Abstract
Background
This study aimed at evaluating HRCT pulmonary manifestations in children with Common Variable Immunodeficiency (CVID) hospitalized in the Pediatric Ward of Masih Daneshvari Hospital during a 10-year period.
Materials and Methods
This retrospective study evaluated 25 children hospitalized with the diagnosis of CVID in the Pediatric Ward of Masih Daneshvari Hospital from 2001 to 2011 and their pulmonary HRCT scans were evaluated.
Results
The most common pulmonary HRCT findings were lymphadenopathy (66.7%), bronchiectasis (50%), air trapping (33.3%) and peribronchial wall thickening (33.3%). The highest percentage of CT-scan findings was detected in patients aged 13-17 yrs.
Conclusion
Most of the pulmonary changes due to CVID are preventable or treatable. Also, it is possible to prevent irreversible complications of disease if it is diagnosed early. Therefore, HRCT is strongly recommended as an accurate and effective method for monitoring and fast recognition of pulmonary manifestations of the disease especially bronchiectasis which is a very common finding indicative of poor prognosis.
Keywords: Common variable immunodeficiency (CVID), CT scan, HRCT
INTRODUCTION
Primary humoral immunodeficiencies that are characterized by lack of antibodies production are the commonest form of primary immunodeficiencies and are divided into 2 groups of X-linked agammaglobulinemia (Bruton's disease) and common variable immunodeficiency (CVID). Pulmonary changes are present in 60% of patients with primary humoral immunodeficiency (1–3).
Abnormal findings detected through thoracic imaging include non-infectious airway diseases, infections, chronic pulmonary diseases, chronic inflammatory reactions (granulomatosis, interstitial pneumonia) and benign and malignant neoplasms.
Recurrent long-term infections are the main clinical manifestations of primary humoral immunodeficiencies and mostly involve airways (2, 3).
It is the most common diagnosis in adult patients with primary immunodeficiencies (3, 4).
It encompasses a group of genetic disorders and is characterized by the defective production of all types of major antibodies (3, 5).
Airway changes in CVID may occur anywhere in the large or small bronchi. These changes include bronchiectasis, peribronchial wall thickening, mucus accumulation and air trapping (3).
Peribronchial wall thickening and bronchiectasis are the most common pulmonary changes observed in patients with primary humoral immunodeficiency (1, 3, 6, 7).
Involvement of small airways results in respiratory disorders and chronic obstructive pulmonary disease that are almost always irreversible (3, 7, 8, 10). On CT-scan, air trapping is demonstrated as areas of low attenuation and sometimes emphysema or bulla (3).
Previous reports have shown a controversy about which abnormality has to be evaluated or looked for on HRCT in patients with CVID (11–14).
There is still uncertainty about the nature and frequency of CVID-related abnormalities manifesting on CT scan (11).
This study aimed at evaluation of CT-scan findings in patients with CVID hospitalized in the Pediatric Ward of Masih Daneshvari Hospital during 2001-2011.
MATERIALS AND METHODS
This retrospective study evaluated 25 children aged 9 months to 20 yrs. who presented and admitted to the Pediatric Ward of Masih Daneshvari Hospital during the last 10 years and diagnosed with CVID (from 2001 to 2011).
Diagnosis of CVID in the understudy subjects was confirmed using clinical and paraclinical diagnostic methods.
Patients’ lung CT-scans were evaluated and data interpreted by the radiology team of the hospital were entered into the questionnaire and statistically analyzed.
