Abstract
This randomized controlled pilot trial tested a 6-week mindfulness-based intervention in a sample of pregnant women experiencing high levels of perceived stress and pregnancy anxiety. Forty-seven women enrolled between 10 and 25 weeks gestation were randomly assigned to either a series of weekly Mindful Awareness Practices (MAPS) classes (n = 24) with home practice or to a reading control condition (n = 23). Hierarchical linear models of between-group differences in change over time demonstrated that participants in the mindfulness intervention experienced larger decreases from pre-to post-intervention in pregnancy-specific anxiety and pregnancy-related anxiety than participants in the reading control condition. However, these effects were not sustained through follow-up at six weeks post-intervention. Participants in both groups experienced increased mindfulness, as well as decreased perceived stress and state anxiety over the course of the intervention and follow-up periods. This study is one of the first randomized controlled pilot trials of a mindfulness meditation intervention during pregnancy and provides some evidence that mindfulness training during pregnancy may effectively reduce pregnancy-related anxiety and worry. We discuss some of the dilemmas in pursuing this translational strategy and offer suggestions for researchers interested in conducting mind-body interventions during pregnancy.
Keywords: Pregnancy, Meditation, Mindfulness, Prenatal Stress, Pregnancy Anxiety
Prenatal maternal stress is significant because of increasingly strong evidence that women who experience high stress or anxiety during pregnancy are more likely to deliver preterm or low birth-weight infants (for reviews see Dunkel Schetter, 2011; Dunkel Schetter & Glynn, 2010; Dunkel Schetter & Lobel, 2012). These adverse birth outcomes are a pressing public health issue in some countries, especially the United States where the national rates of preterm birth and low birth weight average 13% and 8% respectively (Hamilton, Hoyert, Martin, Strobino, & Guyer, 2013). In addition to increasing the likelihood of adverse birth outcomes, prenatal maternal stress has been linked to a variety of negative effects on fetal development, and cognitive, emotional, and developmental outcomes in infancy and childhood (Davis et al., 2004; Davis et al., 2007; DiPietro et al., 2010; DiPietro et al., 2002; Van den Bergh et al., 2005).
Despite mounting evidence that prenatal maternal stress and anxiety present risks to the mother and the baby, few stress-reduction programs have been tested in randomized controlled trials in pregnancy. Preliminary evidence from the limited number of studies exploring mind-body approaches to prenatal maternal stress reduction suggest that progressive muscle relaxation, yoga, and meditation may be helpful for improving maternal psychological well-being and perinatal outcomes (see Beddoe & Lee, 2008 for a review). However, these studies are typically limited by methodological flaws, such as lack of a control group or random assignment, use of nonspecific samples of all consenting pregnant women regardless of risk, and failure to measure process variables. Inclusion of a control group is essential in strong intervention studies, and it is especially important for prenatal stress-reduction interventions to have a randomized design and control group because women’s levels of stress and anxiety may systematically vary across the nine month developmental period of pregnancy (Glynn et al., 2001; Lederman et al., 2004; Roesch et al., 2004). Since women’s levels of anxiety tend to decline across pregnancy even without intervention (Dunkel Schetter & Robbins, 2011), significant effects found using an uncontrolled pretest-posttest design may reflect maturation effects rather than the efficacy of the intervention itself. To demonstrate the potential utility of a particular intervention, it is therefore necessary to assess changes over time for individuals who are randomly assigned to either a treatment or control group, and to show significantly greater changes over time among participants in the treatment group as compared to participants in the control group.
In order to address the scarcity of empirically-tested prenatal maternal stress reduction interventions, we designed a randomized controlled study to evaluate the effects of an existing mindfulness meditation program in a sample of pregnant women who were experiencing elevated levels of stress. Mindfulness refers to a process that cultivates a mental state of awareness and acceptance of present moment experiences, including one’s current sensations, thoughts, bodily states, and environment. In addition to inducing states of relaxation, mindfulness emphasizes not ‘getting caught up’ in emotional reactions and has been shown to aid in affect regulation by moderating emotional reactivity and speeding recovery from unpleasant emotional experiences (Brown et al., 2007). Derived from Buddhist traditions, secular interventions that aim to cultivate the quality of mindfulness commonly provide systematic training in mindfulness meditation as a self-regulation approach to reducing stress and managing difficult emotions (Bishop, 2002). For example, mindfulness-based stress-reduction (MBSR) interventions were developed by Jon Kabat-Zinn in 1979 to help individuals adapt to medical illness (Kabat-Zinn, 2003). Such mindfulness-based approaches are increasingly attracting the attention of health researchers, including those who study pregnancy, because of their demonstrated efficacy in reducing anxiety and psychological distress and improving health outcomes for diverse populations facing a variety of stress-related and medical conditions, including depression, cancer, and HIV (e.g. Creswell et al., 2009; Davidson et al., 2003; Grossman et al., 2004; Smith et al., 2005).
Four uncontrolled pilot trials of mindfulness training for pregnant women have found generally positive effects, including improvements in perceived stress, depressive symptoms, anxiety, and reports of physical pain (Beddoe et al., 2009; Duncan & Bardacke, 2010; Dunn et al., 2012; Muzik, Hamilton, Rosenbulm, Waxler, & Hadi, 2012). One randomized controlled trial of mindfulness training during pregnancy also showed improvements in anxiety and negative affect relative to a wait-list control, although these effects were no longer significant at 3 months post-intervention (Vieten & Astin, 2008). However, the present literature on mindfulness training during pregnancy does not support general conclusions about the efficacy of this stress-reduction approach due to a lack of methodologically rigorous studies.
