Abstract
Falls are a common and serious risk with an aging population. Chiropractors commonly see firsthand the effects of falls and resulting injuries in their senior patients and they can reduce falls risk through active screening. Ongoing research has provided proven approaches for making falls less likely. Screening for falls should be done yearly for all patients 65 years and older or in those with a predisposing medical condition. Additional specific falls prevention professional education would enable the chiropractor to best assist these patients. Collaboration and communication with the patient’s family physician offers an opportunity for improved interprofessional dialogue to enhance patient care related to falls risk. Frequently falls prevention strategies are implemented by an interprofessional team. Chiropractors increasingly contribute within multidisciplinary teams. Collaboration by the chiropractor requires both simple screening and knowledge of health care system navigation. Such awareness can permit optimal participation in the care of their patient and the best outcome.
Keywords: falls, elderly, injury, prevention, chiropractic
Abstract
Les chutes présentent un risque commun et grave chez une population vieillissante. Les chiropraticiens constatent habituellement directement les effets des chutes et les blessures conséquentes chez leurs patients âgés; et ils peuvent en réduire les risques grâce à un dépistage actif. Des recherches continues fournissent des méthodes vérifiées de réduction de la probabilité de chutes. Un dépistage des risques de chute doit être effectué chaque année pour tous les patients de 65 ans et plus, ou pour ceux dont l’état de santé les prédispose. Une formation professionnelle supplémentaire spécifique dans la prévention des chutes permettrait au chiropraticien de mieux aider ces patients. La collaboration et la communication avec le médecin de famille du patient offrent une occasion d’améliorer le dialogue interprofessionnel au profit de meilleurs soins prodigués au patient sur les risques de chute. Souvent les stratégies en matière de prévention des chutes sont mises en place par une équipe interprofessionnelle. Les chiropraticiens œuvrent de plus en plus au sein d’équipes multidisciplinaires. La collaboration des chiropraticiens nécessite des compétences pour de simples dépistages, ainsi que des connaissances pour s’orienter dans le système des soins de santé. De telles connaissances permettront au chiropraticien une participation optimale aux soins de son patient et l’obtention des meilleurs résultats.
Keywords: chutes, personnes âgées, blessures, prévention, chiropratique
Introduction
Falls often have devastating consequences for the elderly.1 Chiropractors commonly see firsthand the effects of falls and resulting injuries in their senior patients. Ongoing research has provided proven approaches for making falls less likely.1 The reduction of falls risk may need to be managed by a referral for a multifactorial fall assessment, through the patient’s family physician.2 Frequently falls prevention strategies are implemented by an interprofessional team. Chiropractors increasingly contribute within multidisciplinary teams.3 Collaboration by the chiropractor requires both simple screening and knowledge of health care system navigation. Such awareness can permit optimal participation in the care of their patient and the best outcome.
“A fall is an unexpected event in which the participant comes to rest on the ground, floor, or lower level”.4 Each year, one in three community living adults aged 65 and older incur a fall.5,6 Falls by seniors are expected to increase in the coming years due to an escalating prevalence of chronic disease.7,8 The cause of falling is multi-factorial.4 In community-based populations, almost half of all falls happen in the home.9 The subsequent effects can lead to distress, disability, fracture, long-term care admission, and mortality.6,9
In 30–73% of those who have fallen, a fear of falling develops which is known as post-fall anxiety syndrome.10 This apprehension can lead to activity restriction, loss of confidence, depression, functional decline, and social isolation.10 Falls represent a significant burden for seniors, their families, and the health care system.11,12 For example, falls are the second most common cause of spinal cord injury and following a fall, a fractured hip has a 1-year mortality rate of over 20% in seniors.13,14 Fortunately, there are community-based methods for chiropractors to help reduce this ever increasing problem.2,6,15
The Centre for Family Medicine Family Health Team in Kitchener, Ontario has developed an interprofessional Mobility Clinic, which provides primary care to patients with physical disabilities. This team includes family physicians, an occupational therapist (OT), nurses, a social worker, a clinical pharmacist, an optometrist, a physiotherapist (PT), and a chiropractor. At the Mobility Clinic, the primary reason for referral is mobility concerns and falls.16 Preventing falls can be challenging because of multifactorial short and long-term causes.17,18 Based on our team’s four years of Mobility Clinic experience and available evidence, we provide an overview of a falls risk assessment, falls prevention measures, and offer steps to tailor our interprofessional approach to a chiropractic office setting. The hope of this paper is to raise awareness among chiropractors to better assist their patients in identifying those at risk of falls and highlight an opportunity to collaborate with other health professionals in limiting this risk.
