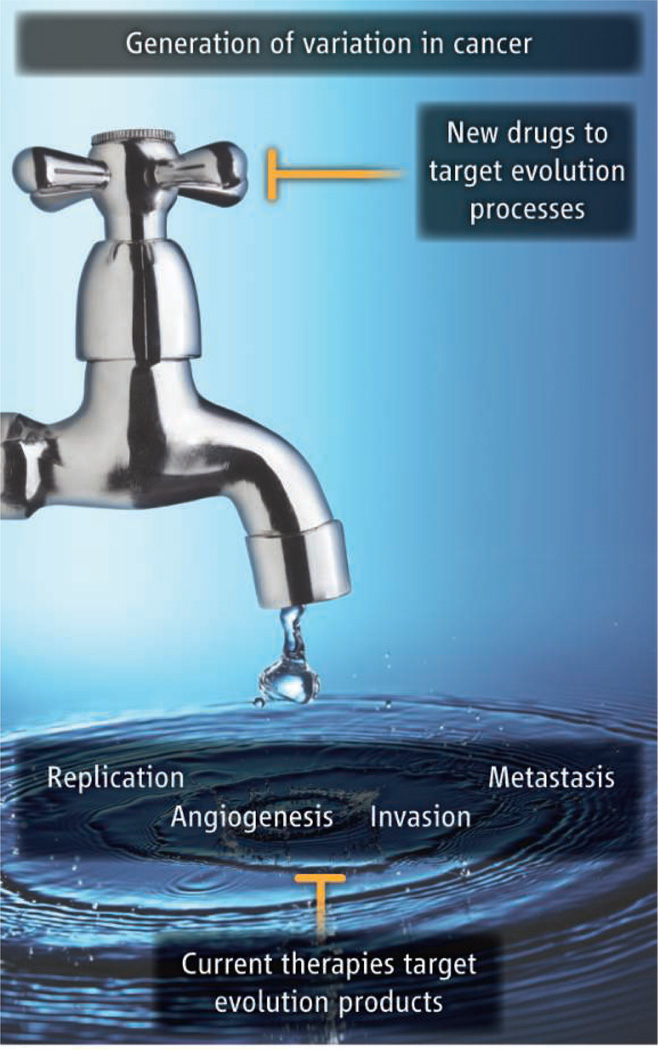
Such a fusion of molecular mechanisms with evolution is needed because cancer and infectious disease are evolutionary problems that could be attacked at the molecular level. For example, when a pathogen defeats a host, it has won an evolutionary arms race with the host immune system; cancer, too, proceeds by the generation of phenotypic variation and selection of those cells that are most fit to propagate (see the figure). Deep understanding of the mechanisms that generate variation at the molecular level invites the possibility of fundamentally new antipathogen and anticancer therapies: ones that block the ability to evolve, instead of (or in addition to) traditional chemotherapies that kill cells or stop them from growing. For example, inhibitors of Hsp90 are succeeding as antifungal therapy adjuncts that block the development of resistance to standard drugs (14) and are in trials as chemotherapeutic agents. Similarly, the heat shock response factor that regulates Hsp90 has emerged as a promising therapeutic target in cancer (15). Conventional cancer chemotherapies target the products of tumor evolution (such as DNA replication, altered cell signaling that promotes rapid proliferation, or the release of factors by cancer cells that spur angiogenesis). “Anti-evolvability” therapies could potentially stem the torrent of generation of variation that creates all of the products of evolution, whether targetable directly by drugs or not, thereby blocking the processes of tumor or pathogen evolution (see the figure).
“Anti-evolvability” therapies.
Multiple molecular mechanisms including mutation, protein conformational change, and epigenetic gene silencing create phenotypic variation that, with selection for the fittest cells, drives cancer initiation, progression, and resistance. Whereas conventional antiproliferative therapies target the products of this somatic cell evolution, proposed new therapies that block the evolutionary processes by which phenotypic variation is generated may be effective.
The evolutionary biologist Theodosius Dobzhansky famously noted that “nothing in biology makes sense except in the light of evolution,” but perhaps, too, “nothing in evolution makes sense except in the light of biology.” Although the latter might be an exaggeration, an important gap is being filled by molecular understanding of the genesis of variation that confers the ability to evolve.
Acknowledgments
Stimulated by the Gordon Research Conference on Molecular Mechanisms in Evolution, June 2013. Supported by NIH Director’s Pioneer Award DP1-CA174424 and NIH grants R01-GM53158 and R01-CA85777 (S.M.R.) and by NIH Director’s New Innovator Award DP2-OD008371 (C.Q.).
References and Notes
- 1.Lindquist S. Cold Spring Harb. Symp. Quant. Biol. 2009;74:103. doi: 10.1101/sqb.2009.74.043. [DOI] [PubMed] [Google Scholar]
- 2.Gordon AJ, et al. PLOS Biol. 2009;7:e44. doi: 10.1371/journal.pbio.1000044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Al Mamun AA, et al. Science. 2012;338:1344. doi: 10.1126/science.1226683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shor E, Fox CA, Broach JR. PLOS Genet. 2013;9:e1003680. doi: 10.1371/journal.pgen.1003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bindra RS, Crosby ME, Glazer PM. Cancer Metastasis Rev. 2007;26:249. doi: 10.1007/s10555-007-9061-3. [DOI] [PubMed] [Google Scholar]
- 6.Gutierrez A, et al. Nat. Commun. 2013;4:1610. doi: 10.1038/ncomms2607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shee C, Gibson JL, Rosenberg SM. Cell Rep. 2012;2:714. doi: 10.1016/j.celrep.2012.08.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nik-Zainal S, et al. Cell. 2012;149:979. [Google Scholar]
- 9.Roberts SA, et al. Mol. Cell. 2012;46:424. doi: 10.1016/j.molcel.2012.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burns MB, et al. Nature. 2013;494:366. doi: 10.1038/nature11881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Girirajan S, Campbell CD, Eichler EE. Annu. Rev. Genet. 2011;45:203. doi: 10.1146/annurev-genet-102209-163544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De S, Michor F. Nat. Biotechnol. 2011;29:1103. doi: 10.1038/nbt.2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fudenberg G, Getz G, Meyerson M, Mirny LA. Nat. Biotechnol. 2011;29:1109. doi: 10.1038/nbt.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cowen LE. Curr. Opin. Microbiol. 2013;16:377. doi: 10.1016/j.mib.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Santagata S, et al. Science. 2013;341:1238303. doi: 10.1126/science.1238303. [DOI] [PMC free article] [PubMed] [Google Scholar]