Abstract
Objective:
The association between alcoholism in parents and related disorders in their offspring is well established in cultures with intermediate/high alcohol consumption, but not in those with low consumption, such as Israel. This study investigated differences in parental transmission of alcohol problems and related psychopathology between immigrants from the former Soviet Union (FSU) to Israel and other Israelis—two Israeli subgroups with differing alcohol consumption behaviors and social norms.
Method:
A total of 1,347 adults from a household sample were interviewed. Regression analyses were used to examine associations between parental alcohol problems and participant disorders: alcohol, nicotine, and cannabis use disorders (AUD, NUD, CUD); antisocial personality disorder (ASPD); major depressive disorder (MDD); and posttraumatic stress disorder (PTSD). We also examined the associations of parental alcohol problems with participant disorders characterized with two latent factors: externalizing (EXT: AUD, NUD, CUD, ASPD) and internalizing (INT: MDD, PTSD). Differential parental transmission of alcohol problems in FSU (n = 315) and non-FSU (n = 1,032) Israelis was examined with statistical interaction.
Results:
Among emigrants from the FSU, parental alcohol problems predicted AUD, NUD, CUD, ASPD, PTSD, EXT, and INT (mean ratios = 1.38–4.83). In non-FSU Israelis, parental alcohol problems predicted only ASPD and PTSD (mean ratios = 1.08–4.09). Significant interactions were observed for AUD, CUD, PTSD, and EXT; each relationship was stronger in FSU Israelis and null (AUD, CUD, EXT) or less robust (PTSD) in other Israelis.
Conclusions:
Parental alcohol problems were related to substance use and psychiatric disorders differently in FSU and other Israelis, two groups with different alcohol consumption levels and drinking norms. We propose that, in social contexts that vary in the degree to which they constrain alcohol behavior, underlying genetic predispositions may manifest as different disorders.
Offspring of parents with alcohol problems are more likely to develop alcohol use disorders (AUDs; Cotton, 1979; Dinwiddie and Reich, 1991; Sher et al., 1991). The etiology of AUDs is complex, with approximately 50%–70% of the risk attributed to genetic factors (Heath et al., 1997). Other risk factors for AUDs can include adverse family environments characterized by disruption, deviant parental role models, and/or inadequate parenting (Enoch, 2006). Because of the shared liability of mental and substance use disorders (Kendler et al., 2003; Krueger et al., 2002), a parental history of alcohol problems also broadly predisposes individuals to other psychopathology, including other substance use disorders, antisocial personality, depression, and anxiety disorders.
Mounting evidence indicates that, in social contexts that limit deviant behaviors (such as heavy alcohol use), genetic influences on those behaviors are attenuated, whereas in less limiting contexts, genetic influences are stronger (Dick and Kendler, 2012; Shanahan and Hofer, 2005). Parental history of alcohol problems has been shown to predict offspring psychopathology in populations with moderate to high per capita alcohol consumption (Sher et al., 1991; van der Zwaluw et al., 2008). But it has not been examined in populations with historically low consumption, such as Israel (Harkin et al., 1997; World Health Organization, 2011).
For several reasons, the epidemiology of alcohol consumption and problems in Israel provides a unique opportunity to examine parental transmission of liability to AUD and other psychopathology under contrasting social contexts. First, alcohol use and social norms related to alcohol in that country have changed over the past 20 years (Hasin et al., 1998; Jaffe et al., 2009; Sznitman et al., 2013). Specifically, compared with earlier years (Levav et al., 1993), cohorts in more recent years are drinking (and using other drugs such as cannabis) more frequently and showing evidence of more alcohol-related problems (Sznitman et al., 2013). These increases in drinking and related problems (Spivak et al., 2007) have the potential to alter parental transmission of alcohol and other related psychopathology in Israelis. Additionally, during the 1990s, events in the former Soviet Union (FSU) precipitated a large-scale immigration to Israel. Since 1989, Israel has absorbed more than 900,000 emigrants from the FSU, increasing the country’s population by ∼16% (Central Bureau of Statistics, 2009). Emigrants from the FSU migrated from a country with one of the world’s highest alcohol consumption levels to a country with much lower per capita alcohol consumption than most Western countries (Harkin et al., 1997; World Health Organization, 2011). Many FSU immigrants have preserved aspects of their culture, attitudes, and behaviors, including considerably greater alcohol consumption and more permissive social norms regarding drinking than other Israelis (Hasin et al., 1998, 2002; Rahav et al., 1999; Remennick, 2002; Schiff et al., 2005; Shmulewitz et al., 2012). Thus, the contrasting drinking-related social contexts of the FSU immigrants and other Israelis would be expected to differ in the degree to which they limit deviant behaviors related to heavy drinking, consequently altering influences on these behaviors.
These ethnic and epidemiological (i.e., age cohort) differences in alcohol consumption and drinking norms may differentially affect the parental transmission of liability for psychiatric and substance use disorders in subgroups (i.e., FSU vs. non-FSU Israelis) of the Israeli population. To our knowledge, no study has explicitly compared the association of parental history of alcohol problems and offspring disorders in two population subgroups exposed to contrasting cultural influences regarding alcohol (e.g., consumption patterns, social norms). Thus, FSU immigrants to Israel and other Israelis provide a unique opportunity to examine the impact of such contextual differences.
In the present study, we first examined the relationship between parental alcohol problems and the risk for offspring psychiatric and substance use disorders in a household sample of Israelis. Next, to test the hypothesis that different social contexts for FSU and non-FSU Israelis could underlie differences in transmission of liability, we examined group differences in these relationships between FSU and non-FSU Israelis by testing for statistical interaction. Given the high degree of comorbidity among substance use and psychiatric disorders, we also examined the distribution of two latent factors reflecting externalizing spectrum disorders and internalizing spectrum disorders and their association with parental history of alcohol problems. Furthermore, we explored an alternate explanation for our results, that immigration-related experiences, which in some cases can influence alcohol use and psychopathology (Borges et al., 2010; Bourque et al., 2012), could underlie differential transmission of liability. Finally, because differences have sometimes been found in the offspring psychopathology associated with paternal or maternal alcoholism (Coffelt et al., 2006; Dinwiddie and Reich, 1991; Sher et al., 1991), we explored this aspect of family history.
Method
Study procedures and sample
Data were collected in 2007-2009 from 1,349 adult household residents as described elsewhere (Shmulewitz et al., 2012). This sample was designed to investigate genetic and environmental influences on alcohol-related traits (Shmulewitz et al., 2012). Adults of Jewish ethnicity (to maximize homogeneity) were selected by the Israeli Bureau of the Census from the Israeli Population Register. The Population Register covers household residents in all areas of Israel; potential respondents were selected directly from the register based on demographic characteristics and area of residence. Men were oversampled because addressing the study goals would have been difficult in Israeli women, who have very low rates of drinking (Shmulewitz et al., 2010). Interviewers received structured training and administered face-to-face computer-assisted interviews after obtaining written informed consent as approved by relevant institutional review boards (Shmulewitz et al., 2010). The overall response rate was 68.9%. Quality control included field observation, review of recorded interviews, and telephone verification of responses. Data from 1,347 participants were used in the present study, after excluding two participants with missing data on biological parents. For these participants, ages ranged from 21 to 67 years (M = 41.2, SD = 13.0); 76.3% (n = 1,030) were male; and 23.4% (n = 315) were emigrants from the FSU.
Among participants originally from the FSU, the mean age at immigration was 24 (range: 1–54, SD = 14); 54.9% did not live in Israel before age 18; more than three quarters (77.3%) immigrated to Israel with at least one of their parents; and 60% immigrated to Israel with both parents.
Measures
Participants were interviewed with the Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDA-DIS), a fully structured instrument designed for experienced lay interviewers (Grant et al., 1995), which has been used in large epidemiological studies internationally (Hasin et al., 1997).
Substance use and psychiatric disorders
We assessed common psychiatric disorders using count indicators of the number of lifetime disorder criteria endorsed (disorder severity), consistent with recent trends to use more informative dimensional variables rather than binary traits (Hasin et al., 2012). Lifetime criteria were used because parental history is associated with psychiatric disorders throughout the life course.
Substance use disorders.
