Significance
Retinal damage and resulting irreversible vision loss are feared complications of rapid and substantially elevated intraocular pressure (IOP) in acute glaucoma. An inflammatory response to retinal ischemia/reperfusion injury involving Toll-like receptor 4 (TLR4) and IL-1β has been implicated in disease pathogenesis; however, the underlying mechanisms remain incompletely understood. This study demonstrates the critical role of caspase-8 in IOP-induced cell death in rodent models of acute glaucoma. TLR4 signaling, mediated by caspase-8, was crucial for the activation of Nod-like receptor family, pyrin domain containing 1 (NLRP1)/NLRP3 inflammasomes and processing of IL-1β. Inhibition of either TLR4 or caspase-8 signaling significantly blocked production of IL-1β and attenuated retinal ischemic damage. These findings identify a mechanism of retinal retinal ganglion cell death and provide a previously unidentified treatment strategy to preserve vision in acute glaucoma.
Keywords: retinal ischemia/reperfusion injury, cell apoptosis
Abstract
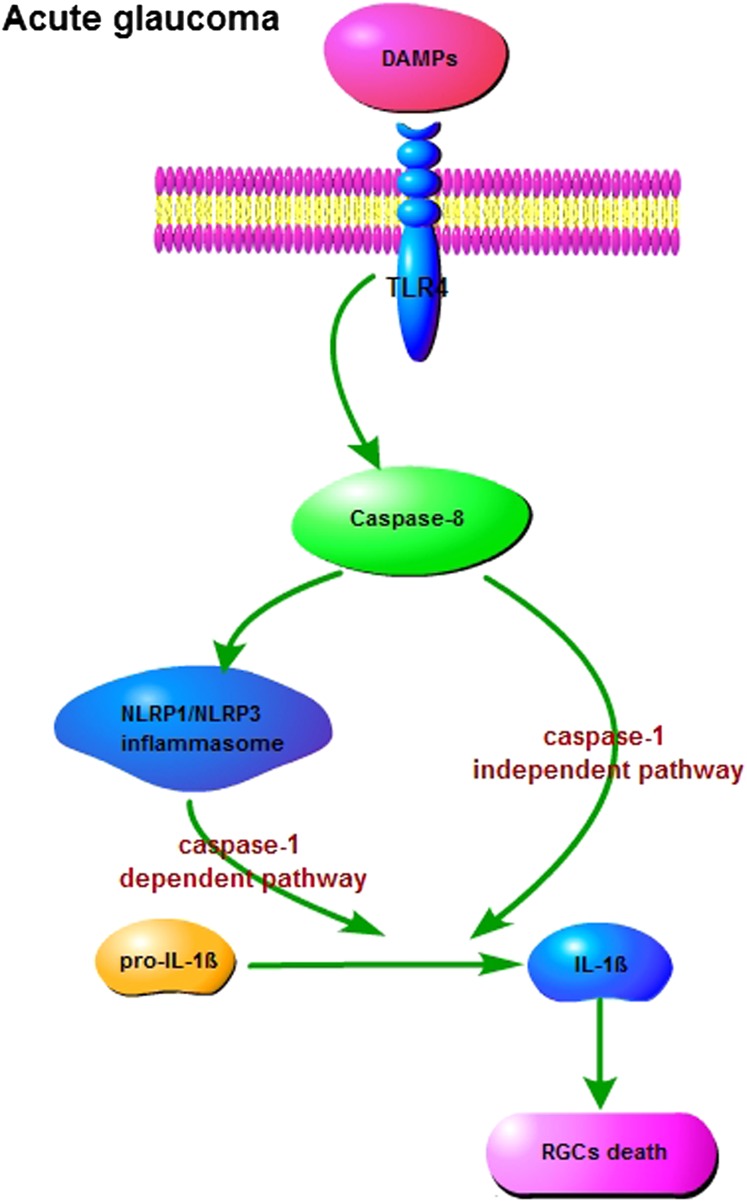
Acute glaucoma is a sight-threatening condition characterized by a sudden and substantial rise in intraocular pressure (IOP) and consequent retinal ganglion cell (RGC) death. Angle closure glaucoma, a common cause of glaucoma in Asia that affects tens of millions of people worldwide, often presents acutely with loss of vision, pain, and high IOP. Even when medical and surgical treatment is available, acute angle closure glaucoma can cause permanent and irreversible loss of vision. Toll-like receptor 4 (TLR4) signaling has been previously implicated in the pathogenesis of IOP-induced RGC death, although the underlying mechanisms are largely unknown. In the present study, we used an acute IOP elevation/glaucoma model to investigate the underlying mechanism of RGC death. We found that TLR4 leads to increased caspase-8 expression; this elevation increases IL-1β expression and RGC death via a caspase-1–dependent pathway involving Nod-like receptor family, pyrin domain containing 1 (NLRP1)/NLRP3 inflammasomes and a caspase-1–independent pathway. We show that inhibition of caspase-8 activation significantly attenuates RGC death by down-regulating the activation of NLRP1 and NLRP3, thus demonstrating the pivotal role of caspase-8 in the TLR4-mediated activation of inflammasomes. These findings demonstrate collectively a critical role of caspase-8 in transducing TLR4-mediated IL-1β production and RGC death and highlight signal transduction in a caspase-1–dependent NLRP1/NLRP3 inflammasome pathway and a caspase-1–independent pathway in acute glaucoma. These results provide new insight into the pathogenesis of glaucoma and point to a treatment strategy.
Acute glaucoma is a significant cause of permanent vision loss and irreversible blindness worldwide (1). It is most common among people of Asian descent, in part due to their having a more crowded anterior chamber (2, 3). With a rapid increase in intraocular pressure (IOP) to levels exceeding retinal perfusion pressure, there is resulting retinal ischemia and retinal ganglion cell (RGC) death. Individuals with angle closure glaucoma are much more likely to lose vision and become blind than those with primary open-angle glaucoma (4). The precise mechanisms by which elevated IOP leads to RGC death are not well understood. Accumulating evidence suggests that overactivated microglia have pivotal roles in triggering neurotoxicity in the CNS, including retinal inflammatory responses (5, 6), by producing proinflammatory factors such as IL-1β. IL-1β production is tightly controlled as part of the innate immune response in the CNS (7).
