Abstract
Objective
Estimating dietary intake is challenging in patients with chronic diseases. The aim of this study was to calibrate the Block Brief 2000 food frequency questionnaire (BFFQ) using 3-day food diary records among patients on dialysis.
Methods
Data from 3-day food diary records from 146 patients new to dialysis were reviewed and entered into National Cancer Institute self-administered 24-hour dietary recall (ASA24), a web-based dietary interview system. The information was then re-entered omitting foods reported in the diaries that were not in the BFFQ to generate a “BFFQ-restricted” set of intakes. We modeled each major dietary component (i.e., energy [total calories], protein, carbohydrate, fat) separately using linear regression. The main independent variables were BFFQ-restricted food diary estimates computed as the average of the 3 days of diaries, restricted to items included in the BFFQ, with the unrestricted 3-day food diary averages as dependent variables.
Results
The BFFQ-restricted diary energy estimate of 1,325 ± 545 kcal was 87% of the energy intake in the full food diary (1,510.3 ± 510.4, P < .0001). The BFFQ-restricted diary carbohydrate intake was 83% of the full food diary (156.7 ± 78.7 g vs. 190.4 ± 72.7, P < .0001). The BFFQ-restricted fat intake was 90% of the full-diary-reported fat intake (50.1 ± 24.1 g vs. 56.4 ± 21.6 g, P < .0001). Daily protein intake assessments were not statistically different by BFFQ-restricted diary and full diary assessment (63.1 ± 28.5 vs. 64.1 ± 21.4 g, P = .60). The associations between BFFQ-restricted diary intake and unrestricted intake were linear. Three-day diary-reported intake could be estimated from BFFQ-restricted intake with r2 ranging from 0.36 to 0.56 (P < .0001 for energy [total calories], protein, carbohydrate, and fat). Final equations did not include adjustments for age, sex, or race because the patterns of associations were not significantly different.
Conclusion
Energy and macronutrient estimates by BFFQ are lower than estimates from 3-day food diaries, but simple calibration equations can be used to approximate total intake from BFFQ responses.
Introduction
MALNUTRITION IS COMMON among patients with end-stage renal disease and is associated with mortality and morbidity.1-3 Several methods for ascertaining dietary intake have been used clinically and for research purposes.1,2,4-6 The most common methods include dietary recall, food diaries, and food frequency questionnaires (FFQs). Short-term dietary recall is less subject to recall bias than FFQs. However, intake ascertained over short periods of time (e.g., 24 hours) can be influenced by day-to-day variability in dietary intake, which may be particularly important in the hemodialysis population because of differences in intake on dialysis and nondialysis days.4 Food diaries can cover a longer period than recall interviews, mitigating the problem of day-to-day variation. However, dietary recall and food diaries are time-consuming for nutritionists to administer and/or for patients to complete.7 FFQs were developed to capture usual or typical intake over even longer periods of time and have been used extensively in research settings to explore associations between nutrient intake and outcomes.8,9
Full-length versions of the Block FFQ for adults have been available since the 1980s and have been validated against diet records and recalls in numerous studies.10-20 The full-length Block 2005 FFQ was designed to estimate usual and customary intake of a wide array of nutrients and food groups using a food list and nutrient database developed from dietary recall data provided in 2 waves of National Health and Nutrition Examination Survey data— 1999 to 2000 and 2001 to 2002. The full-length FFQ (110 food items) takes approximately 40 minutes to complete. A Brief FFQ (BFFQ), which contains a reduced food list of approximately 70 items, was introduced to reduce the time required to collect nutritional intake data. Research comparing an earlier 60-item FFQ with multiple diet records found strong correlations for micro- and macronutrients, as well as similar point estimates of intake for micronutrients, but differences of approximately 20% for point estimates of energy and macronutrients.21,22
Because patients on dialysis are subject to dietary restriction and receive regular dietary counseling by trained dietitians employed by dialysis facilities, their diet differs systematically from that of a healthy population.23 Therefore, we believed it was important to calibrate the BFFQ with respect to self-reported dietary intake in this population, aiming to develop equations to estimate energy, protein, carbohydrate, and fat intake that are based on the subset of food items queried in the BFFQ.
Materials and Methods
Study Participants
We used nutritional data from a cohort of 146 incident dialysis patients seen from July 1996 to August 1997 at 26 dialysis units in Atlanta, GA. These participants were recruited into a previous study on nutritional intake that included 3-day food diaries.24 The Institutional Review Board at Emory University approved the study. All participants provided written informed consent. Demographic information and medical history were obtained by patient interview.
