Abstract
Host immunity is a major driver of pathogen evolution and thus a major determinant of pathogen diversity. Explanations for pathogen diversity traditionally assume simple interactions between pathogens and the immune system, a view encapsulated by the susceptible–infected–recovered (SIR) model. However, there is growing evidence that the complexity of many host–pathogen interactions is dynamically important. This revised perspective requires broadening the definition of a pathogen's immunological phenotype, or what can be thought of as its immunological niche. After reviewing evidence that interactions between pathogens and host immunity drive much of pathogen evolution, I introduce the concept of a pathogen's immunological phenotype. Models that depart from the SIR paradigm demonstrate the utility of this perspective and show that it is particularly useful in understanding vaccine-induced evolution. This paper highlights questions in immunology, evolution, and ecology that must be answered to advance theories of pathogen diversity.
Keywords: infectious diseases, host–pathogen interactions, phylodynamics, evolutionary epidemiology, niche theory, viruses, bacteria, influenza
Introduction
Pathogens comprise an extraordinarily diverse and rapidly evolving community of organisms, including viruses of several thousand base pairs to trypanosomes of 104 genes. Pathogens’ large population sizes, relatively fast generation times, and cosmopolitan methods of varying their genomes make them opportune study populations in which to test ecological and evolutionary models.1–4
Since an organism's fitness is defined by its environment and a pathogen's environment is usually its host, it stands to reason that pathogen fitness—and hence pathogen evolution—is best understood in the context of interactions with the host. These interactions include pathogen exploitation of the host as a resource for replication and transmission, as well as antagonism between the host and pathogen via the host's immune system.
In this article, I argue that these immune-mediated interactions are a major force shaping pathogen evolution, although there is much about them that is not understood. To bridge the gap between immunological observations and models of pathogen evolution, I introduce the concept of the pathogen's immunological phenotype. Expanding classic models of pathogen competition to include more realistic aspects of host–pathogen interactions, such as the simultaneous influence of specific and nonspecific responses of different strengths and durations, increases the breadth of phenomena that can be explained and demonstrates the importance of these interactions for anticipating the evolutionary impacts of vaccines. I argue that progress in this field awaits both empirical and theoretical advances.
Host immunity shapes pathogen evolution
The diversity of pathogens reflects strong and enduring selection to escape host immunity. Escape takes several basic forms. For example, many pathogens have evolved strategies to limit immune detection or to manipulate the immune response to their advantage; selection for these traits is generally purifying. A related approach is variation in appearance to avoid recognition by adaptive immunity; positive selection of this form can sometimes be observed over short timescales. These forms of escape partially explain the different patterns of evolution among pathogens, although a challenge is to identify where phenotypic change may be limited by functional constraints.
Avoidance and suppression
The immune system mounts a multifaceted attack on infectious agents (Box 1). Predictably, pathogens have developed ways to reduce detection by some forms of immunity. Suppression of the immune response is also common. These strategies are usually described as fixed traits of the pathogen, implying that they are strongly conserved.
Box 1. A primer on host defense
Immune systems have evolved, at great cost, partly to attenuate the impacts of pathogens on host fitness.142,143 In vertebrates, they accomplish this goal by reducing the growth rates of pathogen populations through innate and adaptive mechanisms.57 This description focuses on human immunity, although analogues exist to the prokaryotic level.144
Innate immunity includes the activities of the complement system, phagocytes, and natural killer cells. The complement system marks and eliminates pathogens by recognizing surface carbohydrates. Neutrophils, dendritic cells, and macrophages kill bacteria through phagocytosis. Natural killer cells that have been activated by cytokines destroy cells that have been recognized as infected by their low levels of MHC class I expression.
Adaptive immunity consists of two arms: cell-mediated and humoral. Cell-mediated immunity is marked by the proapoptotic activities of CD8+ T cells and other cells that promote the destruction of intracellular pathogens. CD8+ T cells detect peptides presented by MHC class I molecules on cell surfaces. Antibodies, which are generated by the B cells of humoral immunity, enhance the activities of other immune cells and can neutralize extracellular pathogens directly. The antigenic phenotype of a pathogen is defined by interactions with adaptive immune responses, and the sites of interactions with T cells and antibodies are known as epitopes.
There is extensive communication and interaction between the different branches of the immune system, such that many cell types and factors affect both the innate and adaptive components.57 Direct interactions between components of the immune system and pathogens may be neutral to antagonistic,145,146 but some pathogens, like HIV and Epstein–Barr virus, directly benefit from the proliferation of certain immune cells.147–150
Mechanisms to evade the immune system are diverse.5 For example, Streptococcus pneumoniae, Klebsiella pneumoniae, and other bacteria possess polysaccharide capsules that reduce susceptibility to phagocytosis.6–8 Staphylococcus aureus and Treponema pallidum use surface proteins to aggregate host antigens on their surface.9,10 Many pathogens replicate in ways that minimize interaction with the immune system.11 Influenza quickly infects and replicates in respiratory epithelial cells, limiting the window of exposure to CD8+ T cells and antibodies.12 In contrast, after infecting keratinocytes, human papillomaviruses have exceedingly low expression levels and thus avoid detection until they begin replicating inside cells that are about to be shed.13,14 Replication of HIV in macrophages requires several proteins to mask its activities.15
Avoidance is frequently accompanied by suppression. Influenza infection depends critically on viral suppression of type I interferon, a trait conferred by influenza's nonstructural protein 1.16,17 Streptococcus pyogenes and S. aureus secrete compounds that inhibit neutrophil chemotaxis.18 More invasive forms of manipulation occur in chronic viral infections.19 Cytomegalovirus produces a mimic of interleukin (IL)-10, an immunosuppressive host cytokine that inhibits the production of other cytokines and expression of major histocompatibility complex (MHC) class I and II molecules.20
There has been relatively little investigation of the evolutionary dynamics of evasion to nonspecific components of host immunity. Numerous studies have shown that the removal of avoidance-associated genes is lethal,17,21,22 which is consistent with the idea that these traits are under purifying selection. But it is interesting to speculate that the costs of evasion, such as the potential induction of autoimmunity,23 might create directional selection or balanced polymorphism in complex immunological environments.
Changing appearance
Many pathogens avoid specific immune memory by varying their appearance to the adaptive immune system. These pathogens show an array of patterns of positive diversifying selection at epitopes targeted by antibodies and CD8+ and CD4+ T cells (Table 1).
Table 1.
Several pathogens infecting humans, for which positive selection on immune phenotype has been demonstrated
| Pathogen | Variable target | Induced response | Sample references |
|---|---|---|---|
| Viruses | |||
| Influenza | Surface proteins hemagglutinin and neuraminidase | Antibodies, CD8+ T cells, CD4+ T cells | Refs. 44, 157, and 158 |
| Hepatitis C | NS3 and NS5A regions | CD8+ T cells | Ref. 42 |
| Norovirus | Surface proteins | Antibodies | Ref. 33 |
| HIV | Gag protein gp120 | CD8+ T cells, antibodies | Refs. 35, 40, and 159 |
| Rhinovirus | Surface proteins | Antibodies | Ref. 160 |
| Rotavirus | Surface proteins VP3 and VP7 | Antibodies | Ref. 161 |
| Bacteria | |||
| Streptococcus pneumoniae | Polysaccharide capsule, subcapsular protein antigens | Antibodies, CD4+ T cells | Refs. 32 and 85 |
| Neisseria meningitidis | PiLE pilus protein | Antibodies | Refs. 162 |
| Protozoa | |||
| Plasmodium falciparum | PfEMP1 | Antibodies | Ref. 48 |
| Trypanosoma spp. | Surface glycoprotein VSG | Antibodies | Ref. 163 |
This variation can exhibit complex spatiotemporal patterns.8 Influenza viruses infecting humans display two general patterns of antigenic diversity.24 The dominant surface protein hemagglutinin undergoes rapid turnover in all major lineages: type A (subtype H3N2), A (H1N1), and both lineages of B (B/Victoria and B/Yamagata).24,25 For each major lineage, the most recent common ancestor arose less than 10 years before the present, and often much more recently.24,26 This turnover is driven by point mutations and the addition of N-linked glycosylation sites, which confer escape from prevailing antibodies.27–30 These lineages stably coexist at the global level despite competing for hosts, although influenza A subtypes occasionally drive each other extinct. Other pathogens, including Neisseria meningitidis,31 S. pneumoniae,32 noroviruses,33 HIV,34,35 enteroviruses,36 Plasmodium,37 and trypanosomes,38 demonstrate positive selection in sites targeted by antibodies.
