Abstract
Porcine reproductive and respiratory syndrome (PRRS) causes significant economic losses to the swine industry worldwide. Although inactivated and live vaccines are commercially available for the control of PRRS, both types of vaccine have not always proven successful in terms of generating a protective immune response, particularly in the case of inactivated vaccines. In this study, we tested whether an inactivated vaccine could induce a humoral immune response to PRRS during a homologous challenge. Amino acid substitutions were introduced into glycoprotein (GP) 5 of the FL12 strain of the PRRS virus (PRRSV) using site-directed mutagenesis with a pFL12 infectious clone. The substitutions led to double deglycosylation in the putative glycosylation moieties on GP5. The mutant virus was subsequently inactivated with binary ethylenimine. The efficacy of the inactivated mutant virus was compared with that of the inactivated wild-type PRRSV. Only the inactivated mutant PRRSV induced serum neutralizing antibodies at six weeks post-vaccination. The group that was administered the inactivated mutant virus twice exhibited a significantly increased neutralizing antibody titer after a challenge with the virulent homologous strain and exhibited more rapid clearing of viremia compared to other groups, including the groups that were administered either the inactivated mutant or wild-type virus only once and the group that was administered the inactivated wild-type virus twice. Histopathological examination of lung tissue sections revealed that the group that was administered the inactivated mutant virus twice exhibited significantly thinner alveolar septa, whereas the thickness of the alveolar septa of the other groups were markedly increased due to lymphocyte infiltration. These results indicated that the deglycosylation of GP5 enhanced the immunogenicity of the inactivated mutant PRRSV and that twice administrations of the inactivated mutant virus conferred better protection against the homologous challenge. These findings suggest that the inactivated PRRSV that expresses a hypo-glycosylated GP5 is a potential inactivated vaccine candidate and a valuable tool for controlling PRRS for the swine industry.
Keywords: PRRSV, Inactivated virus vaccine, Humoral immune response, Hypo-glycosylation, GP5
1. Introduction
Porcine reproductive and respiratory syndrome (PRRS) is one of the most important infectious diseases in pigs and is responsible for substantial economic losses in the swine industry worldwide. The PRRS virus (PRRSV) causes severe reproductive failure in pregnant sows and is associated with porcine respiratory disease complex (PRDC) in combination with other viral and bacterial infections in young piglets [1–3]. To help control outbreaks of PRRS, strategies, such as management, biosecurity and vaccination, have been applied with various levels of success [4–6]. The control PRRS is complicated due to its pattern of persistent, subclinical infections with occasional epidemic outbreaks, the great heterogeneity of the virus and the poor antibody response that is insufficient to completely block viral re-infection [7–10]. Although the current vaccines need to be improved, and new vaccine technologies are required, vaccination is the most cost-effective and reliable strategy that is currently available.
There are two types of commercially available PRRS vaccines. The first is a modified-live virus (MLV) vaccine, and the second is an inactivated vaccine. The PRRS MLV vaccine is well-recognized for its protective efficacy against PRRSV infection in the field, but this vaccine has a limited efficacy against challenges with heterologous viruses. Additionally, the PRRS MLV vaccine has an intrinsic risk for reversion to a virulent strain [4]. The PRRS inactivated vaccine is much safer than the PRRS MLV vaccine. However, this advantage of the inactivated vaccine is diminished by its insufficient immunogenicity. The commercially available PRRS inactivated vaccine does not induce a sufficient immune response and does not adequately protect pigs from viremia when challenged with PRRSVs [11–13]. Although previous studies have shown that PRRS inactivated vaccines are able to inhibit viral shedding and induce neutralizing antibodies, these results vary depending on the virus strain and the type of tissue culture used to produce the vaccines [11,14]. Numerous efforts have been made to develop an ideal PRRS inactivated vaccine that would offer broad protection and high immunogenicity [15,16], but these efforts have been unsuccessful.
Previous studies have determined that the neutralizing epitopes are located in the structural proteins, including glycoprotein (GP) 3, GP4, GP5 and the non-glycosylated membrane protein (M) [17–19]. Among these, the neutralizing epitopes in GP5 induce the primary neutralizing antibodies [20–23]. GP5 is encoded by open reading frame (ORF) 5 of the PRRSV viral genome and is the major envelope glycoprotein of PRRSV. GP5 has been suggested to be involved in the viral entry and assembly of PRRSV [24]. A small ectodomain located on the N-terminus of GP5 plays an important role in the attachment of PRRSV to the macrophage-specific receptor [24,25]. Two epitopes located in this ectodomain have previously been identified and characterized, based on their neutralizing capabilities, as a decoy epitope and a major neutralizing epitope [22]. The delayed production of neutralizing antibodies to GP5 is a characteristic of the immune response to PRRSV and is caused by the rapid induction of non-neutralizing antibodies against the decoy epitope [24,26]. PRRSV-specific non-neutralizing antibodies have been detected at one week post-inoculation (PI), while neutralizing antibodies have been observed to appear from three weeks PI [27–29].
The GP5 of PRRSV has two to five potential N-linked glycosylation sites located in the ectodomain, and the presence of glycans around the major neutralizing epitopes has been suggested to reduce the immunogenicity of PRRSV [30]. It has been reported that glycan shielding on PRRSV GPs interferes with the neutralizing antibody response [31–34]. Previous studies have also demonstrated that weak neutralizing antibody responses are obtained in the presence of glycans on the GPs of other viruses, such as lactate dehydrogenase-elevating virus, hepatitis B virus, human immunodeficiency virus and influenza virus [35–38].
