Abstract
Background
Cutaneous leishmaniasis (CL) is one of the common tropical protozoal diseases caused by various Leishmania species, and transmitted by the sand-fly vectors, Phlebotomus and Lutzomyia species. Herein, we report for the first time a case of CL that presented as large eczematous plaques occurring on the dorsi of both feet in a Libyan drug addicted, alcoholic patient with HIV infection.
Findings
A 34 year-old HIV-positive, alcoholic, drug addicted Libyan male presented to us with a history of a non-itchy skin lesions on the dorsi of both feet of 5-weeks duration. Systemic and topical antibiotics were given without improvement. Diagnosis of this patient was confirmed by observation of Leishmania amastigote bodies in stained slit-skin smear skin biopsy. After parenteral administration of sodium stiboglyconate (Pentostam) (20 mg/kg/day) for 28 days the lesions did not show any marked improvement. Concurrently, combination therapy of oral rifampicin (600 mg/day) and isoniazide (300 mg/day) was given for 8 weeks. Complete healing of lesions was achieved after this treatment and skin-slit smears turned negative.
Conclusions
Localized cutaneous leishmaniasis should be remembered in deferential diagnosis of unresponsive contact dermatitis especially for HIV-positive patients in CL endemic areas.
This patient was not responding to Pentostam therapy, which is not very common in Libya. Interestingly, combination of oral rifampicin (600 mg/day) and isoniazide (300 mg/day) can be a successful alternative therapy.
Keywords: Cutaneous leishmaniasis, Contact dermatitis, HIV, Sodium stiboglyconate (Pentostam), Libya
Findings
A 34 year-old HIV-positive, alcoholic, drug addicted Libyan male presented to us with a history of non itchy skin lesions on the dorsi of both feet of 5-weeks duration. The lesions started as small non itchy papules which gradually increased in size and then ulcerated with offensive odour. The patient applied warm onion to treat the lesions, which turned painful and for that he sought medical advice. Systemic and topical antibiotics were given without improvement. The patient denied history of trauma, insect bite, unbalanced diabetes, or allergic diseases and no family history of the same illness.
On examination, there were bilateral asymmetrical large well-defined erythematous ulcerated plaques with pus discharge and crusts involving the dorsal surface of both feet and left big toe. Yellowish brown discoloration of the surrounding skin and nails was noticed (Figure 1). In addition, we noticed the presence of painless crusted nodules over the anterior aspect of the right ankle joint and left cheek (Figure 1). No palpable subcutaneous nodules or regional lymph nodes were detected. The patient had a coated tongue and seborrheic dermatitis over his scalp, face and chest. KOH for Candida albicans examination was positive from tongue and negative from nails. Routine laboratory tests showed low leukocyte count (3.5 × 103/ul), lymphopenia (16.6%), low platelets (132 × 103/ul), CD-4 T-cell count was lower than (15/ul), and positive serology for HIV and hepatitis C. Other routine investigations were normal including chest X-ray and ECG. Histopathological features revealed focal hyperkeratosis and focal parakeratosis. Stratum spongiosum showed intercellular oedema, local necrosis, and moderate acanthosis. Dermis showed diffuse and nodular mixed cellular infiltration with many extravasated RBCs (Figure 2). No characteristic tubercular granulomas were seen. The clinical picture was consistent with acute contact dermatitis with secondary bacterial infection. However, a 2 mm punch biopsy and slit-skin smear was obtained from all lesions. Smears were fixed and stained with Giemsa’s stain. Leishmania parasites were heavily seen inside and outside infected macrophages (Figure 2). Molecular identifications of the causative Leishmania species by amplifying the internal transcribed spacer1 (ITS1-PCR) [1] failed due to PCR inhibition problems. After parenteral administration of sodium stiboglyconate (Pentostam) (20 mg/kg/day) for 28 days the lesions did not show any marked improvement, and skin-slit smears were positive for Leishmania parasites after this period. The patient was referred to the infectious department for antiretroviral therapy and further HIV care. Concurrently, combination therapy of oral Rifampicin (600 mg/day) and Isoniazide (300 mg/day) was given for 8 weeks. Complete healing of lesions was achieved after this treatment and skin-slit smears turned negative (Figure 1).
Figure 1.

Painless crusted nodule over left cheek at angle of mandible and bilateral asymmetrical large well-defined erythematous ulcerated plaques with crusts over dorsi of feet (left images). Complete healing after two months treatment by Rifampicin and Isoniazide (right images).