Nutritional Data
A study dietitian provided instructions to participants on completing 3-day food diaries, and completed diaries were returned via mail. For the study presented here, the National Cancer Institute self-administered 24-hour dietary recall (ASA24), a web-based dietary tool, was used for data entry. The ASA24 was developed using the U.S. Department of Agriculture (USDA)’s Automated Multiple Pass Method (AMPM) as a model. The AMPM is used in the National Health and Nutrition Examination Survey. Developers used the USDA’s Food and Nutrient Database for Dietary Studies and the MyPyramid Equivalents Database as well as food portion photographs developed by Baylor College of Medicine as resources for intake estimates.25 The USDA’s AMPM program has demonstrated moderate correlation to 4-day food records.26 No published validity or reliability data are currently available for the ASA24.
Data from the 3-day food diaries completed by the cohort of 146 incident dialysis patients were reviewed and entered into the ASA24 twice by study personnel. Diaries were excluded if they contained unrealistically low intake, suggesting incomplete data (n = 8), or if intake was unrealistically high, suggesting more than 3 days of intake reported. First, all data from the food diary were entered, and estimates of mean daily total energy intake, as well as protein, carbohydrate, and fat intakes, were generated. Next, the information was re-entered excluding any foods and beverages reported in the diary that were not included in the BFFQ (Appendix A, available online at http://dx.doi.org/10.1053/j.jrn.2013.12.004), creating a second “BFFQ-restricted” set of mean intakes. The result was 2 sets of measurements for each dietary intake component for each participant: 1 set based on the complete 3-day diary and 1 set based on the subset of items on the 3-day diary that were included in the BFFQ. Items from the food diaries that were not included in the BFFQ were tabulated.
Statistical Methods
Continuous data were summarized as mean and standard deviation for approximately normally distributed variables (determined by QQ-plots) and as median and interquartile range for non-normally distributed variables. For assessment of hemodialysis adequacy, the 3-treatment average urea reduction ratio for each individual was used to calculate the single-pool Kt/V.27,28 Categorical variables were summarized using proportions.
Dependent variables were mean energy, protein, carbohydrate, and fat intakes that were based on the complete 3-day food diary. Full 3-day diary intake and BFFQ-restricted diary intakes for energy, protein, carbohydrate, and fat were compared using paired t tests. We used multiple linear regression to model each dependent variable with mean BFFQ-restricted diary intake for each component as the main independent (predictor) variable. The full models included the additional covariates of age, sex, race, diabetes, and all 2-way interactions between each covariate and BFFQ-restricted intake. Variables were removed from the full models in a backward stepwise fashion using a criterion of P less than .05 for retention for primary variables and interaction terms. Residual plots were examined for outliers. Analyses were performed using SAS version 9.2 (SAS Institute, Inc., Cary, NC).
Results
Participant Characteristics
There were 154 participant 3-day food diaries available for analysis. Eight individuals had incomplete diary data and were not included in the analysis. The median age of participants was 58.7 (interquartile range 22.0-87.3) years (Table 1). Fifty-three percent of the participants were male and 56% were White. The primary dialysis modality was hemodialysis (66%) with a median time on dialysis of 61 (min-max, 28-161) days. Most participants had a history of hypertension (80.3%), and 48% had diabetes mellitus. The median body mass index (BMI) was 24.1 (min-max, 15.6-54.2) kg/m2.
Table 1.
Participant Characteristics
| N | 146 |
|---|---|
| Male | 77 (52.7%) |
| Age, y | 58.1 (46, 68) |
| African American | 64 (43.8%) |
| Hispanic | 3 (2%) |
| Dialysis vintage, d | 61 (51, 73) |
| Dialysis modality | |
| Hemodialysis | 97 (66%) |
| Peritoneal dialysis | 49 (34%) |
| Peritoneal dialysis Kt/V | 2.3 ± 0.6 |
| Hemodialysis Kt/V | 1.37 ± 0.3 |
| Dry weight (kg) | 72.7 (60, 82) |
| Body mass index, kg/m2 | 24.1 (21.6, 28.6) |
| Clinical characteristics | |
| Diabetes mellitus | 70 (48%) |
| Coronary artery disease | 17 (11.6%) |
| Congestive heart failure | 40 (27.4%) |
| Hypertension | 119 (81.5%) |
| Laboratory parameters | |
| Albumin (mg/dL) (n = 133) | 3.5 ± 0.5 |
| Hematocrit (mg/dL) | 33.2 ± 4.9 |
Median (25th, 75th percentile) reported for age, dialysis vintage, dry weight, and body mass index.
