Abstract
BACKGROUND:
Several risk scoures have been used in predicting acute kidney injury (AKI) of patients undergoing general or specific operations such as cardiac surgery. This study aimed to evaluate the use of two AKI risk scores in patients who underwent non-cardiac surgery but required intensive care.
METHODS:
The clinical data of patients who had been admitted to ICU during the first 24 hours of ICU stay between September 2009 and August 2010 at the Cancer Institute, Chinese Academy of Medical Sciences & Peking Union Medical College were retrospectively collected and analyzed. AKI was diagnosed based on the acute kidney injury network (AKIN) criteria. Two AKI risk scores were calculated: Kheterpal and Abelha factors.
RESULTS:
The incidence of AKI was 10.3%. Patients who developed AKI had a increased ICU mortality of 10.9% vs. 1.0% and an in-hospital mortality of 13.0 vs. 1.5%, compared with those without AKI. There was a significant difference between the classification of Kheterpal’s AKI risk scores and the occurrence of AKI (P<0.001). There was no significant difference between the number of Abelha’s AKI risk scores and the occurrence of AKI (P=0.499). Receiver operating characteristic curves demonstrated an area under the curve of 0.655±0.043 (P=0.001, 95% confidence interval: 0.571–0.739) for Kheterpal’s AKI risk score and 0.507±0.044 (P=0.879, 95% confidence interval: 0.422–0.592) for Abelha’s AKI risk score.
CONCLUSION:
Kheterpal’s AKI risk scores are more accurate than Abelha’s AKI risk scores in predicting the occurrence of AKI in patients undergoing non-cardiac surgery with moderate predictive capability.
KEY WORDS: Risk factor, Acute kidney injury, Surgery
INTRODUCTION
The incidence of acute kidney injury (AKI) varies from 7.5% in general surgery patients to 39.8% in patients at intensive care unit (ICU), and it is associated with increased morbidity, mortality, and duration of hospital stay.[1–4] However, there has little progress in research on prevention and treatment.
Several risk scores have been developed in predicting AKI for patients undergoing general surgery[1,3] or specific operations such as cardiac surgery.[5] These data are of interest to surgeons who attempt to decrease the risk of AKI after surgery. However, the use of a predictive score must be validated before it is used in clinical practice. The aim of the present study is to evaluate the use of two acute kidney injury risk soreses for patients who underwent non-cardiac surgery and required intensive care.[1,3]
METHODS
Patients
This retrospective study was conducted in 536 patients treated at the Intensive Care Unit (ICU), Cancer Hospital (Institute) of the Chinese Academy of Medical Sciences & Peking Union Medical College, China. The ICU is a 10-bed surgical unit. This study was approved by the institutional review board, and informed consent was waived owning to the observational nature of this study.
Measurements
The data of patients who had been admitted to the ICU in the first 24 hours of ICU stay between September 2009 and August 2010 were analyzed retrospectively. The data included age, gender, American Society of Anesthesiologist (ASA) physical status,[6] co-morbidities of hypertension, coronary heart diseases and diabetic mellitus, a history of renal insufficiency, procedures performed (intra-thoracic surgery, intra-peritoneal surgery, or others), presence of AKI based on the Acute Kidney Injury Network (AKIN) criteria,[7] revised cardiac risk index (RCRI),[8] presence of ascites, presence of active congestive heart failure, and type of admission (emergency surgery or elective surgery).
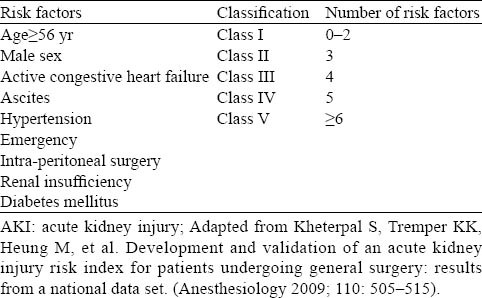
Two AKI risk scores were calculated according to Kheterpal’s[1] and Abelha’s[3] definition. In Kheterpal’s AKI risk score, five classifications were based on nine preoperative risk factors (Table 1). Abelha’s AKI risk score consisted of four risk factors including high ASA physical statue (IV/V), high-risk surgery (defined as intra-peritoneal, intra-thoracic, or supra-inguinal vascular procedures), congestive heart disease and RCRI score >3. One point was appointed to each risk factor, and total score was calculated as the sum of every risk factor in the end.
Table 1.