Screening
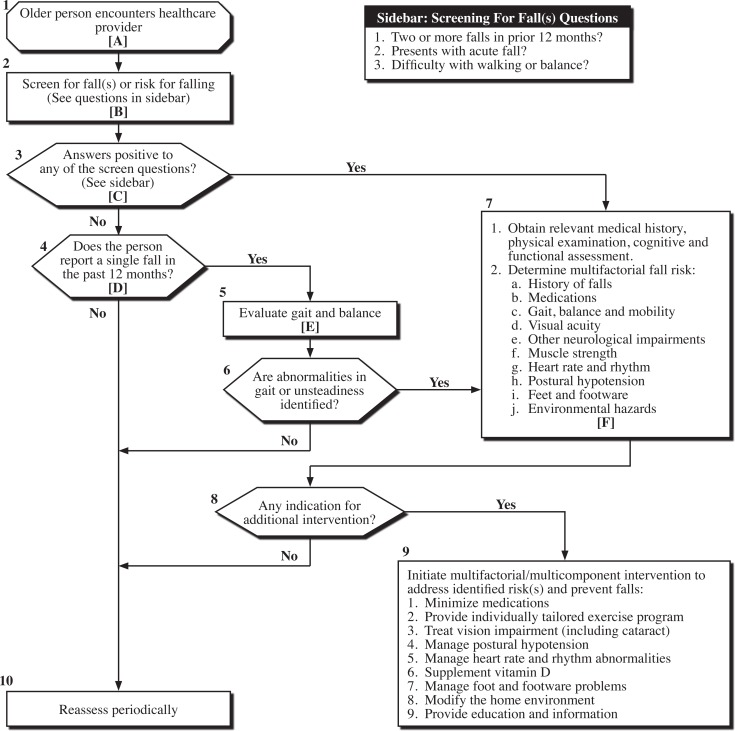
While the topic of falls may come up during a typical patient encounter, screening all chiropractic patients over the age of 65 or those at risk for falling should be done yearly.2,6 Screening can be done by asking if two or more falls have occurred in the last 12 months, in concordance with the American Geriatrics Society, British Geriatrics Society, and NICE clinical practice guidelines.2,6 If there is an affirmation, check their gait and balance (see Physical Examination section) along with frequency and circumstances around the falls.14 Patients positively identified by this screening should be referred to their family physician for consideration of a multifactorial falls risk assessment (figure 1).2,4,6,19,20
Figure 1:
Prevention of Falls in Older Persons Living in the Community
With permission from the American Geriatrics Society: “The AGS/BGS Clinical Practice Guideline: Prevention of Falls in Older Persons” (http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/2010/) from the American Geriatrics Society, www.americangeriatrics.org.
Any patients reporting a single fall should also be evaluated for gait and balance and if significant deficits are detected (see Physical Examination section), they should be referred to their family physician for a multi-factorial fall risk assessment.2,6,19 Some family physicians may not feel they have the expertise to perform a comprehensive falls assessment and may subsequently refer to organizations like the Mobility Clinic or a community-based falls clinic; but these types of resources vary between communities. One might assume that the family physician may be aware of the patient’s falls or risk of falls; however the literature shows that falls are under-reported.21 The chiropractor, as a member of the patient’s health care team, has an important role in identifying an individual’s risk of falls and collaborating with the patient’s family physician to manage it.
History
The following patient questioning is for clinicians who want to have a more detailed history to consider beyond the basic screening information provided above. This would be especially important when access to a multi-factorial falls assessment is not possible. The information gathered will facilitate greater collaboration with other health professionals, and with the patient’s permission, should be brought to the family physician’s attention. This is especially true for the Red and Yellow flags (see Table 1 and Table 2). The 2010 clinical practice guideline of the American Geriatrics Society suggests that if falls have occurred, ask what were the circumstances and frequency?2
Table 1:
Red Flags Requiring Family Physician Notification (with patient permission)
| Additional Symptom Information | |
|---|---|
| • Cardiac symptoms | This includes shortness of breath, chest pain/pressure, and/or palpitations14 A past medical history of heart disease is an independent predictor of cardiac syncope. Absence of cardiac disease excludes cardiac cause24 |
| • Dizziness | If light headed this is possibly caused by reduced blood flow to the brain25 If the entire room sensed as spinning this is possibly caused by benign paroxysmal positional vertigo26 |
| • Turning head brings on symptoms | Possibly vertebrobasilar insufficiency, syncope, or cervicogenic dizziness27,28,29 |
| • Loss of consciousness/seizure | |
| • Amnesia related to circumstances of fall | 30% of patients with witnessed loss of consciousness have amnesia24 |
| • Head injury | |
| • Unreported injuries from past falls | |
| • Substanceabuse | This can increase the risk of falls30,31 Does the patient misuse/abuse alcohol, prescription drugs, and/or use illicit drugs32,33 |
Table 2:
Yellow Flags Requiring Family Physician Notification (with patient permission)
| Additional Symptom Information | |
|---|---|
| • Fear of falling | Ask “Are you are afraid of falling again?” There are validated questionnaires available such as the Activities-specific Balance Confidence Scale and Falls Efficacy Scale to measure this fear34 This fear is a significant contributor to the risk of falls and can result in functional decline, decreased quality of life, and institutionalization6,23 |
| • Dementia | This is an independent risk factor for falls6 Cognitive impairment/dementia can be screened for using the Mini-Cog tool35 |
| • Depression | This is also associated with falls and can be screened for with the PHQ-2 questionnaire36,37 |
| • Sleep disturbance | This includes sleep apnea which can be tested for with a sleep study by the family physician Poor quality sleep is a risk for falls38 |
| • Incontinence | This may cause urgent trips to bathroom, often at night, and lead to a fall6 |
| • Taking 4 or more medications39 |
Falls related questions for patients include those covered by the acronym “SPLAT”:
(S) ymptoms prior to and at the time of the falls2
(P) revious falls, near falls, and/or fear of falling6,22,23
(L) ocation to identify contributing environmental factors (for example, was there poor lighting, was footing poor, did they trip, or were they in a crowd)
(A) ctivity the person was participating in when they fell (for example, were they turning, changing position, or transferring?)