Nutrition Components Assessed by BFFQ-Restricted and Full Diaries
Appendix B (available online at http://dx.doi.org/10.1053/j.jrn.2013.12.004) shows the foods most frequently included in the 3-day food diaries that are not included in the BFFQ. Of the items not included in the BFFQ, only coffee, tea, crackers, and diet soda were reported by more than 20% of participants. Table 2 shows the mean estimated dietary intakes of energy, protein, carbohydrate, and fat. Full diary intakes were normally distributed; thus, diaries were not log-transformed before planned analysis. The BFFQ-restricted estimates for energy, carbohydrate, and fat intakes, respectively, were 87%, 83%, and 90% of the unrestricted estimates (P =.0001 for each comparison). Estimates of protein intake were not statistically different by BFFQ-restricted and full diary assessment (63.1 ± 28.5 vs. 64.1 ± 21.4 g, respectively, P =.60).
Table 2.
Components of Nutrition
| Intake | Full 3-d Diary Average | BFFQ-Restricted Diary Average | Difference (95% CI) | P |
|---|---|---|---|---|
| Energy, kcal | 1,510.3 (510.4) | 1,325.0 (545.1) | 177.9 (116.6-239.1) | <.0001 |
| Protein, g | 64.1 (21.3) | 63.1 (28.5) | 1.0 (−2.8 to 4.8) | .60 |
| Fat, g | 56.4 (21.6) | 50.1 (24.1) | 6.0 (3.0-9.0) | <.0001 |
| Carbohydrate, g | 190.4 (72.7) | 156.8 (78.2) | 32.5 (23.6-41.4) | <.0001 |
BFFQ, Brief Food Frequency Questionnaire; CI, confidence interval.
The average difference in intakes between the BFFQ-restricted diary intakes and the full 3-day diary intakes were statistically significant with the exception of protein. The average difference between the full 3-day diary and BFFQ-restricted diary intake for energy was 177.9 kcal (95% confidence interval [CI] 116.6-239.1 kcal), for carbohydrate it was 32.5 g (95% CI 23.6-41.4 g), for fat it was 6.0 g (95% CI 3.0-9.0 g), and for protein it was 1.0 g (95% CI −2.8 to 4.8 g). Although the BFFQ-restricted diary intakes underestimated intakes derived from the full diaries, there was reasonable correlation between the 2 estimates.
Modeling of Full 3-Day Diary Intake on the Basis of BFFQ-Restricted Estimates
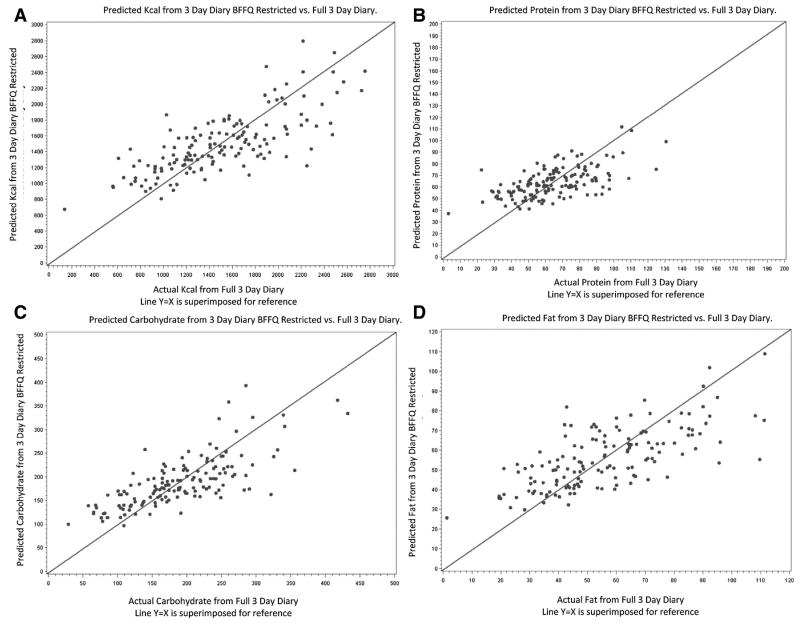
We included age, sex, race, and diabetes as covariates in each of the 4 models examining the association of BFFQ-restricted intakes with unrestricted intakes. Although women had lower intake than men on average, sex was not significantly associated with full intake after adjusting for BFFQ-estimated intake, and the r2 values of the models were not substantively improved with addition of sex or any other covariate. Moreover, there were no significant interactions between covariates and BFFQ-estimated intake, suggesting that in no instance did age, sex, diabetes, or race materially modify the BFFQ-restricted intake–unrestricted intake relation. Thus, the covariates were removed and models were simplified to an intercept and the BFFQ-restricted component estimates. Table 3 shows the final equations deriving complete 3-day diary intakes from the subset of foods included in the BFFQ on the basis of the regression term estimates. Figure 1, A-D shows the predicted versus actual full intake for energy, protein, carbohydrates, and fat. For each macronutrient, particularly protein, there was a tendency for greater underestimation of intake at extremely high levels.