Kheterpal’s AKI risk score (2009)
Patients older than 18 years who had been admitted to the ICU were included in the study. Those who had received non-operative treatments and those had a ICU stay<24 hours were excluded.
Statistical analysis
The SPSS software package 13.0 for Windows was used for statistical analysis. The data were presented as medians (interquartile range) for continuous variables, and percentages for dichotomous variables. Continuous variables were analyzed using Student’s t test, and categorical variables were analyzed using the Chi-square test. The area under the receiver operating characteristic curve (AUROC) was used to evaluate the ability of each model to discriminate between patients who developed AKI from those who did not. P value<0.05 was considered statistically significant.
RESULTS
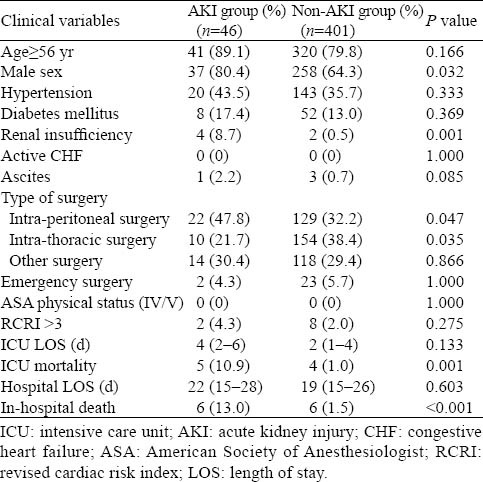
Among the 536 patients admitted consecutively to our surgical ICU in the period of 2009–2010, 14 patients with readmissions, 35 non-operative patients and 70 patients due to ICU LOS<24 hours were excluded. Thus the study group comprised 447 patients, 295 males and 152 females, with a median age of 67 years (range 18–89 years). Forty-six patients were diagnosed with AKI on the first day of ICU admission, giving an incidence of 10.3% for AKI. The patients who developed AKI had an increased ICU mortality and in-hospital mortality (Table 2). Other characteristics of the study group are also shown in Table 2.
Table 2.
Characteristics of the study group on admission to the ICU
There was a significant difference between the classification of Kheterpal’s AKI risk score and occurrence of AKI (Figure 1). In class I patients of Kheterpal’s AKI score (n=251), the occurrence of AKI was 5.6%. The occurrence of AKI in class II (n=132), class III (n=52) and class IV (n=12) patients was 15.2%, 15.4% and 33.3% respectively. There were no class V patients of Kheterpal’s AKI score. On the contrary, there was no significant difference between the number of Abelha’s AKI risk factor and occurrence of AKI (Figure 2). The occurrence of AKI in patients with zero risk factor (n=103), one risk factor (n=162), two risk factors (n=70) and three risk factors (n=10) was 8.7%, 11.4%, 7.1% and 20.0% respectively. There were no patients with four risk factors of Abelha’s AKI risk score. Receiver operating characteristic curves demonstrated an area under the curve of 0.655±0.043 (P=0.001, 95% confidence interval: 0.571–0.739) for Kheterpal’s AKI score and 0.507±0.044 (P=0.879, 95% confidence interval: 0.422–0.592) for Abelha’s AKI risk score (Figure 3).
Figure 1.
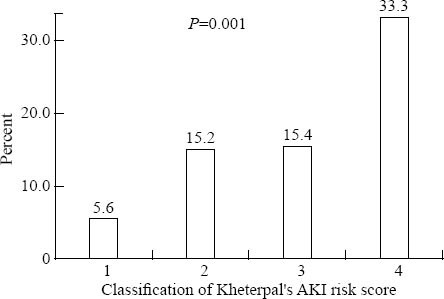
Classification of Kheterpal’s AKI risk score and occurrence of AKI.
Figure 2.
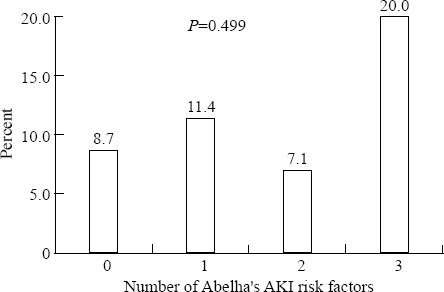
Number of Abelha’s AKI risk factors and occurrence of AKI.
Figure 3.