We sought to address the limitations of the previous research on mindfulness training during pregnancy by targeting participants who were experiencing elevated levels of stress at study entry and utilizing a randomized design with a control condition. We hypothesized that the mindfulness intervention would provide strategies for managing stress and negative emotions, thus contributing to greater decreases in general anxiety, perceived stress, and pregnancy-related anxiety and greater increases in mindfulness as compared to women assigned to a reading control condition.
Method
Participants
This study was approved by the UCLA Institutional Review Board (IRB). Participants were a volunteer sample of pregnant women recruited at a university clinic that primarily serves privately-insured women who receive prenatal care from a large group of physicians and midwives in accordance with American College of Obstetrics & Gynecology standards.. During clinic hours, medical staff introduced potentially eligible patients to research staff, who described the study using a standard verbal script and administered preliminary screening questionnaires. Participants were also recruited through fliers describing the study and listing eligibility criteria that were distributed and displayed at the faculty practice and in locations around the UCLA campus. Women were eligible to participate if they: (1) were pregnant and between 10 and 25 weeks gestation with a singleton pregnancy, (2) could speak and read English fluently, (3) were over the age of 18, (4) were willing and able to attend the 6-week mindfulness course, (5) were willing and able to provide informed consent, and (6) were experiencing elevated levels of perceived stress or pregnancy-specific anxiety, as indicated by responses to the Perceived Stress Scale (PSS) and the Pregnancy-Specific Anxiety scale (PSA) on a screening questionnaire. Women were eligible to participate if their total scores were above 34 on the PSS or 11 on the PSA; these cutoffs reflect mean scores on these measures during the first trimester in an earlier population-based study that demonstrated effects of elevated prenatal maternal stress on timing of delivery (Roesch et al., 2004).
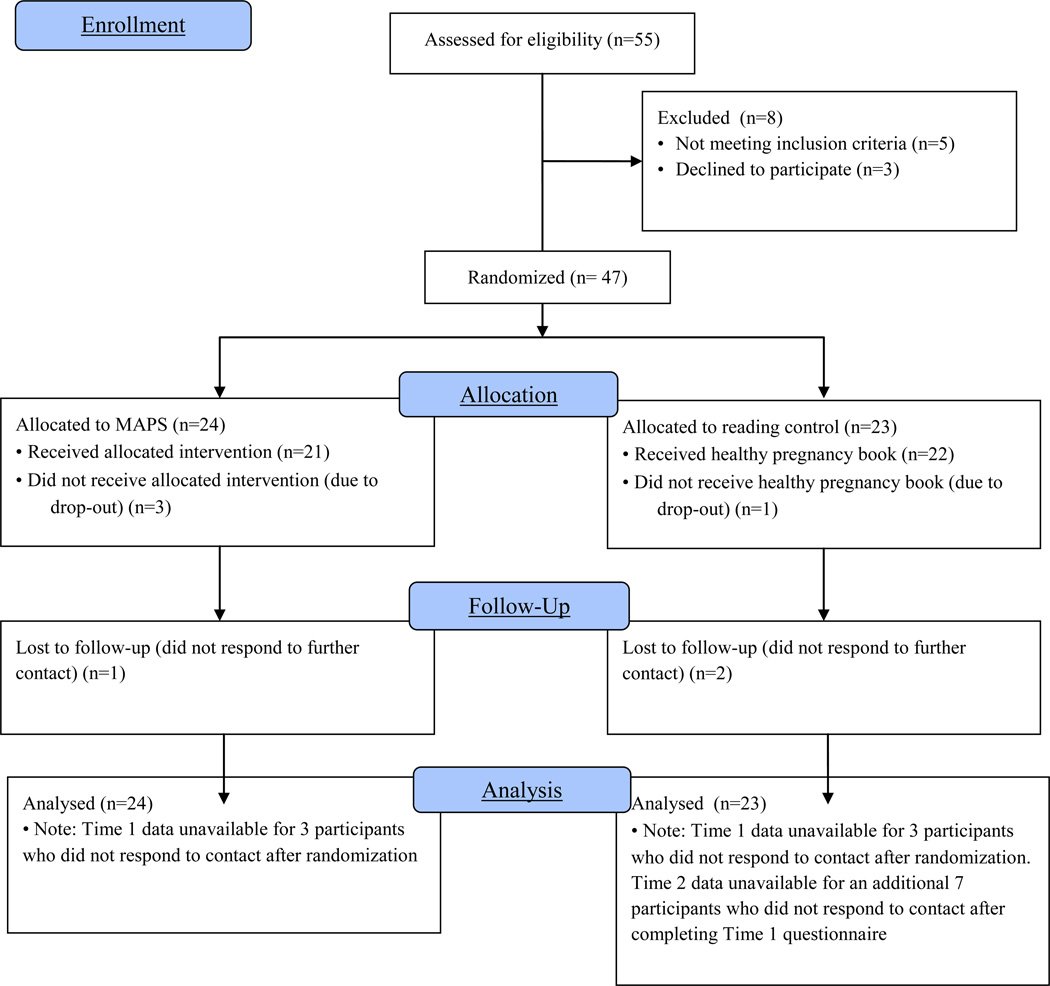
Screening, eligibility, and drop-out rates are presented in Figure 1. We approached 126 potentially eligible women in the UCLA clinic; 31 of these women agreed to participate and provided informed consent. Women who declined most frequently cited lack of time, scheduling conflicts, childcare concerns, and living too far away from the class location as reasons for not wishing to participate. An additional 24 women telephoned (n=11) or e-mailed (n=13) the researcher after viewing the recruitment flier. Of the 55 women who were recruited from the waiting room and fliers, 47 completed the baseline questionnaire and were randomized to either MAPS (n=24) or control (n=23), five were ineligible due to low stress, and three declined to participate. All 47 participants had scores above our screening criteria (>34) on the PSS and 31 of the 47 women had scores above our screening criteria (>11) on the pregnancy-specific anxiety measure. Of the 47 women who were randomized, three women in the mindfulness group and one woman in the control group chose to leave the study after randomization (three women withdrew for personal reasons and one woman withdrew for medical reasons) and an additional three participants were lost to follow-up and did not complete Time 1 questionnaires (one in MAPS and one in control).
