Abstract
The highly infectious bacteria, Francisella tularensis, colonize a variety of organs and replicate within both phagocytic as well as non-phagocytic cells, to cause the disease tularemia. These microbes contain a conserved cluster of important virulence genes referred to as the Francisella Pathogenicity Island (FPI). Two of the most characterized FPI genes, iglC and pdpA, play a central role in bacterial survival and proliferation within phagocytes, but do not influence bacterial internalization. Yet, their involvement in non-phagocytic epithelial cell infections remains unexplored. To examine the functions of IglC and PdpA on bacterial invasion and replication during epithelial cell infections, we infected liver and lung epithelial cells with F. novicida and F. tularensis ‘Type B’ Live Vaccine Strain (LVS) deletion mutants (ΔiglC and ΔpdpA) as well as their respective gene complements. We found that deletion of either gene significantly reduced their ability to invade and replicate in epithelial cells. Gene complementation of iglC and pdpA partially rescued bacterial invasion and intracellular growth. Additionally, substantial LAMP1-association with both deletion mutants was observed up to 12 h suggesting that the absence of IglC and PdpA caused deficiencies in their ability to dissociate from LAMP1-positive Francisella Containing Vacuoles (FCVs). This work provides the first evidence that IglC and PdpA are important pathogenic factors for invasion and intracellular growth of Francisella in epithelial cells, and further highlights the discrete mechanisms involved in Francisella infections between phagocytic and non-phagocytic cells.
Introduction
The intracellular bacteria Francisella tularensis cause the zoonotic disease in humans and other mammals, called tularemia. F. tularensis have multiple subspecies including ssp. ‘type A’ tularensis, ssp. ‘type B’ holarctica and ssp. mediasiatica. Though F. novicida has been considered a fourth subspecies because of its high genomic identity (>97%) with F. tularensis [1]–[4], this taxonomic classification remains controversial due to the distinct evolutionary and ecological profiles between the two bacteria [5]–[7]. Both F. novicida and F. tularensis can enter hosts through multiple routes including the intestinal and respiratory tracts as well as through exposure from infected animals or arthropod vectors. Once internalized, these bacteria colonize various organs, including the lungs and liver [8]–[16]. F. tularensis cause disease from exposure to as few as 10 bacteria, which can result in mortality rates as high as 60% if left untreated [17], [18] whereas F. novicida causes human-like tularemia in mice with as few as 50 bacteria [15], [19]. F. tularensis LVS can causes disease in mice and can infect human cells in culture [15], [16], [20]. All of these microbes infect phagocytic and non-phagocytic cells [15], [16], [20], [21], and contain similar sets of virulence factors [22]–[24]. Because F. tularensis has the potential for aerosolization and is classified by the USA Centers for Disease Control and Prevention as a ‘Category A’ select agent [25], requiring BCL-3 facilities for experimentation, much of the research on Francisella have used F. novicida and F. tularensis LVS (BCL-2) as surrogate pathogens to investigate the genetics, biochemistry and pathogenesis of Francisella [15], [26]–[31].
The Francisella pathogenicity island (FPI) is a highly conserved ∼31 kb region, comprising 16 to 19 protein-coding genes, within the bacterial chromosome. It is thought to exist as a single copy in F. novicida, but is duplicated in all F. tularensis species [32]. Evidence has shown that deletion of a single FPI gene in F. tularensis does not significantly diminish its virulence suggesting that both alleles are phenotypically alike [33]. Though most FPI genes are unique to the Francisellaceae family and remain poorly defined, a subset of genes, including iglA, iglB, dotU, and vgrG, share limited homology with core structural components of a Type VI secretion system (T6SS) [27], [34]–[36]. A thorough study by Bröms and colleagues examining dotU, iglC, iglG, and vgrG suggest that all four genes are needed for the delivery of virulence factors into host macrophages [37].
A commonly associated function of the FPI is its involvement in the replication of Francisella within host macrophages. During the initial intracellular stage of these infections, Francisella transiently reside within phagosomes and associate with early and late stage endosomal markers [38], [39]. In order to evade lysosome-mediated killing, Francisella can escape these vacuoles in as little as 15 min [40]; by 4 h, ∼90% of the bacteria are already present in the host cytosol [41], [42]. Several studies have demonstrated that most FPI-encoded proteins, including IglC and PdpA, are essential for bacterial escape from the phagosomal compartment and/or bacterial replication [27], [32], [43]–[47]. Although we have yet to fully understand how these proteins interact with host cells, recent evidence suggests that IglC, PdpA, and six other FPI-encoded proteins are translocated into the cytoplasm of phagocytes and their delivery is dependent on the expression of Francisella T6SS genes [37]. Despite the importance these T6SS genes play in intracellular replication, their expression does not appear to significantly influence the uptake of Francisella into macrophages [43], [48]–[50].
Non-phagocytic epithelial cell infections are considered to be important for the progression of disease as Francisella colonize and replicate within epithelial cells both in vitro and in vivo [16], [21], [51]–[53]. Although several organs are known to be colonized by these bacteria [8]–[14], two primary sites of Francisella colonization are the lungs and liver. The lungs are susceptible to infection through aerosol delivery, requiring the low infectious doses to trigger disease [54]. Once inside the lungs, F. tularensis can infect alveolar type II epithelial cells, which are considered well positioned for the pathogen to enter the circulation as they reside near the endothelium [16], [55]. The livers of Francisella infected animals have been known for decades to be sites of bacterial colonization [56], [57]. Within the livers of infected mice, ∼12% of the cells are colonized by these microbes; >90% of which are hepatocytes [15]. We have previously shown that Francisella predominantly invade hepatocytes by usurping the host clathrin-mediated endocytic (CME) machinery [15]. Although the precise bacterial mechanisms that Francisella use to hijack the host endocytic machinery has remained elusive, viruses [58]–[60] and other invasive pathogens including Listeria monocytogenes and Yersinia pseudotuberculosis rely on virulence factors encoded within clusters of pathogenic genes to trigger bacterial internalization via. CME [61], [62].
Despite recent work that has alluded to the importance of non-macrophage infections in the Francisella disease process [63], [64], the study of Francisella remains primarily focused on phagocytic cell infections. Given that a previous report has indicated that the FPI likely plays a predominant role in the pathogenesis of Francisella in epithelial cells [65], we examined the involvement of two FPI genes in Francisella invasion and replication during liver and lung epithelial cell infections. We report that iglC and pdpA are required for efficient bacterial invasion and intracellular proliferation during non-phagocytic epithelial cell infections.
Experimental Procedures
Bacterial and growth conditions
F. novicida strain Utah 112, deletion mutants ΔiglC, ΔpdpA, and their gene complements (ΔiglC::iglC-FLAG KmR [ΔiglC::iglC], ΔpdpA::pdpA-FLAG KmR [ΔpdpA::pdpA]) as well as F. tularensis ssp. holarctica Live vaccine strain [LVS], ΔpdpA, and ΔpdpA::pdpA HygR were supplied by Dr. Francis Nano from the University of Victoria. The detailed description of the F. tularensis LVS ΔpdpA mutant will be described elsewhere (Nix et al, in preparation). In brief, the two pdpA alleles in F. tularensis LVS were sequentially removed using the approach previously used to remove the one pdpA allele from F. novicida [26]. Genetic complementation was accomplished by introducing a copy of pdpA on a derivative of plasmid pMP831 [66]. F. tularensis LVS ΔiglC and its complement F. tularensis LVS ΔiglC::iglC KmR were kindly provided by Dr. Anders Sjostedt. All bacteria were grown according to the procedures described previously [36], [47], [48], [67].
Bacterial titre
To estimate the amount of bacterial growth at 24 h post-infection (PI), 10-fold serial dilutions of the Francisella cultures were made in Tryptic soy broth (TSB) supplemented with 0.1% L-cysteine (TSBC). These were performed by plating 10 µL of diluted cultures that ranged from 10−1 to 10−10 onto Tryptic soy agar (TSA) supplemented with 0.1% L-cysteine (TSAC) plates (for F. novicida) or Chocolate blood agar [TSAC and 5% defibrinated horse blood] (CBA) plates (for F. tularensis LVS). When appropriate, bacteria were grown in media containing 10 or 15 µg mL−1 of kanamycin or 100 µg mL−1 of hygromycin B. Plates were incubated overnight at 37°C (for F. novicida) or for up to 3 days (for F. tularensis LVS), at 37°C prior to counting colony forming units (CFUs).