(T) ime of day the falls occurred (for example, falls in the morning could be due to orthostatic hypotension and later in the day could be due to fatigue)
Other falls questions considered at the Mobility Clinic include:
Was the cause unexplained?
Was the fall witnessed?
What kind of shoes was the patient wearing?
This will give you a sense if the fall was a one-time case or a pattern indicating predisposition or an underlying issue.
A systems review should be done to get the patient’s entire medical health history.2 Any number of illnesses can put the patient at greater risk for falls.17 The patient’s current medications and supplements should be recorded.2 There may be a history of previous injuries from one or many falls.2 This may have involved the family physician, ambulance, and hospital emergency room (ER). Determine what injuries were sustained in the fall and their status. Document any other consequences of the falls. Also, be aware that the presence of cognitive impairment may make the patient a poor historian regarding their falls.40
Other questions considered at the Mobility Clinic include:
Is the patient under a specialist’s care for a medical condition?
Does the patient have pain anywhere?
Was there previous rehabilitation/therapy?
What previous imaging was performed?
Has the patient had any fractures and do they have osteoporosis?2
Was the patient able to get up from their fall on their own (this gives a variety of information including if any injuries occurred and possibly whether the patient is deconditioned)?
Does the patient furniture or wall walk (uses furniture and the walls for support when walking in the home as this suggests risk of falls)?
Has the patient ever had hearing difficulty or tinnitus/Meniere’s disease (this could indicate inner ear trouble causing reduced balance)?41,42
When was the patient’s last optometry consult and is their prescription up to date (visual impairment is a falls risk)?6
Do they have cataracts?2
Can the patient feel the ground under their feet when they are standing or walking (this could indicate a peripheral neuropathy, possibly from diabetes)?
Standard chiropractic history taking can gather more information on the presence of pain.43 Pain can cause a fall.44 Possible underlying mechanisms for the pain-falls relationship can be grouped into three categories:
Physical Examination
No gold standard in testing exists for falls risk assessment (Table 3 includes some common tests used at the Mobility Clinic). The chiropractor’s physical exam starts with observing the patient as they walk into the treatment area. Observing the patient’s gait can be extremely informative.45 Increased stride-to-stride variability in stride length, speed, and double-support are independently associated with falling.45 One does not necessarily have to be an expert at gait analysis; but rather be able to identify obvious balance and gait issues (e.g. reaches for furniture/ walls, nearly falls in the office, limps, and/or may use a gait aid). Compare, if safe and possible, between when they do not use and use their walking aid to evaluate the benefit to gait. The Timed Up and Go test is a standardized test for assessing falls risk that may be done in the chiropractor’s office with little equipment or time and may give additional information.46 The patient sits in a chair with armrests and is timed how long it takes them to get up, walk to a line 3 metres away, turn around, walk back, and sit down. They may use their gait, if required, to perform safely. There is one practice trial and then an average of three trials. The literature shows cut-off values distinguishing potential non-fallers and fallers varying from 10 to 32.6 seconds (some suggest 13.5 seconds).47 There is no definitive time for completion and as much of the information may be gained by how the patient performs the test.46
Table 3:
Key Testing To Consider
| Resources (none of the tests are considered the gold standard) | |
|---|---|
| Gait Assessment | Observation48 The University of Utah49 http://library.med.utah.edu/neurologicexam/html/gait_abnormal.html Tinetti test (Performance-Oriented Mobility Assessment)50 |
| Balance Assessment | Tinetti test (Performance-Oriented Mobility Assessment)50 Berg Balance Scale51 |
| Falls Risk Assessment | Timed Up and Go test46 Grip Strength52 Tandem Gait53 |
The following is for practitioners with an interest in a more detailed assessment. The Mobility Clinic has used the University of Utah’s resource for common abnormal gait patterns which can be found at http://library.med.utah.edu/neurologicexam/html/gait_abnormal.html.49 We also use the Tinetti test (Performance-Oriented Mobility Assessment) to determine falls risk and this can be done in 5 minutes with practice.50 The test has a gait component and a balance component. What makes the Tinetti test unique is the inclusion of a perturbation to the patient (a push) to determine how well the patient can react and recover balance. You have to be prepared to catch the patient if they start to fall. The Otago exercise program assessment will help determine which Otago exercises to prescribe.54,55 Others use the Berg Balance Scale.51 Grip strength measures risk of mobility limitation and risk of falls.52,53 Testing tandem gait (heel-to-toe walking) is also useful to assess balance and falls risk.53
Another falls risk the Mobility Clinic tests for is orthostatic hypotension (OH).2 This occurs when blood pressure (BP) is reduced and/or pulse rate changes with the patient going from lying supine to standing and may result in loss of consciousness.56 This OH can be tested with your sphygmomanometer and stethoscope with the patient tested first supine, then standing at one minute, and then three minutes.56 A drop of systolic BP of 20 mmHg, diastolic BP of 10 mmHg, or an increased pulse of 20 beats per minute (bpm) (possibly caused by volume depletion/ dehydration) or reduced pulse of 10 bpm (possibly caused by baroreceptor altered function) is considered significant and should be followed up with the patient’s family physician.56