Positive selection to escape specific T cell memory occurs conspicuously in fast-mutating pathogens that establish persistent infections, and it may also influence the evolution of acutely infecting pathogens. Rapid adaptation to host MHC alleles occurs in the early stages of infections with HIV39,40 and hepatitis C virus (HCV), although strains adapted to heterologous alleles can be found when transmission occurs rapidly, relative to the timescale of infection.41 In a chimpanzee model of HCV infection, increases in viremia correlated with the appearance of amino acid mutations conferring CD4+ T cell escape.42 Influenza A (H3N2) may also experience positive selection for escape from CD8+ T cell epitopes.43,44
Weak selection and functional constraints
Since host immunity has such a large impact on host fitness, it is puzzling that antigenic variation isn't more common. Pathogens’ strategies to evade immunity suggest two explanations. The first hypothesis is that adaptive immunity has a relatively small impact on pathogen fitness. Mycobacterium tuberculosis, which causes tuberculosis, is a widespread intracellular bacterial pathogen that partially escapes adaptive immune responses to establish dormant infections.45 It appears to undergo mostly strong purifying selection, with the few selective sweeps not clearly related to immune escape.46 Similarly, the ability of herpesviruses to establish latent infections, inhibit MHC presentation, and move directly between cells could reduce selective pressure to escape from antibodies and CD8+ T cells. In these cases, escape from specific immune memory may not affect fitness or, if immune pressure is weak, escape phenotypes may be slow to evolve.
The second hypothesis is that functional constraints limit antigenic diversity. Exposed elements of the pathogen capsules are not only potential antibody targets but are also usually involved in host cell receptor tropism or other traits.47 For example, the multigene var family of Plasmodium falciparum encodes the surface protein PfEMP1, which induces immunodominant antibody responses and mediates cytoadherence, a major factor in pathogen survival and virulence.37 This sequential expression of diverse surface antigens might result from the interplay of selection to avoid immunity and the need to transmit to partially immune hosts.48 Another pathogen that appears not to demonstrate variation in immune-escape phenotype is measles. The lack of variation is surprising considering that as an RNA virus, measles has a relatively high mutation rate, and it is also easily transmitted among unvaccinated hosts.1 The basis of its lack of antigenic variability is poorly understood. A few epitopes could be immunodominant and evolutionarily constrained, or the immune response may be so polyclonal that simultaneous escape mutations at all epitopes is unlikely.49
Pathogens may eventually evolve to escape these functional tradeoffs. For example, the regions of the influenza hemagglutinin that are under strong positive selection in humans tend to be near the receptor binding site, which enables viral entry into the host cell. Many mutations in this area interfere with binding or with the complementary function of the neuraminidase protein.50 Influenza may have developed ways to mitigate these costs: the receptor binding site is recessed in hemagglutinin, and an offset protruding loop or hypothesized decoy epitopes could induce immunodominant responses that are less apt to be neutralizing.51 Phylogenetic analysis suggests that even the oldest proteins have not yet fully explored genotype space.52 Since protein fitness landscapes appear rugged,53 current truisms (e.g., that measles is antigenically trapped, that a vaccine-induced antibody neutralizes circulating viruses) may not be robust. Hard-to-predict epistatic interactions should not of course be limited to influenza. They can be expected to shape the antigenic evolution of other pathogens.54,55
Interactions define a pathogen's immunological phenotype
The ways in which pathogens interact with host immune systems and in which immunity shapes pathogen evolution through purifying and positive selection are undoubtedly complex and incompletely understood. The concept of the pathogen's immunological phenotype can help bridge the gap between the complexity of these interactions and theoretical models of pathogen evolution.
The immunophenotype
A pathogen's immunological phenotype, or immunophenotype, is a dimensional reduction of the pathogen's interactions with different parts of the immune response. These parts differ primarily in the strength of their impacts on pathogen fitness. The lipopolysaccharides of Gram-negative bacteria, for example, directly activate macrophages and other innate immune responses but are not well neutralized by antibodies.56 Viruses, which must replicate inside cells, tend to be suppressed by a combination of CD8+ T cell–induced cell suicide and antibody-mediated neutralization.57 The strength of each interaction quantifies its impact on pathogen fitness, which can be defined by the pathogen's within-host growth rate or the infected host's ability to infect another host.
With strength, the duration and breadth of interactions define the immunophenotype. The duration of the pathogen's impact on host immunity ranges from relatively short surges of innate cytokines that last for hours to days58,59 to the establishment and reactivation of memory B cells, which may persist for the lifetime of the host.60 The breadth captures the extent to which each form of immunity is shared with other pathogens. As described later, this trait may be defined in different ways.61
As a low-dimensional approximation, a pathogen's immunophenotype can be imagined to occupy some region in a space defined by the strength, duration, and breadth of its interaction with the immune system (Fig. 1A). These interactions describe the pathogen's role in the community of immune factors and other pathogens, and hence the immunophenotype encompasses several of the definitions of the concept of the ecological niche.62 Following mathematical niche theory,63–65 the immunophenotype P of a pathogen p in host H in a pathogen community C can be formalized as:
| (1) |
with the arguments of F corresponding to the strength, duration, and breadth of interactions, respectively. The host H is a vector defined by the abundances of h immune components, which may be individual cytokines or aggregated responses, such as polyclonal antibodies; H ∈ {n1, n2, …, nh}. Each element in H can affect the growth of the pathogen and, in turn, be affected by the pathogen. These relationships are given by the impact and sensitivity functions,65 which together define the population regulation variable R. Variable R describes the dependence of growth rates of the pathogen and members of H on their population sizes, or the strength of host–pathogen interactions. The duration of these impacts is defined by function D(R). This function could be a simple cutoff, such as the time for cytokine populations to decline from their maximum values in the presence of the pathogen to their values at pathogen-free equilibrium. The breadth of the response, B(C), is analogous to the population regulation variable R of the pathogen p, except the community matrix C includes p as well as all other pathogens in the system. It can also be decomposed into impact and sensitivity vectors, which measure the impact of each pathogen on host immunity and thereby each other.
Figure 1.
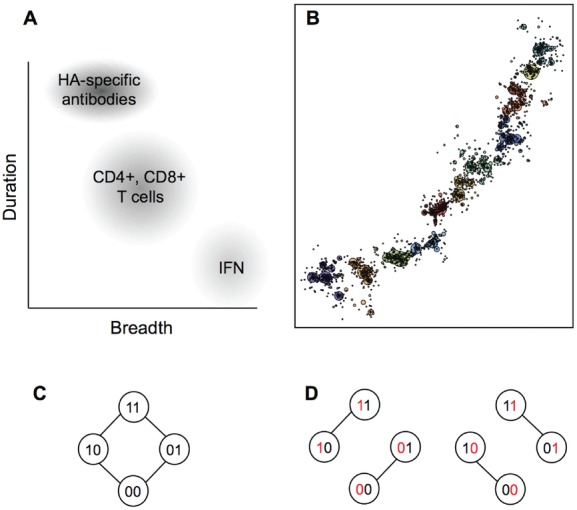
Four views of a pathogen's immune phenotype. (A) The approximate strength, duration, and breadth of influenza virus's interactions with three major components of host immunity. The strength of the response, measured by its impact on fitness, is illustrated by the darkness of the shading. (B) The antigenic evolution of a simulated influenza virus population, collapsed into two arbitrary antigenic dimensions (principal components), from Ref. 100. (C) Network of shared epitopes of a population of four pathogen strains, each with two potential alleles at each of two loci. No population substructure is apparent. (D) Networks of realized relationships for two individual hosts. One host has developed immunity or is restricted (e.g., by MHC) to developing immunity to the first locus, and the other host to the second locus. Each host views a structured population of two phenotypes, but these population structures vary between hosts.
Representations of competitive interactions
The breadth of each response is a window into the pathogen's competitive interactions, mediated indirectly through the host. At one extreme are pathogens that induce less specific responses: to the innate immune system, these pathogens look alike, and competition may be broad. At the other extreme are pathogens that induce more specific responses, such as influenza (Fig. 1B). Hemagglutination inhibition (HI) assays measure the ability of polyclonal antibodies induced by infection with one influenza strain to prevent the same or a different strain from binding to erythrocyte receptors similar to receptors on respiratory epithelial cells. Antibodies specific for one virus that bind well to another virus, thereby preventing agglutination of the erythrocytes, indicate a short antigenic distance (high cross-reactivity) between the two viruses. Techniques adapted from multidimensional scaling visualize strains’ antigenic relationships from the HI data.66,67 HI assays correlate well with more advanced measurements, despite the fact that these assays cannot detect neutralization by stalk antibodies that inhibit intracellular conformational changes.68,69 Although these representations are low-dimensional abstractions of binding patterns that miss, for example, asymmetric interactions,70 they demonstrate a method to simplify complex patterns of cross-reactivity.