Cell cultures and infections
Murine hepatocytes, BNL CL.2 cells (ATCC; TIB-73) and human lung epithelial A549 cells (ATCC; CCL-185) were respectively cultured in high-glucose Dulbecco’s Modified Eagle’s Medium (DMEM) [Thermo] and Kaghn’s F-12 media [Thermo] both containing with 10% fetal bovine serum (FBS) and incubated at 37°C with 5% CO2. These cells were seeded into 24-well plates or onto #1.5 glass coverslips, grown to confluence, then infected with F. novicida at a multiplicity of infection (MOI) of 100∶1 for up to 48 h as done previously [15]. For F. tularensis LVS studies, the cells were infected at an MOI of 200∶1 and immediately centrifuged for 5 min (300×g) at room temperature (RT), as previous described [68]. In this manuscript this is referred to as the 0 h time-point. Antibiotic selection was maintained over the course of the infection by supplementing the cell culture media with appropriate antibiotics. All infections proceeded in a humidified chamber at 37°C with 5% CO2 and were only placed at RT during inoculation, washes, and at the experimental endpoint. At the appropriate time-points, samples were washed 6 times with PBS +/+ (Dulbecco’s PBS containing 0.0133% calcium and 0.01% magnesium) [Sigma] both before and after extracellular bacterial-killing using fresh infection media supplemented with 30 (for LVS) or 100 (for F. novicida) µg mL−1 of gentamicin [15], [55]. When indicated, a lower concentration of gentamicin (10 µg mL−1) was subsequently applied to prevent the growth of extracellular bacteria. Before commencing gentamicin protection assays or immunofluorescence staining, all wells were washed 3 times with PBS +/+.
Gentamicin protection assays
Gentamicin protection assays (4 h invasion assays) were performed following the procedures previously used by our laboratory [15]. To summarize, the samples were washed 6 times with PBS +/+ then incubated with gentamicin at 3 h post inoculation (PI) to kill any extracellular bacteria. At all of the experimental endpoints, uninfected and F. novicida infected cells were lysed with 1% Triton-X in PBS. For F. tularensis LVS infections, cells were lysed with sterile ddH2O because the lysis reagent prohibited the formation of visible colonies. The lysates were serially diluted with TSBC and then plated onto either TSAC (for F. novicida) or CBA (for F. tularensis LVS). Solid agar plates containing appropriate antibiotics were used when necessary and were subsequently incubated at 37°C.
To compare the intracellular growth profiles of wild-type and mutant Francisella between 4 h and 24 h PI, we allowed Francisella to invade epithelial cells for 3 h, washed the samples multiple times and treated them with gentamicin for 1 h. The samples were then either lysed immediately, to measure the initial amount of intracellular bacteria, or replaced with fresh media containing gentamicin (10 µg mL−1), thus permitting the invaded bacteria to replicate for up to 24 h PI. Bacterial replication was measured during the late stages (24–48 h PI) of infection by allowing Francisella to infect epithelial cells for 22 h, washing the samples with PBS, then adding gentamicin to kill uninvaded bacteria for 2 h. At 24 h PI, samples were either lysed to quantify intracellular bacteria or allowed to replicate further within epithelial cells for an additional 24 h in the presence of low concentrations of gentamicin.
Differential bacterial immunolabeling
The method used for differential (inside/outside) bacterial labeling was based on previously published work [31]. To immunolocalize extracellular bacteria, 3% paraformaldehyde-fixed/non-permeabilized samples were washed with PBS, blocked with 5% normal goat serum (NGS) at RT for 20 min, and stained using a 1∶1000 dilution of rabbit anti-Francisella antibody [69] in PBS containing 0.1% BSA (PBS/BSA) supplemented with 1% NGS for 1 h at 37°C. Subsequently, the samples were washed with PBS/BSA and treated with 1 µg mL−1 of Alexa Fluor 594 goat anti-rabbit IgG (H+L) antibody (in PBS/BSA+1% NGS) for 1 h at 37°C. After washing with PBS/BSA, the samples were permeabilized with 0.2% Triton X-100 in PBS for 15 min, washed with PBS/BSA, and blocked with 5% NGS for an additional 20 min at RT. The samples were then treated with the primary rabbit anti-Francisella antibody [diluted 1∶1000 in PBS/BSA containing 0.05% Tween-20 (TPBS/0.1% BSA) and supplemented with 1% NGS] for 1 h, washed with TPBS/BSA, incubated with 1 µg mL−1 Alexa Fluor 488 conjugated goat anti-rabbit IgG (H+L) antibodies prepared in TPBS/BSA+1% NGS for 1 h at 37°C, washed with TPBS/BSA, and mounted using ProLong Gold antifade reagent with DAPI. This procedure labels intracellular bacteria green and extracellular bacteria (red and green in merged panels). Unless otherwise stated, all washes were repeated 3 times and lasted a total of 30 min.
To quantify the proportion of intracellular bacteria and lysosomal-associated membrane protein 1 (LAMP1), all samples were infected for 3 h then treated with gentamicin for 1 h. For 8, 12, and 24 h time-points, the infections were allowed to proceed in the presence of gentamicin (10 µg mL−1) until the experimental endpoints. Localization of Francisella required the use of mouse anti-Francisella 2H1 antibodies (1∶100) [Immunoprecise Antibodies] in combination with Alexa Fluor 350 and 594 goat anti-mouse IgG (H+L) antibodies to discriminate between intracellular (red and blue overlap) and extracellular (blue) bacteria. Following permeabilization of cell membranes, rat anti-LAMP1 1D4B antibodies (1∶50) [Developmental studies hybridoma bank] were used in combination with either Alexa Fluor 488 goat anti-rat (1∶100) to localize LAMP1. These coverslips were mounted with the ProLong Gold antifade reagent.
Image and statistical analysis
A Leica DM4000B inverted fluorescence microscope attached to an Angstrom Grid Confocal system [Quorum Technologies] was used to view the samples and Metamorph Software was used to capture the images. ImageJ version 1.44i (http://imagej.nih.gov/ij) was used to count the number of invaded bacteria from images captured by either epifluorescence or structured illumination microscopy. Adobe Photoshop CS5 was used to process immunofluorescence images without changing the integrity of the data. To calculate the population of cells in each image, we semi-automatically measured the number of DAPI-stained cell nuclei using the “nucleus counter” plug-in, which is part of the McMaster Biophotonics Facility ImageJ bundle (http://www.macbiophotonics.ca/downloads.htm). In the nucleus counter plug-in, the following parameters were adjusted to tally the number of nuclei in each image [taken at 40X magnification]: 2000, ‘Smallest Particle Size’; 6000, ‘Largest Particle Size’, Mean 3×3, ‘Smooth method’; enabled, ‘Watershed filter’. In case there were any miscounted nuclei or multi-nucleated cells, each image was further reviewed by overlaying the DAPI-stained image with the phase-contrast image. Within the population of adherent hepatocytes, infected and uninfected cells were manually tallied. Each infected cell was given a score of ‘1’ based on the presence of F. novicida within the cell boundaries, whereas each uninfected cell that had an absence of intracellular F. novicida was given a score of ‘0’. The proportion of infected cells was calculated based on the number of infected cells divided by the total number of cells in each image. To determine whether Francisella was within a LAMP1 containing vacuole, we looked for bacteria that were at least 50% surrounded or completely co-localized with LAMP1.
Statistical analysis was performed using Graphpad Prism 6 software. Statistical significance was calculated using one-way ANOVA followed by Bonferroni multiple comparison test for data in Fig. 1, 2 and 3. Data in Fig. 4 and 7 were analyzed by Two-way ANOVA followed by Bonferroni multiple comparison test, whereas for Fisher’s LSD test was used for data in Fig. 8.