Toll-like receptors (TLRs) and Nod-like receptors (NLRs) are two key pattern recognition receptors (PRRs) in the initiation of the innate immune response (8–10). TLR4 has been shown to have a central role in retinal and CNS ischemia/reperfusion (I/R) injuries (11–13). Neuronal death following ischemic injury activates intense inflammation, which triggers TLR4 signaling. It has been demonstrated that TLR4-deficient mice are protected against ischemic brain damage (14, 15). TLRs are membrane-spanning receptors and NLRs are cytoplasmic sensors that oligomerize to form a platform for the inflammasome, a multisubunit complex that activates caspase-1 to process pro–IL-1β into its mature form. IL-1β secretion is a well-characterized outcome of TLR and inflammasome cooperation. TLRs induce transcriptional activation of pro–IL-1β, which is proteolytically processed via inflammasome activation (16, 17). Studies have shown that neutralization of inflammasome activity results in less severe tissue pathologies following thromboembolic stroke (18, 19). Currently, the exact function, complex molecular mechanisms, and precise interaction between TLRs and inflammasomes in the development of retinal ischemic injury remain elusive.
Caspases are a family of aspartate-specific cysteine proteases with a well-characterized function in apoptotic signaling. Caspase-8 is implicated as an initiator caspase in death receptor-induced signaling of apoptosis (20, 21). Recent reports have uncovered novel nonapoptotic functions of caspase-8 and caspase-3, showing that they induce microglia neurotoxicity and the production of IL-1β without causing microglia death (22, 23). However, the underlying mechanism of caspase-8 activation in promoting IL-1β secretion is unclear. Thus, the potential roles of TLR4, inflammasomes, and caspase-8 signaling in the development of IOP-induced retinal damage and RGC death remain to be clarified.
In this study, we investigated the signaling pathway mediating RGC death and identified the key players between TLR4 and IL-1β. It is demonstrated that IOP-induced retinal ischemia directly increases TLR4 expression, triggering caspase-8 signaling to activate Nod-like receptor family, pyrin domain containing 1 (NLRP1) and NLRP3 inflammasomes and IL-1β production in both mouse and rat models. Inhibition of caspase-8 could completely suppress IL-1β processing in IOP-induced retinal damage, whereas inhibition of caspase-1 only partially reduced levels of IL-1β, implying that caspase-8 processed IL-1β via a caspase-1–dependent, NLRP1/NLPR3 pathway and a caspase-1-independent pathway. Unlike in vitro LPS stimulating caspase-3 activation in microglia (22), IOP-induced ischemia did not significantly drive caspase-3 activation in the early stage of acute glaucoma, suggesting that caspase-8– rather than caspase-3–induced inflammatory responses may be responsible for RGC death with elevated IOP in the early retinal damage of acute glaucoma. These results demonstrate that caspase-8 is a key link between TLR4 and inflammasomes in IL-1β processing and that it contributes to IOP-induced RGC death. Targeted inhibition of TLR4 and caspase-8 signaling could significantly attenuate retinal ischemic damage and RGC death by regulating the activation of inflammasomes and the production of IL-1β.
Results
TLR4 Signaling Is Involved in the Development of IOP-Induced RGC Death and Knockout of TLR4-Reduced Ischemic Damage.
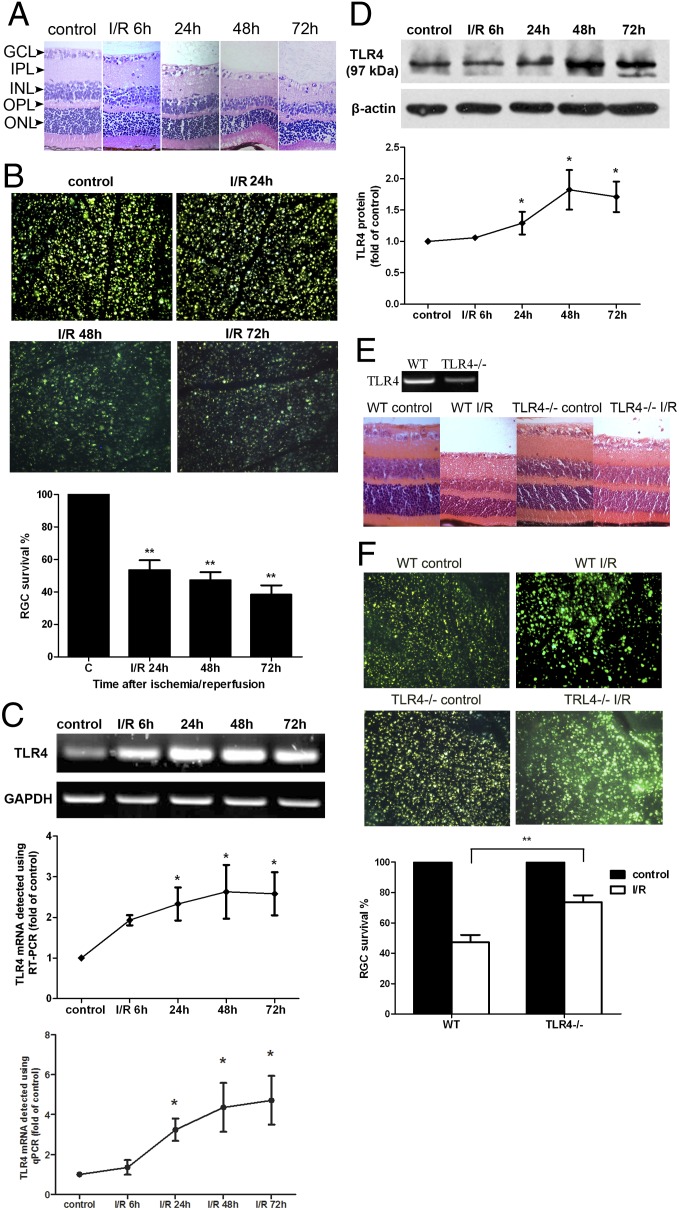
TLR4 signaling activation is actively involved in tissue damage following CNS ischemia (24, 25). We further clarified the role of TLR4 in the development of IOP-induced retinal ischemia by using wild-type (WT) and TLR4−/− mice. When acute elevation of IOP was induced in WT mice, we found that retinal damage occurred rapidly, with retinal edema, vacuolar degeneration, and condensation of nuclear chromatin. Hematoxylin and eosin (H&E) staining showed that retinal thickness was decreased as early as 6 h after reperfusion (Fig. 1A). In addition, Fluorogold (FG)-labeling analysis demonstrated that the number of RGCs began to decrease 24 h after reperfusion (Fig. 1B). Retinal ischemia rapidly increased TLR4 mRNA expression at 6 h after reperfusion-detected by using both semiquantitative reverse transcription PCR (sqRT-PCR) and quantitative real-time PCR (qPCR), and increased TLR4 protein levels (Fig. 1 C and D). The severity of retinal damage and the amount of RGC death was significantly decreased in TLR4 knockout mice compared with WT mice, indicating the pivotal role of TLR4 in mediating the effects of IOP-induced retinal ischemia (Fig. 1 E and F).
Fig. 1.