Between these extremes are pathogens that induce responses of intermediate cross-reactivity. Compared to the diversity of antibody-binding sites on influenza's hemagglutinin, epitopes of CD4+ and CD8+ T cells are relatively conserved,71 and unlike influenza,72 pathogens such as malaria, Trypanosoma spp., and N. meningitidis have a finite set of allelic variants of the surface proteins. For these targets of adaptive immunity, homologous epitopes induce cross-reactive responses. Such relationships can be represented as networks, with edges connecting strains that share identical epitopes (Fig. 1C).73 In any individual host, a small fraction of these links may have the potential to be realized. For example, MHC restriction may prohibit certain epitopes from being recognized in hosts lacking a particular MHC allele, or the immunodominance of one response may interfere with the effectiveness of another.74 Thus, the pathogens that hosts perceive as identical (at least with respect to their interactions with the immune system) or equivalently, the pathogens’ phenotypic identities, vary depending on which individual host is reading it. The multidegenerate mapping of genotype to phenotype can affect strain dynamics (Fig. 1D).75
Immunophenotypes vary and change
The immunophenotype may thus acquire different meanings in individuals and host populations, and its definition in each may change over time. Antibodies and CD4+ and CD8+ T cells induced by infection target a set of pathogen epitopes, but immunodominance can shift.76,77 Depending on a host's infection or vaccination history, the immune response may focus on more or less conserved epitopes, creating individual differences in the breadth of the induced response.78,79 Very young, old, or immunocompromised hosts may mount weaker responses, causing shifts in strength over time.80
These differences may partly explain challenges in measuring the impact of immunity on pathogen fitness. Some induced immune responses have no perceivable effect on the growth rate of the pathogen population. For example, serum antibodies from natural carriage with S. pneumoniae appear uncorrelated with protection from colonization in some adults,81 although in others, they can be associated with protection from rechallenge up to 11 months after experimental infection.82 Multiple approaches may be necessary to characterize interactions. Longitudinal observational studies and vaccine trials correlate protection with immune factors.83–85 Challenge experiments demonstrate reductions in susceptibility or infectiousness (measured through shedding rates) as a function of immune correlates, typically antibody titers.86 Genetic knockout and depletion experiments can demonstrate the aggregated direct and indirect causal impact of particular components of immunity on pathogen fitness,87 although inferences from these studies are usually limited by the fact that the animal model is not a natural host of the pathogen. In the next section, I will describe how models fitted to observational data, especially involving vaccination, can provide another source of insight into host–pathogen interactions.
Theories of immune-mediated pathogen evolution
Although there have been notable exceptions,88 especially for within-host models,89 variations of the susceptible–infected–recovered (SIR) model90,91 (Box 2) have served as the major framework for understanding pathogen diversity and evolution. Recent departures from this model show that a more complex immunological niche, reflecting more complex host–pathogen interactions, can offer new explanations for pathogen diversity.
Box 2. The SIR model and its descendants
The original SIR model90 assumes that host immunity can be described by three states: susceptible, infected, or recovered (immune). Hosts move into the infectious class from becoming infected and into the immune class upon recovery. The model has been extended to include many features, including seasonally varying transmission rates, latent periods, age-assortative mixing of hosts, and births and deaths in the host population. The intrinsic fitness of a pathogen is given by the intrinsic reproductive number, R0, which equals the expected number of secondary cases caused by an infected individual in an otherwise susceptible population.91
The impact of immunity in SIR models has been investigated in two major contexts, multistrain competition and boosting and waning. Seemingly neutral multistrain SIR models can include competition in ways that bias toward particular outcomes.151 Immunity to one strain may reduce susceptibility to, or accelerate clearance of, another, or infection with one strain may alter others’ dynamics.152–155 Waning and boosting are usually modeled by allowing individuals to pass through one or more immune states, which may be associated with reduced susceptibility and/or reduced infectiousness.124,156,15
Evolution of the SIR model
Multistrain derivations of the classic SIR model90,92,93 demonstrate surprisingly different outcomes from simple assumptions. For example, assuming that all strains of a malaria-like pathogen have the same fitness in a susceptible host population and vary only by which antigens (of a fixed repertoire) they express, antigenically structured populations with low or high diversity can result, depending on the transmission rates and strengths of cross-immunity.92 Additionally, these structured populations can persist at a steady prevalence in time, maintain stable limit cycles, or undergo chaotic dynamics, with the latter scenarios reflecting stronger negative frequency-dependent selection. A key result in these models is that each set of co-occurring strains appears to minimize competition by minimizing antigenic competition or antigenic niche overlap: strains sharing fewer alleles tend to co-occur, a result that is broadly consistent with niche models of species diversity.94 These kinds of models can also reproduce qualitative features, such as the incidence and periods of oscillations and of the dynamics of dengue,95 cholera,96 and trypanosomes.97
More recently, SIR models incorporating open-ended evolutionary dynamics have simulated immune-mediated competition and evolution in RNA viruses. A model of influenza that assumed one-dimensional antigenic trait space found that clusters of antigenically similar strains would arise and serially replace one another,98 yielding patterns of strain turnover similar to those of H3N2 hemagglutinin.28,67 Antigenic evolution in more dimensions generally shows that the extent of diversity is sensitive to the mutation rate, the mutational accessibility of antigenically distinct phenotypes, and the strength of competition between strains.88,99–102 Highly accessible beneficial mutations can lead to antigenic branching,100 a form of character displacement suggested in the recent evolution of the hemagglutinin of influenza B.103 Strong competition between strains, potentially from nonspecific immune responses, can restrict diversity.88
A limitation of these models is uncertainty over the plausibility of the representation of phenotypic evolution. It is unclear what fraction of mutations should lead to antigenic escape and if these mutations should be costly. Some models have attempted to incorporate evolutionary constraints by tuning the ruggedness of the fitness landscape during the evolution of the immune phenotype, but there are little data to justify particular parametrizations.30,101,104
Uncertainty over evolutionary constraints and the strength of competition is a sticking point in these models of pathogen evolution. The presence of mutations that could, relative to the wild type, reduce fitness in a completely naive host population but might nonetheless be favored in a partially immune population implies that models of pathogen competition and evolution should accommodate variation in intrinsic fitness, or R0, between strains or species (Box 2). Niche theory predicts that as niche overlap declines, competition decreases, and species with lower fitness more easily coexist.94,105 From the perspective of the immune system, species that induce cross-reactive responses occupy overlapping niches and thus compete with one another. Low niche overlap might, for example, explain the coexistence of influenza B and influenza A subtypes.106 Although H3N2 appears to have higher fitness than influenza B and H1N1,24 observations suggest that low levels of cross-reactivity and hence weak competition between them107 permit coexistence on a global scale.88,106,108
New mechanisms for coexistence and evolution
SIR models typically assume only one form of host immunity, and SIR models of multiple strains typically assume this form drives immune-mediated competition. If strains differ in intrinsic fitness, then coexistence between them should only be possible if they compete very weakly.109,110
The coexistence of dozens of serotypes of S. pneumoniae, or pneumococcus, seemed to violate this logic. Pneumococcal serotypes vary in fitness. They have unique polysaccharide capsules, which vary in their thickness and charge. The thicker serotypes are consistently associated with fitness-enhancing traits, such as resistance to nonopsonic phagocytosis, longer durations of carriage, and resistance to clearance by other co-colonizing types.111,112 Initial simulations of interacting serotypes showed that to obtain diversity on par with observations, antibody-mediated immunity to the capsules had to be much more protective than is indicated by epidemiological studies.85,110 Furthermore, traditional SIR models with strong cross-immunity generate dynamics inconsistent with pneumococcal carriage rates.110,113
Models that include another mechanism of acquired immunity—induction of CD4+ T helper (TH) 17 cells not specific to the capsule114—enable coexistence at plausible levels of antibody protection.110 This noncapsule-specific immune response was assumed to be acquired incrementally and to reduce the duration of carriage of all serotypes; in teenagers and adults, serotypes take, on average, several weeks to clear.115 In this model, the host population becomes a resource gradient bounded by two extremes: naive patches (infants) where the fittest serotypes with thick capsules consistently outcompete other serotypes, and highly immune patches (adults) where all serotypes have comparable fitness. In these latter patches, competition is effectively neutral. This expansion of the immunological niche, which includes the stabilizing effects of serotype-specific immunity and the equalizing effects of nonspecific acquired immunity, encompasses a small breadth of the diversity of host–pathogen interactions. The idea that species’ distributions may arise from such a balance of stabilizing and equalizing mechanisms has been a recent focus of research in community ecology.94,116
Vaccine-induced evolution
An ideal vaccine provides complete protection from infection or disease against a pathogen population. To minimize the chance of vaccine escape, the vaccine would instill herd immunity in the host population, or the pathogen population would display no diversity with respect to the vaccine-induced immunity and would be unable to escape it. In practice, pathogens are diverse, and vaccines usually provide imperfect protection that differs from that induced by natural infection.117 By changing the pathogen's immunological environment, vaccines can thus shape evolution.
Models of competing strains predict that vaccination against a subset of strains will increase the abundance of untargeted strains.118,119 This pattern has been observed with influenza vaccines in poultry120 and following the introduction of the pneumococcal conjugate vaccine, which induces antibody responses more protective than those from natural carriage.85,121 In the United States, high vaccination rates in young children nearly eradicated the targeted serotypes and increased the abundances of the untargeted serotypes such that overall carriage rates have not declined.122 This phenomenon has been named serotype replacement.119
When pathogens interact with multiple components of host immunity, vaccines can have particularly unexpected effects that depend on their mechanism of protection. Models of pneumococcal vaccination showed that transient serotype replacement might arise under two scenarios: when anticapsular immunity from the vaccine is lower than anticapsular immunity from natural carriage, and also when it is higher.110 In both scenarios, targeted serotypes disappear following the introduction of the vaccine, but they can later invade (if introduced through immigration) and cause an epidemic.