A history-focused physical examination, aimed at detecting any physical causes of falls, should include the following: spinal alignment, spinal and lower extremity active/passive ranges of motion, thorough neurological exam (myotomes, reflexes, clonus, plantar reflex, and dermatomes for sharp, dull, vibration and tone sensations) and special orthopedic tests.2,48,57 At the Mobility Clinic, we also consider testing the cranial nerves, gross vision, cerebellar testing (Romberg, finger-to-nose, heel-to-shin, and hand flip), proprioception, monofilament, graphesthesia, and stereognosis.2,48,49 The Trendelenburg and side-lying resisted hip abduction tests are quite useful for assessing pelvic stability.48 Checking lower extremity peripheral pulses should also be considered.48
Examination and assessment of the feet is required. Issues with the feet are common in older people and are connected with reduced balance and function.2 Falls are more likely when bunions, deformed nails, ulcers, toe deformities, and other conditions are present.2 Older adults may also have difficulties with foot position awareness.2 Footwear condition and type may put the patient at risk of falls.2 Therefore, footwear needs to be inspected.2
At the Mobility Clinic, the patient’s weight and height are taken to insure a healthy body mass index and proper medication dosing. Waist circumference is used by others to assess health.58 At the Mobility Clinic, the family physician will perform a medical assessment of the patient where indicated by information gathered in the history. They will listen to the chest for any cardiac irregularities, arrhythmia, palpitations, and lung function.2
At the Mobility Clinic, we screen for osteoporosis to determine fragility fracture risk.6, Densitometry testing through the family physician may be performed along with using the CAROC or FRAX tools.59 Spinal compression fractures due to osteoporosis can be screened for using the wall-occiput, rib-pelvis, historical height loss and prospective height loss measures to determine if an osteoporosis protocol x-ray is required of the spine.59–62 Postural changes with osteoporosis, such as thoracic kyphosis, increase the risk of falls.63
Management
Communicating with the patient’s family physician is essential if you have concerns about a patient’s balance or falls risk. For patients without a family physician, community services can be accessed through a walk-in-clinic or the hospital ER. The chiropractor may be helpful in managing some of the physical deficits found during the assessment; most often this may involve treating abnormalities found in the spine and/or lower kinetic chain. The risk of falling increases in proportion to the severity of chronic musculoskeletal pain, the number of joint groups affected, and the amount of interference with daily activities.64 Specific exercises can be given to the patient where deficits in strength, gait, and balance are noted along with safe manual therapy. Be certain there are no cardiac or other risk factors when prescribing an exercise program (to insure safety, communicate with the patient’s family physician if recommending exercise). Postural retraining may also be considered if there are any concerning discoveries.
The following are part of a multifactorial falls intervention:
Specific balance, strengthening, gait, and coordination exercises are recommended by systematic reviews and clinical practice guidelines.2,4,6,19 For example, the Otago exercise program is validated to help prevent falls.54,55,65 For patients with limited mobility not accustomed to exercising, caution is required when starting an exercise program as this may initially increase their risk of falling.2 To improve patient safety with exercises, an individualized exercise program should be prescribed, and regular monitoring and progression of exercises should occur. Other options for improving patient strength and balance include participating in a community-based group exercise programs designed for seniors to reduce the risk of falls.2,66 Tai chi classes or a referral to a physiotherapist for a home exercise regimen are other considerations.4,66 In addition, flexibility and endurance training could be offered; but not as sole components of a program.2 Not only can exercise be part of a multifactorial intervention; but it can also be considered a single intervention as well.2 It is important to note that exercise programs require monitoring by qualified professionals (such as a chiropractor, kinesiologist, physiotherapist, occupational therapist, athletic therapist, or fitness instructor).2
A home falls risk assessment is helpful to prevent falls.6,66 The Canadian Chiropractic Association (“Best Foot Forward” program. http://www.chiropracticcanada.ca/en-us/members/practice-building/Best-Foot-Forward.aspx) has available resources.67 Also, the HOME FAST screening tool has been shown to predict falls in older people and is responsive to change.68,69 Common areas identified in both initiatives include inspecting the patient’s home inside and outside for slipping and tripping hazards and poor lighting.67,68 Grab bars in the bathroom, a shower chair, raised toilet seat, commode, and bed rail are ideally recommended though an occupational therapist (OT) home assessment.66 The OT is trained in home safety, activities of daily living skills assessment, and functional performance. They can address risks and help implement risk reduction strategies through educating the patient.66 This includes teaching the patient how to get up safely from a fall when alone and how to perform safe transfers. In most provinces, an OT working with a home-care agency will provide a home assessment if referred by a physician. Where OT access is not available, the chiropractor or physiotherapist might provide this assistance. Patients should be given advice in how to summon help and how to avoid lying in a position for a prolonged period of time, which can have serious health consequences.6 Personal emergency response systems (such as Life-line™) or a special senior’s Alert 911 device are an option if the patient is at risk for falls and often alone. This can allow a person to call for help if they are unable to get up. The risk for falls may be reduced with issuing a disabled parking pass. This can be authorized by chiropractors and other professionals in the province of Ontario.