TLR4 signaling was involved in the pathogenesis of IOP-induced RGC death. (A) H&E staining of retinal cross-sections showed degeneration of RGCs and a decrease in the mean thickness of retinal tissue of ischemia/reperfusion (I/R) mice at different time points after reperfusion. GCL, ganglion cell layer; INL, inner nuclear layer; IPL, inner plexiform layer; ONL, outer nuclear layer; OPL, outer plexiform layer (n = 6). (Scale bar: 10 μm.) (B) FG labeling showed that the number of surviving cells in the RGC layer decreased significantly after IOP-induced injury compared with controls (n = 12). (C) sqRT-PCR and qPCR analysis of TLR4 gene expression in ischemic retina at different time points after reperfusion. Levels of TLR4 mRNA were elevated in ischemic retina compared with controls (n = 8). (D) Western blot analysis showed that TLR4 protein levels were also up-regulated in ischemic retina after reperfusion (n = 12). (E and F) Knockdown of TLR4 reduced retinal ischemic damage and RGC death. A sham procedure was performed in the contralateral eyes, which served as controls (n = 8 each for WT and TLR4−/− mice). Representative images are shown. Data are presented as mean ± SD of the fold increase compared with controls. *P < 0.05, **P < 0.001.
Caspase-8 Has a Key Role in IOP-Induced RGC Death and Is Activated by TLR4.
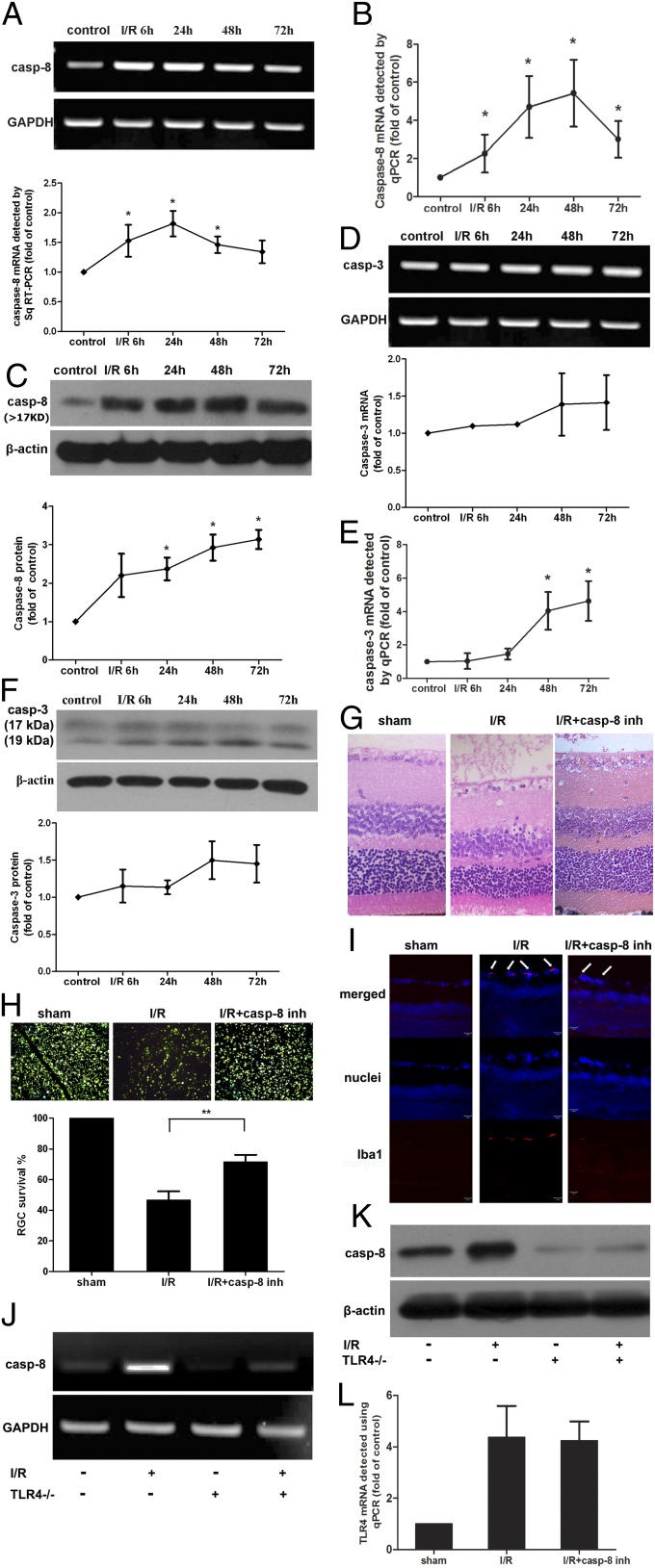
Because activation of caspase-8 and caspase-3 signaling has been implicated in promoting neurotoxicity and IL-1β production in CNS tissue ischemia (22), we therefore explored the potential role of the caspase-8 and caspase-3 pathways in IOP-induced retinal damage. Our data showed that caspase-8 expression was rapidly increased in ischemic retinal tissue as early as 6 h following reperfusion in terms of mRNA levels, detected by using sqRT-PCR and qPCR, and protein levels, which was accordant with the up-regulation of TLR4 (Fig. 2 A–C). The expression of caspase-8 mRNA gradually decreased after 48 h following reperfusion, but its protein levels were continuously elevated until 72 h, implying that caspase-8 protein production might be affected by variable parameters such as synthesis and cleavage in the later stages of IOP-induced retinal injury. However, levels of caspase-3, a well-known executioner protease of apoptosis following brain ischemia, were only slightly up-regulated in ischemic retinal tissue until 48 h after reperfusion (Fig. 2 D–F).
Fig. 2.
Increased production of caspase-8, induced by TLR4, contributed to the pathogenesis of IOP-induced retinal damage. Caspase-8 gene (A and B) (n = 10) and protein expression (C) (n = 15) were significantly up-regulated in ischemic retina compared with controls. Caspase-3 mRNA levels (D and E) (n = 10) and protein levels (F) (n = 15) were mildly increased in ischemic retina until 48 h after reperfusion. Inhibition of caspase-8 via Z-IETD-fmk injection into the vitreous cavity significantly attenuated retinal ischemic damage (G) (n = 9), RGC death (H) (n = 9), and microglia activation (I) (n = 9). By knocking out the TLR4 gene using TLR4−/− mice, the expression of caspase-8 was reduced following IOP-induced injury (J and K) (n = 6) compared with WT mice (n = 6). Inhibition of caspase-8 had no effect on the expression of TLR4 in ischemic retina (L) (n = 6). Representative images taken 48 h after I/R injury are shown. Data are presented as mean ± SD; *P < 0.05, **P < 0.001.