Figure 1.
CONSORT diagram showing flow of participants
A majority of the 47 study participants were White (66%), had completed a four-year university degree (89%), and were married or living with a partner (93.5%). The sample was primarily primiparous (78%), with the remaining 10 women having given birth prior to their current pregnancy. None of the participants had a history of delivering preterm or low birth weight infants. On a standard health history form, 30% of the participants self-reported a previous diagnosis of depression, 31% had been diagnosed with an anxiety disorder, and 10% had been diagnosed with another psychological disorder (e.g. ADD). Participants were an average of 33.13 years old (SD=4.79) and reported a mean gestational week of 17.78 weeks (SD=5.10) at baseline.
Procedure
After determination of eligibility, study participants were asked to complete the baseline questionnaire using an online survey instrument (www.surveymonkey.com). The baseline (Time 0) assessment occurred for all participants during the two weeks prior to the start of the intervention for the MAPS group. After completion of the baseline questionnaire, participants were randomly assigned to either the intervention (MAPS) or control group using a computerized randomization scheme. On-line questionnaires were also completed at post-intervention (Time 1) and six weeks later (Time 2).
Intervention group
Participants assigned to the intervention group were telephoned and informed that they had been assigned to the study group that would attend mindfulness classes. They were given a choice of class time (morning or evening) and were enrolled in the next scheduled 6-week series of 2-hour MAPS classes at the UCLA Semel Institute’s Mindful Awareness Research Center (MARC).d This course series is entirely secular in nature and is designed to provide a comfortable atmosphere for all participants regardless of their spiritual beliefs and backgrounds. Participants were enrolled in the center’s ongoing classes, and the series they attended included members of the UCLA community and general public who were not pregnant or enrolled in this study. Enrolling participants in ongoing classes provided several advantages in addition to cost effectiveness. First, this approach allowed us to enroll participants in the mindfulness classes on a rolling basis. Due to the time sensitive nature of conducting interventions during early pregnancy, we needed aimed to enroll participants in mindfulness classes as quickly as possible after randomization. Because the ongoing mindfulness classes are held every six weeks, participants were able to begin classes more promptly than if we had waited until sufficient numbers of women had been recruited and randomized to the mindfulness condition before beginning a class series. A second advantage was that these classes were open to the general public and thus participants did not attend classes consisting solely of other research participants and/or pregnant women which potentially served to minimize the non-specific effects of social contact with other pregnant women inherent in a group-based prenatal intervention.
Each class series was led by one of three trained instructors following a curriculum outlined in a standardized instructor’s manual (see Table 1 for description of each week’s content). Participants were trained in the practice of mindfulness meditation and its applications to daily life through participation in instructor-led group meditations, lectures about mindfulness practices, and discussions, which allowed participants to share their experiences with one another and for the instructor to address participant questions. To record attendance, participants signed in upon entry to the classroom.
Table 1.
Content of the Mindful Awareness Practices (MAPs) program
| Session number |
Focus of session |
|---|---|
| 1 | What is Mindfulness? Introductory lecture, seated meditation, grape eating meditation, setting up a home practice |
| 2 | Embodiment and Obstacles Obstacles lecture (recognizing sleepiness, restlessness, doubt, craving and aversion), walking meditation listening meditation, breath/body/sound meditation |
| 3 | Working with Pain Science lecture on mindfulness research, working with pain lecture, ice cube meditation, body scan/pain meditation |
| 4 | Working with Difficult Emotions Emotions lecture, emotions meditation, lovingkindness lecture, lovingkindness meditation |
| 5 | Working with Thoughts, Mindful Interactions Thoughts lecture, thoughts meditation, mindful interactions lecture, interactions practice in dyads |
| 6 | Wrap-up Questions & Answers, 30 minute meditation period, closing council, lovingkindness meditation |
At the beginning of the class series, each participant was given a compact disc with recordings of instructor-guided meditations to use at home, and provided with homework assignments each week (daily meditations ranging from 5 to 17 minutes). Participants learned mindfulness meditation practices including sitting and walking meditations, and how to work with difficult thoughts and emotions. Prior to the start of the class series, intervention participants received six weekly diaries to use in recording time spent engaged in at-home mindfulness practice along with six prepaid envelopes which they used to return the diaries at the end of each week.
Control group
Women in the control group were telephoned, informed that they had been assigned to the reading group and then mailed a copy of the book You and Your Baby: Pregnancy authored by Laura Riley, M.D and published in 2006. This book covers each trimester of pregnancy in a week-by-week format and also includes information about labor and delivery, feeding, and postpartum and baby care. We selected this book after reviewing several similar pregnancy books because of its clear, concise content and the strong reputation of the author in the field of obstetrics. Through reading the book, women in the control group had the opportunity to learn about important aspects of healthy pregnancy, including stress management.
