Abstract
Objectives
Assess the influence of sex and age on inpatient rehabilitation outcomes in a large national sample of older adults with TBI.
Design
Prospective case series.
Setting
848 inpatient rehabilitation facilities that subscribe to the UDSMR.
Participants
Patients (n = 18,413) aged 65 years and older admitted for inpatient rehabilitation following TBI from 2005 through 2007.
Intervention
None.
Main Outcome Measures
Rehabilitation length of stay, discharge FIM motor and cognitive ratings, discharge setting, and scheduled home health services at discharge.
Results
Mean age of the sample was 79±7 years and 47% were women. In multi-variable models, higher age was associated with shorter lengths of stay (p < .001), lower discharge FIM motor and cognitive ratings (p < .001), and greater odds of home health services at discharge (p < .001). Women demonstrated shorter lengths of stay (p = .006) and greater odds of being scheduled for home health services at discharge (p < .001) than men. The sex-by-age interaction term was not significant in any outcome model. Sex differences and trends were consistent across the entire age range of the sample.
Conclusions
Sex and age patterns in rehabilitation outcomes among older adults with TBI varied by outcome. The current findings related to rehabilitation length of stay may be helpful for facility-level resource planning. Additional studies are warranted to identify the factors associated with returning to home and to assess the long-term benefits of combined inpatient rehabilitation and home health services for older adults with TBI.
Keywords: aged, brain injuries, rehabilitation
TBI among older adults is a significant public health concern in terms of both patient wellbeing and healthcare system costs. Persons aged 65 years or older are at greater risk of being hospitalized with a TBI than any other age group.1 Falls are responsible for more than half of all TBI-related emergency department visits, hospitalizations, and deaths among adults aged 65 years or older.2 Moreover, the risk of fall-related TBI increases substantially for each 10-year age increase over the age of 65.3 Epidemiologic studies show that both the total number and percentage of older adults with TBI have increased over the past few decades.1,3,4
TBI often leads to permanent impairments in physical, cognitive, behavioral, and/or emotional functioning.5 Many older adults with enduring physical or cognitive impairments following acute hospitalization for a TBI are transferred to inpatient rehabilitation.6 A previous study 7 concluded that age does not affect the degree of functional improvement obtained during inpatient rehabilitation. Other studies, however, have shown that older persons with TBI experience poorer rehabilitation outcomes than younger persons.8,9
Like age, sex is also an established risk factor for TBI. Men are consistently at higher risk of TBI than women, with ratios greater than 2:1 in many age groups. However, the incidence rates among older adults are about the same for men and women.10,11 Prior studies have included sex as an independent predictor of TBI outcomes in acute hospitalization,12,13 inpatient rehabilitation,14,15 and longer-term community settings.16 While the results of these studies are mixed, women achieved better outcomes than men on several short-term measures. However, no study focused exclusively on adults aged 65 years and older.
TBI rehabilitation is a rapidly growing area of research.17,18 Despite the potential importance of age and sex on TBI outcomes, little is known about the influence of sex specifically among older adults who have sustained a TBI. Thompson and colleagues19 claim that there “is a significant gap in the [aging / TBI] literature.” Many factors that are associated with recovery of function following injury, including sex, remain “understudied” in older adults with TBI.19 The purpose of the current study was to assess the independent and interactive effects of sex and age on inpatient rehabilitation outcomes in a large national sample of adults aged 65 years and older with TBI. To our knowledge, this is the first study to examine the interactive effects of sex and age on rehabilitation outcomes in older adults with TBI.
There is no consensus on sex-based differences in TBI outcomes in studies with mostly younger persons and there is no precedent in studies with older adults exclusively. However, given that women, in general, demonstrate greater resilience and longevity than men and that age is an equalizer for many health disparities, we hypothesized that 1) older women would experience better rehabilitation outcomes overall compared to older men, and 2) the magnitude of male-female differences would diminish with increasing age. Information from this study may be useful for estimating responses to rehabilitation and resource needs for older adults with TBI.
METHODS
Data Source
Data were obtained from the UDSMR.20 Admission and discharge information was collected from patient medical records contained within the IRF-PAI.21
Study Sample
The inclusion criteria for this study included patients who were 1) being admitted for initial inpatient rehabilitation services following TBI, 2) aged 65 years or older at the time of admission, 3) living at home prior to injury, and 4) discharged from rehabilitation in 2005 through 2007. Qualifying etiology included traumatic brain dysfunction coded with UDSMR Impairment Group Codes 02.21 (Traumatic, Open Injury) and 02.22 (Traumatic, Closed Injury).21 There were 19,411 patients in the initial sample. Exclusion criteria were 1) duration from injury onset to admission > 365 days (n = 300), 2) program interruption for readmission to acute care (n = 236), and 3) length of stay < 3 days or > 100 days (n = 462). The final sample contained 18,413 patient records from 848 inpatient rehabilitation facilities across the United States. Compared to the final sample, excluded patients were less likely to be women, to have a closed head injury, and to be discharged home following rehabilitation. In addition, excluded patients showed longer duration from injury onset to admission, shorter lengths of stay in rehabilitation, and lower functional status at both admission and discharge.
