Abstract
Background
In asthmatic patients inadequately controlled on inhaled corticosteroids and/or those with moderate persistent asthma, two main options are recommended: the combination of a long-acting inhaled ß2 agonist (LABA) with inhaled corticosteroids (ICS) or use of a higher dose of inhaled corticosteroids.
Objectives
To determine the effect of the combination of long-acting ß2 agonists and inhaled corticosteroids compared to a higher dose of inhaled corticosteroids on the risk of asthma exacerbations, pulmonary function and on other measures of asthma control, and to look for characteristics associated with greater benefit for either treatment option.
Search methods
We identified randomised controlled trials (RCTs) through electronic database searches (MEDLINE, EMBASE and CINAHL), bibliographies of RCTs, clinical trial registries and correspondence with manufacturers until May 2008.
Selection criteria
RCTs that compared the combination of inhaled LABA and ICS to a higher dose of inhaled corticosteroids, in children and adults with asthma.
Data collection and analysis
Two authors independently assessed methodological quality and extracted data. We obtained confirmation from the trialists when possible. The primary endpoint was the number of patients experiencing one or more asthma exacerbations requiring oral corticosteroids.
Main results
This review included 48 studies (15,155 participants including 1155 children and 14,000 adults). Participants were inadequately controlled on their current ICS regimen, experiencing ongoing symptoms and with generally moderate (FEV1 60% to 79% of predicted) airway obstruction. The studies tested the combination of salmeterol or formoterol with a median dose of 400 mcg/day of beclomethasone or equivalent (BDP-eq) compared to a median of 1000 mcg/day of BDP-eq, usually for 24 weeks or less. There was a statistically significantly lower risk of exacerbations requiring systemic corticosteroids in patients treated with LABA and ICS (RR 0.88, 95% CI 0.78 to 0.98, 27 studies, N = 10,578) from 11.45% to 10%, with a number needed to treat of 73 (median study duration: 12 weeks). The study results were dominated by adult studies; trial data from three paediatric studies showed a trend towards increased risk of rescue oral steroids (RR 1.24, 95% CI 0.58 to 2.66) and hospital admission (RR 2.21, 95% CI 0.74 to 6.64) associated with combination therapy. Overall, there was no statistically significant difference in the risk ratios for either hospital admission (RR 1.02, 95% CI 0.67 to 1.56) or serious adverse events (RR 1.12, 95% CI 0.91 to 1.37). The combination of LABA and ICS resulted in significantly greater but modest improvement from baseline in lung function, symptoms and rescue medication use than with higher ICS dose. Despite no significant group difference in the risk of overall adverse events (RR 0.99, 95% CI 0.95 to 1.03), there was an increase in the risk of tremor (RR 1.84, 95% CI 1.20 to 2.82) and a lower risk of oral thrush (RR 0.58, 95% CI 0.40 to 0.86)) in the LABA and ICS compared to the higher ICS group. There was no significant difference in hoarseness or headache between the treatment groups. The rate of withdrawals due to poor asthma control favoured the combination of LABA and ICS (RR 0.65, 95% CI 0.51 to 0.83).
Authors’ conclusions
In adolescents and adults with sub-optimal control on low dose ICS monotherapy, the combination of LABA and ICS is modestly more effective in reducing the risk of exacerbations requiring oral corticosteroids than a higher dose of ICS. Combination therapy also led to modestly greater improvement in lung function, symptoms and use of rescue ß2 agonists and to fewer withdrawals due to poor asthma control than with a higher dose of inhaled corticosteroids. Apart from an increased rate of tremor and less oral candidiasis with combination therapy, the two options appear relatively safe in adults although adverse effects associated with long-term ICS treatment were seldom monitored. In children, combination therapy did not lead to a significant reduction, but rather a trend towards an increased risk, of oral steroid-treated exacerbations and hospital admissions. These trends raised concern about the safety of combination therapy in view of modest improvement in children under the age of 12 years.
Medical Subject Headings (MeSH): Administration, Inhalation; Adrenal Cortex Hormones [*administration & dosage]; Adrenergic beta-Agonists [*administration & dosage]; Anti-Asthmatic Agents [*administration & dosage]; Asthma [*drug therapy]; Drug Therapy, Combination [methods]; Randomized Controlled Trials as Topic
MeSH check words: Adolescent; Adult; Child; Child, Preschool; Humans
BACKGROUND
Beta-2 adrenergic agonists are the major class of medication used for the relief of asthma symptoms. They produce their effects through interaction with specific ß2 adrenergic receptors located in the plasma membrane of virtually all types of cells, including bronchial wall smooth muscle (Nelson 1995). For several decades, short-acting inhaled ß2 agonists have been the primary agents used to treat patients with asthma. Their benefits include rapid onset of bronchodilation within five to 15 minutes (D’Alonzo 1997), highly effective protection against exercise-induced asthma and protection against the early asthmatic response to allergen (Sears 1998). Their duration of action is only three to six hours (Nelson 1995). Short-acting ß2 agonists do not seem to have any effect on overall severity of asthma, nor on inflammation (Sears 1998). Long-acting ß2 agonists, such as salmeterol and formoterol, have been developed for more prolonged control of symptoms (D’Alonzo 1997). Slightly slower in onset of action than short-acting ß2 agonists, inhaled salmeterol exerts its bronchodilating effect within ten to 20 minutes (Adkins 1997). This effect then lasts up to 12 hours due to high affinity binding of the molecule’s side chain to a specific site within the ß2 adrenergic receptor (Adkins 1997; D’Alonzo 1997; Nelson 1995). Formoterol, on the other hand, has an onset of bronchodilation within less than five minutes (Bartow 1998; Moore 1998) and a duration of action similar to that of salmeterol. Due to its ability to enter the cell’s lipid bi-layer, it becomes available over a prolonged period to stimulate the receptor (Nelson 1995). These two long-acting ß2 agonists have been shown to reduce daytime and nighttime symptoms, improve quality of sleep, reduce requirement for short-acting ß2 agonists (D’Alonzo 1997; Sears 1998) and protect against methacholine-induced, cold air-induced and exercise-induced bronchoconstriction (D’Alonzo 1997; Nelson 1995; Moore 1998). Long-acting inhaled ß2 agonists are currently used in the maintenance, rather than in the acute treatment, of children aged six years and older and adults with asthma. At time of publication, these drugs have not yet been marketed for children less than four years old, although such approval may currently be sought in several countries.
The need for frequent use of ß2 agonists generally indicates a significant inflammatory process that should be controlled with anti-inflammatory drugs (Fireman 1995; Nelson 1995; Kemp 1998). Inhaled corticosteroids are currently the most effective anti-inflammatory drugs used for long-term control of asthma (Adams 2008; Manning 2008).
When asthma control is unsatisfactory despite low doses of inhaled corticosteroids, several options have been proposed: increasing the dose of inhaled corticosteroids or adding other agents such as long-acting ß2 agonists, leukotriene receptor antagonists or theophylline. Of all add-on therapies, long-acting ß2 agonists have emerged as the preferred option in terms of efficacy (BTS 2008 (updated June 09); GINA 2008; Lemiere 2004; NIH Publication 2007). Guidelines differ with regards to choosing between increasing the dose of inhaled corticosteroids or adding long-acting ß2 agonists for adults, children, toddlers and infants/toddlers.
In adults, all but the British guidelines prefer the addition of long-acting ß2 agonists to inhaled corticosteroids in cases of sub-optimal control on inhaled corticosteroid monotherapy. The Canadian and Australian Consensus statement recommends the addition of long-acting ß2 agonists if control is unsatisfactory with 400 mcg/day of CFC-beclomethasone dipropionate (BDP) or equivalent (Australia 2006; GINA 2008; Lemiere 2004, ) while doses of 200 to 800 mcg/day are recommended by the British guidelines (BTS 2008 (updated June 09)). In contrast, the American guidelines give equal weight to adding long-acting ß2 agonists or increasing the dose of inhaled corticosteroids (NIH Publication 2007). In children aged 5 years and older with poor control on 400 mcg/day of BDP-equivalent, it is recommended to first increase the dose of inhaled corticosteroids to a medium dose in the Australian (Australia 2006), Canadian (Lemiere 2004) and International (GINA 2008) statements, before adding long-acting ß2 agonists, where the paediatric medium dose is 401 to 800 mcg/ day for all but the Gina guidelines where it is 201 to 400 mcg/ day. The American guidelines give equal weight to increasing the inhaled corticosteroid dose of a moderate dose or adding a long-acting ß2 agonist. In contrast, the British (BTS 2008 (updated June 09)) guidelines recommend the addition of long-acting ß2 agonists at an inhaled corticosteroid dose of 400 mcg/day before increasing the inhaled corticosteroid dose to 800 mcg/day. In infants and preschool-aged children, the American guidelines (NIH Publication 2007) recommend increasing the dose of ICS to a medium dose as the preferred option. The British Thoracic Society guidelines do not recommend the use of long-acting ß2 agonists in this age group (BTS 2008 (updated June 09), while other guidelines have made no specific statement. Clearly, uncertainties persist regarding the severity of airway obstruction and the baseline dose of inhaled corticosteroids to which addition of long-acting ß2 agonists may be preferable to increasing the dose of inhaled corticosteroids. The influence of age for optimising treatment strategies is also unclear.
Two published meta-analyses initially examined the combination of salmeterol with inhaled corticosteroids (Shrewsbury 2000) or with fluticasone specifically (Heyneman 2002) as compared to a double-dose inhaled corticosteroid. Both of these reviews demonstrated clear superiority of combination therapy with regards to lung function, symptoms and use of rescue ß2 agonists. Shrewsbury 2000 also showed that combination therapy was superior in the prevention of asthma exacerbations. However, these meta-analyses were not systematic reviews in that they:
only included trials sponsored by GlaxoSmithKline;
tested only salmeterol as the long-acting ß2 agonist; and
were limited to adult trials.
However, the safety of long-acting ß2 agonists alone or in combination with inhaled corticosteroids has been challenged. There have been clear indications that the use of long-acting ß2 agonists as monotherapy is worse than use in combination with inhaled corticosteroids (Warner 1998). A recent systematic review combining trials in which long-acting ß2 agonists were used alone or in combination with inhaled corticosteroids reported an increase in the risk of serious adverse events associated with long-acting ß2 agonists (Salpeter 2006). The possible protection offered by inhaled corticosteroids has led to recommendations from national and international asthma consensus statements that stipulate the use of long-acting ß2 agonists only in combination with inhaled corticosteroids (Australia 2006; BTS 2008 (updated June 09); Georgitis 1999; GINA 2008; Lemiere 2004; NIH Publication 2007; Warner 1998). Yet concerns about the safety of long-acting ß2 agonists must clearly be addressed in adults and particularly in children, in whom few data are available.
We published a Cochrane Review comparing the combination of any long-acting ß2 agonist preparation and inhaled corticosteroids to increased inhaled corticosteroid dose and documented the beneficial effect of combination therapy on asthma exacerbations requiring systemic corticosteroids, lung function, symptoms and rescue bronchodilators (Greenstone 2005). With the publication of several additional trials since 2005, we believed a systematic review comparing the combination of long-acting ß2 agonist and inhaled corticosteroids to a higher dose of inhaled corticosteroids in patients with a prior trial of inhaled corticosteroids would provide a more unbiased view of the evidence on safety and efficacy and, perhaps, greater insight as to the patient and treatment characteristics associated with greater benefit or harm from either treatment option. We believed this update would strengthen the evidence supporting the safety of long-acting ß2 agonists when used in combination therapy (Ernst 2006).
OBJECTIVES
The objective of this review was to compare the relative benefit and safety profile of the combination of long-acting ß2 agonists (LABAs) and inhaled corticosteroids (ICS) with a higher dose of inhaled corticosteroids in asthmatic patients with or without previous treatment with inhaled corticosteroids. We also wished to examine whether the benefit of either treatment option was influenced by the severity of airway obstruction, age, baseline dose of inhaled corticosteroids to which LABA was added, ICS dose difference between treatment options, use of one or two devices to deliver combination therapy, dose and type of long-acting ß2 agonist and duration of intervention.
METHODS
Criteria for considering studies for this review
Types of studies
Only randomised controlled trials (RCTs) conducted in adults, adolescents and/or children in whom long-acting ß2 agonists were added to inhaled corticosteroids.
Types of participants
Children aged two years and above, adolescents or adults with recurrent or chronic asthma. We did not include studies where pre-treatment excluded inhaled corticosteroids. The comparison of combination therapy with higher dose steroids in steroid naive patients is covered in Ni Chroinin 2009a.
Types of interventions
Long-acting ß2 agonist administered twice a day (e.g. salmeterol or formoterol) combined with inhaled corticosteroids compared to a higher dose of inhaled corticosteroids with or without placebo. Delivery of therapy could be either via one or two inhaler devices. Other co-interventions such as xanthines, anticholinergics and non-steroidal anti-inflammatory medications were accepted, provided that the dose remained unchanged throughout the study. The intervention must have been administered for at least 28 days at fixed doses. Inhaled short-acting ß2 agonists and short courses of oral corticosteroids were permitted rescue interventions.
Types of outcome measures
Primary outcomes
The primary outcome was the proportion of participants with asthma exacerbations requiring a short course of systemic corticosteroids.
Secondary outcomes
Proportion of participants in each group requiring hospital admission for asthma.
Withdrawals.
Serious adverse events.
Pulmonary function tests.
Symptoms (including days and nights without symptoms, and symptom scores.
Quality of life measured with validated scales.
Rescue use of short-acting ß2 agonists.
Measures of inflammation, such as serum eosinophils, serum eosinophil cationic protein and sputum eosinophils.
Clinical and biochemical adverse effects related to treatment were examined for all those that were systematically sought and documented.
Search methods for identification of studies
Electronic searches
A search was carried out in the Cochrane Airways Review Group’s ‘Asthma and Wheez* RCT’ register, which is derived from a comprehensive search of EMBASE (1980 to May 2008), MEDLINE (1966 to May 2008) and CINAHL (1982 to May 2008). In addition, we handsearched 20 of the most productive respiratory care journals and added relevant randomised controlled trials to the register. This register also contains a variety of studies published in foreign languages. We did not exclude trials on the basis of language.
The search of the database used the following terms: (((beta* and agonist*) and long-acting or “long acting”) or ((beta* and adrenergic*) and long-acting or “long acting”) or (bronchodilat* and long-acting or “long acting”) or (salmeterol or formoterol or advair or symbicort)) and (((corticosteroid* or corticosteroid* or corticosteroid*) and inhal*) or (budesonide or beclomethasone or fluticasone or triamcinolone or flunisolide)).
Searching other resources
We searched the clinical trials register of The Cochrane Collaboration (the Central Register of Controlled Trials (CENTRAL)) using the above search strategy. We reviewed reference lists of all included studies and reviews to identify potentially relevant citations.
We also made enquiries regarding other published or unpublished studies known to the authors of the included studies or to the pharmaceutical companies who manufacture the agents (GlaxoSmithKline, Astra Zeneca and Novartis). We searched registers of published and unpublished clinical trial data (http://www.ctr.gsk.co.uk; http://www.clinicalstudyresults.org; http://www.astrazenecaclinicaltrials.com; http://www.novartisclinicaltrials.com).
Data collection and analysis
Selection of studies
From the title, abstract or descriptors, one of the authors (IRG or MNC and FMD or TJL) independently reviewed the literature searches. We excluded all studies that were clearly not randomised controlled trials or that clearly did not fit the inclusion criteria. Two authors (IRG or MNC and FMD or TJL) reviewed all other citations independently in full text, assessing for inclusion based on study design, population, intervention and outcome.
Data extraction and management
Two authors (IRG or MNC and FMD or TJL) independently extracted data for the trials and entered data into the Cochrane Collaboration software program, Review Manager (RevMan) (RevMan 2008). For the 2008 update of the review, one author (TJL) extracted the data.
As a ‘user defined’ item, we recorded the difference in the daily dose of inhaled corticosteroids in the LABA and ICS versus higher ICS groups, reported in chlorofluorocarbon (CFC)-propelled ‘beclomethasone-equivalent’ , where 1 mcg of beclomethasone dipropionate = 1 mcg of budesonide = 0.5 mcg fluticasone propionate (NIH Publication 2007). All doses of inhaled medications are reported based on ex-VALVE, rather than ex-inhaler, values.
Assessment of risk of bias in included studies
We assessed the risk of bias for the allocation, blinding and the handling of missing data from the studies. This is in line with recommendations made in the Cochrane Handbook for Systematic Reviews of Interventions (Handbook 2008). The method for assessing study quality for previous versions of this review is given in Appendix 2.
Dealing with missing data
We contacted study investigators and/or study sponsors for trials with pharmaceutical company sponsorship to obtain verification of study design and information on missing outcome data. We were particularly interested in obtaining verification and missing data for the two outcomes pertaining to exacerbations: those necessitating systemic corticosteroids and those leading to hospital admission. Where we could not determine whether these outcomes had been collected in the studies we contacted the investigators or study sponsors to ascertain whether this information was available for us to use in our analyses.
We sought additional outcome data (such as FEV1 or PEF) which was incompletely reported from the investigators or from the sponsors.
Assessment of heterogeneity
We assessed statistical heterogeneity with the I2 statistic. This gives an estimate of the proportion of heterogeneity between the study results that exceeds what would be expected with the play of chance, expressed as a percentage (Higgins 2003).
Data synthesis
The analysis focused on the following comparison:
Long-acting ß2 agonist (LABA) and inhaled corticosteroids (ICS) versus a higher dose of inhaled corticosteroids as second-line treatment (i.e. in patients who were already taking inhaled corticosteroids at baseline).
Note that given the large size of this review, other comparisons originally stated in the protocol published in 1999 were assessed in two other reviews. This includes comparing the addition of LABA to similar (Ni Chroinin 2005; Ni Chroinin 2009a) and tapering doses of inhaled corticosteroids (Gibson 2005).
If a trial had more than one intervention or control group, we considered additional comparisons, if appropriate. If two comparisons used the same group twice as comparator (e.g. a three-arm study which had two ‘LABA + ICS’ arms but only one ‘higher ICS’ group) (Woolcock 1996a; Woolcock 1996b), we halved the number of participants in the control group (e.g. ICS alone group) to avoid over-representation. For dichotomous outcomes (such as hospitalisation) we halved the control group numerator and denominator.
We calculated treatment effects for dichotomous variables as relative risk (RR) and/or risk difference (RD) with 95% confidence intervals (CI). For continuous outcomes, such as pulmonary function tests, we calculated pooled statistics as mean differences (MD or generic inverse variance) or standardised mean differences (SMD), as indicated, and reported 95% confidence intervals. We tested homogeneity of effect sizes between studies being pooled with the I2 statistic and the Dersimonian & Laird method, with values above 25% and a P < 0.05 being used, respectively, as the cut-off level for statistical significance. In the absence of heterogeneity we used a fixed-effect model (Greenland 1985). If heterogeneity was suggested, we applied the Dersimonian & Laird random-effects model (DerSimonian 1986) to the summary estimates. Unless otherwise specified, the pooled estimates are derived from the fixed-effect model.
We assumed equivalence if the relative risk estimate and its confidence interval were between 0.9 and 1.1. We derived numbers needed to treat (NNT) from the pooled relative risks using Visual Rx (Cates 2002).
Subgroup analysis and investigation of heterogeneity
We planned subgroup analyses to explore possible reasons for heterogeneity of the primary outcome and, in the absence of heterogeneity, to identify potential effect modifiers for which the magnitude of benefit may change according to the value of characteristic (e.g. severity of airway obstruction). We examined the following a priori defined subgroups to explore their influence on the magnitude of effect (effect modification).
Magnitude of airway obstruction at baseline as determined by the mean group percent predicted forced expiratory volume in 1 second (FEV1) classified as mild (FEV1: >= 80%), moderate (FEV1 61% to 79%), or severe (FEV1 <= 60%) (GINA 2008).
- Dose of inhaled corticosteroids examined as:
- mean dose (ex-valve) of inhaled corticosteroids in LABA group, reported in CFC-propelled beclomethasone-equivalent (mcg/day);
- dose difference in dose of inhaled corticosteroids (in CFC-propelled beclomethasone equivalent) between the LABA and the higher ICS groups. When not reported, an estimate of the mean was made based on the provided range.
Long-acting ß2 agonist (salmeterol/formoterol).
Children (< 18 years) versus adults.
Use of one or two devices to deliver the combination of ICS + LABA.
Trial duration (in weeks).
We examined difference in the magnitude of effect attributable to these subgroups with the residual Chi2 test from the Peto odds ratios (Deeks 2001). The number of trials allowed us to conduct a multivariate meta-regression to examine the simultaneous impact of, and interaction between the above-named variables on, the heterogeneity of patients with exacerbations requiring systemic corticosteroids. We built backward and forward models using these subgroups as well as using FEV1 (L), dose of inhaled corticosteroids in the LABA group (mcg/day), dose difference in ICS between LABA and control group (mcg/day) and trial duration as continuous variables, using P < 0.10 as entry and exit criteria (Stata, Version 8.2, Stata Corporation, Texas, USA).
Sensitivity analysis
We performed sensitivity analyses to investigate the potential impact of the following variables on the primary outcome:
risk of bias;
publication bias;
funding source.
We used funnel plots to examine the possibility of publication bias (Egger 1997). The fail-safe N test was used to estimate the number of unpublished studies required to reverse the observed group difference (Gleser 1996).
RESULTS
Description of studies
See: Characteristics of included studies; Characteristics of excluded studies.
Results of the search
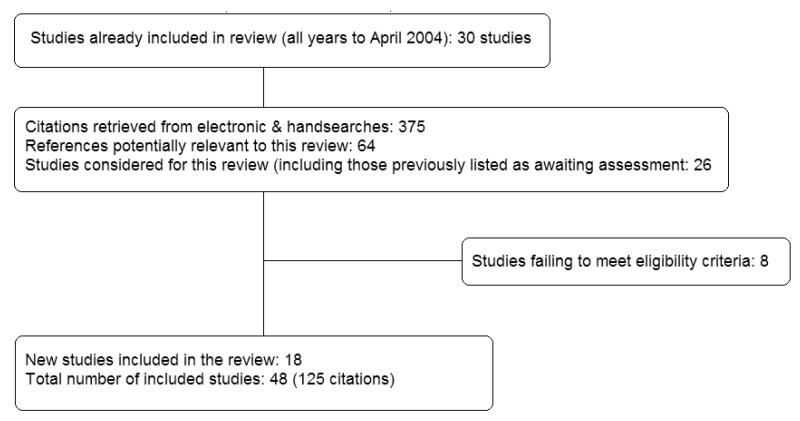
For an archive of previous search detail see Table 1. Literature searches conducted between April 2004 and May 2008 yielded 375 citations, from which we included 18 studies. Figure 1 illustrates the handling of literature search results and inclusion of studies in this update.
Table 1.
Search history
| Years | Detail |
|---|---|
| All years to April 2004 | Citations identified: 593 |
| Excluded: 551 for the following reasons | |
|
|
| Due to the large number of citations considered, the reasons for exclusion are provided only for published randomised controlled trials |
Figure 1.
Literature flow diagram for June 2008 update of the review.
The current review aggregates 47 trials recruiting 15,155 participants. One trial contributed two intervention groups which were both compared to the same control group (Woolcock 1996a;Woolcock 1996b). Therefore we evaluated 48 different studies since we considered them as separate data sets in this review for ease of description. A total of 125 citations reported the 48 included studies.
Two studies are available as conference abstracts (Joshi 2005;Ortega-Cisneros 1998). We downloaded 12 studies from manufacturers’ online trial results registries, and we have not been able to identify a full-text journal article for them: D5896C00001;SAM30013; SAM30022; SAM40012; SAM40090; SAM40120;SAS40013; SAS40026; SD 039 0726; SD 039 0728; SFCF4026;SLGA5021. From a further 12 reports identified from these web-sites, we were able to identify and include data previously unavailable from full-text trial reports (Bateman 2003; Bergmann 2004;Busse 2003; Condemi 1999; Greening 1994; Ind 2003; Jenkins 2000; Johansson 2001; Kelsen 1999; Murray 1999; Verberne 1998; Woolcock 1996a; Woolcock 1996b).
Included studies
Forty-six studies had a parallel design while two were cross-overs (Green 2006; Heuck 2000). Detailed descriptions of each study are given in the ‘Characteristics of included studies’ table. An overview of these studies is given below.
Participants
Forty studies focused on adults and six on children exclusively (Heuck 2000; Ortega-Cisneros 1998; SAM104926; SAM40012;SAM40100; Verberne 1998). Two studies included both children and adults (LOCCS; O’Byrne 2005). There were a total of 1155 children and 14,000 adults recruited to the studies.
Participants had inadequate control of their asthma at the time of enrolment in all but three studies (LOCCS; Pearlman 1999;Vermetten 1999). Severity of airway obstruction was generally moderate, with a baseline FEV1 or PEF 60% to 80% of predicted in 23 studies. Twelve studies recruited patients with minimal airway obstruction, with a mean baseline FEV1 or PEF of 80% of predicted or more (Busse 2003; Green 2006; Kips 2000;Lalloo 2003; Li 1999; LOCCS; O’Byrne 2001; SAM104926;SAM40012; SFCF4026; Verberne 1998; Vermetten 1999; Wallin 2003). Three of the paediatric trials failed to report baseline severity (Heuck 2000; Ortega-Cisneros 1998; SAM40100). In the majority of manufacturer’s study reports available from the Glaxo-SmithKline website, baseline FEV1 predicted was not available.
All but four studies required the intake of inhaled corticosteroids for a minimum of one to three months prior to randomisation.Condemi 1999 included a proportion of patients who were corticosteroid-naive prior to enrolment, but who remained symptomatic despite inhaled corticosteroids during the two to four-week run-in phase. We considered this study to have recruited patients with sub-optimal control on inhaled corticosteroids.
The presence of atopic disease at baseline was reported in four studies. Two of these trials reported atopy in more than 80% of its participants (Li 1999; Verberne 1998), while 60% were atopicin Wallin 2003.
Smoking status was reported in 22 trials. Thirteen trials specifically reported the absence or exclusion of active smokers (>= 10 cigarettes/day) (Baraniuk 1999; Bateman 2006; Bergmann 2004; Condemi 1999; Johansson 2001; Kelsen 1999; Lalloo 2003;Li 1999; Pearlman 1999; SAM40120; SAS40013; SAS40026;SFCF4026; SLGA5021). Six trials reported the proportion of active smokers as being between 1% to 10% (Bateman 2003;Mitchell 2003) and 15% to 33% (Greening 1994; Vermetten 1999; Woolcock 1996a; Woolcock 1996b).
Type of long-acting ß2 agonist, delivery device, inhaled steroid and co-treatment
The long-acting ß2 agonist preparation was salmeterol xinafoate in 35 studies and formoterol in the remaining 13. All but three tested the standard dose of the long-acting ß2 agonist (salmeterol 50 mcg bid and formoterol 12 mcg bid). One study tested a double dose of salmeterol, i.e. 100 mcg bid (Woolcock 1996a), one study assessed a double dose of formoterol (SD 039 0728) and two studies tested a 6 mcg bid dose of formoterol (Bateman 2003; Lalloo 2003).
Twenty-five studies examined long-acting ß2-agonists in combination with corticosteroids in the same device (Bateman 2003;Bateman 2006; Bergmann 2004; Busse 2003; D5896C00001; Ind 2003; Jenkins 2000; Johansson 2001; Joshi 2005; Lalloo 2003;LOCCS; O’Byrne 2005; SAM104926; SAM30013; SAM30022;SAM40012; SAM40090; SAM40100; SAM40120; SAS40013;SAS40026; SD 039 0726; SD 039 0728; SFCF4026; Zhong 2005). The remaining studies tested the delivery of LABA and ICS by separate devices. Adherence to study medication was monitored during the run-in and/or the treatment period in 13 studies (Baraniuk 1999; Bateman 2003; Busse 2003; Fowler 2002;Greening 1994; Heuck 2000; Kelsen 1999; Kips 2000; Lalloo 2003; Murray 1999; O’Byrne 2005; Pauwels 1997; Pearlman 1999), but adherence observed during the trial was seldom reported, nor used for efficacy or subgroup analyses.
The type of inhaled corticosteroid varied among the studies. Forty-three studies compared the same inhaled corticosteroid preparation in both the LABA and the control groups. Ten studies compared CFC-beclomethasone, 11 trials assessed budesonide and 22 assessed fluticasone.
Five studies compared the combination of fluticasone propionate and long acting ß2 agonist to CFC-beclomethasone (Jenkins 2000; SAM30022), budesonide (Johansson 2001; Zhong 2005) or HFABDP (Fowler 2002) in the higher ICS group. One study compared the combination of LABA and the patients’ own pre-study corticosteroid to additional fluticasone in the higher ICS group (Li 1999). Finally, one study compared budesonide and long acting ß2 agonist to fluticasone propionate in the higher ICS group (Bateman 2003).
After conversion of all doses of inhaled corticosteroids in CFC-equivalent (NIH Publication 2007), the median dose (25th, 75th) of inhaled corticosteroids in the LABA group was 400 (400, 800) with a range of 200 to 1000 mcg/day, while the median dose in the higher ICS group was 1000 (800, 1000) with a range of 400 to 2000. The median absolute dose difference between the intervention and the control group was 600 (400, 600) mcg/day with a range of 200 to 1200. When stated as median relative ICS dose difference, the control group tested a quite homogenous 2.5-fold (2, 2.5) increase in ICS dose as compared to the LABA group. Of note, in absence of adequate details provided by the study by Van Noord 1999, we assumed that an equal proportion of patients of the intervention group received 100 and 250 mcg/ day of fluticasone, respectively, for an average daily intake of 700 mcg/day of beclomethasone-equivalent in the LABA + ICS group and double in the higher ICS group.
Co-interventions with other prophylactic medications, such as xanthines, sodium cromoglycate and anticholinergics, was permitted in nine studies provided that doses remained unchanged throughout the trial (Baraniuk 1999; Bergmann 2004; Greening 1994; Ind 2003; Johansson 2001; Murray 1999; Van Noord 1999;Woolcock 1996a; Woolcock 1996b). Inhaled short-acting ß2 agonist was permitted in all the trials as rescue medication.
Study duration
The duration of the trials was variable: four weeks (Fowler 2002; Green 2006; Pearlman 1999), six weeks (Heuck 2000;SAM40100; Zhong 2005), 12 weeks (Baraniuk 1999; Bateman 2003; Bateman 2006; Bergmann 2004; Bouros 1999; Busse 2003;Johansson 2001; Joshi 2005; Lalloo 2003; Li 1999; Mitchell 2003;Ortega-Cisneros 1998; SAM30013; SAM30022; SAM40090;SAM40120; SAS40026; Van Noord 1999; Vermetten 1999;Wallin 2003), 24 weeks (Condemi 1999; Greening 1994; Ind 2003; Jenkins 2000; Kelsen 1999; Murray 1999; SAM40012;SFCF4026; SLGA5021; Woolcock 1996a; Woolcock 1996b); 52 weeks (Kips 2000; O’Byrne 2001; O’Byrne 2005; Pauwels 1997) and 54 weeks (SAS40013; Verberne 1998). In Busse 2003, to avoid over-representation of patients randomised to the 24-week arm and who contribute data both at 12 weeks and 24 weeks, we only used the 12-week data for all patients irrespective of whether they were randomised to the 12-week (part 1) or the 24-week (part 2) study.
Funding source
Most of the studies (44) were funded by producers of long-acting ß2 agonists. Thirty-three studies were supported by GlaxoSmithK-line, seven by Astra Zeneca (Bateman 2003; D5896C00001;Lalloo 2003, O’Byrne 2001; O’Byrne 2005; SD 039 0726; SD 039 0728), two by Astra Draco (Kips 2000; Pauwels 1997) and two by Novartis (Bouros 1999; Mitchell 2003). Source of funding was unspecified in three trials (Heuck 2000; Joshi 2005; Ortega-Cisneros 1998) and one trial was supported by an anonymous grant (Fowler 2002).
Excluded studies
A total of 286 studies (392 citations) failed to meet the eligibility criteria of this review. The reasons for their exclusion are detailed in the ‘Characteristics of excluded studies’ table.
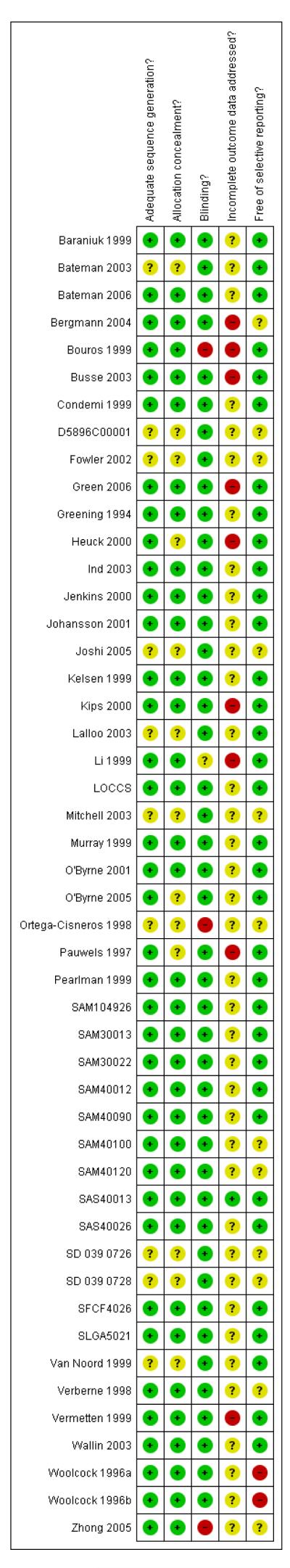
Risk of bias in included studies
An overview of our judgements of bias protection for each study is given in Figure 2. We confirmed the methodology of 15 trials directly with the authors of the published trial reports.
Figure 2.
Methodological quality summary: review authors’ judgements about each methodological quality item for each included study.
Allocation
Following correspondence we have ascertained the randomisation procedure for a number of GlaxoSmithKline-sponsored studies. We have judged that the procedures for generating and concealing allocation put the GlaxoSmithKline-sponsored studies at a low risk of selection bias (Appendix 3).
Blinding
With the exception of three studies, blinding with identical inhaler devices to deliver therapy, or a double-dummy design as a means of protecting against detection bias, was used in the studies. The remaining study designs were open label (Bouros 1999; Ortega-Cisneros 1998; Zhong 2005).
Incomplete outcome data
The meaning of ‘intention-to-treat’ populations was left undefined in all the studies where this was mentioned. In nine studies the population analysed was either restricted to completers or the last observation was carried forward (see Figure 2). In the remaining trials we could not ascertain how the population analysed was composed.
Other potential sources of bias
One small study stated how many patients were screened for eligibility. Eighteen trials reported the percentage of run-in participants that were successfully randomised. This ranged from 35% (Busse 2003) to 100% (Fowler 2002) of recruited patients.
Effects of interventions
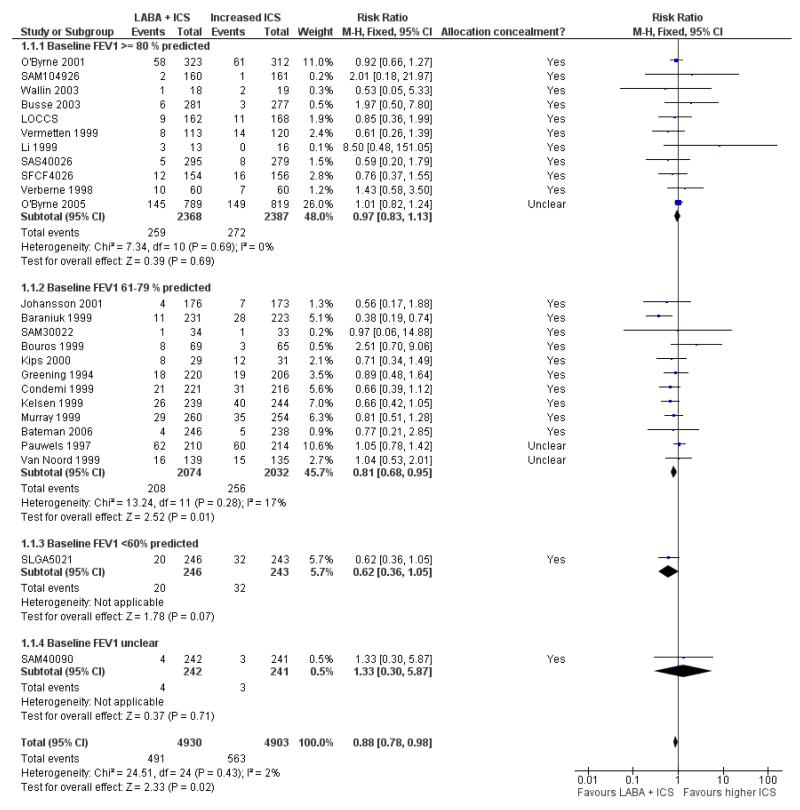
Primary outcome: oral steroid-treated exacerbations
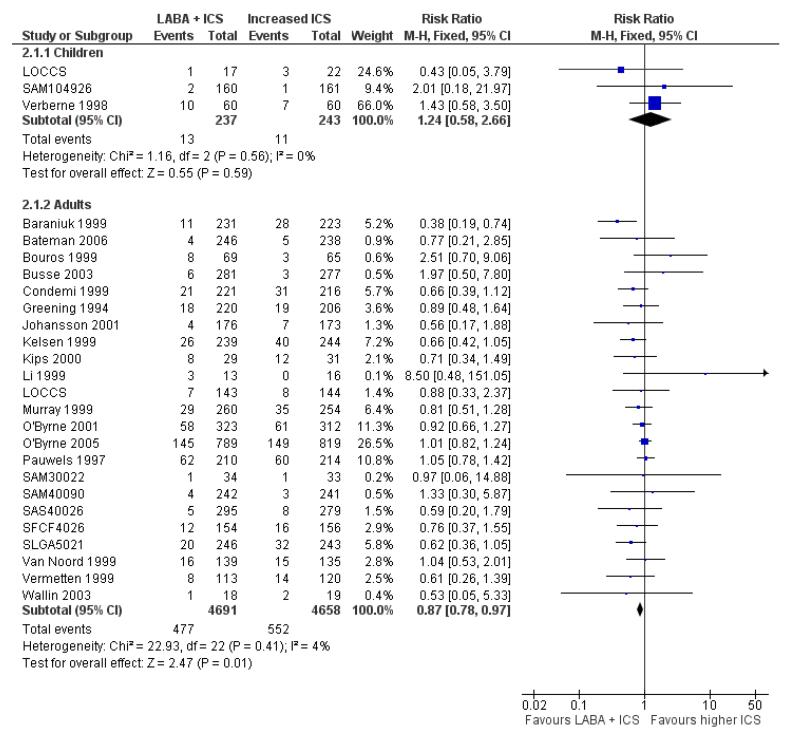
Beta-2 adrenergic agonist (LABA) + inhaled corticosteroid (ICS) treatment led to a lower risk of oral steroid-treated exacerbations than higher doses of ICS (RR 0.88, 95% CI 0.78 to 0.98, P = 0.02; Figure 3, N = 25 studies, 9833 participants). There was no evidence of publication bias as the Egger’s test for bias was −0.23(95% CI −1.95 to 1.48). There was no evidence of statistical heterogeneity between studies (I 2 = 2%).
Figure 3.
Forest plot of comparison: 1 LABA + ICS versus higher dose ICS, outcome: 1.1 # patients with exacerbations requiring oral steroids.
The risk difference was −0.01 (−0.02 to −0.00). Based on the total number of participants with oral steroid-treated exacerbations, the effect of LABA was to reduce the risk of exacerbations from 11.45% in the higher ICS group to 10% in the combination groups. This is compatible with a number needed to treat (NNT) of 73(95% CI 42 to 437) from studies with a median duration of 12 weeks. However, due to variation in the rate of rescue oral corticosteroids in the control groups, we also calculated NNTs for four different control group risks based on control group risk quartiles (see Table 2):
| Risk status | Median control group risk (%) [range] | Median study duration (weeks) [range] | Mean FEV1 [range] | NNT (benefit) |
|---|---|---|---|---|
| Low | 1.24 [0 to 3.03] | 12 [12 to 12] | 81.7 [70 to 102] | 673 |
| Low to medium | 7.89 [2.86 to 9.43] | 12 [12 to 24] | 83.8 [74 to 92] | 106 |
| Medium to high | 12.11 [11.11 to 13.78] | 18 [12 to 54] | 72 [61 to 88] | 69 |
| High | 18.87 [14.35 to 38.71] | 52 [24 to 52] | 73.4 [61 to 87] | 45 |
Table 2.
Risk status
| Study | Control group rate | Risk quartile |
|---|---|---|
| Li 1999 | 0.00 | Low |
| SAM104926 | 0.01 | Low |
| Busse 2003 | 0.01 | Low |
| SAM40090 | 0.01 | Low |
| Bateman 2006 | 0.02 | Low |
| SAS40026 | 0.03 | Low |
| SAM30022 | 0.03 | Low |
| Johansson 2001 | 0.04 | Low/medium |
| Bouros 1999 | 0.05 | Low/medium |
| LOCCS | 0.07 | Low/medium |
| Greening 1994 | 0.09 | Low/medium |
| SFCF4026 | 0.09 | Low/medium |
| Wallin 2003 | 0.11 | Low/medium |
| Van Noord 1999 | 0.11 | Medium/high |
| Verberne 1998 | 0.12 | Medium/high |
| Vermetten 1999 | 0.12 | Medium/high |
| Baraniuk 1999 | 0.13 | Medium/high |
| SLGA5021 | 0.13 | Medium/high |
| Murray 1999 | 0.14 | Medium/high |
| Condemi 1999 | 0.14 | High |
| Kelsen 1999 | 0.16 | High |
| O’Byrne 2005 | 0.18 | High |
| O’Byrne 2001 | 0.20 | High |
| Pauwels 1997 | 0.28 | High |
| Kips 2000 | 0.39 | High |
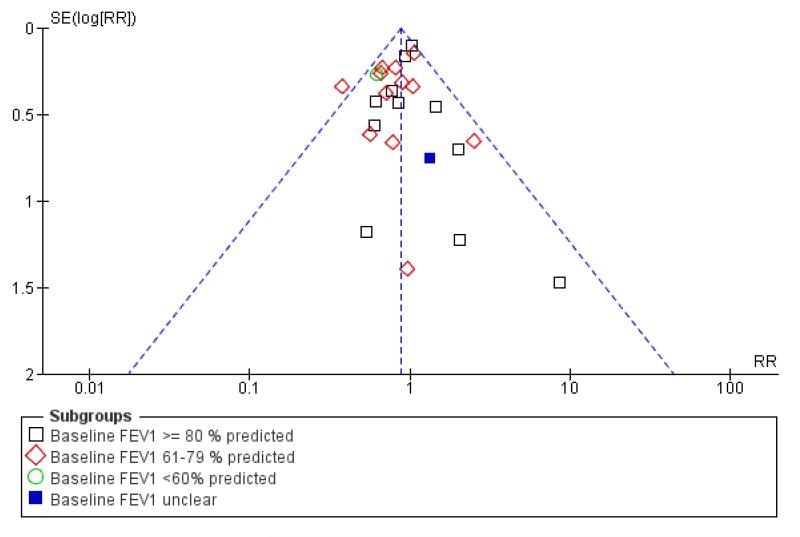
Visual inspection of the funnel plot did not suggest any significant asymmetry in the analyses we assembled (Figure 4). The fail-safe N test estimated that 154 studies would be needed to reverse the observed group difference.
Figure 4.
Funnel plot of comparison: 1 LABA + ICS versus higher dose ICS, outcome: 1.1 # patients with exacerbations requiring oral steroids.
Sensitivity analysis by allocation sequence generation, allocation concealment and blinding did not materially affect the strength or direction of the results (Analysis 2.9; Analysis 2.10; Analysis 2.11).
Among studies contributing data to the main outcome, the median dose (interquartile range) of inhaled corticosteroids in the LABA group was quite homogeneous at 400 (400 to 400) with a range of 200 to 1000 mcg/day, while the median dose in the higher ICS group was 1000 (800 to 1000). The median absolute dose difference between the intervention and the control group was 600 (400 to 600) mcg/day. The median FEV1 was 77 (71 to 85)% of predicted and the median treatment duration was 12 (12 to 24) weeks. All studies were funded by the manufacturer.