In previous studies, multiple mutants of PRRSV containing various combinations of deglycosylations on GP5 have been produced using reverse genetics [31,33,39,40]. Among these mutants, the mutant virus containing a double deglycosylation of N34 and N51 of GP5 shows decreased viral replication but induces a higher level of neutralizing antibodies in in vivo experiments compared to its parental strain of PRRSV [31]. In this study, we attempted to develop an inactivated PRRSV vaccine using this mutant strain of PRRSV, which contains a double deglycosylation of GP5 and evaluated the efficacy of this vaccine using a challenge infection with a homologous strain of PRRSV.
2. Materials and methods
2.1. cDNA clone, cells and viruses
A full-length PRRSV infectious cDNA clone (pFL12) generated from the North American type II PRRSV isolate was used to construct a mutant plasmid carrying mutations in the putative N-glycosylation sites by site-directed mutagenesis as previously described [41]. To produce wild-type (wt) and mutant viruses, the pFL12 and mutant plasmids were linearized by digestion with AclI and transcribed in vitro using the mMESSAGE mMACHINE Ultra T7 kit (Ambion, Austin, TX). The produced RNAs were electroporated into the MARC-145 cell lines, cultured in low-glucose Dulbecco's Modified Eagle's Medium (DMEM) and supplemented with 10% fetal bovine serum (FBS) [42] All of the rescued wt and mutant viruses were subjected to RT-PCR amplification using appropriate primers, and the PCR fragments were subjected to DNA sequencing to confirm the presence of the desired mutations and the absence of unwanted mutations. The N-glycosylation profiles of the GP5 for the wt and deglycosylated mutant viruses were confirmed by western blotting. The viruses were treated for 16 h at 37 °C with the 10 U peptide N-glycosidase F (PNGaseF) according to the manufacturer's instructions (NEB, Beverly, MA). Subsequently, the proteins were separated by 12% SDS-polyacrylamide gel electrophoresis and transferred onto a nitrocellulose membrane (GE Healthcare, Milwaukee, WI). The membrane was blocked with 5% skim milk in phosphate-buffered saline-Tween 20 and incubated with porcine serum containing a high level of PRRSV-specific primary antibody and horseradish peroxidase-conjugated goat anti-porcine IgG (Southern Biotech, Birmingham, AL) secondary antibody. The blots were imaged using Amersham ECL Prime Western Blotting Detection Reagent (GE Healthcare).
2.2. Production of inactivated PRRSV vaccines
Both wt FL12 and the mutant virus FL12/GP5DM containing double-amino acid substitutions at the 34 and 51 potential N-glycosylation residues in GP5 [31] were used to produce the inactivated vaccines used in this study.
Both the wt and mutant viruses were concentrated at 108 TCID50/ml and inactivated with binary ethylenimine (BEI) as described previously [43]. Briefly, BEI was prepared as a 0.1 M stock solution by stirring 0.1 M 2-bromoethylamine hydrobromide (Sigma-Aldrich, St. Louis, MO) in 0.175 M NaOH at 37 °C for 1 h. The BEI stock solution was added to the virus suspension, and the mixture was incubated at 37 °C for 24 h. The remaining BEI was subsequently neutralized with 0.1 mM sodium thiosulfate (Sigma-Aldrich) for 2 h. To confirm the inactivation of the virus, MARC-145 cells were inoculated with BEI-treated virus suspension and cultured at 37°C for five days. A total of 1 ml of inactivated viral antigen containing 108 TCID50/ml of the BEI-inactivated PRRSV was mixed with an equal volume of Montanide™ IMS1313 VG adjuvant (SEPPIC, Paris, France). The aqueous adjuvant was suitable for inactivated and live vaccines in pigs [44,45].
2.3. Evaluation of the efficacy of the inactivated PRRSV vaccine
The experimental design involving the inactivated PRRSV vaccination and the challenge is summarized in Table 1. Fifteen three-week old piglets were purchased from a PRRS-free farm and confirmed to be serologically PRRSV-negative. The piglets were randomly allocated into five groups (G1 to G5). The piglets in G1 and G2 were intramuscularly administered inactivated wt virus vaccine, and the piglets in G3 and G4 were intramuscularly administered inactivated mutant virus vaccine. The G5 piglets were injected with DMEM alone as a control. Three weeks after the primary vaccination, the piglets in G2 and G4 were boost-vaccinated using the same vaccines they had received earlier. Serum samples were collected at 14, 28, 42, 49 and 56 days post-vaccination and stored in −20 °C. Five weeks after the booster vaccination, all of the groups were intramuscularly challenged with 105 TCID50/ml of wt virus. Serum samples were collected at 2, 3, 4, 7, 8, 9 and 13 days after the challenge. The collected sera were examined for viremia via immunofluorescence assay in MARC-145 cells. Twenty-one days after the challenge, the pigs were humanely euthanized according to the guidelines of the Institutional Animal Care and Use Committee of Konkuk University.
Table 1.