Variables
Demographic information
Age was recorded in years. The age variable was centered at 65 years (centered age = patient age – 65) for entry in the multi-variable models in order to facilitate interpretation and accuracy of the regression coefficients.22 Sex and marital status (married vs. not married) were coded dichotomously. Self-reported race/ethnicity was coded as black, Hispanic, white, and other categories. ‘Other’ included Asian, Hawaiian / Pacific Islander, Native American / Alaskan, or unspecified. The race/ethnic groups were dummy coded (0,1: reference = white) for entry in the regression models.
Living situation and home health
Self-reported living arrangement (alone vs. not alone) and setting (home vs. not home) were coded dichotomously and recorded for both pre- and post-hospitalization. As described above, living at home pre-hospitalization was an inclusion criterion for this study. A dichotomous (yes vs. no) variable was also coded to identify patients discharged home who were scheduled for continued services through a home health agency.
Admission delay and length of stay
Admission delay refers to the time between injury onset and admission to inpatient rehabilitation. Length of stay refers to the time from rehabilitation admission to discharge. Both were measured in days.
Comorbidities and injury type
A summary score was calculated for the total number of additional health conditions (range: 0–10) beyond the primary diagnosis: all ICD-9 codes (maximum of 10) recorded in each patient’s medical record. Skull integrity was recorded dichotomously (open vs. closed head injury).
Functional status
Functional status data were obtained using the FIM instrument at admission and discharge. The FIM instrument contains 18 items covering six domains of functioning: self-care (activities of daily living), sphincter control, transfers, locomotion, communication, and social cognition. Each item is scored on a on a scale from 1 (complete dependence) to 7 (complete independence); i.e., higher scores represent better functioning/greater independence. The FIM motor subscale contains 13 items (range of possible scores: 13–91) and the FIM cognitive subscale contains 5 items (range of possible scores: 5–35). The reliability, validity, and responsiveness of the FIM instrument are well documented.23
Efficiency
Rehabilitation efficiency was defined as the average functional improvement per day. It is calculated by subtracting admission FIM total from discharge FIM total to obtain FIM total gain and then dividing this value by length of stay in days.
Data Analysis
Univariate differences between older women and men were tabulated for all variables. Independent t-tests were used for numerical variables, and chi-square tests for categorical data. Multiple linear regression models were used to assess the independent effects of sociodemographic, case complexity, and functional status factors on length of stay, discharge FIM motor ratings, and discharge FIM cognitive ratings. Logistic regression was performed to examine the effects of these factors on discharge setting (not home vs. home) and being scheduled to receive home health services (no vs. yes). An interaction variable linking sex with age was also included in all five outcome models. The interaction variable was created by dummy coding the sex variable (reference category = men) and then multiplying this by the value of the (numerical) age variable. All variables were entered as a single block. The lists of variables included in each model are displayed in the two consolidated regression tables (Tables 2 and 3). Lastly, we calculated and graphed expected values for each outcome by sex and age. For these calculations, the most likely sex-specific values (group means or modes) for all variables in the models were multiplied by the respective regression coefficients. Alpha was set to 0.05. SPSS version14 softwarea was used for all statistical analysis.
Table 2.
Multiple linear regressions of rehabilitation outcomes on demographic and clinical factors.
| LOS
|
Discharge FIM motor
|
Discharge FIM cognitive
|
||||
|---|---|---|---|---|---|---|
| b (se) | p-value | b (se) | p-value | b (se) | p-value | |
| Women | −0.66 (0.24) | .006 | −0.51 (0.42) | .223 | 0.05 (0.15) | .740 |
| Age, years | −0.07 (0.01) | <.001 | −0.27 (0.02) | <.001 | −0.05 (0.01) | <.001 |
| White | ref | ref | ref | |||
| Black | −0.18 (0.25) | .472 | −2.45 (0.44) | <.001 | −0.86 (0.16) | <.001 |
| Hispanic | −0.79 (0.27) | .003 | −0.54 (0.48) | .253 | −0.20 (0.17) | .253 |
| Other | −0.15 (0.28) | .576 | 0.64 (0.48) | .187 | −0.60 (0.18) | .001 |
| Married | −0.70 (0.12) | <.001 | −0.07 (0.20) | .724 | 0.07 (0.08) | .344 |
| Closed injury | 0.75 (0.34) | .027 | −0.39 (0.60) | .512 | −0.29 (0.22) | .188 |
| Admission delay, days | 0.04 (0.00) | <.001 | −0.06 (0.00) | <.001 | −0.01 (0.00) | <.001 |
| Comorbidities, count | 0.19 (0.02) | <.001 | −0.16 (0.04) | <.001 | 0.01 (0.01) | .671 |
| FIM motor: admit | −0.25 (0.00) | <.001 | 0.88 (0.01) | <.001 | 0.07 (0.00) | <.001 |
| FIM cognitive: admit | −0.09 (0.01) | <.001 | 0.22 (0.01) | <.001 | 0.69 (0.01) | <.001 |
| Length of stay, days | 0.47 (0.01) | <.001 | 0.14 (0.00) | <.001 | ||
| Women * Age | 0.03 (0.01) | .064 | 0.05 (0.03) | .059 | 0.00 (0.01) | .663 |
| Adjusted R square | 25% | 47% | 60% | |||
b = regression coefficient, se = standard error. Women * Age = interaction term. Note: Age variable is centered at 65 years.
Table 3.