Measures
Mindfulness
Mindfulness was assessed using the Five Factor Mindfulness Questionnaire (Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006), a 39-item measure based on a factor analytic study of five independently developed mindfulness questionnaires. The measure assesses five conceptual facets of mindfulness: observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience on a scale ranging from 1 (almost always) to 6 (almost never). Cronbach’s α for the overall scale ranged at each of the three time points ranged between 0.86 and 0.94 in the present sample.
Perceived stress
Perceived stress was measured using the 14-item version of the Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983). This scale measures the perceived unpredictability and uncontrollability of general life stress using items such as ‘how often have you felt you were effectively coping with important changes that were occurring in your life?’ and ‘how often have you been upset because of something that happened unexpectedly?’ Participants were asked to indicate how frequently they had felt each way ‘over the past seven days (including today) on a scale ranging from 1 (never) to 5 (always). Cronbach’s α at each of the three time points ranged from 0.87 to 0.90 in the present sample.
Prenatal stress/anxiety
In order to assess participants’ baseline and post-treatment levels of prenatal anxiety, we administered a brief 4-item scale measuring Pregnancy-Specific Anxiety (PSA; Roesch et al., 2004). Study participants were prompted to think about how they felt about being pregnant and then asked to indicate how often they had felt anxious, concerned, afraid or panicky in the last week on a scale ranging from 1 (never) to 5 (always). Cronbach’s α at each of the three time points ranged from 0.74 to 0.85 in the present sample.
We also administered the Pregnancy-Related Anxiety scale (PRA; Rini, Dunkel-Schetter, Wadhwa, & Sandman, 1999), which consists of 10 items assessing the frequency or extent of participant worry or concern about their health, their baby’s heath, labor and delivery, and caring for a baby during the previous seven days on a scale ranging from 1 (never or not at all) to 4 (a lot of the time or very much). Sample items include ‘I am concerned (worried) about how the baby is growing and developing inside me’ and ‘I am afraid that I will be harmed during delivery.’ Cronbach’s α at each of the three time points ranged between 0.76 and 0.87 in the present sample.
General Anxiety
General anxiety was measured using the 20-item State Anxiety Scale from Spielberger, Gorsuch, and Lushene’s (1970) State-Trait Anxiety Inventory. Items assessed the extent to which participants experienced feelings of apprehension, tension, nervousness, and worry during ‘the last 7 seven days, including today’ by using a 4-point scale ranging from 1 (not at all) to 4 (very much). Cronbach’s α at each of the three time points ranged between 0.90 and 0.92 in the present sample.
Adherence
Adherence to the intervention was assessed by class attendance and time spent engaged in mindfulness meditation outside of class sessions. To record attendance, participants were asked to sign in upon entry to the classroom each week. Participants also completed and returned weekly practice diaries throughout the duration of the class series. At the end of the six week intervention period, participants in the reading control group were asked to report if they had read the book and, if so, how much time they had spent reading it at each of the follow-up points.
Demographic and medical risk variables
We included a comprehensive demographic and medical history questionnaire at baseline in order to gather sociodemographic and medical risk information. Sociodemographic variables included self-identified race/ethnicity, age, income, education, employment, and marital and cohabitation status. Medical risk variables included a number of possible risk conditions including medical history (e.g., diabetes) and pregnancy history (e.g., complications of pregnancy).
Statistical analyses
To assess success of randomization, we examined group differences at baseline using t-tests for continuous variables and chi-square tests for categorical variables. Two-level hierarchical linear model (HLM) analyses were performed using Stata 12 to assess the effects of the intervention on changes in stress and anxiety over time (Rabe-Hesketh & Skrondal, 2008). This technique allows for the determination of between-person differences (i.e., group assignment) in within-person trajectories (i.e. changes in mindfulness, stress and anxiety over time). We selected this analytic strategy because the HLM procedure weights cases with complete data more heavily, but all cases are included when estimating effects allowing us to utilize data from those participants who completed assessments at Time 0 but not at Time 1 and/or Time 2. Though HLM is often used to conduct growth curve analyses when repeated measurements are conducted on more than three occasions, these models tested linear effects because repeated measures were collected at only three time points.
Separate two-level linear models were run for each of the outcome variables. Level-1 captured parameters that change within an individual. Time-invariant, between-individual predictors were introduced at level 2. These level-2 variables included group assignment as well as covariates. We also included a group X time interaction term to determine if change across time varied as a function of group assignment. Time was centered at baseline so that intercepts represented the mean on each variable prior to randomization. After estimating the models for each of the outcome variables, Wald tests were used to test the significance of the overall time and group X time coefficients. The results of these postestimation tests are reported as chi-square statistics below, with significant chi-squares indicating that coefficients are significantly different from zero at the p<.05 level.
Results
Baseline Comparisons by Study Condition
Examination of baseline psychological characteristics revealed that there were no significant differences between the reading control and mindfulness intervention groups on any of the dependent variables (see Table 2). No group differences were observed on any demographic characteristics (i.e., age, ethnicity, employment status, marital status, educational level, parity).
Table 2.