The measures of alcohol use disorder (AUD), nicotine use disorder (NUD), and cannabis use disorder (CUD) have been described previously (AUD: Shmulewitz et al., 2010; NUD: Shmulewitz et al., 2011; CUD: Walsh et al., 2014). Lifetime Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR), criteria (American Psychiatric Association, 2000) were assessed using the AUDADIS (Grant et al., 2003). AUD was assessed among lifetime drinkers (at least one drink, n = 1,169, 86.8%); NUD among lifetime smokers (≥100 cigarettes, n = 734, 54.4%); and CUD among lifetime users (ever used, n = 322, 23.9%). Individuals who had never used the substance were coded as zero for disorder severity. The AUDADIS alcohol and drug dependence diagnoses have demonstrated good to excellent test-retest reliability (κ = .67–.84) in clinical and general population samples (Hasin et al., 2007, 2012) and good to excellent convergent, discriminant, and construct validity in samples within the United States (Demyttenaere et al., 2004; Hasin et al., 1997, 1998) and internationally (Canino et al., 1999). Maxdrinks, or the maximum number of drinks consumed per day, was assessed with the AUDADIS (Grant et al., 1995; Hasin et al., 2007) adapted for the present study. The AUDADIS measure of maxdrinks has very good interrater reliability (intraclass correlation coefficients of .70 [Hasin et al., 2007]).
Major depressive disorder and posttraumatic stress disorder.
Assessment of major depressive disorder (MDD) has been described previously (Shoval et al., 2014). In brief, lifetime DSM-IV criteria for MDD were assessed using the major depression module from the PRISM (Psychiatric Research Interview for Substance Use and Mental Disorders; Hasin et al., 2006) among individuals who had experienced at least 2 weeks of depressed mood or anhedonia (n = 483, 35.8%). The PRISM shows good to excellent test-retest reliability for MDD diagnosis in clinical (κ = .64–.87) samples. Posttraumatic stress disorder (PTSD) has been described previously (Walsh et al., 2014). In brief, lifetime DSM-IV criteria for PTSD were assessed using AUDADIS among individuals who reported experiencing a serious traumatic event (n = 1,127, 84.2%). This scale has shown good (κ = .66) test-retest reliability in previous research (Grant et al., 1995). Individuals who were not assessed for a mood disorder or PTSD were coded as zero for disorder severity.
Antisocial personality disorder.
DSM-IV criteria for antisocial personality disorder (ASPD) were assessed among all respondents, using the AUDADIS. ASPD criteria consisted of 15 DSM-IV conduct disorder criteria with onset before age 15 years and 7 adult antisocial behavior criteria (e.g., repeatedly performing acts that are ground for arrest, deceitfulness, lack of remorse) since age 15. Test-retest reliability of the AUDADIS-IV ASPD diagnosis is excellent (κ = .79) (Grant et al., 2003) and compares favorably with results using semistructured personality interviews in treatment samples (Zimmerman et al., 2004). Convergent validity of ASPD has been shown to be good to excellent (Compton et al., 2005).
Latent trait structure.
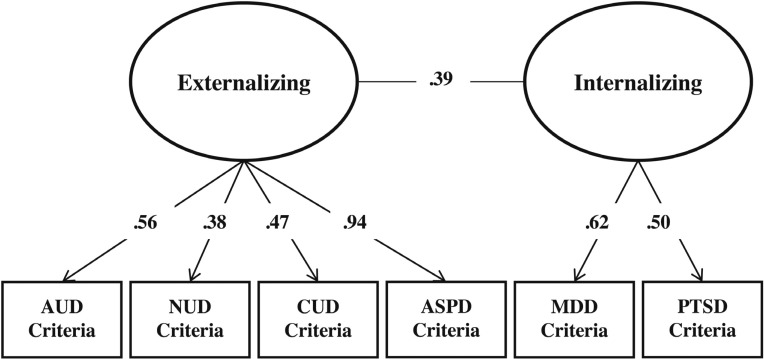
Using the established meta-structure for these disorders (Kendler et al., 2003; Krueger et al., 2002), we created an externalizing (EXT) factor (AUD, NUD, CUD, ASPD) and an internalizing (INT) factor (MDD, PTSD), using confirmatory factor analysis in Mplus (Muthén and Muthén, 2002). A two-factor solution provided an excellent fit to the data (Tucker–Lewis index = .99; comparative fit index = .99; root mean square error of approximation = .02). In this sample, EXT is largely influenced by ASPD, moderately by AUD, and slightly less so by CUD and NUD (factor loadings: 0.94, 0.56, 0.47, 0.38, respectively). Factor loadings for INT are 0.62 for MDD and 0.50 for PTSD. Factor structure and loadings are depicted in Figure 1.
Figure 1.
Factor structure of substance use and psychiatric disorders by in 1,347 Israeli household adults. Notes: Values are standardized factor loadings (all significant p < .001); the externalizing spectrum and internalizing spectrum latent factors are related (Pearson correlation = .39). AUD = alcohol use disorder; NUD = nicotine use disorder; CUD = cannabis use disorder; ASPD = antisocial personality disorder; MDD = major depressive disorder; PTSD = posttraumatic stress disorder.
Parental history of alcohol problems
Parental histories of alcohol problems were assessed using the AUDADIS module, which followed the module evaluating the respondent’s own AUD history. In the parental history module, interviewers read examples of the respective diagnostic criteria, including readily observable manifestations of the disorder, because these are most likely to be known to offspring (Andreasen et al., 1977; Heiman et al., 2008; Slutske et al., 1996). Then the interviewers asked separately about whether respondents’ biological father or mother experienced the condition as defined. The AUDADIS family history of AUD measure has excellent test-retest reliability (Dawson and Grant, 1998). Binary variables were created representing parental history of alcohol problems for either father or mother, because the frequency of participants with a maternal-only history of alcohol problems (n = 35; 2.6%) was too low for separate analysis.
Immigration-related experiences
The difficulty of the immigration experience for FSU Israelis was assessed with the following response options: easier than expected (14.5%), about what I expected (34.7%), harder than expected (34.1%), and I did not have expectations (16.8%). Reasons for immigrating (possible indicators of selection into immigration) were assessed by asking, “What were your main reasons for moving from the FSU to Israel?” The most frequently endorsed responses were (a) parents decided to immigrate to Israel (46.3%), (b) wanted the children to have a better life financially (26.0%), and (c) fear of anti-Semitism in the country where I was living (19.0%).
Statistical analyses
First, we examined the mean number of lifetime disorder criteria (severity) in the full sample and the significant differences in mean severity and latent factor (EXT, INT) scores by demographic characteristics previously shown to influence risk for substance and psychiatric disorders in this sample (sex, age, and FSU immigrant status; Shmulewitz et al., 2010, 2011). These analyses were conducted using Kruskal–Wallis tests in SAS Version 9.3 (SAS Institute Inc., Cary, NC). Next, the associations of parental history of alcohol problems with each offspring psychiatric and substance use disorder (severity) were assessed using zero-inflated negative binomial regression models, adjusted for sex and age. The appropriate distribution for disorder severity phenotypes was determined using traditional fit statistics (Akaike’s Information Criterion, difference in chi-square) for the data modeled using normal, Poisson, negative binomial, and zero-inflated distributions; data best fit the zero-inflated negative binomial. The latent factors (EXT and INT) were analyzed using linear regression, because they are normally distributed (M = 0, SD = 1).
To determine whether parental transmission differed significantly between FSU and non-FSU Israelis, we assessed interaction between parental history of alcohol problems and FSU status on the additive scale, because additive interactions reflect the current conceptual understanding of biological interaction and causal synergism (Spiegelman and Hertzmark, 2005; Spiegelman et al., 2007). Additive interaction was assessed by including an interaction term (Parental History × FSU Status) in separate zero-inflated negative binomial regression models (Spiegelman and Hertzmark, 2005) for each disorder severity outcome. These analyses were performed in proc GENMOD using SAS 9.3 (SAS Institute, Inc., Cary, NC). A structural equation-modeling framework conducted in Mplus (Muthén and Muthén, 2002) was used for the association and interaction analyses involving the latent EXT and INT factors. The estimate for the interaction term (Parental History × FSU Status) represented the interaction contrast (IC), a “difference in differences” effect. This “difference in differences” was evaluated as follows. First, the mean difference in participant disorder severity between FSU and other Israelis was evaluated among those with a parental history of alcohol problems. Next, this difference was evaluated among those without a parental history of alcohol problems. Last, the IC—that is, the difference in these two mean differences—was evaluated to determine whether the effect of parental alcohol problems was greater among Israelis who emigrated from the FSU compared with Israelis who did not. Likelihood ratio chi-square tests were used to assess the statistical significance of the IC and the mean differences.