To explore the role and mechanism of caspase-8 activation in IOP-induced retinal damage, we then injected a caspase-8 inhibitor, Z-IETD-FMK-fmk, into the vitreous of C57BL/6 mice after the onset of retinal ischemia and killed the mice 48 h after reperfusion. Inhibiting caspase-8 in the vitreous of the mice significantly attenuated retinal damage and RGC death compared with untreated mice, indicating that caspase-8 signaling was actively involved in IOP-induced retinal ischemia (Fig. 2 G and H). The activation of microglia was also suppressed by inhibiting caspase-8 activity (Fig. 2I).
Because the expression levels of both TLR4 and caspase-8 increased after IOP-induced retinal damage, we investigated whether TLR4 signaling contributes to the activation of caspase-8. In TLR4−/− mice, IOP-induced retinal injury did not increase caspase-8 production (Fig. 2 J and K). Therefore, TLR4 signaling plays a predominant role in the innate immune response of retinal ischemia by promoting the activation of caspase-8 signaling. Inhibition of caspase-8 had no influence on the production of TLR4 in IOP-induced retinal injury (Fig. 2L).
NLRP1 and NLRP3 Inflammasomes Are Activated by TLR4 Signaling.
Recent studies have demonstrated that inflammasomes have a key role in the processing of IL-1β, impacting the course of CNS infection, autoimmune disease, and injury (26–28). However, the potential role of inflammasomes in IOP-induced RGC death has not been explored. We therefore tested the involvement of the best-characterized inflammasomes, NLRP1 and NLRP3, in IOP-induced retinal damage in mice.
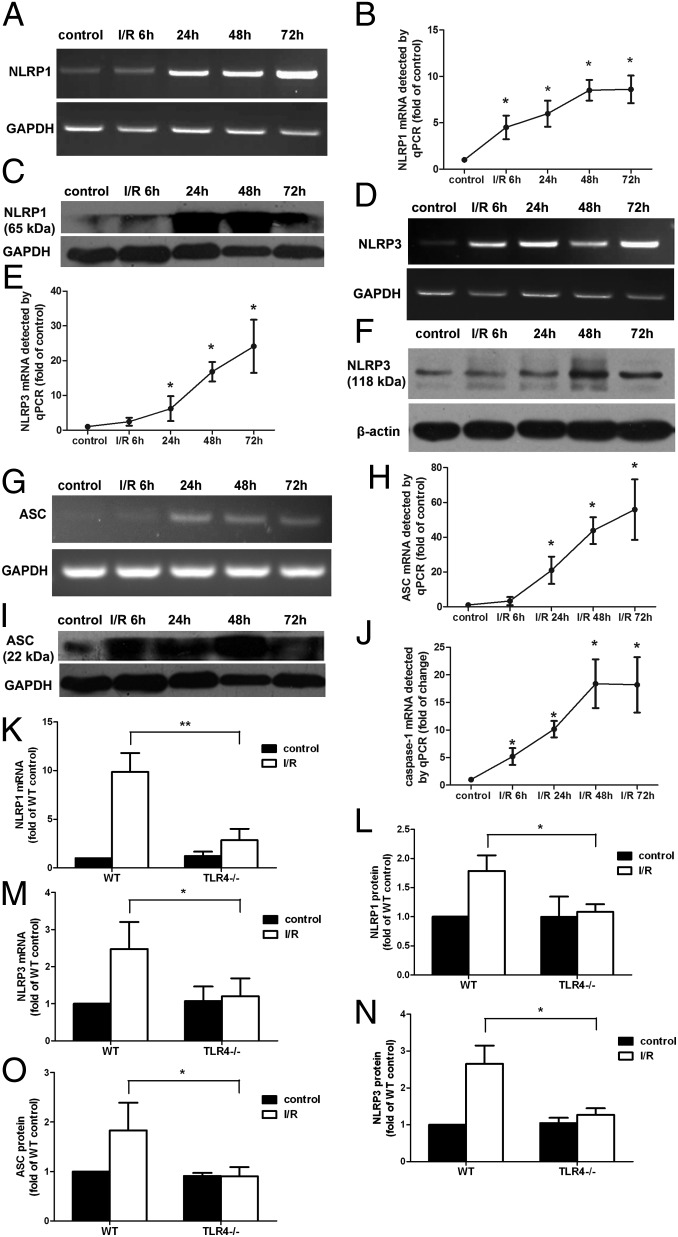
Our findings showed that the expression of NLRP1, NLRP3, Apoptosis-associated speck-like protein containing CARD (ASC), and caspase-1 were elevated as rapidly as 6 h after reperfusion in retinal I/R injury (Fig. 3 A–J). We then examined the role of TLR4 in inflammasome activation after IOP-induced retinal damage. Selective knockdown of TLR4 was associated with reduced activation of NLRP1, NLRP3, and ASC, demonstrating that TLR4 induces the activation of NLRP1 and NLRP3 inflammasomes in IOP-induced RGC death (Fig. 3 K–O and Fig. S1).
Fig. 3.
The production of NLRP1 and NLRP3 inflammasomes was increased in ischemic retina, mediated by TLR4 signaling. NLRP1 and NLRP3 gene expression (A, B, D, and E) (n = 10, both) and protein expression (C and F) (n = 15, both) in ischemic retina were significantly up-regulated compared with controls. ASC mRNA levels detected using sqRT-PCR (G) and qPCR (H) (n = 6, both) and protein expression (I) (n = 15) were also up-regulated in IOP-induced retinal injury. (J) The expression of caspase-1 was correspondingly elevated in ischemic retinal tissue (n = 6). Knockdown of TLR4 reduced the production of NLRP1 and NLRP3 inflammasomes and ASC (K–O) (n = 12, all). Representative images are shown. Data are presented as mean ± SD; *P < 0.05, **P < 0.001.
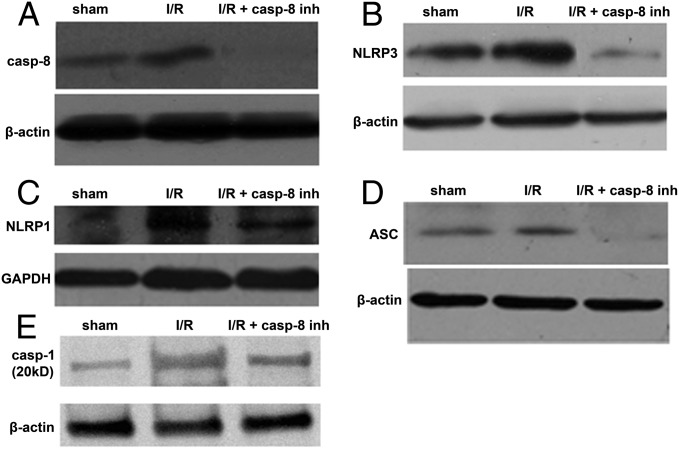
Caspase-8 Regulates the Activation of NLRP1 and NLRP3 Inflammasomes.