In vivo experimental design.
| Groups | Number of piglets | Vaccination (inactivated virus vaccines) | Challenge virus (FL12) | |
|---|---|---|---|---|
|
| ||||
| 1st | 2nd | |||
| G1 | 3 | + (FL12) | – | + |
| G2 | 3 | + (FL12) | + (FL12) | + |
| G3 | 3 | + (FL12/GP5DM) | – | + |
| G4 | 3 | + (FL12/GP5DM) | + (FL12/GP5DM) | + |
| G5 | 3 | – | – | + |
2.4. Serum neutralizing assay
The serum neutralizing (SN) assay was conducted in 96-well plates that contained confluent MARC-145 cells that had been seeded 48 h before the experiment. Equal volumes of two-fold serially diluted serum samples were mixed with 50 μl of 100 TCID50 of the wt virus and incubated at 37 °C for 1 h. The mixture was applied to a monolayer of MARC-145 cells and incubated at 37 °C for two days. The cells were fixed and stained with nucleocapsid (N) protein-specific SDOW17, which was followed by incubation with anti-mouse Alexa Fluor 488 conjugate (Life Technologies, US). The SN antibody titers are expressed as the reciprocal of the highest dilution that exhibited a 90% or greater reduction in the number of fluorescent foci present in the control wells.
2.5. Histopathological examination
The cranial lobes of the lungs were collected from all euthanized animals in postmortem procedures and fixed in 10% neutral buffered formalin. The fixed tissues were processed for histopathological examination. The severities of the histopathological lesions were compared by measuring the thicknesses of the alveolar septa. Fifty hematoxylin and eosin-stained sections were randomly selected from each pig, and each section was viewed at 200-fold magnification. The thicknesses of the alveolar septa were analyzed with ImageJ software. The septal thicknesses of at least 50 alveoli per each section were measured by drawing straight lines across the entire widths of the septa. At least three sections from each pig were used, and the average septal thickness was then calculated for each group.
2.6. Statistical analyses
The SN antibody levels, viremia and microscopic lung lesions were analyzed for significant differences between groups using Mann–Whitney U tests and Student t-tests that were performed with SPSS 19 (SPSS, Chicago, IL). A P value less than 0.05 was considered statistically significant.
3. Results
3.1. Development of the deglycosylated mutant virus and inactivated vaccines
After genetically engineering the infectious clone pFL12, mutations at the amino acidsites 34 and 51 in GP5 were confirmed by sequencing. The wt virus and the mutant containing thedouble deglycosylation on GP5 were successfully rescued from the transfected MARC-145 cells (Fig. S1A). Western blotting revealed that the migration of the GP5 from the wt virus indicated a mass of 25 kDa, whereas the migration of the GP5 from the mutant virus indicated a smaller size (20.5 kDa) that nearly overlapped with that of the M envelope protein. The treatment of the viruses with PNGaseF reduced the sizes of the GP5s to 17 kDa in both viruses (Fig. S1B). After treatment with BEI, both the wt and mutant viruses did not induce any detectable cytopathological effects in the MARC-145 cell monolayers over five days; these results were confirmed by observation under the microscope and by immunofluorescence staining with the N-specific SDOW17 antibody (data not shown).
3.2. Immune responses of the inactivated vaccines
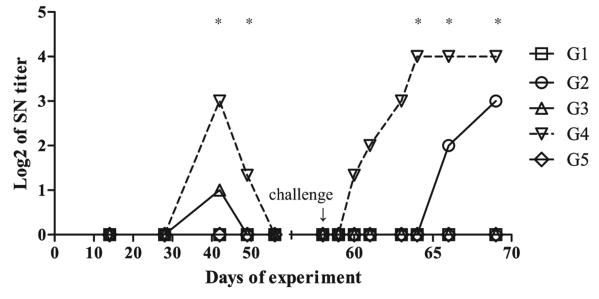
To determine whether the inactivated PRRSV vaccine containing the mutant virus elicited a humoral immune response, the piglets were inoculated with the vaccine, and the vaccine's immunogenicity was assessed. Interestingly, SN antibodies were observed at six weeks post-vaccination only in the groups that were inoculated with an inactivated mutant virus (i.e., G3 and G4) (Fig. 1). However, the SN antibodies did not persist for long and were not detectable at eight weeks post-vaccination (Fig. 1). The SN antibody titer of the group that was vaccinated twice with the inactivated mutant virus (G4) was much higher and was maintained for a longer period compared to that of the group that received only the primary vaccination (G3). SN antibodies were not observed in either the group that was vaccinated with the inactivated wt virus (G1 and G2) or the control group (G5).
Fig. 1. PRRSV-specific SN antibody titers following vaccination and challenge.
Piglets were injected once with wt virus (G1), twice with wt virus (G2), once with mutant virus (G3), twice with mutant virus (G4), or sterile media (G5). The levels of serum neutralizingantibodies against PRRSV were measured using the wt virus and MARC-145. Asterisks indicate significant differences (P < 0.05) compared to the control group (G5).
3.3. Efficacy of the inactivated vaccines
Five weeks after the boost vaccination, all groups were challenged with the wt virus, and viremia and SN antibody titers were evaluated. The SN antibodies of the group that was vaccinated twice with the inactivated mutant virus (G4) was re-evaluated at four days post-challenge, reached a titer of 1:16 at eight days post-challenge and maintained that level until the end of experiment (Fig. 1). SN antibodies were also detected 10 days post-challenge in the group that was vaccinated twice with the inactivated wt virus (G2), and these antibodies reached a titer of 1:8 at 13 days post-challenge. PRRSV-specific SN antibodies were not detected in the serum samples from the G1, G3 and G5 piglets at any point in the experimental challenge period.