We had planned a priori analyses to explore the influence of the a number of variables on the magnitude of effect (effect modification or confounding). From the subgroup analyses both LABA type and study duration gave statistically significant results. Studies testing salmeterol show a significantly greater group difference in favour of combination therapy than those testing formoterol (RR 0.75 versus 1.00). The ratio of these risk ratios (RRR) was 1.33, 95% CI 1.07 to 1.67 (Analysis 2.4). Studies of six months duration or less were also significantly more likely to be associated with a reduced risk of rescue oral steroids (i.e. a larger effect size) than longer duration trials (RR 0.72 versus 1.00; RRR 1.37, 95% CI 1.05 to 1.78, Analysis 2.6). Both variables were highly correlated (r = −0.70), and the correlation made it impossible to disentangle the relative contribution of either LABA type or duration of study to the size of effect. It is noteworthy that the dose of LABA, dose of ICS dose combined with LABA, ICS dose difference between the two groups, number of devices to deliver combination therapy, and publication status were not important effect modifiers. The majority of studies recruited adults: the subgroup estimate for these studies favoured the use of LABA in reducing the risk of oral steroid treatment (RR 0.87, 95% CI 0.78 to 0.97). In children the result was not statistically significant (RR 1.28, 95% CI 0.58 to 2.66, Figure 5). Although the test for interaction between these subgroup analyses gave a non-statistically significant result (P = 0.29), the RRR included the possibility that children could be almost three times more likely than adults to require oral-steroids when treated with a LABA than they were when treated with increased steroids (RRR 1.42, 95% CI 0.73 to 2.77).
Figure 5.
Forest plot of comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), outcome: 2.4 # patients requiring oral steroids: children versus adults.
The meta-regression provided additional information. Since one study included a group with zero events (Li 1999), we entered 0.1 for missing data to allow the meta-regression to be performed on all 27 studies contributing to the main outcome: sensitivity analysis excluding Li 1999 did not affect the results. The multivariate regression suggested that higher baseline FEV1, children and formoterol were associated with increased risk of poor response to combination therapy.
Secondary outcomes
Hospital admission and withdrawal
There was no significant group difference in the risk of patients with exacerbation requiring hospitalisation (RR 1.02, 95% CI 0.67 to 1.56, N = 33) (Analysis 1.2). In 10 studies there were no confirmed events.
A post-hoc subgroup analysis on age gave two non-statistically significant subgroup results, but where the effect was in opposite directions (adults: RR 0.87, 95% CI 0.54 to 1.38; children: RR 2.21, 95% CI 0.74 to 6.64) (Analysis 2.12). The confidence interval around the RRR included unity, but does not rule out a greater than eight-fold greater risk of hospitalisation with LABA in children when compared with adults (RRR 2.66, 95% CI 0.81 to 8.78).
The use of LABA significantly reduced the number of withdrawals due to poor asthma control (RR 0.71, 95% CI 0.56 to 0.91, 29 studies) (Analysis 1.3). There was a borderline difference favouring combination therapy in the number of overall withdrawals (RR 0.92, 95% CI 0.84 to 1.00, 39 studies) (Analysis 1.4). There was no significant difference in the risk of withdrawals due to adverse events (RR 0.99, 95% CI 0.78 to 1.26, 30 studies) (Analysis 1.5).
Lung function - end of treatment values
The combination of LABA and ICS provided significantly higher lung function at endpoint compared to increased dose of ICS for: FEV1 (0.08 L, 95% CI 0.03 to 0.13, 11 studies)(Analysis 1.6); % predicted FEV1 (1.78%, 95% CI 0.39 to 3.18, seven studies) (Analysis 1.7), morning PEF (23.31 L/min, 95% CI 18.09 to 28.52, random-effects model, 14 studies) (Analysis 1.11) or in % predicted (3.45%, 95% CI 1.28 to 5.63, five studies)(Analysis 1.13); and evening PEF (16.79 L/min, 95% CI 10.72 to 22.85, four studies) (Analysis 1.14). There were insufficient data (less than two trials) to aggregate the PEF variability at endpoint.
Lung function - change from baseline
The combination of LABA and ICS provided significantly greater improvement in lung function compared to increased dose of ICS for: FEV1 (0.08 L, 95% CI 0.06 to 0.09, 22 studies) (Analysis 1.8), in morning or clinic PEF in L/min at endpoint (16.30 L/ min, 95% CI 13.48 to 19.11, random-effects model, 30 studies) (Analysis 1.12), and in evening PEF in L/min at endpoint ((13.70 L/min, 95% CI 10.28 to 17.12, random-effects model, 22 studies) (Analysis 1.16). The change in PEF variability also supported the use of combination therapy (−4.55, 95% CI −6.32 to −2.78, seven studies) (Analysis 1.19).
Change from baseline in % predicted FEV1 was not significant (0.35%, 95% CI −0.18 to 0.87, random-effects model, four studies) (Analysis 1.10). The improvement in FEV1 observed within six weeks (+ 90 mL) is sustained until 12 (+ 100 mL), 24 weeks (+ 90 mL) and 52 weeks (+ 70 mL), with no significant effect of timing (P = 0.75) (Analysis 1.9).
Symptoms
The change in daytime symptom score (SMD −0.26, 95% CI −0.35 to −0.17, five studies) (Analysis 1.20); overall (24 hours) symptom score (SMD −0.23, 95% CI −0.37 to −0.08, random-effects model, six studies) (Analysis 1.21); change in percent symptom-free days at endpoint (9.18%, 95% CI 6.02 to 12.33, random-effects model, 12 studies) (Analysis 1.22) and % nighttime awakenings at endpoint (−0.40; 95% CI −0.55 to −0.25, fixed-effect model, two studies) (Analysis 1.29); all favoured combination therapy. However, there was no significant group difference in percentage of symptom-free days at endpoint (5.81%, 95% CI −1.14 to 12.76, random-effects model, eight studies) (Analysis 1.23); daytime symptoms at endpoint (SMD −0.28, 95% CI −0.67 to 0.11, random-effects model, five studies) (Analysis 1.24); nighttime symptoms at endpoint (SMD −0.24, 95% CI −0.49 to 0.01, three studies) (Analysis 1.25); change in nighttime symptoms (SMD −0.01, 95% CI −0.04 to 0.01, two studies) (Analysis 1.26); percentage of symptom-free nights at endpoint (−2.10%; 95% CI −7.98 to 3.79, two studies) (Analysis 1.27), and in the change from baseline in nighttime awakenings (SMD −0.03, 95% CI −0.10 to 0.04, seven studies) (Analysis 1.28). Because of insufficient data, the following outcomes could not be pooled: % nights with no awakenings at endpoint (Analysis 1.30) and change in % nights with no awakenings (Analysis 1.30).
Rescue medication use
The change in daytime rescue inhalations of short-acting ß2 agonist favoured the combination of LABA and ICS (−0.48 puffs/ d, 95% CI −0.77 to −0.20, random-effects model, five studies) (Analysis 1.32) as did the change in nighttime inhalations (SMD −0.13, 95% CI −0.21 to −0.05, random-effects model, four studies) (Analysis 1.33), the change in rescue inhalations over 24 hours (−0.20, 95% CI −0.29 to −0.11, 12 studies) (Analysis 1.34) and the change in mean percent of rescue-free days at endpoint (11.48%, 95% CI 7.98 to 14.98, fixed-effect model, three studies) (Analysis 1.39). There was no group difference at endpoint in the number of daytime rescue inhalations (−0.44, 95% CI −0.94 to 0.06, five studies) (Analysis 1.35); nighttime rescue inhalations (−0.09, 95% CI −0.23 to 0.04, random-effects model, four studies) (Analysis 1.36); % overall rescue-free days (5.14%, 95% CI −2.79 to 13.08, random-effects model, three studies (Analysis 1.37). No pooling was possible for the change in asthma control days (Analysis 1.40), percent asthma control days at endpoint (Analysis 1.44) and the change in percent symptom-free days (Analysis 1.38).
Quality of life
There was no group difference in the change from baseline in quality of life measured by the Juniper Questionnaire (0.10, 95% CI −0.06 to 0.26, four studies) (Analysis 1.41).
Inflammatory markers
Few trials reported inflammatory markers. There was no group difference in the change from baseline in serum ECP (0.62 mcg/ L, 95% CI −2.45 to 3.70, two studies) (Analysis 1.45). Only one trial reported total exhaled nitric oxide at endpoint, preventing pooling.
Adverse events
The risk ratio of serious adverse events (including all cause hospital admission) was 1.12 (95% CI 0.91 to 1.37) (Analysis 1.52). This estimate is based on data from 35 studies.
There was significantly more tremor in the LABA group (RR 1.84, 95% CI 1.20 to 2.82, 11 studies) (Analysis 1.53), although this result became non-significant when the one study using a higher dose of LABA was excluded (Woolcock 1996a). There was significantly less oral thrush on LABA and ICS compared with the higher dose of ICS (RR 0.58, 95% CI 0.40 to 0.86, 14 studies) (Analysis 1.54).
One study assessed growth in children, with a significantly better short-term rate of growth in the LABA and ICS group over 12 months (0.9 cm, 95% CI 0.20 to 1.60). There were insufficient trials reporting these outcomes to aggregate adrenal suppression and osteopenia.
There was no group difference in the following.
Overall side effects (RR 0.99, 95% CI 0.95 to 1.03, 30 studies) (Analysis 1.55).
Adverse cardiovascular events (RR 0.99, 95% CI 0.49 to 2.01, random-effects model, nine studies) (Analysis 1.56).
Headache (RR 1.02, 95% CI 0.92 to 1.12, 25 studies) (Analysis 1.57).
Hoarseness (RR 0.95, 95% CI 0.79 to 1.14, nine studies) (Analysis 1.58).
Tachycardia/palpitations (RR 1.20, 95% CI 0.78 to 1.84, 15 studies) (Analysis 1.59).
DISCUSSION
The review demonstrates that the addition of long-acting inhaled ß2 agonists (LABA) to moderate doses of inhaled steroids (ICS) reduces the relative risk of oral steroid-treated exacerbations by around 12% and the absolute risk by about 1%. The evidence that forms the basis of this result is predominantly from adults. In children the evidence for the use of LABAs over increased doses of inhaled steroids is less favourable towards LABA, and includes the possibility that increased steroids is superior in reducing the requirement for oral steroids and hospital admissions. Overall 73 patients need to be treated with combination therapy to prevent one use of rescue oral corticosteroids. Based on number needed to treat (NNT) calculations for the different control group risks in the studies included in our analyses, this would mean that 45 patients in the high-risk trials (where study duration was between six and 12 months and study populations had significant airway obstruction), and 673 patients in the low-risk trials (where study duration was between three and six months and study populations had less severe airway obstruction) would need to be treated with a LABA instead of increased dose of ICS in order to prevent one experiencing an exacerbation requiring oral steroids. Although neither the dose of ICS to which LABA was added nor the difference in ICS dose between groups influenced the effect size. These findings predominantly apply to patients who remained symptomatic at baseline despite a median ICS dose of 400 mcg/day.
Neither the dose of ICS to which LABA was added nor the number of devices to administer combination therapy appear to affect the magnitude of protection conferred by LABA, as supported by the subgroup analyses and meta-regression. While no definitive conclusions can be derived from the subgroup analyses and the meta-regression, the findings highlight several factors that appear to influence the magnitude of response to combination therapy compared to higher doses of ICS. These factors, difficult to disentangle due to their correlation, are the LABA used, the duration of treatment, the mean FEV1 and the age group: formoterol, longer duration of treatment, higher mean FEV1 at baseline, and children (versus adults) appear to decrease the efficacy of combination therapy. These apparent effect modifiers should be explored in future studies with a long-term duration (of one year and beyond), to provide confirmatory evidence of the findings our primary analysis.
There is a theoretical possibility that in the long-run higher doses of ICS may be superior to lower doses of ICS in combination with LABA for preventing exacerbations. One cannot rule out the possibility that the addition of LABA to corticosteroids allows the progression or the ongoing presence of airway inflammation, a factor that could become more evident with prolonged exposure to treatment (Reddel 2000). Despite several trials investigating inflammation, most inflammatory markers could not be aggregated due to the various markers measured in different media (serum (Heuck 2000; Fowler 2002), sputum (Li 1999; Kips 2000), bronchoalveolar lavage and bronchial biopsy (Wallin 2003), urine (Heuck 2000) and expired air (Fowler 2002)). This prevented us from examining the impact of either treatment option on most inflammatory markers. Serum ECP (measured in two trials) revealed no group difference after four to six weeks of treatment with 200 to 400 mcg/day of beclomethasone-equivalent combined with LABA. Moreover, the absence of characterisation of the type and amount of airway inflammation, measured for example by sputum analysis, prevented the identification of the best therapy (and the amount of inhaled corticosteroids) needed for individual patients.
Could the beneficial effect of combination therapy be explained by an initial better compliance with combination therapy that tapers down with time to that observed with inhaled corticosteroids alone? Surprisingly, although 13 trials monitored it during the treatment period, compliance was seldom reported, nor were analyses stratified based on compliance. In the absence of these data this hypothesis cannot be tested. Conversely, LABA may have a more rapid effect on lung function and symptoms than ICS and be more effective when needed, that is, when baseline FEV1 is lower. Moreover, the dose of ICS and duration of treatment may differentially affect different manifestations of asthma. Indeed, rapid improvement in lung function and symptoms have been documented with a higher ICS dose (Currie 2003b; Reddel 2000), while the beneficial effect of low doses of ICS on airway hyperreactivity, severe exacerbations and death requires prolonged (more than one year) treatment (Suissa 2001).
With only limited data for our primary outcome available from the seven small paediatric trials and two which recruited adults and children (accounting for 2% of the weight in the results) together with the unreported proportion of adolescents in recruited to the adult studies, there are insufficient data to comment firmly on a differential effect associated with age. However, the trends toward an increased risk of rescue oral corticosteroids and hospital admissions in children on combination therapy merits caution. Careful risk-benefit assessment should be done before using combination therapy instead of higher dose ICS in children aged 12 years or less with due consideration of the uncertain impact on the severity of exacerbations, against the known risk of growth retardation associated with steroids (Sharek 1999). One study measured linear growth in children in this review, and reported a significantly lower growth rate over one year in the higher dose steroid group compared with combination therapy (Analysis 1.60).
Secondary outcomes were uniformly supportive of the beneficial effect of LABA, although the magnitude of benefit on lung function, symptoms and rescue ß2 agonists use appears modest. It is of note that two of the 52-week trials graphically displayed the change in lung function over time and identified an initial improvement favouring combination therapy over higher ICS in the first 24 weeks, with gradually overlapping values thereafter (Kips 2000;Verberne 1998). These downward trends after 24 weeks were less pronounced in the other two trials (O’Byrne 2001; Pauwels 1997). Yet the sustained improvement in FEV1 observed over time makes tachyphylaxis a difficult explanation for the apparent waning protection against exacerbations, particularly since it has been described as occurring within a few weeks of treatment. Morning and evening PEF, whether reported as change or value at endpoint, also favour the use of LABA. The 12% increase in symptom-free days favoured the addition of LABA to ICS. Surprisingly, the use of LABA only reduced the use of rescue ß2 agonists by less than half a puff per day, with a non-significant group difference in nighttime use of rescue medication. No post hoc subgroup analyses on trial duration or dose of ICS were done on secondary outcomes to avoid multiple comparisons. The representation of long-term studies in most secondary outcomes was minimal. In this review the addition of LABA appears somewhat superior to increased ICS in controlling day-to-day symptoms and improving lung function.
With the exception of tremor, the addition of LABA was not associated with any difference compared with higher doses of ICS in overall or specific adverse effects. Removing the study using a higher than licensed dose of LABA yielded a non-statistically significant result between the treatments in tremor. As might be expected, oral candidiasis was more frequent in patients treated with a higher dose of ICS than in those treated with combination therapy. The safety of LABAs remains a question of some controversy since the uncertainty around the pooled effect from combination studies has not ruled important differences in the likelihood of serious adverse events from clinical trial data (Cates 2009a; Cates 2009b). Similarly, our review does not provide conclusive proof of the safety of LABAs when compared with high-dose steroids alone, even though the pooled result includes unity. In the absence of systematic documentation of the adverse effects specific to inhaled corticosteroids (i.e. adrenal dysfunction, osteopenia and growth in children) or LABAs, the long-term safety of either strategy, particularly in children remains to be demonstrated. There is an urgent need to conduct studies addressing this question with systematic assessment of these potential adverse effects. In summary, while the data provide some reassurance, there is some uncertainty around the risk of severe adverse health events associated with the use of LABA even in presence of inhaled corticosteroids, and particularly so in children.
To whom can these results be generalised? Patients included in the eligible trials were largely adults, who were symptomatic on their current inhaled corticosteroids dose, demonstrated significant (>= 12% or 15%) reversibility in FEV1 with ß2 agonist and did not have severe airway obstruction or recent asthma exacerbations. The reversibility to bronchodilator tends to favour the LABA option over inhaled corticosteroids and may seriously limit generalisability since reversibility to bronchodilator is a criteria met in less than 10% of patients at a given point in time (Storms 2003). Since pregnant or lactating women as well as those of childbearing age without appropriate contraception were generally not eligible, a large proportion of females were probably excluded. Few studies reported the smoking status of their patients. This raises an important question regarding applicability of findings to smokers, a group that has been shown to display significant resistance to both oral (Chaudhuri 2003) and inhaled (Chalmers 2002) corticosteroids. Recognising the possibility of patient selection bias, the findings may be applied to adult asthmatics who remain symptomatic on 400 mcg/day of beclomethasone or equivalent, with a mild or moderate airway obstruction reversible with bronchodilator. With the small weight carried by paediatric trials, generalising these results to children would be inappropriate (Ni Chroinin 2009b). No data are available for preschool-aged children.
To our knowledge, this systematic review is the largest meta-analysis comparing the relative benefit and harms of the combination of LABA and inhaled corticosteroids to a higher dose of inhaled corticosteroids. It provides complementary information to another Cochrane Review examining the relative benefit of adding LABA or a leukotriene receptor antagonist to inhaled corticosteroids (Ducharme 2006). The three options currently recommended by international consensus statements in the face of sub-optimal asthma control on inhaled corticosteroids have now been covered by Cochrane Reviews. The results of this review are strengthened by the overall high methodological quality of the included trials and confirmation of methodology and data by authors or sponsors of several trials, including the provision of unpublished data. The present review had sufficient power to explore variables associated with the effectiveness of either treatment option. In future research priority should be given to addressing the large gap in knowledge related to these two treatment options in children and adolescents.
AUTHORS’ CONCLUSIONS
Implications for practice
In adult patients who remain symptomatic on 400 mcg/day of beclomethasone or equivalent, two strategies may be considered: adding a long-acting ß2 agonist (LABA) or increasing the dose of inhaled corticosteroids (ICS) to 800 or 1000 mcg/day. There is a slight but significant difference favouring LABA in offering protection against the risk of exacerbations requiring systemic corticosteroids. The reduction in the relative risk is 12% while the absolute reduction is about 1%, with an overall number needed to treat to prevent an exacerbation of 72, which varies from 45 from high-event studies(predominantly long-term ones) to 772 in low-event studies. Baseline FEV1, treatment duration and type of LABA may modify the magnitude of effect, although we can only speculate about their true relationship to the overall effect as the latter two are themselves highly correlated with each other. The combination of long-acting ß2 agonists with inhaled corticosteroids leads to greater but modest improvement in FEV1 (+ 80 mL), symptoms and rescue ß2 agonists (−0.5 puff/day) than a 2 to 2.5-fold higher dose of inhaled corticosteroids, although most of the data come from trials of six months or less. Studies conducted in school-aged children contributed few data to the primary outcome and we cannot comment firmly on the relative treatment effect in children and adolescents. Due to the apparent trend toward higher risk of exacerbations requiring systemic steroids and hospital admission, caution should be advised when considering use of combination therapy in children as higher ICS dose may be preferable. However, impaired growth in children treated with higher doses of inhaled steroids has been identified in one study, and this should be weighed against the uncertain (and possibly unfavourable) effects of combination therapy on oral steroid requirement in children. The lack of group difference in reported side effects should be interpreted with caution in the absence of systematic documentation of airway inflammation parameters, as well as adverse effects typically associated with long-term use of inhaled corticosteroids (osteopenia, growth and adrenal suppression), particularly in children.
Implications for research
To address the current gaps in knowledge, future trials should focus on the paediatric and adolescent populations, in whom the gap in knowledge is particularly pressing, and investigate the impact of treatment duration of LABA of the effect size. Moreover, there is a need to characterise patients at baseline better (in terms of type and amount of airway inflammation, phenotype, genotype, smoking status, etc.) to examine the relative efficacy of each treatment strategy for individual patient characteristics.
Studies should consider the following design characteristics.
Long-term interventions >= 52 weeks.
Stratifying on, and providing subgroup analyses for, children and adolescents.
Stratifying on, and providing subgroup analyses for, patients with mild, moderate and severe obstruction.
Stratifying on, and providing subgroup analyses for, smoking status.
Characterising patients in terms of type and amount of airway inflammation by induced sputum (genotype, smoking status, etc.) and perform randomisation stratified on these characteristics.
Providing subgroup analyses for the effect size at different points in time during the trial.
Relaxing eligibility criteria to allow the inclusion of patients in whom the diagnosis of asthma has been confirmed in the past (either by provocation or documented reversibility to bronchodilator or corticosteroids), even if the patients do not exhibit reversibility to bronchodilator at enrolment.
Monitoring, reporting and providing subgroup analyses on compliance.
Stratifying, providing subgroup analyses using different dose of ICS to which LABA is added.
Examining inflammatory markers.
Monitoring and reporting side effects that may be associated with the long-term use of inhaled corticosteroids (osteopenia, adrenal suppression and, in children, growth).
Future trials should aim for the following design characteristics.
Double-blinding, adequate randomisation and complete reporting of withdrawals and drop-outs with intention-to-treat analysis.
Intervention period of 52 weeks or more to assess the impact on patients with exacerbations requiring oral corticosteroids properly.
Clear reporting of the percentage and reasons for non-eligibility of approached patients and of those enrolled in the run-in period.
Complete reporting of continuous (denominators, mean change and mean standard deviation of change) and dichotomous (denominators and rate) data.
Outcomes of particular importance to include are as follows.
Proportion of patients with one or more exacerbations requiring systemic corticosteroids.
Change in symptoms, symptom-free days and nights, pulmonary function tests, use of rescue ß2 agonists, quality of life.
Change in inflammatory markers.
Safety, particularly regarding long-term side effects of inhaled corticosteroids (growth, osteopenia, adrenal suppression) and/or long-acting ß2 agonists (severe adverse effects and mortality).
PLAIN LANGUAGE SUMMARY.
The addition of long-acting beta2-agonists to inhaled steroids compared to higher doses of inhaled steroids alone as maintenance treatment for chronic asthma
When asthma is inadequately controlled with inhaled corticosteroids, either adding medication such as long-acting beta2-agonists (LABAs) or increasing the dose of inhaled corticosteroids is recommended. The purpose of this review was to establish the benefits and safety of adding long-acting beta2-agonists or increasing the dose of inhaled corticosteroids in patients with asthma that is inadequately controlled on their current dose of inhaled corticosteroids. This review analysed data from identified randomised controlled trials comparing the addition of long-acting beta2-agonists to inhaled corticosteroids versus increasing to a higher dose of inhaled corticosteroids in asthmatic children and adults.
Based on the identified trials:
There is a modest advantage in adding long-acting beta2-agonists to inhaled corticosteroids, compared with increasing the dose of inhaled corticosteroids, in preventing exacerbations but many patients (more than 70) need to be treated for one to have an exacerbation prevented. The results apply particularly to adults, as no group differences were observed in children. Reduction in symptoms and use of rescue beta2-agonists as well as improvement in lung function tests also slightly favour the combination of long-acting beta2-agonists to inhaled corticosteroids over a higher corticosteroid dose.
Apart from an increased rate of tremor and less oral thrush, there is no apparent difference in the risk of side effects or rates of withdrawal from treatment because of side effects between the treatment options, but the long-term side effects of inhaled corticosteroids were seldom monitored. However, the trends towards an increased risk of moderate and severe exacerbations in children receiving combination therapy raises concern about this therapy, particularly in view of the modest improvement shown.
ACKNOWLEDGEMENTS
We thank the Cochrane Airways Review Group, namely Elizabeth Arnold, Susan Hansen, Stephen Milan, Karen Blackhall, Veronica Stewart and Bettina Reuben for the literature search and ongoing support, and Christopher Cates, Peter Gibson and Paul Jones for their constructive comments. We are indebted to the following study investigators who provided further information and/or data from their studies: Janet Holbrook (LOCCS), Boorsma, Christine Sorkness and Dave Mauger, JP Kemp, RA Pauwels, Richards, G Russell and AAPH Verberne. We also gratefully received additional information and data from the following study sponsors: Glaxo-SmithKline (Richard Follows, Shailesh Patel and Rob Pearson) and AstraZeneca (Steve Edwards, Nils Grundstrom and Roger Metcalf).
SOURCES OF SUPPORT
Internal sources
Canadian Cochrane Network - McGill University, Canada.
External sources
Francine Ducharme was supported by a senior clinical scientist award from the Fonds de la Santé du Québec, Canada.
CHARACTERISTICS OF STUDIES
Characteristics of included studies [ordered by study ID]
| Methods | Parallel-group, multicentre study (50 centres). Three groups of which 2 considered here, namely: FP 250 bid; FP 100 + SL 50 bid Jadad quality score = 5 |
|
| Participants | Symptomatic asthmatic children >= 12 years and adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 454 (FP100 + Salm50: 231; FP250: 223) WITHDRAWALS: FP100 + Salm50: 16; FP250: 13 AGE: mean (range): 41 (12 to 79) GENDER (% male): 40 SEVERITY: Moderate BASELINE % PREDICTED FEV1: 63.1 BASELINE DOSE OF ICS (start of run-in): Not reported ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: Non-smokers; >= 12 years of age who had asthma defined in accordance with American Thoracic Society criteria; low dose of beclomethasone dipropionate or fluticasone for at least 3 months preceding the study; the daily dosing schedule for the inhaled corticosteroid had to be constant for the 14-day run-in period prior to the study; FEV1 of 40% to 85% of predicted normal values for age, gender and height; reversibility of airway obstruction was demonstrated by >= 15% increase in FEV1 within 30 minutes after 2 puffs of albuterol EXCLUSION CRITERIA: Pregnant/lactating mothers; use of methotrexate, gold, cyclosporine or azathioprine for control of asthma within 30 days prior to study; use of inhaled cromolyn or inhaled nedocromil within weeks prior to the study; use of oral or injectable corticosteroids within 4 weeks prior to the study; significant concomitant illness or concurrent use of any other prescription or over-the-counter medication that might affect the course of asthma or interact with sympathomimetic amines CRITERIA FOR RANDOMISATION DURING RUN-IN: FEV1 between 40% to 65%, if FEV1 65.1% to 85% had to have asthma symptoms; demonstrate compliance and complete diary cards; not to have experienced clinical exacerbation during screening period |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES: Reported at 1, 2, 4, 6, 8 and 12 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: Usual ICS DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (FP 100 + Salm 50) fluticasone 100 mcg bid + salmeterol 50 mcg bid CONTROL GROUP: (FP 250) fluticasone 250 mcg bid DEVICE: MDI NUMBER OF DEVICES: 2 COMPLIANCE: Assessed CO-TREATMENT: prn SABA and theophylline as needed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1*; am PEF; pm PEF SYMPTOM SCORES: Symptom scores (score of 0 to 5) FUNCTIONAL STATUS: Rescue medication use; nocturnal awakenings; symptom-free days; physician global assessment INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Described WITHDRAWALS: Described Primary outcome measure* |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data obtained User-defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers |
| Allocation concealment? | Yes | Numbered coded inhalers supplied by pharmacy |
| Blinding? All outcomes |
Yes | Double-dummy design; use of identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | “Analyses were based on data from the intent-to-treat population, consisting of all patients exposed to the study drug.” |
| Free of selective reporting? | Yes | Data available for meta-analysis |
| Methods | Parallel-group, multicentre (37 centres in 6 countries) Jadad quality score = 5 |
|
| Participants | Patients with asthma >= 18 years % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 92 RANDOMISED: 344 (BUD 200 + Form 6: 168; FP250: 176) WITHDRAWALS: BUD 200 + Form 12: 3; FP250: 8 AGE: mean (range): 42 (17 to 75) GENDER (% male): BUD 200/Form 6: 42; FP250: 44 SEVERITY: Moderate BASELINE % PREDICTED FEV1(mean): 78 BASELINE DOSE OF ICS: Mean mcg/day BDP equivalent: 594 ASTHMA DURATION mean (range) years: 16.3 (0 to 66) ATOPY (%): Not reported SMOKERS (%): 6 ELIGIBILITY CRITERIA: >= 18 years of age with a diagnosis of persistent asthma (minimum duration 6 months) as defined by the Global Initiative for Asthma (GINA) guidelines; using any inhaled glucocorticoid at a constant dose of 200 to 1000 mcg/day for at least 30 days before study entry; FEV1 of 60% to 90% of predicted normal values; reversibility of airway obstruction was demonstrated by >= 12% increase in FEV1 within 30 minutes after bronchodilator EXCLUSION CRITERIA: Female patients of childbearing potential not using adequate contraception; use of oral, parenteral or rectal corticosteroids or respiratory tract infection within 30 days prior to the study; heavy smoking (>= 10 pack years) CRITERIA FOR RANDOMISATION DURING RUN-IN: Required to have diary data for at least 7 of the last 10 days of run-in period |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: Reported at 4, 8 and 12 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BUD 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (BUD 200 + Fom 6) budesonide 200 mcg bid + formoterol 6 mcg bid CONTROL GROUP: (FP 250) fluticasone 250 mcg bid DEVICE: Diskhaler NUMBER OF DEVICES: 1 COMPLIANCE: Assessed using diary cards CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF*; pm PEF SYMPTOM SCORES: Change in symptom score (score of 0 to 3) FUNCTIONAL STATUS: Rescue medication use; % nocturnal awakenings; % of symptom-free days; % asthma-control days INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Described WITHDRAWALS: Described Primary outcome measure* |
|
| Notes | Full-text publication Funded by Astra Zeneca Confirmation of methodology and data: Not obtained User-defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; other information not available |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Double-dummy; identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | Described as intention-to-treat analysis; explicit details of how missing data were handled not reported |
| Free of selective reporting? | Yes | Severe exacerbations (including OCS treated exacerbations) extracted as proxy for OCS-treated exacerbations (see Analysis 3.1) |
| Methods | Parallel-group, multicentre study (37 centres: 36 in USA, 1 in Puerto Rico) Jadad quality score = 4 |
|
| Participants | Persistent symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 484 (FP/SAL: 246; FP: 238) WITHDRAWALS: FP/SAL: 6; FP: 4 AGE: mean: 41 GENDER: (% male): 41 SEVERITY: Moderate BASELINE % PRED FEV1 (mean): 70 BASELINE DOSE OF ICS: FP500 ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: > 12 and < 80 years; diagnosis of persistent (non-seasonal) asthma for more than 6 months; treated with short-acting beta-agonists; FEV1 > 60 and < 80% predicted; reversibility to SABA of 15% OR PEF < 85% predicted; achievement of good asthma control in last 4 weeks of open label period; score of >= 2 on combined day and nighttime score on 4 of last 7 days of run-in period EXCLUSION CRITERIA: Treatment with corticosteroids (within 12 weeks) antileukotriene agents, sodium cromoglycate, long-acting beta-agonists, nedocromil sodium, ketotifen, methylxanthines, anti-cholinergic agents (within 4 weeks); participants with acute asthma exacerbation in 6 weeks prior to study; participants with respiratory tract infection within 4 weeks prior to study; significant smoking history |
|
| Interventions | LABA/ICS versus INCREASED dose of ICS OUTCOMES: TIMING 12 weeks RUN-IN: 2 weeks on SABA; −12 weeks open label with combination FP/SAL DOSE OF ICS DURING RUN-IN: 250 mcg bid INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone 100 mcg and salmeterol 50 mcg bid CONTROL GROUP: Fluticasone 250 mcg bid DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORES: Daytime symptoms; nighttime symptoms; % symptom-free days; % symptom-free nights FUNCTIONAL STATUS: Rescue medication use; exacerbations (moderate: OCS treatment; severe: hospitalisation) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text article (additional data from available from http://www.ctr.gsk.co.uk) Source of funding: GSK Confirmation of methodology and data: obtained User defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical devices |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The Intent-to-Treat (ITT) population (all subjects who were randomised to treatment and received ≥ 1 dose of double-blind study medication) were used for the safety and efficacy analyses.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from study sponsors |
| Methods | Parallel-group, multicentre study (76 centres) Jadad quality score = 4 |
|
| Participants | Patients with asthma 18 to 70 years % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 91 RANDOMISED: 365 (FP250/SM 50 bid: 179; FP500 bid: 186) WITHDRAWALS: FP250/SM 50 bid: 13; FP500 bid: 18 AGE mean: 49 GENDER (% male): 47 SEVERITY: Moderate BASELINE % PREDICTED FEV1 mean: 75 BASELINE DOSE OF ICS: Mean mcg/day BDP equivalent: 800 to 1000 of BDP or BUD ASTHMA DURATION (mean (range) years): Not reported ATOPY (%): Not reported SMOKERS: 0 ELIGIBILITY CRITERIA: 18 to 70 years of age with a diagnosis of persistent asthma (minimum duration 6 months) as defined by the German asthma guidelines; asthma of moderate severity (i.e., symptoms < 1/day but no more than 2/week during daytime, or symptoms >= 2/month but less than 1/week at night; FEV1 50% to 80% of predicted; reversibility of airway obstruction was demonstrated by >= 15% increase in FEV1 after 200 mcg salbutamol; non- or ex-smoker; asthma treated with 800 to 1000 mcg/day of BUD or BDP (or 500 FP) per day for at least 3 months prior to study EXCLUSION CRITERIA: Previous therapy with inhaled LABA, oral beta-agonists, oral or parental steroids in preceding 4 weeks; change in asthma medication, treatment with other study medication, respiratory tract infection or hospital stay due to respiratory problems in receding 4 weeks; inability to correctly administer study drugs, known allergy to components of study drugs; severe concomitant illness or other chronic respiratory diseases (such as cystic fibrosis or interstitial fibrosis); in women, inadequate contraception, pregnancy or lactation CRITERIA FOR RANDOMISATION DURING RUN-IN: At least one of the following criteria: use of rescue medication >= 7 of 14 days; total asthma symptoms score >= 10 points (sums of scores from 14 days and nights); excluded if incomplete diary or considered not reliable or respiratory tract infection during run-in |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: Reported at 4, 8 and 12 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BUD 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (FLUT 200 + SALM50) fluticasone 200 mcg bid + salmeterol 50 mcg bid (1 inhaler) CONTROL GROUP: (FP 500) fluticasone 500 mcg bid DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: Assessed using diary cards CO-TREATMENT: Theophylline, cholinergic drugs or leukotrienes if dose was not changed during the trial. Prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF*; pm PEF SYMPTOM SCORES: Change in daytime and nighttime symptom score (score of 0 to 4) FUNCTIONAL STATUS: Rescue medication use; % of symptom-free days INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Described WITHDRAWALS: Described Primary outcome measure* |
|
| Notes | Full-text publication Funded by Glaxo Welcome Germany Confirmation of methodology and data: Not obtained User-defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices |
| Incomplete outcome data addressed? All outcomes |
No | “The full analysis set (FAS) consisted of those patients who inhaled at least one dose of study medication and had no critical protocol violation (e.g. a missing diary from the screening period). The last observation carried forward (LOCF) principle was applied to the efficacy variables.” |
| Free of selective reporting? | Unclear | Unclear whether exacerbations were recorded in the study |
| Methods | Parallel-group, multicentre study (11 centres) Jadad quality score = 2 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 84 RANDOMISED: 134 (BDP250 + Form 12: 69; BDP500: 65) WITHDRAWALS: BDP250 + Form 12: 4; BDP500: 6 AGE mean: 43 Gender (% male): 35 SEVERITY: Moderate BASELINE % PREDICTED FEV1: 60% to 79% (estimated) BASELINE DOSE OF ICS: BDP 500 mcg/day ASTHMA DURATION: Not described ATOPY (%): Not described SMOKING STATUS: Not described ELIGIBILITY CRITERIA: >= 18 years old; use of inhaled BDP aerosol for at least 1 month prior to enrolment, at a constant daily dose of 500 mg EXCLUSION CRITERIA: Other clinically significant diseases; pregnant or lactating women; patients on B-blocker therapy or hypersensitivity of sympathomimetic amines; received a short course of oral corticosteroid in the 6 weeks prior to enrolment; more then 3 oral corticosteroid short courses during the year prior to enrolment CRITERIA FOR RANDOMISATION DURING RUN-IN: A symptom score of 2 or greater on at least 4 of the 7 days during the second week of the run-in; FEV1 before administration of an inhaler agonist 40% to 85% of the predicted value; a reversibility test with 200 mg salbutamol demonstrating an increase in FEV1 of at least 15% from baseline value |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: Reported at 4, 8 and 12 weeks RUN-IN PERIOD: 2 weeks to document symptoms and beta2 use DOSE OF ICS DURING RUN-IN: BDP 500 mcg/day DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (BDP500 + Form 12) beclomethasone 250 mcg bid + formoterol fumarate 12 mcg bid CONTROL GROUP: (BDP1000) beclomethasone 500 mcg bid DEVICE: MDI NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA (used with a spacer device) |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORE: Morning and evening score (score of 0 to 4) FUNCTIONAL STATUS: Mean rescue B2-agonist (inhalations per day or night); exacerbations requiring systemic steroids INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Described WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data: Not obtained User-defined number: 500 (1000-500) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
No | Open label |
| Incomplete outcome data addressed? All outcomes |
No | Completers analysed |
| Free of selective reporting? | Yes | OCS-treated exacerbations available |
| Methods | Parallel-group, multicentre study (90 centres in US). Study had 2 treatment periods: fixed dosing during period 1 (up to week 12), and variable dosing in period 2 (weeks 12 to 24) Jadad quality score = 3 |
|
| Participants | Stable asthmatic patients 12 years and over % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PATIENTS RANDOMISED: 558/1596 = 35% RANDOMISED: 558 (Salmeterol 50 bid + ICS: 281; ICS + placebo: 277) WITHDRAWALS: S + ICS: 35; ICS: 42 AGE mean (range): 39 (12 to 77) GENDER (% male): 42 BASELINE % PREDICTED FEV1 mean: 80.5 BASELINE DOSE OF ICS (mean): Not reported by treatment groups BDP 400 to 800 mcgs/day; triamcinolone acetate 1200 to 1600 mcgs/day; flunisolide 1000 to 1500 mcgs/day; FP 440 to 660 mcgs/day ASTHMA DURATION: Not reported ATOPY (%): Not described SMOKING STATUS: Not reported ELIGIBILITY CRITERIA: Asthma for at least 6 months and treated with medium dose ICS for at least 30 days before screening; baseline FEV1 of 65% to 95% normal; >= 12% improvement from baseline in lung function following inhaled bronchodilator; best FEV1 within +/− 15% of the best predose FEV1 obtained at screening; no more than 1 nighttime awakening requiring albuterol and fewer than 18 puffs albuterol during the previous week EXCLUSION CRITERIA: Pregnancy and/or lactating; life-threatening asthma; asthma hospitalisation within 3 months of screening; change in asthma regimen 30 days before screening; significant concurrent diseases including recent URTI; systemic corticosteroids in 30 days before screening CRITERIA TO ENTER RUN-IN PERIOD 2: 20% decrease from the screening visit pre-dose FEV1; >= 20% decrease from the mean morning baseline PEF on any one of the 7 days immediately preceding the visit; total symptom score of >= 8 during any week before run-in visit; 2 or more nighttime awakenings due to asthma requiring treatment with albuterol during any week period before run-in visit CRITERIA FOR RANDOMISATION FOLLOWING RUN-IN PERIODS: Patients who regained asthma control following step-up treatment during run-in period 2; best FEV1 >= 65% of predicted and >= 15% of the best predose FEV1 obtained at visit IA |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: Reported at 1, 4, 8 and 12 and 24 weeks (only those at 12 weeks used) DOSEOPTIMISATION PERIOD: 10 weeks; patients commenced on FP 250 mcg bid or equivalent for 2 weeks. Stable patients had their dose dropped to FP 100 bid. Patients who became unstable on this were eligible to continue. FP 250 bid was commenced and patients stable on this were eligible to continue INTERVENTION PERIOD: 12 to 24 weeks (data at 12 weeks used) TEST GROUP: (FP 100 bid + S 50 bid) salmeterol 50 mcg bid + fluticasone propionate 100 bid CONTROL GROUP: Fluticasone propionate 250 bid DEVICE: Diskhaler NUMBER OF DEVICES: 1 COMPLIANCE: Monitored during study CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF SYMPTOMSCORE: Mean change in daily symptom score (score of 0 to 5 Likert scale) FUNCTIONAL STATUS: Exacerbations (defined as any worsening of asthma that required asthma medication beyond blinded study drugs or albuterol); rescue medication use; nocturnal awakening; % rescue-free days; % symptom-free days INFLAMMATORY MARKERS: Not assessed ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure: proportion of patients who remained in study after 12 weeks and who did not withdraw due to lack of efficacy |
|
| Notes | Full-text publication. Additional data available from GSK trials register Funded by Glaxo Wellcome Confirmation of methodology and data obtained User-defined number: 600 (1000-400) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices |
| Incomplete outcome data addressed? All outcomes |
No | Last observation carried forward: “All analyses for efficacy and safety were conducted through use of the intent-to-treat population (all randomised patients). All data from patients who were withdrawn from the study early were included in the analyses, data available up to the time of study discontinuation being used. No interpolation was used for missing data.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from GSK |