Our above findings showed that caspase-8 has a pivotal role in retinal ischemic damage and is activated by TLR4. TLR4 signaling also induces NLRP1/NLRP3 inflammasome activation in IOP-induced RGC death. We then hypothesized that TLR4-induced inflammasome activation may be mediated by caspase-8 signaling in retinal ischemia. The caspase-8 inhibitor Z-IETD-FMK-fmk was injected into the vitreous of C57BL/6 mice just after the onset of retinal ischemia, and the mice were killed 48 h after reperfusion. The expression of NLRP1, NLRP3, ASC, and caspase-1 decreased significantly after the inhibition of intraocular caspase-8 (Fig. 4). Together, these results reveal a previously unidentified role for caspase-8 signaling in IOP-induced retinal damage. TLR4 signaling in response to highly elevated IOP induces caspase-8, which regulates the activation of NLRP1 and NLRP3 inflammasomes.
Fig. 4.
Caspase-8 signaling regulated the activation of NLRP1 and NLRP3 inflammasomes in IOP-induced retinal damage. The intravitreous injection of the caspase-8 inhibitor Z-IETD-fmk (20 μM) (A) significantly attenuated the activation of NLRP3 (B), NLRP1 (C), ASC (D), and caspase-1 (E) (n = 9, all) following retinal ischemic injury. Representative images are shown.
Caspase-8 Is Required for Processing of IL-1β in IOP-Induced RGC Death.
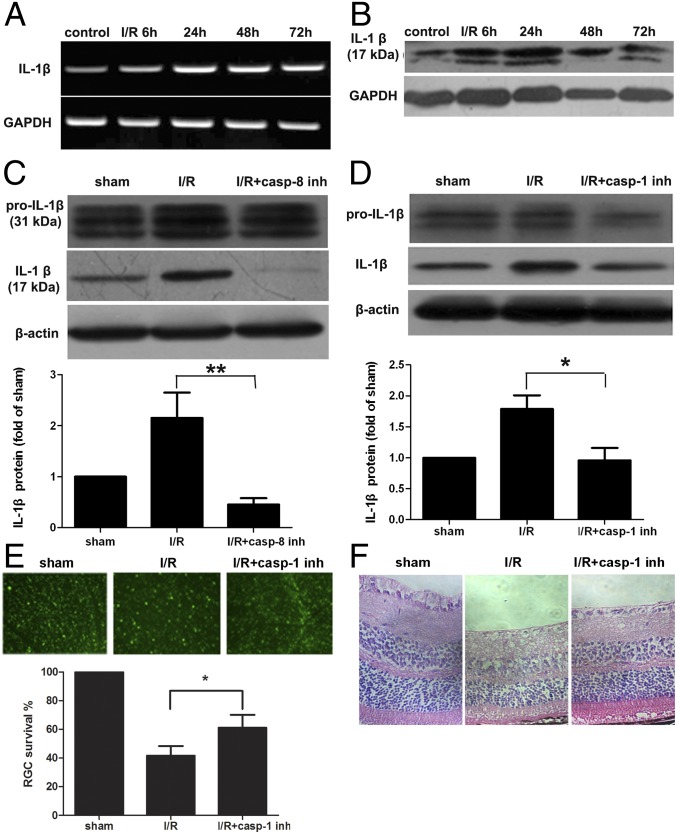
Caspase-8 has been linked to IL-1β processing in response to lipopolysaccharide stimulation of TLR4 signaling (29, 30). The above data showed that TLR4-induced caspase-8 regulated NLRP1/NLRP3 inflammasome activation in IOP-induced RGC death. We therefore explored the potential role and underlying mechanism of caspase-8 in processing IL-1β after IOP-induced retinal damage. The expression of IL-1β was detected at different time points following reperfusion. IL-1β was up-regulated in ischemic retinal tissue as rapidly as 6 h after IOP elevation and peaked after 48 h, as shown by mRNA and protein levels (Fig. 5 A and B). Accordingly, IL-1β processing was almost completely blocked following intravitreous injection of caspase-8 inhibitor (Fig. 5C).
Fig. 5.
Caspase-8 signaling was required for processing of IL-1β only partially through caspase-1–dependent NLRP1 and NLRP3 inflammasome activation. Gene expression (A) (n = 10) and protein expression of IL-1β (B) (n = 15) were elevated in ischemic retina at different time points after reperfusion. (C) The intravitreous injection of caspase-8 inhibitor, Z-IETD-fmk (20 μM), completely inhibited the processing of IL-1β (n = 9). (D) The intravitreous injection of caspase-1 inhibitor, Z-YVAD-fmk (20 μM), partially reduced the processing of IL-1β (n = 9). (E and F) Inhibition of caspase-1 attenuated the damage and RGC death from retinal ischemia (n = 12). Representative images are shown. Data are presented as mean ± SD; *P < 0.05, **P < 0.001.
NLR-mediated caspase-1 activation is considered important for the processing of IL-1β in pathogenic stimulation (23, 31). The role of caspase-1–dependent NLRP1/NLRP3 inflammasomes in the processing of IL-1β was further investigated by using intravitreous injection of a caspase-1 inhibitor, z-YVAD-fmk. Caspase-1 inhibition only partially prevented IL-1β processing in mice with IOP-induced retinal injury (Fig. 5D), in contrast to complete inhibition of IL-1β production by caspase-8 inhibition. Furthermore, inhibition of caspase-1 decreased the extent of retinal injury and RGC death in IOP-induced retinal damage (Fig. 5 E and F), implying that caspase-1 exerts its effect in a retinal injury model via IL-1β production. Overall, these results indicate that TLR4-induced caspase-8 activation promotes the processing of IL-1β in retinal ischemic damage, not only by the caspase-1–dependent NLRP1/NLRP3 pathway but also by a caspase-1–independent pathway.
TLR4/Caspase-8/IL-1β Axis Is also Activated in a Rat Model of Acute Glaucoma.
We further validated the role of the TLR4/caspase-8/IL-1β axis in retinal ischemic injury by using a rat model of acute glaucoma (Fig. 6). mRNA levels of TLR4, caspase-8, NLRP1, NLRP3, ASC, and IL-1β were significantly up-regulated in rat retinal tissue as early as 6 h after IOP elevation (Fig. S2 A, B, and D–G). In contrast, expression of caspase-3 was not significantly increased in the early stage of acute glaucoma, but was increased 48 h after IOP elevation (Fig. S2C). Furthermore, we demonstrated that inhibition of caspase-8 in the vitreous reduced the activation of NLRP1 and NLRP3 and completely suppressed the production of IL-1β in rat models of acute glaucoma (Fig. S3 A–C). Inhibition of caspase-1 only partially suppressed the production of IL-1β (Fig. S3D). These results are similar to those seen in mouse models. In summary, the TLR4/caspase-8/IL-1β axis is activated in rats with IOP-induced retinal injury, and caspase-8 is necessary for the production of IL-1β partially through the activation of NLRP1/NLRP3 inflammasomes.