RESULTS
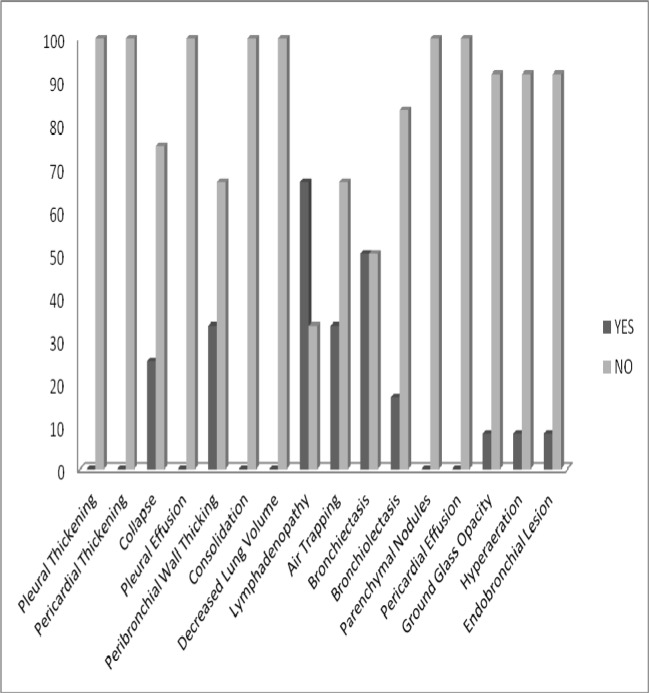
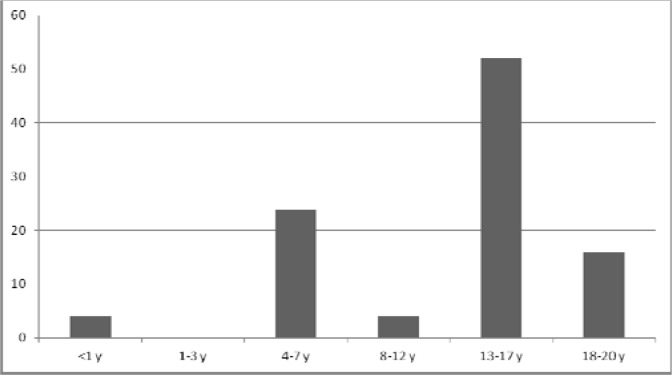
There were 25 children including 15 girls (60%) and 10 boys (40%) with age range of 9 months to 20 years. The most common radiologic findings were detected on lung CT scan of patients aged 13-17 yrs. including lymphadenopathy (66.7%), bronchiectasis (50%), air trapping and peribronchial wall thickening (each 33.3%) (Figure 1, 2).
Figure 1.
Distribution of the pulmonary findings present in HRCT of children with CVID
Figure 2.
Pulmonary CT scan manifestations based on the age distribution of children with CVID
DISCUSSION
All understudy patients were Caucasian with a mean age of 12.27 yrs.
The most common HRCT findings were lymphadenopathy (66.7%), bronchiectasis (50%), air trapping and peribronchial wall thickening (each 33.3%).
In a study performed on 65 Caucasian patients with CVID and a mean age of 48 yrs in Rikshospitalet Hospital (affiliated to Oslo University) in Norway, the most frequent HRCT findings were peribronchial wall thickening (68%), bronchiectasis (57%) and air trapping (54%). In the lung parenchyma, linear and/or irregular opacities (53%), nodules and micro-nodules (51%) were the most common findings (10).
In another study by Gharagozlou et al. (14) peribronchial wall thickening was a more common finding than bronchiectasis. The mentioned two studies in this respect were not in accord with our study finding.
In Bondioni et al. study conducted during 1993-2005 on 45 patients with congenital immunodeficiency (18 patients with agammaglobulinemia and 27 patients with CVID) with a mean age of 22.9 yrs, the most common HRCT findings were bronchiectasis and parenchymal consolidations (each with 64.2% prevalence)(1).
In a study by Costa-Carvalho et al., pulmonary HRCT-scans of 30 patients over the age of 6 yrs including 8 with XLA (X-linked agammaglobulinemia) and 22 with CVID were evaluated. Among 16 patients with chest CT-scan abnormalities, bronchiectasis (12/16) and air trapping (5/16) were the most common findings in patients with antibody deficiencies (15).
Differences between our study results and those of others may be attributed to several factors such as ethnicity, age and sex of the understudy population (demographic characteristics), epidemiologic factors and subjective opinions of different radiologists when interpreting the graphs.
CONCLUSION
CVID is a relatively common disease (1/10,000 to 1/30,000) and pulmonary changes (such as recurrent infections, airway involvement and chronic pulmonary changes) are seen in the majority of patients. However, many of these changes are preventable and treatable if diagnosed early and thus irreversible pulmonary complications can be prevented. Pulmonary HRCT is an accurate and effective means for diagnosis of pulmonary disorders. Therefore, use of this method for monitoring of patients with CVID and prompt diagnosis of pulmonary manifestations of disease (especially bronchiectasis which is among the commonest radiologic findings in CVID and is indicative of a poor prognosis) is strongly recommended.