Multi-variable logistic regressions of discharge setting (not home [0] vs. home [1]) and scheduled for home healthcare (no [0] vs. yes [1]) on demographic and clinical factors.
| Home discharge
|
Home healthcare
|
|||
|---|---|---|---|---|
| OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Women | 1.15 (0.97, 1.37) | .113 | 1.51 (1.28, 1.78) | <.001 |
| Age, years | 1.00 (0.99, 1.01) | .835 | 1.05 (1.04, 1.06) | <.001 |
| White | ref | ref | ||
| Black | 1.78 (1.48, 2.14) | <.001 | 1.25 (1.04, 1.50) | .019 |
| Hispanic | 1.82 (1.49, 2.24) | <.001 | 0.95 (0.78, 1.15) | .594 |
| Other | 1.74 (1.41, 2.16) | <.001 | 0.82 (0.68, 0.99) | .035 |
| Married | 1.48 (1.34, 1.64) | <.001 | 0.82 (0.74, 0.91) | <.001 |
| Live alone pre-injury | 0.42 (0.38, 0.46) | <.001 | 1.14 (1.02, 1.27) | .024 |
| Closed injury | 1.19 (0.93, 1.52) | .174 | 0.92 (0.71, 1.18) | .492 |
| Admission delay, days | 1.01 (1.00, 1.01) | <.001 | 1.00 (1.00, 1.00) | .569 |
| Comorbidities, count | 0.99 (0.98, 1.01) | .387 | 1.01 (1.00, 1.03) | .165 |
| FIM motor: discharge | 1.09 (1.08, 1.09) | <.001 | 0.95 (0.95, 0.96) | <.001 |
| FIM cognitive: discharge | 1.05 (1.04, 1.05) | <.001 | 1.03 (1.02, 1.04) | <.001 |
| Length of stay, days | 1.00 (1.00, 1.01) | .491 | 1.02 (1.01, 1.03) | <.001 |
| Women * Age | 1.00 (0.99, 1.01) | .877 | 0.99 (0.98, 1.00) | .136 |
| Nagelkerke R square | 44% | 15% | ||
OR = odds ratio, CI = confidence interval. Women * Age = interaction term. Note: Age variable is centered at 65 years.
RESULTS
Sample Characteristics
Women represented 47% of the 18,413 older adults (79±7 years) in our sample who received inpatient rehabilitation following TBI from 2005 through 2007. The sample was predominantly white, slightly more than half were married, and approximately one-third was living alone at the time of the injury. More than 97% of patients experienced closed head injuries and the mean rehabilitation admission delay was 13 days. On average, patients had 8 comorbid conditions and admission FIM total scores of 56. Following a mean length of stay of nearly 15 days and average FIM total gain (efficiency) of approximately 2 points per day, discharge FIM total scores averaged 81 and nearly two-thirds of patients were discharged home. Table 1 displays summaries of all variables for the total sample and for men and women.
Table 1.
Patient characteristics and outcomes for TBI rehabilitation by sex.
| Total | Men | Women | p-value | |
|---|---|---|---|---|
| N | 18,413 | 9,763 | 8,650 | |
| Age, yrs | 79.19 (7.39) | 78.29 (7.35) | 80.22 (7.30) | <.001 |
| Race/ethnicity | .002 | |||
| White | 86.5% | 85.7% | 87.5% | |
| Black | 5.1% | 5.6% | 4.5% | |
| Hispanic | 4.2% | 4.4% | 4.1% | |
| Other | 4.1% | 4.3% | 3.9% | |
| Married | 51.6% | 67.6% | 33.6% | <.001 |
| Living alone pre injury | 32.5% | 22.8% | 43.4% | <.001 |
| Closed injury | 97.4% | 97.2% | 97.7% | .058 |
| Admission delay, days | 12.98 (19.43) | 14.66 (21.38) | 11.08 (16.77) | <.001 |
| Comorbidities, number | 8.02 (2.43) | 8.02 (2.45) | 8.01 (2.41) | .661 |
| FIM motor: admit | 36.77 (13.49) | 36.05 (13.87) | 37.58 (13.01) | <.001 |
| FIM cognitive: admit | 18.94 (7.77) | 18.08 (7.78) | 19.90 (7.66) | <.001 |
| FIM total: admit | 55.71 (19.04) | 54.13 (19.47) | 57.49 (18.37) | <.001 |
| Length of stay, days | 14.92 (8.36) | 15.30 (8.96) | 14.49 (7.60) | <.001 |
| FIM motor: discharge | 57.76 (17.51) | 57.12 (18.12) | 58.48 (16.77) | <.001 |
| FIM cognitive: discharge | 23.28 (7.35) | 22.67 (7.47) | 23.98 (7.15) | <.001 |
| FIM total: discharge | 81.04 (22.87) | 79.78 (23.62) | 82.46 (21.90) | <.001 |
| Efficiency | 1.96 (1.69) | 1.96 (1.77) | 1.96 (1.58) | .996 |
| Discharged home | 65.6% | 65.5% | 65.7% | .729 |
| Scheduled for home healthcare* | 60.9% | 56.0% | 66.3% | <.001 |
Values are mean (sd) or percentage.
Percentages are based on the 12,082 patients who were discharged home.
Univariate Analyses of Sex Differences
Sociodemographic variables
Significant sex differences were observed in age, race, marital status, and pre-morbid living situation. Overall, women were approximately two years older than men and a slightly higher percentage of women were white. Women were also half as likely to be married and nearly twice as likely to be living alone prior to their injury.