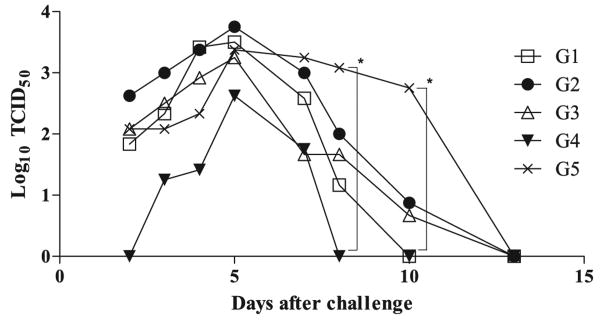
Viremia was evident in the four challenged groups (G1–G3, G5) at two dayspost-challenge, and the G4 piglets exhibited a delayed-onset viremia at three days post-challenge (Fig. 2). Although the viremia gradually increased and peaked at five days post-challenge in all of the challenged groups, the magnitude and duration of the viremia in G4 was significantly lower and shorter than those of other groups. As shown in Fig. 2, the viremia of G4 rapidly decreased and was undetectable at eight days post-challenge. However, the viremia in the other groups lasted longer and decreased more gradually until 13 days post-challenge.
Fig. 2. Viremia in the sera following challenge.
The piglets were challenged following vaccination, and viremia was measured at different times. The piglets were injected once with wt virus (G1), twice with wt virus (G2), once with mutant virus (G3), twice with mutant virus (G4), or sterile media (G5). Asterisks indicate significant differences (P < 0.05) compared to the control group (G5).
The efficacy of the vaccine was investigated using challenge inoculations with a homologous strain. The piglets that were inoculated with the wt virus exhibited moderate sneezing and lachrymal discharge. The body weights and rectal temperatures of the piglets were not significantly different across groups (data not shown). During necropsy, moderate pneumonic lesions, including severe edema in the lungs and enlargement of the tracheobronchial lymph nodes, were observed in nearly all of the challenged piglets with the exception of the G4 piglets (data not shown). Histopathological examination revealed that all of the piglets in the four groups (G1–G3, G5) exhibited moderate interstitial pneumonia, significant increases in the thickness of the alveolar septa and lymphocyte infiltrations; in contrast, the G4 piglets exhibited mild pneumonia, average alveolar septa of 15 μm and minimal infiltration (Fig. 3).
Fig. 3. Histopathological examination.
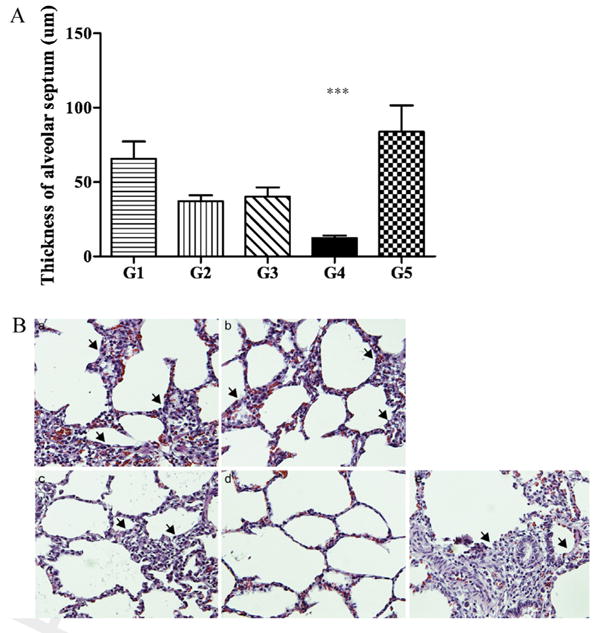
The graph depicts the thicknesses of the alveolar septa (A), and the photomicrographs (B) show hematoxylin and eosin-stained sections of the cranial lobes of the lungs following the in vivo experiments. The piglets were injected once with wt virus (G1, a), twice with wt virus (G2, b), once with mutant virus (G3, c), twice with mutant virus (G4, d), or sterile media (G5, e). Asterisks indicate significant differences (P < 0.05) between the indicated pairs of groups. The arrows indicate the localized regions of severe interstitial pneumonia and thickened alveolar septa. Magnification: ×200.
4. Discussion
In this study, a mutant virus strain of PRRSV, FL12/GP5DM that possesses deglycosylated GP5 was created and used to produce an inactivated vaccine. The viruses used to develop inactivated vaccines were produced using reverse genetics as described in a previous study [31]. The rescued mutant virus exhibited slightly delayed growth properties compared to the wt virus (data not shown). Consistent with our results, many mutant viruses have been found to exhibit reduced viral titers compared with the wt viruses in previous studies [31,46,47]. In in vivo experiments, the inactivated PRRSV vaccine based on the mutant virus induced a higher SN antibody titer and resulted in faster clearing of viremia compared to the inactivated PRRSV vaccine that was based on the wt virus. Moreover, histopathological examinations revealed that the symptoms of interstitial pneumonia were remarkably reduced in the group that was vaccinated with the inactivated mutant virus. While microscopic observation revealed obvious lymphocyte infiltration and interstitial pneumonia in all other groups, the markedly thin alveolar septa and lack of or minimal infiltration in G4 clearly indicated that the inactivated vaccine prepared with the mutant virus effectively protected the piglets from a homologous challenge infection.
A possible explanation for this effect of the hypo-glycosylated PRRSV has been provided in previous studies; this explanation postulates that the deglycosylation of GP3 and/or GP5 enhances the immunogenicity of a live virus despite decreasing the replication of the mutant viruses to some extent [31,33,34,39,40]. These results revealed that the removal of glycans from either GP3 or GP5 might expose hidden neutralizing epitope(s) and can improve SN antibody responses. The present study demonstrated that the deglycosylation of GP5 also successfully improved the immunogenicity of an inactivated virus that was incapable of viral replication and endogenous viral protein synthesis to a level similar to that of a live virus. In previous studies, enhanced developments of SN antibodies have not always been associated with blocking viremia [48,49]. However, Osorio et al. [50] previously demonstrated that the SN antibody response is relatively correlated with protective immunity in PRRSV infection, particularly regarding the clearance of viremia; our results are in agreement with their findings [50].