REFERENCES
- 1.Bondioni MP, Duse M, Plebani A, Soresina A, Notarangelo LD, Berlucchi M, et al. Pulmonary and sinusal changes in 45 patients with primary immunodeficiencies: computed tomography evaluation. J Comput Assist Tomogr. 2007;31(4):620–8. doi: 10.1097/RCT.0b013e31802e3c11. [DOI] [PubMed] [Google Scholar]
- 2.Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: clinical and immunological features of 248 patients. Clin Immunol. 1999;92(1):34–48. doi: 10.1006/clim.1999.4725. [DOI] [PubMed] [Google Scholar]
- 3.Bierry G, Boileau J, Barnig C, Gasser B, Korganow AS, Buy X, et al. Thoracic manifestations of primary humoral immunodeficiency: a comprehensive review. Radiographics. 2009;29(7):1909–20. doi: 10.1148/rg.297095717. [DOI] [PubMed] [Google Scholar]
- 4.Cunningham-Rundles C. Common variable immunodeficiency. Curr Allergy Asthma Rep. 2001;1(5):421–9. doi: 10.1007/s11882-001-0027-1. [DOI] [PubMed] [Google Scholar]
- 5.Oksenhendler E, Gérard L, Fieschi C, Malphettes M, Mouillot G, Jaussaud R, et al. Infections in 252 patients with common variable immunodeficiency. Clin Infect Dis. 2008;46(10):1547–54. doi: 10.1086/587669. [DOI] [PubMed] [Google Scholar]
- 6.Feydy A, Sibilia J, De Kerviler E, Zagdanski AM, Chevret S, Fermand JP, et al. Chest high resolution CT in adults with primary humoral immunodeficiency. Br J Radiol. 1996;69(828):1108–16. doi: 10.1259/0007-1285-69-828-1108. [DOI] [PubMed] [Google Scholar]
- 7.Martínez García MA, de Rojas MD, Nauffal Manzur MD, Muñoz Pamplona MP, Compte Torrero L, Macián V, et al. Respiratory disorders in common variable immunodeficiency. Respir Med. 2001;95(3):191–5. doi: 10.1053/rmed.2000.1020. [DOI] [PubMed] [Google Scholar]
- 8.Cadranel J, Bouvry D, Wislez M. Respiratory manifestations of common variable immunodeficiency in adults. Rev Mal Respir. 2003;20(1 Pt 1):126–33. [PubMed] [Google Scholar]
- 9.Popa V. Airway obstruction in adults with recurrent respiratory infections and IgG deficiency. Chest. 1994;105(4):1066–72. doi: 10.1378/chest.105.4.1066. [DOI] [PubMed] [Google Scholar]
- 10.Gregersen S, Aaløkken TM, Mynarek G, Kongerud J, Aukrust P, Frøland SS, et al. High resolution computed tomography and pulmonary function in common variable immunodeficiency. Respir Med. 2009;103(6):873–80. doi: 10.1016/j.rmed.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 11.Tanaka N, Kim JS, Bates CA, Brown KK, Cool CD, Newell JD, et al. Lung diseases in patients with common variable immunodeficiency: chest radiographic, and computed tomographic findings. J Comput Assist Tomogr. 2006;30(5):828–38. doi: 10.1097/01.rct.0000228163.08968.26. [DOI] [PubMed] [Google Scholar]
- 12.Feydy A, Sibilia J, De Kerviler E, Zagdanski AM, Chevret S, Fermand JP, et al. Chest high resolution CT in adults with primary humoral immunodeficiency. Br J Radiol. 1996;69(828):1108–16. doi: 10.1259/0007-1285-69-828-1108. [DOI] [PubMed] [Google Scholar]
- 13.Kainulainen L, Nikoskelainen J, Ruuskanen O. Diagnostic findings in 95 Finnish patients with common variable immunodeficiency. J Clin Immunol. 2001;21(2):145–9. doi: 10.1023/a:1011012023616. [DOI] [PubMed] [Google Scholar]
- 14.Gharagozlou M, Ebrahimi FA, Farhoudi A, Aghamohammadi A, Bemanian MH, Chavoshzadeh Z, et al. Pulmonary complications in primary hypogammaglobulinemia: a survey by high resolution CT scan. Monaldi Arch Chest Dis. 2006;65(2):69–74. doi: 10.4081/monaldi.2006.567. [DOI] [PubMed] [Google Scholar]
- 15.Costa-Carvalho BT, Wandalsen GF, Pulici G, Aranda CS, Solé D. Pulmonary complications in patients with antibody deficiency. Allergol Immunopathol (Madr) 2011;39(3):128–32. doi: 10.1016/j.aller.2010.12.003. [DOI] [PubMed] [Google Scholar]