Table 3.
Final BFFQ-Restricted Calibrated Equations
| Full Nutrition Components |
BFFQ Equations for Estimating 3-d Diary Average |
|---|---|
| kcal | 108.26 + 0.81(BFFQ kcal) |
| Protein | 11.37 + 0.81(BFFQ protein) |
| Carbohydrate | 4.05 + 0.81(BFFQ carbohydrate) |
| Fat | 6.40 + 0.78(BFFQ fat) |
BFFQ, Brief Food Frequency Questionnaire.
Figure 1.
(A) Predicted kilocalories from 3-day diary BFFQ-restricted vs. full 3-day diary. Actual kilocalories from full 3-day diary line Y = X is superimposed for reference. (B) Predicted protein from 3-day diary BFFQ-restricted vs. full 3-day diary. Actual protein from full 3-day diary line Y = X is superimposed for reference. (C) Predicted carbohydrate from 3-day diary BFFQ-restricted vs. full 3-day diary. Actual carbohydrate from full 3-day diary line Y = X is superimposed for reference. (D) Predicted fat from 3-day diary BFFQ-restricted vs. full 3-day diary. Actual fat from full 3-day diary line Y = X is superimposed for reference.
Discussion
We found that the BFFQ-restricted diaries captured approximately 87% of total energy, 83% of carbohydrate intake, 98% of protein intake, and 90% of fat intake reported in 3-day diaries. The BFFQ-restricted diaries underestimated intakes to a similar extent in younger and older, male and female, and Black and White participants. We found that simple equations can translate BFFQ-restricted intakes into estimates of complete 3-day food diary intake with reasonable accuracy.
On the basis of our findings, the BFFQ may be a useful tool for estimating nutritional intake among patients on dialysis. An FFQ for patients on dialysis has also been developed20 that focuses on inclusion of most food items reported in the 3-day food diaries of a cohort of dialysis patients from southern California. Indeed, the authors reported that the final Dialysis FFQ included approximately 90% of the dietary intake reported by the developmental cohort.20 It is encouraging that although the BFFQ is not tailored to patients with end-stage renal disease, the foods and beverages included on the BFFQ accounted for 87% of energy intake and 98% of protein intake in our cohort. Compared with the Dialysis FFQ, the BFFQ lacks specific information on dietary supplements commonly used among patients on dialysis. However, a potential advantage of using a generic instrument such as the BFFQ is, for example, the ability to compare intake across populations, comparing patients on dialysis to persons with normal kidney function or with mild to moderate chronic kidney disease.
The fact that the means of the protein estimates are similar, yet the correlation for protein is relatively low, could be explained by the large standard deviation, which suggests a higher variability in protein estimates. In this situation, estimates would be affected by the removal of a protein source or sources that were important for only a few individuals, which could alter the variability without changing the overall mean. Examination of the missing items supports this possibility. The most frequent items “missed” by the BFFQ were not major sources of protein (Appendix B, available online at http://dx.doi.org/10.1053/j.jrn.2013.12.004). However, there were some high-protein items reported by only a few individuals, such as cottage cheese, which was reported by 7 individuals (4.8%), and several unusual meat items such as venison, which was reported by even fewer participants.
Our study has some important limitations. First, because this study was based on the dietary intake of patients from a single region, some variability in intake estimates from other geographic locations can be expected. Validation of the BFFQ against 3-day diary records in a new cohort will be necessary to determine whether the promising results we obtained can be replicated. Second, 3-day diary records were used as the gold standard to calibrate the BFFQ, and it is entirely possible that some foods that are part of patients’ usual intake over a longer period of time were not consumed over the 3-day study period. Nevertheless, 3-day diaries were also used as the basis of development of the Dialysis FFQ,20 and subsequent validation in a new cohort should also address this possibility. Furthermore, estimates produced using the equations we have developed should serve to rank individuals against others within a population.