Figure 2.
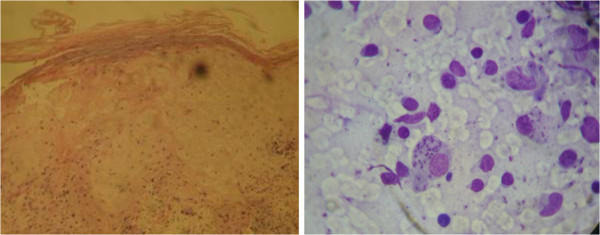
Intra-and extra cellular Leishmania parasites as shown in Giemsa-stained slit-skin smear (Left). Histopathological findings of lesions obtained from dorsal surface of right foot (right).
Cutaneous leishmaniasis (CL) is one of the common tropical protozoal diseases caused by various Leishmania species, and transmitted by the sand-fly vector of Phlebotomus and Lutzomyia species. About 1.5 million new cases are reported each year, and over 350 million people live in areas of active parasite transmission [2–5]. CL is a major public health problem in Libya caused by L. major and L. tropica [6]. Leishmania species can cause a wide spectrum of cutaneous lesions such as localized cutaneous, muco-cutaneous, diffuse cutaneous, or post-kala-azar dermal leishmaniasis [7, 8]. In HIV-positive patients: asymptomatic and mucosal leishmaniasis has been reported in addition to other usual types [9]. However, HIV-positive intravenous drug users (IVDUs) can be infected with Leishmania by sharing of contaminated syringes and needles [9]. Clinical variation of leishmaniasis –HIV co-infection is determined by parasite species and host cell mediated immunity (CMI) response [2]. Recently, clinical variants of CL with or without HIV co-infection have been reported such as; sporotrichoid, psoriasiform, warty, erysipeloid, impetigo like, cold cellulitis, zosteriform, acneiform, and eczematoid variant [10–12]. The incidence of eczematoid variant of localized CL seems not to be very common and reported to be 2.3% [11].
Herein, we report for the first time a case of Pentostam unresponsive CL that presented as large eczematous plaques occurring on the dorsi of both feet in a Libyan drug addicted patient with HIV infection. Localized CL typically presented as papules, nodules, plaques, ulcerated or crusted nodules. A contact dermatitis like morphology of localized CL lesions is unusual. Diagnosis of CL was confirmed by observation of parasites in stained slit-skin smears. This patient was unresponsive to Pentostam, which is not very common in Libya. Combination therapy of oral rifampicin and isoniazide completely cured the lesions. This combination therapy is used in Libya to treat cutaneous tuberculosis and to treat CL cases unresponsive to parenteral administration of Pentostam [6]. A previous study by Peters et al. [13] descried a striking remission of CL in a Brazilian patient by using this combination. Small scale studies on oral rifampicin treatment of CL have shown a healing rate of 73.9%, 75% and 83.3% [14–16] respectively. However, no clinical trial was carried out to approve combination therapy of rifampicin and isoniazide in treatment of CL [13].
The patient denied insect bites though he came from Gabel Garby where CL is endemic, possibly the patient was unnoticeably bitten during drug and alcohol intake.
According to ethical approval of this study, the patient agreed to publish his photos and case history anonymously. Written informed consent was obtained from the patient. The study was revised and approved by (Research Ethics committee, University of Tripoli, Libya).
Conclusion
The learning points from this short report is that localized cutaneous leishmaniasis should be considered in differential diagnosis of unresponsive contact dermatitis especially for HIV-positive patients in CL endemic areas. A combination of oral rifampicin (600 mg/day) and isoniazide (300 mg/day) can be successful alternative therapy for Pentostam unresponcive CL patients in Libya. However, this combination therapy has to be assessed at a larger scale.
Footnotes
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HA and AA designed the study, AG, AMM and SE investigated the patient and have done the clinical evaluation and laboratory tests. AA and HA have done the molecular experiments. HA and AA have written the manuscript. All authors read and approved the final version of the manuscript.
Contributor Information
Hamida Al-Dwibe, Email: ahmadymm@hotmail.com.
Aisha Gashout, Email: a-gashout@hotmail.com.
Abdu-Maged Morogum, Email: al-dwibeh@yahoo.co.uk.
Said El-Zubi, Email: al-dwibeh@yahoo.co.uk.
Ahmad Amro, Email: aamro@pharm.alquds.edu.