Fig. 6.
Diagram illustrating the proposed pathway by which TLR4/caspase-8/inflammasome up-regulation induces the processing of IL-1β and promotes the inflammatory response in acute glaucoma.
Discussion
In this study, we found that elevated IOP triggers increased expression of TLR4, initiating increased caspase-8 and NLRP1/NLRP3 expression, and production of IL-1β, all of which participate in the innate immune response to IOP-induced retinal ischemia. Consistent with this notion, knockout of TLR4 signaling significantly attenuated retinal ischemic damage and RGC death and suppressed the activation of caspase-8 signaling. Further support came from the inhibition of caspase-8, which had a therapeutic effect on IOP-induced retinal injury by down-regulating the expression of NLRP1 and NLRP3. We showed that the inflammasome processes IL-1β via caspase-1 activation, but inhibition of caspase-1 only partially blocked IL-1β maturation. Thus, caspase-8 signaling promotes the processing of IL-1β by both the caspase-1–dependent NLRP1/NLRP3 pathway and the caspase-1–independent pathway. The present study elucidated the role and mechanisms of TLR4 in the development of IOP-induced retinal damage. It remains to be determined whether these results are translatable to acute angle closure glaucoma in humans. Particularly at the lamina cribrosa, the site of putative pressure-induced damage in glaucoma (32), the anatomy of the optic nerve of the mouse is different from that of the human. Moreover, the high levels of induced IOP used in the current study may exceed those measured in patients with acute angle closure. Further study is needed to verify this.
Inflammasomes are molecular platforms for caspase-1 activation and IL-1β maturation, and are engaged in the innate immune responses triggered by cellular infection or stress (17). Our findings demonstrated that up-regulated NLRP1 and NLRP3 were associated with elevated IOP and that elimination of TLR4 diminishes the increase in inflammasome activity, indicating that TLR4 regulates the activation of NLRP1 and NLRP3 during the development of IOP-induced RGC death.
Caspase-8 is mainly considered an initiator of apoptotic cell death that is activated by receptors of the TNF/NGF family (33). Recently, multiple nonapoptotic roles of caspase-8 have been uncovered, especially its neuroinflammatory functions (22, 23, 31). Microglia activation releases proinflammatory factors, which mediate the pathogenesis of CNS diseases, including those affecting the retina (34). Our findings demonstrated that inhibition of caspase-8 signaling decreased the activation of NLRP1, NLRP3, ASC, and caspase-1, implicating caspase-8 as an important link between TLR4 and inflammasomes and a mediator of IOP-induced RGC death. Gurung et al. also observed that caspase-8 could regulate the activation of caspase-1 in cultured macrophages (35).
Although NLR-assembled inflammasomes are believed to be responsible for caspase-1–dependent processing of pro–IL-1β (36), some reports have found that inhibiting caspase-1 only slightly reduces pro–IL-1β processing in macrophages, indicating that a caspase-1–independent pathway also mediates the processing of pro–IL-1β (37). The present study illustrated that inhibition of caspase-8 signaling almost completely suppressed the processing of IL-1β in mice with IOP-induced retinal damage compared with untreated controls, suggesting that caspase-8 signaling plays a central role in the maturation of IL-1β during retinal ischemic damage. Recent studies have reported that recombinant caspase-8 can cleave pro–IL-1β in vitro at exactly the same site that caspase-1 does (23). Given these findings, it is conceivable that caspase-8 might assemble inflammasomes and directly cleave pro–IL-1β in the pathogenesis of IOP-induced RGC death.
In conclusion, our study showed that TLR4 signaling induced the activation of caspase-8, NLRP1, NLRP3, and the IL-1β cascade. Caspase-8 signaling is a pivotal link between TLR4 and inflammasomes and is essential for the maturation of IL-1β via a caspase-1–dependent, NLRP1/NLRP3-mediated pathway and a caspase-1–independent pathway. Our study provides insight into the role of inflammatory response in IOP-induced RGC death and indicates that suppression of the TLR4/caspase-8/IL-1β axis is a potential therapeutic strategy for treatment of RGC death and glaucoma.
Methods
Animal Model of Acute Glaucoma.
Adult male C57BL/6 mice, TLR4−/− mice, and female Sprague–Dawley rats were purchased from the model animal research center of Zhongshan University and Nanjing University. Animal care and use strictly conformed to the Association for Research in Vision and Ophthalmology Statement for the Use of Animals in Ophthalmic and Vision Research, and the study was approved by the Committee of Animal Care of the Zhongshan Ophthalmic Center (2011-038).
The mice and rats were anesthetized by using an i.p. injection of a mixture of 100 mg/kg ketamine and 10 mg/kg xylazine. The corneas were topically anesthetized with 0.5% tetracaine hydrochloride, and the pupils were dilated with 1% tropicamide. The anterior chamber of the right eye was cannulated with a 30-gauge infusion needle connected to a normal saline reservoir, which was elevated to maintain an intraocular pressure of 110 mmHg (Tono-Pen; Medtronic Solan) for 60 min. Retinal ischemia was confirmed by whitening of the iris and loss of the red reflex, and subsequent reperfusion was evident by the return of the red reflex. A sham procedure performed without elevating the pressure in the contralateral left eye served as the control. After 1 h, the needle was withdrawn, and intraocular pressure was normalized. The animals were allowed to recover for 6, 24, 48, or 72 h before sacrifice.
Intravitreal Injections.
The experimental eyes were injected with the caspase-8 inhibitor Z-IETD-fmk, the caspase-1 inhibitor Z-YVAD-fmk (20 μM/2 μL; Calbiochem), or 2 μL of control vehicle into the vitreous cavity before the onset of reperfusion.
Histological Examination.
At designated time points, the eyes were fixed in formalin and embedded in paraffin. Three sections (thickness: 5 μm) through the optic disk of each eye were prepared in a standard manner and stained with H&E. Morphometric analysis was performed to quantify ischemic injury. The total retinal thickness (from the internal to the outer limiting membrane) was measured in four adjacent areas of the inferior retina within 1 mm of the optic nerve by using Axiovision software (Carl Zeiss), and the mean value was calculated.
RGC Labeling and Quantification.