Unadjusted group means on outcome measures at baseline (Time 0), post-intervention (Time 1), and six week follow-up (Time 2)
| Measure | Value for Group | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Intervention | Control | |||||||||||
| Baseline | Time 1 | Time 2 | Baseline | Time 1 | Time 2 | |||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| STAI | 45.69 | 7.64 | 39.47 | 6.27 | 38.11 | 8.78 | 44.37 | 10.98 | 37.35 | 11.51 | 36.19 | 10.84 |
| PSS | 41.81 | 6.00 | 37.30 | 5.38 | 36.17 | 5.90 | 39.91 | 8.55 | 35.80 | 8.01 | 37.42 | 7.27 |
| PRA | 24.42 | 3.79 | 22.70 | 3.84 | 20.65 | 5.10 | 23.22 | 4.95 | 22.65 | 5.93 | 20.15 | 4.72 |
| PSA | 11.63 | 2.96 | 7.65 | 1.73 | 9.20 | 2.35 | 10.70 | 2.79 | 8.95 | 3.00 | 9.00 | 2.23 |
| FFMQ | 119.64 | 13.04 | 134.24 | 15.48 | 132.68 | 16.58 | 123.61 | 16.41 | 134.66 | 20.17 | 136.73 | 23.00 |
Potential Confounding Variables
Before conducting primary analyses, we assessed a number of potential confounding variables that might explain some of the variance observed in psychological outcomes. Women who had previous live births had marginally lower scores on the PSS, PSA, and STAI at Times 0, 1 or 2 (all t-tests significant at p<.10). Thus, parity was controlled in subsequent analyses.
Adherence
Of the twenty-four women who were randomized to MAPS, twenty women attended the mindfulness meditation classes and completed Time 1 and Time 2 questionnaires. Women attended an average of 4.75 (SD=1.07) of the 6 classes. Twenty percent attended all 6 classes (n=4), 55% attended 5 classes (n=11), 10% attended 4 classes (n=5), 10% attended 3 classes (n=5), and 2.5% attended only 2 of the classes (n=1). During the first three weeks of the class series, women reported practicing the techniques taught in class an average of 4.2 days per week for 9 minutes per day. During the last three weeks, they practiced an average of 3.25 days per week for 10 minutes per day.
The control group consisted of 23 women, 22 of whom received a copy of the healthy pregnancy book and 20 of whom completed Time 1 questionnaires. All but one of the control group participants reported reading or referring to the book during the first six weeks after they received it. On average, participants read or referred to the book for 2.63 hours (SD=2.89) over the six weeks. Seven participants in the control group did not complete the post-intervention questionnaire that was administered six-weeks after the first follow-up (Time 2). Participants who completed the Time 1 but not the Time 2 questionnaire did not differ from the remaining members of the control group on any demographic characteristics or baseline variables, except that those who did not complete the final questionnaire entered the study later in their pregnancies and were randomized at an average of 21 weeks gestation (SD=3.93) while those who did complete the final questionnaire were randomized at an average of 16 weeks gestation (SD=4.83).
Baseline correlations
We first examined the associations between dispositional mindfulness and psychological variables at Time 0. In the full sample, FFMQ scores were negatively correlated with PSS (r=−.59, p<.0001) and STAI (r=−.46, p<.001), such that women who reported higher levels of mindfulness had lower perceived stress and general anxiety. Correlations between baseline FFMQ scores and baseline PRA (r=−.26) and PSA (−.23) were not statistically significant.
Psychosocial Changes over Time by Intervention Condition
Unadjusted mean scores on all outcome variables for the mindfulness intervention and control groups at baseline (Time 0), post-intervention follow-up (Time 1), and six weeks later (Time 2) are given in Table 1.
Change from baseline to post-intervention
We hypothesized that participation in the MAPS classes would result in decreased perceived stress (PSS), pregnancy-related anxiety (PRA), pregnancy-specific anxiety (PSA), and general state anxiety (STAI). Consistent with hypotheses, a significant group X time interaction was found in the model predicting the PSA-time slope (χ2(2)=8.73 p=.01). Posthoc probing of the interaction revealed a significantly larger decrease in PSA scores in the mindfulness group (b=−4.25, p<.05) than in the control group (b=−1.61, p<.05) between Time 0 and Time 1. These intervention effects were not sustained through Time 2 assessment, such that there was a significant decrease in pregnancy-specific anxiety from baseline to 6 week follow-up in both the intervention group (b=−2.62, p<.05) and in the control group (b=−1.90, p<.05), with no significant difference between the two slopes.
There was also a marginally significant group X time interaction in the model predicting change in PRA scores over time, χ2(2)=5.41, p=0.07. Posthoc analyses showed a significant decrease in PRA scores in the mindfulness group (b=−2.08, p<.05) but not in the control group (b=−.44) between Time 0 and Time 1. However, these effects were not sustained through Time 2 assessment; pregnancy-related anxiety significantly decreased in both the intervention (b=−3.90, p<.05) and control groups (b=−3.92, p<.05) from baseline to 6 week follow-up.
Contrary to hypotheses, no significant group X time interactions were found in models predicting change in PSS, STAI, or FFMQ (all p’s<0.10). However, there was a significant main effect of time in the FFMQ, χ2(2)=18.26, p<.0001, PSS, χ2(2)=0.69, p<.05; STAI, χ2(2)=13.09, p=.001; and PA, χ2(2)=13.77, p=.001 models, such that both groups experienced significant decreases in perceived stress and general anxiety and significant increases in mindfulness from Time 0 to Time 1 and from Time 0 to Time 2.
Discussion
This study was a randomized controlled trial of mindfulness meditation training in a sample of pregnant women screened for elevated levels of perceived stress and pregnancy-related anxiety in the first or second trimesters of their pregnancies. The mindfulness intervention led to greater declines in pregnancy-specific anxiety and pregnancy-related anxiety from baseline to post-intervention in comparison to a reading control condition. Perceived stress and state anxiety also declined in the mindfulness intervention group while mindfulness increased in the intervention group; however, these changes were not significantly different from changes in the control group.