Exploratory analyses
To explore an alternate explanation for the study results—that immigration-related experiences explained the observed differences in transmission of liability between FSU immigrants and other Israelis—we investigated the effects of immigration-related variables on the primary association/interaction analysis.
First, we explored whether there was a post-immigration increase in AUD severity. FSU Israelis were asked whether there was there ever a period before they immigrated to Israel when they drank more heavily than in the past 12 months. Forty percent of the FSU Israeli participants who responded to this question said “yes” and continued to answer interview questions about drinking behaviors before immigration. Similarly, FSU Israelis were asked whether there was a period since they immigrated to Israel when they drank more heavily than in the past 12 months. Twenty-eight percent of the FSU Israeli participants who responded to this question said “yes” and continued to answer questions about drinking behaviors since immigration. Because drinking increases among those immigrating before age 18 would be expected because they were entering the age of risk for regular drinking and drinking problems (Hasin et al., 2007), we conducted analyses separately in participants who immigrated to Israel before age 18 (41.5%) and at age 18 or later (54.9%). Post-immigration drinking increases in those immigrating after age 18 could be attributed to immigration. This exploration was conducted in SAS with paired-sample t tests comparing AUD severity of FSU immigrants before and after immigration to Israel among those who immigrated to Israel before age 18 and after age 18.
Second, we repeated the primary analyses replacing lifetime with current criteria scores, given the potential interpretation that the current criterion may better reflect drinking-related problems in Israel (after immigration). Third, to assess effects of immigration difficulty on the differential associations of parental history of alcohol problems and psychopathology between FSU immigrants and other Israelis, we repeated the primary analyses, adjusting for the immigration difficulty variable. Fourth, to assess the effects of possible migration-related selection bias on the differential associations, we repeated the primary analyses, adjusted for each of the individual reasons for immigration.
Last, to assess whether these participants with a maternal-only history of alcohol problems affected the main results, we conducted post hoc analyses that paralleled the primary analyses, excluding the 35 participants with a maternal-only history of alcohol problems.
Results
Descriptive information
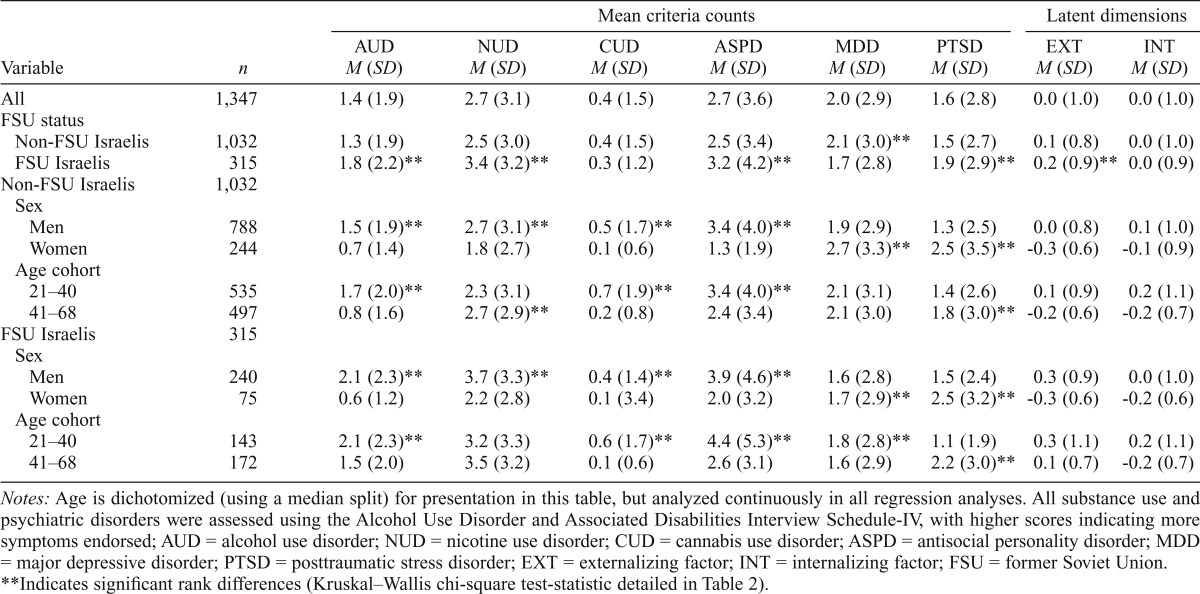
For each substance use and psychiatric disorder, the mean number of criteria endorsed is shown in Table 1. In the full sample (N = 1,347), means of AUD, NUD, CUD, and ASPD criteria were higher in males (p < .001), whereas means of MDD and PTSD criteria were higher in females (p < .001). Higher AUD, NUD, ASPD, and PTSD means, and lower means of MDD criteria, were endorsed by FSU Israelis compared with non-FSU Israelis (p < .001). Similarly, the externalizing latent factor (EXT) showed a higher mean in FSU Israelis (p < .001). Although age was analyzed continuously in all regression analyses, we dichotomized age in Table 1 to display age differences in disorder criteria severity. Mean criteria counts for AUD, CUD, ASPD, and EXT were significantly higher in younger (ages 21–40) than in older (ages 41-68) participants (p < .001), whereas NUD, PTSD, and INT were significantly greater in older participants (p < .001) (Table 1 and Table 2).
Table 1.
Mean criteria counts for lifetime substance use and psychiatric disorders by key demographics in 1,347 Israeli household adults
| Variable | n | Mean criteria counts |
Latent dimensions |
||||||
| AUD M (SD) | NUD M (SD) | CUD M (SD) | ASPD M (SD) | MDD M (SD) | PTSD M (SD) | EXT M (SD) | INT M (SD) | ||
| All | 1,347 | 1.4 (1.9) | 2.7 (3.1) | 0.4 (1.5) | 2.7 (3.6) | 2.0 (2.9) | 1.6 (2.8) | 0.0 (1.0) | 0.0 (1.0) |
| FSU status | |||||||||
| Non-FSU Israelis | 1,032 | 1.3 (1.9) | 2.5 (3.0) | 0.4 (1.5) | 2.5 (3.4) | 2.1 (3.0)** | 1.5 (2.7) | 0.1 (0.8) | 0.0 (1.0) |
| FSU Israelis | 315 | 1.8 (2.2)** | 3.4 (3.2)** | 0.3 (1.2) | 3.2 (4.2)** | 1.7 (2.8) | 1.9 (2.9)** | 0.2 (0.9)** | 0.0 (0.9) |
| Non-FSU Israelis | 1,032 | ||||||||
| Sex | |||||||||
| Men | 788 | 1.5 (1.9)** | 2.7 (3.1)** | 0.5 (1.7)** | 3.4 (4.0)** | 1.9 (2.9) | 1.3 (2.5) | 0.0 (0.8) | 0.1 (1.0) |
| Women | 244 | 0.7 (1.4) | 1.8 (2.7) | 0.1 (0.6) | 1.3 (1.9) | 2.7 (3.3)** | 2.5 (3.5)** | -0.3 (0.6) | -0.1 (0.9) |
| Age cohort | |||||||||
| 21–40 | 535 | 1.7 (2.0)** | 2.3 (3.1) | 0.7 (1.9)** | 3.4 (4.0)** | 2.1 (3.1) | 1.4 (2.6) | 0.1 (0.9) | 0.2 (1.1) |
| 41–68 | 497 | 0.8 (1.6) | 2.7 (2.9)** | 0.2 (0.8) | 2.4 (3.4) | 2.1 (3.0) | 1.8 (3.0)** | -0.2 (0.6) | -0.2 (0.7) |
| FSU Israelis | 315 | ||||||||
| Sex | |||||||||
| Men | 240 | 2.1 (2.3)** | 3.7 (3.3)** | 0.4 (1.4)** | 3.9 (4.6)** | 1.6 (2.8) | 1.5 (2.4) | 0.3 (0.9) | 0.0 (1.0) |
| Women | 75 | 0.6 (1.2) | 2.2 (2.8) | 0.1 (3.4) | 2.0 (3.2) | 1.7 (2.9)** | 2.5 (3.2)** | -0.3 (0.6) | -0.2 (0.6) |
| Age cohort | |||||||||
| 21–10 | 143 | 2.1 (2.3)** | 3.2 (3.3) | 0.6 (1.7)** | 4.4 (5.3)** | 1.8 (2.8)** | 1.1 (1.9) | 0.3 (1.1) | 0.2 (1.1) |
| 41–68 | 172 | 1.5 (2.0) | 3.5 (3.2) | 0.1 (0.6) | 2.6 (3.1) | 1.6 (2.9) | 2.2 (3.0)** | 0.1 (0.7) | -0.2 (0.7) |
Notes: Age is dichotomized (using a median split) for presentation in this table, but analyzed continuously in all regression analyses. All substance use and psychiatric disorders were assessed using the Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV, with higher scores indicating more symptoms endorsed; AUD = alcohol use disorder; NUD = nicotine use disorder; CUD = cannabis use disorder; ASPD = antisocial personality disorder; MDD = major depressive disorder; PTSD = posttraumatic stress disorder; EXT = externalizing factor; INT = internalizing factor; FSU = former Soviet Union.