Inactivated PRRSV vaccines are well-known to induce insufficient protective immune responses against both homologous and heterologous PRRSV challenges [12,51]. In this study, an inactivated mutant virus vaccine elicited a considerable increase in the level of SN antibodies following vaccination, whereas the inactivated wt virus vaccine did not induce SN antibodies prior to the challenge (Fig. 1). As the extent of our knowledge, this is the first report to show that a single intramuscular administration of inactivated PRRSV vaccine can induce detectable humoral immune responses. Although both G3 and G4 exhibited SN antibody induction following vaccination, only G4 received a boost vaccination, which re-induced high levels of SN antibodies following the challenge. After the challenge with the wt virus, a PRRSV-specific SN antibody response was evident in the G4 piglets. The SN antibody titer had quickly increased again by four days post-challenge and was maintained at a titer of 1:16 until the end of the experiment. These results indicate that a boost vaccination of the inactivated PRRSV vaccine is necessary to induce a sufficient humoral immune response. In a previous study that utilized a commercially inactivated vaccine, a clear anamnestic humoral immune response was observed following a heterologous challenge with wt virus, but this response was much slower and weaker than that observed in G4 [13]. Compared to the unvaccinated pigs, the G4 piglets exhibited a significantly delayed onset of viremia and subsequently rapidly cleared the viremia; these results are consistent with those of previous studies [12,52]. The inactivated vaccine containing the FL12/GP5DM strain was able to induce an SN antibody response after a single intramuscular administration and significantly reduced lung pathology, whereas the inactivated vaccine used in a previous study failed to induce an efficacious humoral immune response [13]. Although our observations are, on the one hand, in agreement with findings of the authors of this previous study that an inactivated vaccine can induce a humoral immune response after a challenge, on the other hand, these authors postulated that the post-challenge anamnestic response comprised of PRRSV-specific SN antibodies was not sufficient to provide humoral immunity based on the viremia and viral loads these authors detected in the tissues during the post-challenge period. However, a direct comparison between these two findings is not relevant because we used a tissue culture method to detect viable viruses, and the authors of the other study used quantitative PCR to detect the presence of any viral RNA. Furthermore, we did not observe anamnestic responses in the groups that were inoculated once (G1 and G3), which contrasts with the previous findings; however, we did observe this response in the groups that were inoculated twice. It is also not appropriate to conclude that the co-existence of SN antibodies and viral RNA constitutes evidence of ineffective protection unless other parameters of protective efficacy, such as clinical outcome, lung pathology and cell-mediated immunity, are considered. Nonetheless, our findings indicated that the inactivated vaccine is capable of inducing a sustained SN antibody response following the vaccination and enhancing the memory response after the challenge when the inactivated vaccine is suitably formulated with a benign immunostimulating adjuvant and applied according to proper vaccination regimen. These results suggest that the inactivated vaccine we produced with a mutant virus that possesses a hypo-glycosylated GP5 may be a promising alternative PRRSV vaccine that is capable of inducing humoral immune responses that are comparable to those induced by MLV in the field; this alternative vaccine may be particularly useful in areas and countries in which the use of the live virus vaccine is not feasible.
It has been speculated that the efficacy of an inactivated vaccine is potentiallydetermined by the inactivation agent and/or the adjuvant [52–54]. In this study, the BEI-inactivated vaccine successfully induced the SN antibody response and partially inhibited viremia. These results are consistent with the results of the previous study that used a BEI-inactivated vaccine [52]. In this previous study, BEI was used as an inactivating reagent instead of formaldehyde, which is generally the most widely used reagent in such cases. The inactivating reagent and method may affect the efficacies of inactivated vaccines and should be strongly considered during the development of inactivated vaccines. BEI was used to inactivate the virus due to its specific effects on the viral genome that do not damage the viral epitopes [55]. In a previous study, BEI was found to have a minimal slight effect on the epitopes, whereas formaldehyde substantially alters the conformations of the epitopes [56]. BEI is the most promising of the methods of inactivating PRRSV, which include the following: gamma irradiation, formaldehyde, UV modification, and pH modification. BEI has successfully been used to inactivate PRRSV in previous studies [52,57,58]. In these previous studies, inactivated PRRSV vaccine induced effective immune responses after single intranasal administrations [53,54]. However, the intranasal vaccine delivery route requires an additional vaccine spray machine and has to be performed by well-trained staff. Currently, vaccines that can be administered via the intramuscular route and are composed of an oil adjuvant and inactivated with BEI are the most popular type of inactivated vaccine with the pig industry [52].
In summary, the double amino acid substitutions at the N-glycosylated sites near the major neutralizing epitope in GP5 remarkably increased the immunogenicity of PRRSV, particularly in terms of the SN antibody response, and rapidly reduced the viral loads in the sera. The mutant virus FL12/GP5DM was able to act as an inactivated vaccine candidate against PRRSV. Although a single administration of the inactivated PRRSV vaccine based on the mutant virus induced a humoral immune response, a boost administration is recommended to ensure efficacy. A variety of additional adjuvants that may improve the immune response to KV vaccines should be considered in further studies.
Supplementary Material
Acknowledgments
This study was supported by grant no. 610001-03-1-SU000 from the Technology Development Program for the Korea Institute of Planning and Evaluation for Technology in Food, Agriculture, Forestry and Fisheries.