Why didn’t women in the intervention group show greater changes on all of the outcome variables compared to women in the control group? Perhaps because eligibility criteria for the study required screening for high stress levels as well as willingness and ability to attend a weekly mindfulness class if randomized to that condition. Thus, participants in both groups may have already been conscious of and motivated to reduce their high levels of prenatal stress or anxiety such that when informed they were not randomized to the treatment, women in the control group may have made efforts to manage stress and anxiety on their own. In fact, 30% of participants in the control group reported at the study’s end that they took a prenatal yoga class during their pregnancies.
The use of a reading control condition in this study also presents the possibility that these materials reduced stress in the control group, not necessarily directly through learning stress management but by gaining greater knowledge about pregnancy. For ethical reasons, we wanted to give women who were high in stress/anxiety at the study’s outset and who agreed to participate more than simply usual care. Although the written materials did not contain explicit instructions in stress management techniques, the book presented a great deal of information about pregnancy, labor and delivery, and parenting in an accessible way that could have been anxiety reducing. Thus providing this resource to women in the control group for ethical reasons may have inadvertently contributed to their reduced levels of perceived stress and state anxiety. Improvements in the control group may also have occurred as a result of the well-documented and normal attenuation of affective and physiological stress responsivity over the course of pregnancy (Glynn et al., 2001).
Unexpectedly, mindfulness also increased significantly over time in both the intervention and control groups. This pattern could be due to measurement effects, as completing two extensive questionnaires on mindfulness may have primed participants to become more aware of their thoughts, emotions, and behaviors. Yet suggestion alone seems unlikely. Another possibility is that the experience of pregnancy contributes to increases in dispositional mindfulness. Because longitudinal data including these measures are not available in pregnancy, we cannot compare these changes to the trajectory that would be expected during pregnancy in general but the psychological changes that occur for women of this demographic profile may involve becoming calmer and more thoughtful about life as pregnancy progresses. A final point is that the mindfulness classes that participants attended were designed as an educational program for the general community, not a clinical treatment for anxiety, depression or any other physical or mental health condition and perhaps not as powerful as necessary to produce large effects among individuals experiencing high levels of distress.
Although there were not consistent effects across the full set of outcome variables considered in this exploratory study, the declines in pregnancy-related anxiety and pregnancy-specific anxiety among participants in the mindfulness intervention group over the 6-week intervention period are notable because increasingly strong evidence suggests that anxiety concerning a pregnancy may be particularly risky for mothers and babies (Lobel et al., 2008; Kramer et al, 2009; Mancuso, Schetter, Rini, Roesch, & Hobel, 2004; Orr, Reiter, Blazer, & James, 2007). Interventions that effectively reduce pregnancy-linked anxiety are empirically justifiable for women at risk of adverse birth outcomes. However, given that the effects of mindfulness training on pregnancy anxiety and worry were not sustained for 6 weeks after the intervention had ended, future interventions might consider a more powerful dose of mindfulness training and possibly an adaptation for pregnancy to directly address common sources of worry during pregnancy. For example, women who are fearful about labor and delivery might benefit from additional instruction in mindfulness-based pain management techniques. Several women in the intervention group provided feedback suggesting that a class geared specifically to pregnant women would have been more helpful. As one participant wrote: ‘It would be nice to have more of a focus on applying mindfulness techniques to pregnancy related issues in order to cope better (i.e. morning sickness, bloating, anxiousness about the birth) and to apply mindfulness to cope with the pain of labor and delivery.’ Thus, a mindfulness-based course that combines mindfulness training with information and coping methods regarding pregnancy, childbirth, and parenting concerns is more likely to optimize maternal well-being during this unique and important reproductive interval. Such interventions are currently being piloted by some researchers and may be a promising avenue for future randomized controlled trials (Beddoe et al., 2009; Duncan & Berdacke, 2010; Vieten & Astin, 2008).
This pilot study also revealed some of the difficulties that can occur in recruiting participants for stress reduction interventions during pregnancy. A majority of the women approached during recruitment were unwilling to participate in the mindfulness intervention due to lack of time, scheduling conflicts, childcare issues, and commuting distance to classes. These barriers to enrollment were very common even in the relatively affluent population that we attempted to recruit, suggesting that an intervention requiring regular weekly attendance may not be feasible for low income women who may face even greater demands with fewer resources during pregnancy. To overcome these barriers to enrollment, a practical intervention is needed, one that can be accessed perhaps by training in the clinic and then practiced at home. One option might be brief mindfulness training, such as a one-day intensive retreat with support for subsequent at-home practice, with the caveat that strong incentives to practice and monitoring are essential. In this study, participants generally demonstrated good attendance at the mindfulness classes, with 85% of participants attending 4 or more of the 6 class sessions, but there were no significant correlations between the number of class sessions attended or amount of time spent practicing outside of class with change on outcome variables. This lack of a dose-response effect is consistent with a review of 30 studies evaluating MBSR intervention programs that found no difference in effect sizes between total number of in-class hours (range 6–28 hours) and psychological outcome variables (Carmody & Baer, 2009). While longer interventions provide participants with the incentive to practice, and the opportunity to discuss mindfulness skills with an instructor and other students, the advantages of additional class time must be weighed against the possibility that longer interventions may impose greater barriers to the pregnant women who could benefit most. In fact, the sooner in pregnancy an intervention like this is started, the more likely it is to have effects and interventions of long duration cannot be started late in pregnancy or they risk attrition due to early delivery. These factors are critical for researchers to consider in future intervention study planning. Based on the findings of this study, we conclude that interventions integrating childbirth and parenting education may make the most of the limited time that pregnant women have available to invest in stress management training, and that powerful short dose interventions for those who begin them mid pregnancy may be worth consideration.