Indicates significant rank differences (Kruskal–Wallis chi-square test-statistic detailed in Table 2).
Table 2.
Mean differences in criteria counts for substance use and psychiatric disorders by key demographics in 1,347 Israeli household adults
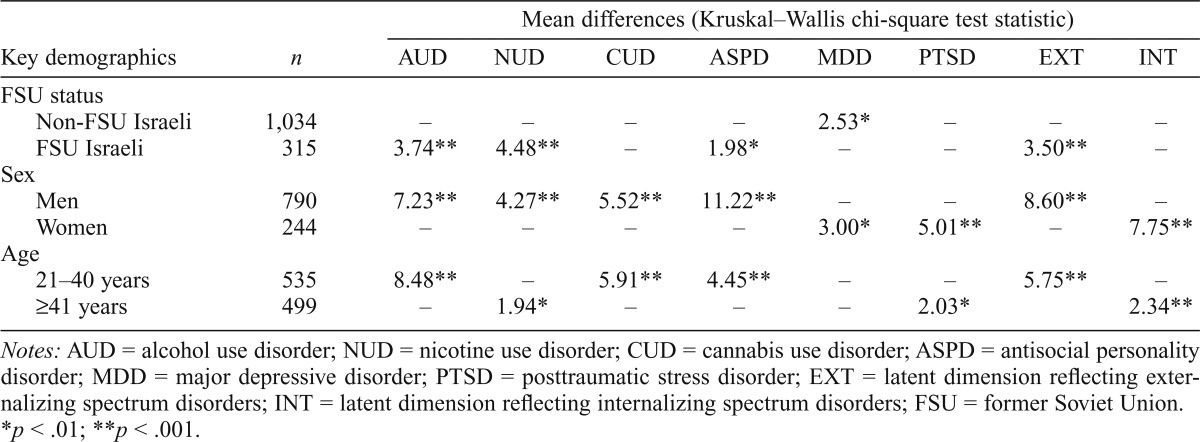
| Key demographics | n | Mean differences (Kruskal–Wallis chi-square test statistic) |
|||||||
| AUD | NUD | CUD | ASPD | MDD | PTSD | EXT | INT | ||
| FSU status | |||||||||
| Non-FSU Israeli | 1,034 | – | – | – | – | 2.53* | – | – | – |
| FSU Israeli | 315 | 3.74** | 4.48** | – | 1.98* | – | – | 3.50** | – |
| Sex | |||||||||
| Men | 790 | 7.23** | 4.27** | 5.52** | 11.22** | – | – | 8.60** | – |
| Women | 244 | – | – | – | – | 3.00* | 5.01** | – | 7.75** |
| Age | |||||||||
| 21–40 years | 535 | 8.48** | – | 5.91** | 4.45** | – | – | 5.75** | – |
| ≥41 years | 499 | – | 1.94* | – | – | – | 2.03* | 2.34** | |
Notes: AUD = alcohol use disorder; NUD = nicotine use disorder; CUD = cannabis use disorder; ASPD = antisocial personality disorder; MDD = major depressive disorder; PTSD = posttraumatic stress disorder; EXT = latent dimension reflecting externalizing spectrum disorders; INT = latent dimension reflecting internalizing spectrum disorders; FSU = former Soviet Union.
p < .01;
p < .001.
Parental history of alcohol problems and offspring disorders
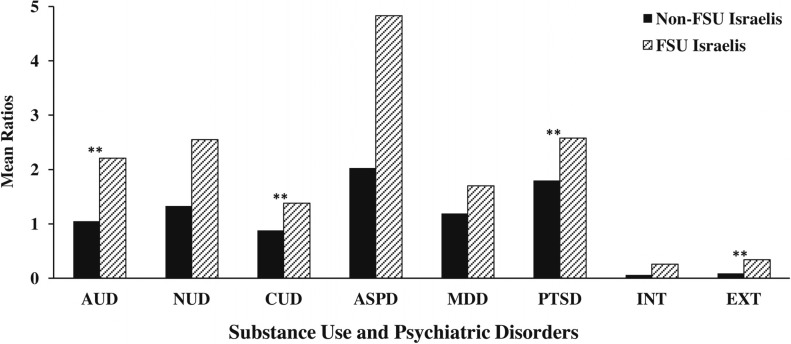
Parental alcohol problems were found in 15.7% of the full sample: 13.8% among non-FSU Israelis and 21.9% among FSU Israelis. Parental alcohol problems were significantly associated with greater NUD, ASPD, PTSD, and EXT in offspring (Table 3 includes mean ratios for NUD, ASPD, and PTSD and linear regression [β] coefficients for INT and EXT). Among non-FSU Israelis, parental alcohol problems were significantly associated with ASPD and PTSD (mean ratios, Table 3). Among FSU Israelis, parental alcohol problems were associated with AUD, NUD, CUD, ASPD, PTSD, EXT, and INT (mean ratios/β coefficients, Table 3). The association between parental history of alcohol problems and each disorder is depicted in Figure 2 separately for FSU and non-FSU Israelis.
Table 3.
Association between parental history of problems related to alcohol and participant psychiatric and substance use disorders: Israeli household adults stratified by former Soviet Union (FSU) status
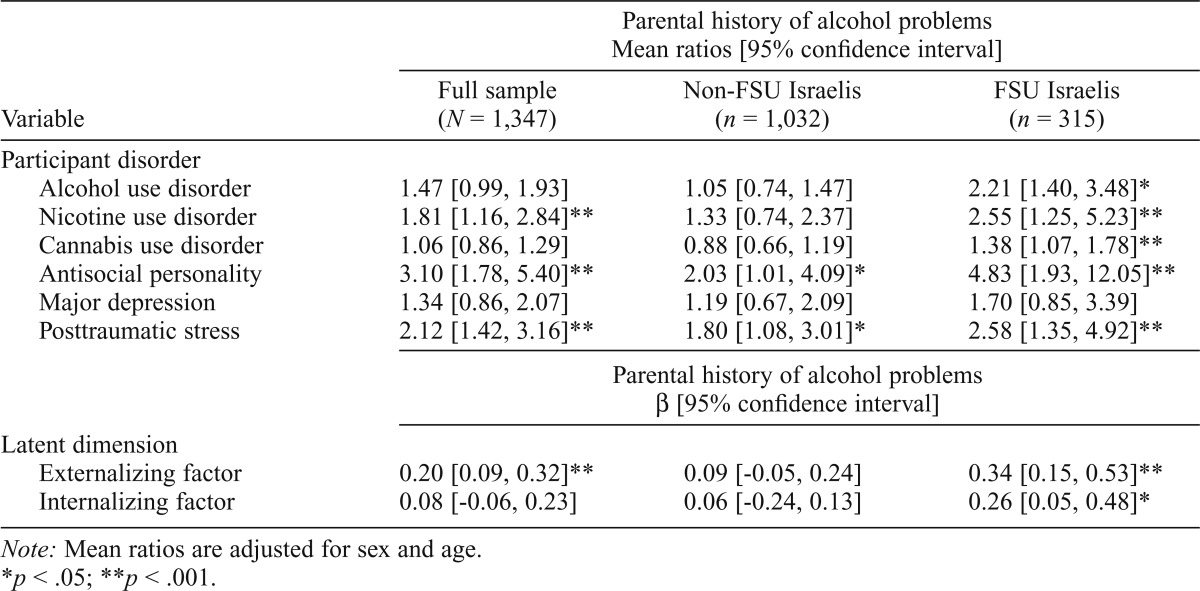
| Parental history of alcohol problems Mean ratios [95% confidence interval] |
||||
| Variable | Full sample (N = 1,347) | Non-FSU Israelis (n = 1,032) | FSU Israelis (n = 315) | |
| Participant disorder | ||||
| Alcohol use disorder | 1.47 [0.99, 1.93] | 1.05 [0.74, 1.47] | 2.21 [1.40, 3.48]* | |
| Nicotine use disorder | 1.81 [1.16, 2.84]** | 1.33 [0.74, 2.37] | 2.55 [1.25, 5.23]** | |
| Cannabis use disorder | 1.06 [0.86, 1.29] | 0.88 [0.66, 1.19] | 1.38 [1.07, 1.78]** | |
| Antisocial personality | 3.10 [1.78, 5.40]** | 2.03 [1.01, 4.09]* | 4.83 [1.93, 12.05]** | |
| Major depression | 1.34 [0.86, 2.07] | 1.19 [0.67, 2.09] | 1.70 [0.85, 3.39] | |
| Posttraumatic stress | 2.12 [1.42, 3.16]** | 1.80 [1.08, 3.01]* | 2.58 [1.35, 4.92]** | |
| Parental history of alcohol problems β [95% confidence interval] |
||||
| Latent dimension | ||||
| Externalizing factor | 0.20 [0.09, 0.32]** | 0.09 [-0.05, 0.24] | 0.34 [0.15, 0.53]** | |
| Internalizing factor | 0.08 [-0.06, 0.23] | 0.06 [-0.24, 0.13] | 0.26 [0.05, 0.48]* | |
Note: Mean ratios are adjusted for sex and age.