The BFFQ was administered to participants in the nutrition substudy of the Comprehensive Dialysis Study, which also includes serial measurements of laboratory markers of nutritional status and inflammation.29 The results we have generated in this calibration study suggest that the BFFQ provides an efficient tool for examining relations among dietary intake, inflammatory markers, and clinical outcomes in the Comprehensive Dialysis Study with calibration. Our findings indicate that the BFFQ, in conjunction with simple calibration equations, can be used to approximate total intake from 3-day food intake diaries in patients receiving dialysis.
Practical Application
Accurately estimating dietary intake—whether with 3-day food diary records, 24-hour recall, or FFQs—is particularly challenging in patients with chronic diseases. Energy and macronutrient estimates by BFFQ are lower than estimates from 3-day food diaries, but simple calibration equations can be used to approximate total intake from BFFQ responses that are more time-efficient to obtain.
Supplementary Material
Acknowledgments
This project is sponsored by the USRDS Nutrition Special Studies Center (N01-DK-7-0005). The interpretation and reporting of the data presented here are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government.
Support: Supported by contract N01-DK-7-0005 from the National Institutes of Health, National Institute of Diabetes, Digestive and Kidney Disease. C.D. was supported by grant number 1-IK2-CX000527-01A2 from the Department of Veteran’s Affairs.
Footnotes
Financial Disclosure: T.B. is co-owner of Nutritionquest, the company responsible for the development of the Brief 2000 FFQ. All other authors declare that they have no relevant financial interests.
Appendix
Supplementary data associated with this article can be found in the online version at http://dx.doi.org/10.1053/j.jrn.2013.12.004.
References
- 1.Dwyer JT, Larive B, Leung J, et al. Nutritional status affects quality of life in Hemodialysis (HEMO) Study patients at baseline. J Ren Nutr. 2002;12:213–223. doi: 10.1053/jren.2002.35297. [DOI] [PubMed] [Google Scholar]
- 2.Araujo IC, Kamimura MA, Draibe SA, et al. Nutritional parameters and mortality in incident hemodialysis patients. J Ren Nutr. 2006;16:27–35. doi: 10.1053/j.jrn.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Allen KL, Miskulin D, Yan G, et al. Association of nutritional markers with physical and mental health status in prevalent hemodialysis patients from the HEMO study. J Ren Nutr. 2002;12:160–169. doi: 10.1053/jren.2002.33512. [DOI] [PubMed] [Google Scholar]
- 4.Burrowes JD, Larive B, Cockram DB, et al. Effects of dietary intake, appetite, and eating habits on dialysis and non-dialysis treatment days in hemodialysis patients: cross-sectional results from the HEMO study. J Ren Nutr. 2003;13:191–198. doi: 10.1016/s1051-2276(03)00069-4. [DOI] [PubMed] [Google Scholar]
- 5.Bossola M, Muscaritoli M, Tazza L, et al. Variables associated with reduced dietary intake in hemodialysis patients. J Ren Nutr. 2005;15:244–252. doi: 10.1053/j.jrn.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 6.Campbell KL, Ash S, Zabel R, McFarlane C, Juffs P, Bauer JD. Implementation of standardized nutrition guidelines by renal dietitians is associated with improved nutrition status. J Ren Nutr. 2009;19:136–144. doi: 10.1053/j.jrn.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Cantwell MM, Millen AE, Carroll R, et al. A debriefing session with a nutritionist can improve dietary assessment using food diaries. J Nutr. 2006;136:440–445. doi: 10.1093/jn/136.2.440. [DOI] [PubMed] [Google Scholar]
- 8.Brunner E, Stallone D, Juneja M, Bingham S, Marmot M. Dietary assessment in Whitehall II: comparison of 7 d diet diary and food-frequency questionnaire and validity against biomarkers. Br J Nutr. 2001;86:405–414. doi: 10.1079/bjn2001414. [DOI] [PubMed] [Google Scholar]
- 9.Willett WC, Sampson L, Stampfer MJ, et al. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol. 1985;122:51–65. doi: 10.1093/oxfordjournals.aje.a114086. [DOI] [PubMed] [Google Scholar]
- 10.Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124:453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 11.Block G, Coyle LM, Hartman AM, Scoppa SM. Revision of dietary analysis software for the Health Habits and History Questionnaire. Am J Epidemiol. 1994;139:1190–1196. doi: 10.1093/oxfordjournals.aje.a116965. [DOI] [PubMed] [Google Scholar]