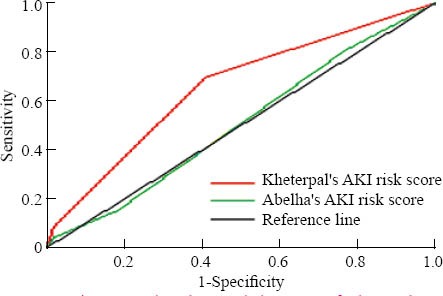
Receiver operating characteristic curves of Kheterpal’s AKI risk score and Abelha’s AKI score.
DISCUSSION
Many AKI risk scores have been developed and used to predict the risk of AKI.[1–4] But there were no validation studies of these risk scores, which restrict the use of these indexes. Thus, the assessment of these AKI risk scores is important before its use in clinical practice.
The overall incidence of AKI in this study was 10.3%, which is in the range of numbers reported elsewhere.[1–4] But this is higher than that we reported previously (only 3.1% by the RIFLE diagnosis system).[9] Joannidis et al[10] reported that increased sensitivity could be determined by the AKIN criteria compared with the RIFLE diagnosis system. More importantly, there was no significant difference in outcome prediction between the two systems of diagnosis.[11] AKI was found to be associated with ICU mortality and hospital mortality in our study.[1–4,10,11]
Our study demonstrated moderate predictive capability for Kheterpal’s AKI risk score with AUROC of 0.655. In the study of Kheterpal et al,[1] nine independent preoperative predictors were identified in 57 080 patients and validated in 18 872 patients. In their study AKI risk index was 0.80 in both derivation and validation groups but postoperative factors such as nephrotoxic agents and sepsis were not considered. Large epidemiologic studies[12] showed that nephrotoxic drugs are contributing factors in 19% to 25% of critically ill patients with severe acute renal failure. Sepsis has been found to be a leading contributing factor for AKI in critical illness.[13–15] Therefore, analysis by incorporating these two factors into new AKI risk scoremay be more accurate in predicting the occurrence of AKI.
In our study AUROC of 0.507 was not used for Abelha’s AKI score. In Abelha’s study, the most important limitation is the exclusion of patients with preoperative renal dysfunction. Thakar[16] pointed out that chronic kidney disease has been identified as a major risk factor for perioperative AKI in most studies.[17] In our study, renal insufficiency was considered as a risk factor in unvariate analysis (Table 2). Lack of information about the use of nephrotoxic agents is another limitation discussed earlier.
In short, the first limitation is the small sample of the study. But the incidence and short-term outcome of AKI in this study are comparable to other studies. Thus the result of the study is credible. The second limitation is that patients of this study suffered from cancer, which prevents the application of general surgery.
In conclusion, Kheterpal’s AKI risk index is accurate than Abelha’s AKI risk index in predicting the occurrence of AKI in patients undergoing non-cardiac surgery with moderate predictive capability. Perioperative factors including preoperative, operative and postoperative ones such as sepsis and nephrotoxic agents must be considered in predicting the risk of occurrence of AKI.[18–20] Prospective studies are needed to identify a robust score to predict AKI after surgery, thus leading to successful clinical trials of prophylactic strategies to prevent this devastating syndrome.
Footnotes
Funding: This study was supported by a grant from the Beijing Hope Run Special Fund (LC2011B38).
Ethical approval: This study was approved by the institutional review board.
Conflicts of interest: No competing interests.
Contributors: Xing XZ designed the research, analyzed the data, and wrote the paper. All authors read and approved the final version.