p < .05;
p < .001.
Figure 2.
Association between parental history of alcohol problems and participants’ psychiatric and substance use disorders in 1,347 Israeli household adults. Notes: Mean ratios from zero-inflated negative binomial regression, adjusted for sex and age. AUD = alcohol use disorder; NUD = nicotine use disorder; CUD = cannabis use disorder; ASPD = antisocial personality disorder; MDD = major depressive disorder; PTSD = posttraumatic stress disorder; FSU = former Soviet Union; INT = latent dimension reflecting internalizing spectrum disorders; EXT = latent dimension reflecting externalizing spectrum disorders. **Indicates significant differences by FSU immigrant status (p < .05).
Interaction between parental history of alcohol problems and FSU status
FSU status and parental alcohol problems showed a significant additive interaction effect on AUD (IC = 0.55, p < .01), CUD (IC = 0.48, p < .01), PTSD severity (IC = 1.11, p < .001), and EXT (IC = 1.13, p < .001). The associations between parental alcohol problems and participant outcomes (AUD, CUD, PTSD, EXT) were stronger in FSU Israelis, whereas these associations were weaker (PTSD) or null (AUD, CUD, EXT) in non-FSU Israelis (Table 4).
Table 4.
Interactions between parental history of alcohol problems and former Soviet Union (FSU) immigrant status, and effects on substance use and psychiatric disorders in 1,347 Israeli household adults
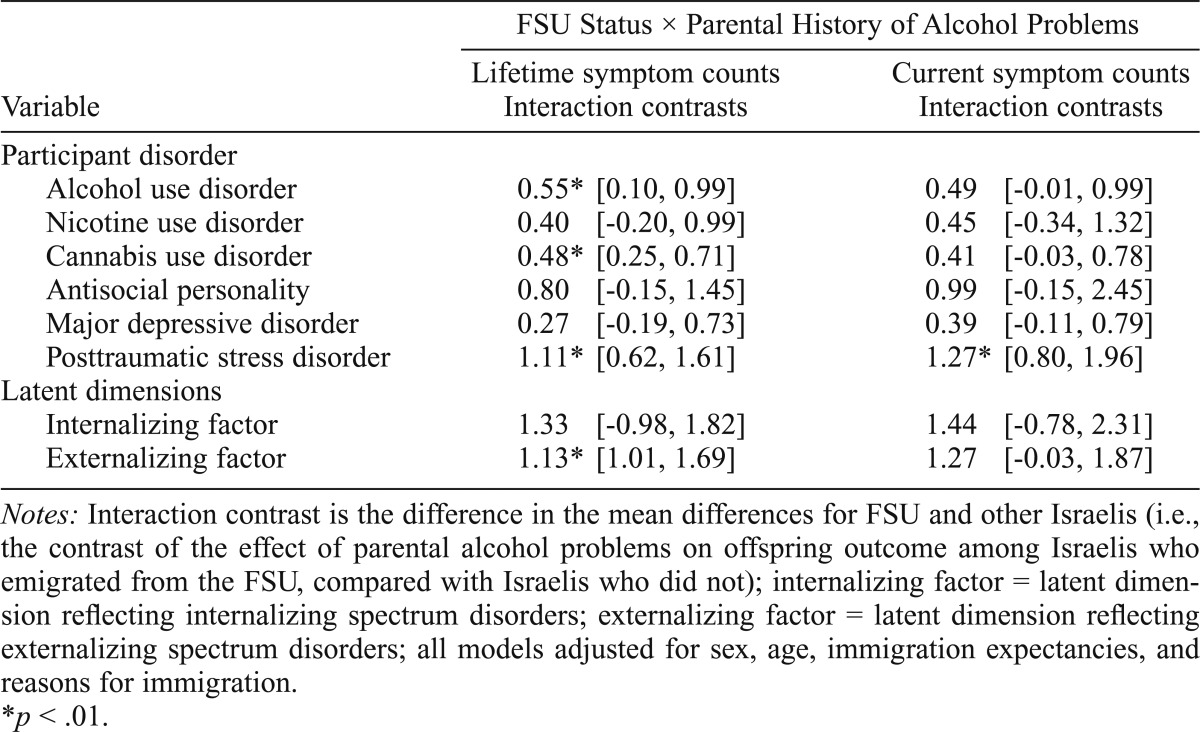
| Variable | FSU Status × Parental History of Alcohol Problems |
|
| Lifetime symptom counts Interaction contrasts | Current symptom counts Interaction contrasts | |
| Participant disorder | ||
| Alcohol use disorder | 0.55* [0.10, 0.99] | 0.49 [-0.01, 0.99] |
| Nicotine use disorder | 0.40 [-0.20, 0.99] | 0.45 [-0.34, 1.32] |
| Cannabis use disorder | 0.48* [0.25, 0.71] | 0.41 [-0.03, 0.78] |
| Antisocial personality | 0.80 [-0.15, 1.45] | 0.99 [-0.15, 2.45] |
| Major depressive disorder | 0.27 [-0.19, 0.73] | 0.39 [-0.11, 0.79] |
| Posttraumatic stress disorder | 1.11* [0.62, 1.61] | 1.27* [0.80, 1.96] |
| Latent dimensions | ||
| Internalizing factor | 1.33 [-0.98, 1.82] | 1.44 [-0.78, 2.31] |
| Externalizing factor | 1.13* [1.01, 1.69] | 1.27 [-0.03, 1.87] |
Notes: Interaction contrast is the difference in the mean differences for FSU and other Israelis (i.e., the contrast of the effect of parental alcohol problems on offspring outcome among Israelis who emigrated from the FSU, compared with Israelis who did not); internalizing factor = latent dimension reflecting internalizing spectrum disorders; externalizing factor = latent dimension reflecting externalizing spectrum disorders; all models adjusted for sex, age, immigration expectancies, and reasons for immigration.
p < .01.