Walking aids, such as a cane or wheeled walker, can help prevent falls.66 A simple test to determine if your patient requires a gait aid is to offer your hand for support while they walk.64 If this is of benefit, it may indicate a cane would be helpful.70 If they prefer using two of your hands or a grocery cart while shopping, this may indicate that a wheeled walker would be more suitable.70 A simple sizing guide is to have the top of the handle of the cane or wheeled walker at their wrist crease with arms at their sides, the patient having good posture, and looking straight ahead.70 If they tend to fall backwards, you could reduce the device height a little till they feel more secure. Walking aids improve posture and reduce any secondary musculoskeletal pain. To ensure patients have the appropriate device, a consultation with an OT or PT is recommended. It is important for patients to be properly fit for these aids and be provided with education about how to safely use the device. Improper use can lead to a fall. An OT or PT can also facilitate funding through government sources. (e.g. in Ontario, the Assistive Devices Program (ADP) may cover up to 75% of the cost of a walker).
The family physician will order any special testing required to optimally medically manage the patient. This would include lab work, diagnostic testing, and imaging. Before any test is ordered, consideration as to whether the results would change treatment should occur. Medical management, possibly involving specialist referral, would be discussed with the patient. If present, heart rate and rhythm abnormalities and orthostatic hypotension treatment may be recommended.2 In some cases, heart conditions require cardiac surgery and/or dual-chamber cardiac pacing (in the case of cardioinhibitory carotid sinus hypersensitivity).2,6,66
Many studies have shown that a medication and supplement review by a clinical pharmacist can be effective in reducing falls risk. Comorbidities increase the pill burden resulting adverse drug events, and drug interactions, which may further increase the risk of falls. Furthermore, changes in renal function, liver function, body mass, and adipose result in changes in the pharmacokinetic parameters of medications, which in turn, affect the pharmacological effect of medications. Taking 4 or more prescription medications increases the risk of falls.39 Finally, medications or classes of medications are known to increase the risk of falls in the elderly.66,71 Agents most frequently associated with increasing the risk of falls include antihypertensive and cardiovascular agents, diuretics, beta-blockers, psychotropics, antidepressants, benzodiazepines, antipsychotics, sedative/hypnotics, hypoglycemics, opioids, and non-steroidal anti-inflammatory drugs (NSAIDs).71
Sudden discontinuation of any of the medications listed is not prudent without a thorough review, and patients taking any of the listed medications should be referred to either their physician or pharmacist so that appropriate reduction in dose, slow discontinuation, or replacement with safer alternative agents may be attempted. In Ontario, if a patient is on three or more medications they can have a medication review with their pharmacist paid for by government health insurance (OHIP). Unless indicated otherwise by their physician, total dietary intake of elemental calcium from all sources (diet and/or supplementation) for patients age 50 years and over should be 1200 mg/day to reduce osteoporosis fragility fracture risk.6,59 In addition to the above advised calcium, supplementation of 800–2000 iu/day of vitamin D for patients age 50 years and older is recommended for optimum bone health.59,72 New research shows that such vitamin D intake doesn’t prevent falls, as was previously thought.73
A full oculo-visual assessment and intervention may be required.2,6 An eye exam is recommended when a patient reports that they have not had one recently (within a year) or if any reduction in visual function is described. An older patient is advised not to wear multifocal lens while walking, especially on stairs.2 Single-lens distance-vision glasses are suggested for outdoor use in multifocal-lens users who participate in regular outdoor activities.74 In addition, cataract surgery has been shown to be effective for reducing falls.2
Problems noted with the feet should be referred to an appropriate professional, such as a chiropodist, for treatment.2 Footwear should be laced or buckled, have a low heel, a non-slip high surface contact area sole, and be inspected for wear.2 Closed heel footwear that fits properly should be considered. Anti-slip footwear devices worn in slippery conditions were noted to reduced outside falls.70,75 Custom foot orthotics, if indicated by the examination, may be prescribed.70
Educational and information programs should be contemplated for community-based patients.2,6 Topics discussed include falls prevention and where to get further assistance and advice.6 Regional health units or community agencies may have such evidenced-informed programs.
Conclusion
With the increase in physical, emotional and economic costs associated in the aging population, it is important that chiropractors are aware of and evaluate for falls risks. This overview intended to offer clinicians a greater appreciation of the prevalence, complexity, and importance of fall prevention in the community. Chiropractors are well positioned to fill healthcare gaps in this area. Knowledge on falls prevention has the potential to improve the quality of life for patients and may also be a source of improved professional satisfaction.
Key Points
Falls are a common and serious risk with an aging population.
Chiropractors can reduce falls risk through active screening.
Screening for falls should be done yearly for all patients 65 years and older or in those with a pre-disposing medical condition.
Additional specific falls prevention professional education would enable the chiropractor to better assist these patients.
Collaboration and communication with the patient’s family physician offers an opportunity for improved interprofessional dialogue and enhanced patient care related to falls risk.
Footnotes
Funding: No funds were received for the preparation of this manuscript. The Centre for Family Medicine Mobility Clinic receives funding from the Ontario Neurotrauma Foundation. Dr. Bauman and Dr. Riva are members of the McMaster Chiropractic Working Group, which receives in-kind support from the Canadian Chiropractic Association.
Competing Interests: None
References
- 1.Al-Faisal W. World health organization global report on falls prevention in older age. 2007. http://www.who.int/ageing/publications/Falls_prevention7March.pdf.