Results
IglC and PdpA are required for efficient epithelial cell invasion
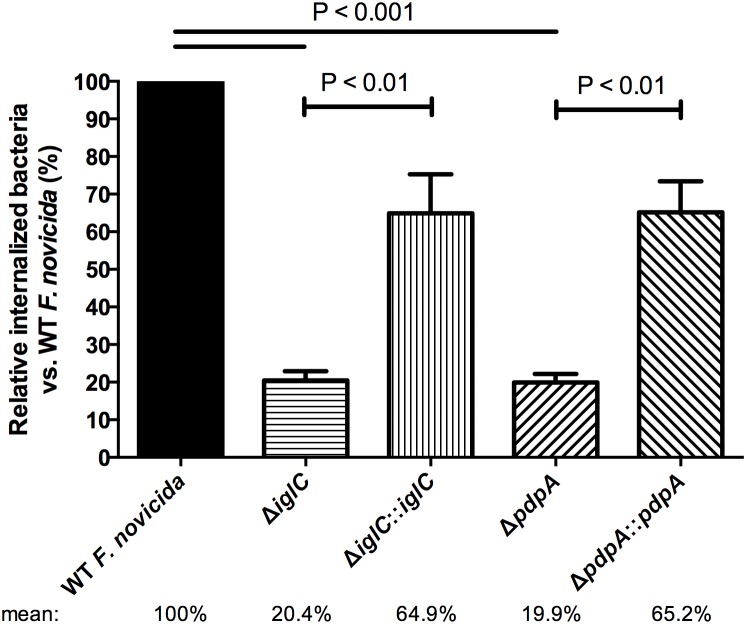
The involvement of the FPI genes iglC and pdpA has been examined during macrophage infections and was shown to be important for intracellular replication, but not for the uptake of Francisella into those cells [34], [48], [49]. To begin to investigate whether iglC and pdpA play a role in bacterial entry into epithelial cells, we evaluated the internalization of wild-type F. novicida, deletion mutants (ΔiglC, ΔpdpA), and their respective gene complemented strains during murine liver BNL CL.2 cell infections using gentamicin protection/invasion assays. These assays are common microbiological experiments used to quantify the amount of intracellular bacteria in an entire sample. Because minimizing the amount of intracellular bacterial replication is a general concern when performing these assays [21], [42], [70], we allowed F. novicida to contact and invade BNL CL.2 cells for 3 h before treating the samples with gentamicin for 1 h to kill the extracellular microbes. This time-point was selected because there are extremely few bacteria that are detectable by plating during infections lasting <3 h (unpublished data). Thus, at 4 h PI, host cells were lysed and intracellular bacteria were plated onto solid media. Using this procedure, we found a significant reduction of intracellular bacteria in samples infected with ΔiglC [20.4%] and ΔpdpA [19.9%] when normalized against wild-type F. novicida invasion [100%] (Figure 1). Invasion was significantly restored for both ΔiglC::iglC [64.9%] and ΔpdpA::pdpA [65.2%] when genes were re-introduced back into the microbe (Figure 1). Our bacterial deletion data at this early time-point suggest that IglC and PdpA influence F. novicida invasion into epithelial cells.
Figure 1. Deletion of genes encoding IglC and PdpA perturb F. novicida invasion.
Murine BNL CL.2 hepatocytes were infected with wild-type F. novicida, deletion mutants (ΔiglC and ΔpdpA) as well as complement strains (ΔiglC::iglC and ΔpdpA::pdpA) for 3 h. Subsequently, samples were washed and treated with gentamicin for 1 h. At 4 h PI, lysates were plated onto agar-containing media and bacterial colonies were enumerated the following day. Error bars, S.E.M. (n = 4).
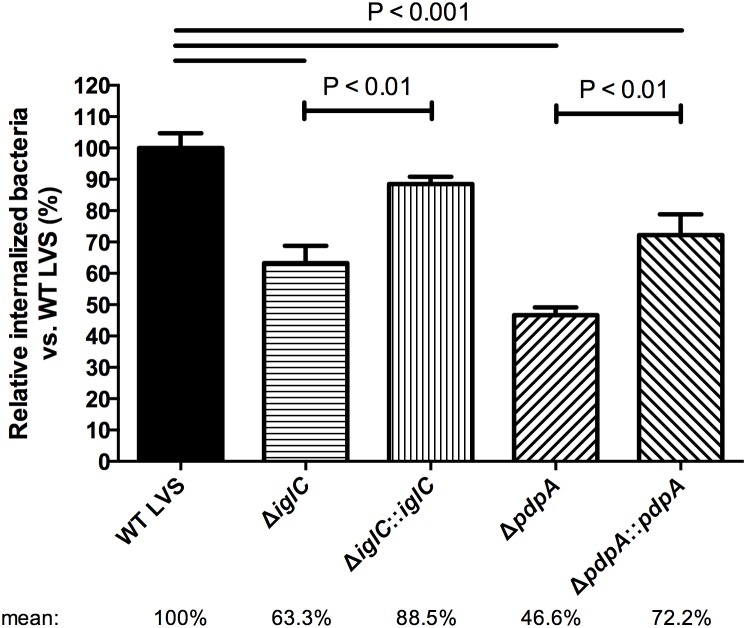
To determine whether these findings were F. novicida specific or if they were more broadly applicable to Francisella in general we ran similar assays using F. tularensis LVS infected A549 epithelial cells. We chose human lung A549 cells over BNL CL.2 cells for this assay primarily because of the low infections rates BNL CL.2 cells show at 4 h when infected with F. tularensis LVS. We found that F. tularensis LVS ΔiglC and ΔpdpA infected at a rate of 63.3% and 46.6% as compared to wild-type [100%] (Figure 2). Although this was significantly lower than wild-type F. tularensis LVS, it was not as dramatic as the decrease seen with F. novicida (Figure 1). A significant improvement in the numbers of intracellular bacteria was found when complemented strains were used (Figure 2), thus supporting our hypothesis that IglC and PdpA both play a role in the epithelial internalization process.
Figure 2. F. tularensis LVS ΔiglC and ΔpdpA mutants lung epithelial cell infections.
Bacteria were centrifuged onto human A549 cells and allowed to invade for 3 h. To determine the amount of invaded bacteria, gentamicin protection assay (invasion assay) was performed at 4 h PI and bacterial titre was measured after a 3-day incubation. Error bars, S.E.M. (n = 3).
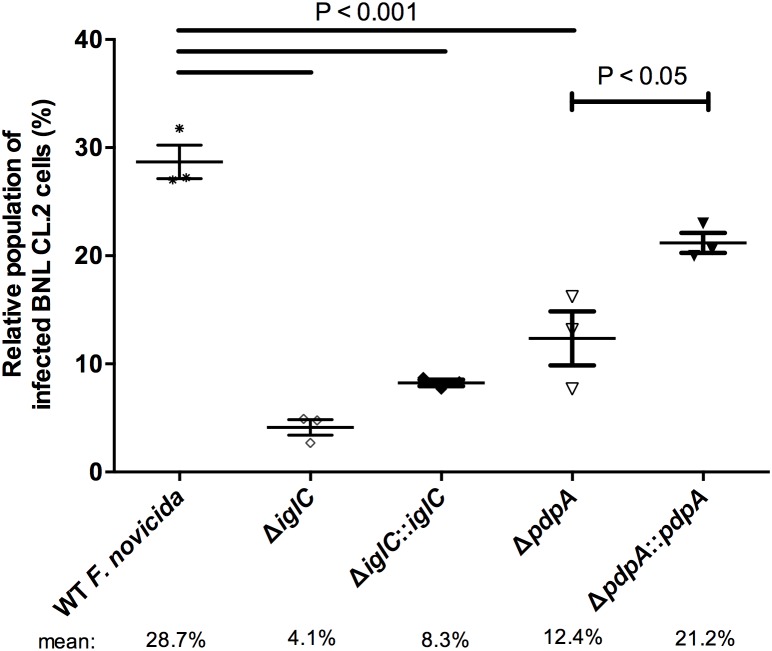
Given that our evidence showed that gene deletion of iglC and pdpA decreased the levels of intracellular bacteria, we then further studied this phenotype with F. novicida using fluorescence microscopy. These infections were performed for 24 h, instead of 4 h, because short infections resulted in <1% of total colonized hepatic cells when examined by microscopy. To distinguish infected and uninfected cells, hepatocytes were infected separately with wild-type F. novicida, deletion mutants (ΔiglC and ΔpdpA) and their respective complement strains. Samples were then fixed and labeled using differential bacterial staining, which allows extracellular (Figure S1; arrow) and intracellular bacteria (Figure S1; arrowhead) to be distinguished. After enumerating >1,000 cells, we found that wild-type F. novicida infected approximately 28.7% of BNL CL.2 cells (Figure 3), which is in-line with previous reports [15], [31]. The microscopic images point to both invasion and bacterial replication deficiencies during these mutant F. novicida infections, as extremely few bacteria were found in the cells in general. In cells that had intracellular bacteria, clusters of F. novicida that would be expected if bacterial replication were functional were not observed. Additionally, the population of cells colonized by ΔiglC [4.1%] and ΔpdpA [12.4%] mutants were significantly lower as compared to wild-type (Figure 3). Gene complementation of pdpA back into its respective deletion mutant significantly increased colonization [21.2%]. Although we observed a similar doubling in bacterial colonization for ΔiglC::iglC [8.3%] over the mutant strain, this increase was not significant (Figure 3). Together, our 24 h microscopic data provided similar results to the F. novicida gentamicin protection/invasion assays taken at 4 h, suggesting that iglC and pdpA genes are involved in both bacterial invasion and early stage replication within epithelial cells.
Figure 3. F. novicida lacking either IglC or PdpA reduces liver epithelial cell colonization.
Samples were fixed at 24 h PI, differentially stained for intracellular and extracellular bacteria, and then visualized by fluorescence microscopy. The proportion of infected cells was tallied from over 1,000 cells. Cells containing one or more intracellular bacteria are considered ‘infected’. Error bars, S.E.M. (n = 3).