Exploratory analysis
Exploratory analyses investigated immigration experiences as an alternative explanation for FSU/non-FSU differences in liability transmission. Taken as a whole, FSU Israelis (n = 315) reported similar average maxdrinks before (7.2, SD = 5.5) and after (7.1, SD = 4.6) immigration (p = .387). For those who immigrated to Israel before age 18, there was a significant increase in AUD severity after immigration (p < .001), with the average AUD severity increasing from 0.01 (SD = 0.08) before immigration to 0.20 (SD = 0.41) after immigration. However, among those who immigrated to Israel after age 18, mean post-immigration AUD severity was significantly lower than before immigration (p = .018), with average AUD severity decreasing from 0.17 (SD = 0.38) before immigration to 0.10 (SD = 0.30) after immigration. Using current criteria scores, results were significant for PTSD (IC = 1.27, p = .03) and in the same direction as the lifetime criteria scores for AUD, CUD, and EXT but not statistically significant, most likely because of the lower prevalence of current than lifetime criteria. The results of the interaction analysis remained unchanged after we adjusted for either immigration difficulty or reasons for immigration (Table 4).
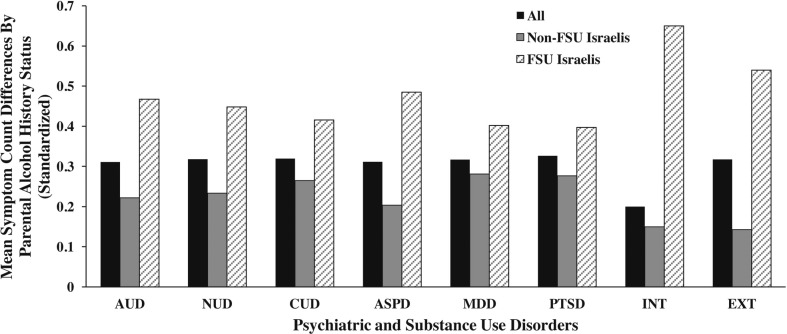
Finally, we explored the effects of maternal versus paternal history of alcohol problems. In analyses excluding participants with maternal-only alcohol problems, the interaction contrasts for AUD and PTSD increased nominally (AUD: IC = 0.62, p < .01; PTSD: IC = 1.21, p < .001), whereas CUD and EXT remained unchanged (CUD: IC = 0.48, p < .01; EXT: IC = 1.13, p < .001). These results are depicted in Figure 3.
Figure 3.
Differences in mean symptom counts of disorders between participants with and without a positive parental history of alcohol problems. Notes: FSU = former Soviet Union; AUD = alcohol use disorder; NUD = nicotine use disorder; CUD = cannabis use disorder; ASPD = antisocial personality disorder; MDD = major depressive disorder; PTSD = posttraumatic stress disorder; INT = latent dimension reflecting internalizing spectrum disorders; EXT = latent dimension reflecting externalizing spectrum disorders; all mean differences are adjusted for sex and age.
Discussion
This Israeli sample includes two groups (FSU and non-FSU Israelis) with different alcohol consumption behaviors and norms (Shmulewitz et al., 2012), enabling examination of social context on the transmission of liability for AUDs and psychopathology. The findings indicated that parental history of alcohol problems was differentially related to substance use and psychiatric disorders in Israelis who emigrated from the FSU. Specifically, associations between parental history of alcohol problems and offspring AUD, CUD, PTSD, and EXT were stronger in FSU Israelis than in non-FSU Israelis. Because of the “agnostic” nature of statistical interaction analysis, results also support the alternative interpretation that participant disorder severity differences between those with a parental history of alcohol problems and those without a parental history are different among FSU participants than among non-FSU participants. These findings support the concept that, although shared risk factors may influence each of these disorders, their manifestation may depend on social context (Shanahan and Hofer, 2005).
We propose that, in social contexts that vary in the degree to which they constrain specific behavior, underlying genetic predispositions may manifest as different disorders. In contrast to earlier age cohorts of Israelis (Levav et al., 1993), younger cohorts have begun drinking and using cannabis more and have shown more alcohol-related problems (Jaffe et al., 2009). This may be attributable to multiple influences, such as alcohol marketing, increases in availability (Jaffe et al., 2009), and changing norms. In Israel, where heavy drinking and other drug problems have historically been limited (Levav et al., 1993) but are increasing among younger Israelis (Jaffe et al., 2009; Sznitman et al., 2013), an underlying predisposition to psychopathology may manifest as disorders other than AUDs or other substance use disorders in parents of non-FSU Israelis but as substance use disorders in their children, among whom more accepting social norms of regular/heavy alcohol consumption and other drug use are evidently becoming more common. Conversely, predisposition to psychopathology manifested more similarly among FSU parents and offspring, because both had similar cultural and social contexts for drinking and other drug use behaviors.
Therefore, alcohol consumption and attitudes toward drinking not only differ between emigrants from the FSU and other Israelis, but they also differ between older and younger cohorts of Israelis (Sznitman et al., 2013). We did not observe these effects with NUDs; a parental history of alcohol problems was related to offspring NUD in both FSU and non-FSU groups. We believe that this is a result of the consistent and moderate to heavy use of nicotine in both older and younger cohorts of Israelis (Levav et al., 2009), which is in contrast to alcohol and cannabis consumption. Although this study focused on group differences between FSU and non-FSU Israelis, future studies should examine specific cultural and psychosocial factors that may be contributing to the group differences in parental transmission found in this study.
In addition to the findings specific to the transmission of parental alcohol problems to offspring substance use disorders, this study’s findings indicate that there is a stronger association between parental history of alcohol problems and offspring PTSD in FSU Israelis than in non-FSU Israelis. Previous studies have found an association between parental alcohol problems and offspring mood and anxiety disorders (Kendler et al., 1997, 2003; Krueger et al., 2002). In addition to genetic liability, children of alcoholics are more likely to be exposed to adverse and potentially traumatic events (Hall and Webster, 2002). Moreover, previous studies suggest that the adult children of alcoholics may develop less effective stress management strategies and present more clinically at-risk patterns of responses than their counterparts (Hall and Webster, 2002). Furthermore, data from the present study indicate that there is increased PTSD severity in FSU Israelis compared with non-FSU Israelis, suggesting that potentially adverse or traumatizing experiences related to FSU immigrant status may be mediating the association between parental alcohol problems and PTSD in the FSU-Israeli subgroup.
In this study, we examined the impact of social context on the transmission of liability for AUDs and psychopathology. However, because some studies show recent immigration as a risk for psychopathology (Bourque et al., 2012), including alcohol use and related disorders (Adrian, 2002; Johnson et al., 2002; Krupinski et al., 1984), we explored whether the impact of immigration could be an alternative explanation for the differential transmission of liability. First, we found no significant increase in AUD severity following immigration among those who were older than 18 when they immigrated to Israel, only among those who were younger than 18 before immigration. This finding was expected because of the typical age at onset for drinking behaviors in late adolescence or early adulthood (the subset of immigrants who came to Israel before age 18 would have entered the age of risk after they arrived in Israel). Second, results using current rather than lifetime criteria of disorders operated in the same direction. Furthermore, when immigration difficulty and reasons for immigration were modeled in the interaction analysis, results were unchanged.
Taken together, these findings do not support immigration-related experiences as an alternative explanation for the study results. Although immigration-related stress has been shown to increase drinking in previous studies, much of this research is based on studies of individuals migrating to countries with moderate to high alcohol consumption from countries with less alcohol consumption. The FSU-Israeli group examined in this study differs from previously studied immigrant groups in that there is significantly greater alcohol consumption in their country of origin (the former Soviet Union) compared with Israel. However, future studies specifically designed to study immigration experiences of FSU Israelis should address this question further.
Previous studies have demonstrated differences in offspring psychopathology among those with a paternal history of alcoholism as compared with a maternal history of alcoholism (Coffelt et al., 2006; Dinwiddie and Reich, 1991; Sher et al., 1991). However, taken as a whole, this literature is largely inconclusive regarding whether maternal or paternal alcoholism is related to more severe psychopathology (Pearson et al., 2012). Yet, post hoc analyses that excluded the subset of participants with a positive maternal history of problems with alcohol remained largely unchanged (the interaction contrasts for PTSD and AUD increased nominally). This finding indicates that paternal alcoholism may have a greater impact on a participant’s PTSD and AUD severity within this sample.
Limitations of the study are noted. The transmission of parental substance use problems and psychopathology to offspring outcomes is influenced by both genetics and home environment. Exposure to parents with psychopathology increases the likelihood of environmental risk factors for psychopathology (e.g., abuse, neglect, poor living conditions, lack of parental monitoring or warmth, and parental divorce) (Enoch, 2006). The relationships between the effects of genetics and the home environment are complex and beyond the scope of the present analysis, but future studies incorporating these effects are warranted. These analyses assume that parental problems preceded offspring lifetime psychopathology. However, when analyses were repeated using current symptom scores, the results operated in the same direction as lifetime symptom scores with decreased statistical significance (likely because of the decreased number of individuals endorsing criteria). This finding indicates that this assumption did not bias the findings.