- 2.Developed by the panel on prevention of falls in older persons, American geriatrics society and British geriatrics society summary of the updated American geriatrics society/British geriatrics society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2010 doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 3.Kopansky-Giles D. Inclusion of a CAM therapy (chiropractic care) for the management of musculoskeletal pain in an integrative, inner city, hospital-based primary care setting. J Alternative Med Res. 2010;2:61–74. [Google Scholar]
- 4.Michael Y. Evidence synthesis number 80. Interventions to prevent falls in older adults: An updated systematic review. Oregon evidence-based practice center. 2010 Dec; AHRQ publication no. 11-05150-EF-1. [PubMed] [Google Scholar]
- 5.Centers for disease control and prevention Falls among older adults: An overview. http://www.cdc.gov/homeandrecreationalsafety/falls/adultfalls.html. Updated September 20, 2012. Viewed April 2014.
- 6.Falls: assessment and prevention of falls in older people. Jun, 2013. National institute for health and care excellence. Issued. [DOI] [PubMed] [Google Scholar]
- 7.Campbell A. Examination by logistic regression modeling the variables which increase the relative risk of elderly women falling compared to elderly men. J Clin Epidemiol. 1990;43:1415–20. doi: 10.1016/0895-4356(90)90110-b. [DOI] [PubMed] [Google Scholar]
- 8.Rubenstein L. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18:141–58. doi: 10.1016/s0749-0690(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 9.Nikolaus T. Preventing falls in community-dwelling frail older people using a home intervention team (HIT): results from the randomized falls-HIT trial. J Am Geriatr Soc. 2003;51:300–5. doi: 10.1046/j.1532-5415.2003.51102.x. [DOI] [PubMed] [Google Scholar]
- 10.Rubenstein L. Falls and their prevention in elderly people: what does the evidence show? Med Clin N Am. 2006;90:807–24. doi: 10.1016/j.mcna.2006.05.013. [DOI] [PubMed] [Google Scholar]
- 11.Division of aging and seniors, public health agency of Canada. 2005. Report on seniors’ falls in Canada. Minister of public works and government services Canada. www.phac-aspc.gc.ca/seniors-aines/pubs/seniors_falls/index.
- 12.Sattin R. Falls among older persons: A public health perspective. Annu Rev Public Health. 1992;13:489–508. doi: 10.1146/annurev.pu.13.050192.002421. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy P. Spinal cord injuries as a consequence of falls: are there differential rehabilitation outcomes? Spinal Cord. 2013;51:209–13. doi: 10.1038/sc.2012.124. [DOI] [PubMed] [Google Scholar]
- 14.Leslie W. Trends in hip fracture rates in Canada. JAMA. 2009;302:883–9. doi: 10.1001/jama.2009.1231. [DOI] [PubMed] [Google Scholar]
- 15.Gleberzon B. A narrative review of the published chiropractic literature regarding older patients from 2001–2010. J Can Chiropr Assoc. 2011;55:76–95. [PMC free article] [PubMed] [Google Scholar]
- 16.Hillier L. 2011 Dec 20; Centre for family medicine family health team mobility clinic evaluation report. [Google Scholar]
- 17.Al-Aama T. Falls in the elderly. Spectrum and prevention. Can Fam Physician. 2011;57:771–6. [PMC free article] [PubMed] [Google Scholar]
- 18.Bueno-Cavanillas A. Risk factors in falls among the elderly according to extrinsic and intrinsic precipitating causes. Eur J Epidem. 2000;16:849–59. doi: 10.1023/a:1007636531965. [DOI] [PubMed] [Google Scholar]
- 19.Michael Y. Primary care- Relevant interventions to prevent falling in older adults: A systematic evidence review for the U.S. preventive services task force. Ann Intern Med. 2010;153:815–25. doi: 10.7326/0003-4819-153-12-201012210-00008. [DOI] [PubMed] [Google Scholar]
- 20.Muir S. Application of a fall screening algorithm stratified fall risk but missed preventive opportunities in community-dwelling older adults: A prospective study. J Geriatr Phys Ther. 2010;33:165–72. [PubMed] [Google Scholar]
- 21.Ungar A. Fall prevention in the elderly. Clinical Cases in Mineral and Bone Metabolism. 2013;10:91–5. [PMC free article] [PubMed] [Google Scholar]
- 22.Steinberg M. A sustainable programme to prevent falls and near falls in community dwelling older people: results of a randomised trial. J Epidemiol Community Health. 2000;54:227–32. doi: 10.1136/jech.54.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Friedman S. Falls and fear of falling: which comes first? A longitudinal prediction model suggests strategies for primary and secondary prevention. J Am Geriatric Soc. 2002;50:1329–35. doi: 10.1046/j.1532-5415.2002.50352.x. [DOI] [PubMed] [Google Scholar]
- 24.Tan M. Cardiovascular assessment of falls in older people. Clin Interv Aging. 2006;1:57–66. doi: 10.2147/ciia.2006.1.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bresseleers J. Feeling lightheaded: the role of cerebral blood flow. Psychosom Med. 2010;72:672–80. doi: 10.1097/PSY.0b013e3181e68e94. [DOI] [PubMed] [Google Scholar]
- 26.Parnes L. Diagnosis and management of benign paroxysmal positional vertigo (BPPV) CMAJ. 2003;169:681–93. [PMC free article] [PubMed] [Google Scholar]
- 27.Fox M. Anterolateral decompression of the atlantoaxial vertebral artery for positional occlusion of the vertebral artery: case report. J Neurosurg. 1995;83:737–40. doi: 10.3171/jns.1995.83.4.0737. [DOI] [PubMed] [Google Scholar]
- 28.Kapoor W. Clinical methods: The history, physical, and laboratory examinations. 3rd ed. Boston, MA: Butterworths; 1990. Chapter 12, Syncope. http://www.ncbi.nlm.nih.gov/books/NBK224/. Viewed April 2014. [PubMed] [Google Scholar]
- 29.Lystad R. Manual therapy with and without vestibular rehabilitation for cervicogenic dizziness: a systematic review. Chiropr Man Therap. 2011;19:21. doi: 10.1186/2045-709X-19-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mukamal K. Self-reported alcohol consumption and falls in older adults: cross-sectional and longitudinal analyses of the cardiovascular health study. J Am Geriatr Soc. 2004;52:1174–9. doi: 10.1111/j.1532-5415.2004.52318.x. [DOI] [PubMed] [Google Scholar]
- 31.National Institutes of Health Prescription and illicit drug abuse is timely new topic on nihseniorhealth.gov. Information on worrisome trend among older adults; tips on prevention, treatment. http://www.nih.gov/news/health/jun2012/nia-06.htm. Updated June 6, 2012. Viewed April 2014.