References
- 1.Schonian G, Nasereddin A, Dinse N, Schweynoch C, Schallig HD, Presber W, Jaffe CL. PCR diagnosis and characterization of Leishmania in local and imported clinical samples. Diagn Micr Infect Dis. 2003;47(1):349–358. doi: 10.1016/S0732-8893(03)00093-2. [DOI] [PubMed] [Google Scholar]
- 2.Chaudhary RG, Bilimoria FE, Katare SK. Diffuse cutaneous leishmaniasis: co-infection with human immunodeficiency virus (HIV) Indian J Dermatol Venereol Leprol. 2008;74(6):641–643. doi: 10.4103/0378-6323.45111. [DOI] [PubMed] [Google Scholar]
- 3.Hepburn NC. Cutaneous leishmaniasis: an overview. J Postgrad Med. 2003;49(1):50–54. doi: 10.4103/0022-3859.928. [DOI] [PubMed] [Google Scholar]
- 4.WHO technical report seriesControl of the Leishmaniases 2010. (949):xii-xiii, 1–186, back cover [PubMed]
- 5.Alvar J, Velez ID, Bern C, Herrero M, Desjeux P, Cano J, Jannin J, den Boer M. Leishmaniasis worldwide and global estimates of its incidence. PLoS One. 2012;7(5):e35671. doi: 10.1371/journal.pone.0035671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Amro A, Gashout A, Al-Dwibe H, Zahangir Alam M, Annajar B, Hamarsheh O, Shubar H, Schonian G. First molecular epidemiological study of cutaneous leishmaniasis in Libya. PLoS NTD. 2012;6(6):e1700. doi: 10.1371/journal.pntd.0001700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Manzur A, Butt UA. Atypical cutaneous leishmaniasis resembling eczema on the foot. Dermatol Online J. 2006;12(3):18. [PubMed] [Google Scholar]
- 8.WHO publicationsManual for case management of cutaneous leishmaniasis in the WHO Eastern Mediterranean Region 2012, 9–18.
- 9.Puig L, Pradinaud R. Leishmania and HIV co-infection: dermatological manifestations. Ann Trop Med Parasitol. 2003;97(Suppl 1):107–114. doi: 10.1179/000349803225002589. [DOI] [PubMed] [Google Scholar]
- 10.Kubba R, Al-Gindan Y, el-Hassan AM, Omer AH. Clinical diagnosis of cutaneous leishmaniasis (oriental sore) J Am Acad Dermatol. 1987;16(6):1183–1189. doi: 10.1016/S0190-9622(87)70155-8. [DOI] [PubMed] [Google Scholar]
- 11.Momeni AZ, Aminjavaheri M. Clinical picture of cutaneous leishmaniasis in Isfahan. Iran Int J Parasitol. 1994;33(4):260–265. doi: 10.1111/j.1365-4362.1994.tb01039.x. [DOI] [PubMed] [Google Scholar]
- 12.Cabello I, Caraballo A, Millan Y. Leishmaniasis in the genital area. Rev Inst Med Trop Sao Paulo. 2002;44(2):105–107. doi: 10.1590/S0036-46652002000200009. [DOI] [PubMed] [Google Scholar]
- 13.Peters W, Lainson R, Shaw JJ, Robinson BL, Leao AF. Potentiating action of rifampicin and isoniazid against Leishmania mexicana amazonensis. Lancet. 1981;1(8230):1122–1124. doi: 10.1016/S0140-6736(81)92296-0. [DOI] [PubMed] [Google Scholar]
- 14.Even-Paz Z, Weinrauch L, Livshin R, El-On J, Greenblatt CL. Rifampicin treatment of cutaneous leishmaniasis. Int J Dermatol. 1982;21(2):110–112. doi: 10.1111/j.1365-4362.1982.tb00517.x. [DOI] [PubMed] [Google Scholar]
- 15.Kochar DK, Aseri S, Sharma BV, Bumb RA, Mehta RD, Purohit SK. The role of rifampicin in the management of cutaneous leishmaniasis. QJM. 2000;93(11):733–737. doi: 10.1093/qjmed/93.11.733. [DOI] [PubMed] [Google Scholar]
- 16.Bumb RA, Mehta RD. Oral rifampicin in cases of cutaneous leishmaniasis with multiple lesions (a pilot study) Indian J Dermatol Venereol Leprol. 2002;68(5):272. [PubMed] [Google Scholar]