This study was also supported by the Veterinary Science Research Institute of Konkuk University.
Footnotes
Appendix A. Supplementary data: Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.vaccine.2014.04.083.
References
- 1.Wee GJ, et al. Efficacy of porcine reproductive and respiratory syndrome virus vaccine and porcine interleukin-12. Vet Ther. 2001;2(2):112–9. [PubMed] [Google Scholar]
- 2.Christianson WT, et al. Experimental reproduction of swine infertility and respiratory syndrome in pregnant sows. Am J Vet Res. 1992;53(4):485–8. [PubMed] [Google Scholar]
- 3.Nodelijk G, et al. A quantitative assessment of the effectiveness of PRRSV vaccination in pigs under experimental conditions. Vaccine. 2001;19(27):3636–44. doi: 10.1016/s0264-410x(01)00099-8. [DOI] [PubMed] [Google Scholar]
- 4.Kwang J, et al. Antibody and cellular immune responses of swine following immunisation with plasmid DNA encoding the PRRS virus ORF's 4, 5, 6 and 7. Res Vet Sci. 1999;67(2):199–201. doi: 10.1053/rvsc.1998.0291. [DOI] [PubMed] [Google Scholar]
- 5.Neumann EJ, et al. Assessment of the economic impact of porcine reproductive and respiratory syndrome on swine production in the United States. J Am Vet Med Assoc. 2005;227(3):385–92. doi: 10.2460/javma.2005.227.385. [DOI] [PubMed] [Google Scholar]
- 6.Corzo CA, et al. Control and elimination of porcine reproductive and respiratory syndrome virus. Virus Res. 2010;154(1–2):185–92. doi: 10.1016/j.virusres.2010.08.016. [DOI] [PubMed] [Google Scholar]
- 7.Blaha T. The “colorful” epidemiology of PRRS. Vet Res. 2000;31(1):77–83. doi: 10.1051/vetres:2000109. [DOI] [PubMed] [Google Scholar]
- 8.Meng XJ. Heterogeneity of porcine reproductive and respiratory syndrome virus: implications for current vaccine efficacy and future vaccine development. Vet Microbiol. 2000;74(4):309–29. doi: 10.1016/S0378-1135(00)00196-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murtaugh MP, Xiao Z, Zuckermann F. Immunological responses of swine to porcine reproductive and respiratory syndrome virus infection. Viral Immunol. 2002;15(4):533–47. doi: 10.1089/088282402320914485. [DOI] [PubMed] [Google Scholar]
- 10.Batista L, et al. Detection of porcine reproductive and respiratory syndrome virus in pigs with low positive or negative ELISA s/p ratios. Vet Rec. 2004;154(1):25–6. doi: 10.1136/vr.154.1.25. [DOI] [PubMed] [Google Scholar]
- 11.Nilubol D, et al. The effect of a killed porcine reproductive and respiratory syndrome virus (PRRSV) vaccine treatment on virus shedding in previously PRRSV infected pigs. Vet Microbiol. 2004;102(1–2):11–8. doi: 10.1016/j.vetmic.2004.05.006. [DOI] [PubMed] [Google Scholar]
- 12.Scortti M, et al. Failure of an inactivated vaccine against porcine reproductive and respiratory syndrome to protect gilts against a heterologous challenge with PRRSV. Vet Rec. 2007;161(24):809–13. [PubMed] [Google Scholar]
- 13.Zuckermann FA, et al. Assessment of the efficacy of commercial porcine reproductive and respiratory syndrome virus (PRRSV) vaccines based on measurement of serologic response, frequency of gamma-IFN-producing cells and virological parameters of protection upon challenge. Vet Microbiol. 2007;123(1–3):69–85. doi: 10.1016/j.vetmic.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 14.Misinzo G, et al. Efficacy of an inactivated PRRSV vaccine: induction of virus-neutralizing antibodies and partial virological protection upon challenge. Adv Exp Med Biol. 2006;581:449–54. doi: 10.1007/978-0-387-33012-9_81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Huang YW, Meng XJ. Novel strategies and approaches to develop the next generation of vaccines against porcine reproductive and respiratory syndrome virus (PRRSV) Virus Res. 2010;154(1–2):141–9. doi: 10.1016/j.virusres.2010.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kimman TG, et al. Challenges for porcine reproductive and respiratory syndrome virus (PRRSV) vaccinology. Vaccine. 2009;27(28):3704–18. doi: 10.1016/j.vaccine.2009.04.022. [DOI] [PubMed] [Google Scholar]
- 17.van Nieuwstadt AP, et al. Proteins encoded by open reading frames 3 and 4 of the genome of Lelystad virus (Arteriviridae) are structural proteins of the virion. J Virol. 1996;70(7):4767–72. doi: 10.1128/jvi.70.7.4767-4772.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yang L, et al. Categorization of North American porcine reproductive and respiratory syndrome viruses: epitopic profiles of the N, M, GP5 and GP3 proteins and susceptibility to neutralization. Arch Virol. 2000;145(8):1599–619. doi: 10.1007/s007050070079. [DOI] [PubMed] [Google Scholar]
- 19.Cancel-Tirado SM, Evans RB, Yoon KJ. Monoclonal antibody analysis of porcine reproductive and respiratory syndrome virus epitopes associated with antibody-dependent enhancement and neutralization of virus infection. Vet Immunol Immunopathol. 2004;102(3):249–62. doi: 10.1016/j.vetimm.2004.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gonin P, et al. Seroneutralization of porcine reproductive and respiratory syndrome virus correlates with antibody response to the GP5 major envelope glycoprotein. J Vet Diagn Invest. 1999;11(1):20–6. doi: 10.1177/104063879901100103. [DOI] [PubMed] [Google Scholar]