REFERENCES
- 1.Kheterpal S, Tremper KK, Heung M, Rosenberg AL, Englesbe M, Shanks AM, et al. Development and validation of an acute kidney injury risk index for patients undergoing general surgery: results from a national data set. Anesthesiology. 2009;110:505–515. doi: 10.1097/ALN.0b013e3181979440. [DOI] [PubMed] [Google Scholar]
- 2.Bihorac A, Yavas S, Subbiah S, Hobson CE, Schold JD, Gabrielli A, et al. Long-term risk of mortality and acute kidney injury during hospitalization after major surgery. Ann Surg. 2009;249:851–858. doi: 10.1097/SLA.0b013e3181a40a0b. [DOI] [PubMed] [Google Scholar]
- 3.Abelha FJ, Botelho M, Fernandes V, Barros H. Determinants of postoperative acute kidney injury. Crit Care. 2009;13:R79. doi: 10.1186/cc7894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fonseca Ruiz NJ, Castro DP, Guerra AM, Saldarriaga FM, Hernández JD. Renal injury study in critical ill patients in accordance with the new definition given by the Acute Kidney Injury Network. J Crit Care. 2011;26:206–212. doi: 10.1016/j.jcrc.2010.06.011. [DOI] [PubMed] [Google Scholar]
- 5.Palomba H, de Castro I, Neto AL, Lage S, Yu L. Acute kidney injury prediction following elective cardiac surgery: AKICS Score. Kidney Int. 2007;72:624–631. doi: 10.1038/sj.ki.5002419. [DOI] [PubMed] [Google Scholar]
- 6.Sweitzer BJ. Overview of Preoperative Evaluation and Testing. In: Sweitzer BJ, editor. Preoperative Assessment and Management. 2nd Ed. LWW; 2008. pp. 14–50. [Google Scholar]
- 7.Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG, et al. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care. 2007;11:R31. doi: 10.1186/cc5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee TH, Marcantonio ER, Mangione CM, Thomas EJ, Polanczyk CA, Cook EF, et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation. 1999;100:1043–1049. doi: 10.1161/01.cir.100.10.1043. [DOI] [PubMed] [Google Scholar]
- 9.Xing X, Wang H, Xu H. Incidence and risk factors of supraventricular arrhythmias in postoperative cancer patients in intensive care unit. Clin Med of China. 2011;27:290–293. [Google Scholar]
- 10.Joannidis M, Metnitz B, Bauer P, Schusterschitz N, Moreno R, Druml W, et al. Acute kidney injury in critically ill patients classified by AKIN versus RIFLE using the SAPS 3 database. Intensive Care Med. 2009;35:1692–1702. doi: 10.1007/s00134-009-1530-4. [DOI] [PubMed] [Google Scholar]
- 11.Bagshaw SM, George C, Bellomo R ANZICS Database, Management Committe. A comparison of the RIFLE and AKIN criteria for acute kidney injury in critically ill patients. Nephrol Dial Transplant. 2008;23:1569–1574. doi: 10.1093/ndt/gfn009. [DOI] [PubMed] [Google Scholar]
- 12.Pannu N, Nadim MK. An overview of drug-induced acute kidney injury. Crit Care Med. 2008;36:S216–223. doi: 10.1097/CCM.0b013e318168e375. [DOI] [PubMed] [Google Scholar]
- 13.Bagshaw SM, George C, Bellomo R ANZICS Database, Management Committee. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47. doi: 10.1186/cc6863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Su LX, Feng L, Zhang J, Xiao YJ, Jia YH, Yan P, et al. Diagnostic value of urine sTREM-1 for sepsis and relevant acute kidney injuries: a prospective study. Crit Care. 2011;15:R250. doi: 10.1186/cc10508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Medve L, Antek C, Paloczi B, Kocsi S, Gartner B, Marjanek Z, et al. Epidemiology of acute kidney injury in Hungarian intensive care units: a multicenter, prospective, observational study. BMC Nephrol. 2011;12:43. doi: 10.1186/1471-2369-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP. A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol. 2005;16:12–14. doi: 10.1681/ASN.2004040331. [DOI] [PubMed] [Google Scholar]
- 17.Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT. Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. Ann Intern Med. 1998;128:194–203. doi: 10.7326/0003-4819-128-3-199802010-00005. [DOI] [PubMed] [Google Scholar]
- 18.Brochard L, Abroug F, Brenner M, Broccard AF, Danner RL, Ferrer M, et al. An Official ATS/ERS/ESICM/SCCM/SRLF statement: prevention and management of acute renal failure in the ICU patient: an international consensus conference in intensive care medicine. Am J Respir Crit Care Med. 2010;181:1128–1155. doi: 10.1164/rccm.200711-1664ST. [DOI] [PubMed] [Google Scholar]
- 19.Arora P, Rajagopalam S, Ranjan R, Kolli H, Singh M, Venuto R, et al. Preoperative use of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers is associated with increased risk for acute kidney injury after cardiovascular surgery. Clin J Am Soc Nephrol. 2008;3:1266–1273. doi: 10.2215/CJN.05271107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Valette X, Parienti JJ, Plaud B, Lehoux P, Samba D, Hanouz JL. Incidence, morbidity, and mortality of contrast-induced acute kidney injury in a surgical intensive care unit: a prospective cohort study. J Crit Care. 2012;27:322. doi: 10.1016/j.jcrc.2011.08.005. [DOI] [PubMed] [Google Scholar]