In the first scenario, vaccine-induced immunity temporarily eradicates targeted serotypes even when the immunity conferred by vaccination is weaker than that from natural carriage (Fig. 2A). The eradication arises from a net increase in the level of anticapsular immunity in the population due to widespread vaccination on top of natural immunity. After the targeted serotypes go locally extinct, anticapsular immunity in the population decays to levels provided by the vaccine. A lack of herd immunity can cause targeted serotypes to reinvade.
Figure 2.
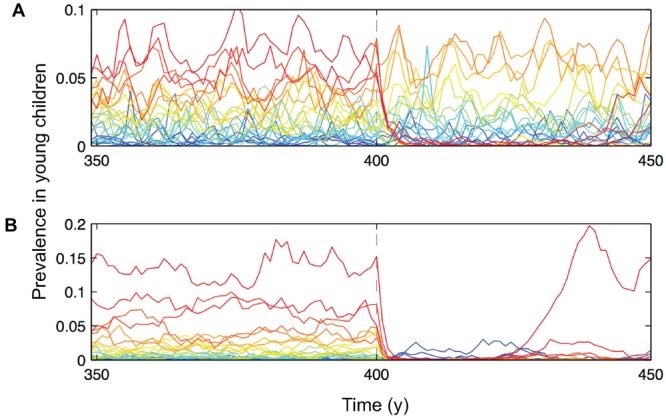
The potential effects of a multivalent vaccine on the evolution of pneumococcal serotypes depend on two mechanisms of immune interaction and differences between natural and vaccine-induced immunity. Natural immunity to pneumococcus includes serotype-specific (antibody-mediated) and nonspecific (CD4+ T cell–mediated) components. Vaccine-induced immunity confers antibody protection only. Acquired serotype-specific immunity from natural carriage is assumed to reduce susceptibility to future colonizations with that serotype by a fraction σc (with σc = 1, implying complete protection; estimates are σc ∼ 0.3–0.6). Figures show the prevalence of each serotype in pre- and postvaccine eras. Simulations assume 100% of the population is vaccinated beginning in the year 400.110 (A) Vaccine-induced serotype-specific immunity σv is slightly weaker than natural serotype-specific immunity σc (σc > σv). Some of the targeted serotypes (red) return a few decades following vaccination. (B) Vaccine-induced serotype-specific immunity is stronger than natural serotype-specific immunity (σc < σv). A vaccine with high valency can allow targeted serotypes to return due to the gradual loss of nonspecific immunity.
In the second scenario, even when vaccine-induced anticapsular immunity is stronger than natural anticapsular immunity, serotype replacement can be transient due to the waning of acquired nonspecific immunity in the population: natural infection induces nonspecific immune memory but the vaccine does not. This erosion of nonspecific immunity can also allow targeted serotypes to return if anticapsular immunity is imperfect (Fig. 2B). Related dynamics might underlie the recent resurgence of pertussis. Usage of the cellular vaccine was discontinued when an acellular vaccine associated with fewer side effects became available. Immunity conferred by the acellular vaccine is shorter lasting, which has led to an increase in cases.123 This effect may have been amplified by the waning of natural immunity during the era of the cellular vaccine from the absence of asymptomatic boosting infections.124
The concept of the immunophenotype illustrates how a successful vaccination campaign against one pathogen may affect competing pathogens in unexpected ways. A randomized controlled trial found that rates of respiratory illness were higher in individuals who received the inactivated influenza vaccine than in unvaccinated individuals,125 suggesting that natural infection with influenza may partially protect against infection with other respiratory pathogens (and may promote others126). The absence of known cross-reactive antigens between the different pathogens suggests that this protection is conferred by innate immunity or is specific but concentrated in infected tissues. Such a result raises the hypothesis that receipt of the live attenuated vaccine, which induces cellular as well as humoral immunity, may protect broadly against respiratory viruses. Similar issues arise with respect to vaccination against individual strains of influenza.127,128 If most competition between influenza types and subtypes comes from cellular or innate immunity, then protection against all influenza may be best conferred by vaccines that mimic natural infection rather than inactivated vaccines, which currently generate only strain-specific antibodies.107,129
Questions for a general theory
Advancing models of immune-mediated pathogen evolution requires progress on empirical and theoretical questions. The most pressing empirical questions are: How do different pathogens interact with host immunity, and how do these interactions vary within host populations? Immunity to several common pathogens has been heavily studied (Table 1), but the strength, duration, and breadth of most host–pathogen interactions have not been systematically analyzed, and even the heavily studied pathogens retain mysteries. Progress in this direction could arise from animal experiments and from examining homologous pathogens of nonhuman hosts.130,131 Observational longitudinal analyses of antibody repertoires76,132–134 and other immune responses, especially when accompanied by infection history, will be especially useful for revealing differences between individuals and test predictions from animal experiments. Inferential population genetic and phylodynamic models that include phenotypic information can shed further light on how pathogen diversity arises from evolutionary pressures.24,135,136 A more complete picture of the immunophenotype should help predict vaccine efficacy and the potential for vaccine-induced evolution.
The largest theoretical challenges echo basic questions in ecology and evolution. First, how many pathogens can coexist in a host population described by a particular set of resources (e.g., tissue types) and immune environment? This is closely related to the question of limiting similarity in ecology: How similar can species be and still coexist?137 Dynamical models of interacting species in environments of varying complexity138 and analytic insights63 could be feasible. Second, will pathogens’ evolutionary constraints in avoiding immunity persist indefinitely? In other words, how robust are any conclusions about phenotypic tradeoffs and the accessibility of new traits? The evolution of resistance to neuraminidase in H1N1 viruses required the accumulation of permissive mutations whose importance had not been anticipated.139 Such concerns about the generalizability of molecular evolution have motivated criticisms of the utility of gain-of-function experiments in influenza viruses.112 Progress in this area may first come from massive experimental evolution studies in simpler systems,140 which might reveal whether predictive models are feasible, or possibly from fitting models to well-sampled pathogen populations.30,141
Acknowledgments
I thank G. Barabas, L. Childs, G. Dwyer, Y. Grad, M. Lipsitch, D. Weinberger, and three anonymous reviewers for helpful comments.
Conflict of interest
The author declares no conflicts of interest.