Mice were anesthetized with a mixture of 100 mg/kg ketamine and 10 mg/kg xylazine by i.p. injection and placed in a stereotactic apparatus (Stoelting). FG [1 μL per injection of 4% (wt/vol); Invitrogen] diluted in saline was injected into both superior colliculi. To ensure proper RGC labeling, the animals were allowed 7 d for retrograde transport of FG before sacrifice. At 24, 48, and 72 h after reperfusion, FG-positive RGCs were identified with a fluorescent microscope (AxioImager; Carl Zeiss) after retinal flat mount preparation. Surviving RGCs (gold dots) were counted by using Image Pro Plus (Version 6.0; Media Cybernetics).
Immunofluorescence and Evaluation of Microglia Activation.
Mice were perfused by 4% (wt/vol) paraformaldehyde transcardially through the ascending aorta after being anesthetized, and their eyes were enucleated and bisected equatorially. The posterior halves were immersed in fixative (4% paraformaldehyde) for 2 h and infiltrated with increasing concentrations of sucrose. Tissue was then embedded in optimum cutting temperature (OCT) medium, frozen, and sectioned to a thickness of 6 μm. The presence of ionized calcium binding adaptor molecule 1 (Iba1) was detected to evaluate microglia activation by using polyclonal rabbit anti-Iba1 (1:300; Wako Chemicals). Antibody binding was visualized by incubation with Alexa Fluor 555 donkey anti-rabbit IgG (1:500; Invitrogen). The nuclei of cells in the retina were stained with DAPI (Sigma). Images were obtained by using a Zeiss LSM 710 META confocal laser scanning microscope (Carl Zeiss).
sqRT-PCR and qPCR.
Total RNA was isolated from the retina by using TRIzol reagent (Invitrogen), and cDNA was synthesized with PrimeScript RT Master Mix (TaKaRa). The mouse and rat primers and annealing temperatures are listed in Tables S1 and S2. SqRT-PCR was carried out by using Premix EX Taq Kit (TaKaRa) according to the standard protocol. The reaction was performed with 25 cycles for GAPDH and 30–32 cycles for the other transcripts. PCR products were run on 2% agarose gel, and semiquantification of gene expression was determined by relative pixel densitometry using ImageJ software after normalization to GAPDH. Amplification and qPCR measurements were performed by using the Light Cycler 480 Real-Time PCR System, with version LCS480 1.5.1.62 software. Quantitative analysis was performed by real-time qPCR using SYBR Advantage qPCR Premix Master Mix (TaKaRa) following the standard protocol. The amount of target mRNA in test samples was measured and normalized to GAPDH. The comparative Cp method was used to evaluate expression.
Western Blot Analysis.
For analysis of protein expression, retinal tissue was harvested at 6, 24, 48, and 72 h after temporary elevation of IOP. Total protein was extracted and processed for Western blot. The membranes were blocked with 5% (wt/vol) BSA in Tween 20/PBS and incubated at 4 °C overnight in primary antibodies, which were diluted in blocking solution. Primary antibodies consisted of TLR4 (1:500; Abgent), cleaved caspase-8 (1:500; Cell Signaling Technology), cleaved caspase-3 (1:1,000; Cell Signaling Technology), NLRP1 (1:500; Aviva), NLRP3 (1:1,000; Novus), ASC (1:100; Millipore), IL-1β (1:500; Cell Signaling Technology), β-actin (1:3,000; Multi Sciences Biotech), and GAPDH (1:1,000; Cell Signaling Technology). Relative changes in protein expression were calculated in relation to nonischemic retinas and expressed as the “x-fold change”.
Statistical Analysis.
Data were presented as mean ± SD. One-way analysis of variance (ANOVA) was performed, followed by the Bonferroni multiple comparison tests and two-way ANOVA using GraphPad Prism data analysis software (version 5.0; GraphPad Software). A P value less than 0.05 was considered statistically significant.
Supplementary Material
Acknowledgments
We thank Dr. Changyou Wu and Dr. Qiang Liu for data analysis. This study was supported in part by National Natural Science Foundation of China Grant 81270992 and 973 Program Grant 2013CB967504.
Footnotes
The authors declare no conflict of interest.
*This Direct Submission article had a prearranged editor.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1402819111/-/DCSupplemental.
References
- 1.Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: A review. JAMA. 2014;311(18):1901–1911. doi: 10.1001/jama.2014.3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang N, Wu H, Fan Z. Primary angle closure glaucoma in Chinese and Western populations. Chin Med J (Engl) 2002;115(11):1706–1715. [PubMed] [Google Scholar]
- 3.Ang LP, Ang LP. Current understanding of the treatment and outcome of acute primary angle-closure glaucoma: An Asian perspective. Ann Acad Med Singapore. 2008;37(3):210–215. [PubMed] [Google Scholar]
- 4.Quek DT, et al. Blindness and long-term progression of visual field defects in chinese patients with primary angle-closure glaucoma. Am J Ophthalmol. 2011;152(3):463–469. doi: 10.1016/j.ajo.2011.02.023. [DOI] [PubMed] [Google Scholar]
- 5.Ousman SS, Kubes P. Immune surveillance in the central nervous system. Nat Neurosci. 2012;15(8):1096–1101. doi: 10.1038/nn.3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang C, Lam TT, Tso MO. Heterogeneous populations of microglia/macrophages in the retina and their activation after retinal ischemia and reperfusion injury. Exp Eye Res. 2005;81(6):700–709. doi: 10.1016/j.exer.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 7.Yamasaki Y, et al. Interleukin-1 as a pathogenetic mediator of ischemic brain damage in rats. Stroke. 1995;26(4):676–680, discussion 681. doi: 10.1161/01.str.26.4.676. [DOI] [PubMed] [Google Scholar]
- 8.Hanamsagar R, Hanke ML, Kielian T. Toll-like receptor (TLR) and inflammasome actions in the central nervous system. Trends Immunol. 2012;33(7):333–342. doi: 10.1016/j.it.2012.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lehnardt S. Innate immunity and neuroinflammation in the CNS: The role of microglia in Toll-like receptor-mediated neuronal injury. Glia. 2010;58(3):253–263. doi: 10.1002/glia.20928. [DOI] [PubMed] [Google Scholar]