Case complexity
Only rehabilitation admission delay reached statistical significance; on average, women were admitted to rehabilitation following TBI nearly three days sooner than men. No sex differences in injury type or number of comorbidities were observed.
Functional status, length of stay, and discharge situation
Women displayed slightly higher function on motor and cognitive tasks at both admission and discharge, they were discharged nearly one day earlier than men, and they were more likely to be scheduled for post-discharge home healthcare. However, there was no sex difference in rehabilitation efficiency or in the percentage of women and men discharged home.
Multi-Variable Models
The multi-variable models are shown in Tables 2 and 3. The sex-by-age interaction variable did not reach statistical significance in any of the outcome models.
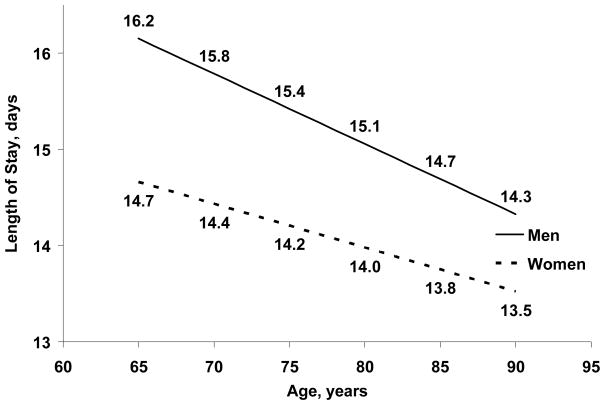
Length of stay
While controlling for sociodemographic information, case complexity factors, and admission functional status, both sex (p = .006) and age (p < .001) were significantly related to rehabilitation length of stay. Length of stay was approximately two-thirds of a day (b = −0.66) shorter for women than for men. The age coefficient (b = −0.07) suggests that each 10 year increase in age was also associated with approximately two-thirds of a day shorter stay. Figure 1 displays projected lengths of stay for both women and men by age, adjusted for all variables listed in Table 2.
Figure 1.
Predicted values for length of stay by age and sex adjusted for all other variables listed in Table 2.
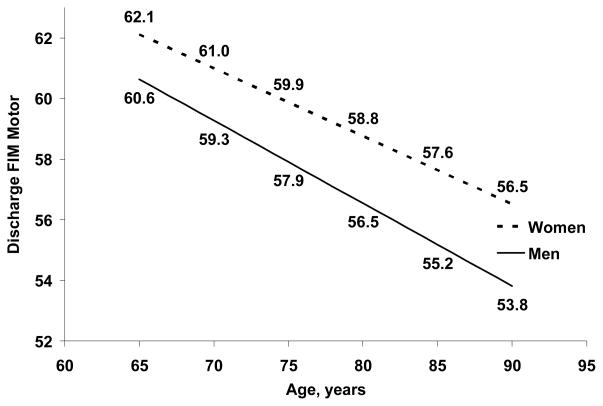
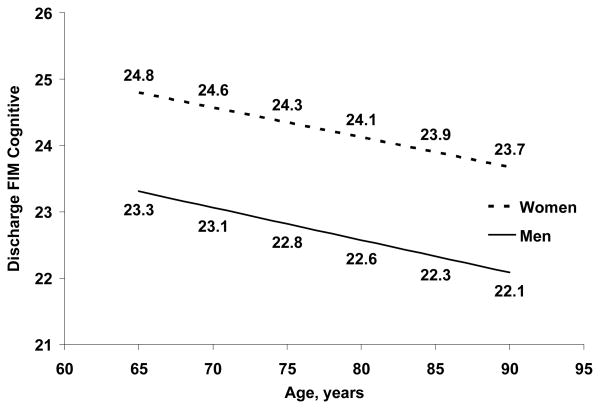
Functional status
After controlling for sociodemographic information, case complexity, admission functional status, and length of stay, sex was not significantly associated with either FIM motor (p = .223) or FIM cognitive (p = .740) ratings at discharge. Age was significantly related to both FIM subscales (p < .001). The main effect for age suggests that discharge FIM motor (b = −0.27) decreases nearly 3 points and discharge FIM cognitive (b = −0.05) decreases one-half point with a 10 year increase in age. Figures 2 and 3 highlight the significant main effects of age and the trends for sex differences and provide FIM subscale ratings adjusted for all variables listed in Table 2.
Figure 2.
Predicted values for discharge FIM motor ratings by age and sex adjusted for all other variables listed in Table 2.
Figure 3.
Predicted values for discharge FIM cognitive ratings by age and sex adjusted for all other variables listed in Table 2.