Nonetheless, the moderate-to-high levels of perceived stress and pregnancy-related anxiety reported by all but a few potential participants on screening questionnaires confirmed the need to equip this population with effective stress management strategies. It was somewhat unexpected that more than 90% of the women screened were eligible due to high scores and fewer than 10% of the women we screened were ineligible due to their low scores on the screening questionnaire, The criteria we set for eligibility were based on the sample means reported in a large study of pregnant women in the same region assessed during the first trimester. One possible explanation for the small number of ineligible women is women experiencing low levels of stress may have been less likely to consent to screening and self selected out, thus our figures are not indicative of this site or general levels of anxiety and stress in prenatal care. If screening is done routinely in prenatal care settings, better estimates can be obtained. Because the protocol approved by the IRB required us to consent participants prior to screening, we do not know how our sample compared to the larger population of women receiving care in this clinic. Researchers planning similar trials may benefit from conducting pilot testing to establish population norms for their recruitment sites prior to screening and enrolling participants in intervention studies.
Our study has notable limitations. The relatively small size of the sample in this pilot trial provided limited power to detect significant differences between groups especially given the positive changes over time in both the control and intervention groups but funding did not permit conduct of a larger pilot study. Several nonsignificant effects were in the predicted direction, yet failed to reach statistical significance. While inclusion of a control group is a strength of the study design, we did not include a third arm of usual care to control for possible placebo effects in the reading condition. This pilot study also has limited generalizability, as the sample was largely White, educated, and of medium to high socioeconomic status.
In sum, stress, anxiety and specific worries about a pregnancy are now well documented as posing risk for women and their babies (Dunkel Schetter, 2011). Many researchers are suggesting that the popular mindfulness-based meditation intervention methods that have shown efficacy in other contexts be applied in pregnancy. This pilot trial of mindfulness-based stress reduction during pregnancy demonstrates some of the strengths and weaknesses of such an approach. First, the acceptability of the intervention for at least some women was illustrated, as well as the inaccessibility for others. Second, the effects of mindfulness training on two measures of distress specific to pregnancy were demonstrated, but not on other general psychological measures. The results of this pilot trial suggest that brief mindfulness training alone may not be a powerful enough intervention to consistently reduce levels of perceived stress and anxiety during pregnancy. While learning and practicing mindfulness may be a useful life skill for many women, a more powerful approach to reducing prenatal maternal stress is probably necessary if the ultimate aim of such interventions is to reduce risk of adverse birth outcomes. The results suggest that although mindfulness may provide some benefits, researchers and clinicians should continue to consider other treatment approaches that may be more appropriate and effective for reducing stress among pregnant women.
Acknowledgments
This research was supported by funds from the UCLA Academic Senate and the UCLA Center for the Study of Women. Christine M. Guardino was supported by National Institute of Mental Health Training Grant #15750. Thank you to the Dunkel Schetter and Stanton research labs for constructive comments on the research design and manuscript.
Footnotes
Fees for enrollment in the MAPS classes were reduced through arrangement with the UCLA Mindful Awareness Research Center and were paid directly from study funds. Participants did not pay any fees for attending the classes.
References
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13:27–25. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Beddoe AE, Lee KA. Mind-body interventions during pregnancy. Journal of Obstetric, Gynecologic and Neonatal Nursing. 2008;37(2):165–175. doi: 10.1111/j.1552-6909.2008.00218.x. [DOI] [PubMed] [Google Scholar]
- Beddoe AE, Yang CP, Kennedy HP, Weiss SJ, Lee KA. The effects of mindfulness-based yoga during pregnancy on maternal psychological and physical distress. Journal of Obstetric, Gynecologic and Neonatal Nursing. 2009;38(3):310–319. doi: 10.1111/j.1552-6909.2009.01023.x. [DOI] [PubMed] [Google Scholar]
- Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine. 2002;64(1):71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM, Creswell JD. Mindfulness: theoretical foundations and evidence for its salutary effects. Psychological Inquiry. 2007;18(4):211–237. [Google Scholar]
- Carmody J, Baer R. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. Journal of Clinical Psychology. 2009;65(6):627–638. doi: 10.1002/jclp.20555. [DOI] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Creswell JD, Myers HF, Cole SW, Irwin MR. Mindfulness meditation training effects on CD4+ T lymphocytes in HIV-1 infected adults: A small randomized controlled trial. Brain Behavior and Immunity. 2009;23(2):184–188. doi: 10.1016/j.bbi.2008.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65:564–570. doi: 10.1097/01.psy.0000077505.67574.e3. [DOI] [PubMed] [Google Scholar]
- Davis EP, Glynn LM, Dunkel Schetter C, Hobel C, Chicz-Demet A, Sandman CA. Prenatal exposure to maternal depression and cortisol influences infant temperament. Journal of American Academy of Child and Adolescent Psychiatry. 2007;46(6):737–746. doi: 10.1097/chi.0b013e318047b775. [DOI] [PubMed] [Google Scholar]