| Methods | Parallel-group, multicentre study (36 research centres) Jadad quality score = 5 Confirmation of methodology obtained |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 85 RANDOMISED: 437 (FP100 + Salm50: 221; FP250: 216) WITHDRAWALS: FP100 + Salm50: 19; F250: 30 AGE mean: 36.9 years GENDER (% male): 39 SEVERITY: Moderate BASELINE % PREDICTED FEV1: 61 BASELINE DOSE OF ICS: Not reported ASTHMA DURATION: < 10 years: 23%; >= 10 years: 87% ATOPY(%): Not reported SMOKERS: None ELIGIBILITY CRITERIA: >= 12 years old; asthma for at least 6 months; increase in FEV1 by 15% or greater after the inhalation of 200 mg of albuterol; FEV1 of 40% to 80% of predicted value; used short-acting bronchodilator on a regular basis for 3 months EXCLUSION CRITERIA: Current tobacco use; hospital admissions for asthma in the past 30 days; upper or lower respiratory infection within 30 days; positive pregnancy test or lactating; excluded during screening if they had an asthma exacerbation CRITERIA FOR RANDOMISATION FOLLOWING RUN-IN: FEV1 40% to 65% of predicted normal; at least one of the following over the 7 days prior to randomisation: an average of >= 4 puffs of albuterol per day; 2 or more days when evening PEF variation was >= 20%; 2 or more nights with awakenings due to asthma; 3 or more days with scores of >= 2 for any of the daytime symptoms of wheeze, chest tightness, shortness of breath or cough |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: Reported at 2,4,8,12,16,20 and 24 weeks RUN-IN: 2 to 4 weeks DOSE OF ICS DURING RUN-IN: FP 100 bid INTERVENTION PERIOD: 24 weeks TEST GROUP: (FP100 + Sal50) fluticasone propionate 100 mg bid + salmeterol 50 mg bid CONTROL GROUP: (FP250) fluticasone propionate 250 mg bid DEVICE: Metered-dose inhalers NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: Albuterol on an as-needed basis |
|
| Outcomes | PULMONARY FUNCTION TEST: Change in morning* and evening PEF; change in FEV1(L) SYMPTOM SCORES: Change in daytime symptom scores (scores of 0 to 5) FUNCTIONAL STATUS: Change in mean rescue B2-agonist use ( number of puffs); change in number of nighttime awakenings; change in % nights with no awakenings; exacerbations requiring systemic steroids INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Described Primary outcome measure* |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data obtained User defined number: 600 (1000-400) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Random computer-generated numbers |
| Allocation concealment? | Yes | Letter coded inhalers supplied by pharmacy |
| Blinding? All outcomes |
Yes | Double-dummy design; identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | “All statistical analyses were performed on the intent-to-treat (ITT) population consisting of all subjects who were randomised to blinded study drug.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Parallel-group, multicentre 4-arm trial, 2 of which are considered in this review | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: 44 % RUN-IN PARTICIPANTS RANDOMISED: 63 RANDOMISED: 306 (BUD/F: 153; BUD 153) WITHDRAWALS: Not stated AGE mean (range) or mean (SD): 35 (15) SEVERITY: Not stated BASELINE % PREDICTED FEV1: 76% BASELINE DOSE OF ICS: 375 mcg ASTHMA DURATION: Not stated ATOPY (%): Not stated ELIGIBILITY CRITERIA: > 12 years; documented clinical diagnosis of asthma for 6 months prior to screening; stable; maintenance asthma treatment with inhaled corticosteroids (ICS) for at least 4 weeks; FEV1 60% to 90% predicted EXCLUSION CRITERIA: Not stated ELIGIBILITY CRITERIA DURING RUN-IN: Not stated |
|
| Interventions | LABA and ICS versus HIGHER dose ICS OUTCOMES 12 weeks RUN-IN PERIOD: 4 to 5 weeks (combination therapy) INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination budesonide and formoterol 200/12 mcg qd CONTROL GROUP: Budesonide 400 mcg qd NUMBER OF DEVICES: 1 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF SYMPTOM SCORES: Total symptoms FUNCTIONAL STATUS: Rescue medication use INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Stated for adverse events only |
|
| Notes | Trial report available as download from AZ clinical trials website Funded by AZ Confirmation of methodology and data extraction not obtained User defined: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; no other information presented |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | “To maintain blinding with the twice-daily dosing regimen, all subjects randomised to receive once-daily dosing were to take the active treatment in the evening and a matched placebo device (Batch numbers P6492 and P6856) in the morning.” |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The efficacy analysis set (EAS), defined as all randomised subjects who took at least 1 dose of double-blind treatment and for whom the primary efficacy endpoint could be calculated, was used in the primary analysis of efficacy. Sensitivity analyses were performed using the per protocol (PP) analysis set, which excluded subjects with major violations of inclusion or exclusion criteria.” |
| Free of selective reporting? | Unclear | Not clear whether the study collected information on exacerbations treated with OCS |
| Methods | Parallel-group, single centre study Jadad quality score = 4 Confirmation of methodology not obtained |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 100 RANDOMISED: 39 (Salm50/FP: 19; HFA BDP: 20) WITHDRAWALS: 0 AGE mean: 44 GENDER (% male): 51 SEVERITY: Moderate-severe BASELINE FEV1% predicted: 69% BASELINE DOSE OF ICS: >= 800 mcg CFC-BDP or equivalent or >= 200 mcg CFC-BDP as second-line therapy ASTHMA DURATION: Not reported ATOPY (%): Not reported SMOKING STATUS: Not reported ELIGIBILITY CRITERIA: FEV1 55% to 85% predicted; >= 15% improvement from baseline in PEF or FEV1 following an inhaled beta2-agonist; PD 20 methacholine < 200 mcg; use of > 2 puffs of rescue medication/ day and symptoms at least 5 days per week; at least 80% compliance with dose prescribed as per dose counters EXCLUSION CRITERIA: Patients receiving oral corticosteroids; asthma exacerbation in the 3 months before study entry CRITERIA FOR RANDOMISATION FOLLOWING RUN-IN: Diary card evidence over the previous month of using at lease 2 puffs per day of rescue medication and having symptoms at least 5 days per week; patients who did not meet these criteria had their treatment tapered in a stepwise fashion at 1 to 2-week intervals until they were taking less than 200 mcg CFC-BDP or equivalent at which point they were withdrawn from the study or their beta-2 agonist use met the above criteria |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: Reported 1, 2 and 4 weeks RUN-IN PERIOD: 4 weeks DOSE OF ICS DURING RUN-IN: BDP 2000 mcg/day TREATMENT DURATION: 4 weeks DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 4 weeks TEST GROUP: (FP 100 mg + SAL50 mg): Fluticasone dipropionate 100 mcg bid + salmeterol 50 mcg bid CONTROLGROUP: (HFA BDP 200 mcg bid) beclomethasone dipropionate 200 mcg bid DEVICE: FP + S via diskhaler; HFA-BDP via metered dose inhaler NUMBER OF DEVICES: 2 COMPLIANCE: Dose counters used to check compliance CO-TREATMENT: Albuterol DPI via clickhaler |
|
| Outcomes | PULMONARY FUNCTION TEST: Diurnal variation in PEF (%); FEV1 % predicted; PD 20 SYMPTOM SCORES: Not reported FUNCTIONAL STATUS: AQLQ 32 questions with 7-point scale; rescue B2-agonist use INFLAMMATORY MARKERS: Serum ECP; nitric oxide OTHER: Plasma cortisol ADVERSE EFFECTS: Reported WITHDRAWALS: Described Primary outcome: Not reported |
|
| Notes | Full-text publication Funded by anonymous research grant and received HFA-BDP and placebo free from 3M healthcare Confirmation of methodology and data not obtained User defined number: 400 (800-400) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised, no other information available |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Double-dummy study |
| Incomplete outcome data addressed? All outcomes |
Unclear | Described as intention-to-treat |
| Free of selective reporting? | Unclear | Not clear whether the study collected information on exacerbations treated with OCS |
| Methods | Cross-over, single centre study in UK | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: Not specified % RUN-IN PARTICIPANTS RANDOMISED: 74 RANDOMISED: 49 WITHDRAWALS: 10 GENDER: (% male): 51 MEAN AGE: 42 SEVERITY: Not stated BASELINE FEV1 % PREDICTED: 74.8 BASELINE DOSE OF ICS: </−400 BDP ASTHMA DURATION: Not available ATOPIC: 93% SMOKING STATUS: Non or ex-smokers eligible INCLUSION CRITERIA: 18 to 75 years, diagnosed with asthma; receiving treatment with 400 mcg/day beclomethasone dipropionate; one or more of 1) > 15% increase in FEV1 post-SABA; 2) > 20% within-day variability in PEF assessed twice daily over a 2-week period; 3) provocative concentration of methacholine causing a 20% fall in FEV1 (PC20) < 8mg/mL-1; following run-in on 200 mcg day BUD, participants were eligible if they had recorded day or nighttime asthma symptoms on their diary cards on at least 4 days in the third or fourth baseline week EXCLUSION: Current smokers or smoking history of > 10 pack-years, significant comorbidity, treated with oral corticosteroids, long-acting b2-agonists, leukotriene antagonists or theophylline; asthma exacerbation or lower respiratory tract infection within the 4 weeks prior to trial entry |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: 4 weeks RUN-IN PERIOD: 4 weeks DOSE OF ICS DURING RUN-IN: BUD 100 mcg bid TREATMENT DURATION: 4 weeks DOSE OPTIMISATION PERIOD: None TEST GROUP: Budesonide 100 mg bid + formoterol 12 mg bid CONTROL GROUP: Budesonide 400 mg bid DEVICE: Turbohaler NUMBER OF DEVICES: 2 (double-dummy) COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TESTS: am PEF; FEV1 SYMPTOM SCORES: *VAS; daytime symptoms; nocturnal symptoms FUNCTIONAL STATUS Quality of life (AQLQ); exacerbations (deterioration in PEF or requirement for OCS. Patients who experienced 2 or more exacerbations were withdrawn from the study) INFLAMMATORY MARKERS: *Sputum eosinophils; exhaled nitric oxide; *PC20 ADVERSE EFFECTS: Not reported WITHDRAWALS: Stated (not by treatment group) Primary outcome measure* |
|
| Notes | Full-text article Funding source: Not disclosed Methodology and data: TJL emailed 17 April 2008. Response from RG with details of randomisation and data User defined: 800 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “I believe that this was generated using a computer statistical package generating a random sequence. I don’t know the package that was used and unfortunately the individual has left our organisation but had extensive clinical trials expertise.” |
| Allocation concealment? | Yes | “…this was indeed generated by a third party, namely the pharmacist responsible for dispensing the double blind medication (…) None of the study investigators were aware of the randomisation schedule until the last patient had completed the cross-over study” |
| Blinding? All outcomes |
Yes | Double-dummy |
| Incomplete outcome data addressed? All outcomes |
No | Completers used for analysis |
| Free of selective reporting? | Yes | OCS-treated exacerbations reported. Data could not be extracted as only data on events and not number of participants were made available |
| Methods | Parallel-group, multicentre study Jadad quality score = 5 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 426 (Salm50/BDP: 220; BDP: 206) WITHDRAWALS: Salm50/BDP: 71; BDP: 65 AGE mean: 48 years GENDER (% male): 44 SEVERITY: Moderate BASELINE FEV1: 2.13 Litres/sec Baseline % predicted PEF: 74 BASELINE DOSE OF ICS: Not reported ASTHMA DURATION: 11 years ATOPY (%): Information not available SMOKING STATUS: Current/previous smokers: 50% ELIGIBILITY CRITERIA: FEV1 >= 50% predicted; >= 15% improvement from baseline in PEF or FEV1 following an inhaled beta2-agonist; no courses of oral steroids during the previous 6 weeks or <= 4 short courses during the past year EXCLUSION CRITERIA: Patients receiving regular oral corticosteroids or who had received short course of oral corticosteroids in the 6 weeks prior to start of study or who had received 4 or more short courses in the last year. Patients who had received newly prescribed asthma therapy or who had changed asthma therapy in the 6 weeks prior to entering the study. Patients with FEV1 < 50% or predicted at the start of baseline. Patients who had a medical or physiological condition which in the investigator’s opinion should preclude them from the study, or one or more of the concurrent medical conditions: severe cardiac disease, clinically significant hepatic or renal dysfunction, thyrotoxicosis, uncontrolled diabetes mellitus, history of active neoplastic disease, tuberculosis, acute respiratory infection which required prescribed therapy 2 weeks prior to study, patients receiving beta-blockers, patients currently receiving other long-acting B2-adrenoreceptor agonists, female patients who were pregnant or lactating or were not taking adequate contraceptive precautions, patients whose history over the previous year was not documented, patients who were receiving or had received research medication in the previous month, patients previously enrolled in this study, patients with evidence of alcohol abuse, known hypersensitivity to salbutamol, salmeterol or beclomethasone dipropionate CRITERIA FOR RANDOMISATION DURING RUN-IN: Period variation in PEF over 1 week of >= 15% (highest evening PEF minus lowest morning PEF as a percentage of highest value); symptoms on >= 4 of 7 days during the second baseline week |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: 1, 3, 6 months RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BDP 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 6 months TEST GROUP: Beclomethasone (MDI) 200 mcg bid + salmeterol (Diskhaler) 50 mcg bid CONTROL GROUP: Beclomethasone (MDI) 500 mcg bid + placebo DEVICE: Diskhaler and MDI NUMBER OF DEVICES: 2 COMPLIANCE: Evaluated CO-TREATMENT: prn SABA. Other asthma drugs (xanthines) if already started prior to study |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; pm PEF SYMPTOM SCORES: Not given FUNCTIONAL STATUS: Nighttime disturbance (% patients with disturbance every night, >= 50% nights , < 50% nights and no night disturbance); daytime symptoms (% patients with symptoms every day, >= 50% of days, < 50% days, and no symptoms); rescue medication use; exacerbations mild (increase in relief medication); moderate (requiring a short course in oral corticosteroids); or severe (requiring hospital admission) INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text publication Supported by Allen & Hanburys Ltd, Uxbridge, Glaxo Pharmaceuticals Ltd, Uxbridge and Access Ltd, London (data and statistical advice) Confirmation of methodology and data extraction obtained User defined number: 600 (1000-400) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers |
| Allocation concealment? | Yes | Numbered coded medication allocated on sequential basis |
| Blinding? All outcomes |
Yes | Use of identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | “All analyses were performed on an intention- to-treat (ITT) basis, i.e. all subjects randomised and who had verifiable data.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Cross-over study, single treatment centre Jadad quality score:4 |
|
| Participants | Asthmatic children % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 27 WITHDRAWALS: 2 MEAN AGE (RANGE): 9.6 (6.1 to 13.5) GENDER (% male): 52 SEVERITY: Mild to moderate BASELINE FEV1 L (range): Not reported BASELINE PEF L/min (range): 280 l/min BASELINE DOSE OF ICS Mean: BUD 200 bid or equivalent ASTHMA DURATION (range in years): 4.5 (1.4 to 9.5) ATOPY (%): Not reported ELIGIBILITY CRITERIA: Not described EXCLUSION CRITERIA: Not described |
|
| Interventions | LABA + ICS versus INCREASED DOSE ICS OUTCOMES: Reported weekly RUN-IN: None DOSE OF ICS DURING RUN-IN: N/A INTERVENTION PERIOD: 12 weeks TEST GROUP: (Form + ICS) formoterol 12 mcg bid + budesonide 100 bid CONTROL GROUP: Placebo + budesonide 200 bid DEVICE: Turbuhaler (ICS); Aerolizer (formoterol) NUMBER OF DEVICES: 2 COMPLIANCE: Turbuhalers weighed and number of formoterol capsules counted CO-TREATMENT: Terbutaline via turbuhaler but no other co-treatments allowed |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF SYMPTOM SCORE: Daytime and nighttime score (score of 0 to 4) FUNCTIONAL STATUS: Exacerbations; rescue medication use; lower leg growth; serum and urinary markers of type I and III collagen turnover INFLAMMATORY MARKERS: Inflammatory markers in serum ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure: Not reported |
|
| Notes | Full-text publication Source of funding not stated Confirmation of methodology and data not obtained User-defined number: 200 (400-200) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “Treatment order was allocated by a computerised randomisation scheme prepared in balanced blocks.” |
| Allocation concealment? | Unclear | Information on concealment of allocation not provided |
| Blinding? All outcomes |
Yes | Double-blind; double-dummy |
| Incomplete outcome data addressed? All outcomes |
No | Completers used for analysis |
| Free of selective reporting? | Yes | Data on OCS-treated exacerbations available |
| Methods | Parallel-group, multicentre study in 100 hospitals and general practices in 6 countries (3 groups of which 2 are considered for this review | |
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 58%; of 859 recruited 357 not randomised (improved during run-in period) RANDOMISED: 502 (496 with completed case report forms included in intention-to-treat population). 336 for this review: FP/SAL: 171; FP: 165 WITHDRAWALS: FP/SAL: 27; FP: 22 Mean AGE years: 44.4 GENDER (% male): 45 SEVERITY: Moderate to severe BASELINE FEV1: 2.3 L % PREDICTED PEF am: 75 BASELINE DOSE OF ICS (median): 1000 mcg ASTHMA DURATION (range in years): 0.2 to 68 ATOPY (%): Information not available SMOKING STATUS: Not reported ELIGIBILITY CRITERIA: Aged 15 to 75; symptomatic on BDP 500 to 800 mcg bid or equivalent via MDI with good technique; 2 documented exacerbations needing hospitalisation or change in treatment with one occurring in last 6 months; PEF less than 85% of post-bronchodilator PEF at first clinic visit INCLUSION CRITERIA FOR RANDOMISATION DURING RUN-IN: Period variation in PEF over 10 days of >= 15% (highest evening PEF minus lowest morning PEF as a percentage of highest value); PEF not exceeding 90% of the post-bronchodilator PEF at first clinic visit; EXCLUSION CRITERIA: Patients receiving regular oral corticosteroid; patients who had serious uncontrolled systemic disease; participation was deemed unsuitable by their physician from the study |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: 6, 12 18 and 24 weeks RUN-IN PERIOD: 4 weeks DOSE OF ICS DURING RUN-IN: FP 250 mcg bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 6 months TEST GROUP: Combination fluticasone propionate/salmeterol 250/50 mcgs bid (in one device) INCREASED DOSE: FP 500 mcgs bid DEVICE: MDI NUMBER OF DEVICES: 1 COMPLIANCE: Not reported CO-TREATMENT: prn SABA. Other asthma drugs as needed except LABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF SYMPTOM SCORES: Nighttime scores 0 to 4; day-time score 0 to 5 FUNCTIONAL STATUS: % symptom-free days and nights; rescue medication use; exacerbations (defined as: mild (requiring increase in relief medication); moderate (requiring the use of additional corticosteroid); severe (requiring emergency hospital treatment) INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text publication Supported by Glaxo Wellcome Research and Development Confirmation of methodology and data extraction not obtained User defined number: 1000 (2000-1000) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | “intent-to-treat population (…) included all patients randomised to treatment with completed case report forms and verifiable data.” |
| Free of selective reporting? | Yes | Moderate exacerbations extracted as proxy for OCS-treated exacerbations (see Analysis 3.1) |
| Methods | Parallel-group, multicentre study (44 centres) Jadad quality score = 4 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 353 (FP/SAL: 180; BUD: 173) WITHDRAWALS: FP/SAL: 29; BUD: 30 Mean AGE years: 47 GENDER (% male): 50 SEVERITY: Moderate to severe BASELINE FEV1 % PRED: 70 BASELINE DOSE OF ICS median mcg/day prior to randomisation (n): FP500 (85*); BUD 800 (168); BDP 1000 (101*) *One patient was receiving both FP and BDP prior to study entry ASTHMA DURATION: < 1 year: 6%; 1 to 5 =18%; 5 to 10 = 16%; > 10: 60% ATOPY (%): Information unavailable SMOKING STATUS: Not reported ELIGIBILITY CRITERIA: > 12 years; documented reversible airways obstruction receiving ICS (BUD or BDP 800 to 1600 mcg/day or FP 400 to 600 mcg/day for > 4 weeks); baseline FEV1 or PEF 50% to 85% of normal; 15% increase in FEV1 or PEF 85% of maximum after bronchodilator; using rescue bronchodilator more than twice per day or total symptom score > 2 on > 4 of 7 days EXCLUSION CRITERIA: Acute exacerbation requiring hospitalisation, systemic corticosteroids, lower respiratory tract infection or change in asthma medication in 4 weeks prior to recruitment; LABA treatment or slow release bronchodilator in 2 weeks before recruitment; smoking history > 10 pack-years; pregnant or lactating females; regular oral corticosteroid treatment; serious uncontrolled systemic disease CRITERIA FOR RANDOMISATION DURING RUN-IN: No other additional criteria |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES: 4, 12 and 24 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: Usual ICS DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 24 weeks TEST GROUP: (FP/SAL) Combination fluticasone and salmeterol 250/50 mcg bid in single device, plus placebo turbuhaler INCREASED dose: BUD (DPI): Budesonide 800 mcg bid by turbuhaler + placebo Diskus DEVICE: Diskus (FP/SAL) and Turbuhaler (BUD) NUMBER OF DEVICES: 1 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORES: Not reported FUNCTIONAL STATUS: Symptom-free days and nights; % salbutamol-free days in each group; % symptom-free days in each group; exacerbations severe (requiring emergency hospital treatment); moderate (requiring additional inhaled corticosteroids); mild (requiring increase in use of relief medication which physician considered to be clinically relevant) INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text publication Supported by Glaxo Wellcome Research and Development Confirmation of methodology and data extraction not obtained User defined number: 600 (1600-1000) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Double-dummy design |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The Intent-to-Treat (ITT) population was defined as all patients who entered the study, were randomised, and received at least one dose of study treatment, was used for assessment of safety data as well as for all efficacy analyses.” |
| Free of selective reporting? | Yes | Moderate exacerbations extracted as proxy for OCS-treated exacerbations (see Analysis 3.1) |
| Methods | Parallel-group, multicentre study (39 centres in North America, Europe and South Africa) Jadad quality score = 5 |
|
| Participants | Symptomatic asthmatic patients % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 80 RANDOMISED: 349 (FP/SAL: 176; BUD: 173) WITHDRAWALS: FP/SAL: 23; BUD: 15 AGE mean (years): 36 GENDER (% male): 43 SEVERITY: moderate BASELINE % PREDICTED FEV1: 77 BASELINE DOSE OF ICS: mean in mcg (note: 19% of Sal FP group and 40% of BUD group on no corticosteroids before randomisation): FP 375; BUD 400; BDP 500 ASTHMA DURATION: Not reported ATOPY (%): Not reported SMOKING STATUS: Not reported ELIGIBILITY CRITERIA (including run-in criteria for randomisation): Mild to moderate asthma; symptomatic patients determined either by use of rescue salbutamol (on more than 2 occasions per 24 hours) or symptoms (total daytime and nighttime diary card symptom score of >= 2) on at least 4 of the last 7 days of the run-in period EXCLUSION CRITERIA: If patients had changed their regular asthma medication or received any long-acting or slow-release bronchodilators within the previous 2 weeks, had had a lower respiratory tract infection within the previous 4 weeks, or were smokers with a history of 10 pack years or more; if in the previous 4 weeks patients had had an asthma exacerbation requiring hospitalisation and/or treatment with oral, parenteral or depot corticosteroids; patients with serious uncontrolled diseases likely to interfere with the study or who showed evidence of alcohol or drug abuse; pregnant or lactating females, or those likely to become pregnant |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES: Reported at 12 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: Usual ICS DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone/salmeterol 100/50 mcg bid CONTROL GROUP: Budesonide 400 mcg bid DEVICE: FP/SAL: Diskus, BUD: Turbuhaler NUMBER OF DEVICES: 1 COMPLIANCE: Not reported CO-TREATMENT: prn SABA (use of stable asthma medications permitted) |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; diurnal variation in PEF post-treatment in each group SYMPTOM SCORES: % days and nights when symptom score < 2 (daytime 0 to 5; nighttime 0 to 4) FUNCTIONAL STATUS: Rescue medication use; symptom-free days/nights INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text publication Funded by GlaxoSmithKline Confirmation of methodology and data extraction: Not obtained User defined number: 400 (800-400) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Use of identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The Intent-to-Treat (ITT) population was defined as all patients who entered the study, were randomised, and received at least one dose of study treatment: it was used for assessment of safety data as well as for all efficacy analyses.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from study sponsor |
| Methods | Parallel-group study. Other details not available. Jadad quality score = 2 |
|
| Participants | Unclear severity % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 115 (FP/SAL: 59; FP: 56) WITHDRAWALS: Not stated AGE mean: Not reported GENDER (% male): Not reported SEVERITY: Not reported BASELINE % PREDICTED FEV1 (mean): Not reported BASELINE DOSE OF ICS: Not reported ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: >= 18 years of age EXCLUSION CRITERIA: Not stated |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOME TIMING: 12 weeks RUN-IN: 4 weeks DOSE OF ICS DURING RUN-IN: Not stated INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Fluticasone 200 mcg bid DEVICE: Rotahaler NUMBER OF DEVICES: 1 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; FEV1 SYMPTOM SCORES: Daily symptom scores; nighttime symptom scores FUNCTIONAL STATUS: Rescue-free days INFLAMMATORY MARKERS: Not stated ADVERSE EFFECTS: Not stated WITHDRAWALS: Not stated Primary outcome measure* |
|
| Notes | Conference abstract publication Source of funding: Not stated Confirmation of methodology and data: Not obtained User defined number: 800 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; other information not available |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | Information not available |
| Free of selective reporting? | Unclear | Unclear whether exacerbations were recorded in the study |
| Methods | Parallel-group, multicentre study (34 centres) Jadad quality score: 5 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 483/639 = 76% RANDOMISED: 483 (BDP + Sal: 239; BDP: 244) WITHDRAWALS: BDP + Sal: 48; BDP: 49 AGE mean (years): 42 GENDER (% male): 39 SEVERITY: Moderate BASELINE % PREDICTED FEV1: 64.5 BASELINE DOSE OF ICS: at least 400 mcg BDP or 800 mcg triamcinolone acetonide ASTHMA DURATION: Not reported ATOPY(%): Not reported SMOKING STATUS: No smokers ELIGIBILITY CRITERIA: Non-smokers; >= 18 years and up; baseline FEV1 of 45% to 80% of predicted value; FEV1 of >= 12 % after inhalation of 2 puffs of albuterol; using inhaled corticosteroids regularly for at least 3 months prior to enrolment; 14 days prior to enrolment must have taken 400 mg of beclomethasone daily or 800 mg of triamcinolone EXCLUSION CRITERIA: Not described CRITERIA FOR RANDOMISATION DURING RUN-IN: Must have symptomatic asthma defined as: >= 3 nights with nighttime awakening; >= 3 days with daytime symptoms; >= 3 days with albuterol used as a rescue medication occurring during the 7 days prior to randomisation |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES: Reported at 4, 12 and 24 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BDP 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 24 weeks TEST GROUP: (BDP 200 + Salm50) beclomethasone 200 mcg + salmeterol 50 mcg bid CONTROL GROUP: (BDP 400) beclomethasone 400 mcg bid DEVICE: Inhalation aerosol NUMBER OF DEVICES: 2 COMPLIANCE: Recorded in diary cards CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF*; pm PEF SYMPTOM SCORES: Mean symptom score (score of 0 to 4) FUNCTIONAL STATUS: Rescue medication use; symptom-free days; nocturnal disturbance; severe exacerbation (requiring systemic steroids) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data: obtained User-defined number: 400 (800-400) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Use of identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | Analysis population described as all participants randomised to double-blind treatment |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis (from GSK; study data included non-OCS exacerbations) |
| Methods | Parallel-group, multicentre study (3 centres) Jadad quality score = 4 |
|
| Participants | Well-controlled asthmatic adults (acute ICS reduction): considered as SYMPTOMATIC % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 86 RANDOMISED: 60 BUD + F: 29; BUD: 31 WITHDRAWALS: Not described AGE mean years (range): 36 (19 to 69) GENDER (% male): 40 SEVERITY: Mild BASELINE % PREDICTED FEV1 mean: 79 BASELINE DOSE OF ICS (start of run-in) mean (range): 691 (50 to 1500) mcg ASTHMA DURATION: Not described ATOPY (%): Not described SMOKING STATUS: Not described ELIGIBILITY CRITERIA: Established diagnosis of asthma for 6 months; treated with inhaled corticosteroids (ICS) for at least 3 months; baseline FEV1 > 50% of predicted; >= 15% increase in FEV1 or >= 9% in % predicted FEV1 after 1 mg of inhaled terbutaline EXCLUSION CRITERIA: Treated daily with >= 2000 mg of beclomethasone, >= 1600 mg of budesonide via pressure metered dose inhaler, >= 800 mg of budesonide via Turbuhaler, >= 800 mg of fluticasone; 3 courses of oral steroids in < 6 months; hospital admission due to asthma < 6 months CRITERIA FOR RANDOMISATION DURING RUN-IN: Compliance between 75% and 125% of recommended doses stable asthma for the last 10 days of run-in period; unstable asthma defined as: diurnal variation in PEF exceeded 20% on 2 consecutive days; B2 agonist use exceeded 4 inhalations per day; awakenings due to asthma occurred on 2 consecutive nights; patient needed oral corticosteroids |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES reported at 6, 12, 24 and 52 weeks RUN-IN PERIOD: 4 weeks with budesonide 800 mcg bid to monitor compliance and document asthma stability DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 months TEST GROUP: (BUD200 + F) budesonide 100 mcg + formoterol 12 mcg bid CONTROL GROUP: (BUD800) budesonide 400 mcg + placebo bid DEVICE: Turbuhaler NUMBER OF DEVICES: 2 COMPLIANCE: Measured by means of hidden counter in inhaler CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; PEF SYMPTOM SCORES: Change in symptom score (score of 0 to 3) FUNCTIONAL STATUS: Rescue medication use; nocturnal awakenings in each group; severe exacerbation (requiring systemic steroids); episode-free days INFLAMMATORY MARKERS: sputum eosinophils*; sputum EG2 + cells; sputum eosinophil cationic protein; sputum differential cell count ADVERSE EFFECTS: Not described WITHDRAWALS: Not described Primary outcome measure* |
|
| Notes | Full-text publication Funded by Astra Draco Confirmation of methodology and data obtained User-defined number: 600 (800-200) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers |
| Allocation concealment? | Yes | Opaque consecutive numbered envelopes containing assignment |
| Blinding? All outcomes |
Yes | Identical placebo used |
| Incomplete outcome data addressed? All outcomes |
No | “The analysis is based on a “per protocol” approach. Data from patients violating the protocol were included up to the violation time.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Parallel-group, multicentre study (51 centres in 7 countries) Jadad quality score: 3 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 94 RANDOMISED: 467 (BDP + F: 230; BDP: 237) WITHDRAWALS: BDP + F: 15; BUD: 22 Mean AGE years (range): 41 (18 to 78) GENDER (% male): 43 SEVERITY: Mild to moderate BASELINE FEV1 % predicted (range): 81 (38 to 157) BASELINE DOSE OF ICS mean (range): 387 (200 to 500) ASTHMA DURATION (range in years): 0 to 53 years ATOPY (%): Information not available ELIGIBILITY CRITERIA: Aged >= 18; diagnosis of asthma minimum 6 months; FEV1 60% to 90% predicted normal; 12% reversibility post-bronchodilator; ICS at constant dose 200 to 500 mcgs /day for at least 1 month prior to study entry EXCLUSION CRITERIA: Patients receiving systemic corticosteroids within 30 days of study entry; respiratory infection within previous 4 weeks; known hypersensitivity to study medication or inhaled lactose; patients with severe cardiovascular disorders or other serious diseases; current or previous smokers with a history of smoking > or = 10 pack years; all female patients were required to be postmenopausal, sterile or using contraception CRITERIA FOR RANDOMISATION DURING RUN-IN: No other additional criteria |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES reported at 4, 8 and 12 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BDP 100 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination budesonide and formoterol 100/6 mcg bid in a single inhaler CONTROL GROUP: Budesonide 200 mcg bid DEVICE: Turbuhaler NUMBER OF DEVICES: 1 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; am PEF; pm PEF SYMPTOM SCORES: Score of 0 to 3 FUNCTIONAL STATUS: Rescue medication use; % symptom-free days; nighttime awakening; asthma control days; exacerbations (defined as requirement for OCS or fall in PEF of > 30%) INFLAMMATORY MARKERS: None ADVERSE EFFECTS: Reported WITHDRAWALS: Described Primary outcome measure: Not described |
|
| Notes | Full-text publication Funded by Astra Zeneca Confirmation of methodology and data: Not obtained User-defined number: 200 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; other information not available |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Identical inhaler devices |
| Incomplete outcome data addressed? All outcomes |
Unclear | “Efficacy analyses were carried out on all randomised patients (intention-to-treat approach).” |
| Free of selective reporting? | Yes | Severe exacerbations included OCS exacerbations; added as additional study to sensitivity analysis |
| Methods | Parallel-group study. Three treatment arms, 2 of which are considered for this review Jadad quality score = 5 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 70 RANDOMISED: 32 Sal + usual ICS: 16; FP + usual ICS: 16 WITHDRAWALS: Sal + usual ICS: 3; FP + usual ICS: 0 AGE mean years: 40 GENDER (% male): 66 SEVERITY: Mild to moderate BASELINE FEV1 % predicted median (range): 82 BASELINE DOSE OF ICS: Mean (range): 400 (200 to 500) ASTHMA DURATION (range in years): Not reported ATOPY (%): 83 ELIGIBILITY CRITERIA: Aged 20 to 70 years; diagnosis of asthma; FEV1 >= 60 % predicted normal; treated with ICS for minimum 12 months in dose up to 500 mcg / day of BDP or BUD EXCLUSION CRITERIA: Respiratory infection within previous 4 weeks; any change in asthma medication in previous 4 weeks; hospital admission with airway disease in previous 4 weeks CRITERIA FOR RANDOMISATION DURING RUN-IN: At least one of the following: symptom score >= 2 on 7 of last 14 days; prn SABA >= 7 of 14 last days variation > 15% in PEF over a 24 hour period on >= 7 of last 14 days with some degrees of symptoms and rescue medication use during that time |
|
| Interventions | LABA + ICS vs INCREASED dose ICS OUTCOMES: measured at 12 weeks RUN-IN PERIOD: 2 to 6 weeks DOSE OF ICS DURING RUN-IN: Same as baseline dose of ICS DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (Salm50 + ICS) Salmeterol 50 mg bid + usual ICS CONTROL GROUP: (FP100 + usual ICS) fluticasone 100 mcg bid + usual ICS (‘double dose’) DEVICE: Dry powder diskhaler NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; FEV1 SYMPTOM SCORES: score of 0 to 4 (mean/day) FUNCTIONAL STATUS: Rescue medication use; nocturnal awakenings; exacerbations requiring OCS OTHER: Methacholine challenge PD 20 methacholine before and after treatment INFLAMMATORY MARKERS: on BAL and bronchial biopsy; mast cells in BAL; eosinophils in BAL; lymphocytes in BAL; macrophages in BAL and bronchial biopsies ADVERSE EFFECTS: Not reported WITHDRAWALS: Reported PRIMARY OUTCOME: Not specified |
|
| Notes | Full-text publication Funded by Glaxo Wellcome, Alfred Foundation and the NH&MRC of Australia Confirmation of methodology and data obtained User-defined number: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated numbers in balanced blocks |
| Allocation concealment? | Yes | Opaque consecutive numbered envelopes containing assignment |
| Blinding? All outcomes |
Unclear | Identical inhaler devices |
| Incomplete outcome data addressed? All outcomes |
No | Completers analysed |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Parallel-group, multicentre 3-arm study conducted in USA | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: 60 % RUN-IN PARTICIPANTS RANDOMISED: 63 RANDOMISED: 334 (FP 169; FP/SAL:165) WITHDRAWALS: 29 (FP 13; FP/SAL 16) AGE mean (range) or mean (SD): 30 (14) SEVERITY: Mild BASELINE % PRED FEV1: 92 BASELINE DOSE OF ICS: 400 mcg BDP equivalent ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: physician-diagnosed asthma; > 6 years; FEV1 predicted 60% or more; > 12% reversibility to SABA or a pc20 of 8 mg per millilitre or less within previous 2 years EXCLUSION CRITERIA: hospitalisation, urgent medical care, oral corticosteroid use, or use of additional asthma medication during run-in; presence of temperature exceeding 38.0 °C, or 100.4 °F) within previous 24 hours ELIGIBILITY CRITERIA DURING RUN-IN: adequate adherence with diary card; FEV1 > 80% predicted; Asthma Control Questionnaire score < 1.5; < 16 puffs of a rescue beta-agonist per week during final 2 weeks of run-in |
|
| Interventions | LABA + ICS versus HIGHER dose ICS OUTCOMES: 16 weeks RUN-IN PERIOD: 4 to 6 weeks DOSE OPTIMISATION PERIOD: NA TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg (once daily, evening) CONTROL GROUP: Fluticasone 100 mcg bid NUMBER OF DEVICES: 1 (double-dummy design as combination given twice daily) COMPLIANCE: Assessed by counters on inhalers and counts of pills CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; FVC predicted; PEF predicted SYMPTOM SCORES: Daytime symptoms FUNCTIONAL STATUS: Treatment failure*; oral steroid use; quality of life (AQLQ); rescue medication use INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Stated |
|
| Notes | Full-text publication Funding source: GSK Confirmation of data and methodology: Not obtained. TJL contacted for separate OCS requirement between adults and children User defined: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | “The randomization schedule was a permuted block design stratified by clinic and pediatric status” |
| Allocation concealment? | Yes | Central randomisation |
| Blinding? All outcomes |
Yes | Treble dummy: “At randomization each participant was instructed to use two Diskus inhalers each day, one in the morning and the other in the evening. The inhalers either were two containing fluticasone for the fluticasone group, one containing fluticasone and salmeterol and one placebo inhaler for the fluticasone/salmeterol group, or two placebo inhalers for the montelukast group. Inhalers were labelled AM or PM and had yellow or blue dots, respectively, to ensure compliance to the protocol. Each participant also took a capsule (or chewable tablet for 5 mg dose) containing montelukast or placebo once a day in the evening.” |
| Incomplete outcome data addressed? All outcomes |
Unclear | “Analyses were performed on the basis of the intention-to-treat principle; all available data from all patients were included in all analyses.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Parallel-group, multicentre trial (16 centres) Jadad quality score: 4 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 203/274 (74%) RANDOMISED: 203 (BDP/F: 102; BDP: 101) WITHDRAWALS: BDP/F: 7; BDP: 12 AGE mean: 43.9 GENDER (% males): 44.6 SEVERITY: Moderate to severe BASELINE % PREDICTED FEV1 mean: 72 BASELINE DOSE OF ICS: Not reported ASTHMA DURATION mean: 27 years ATOPY (%): Not reported SMOKING STATUS: Current smokers: 8%; previous smokers: 40 ELIGIBILITY CRITERIA: Aged 18 years or more; moderate to severe asthma; FEV1 >= of predicted and increased by 15% or more within 30 minutes after beta2 agonists or historical evidence of reversibility; had to have received Rx with ICS (metered dose inhaler) at a constant daily dose of 1000 mcg beclomethasone dipropionate or 800 mcg budesonide for at least 1 month before screening EXCLUSION CRITERIA: Change in daily dose of ICS in the previous month; use of a LABA or having received a course of oral corticosteroid in the month before the screening; problems using the Aeroliser (R) despite proper instruction CRITERIA FOR RANDOMISATION DURING RUN-IN: Presence of at least 2 of the following on at least 2 of the last 7 days of the run-in period: waking at least once/night because of asthma; asthma interfering with daily activities on at least 1 day; at least 4 puffs of salbutamol rescue medication a day; diurnal variation in PEF of at least 15% |
|
| Interventions | LABA + ICS vs INCREASED dose ICS OUTCOMES: measured at 4, 8 and 12 weeks RUN-IN PERIOD: 2 to 4 weeks DOSE OF ICS DURING RUN-IN: 500 BDP bid DOSE OPTIMISATION PERIOD: Not reported INTERVENTION PERIOD: 12 weeks TEST GROUP: (BDP/F) beclomethasone 500 mcg bid and formoterol 12 mcg bid CONTROL GROUP: (BDP) beclomethasone 1000 mcg bid and placebo INHALER DEVICE: Formoterol: Aerolizer; BDP: dry powder inhaler NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; FEV1 SYMPTOM SCORES: Score of 0 to 4 (day and night ) FUNCTIONAL STATUS: Rescue medication use; exacerbations INFLAMMATORY MARKERS: None ADVERSE EFFECTS: Reported WITHDRAWALS: Described *Primary outcome measure |
|
| Notes | Full-text publication Funded by Novartis Pharmaceutical Australia Pty Ltd Confirmation of methodology and data: not obtained User-defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; no other information available |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Double-dummy design |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The analysis of efficacy was carried out in the intention-to-treat analysis and, in addition, a confirmatory analysis was carried out on the mean morning pre-medication PEF measured during the last 7 days of treatment in the patients who had completed the whole treatment period.” |
| Free of selective reporting? | Unclear | Moderate exacerbations included OCS exacerbations; added as additional study to sensitivity analysis (see Analysis 3.1) |
| Methods | Parallel-group, multicentre study (35 centres) Jadad quality score: 5 |
|
| Participants | Symptomatic asthmatic patients % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 514 (BDP + Sal: 260; BDP: 254) WITHDRAWAL: BDP + Sal: 50; BDP: 57 AGE: mean (range): 42 (18 to 82) GENDER (% males): 43 SEVERITY: Moderate BASELINE % PREDICTED FEV1 mean: 65 BASELINE DOSE OF ICS: BDP 400 mcg daily or triamcinolone 800 mcg daily at study entry ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: FEV1 of 45% to 80% of the predicted value based on Capro standards adjusted for race; increase in FEV1 of at least 12% following the inhalation of 200 mg of albuterol; symptomatic while taking 400 mg of inhaled beclomethasone dipropionate or 800 mg triamcinolone acetonide daily EXCLUSION CRITERIA: Pregnant females or those planning a pregnancy; concurrent use of any medication affecting the course of asthma; interacting with sympathomimetic amines or corticosteroids; immunotherapy allowed if patient had received a constant dose for at least 12 weeks before enrolment with a continuation of the same regimen during the study CRITERIA FOR RANDOMISATION DURING RUN-IN: >= 3 nocturnal awakenings due to asthma symptoms during the 7 days before randomisation; >= 3 days with daytime symptoms during the 7 days before randomisation; >= 3 days with albuterol used as a relief medication during the 7 days before randomisation |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES reported at 4, 12 and 24 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BDP 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 24 weeks TEST GROUP: Beclomethasone 200 mg plus salmeterol 50 mg twice daily CONTROL GROUP: Beclomethasone 400 mg twice daily DEVICE: MDI NUMBER OF DEVICES: 2 COMPLIANCE: Evaluated CO-TREATMENT: prn SABA; maintenance theophylline |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; am PEF*; pm PEF SYMPTOM SCORES: Change in symptom score (score of 0 to 4) FUNCTIONAL STATUS: Rescue medication use; nocturnal awakening; exacerbation (defined as events requiring treatment with any asthma medication excluded during study participation); mean % symptom-free days INFLAMMATORY MARKERS: No laboratory analysis was performed ADVERSE EFFECTS: Reported WITHDRAWALS: Reported |
|
| Notes | Full-text publication Funded by Glaxo Welcome Confirmation of methodology and data obtained User-defined number: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers |
| Allocation concealment? | Yes | Number coded inhalers supplied by pharmacy |
| Blinding? All outcomes |
Yes | Identical placebos used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “All efficacy and safety analyses were performed on the intent-to-treat (ITT) population consisting of all subjects randomised to blinded study medication.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from GSK |
| Methods | Parallel-group, multicentre study. Four treatment groups of which 2 considered for this review, namely: BUD 200 + F12 bid and BUD 400 bid Jadad quality score: 4 |
|
| Participants | Symptomatic asthmatic teenagers >= 12 years and adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 634 (BUD200 + F: 323; BUD400: 312) WITHDRAWALS: Not reported by subgroup AGE mean: 37 GENDER (% male): 43.6 SEVERITY: Mild BASELINE % PREDICTED FEV1: 87 BASELINE DOSE OF ICS : <= 400 mcg/d BUD ASTHMA DURATION: Not reported ATOPY(%): Not reported ELIGIBILITY CRITERIA: >= 12 years of age with mild asthma; taking <= 400 mcg/daily of inhaled budesonide or its equivalent for >= 3 months; FEV1 >= 70% predicted normal after terbutaline EXCLUSION CRITERIA: Experience 3 severe exacerbations during the initial 6 months or 5 exacerbations in total; 2 poorly controlled asthma days, defined as days with morning PEF values >= 2 above baseline, or with asthma awakening CRITERIA FOR RANDOMISATION DURING RUN-IN: Randomised patients demonstrated a need for 2 or more inhalations per week of rescue medication during the last 2 weeks of run-in, a >= 15% variability in peak expiratory flows, or a >= 12% increase in FEV1 after terbutaline |
|
| Interventions | LABA + ICS vs INCREASED dose ICS OUTCOMES reported at 52 weeks RUN-IN PERIOD: 4 weeks DOSE OF ICS DURING RUN-IN: BUD 100 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 52 weeks TEST GROUP: Budesonide 100 mcg bid + formoterol 12 mcg bid CONTROL GROUP: Budesonide 200 mcg bid DEVICE: Turbuhaler NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; FEV1 SYMPTOM SCORES: Not reported FUNCTIONAL STATUS: Asthma symptom days; nocturnal awakenings; rescue medication use; exacerbations INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Not reported WITHDRAWAL: Not reported *Primary outcome: time to the first severe asthma exacerbation defined as need for treatment with oral corticosteroids or hospital admission or emergency treatment for worsening asthma or a decrease in morning PEF > 25% from baseline |
|
| Notes | Full-text publication Funded by AstraZeneca Confirmation of methodology obtained User-defined number: 200 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers |
| Allocation concealment? | Yes | Opaque consecutive numbered envelopes containing assignment |
| Blinding? All outcomes |
Yes | Use of identical placebo |
| Incomplete outcome data addressed? All outcomes |
Unclear | Intention-to-treat analysis stated, but explicit description of its composition not available |