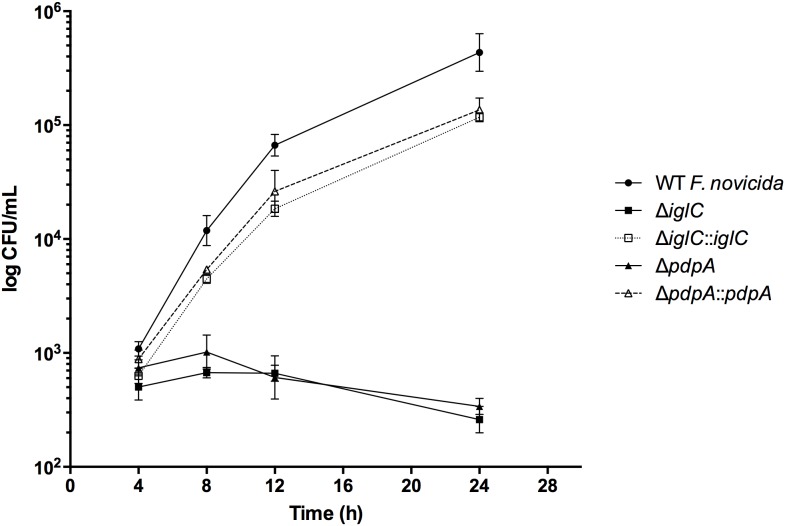
To further study the influence that iglC and pdpA have on intracellular replication, we infected mouse BNL CL.2 cells with wild-type F. novicida and mutants (ΔiglC, ΔiglC::iglC, ΔpdpA, and ΔpdpA::pdpA) and allowed them to invade for 3 h. The hepatocytes were then kept in gentamicin-containing media for up to 24 h, when the total intracellular bacterial loads were measured. We found that F. novicida deletion mutants ΔiglC and ΔpdpA did not show significant growth over the course of the infection (Figure 4), but rather, the population of intracellular ΔiglC and ΔpdpA declined marginally as early as 8 h PI (Figure 4). In contrast, wild-type F. novicida grew very rapidly from 4 to 8 h (Figure 4), with an average doubling time of 1.16 h, which slightly outpaced that of ΔiglC::iglC [1.53 h] and ΔpdpA::pdpA [1.41 h] (Table S1). By 12 h, the live growth was about 3-fold less and the doubling time for wild-type F. novicida, ΔiglC::iglC, and ΔpdpA::pdpA respectively increased to 4.44, 4.49, and 5.05 h (Table S1). These results demonstrate that the early stage replicative deficiencies seen with F. novicida ΔiglC and ΔpdpA at 4 h PI were maintained up to 24 h following epithelial cell infections.
Figure 4. Intracellular growth kinetics of F. novicida mutants during hepatocyte infections.
BNL CL.2 cells were infected with wild-type F. novicida, deletion mutants (ΔiglC and ΔpdpA) and their respective complements. Bacteria were allowed to invade for 3 h after which extracellular bacteria were rapidly washed with PBS and killed with 100 µg mL−1 of gentamicin for 1 h. Low concentrations of gentamicin (10 µg mL−1) remained in the media (to inhibit extracellular bacteria) until experimental endpoint. Intracellular bacteria were then released by lysing host cells, diluted with TSBC, and plated for bacterial enumeration. Error bars, S.E.M. (n = 3).
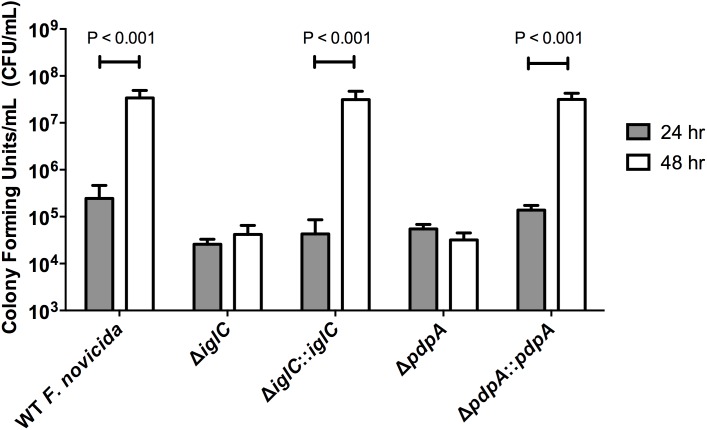
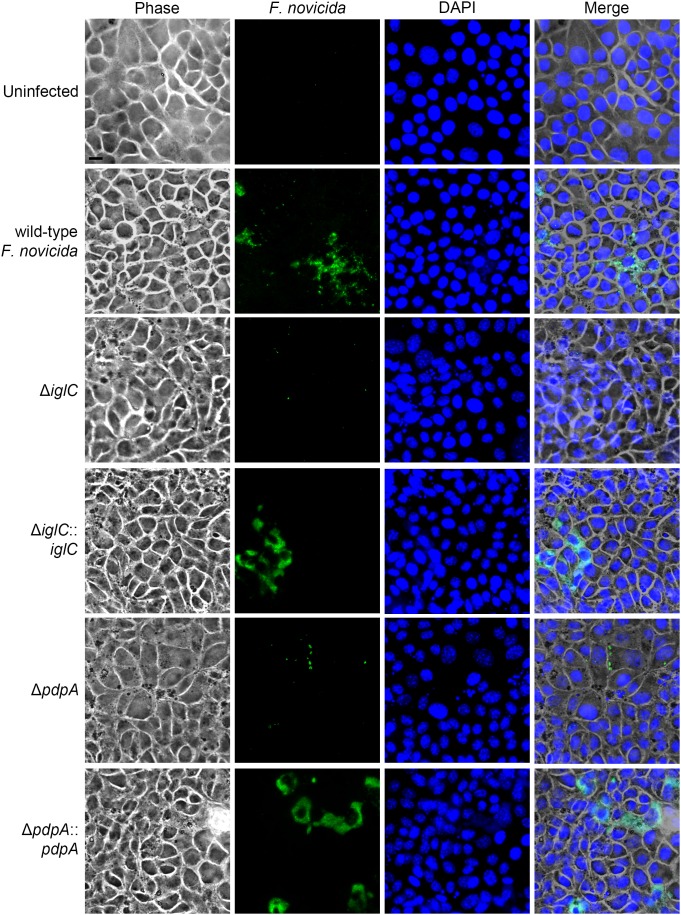
We also examined whether IglC and PdpA were important for bacterial replication during the late phase of its intracellular lifecycle. To test this, we compared the bacterial burden of F. novicida in BNL CL.2 cells at 24 h post-inoculation with a ‘prolonged’ 48 h infection in the absence of additional bacterial internalization by treating the cells with fresh media containing 100 µg mL−1 of gentamicin at the 22 h time-point, which was followed and maintained by 10 µg mL−1 of gentamicin from 24–48 h. We found that the amount of internalized wild-type F. novicida had increased by ∼100-fold in the final 24 h of infection (by the 48 h time-point) (Figure 5). During the same period, the ΔiglC and ΔpdpA F. novicida mutants both did not have a replicative burst (Figure 5). In contrast, gene complementation of ΔiglC::iglC and ΔpdpA::pdpA replicated to nearly wild-type F. novicida levels (Figure 5). Concurrently, we qualitatively assessed intracellular bacterial replication by fluorescence microscopy. Clusters of bacteria were found in colonized BNL CL.2 cells infected with wild-type F. novicida, as well as ΔiglC::iglC and ΔpdpA::pdpA complement strains; many of which were completely filled with bacteria (Figure 6). In contrast, F. novicida-filled cells were rarely (if ever) observed when hepatocytes were infected with ΔiglC and ΔpdpA deletion mutants and most infected cells contained only a small number of bacteria (Figure 6).
Figure 5. Intracellular bacterial replication is severely compromised when genes encoding iglC and pdpA are deleted.
24 h and 48 h gentamicin protection assays were performed on liver BNL CL.2 cells infected with wild-type F. novicida, deletion mutants (ΔiglC and ΔpdpA), and their respective complement strains (ΔiglC::iglC and ΔpdpA::pdpA). Samples were then treated with gentamicin starting from 22 h post-inoculation until the experimental endpoint. After host cells were lysed, the released bacteria were diluted and plated for CFU enumeration. Error bars, S.D. (n = 4).
Figure 6. IglC and PdpA are essential for robust F. novicida growth within hepatocytes.
Phase and fluorescence microscopic images were taken of BNL CL.2 cells infected with wild-type F. novicida, deletion mutants (ΔiglC and ΔpdpA), and complement strains (ΔiglC::iglC and ΔpdpA::pdpA) for 48 h. At 22 h post-inoculation, the samples were washed with PBS and replaced with media containing gentamicin to prohibit further bacterial invasion. F. novicida (green) and DNA (blue, DAPI) were stained in the fixed samples. Each image represents a ‘maximum intensity’ Z-projection comprising a stack through the cell body. Images taken by fluorescence and phase microscopy were merged together to illustrate the cell borders. Scale bar = 10 µm.