- Davis EP, Snidman N, Wadhwa PD, Glynn LM, Dunkel Schetter C, Sandman CA. Prenatal maternal anxiety and depression predict negative behavioral reactivity in infancy. Infancy. 2004;6(3):319–331. [Google Scholar]
- DiPietro JA, Hilton SC, Hawkins M, Costigan KA, Pressman EK. Maternal stress and affect influence fetal neurobehavioral development. Developmental Psychology. 2002;38(5):659–668. [PubMed] [Google Scholar]
- DiPietro JA, Kivlighan KT, Costigan KA, Rubin SE, Shiffler DE, Henderson JL, Pillion JP. Prenatal antecedents of newborn neurological maturation. Child Development. 2010;81(1):115–130. doi: 10.1111/j.1467-8624.2009.01384.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan LG, Bardacke N. Mindfulness-based childbirth and parenting education: Promoting family mindfulness during the perinatal period. Journal of Child and Family Studies. 2010;19(2):190–202. doi: 10.1007/s10826-009-9313-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- Dunn C, Hanieh E, Roberts R, Powrie R. Mindful pregnancy and childbirth: Effects of a mindfulness-based intervention on women’s psychological distress and well-being in the perinatal period. Archives of Women’s Mental Health. 2012;15:139–143. doi: 10.1007/s00737-012-0264-4. [DOI] [PubMed] [Google Scholar]
- Dunkel Schetter C, Glynn LM. Stress in Pregnancy: Empirical Evidence and Theoretical Issues to Guide Interdisciplinary Research. In: Contrada R, Baum A, editors. Handbook of Stress. New York: Springer; 2011. [Google Scholar]
- Dunkel Schetter C, Lobel M. Pregnancy and birth: a multilevel analysis of stress and birth weight. In: Revenson TA, Baum A, Singer J, editors. Handbook of Health Psychology. 2nd ed. London: Psychol. Press; 2012. [Google Scholar]
- Dunkel Schetter C, Robbins CM. Correlates and Predictors of Pregnancy-Related Anxiety. In: Davis E, editor. The Developmental Consequences of Prenatal Maternal Stress and Anxiety; Symposium conducted at the meeting of the Western Psychological Association; Los Angeles, California. 2011. Apr, [Google Scholar]
- Glynn LM, Wadhwa PD, Dunkel-Schetter C, Chicz-DeMet A, Sandman CA. When stress happens matters: Effects of earthquake timing on stress responsivity in pregnancy. American Journal of Obstetrics and Gynecology. 2001;184(4):637–642. doi: 10.1067/mob.2001.111066. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Hamilton BE, Hoyert DL, Martin JA, Strobino DM, Guyer B. Annual summary of vital statistics: 2010–2011. Pediatrics. 2013;131(3):548–558. doi: 10.1542/peds.2012-3769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology Science and Practice. 2003;10(2):144–156. [Google Scholar]
- Kramer MS, Lydon J, Seguin L, Goulet L, Kahn SR, McNamara H, et al. Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. American Journal of Epidemiology. 2009;169(11):1319–1326. doi: 10.1093/aje/kwp061. [DOI] [PubMed] [Google Scholar]
- Lederman S, Rauh V, Weiss L, Stein J, Hoepner L, Becker M, Perera F. The effects of the World Trade Center event on birth outcomes among term deliveries at three lower Manhattan hospitals. Environmental Health Perspectives. 2004;112(17):1772–1778. doi: 10.1289/ehp.7348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobel M, Cannella DL, Graham JE, DeVincent C, Schneider J, Meyer BA. Pregnancy-specific stress, prenatal health behaviors, and birth outcomes. Health Psychology. 2008;27(5):604–615. doi: 10.1037/a0013242. [DOI] [PubMed] [Google Scholar]
- Mancuso RA, Dunkel Schetter C, Rini CM, Roesch SC, Hobel CJ. Maternal prenatal anxiety and corticotropin-releasing hormone associated with timing of delivery. Psychosomatic Medicine. 2004;66(5):762–769. doi: 10.1097/01.psy.0000138284.70670.d5. [DOI] [PubMed] [Google Scholar]
- Muzik M, Hamilton S, Rosenblum KL, Waxler E, Hadi Z. Mindfulness yoga during pregnancy for psychiatrically at-risk women: Preliminary results from a pilot feasibility study. Complemenary Therapies in Clinical Practice. 2012;18:235–240. doi: 10.1016/j.ctcp.2012.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr ST, Reiter JP, Blazer DG, James SA. Maternal prenatal pregnancy-related anxiety and spontaneous preterm birth in Baltimore, Maryland. Psychosomatic Medicine. 2007;69(6):566–570. doi: 10.1097/PSY.0b013e3180cac25d. [DOI] [PubMed] [Google Scholar]
- Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using Stata. 2nd ed. College Station, TX: Stata Press; 2008. [Google Scholar]
- Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: The role of personal resources, stress, and sociocultural context in pregnancy. Health Psychology. 1999;18:333–345. doi: 10.1037//0278-6133.18.4.333. [DOI] [PubMed] [Google Scholar]
- Roesch SC, Dunkel Schetter C, Woo G, Hobel CJ. Modeling the types and timing of stress in pregnancy. Anxiety, Stress and Coping. 2004;17(1):87–102. [Google Scholar]
- Smith JE, Richardson J, Hoffman C, Pilkington K. Mindfulness-based stress reduction as supportive therapy in cancer care: systematic review. Journal of Advanced Nursing. 2005;52(3):315–327. doi: 10.1111/j.1365-2648.2005.03592.x. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch I, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1970. [Google Scholar]
- Van den Bergh BRH, Mulder EJH, Mennes M, Glover V. Antenatal maternal anxiety and stress and the neurobehavioural development of the fetus and child: Links and possible mechanisms. A review. Neuroscience and Biobehavioral Reviews. 2005;29(2):237–258. doi: 10.1016/j.neubiorev.2004.10.007. [DOI] [PubMed] [Google Scholar]
- Vieten C, Astin J. Effects of a mindfulness-based intervention during pregnancy on prenatal stress and mood: Results of a pilot study. Archives of Women’s Mental Health. 2008;11(1):67–74. doi: 10.1007/s00737-008-0214-3. [DOI] [PubMed] [Google Scholar]