- 21.Weiland E, et al. Monoclonal antibodies to the GP5 of porcine reproductive and respiratory syndrome virus are more effective in virus neutralization than monoclonal antibodies to the GP4. Vet Microbiol. 1999;66(3):171–86. doi: 10.1016/s0378-1135(99)00006-1. [DOI] [PubMed] [Google Scholar]
- 22.Ostrowski M, et al. Identification of neutralizing and nonneutralizing epitopes in the porcine reproductive and respiratory syndrome virus GP5 ectodomain. J Virol. 2002;76(9):4241–50. doi: 10.1128/JVI.76.9.4241-4250.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Plagemann PG, Rowland RR, Faaberg KS. The primary neutralization epitope of porcine respiratory and reproductive syndrome virus strain VR-2332 is located in the middle of the GP5 ectodomain. Arch Virol. 2002;147(12):2327–47. doi: 10.1007/s00705-002-0887-2. [DOI] [PubMed] [Google Scholar]
- 24.Delputte PL, et al. Effect of virus-specific antibodies on attachment, internalization and infection of porcine reproductive and respiratory syndrome virus in primary macrophages. Vet Immunol Immunopathol. 2004;102(3):179–88. doi: 10.1016/j.vetimm.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 25.Delputte PL, et al. Porcine arterivirus attachment to the macrophage-specific receptor sialoadhesin is dependent on the sialic acid-binding activity of the N-terminal immunoglobulin domain of sialoadhesin. J Virol. 2007;81(17):9546–50. doi: 10.1128/JVI.00569-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lopez OJ, Osorio FA. Role of neutralizing antibodies in PRRSV protective immunity. Vet Immunol Immunopathol. 2004;102(3):155–63. doi: 10.1016/j.vetimm.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 27.Yoon KJ, et al. Characterization of the humoral immune response to porcine reproductive and respiratory syndrome (PRRS) virus infection. J Vet Diagn Invest. 1995;7(3):305–12. doi: 10.1177/104063879500700302. [DOI] [PubMed] [Google Scholar]
- 28.Albina E, et al. Immune responses in pigs infected with porcine reproductive and respiratory syndrome virus (PRRSV) Vet Immunol Immunopathol. 1998;61(1):49–66. doi: 10.1016/S0165-2427(97)00134-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Labarque GG, et al. Effect of cellular changes and onset of humoral immunity on the replication of porcine reproductive and respiratory syndrome virus in the lungs of pigs. J Gen Virol. 2000;81(Pt 5):1327–34. doi: 10.1099/0022-1317-81-5-1327. [DOI] [PubMed] [Google Scholar]
- 30.Music N, Gagnon CA. The role of porcine reproductive and respiratory syndrome (PRRS) virus structural and non-structural proteins in virus pathogenesis. Anim Health Res Rev. 2010;11(2):135–63. doi: 10.1017/S1466252310000034. [DOI] [PubMed] [Google Scholar]
- 31.Ansari IH, et al. Influence of N-linked glycosylation of porcine reproductive and respiratory syndrome virus GP5 on virus infectivity, antigenicity, and ability to induce neutralizing antibodies. J Virol. 2006;80(8):3994–4004. doi: 10.1128/JVI.80.8.3994-4004.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Faaberg KS, et al. Neutralizing antibody responses of pigs infected with natural GP5 N-glycan mutants of porcine reproductive and respiratory syndrome virus. Viral Immunol. 2006;19(2):294–304. doi: 10.1089/vim.2006.19.294. [DOI] [PubMed] [Google Scholar]
- 33.Jiang W, et al. Influence of porcine reproductive and respiratory syndrome virus GP5 glycoprotein N-linked glycans on immune responses in mice. Virus Genes. 2007;35(3):663–71. doi: 10.1007/s11262-007-0131-y. [DOI] [PubMed] [Google Scholar]
- 34.Vu HL, et al. Immune evasion of porcine reproductive and respiratory syndrome virus through glycan shielding involves both glycoprotein 5 as well as glycoprotein 3. J Virol. 2011;85(11):5555–64. doi: 10.1128/JVI.00189-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skehel JJ, et al. A carbohydrate side chain on hemagglutinins of Hong Kong influenza viruses inhibits recognition by a monoclonal antibody. Proc Nat Acad Sci USA. 1984;81(6):1779–83. doi: 10.1073/pnas.81.6.1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen Z, Li K, Plagemann PG. Neuropathogenicity and sensitivity to antibody neutralization of lactate dehydrogenase-elevating virus are determined by polylactosaminoglycan chains on the primary envelope glycoprotein. Virology. 2000;266(1):88–98. doi: 10.1006/viro.1999.0050. [DOI] [PubMed] [Google Scholar]
- 37.Lee CM, et al. Prevalence and clinical implications of hepatitis B virus genotypes in southern Taiwan. Scand J Gastroenterol. 2003;38(1):95–101. doi: 10.1080/00365520310000500. [DOI] [PubMed] [Google Scholar]
- 38.Wei X, et al. Antibody neutralization and escape by HIV-1. Nature. 2003;422(6929):307–12. doi: 10.1038/nature01470. [DOI] [PubMed] [Google Scholar]
- 39.Li B, et al. Immunogenicity of the highly pathogenic porcine reproductive and respiratory syndrome virus GP5 protein encoded by a synthetic ORF5 gene. Vaccine. 2009;27(13):1957–63. doi: 10.1016/j.vaccine.2009.01.098. [DOI] [PubMed] [Google Scholar]