| Free of selective reporting? | Yes | Primary outcome data available from study publication |
| Methods | Parallel-group, multicentre study (246 centres in 22 countries). Three treatment groups: BUD; BUD/F and BUD/F (with BUD/F also as reliever) Jadad quality score: 4 |
|
| Participants | Symptomatic asthmatic adults and children % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 85 RANDOMISED: 1835 (BUD: 926; BUD/F: 909) WITHDRAWALS: BUD/F: 148; BUD: 142 AGE mean (range): 35 (4 to 79) GENDER (% male): 44 SEVERITY: Moderate BASELINE % PREDICTED FEV1 (mean): 73 BASELINE DOSE OF ICS: 615 mcg/d ASTHMA DURATION: 9 years ATOPY (%): Not reported ELIGIBILITY CRITERIA: 4 to 80 years; treatment with 400 to 1000 mcg/d ICS (200 to 500 mcg/d for participants aged 4 to 11 years) for 3 or more months; FEV1 predicted 60% to 100%; 12 or more inhalations during last 10 days of run-in (8 for participants aged 4 to 11 years) EXCLUSION CRITERIA: Participants using 10 or more inhalations on one day during run-in (7 or more for participants aged 4 to 11 years); participants experiencing an exacerbation of asthma during run-in period |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES: TIMING 12 months RUN-IN: 14 to 18 days DOSE OF ICS DURING RUN-IN: Same as pre-study ICS dose (+ terbutaline) INTERVENTION PERIOD: 12 months TEST GROUP: Combination budesonide and formoterol (100/6 mcg) bid CONTROL GROUP: Budesonide 400 mcg bid (plus as needed terbutaline) DEVICE: Turbohaler NUMBER OF DEVICES: 1 COMPLIANCE: Self-reported compliance on 84% of days; self-reported non-compliance on 3% of days; incomplete records on 13% of days CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF SYMPTOM SCORES: Daytime scores; nighttime scores; % symptom-free days FUNCTIONAL STATUS: Exacerbations (treated with oral steroids, hospitalisation or ED visit)*; rescue medication use; night awakenings INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full-text publication Source of funding Astra Zeneca Confirmation of methodology and data: Requested, obtained for adults. Data on children were requested directly from the study sponsors concurrently. The data for OCS-treated exacerbations for children were not available User defined number: 800 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated randomisation scheme |
| Allocation concealment? | Unclear | Eligible patients were randomised in balanced blocks by allocating patient numbers in consecutive order |
| Blinding? All outcomes |
Yes | Double-blind; identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “All analyses were performed on an intention-to-treat basis.” Additional information on the composition of the ITT population was not provided |
| Free of selective reporting? | Yes | Data on OCS-treated exacerbations reported as composite with ED visits/hospitalisations, PEF falls and requirement for medical intervention. Separate data for OCS-treated exacerbations and hospital admission received. Data on adults were received from study sponsors directly. We requested data for children from the study sponsors concurrently but these were not available |
| Methods | Parallel-group study Jadad quality score: 1 |
|
| Participants | Symptomatic asthmatic children % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 20 (BDP/Sal: 10; BDP: 10) WITHDRAWALS: Not described AGE range: 6 to 19 years GENDER (% male): Not described SEVERITY: Moderate BASELINE % PREDICTED FEV1: Not described ASTHMA DURATION: Not reported ATOPY(%): Not reported ELIGIBILITY CRITERIA: Still symptomatic despite maintenance treatment with 200 mcg bid of BDP EXCLUSION CRITERIA: Not described |
|
| Interventions | LABA + ICS vs INCREASED dose ICS OUTCOMES: reported at 8,12 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BDP 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: Salmeterol 50 mcg bid + beclomethasone 200 mcg bid CONTROL GROUP: Beclomethasone 400 bid DEVICE: Not specified NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: Not specified |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; PEF; FEF 25% to 75% SYMPTOM SCORES: Daily symptoms (no data for control group) FUNCTIONAL STATUS: Not reported INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Not reported WITHDRAWAL: Not reported |
|
| Notes | Abstract Funding not reported Confirmation of methodology and data extraction: Not obtained User-defined order: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; no other information presented |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
No | Open label |
| Incomplete outcome data addressed? All outcomes |
Unclear | No information provided |
| Free of selective reporting? | Unclear | Unclear whether data on OCS-treated exacerbations were collected in the study |
| Methods | Parallel-group, multicentre study (71 centres). Four treatment groups of which 2 considered here, namely: F12 + BUD 100 bid and BUD 400 + placebo bid Jadad quality score: 5 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 77 RANDOMISED: 424 (F12 bid + BUD 100 bid: 210; BUD 400 mcg bid: 214) WITHDRAWAL: BUD/F: 39; BUD: 37 AGE: mean (range): 42 (18 to 70) GENDER (% male): 49 ASTHMA SEVERITY: Moderate BASELINE % PREDICTED FEV1 mean: 75.6 BASELINE DOSE OF ICS (start of run-in): 820 (100 to 2000) ASTHMA DURATION: Not reported ATOPY(%): Not reported ELIGIBILITY CRITERIA: Asthma for at least 6 months; treated with an inhaled corticosteroid for at least 3 months; baseline FEV1 >= 50% predicted; >= 15% improvement following inhalation of 1 mg of terbutaline EXCLUSION CRITERIA: Use of beclomethasone > 2000 mcg/day or budesonide by MDI > 1600 mcg/day or budesonide by turbuhaler > 800 mcg/day or fluticasone > 800 mcg/day; >= 3 courses of oral steroids in past 6 months; hospitalisation for asthma in past 6 months CRITERIA FOR RANDOMISATION DURING RUN-IN: Compliance with 75% to 125% of the recommended dose of budesonide; stable asthma over the preceding 10 days as defined by the absence of the following criteria: diurnal variation of more than 20% in PEF on 2 consecutive days; use of 4 or more inhalations of rescue medication per day on 2 consecutive days; awakening due to asthma on 2 consecutive nights or the need to use oral glucocorticoids |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES reported at 1, 2, 3, 6, 9 and 12 months RUN-IN PERIOD: 4 weeks to document stability and compliance DOSE OF ICS DURING RUN-IN: BUD 800 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 months TEST GROUP: (BUD/F) formoterol 12 mcg bid + budesonide 100 mcg bid CONTROL GROUP: (BUD) budesonide 400 mcg bid + placebo DEVICE: Turbuhaler NUMBER OF DEVICES: 2 COMPLIANCE: Yes - hidden mechanical counter built into inhaler which could only be seen by investigators CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 predicted; am PEF; pm PEF SYMPTOM SCORES: Mean daytime and nighttime symptom scores at end of study (4-point scale: averaged over 10 days) FUNCTIONAL STATUS: Rescue medication use; nocturnal awakening (number per night); severe exacerbation (requiring systemic steroids); episode free days (mean % of year) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWAL: Reported *Primary outcome: rates of severe and mild exacerbations of asthma per patient per year |
|
| Notes | Full-text publication Funded by Astra Draco, Lund, Sweden Confirmation of methodology and data obtained User-defined order: 600 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers list |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Identical inhaler devices |
| Incomplete outcome data addressed? All outcomes |
No | Last observation carried forward: “The analysis included all randomised patients (intention-to-treat approach). Data for patients who withdrew or discontinued therapy were included up to the time of their withdrawal.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available from study report |
| Methods | Parallel-group, multicentre study (11 centres). Six treatment groups of which 2 are considered for this review, namely: FP 100 bid + SL 50 bid; FP250 bid + placebo Jadad quality score = 5 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 48 (FP/Sal: 25; FP: 23) WITHDRAWALS: FP/Sal: 2; FP: 2 AGE: mean (range): 32 (14 to 61) GENDER (% male): 48 SEVERITY: Moderate BASELINE % PREDICTED FEV1: 66 BASELINE DOSE OF ICS (SE): Steroid-naive for at least 30 days prior to study onset ASTHMA DURATION: >= 6 months and < 1 year: 0; >= 1 year and < 5 years: 8; >= 5 years and < 10 years: 5; >= 10 years and < 15 years: 6; >= 15 years: 29 ATOPY(%): Not recorded ELIGIBILITY CRITERIA: >= 12 years; FEV1 between 50% and 80% of predicted value for age, sex, height and race; medical history of asthma of at least 6 months requiring pharmacotherapy; >= 15% increase in FEV1 15 minutes after 2 puffs of inhaled albuterol; being treated with daily or as-needed short-acting beta-sympathomimetic bronchodilators; females had negative pregnancy tests, or be surgically sterile, or postmenopausal for at least 1 year, or using acceptable birth control for at least 1 month prior to participation EXCLUSION CRITERIA: History of life-threatening asthma; hypersensitivity reaction to sympathomimetic drugs or corticosteroids; smoking within the previous year or a history of > 10 pack-years; use of oral, inhaled, injectable, or intranasal corticosteroid therapy within the previous month; use of daily oral corticosteroid treatment within the previous 6 months; use of any other prescription or over-the-counter medication that may affect the course of asthma or interact with sympathomimetic amines; abnormal chest X-rays; clinically significant abnormal 12-lead electrocardiograms; history of significant concurrent disease CRITERIA FOR RANDOMISATION DURING RUN-IN: Completion of daily diary cards and report medication compliance; patients were not eligible for inclusion if they used 12 or more puffs of albuterol daily for more than 2 days or if they had more than 2 nighttime awakenings due to asthma requiring treatment with albuterol during the 7 days immediately preceding the randomisation period; FEV 1 had to be between 50% and 80% of the predicted value and within 15% of the FEV1 obtained at the beginning of the screening period |
|
| Interventions | LABA + ICS vs INCREASED dose ICS OUTCOMES reported at 2 and 4 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: Same as usual DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 4 weeks TEST GROUP: (SL50 + FP100) salmeterol 50 mg bid + fluticasone propionate 100 mg bid CONTROL GROUP: (FP 250) fluticasone propionate 250 mg bid DEVICE: Metered-dose inhaler NUMBER OF DEVICES: 2 COMPLIANCE: Evaluated CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF SYMPTOM SCORE: Score of 0 to 4 mean change from baseline FUNCTIONAL STATUS: Rescue medication use; mean change in % nights with no awakenings; episode-free days INFLAMMATORY MARKERS: Not measured ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure: Not reported |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data confirmed User defined number: 600 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Use of identical placebo (double-dummy design) |
| Incomplete outcome data addressed? All outcomes |
Unclear | Intention-to-treat population defined as “all randomised subjects exposed to the study drug”. Handling of withdrawals not explicit |
| Free of selective reporting? | Yes | Exacerbations not assessed |
| Methods | Parallel-group, multicentre study | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 321 (FP/SAL: 160; FP: 161) WITHDRAWALS: FP/SAL: 3; FP: 6 AGE mean: 8 SEVERITY: Not reported BASELINE % PREDICTED FEV1: 102 BASELINE DOSE OF ICS: Not stated ASTHMA DURATION: Not stated ATOPY (%): Not stated ELIGIBILITY CRITERIA: 4 to 1 years; diagnosis of asthma for aminimum of 6 months; airway reversibility of = 15% based either on FEV1 or PEF; treatment with medium dose ICS (beclomethasone dipropionate (BDP) equivalent 400 to 500 mcg/day for 3 months prior to Visit 1 EXCLUSION CRITERIA: Respiratory tract infection in previous 4 weeks; acute asthma exacerbation requiring emergency room treatment within the last 4 weeks/hospitalisation within last 12 weeks; use of systemic corticosteroid within the last 12 weeks, or use of LABA, oral ß2-agonists, leukotriene antagonists or theophyllines during 4 weeks prior to screening visit; ineligible for randomisation if, during the run-in period, change in asthma medication including use of systemic corticosteroids, or respiratory tract infection or asthma exacerbation ELIGIBILITY CRITERIA DURING RUN-IN: Asthma assessed as not “well-controlled” for at least 2 of 4 weeks of run-in; FEV1 > 60% during run-in |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES: 12 weeks RUN-IN PERIOD: 4 weeks DOSE OPTIMISATION PERIOD: N/A INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Fluticasone 200 mcg bid INHALER DEVICE: Dry powder inhaler NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF SYMPTOM SCORES: NA FUNCTIONAL STATUS: N achieving well-controlled asthma INFLAMMATORY MARKERS: NA ADVERSE EFFECTS: Reported WITHDRAWALS: Reported |
|
| Notes | Unpublished study Funding source: GSK Confirmation of methodology and data: obtained for methods User defined: 800 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Double-blind; double-dummy |
| Incomplete outcome data addressed? All outcomes |
Unclear | No detailed information on how intention-to-treat population was composed |
| Free of selective reporting? | Yes | OCS-exacerbations available on request from study sponsor |
| Methods | Parallel-group, multicentre study (40 centres in Canada) Jadad quality score = 4 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 237 (FP/SAL: 121; FP: 116) WITHDRAWALS: FP/SAL: 4; FP: 7 AGE mean: 37 GENDER (% male): 35 SEVERITY: Moderate BASELINE % PREDICTED FEV1 (mean): Not reported BASELINE DOSE OF ICS: 100 mcg/d FP ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: >= 12 years of age; symptomatic despite low doses of ICS (<= 500 mcg/d or equivalent of BUD) for less than 4 weeks (criterion for run-in phase - participants who met the above criterion but had been on ICS for longer bypassed the run-in phase); symptomatic at end of run-in phase (on low-dose FP) EXCLUSION CRITERIA: < 60% or > 90% predicted of PEF at visit 1 |
|
| Interventions | LABA + ICS versus INCREASED dose of FP OUTCOMES - TIMING 12 weeks RUN-IN: 2 weeks DOSE OF ICS DURING RUN-IN: 100 mcg/d FP INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 bid CONTROL GROUP: Fluticasone 250 mcg bid DEVICE: Metered dose inhaler NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORES: Not reported FUNCTIONAL STATUS: Not reported INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Unpublished full data-set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Not obtained User defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The Intent-to-Treat (ITT) population was used for all analyses including demographic, efficacy, safety and health outcome endpoints. This population consisted of all subjects who entered the study and were randomised to treatment.” |
| Free of selective reporting? | Yes | Moderate exacerbations used as proxy for steroid-treated exacerbations (see Analysis 3.1) |
| Methods | Parallel-group, multicentre study (61 centres in UK) Jadad quality score = 4 |
|
| Participants | Moderately severe steroid using asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 68 (FP/SAL: 35; BDP: 33) WITHDRAWALS: FP/SAL: 10; BDP: 10 AGE: mean: 44 GENDER (% male): 50 SEVERITY: Moderate BASELINE % PREDICTED FEV1 (mean): 75 BASELINE DOSE OF ICS: 400 to 500 mcg/d BDP ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: >= 12 years of age; 400-500 mcg/d BDP equivalent; >= 50% < 85% predicted PEF during run-in; relief medication on >= 2 occasions on 3 of last 7 days; >= 2 on symptom scores on 3 of last 7 days on baseline OR >= 1 on night symptoms during same period EXCLUSION CRITERIA: Not reported |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES: TIMING 12 weeks RUN-IN: 2 weeks DOSE OF ICS DURING RUN-IN: Current ICS treatment INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Beclomethasone 400 mcg bid DEVICE: FP/SAL: Evohaler; BDP: Accuhaler NUMBER OF DEVICES: 1 (double-dummy design meant that participants given 2 inhalers) COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF SYMPTOM SCORES: Percentage symptom-free days* FUNCTIONAL STATUS: Rescue medication usage; health-related quality of life (AQLQ) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measures* |
|
| Notes | Unpublished full data set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Obtained for methods User defined number: 800 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Double-dummy design |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The intention-to-treat (ITT) sample was used for the efficacy and safety analyses. This consisted of all subjects randomised to and receiving at least one dose of study medication.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from study sponsor |
| Methods | Parallel-group, multicentre study Jadad quality score = 4 |
|
| Participants | Steroid-using asthmatic children % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 367 (FP/SAL: 181; FP: 186) WITHDRAWAL: FP/SAL: 3; FP: 5 AGE mean: 7.8 years GENDER (male %): 72 ASTHMA SEVERITY: Moderate BASELINE % PREDICTED FEV1: Not reported (PEF: 88%) BASELINE DOSE OF ICS (start of run-in): Not reported ASTHMA DURATION: Not reported ATOPY(%): Not reported ELIGIBILITY CRITERIA: 4 to 11 years, inclusive; documented evidence of asthma; BDP, BUD or equivalent 400 to 500 mcg/day/FP 200 to 250 mcg/day for at least 4 weeks before Visit 1 EXCLUSION CRITERIA: Not reported Criteria for randomisation post-run-in: Symptom score >= 2 on 3 of last 7 days of run-in; mean morning PEF > 50% and < 85%; dairy card completion of 70% |
|
| Interventions | LABA + ICS versus SAME dose of ICS OUTCOMES: Reported at 6 months RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: Not clear DOSE OPTIMISATION PERIOD: None reported INTERVENTION PERIOD: 6 months TEST GROUP: Combination salmeterol 50/fluticasone 100 mcg bid CONTROL GROUP: Fluticasone 200 mcg bid DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; pm PEF; FEV1 SYMPTOM SCORES: % Symptom-free days*; % symptom-free nights* FUNCTIONAL STATUS: Use of reliever medication; exacerbations (undefined) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWAL: Reported Primary outcome measure* |
|
| Notes | Full unpublished data set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Obtained for methods, not obtained for data User defined number: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices |
| Incomplete outcome data addressed? All outcomes |
Unclear | “To be evaluable, subjects had to meet the entry and randomisation criteria, receive at least one dose of study medication and have completed at least one day’s post-randomisation diary information.” |
| Free of selective reporting? | Yes | Exacerbations described in trial report available; OCS-treated exacerbations could not be identified from the data available. Data used in sensitivity analysis (see Analysis 3.1) |
| Methods | Parallel-group, multicentre study (79 centres in Canada) Jadad quality score = 4 |
|
| Participants | Controlled moderately severe asthmatic adults % ELIGIBLE OF SCREENED POPULATION: 71 % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 483 (FP/SAL: 242; FP: 241) WITHDRAWALS: FP/SAL: 43; FP: 41 AGE: mean: 39 GENDER (% male): 42 SEVERITY: Moderate BASELINE % PREDICTED FEV1: Not reported BASELINE DOSE OF ICS: >= BUD 400 mcg/d or equivalent ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: 12 to 70 years of age; clinical diagnosis of persistent asthma; ability to use HFA-salbutamol as prn SABA; >= BUD 400 mcg/d or equivalent; asthma control during run-in (defined by Canadian guidelines) EXCLUSION CRITERIA: Not reported |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES TIMING: 12 weeks RUN-IN: 2 weeks DOSE OF ICS DURING RUN-IN: FP 250 mcg bid INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Fluticasone 250 mcg bid DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF SYMPTOM SCORES: % symptom-free days FUNCTIONAL STATUS: Rescue medication use; nocturnal awakenings INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Unpublished full data-set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Obtained for methods, not obtained for data User defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The primary population was the Intent-to-Treat (ITT) population. The ITT population was defined as subjects who were randomised and treated with at least one dose of investigational product.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from study sponsor |
| Methods | Parallel-group, multicentre study | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 24 (FP/SAL: 12; FP: 12) WITHDRAWALS: F/SAL: 1; FP: 1 AGE mean: 7.3 SEVERITY: Not stated BASELINE % PREDICTED FEV1: Not reported BASELINE DOSE OF ICS: Not stated ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: 4 to 8 years; history of asthma for at least 3 months; maintenance ICS dose of 200 to 800 mcg /day BDP or equivalent for at least 4 weeks; sufficiently stable to receive FP 200 mcg/day during 2-week run-in; sRAW value of = 1.3 kPa.s for entry into the screening and treatment period EXCLUSION CRITERIA: Use of systemic steroids in 4 weeks prior to study entry; required 3 or more courses of oral corticosteroids in 12 months prior to study entry; admitted to intensive care for asthma within 3 months prior to study entry ELIGIBILITY CRITERIA DURING RUN-IN: Participants who had a change in medication following an exacerbation during run-in were excluded |
|
| Interventions | LABA + ICS versus INCREASED DOSE ICS OUTCOMES: 6 weeks RUN-IN PERIOD: 2 weeks DOSE OPTIMISATION PERIOD: 2 weeks INTERVENTION PERIOD: 6 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid via DPI CONTROL GROUP: Fluticasone 200 mcg bid via DPI NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1 SYMPTOM SCORES: Day and nocturnal scores FUNCTIONAL STATUS: Rescue medication use INFLAMMATORY MARKERS: sRAW* ADVERSE EFFECTS: Reported WITHDRAWALS: Reported |
|
| Notes | Unpublished data sourced from http://ctr.gsk.co.uk
Funding source: GSK Confirmation of methodology and data not obtained User defined: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Double-blind; identical devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | No detailed information on how intention-to-treat population was composed |
| Free of selective reporting? | Unclear | Unclear whether data on OCS-treated exacerbations were collected. Request for data from study sponsors has not been successful |
| Methods | Parallel-group, multicentre study (10 centres in UK) Jadad quality score = 4 |
|
| Participants | Moderately severe asthmatic adults with smoking history % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 18 (FP/SAL: 8; FP: 10) WITHDRAWALS: FP/SAL: 1; FP: 2 AGE mean: 55 GENDER (% male): 56 SEVERITY: Moderate BASELINE % PREDICTED FEV1: Not reported BASELINE DOSE OF ICS: 200 to 400 mcg/d FP ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: Current/former smokers with >= 10 pack years; >= 200 mcg/d to <= 400 mcg/d FP or equivalent; PEF between 50% and 85% predicted during last 7 days of run-in OR symptom score < 2 on >= 3 of last 7 days of run-in OR night symptoms of >= 1 on >= 3 days of last 7 days of run-in EXCLUSION CRITERIA: Not reported |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES TIMING: 12 weeks RUN-IN: 2 weeks DOSE OF ICS DURING RUN-IN: Not clear INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Fluticasone 250 mcg bid DEVICE: Evohaler NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF* SYMPTOM SCORES: Not reported FUNCTIONAL STATUS: AQLQ INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Unpublished full data set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Obtained for methods, not obtained for data User defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler device used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The sample used for the analysis was the intention-to-treat sample (all subjects randomised & receiving at least one dose of study medication).” |
| Free of selective reporting? | Unclear | Unclear whether data on OCS-treated exacerbations were collected. Request for data from study sponsors has not been successful |
| Methods | Parallel-group trial, single centre in Netherlands Jadad quality score = 4 |
|
| Participants | Moderately severe asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 12 (FP/SAL: 5; FP: 7) WITHDRAWALS: 0 AGE: mean: 39 GENDER (% male): 5 SEVERITY: Moderate BASELINE % PREDICTED FEV1: Not reported BASELINE DOSE OF ICS: 500 to 1000 mcg/d FP ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: Requirement for 500 to 1000 mcg/d FP; morning PEF during run-in 50% to 85%; cumulative symptom score indicating moderate asthma; PC20 > 4 mg/ml histamine EXCLUSION CRITERIA: Dermatitis; recent lower RTI; exacerbation in last 3 months; smoking history of at least 10 pack-years |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES TIMING: 58 weeks RUN-IN: Not specified DOSE OF ICS DURING RUN-IN: Not specified INTERVENTION PERIOD: 58 weeks TEST GROUP: Combination fluticasone and salmeterol 250/50 mcg bid CONTROL GROUP: Fluticasone 500 mcg bid DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: Not reported SYMPTOM SCORES: Not reported FUNCTIONAL STATUS: Exacerbations (not defined) INFLAMMATORY MARKERS: PC20* ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Unpublished full data set from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Not obtained User defined number: 2000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Yes | No withdrawals occurred |
| Free of selective reporting? | Yes | Exacerbations described in trial report available; OCS-treated exacerbations could not be identified from the data available. Data used in sensitivity analysis (see Analysis 3.1) |
| Methods | Parallel-group, multicentre study (95 centres in North America) Jadad quality score = 4 |
|
| Participants | Moderately severe asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 636 (FP/SAL: 321; FP: 315) WITHDRAWALS: FP/SAL: 32; FP: 44 AGE mean: 39 GENDER (% male): 38 SEVERITY: Moderate BASELINE % PREDICTED FEV1: 80.4 BASELINE DOSE OF ICS: Not reported ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: 12 years or older - medium dose of ICS for at least 30 days prior to randomisation (dose not specified); ATS defined asthma for at least 6 months; FEV1 65% to 95% predicted; >= 12% reversibility post-SABA EXCLUSION CRITERIA: Life-threatening asthma/hospitalisation within 3 months of study entry; OCS within 30 days of screening OR 2 courses within 90 days; other concurrent respiratory disease; more than a 10 pack-year history of smoking |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES TIMING: 12, 24 weeks (trial extension) RUN-IN: Not reported DOSE OF ICS DURING RUN-IN: Not reported INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Fluticasone 250 mcg bid DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; FEV1 SYMPTOM SCORES: % symptom-free days FUNCTIONAL STATUS: Rescue medication usage INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Due to lack of efficacy*, other reasons reported Primary outcome measure* |
|
| Notes | Full unpublished data set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Obtained for methods, not for data User defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “Efficacy and safety analyses were performed on the intent-to-treat (ITT) population which consisted of all subjects who were randomised to study drug regardless of enrolment date.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from GSK |
| Methods | Parallel-group, multicentre study (151 centres in USA). Five treatment arms of which 2 are considered here | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: 28 % RUN-IN PARTICIPANTS RANDOMISED: 63 RANDOMISED: 297 (BUD/F 200 qd: 152; BUD 400 qd: 145) WITHDRAWALS: BUD/F 200 qd: 19;BUD/F 400 qd: 28 AGE mean: 38 SEVERITY: Not reported BASELINE % PREDICTED FEV1: 75.3% BASELINE DOSE OF ICS: 382 ASTHMA DURATION: 19.7 ATOPY (%): Not reported ELIGIBILITY CRITERIA: > 16 years; documented clinical diagnosis of asthma for at least 6 months prior to screening; stable condition; maintenance asthma treatment with a low to medium dose ICS for at least 4 weeks prior to the screening; FEV1 60% to 90% predicted EXCLUSION CRITERIA: Not reported ELIGIBILITY CRITERIA DURING RUN-IN: Stable during run-in period |
|
| Interventions | OUTCOMES: 12 weeks RUN-IN PERIOD: 4 to 5 weeks DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination budesonide and formoterol (200/12 mcg) qd CONTROL GROUP: Budesonide 400 mcg qd NUMBER OF DEVICES: 2 (double-dummy design; LABA co-delivered with ICS in 1 inhaler) COMPLIANCE: Not assessed CO-TREATMENT prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; pm PEF; FEV1 SYMPTOM SCORES: Day symptoms; night symptoms FUNCTIONAL STATUS: Quality of life (AQLQ) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported |
|
| Notes | Unpublished trial data from www.astrazenecaclinicaltrials.com
Funding source: AZ Confirmation of data and methodology: Not obtained User defined number: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; other information not available |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Double-dummy |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The efficacy analysis set (EAS), defined as all randomised subjects who took at least 1 dose of double-blind treatment and who contributed at least 1 evening PEF diary entry after receiving randomised study medication, was used in the primary analysis. Sensitivity analyses of evening PEF were performed using the per protocol (PP) analysis set.” |
| Free of selective reporting? | Unclear | Not clear whether OCS-treated exacerbations collected in the study |
| Methods | Parallel-group, multicentre study (77 centres in USA). Three treatment arms, of which 2 are considered here | |
| Participants | % ELIGIBLE OF SCREENED POPULATION: 62 % RUN-IN PARTICIPANTS RANDOMISED: 88 RANDOMISED: 265 (BUD/F 132; BUD: 133) WITHDRAWALS: Not reported AGE mean (SD): 40 (16.5) SEVERITY: Moderate to severe asthma BASELINE % PREDICTED FEV1: 73 BASELINE DOSE OF ICS: 500 mcg/d ASTHMA DURATION: 22.7 years ATOPY (%) Not reported ELIGIBILITY CRITERIA: > 12 years of age; documented clinical diagnosis of moderate-to-severe asthma for at least 6 months prior to screening; stable condition; maintenance asthma treatment with a stable dose of inhaled corticosteroids (ICS) for at least 4 weeks; FEV1 > 45% of predicted normal EXCLUSION CRITERIA: Not reported ELIGIBILITY CRITERIA DURING RUN-IN: Not reported |
|
| Interventions | LABA + ICS versus HIGHER dose ICS OUTCOMES: 52 weeks RUN-IN PERIOD: 2 weeks DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 52 weeks TEST GROUP: Combination budesonide and formoterol 400/12 mcg bid CONTROL GROUP: Budesonide 800 mcg bid NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF; pm PEF; FEV1 SYMPTOM SCORES: Not measured FUNCTIONAL STATUS: Days without symptoms; exacerbations (defined as requirement for OCS, ED visit and hospitalisation); rescue medication use INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported due to adverse events |
|
| Notes | Unpublished data set available from www.astrazenecaclinicaltrials.com
Funding source: AZ Data and methodology: Not obtained User defined: 800 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised; other information not available |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “…all randomised subjects who received at least 1 dose of randomised study drug, the post-dose analysis set, consisting of all subjects who had clinic visit safety assessments measured 1-2 hours after randomised treatment at all visits, was also used in the analysis of some safety data.” |
| Free of selective reporting? | Unclear | Not clear whether OCS-treated exacerbations collected in the study |
| Methods | Parallel-group, multicentre study (124 centres in France). Three treatment groups (FP/SAL 250/50; FP/SAL 100/50; FP250) Jadad quality score = 4 |
|
| Participants | Moderately severe well-controlled asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 318 (FP/SAL: 158; FP: 159) WITHDRAWALS: FP/SAL: 15; FP: 30 AGE mean: 45 GENDER (% male): 50 SEVERITY: Moderately severe BASELINE % PREDICTED FEV1: 90 BASELINE DOSE OF ICS: 1000 mcg/d BDP ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: >= 18 years of age; documented history of asthma for at least 6 months; treatment with high dose BDP and LABA for 4 weeks; symptoms < 2 days per week; use of rescue medication < 2 days and < 4 occasions per week; PEF > 80% every day during run-in EXCLUSION CRITERIA: Significant smoking history; RTI in 4 weeks prior to randomisation; exacerbation in 4 weeks prior to baseline; use of depot steroid in 12 weeks prior to visit 1; change in asthma medication |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES TIMING: 24 weeks RUN-IN: 8 weeks DOSE OF ICS DURING RUN-IN: 500 mcg/d (combination FP/SAL 250/50 mcg bid) INTERVENTION PERIOD: 12 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Fluticasone 250 mcg bid DEVICE: Diskus NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORES: Not reported FUNCTIONAL STATUS: Exacerbations (not defined) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full unpublished data set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: Obtained for methods, not obtained for data User defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices used |
| Incomplete outcome data addressed? All outcomes |
Unclear | “Full Analysis Set (FAS) population consisted of all subjects who received at least one dose of study medication and for whom the assessment data for at least one assessment criterion was available.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from study sponsor |
| Methods | Parallel-group, multicentre study Jadad quality score = 5 |
|
| Participants | Symptomatic asthmatic adults on prn SABA % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 488 (FP/SAL: 246; FP: 242) WITHDRAWALS: FP/SAL: 31; FP: 35 AGE mean: 37.5 years GENDER (% male): 50.2 SEVERITY: Moderate to severe persistent asthma BASELINE % PREDICTED FEV1(mean): 60.5% BASELINE DOSE OF ICS: Not described ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: FEV1 40% to 80% predicted; FEV1 reversibility >= 15% post-SABA; if participant’s FEV1 between 65% to 80% also required to: i) average > 4 puffs/d of SABA in 7 days prior to screening ii) nocturnal awakenings on 3 nights/week over 2 weeks prior to screening) asthma symptoms on half run-in days EXCLUSION CRITERIA: Current tobacco use, a hospital admission for asthma in the past 30 days, an upper or lower respiratory tract infection within 30 days; female patients who had a positive pregnancy test result or were lactating; the following medications were not allowed for the indicated times before screening: oral or parenteral corticosteroid therapy within 30 days, oral or long-acting inhaled bronchodilators within 48 hours, and cromolyn or nedocromil within 30 days |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES reported at 2, 4, 8, 12, 16, 20 and 24 weeks RUN-IN: 2 weeks (prn SABA) DOSE OF ICS DURING RUN-IN: 0 INTERVENTION PERIOD: 24 weeks TEST GROUP: Fluticasone 100 mcg bid plus salmeterol 50 mcg bid CONTROL GROUP: Fluticasone 250 mcg bid DEVICE: MDI NUMBER OF DEVICES: 2 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORES: Combined symptoms FUNCTIONAL STATUS: Awakenings per night; rescue medication usage; exacerbations (OCS treatment) INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported Primary outcome measure* |
|
| Notes | Full unpublished data set available from http://www.ctr.gsk.co.uk
Source of funding: GSK Confirmation of methodology and data: obtained User defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices used in double-dummy design |
| Incomplete outcome data addressed? All outcomes |
Unclear | “All statistical analyses were performed on the intent-to-treat (ITT) population. The ITT population consisted of all subjects who had been randomised to study drug.” |
| Free of selective reporting? | Yes | OCS-treated exacerbations available on request from GSK |
| Methods | Parallel-group, multicentre study (27 centres) Jadad quality score = 4 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 74 RANDOMISED: 274 (FP + Sal: 139; FP: 135) WITHDRAWALS: FP + Sal: 6; FP: 9 AGE mean: 47 years GENDER (% males): 48 SEVERITY: Moderate BASELINE % PREDICTED FEV1: 72 BASELINE DOSE OF ICS: 400 to 1200 ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: Aged at least 18 years; receiving 400 to 600 mcg BDP or 800 to 1200 mcg BUD daily CRITERIA FOR RANDOMISATION DURING RUN-IN: FEV1 at least 50% of predicted value at visit 3 ; >= 10% improvement from baseline of FEV1 following inhaled salbutamol; daytime and nighttime symptom score >= 1 or diurnal variation in PEF of >= 15% or use of rescue salbutamol >= 2 times/24 hours on >= 4 days of the last 2 weeks of the run-in EXCLUSION CRITERIA: Change in asthma medication in pervious 6 weeks; use of oral steroids in previous 3 months; upper or lower tract infection needing antibiotics or admission to hospital for asthma in the previous month |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES: Reported at 1,4 and 12 weeks RUN-IN PERIOD: 4 weeks DOSE OF ICS DURING RUN-IN: If pre-trial dose 400 to 600 run-in dose was FP 100 bid. If pre-trial dose ICS 800 to 1200 run-in dose was FP 250 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (Salm 50 + FP100) salmeterol 50 mg bid + fluticasone propionate 100 mg bid or high-dose (Salm 50 + FP250) salmeterol 50 mg bid + fluticasone propionate 250 mg bid CONTROL GROUP: (FP200) fluticasone propionate 200 mg bid or (FP500) fluticasone propionate 500 mg bid DEVICE: Diskhaler NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA; stable dose of methylxanthines or anticholinergics |
|
| Outcomes | PULMONARY FUNCTIONTEST: am PEF; pm PEF; diurnal variation in PEF; FEV1 SYMPTOM SCORES: score of 0 to 4 FUNCTIONAL STATUS: Rescue medication use; nocturnal awakenings; severe exacerbation (requiring systemic steroids) INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Reported WITHDRAWALS: Described *Primary outcome: daily records of PEF, symptom scores and clinic lung function |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data: not obtained User-defined number: 400 or 1000 (reported as 700) |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Unclear | Described as randomised. Patients were stratified prior to randomisation according to the baseline dose of ICS. Those with a pre-trial dose of 400 to 600 mcg/day received FP 100 bid (low-dose group) and those on a pre-trial dose of 800 to 1200 mcg/day received FP 250 bid (high-dose group). The statistical analyses were only performed on both groups combined i.e. comparison of doubling existing dose of FP or addition of salmeterol 50 bid |
| Allocation concealment? | Unclear | Information not available |
| Blinding? All outcomes |
Yes | Identical inhalers used in double-dummy design |
| Incomplete outcome data addressed? All outcomes |
Unclear | No information reported |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Parallel-group, multicentre study (9 centres). Three groups of which 2 are considered in this review Jadad quality score = 5 |
|
| Participants | Asthmatic children % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 120 (BDP400 + Sal: 60; BDP800: 60) WITHDRAWALS: BDP400 + Sal: 5; BDP800: 6 AGE mean: 11.1 years GENDER (% male): 63 SEVERITY: Mild BASELINE % PREDICTED FEV1: 87.5 BASELINE DOSE OF ICS: 497 mcg ASTHMA DURATION means: 8.5 years ATOPY (%): 90 ELIGIBILITY CRITERIA: FEV1 between 55% and 90% predicted or a FEV1/FVC ratio of 50% to 75%; >= 10% improvement in FEV1 after inhalation of salbutamol; airway hyper-responsiveness to methacholine (PD20); ability to reproduce lung function test; history of stable asthma for >= 1 month without exacerbation or respiratory tract infection; use of inhaled steroids between 200 and 800 mg/day for at least 3 months prior to the beginning of the study EXCLUSION CRITERIA: Operations for congenital heart disease, oesophageal atresia, congenital or acquired anatomical malformation of the lungs or airways, dyskinetic cilia syndrome bronchiectasis; bronchopulmonary dysplasia; diabetes; renal disease; other serious conditions which may influence the possibility of continuation of the study; were using oral corticosteroids continuously or inhaled corticosteroids at a dose of more than 800 mcg daily; were using B-blocking agents or had used cromoglycate or nedocromil sodium within the previous 2 weeks; were allergic to B-agonists; were pregnant or lactating, or females of childbearing age who in the opinion of the supervising physician were not taking adequate contraceptive precautions; an ongoing desensitisation programme; inability to follow therapy instructions, inability to inhale medications adequately or inability to use peak flow meter. During study: non-compliance with respect to study medication, completing the diary cards, clinic visits; withdrawal at own or investigators discretion; total number of course of oral corticosteroids more than allowed in study CRITERIA FOR RANDOMISATION DURING RUN-IN: No additional criteria |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES: Reported at 6, 12, 18, 24, 30, 36, 42, 48 and 54 RUN-IN PERIOD: 6 weeks DOSE OF ICS DURING RUN-IN: BDP 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 54 weeks TEST GROUP: (Salm50 + BDP200) salmeterol 50 mcg bid + beclomethasone dipropionate 200 mcg bid CONTROL GROUP: (BDP400 + placebo) beclomethasone dipropionate 400 mcg/day + placebo DEVICE: Rotadisks in combination with a diskhaler NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: FEV1; am PEF; pm PEF; FVC SYMPTOM SCORES: Asthma symptoms like wheezing, dyspnoea, exercise induced asthma and cough were scored in the morning and evening using a scale from 1 to 3; % children reporting no symptoms FUNCTIONAL STATUS: Rescue medication use; exacerbation (requiring systemic steroids); height, body weight, heart rate, systolic and diastolic blood pressure were measured INFLAMMATORY MARKERS: Total IgE ADVERSE EFFECTS: Reported WITHDRAWALS: Reported *Primary outcome: airway calibre measured as FEV1 and airway responsiveness to methacholine |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data obtained up to 24 weeks User-defined number: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers |
| Allocation concealment? | Yes | Telephone notification of assignment by co-ordinating centre |
| Blinding? All outcomes |
Yes | Double-blind; identical placebo used |
| Incomplete outcome data addressed? All outcomes |
Unclear | Not clear how population for primary outcome Incomplete diary card data not included in analysis: “Where patients failed to complete their daily record cards for more than 7 d in any 14-d period such assessments were not included in the analysis. Otherwise, when there were missing days in the record, pro rata adjustment was made to give a 2-wk assessment.” |
| Free of selective reporting? | Unclear | OCS-treated exacerbation data available |
| Methods | Parallel-group Jadad quality score = 3 |
|
| Participants | Well-controlled asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 57 RANDOMISED: 233 (BDP + Sal: 113; BDP: 120) WITHDRAWALS: 31; not described by group AGE mean: 42 GENDER (% male): 45 SEVERITY: Mild BASELINE MORNING % PREDICTED PEF: 84 BASELINE DOSE OF ICS: 360 ASTHMA DURATION: Not described ATOPY(%): Not described ELIGIBILITY CRITERIA: > 18 to 66 years old; BDP 200 to 400/day for more than 6 weeks; no recent exacerbation; no additional anti-asthmatic Rx CRITERIA FOR RANDOMISATION DURING RUN-IN: Baseline PEF at the randomisation visit had to be at least 60% predicted; ability to inhale medication correctly, proper PEF technique and complete daily records; reversibility of 15% of the baseline value was required on one of the visits EXCLUSION CRITERIA: Exacerbation requiring new medication |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES: 7 and 12 weeks RUN-IN PERIOD: 2 weeks DOSE OF ICS DURING RUN-IN: BDP 100 or 200 bid DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (BDP200 + Sal 50 bid) beclomethasone 200 mcg bid + salmeterol 50 mcg bid CONTROL GROUP: (BDP400) beclomethasone 400 mcg bid DEVICE: Diskhaler (dry powder inhaler) NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: % of run-in am and pm PEF; diurnal variation in PEF SYMPTOM SCORES: Score of 0 to 3 (averaged over 1 to 2 weeks) FUNCTIONAL STATUS: Rescue medication use; Hyland quality of life INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported but not described *Primary outcome: Not specified |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data obtained User-defined number: 400 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Double-dummy design |
| Incomplete outcome data addressed? All outcomes |
No | Patients who were withdrawn during the treatment period were evaluated up to the day of withdrawal |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Parallel-group, multicentre study. Three treatment groups of which 2 are considered here Jadad quality score = 3 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 37 (FP + Sal: 18; FP: 19) WITHDRAWALS: FP + Sal: 0; FP: 3 AGE mean: 41.5 GENDER (% male): 55.5 SEVERITY: Not stated BASELINE FEV1 % PRED: 86 BASELINE DOSE OF ICS BDP equivalent (range): 600 to 1200 ASTHMA DURATION months: 189 ATOPY (%): 59 ELIGIBILITY CRITERIA: Free of respiratory tract infection for 4 weeks before study CRITERIA FOR RANDOMISATION DURINGRUN-IN: Despite use of BUD/BDP 800 to 1200 mcg/day or FP 400 to 500 mcg/day patients were included if they had: one or more of the following symptoms: symptoms on 6 or more days, symptoms on 4 or more nights, need for rescue bronchodilator on 6 or more nights, greater than 20% variation between AM and PM PEF on 4 or more days. One or more of the following pulmonary function criteria: at least 15% improvement in FEV1 after bronchodilator, 15% increase in PEF post-bronchodilator compared to mean PEF on previous week, more than 20% variation between am and pm PEF on at least 4 consecutive days, PC20 methacholine < 4 mg/ml EXCLUSION CRITERIA: None specified |
|
| Interventions | LABA + ICS vs INCREASED dose of ICS OUTCOMES before and after 12 weeks treatment RUN-IN PERIOD: 2 to 4 weeks DOSE OF ICS DURING RUN-IN (mean): 805 DOSE OPTIMISATION PERIOD: None INTERVENTION PERIOD: 12 weeks TEST GROUP: (FP200 + Sal 50 bid) fluticasone propionate 200 mcg bid + salmeterol 50 mcg bid CONTROL GROUP: Fluticasone propionate 500 mcg bid DEVICE: Diskhaler (dry powder inhaler) NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF predicted; pm PEF predicted; FEV1 SYMPTOM SCORES: None FUNCTIONAL STATUS: Exacerbations requiring OCS treatment INFLAMMATORY MARKERS: Submucosal mast cells; submucosal eosinophils; adhesion molecules and cytokines ADVERSE EFFECTS: Not reported by group WITHDRAWALS: Reported Primary outcome measure: Not reported |
|
| Notes | Full-text publication Funded by Glaxo Wellcome Confirmation of methodology and data not obtained User-defined number: 1200 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical inhaler devices |
| Incomplete outcome data addressed? All outcomes |
Unclear | Information not available |
| Free of selective reporting? | Yes | OCS-treated exacerbations available for meta-analysis |