- 12.Mares-Perlman JA, Klein BE, Klein R, Ritter LL, Fisher MR, Freudenheim JL. A diet history questionnaire ranks nutrient intakes in middle-aged and older men and women similarly to multiple food records. J Nutr. 1993;123:489–501. doi: 10.1093/jn/123.3.489. [DOI] [PubMed] [Google Scholar]
- 13.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 14.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: the Eating at America’s Table Study. Am J Epidemiol. 2001;154:1089–1099. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 15.Boucher B, Cotterchio M, Kreiger N, Nadalin V, Block T, Block G. Validity and reliability of the Block98 food-frequency questionnaire in a sample of Canadian women. Public Health Nutr. 2006;9:84–93. doi: 10.1079/phn2005763. [DOI] [PubMed] [Google Scholar]
- 16.Johnson BA, Herring AH, Ibrahim JG, Siega-Riz AM. Structured measurement error in nutritional epidemiology: applications in the Pregnancy, Infection, and Nutrition (PIN) Study. J Am Stat Assoc. 2007;102:856–866. doi: 10.1198/016214506000000771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bingham SA, Gill C, Welch A, et al. Comparison of dietary assessment methods in nutritional epidemiology: weighed records v. 24 h recalls, food-frequency questionnaires and estimated-diet records. Br J Nutr. 1994;72:619–643. doi: 10.1079/bjn19940064. [DOI] [PubMed] [Google Scholar]
- 18.Schroder H, Covas MI, Marrugat J, et al. Use of a three-day estimated food record, a 72-hour recall and a food-frequency questionnaire for dietary assessment in a Mediterranean Spanish population. Clin Nutr. 2001;20:429–437. doi: 10.1054/clnu.2001.0460. [DOI] [PubMed] [Google Scholar]
- 19.Yang YJ, Kim MK, Hwang SH, Ahn Y, Shim JE, Kim DH. Relative validities of 3-day food records and the food frequency questionnaire. Nutr Res Pract. 2010;4:142–148. doi: 10.4162/nrp.2010.4.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalantar-Zadeh K, Kovesdy CP, Bross R, et al. Design and development of a dialysis food frequency questionnaire. J Ren Nutr. 2011;21:257–262. doi: 10.1053/j.jrn.2010.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bross R, Noori N, Kovesdy CP, et al. Dietary assessment of individuals with chronic kidney disease. Semin Dial. 2010;23:359–364. doi: 10.1111/j.1525-139X.2010.00743.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Block G, Hartman AM, Naughton D. A reduced dietary questionnaire: development and validation. Epidemiology. 1990;1:58–64. doi: 10.1097/00001648-199001000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Kalantar-Zadeh K, Kopple JD, Deepak S, Block D, Block G. Food intake characteristics of hemodialysis patients as obtained by food frequency questionnaire. J Ren Nutr. 2002;12:17–31. doi: 10.1053/jren.2002.29598. [DOI] [PubMed] [Google Scholar]
- 24.Kutner NG, Clow PW, Zhang R, Aviles X. Association of fish intake and survival in a cohort of incident dialysis patients. Am J Kidney Dis. 2002;39:1018–1024. doi: 10.1053/ajkd.2002.32775. [DOI] [PubMed] [Google Scholar]
- 25.Subar AF, Kirkpatrick SI, Mittl B, et al. The Automated Self-Administered 24-hour dietary recall (ASA24): a resource for researchers, clinicians, and educators from the National Cancer Institute. J Acad Nutr Diet. 2012;112:1134–1137. doi: 10.1016/j.jand.2012.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Frankenfeld CL, Poudrier JK, Waters NM, Gillevet PM, Xu Y. Dietary intake measured from a self-administered, online 24-hour recall system compared with 4-day diet records in an adult US population. J Acad Nutr Diet. 2012;112:1642–1647. doi: 10.1016/j.jand.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 27.Jindal KK, Manuel A, Goldstein MB. Percent reduction in blood urea concentration during hemodialysis (PRU). A simple and accurate method to estimate Kt/V urea. ASAIO Trans. 1987;33:286–288. [PubMed] [Google Scholar]
- 28.Daugirdas JT. Rapid methods of estimating Kt/V: three formulas compared. ASAIO Trans. 1990;36:M362–M364. [PubMed] [Google Scholar]
- 29.Kutner NG, Johansen KL, Kaysen GA, et al. The comprehensive dialysis study (CDS): a USRDS special study. Clin J Am Soc Nephrol. 2009;4:645–650. doi: 10.2215/CJN.05721108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.