- 40.Wei Z, et al. N-linked glycosylation of GP5 of porcine reproductive and respiratory syndrome virus is critically important for virus replication in vivo. J Virol. 2012;86(18):9941–51. doi: 10.1128/JVI.07067-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Truong HM, et al. A highly pathogenic porcine reproductive and respiratory syndrome virus generated from an infectious cDNA clone retains the in vivo virulence and transmissibility properties of the parental virus. Virology. 2004;325(2):308–19. doi: 10.1016/j.virol.2004.04.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kim HS, et al. Enhanced replication of porcine reproductive and respiratory syndrome (PRRS) virus in a homogeneous subpopulation of MA-104 cell line. Arch Virol. 1993;133(3–4):477–83. doi: 10.1007/BF01313785. [DOI] [PubMed] [Google Scholar]
- 43.Bahnemann HG. Inactivation of viral antigens for vaccine preparation with particular reference to the application of binary ethylenimine. Vaccine. 1990;8(4):299–303. doi: 10.1016/0264-410X(90)90083-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jang SI, et al. Montanide IMS 1313 N VG PR nanoparticle adjuvant enhances antigen-specific immune responses to profilin following mucosal vaccination against Eimeria acervulina. Vet Parasitol. 2011;182(2–4):163–70. doi: 10.1016/j.vetpar.2011.05.019. [DOI] [PubMed] [Google Scholar]
- 45.Cloete M, et al. Evaluation of different adjuvants for foot-and-mouth disease vaccine containing all the SAT serotypes. Onderstepoort J Vet Res. 2008;75(1):17–31. doi: 10.4102/ojvr.v75i1.84. [DOI] [PubMed] [Google Scholar]
- 46.Bentley K, Armesto M, Britton P. Infectious bronchitis virus as a vector for the expression of heterologous genes. PLoS One. 2013;8(6):e67875. doi: 10.1371/journal.pone.0067875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ni YY, et al. Attenuation of porcine reproductive and respiratory syndrome virus by molecular breeding of virus envelope genes from genetically divergent strains. J Virol. 2013;87(1):304–13. doi: 10.1128/JVI.01789-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Bastos RG, et al. Immune response of pigs inoculated with Mycobacterium bovis BCG expressing a truncated form of GP5 and M protein of porcine reproductive and respiratory syndrome virus. Vaccine. 2004;22(3–4):467–74. doi: 10.1016/s0264-410x(03)00572-3. [DOI] [PubMed] [Google Scholar]
- 49.Kheyar A, et al. Alternative codon usage of PRRS virus ORF5 gene increases eucaryotic expression of GP(5) glycoprotein and improves immune response in challenged pigs. Vaccine. 2005;23(31):4016–22. doi: 10.1016/j.vaccine.2005.03.012. [DOI] [PubMed] [Google Scholar]
- 50.Osorio FA, et al. Passive transfer of virus-specific antibodies confers protection against reproductive failure induced by a virulent strain of porcine reproductive and respiratory syndrome virus and establishes sterilizing immunity. Virology. 2002;302(1):9–20. doi: 10.1006/viro.2002.1612. [DOI] [PubMed] [Google Scholar]
- 51.Nielsen TL, et al. Examination of virus shedding in semen from vaccinated and from previously infected boars after experimental challenge with porcine reproductive and respiratory syndrome virus. Vet Microbiol. 1997;54(2):101–12. doi: 10.1016/s0378-1135(96)01272-2. [DOI] [PubMed] [Google Scholar]
- 52.Vanhee M, et al. Development of an experimental inactivated PRRSV vaccine that induces virus-neutralizing antibodies. Vet Res. 2009;40(6):63. doi: 10.1051/vetres/2009046. [DOI] [PubMed] [Google Scholar]
- 53.Dwivedi V, et al. Biodegradable nanoparticle-entrapped vaccine induces cross-protective immune response against a virulent heterologous respiratory viral infection in pigs. PLoS One. 2012;7(12):e51794. doi: 10.1371/journal.pone.0051794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dwivedi V, et al. PLGA nanoparticle entrapped killed porcine reproductive and respiratory syndrome virus vaccine helps in viral clearance in pigs. Vet Microbiol. 2013;166(1–2):47–58. doi: 10.1016/j.vetmic.2013.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Delrue I, Delputte PL, Nauwynck HJ. Assessing the functionality of viral entry-associated domains of porcine reproductive and respiratory syndrome virus during inactivation procedures, a potential tool to optimize inactivated vaccines. Vet Res. 2009;40(6):62. doi: 10.1051/vetres/2009047. [DOI] [PubMed] [Google Scholar]
- 56.Habib M, et al. Inactivation of infectious bursal disease virus by binary ethylenimine and formalin. J Zhejiang Univ Sci B. 2006;7(4):320–3. doi: 10.1631/jzus.2006.B0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim H, et al. The assessment of efficacy of porcine reproductive respiratory syndrome virus inactivated vaccine based on the viral quantity and inactivation methods. Virol J. 2011;8:323. doi: 10.1186/1743-422X-8-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Geldhof MF, et al. Comparison of the efficacy of autogenous inactivated Porcine Reproductive and Respiratory Syndrome Virus (PRRSV) vaccines with that of commercial vaccines against homologous and heterologous challenges. BMC Vet Res. 2012;8:182. doi: 10.1186/1746-6148-8-182. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.