References
- Grenfell BT, Pybus OG, Gog JR, et al. Unifying the epidemiological and evolutionary dynamics of pathogens. Science. 2004;303:327–332. doi: 10.1126/science.1090727. [DOI] [PubMed] [Google Scholar]
- Domingo E, Sheldon J, Perales C. Viral quasispecies evolution. Microbiol. Mol. Biol. Rev. 2012;76:159–216. doi: 10.1128/MMBR.05023-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman JR, Papamichail D, Skiena S, et al. Virus attenuation by genome-scale changes in codon pair bias. Science. 2008;320:1784–1787. doi: 10.1126/science.1155761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crotty S, Cameron CE, Andino R. RNA virus error catastrophe: direct molecular test by using ribavirin. Proc. Natl. Acad. Sci. U.S.A. 2001;98:6895–6900. doi: 10.1073/pnas.111085598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801. doi: 10.1016/j.cell.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Hyams C, Camberlein E, Cohen JM, et al. The Streptococcus pneumoniae capsule inhibits complement activity and neutrophil phagocytosis by multiple mechanisms. Infect. Immun. 78:704–715. doi: 10.1128/IAI.00881-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Domenico P, Salo RJ, Cross AS, Cunha BA. Polysaccharide capsule-mediated resistance to opsonophagocytosis in Klebsiella pneumoniae. Infect. Immun. 1994;62:4495–4499. doi: 10.1128/iai.62.10.4495-4499.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M, O'Hagan JJ. Patterns of antigenic diversity and the mechanisms that maintain them. J. R. Soc. Interf. 2007;4:787–802. doi: 10.1098/rsif.2007.0229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster TJ. Immune evasion by staphylococci. Nat. Rev. Microbiol. 2005;3:948–958. doi: 10.1038/nrmicro1289. [DOI] [PubMed] [Google Scholar]
- Fitzgerald TJ, Johnson RC. Surface mucopolysaccharides of Treponema pallidum. Infect Immun. 1979;24:244–251. doi: 10.1128/iai.24.1.244-251.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Regoes RR, Hamblin S, Tanaka MM. Viral mutation rates: modelling the roles of within-host viral dynamics and the trade-off between replication fidelity and speed. Proc. Biol. Sci. R. Soc. 2013;280:2012–2047. doi: 10.1098/rspb.2012.2047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas PG, Keating R, Hulse-Post DJ, Doherty PC. Cell-mediated protection in influenza infection. Emerg. Infect. Dis. 2006;12:48–54. doi: 10.3201/eid1201.051237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cutts FT, Franceschi S, Goldie S, et al. Human papillomavirus and HPV vaccines: a review. Bull. World Health Org. 2007;85:719–726. doi: 10.2471/BLT.06.038414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doorbar J. The papillomavirus life cycle. J. Clin. Virol. 2005;32(Suppl 1):S7–S15. doi: 10.1016/j.jcv.2004.12.006. [DOI] [PubMed] [Google Scholar]
- Rasaiyaah J, Tan CP, Fletcher AJ, et al. HIV-1 evades innate immune recognition through specific cofactor recruitment. Nature. 2013;503:402–405. doi: 10.1038/nature12769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia-Sastre A, Durbin RK, Zheng H, et al. The role of interferon in influenza virus tissue tropism. J. Virol. 1998;72:8550–8558. doi: 10.1128/jvi.72.11.8550-8558.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochs G, Garcia-Sastre A, Martinez-Sobrido L. Multiple anti-interferon actions of the influenza A virus NS1 protein. J. Virol. 2007;81:7011–7021. doi: 10.1128/JVI.02581-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin A, Loughman JA, Zinselmeyer BH, et al. Streptolysin S inhibits neutrophil recruitment during the early stages of Streptococcus pyogenes infection. Infect. Immun. 2009;77:5190–5201. doi: 10.1128/IAI.00420-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dagna L, Pritchett JC, Lusso P. Immunomodulation and immunosuppression by human herpesvirus 6A and 6B. Future Virol. 2013;8:273–287. doi: 10.2217/fvl.13.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer JV, Lockridge KM, Barry PA, et al. Potent immunosuppressive activities of cytomegalovirus-encoded interleukin-10. J. Virol. 2002;76:1285–1292. doi: 10.1128/JVI.76.3.1285-1292.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biegalke BJ, Lester E, Branda A, Rana R. Characterization of the human cytomegalovirus UL34 gene. J. Virol. 2004;78:9579–9583. doi: 10.1128/JVI.78.17.9579-9583.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina-Cruz A, Garver LS, Alabaster A, et al. The human malaria parasite Pfs47 gene mediates evasion of the mosquito immune system. Science. 2013;340:984–987. doi: 10.1126/science.1235264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurford A, Day T. Immune evasion and the evolution of molecular mimicry in parasites. Evolution: Int. J. Organ. Evol. 2013;67:2889–2904. doi: 10.1111/evo.12171. [DOI] [PubMed] [Google Scholar]
- Bedford T, Suchard MA, Lemey P, et al. Integrating influenza antigenic dynamics with molecular evolution. eLife. 2014;3:e01914. doi: 10.7554/eLife.01914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rambaut A, Pybus OG, Nelson MI, et al. The genomic and epidemiological dynamics of human influenza A virus. Nature. 2008;453:615–620. doi: 10.1038/nature06945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bedford T, Cobey S, Pascual M. Strength and tempo of selection revealed in viral gene genealogies. BMC Evolut. Biol. 2011;11:220. doi: 10.1186/1471-2148-11-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hensley SE, Das SR, Bailey AL, et al. Hemagglutinin receptor binding avidity drives influenza A virus antigenic drift. Science. 2009;326:734–736. doi: 10.1126/science.1178258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitch WM, Bush RM, Bender CA, Cox NJ. Long term trends in the evolution of H(3) HA1 human influenza type A. Proc. Natl. Acad. Sci. U. S. A. 1997;94:7712–7718. doi: 10.1073/pnas.94.15.7712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das SR, Puigbo P, Hensley SE, et al. Glycosylation focuses sequence variation in the influenza A virus H1 hemagglutinin globular domain. PLoS Pathog. 2010;6:e1001211. doi: 10.1371/journal.ppat.1001211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luksza M, Lassig M. A predictive fitness model for influenza. Nature. 2014;507:57–61. doi: 10.1038/nature13087. [DOI] [PubMed] [Google Scholar]
- Buckee CO, Jolley KA, Recker M, et al. Role of selection in the emergence of lineages and the evolution of virulence in Neisseria meningitidis. Proc. Natl. Acad. Sci. U.S.A. 2008;105:15082–15087. doi: 10.1073/pnas.0712019105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Gierahn T, Thompson CM, et al. Distinct effects on diversifying selection by two mechanisms of immunity against Streptococcus pneumoniae. PLoS Pathog. 2012;8:e1002989. doi: 10.1371/journal.ppat.1002989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debbink K, Lindesmith LC, Donaldson EF, et al. Emergence of new pandemic GII.4 Sydney norovirus strain correlates with escape from herd immunity. J. Infect. Dis. 2013;208:1877–1887. doi: 10.1093/infdis/jit370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao HX, Lynch R, Zhou T, et al. Co-evolution of a broadly neutralizing HIV-1 antibody and founder virus. Nature. 2013;496:469–476. doi: 10.1038/nature12053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bar KJ, Tsao CY, Iyer SS, et al. Early low-titer neutralizing antibodies impede HIV-1 replication and select for virus escape. PLoS Pathog. 2012;8:e1002721. doi: 10.1371/journal.ppat.1002721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tee KK, Lam TT, Chan YF, et al. Evolutionary genetics of human enterovirus 71: origin, population dynamics, natural selection, and seasonal periodicity of the VP1 gene. J. Virol. 2010;84:3339–3350. doi: 10.1128/JVI.01019-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon MJ, Marsh K. The selection landscape of malaria parasites. Science. 2010;328:866–871. doi: 10.1126/science.1185410. [DOI] [PubMed] [Google Scholar]
- Emes RD, Yang Z. Duplicated paralogous genes subject to positive selection in the genome of Trypanosoma brucei. PloS One. 2008;3:e2295. doi: 10.1371/journal.pone.0002295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen TM, Altfeld M, Geer SC, et al. Selective escape from CD8+ T-cell responses represents a major driving force of human immunodeficiency virus type 1 (HIV-1) sequence diversity and reveals constraints on HIV-1 evolution. J. Virol. 2005;79:13239–13249. doi: 10.1128/JVI.79.21.13239-13249.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ganusov VV, Goonetilleke N, Liu MK, et al. Fitness costs and diversity of the cytotoxic T lymphocyte (CTL) response determine the rate of CTL escape during acute and chronic phases of HIV infection. J. Virol. 2011;85:10518–10528. doi: 10.1128/JVI.00655-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon AF, Kosakovsky Pond SL, Bennett P, et al. Adaptation to human populations is revealed by within-host polymorphisms in HIV-1 and hepatitis C virus. PLoS Pathog. 2007;3:e45. doi: 10.1371/journal.ppat.0030045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puig M, Mihalik K, Tilton JC, et al. CD4+ immune escape and subsequent T-cell failure following chimpanzee immunization against hepatitis C virus. Hepatology. 2006;44:736–745. doi: 10.1002/hep.21319. [DOI] [PubMed] [Google Scholar]