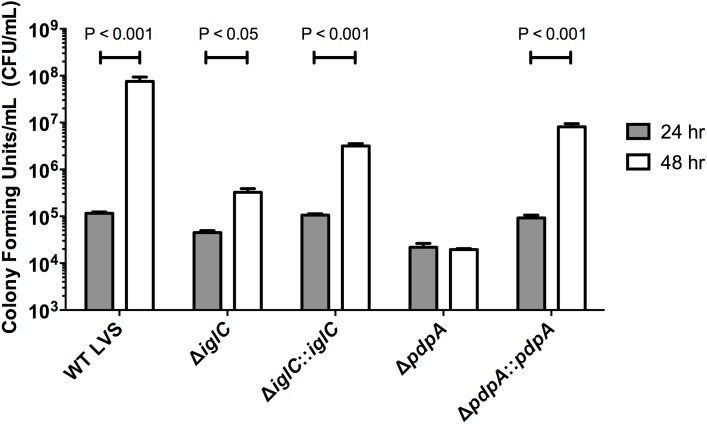
To determine whether this late-stage replicative phenotype was F. novicida specific we performed identical assays on F. tularensis LVS-infected A549 cells and found similar results; that F. tularensis LVS ΔiglC and ΔpdpA were both attenuated in their abilities to rapidly grow within infected cells at 48 h as compared to wild-type Francisella LVS (Figure 7). Interestingly, we noticed a gain in the amount of intracellular ΔiglC (Figure 7), which was not apparent when assayed with F. novicida (Figure 5). Increased bacterial levels were again seen with the gene complement strains ΔiglC::iglC and ΔpdpA::pdpA (Figure 7). Taken together this supporting evidence indicates that iglC and pdpA genes are important for efficient bacterial proliferation during all stages of epithelial cell infection.
Figure 7. During the late intracellular phase, IglC and PdpA are necessary for efficient proliferation in lung epithelial cells.
Human A549 cells were infected by wild-type F. tularensis LVS, ΔiglC, ΔpdpA, ΔiglC::iglC and ΔpdpA::pdpA. Intracellular bacteria were enumerated at 24 and 48 h time-points using gentamicin protection assay. At 24 h PI, the sample was switched to a low gentamicin concentration (10 µg mL−1) in order to inhibit growth of extracellular microbes. Intracellular bacteria were titred after they were released from host cells and serial diluted onto agar-containing media. Error bars, S.E.M (n = 3).
IglC and PdpA are crucial virulence factors for intracellular proliferation and LAMP1-positive FCV dissolution
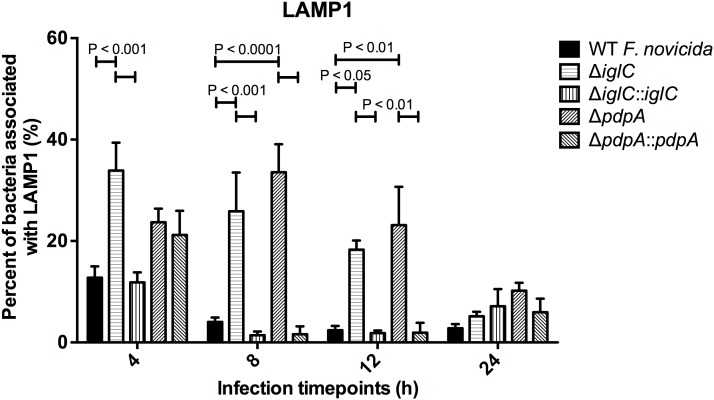
Following bacterial entry in macrophages, Francisella are found enclosed within a membrane-bound compartment referred to as the Francisella-containing vacuole (FCV) [42]. The bacteria can reside within FCVs for up to few hours [70] until they escape into the cytoplasm where it is favorable for replication [42], [49]. Previous phagocytic cell studies have demonstrated that proficient escape from FCVs requires the presence of IglC [45], [46]. Yet, it is not known whether the same is true for PdpA. LAMP1 is a commonly used marker of FCVs and its presence or absence is indicative of the maintenance or dissolution of the FCV. Given that iglC and pdpA influence intracellular bacterial growth in both macrophages [32], [71] and epithelial cells, and because it is known that replication occurs after Francisella escape from the FCVs during macrophage infections [70], we investigated the temporal dynamics of LAMP1 around intracellular F. novicida at 4, 8, 12 and 24 h PI in order to determine whether iglC and pdpA affected its localization. To investigate this, we infected BNL CL.2 cells for 3 h with wild-type F. novicida as well as iglC and pdpA mutants and their complemented strains. Extracellular bacteria were then washed away and exposed to gentamicin for up to 24 h then processed for bacterial and LAMP1 localization.
We found that there was a significant increase in the number of bacteria associated with LAMP1 when ΔiglC [33.9%, 4 h; 25.9%, 8 h; 18.3%, 12 h] was compared to wild-type F. novicida [12.8%, 4 h; 4.0%, 8 h; 2.4%, 12 h] up to 12 h PI (Figure 8). Similarly ΔpdpA (33.6%, 8 h; 23.1%, 12 h) showed a significant increase in localization events around F. novicida between 8 and 12 h PI when compared to wild-type F. novicida (Figure 8). Although there was a was a delay in the phenotypic effects of the pdpA complementation until the 8 h time-point, the observation of increased association of LAMP1 around the mutant F. novicida suggests that those microbes were impaired in their ability to break out of the FCV, thus remaining in the vacuolar compartment.
Figure 8. Proportion of F. novicida associated with LAMP1 during murine hepatocyte infections.
(A) wild-type F. novicida, deletion mutants (ΔpdpA, ΔiglC) and complements strains (ΔpdpA::pdpA, ΔiglC::iglC) invaded BNL CL.2 cells for 3 h, after which extracellular bacteria were washed off and then killed with gentamicin (100 µg mL−1). Subsequently, samples were exposed to low gentamicin concentration until the experimental endpoint was reached. Image stacks were assembled and used to determine the frequency of LAMP1-associated bacteria. For time-points 4, 8 and 12 h, between 30 and 50 intracellular bacteria were counted. For the 24 h time-point, more than 50 intracellular bacteria were counted. Error bars, S.E.M. (n = 3).
Discussion
Research on the sub-cellular events underlying Francisella pathogenesis has primarily concentrated on phagocytic cell infections, while those involved in non-phagocytic epithelial cell infections have remained largely unexplored. This has occurred despite epithelial cells being a primary site of infection and carrying a considerable bacterial load [15], [63], [64], [72]. Given the FPI’s importance for phagocytic cell infections, we began by investigating whether two of the FPI components, IglC and PdpA, affected bacterial entry and replication in epithelial cells. In order to examine this, we used iglC and pdpA deletion mutants from 2 Francisella bacteria; F. novicida and Francisella LVS. We initially found that both iglC and pdpA were required for bacterial internalization into liver and lung epithelial cells. To investigate a potential mechanism responsible for the replication impedance that the ΔiglC and ΔpdpA mutants showed, we turned to the FCVs. Francisella is known to rapidly replicate in the cytosol of macrophages and both IglC and PdpA are needed for that process to occur efficiently. By using a common marker for FCVs, LAMP1, we found that LAMP1 localization to ΔiglC and ΔpdpA F. novicida was maintained long after the wild-type bacteria had shed the LAMP1 protein, suggesting that the FCVs were maintained for a longer duration during the mutant infections as compared to the wild-type bacteria. This is consistent with past epithelial [55] and phagocyte studies [38], [42]. The increased time housed within the FCVs could conceivably impede replication during that time, thus contributing to the decreased bacterial levels seen with the mutants. Although LAMP1 localization was essentially gone by 24 hours in all samples, the delay in FCV breakdown could explain the significant differences seen throughout the 48 h time-points. If FCV escape is inhibited there is the possibility that gentamicin that was added to kill the extracellular Francisella could have accumulated within endosomes and fused with the FCVs to kill the FCV contained bacteria. However in other systems where the influence of gentamicin on epithelial cell infections had been assayed this was found to not be the case [73]. In a study that looked directly at this possibility Martinez-Moya and co-workers found that in epithelial cells infected with Salmonella Typhimurium for up to 72 hours and had gentamicin in the extracellular milieu, gentamicin did not accumulate in intracellularly [73]. This was contrary to phagocytic dendritic cells, which did have gentamicin accumulation [73].
Francisella use different strategies to gain entry into non-phagocytic and phagocytic cells. During phagocytic cell (macrophage) infections, Francisella are engulfed by host cells through phagocytic mechanisms [74]–[76]. In contrast to macrophage invasion, we previously found that F. novicida and F. tularensis LVS utilize clathrin-dependent mechanisms together with cholesterol- to enter hepatocytes [15]. The additional strategy of macropinocytosis has been met with controversy as one group claims an involvement [77], whereas others exclude the possibility [15], [55]. Worth noting is that clear actin-based membrane ruffling at sites of bacterial entry that are required for macropinocytosis have never been documented.