Finally, although this study used a measure of parental alcohol history that has been used in many health-related studies (McLaughlin et al., 2012), this measure reflects the participants’ perception of their parents’ alcohol history and may be biased by the participants’ individual experiences (Kendler et al., 1991). However, a recent study in Sweden comparing the prevalence of a child’s perception of family alcohol problems to true prevalence indicates that this is an acceptable proxy (Kendler et al., 2012). In addition, a statistical power analysis conducted in this sample confirmed that, given the parameters of this study (i.e., sample and effect sizes), there was not complete power to detect interaction effects for all outcomes. Specifically, there was only 84.3% power and 89.6% power to detect interaction effects for ASPD and MDD, respectively.
In conclusion, findings from this study demonstrate the importance of understanding the cultural milieu of populations in terms of risk factors for psychiatric and substance use disorders. Specifically, this study indicated that associations between a parental history of alcohol problems and offspring AUD, CUD, PTSD, and EXT were stronger in FSU Israelis than in non-FSU Israelis, two Israeli groups that differ in alcohol use patterns and related social norms. These results support the concept that, in social contexts that limit deviant behaviors (such as heavy alcohol use), genetic influences on those behaviors are attenuated, whereas, in less limiting contexts, genetic influences are stronger (Dick and Kendler, 2012; Shanahan and Hofer, 2005). These findings also have implications for clinicians. Health care professionals should recognize that individuals who have parents with a history of alcohol problems could be more vulnerable to developing several related psychiatric and substance use disorders, in addition to AUD. Finally, clinicians should consider the cultural context of their patients in terms of predisposing factors for psychiatric and substance use disorders.
Footnotes
This research was funded by National Institutes of Health Grants U01AA018111,R01AA013654,R01DA018652,K05AA014223 (to Deborah Hasin); K23DA016743 (to Efrat Aharonovich); and T32MH13043 (to Jacquelyn L. Meyers) and the New York State Psychiatric Institute (to Deborah Hasin).
References
- Adrian M. A critical perspective on cross-cultural contexts for addiction and multiculturalism: Their meanings and implications in the substance use field. Substance Use & Misuse. 2002;37:853–900. doi: 10.1081/ja-120004157. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Endicott J, Spitzer RL, Winokur G. The family history method using diagnostic criteria. Reliability and validity. Archives of General Psychiatry. 1977;34:1229–1235. doi: 10.1001/archpsyc.1977.01770220111013. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, text revision. 4th ed. Washington, DC: Author; 2000. [Google Scholar]
- Borges G, Ye Y, Bond J, Cherpitel CJ, Cremonte M, Moskalewicz J, Rubio-Stipec M. The dimensionality of alcohol use disorders and alcohol consumption in a cross-national perspective. Addiction. 2010;105:240–254. doi: 10.1111/j.1360-0443.2009.02778.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bourque F, van der Ven E, Fusar-Poli P, Malla A. Immigration, social environment and onset of psychotic disorders. Current Pharmaceutical Design. 2012;18:518–526. doi: 10.2174/138161212799316028. [DOI] [PubMed] [Google Scholar]
- Canino G, Bravo M, Ramírez R, Febo VE, Rubio-Stipec M, Fernández RL, Hasin D. The Spanish Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability and concordance with clinical diagnoses in a Hispanic population. Journal of Studies on Alcohol. 1999;60:790–799. doi: 10.15288/jsa.1999.60.790. [DOI] [PubMed] [Google Scholar]
- Central Bureau of Statistics. Table 2—Immigrants, by continent and selected last country of residence. State of Israel, Jerusalem: 2009. Retrieved from http://www1.cbs.gov.il/hodaot2014n/21_14_106t2.pdf. [Google Scholar]
- Coffelt NL, Forehand R, Olson AL, Jones DJ, Gaffney CA, Zens MS. A longitudinal examination of the link between parent alcohol problems and youth drinking: The moderating roles of parent and child gender. Addictive Behaviors. 2006;31:593–605. doi: 10.1016/j.addbeh.2005.05.034. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Cotton NS. The familial incidence of alcoholism: A review. Journal of Studies on Alcohol. 1979;40:89–116. doi: 10.15288/jsa.1979.40.89. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF. Family history of alcoholism and gender: Their combined effects on DSM-IV alcohol dependence and major depression. Journal of Studies on Alcohol. 1998;59:97–106. doi: 10.15288/jsa.1998.59.97. [DOI] [PubMed] [Google Scholar]
- Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, Chatterji S the WHO World Mental Health Survey Consortium. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Journal of the American Medical Association. 2004;291:2581–2590. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- Dick DM, Kendler KS. The impact of gene-environment interaction on alcohol use disorders. Alcohol Research: Current Reviews. 2012;34:318–324. [PMC free article] [PubMed] [Google Scholar]
- Dinwiddie SH, Reich T. Epidemiological perspectives on children of alcoholics. Recent Developments in Alcoholism: An Official Publication of the American Medical Society on Alcoholism, the Research Society on Alcoholism, and the National Council on Alcoholism. 1991;9:287–299. [PubMed] [Google Scholar]
- Enoch MA. Genetic and environmental influences on the development of alcoholism: Resilience vs. risk. Annals of the New York Academy of Sciences. 2006;1094:193–201. doi: 10.1196/annals.1376.019. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Harford TC, Dawson DA, Chou PS, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview schedule (AUDADIS): Reliability of alcohol and drug modules in a general population sample. Drug and Alcohol Dependence. 1995;39:37–44. doi: 10.1016/0376-8716(95)01134-k. [DOI] [PubMed] [Google Scholar]
- Hall CW, Webster RE. Traumatic symptomatology characteristics of adult children of alcoholics. Journal of Drug Education. 2002;32:195–211. doi: 10.2190/U29W-LF3W-748L-A48M. [DOI] [PubMed] [Google Scholar]
- Harkin AM, Anderson P, Goos C. Smoking, drinking, and drug taking in the European Region. Copenhagen, Denmark: World Health Organization Regional Office for Europe; 1997. [Google Scholar]
- Hasin D, Aharonovich E, Liu X, Mamman Z, Matseoane K, Carr LG, Li T-K. Alcohol dependence symptoms and alcohol dehydrogenase 2 polymorphism: Israeli Ashkenazis, Sephardics, and recent Russian immigrants. Alcoholism: Clinical and Experimental Research. 2002;26:1315–1321. doi: 10.1097/01.ALC.0000029597.07916.A9. [DOI] [PubMed] [Google Scholar]
- Hasin D, Carpenter KM, McCloud S, Smith M, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule (AUDADIS): Reliability of alcohol and drug modules in a clinical sample. Drug and Alcohol Dependence. 1997;44:133–141. doi: 10.1016/s0376-8716(97)01332-x. [DOI] [PubMed] [Google Scholar]
- Hasin D, Rahav G, Meydan J, Neumark Y. The drinking of earlier and more recent Russian immigrants to Israel: Comparison to other Israelis. Journal of Substance Abuse. 1998;10:341–353. doi: 10.1016/s0899-3289(99)00010-3. [DOI] [PubMed] [Google Scholar]
- Hasin D, Samet S, Nunes E, Meydan J, Matseoane K, Waxman R. Diagnosis of comorbid psychiatric disorders in substance users assessed with the Psychiatric Research Interview for Substance and Mental Disorders for DSM-IV. American Journal of Psychiatry. 2006;163:689–696. doi: 10.1176/ajp.2006.163.4.689. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Fenton MC, Beseler C, Park JY, Wall MM. Analyses related to the development of DSM-5 criteria for substance use related disorders: 2. Proposed DSM-5 criteria for alcohol, cannabis, cocaine and heroin disorders in 663 substance abuse patients. Drug and Alcohol Dependence. 2012;122:28–37. doi: 10.1016/j.drugalcdep.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Keyes KM, Hatzenbuehler ML, Aharonovich EA, Alderson D. Alcohol consumption and posttraumatic stress after exposure to terrorism: Effects of proximity, loss, and psychiatric history. American Journal of Public Health. 2007;97:2268–2275. doi: 10.2105/AJPH.2006.100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath AC, Bucholz KK, Madden PAF, Dinwiddie SH, Slutske WS, Bierut LJ, Martin NG. Genetic and environmental contributions to alcohol dependence risk in a national twin sample: Consistency of findings in women and men. Psychological Medicine. 1997;27:1381–1396. doi: 10.1017/s0033291797005643. [DOI] [PubMed] [Google Scholar]