- Gog JR, Rimmelzwaan GF, Osterhaus ADME, Grenfell BT. Population dynamics of rapid fixation in cytotoxic T lymphocyte escape mutants of influenza A. Proc. Natl. Acad. Sci. U. S. A. 2003;100:11143–11147. doi: 10.1073/pnas.1830296100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suzuki Y. Natural selection on the influenza virus genome. Mol. Biol. Evol. 2006;23:1902–1911. doi: 10.1093/molbev/msl050. [DOI] [PubMed] [Google Scholar]
- Gupta A, Kaul A, Tsolaki AG, et al. Mycobacterium tuberculosis: immune evasion, latency and reactivation. Immunobiology. 2012;217:363–374. doi: 10.1016/j.imbio.2011.07.008. [DOI] [PubMed] [Google Scholar]
- Pepperell CS, Casto AM, Kitchen A, et al. The role of selection in shaping diversity of natural M. tuberculosis populations. PLoS Pathog. 2013;9:e1003543. doi: 10.1371/journal.ppat.1003543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baranowski E, Ruiz-Jarabo CM, Domingo E. Evolution of cell recognition by viruses. Science. 2001;292:1102–1105. doi: 10.1126/science.1058613. [DOI] [PubMed] [Google Scholar]
- Recker M, Buckee CO, Serazin A, et al. Antigenic variation in Plasmodium falciparum malaria involves a highly structured switching pattern. PLoS Pathog. 2011;7:e1001306. doi: 10.1371/journal.ppat.1001306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santibanez S, Niewiesk S, Heider A, et al. Probing neutralizing-antibody responses against emerging measles viruses (MVs): immune selection of MV by H protein-specific antibodies. J. Gen. Virol. 2005;86:365–374. doi: 10.1099/vir.0.80467-0. [DOI] [PubMed] [Google Scholar]
- Mitnaul LJ, Matrosovich MN, Castrucci MR, et al. Balanced hemagglutinin and neuraminidase activities are critical for efficient replication of influenza A virus. J. Virol. 2000;74:6015–6020. doi: 10.1128/jvi.74.13.6015-6020.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndifon W, Wingreen NS, Levin SA. Differential neutralization efficiency of hemagglutinin epitopes, antibody interference, and the design of influenza vaccines. Proc. Natl. Acad. Sci. U. S. A. 2009;106:8701–8706. doi: 10.1073/pnas.0903427106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Povolotskaya IS, Kondrashov FA. Sequence space and the ongoing expansion of the protein universe. Nature. 2010;465:922–926. doi: 10.1038/nature09105. [DOI] [PubMed] [Google Scholar]
- Szendro IG, Schenk MF, Franke J, Krug J, et al. Quantitative analyses of empirical fitness landscapes. J. Stat. Mech. 2013 P01005 doi: 10.1088/1742-5468/2013/01/P01005. [Google Scholar]
- Cobey S, Koelle K. Capturing escape in infectious disease dynamics. Trends Ecol. Evol. 2008;23:572–577. doi: 10.1016/j.tree.2008.06.008. [DOI] [PubMed] [Google Scholar]
- Chu PY, Ke GM, Chen PC, et al. Spatiotemporal dynamics and epistatic interaction sites in dengue virus type 1: a comprehensive sequence-based analysis. PloS One. 2013;8:e74165. doi: 10.1371/journal.pone.0074165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander C, Rietschel ET. Bacterial lipopolysaccharides and innate immunity. J. Endotoxin Res. 2001;7:167–202. [PubMed] [Google Scholar]
- Murphy K. “Janeway's immunobiology.”. In: Murphy C, editor. Garland Sciences. 8th ed. New York: Taylor & Francis Group, LLC; 2012. pp. 202–216. Ed.: 412–413. [Google Scholar]
- Baccam P, Beauchemin C, Macken CA, et al. Kinetics of influenza A virus infection in humans. J. Virol. 2006;80:7590–7599. doi: 10.1128/JVI.01623-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Reeth K. Cytokines in the pathogenesis of influenza. Veterin. Microbiol. 2000;74:109–116. doi: 10.1016/s0378-1135(00)00171-1. [DOI] [PubMed] [Google Scholar]
- Maruyama M, Lam KP, Rajewsky K. Memory B-cell persistence is independent of persisting immunizing antigen. Nature. 2000;407:636–642. doi: 10.1038/35036600. [DOI] [PubMed] [Google Scholar]
- Cobey S, Lipsitch M. Pathogen diversity and hidden regimes of apparent competition. Amer. Natur. 2013;181:12–24. doi: 10.1086/668598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lloyd-Smith JO. Vacated niches, competitive release and the community ecology of pathogen eradication. Philos. Trans. R Soc. Lond. B Biol. Sci. 2013;368:20120150. doi: 10.1098/rstb.2012.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barabas G, Meszena G, Ostling A. Community robustness and limiting similarity in periodic environments. Theor. Ecol. 2012;5:265. [Google Scholar]
- Szilagyi A, Meszena G. Limiting similarity and niche theory for structured populations. J. Theor. Biol. 2009;258:27–37. doi: 10.1016/j.jtbi.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Meszena G, Gyllenberg M, Pasztor L, Metz JA. Competitive exclusion and limiting similarity: a unified theory. Theor. Populat. Biol. 2006;69:68–87. doi: 10.1016/j.tpb.2005.07.001. [DOI] [PubMed] [Google Scholar]
- Lapedes A, Farber R. The geometry of shape space: application to influenza. J. Theoret. Biol. 2001;212:57–69. doi: 10.1006/jtbi.2001.2347. [DOI] [PubMed] [Google Scholar]
- Smith DJ, Lapedes AS, de Jong JC, et al. Mapping the antigenic and genetic evolution of influenza virus. Science. 2004;305:371–376. doi: 10.1126/science.1097211. [DOI] [PubMed] [Google Scholar]
- Grund S, Adams O, Wahlisch S, Schweiger B. Comparison of hemagglutination inhibition assay, an ELISA-based micro-neutralization assay and colorimetric microneutralization assay to detect antibody responses to vaccination against influenza A H1N1 2009 virus. J. Virol. Meth. 2011;171:369–373. doi: 10.1016/j.jviromet.2010.11.024. [DOI] [PubMed] [Google Scholar]
- Katz JM, Hancock K, Xu X. Serologic assays for influenza surveillance, diagnosis and vaccine evaluation. Expert Rev. Anti-infect. Ther. 2011;9:669–683. doi: 10.1586/eri.11.51. [DOI] [PubMed] [Google Scholar]
- Underwood PA. Serology and energetics of cross-reactions among the H-3 antigens of influenza-viruses. Infect. Immun. 1980;27:397–404. doi: 10.1128/iai.27.2.397-404.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rimmelzwaan GF, Kreijtz JH, Bodewes R, et al. Influenza virus CTL epitopes, remarkably conserved and remarkably variable. Vaccine. 2009;27:6363–6365. doi: 10.1016/j.vaccine.2009.01.016. [DOI] [PubMed] [Google Scholar]
- Recker M, Pybus OG, Nee S, Gupta S. The generation of influenza outbreaks by a network of host immune responses against a limited set of antigenic types. Proc. Natl. Acad. Sci. U.S.A. 2007;104:7711–7716. doi: 10.1073/pnas.0702154104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckee CO, Bull PC, Gupta S. Inferring malaria parasite population structure from serological networks. Proc. Biol. Sci.: R. Soc. 2009;276:477–485. doi: 10.1098/rspb.2008.1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe SR, Turner SJ, Miller SC, et al. Differential antigen presentation regulates the changing patterns of CD8(+) T cell immunodominance in primary and secondary influenza virus infections. J. Exp. Med. 2003;198:399–410. doi: 10.1084/jem.20022151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobey S, Pascual M. Consequences of host heterogeneity, epitope immunodominance, and immune breadth for strain competition. J. Theor. Biol. 2011;270:80–87. doi: 10.1016/j.jtbi.2010.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrammert J, Koutsonanos D, Li GM, et al. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J. Exp. Med. 2011;208:181–193. doi: 10.1084/jem.20101352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welsh RM, Che JW, Brehm MA, Selin LK. Heterologous immunity between viruses. Immunol. Rev. 2010;235:244–266. doi: 10.1111/j.0105-2896.2010.00897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Myers JL, Bostick DL, et al. Immune history shapes specificity of pandemic H1N1 influenza antibody responses. J. Exp. Med. 2013;210:1493–1500. doi: 10.1084/jem.20130212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wherry EJ, Blattman JN, Murali-Krishna K, et al. Viral persistence alters CD8 T-cell immunodominance and tissue distribution and results in distinct stages of functional impairment. J. Virol. 2003;77:4911–4927. doi: 10.1128/JVI.77.8.4911-4927.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goronzy JJ, Weyand CM. Understanding immunosenescence to improve responses to vaccines. Nature Immunol. 2013;14:428–436. doi: 10.1038/ni.2588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malley R, Lipsitch M, Bogaert D, et al. Serum antipneumococcal antibodies and pneumococcal colonization in adults with chronic obstructive pulmonary disease. J. Infect. Dis. 2007;196:928–935. doi: 10.1086/520937. [DOI] [PubMed] [Google Scholar]
- Ferreira DM, Neill DR, Bangert M, et al. Controlled human infection and rechallenge with Streptococcus pneumoniae reveals the protective efficacy of carriage in healthy adults. Am. J. Respir. Crit. Care Med. 2013;187:855–864. doi: 10.1164/rccm.201212-2277OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng S, Fang VJ, Ip DK, et al. Estimation of the association between antibody titers and protection against confirmed influenza virus infection in children. J. Infect. Dis. 2013;208:1320–1324. doi: 10.1093/infdis/jit372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohmit SE, Petrie JG, Cross RT, et al. Influenza hemagglutination-inhibition antibody titer as a correlate of vaccine-induced protection. J. Infect. Dis. 2011;204:1879–1885. doi: 10.1093/infdis/jir661. [DOI] [PubMed] [Google Scholar]