- 32.Nihseniorhealth Prescription and illicit Drug. Jun, 2012. http://nihseniorhealth.gov/drugabuse/improperuse/01.html. Updated June 2012. Viewed April 2014.
- 33.Taylor M. The growing problem of illicit substance abuse in the elderly: a review. Prim Care Companion CNS Disord. 2012;14(4) doi: 10.4088/PCC.11r01320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Powell L. The activities-specific balance confidence (ABC) scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 35.Borson S. The mini-cog as a screen for dementia: Validation in a population-based sample. J Am Geriatr Soc. 2003;51:1451–4. doi: 10.1046/j.1532-5415.2003.51465.x. [DOI] [PubMed] [Google Scholar]
- 36.Kvelde T. Depressive symptomatology as a risk factor for falls in older people: systematic review and meta-analysis. J Am Geriatr Soc. 2013;61:694–706. doi: 10.1111/jgs.12209. [DOI] [PubMed] [Google Scholar]
- 37.Li C. Validity of the patient health questionnaire 2 (PHQ-2) in identifying major depression in older people. J Am Geriatr Soc. 2007;55:596–602. doi: 10.1111/j.1532-5415.2007.01103.x. [DOI] [PubMed] [Google Scholar]
- 38.Onen F. Falling-asleep-related injured falls in the elderly. J Am Med Dir Assoc. 2009;10:207–10. doi: 10.1016/j.jamda.2008.10.008. [DOI] [PubMed] [Google Scholar]
- 39.Tinetti M. Preventing falls in the elderly. N Engl J Med. 2003;348:42–9. doi: 10.1056/NEJMcp020719. [DOI] [PubMed] [Google Scholar]
- 40.Zieschang T. Feasibility and accuracy of fall reports in persons with dementia: a prospective observational study. Int Psychogeriatr. 2012;24:587–98. doi: 10.1017/S1041610211002122. [DOI] [PubMed] [Google Scholar]
- 41.Viljanen A. Hearing as a predictor of falls and postural balance in older female twins. J Gerontol A Biol Sci Med Sci. 2009;64A:312–7. doi: 10.1093/gerona/gln015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.U.S. department of health and human services National institutes of health. National institute on deafness and other communication disorders (NIDCD). Ménière’s disease. http://www.nidcd.nih.gov/health/balance/pages/meniere.aspx. Updated July 2010. Viewed April 2014.
- 43.US department of health & human services Agency for health care research and quality. National guideline clearinghouse. Manual medicine guidelines for musculoskeletal injuries. Recommendations. Major recommendations. History. http://www.guideline.gov/content.aspx?id=15135#Section420. Updated March 2010. Viewed April 2014.
- 44.Leveille S. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302:2214–21. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Maki B. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45:313–20. doi: 10.1111/j.1532-5415.1997.tb00946.x. [DOI] [PubMed] [Google Scholar]
- 46.Schoene D. Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatric Soc. 2013;61:202–8. doi: 10.1111/jgs.12106. [DOI] [PubMed] [Google Scholar]
- 47.Beauchet O. Timed up and go test and risk of falls in older adults: a systematic review. J Nutr Health Aging. 2011 Dec;15:933–8. doi: 10.1007/s12603-011-0062-0. [DOI] [PubMed] [Google Scholar]
- 48.Magee D. Orthopedic physical assessment. 5th ed. St Louis, MO: Saunders Elsevier; 2008. [Google Scholar]
- 49.The University of Utah http://library.med.utah.edu/neurologicexam/html/gait_abnormal.html. Updated September 2013. Viewed April 2014.