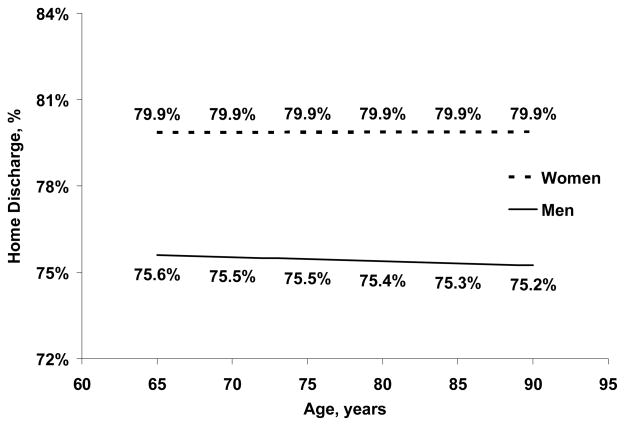
Discharge situation
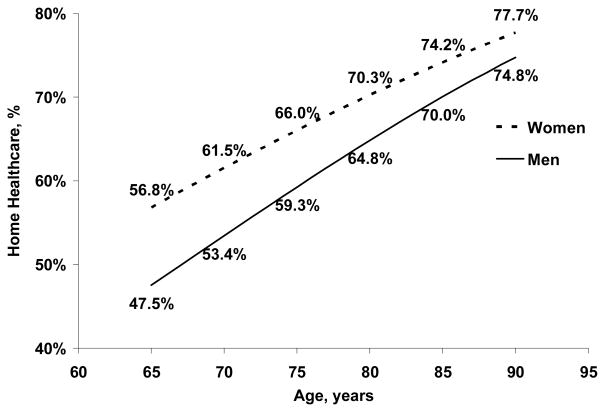
After controlling for sociodemographic information, including living situation prior to admission, case complexity factors, and discharge functional status, neither sex (p = .113) nor age (p = .835) was related to likelihood of home discharge. Conversely, among those discharged home, both variables (p < .001) were associated with probability of being scheduled for home healthcare services following discharge. Women demonstrated approximately 50% greater odds of being scheduled for home health services than men (OR = 1.51). Using the coefficient for the age effect (OR for single year = 1.05) to calculate the odds ratio for a 10-year age difference, suggests that a 75 year old had a 61% greater odds of scheduled home health services than a 65 year old. Figures 4 and 5 display percentages of home discharge and home healthcare, respectively, for women and men by age, while controlling for all variables listed in Table 3.
Figure 4.
Predicted percentages of patients discharged home by age and sex adjusted for all other variables listed in Table 3.
Figure 5.
Predicted percentages of home-discharged patients scheduled to receive home healthcare services by age and sex adjusted for all other variables listed in Table 3.
DISCUSSION
Few studies have examined older adults with TBI exclusively19 and relatively little is known regarding the differences within and between groups of older women and men.24 This study provides a broad snapshot of admission characteristics and outcomes for adults aged 65 years and older admitted to inpatient rehabilitation following TBI, and it highlights the influence of sex and age on these latter measures. We hypothesized that women would generally fare better than men and that the sex advantage would be moderated at older ages. Multi-variable analyses showed that sex differences were not uniform across rehabilitation outcomes. Specifically, women experienced shorter stays in rehabilitation and were more likely to be scheduled for home health services at discharge than men, but functional status and discharge setting did not significantly differ by sex. In addition, these sex differences and trends were not significantly moderated by patient age.
On average these older adults with TBI stayed in inpatient rehabilitation for just over two weeks. Two previous studies, involving TBI Model Systems subjects, reported longer lengths of stay (mean of approximately 20 days). In contrast to our sample, those studies included patients of all ages (means = 38 and 52 years) and larger proportions were men (> 70% in both studies).15,25 A relatively older study using TBI Model Systems data showed that those 55 years and older stayed in inpatient rehabilitation almost twice as long as those younger than 55 years (mean 56 days in the older compared to 31 days in the younger group).9 It should be noted that all three prior studies used data that preceded the PPS for inpatient rehabilitation, whereas the current study sample was admitted entirely in the PPS era. Introduction of the PPS likely had a substantial influence on TBI rehabilitation length of stay.25 None of these prior studies investigated outcome differences by sex.
Both sex and age were significant factors in the amount of time our sample of older adults with TBI spent in rehabilitation (Table 2). A prior study15 using a similar multiple linear regression analysis, but in a younger sample with complicated mild TBI, yielded no significant relationship between sex and rehabilitation length of stay. The authors of that study did report a significant relationship between age and rehabilitation length of stay, but regression coefficients were not provided. Figure 1 displays the main effects of sex and age on length of stay for the current study and converts the regression statistics to clinically-relevant values.
While the sex differences in length of stay may seem trivial at the individual level, these differences can have substantial implications at the facility and national levels. The current sample contained comparable numbers of women and men; approximately 9,000 each. Multiplying these numbers by the predicted mean difference of two-thirds of a day translates to 5,940 more days that men spent in rehabilitation than women, over the 3 years included in this study. Although sex is not a factor in the current prospective payment environment, it is reasonable to assume that over time sex may impact facility resource and staffing needs associated with caring for older adults with TBI.
Age was significantly related to both FIM motor and cognitive subscales at discharge; however, the implications of these relationships (b = −0.27 and b = −0.05, respectively) are not clinically meaningful. The impact of age on various health and function outcomes following TBI has been addressed in numerous studies. Reeder et al.7 found that after controlling for injury etiology, injury severity, and demographic information, age was not a significant predictor of inpatient rehabilitation functional outcomes. On the other hand, Cifu et al.9 showed that older persons with TBI had significantly longer rehabilitation lengths of stay, higher total rehabilitation charges, and a lower rate of functional change, with no statistically significant differences in rehabilitation discharge disposition. Similarly, Frankel et al.8 found that older rehabilitation patients with TBI progressed with less efficiency on the Disability Rating Scale and FIM instrument. Older age also has an impact on longer-term outcomes after rehabilitation,26 as well as on decline over time post-injury.27,28 Hammond and colleagues 29 reported that age was predictive of improvement on the FIM items of comprehension and expression from year 1 to year 5 post-injury, but not predictive of decline in these items, nor was age predictive of positive or negative changes in memory and problem solving or social interaction.