- Weinberger DM, Dagan R, Givon-Lavi N, et al. Epidemiologic evidence for serotype-specific acquired immunity to pneumococcal carriage. J. Infect. Dis. 2008;197:1511–1518. doi: 10.1086/587941. [DOI] [PubMed] [Google Scholar]
- Hobson D, Curry RL, Beare AS, Ward-Gardner A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J. Hyg. (Lond.) 1972;70:767–777. doi: 10.1017/s0022172400022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tate MD, Brooks AG, Reading PC. The role of neutrophils in the upper and lower respiratory tract during influenza virus infection of mice. Respir. Res. 2008;9:57. doi: 10.1186/1465-9921-9-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson NM, Galvani AP, Bush RM. Ecological and immunological determinants of influenza evolution. Nature. 2003;422:428–433. doi: 10.1038/nature01509. [DOI] [PubMed] [Google Scholar]
- Ganusov VV, Neher RA, Perelson AS. Mathematical modeling of escape of HIV from cytotoxic T lymphocyte responses. J. Statist. Mech. 2013;2013:P01010. doi: 10.1088/1742-5468/2013/01/P01010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kermack WO, McKendrick AG. A contribution to the mathematical theory of epidemics. Proc. R. Soc. Lond. Ser. A. 1927;115:700–721. [Google Scholar]
- Keeling MJ, Rohani P. Modeling Infectious Diseases in Humans and Animals. Princeton, NJ: Princeton University Press; 2007. [Google Scholar]
- Gupta S, Ferguson NM, Anderson RM. Chaos, persistence, and evolution of strain structure in antigenically diverse infectious agents. Science. 1998;280:912–915. doi: 10.1126/science.280.5365.912. [DOI] [PubMed] [Google Scholar]
- Andreasen V, Lin J, Levin SA. The dynamics of cocirculating influenza strains conferring partial cross-immunity. J. Math. Biol. 1997;35:825–842. doi: 10.1007/s002850050079. [DOI] [PubMed] [Google Scholar]
- Chesson P. Mechanism of maintenance of species diversity. Annu. Rev. Ecol. Syst. 2000;31:343–366. [Google Scholar]
- Reich NG, Shrestha S, King AA, et al. Interactions between serotypes of dengue highlight epidemiological impact of cross-immunity. J. R. Soc. Interf. 2013;10:20130414. doi: 10.1098/rsif.2013.0414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koelle K, Pascual M, Yunus M. Serotype cycles in cholera dynamics. Proc. R. Soc. B-Biol. Sci. 2006;273:2879–2886. doi: 10.1098/rspb.2006.3668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agur Z, Abiri D, Van der Ploeg LH. Ordered appearance of antigenic variants of African trypanosomes explained in a mathematical model based on a stochastic switch process and immune-selection against putative switch intermediates. Proc. Natl. Acad. Sci. U.S.A. 1989;86:9626–9630. doi: 10.1073/pnas.86.23.9626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gog JR, Grenfell BT. Dynamics and selection of many-strain pathogens. Proc. Natl. Acad. Sci. U. S. A. 2002;99:17209–17214. doi: 10.1073/pnas.252512799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omori R, Adams B, Sasaki A. Coexistence conditions for strains of influenza with immune cross-reaction. J. Theor. Biol. 2010;262:48–57. doi: 10.1016/j.jtbi.2009.09.015. [DOI] [PubMed] [Google Scholar]
- Bedford T, Rambaut A, Pascual M. Canalization of the evolutionary trajectory of the human influenza virus. BMC Biol. 2012;10:38. doi: 10.1186/1741-7007-10-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koelle K, Cobey S, Grenfell B, Pascual M. Epochal evolution shapes the phylodynamics of interpandemic influenza. Science. 2006;314:1898–1903. doi: 10.1126/science.1132745. [DOI] [PubMed] [Google Scholar]
- Zinder D, Bedford T, Gupta S, Pascual M. The roles of competition and mutation in shaping antigenic and genetic diversity in influenza. PLoS Pathog. 2013;9:e1003104. doi: 10.1371/journal.ppat.1003104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen RB, Holmes EC. The evolutionary dynamics of human influenza B virus. J. Mol. Evol. 2008;66:655–663. doi: 10.1007/s00239-008-9119-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tria F, Lassig M, Peliti L, Franz S. A minimal stochastic model for influenza evolution. J. Stat. Mech. Theory E. 2005 P07008 doi: 10.1088/1742-5468/2005/07/P07008. [Google Scholar]
- Hutchinson GE. Concluding remarks. Cold Spring Harbor Symposium. Quantit. Biol. 1957;22:415–427. [Google Scholar]
- Goldstein E, Cobey S, Takahashi S, et al. Predicting the epidemic sizes of influenza A/H1N1, A/H3N2, and B: a statistical method. PLoS Med. 2011;8:e1001051. doi: 10.1371/journal.pmed.1001051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laidlaw BJ, Decman V, Ali MA, et al. Cooperativity between CD8+ T cells, non-neutralizing antibodies, and alveolar macrophages is important for heterosubtypic influenza virus immunity. PLoS Pathog. 2013;9:e1003207. doi: 10.1371/journal.ppat.1003207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelman BS, Viboud C, Koelle K, et al. Global patterns in seasonal activity of influenza A/H3N2, A/H1N1, and B from 1997 to 2005: viral coexistence and latitudinal gradients. PloS One. 2007;2:e1296. doi: 10.1371/journal.pone.0001296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gause GF. Experimental studies on the struggle for existence. I. Mixed population of two species of yeast. J. Exp. Biol. 1932;9:389–402. [Google Scholar]
- Cobey S, Lipsitch M. Niche and neutral effects of acquired immunity permit coexistence of pneumococcal serotypes. Science. 2012;335:1376–1380. doi: 10.1126/science.1215947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger DM, Trzcinski K, Lu YJ, et al. Pneumococcal capsular polysaccharide structure predicts serotype prevalence. PLoS Pathog. 2009;5:e1000476. doi: 10.1371/journal.ppat.1000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M, Abdullahi O, D'Amour A, et al. Estimating rates of carriage acquisition and clearance and competitive ability for pneumococcal serotypes in Kenya with a Markov transition model. Epidemiology. 2012;23:510–519. doi: 10.1097/EDE.0b013e31824f2f32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flasche S, Edmunds WJ, Miller E, Goldblatt D, Robertson C, Choi YH. The impact of specific and non-specific immunity on the ecology of Streptococcus pneumoniae and the implications for vaccination. Proc. Biol. Sci.: R. Soc. 2013;280:20131939. doi: 10.1098/rspb.2013.1939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malley R, Trzcinski K, Srivastava A, et al. CD4+ T cells mediate antibody-independent acquired immunity to pneumococcal colonization. Proc. Natl. Acad. Sci. U. S. A. 2005;102:4848–4853. doi: 10.1073/pnas.0501254102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogberg L, Geli P, Ringberg H, et al. Age- and serogroup-related differences in observed durations of nasopharyngeal carriage of penicillin-resistant pneumococci. J. Clin. Microbiol. 2007;45:948–952. doi: 10.1128/JCM.01913-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler PB, Hillerislambers J, Levine JM. A niche for neutrality. Ecol. Lett. 2007;10:95–104. doi: 10.1111/j.1461-0248.2006.00996.x. [DOI] [PubMed] [Google Scholar]
- Wendelboe AM, Van Rie A, Salmaso S, Englund JA. Duration of immunity against pertussis after natural infection or vaccination. Pediatr. Infect. Dis. J. 2005;24:S58–S61. doi: 10.1097/01.inf.0000160914.59160.41. [DOI] [PubMed] [Google Scholar]
- Lipsitch M. Vaccination against colonizing bacteria with multiple serotypes. Proc. Natl. Acad. Sci. U.S.A. 1997;94:6571–6576. doi: 10.1073/pnas.94.12.6571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M. Bacterial vaccines and serotype replacement: lessons from Haemophilus influenzae and prospects for Streptococcus pneumoniae. Emerg. Infect. Dis. 1999;5:336–345. doi: 10.3201/eid0503.990304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee CW, Senne DA, Suarez DL. Effect of vaccine use in the evolution of Mexican lineage H5N2 avian influenza virus. J. Virol. 2004;78:8372–8381. doi: 10.1128/JVI.78.15.8372-8381.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinta-Kokko H, Dagan R, Givon-Lavi N, Auranen K. Estimation of vaccine efficacy against acquisition of pneumococcal carriage. Vaccine. 2009;27:3831–3837. doi: 10.1016/j.vaccine.2009.04.009. [DOI] [PubMed] [Google Scholar]
- Hanage WP, Finkelstein JA, Huang SS, et al. Evidence that pneumococcal serotype replacement in Massachusetts following conjugate vaccination is now complete. Epidemics. 2010;2:80–84. doi: 10.1016/j.epidem.2010.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witt MA, Katz PH, Witt DJ. Unexpectedly limited durability of immunity following acellular pertussis vaccination in preadolescents in a North American outbreak. Clin. Infect. Dis. 2012;54:1730–1735. doi: 10.1093/cid/cis287. [DOI] [PubMed] [Google Scholar]