During Francisella infections, nearly all of the genes within the FPI are necessary for full virulence in vivo as well as for replication within macrophages [26], [28], [32], [34], [50], [78]–[82], but are not required for entry during phagocytic cell infections [27]. We speculate that the FPI does not significantly influence the phagocytic process and thus does not alter other bacterial surface molecules recognized by host phagocytic receptors. Conversely, when Francisella invade epithelial cells, our findings suggest that both IglC and PdpA are required for efficient Francisella internalization, this further suggests that these components could somehow influence the clathrin-based internalization processes occurring in the host. Whether this alters bacterial ligands, host receptors, or intracellular host internalization mechanisms remains to be elucidated. IglC has been implicated as a component of the Francisella T6SS itself [27] and evidence from other systems has indicated that the T6SS can influence bacterial invasion. Studies on Campylobacter jejuni and Pseudomonas aeruginosa have shown that these microbes utilize T6SSs to enhance bacterial invasion into epithelial cells [83], [84]. Because IglC and PdpA have been detected within the cytoplasm of macrophages, it is conceivable that they could also act as T6SS-dependent effectors [37]. However, the binding partners and precise functions of those factors remain unknown. Because ΔiglC and ΔpdpA mutants retained some ability to invade, we surmise that Francisella employ additional mechanisms for entry into epithelial cells.
An inconsistency that we are faced when we examined bacterial invasion was that while the ΔpdpA::pdpA and ΔiglC::iglC F. novicida both had about 3 times the CFUs at 4 h over the mutant strains (Figure 1) and about double the number of cells invaded when examined microscopically, the ΔiglC::iglC complement did not increase invasion levels significantly over ΔiglC when tested by differential staining. What factors could have influenced this? Potential reasons for this could lie in the abundance, proper localization or proper orientation of IglC in the microbe when ectopically expressed. These features could have influenced individual invasion events, while not impeding replication once the bacteria had invaded. Because the 4 h CFU-based invasion assays assessed both the invasion and early stages of replication while the 24 h microscopic assays only examined the number of invaded cells, without addressing the number of individual bacterial cells within each host cell, this could have also compounded our differing complementation results.
Even though others have used centrifugation to force the attachment of Francisella to the cell surface thereby allowing bacterial invasion to be assessed at earlier time-points and to “synchronize” the infections [21], [42], [55], [85], we would prefer to not introduce additional variables into the experiments and thus not force bacterial contact with the host cells if this can be avoided. Consequently, we allowed F. novicida to naturally contact the cell surface and elicit its own internalization. We are confident that the vast majority of the bacteria we measured at the 4 h time-point are those of invaded bacteria, because significant bacterial replication is not detected until >4 h post-infection, even when centrifugation is used [21], [42], [70]. However, when we used this infection approach on F. tularensis LVS, we were unable to detect F. tularensis LVS invasion at 4 h. Thus, in order to obtain sufficient invasion, we found that we needed to centrifuge the bacteria onto the cells. To ensure that only intracellular bacteria were counted, we performed concurrent infections in order to detect that no Francisella appeared on plates in the absence of epithelial cells (to mimic the extracellular bacteria present during the invasion assays). This indicated to us that the gentamicin was effective at killing any extreacellular Francisella (data not shown).
Our work studying the influence of two of the FPI genes, IglC and PdpA, during Francisella epithelial cell infections has highlighted important differences in epithelial versus macrophage internalization, while demonstrating that Francisella replication is likely governed through similar mechanisms regardless of the cell-type infected. This study provides a framework for elucidating the detailed roles of individual FPI components in both the internalization and replicative phases of the bacterial lifecycle and will ultimately demonstrate how host epithelial cell processes can be subverted by foreign proteins.
Supporting Information
Phase and fluorescence micrographs were taken of uninfected and F. novicida infected hepatocytes at 24 h PI. Mouse BNL CL.2 cells were infected with wild-type F. novicida and mutants ΔiglC, ΔiglC::iglC, ΔpdpA and ΔpdpA::pdpA for 22 h. Afterwards, samples were washed, treated with gentamicin for 2 h, and then fixed with 3% paraformaldehyde. Fixed samples were prepared using an immunolocalization technique that can differentiate extracellular (green and red co-localization, arrows) and intracellular bacteria (green only, arrowheads). Each fluorescence image represents a superimposed ‘maximum intensity’ Z-projection image around the cell nucleus (blue). Scale bar = 10 µm.
(TIF)
Bacterial doubling time during the early intracellular stages in hepatocytes.
(DOCX)
Acknowledgments
We would like to thank Dr. Anders Sjostedt (Umeå University) for providing the ΔiglC F. tularensis LVS and complemented bacterial strains. The LAMP1 monoclonal antibody developed by J. Thomas August was obtained from the Developmental Studies Hybridoma Bank, created by the NICHD of the NIH and maintained at The University of Iowa, Department of Biology, Iowa City, IA 52242.
Funding Statement
This work was supported by the Canadian Institute for Health Research (http://www.cihr-irsc.gc.ca/) and Natural Sciences and Engineering Research Council of Canada (NSERC) (http://www.nserc-crsng.gc.ca/). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Sjöstedt AB (2005) Francisella. In The Proteobacteria, Part B. In: Brenner DJ, Staley JT, Garrity GM, editors. Bergey’s Manual of Systematic Bacteriology. 2 ed. New York, NY: Springer. 200–210.
- 2. Santic M, Al-Khodor S, Abu Kwaik Y (2010) Cell biology and molecular ecology of Francisella tularensis . Cell Microbiol 12: 129–139. [DOI] [PubMed] [Google Scholar]
- 3. Rohmer L, Fong C, Abmayr S, Wasnick M, Larson Freeman TJ, et al. (2007) Comparison of Francisella tularensis genomes reveals evolutionary events associated with the emergence of human pathogenic strains. Genome Biol 8: R102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Huber B, Escudero R, Busse HJ, Seibold E, Scholz HC, et al. (2010) Description of Francisella hispaniensis sp. nov., isolated from human blood, reclassification of Francisella novicida (Larson, et al. 1955) Olsufiev, et al. 1959 as Francisella tularensis subsp. novicida comb. nov. and emended description of the genus Francisella. Int J Syst Evol Microbiol 60: 1887–1896. [DOI] [PubMed] [Google Scholar]
- 5. Busse HJ, Huber B, Anda P, Escudero R, Scholz HC, et al. (2010) Objections to the transfer of Francisella novicida to the subspecies rank of Francisella tularensis - response to Johansson, et al. Int J Syst Evol Microbiol 60: 1718–1720. [DOI] [PubMed] [Google Scholar]
- 6.Johansson A, Celli J, Conlan W, Elkins KL, Forsman M, et al. (2010) Objections to the transfer of Francisella novicida to the subspecies rank of Francisella tularensis. Int J Syst Evol Microbiol 60: 1717–1718; author reply 1718–1720. [DOI] [PMC free article] [PubMed]
- 7. Larsson P, Elfsmark D, Svensson K, Wikstrom P, Forsman M, et al. (2009) Molecular evolutionary consequences of niche restriction in Francisella tularensis, a facultative intracellular pathogen. PLoS Pathog 5: e1000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kitamura S, Fukada M, Takeda H, Ouchi S, Nakano S, et al. (1956) Pathology of Tularemia. Pathology International 6: 46. [Google Scholar]
- 9. Evans ME, Gregory DW, Schaffner W, McGee ZA (1985) Tularemia: a 30-year experience with 88 cases. Medicine (Baltimore) 64: 251–269. [PubMed] [Google Scholar]
- 10. Roth KM, Oghumu S, Satoskar AA, Gunn JS, van Rooijen N, et al. (2008) Respiratory infection with Francisella novicida induces rapid dystrophic cardiac calcinosis (DCC). FEMS Immunol Med Microbiol 53: 72–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Park CH, Nakanishi A, Hatai H, Kojima D, Oyamada T, et al. (2009) Pathological and microbiological studies of Japanese Hare (Lepus brachyurus angustidens) naturally infected with Francisella tularensis subsp. holarctica . J Vet Med Sci 71: 1629–1635. [DOI] [PubMed] [Google Scholar]