Women exhibited higher motor and cognitive functioning than men at both admission and discharge (Table 1). However, in the multi-variable models for functional status at discharge, sex was not a significant factor when controlling for sociodemographic, injury complexity, functional status at admission, and length of stay variables (Table 2). In addition, women and men made similar functional gains during their inpatient rehabilitation stay. Thus, from a functional independence perspective, it is reasonable to conclude that the response to rehabilitation was similar among older women and men with TBI. The mean functional improvement (efficiency) observed in the current study was 1.96 FIM points per day, which is similar to a previously reported value in a study of younger and predominately male TBI patients (median = 1.98 FIM points per day).25
Prior studies addressing sex effects on TBI outcomes have yielded mixed results across a broad range of measures. Kraus et al.12 reported women to have higher mortality rates and to be more severely disabled than men 18 months post injury. Additionally, a meta-analysis of 8 TBI studies concluded that women did worse than men on 85% of outcome measures.24 Outcomes included length of post-traumatic amnesia, number of postconcussive symptoms, and the development of new psychiatric symptoms. Conversely, Slewa-Younan et al.13 found that women aged 50 years and younger demonstrated better Glasgow Outcome Scale scores and shorter hospital lengths of stay than men. Ratcliff and colleagues16 evaluated sex differences in neuropsychologic performance one-year post-injury, using TBI Model Systems data. Women performed significantly better than men on tests of attention/working memory and language, while men outperformed women on visual tests. Given that these studies included relatively younger patients, these results may not be readily generalized to older persons19 such as the current sample.
Neither sex nor age was significantly related to home discharge. The strongest predictors of home discharge in the multi-variable logistic model were race/ethnicity, living situation prior to TBI, and marital status (Table 3). Using multinomial logistic regression, Chang and colleagues30 recently reported robust race/ethnicity differences in discharge disposition following inpatient rehabilitation among older adults with TBI; with institutionalization as the reference category, they showed that black patients, for example, had two times greater odds of going home and 78% lesser odds of going to assisted living compared to white patients. In the current study, all 3 non-white cohorts demonstrated greater odds of home discharge than whites. Married persons also showed greater odds of home discharge than unmarried ones. And, individuals living alone prior to their injury had lesser odds of home discharge than those living with someone. Interestingly, fewer women than men in our study were white or married and more were living alone pre-injury. Thus, given the independent relationships between these variables and home discharge, it would be logical to assume that women were less likely to go directly home following rehabilitation. However, there was no unadjusted (Table 1) or adjusted (Table 3) difference in the percentages of older women and men discharged home. Figure 4 does show a trend for a higher percentage of women discharged home compared to men across the entire age range of older adults.
Better family and/or social structure is believed to underlie race/ethnicity-based increases in likelihood of home discharge.31,32 Given that women were half as likely to be married and twice as likely to be living alone, the current data do not support this assumption for home discharge by sex among older adults with TBI. One plausible explanation for the current findings may be that women are more proficient than men at common activities of daily living such as managing finances, housework, cooking, and grocery shopping following TBI.33 Conversely, Whiteneck et al.34 showed that a higher proportion of women needed assistance with both physical and cognitive activities one year post injury compared to men, in a population-based TBI sample ranging in age from 16 to 96 years.
This study also included scheduled home health services as an inpatient rehabilitation outcome; i.e., a perceived need for continued services as determined by the rehabilitation team at discharge. More women were scheduled to receive home healthcare services than men, suggesting that sex either directly or indirectly (home circumstances) factored into the discharge planning process. In the multi-variable logistic regression model (Table 3), women demonstrated 51% greater odds of being scheduled for home healthcare services after discharge than men. Age was also positively associated with increased odds of scheduled home health services. The availability of home healthcare is likely allowing more people to be discharged home than would be possible without the availability of these services. Further study is needed to ascertain the set of factors and complex relationships underlying home discharge following inpatient rehabilitation among older adults with TBI. In addition, investigations on the benefits of combination therapy (inpatient rehabilitation + home health and/or outpatient services) in promoting independence and preventing secondary complications are needed to increase our understanding of the long-term recovery potential of older adults with TBI.
Study Limitations
The lack of information on the patients’ status and experiences prior to rehabilitation admission is a limitation of this study. Knowledge of factors such as pre-injury disability status as well as the original severity and cause of the injury would increase our understanding of the TBI recovery process and of sex differences among older adults. We controlled for admission functional status, number of comorbidities, and days from TBI onset to rehabilitation admission when assessing outcomes. However, it was not possible to evaluate the degree of recovery relative to pre-TBI functioning or the relationship between post-rehabilitation functional status and original injury severity. Also, we did not identify and include specific comorbidities that may have been disproportionately prevalent in women or men. Rather, we used an index of comorbidity. Lastly, we did not have a measure of extended-family or social support that might have helped to explain the apparent discrepancy between living situation (e.g. alone) and home discharge. A key strength of this study is the use of a large national sample, which provides sufficient statistical power and generalizable findings. In addition, this is the first investigation on the influence of sex and age, including a sex-by-age interaction term, on rehabilitation outcomes among older adults with TBI.