| Methods | Parallel-group, multicentre study (72 centres in 14 countries). Three groups of which 2 are considered here Jadad quality score = 5 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: 75 RANDOMISED: 495 (BDP 1000: 251; BDP 500 + Salm 100: 244) WITHDRAWALS: BDP 1000: 35; BDP500 + Salm 100: 29 AGE: mean (range): 44 (17 to 75) GENDER (% male): 52.5 SEVERITY: Moderate BASELINE % PREDICTED FEV1 mean: 73 BASELINE DOSE OF ICS : BDP 800 to 1000 or equivalent ASTHMA DURATION: Not described ATOPY (%): Not described ELIGIBILITY CRITERIA: Male and female patients at least 17 years; receiving 400 to 500 mcg bid of BDP or equivalent CRITERIA FOR RANDOMISATION FOLLOWING RUN-IN: FEV1 or mean PEF over the 7 days prior to randomisation > 50% predicted; 15% improvement in baseline FEV1 following inhaled salbutamol; either a total daytime symptom score >= 2, diurnal variation in PEF > 15% or use of rescue salbutamol >= 4 times/24 hours on 4 of the 7 days immediately prior to randomisation EXCLUSION CRITERIA: Change in asthma medication; hospitalisation for asthma or upper respiratory tract infection requiring antibiotics or a lower respiratory tract infection in the previous month; maintenance oral or parenteral corticosteroids |
|
| Interventions | LABA + ICS versus INCREASED dose of ICS OUTCOMES: Reported at 4,8,16 and 24 weeks RUN-IN PERIOD #1: 1 week for patients receiving beclomethasone 500 mcg bid; 4 weeks for patients receiving beclomethasone 400 mcg bid or other steroid equivalent RUN-IN PERIOD #2: 1 week (baseline period) DOSE OF ICS DURING RUN-IN: BDP 500 bid TREATMENTGROUP: (Salm 100 + BDP 500) salmeterol 100 mcg bid + beclomethasone 500 mcg bid CONTROL GROUP: (BDP 1000) beclomethasone 1000 mcg bid DEVICE: Metered dose inhaler NUMBER OF DEVICES: 2 COMPLIANCE: Not reported CO-TREATMENT: prn SABA. Usual doses of methylxanthines - sodium cromoglycate and inhaled anticholinergics |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF predicted; pm PEF predicted; FEV1; bronchial hyper-responsiveness (PD20) SYMPTOM SCORES: Score of 0 to 5 FUNCTIONAL STATUS: Symptom-free days; % nights with no awakenings; % rescue-free days; exacerbations (defined as any worsening of asthma symptoms requiring a change in prescribed therapy other than an increase in rescue medication); number of patients requiring hospitalisation INFLAMMATORY MARKERS: Not described ADVERSE EFFECTS: Described WITHDRAWALS: Described Primary outcome measure: Not reported |
|
| Notes | Full-text publication Funded by Glaxo Research and Development Confirmation of methodology and data confirmed User-defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | Computer-generated random numbers. See Appendix 3 |
| Allocation concealment? | Yes | Numbered coded solutions supplied by pharmacy. See Appendix 3 |
| Blinding? All outcomes |
Yes | Identical placebo devices |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The Intent-to-Treat (ITT) Population consisted of all subjects randomised to treatment and was used for the assessment of efficacy and safety.” |
| Free of selective reporting? | No | OCS-treated exacerbations not available for meta-analysis after request |
| Methods | See Woolcock 1996a | |
| Participants | See Woolcock 1996a, except for RANDOMISED: 494 (BDP500 + Salm 50: 243; BDP 1000: 251) WITHDRAWALS: BDP500 + Salm 50: 25; BDP 1000: 35) AGE: mean (range): 43 (17 to 79) GENDER (% male): 52.5 SEVERITY: Moderate BASELINE % PREDICTED FEV1 mean: 73.5 |
|
| Interventions | LABA ICS versus INCREASED dose of ICS See Woolcock 1996a, except for: TEST GROUP: (Salm 50 + BDP 500) salmeterol 50 mcg bid + beclomethasone 500 mcg bid |
|
| Outcomes | See Woolcock 1996a | |
| Notes | Full-text publication Funded by Glaxo Research and Development Confirmation of methodology and data confirmed User-defined number: 1000 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
Yes | See Woolcock 1996a |
| Incomplete outcome data addressed? All outcomes |
Unclear | See Woolcock 1996a |
| Free of selective reporting? | No | See Woolcock 1996a |
| Methods | Parallel-group, multicentre study (21 centres in China) Jadad quality score = 2 |
|
| Participants | Symptomatic asthmatic adults % ELIGIBLE OF SCREENED POPULATION: Not reported % RUN-IN PARTICIPANTS RANDOMISED: Not reported RANDOMISED: 398 (FP/SAL: 202; BUD: 169) WITHDRAWALS: FP/SAL: 20; BUD: 18 AGE: mean (range): 46 (44 to 47) GENDER (% male): 54 SEVERITY: Unclear BASELINE % PRED FEV1: Not reported BASELINE DOSE OF ICS: Not reported ASTHMA DURATION: Not reported ATOPY (%): Not reported ELIGIBILITY CRITERIA: 18 to 70 years; symptom score > 2 on 4 of last 7 days of run-in; documented reversibility to SABA-FEV1 40% to 85% predicted EXCLUSION CRITERIA: Not reported |
|
| Interventions | LABA + ICS versus INCREASED dose ICS OUTCOMES TIMING: 6 weeks RUN-IN: 2 weeks DOSE OF ICS DURING RUN-IN: Not specified (routine ICS and prn SABA for duration of run-in) INTERVENTION PERIOD: 6 weeks TEST GROUP: Combination fluticasone and salmeterol 100/50 mcg bid CONTROL GROUP: Budesonide 400 mcg bid DEVICE: FP/SAL: Accuhaler; BUD: Turbuhaler NUMBER OF DEVICES: 1 COMPLIANCE: Not assessed CO-TREATMENT: prn SABA |
|
| Outcomes | PULMONARY FUNCTION TEST: am PEF*; pm PEF; FEV1 SYMPTOM SCORES: % symptom-free days FUNCTIONAL STATUS: Not reported INFLAMMATORY MARKERS: Not reported ADVERSE EFFECTS: Reported WITHDRAWALS: Reported by treatment group Primary outcome measure* |
|
| Notes | Full unpublished data-set available from http://www.ctr.gsk.co.uk
Source of funding GSK Confirmation of methodology and data: Obtained for methods, not obtained for data User defined number: 800 |
|
| Risk of bias | ||
| Item | Authors’ judgement | Description |
| Adequate sequence generation? | Yes | See Appendix 3 |
| Allocation concealment? | Yes | See Appendix 3 |
| Blinding? All outcomes |
No | Open label study |
| Incomplete outcome data addressed? All outcomes |
Unclear | “The Intent-to-Treat (ITT) population for analysis included all the subjects who were randomised and received at least one dose of study medication, and who had no post-treatment efficacy data recorded (ITT). This population was used for statistical analysis and summaries of efficacy data.” |
| Free of selective reporting? | Unclear | Not clear whether OCS-treated exacerbations collected in the study |
ATS = American Thoracic Society
BDP = beclomethasone
bid = twice a day
BUD = budesonide
ED = emergency department
F = formoterol
FEV1 = forced expiratory volume in one second
Form = formoterol
FP = fluticasone
GSK = GlaxoSmithKline
ICS = inhaled corticosteroids
ITT = intention-to-treat
LABA = long-acting ß2 agonist
mcg = microgram
qd = four times a day
RTI = respiratory tract infection
SABA = short-acting ß2 agonist
SAL = salmeterol
Salm = salmeterol
SL = salmeterol
URTI = upper respiratory tract infection
vs = versus
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aalbers 2004 | No group with inhaled corticosteroids alone |
| Adinoff 1998 | No consistent use of inhaled corticosteroids in either the intervention or control groups - co-intervention with other non-steroidal anti-asthmatic drugs not stable during the intervention period |
| AkpinarLi 1999 | LABA added to same dose of ICS |
| Ankerst 2003 | Cross-over study of inadequate duration |
| Anonymous 1999 | Wrong type of beta-agonist |
| Anonymous a 2003 | Control intervention not ICS alone |
| Anonymous b 2003 | Review article |
| Anonymous c 2003 | Description of SMART trial |
| Arvidsson 1991 | Control intervention not inhaled glucocorticoids alone |
| Aubier 1999 | The treatment and intervention groups compared the same classes of medications either in combination or with different delivery devices |
| Aziz 1998 | Inadequate duration |
| Aziz 1999a | Intervention duration < 30 days |
| Aziz 1999b | Outcome measure did not reflect asthma control |
| Aziz 2000 | Duration of intervention < 30 days |
| Bacci 2002 | No consistent co-intervention with ICS |
| Baki 1998 | No consistent intervention with ICS |
| Balachandran 2001 | Review article |
| Balzano 2002 | Review article |
| Bateman 1998 | Intervention and control groups compared the same medications either in combination or with different delivery devices |
| Bateman 2001 | Both the treatment and intervention groups compared ICS and LAB2 agonists, using different propellants (FP/SAL delivered as HFA MDI, FP as CFC Diskus) |
| Baumgarten 2002 | Non-randomised before and after study |
| Beckett 2003 | Mixed population at baseline |
| Beeh 2002 | Not randomised |
| Behling 1999 | Inadequate duration |
| Bennett 2002 | Review article |
| Bensch 2002 | ICS in control groups not increased |
| Berggren 2001 | Intervention not regular but prn inhaled long-acting beta2-agonists |
| Berlinski 2001 | Assessment of different inhaler devices |
| Bernstein 2002 | Not randomised |
| Bessmertny 2002 | Intervention not LAB2 agonists |
| Bijl-Hofland 2001 | No consistent co -treatment with ICS |
| Bjermer 2000 | Control intervention not inhaled glucocorticoids alone but montelukast |
| Boonsawat 2003 | Outcome measures not asthma control |
| Booth 1993 | No consistent co-intervention with ICS |
| Boulet 1998 | No prior ICS exposure |
| Boyd 1995 | Addition of LABA to ICS compared to same dose ICS |
| Brambilla 1994 | Control intevention not ICS but rather slow-release oral beta2-agonist |
| Braunstein 2002 | Review article |
| Brenner 1988 | Intervention not regular inhaled long-acting beta2-agonists. Control intervention not ICS alone |
| Britton 1992 | No group with inhaled corticosteroids alone (control is regular SAB2). No consistent intervention with inhaled glucocorticoids in all subjects |
| Britton 1998 | The treatment and intervention groups compared the same classes of medications either in combination or with different delivery devices |
| Brogden 1991 | Not randomised |
| Buchvald 2003 | No group receiving ICS alone |
| Buhl 2003a | Addition of LABA to ICS compared to same dose ICS |
| Buhl 2003b | No regular LABA |
| Buhl 2003c | Addition of LABA to ICS compared to same dose ICS |
| Busse 1999 | Control intervention not inhaled glucocorticoids alone |
| Byrnes 2000 | Control intervention not inhaled glucocorticoids alone |
| Calhoun 2001 | Control intervention is not ICS (but rather anti-leukotrienes) |
| Calverley 2002 | Not asthma |
| Castle 1993 | Not randomised |
| Cazzola 2000 | Not asthma |
| Chalmers 1999 | Inadequate duration |
| Chan 2001 | I ntervention not regular inhaled long -acting beta2- agonist |
| Chapman 1999 | Tx and Intervention compared LAB2 and ICS but in combined vs concurrent devices |
| Cheer 2003 | Review article |
| Chuchalin 2002 | Addition of LABA to ICS compared to same dose ICS |
| Chuchalin 2008 | Steroid naive patients |
| Cloosterman 2001 | No consistent co-intervention with ICS Control intervention is not ICS alone (but rather regular short-acting beta2-agonist) |
| Condemi 2001 | Control intervention not ICS alone (but rather another LAB2) |
| Creticos 1999 | Addition of LABA to ICS compared to same dose ICS |
| Crompton 1999 | Control intervention not ICS alone but oral bambuterol |
| Currie 2003a | Inadequate duration |
| Currie 2003b | Co -intervention with non -permitted treatment |
| Currie 2003c | Assessment of anti-leukotriene agent in asthma |
| D’Alonzo 1994 | No consistent co-intervention with ICS - approximately 1/4 of participants were taking regular inhaled corticosteroids at baseline. Control intervention was a short-acting beta2 agonist |
| D’Urzo 2001 | Addition of LABA to ICS compared to same dose ICS |
| Dahl 1989 | Intervention not i nhaled LAB2 |
| Dahl 1991 | No consistent co-treatment with ICS |
| Dal Negro 2001a | Not randomised |
| Dal Negro 2001b | The treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Dal Negro 2002 | Not randomised |
| Davis 2001 | Not randomised |
| Dekhuijzen 2002 | Review article on anti-leukotriene agent |
| Del Rio Navarro 2001a | Outcome measures do not reflect asthma control (but rather serum potassium, CPK-MB and ECG) |
| Del Rio Navarro 2001b | Outcome measures do not reflect asthma control (but rather saliva flow and IgA) |
| Dente 2001 | Not randomised |
| Di Franco 1999 | Addition of LABA to ICS compared to same dose ICS |
| Dicpinigaitis 2002 | Intervention not regular inhaled long- acting beta2 -agonist |
| Didier 1997 | Control intervention is not ICS: this is a randomised, open, parallel-group, multicentre study comparing salmeterol with an oral bronchodilator, terbutaline |
| Dorinsky 2001 | Not randomised |
| Dorinsky 2002 | ICS given at same dose in both groups |
| Durham 1999 | Review article |
| Ek 2000 | Healthy volunteers |
| Eliraz 2001a | Inadequate duration |
| Eliraz 2001b | LABA compared with different inhaler devices |
| Eliraz 2002 | Not randomised |
| Ericsson 2001 | Not randomised |
| Everden 2002 | The treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Faurschou 1994 | Duration < 30 days |
| Faurschou 1996 | Control intervention not ICS alone (but regular SAB2) |
| Fish 2001 | Control intervention is not ICS (but rather anti-leukotrienes) |
| Fitzgerald 1999 | Addition of LABA to ICS compared to same dose ICS |
| Fitzpatrick 1990 | Duration of intervention < 30 days: the treatment period was only 2 weeks. No consistent intervention with ICS in all patients: 19/20 participants were taking regular ICS and 6 were taking oral steroids at baseline. Both treatment groups received different doses of long-acting beta2-agonists |
| Fuglsang 1995 | Duration < 30 days |
| Garcia-Marcos 2003 | Review article |
| Gardiner 1994 | Addition of LABA to ICS compared to same dose ICS |
| Gessner 2003 | Before and after study |
| Giannini 1996 | Inadequate duration |
| Giannini 1998 | Inadequate duration |
| Giannini 1999 | Duration < 30 days |
| Giannini 2000 | Duration < 30 days |
| Giannini 2001 | Inadequate duration |
| Giannini 2002 | No consistent intervention with inhaled glucocorticoids in all subjects |
| Gizycki 2000 | No consistent intervention with inhaled glucocorticoids in all subjects |
| GOAL | Assessment of combination therapy against same dose ICS |
| Gold 2001 | Control intervention not inhaled glucocorticoids alone |
| Grootendorst 2001 | Before and after study |
| Grutters 1999 | Addition of LABA to ICS compared to same dose ICS |
| Gustafsson 1994 | Tx and intervention compared ICS + LAB2 combination therapy using 2 different devices |
| Hacki 2001 | Review article |
| Hasani 2003 | No consistent intervention with inhaled glucocorticoids in all subjects |
| Heyneman 2002 | Review article |
| Hultquist 2000 | Addition of LABA to ICS compared to same dose ICS |
| Ind 2002 | No ICS alone |
| Isabelle 2001 | Not randomised |
| Jarvis 1999 | Review article |
| Jeffery 2002 | Control intervention not inhaled glucocortocoids alone |
| Jenkins 2002a | The treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Jenkins 2002b | The treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Johansson 1999 | Same dose ICS given to both treatment groups |
| Jones 1994 | No consistent intervention with ICS - < 1/3 of participants were taking regular ICS at entry |
| Juniper 1995 | No consistent co-intervention with ICS - 80% were taking regular ICS at entry. No subgroup analyses available |
| Juniper 1999 | Duplicate of Pauwel’s study (NEJM 1997;337:1405-11) |
| Kalra 1996 | Duration < 30 days |
| Kardos 2001 | Tx and intervention compared ICS + LAB2 in a fixed versus flexible schedule |
| Kavuru 2000 | Addition of LABA to ICS compared to same dose ICS |
| Keating 2002 | Review article |
| Keith 2001 | Combination versus combination |
| Kemp 1984 | Comparison of beta-agonist with theophylline |
| Kemp 1998 | Addition of LABA to ICS compared to same dose ICS |
| Ketchell 2002 | Duration of intervention < 30 days |
| Kidney 1995 | No consistent intervention with inhaled glucocorticoids in all subjects |
| Kirby 2000 | Subjects not asthmatics |
| Knobil 2000 | Control intervention not inhaled glucocorticoids alone |
| Knorr 2001 | Intervention is not LAB2 (but rather an anti-leukotriene agent: montelukast) |
| Kopp 2002 | Review article |
| Kraft 2003 | No consistent co-treatment with ICS |
| Kuna 2002 | Review article |
| LaForce 1994 | Not randomised |
| Lai 1995 | Control intervention was not ICS alone but regular short-acting beta2-agonist instead of placebo Duration of intervention < 30 day: the treatment period was only 2 weeks long Co-intervention with non-permitted drugs: oral steroids |
| Lange 2001 | Inadequate duration |
| Langton Hewer 1995 | Addition of LABA to ICS compared to same dose ICS |
| Lazarus 2001 | No consistent co-intervention with ICS - intervention is monotherapy with LAB2 |
| Leblanc 1996 | Addition of LABA to ICS compared to same dose ICS |
| Lemanske 2001 | Complicated protocol. No data provided for comparison groups of interest |
| Lenney 1995 | Not randomised |
| LHSRG 2000 | Subjects have COPD |
| Lindqvist 2001 | No consistent co- treatment with ICS |
| Lipworth 1998 | Inadequate duration |
| Lipworth 1999a | Not randomised |
| Lipworth 1999b | Inadequate duration |
| Lipworth 2000 a | Inadequate duration |
| Lipworth 2000 b | Inadequate duration |
| Lipworth 2002 | Correspondence |
| Lockey 1999 | No consistent co-intervention with inhaled corticosteroids |
| Lowhagen 2002 | Intervention not regular inhaled long-acting beta2-agonists |
| Lucioni 2002 | Economic evaluation |
| Lötvall 2002 | Comparison of the onset of different combination therapies |
| Magadle 2001 | Duration < 30 days |
| Malmqvist-Granlund 2000 | Not randomised |
| Malolepszy 2002 | Control intervention not ICS (but oral theophylline) |
| McCarthy 2000 | Control intervention not inhaled glucocorticoids alone |
| McCarthy 2002 | Not randomised |
| Mcivor 1998 | No consistent co-treatment with a stable dose of ICS (tapering) |
| Meier 1997 | Open cohort study |
| Meijer 1995 | Addition of LABA to ICS compared to same dose ICS |
| Michel 2000 | Duration < 30 days |
| Midgren 1992 | Control intervention not ICS alone |
| Miraglia del Giudice | No prior ICS exposure |
| Molimard 2001 | Addition of LABA to ICS compared to same dose ICS |
| Murray 1998 | No consistent intervention with inhaled glucocorticoids in all subjects |
| Nagel 2002 | Duplicate |
| Nathan 1998 | Comparison of salmeterol and beclomethasone |
| Nathan 2001 | Same dose of ICS given to both groups |
| Nelson 1999 | Not randomised |
| Nelson 2000 | No prior ICS exposure |
| Nelson 2001 | Control intervention ICS alone (but LTRA - zafirlukast) |
| Nelson 2003 | Addition of LABA to ICS compared to same dose ICS |
| Newnham 1995 | No consistent co-treatment with ICS |
| Nielsen 1999 | Not randomised |
| Nightingale 2002 | Treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Norhaya 1999 | Addition of LABA to ICS compared to same dose ICS |
| Nsouli 2001 | Control intervention not inhaled glucocorticoids alone |
| O’Brian 2001 | Duration of intervention < 30 days |
| O’Connor 2002 | Retrospective study |
| Orsida 2001 | Control population did not have asthma |
| Palmer 1992 | Control intervention is not ICS alone: both treatment groups received long-acting beta2-agonists but in different doses |
| Palmqvist 2001 | Both the treament and control groups compared ICS and LAB2 with different drugs and inhaler devices |
| Paterson 1999 | Treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Pauwels 1998 | Intervention not LAB2 but another ICS |
| Pearlman 1992 | No consistent co-intervention with ICS - < 1/2 the participants were taking regular inhaled corticosteroids at entry Control intervention was not ICS but short-acting beta2-agonist |
| Pearlman 1994 | No consistent co-treatment with ICS 26% |
| Pearlman 2001 | Not randomised |
| Pearlman 2002 | Control intervention is not ICS alone (but anti-leukotriene montelukast as maintenance) |
| Perez 2000 | Overview of antileukotriene agent |
| Peters 2000 | Control intervention is not ICS alone (but oral steroids, SAB2 and anticholinergics- in hospital setting) |
| Pifferi 2002 | Before and after study |
| Pinnas 1998 | No consistent intervention with inhaled glucocorticoids in all subjects |
| Pizzichini 1996 | Duration < 30 days |
| Pljaskic-Kamenov 2000 | Cannot determine prior ICS exposure |
| Pohl 2006 | Adjustable dosing regimens |
| Pohunek 2006 | Similar dose ICS |
| Price 2002 | Addition of LABA to ICS compared to same dose ICS |
| Pujet 1995 | Intervention is not LAB2 (but theophylline) |
| Pyke 2001 | Comparison of LABA and ICS in separate versus combination devices |
| Rance 2002 | Unable to determine eligibility from abstract details |
| Remington 2002 | Review article |
| Rickard 1999 | Outcomes measures did not reflect asthma control |
| Rickard 2001 | Control intervention not inhaled glucocorticoids alone |
| Rijssenbeek-Nouwens | Intervention is not LAB2 (but anti-allergic casing) |
| Ringbaek 1996 | Control intervention not ICS alone but oral SAB2 as maintenance |
| Ringdal 1997 | Not randomised |
| Ringdal 2002 | Comparison of combination ICS and LABA against separately administered ICS and LABA |
| Robert 2002 | Control group did not receive increase in ICS dose |
| Rocca-Serra 2002 | Intervention not regular long -acting beta2 -agonist |
| Rosenhall 2002 | Treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Rosenhall 2003 | Treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Rosenthal 1999 | No consistent co-intervention with ICS |
| Roth 2002 | In vitro study |
| Russell 1995 | Addition of LABA to ICS compared to same dose ICS |
| Saari 2002 | Before and after study |
| SAM40034 | Steroid naive patients |
| SAM40036 | Steroid naive patients |
| SAS30015 | Comparison between combination HFA and CFC BDP |
| Schreurs 1996 | No consistent co-intervention with ICS - 90% used regular ICS at entry |
| Seares 2003 | Not randomised |
| Serrier 2003 | Treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Shapiro 2000 | Addition of LABA to ICS compared to same dose ICS |
| Shapiro 2001 | Intervention is not LAB2 |
| Sheth 2002 | Control intervention not inhaled glucocorticoids alone |
| Sienra-Monge 2001 | The treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Simons 1997 a | Addition of LABA to ICS compared to same dose ICS |
| Simons 1997 b | No consistent co-intervention with inhaled corticosteroids. Treatment groups compared ICS to longacting beta2-agonist alone |
| Sorkness 2007 | Steroid naive patients |
| Sovani 2008 | Comparison of combination therapy with best practice |
| Staehr 1995 | Control intervention not ICS (but SAB2 maintenance) |
| Stanford 2002 | Outcomes measures did not reflect asthma control |
| Stelmach 2002a | No co-intervention with ICS |
| Stelmach 2002b | No co-intervention with ICS |
| Stempel 2002 | Non-randomised economic analysis |
| Stoloff 2002 | Not randomised |
| Strand 2003 | Sreroid naive patients |
| Tal 2003 | Addition of LABA to ICS compared to same dose ICS |
| Tan 1997 | Outcomes measures did not reflect asthma control |
| Tattersfield 2001 | Intervention is not daily LAB2 (but rather on-demand LAB2) |
| Thomson 2003 | Assessment of anti-leukotriene agents |
| Tonelli 2001 | No consistent intervention with inhaled glucocorticoids in all subjects |
| Trautmann 2001 | Not randomised |
| Turner 1998 | No consistent co-intervention with ICS |
| Ullman 1990 | Duration < 30 days |
| Vagaggini 1999 | Asthma patients with different severities compared |
| Van Asperen 2002 | Position statament on use of ICS |
| Van den Berg 2000 | No consistent co-intervention with LAB2-both groups received LAB2 but compared delivery devices |
| Van der Molen 1997a | Addition of LABA to ICS compared to same dose ICS |
| Van der Woude 2001 | The treatment and intervention groups compared the same medications either in combination or with different delivery devices |
| Van Noord 2001 | Both the treament and control groups compared ICS and LAB2 with different inhaler devices |
| Verberne 1997 | No consistent co-intervention with ICS - approximately 20% were taking regular ICS at entry |
| Vestbo 2000 | Patients are not asthmatics (but rather have COPD) |
| Vickers 2000 | The intervention is not LAB2 but placebo No consistent co-intervention with ICS Ongoing study - protocol only published |
| Vilsvik 2001 | Outcome measures did not reflect asthma control |
| Von Berg 1989 | Duration < 30 days |
| Wallaert 1999 | Control intervention not ICS alone (but another LAB2) |
| Wallin 1990 | Control intervention not ICS alone (but regular SAB2) |
| Wallin 2002 | Comparison of ICS with LABA |
| Warner 2001 | Review article of anti-leukotriene agents |
| Weersink 1997 | Addition of LABA to ICS compared to same dose ICS |
| Weinstein 1998 | No consistent co-intervention with ICS - only 57% were on ICS |
| Weinstein 2001 | Not randomised |
| Wempe 1992 | No consistent co-treatment with ICS |
| Wilcke 1998 | Duration < 30 days |
| Wilding 1997 | Not randomised |
| Wilson 2001a | Control intervention is not ICS alone (but rather ICS with an anti-leukotriene agent - montelukast) |
| Wilson 2001b | Not randomised |
| Wong 1992 | Duration < 30 days |
| Woolcock 1995 | Not randomised |
| Wooltorton 2003 | Correspondence |
| Yancey 1997 | Comparison of LABA with theophylline |
| Yates 1995 | Duration < 30 days. No co-treatment with ICS. |
| Yates 1996 | Duration < 30 days |
| Youngchaiyud 1995 | Intervention not LAB2 (but theophylline) |
| Yurdakul 2002 | Control intervention not regular inhaled long -acting beta2 -agonists alone |
| Zarkovic 1998 | No consistent co-intervention with ICS Control intervention is placebo |
| Zetterstrom 2001 | Addition of LABA to ICS compared to same dose ICS |
| Zhong 2002 | Concomitant delivery versus combined delivery of ICS and LABA |
| Zimmerman 2004 | Addition of LABA to ICS compared to same dose ICS |
BDP = beclomethasone
COPD = chronic obstructive pulmonary disease
FEV1 = forced expiratory volume in one second
FP = fluticasone
ICS = inhaled corticosteroids
LABA = long-acting ß2 agonist
LTRA = leukotriene receptor agonist
SAB2 = short-acting ß2 agonist
SAL = salmeterol
DATA AND ANALYSES
Comparison 1.
LABA + ICS versus higher dose ICS
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 # patients with exacerbations requiring oral steroids | 25 | 9833 | Risk Ratio (M-H, Fixed, 95% CI) | 0.88 [0.78, 0.98] |
| 1.1 Baseline FEV1 >= 80 % predicted | 11 | 4755 | Risk Ratio (M-H, Fixed, 95% CI) | 0.97 [0.83, 1.13] |
| 1.2 Baseline FEV1 61-79 % predicted | 12 | 4106 | Risk Ratio (M-H, Fixed, 95% CI) | 0.81 [0.68, 0.95] |
| 1.3 Baseline FEV1 <60% predicted | 1 | 489 | Risk Ratio (M-H, Fixed, 95% CI) | 0.62 [0.36, 1.05] |
| 1.4 Baseline FEV1 unclear | 1 | 483 | Risk Ratio (M-H, Fixed, 95% CI) | 1.33 [0.30, 5.87] |
| 2 # patients with exacerbations requiring hospitalisation | 33 | 12573 | Risk Ratio (M-H, Fixed, 95% CI) | 1.02 [0.67, 1.56] |
| 2.1 Baseline FEV1 >= 80 % predicted | 8 | 2721 | Risk Ratio (M-H, Fixed, 95% CI) | 3.04 [0.48, 19.15] |
| 2.2 Baseline FEV1 61-79 % predicted | 20 | 8266 | Risk Ratio (M-H, Fixed, 95% CI) | 1.00 [0.63, 1.57] |
| 2.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 0.98 [0.06, 15.64] |
| 2.4 Baseline FEV1 unclear | 4 | 1098 | Risk Ratio (M-H, Fixed, 95% CI) | 0.33 [0.03, 3.18] |
| 3 # withdrawals due to poor asthma control or exacerbation | 29 | 10923 | Risk Ratio (M-H, Fixed, 95% CI) | 0.71 [0.56, 0.91] |
| 3.1 Baseline FEV1 >= 80 % predicted | 9 | 2443 | Risk Ratio (M-H, Fixed, 95% CI) | 0.65 [0.45, 0.93] |
| 3.2 Baseline FEV1 61-79 % predicted | 17 | 7111 | Risk Ratio (M-H, Fixed, 95% CI) | 0.81 [0.58, 1.12] |
| 3.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 0.14 [0.01, 2.71] |
| 3.4 Baseline FEV1 predicted not reported | 2 | 881 | Risk Ratio (M-H, Fixed, 95% CI) | 0.33 [0.01, 8.11] |
| 4 Total # withdrawals | 39 | 13654 | Risk Ratio (M-H, Fixed, 95% CI) | 0.92 [0.84, 1.00] |
| 4.1 Baseline FEV1 >= 80 % predicted | 9 | 2799 | Risk Ratio (M-H, Fixed, 95% CI) | 0.76 [0.61, 0.95] |
| 4.2 Baseline FEV1 61-79 % predicted | 23 | 8851 | Risk Ratio (M-H, Fixed, 95% CI) | 0.95 [0.86, 1.05] |
| 4.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 0.87 [0.56, 1.37] |
| 4.4 Baseline FEV1 predicted not reported | 6 | 1516 | Risk Ratio (M-H, Fixed, 95% CI) | 0.99 [0.73, 1.34] |
| 5 # withdrawals due to adverse events | 30 | 10017 | Risk Ratio (M-H, Fixed, 95% CI) | 0.99 [0.78, 1.26] |
| 5.1 Baseline FEV1 >= 80 % predicted | 9 | 2799 | Risk Ratio (M-H, Fixed, 95% CI) | 0.92 [0.48, 1.76] |
| 5.2 Baseline FEV1 61-79 % predicted | 18 | 6095 | Risk Ratio (M-H, Fixed, 95% CI) | 0.95 [0.72, 1.25] |
| 5.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 1.18 [0.37, 3.82] |
| 5.4 Baseline FEV1 predicted not reported | 2 | 635 | Risk Ratio (M-H, Fixed, 95% CI) | 2.35 [0.68, 8.08] |
| 6 FEV1 at endpoint | 11 | 2841 | L (Fixed, 95% CI) | 0.08 [0.03, 0.13] |
| 6.1 Baseline FEV1 >= 80 % predicted | 0 | 0 | L (Fixed, 95% CI) | Not estimable |
| 6.2 Baseline FEV1 61-79 % predicted | 10 | 2841 | L (Fixed, 95% CI) | 0.09 [0.03, 0.14] |
| 6.3 Baseline FEV1 <= 60 % predicted | 0 | 0 | L (Fixed, 95% CI) | Not estimable |
| 6.4 Baseline FEV1 not reported | 1 | 0 | L (Fixed, 95% CI) | −0.14 [−0.50, 0.22] |
| 7 FEV1 (predicted) at endpoint | 7 | Mean Difference (Fixed, 95% CI) | 1.78 [0.39, 3.18] | |
| 7.1 Baseline FEV1 >= 80 % predicted | 2 | Mean Difference (Fixed, 95% CI) | 4.46 [1.38, 7.53] | |
| 7.2 Baseline FEV1 61-79 % predicted | 5 | Mean Difference (Fixed, 95% CI) | 1.10 [−0.46, 2.66] | |
| 8 Change in FEV1 at endpoint | 22 | 8888 | L (Fixed, 95% CI) | 0.08 [0.06, 0.09] |
| 8.1 Baseline FEV1 >= 80 % predicted | 4 | 1798 | L (Fixed, 95% CI) | 0.07 [0.05, 0.10] |
| 8.2 Baseline FEV1 61-79 % predicted | 14 | 5874 | L (Fixed, 95% CI) | 0.09 [0.06, 0.11] |
| 8.3 Baseline FEV1 <= 60 % predicted | 1 | 478 | L (Fixed, 95% CI) | 0.01 [−0.07, 0.09] |
| 8.4 Baseline FEV1 not reported | 3 | 738 | L (Fixed, 95% CI) | 0.05 [−0.00, 0.11] |
| 9 Change in FEV1 stratifying on treatment period | 19 | L (Fixed, 95% CI) | 0.09 [0.08, 0.11] | |
| 9.1 At 6 +/− 2 weeks | 5 | L (Fixed, 95% CI) | 0.09 [0.05, 0.13] | |
| 9.2 At 12 +/− 4 weeks | 10 | L (Fixed, 95% CI) | 0.10 [0.08, 0.12] | |
| 9.3 At 24 +/− 4 weeks | 8 | L (Fixed, 95% CI) | 0.09 [0.06, 0.12] | |
| 9.4 At 52 +/− 4 weeks | 2 | L (Fixed, 95% CI) | 0.07 [0.03, 0.12] | |
| 10 Change in FEV1 (predicted) at endpoint | 2 | % (Fixed, 95% CI) | 0.35 [−0.18, 0.87] | |
| 10.1 Baseline FEV1 >= 80 % predicted | 1 | % (Fixed, 95% CI) | 0.28 [−0.25, 0.81] | |
| 10.2 Baseline FEV1 61-79 % predicted | 1 | % (Fixed, 95% CI) | 3.9 [−0.01, 7.81] | |
| 11 Morning PEF at endpoint | 14 | 2938 | L/min (Random, 95% CI) | 23.31 [18.09, 28.52] |
| 11.1 Baseline FEV1 >= 80 % predicted | 2 | 77 | L/min (Random, 95% CI) | 26.43 [−11.11, 63.97] |
| 11.2 Baseline FEV1 61-79 % predicted | 12 | 2861 | L/min (Random, 95% CI) | 23.86 [17.94, 29.77] |
| 11.3 Baseline FEV1 <=60% predicted | 0 | 0 | L/min (Random, 95% CI) | Not estimable |
| 12 Change in morning or clinic PEF at endpoint | 30 | 11143 | L/min (Random, 95% CI) | 16.30 [13.48, 19.11] |
| 12.1 Baseline FEV1 >= 80 % predicted | 7 | 2314 | L/min (Random, 95% CI) | 11.74 [8.47, 15.00] |
| 12.2 Baseline FEV1 61-79 % predicted | 17 | 6788 | L/min (Random, 95% CI) | 18.64 [13.93, 23.34] |
| 12.3 Baseline FEV1 <=60% pedicted | 1 | 478 | L/min (Random, 95% CI) | 13.70 [4.13, 23.27] |
| 12.4 Baseline FEV1 not reported | 5 | 1563 | L/min (Random, 95% CI) | 16.30 [9.03, 23.56] |
| 13 Morning PEF (% predicted) at endpoint | 5 | 1646 | Mean Difference (IV, Random, 95% CI) | 3.45 [1.28, 5.63] |
| 13.1 Baseline FEV1 >=80% predicted | 4 | 1299 | Mean Difference (IV, Random, 95% CI) | 3.86 [1.37, 6.35] |
| 13.2 Baseline FEV1 61-79% of predicted | 1 | 347 | Mean Difference (IV, Random, 95% CI) | 1.0 [−4.68, 6.68] |
| 14 Evening PEF at endpoint | 4 | L/min (Fixed, 95% CI) | 16.79 [10.72, 22.85] | |
| 14.1 Baseline FEV1 >=80% predicted | 1 | L/min (Fixed, 95% CI) | 4.0 [−37.59, 45.59] | |
| 14.2 Baseline FEV1 61-79% of predicted | 3 | L/min (Fixed, 95% CI) | 17.07 [10.93, 23.20] | |
| 14.3 Baseline FEV1 <= 60 % predicted | 0 | L/min (Fixed, 95% CI) | Not estimable | |
| 15 Change in morning PEF (predicted) | 0 | % (Random, 95% CI) | Not estimable | |
| 15.1 Baseline FEV1 >= 80 % predicted | 0 | % (Random, 95% CI) | Not estimable | |
| 15.2 Baseline FEV1 61-79 % predicted | 0 | % (Random, 95% CI) | Not estimable | |
| 15.3 Baseline FEV1 <=60% predicted | 0 | % (Random, 95% CI) | Not estimable | |
| 15.4 Baseline FEV1 not reported | 0 | % (Random, 95% CI) | Not estimable | |
| 16 Change in evening PEF at endpoint | 22 | 8544 | L/min (Random, 95% CI) | 13.70 [10.28, 17.12] |
| 16.1 Baseline FEV1 >=80% predicted | 6 | 2737 | L/min (Random, 95% CI) | 12.01 [7.99, 16.02] |
| 16.2 Baseline FEV1 61-79% of predicted | 11 | 4332 | L/min (Random, 95% CI) | 15.05 [8.98, 21.12] |
| 16.3 Baseline FEV1 <=60% predicted | 1 | 478 | L/min (Random, 95% CI) | 14.5 [5.47, 23.53] |
| 16.4 Baseline FEV1 not reported | 4 | 997 | L/min (Random, 95% CI) | 11.31 [3.85, 18.78] |
| 17 Change in evening PEF predicted | 0 | % (Random, 95% CI) | Totals not selected | |
| 17.1 Baseline FEV1 >=80% predicted | 0 | % (Random, 95% CI) | Not estimable | |
| 17.2 Baseline FEV1 61-79% of predicted | 0 | % (Random, 95% CI) | Not estimable | |
| 17.3 Baseline FEV1 not reported | 0 | % (Random, 95% CI) | Not estimable | |
| 18 PEF variability at endpoint | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 18.1 Baseline FEV1 61-79 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 19 Change in PEF variability at endpoint | 7 | 2353 | Mean Difference (IV, Fixed, 95% CI) | −4.55 [−6.32, −2.78] |
| 19.1 Baseline FEV1 >= 80 % predicted | 1 | 232 | Mean Difference (IV, Fixed, 95% CI) | −5.4 [−7.83, −2.97] |
| 19.2 Baseline FEV1 61-79 % predicted | 4 | 1245 | Mean Difference (IV, Fixed, 95% CI) | −4.66 [−7.95, −1.36] |
| 19.3 Baseline FEV1 <= 60 % predicted | 2 | 876 | Mean Difference (IV, Fixed, 95% CI) | −1.90 [−6.05, 2.26] |
| 20 Change in daytime symptom score at endpoint | 5 | 1965 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.26 [−0.35, −0.17] |
| 20.1 Baseline FEV1 >= 80 % predicted | 1 | 225 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.14 [−0.40, 0.13] |
| 20.2 Baseline FEV1 61-79 % predicted | 4 | 1740 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.27 [−0.37, −0.18] |
| 20.3 Baseline FEV1 <= 60 % predicted | 0 | 0 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 21 Change in overall (24 hrs) symptom score at endpoint | 6 | 2279 | Std. Mean Difference (IV, Random, 95% CI) | −0.23 [−0.37, −0.08] |
| 21.1 Baseline FEV1 >= 80 % predicted | 1 | 558 | Std. Mean Difference (IV, Random, 95% CI) | −0.12 [−0.29, 0.05] |
| 21.2 Baseline FEV1 61-79 % predicted | 4 | 1243 | Std. Mean Difference (IV, Random, 95% CI) | −0.27 [−0.52, −0.03] |
| 21.3 Baseline FEV1 % <= 60% | 1 | 478 | Std. Mean Difference (IV, Random, 95% CI) | −0.26 [−0.44, −0.08] |
| 22 Change in % symptom-free days at endpoint | 12 | 6039 | % (Random, 95% CI) | 9.18 [6.02, 12.33] |
| 22.1 Baseline FEV1 >=80% predicted | 3 | 1646 | % (Random, 95% CI) | 5.67 [2.87, 8.46] |
| 22.2 Baseline FEV1 61-79% of predicted | 8 | 3925 | % (Random, 95% CI) | 12.32 [8.44, 16.21] |
| 22.3 Baseline FEV1 <=60% predicted | 0 | 0 | % (Random, 95% CI) | Not estimable |
| 22.4 Baseline FEV1 % predicted not reported | 1 | 468 | % (Random, 95% CI) | 1.9 [−1.18, 4.98] |
| 23 % symptom-free days at endpoint | 8 | 3901 | Mean Difference (IV, Random, 95% CI) | 5.81 [−1.14, 12.76] |
| 23.1 Baseline FEV1 >= 80 % predicted | 2 | 555 | Mean Difference (IV, Random, 95% CI) | −2.38 [−6.92, 2.17] |
| 23.2 Baseline FEV1 61-79 % predicted | 5 | 2960 | Mean Difference (IV, Random, 95% CI) | 6.58 [−1.73, 14.90] |
| 23.3 Baseline FEV1 % predicted not reported | 1 | 386 | Mean Difference (IV, Random, 95% CI) | 18.80 [9.64, 27.96] |
| 24 Daytime symptom score at endpoint | 5 | 2465 | Std. Mean Difference (IV, Random, 95% CI) | −0.28 [−0.67, 0.11] |
| 24.1 Baseline FEV1 >= 80 % predicted | 1 | 48 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [−0.45, 0.69] |
| 24.2 Baseline FEV1 61-79 % predicted | 4 | 2417 | Std. Mean Difference (IV, Random, 95% CI) | −0.38 [−0.84, 0.07] |
| 25 Nighttime symptom score at endpoint | 3 | 2082 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.24 [−0.49, 0.01] |
| 25.1 Baseline FEV1 >= 80% predicted | 1 | 48 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.16 [−0.73, 0.41] |
| 25.2 Baseline FEV1 61-79 % predicted | 2 | 2034 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.26 [−0.54, 0.02] |
| 26 Change in nighttime symptom score at endpoint | 2 | 710 | Mean Difference (IV, Fixed, 95% CI) | −0.01 [−0.04, 0.01] |
| 26.1 Baseline FEV1 61-79 % predicted | 1 | 484 | Mean Difference (IV, Fixed, 95% CI) | −0.01 [−0.04, 0.02] |
| 26.2 Baseline FEV1 >= 80 % predicted | 1 | 226 | Mean Difference (IV, Fixed, 95% CI) | −0.08 [−0.19, 0.03] |
| 27 % symptom-free nights at endpoint | 2 | 580 | Mean Difference (IV, Fixed, 95% CI) | −2.10 [−7.98, 3.79] |
| 27.1 Baseline FEV1 >= 80 % predicted | 1 | 231 | Mean Difference (IV, Fixed, 95% CI) | 1.60 [−8.49, 11.69] |
| 27.2 Baseline FEV1 61-79 % predicted | 1 | 349 | Mean Difference (IV, Fixed, 95% CI) | −4.0 [−11.24, 3.24] |
| 28 Change in night time awakenings ( number of nights) at endpoint | 7 | 3172 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.03 [−0.10, 0.04] |
| 28.1 Baseline FEV1 >= 80 % predicted | 1 | 558 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [−0.13, 0.20] |
| 28.2 Baseline FEV1 61-79 % predicted | 4 | 167 | Std. Mean Difference (IV, Fixed, 95% CI) | −0.07 [−0.16, 0.03] |
| 28.3 Baseline FEV1 <= 60 % predicted | 1 | 478 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.03 [−0.15, 0.20] |
| 28.4 Baseline FEV1 % predicted not reported | 1 | 469 | Std. Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 29 % nighttime awakenings at endpoint | 2 | 2175 | Mean Difference (IV, Fixed, 95% CI) | −0.40 [−0.55, −0.25] |
| 29.1 Baseline FEV1 61-79% predicted | 2 | 2175 | Mean Difference (IV, Fixed, 95% CI) | −0.40 [−0.55, −0.25] |
| 30 % nights with no awakenings at endpoint | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 30.1 Baseline FEV1 61-79 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 31 Change in % nights with no awakenings at endpoint | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 31.1 Baseline FEV1 61-79 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 32 Change in # daytime rescue inhalations at endpoint | 5 | 3455 | Mean Difference (IV, Random, 95% CI) | −0.48 [−0.77, −0.20] |
| 32.1 Baseline FEV1 >= 80 % predicted | 0 | 0 | Mean Difference (IV, Random, 95% CI) | Not estimable |
| 32.2 Baseline FEV1 61-79 % predicted | 5 | 3455 | Mean Difference (IV, Random, 95% CI) | −0.48 [−0.77, −0.20] |
| 32.3 Baseline FEV1 <= 60 % predicted | 0 | 0 | Mean Difference (IV, Random, 95% CI) | Not estimable |
| 33 Change in # nighttime rescue inhalations at endpoint | 4 | 2980 | Std. Mean Difference (IV, Random, 95% CI) | −0.13 [−0.21, −0.05] |
| 33.1 Baseline FEV1 61-79 % predicted | 4 | 2980 | Std. Mean Difference (IV, Random, 95% CI) | −0.13 [−0.21, −0.05] |
| 33.2 Baseline FEV1 <= 60 % predicted | 0 | 0 | Std. Mean Difference (IV, Random, 95% CI) | Not estimable |
| 34 Absolute (or %) change in # rescue inhalations (per 24 hrs) at endpoint | 12 | 4631 | Std. Mean Difference (IV, Random, 95% CI) | −0.20 [−0.29, −0.11] |
| 34.1 Baseline FEV1 >= 80% predicted | 4 | 1870 | Std. Mean Difference (IV, Random, 95% CI) | −0.14 [−0.23, −0.05] |
| 34.2 Baseline FEV1 61-79 % predicted | 6 | 1815 | Std. Mean Difference (IV, Random, 95% CI) | −0.26 [−0.35, −0.17] |
| 34.3 Baseline FEV1 <= 60 % predicted | 1 | 478 | Std. Mean Difference (IV, Random, 95% CI) | −0.42 [−0.60, −0.24] |
| 34.4 Baseline FEV1 not reported | 1 | 468 | Std. Mean Difference (IV, Random, 95% CI) | 0.12 [−0.07, 0.30] |
| 35 # daytime rescue inhalations (puffs/day) at endpoint | 5 | 544 | Mean Difference (IV, Random, 95% CI) | −0.44 [−0.94, 0.06] |
| 35.1 Baseline FEV1 >= 80 % predicted | 2 | 278 | Mean Difference (IV, Random, 95% CI) | −0.15 [−0.38, 0.07] |
| 35.2 Baseline FEV1 61-79 % predicted | 2 | 242 | Mean Difference (IV, Random, 95% CI) | −1.44 [−1.96, −0.93] |
| 35.3 Baseline FEV1 not reported | 1 | 24 | Mean Difference (IV, Random, 95% CI) | 0.04 [−0.28, 0.36] |
| 36 # nighttime rescue inhalations at endpoint (puffs/day) | 4 | 941 | Mean Difference (IV, Random, 95% CI) | −0.09 [−0.23, 0.04] |
| 36.1 Baseline FEV1 >=80% predicted | 2 | 714 | Mean Difference (IV, Random, 95% CI) | −0.04 [−0.10, 0.01] |
| 36.2 Baseline FEV1 61-79 % predicted | 1 | 203 | Mean Difference (IV, Random, 95% CI) | −0.74 [−1.13, −0.35] |
| 36.3 Baseline FEV1 not reported | 1 | 24 | Mean Difference (IV, Random, 95% CI) | Not estimable |
| 37 % overall rescue-free days at endpoint | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 37.1 Baseline FEV1 61-79 % predicted | 3 | 2516 | Mean Difference (IV, Random, 95% CI) | 5.14 [−2.79, 13.08] |
| 38 Change in % symptom-free days at endpoint | 1 | % (Random, 95% CI) | −0.24 [−1.20, 0.72] | |
| 38.1 Baseline FEV1 >= 80% predicted | 0 | % (Random, 95% CI) | Not estimable | |
| 38.2 Baseline FEV1 61% to 79% of predicted | 1 | % (Random, 95% CI) | −0.24 [−1.20, 0.72] | |
| 38.3 Baseline FEV1 <= 60% predicted | 0 | % (Random, 95% CI) | Not estimable | |
| 38.4 Baseline FEV1 % predicted not reported | 0 | % (Random, 95% CI) | Not estimable | |
| 39 Change in mean % rescue-free days at endpoint | 3 | 1332 | Mean Difference (IV, Fixed, 95% CI) | 11.48 [7.98, 14.98] |
| 39.1 Baseline FEV1 >= 80 % predicted | 1 | 558 | Mean Difference (IV, Fixed, 95% CI) | 5.40 [−0.14, 10.94] |
| 39.2 Baseline FEV1 61% to 79% predicted | 2 | 774 | Mean Difference (IV, Fixed, 95% CI) | 15.50 [10.99, 20.02] |
| 40 Change in asthma control days at endpoint (%) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 40.1 Baseline FEV1 >= 80 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 41 Change in quality of life (AQLQ score) at endpoint | 4 | 341 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [−0.06, 0.26] |
| 41.1 Baseline FEV1 61% to 79 % predicted | 3 | 323 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [−0.06, 0.26] |
| 41.2 Baseline FEV1 not reported | 1 | 18 | Mean Difference (IV, Fixed, 95% CI) | 0.18 [−0.72, 1.08] |
| 42 Change in Hyland QOL at endpoint | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 42.1 Baseline FEV1 >= 80 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 43 # Achieving good asthma control | 1 | Risk Ratio (M-H, Fixed, 95% CI) | Totals not selected | |
| 43.1 Baseline FEV1 >= 80 % predicted | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable | |
| 43.2 Baseline FEV1 61% to 79 % predicted | 1 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable | |
| 43.3 Baseline FEV1 <= 60 % predicted | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable | |
| 44 % asthma control days at endpoint | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 44.1 Baseline FEV1 61% to 79 % predicted | 2 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 45 Serum ECP( microg /L) | 2 | 87 | Mean Difference (IV, Fixed, 95% CI) | 0.62 [−2.45, 3.70] |
| 45.1 Baseline FEV1 >= 80% predicted | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | −0.70 [−4.51, 3.11] |
| 45.2 Baseline FEV1 61% to 79 % predicted | 1 | 39 | Mean Difference (IV, Fixed, 95% CI) | 3.10 [−2.11, 8.31] |
| 46 Plasma cortisol ( nmol/L) 8am at 8 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 46.1 Baseline FEV1 61% to 79 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 47 Tidal exhaled NO(ppb) | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 47.1 Baseline FEV1 61% to 79 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 48 PD20 @ 8 weeks | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 48.1 Baseline FEV1 61% to 79 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 49 PC20 | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 49.1 Baseline FEV1 not reported | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 50 Change in mean urine Cortisol/Creatinine ratio | 1 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 50.1 Baseline FEV1 61% to 79 % predicted | 1 | Mean Difference (IV, Fixed, 95% CI) | Not estimable | |
| 51 Change in PC20 | 0 | Doubl’g doses (Fixed, 95% CI) | Totals not selected | |
| 51.1 Baseline FEV1 >= 80 % predicted | 0 | Doubl’g doses (Fixed, 95% CI) | Not estimable | |
| 51.2 Baseline FEV1 61% to 79 % predicted | 0 | Doubl’g doses (Fixed, 95% CI) | Not estimable | |
| 51.3 Baseline FEV1 <= 60 % predicted | 0 | Doubl’g doses (Fixed, 95% CI) | Not estimable | |
| 51.4 Baseline FEV1 not reported | 0 | Doubl’g doses (Fixed, 95% CI) | Not estimable | |
| 52 Serious adverse events | 35 | 13640 | Risk Ratio (M-H, Fixed, 95% CI) | 1.12 [0.91, 1.37] |
| 52.1 Baseline FEV1 >= 80 % predicted | 6 | 2345 | Risk Ratio (M-H, Fixed, 95% CI) | 0.82 [0.50, 1.34] |
| 52.2 Baseline FEV1 61% to 79% predicted | 18 | 7978 | Risk Ratio (M-H, Fixed, 95% CI) | 1.23 [0.97, 1.56] |
| 52.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 1.38 [0.44, 4.28] |
| 52.4 Baseline FEV1 not reported | 10 | 2829 | Risk Ratio (M-H, Fixed, 95% CI) | 0.77 [0.35, 1.72] |
| 53 # patients with tremor | 11 | 5562 | Risk Ratio (M-H, Fixed, 95% CI) | 1.84 [1.20, 2.82] |
| 53.1 Baseline FEV1 >= 80 % predicted | 1 | 233 | Risk Ratio (M-H, Fixed, 95% CI) | 0.15 [0.01, 2.90] |
| 53.2 Baseline FEV1 61% to 79 % predicted | 9 | 4841 | Risk Ratio (M-H, Fixed, 95% CI) | 2.03 [1.29, 3.19] |
| 53.3 Baseline FEV1 <= 60% predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 1.97 [0.18, 21.56] |
| 54 # patients with oral thrush | 14 | 7727 | Risk Ratio (M-H, Random, 95% CI) | 0.58 [0.40, 0.86] |
| 54.1 Baseline FEV1 >= 80 % predicted | 3 | 1427 | Risk Ratio (M-H, Random, 95% CI) | 0.38 [0.14, 1.05] |
| 54.2 Baseline FEV1 61-79 % predicted | 9 | 5329 | Risk Ratio (M-H, Random, 95% CI) | 0.74 [0.44, 1.24] |
| 54.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Random, 95% CI) | 0.33 [0.13, 0.81] |
| 54.4 Baseline FEV1 predicted not reported | 1 | 483 | Risk Ratio (M-H, Random, 95% CI) | 0.50 [0.05, 5.45] |
| 55 Total # adverse events | 30 | 11483 | Risk Ratio (M-H, Random, 95% CI) | 0.99 [0.95, 1.03] |
| 55.1 Baseline FEV1 >= 80 % predicted | 7 | 2634 | Risk Ratio (M-H, Random, 95% CI) | 0.99 [0.90, 1.09] |
| 55.2 Baseline FEV1 61-79 % predicted | 17 | 7326 | Risk Ratio (M-H, Random, 95% CI) | 0.99 [0.93, 1.05] |
| 55.3 Baseline FEV1<=60 % predicted | 1 | 488 | Risk Ratio (M-H, Random, 95% CI) | 1.03 [0.95, 1.11] |
| 55.4 Baseline FEV1 predicted not reported | 5 | 1035 | Risk Ratio (M-H, Random, 95% CI) | 0.94 [0.83, 1.07] |
| 56 # patients with adverse cardiovascular events | 9 | 3439 | Risk Ratio (M-H, Random, 95% CI) | 0.99 [0.49, 2.01] |
| 56.1 Baseline FEV1 >= 80 % predicted | 1 | 233 | Risk Ratio (M-H, Random, 95% CI) | 0.27 [0.03, 2.34] |
| 56.2 Baseline FEV1 61% to 79 % predicted | 7 | 2718 | Risk Ratio (M-H, Random, 95% CI) | 1.04 [0.47, 2.29] |
| 56.3 Baseline FEV1 <= 60% predicted | 1 | 488 | Risk Ratio (M-H, Random, 95% CI) | 2.95 [0.31, 28.17] |
| 57 # patients with headache | 25 | 10824 | Risk Ratio (M-H, Fixed, 95% CI) | 1.02 [0.92, 1.12] |
| 57.1 Baseline FEV1 >= 80 % predicted | 6 | 2179 | Risk Ratio (M-H, Fixed, 95% CI) | 1.11 [0.96, 1.28] |
| 57.2 Baseline FEV1 61% to 79 % predicted | 15 | 7070 | Risk Ratio (M-H, Fixed, 95% CI) | 0.94 [0.82, 1.07] |
| 57.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 1.23 [0.70, 2.15] |
| 57.4 Baseline FEV1 predicted not reported | 3 | 1087 | Risk Ratio (M-H, Fixed, 95% CI) | 1.26 [0.70, 2.26] |
| 58 # patients with hoarseness | 9 | 4963 | Risk Ratio (M-H, Fixed, 95% CI) | 0.95 [0.79, 1.14] |
| 58.1 Baseline FEV1 >/= 80% predicted | 2 | 646 | Risk Ratio (M-H, Fixed, 95% CI) | 1.00 [0.82, 1.22] |
| 58.2 Baseline FEV1 61% to 79 % predicted | 4 | 2957 | Risk Ratio (M-H, Fixed, 95% CI) | 0.86 [0.54, 1.36] |
| 58.3 Baseline FEV1 <= 60% predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 0.98 [0.43, 2.23] |
| 58.4 Baseline FEV1 predicted not reported | 2 | 872 | Risk Ratio (M-H, Fixed, 95% CI) | 0.62 [0.16, 2.37] |
| 59 # patients with tachycardia or palpitations | 15 | 7284 | Risk Ratio (M-H, Fixed, 95% CI) | 1.20 [0.78, 1.84] |
| 59.1 Baseline FEV1 >= 80 % predicted | 1 | 233 | Risk Ratio (M-H, Fixed, 95% CI) | 0.15 [0.01, 2.90] |
| 59.2 Baseline FEV1 61% to 79 % predicted | 11 | 5691 | Risk Ratio (M-H, Fixed, 95% CI) | 1.11 [0.61, 2.02] |
| 59.3 Baseline FEV1 <= 60 % predicted | 1 | 488 | Risk Ratio (M-H, Fixed, 95% CI) | 6.89 [0.36, 132.62] |
| 59.4 Baseline FEV1 predicted not reported | 2 | 872 | Risk Ratio (M-H, Fixed, 95% CI) | 1.39 [0.70, 2.74] |
| 60 Growth (paediatric data) | 1 | cm (Random, 95% CI) | Totals not selected |
Comparison 2.
LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 # patients with exacerbations requiring oral steroids: children versus adults | 25 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 1.1 Children | 3 | 480 | Risk Ratio (M-H, Fixed, 95% CI) | 1.24 [0.58, 2.66] |
| 1.2 Adults | 23 | 9349 | Risk Ratio (M-H, Fixed, 95% CI) | 0.87 [0.78, 0.97] |
| 2 # patients with exacerbations requiring oral steroids: ICS dose associated with LABA | 25 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 2.1 ICS dose <=400 mcg/day or equivalent in LABA group | 22 | 9388 | Risk Ratio (M-H, Fixed, 95% CI) | 0.86 [0.77, 0.97] |
| 2.2 ICS dose 400-1000 mcg/day of BDP-equivalent in LABA group | 3 | 445 | Risk Ratio (M-H, Fixed, 95% CI) | 1.21 [0.69, 2.12] |
| 3 # patients with exacerbations requiring oral steroids: ICS dose difference between LABA and higher ICS groups | 25 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 3.1 ICS dose difference of <= 400 mcg/day of BDP-equivalent | 10 | 3081 | Risk Ratio (M-H, Fixed, 95% CI) | 0.84 [0.69, 1.03] |
| 3.2 ICS dose difference of >= 500 mcg/day of BDP-equivalent | 15 | 6752 | Risk Ratio (M-H, Fixed, 95% CI) | 0.89 [0.78, 1.02] |
| 4 # patients with exacerbations requiring oral steroids: formoterol versus salmeterol | 25 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 4.1 Formoterol | 5 | 2861 | Risk Ratio (M-H, Fixed, 95% CI) | 1.00 [0.87, 1.16] |
| 4.2 Salmeterol | 20 | 6972 | Risk Ratio (M-H, Fixed, 95% CI) | 0.75 [0.63, 0.89] |
| 5 # patients with exacerbations requiring oral steroids: 1 versus 2 devices to deliver LABA + ICS | 25 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 5.1 One device (combination therapy) | 11 | 5573 | Risk Ratio (M-H, Fixed, 95% CI) | 0.92 [0.77, 1.09] |
| 5.2 Two devices (concomitant terapy) | 14 | 4260 | Risk Ratio (M-H, Fixed, 95% CI) | 0.85 [0.73, 0.98] |
| 6 # patients with exacerbations requiring oral steroids: duration of trial | 24 | 9350 | Risk Ratio (M-H, Fixed, 95% CI) | 0.87 [0.78, 0.98] |
| 6.1 <= 24 weeks | 19 | 6503 | Risk Ratio (M-H, Fixed, 95% CI) | 0.74 [0.63, 0.89] |
| 6.2 > 24 weeks | 5 | 2847 | Risk Ratio (M-H, Fixed, 95% CI) | 1.00 [0.86, 1.15] |
| 7 # patients with exacerbations requiring oral steroids: publication status of data | 25 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 7.1 Data available from study report | 9 | 2242 | Risk Ratio (M-H, Fixed, 95% CI) | 0.95 [0.78, 1.17] |
| 7.2 Data available from correspondence or study sponsor trial report | 16 | 7591 | Risk Ratio (M-H, Fixed, 95% CI) | 0.85 [0.74, 0.97] |
| 8 # patients with exacerbations requiring oral steroids: funding status | 25 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 8.1 Manufacturer sponsorship | 25 | 9833 | Risk Ratio (M-H, Fixed, 95% CI) | 0.88 [0.78, 0.98] |
| 8.2 Non-manufacturer sponsorship | 0 | 0 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 9 # patients with exacerbations requiring oral steroids: sensitivity analysis by allocation sequence generation | 23 | 9229 | Risk Ratio (M-H, Fixed, 95% CI) | 0.87 [0.78, 0.98] |
| 10 # patients with exacerbations requiring oral steroids: sensitivity analysis by allocation concealment | 22 | 7527 | Risk Ratio (M-H, Fixed, 95% CI) | 0.78 [0.67, 0.91] |
| 11 # patients with exacerbations requiring oral steroids: sensitivity analysis by blinding | 23 | 9670 | Risk Ratio (M-H, Fixed, 95% CI) | 0.86 [0.77, 0.96] |
| 12 # patients with exacerbations requiring hospitalisation: children versus adults | 33 | Risk Ratio (M-H, Fixed, 95% CI) | Subtotals only | |
| 12.1 Adults | 29 | 11215 | Risk Ratio (M-H, Fixed, 95% CI) | 0.87 [0.54, 1.38] |
| 12.2 Children and adults | 1 | 332 | Risk Ratio (M-H, Fixed, 95% CI) | Not estimable |
| 12.3 Children | 4 | 1026 | Risk Ratio (M-H, Fixed, 95% CI) | 2.21 [0.74, 6.64] |
Comparison 3.
WMD archive
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 FEV1 (L) at endpoint | 12 | 4688 | Mean Difference (IV, Random, 95% CI) | 0.08 [0.03, 0.14] |
| 2 FEV1 (% predicted) at endpoint | 5 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Change in FEV1 (L) at endpoint | 19 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 4 Change in FEV1 (L) stratifying on treatment period | 10 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 4.1 At 6 +/− 2 weeks | 4 | 1346 | Mean Difference (IV, Fixed, 95% CI) | 0.11 [0.06, 0.15] |
| 4.2 At 12 +/− 4 weeks | 8 | 3484 | Mean Difference (IV, Fixed, 95% CI) | 0.09 [0.07, 0.11] |
| 4.3 At 24 +/− 4 weeks | 4 | 1463 | Mean Difference (IV, Fixed, 95% CI) | 0.10 [0.06, 0.14] |
| 4.4 New Subgroup | 0 | 0 | Mean Difference (IV, Fixed, 95% CI) | Not estimable |
| 5 Morning PEF (L/min) at endpoint | 14 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6 Evening PEF (L/min) at endpoint | 3 | 425 | Mean Difference (IV, Fixed, 95% CI) | 20.18 [12.75, 27.62] |
| 6.1 Baseline FEV1 >= 80% predicted | 1 | 48 | Mean Difference (IV, Fixed, 95% CI) | 4.0 [−37.59, 45.59] |
| 6.2 Baseline FEV1 61% to 79 % predicted | 2 | 377 | Mean Difference (IV, Fixed, 95% CI) | 20.72 [13.16, 28.27] |
| 7 Change in morning or clinic PEF (L/min) at endpoint | 28 | 10784 | Mean Difference (IV, Random, 95% CI) | 16.25 [13.59, 18.90] |
| 8 Change in evening PEF (L/min) at endpoint | 18 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 9 Change in FEV1 (% predicted) at endpoint | 2 | 467 | Mean Difference (IV, Random, 95% CI) | 1.55 [−1.84, 4.94] |
| 9.1 Baseline FEV1 >= 80 % predicted | 1 | 120 | Mean Difference (IV, Random, 95% CI) | 0.28 [−0.25, 0.81] |
| 9.2 Baseline FEV1 61% to 79 % predicted | 1 | 347 | Mean Difference (IV, Random, 95% CI) | 3.90 [−0.01, 7.81] |
| 10 Change in % symptom-free days at endpoint | 11 | 4470 | Mean Difference (IV, Random, 95% CI) | 9.66 [6.04, 13.29] |
| 11 # patients with exacerbations requiring oral steroids | 25 | 9833 | Risk Ratio (M-H, Fixed, 95% CI) | 0.88 [0.78, 0.98] |
Analysis 1.1. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 1 # patients with exacerbations requiring oral steroids
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 1 # patients with exacerbations requiring oral steroids
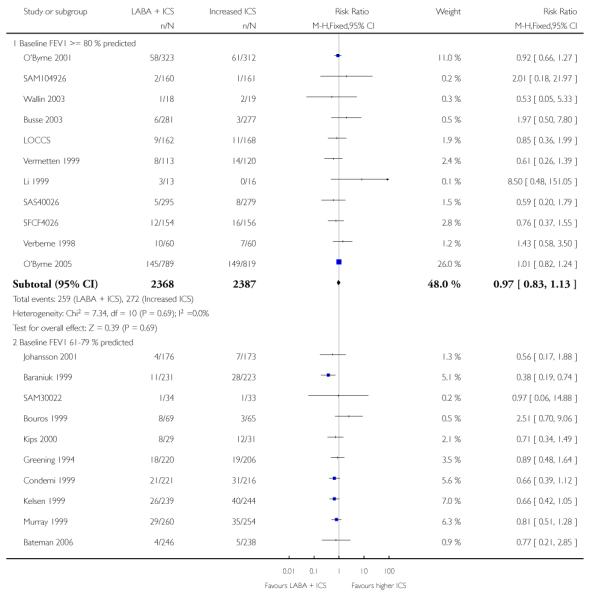
|
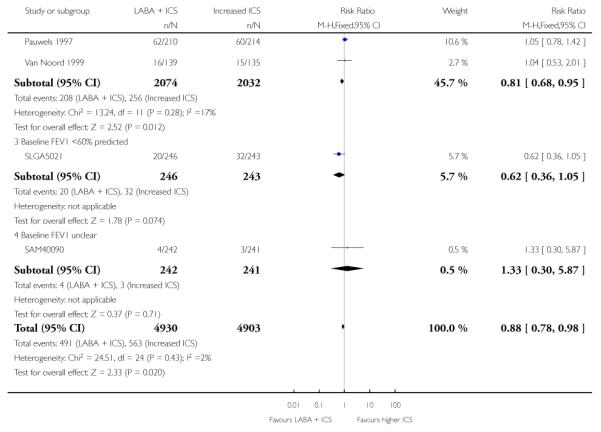
|
Analysis 1.2. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 2 # patients with exacerbations requiring hospitalisation
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 2 # patients with exacerbations requiring hospitalisation
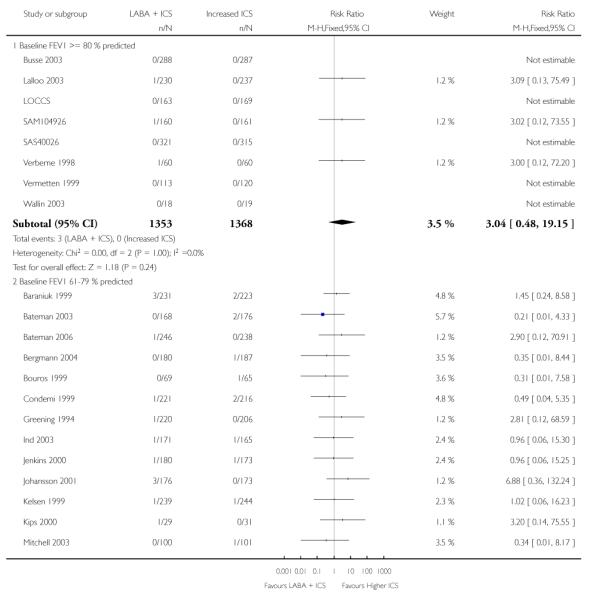
|
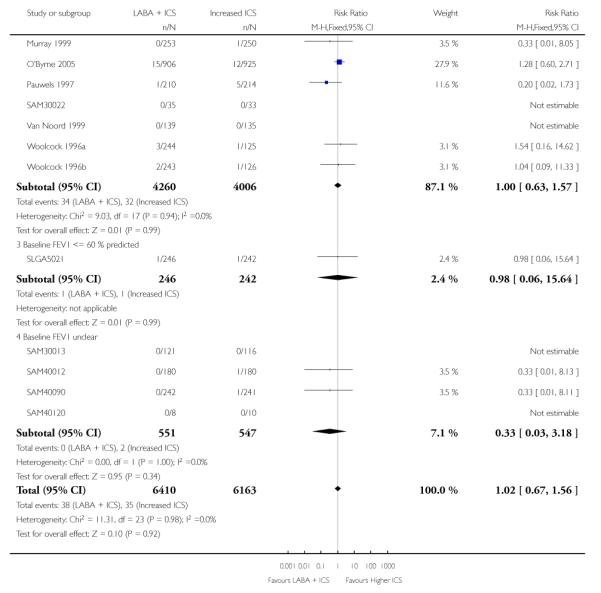
|
Analysis 1.3. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 3 # withdrawals due to poor asthma control or exacerbation
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 3 # withdrawals due to poor asthma control or exacerbation
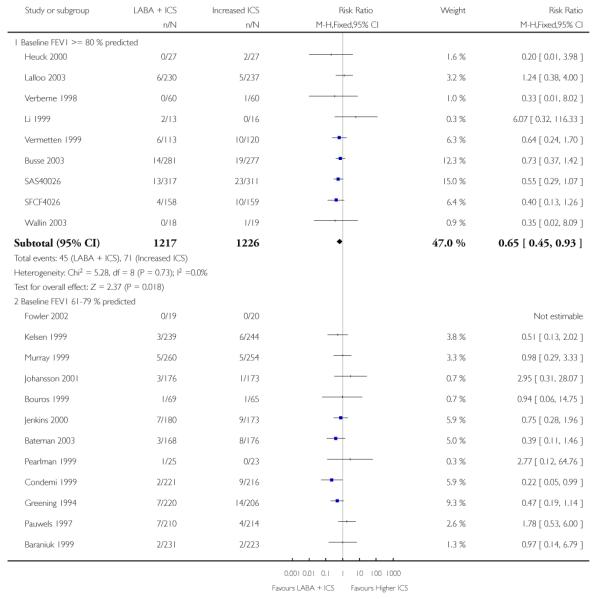
|
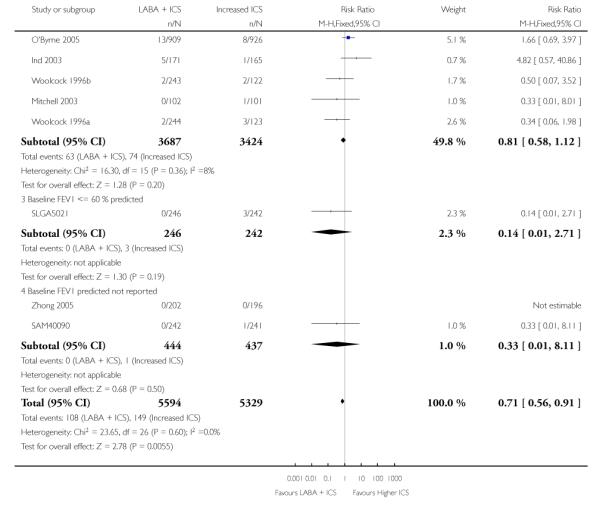
|
Analysis 1.4. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 4 Total # withdrawals
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 4 Total # withdrawals
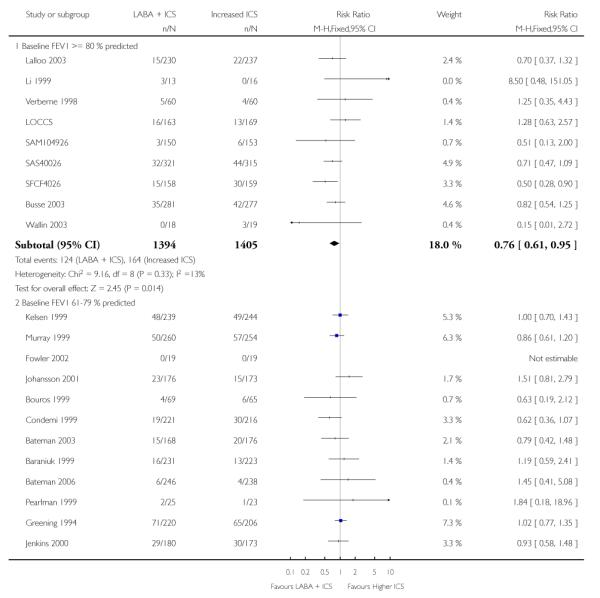
|
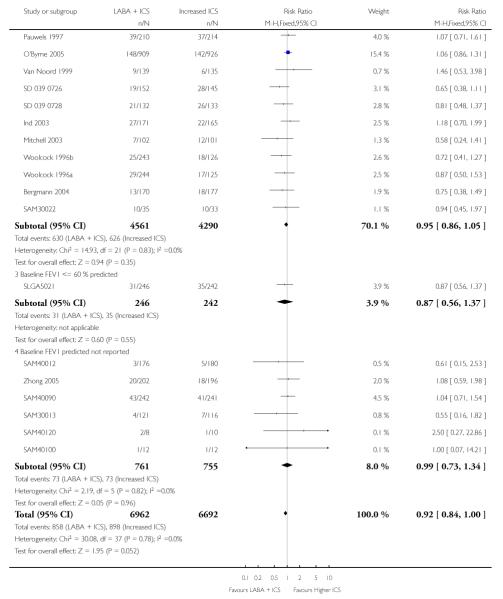
|
Analysis 1.5. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 5 # withdrawals due to adverse events
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 5 # withdrawals due to adverse events
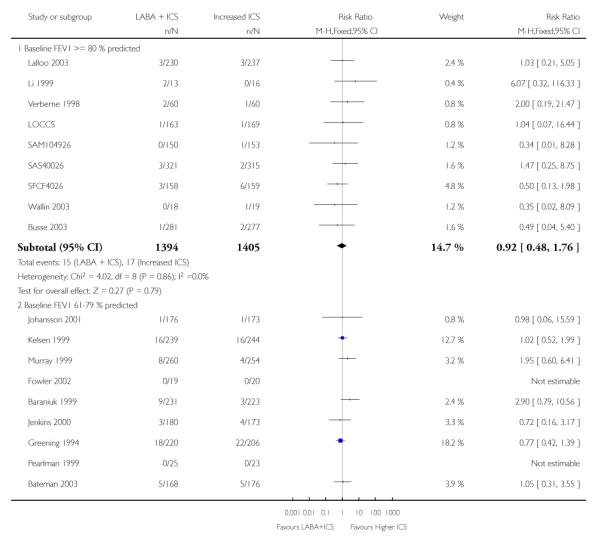
|
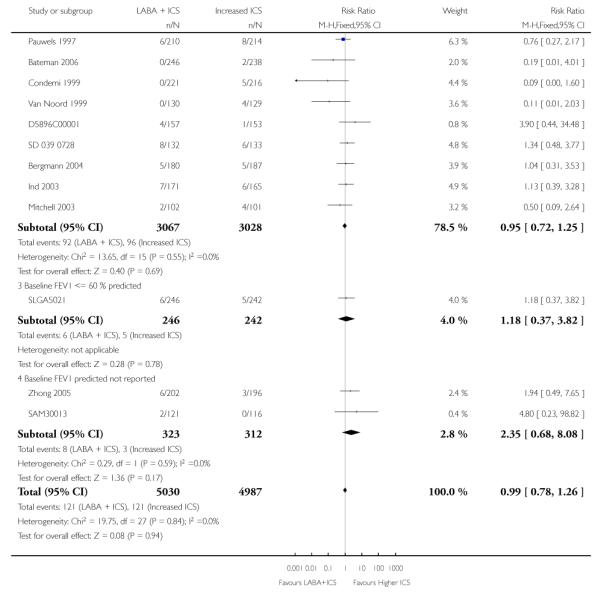
|
Analysis 1.6. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 6 FEV1 at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 6 FEV1 at endpoint
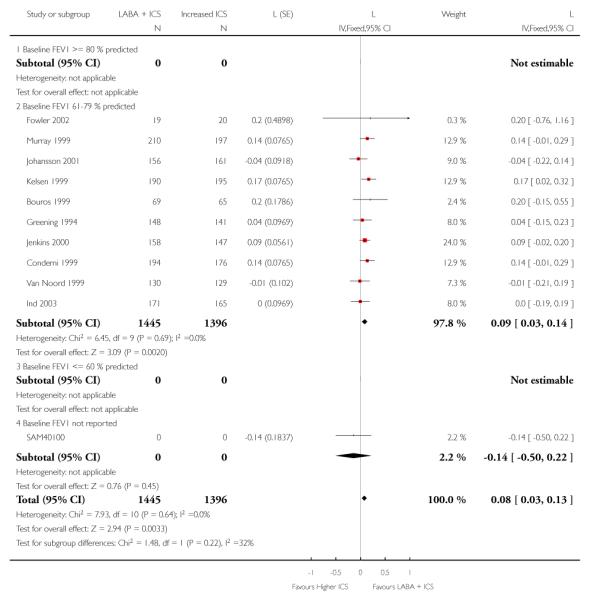
|
Analysis 1.7. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 7 FEV1 (predicted) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 7 FEV1 (predicted) at endpoint
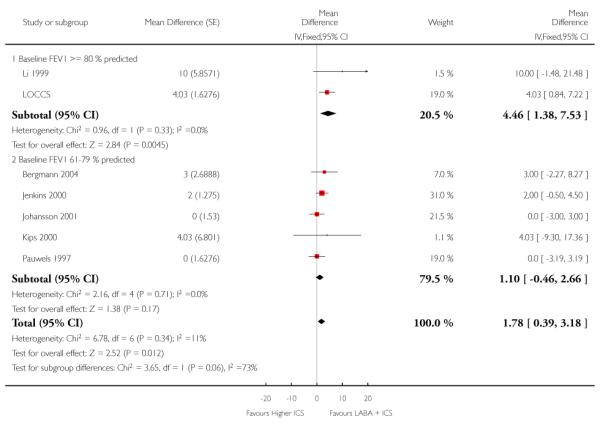
|
Analysis 1.8. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 8 Change in FEV1 at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 8 Change in FEV1 at endpoint
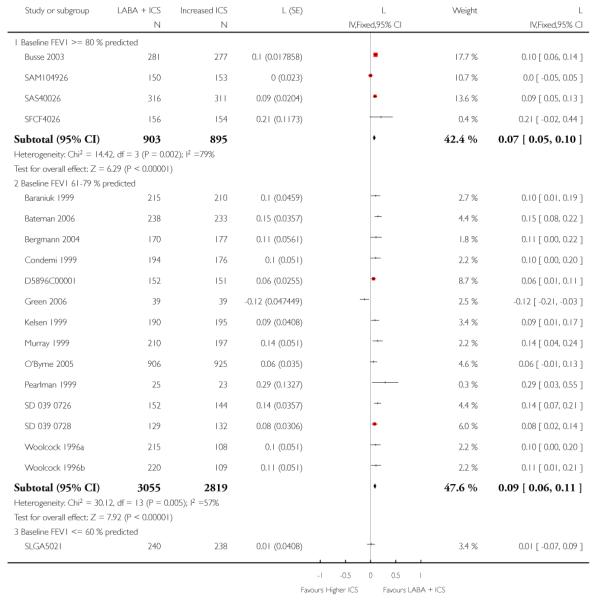
|
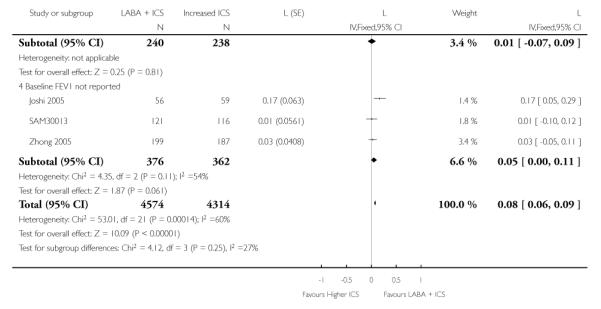
|
Analysis 1.9. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 9 Change in FEV1 stratifying on treatment period
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 9 Change in FEV1 stratifying on treatment period
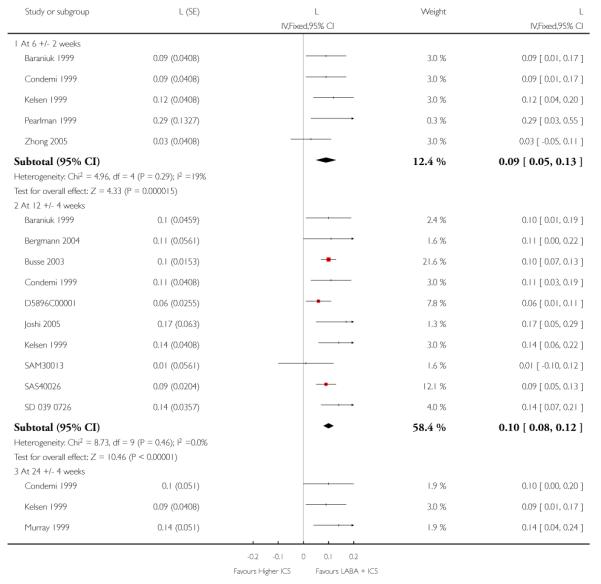
|
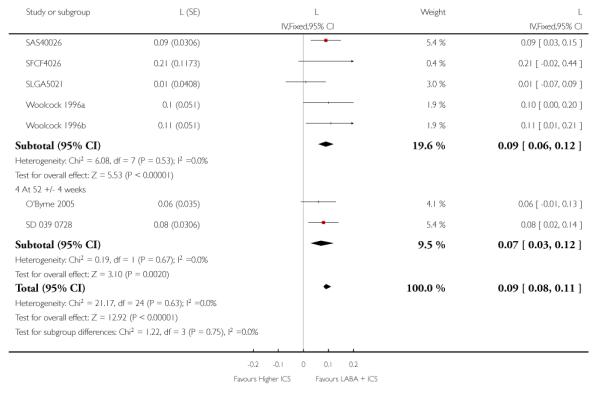
|
Analysis 1.10. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 10 Change in FEV1 (predicted) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 10 Change in FEV1 (predicted) at endpoint
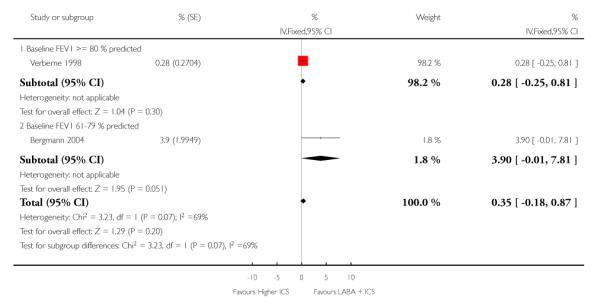
|
Analysis 1.11. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 11 Morning PEF at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 11 Morning PEF at endpoint
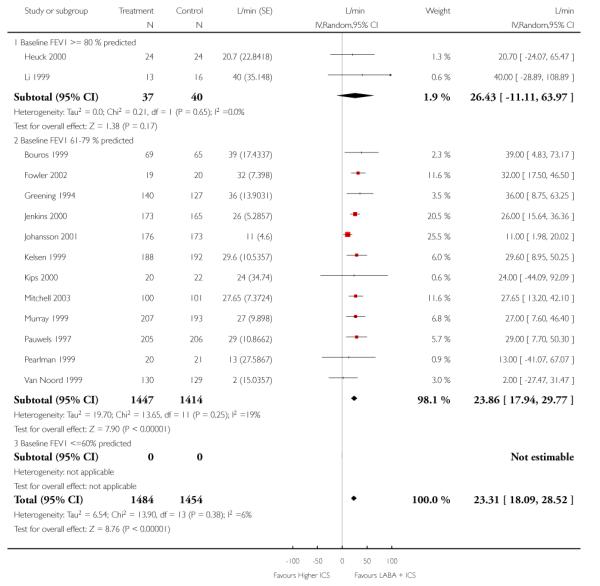
|
Analysis 1.12. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 12 Change in morning or clinic PEF at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 12 Change in morning or clinic PEF at endpoint
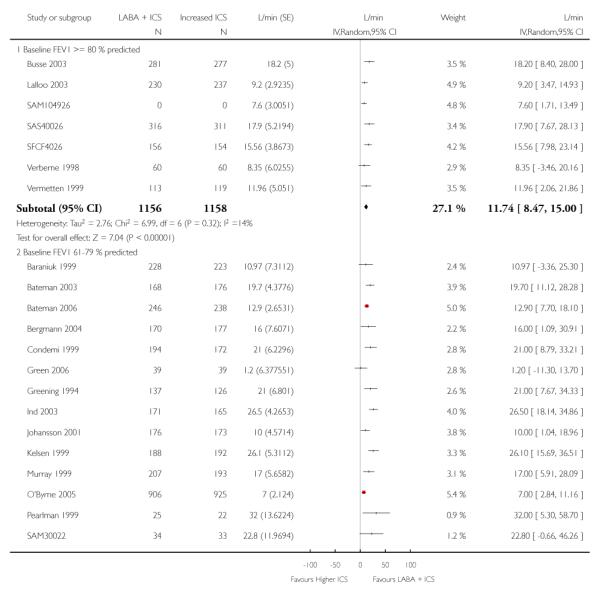
|
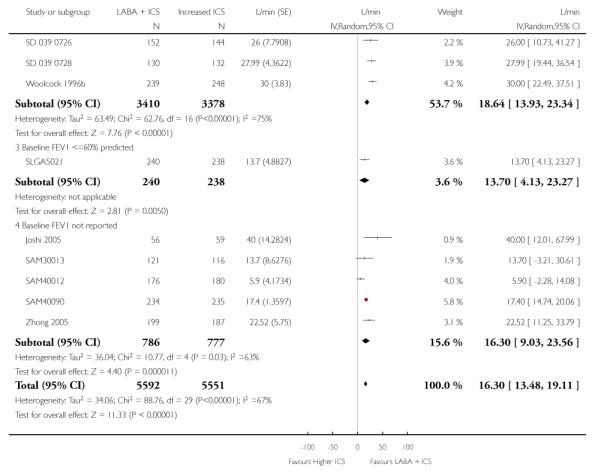
|
Analysis 1.13. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 13 Morning PEF (% predicted) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 13 Morning PEF (% predicted) at endpoint
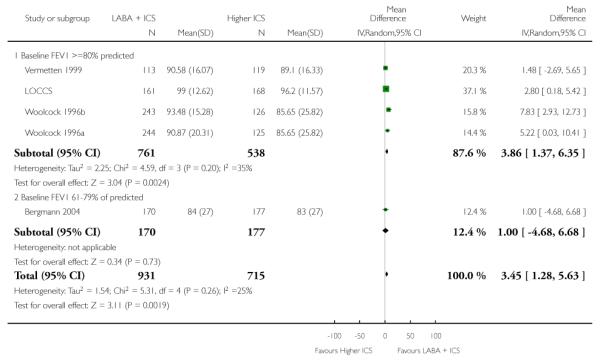
|
Analysis 1.14. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 14 Evening PEF at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 14 Evening PEF at endpoint
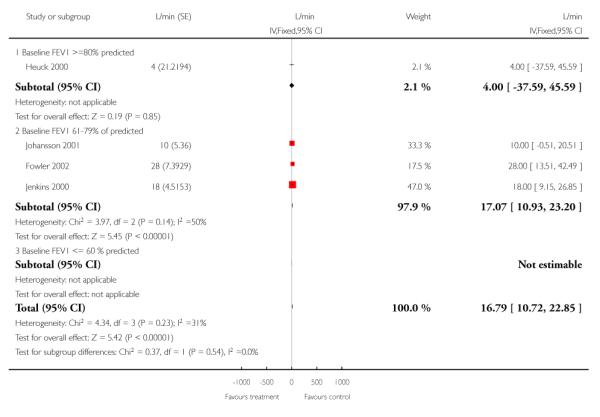
|
Analysis 1.16. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 16 Change in evening PEF at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 16 Change in evening PEF at endpoint
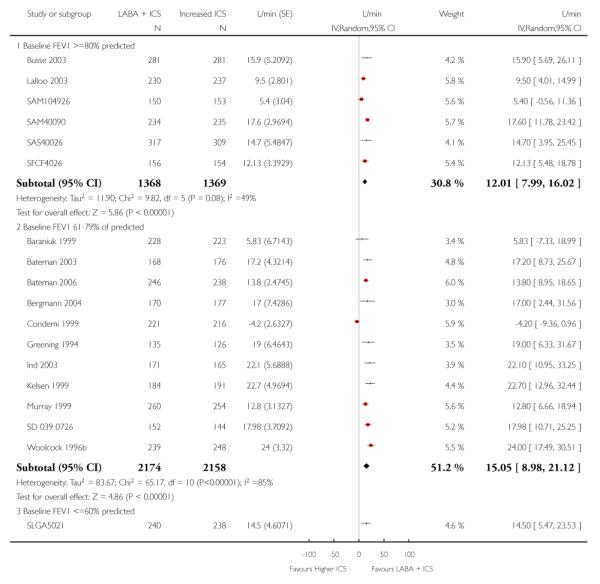
|
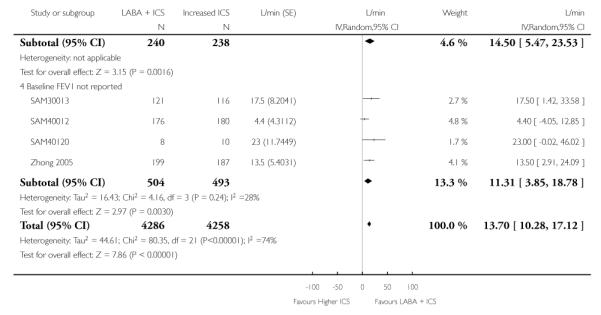
|
Analysis 1.18. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 18 PEF variability at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 18 PEF variability at endpoint
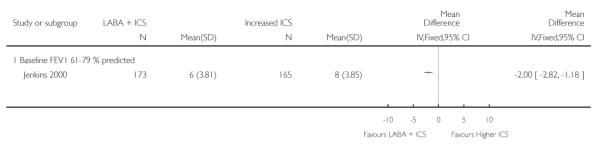
|
Analysis 1.19. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 19 Change in PEF variability at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 19 Change in PEF variability at endpoint
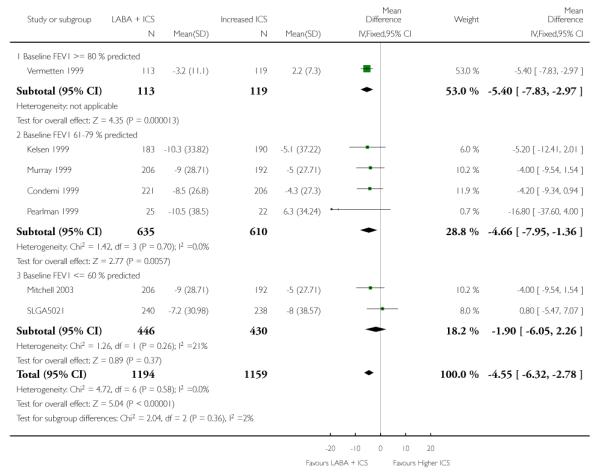
|
Analysis 1.20. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 20 Change in daytime symptom score at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 20 Change in daytime symptom score at endpoint
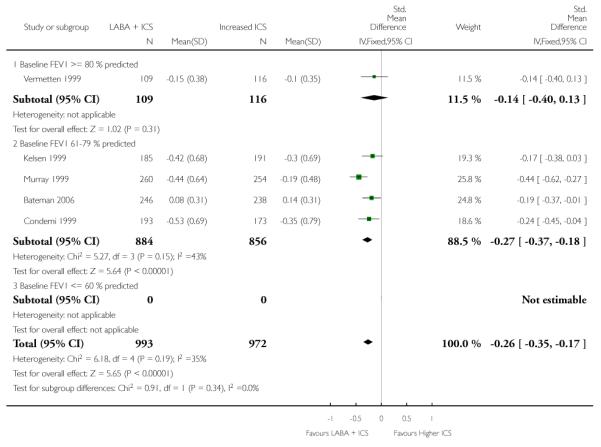
|
Analysis 1.21. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 21 Change in overall (24 hrs) symptom score at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 21 Change in overall (24 hrs) symptom score at endpoint
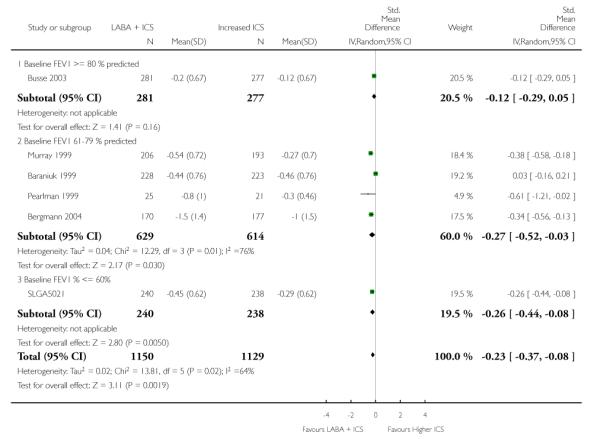
|
Analysis 1.22. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 22 Change in % symptom-free days at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 22 Change in % symptom-free days at endpoint
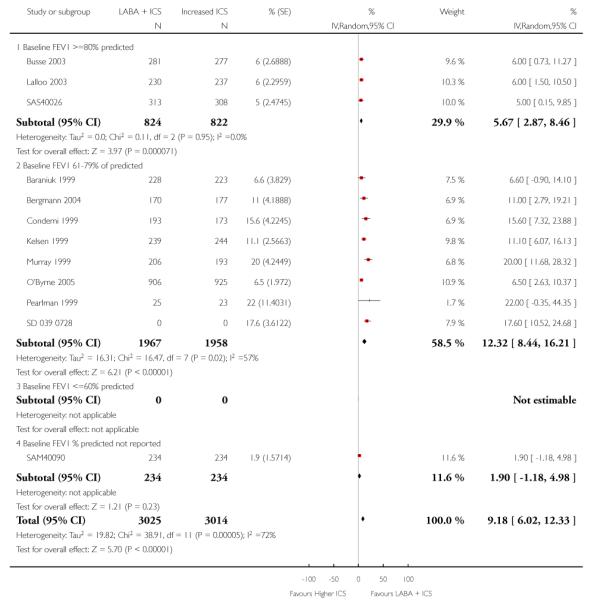
|
Analysis 1.23. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 23 % symptom-free days at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 23 % symptom-free days at endpoint
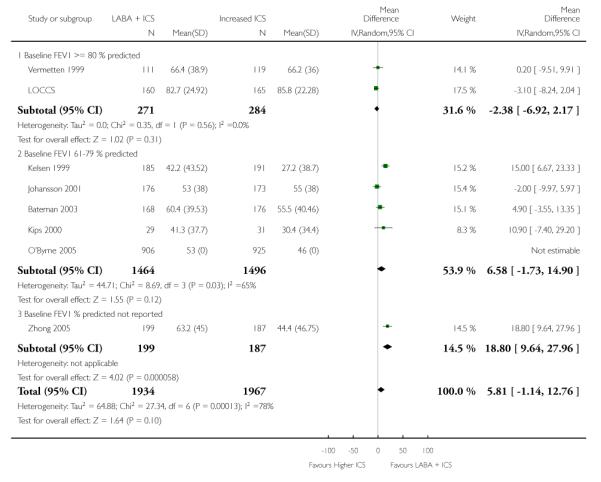
|
Analysis 1.24. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 24 Daytime symptom score at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 24 Daytime symptom score at endpoint
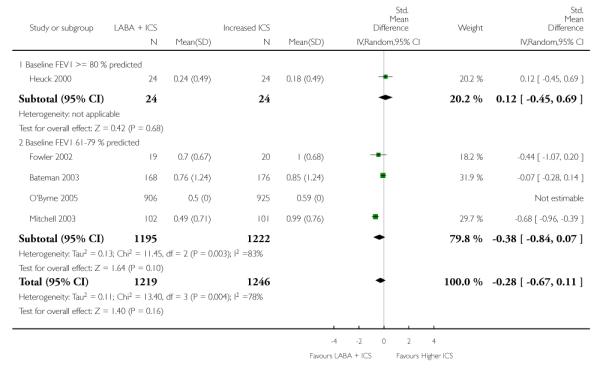
|
Analysis 1.25. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 25 Nighttime symptom score at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 25 Nighttime symptom score at endpoint
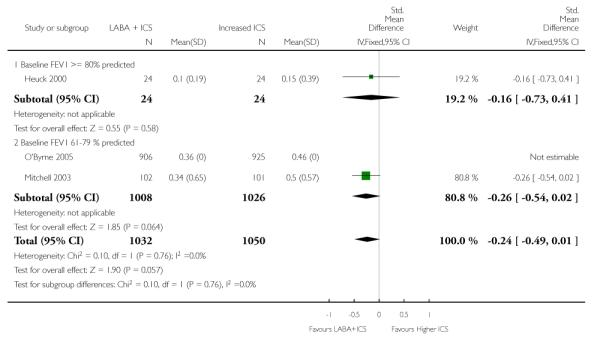
|
Analysis 1.26. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 26 Change in nighttime symptom score at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 26 Change in nighttime symptom score at endpoint
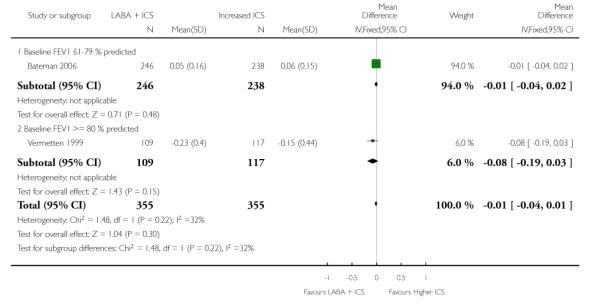
|
Analysis 1.27. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 27 % symptom-free nights at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 27 % symptom-free nights at endpoint
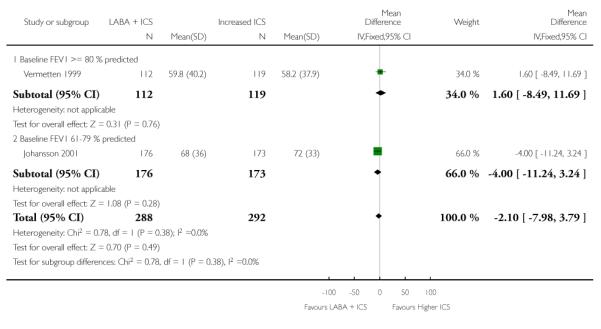
|
Analysis 1.28. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 28 Change in night time awakenings ( number of nights) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 28 Change in night time awakenings ( number of nights) at endpoint
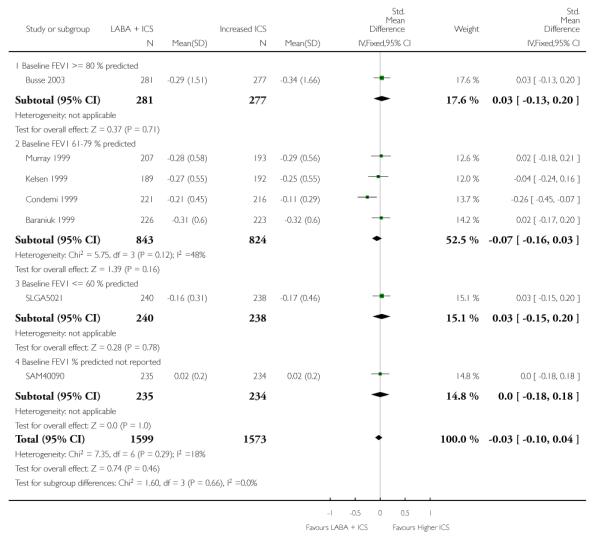
|
Analysis 1.29. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 29 % nighttime awakenings at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 29 % nighttime awakenings at endpoint
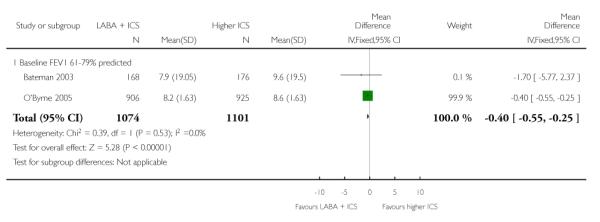
|
Analysis 1.30. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 30 % nights with no awakenings at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 30 % nights with no awakenings at endpoint
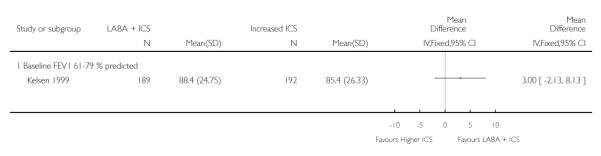
|
Analysis 1.31. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 31 Change in % nights with no awakenings at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 31 Change in % nights with no awakenings at endpoint
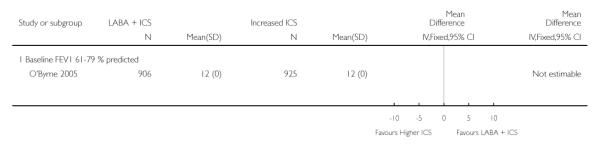
|
Analysis 1.32. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 32 Change in # daytime rescue inhalations at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 32 Change in # daytime rescue inhalations at endpoint
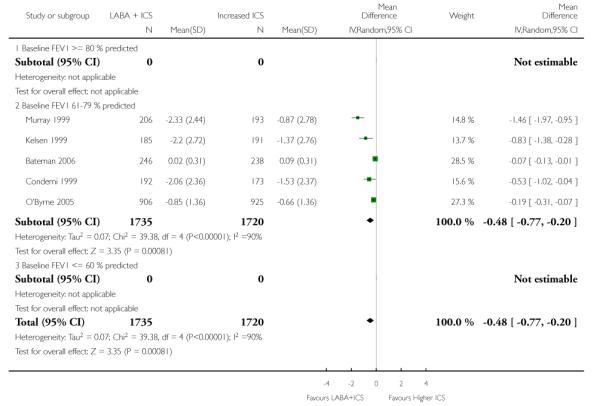
|
Analysis 1.33. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 33 Change in # nighttime rescue inhalations at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 33 Change in # nighttime rescue inhalations at endpoint
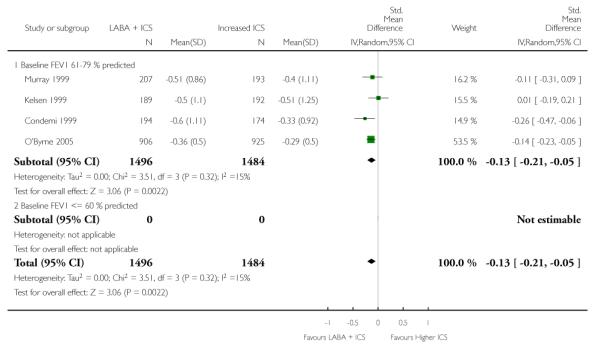
|
Analysis 1.34. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 34 Absolute (or %) change in # rescue inhalations (per 24 hrs) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 34 Absolute (or %) change in # rescue inhalations (per 24 hrs) at endpoint
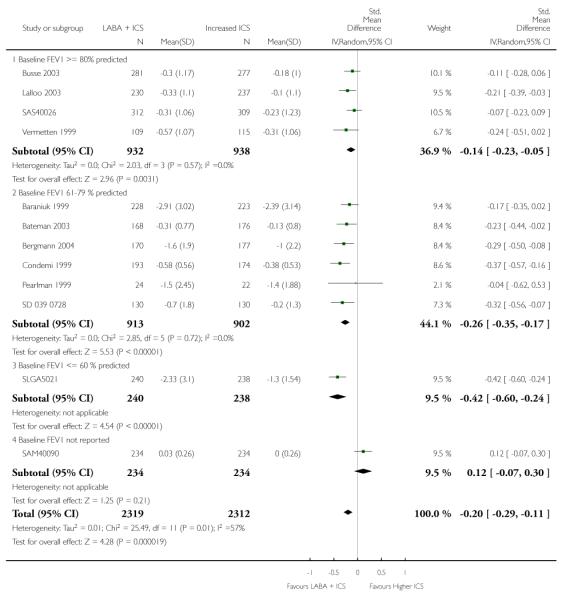
|
Analysis 1.35. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 35 # daytime rescue inhalations (puffs/day) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 35 # daytime rescue inhalations (puffs/day) at endpoint
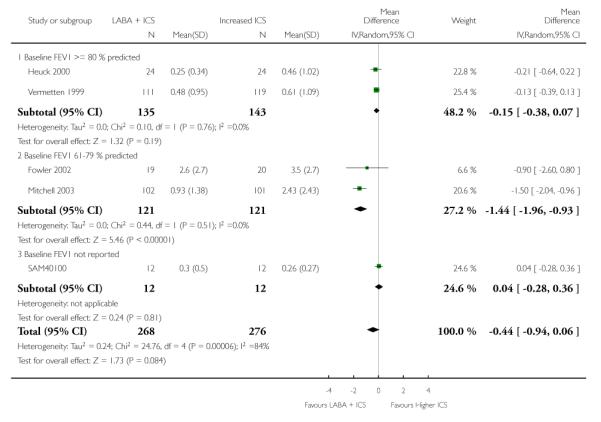
|
Analysis 1.36. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 36 # nighttime rescue inhalations at endpoint (puffs/day)
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 36 # nighttime rescue inhalations at endpoint (puffs/day)
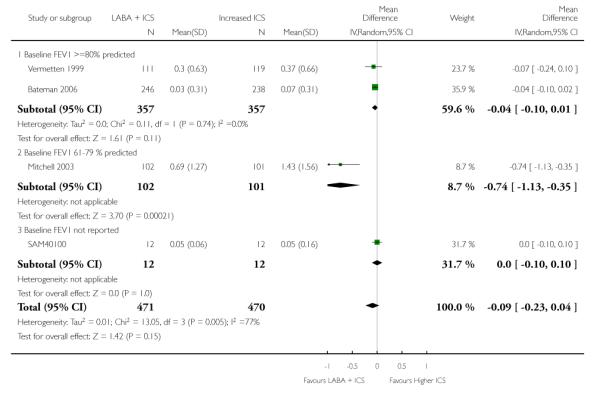
|
Analysis 1.37. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 37 % overall rescue-free days at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 37 % overall rescue-free days at endpoint
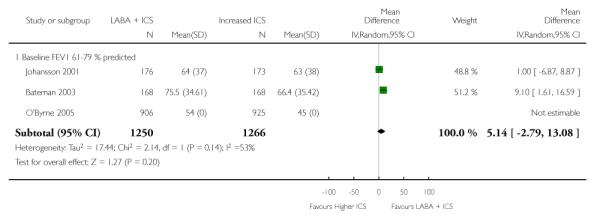
|
Analysis 1.38. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 38 Change in % symptom-free days at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 38 Change in % symptom-free days at endpoint