- Heiman GA, Ogburn E, Gorroochurn P, Keyes KM, Hasin D. Evidence for a two-stage model of dependence using the NESARC and its implications for genetic association studies. Drug and Alcohol Dependence. 2008;92:258–266. doi: 10.1016/j.drugalcdep.2007.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaffe DH, Savitsky B, Zaistev K, Hiss J, Peleg K. Alcohol and driver fatalities in Israel: An examination of the current problem. Israel Medical Association Journal. 2009;11:725–729. [PubMed] [Google Scholar]
- Johnson TP, VanGeest JB, Cho YI. Migration and substance use: Evidence from the U.S. National Health Interview Survey. Substance Use & Misuse. 2002;37:941–972. doi: 10.1081/ja-120004160. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Davis CG, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: A family history study. British Journal of Psychiatry. 1997;170:541–548. doi: 10.1192/bjp.170.6.541. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of General Psychiatry. 2003;60:929–937. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Silberg JL, Neale MC, Kessler RC, Heath AC, Eaves LJ. The family history method: Whose psychiatric history is measured? American Journal of Psychiatry. 1991;148:1501–1504. doi: 10.1176/ajp.148.11.1501. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Sundquist K, Ohlsson H, Palmér K, Maes H, Winkleby MA, Sundquist J. Genetic and familial environmental influences on the risk for drug abuse: A national Swedish adoption study. Archives of General Psychiatry. 2012;69:690–697. doi: 10.1001/archgenpsychiatry.2011.2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger RF, Hicks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Etiologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. Journal of Abnormal Psychology. 2002;111:411–424. [PubMed] [Google Scholar]
- Krupinski J. Changing patterns of migration to Australia and their influence on the health of migrants. Social Science & Medicine. 1984;18:927–937. doi: 10.1016/0277-9536(84)90263-6. [DOI] [PubMed] [Google Scholar]
- Levav I, Kohn R, Dohrenwend BP, Shrout PE, Skodol AE, Schwartz S, Naveh G. An epidemiological study of mental disorders in a 10-year cohort of young adults in Israel. Psychological Medicine. 1993;23:691–707. doi: 10.1017/s0033291700025472. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Gadermann AM, Hwang I, Sampson NA, Al-Hamzawi A, Andrade LH, Kessler RC. Parent psychopathology and offspring mental disorders: Results from the WHO World Mental Health Surveys. British Journal of Psychiatry. 2012;200:290–299. doi: 10.1192/bjp.bp.111.101253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles, CA: Authors; 2002. [Google Scholar]
- Pearson MR, D’Lima GM, Kelley ML. Maternal and paternal alcohol misuse and alcohol-related outcomes among college students. Substance Use & Misuse. 2012;47:708–717. doi: 10.3109/10826084.2012.664237. [DOI] [PubMed] [Google Scholar]
- Rahav G, Hasin D, Paykin A. Drinking patterns of recent Russian immigrants and other Israelis: 1995 national survey results. American Journal of Public Health. 1999;89:1212–1216. doi: 10.2105/ajph.89.8.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remennick LI. Immigrants from Chernobyl-affected areas in Israel: The link between health and social adjustment. Social Science & Medicine. 2002;54:309–317. doi: 10.1016/s0277-9536(01)00030-2. [DOI] [PubMed] [Google Scholar]
- Schiff M, Rahav G, Teichman M. Israel 2000: Immigration and gender differences in alcohol consumption. American Journal on Addictions /American Academy of Psychiatrists in Alcoholism and Addictions. 2005;14:234–247. doi: 10.1080/10550490590949578. [DOI] [PubMed] [Google Scholar]
- Shanahan MJ, Hofer SM. Social context in gene-environment interactions: Retrospect and prospect. Journals of Gerontology: Series B Psychological Sciences and Social Sciences, 60, Special Issue. 2005;1:65–76. doi: 10.1093/geronb/60.special_issue_1.65. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: Putative risk factors, substance use and abuse, and psychopathology. Journal of Abnormal Psychology. 1991;100:427–448. doi: 10.1037//0021-843x.100.4.427. [DOI] [PubMed] [Google Scholar]
- Shmulewitz D, Keyes K, Beseler C, Aharonovich E, Aivadyan C, Spivak B, Hasin D. The dimensionality of alcohol use disorders: Results from Israel. Drug and Alcohol Dependence. 2010;111:146–154. doi: 10.1016/j.drugalcdep.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmulewitz D, Keyes KM, Wall MM, Aharonovich E, Aivadyan C, Greenstein E, Hasin D. Nicotine dependence, abuse and craving: Dimensionality in an Israeli sample. Addiction. 2011;106:1675–1686. doi: 10.1111/j.1360-0443.2011.03484.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shmulewitz D, Wall MM, Keyes KM, Aharonovich E, Aivadyan C, Greenstein E, Hasin D. Alcohol use disorders and perceived drinking norms: Ethnic differences in Israeli adults. Journal of Studies on Alcohol and Drugs. 2012;73:981–990. doi: 10.15288/jsad.2012.73.981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoval G, Shmulewitz D, Wall M, Aharonovich E, Spivak B, Weizman A, Hasin D. Alcohol dependence and suicide-related ideation/behaviors in an Israeli household sample, with and without major depression. Alcoholism: Clinical and Experimental Research. 2014;38:820–825. doi: 10.1111/acer.12290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slutske WS, Heath AC, Madden PAF, Bucholz KK, Dinwiddie SH, Dunne MP, Martin NG. Reliability and reporting biases for perceived parental history of alcohol-related problems: Agreement between twins and differences between discordant pairs. Journal of Studies on Alcohol. 1996;57:387–395. doi: 10.15288/jsa.1996.57.387. [DOI] [PubMed] [Google Scholar]
- Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. American Journal of Epidemiology. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- Spiegelman D, Hertzmark E, Wand HC. Point and interval estimates of partial population attributable risks in cohort studies: Examples and software. Cancer Causes and Control. 2007;18:571–579. doi: 10.1007/s10552-006-0090-y. [DOI] [PubMed] [Google Scholar]
- Spivak B, Frisch A, Maman Z, Aharonovich E, Alderson D, Carr LG, Hasin D. Effect of ADH1B genotype on alcohol consumption in young Israeli Jews. Alcoholism: Clinical and Experimental Research. 2007;31:1297–1301. doi: 10.1111/j.1530-0277.2007.00438.x. [DOI] [PubMed] [Google Scholar]
- Sznitman SR, Baron-Epel O, Boker-Keinan L. Convergence of drinking patterns of young Russian immigrants and veteran Israelis decades after mass immigration: Results from a bidirectional acculturation model. Journal of Studies on Alcohol and Drugs. 2013;74:437–446. doi: 10.15288/jsad.2013.74.437. [DOI] [PubMed] [Google Scholar]
- van der Zwaluw CS, Scholte RHJ, Vermulst AA, Buitelaar JK, Verkes RJ, Engels RCME. Parental problem drinking, parenting, and adolescent alcohol use. Journal of Behavioral Medicine. 2008;31:189–200. doi: 10.1007/s10865-007-9146-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K, Elliott JC, Shmulewitz D, Aharonovich E, Strous R, Frisch A, Hasin D. Trauma exposure, posttraumatic stress disorder and risk for alcohol, nicotine, and marijuana dependence in Israel. Comprehensive Psychiatry. 2014;55:621–630. doi: 10.1016/j.comppsych.2013.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Geneva, Switzerland: Author; 2011. Global status report on alcohol and health. Retrieved from http://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf. [Google Scholar]
- Zimmerman M, Sheeran T, Young D. The Diagnostic Inventory for Depression: A self-report scale to diagnose DSM-IV major depressive disorder. Journal of Clinical Psychology. 2004;60:87–110. doi: 10.1002/jclp.10207. [DOI] [PubMed] [Google Scholar]