- Lavine JS, King AA, Bjornstad ON. Natural immune boosting in pertussis dynamics and the potential for long-term vaccine failure. Proc. Natl. Acad. Sci. U.S.A. 2011;108:7259–7264. doi: 10.1073/pnas.1014394108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling BJ, Fang VJ, Nishiura H, et al. Increased risk of noninfluenza respiratory virus infections associated with receipt of inactivated influenza vaccine. Clin. Infect. Dis. 2012;54:1778–1783. doi: 10.1093/cid/cis307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AM, Adler FR, Ribeiro RM, et al. Kinetics of coinfection with influenza A virus and Streptococcus pneumoniae. PLoS Pathog. 2013;9:e1003238. doi: 10.1371/journal.ppat.1003238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodewes R, Kreijtz JH, Geelhoed-Mieras MM, et al. Vaccination against seasonal influenza A/H3N2 virus reduces the induction of heterosubtypic immunity against influenza A/H5N1 virus infection in ferrets. J. Virol. 2011;85:2695–2702. doi: 10.1128/JVI.02371-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodewes R, Kreijtz JH, Hillaire ML, et al. Vaccination with whole inactivated virus vaccine affects the induction of heterosubtypic immunity against influenza virus A/H5N1 and immunodominance of virus-specific CD8+ T-cell responses in mice. J. Gen. Virol. 2010;91:1743–1753. doi: 10.1099/vir.0.020784-0. [DOI] [PubMed] [Google Scholar]
- Bodewes R, Fraaij PL, Kreijtz JH, et al. Annual influenza vaccination affects the development of heterosubtypic immunity. Vaccine. 2012;30:7407–7410. doi: 10.1016/j.vaccine.2012.04.086. [DOI] [PubMed] [Google Scholar]
- Neuman de Vegvar HE, Amara RR, Steinman L, et al. Microarray profiling of antibody responses against simian-human immunodeficiency virus: postchallenge convergence of reactivities independent of host histocompatibility type and vaccine regimen. J. Virol. 2003;77:11125–11138. doi: 10.1128/JVI.77.20.11125-11138.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stephens R, Culleton RL, Lamb TJ. The contribution of Plasmodium chabaudi to our understanding of malaria. Trends Parasitol. 2012;28:73–82. doi: 10.1016/j.pt.2011.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller MS, Gardner TJ, Krammer F, et al. Neutralizing antibodies against previously encountered influenza virus strains increase over time: a longitudinal analysis. Sci. Translat. Med. 2013;5:198ra07. doi: 10.1126/scitranslmed.3006637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang N, He J, Weinstein JA, et al. Lineage structure of the human antibody repertoire in response to influenza vaccination. Sci. Translat. Med. 2013;5:171ra19. doi: 10.1126/scitranslmed.3004794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li GM, Chiu C, Wrammert J, et al. Pandemic H1N1 influenza vaccine induces a recall response in humans that favors broadly cross-reactive memory B cells. Proc. Natl. Acad. Sci. U.S.A. 2012;109:9047–9052. doi: 10.1073/pnas.1118979109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koelle K, Khatri P, Kamradt M, Kepler TB. A two-tiered model for simulating the ecological and evolutionary dynamics of rapidly evolving viruses, with an application to influenza. J. R. Soc. Interf. 2010;7:1257–1274. doi: 10.1098/rsif.2010.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessinger TA, Perelson AS, Neher RA. Inferring HIV escape rates from multi-locus genotype data. Front. Immunol. 2013;4:252. doi: 10.3389/fimmu.2013.00252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abrams P. The theory of limiting similarity. Annu. Rev. Ecol. Systemat. 1983;14:359–376. [Google Scholar]
- Polis GA, Strong DR. Food web complexity and community dynamics. Amer. Natural. 1996;147:813–846. [Google Scholar]
- Bloom JD, Gong LI, Baltimore D. Permissive secondary mutations enable the evolution of influenza oseltamivir resistance. Science. 2010;328:1272–1275. doi: 10.1126/science.1187816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jimenez JI, Xulvi-Brunet R, Campbell GW, et al. Comprehensive experimental fitness landscape and evolutionary network for small RNA. Proc. Natl. Acad. Sci. U.S.A. 2013;110:14984–14989. doi: 10.1073/pnas.1307604110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson AL, Mann JK, Omarjee S, et al. Translating HIV sequences into quantitative fitness landscapes predicts viral vulnerabilities for rational immunogen design. Immunity. 2013;38:606–617. doi: 10.1016/j.immuni.2012.11.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Hayward AD, Watt KA, et al. Fitness correlates of heritable variation in antibody responsiveness in a wild mammal. Science. 2010;330:662–665. doi: 10.1126/science.1194878. [DOI] [PubMed] [Google Scholar]
- Cooper GS, Bynum ML, Somers EC. Recent insights in the epidemiology of autoimmune diseases: improved prevalence estimates and understanding of clustering of diseases. J. Autoimmun. 2009;33:197–207. doi: 10.1016/j.jaut.2009.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Childs LM, Held NL, Young MJ, et al. Multiscale model of CRISPR-induced coevolutionary dynamics: diversification at the interface of Lamarck and Darwin. Evol.: Int. J. Org. Evol. 2012;66:2015–2029. doi: 10.1111/j.1558-5646.2012.01595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- To KK, Zhang AJ, Hung IF, et al. High titer and avidity of nonneutralizing antibodies against influenza vaccine antigen are associated with severe influenza. Clin. Vaccine Immunol. 2012;19:1012–1018. doi: 10.1128/CVI.00081-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe SR, Miller SC, Woodland DL. Identification of protective and non-protective T cell epitopes in influenza. Vaccine. 2006;24:452–456. doi: 10.1016/j.vaccine.2005.07.090. [DOI] [PubMed] [Google Scholar]
- Khurana S, Loving CL, Manischewitz J, et al. Vaccine-induced anti-HA2 antibodies promote virus fusion and enhance influenza virus respiratory disease. Sci. Translat. Med. 2013;5:200ra114. doi: 10.1126/scitranslmed.3006366. [DOI] [PubMed] [Google Scholar]
- Kinter AL, Ostrowski M, Goletti D, et al. HIV replication in CD4+ T cells of HIV-infected individuals is regulated by a balance between the viral suppressive effects of endogenous beta-chemokines and the viral inductive effects of other endogenous cytokines. Proc. Natl. Acad. Sci. U.S.A. 1996;93:14076–14081. doi: 10.1073/pnas.93.24.14076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buzon MJ, Sun H, Li C, et al. HIV-1 persistence in CD4+ T cells with stem cell-like properties. Nature Med. 2014;20:139–142. doi: 10.1038/nm.3445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon-Lowe CD, Neuhierl B, Baldwin G, et al. Resting B cells as a transfer vehicle for Epstein-Barr virus infection of epithelial cells. Proc. Natl. Acad. Sci. U.S.A. 2006;103:7065–7070. doi: 10.1073/pnas.0510512103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M, Colijn C, Cohen T, et al. No coexistence for free: neutral null models for multistrain pathogens. Epidemics. 2009;1:2–13. doi: 10.1016/j.epidem.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J, Andreasen V, Levin SA. Dynamics of influenza A drift: the linear three-strain model. Math. Biosci. 1999;162:33–51. doi: 10.1016/s0025-5564(99)00042-5. [DOI] [PubMed] [Google Scholar]
- Gog JR, Swinton J. A status-based approach to multiple strain dynamics. J. Math. Biol. 2002;44:169–184. doi: 10.1007/s002850100120. [DOI] [PubMed] [Google Scholar]
- Kryazhimskiy S, Dieckmann U, Levin SA, Dushoff J. On state-space reduction in multi-strain pathogen models, with an application to antigenic drift in influenza A. Plos Computat. Biol. 2007;3:1513–1525. doi: 10.1371/journal.pcbi.0030159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koelle K, Rodo X, Pascual M, et al. Refractory periods and climate forcing in cholera dynamics. Nature. 2005;436:696–700. doi: 10.1038/nature03820. [DOI] [PubMed] [Google Scholar]
- King AA, Ionides EL, Pascual M, Bouma MJ. Inapparent infections and cholera dynamics. Nature. 2008;454:877–880. doi: 10.1038/nature07084. [DOI] [PubMed] [Google Scholar]
- Knossow M, Gaudier M, Douglas A, et al. Mechanism of neutralization of influenza virus infectivity by antibodies. Virology. 2002;302:294–298. doi: 10.1006/viro.2002.1625. [DOI] [PubMed] [Google Scholar]
- Fitch WM, Leiter JME, Li X, Palese P. Positive Darwinian evolution in human influenza A viruses. Proc. Natl. Acad. Sci. U. S. A. 1991;88:4270–4274. doi: 10.1073/pnas.88.10.4270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips RE, Rowland-Jones S, Nixon DF, et al. Human immunodeficiency virus genetic variation that can escape cytotoxic T cell recognition. Nature. 1991;354:453–459. doi: 10.1038/354453a0. [DOI] [PubMed] [Google Scholar]
- Lewis-Rogers N, Bendall ML, Crandall KA. Phylogenetic relationships and molecular adaptation dynamics of human rhinoviruses. Mol. Biol. Evol. 2009;26:969–981. doi: 10.1093/molbev/msp009. [DOI] [PubMed] [Google Scholar]
- Taniguchi K, Maloy WL, Nishikawa K, et al. Identification of cross-reactive and serotype 2-specific neutralization epitopes on VP3 of human rotavirus. J. Virol. 1988;62:2421–2426. doi: 10.1128/jvi.62.7.2421-2426.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrews TD, Gojobori T. Strong positive selection and recombination drive the antigenic variation of the PilE protein of the human pathogen Neisseria meningitidis. Genetics. 2004;166:25–32. doi: 10.1534/genetics.166.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barry JD, McCulloch R. Antigenic variation in trypanosomes: enhanced phenotypic variation in a eukaryotic parasite. Adv. Parasitol. 2001;49:1–70. doi: 10.1016/s0065-308x(01)49037-3. [DOI] [PubMed] [Google Scholar]