- 50.Faber M. Clinimetric properties of the performance-oriented mobility assessment. Phys Ther. 2006;86:944–54. [PubMed] [Google Scholar]
- 51.Berg K. Measuring balance in the elderly: validation of an instrument. Can J Public Health. 1992;83(Suppl 2):S7–11. [PubMed] [Google Scholar]
- 52.Sallinen J. Hand-grip strength cut points to screen older persons at risk for mobility limitation. J Am Geriatric Soc. 2010;58:1721–6. doi: 10.1111/j.1532-5415.2010.03035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kikuchi R. Evaluation of risk of falls in patients at a memory impairment outpatient clinic. Geriatr Gerontol Int. 2009;9:298–393. doi: 10.1111/j.1447-0594.2009.00539.x. [DOI] [PubMed] [Google Scholar]
- 54.Thomas S. Does the ‘Otago exercise programme’ reduce mortality and falls in older adults?: A systematic review and meta-analysis. Age Aging. 2010;39:681–7. doi: 10.1093/ageing/afq102. [DOI] [PubMed] [Google Scholar]
- 55.Stevens J. A compendium of effective fall interventions: What works for community-dwelling older adults. 2nd edition. Centres for Disease Control and Prevention; Atlanta, Georgia: 2010. [Google Scholar]
- 56.Sclater A. Orthostatic hypotension. A primary care primer for assessment and treatment. Geriatrics. 2004;59:22–6. [PubMed] [Google Scholar]
- 57.Canadian Chiropractic Protective Association. Risk management project. 2012 [Google Scholar]
- 58.Janssen I. Waist circumference and not body mass index explains obesity related health risk. Am J Clin Nutr. 2004;79:379–84. doi: 10.1093/ajcn/79.3.379. [DOI] [PubMed] [Google Scholar]
- 59.Papaioannou A. Osteoporosis Canada guidelines Clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. 2010. Background and technical report. http://www.cmaj.ca/content/early/2010/10/12/cmaj.100771.full.pdf+html?ijkey=edc6c6048e7d4acdc41368fe3f1e622bf5a2deac&keytype2=tf_ipsecsha.
- 60.Siminoski K. The accuracy of historical height loss for the detection of vertebral fracture in postmenopausal women. Osteoporos Int. 2006;17:290. doi: 10.1007/s00198-005-2017-y. [DOI] [PubMed] [Google Scholar]
- 61.Siminoski K. Accuracy of height loss during prospective monitoring for detection of incident vertebral fractures. Osteoporos Int. 2005;16:403–10. doi: 10.1007/s00198-004-1709-z. [DOI] [PubMed] [Google Scholar]
- 62.Green A. Does this woman have osteoporosis? JAMA. 2004;292:2890–900. doi: 10.1001/jama.292.23.2890. [DOI] [PubMed] [Google Scholar]
- 63.Sinaki M. Balance disorder and increased risk of falls in osteoporosis and kyphosis: Significance of kyphotic posture and muscle strength. Osteoporos Int. 2005;16:1004–10. doi: 10.1007/s00198-004-1791-2. [DOI] [PubMed] [Google Scholar]
- 64.Leveille S. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302:2214–21. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Otago exercise programme to prevent falls in older adults. Mar, 2003. http://www.acc.co.nz/PRD_EXT_CSMP/groups/external_providers/documents/publications_promotion/prd_ctrb118334.pdf.
- 66.Gillespie L. Interventions for preventing falls in older people living in the community (review) doi: 10.1002/14651858.CD007146.pub3. The Cochrane Library 2012, Issue 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.The Canadian Chiropractic Association “Best Foot Forward” program. http://www.chiropracticcanada.ca/enus/members/practice-building/Best-Foot-Forward.aspx. Updated 2013. Viewed April 2014.
- 68.The home falls and accidents screening tool (HOME FAST) http://www.health.vic.gov.au/agedcare/maintaining/falls_dev/downloads/B1C1%20Home%20Falls%20and%20Accidents%20Screening%20Tool%20(Home%20Fast).pdf. Updated 2009. Viewed April 2014.
- 69.Mackenzie L. Longitudinal study of the home falls and accidents screening tool in identifying older people at increased risk of falls. Australas J Ageing. 2009;28:64–9. doi: 10.1111/j.1741-6612.2009.00361.x. [DOI] [PubMed] [Google Scholar]
- 70.Lam R. Choosing the correct walking aid for patients. Can Fam Phys. 2007;53:2115–6. [PMC free article] [PubMed] [Google Scholar]
- 71.Huang A. Medication-related falls in the elderly: Causative factors and preventive strategies. Drugs Aging. 2012;29:359–76. doi: 10.2165/11599460-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 72.Avenell A. Vitamin D and vitamin D analogues for preventing fractures in post-menopausal women and older men (review) The Cochrane Library. 2014 doi: 10.1002/14651858.CD000227.pub4. Issue 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Theodoratou E. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomized trials. BMJ. 2014;348:g2035. doi: 10.1136/bmj.g2035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Haran M. Effect on falls of providing single lens distance vision glasses to multifocal glasses wearers: VISIBLE randomised controlled trial. BMJ. 2010;340:c2456. doi: 10.1136/bmj.c2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.McKiernan F. A simple gait-stabilizing device reduces outdoor falls and nonserious injurious falls in fall-prone older people during the winter. J Am Geriatr Soc. 2005;53:943–7. doi: 10.1111/j.1532-5415.2005.53302.x. [DOI] [PubMed] [Google Scholar]