CONCLUSION
We identified certain differences in inpatient rehabilitation outcomes between older women and men with TBI. Age was significantly related to four of the five outcomes included in this study. Home discharge was the only outcome not significantly associated with age. The sex-by-age interaction term did not reach significance in any models, suggesting that the main effects for sex are consistent across the entire age range of older adults in our sample. Multivariable analyses showed that motor and cognitive functional status at discharge as well as odds of home discharge were similar for women and men, whereas length of stay and home healthcare outcomes differed by sex. Women were discharged from rehabilitation sooner than men and this information may improve resource planning at the facility level. Women were also more likely to be scheduled for home health services at discharge. Future studies should address the interconnected factors associated with returning home and the long-term benefits of combined inpatient rehabilitation and home health services for older adults with TBI.
Acknowledgments
Supported in part by the National Institute on Disability and Rehabilitation Research (grant no. H133G080163) and the National Institutes of Health, National Institute for Child Health and Human Development and National Institute for Neurological Disorders and Stroke (grant no. K12-H0055929).
List of Abbreviations
- FIM
FIM® instrument
- IRF-PAI
inpatient rehabilitation facility – patient assessment instrument
- PPS
prospective payment system
- TBI
traumatic brain injury
- UDSMR
Uniform Data System for Medical Rehabilitation
Footnotes
SPSS version 14.0; SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit on the authors or on any organization with which the authors are associated. Granger is employed by the State University of New York at Buffalo, which is affiliated with the Uniform Data System for Medical Rehabilitation. The Uniform Data System for Medical Rehabilitation owns the copyright and trademark for the FIM instrument.
References
- 1.Rutland-Brown W, Langlois JA, Thomas KE, Xi YL. Incidence of traumatic brain injury in the United States, 2003. J Head Trauma Rehabil. 2006;21(6):544–548. doi: 10.1097/00001199-200611000-00009. [DOI] [PubMed] [Google Scholar]
- 2.Langlois JA, Rutland-Brown W, Thomas KE. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2006. [Google Scholar]
- 3.Coronado VG, Thomas KE, Sattin RW, Johnson RL. The CDC traumatic brain injury surveillance system: characteristics of persons aged 65 years and older hospitalized with a TBI. J Head Trauma Rehabil. 2005;20(3):215–228. doi: 10.1097/00001199-200505000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Fletcher AE, Khalid S, Mallonee S. The epidemiology of severe traumatic brain injury among persons 65 years of age and older in Oklahoma, 1992–2003. Brain Inj. 2007;21(7):691–699. doi: 10.1080/02699050701426873. [DOI] [PubMed] [Google Scholar]
- 5.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–378. doi: 10.1097/00001199-200609000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Flanagan SR, Hibbard MR, Riordan B, Gordon WA. Traumatic brain injury in the elderly: diagnostic and treatment challenges. Clin Geriatr Med. 2006;22(2):449–468. doi: 10.1016/j.cger.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Reeder KP, Rosenthal M, Lichtenberg P, Wood D. Impact of age on functional outcome following traumatic brain injury. J Head Trauma Rehabil. 1996;11(3):22–31. [Google Scholar]
- 8.Frankel JE, Marwitz JH, Cifu DX, Kreutzer JS, Englander J, Rosenthal M. A follow-up study of older adults with traumatic brain injury: taking into account decreasing length of stay. Arch Phys Med Rehabil. 2006;87(1):57–62. doi: 10.1016/j.apmr.2005.07.309. [DOI] [PubMed] [Google Scholar]
- 9.Cifu DX, Kreutzer JS, Marwitz JH, Rosenthal M, Englander J, High W. Functional outcomes of older adults with traumatic brain injury: a prospective, multicenter analysis. Arch Phys Med Rehabil. 1996;77(9):883–888. doi: 10.1016/s0003-9993(96)90274-9. [DOI] [PubMed] [Google Scholar]
- 10.Bruns J, Hauser WA. The epidemiology of traumatic brain injury: a review. Epilepsia. 2003;44(Suppl 10):2–10. doi: 10.1046/j.1528-1157.44.s10.3.x. [DOI] [PubMed] [Google Scholar]
- 11.Tieves KS, Yang H, Layde PM. The epidemiology of traumatic brain injury in Wisconsin, 2001. Wis Med J. 2005;104(2):22–25. [PubMed] [Google Scholar]
- 12.Kraus JF, Peek-Asa C, McArthur D. The independent effect of gender on outcomes following traumatic brain injury: a preliminary investigation. Neurosurg Focus. 2000;8(1):e5. doi: 10.3171/foc.2000.8.1.156. [DOI] [PubMed] [Google Scholar]
- 13.Slewa-Younan S, Baguley IJ, Heriseanu R, et al. Do men and women differ in their course following traumatic brain injury? A preliminary prospective investigation of early outcome. Brain Inj. 2008;22(2):183–191. doi: 10.1080/02699050801888808. [DOI] [PubMed] [Google Scholar]
- 14.Groswasser Z, Cohen M, Keren O. Female TBI patients recover better than males. Brain Inj. 1998;12(9):805–808. doi: 10.1080/026990598122197. [DOI] [PubMed] [Google Scholar]
- 15.Kennedy RE, Livingston L, Marwitz JH, Gueck S, Kreutzer JS, Sander AM. Complicated mild traumatic brain injury on the inpatient rehabilitation unit: a multicenter analysis. J Head Trauma Rehabil. 2006;21(3):260–271. doi: 10.1097/00001199-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Ratcliff JJ, Greenspan AI, Goldstein FC, et al. Gender and traumatic brain injury: do the sexes fare differently? Brain Inj. 2007;21(10):1023–1030. doi: 10.1080/02699050701633072. [DOI] [PubMed] [Google Scholar]
- 17.Gordon WA, Zafonte R, Cicerone K, et al. Traumatic brain injury rehabilitation: state of the science. Am J Phys Med Rehabil. 2006;85(4):343–382. doi: 10.1097/01.phm.0000202106.01654.61. [DOI] [PubMed] [Google Scholar]
- 18.Ragnarsson KT. Traumatic brain injury research since the 1998 NIH Consensus Conference: accomplishments and unmet goals. J Head Trauma Rehabil. 2006;21(5):379–387. doi: 10.1097/00001199-200609000-00002. [DOI] [PubMed] [Google Scholar]
- 19.Thompson HJ, McCormick WC, Kagan SH. Traumatic brain injury in older adults: epidemiology, outcomes, and future implications. J Am Geriatr Soc. 2006;54(10):1590–1595. doi: 10.1111/j.1532-5415.2006.00894.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.UDSMR. Uniform Data System for Medical Rehabilitation. [Accessed May 4, 2009];2009 http://udsmr.org.