- 12. Fortier AH, Slayter MV, Ziemba R, Meltzer MS, Nacy CA (1991) Live vaccine strain of Francisella tularensis: infection and immunity in mice. Infect Immun 59: 2922–2928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Miller MA, Stabenow JM, Parvathareddy J, Wodowski AJ, Fabrizio TP, et al. (2012) Visualization of murine intranasal dosing efficiency using luminescent Francisella tularensis: effect of instillation volume and form of anesthesia. PLoS One 7: e31359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Abril C, Nimmervoll H, Pilo P, Brodard I, Korczak B, et al. (2008) Rapid diagnosis and quantification of Francisella tularensis in organs of naturally infected common squirrel monkeys (Saimiri sciureus). Vet Microbiol 127: 203–208. [DOI] [PubMed] [Google Scholar]
- 15. Law HT, Lin AE, Kim Y, Quach B, Nano FE, et al. (2011) Francisella tularensis uses cholesterol and clathrin-based endocytic mechanisms to invade hepatocytes. Sci Rep 1: 192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hall JD, Craven RR, Fuller JR, Pickles RJ, Kawula TH (2007) Francisella tularensis replicates within alveolar type II epithelial cells in vitro and in vivo following inhalation. Infect Immun 75: 1034–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ellis J, Oyston PC, Green M, Titball RW (2002) Tularemia. Clin Microbiol Rev 15: 631–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Stuart BM, Pullen RL, Roscoe L (1945) Tularemic pneumonia: Review of American literature and report of 15 additional cases. Am J Med Sci 210: 14. [Google Scholar]
- 19. Santic M, Molmeret M, Klose KE, Abu Kwaik Y (2006) Francisella tularensis travels a novel, twisted road within macrophages. Trends Microbiol 14: 37–44. [DOI] [PubMed] [Google Scholar]
- 20. Anthony LD, Burke RD, Nano FE (1991) Growth of Francisella spp. in rodent macrophages. Infect Immun 59: 3291–3296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lindemann SR, McLendon MK, Apicella MA, Jones BD (2007) An in vitro model system used to study adherence and invasion of Francisella tularensis live vaccine strain in nonphagocytic cells. Infect Immun 75: 3178–3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kraemer PS, Mitchell A, Pelletier MR, Gallagher LA, Wasnick M, et al. (2009) Genome-wide screen in Francisella novicida for genes required for pulmonary and systemic infection in mice. Infect Immun 77: 232–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. McRae S, Pagliai FA, Mohapatra NP, Gener A, Mahmou AS, et al. (2010) Inhibition of AcpA phosphatase activity with ascorbate attenuates Francisella tularensis intramacrophage survival. J Biol Chem 285: 5171–5177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Nano FE, Schmerk C (2007) The Francisella pathogenicity island. Ann N Y Acad Sci 1105: 122–137. [DOI] [PubMed] [Google Scholar]
- 25. Rotz LD, Khan AS, Lillibridge SR, Ostroff SM, Hughes JM (2002) Public health assessment of potential biological terrorism agents. Emerg Infect Dis 8: 225–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schmerk CL, Duplantis BN, Wang D, Burke RD, Chou AY, et al. (2009) Characterization of the pathogenicity island protein PdpA and its role in the virulence of Francisella novicida . Microbiology 155: 1489–1497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. de Bruin OM, Duplantis BN, Ludu JS, Hare RF, Nix EB, et al. (2011) The biochemical properties of the Francisella pathogenicity island (FPI)-encoded proteins IglA, IglB, IglC, PdpB and DotU suggest roles in type VI secretion. Microbiology 157: 3483–3491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cong Y, Yu JJ, Guentzel MN, Berton MT, Seshu J, et al. (2009) Vaccination with a defined Francisella tularensis subsp. novicida pathogenicity island mutant (ΔiglB) induces protective immunity against homotypic and heterotypic challenge. Vaccine 27: 5554–5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mares CA, Sharma J, Ojeda SS, Li Q, Campos JA, et al. (2010) Attenuated response of aged mice to respiratory Francisella novicida is characterized by reduced cell death and absence of subsequent hypercytokinemia. PLoS One 5: e14088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jones CL, Weiss DS (2011) TLR2 signaling contributes to rapid inflammasome activation during F. novicida infection. PLoS One 6: e20609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lo KY, Chua MD, Abdulla S, Law HT, Guttman JA (2013) Examination of in vitro epithelial cell lines as models for Francisella tularensis non-phagocytic infections. J Microbiol Methods 93: 153–160. [DOI] [PubMed] [Google Scholar]
- 32. Nano FE, Zhang N, Cowley SC, Klose KE, Cheung KK, et al. (2004) A Francisella tularensis pathogenicity island required for intramacrophage growth. J Bacteriol 186: 6430–6436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Golovliov I, Sjostedt A, Mokrievich A, Pavlov V (2003) A method for allelic replacement in Francisella tularensis. FEMS Microbiol Lett 222: 273–280. [DOI] [PubMed] [Google Scholar]
- 34. Broms JE, Sjostedt A, Lavander M (2010) The role of the Francisella tularensis pathogenicity Island in type VI secretion, intracellular survival, and modulation of host cell signaling. Front Microbiol 1: 136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Broms JE, Meyer L, Lavander M, Larsson P, Sjostedt A (2012) DotU and VgrG, Core Components of Type VI Secretion Systems, Are Essential for Francisella LVS Pathogenicity. PLoS One 7: e34639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. de Bruin OM, Ludu JS, Nano FE (2007) The Francisella pathogenicity island protein IglA localizes to the bacterial cytoplasm and is needed for intracellular growth. BMC Microbiol 7: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Broms JE, Meyer L, Sun K, Lavander M, Sjostedt A (2012) Unique substrates secreted by the type VI secretion system of Francisella tularensis during intramacrophage infection. PLoS One 7: e50473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Golovliov I, Baranov V, Krocova Z, Kovarova H, Sjostedt A (2003) An attenuated strain of the facultative intracellular bacterium Francisella tularensis can escape the phagosome of monocytic cells. Infect Immun 71: 5940–5950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Clemens DL, Lee BY, Horwitz MA (2004) Virulent and avirulent strains of Francisella tularensis prevent acidification and maturation of their phagosomes and escape into the cytoplasm in human macrophages. Infect Immun 72: 3204–3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Santic M, Molmeret M, Barker JR, Klose KE, Dekanic A, et al. (2007) A Francisella tularensis pathogenicity island protein essential for bacterial proliferation within the host cell cytosol. Cell Microbiol 9: 2391–2403. [DOI] [PubMed] [Google Scholar]
- 41. Wehrly TD, Chong A, Virtaneva K, Sturdevant DE, Child R, et al. (2009) Intracellular biology and virulence determinants of Francisella tularensis revealed by transcriptional profiling inside macrophages. Cell Microbiol 11: 1128–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Checroun C, Wehrly TD, Fischer ER, Hayes SF, Celli J (2006) Autophagy-mediated reentry of Francisella tularensis into the endocytic compartment after cytoplasmic replication. Proc Natl Acad Sci USA 103: 14578–14583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gray CG, Cowley SC, Cheung KK, Nano FE (2002) The identification of five genetic loci of Francisella novicida associated with intracellular growth. FEMS Microbiol Lett 215: 53–56. [DOI] [PubMed] [Google Scholar]
- 44. Santic M, Molmeret M, Klose KE, Jones S, Kwaik YA (2005) The Francisella tularensis pathogenicity island protein IglC and its regulator MglA are essential for modulating phagosome biogenesis and subsequent bacterial escape into the cytoplasm. Cell Microbiol 7: 969–979. [DOI] [PubMed] [Google Scholar]
- 45. Chong A, Wehrly TD, Nair V, Fischer ER, Barker JR, et al. (2008) The early phagosomal stage of Francisella tularensis determines optimal phagosomal escape and Francisella pathogenicity island protein expression. Infect Immun 76: 5488–5499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Lindgren H, Golovliov I, Baranov V, Ernst RK, Telepnev M, et al. (2004) Factors affecting the escape of Francisella tularensis from the phagolysosome. J Med Microbiol 53: 953–958. [DOI] [PubMed] [Google Scholar]
- 47. Bonquist L, Lindgren H, Golovliov I, Guina T, Sjostedt A (2008) MglA and Igl proteins contribute to the modulation of Francisella tularensis live vaccine strain-containing phagosomes in murine macrophages. Infect Immun 76: 3502–3510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Schmerk CL, Duplantis BN, Howard PL, Nano FE (2009) A Francisella novicida pdpA mutant exhibits limited intracellular replication and remains associated with the lysosomal marker LAMP-1. Microbiology 155: 1498–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lai XH, Golovliov I, Sjostedt A (2004) Expression of IglC is necessary for intracellular growth and induction of apoptosis in murine macrophages by Francisella tularensis . Microb Pathog 37: 225–230. [DOI] [PubMed] [Google Scholar]