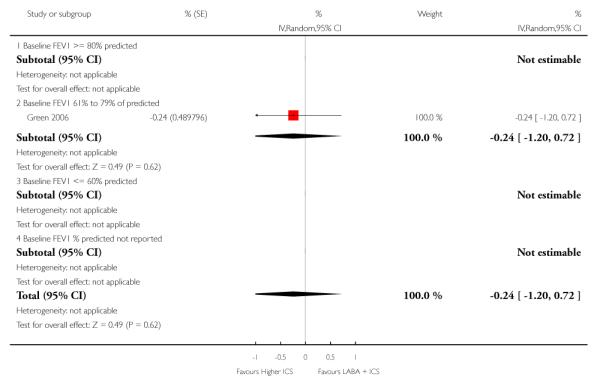
|
Analysis 1.39. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 39 Change in mean % rescue-free days at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 39 Change in mean % rescue-free days at endpoint
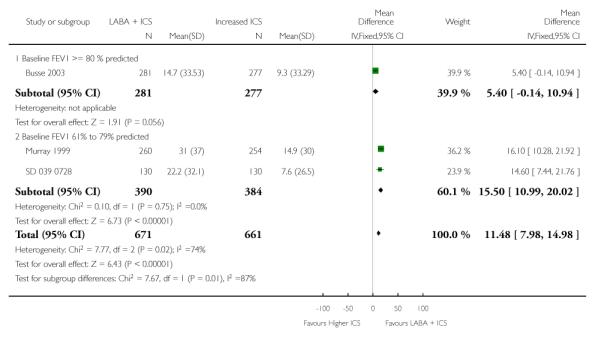
|
Analysis 1.40. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 40 Change in asthma control days at endpoint (%)
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 40 Change in asthma control days at endpoint (%)
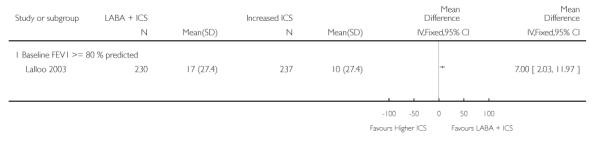
|
Analysis 1.41. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 41 Change in quality of life (AQLQ score) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 41 Change in quality of life (AQLQ score) at endpoint
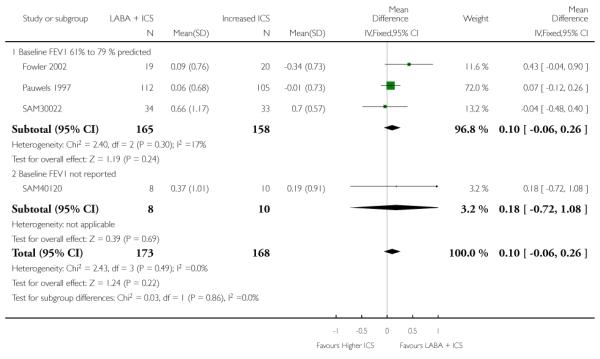
|
Analysis 1.42. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 42 Change in Hyland QOL at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 42 Change in Hyland QOL at endpoint
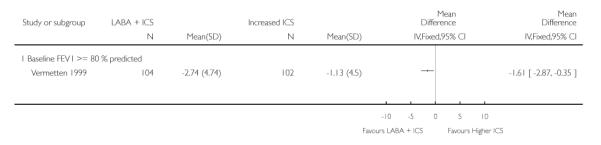
|
Analysis 1.43. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 43 # Achieving good asthma control
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 43 # Achieving good asthma control
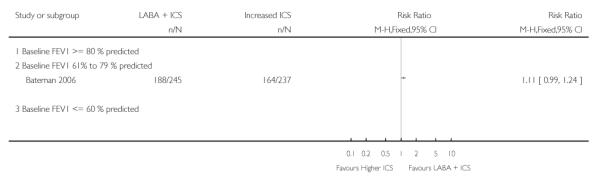
|
Analysis 1.44. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 44 % asthma control days at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 44 % asthma control days at endpoint
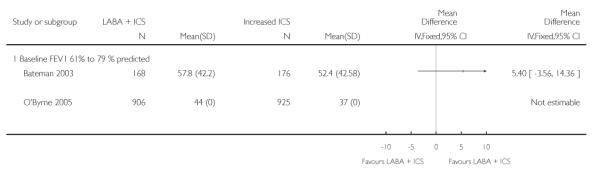
|
Analysis 1.45. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 45 Serum ECP( microg /L)
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 45 Serum ECP( microg /L)
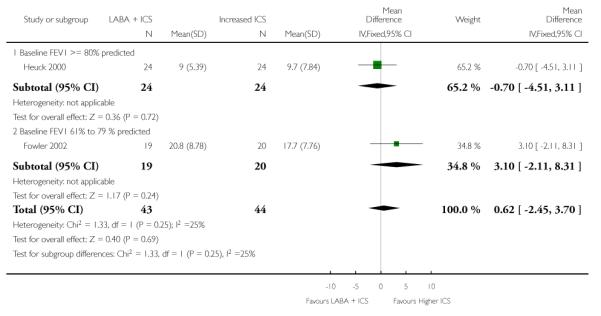
|
Analysis 1.46. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 46 Plasma cortisol ( nmol/L) 8am at 8 weeks
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 46 Plasma cortisol ( nmol/L) 8am at 8 weeks
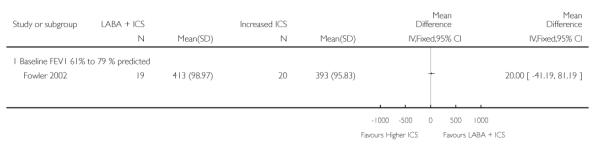
|
Analysis 1.47. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 47 Tidal exhaled NO(ppb)
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 47 Tidal exhaled NO(ppb)
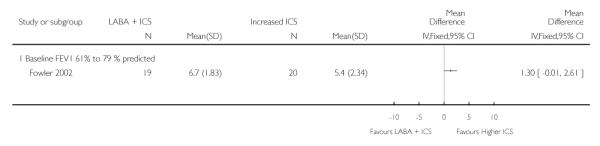
|
Analysis 1.48. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 48 PD20 @ 8 weeks
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 48 PD20 @ 8 weeks
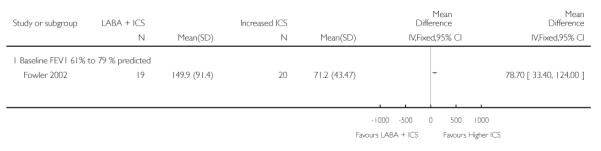
|
Analysis 1.49. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 49 PC20
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 49 PC20
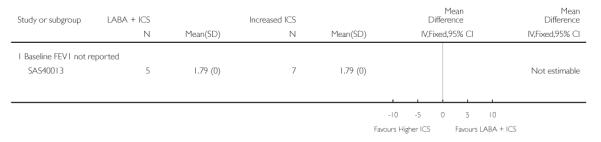
|
Analysis 1.50. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 50 Change in mean urine Cortisol/Creatinine ratio
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 50 Change in mean urine Cortisol/Creatinine ratio
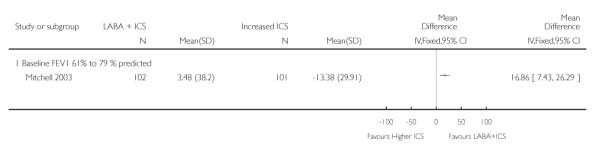
|
Analysis 1.52. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 52 Serious adverse events
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 52 Serious adverse events
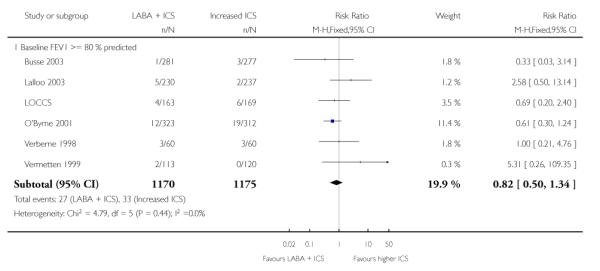
|
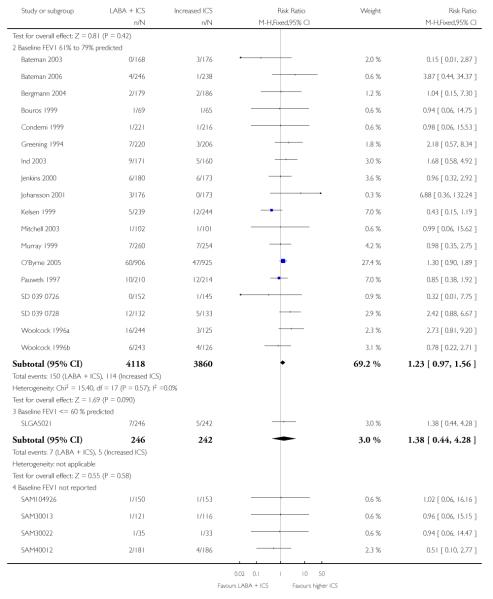
|
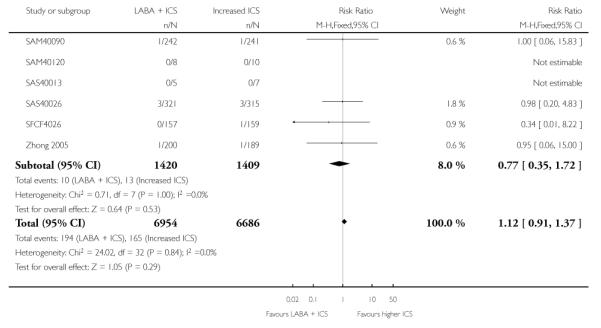
|
Analysis 1.53. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 53 # patients with tremor
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 53 # patients with tremor
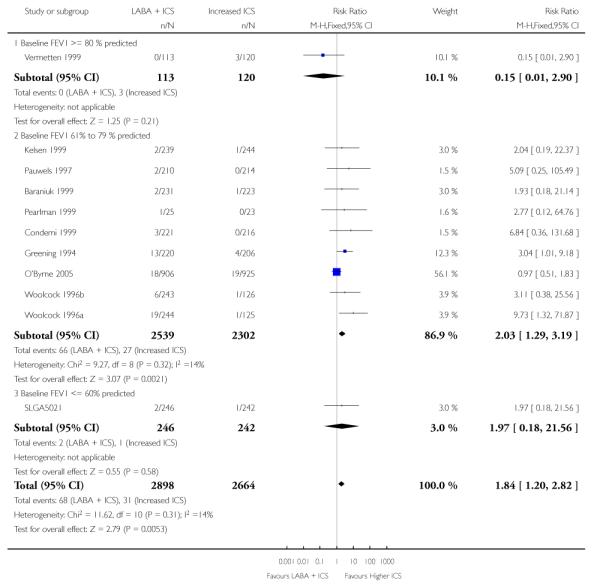
|
Analysis 1.54. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 54 # patients with oral thrush
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 54 # patients with oral thrush
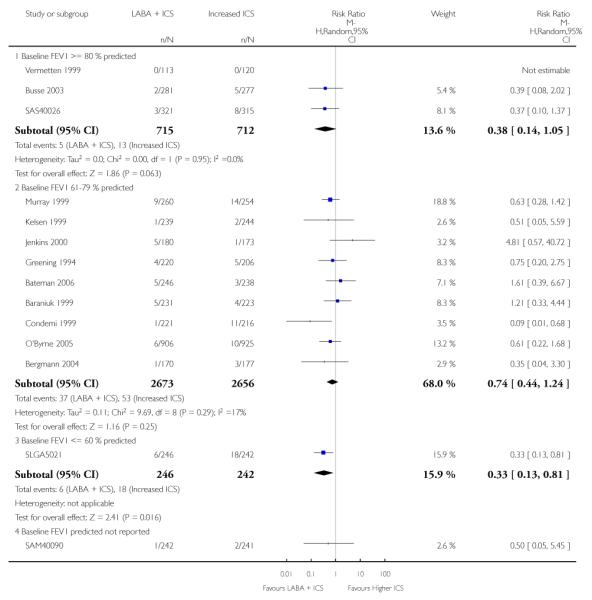
|
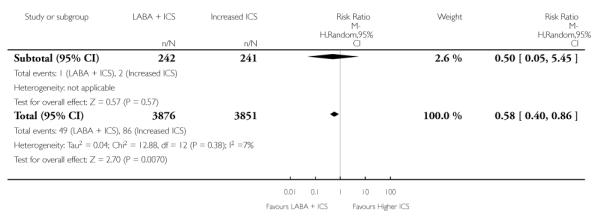
|
Analysis 1.55. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 55 Total # adverse events
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 55 Total # adverse events
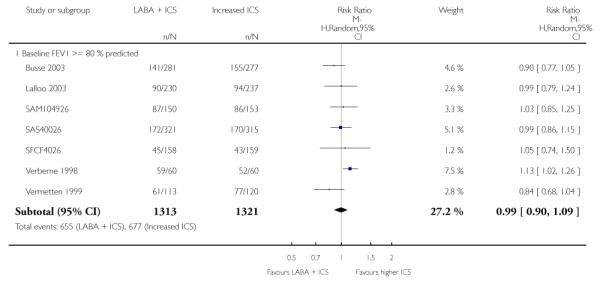
|
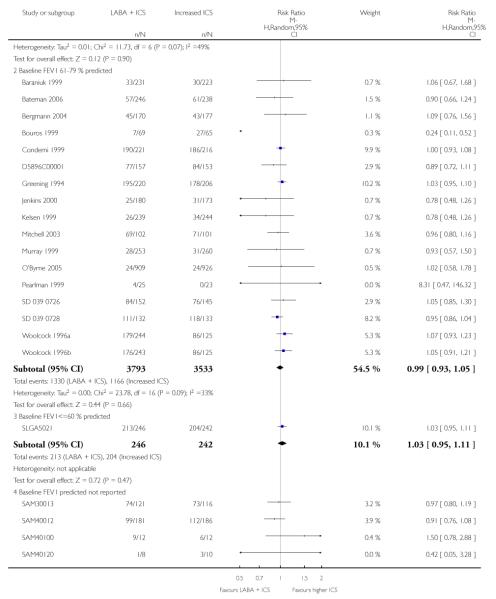
|
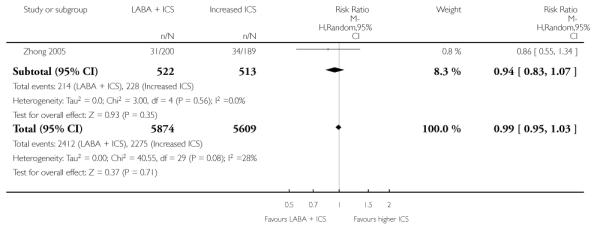
|
Analysis 1.56. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 56 # patients with adverse cardiovascular events
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 56 # patients with adverse cardiovascular events
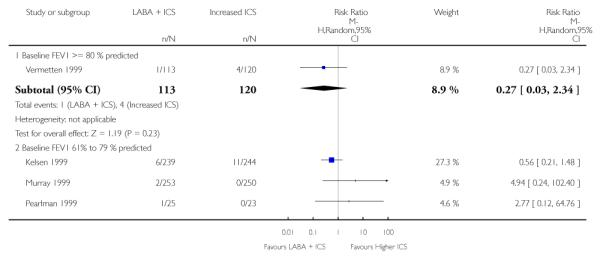
|
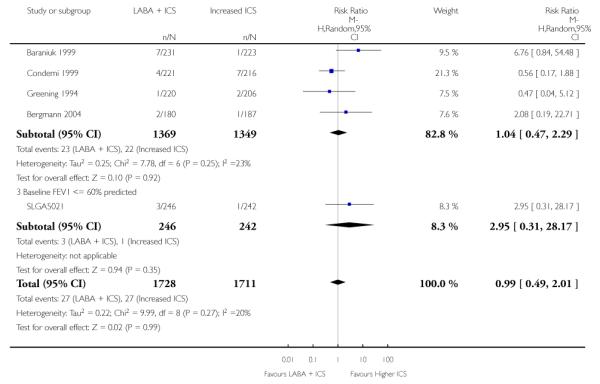
|
Analysis 1.57. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 57 # patients with headache
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 57 # patients with headache
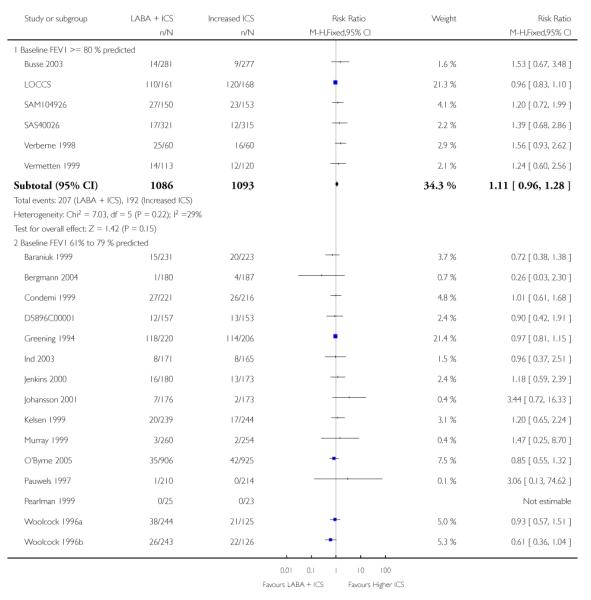
|
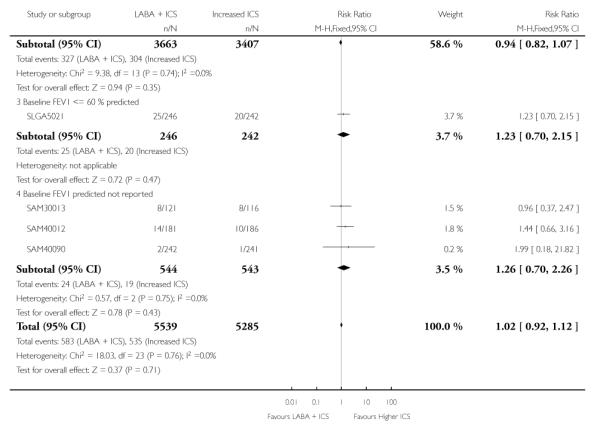
|
Analysis 1.58. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 58 # patients with hoarseness
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 58 # patients with hoarseness
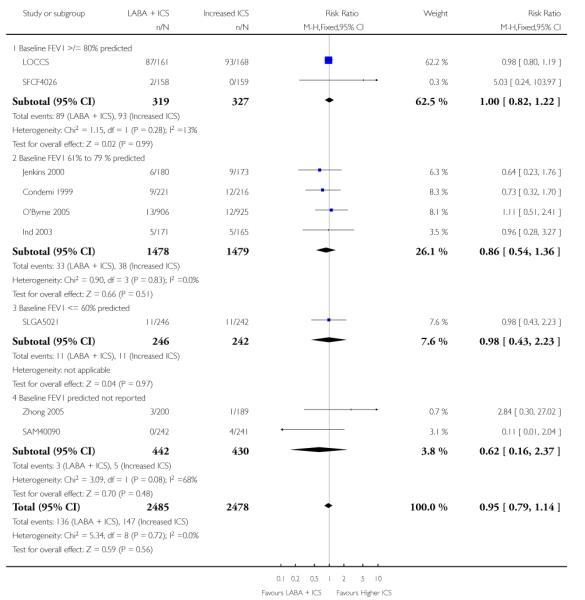
|
Analysis 1.59. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 59 # patients with tachycardia or palpitations
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 59 # patients with tachycardia or palpitations
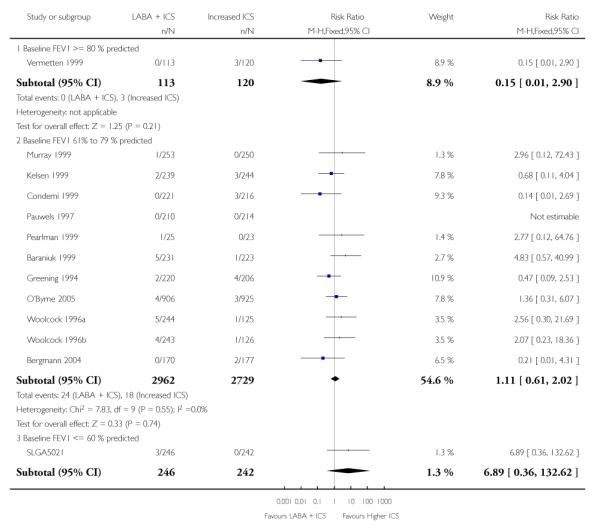
|
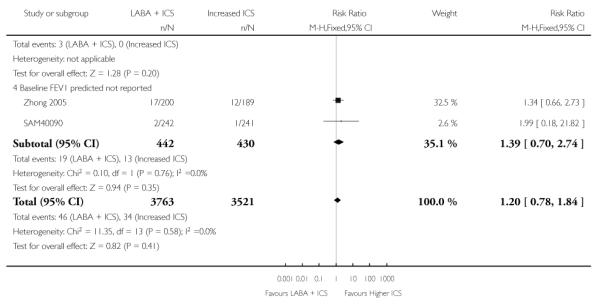
|
Analysis 1.60. Comparison 1 LABA + ICS versus higher dose ICS, Outcome 60 Growth (paediatric data)
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 1 LABA + ICS versus higher dose ICS
Outcome: 60 Growth (paediatric data)
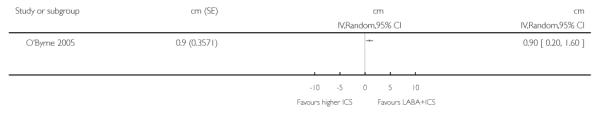
|
Analysis 2.1. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 1 # patients with exacerbations requiring oral steroids: children versus adults
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 1 # patients with exacerbations requiring oral steroids: children versus adults
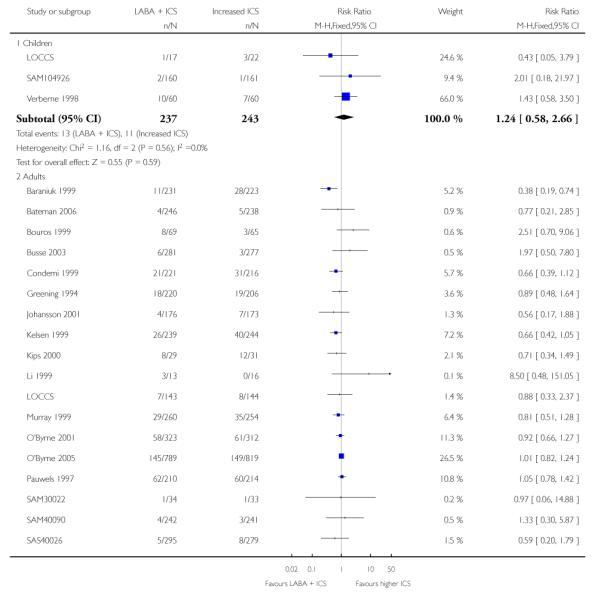
|
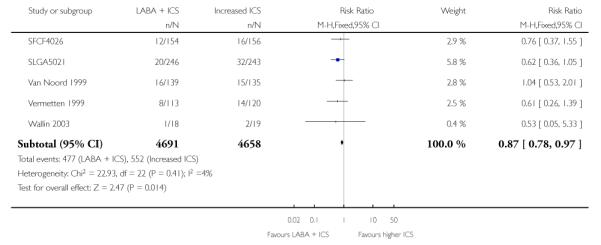
|
Analysis 2.2. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 2 # patients with exacerbations requiring oral steroids: ICS dose associated with LABA
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 2 # patients with exacerbations requiring oral steroids: ICS dose associated with LABA
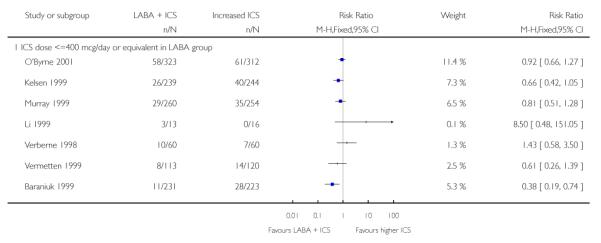
|
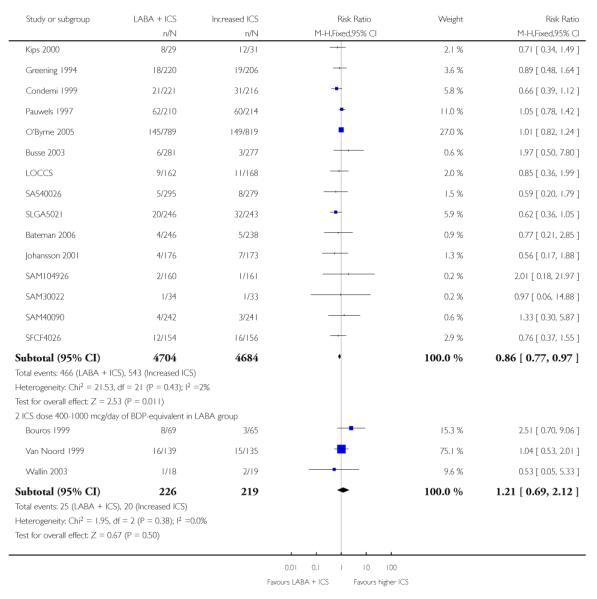
|
Analysis 2.3. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 3 # patients with exacerbations requiring oral steroids: ICS dose difference between LABA and higher ICS groups
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 3 # patients with exacerbations requiring oral steroids: ICS dose difference between LABA and higher ICS groups
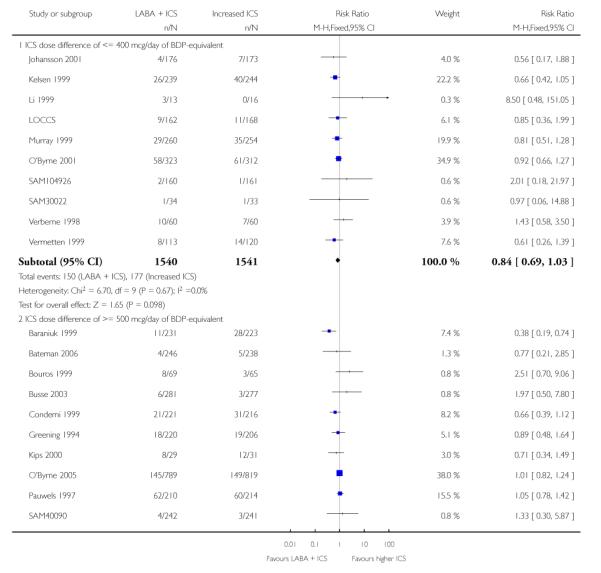
|
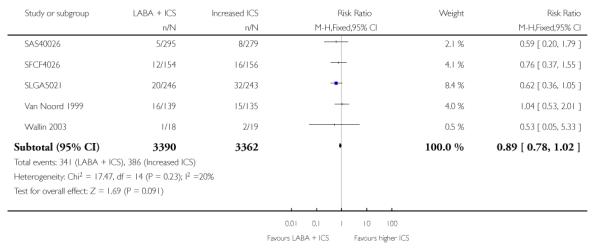
|
Analysis 2.4. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 4 # patients with exacerbations requiring oral steroids: formoterol versus salmeterol
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 4 # patients with exacerbations requiring oral steroids: formoterol versus salmeterol
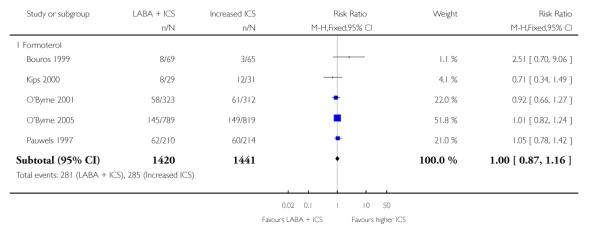
|
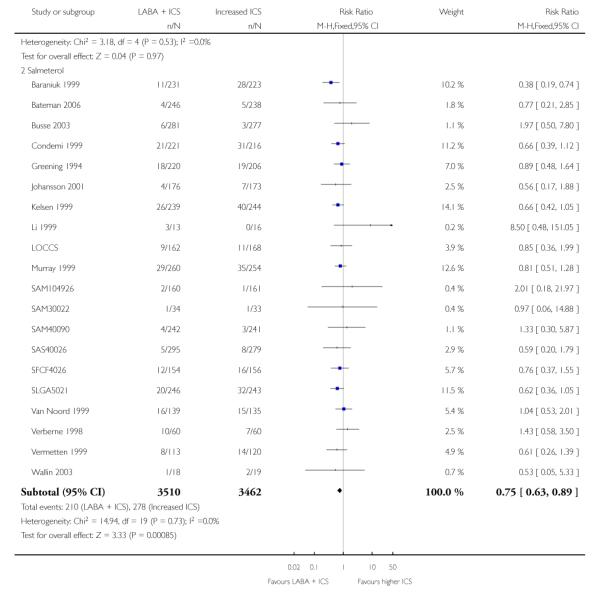
|
Analysis 2.5. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 5 # patients with exacerbations requiring oral steroids: 1 versus 2 devices to deliver LABA + ICS
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 5 # patients with exacerbations requiring oral steroids: 1 versus 2 devices to deliver LABA + ICS
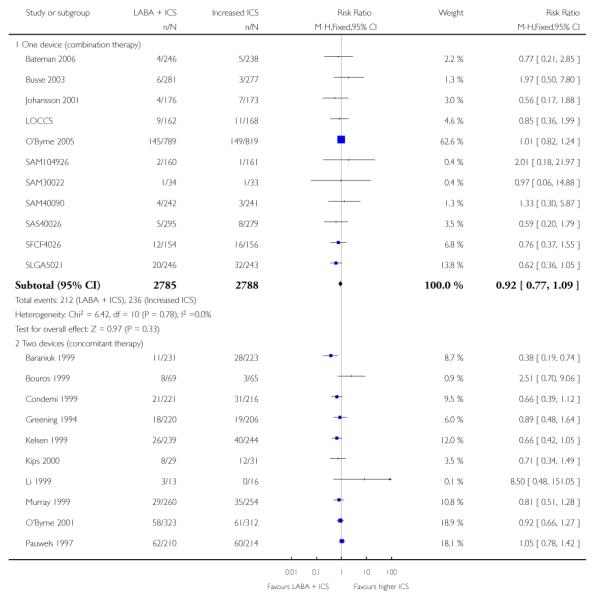
|
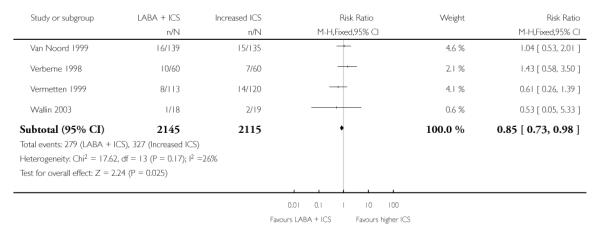
|
Analysis 2.6. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 6 # patients with exacerbations requiring oral steroids: duration of trial
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 6 # patients with exacerbations requiring oral steroids: duration of trial
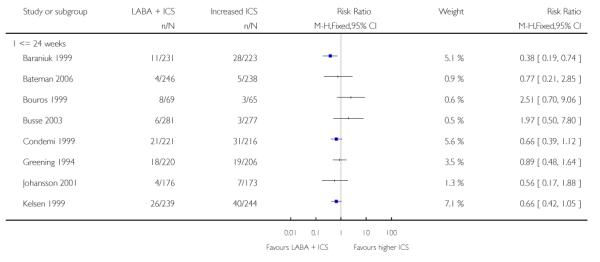
|
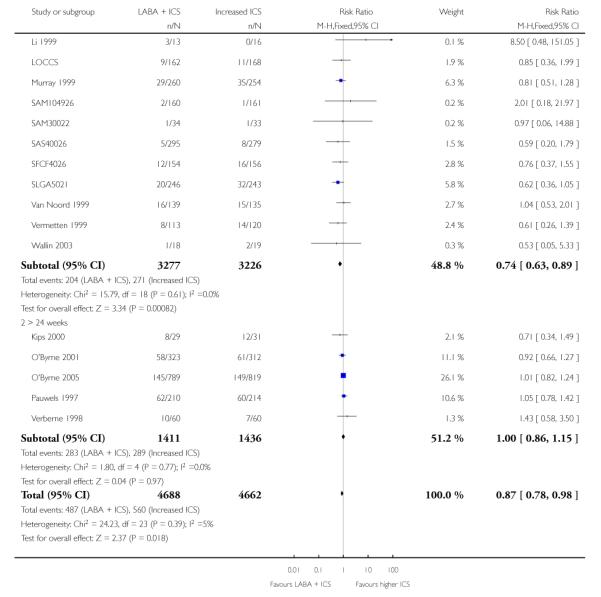
|
Analysis 2.7. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 7 # patients with exacerbations requiring oral steroids: publication status of data
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 7 # patients with exacerbations requiring oral steroids: publication status of data
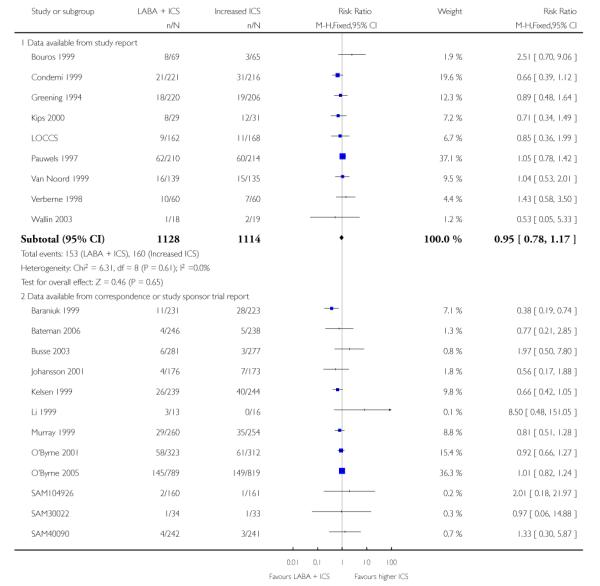
|
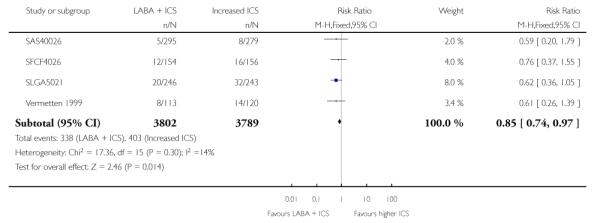
|
Analysis 2.8. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 8 # patients with exacerbations requiring oral steroids: funding status
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 8 # patients with exacerbations requiring oral steroids: funding status
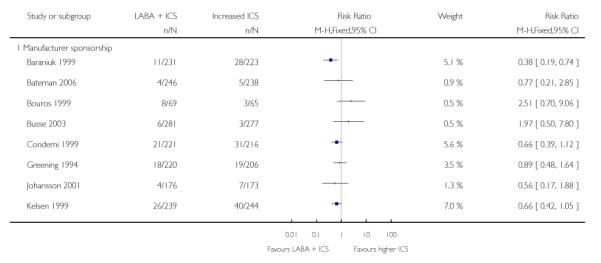
|
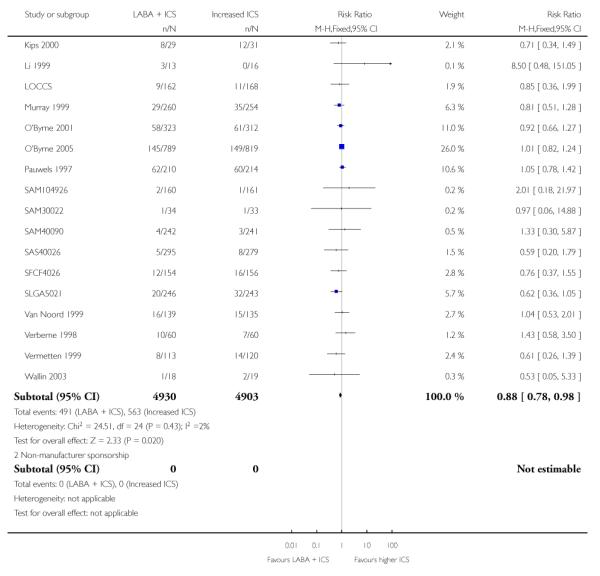
|
Analysis 2.9. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 9 # patients with exacerbations requiring oral steroids: sensitivity analysis by allocation sequence generation
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 9 # patients with exacerbations requiring oral steroids: sensitivity analysis by allocation sequence generation
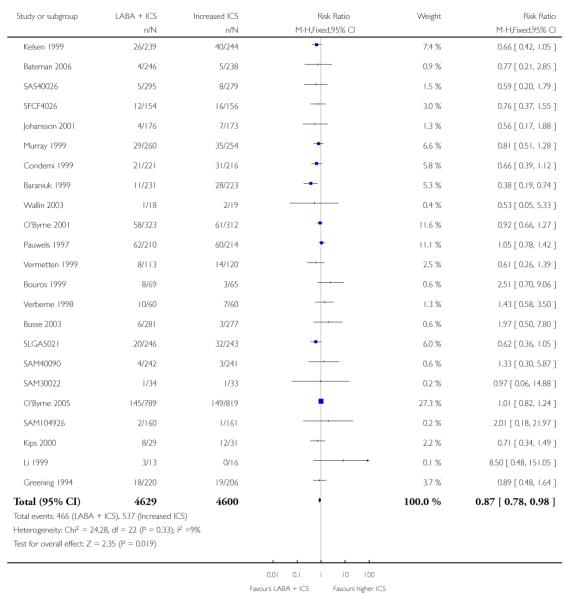
|
Analysis 2.10. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 10 # patients with exacerbations requiring oral steroids: sensitivity analysis by allocation concealment
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 10 # patients with exacerbations requiring oral steroids: sensitivity analysis by allocation concealment
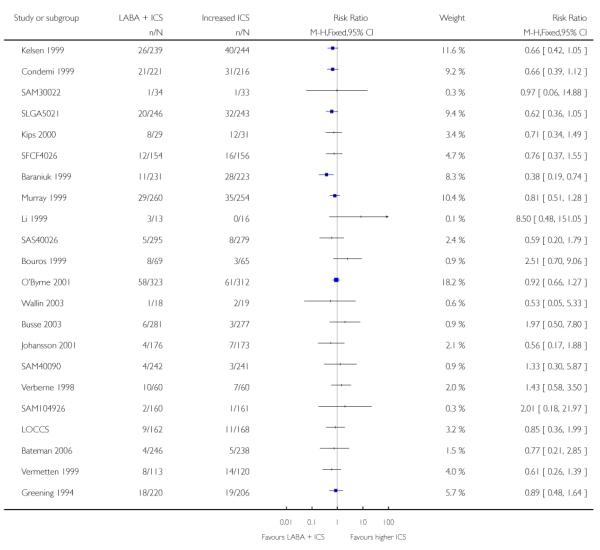
|
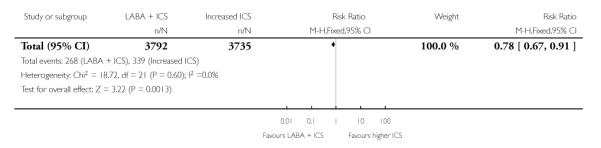
|
Analysis 2.11. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 11 # patients with exacerbations requiring oral steroids: sensitivity analysis by blinding
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 11 # patients with exacerbations requiring oral steroids: sensitivity analysis by blinding
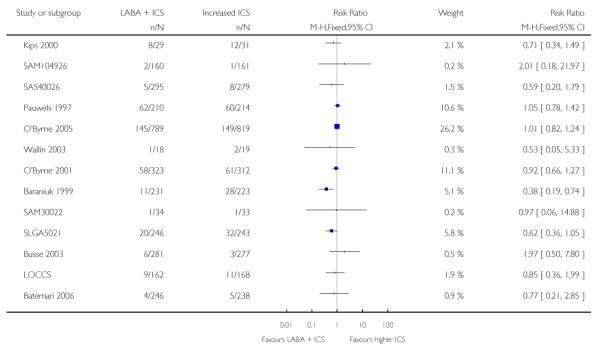
|
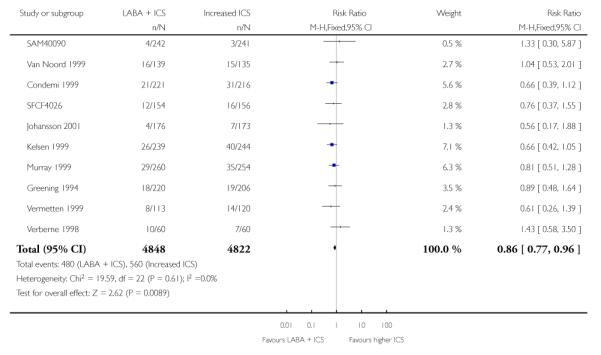
|
Analysis 2.12. Comparison 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses), Outcome 12 # patients with exacerbations requiring hospitalisation: children versus adults
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 2 LABA + ICS versus higher dose ICS (subgroup and sensitivity analyses)
Outcome: 12 # patients with exacerbations requiring hospitalisation: children versus adults
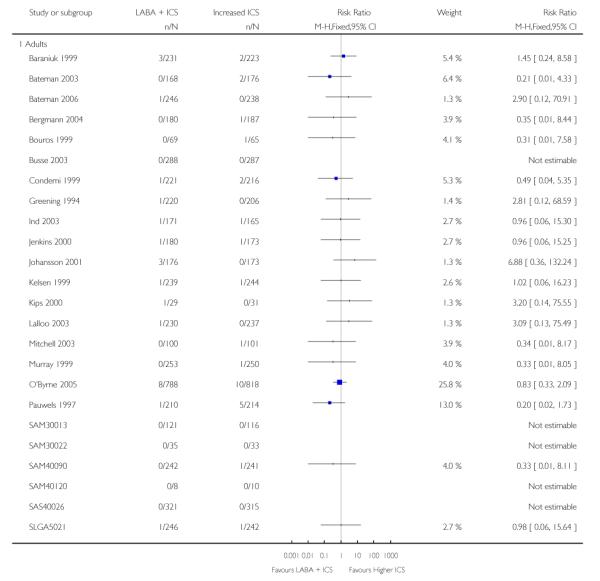
|
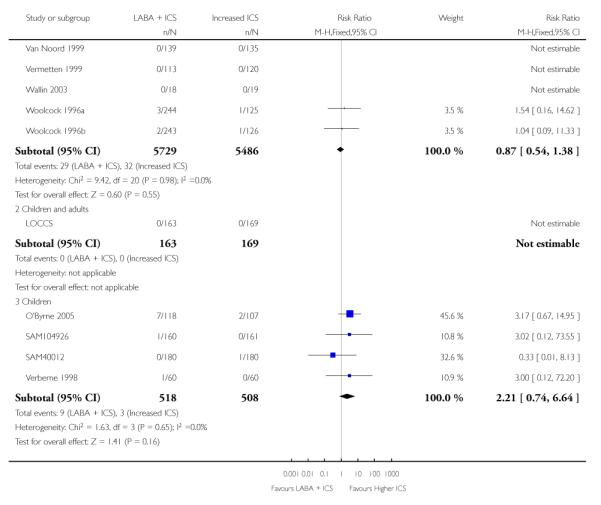
|
Analysis 3.1. Comparison 3 WMD archive, Outcome 1 FEV1 (L) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 1 FEV1 (L) at endpoint
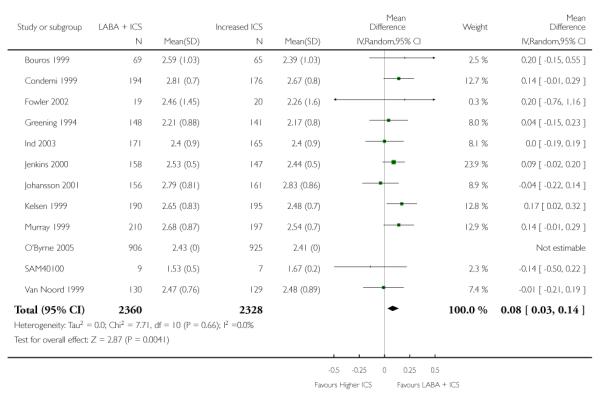
|
Analysis 3.2. Comparison 3 WMD archive, Outcome 2 FEV1 (% predicted) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 2 FEV1 (% predicted) at endpoint
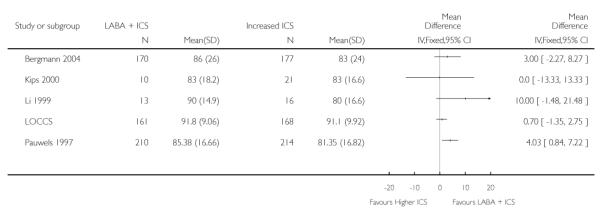
|
Analysis 3.3. Comparison 3 WMD archive, Outcome 3 Change in FEV1 (L) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 3 Change in FEV1 (L) at endpoint
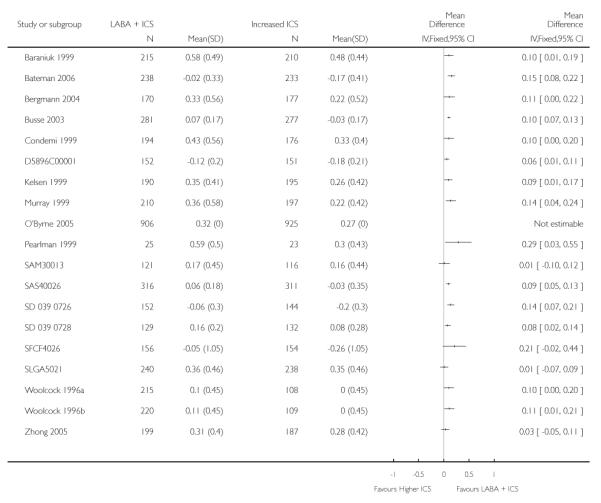
|
Analysis 3.4. Comparison 3 WMD archive, Outcome 4 Change in FEV1 (L) stratifying on treatment period
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 4 Change in FEV1 (L) stratifying on treatment period
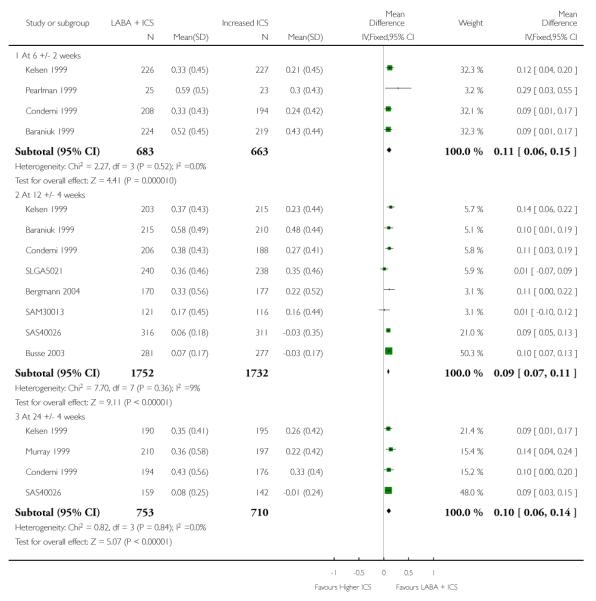
|
|
Analysis 3.5. Comparison 3 WMD archive, Outcome 5 Morning PEF (L/min) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 5 Morning PEF (L/min) at endpoint
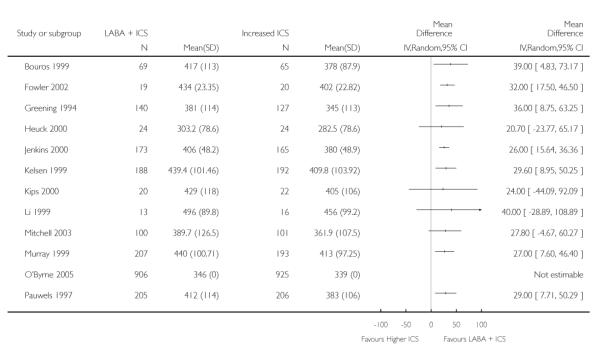
|
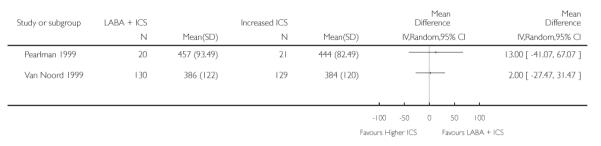
|
Analysis 3.6. Comparison 3 WMD archive, Outcome 6 Evening PEF (L/min) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 6 Evening PEF (L/min) at endpoint
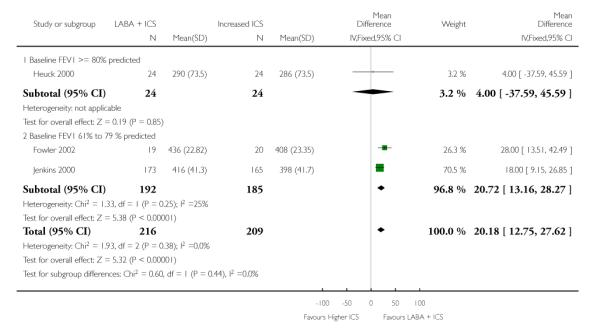
|
Analysis 3.7. Comparison 3 WMD archive, Outcome 7 Change in morning or clinic PEF (L/min) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 7 Change in morning or clinic PEF (L/min) at endpoint
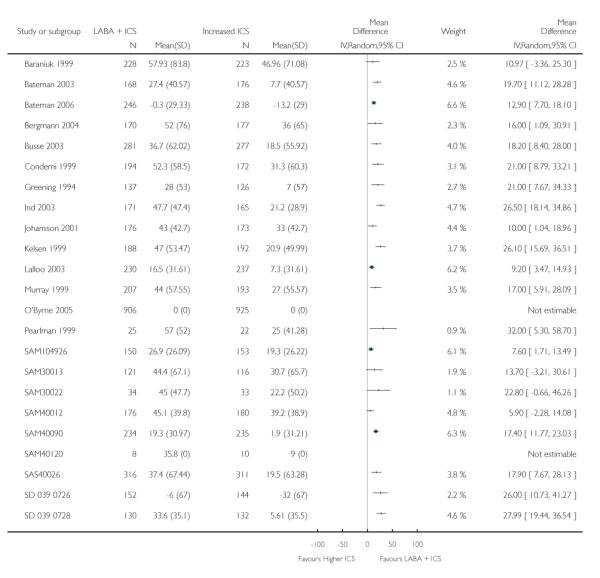
|
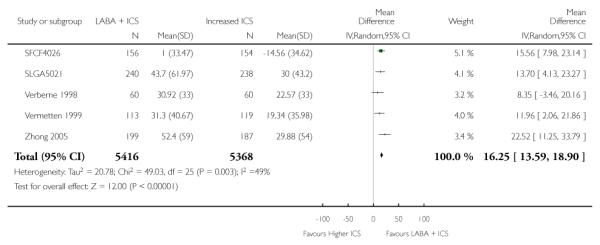
|
Analysis 3.8. Comparison 3 WMD archive, Outcome 8 Change in evening PEF (L/min) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 8 Change in evening PEF (L/min) at endpoint
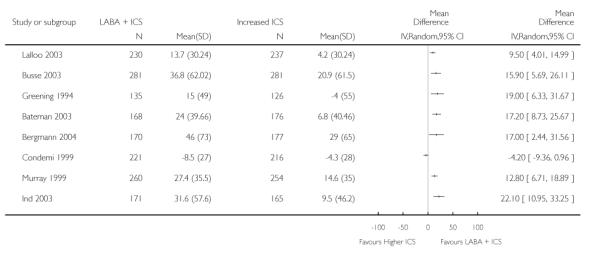
|
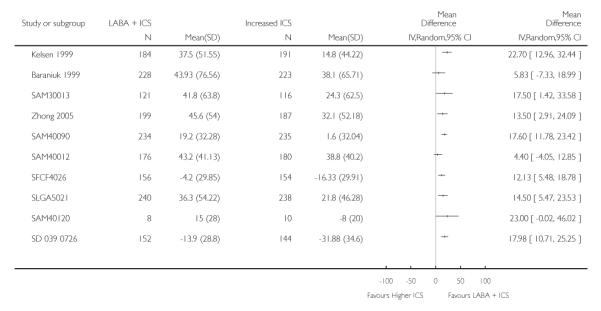
|
Analysis 3.9. Comparison 3 WMD archive, Outcome 9 Change in FEV1 (% predicted) at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 9 Change in FEV1 (% predicted) at endpoint
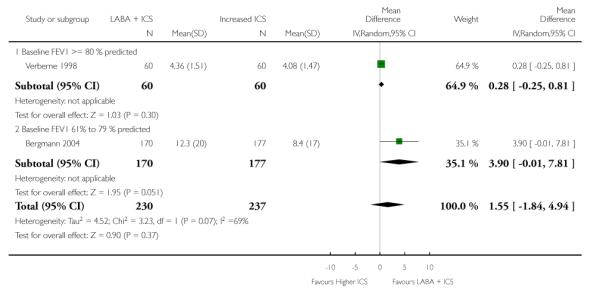
|
Analysis 3.10. Comparison 3 WMD archive, Outcome 10 Change in % symptom-free days at endpoint
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 10 Change in % symptom-free days at endpoint
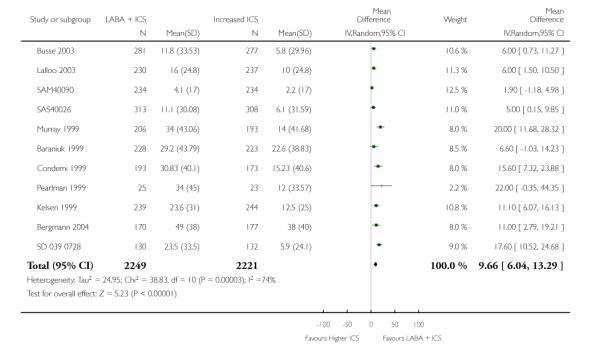
|
Analysis 3.11. Comparison 3 WMD archive, Outcome 11 # patients with exacerbations requiring oral steroids
Review: Addition of long-acting beta2-agonists to inhaled steroids versus higher dose inhaled steroids in adults and children with persistent asthma
Comparison: 3 WMD archive
Outcome: 11 # patients with exacerbations requiring oral steroids
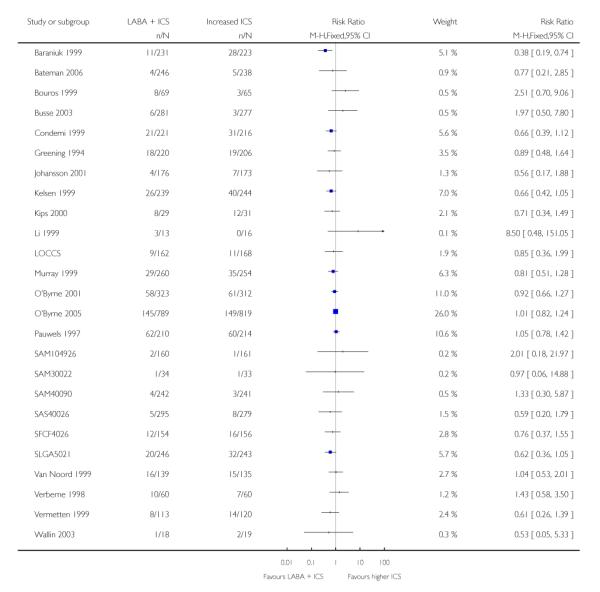
|
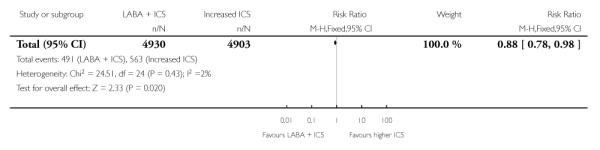
|
Appendix 1. 2009 update: new studies included
Bateman 2006; D5896C00001; Green 2006; Joshi 2005; LOCCS; O’Byrne 2005; SAM30013; SAM30022; SAM40012; SAM40090;SAM40120; SAS40013; SAS40026; SD 039 0726; SD 039 0728; SFCF4026; SLGA5021; Zhong 2005.
Appendix 2. Assessment of study quality
Assessment of methodological quality
Studies to be included underwent quality assessment, performed independently by two reviewers (IRG or MNC and FMD), using two methods. First, using the Cochrane approach to assess allocation of concealment, trials were scored using the following principles:
Grade A: Adequate concealment
Grade B: Unclear concealment
Grade C: Clearly inadequate concealment
In addition, each study was assessed using a 0 to 5 scale described by Jadad 1996 and summarised as follows:
Was the study described as randomised (1 = yes; 0 = no)?
Was the study described as double-blind (1 = yes; 0 = no)?
Was there a description of withdrawals and dropouts(1 = yes; 0 = no)?
Was the method of randomisation well described and appropriate (1 = yes; 0 = no)?
Was the method of double blinding well described and appropriate (1 = yes; 0 = no)?
Deduct one point if methods for randomisation or blinding were inappropriate.
Appendix 3. GSK randomisation procedures
The procedures for randomising GSK sponsored studies has been detailed in correspondence between Richard Follows and TL, the details of which are given below:
The randomisation software is a computer-generated, centralised programme (RandAll). After verification that the randomisation sequence is suitable for the study design (cross-over, block or stratification), Clinical Supplies then package the treatments according the randomisation list generated. Concealment of allocation is maintained by a third party, since the sites phone in and are allocated treatments on that basis. Alternatively a third party may dispense the drug at the sites. Unblinding of data for interim analyses can only be done through RandAll, and is restricted so that only those reviewing the data are unblinded to treatment group allocation.
HISTORY
Protocol first published: Issue 1, 2000
Review first published: Issue 4, 2005
| Date | Event | Description |
|---|---|---|
| 21 April 2008 | Amended | Converted to new review format. |
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