- 21.UB Foundation Activities. The IRF-PAI Training Manual. 2004 http://www.cms.hhs.gov/InpatientRehabFacPPS/downloads/irfpaimanual040104.pdf. Available from: Centers for Medicare and Medicaid Services.
- 22.Kraemer HC, Blasey CM. Centring in regression analyses: A strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research. 2004;13(3):141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the Functional Independence Measure: a quantitative review. Arch Phys Med Rehabil. 1996;77(12):1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 24.Farace E, Alves WM. Do women fare worse: a metaanalysis of gender differences in traumatic brain injury outcome. J Neurosurg. 2000;93(4):539–545. doi: 10.3171/jns.2000.93.4.0539. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman JM, Doctor JN, Chan L, Whyte J, Jha A, Dikmen S. Potential impact of the new Medicare prospective payment system on reimbursement for traumatic brain injury inpatient rehabilitation. Arch Phys Med Rehabil. 2003;84(8):1165–1172. doi: 10.1016/s0003-9993(03)00232-6. [DOI] [PubMed] [Google Scholar]
- 26.Brown AW, Malec JF, McClelland RL, Diehl NN, Englander J, Cifu DX. Clinical elements that predict outcome after traumatic brain injury: a prospective multicenter recursive partitioning (decision-tree) analysis. J Neurotrauma. 2005;22(10):1040–1051. doi: 10.1089/neu.2005.22.1040. [DOI] [PubMed] [Google Scholar]
- 27.Marquez de la Plata CD, Hart T, Hammond FM, et al. Impact of age on long-term recovery from traumatic brain injury. Arch Phys Med Rehabil. 2008;89(5):896–903. doi: 10.1016/j.apmr.2007.12.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Millis SR, Rosenthal M, Novack TA, et al. Long-term neuropsychological outcome after traumatic brain injury. J Head Trauma Rehabil. 2001;16(4):343–355. doi: 10.1097/00001199-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 29.Hammond FM, Hart T, Bushnik T, Corrigan JD, Sasser H. Change and predictors of change in communication, cognition, and social function between 1 and 5 years after traumatic brain injury. J Head Trauma Rehabil. 2004;19(4):314–328. doi: 10.1097/00001199-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Chang PF, Ostir GV, Kuo YF, Granger CV, Ottenbacher KJ. Ethnic differences in discharge destination among older patients with traumatic brain injury. Arch Phys Med Rehabil. 2008;89(2):231–236. doi: 10.1016/j.apmr.2007.08.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lum TY. Understanding the racial and ethnic differences in caregiving arrangements. J Gerontol Soc Work. 2005;45(4):3–21. doi: 10.1300/J083v45n04_02. [DOI] [PubMed] [Google Scholar]
- 32.Scharlach AE, Kellam R, Ong N, Baskin A, Goldstein C, Fox PJ. Cultural attitudes and caregiver service use: lessons from focus groups with racially and ethnically diverse family caregivers. J Gerontol Soc Work. 2006;47(1–2):133–156. doi: 10.1300/J083v47n01_09. [DOI] [PubMed] [Google Scholar]
- 33.Goranson TE, Graves RE, Allison D, La Freniere R. Community integration following multidisciplinary rehabilitation for traumatic brain injury. Brain Inj. 2003;17(9):759–774. doi: 10.1080/0269905031000088513. [DOI] [PubMed] [Google Scholar]
- 34.Whiteneck G, Brooks CA, Mellick D, Harrison-Felix C, Terrill MS, Noble K. Population-based estimates of outcomes after hospitalization for traumatic brain injury in Colorado. Arch Phys Med Rehabil. 2004;85(Suppl 2):S73–S81. doi: 10.1016/j.apmr.2003.08.107. [DOI] [PubMed] [Google Scholar]