- 10.Saijo K, Crotti A, Glass CK. Regulation of microglia activation and deactivation by nuclear receptors. Glia. 2013;61(1):104–111. doi: 10.1002/glia.22423. [DOI] [PubMed] [Google Scholar]
- 11.Dvoriantchikova G, Barakat DJ, Hernandez E, Shestopalov VI, Ivanov D. Toll-like receptor 4 contributes to retinal ischemia/reperfusion injury. Mol Vis. 2010;16:1907–1912. [PMC free article] [PubMed] [Google Scholar]
- 12.Marsh BJ, Williams-Karnesky RL, Stenzel-Poore MP. Toll-like receptor signaling in endogenous neuroprotection and stroke. Neuroscience. 2009;158(3):1007–1020. doi: 10.1016/j.neuroscience.2008.07.067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crack PJ, Bray PJ. Toll-like receptors in the brain and their potential roles in neuropathology. Immunol Cell Biol. 2007;85(6):476–480. doi: 10.1038/sj.icb.7100103. [DOI] [PubMed] [Google Scholar]
- 14.Tang SC, et al. Pivotal role for neuronal Toll-like receptors in ischemic brain injury and functional deficits. Proc Natl Acad Sci USA. 2007;104(34):13798–13803. doi: 10.1073/pnas.0702553104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hyakkoku K, et al. Toll-like receptor 4 (TLR4), but not TLR3 or TLR9, knock-out mice have neuroprotective effects against focal cerebral ischemia. Neuroscience. 2010;171(1):258–267. doi: 10.1016/j.neuroscience.2010.08.054. [DOI] [PubMed] [Google Scholar]
- 16.Netea MG, van de Veerdonk FL, Kullberg BJ, Van der Meer JW, Joosten LA. The role of NLRs and TLRs in the activation of the inflammasome. Expert Opin Biol Ther. 2008;8(12):1867–1872. doi: 10.1517/14712590802494212. [DOI] [PubMed] [Google Scholar]
- 17.Schroder K, Tschopp J. The inflammasomes. Cell. 2010;140(6):821–832. doi: 10.1016/j.cell.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 18.Abulafia DP, et al. Inhibition of the inflammasome complex reduces the inflammatory response after thromboembolic stroke in mice. J Cereb Blood Flow Metab. 2009;29(3):534–544. doi: 10.1038/jcbfm.2008.143. [DOI] [PubMed] [Google Scholar]
- 19.de Rivero Vaccari JP, et al. Therapeutic neutralization of the NLRP1 inflammasome reduces the innate immune response and improves histopathology after traumatic brain injury. J Cereb Blood Flow Metab. 2009;29(7):1251–1261. doi: 10.1038/jcbfm.2009.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crawford ED, Wells JA. Caspase substrates and cellular remodeling. Annu Rev Biochem. 2011;80:1055–1087. doi: 10.1146/annurev-biochem-061809-121639. [DOI] [PubMed] [Google Scholar]
- 21.Crowder RN, El-Deiry WS. Caspase-8 regulation of TRAIL-mediated cell death. Exp Oncol. 2012;34(3):160–164. [PubMed] [Google Scholar]
- 22.Burguillos MA, et al. Caspase signalling controls microglia activation and neurotoxicity. Nature. 2011;472(7343):319–324. doi: 10.1038/nature09788. [DOI] [PubMed] [Google Scholar]
- 23.Maelfait J, Beyaert R. Non-apoptotic functions of caspase-8. Biochem Pharmacol. 2008;76(11):1365–1373. doi: 10.1016/j.bcp.2008.07.034. [DOI] [PubMed] [Google Scholar]
- 24.Cao CX, et al. Reduced cerebral ischemia-reperfusion injury in Toll-like receptor 4 deficient mice. Biochem Biophys Res Commun. 2007;353(2):509–514. doi: 10.1016/j.bbrc.2006.12.057. [DOI] [PubMed] [Google Scholar]
- 25.Hamanaka J, Hara H. Involvement of Toll-like receptors in ischemia-induced neuronal damage. Cent Nerv Syst Agents Med Chem. 2011;11(2):107–113. doi: 10.2174/187152411796011312. [DOI] [PubMed] [Google Scholar]
- 26.Chakraborty S, Kaushik DK, Gupta M, Basu A. Inflammasome signaling at the heart of central nervous system pathology. J Neurosci Res. 2010;88(8):1615–1631. doi: 10.1002/jnr.22343. [DOI] [PubMed] [Google Scholar]
- 27.Savage CD, Lopez-Castejon G, Denes A, Brough D. NLRP3-inflammasome activating DAMPs stimulate an inflammatory response in glia in the absence of priming which contributes to brain inflammation after injury. Front Immunol. 2012;3:288. doi: 10.3389/fimmu.2012.00288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yoneda S, et al. Interleukin-1beta mediates ischemic injury in the rat retina. Exp Eye Res. 2001;73(5):661–667. doi: 10.1006/exer.2001.1072. [DOI] [PubMed] [Google Scholar]
- 29.Gringhuis SI, et al. Dectin-1 is an extracellular pathogen sensor for the induction and processing of IL-1β via a noncanonical caspase-8 inflammasome. Nat Immunol. 2012;13(3):246–254. doi: 10.1038/ni.2222. [DOI] [PubMed] [Google Scholar]
- 30.Maelfait J, et al. Stimulation of Toll-like receptor 3 and 4 induces interleukin-1beta maturation by caspase-8. J Exp Med. 2008;205(9):1967–1973. doi: 10.1084/jem.20071632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lemmers B, et al. Essential role for caspase-8 in Toll-like receptors and NFkappaB signaling. J Biol Chem. 2007;282(10):7416–7423. doi: 10.1074/jbc.M606721200. [DOI] [PubMed] [Google Scholar]
- 32.Minckler DS, Bunt AH, Johanson GW. Orthograde and retrograde axoplasmic transport during acute ocular hypertension in the monkey. Invest Ophthalmol Vis Sci. 1977;16(5):426–441. [PubMed] [Google Scholar]
- 33.Wallach D, et al. How are the regulators regulated? The search for mechanisms that impose specificity on induction of cell death and NF-kappaB activation by members of the TNF/NGF receptor family. Arthritis Res. 2002;4(Suppl 3):S189–S196. doi: 10.1186/ar585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hanisch UK, Kettenmann H. Microglia: Active sensor and versatile effector cells in the normal and pathologic brain. Nat Neurosci. 2007;10(11):1387–1394. doi: 10.1038/nn1997. [DOI] [PubMed] [Google Scholar]
- 35.Gurung P, et al. FADD and caspase-8 mediate priming and activation of the canonical and noncanonical Nlrp3 inflammasomes. J Immunol. 2014;192(4):1835–1846. doi: 10.4049/jimmunol.1302839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kanneganti TD, et al. Critical role for Cryopyrin/Nalp3 in activation of caspase-1 in response to viral infection and double-stranded RNA. J Biol Chem. 2006;281(48):36560–36568. doi: 10.1074/jbc.M607594200. [DOI] [PubMed] [Google Scholar]
- 37.Guma M, et al. Caspase 1-independent activation of interleukin-1beta in neutrophil-predominant inflammation. Arthritis Rheum. 2009;60(12):3642–3650. doi: 10.1002/art.24959. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.