- 50. Barker JR, Chong A, Wehrly TD, Yu JJ, Rodriguez SA, et al. (2009) The Francisella tularensis pathogenicity island encodes a secretion system that is required for phagosome escape and virulence. Mol Microbiol 74: 1459–1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Conlan JW, North RJ (1992) Early pathogenesis of infection in the liver with the facultative intracellular bacteria Listeria monocytogenes, Francisella tularensis, and Salmonella typhimurium involves lysis of infected hepatocytes by leukocytes. Infect Immun 60: 5164–5171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. KuoLee R, Zhao X, Austin J, Harris G, Conlan JW, et al. (2007) Mouse model of oral infection with virulent type A Francisella tularensis . Infect Immun 75: 1651–1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, et al. (2001) Tularemia as a biological weapon: medical and public health management. JAMA 285: 2763–2773. [DOI] [PubMed] [Google Scholar]
- 54. Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S (1961) Tularemia vaccine study. II. Respiratory challenge. Arch Intern Med 107: 702–714. [DOI] [PubMed] [Google Scholar]
- 55. Craven RR, Hall JD, Fuller JR, Taft-Benz S, Kawula TH (2008) Francisella tularensis invasion of lung epithelial cells. Infect Immun 76: 2833–2842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Larson CL, Wicht W, Jellison WL (1955) A new organism resembling P. tularensis isolated from water. Public Health Rep 70: 253–258. [PMC free article] [PubMed] [Google Scholar]
- 57. Eigelsbach HT, Downs CM (1961) Prophylactic effectiveness of live and killed tularemia vaccines. I. Production of vaccine and evaluation in the white mouse and guinea pig. J Immunol 87: 415–425. [PubMed] [Google Scholar]
- 58. DeTulleo L, Kirchhausen T (1998) The clathrin endocytic pathway in viral infection. EMBO J 17: 4585–4593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Blanchard E, Belouzard S, Goueslain L, Wakita T, Dubuisson J, et al. (2006) Hepatitis C virus entry depends on clathrin-mediated endocytosis. J Virol 80: 6964–6972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Helenius A, Kartenbeck J, Simons K, Fries E (1980) On the entry of Semliki forest virus into BHK-21 cells. J Cell Biol 84: 404–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Veiga E, Guttman JA, Bonazzi M, Boucrot E, Toledo-Arana A, et al. (2007) Invasive and adherent bacterial pathogens co-opt host clathrin for infection. Cell Host Microbe 2: 340–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Van Nhieu GT, Krukonis ES, Reszka AA, Horwitz AF, Isberg RR (1996) Mutations in the cytoplasmic domain of the integrin beta1 chain indicate a role for endocytosis factors in bacterial internalization. J Biol Chem 271: 7665–7672. [DOI] [PubMed] [Google Scholar]
- 63. Horzempa J, O’Dee DM, Shanks RM, Nau GJ (2010) Francisella tularensis ΔpyrF mutants show that replication in nonmacrophages is sufficient for pathogenesis in vivo. Infect Immun 78: 2607–2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Qin A, Mann BJ (2006) Identification of transposon insertion mutants of Francisella tularensis tularensis strain Schu S4 deficient in intracellular replication in the hepatic cell line HepG2. BMC Microbiol 6: 69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Buchan BW, McCaffrey RL, Lindemann SR, Allen LA, Jones BD (2009) Identification of migR, a regulatory element of the Francisella tularensis live vaccine strain iglABCD virulence operon required for normal replication and trafficking in macrophages. Infect Immun 77: 2517–2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. LoVullo ED, Molins-Schneekloth CR, Schweizer HP, Pavelka MS Jr (2009) Single-copy chromosomal integration systems for Francisella tularensis. Microbiology 155: 1152–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Ludu JS, Nix EB, Duplantis BN, de Bruin OM, Gallagher LA, et al. (2008) Genetic elements for selection, deletion mutagenesis and complementation in Francisella spp. FEMS Microbiol Lett 278: 86–93. [DOI] [PubMed] [Google Scholar]
- 68. Barrigan LM, Tuladhar S, Brunton JC, Woolard MD, Chen CJ, et al. (2013) Infection with Francisella tularensis LVS clpB leads to an altered yet protective immune response. Infect Immun 81: 2028–2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Nano FE (1988) Identification of a heat-modifiable protein of Francisella tularensis and molecular cloning of the encoding gene. Microb Pathog 5: 109–119. [DOI] [PubMed] [Google Scholar]
- 70. Santic M, Molmeret M, Abu Kwaik Y (2005) Modulation of biogenesis of the Francisella tularensis subsp. novicida-containing phagosome in quiescent human macrophages and its maturation into a phagolysosome upon activation by IFN-gamma. Cell Microbiol 7: 957–967. [DOI] [PubMed] [Google Scholar]
- 71. Golovliov I, Ericsson M, Sandstrom G, Tarnvik A, Sjostedt A (1997) Identification of proteins of Francisella tularensis induced during growth in macrophages and cloning of the gene encoding a prominently induced 23-kilodalton protein. Infection and immunity 65: 2183–2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Conlan JW, Chen W, Shen H, Webb A, KuoLee R (2003) Experimental tularemia in mice challenged by aerosol or intradermally with virulent strains of Francisella tularensis: bacteriologic and histopathologic studies. Microb Pathog 34: 239–248. [DOI] [PubMed] [Google Scholar]
- 73. Martinez-Moya M, de Pedro MA, Schwarz H, Garcia-del Portillo F (1998) Inhibition of Salmonella intracellular proliferation by non-phagocytic eucaryotic cells. Res Microbiol 149: 309–318. [DOI] [PubMed] [Google Scholar]
- 74. Clemens DL, Lee BY, Horwitz MA (2005) Francisella tularensis enters macrophages via a novel process involving pseudopod loops. Infect Immun 73: 5892–5902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Tamilselvam B, Daefler S (2008) Francisella targets cholesterol-rich host cell membrane domains for entry into macrophages. J Immunol 180: 8262–8271. [DOI] [PubMed] [Google Scholar]
- 76. Geier H, Celli J (2011) Phagocytic receptors dictate phagosomal escape and intracellular proliferation of Francisella tularensis . Infect Immun 79: 2204–2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bradburne CE, Verhoeven AB, Manyam GC, Chaudhry SA, Chang EL, et al.. (2013) Temporal transcriptional response during infection of Type II alveolar epithelial cells with Francisella tularensis LVS supports a general host suppression and bacterial uptake by macropinocytosis. J Biol Chem. [DOI] [PMC free article] [PubMed]
- 78. Tempel R, Lai XH, Crosa L, Kozlowicz B, Heffron F (2006) Attenuated Francisella novicida transposon mutants protect mice against wild-type challenge. Infect Immun 74: 5095–5105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kadzhaev K, Zingmark C, Golovliov I, Bolanowski M, Shen H, et al. (2009) Identification of genes contributing to the virulence of Francisella tularensis SCHU S4 in a mouse intradermal infection model. PLoS One 4: e5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Twine S, Bystrom M, Chen W, Forsman M, Golovliov I, et al. (2005) A mutant of Francisella tularensis strain SCHU S4 lacking the ability to express a 58-kilodalton protein is attenuated for virulence and is an effective live vaccine. Infect Immun 73: 8345–8352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Weiss DS, Brotcke A, Henry T, Margolis JJ, Chan K, et al. (2007) In vivo negative selection screen identifies genes required for Francisella virulence. Proc Natl Acad Sci USA 104: 6037–6042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Robertson GT, Child R, Ingle C, Celli J, Norgard MV (2013) IglE is an outer membrane-associated lipoprotein essential for intracellular survival and murine virulence of type A Francisella tularensis. Infect Immun 81: 4026–4040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Lertpiriyapong K, Gamazon ER, Feng Y, Park DS, Pang J, et al. (2012) Campylobacter jejuni type VI secretion system: roles in adaptation to deoxycholic acid, host cell adherence, invasion, and in vivo colonization. PLoS One 7: e42842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sana TG, Hachani A, Bucior I, Soscia C, Garvis S, et al. (2012) The second type VI secretion system of Pseudomonas aeruginosa strain PAO1 is regulated by quorum sensing and Fur and modulates internalization in epithelial cells. J Biol Chem 287: 27095–27105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Santic M, Asare R, Skrobonja I, Jones S, Abu Kwaik Y (2008) Acquisition of the vacuolar ATPase proton pump and phagosome acidification are essential for escape of Francisella tularensis into the macrophage cytosol. Infect Immun 76: 2671–2677. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Phase and fluorescence micrographs were taken of uninfected and F. novicida infected hepatocytes at 24 h PI. Mouse BNL CL.2 cells were infected with wild-type F. novicida and mutants ΔiglC, ΔiglC::iglC, ΔpdpA and ΔpdpA::pdpA for 22 h. Afterwards, samples were washed, treated with gentamicin for 2 h, and then fixed with 3% paraformaldehyde. Fixed samples were prepared using an immunolocalization technique that can differentiate extracellular (green and red co-localization, arrows) and intracellular bacteria (green only, arrowheads). Each fluorescence image represents a superimposed ‘maximum intensity’ Z-projection image around the cell nucleus (blue). Scale bar = 10 µm.
(TIF)
Bacterial doubling time during the early intracellular stages in hepatocytes.
(DOCX)