We have adopted a risk of bias assessment rather than using Jadad scores as a basis for judging the degree to which the design of the eligible studies protects against bias.
WHAT’S NEW
Last assessed as up-to-date: 25 June 2008.
| Date | Event | Description |
|---|---|---|
| 26 June 2008 | New citation required and conclusions have changed | 18 new studies included in the review (see Appendix 1). We obtained unpublished and published data on exacerbations requiring steroids and hospitalisation; lung function (am PEF; pm PEF; FEV1); symptoms; rescue medication use and adverse events We applied the Cochrane Collaboration ‘Risk of bias’ tool to the studies included in the review. Generic inverse variance has also been used to calculate effect estimates for continuous data where only mean differences and 95% confidence intervals or standard errors were available in the original trial reports The addition of evidence from the new studies and the incorporation of unpublished data from the original studies tightened the confidence interval around the pooled estimate of the primary outcome. The previous effect estimate was borderline non-statistically significant (risk ratio 0.88, P = 0.08). The estimate became statistically significant with the new data (risk ratio 0.88, P = 0.02) |
| 2 May 2008 | New search has been performed | Literature searches re-run. |
Footnotes
DECLARATIONS OF INTEREST In the past five years, Francine Ducharme received some research funding from Glaxo Wellcome and Merck and gave CME conferences supported by Merck Frost. No conflict of interest reported by Muireann Ni Chroinin, Ilana Greenstone, Toby Lasserson, A Danish, H Magdalinos, V Masse and M Julien.
References to studies included in this review
- Baraniuk 1999 {published data only} .Baraniuk J, Murray JJ, Nathan RA, Berger WE, Johnson M, Edwards LD, et al. Fluticasone alone or in combination with salmeterol versus triamcinolone in asthma. Chest. 1999;116(3):625–32. doi: 10.1378/chest.116.3.625. [DOI] [PubMed] [Google Scholar]; Cook D, Srebro SH, Rogenes PR, Rickard K, Edwards L, Johnson MC. A comparison of the safety and efficacy of fluticasone, triamcinolone, and fluticasone plus salmeterol in patients with mild to moderate asthma. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A416. [Google Scholar]; *; Johnson MC, Srebro SH, Rogenes PR, Rickard K, Edwards L. A comparison of physician-rated and patient-rated outcomes in a study with fluticasone, triamcinolone, and fluticasone plus salmeterol. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A414. [Google Scholar]
- Bateman 2003 {published and unpublished data} .Bateman ED, Bantje TA, Gomes MJ, Toumbis MG, Huber RM, Naya I, et al. Combination therapy with a single inhaler budesonide/formoterol compared with high dose fluticasone propionate alone in patients with moderate persistent asthma. American Journal of Respiratory Medicine. 2003;2(3):275–81. doi: 10.1007/BF03256655. [DOI] [PubMed] [Google Scholar]; Bateman ED, Bantje TA, Joao Gomes M, Toumbis M, Huber R, Eliraz A. Early and sustained benefits of budesonide and formoterol in a single inhaler versus fluticasone in moderate asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):157s. [Google Scholar]; Bateman ED, Bantje TA, Joao Gomes M, Toumbis M, Huber R, Eliraz A, et al. Symbicort (budesonide/ eformoterol) turbohaler controls asthma more effectively than fluticasone diskus. Thorax. 2001;Vol. 56(issue Suppl 3):iii 63. [Google Scholar]; Ericsson K, Bantje TA, Huber H, Borg S. Symbicort® turbuhaler® is more cost effective than fluticasone diskus™ in the treatment of asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; Ericsson K, Bantje TA, Huber R, Borg S, Anderson F. Cost-effectiveness of budesonide and formoterol in a single inhaler compared to fluticasone in the treatment of asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):157s. [Google Scholar]; Ericsson K, Bantje TA, Huber RM, Borg S, Bateman ED. Cost-effectiveness analysis of budesonide/formoterol compared with fluticasone in moderate-persistent asthma. Respiratory Medicine. 2006;100(4):586–94. doi: 10.1016/j.rmed.2005.09.032. [DOI] [PubMed] [Google Scholar]; *; SD-039-0618 Efficacy of Symbicort Turbuhaler® compared with fluticasone Diskus in asthmatic patients. 2005 http://www.astrazeneca.com.
- Bateman 2006 {published and unpublished data} .Bateman E, Atienza T, Mihaescu T, Duggan M, Jacques L, Goldfrad C. Asthma control is maintained if treatment with fluticasone propionate/salmeterol (FSC; Advair®/ Seretide®) is stepped down. Annual American Thoracic Society 101st International Conference.2005. p. C12. [Google Scholar]; Bateman ED, Jacques L, Goldfrad C, Atienza T, Mihaescu T, Duggan M. Asthma control can be maintained when fluticasone propionate/salmeterol in a single inhaler is stepped down. Journal of Allergy and Clinical Immunology. 2006;117(3):563–70. doi: 10.1016/j.jaci.2005.11.036. [DOI] [PubMed] [Google Scholar]; *; Glaxo Smith Kline (SAS30040) A 12-week, randomised, double-blind, parallel-group study to compare the efficacy and tolerability of salmeterol/fluticasone propionate combination 50/100mcg bd with fluticasone propionate 250mcg bd, all via the DISKUS™/ACCUHALER™ on maintaining asthma control in moderate persistent asthmatic subjects whose symptoms have been well-controlled following an initial maintenance therapy with salmeterol/fluticasone propionate 50/250mcg combination twice-daily for 12 weeks. 2005 http://www.ctr.gsk.co.uk.
- Bergmann 2004 {published and unpublished data} .Bergmann KC, Lindemann L, Braun R, Steinkamp G. Salmeterol/fluticasone propionate (50/250 mug) combination is superior to double dose fluticasone (500 mug) for the treatment of symptomatic moderate asthma: a prospective, double-blind trial. Swiss Medical Weekly. 2004;134(3-4):50–8. doi: 10.4414/smw.2004.10403. [DOI] [PubMed] [Google Scholar]; *; Glaxo Smith Kline (SAS40009) A multi-centre, randomised, double-blind, parallel group comparison of the salmeterol/ fluticasone propionate combination product (50/250μg) via Diskus twice daily versus fluticasone propionate (500μg) via Diskus twice daily in patients with moderate asthma (SAS 40009 local German study) 2005 http://www.ctr.gsk.co.uk.
- Bouros 1999 {published data only} .Bouros D, Bachlitzanakis N, Kottakis J, Pfister P, Polychronopoulos V, Papadakis E, et al. Foromoterol and beclomethasone versus higher dose beclomethasone as maintenance therapy in adult asthma. European Respiratory Journal. 1999;14(3):627–32. doi: 10.1034/j.1399-3003.1999.14c24.x. [DOI] [PubMed] [Google Scholar]
- Busse 2003 {published and unpublished data} .Busse W, Koenig SM, Oppenheimer J, Sahn SA, Yancey SW, Reilly D, et al. Steroid-sparing effects of fluticasone propionate 100mcg and salmeterol 50mcg administered twice daily in a single product in patients previously controlled with fluticasone propionate 250mcg administered twice daily. Journal of Allergy and Clinical Immunology. 2003;111(2):57–65. doi: 10.1067/mai.2003.38. [DOI] [PubMed] [Google Scholar]; Dorinsky P, Yancey S, Reilly D, Edwards L, Rickard K, Nelson H. Effect of fluticasone propionate (FP)/salmeterol 100/50mcg or FP 250mcg on small airway function. European Respiratory Journal. 2003;22(Suppl 22):260s. [Google Scholar]; Dorinsky P, Yancey S, Reilly D, Edwards L, Rickard K, Nelson H. Long-term effectiveness of the fluticasone propionate/salmeterol (FSC) combination product as an inhaled corticosteroid-sparing agent. Journal of Allergy and Clinical Immunology. 2003;11(2):125s. [Google Scholar]; Glaxo Smith Kline (SAS40027) A randomized, double-blind, parallel group, comparative trial of fluticasone propionate/salmeterol combination product 100/50mcg DISKUS inhaler BID versus fluticasone propionate 250mcg DISKUS inhaler BID in adolescents and adults with moderate persistent asthma. 2005 http://www.ctr.gsk.co.uk.; Matz J, Kalberg C, Emmett A, Yancey S, Dorinsky P, Rickard K. The combination of salmeterol and low-dose fluticasone versus higher-dose fluticasone: an analysis of exacerbations. American Academy of Allergy, Asthma and Immunology; 2000. [DOI] [PubMed] [Google Scholar]; *; Sahn S, Yancey S, Reilly D, Edwards L, Rickard K, Dorinsky P. The fluticasone propionate/salmeterol (FSC) combination product 100/50 mcg BID is steroid sparing in patients who require FP250 mcg BID for asthma stability. Chest 2002 (conference); San Diego, CA. 2002. [Google Scholar]
- Condemi 1999 {published and unpublished data} .Baker J, Yancey S, Kalberg C, Petrocella V, Emmett A, Bowers B, et al. Added salmeterol versus increased-dose fluticasone in patients symptomatic on low-dose fluticasone. American Journal of Respiratory and Critical Care Medicine. 1998;157(Suppl 3):A406. [Google Scholar]; Condemi JJ, Goldstein S, Kalberg C, Yancey S, Emmett A, Rickard K. The addition of salmeterol to fluticasone propionate versus increasing the dose of fluticasone propionate in patients with persistent asthma. Annals of Allergy, Asthma, and Immunology. 1999;82(107):383–89. doi: 10.1016/s1081-1206(10)63288-7. [DOI] [PubMed] [Google Scholar]; Glaxo Smith Kline (SLGA5022) A randomised, double-blind clinical trial comparing the efficacy and safety of salmeterol xinafoate 42mcg b.i.d.* plus fluticasone propionate 88mcg b.i.d.* versus fluticasone propionate 220mcg b.i.d.* alone in subjects with asthma not well controlled on fluticasone propionate 88mcg b.i.d.*(*Doses quoted are ex-actuator: equivalent ex-valve doses are 50mcg, 100mcg and 250mcg, respectively) 2005 http://ctr.gsk.co.uk.; *; Matz J, Emmett A, Rickard K, Kalberg C. Addition of salmeterol to low-dose fluticasone versus higher-dose fluticasone: an analysis of asthma exacerbations. Journal of Allergy and Clinical Immunology. 2001;107(5):783–9. doi: 10.1067/mai.2001.114709. [DOI] [PubMed] [Google Scholar]
- D5896C00001 {unpublished data only} .AstraZeneca (D5896C00001) [accessed 30 April 2008];A randomized, double-blind, active-controlled, parallel-group, single dummy, multicenter, 12 week study to assess the efficacy and safety ofSYMBICORT® pMDI 160/4.5 μg x 2 actuations once-daily (qd) compared to SYMBICORT pMDI 80/4.5 μg x 2 actuations qd, SYMBICORT pMDI80/4.5 μg x 2 actuations twice-daily (bid) and to budesonide pMDI 160 μg x 2 actuations qd in asthmatic subjects 12 years of age and older. 2007 http://www.astrazenecaclinicaltrials.com.
- Fowler 2002 {published data only} .Fowler SJ, Currie PC, Lipworth BJ. Step down therapy with low dose fluticasone-salmeterol combination or medium dose hydrofluoroalkane 134a-beclomethasone alone. Journal Allergy and Clinical Immunology. 2002;109(6):929–35. doi: 10.1067/mai.2002.123869. [DOI] [PubMed] [Google Scholar]
- Green 2006 {published and unpublished data} .Green RH, Brightling CE, McKenna S, Hargadon B, Neale N, Parker D, et al. Comparison of asthma treatment given in addition to inhaled corticosteroids on airway inflammation and responsiveness. European Respiratory Journal. 2006;27(6):1144–51. doi: 10.1183/09031936.06.00102605. [DOI] [PubMed] [Google Scholar]; Green RH, Brightling CE, McKenna S, Hargadon B, Parker D, Wardlaw AJ, et al. A placebo controlled comparison of formoterol, montelukast or higher dose of inhaled corticosteroids in subjects with symptomatic asthma despite treatment with low dose inhaled corticosteroids. Thorax. 2002;Vol. 57(issue Suppl III):iii 11. [Google Scholar]; *; Green RH, Brightling CE, McKenna S, Hargadon B, PArker D, Pavord ID. A placebo controlled comparison of formoterol, montelukast or higher dose of inhaled budesonide in subjects with symptomatic asthma despite treatment with low dose inhaled budesonide. American Thoracic Society 99th International Conference; Poster H82; 2003. [Google Scholar]
- Greening 1994 {published and unpublished data} .Glaxo Smith Kline (SLGQ85) A phase IV, multi-centre, double-blind, double-dummy, parallel group study to determine whether adult asthmatic patients, currently symptomatic on 400mcg daily inhaled corticosteroid therapy, are better maintained by an increase in corticosteroid dose to 1000mcg daily beclomethasone dipropionate (Becloforte) or by the combined therapy of salmeterol xinafoate (Serevent) 50mcg twice daily plus 400mcg daily inhaled beclomethasone dipropionate (Becotide) 2006 http://www.ctr.gsk.co.uk.; Greening AP, Ind PW, Northfield M, Shaw G. Added salmeterol versus higher-dose corticosteroid in asthma patients with symptoms on existing inhaled corticosteroid. Lancet. 1994;344(8891):219–24. doi: 10.1016/s0140-6736(94)92996-3. [DOI] [PubMed] [Google Scholar]; *; Hyland ME, Crocker GR. Validation of an asthma quality of life diary in a clinical trial. Thorax. 1995;50(7):724–30. doi: 10.1136/thx.50.7.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuck 2000 {published data only} .Heuck C, Heickendorff L, Wolthers OD. A randomized controlled trial of short term growth and collagen turnover in asthmatics with inhaled formoterol and budesonide. Archives of Disease in Childhood. 2000;83:334–9. doi: 10.1136/adc.83.4.334. [DOI] [PMC free article] [PubMed] [Google Scholar]; Heuck C, Heickendorff L, Wolthers OD, Sygehus S. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Short term growth and collagen turnover in asthmatics treated inhaled formoterol and budesonide; p. 364. [Google Scholar]
- Ind 2003 {published and unpublished data} .Glaxo Smith Kline (SLGQ97) A multi-centre double-blind, parallel group study to evaluate the relative clinical benefits of three treatment interventions: i) salmeterol xinafoate 50 mcg bd plus fluticasone propionate 250 mcg bd; ii) fluticasone propionate 500 mcg bd; iii) fluticasone propionate 250 mcg bd, in adult asthmatic subjects poorly controlled on current inhaled corticosteroids. 2005 http://ctr.gsk.co.uk.; Ind PW, Dal Negro R, Colman N, Fletcher CP, Browning DC, James MH. Inhaled fluticasone propionate and salmeterol in moderate adult asthma I: lung function and symptoms. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A416. [Google Scholar]; Ind PW, Dal Negro R, Colman N, Fletcher CP, Browning DC, James MH. Inhaled fluticasone propionate and salmeterol in moderate adult asthma II: exacerbations. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A415. [Google Scholar]; Ind PW, Dal Negro R, Colman NC, Fletcher CP, Browning D, James MH. Addition of salmeterol to fluticasone propionate treatment in moderate to severe asthma. Respiratory Medicine. 2003;97(5):555–6. doi: 10.1053/rmed.2003.1483. [DOI] [PubMed] [Google Scholar]; *; Ind PW, Dal Negro R, Fletcher CP, Browning DC, James MH. Inhaled salmeterol and fluticasone propionate therapy in moderate adult asthma. European Respiratory Journal. 1997;10:1S. doi: 10.1053/rmed.2003.1483. [DOI] [PubMed] [Google Scholar]
- Jenkins 2000 {published and unpublished data} .Becker I, Kielborn A, Price MJ, Volmer T, Lloyd AC. European Respiratory Society. 9-13. Madrid, Spain: Oct, 1999. Cost-effectiveness of salmeterol/fluticasone combination product and budesonide in asthma patients in Germany; p. 854. 1999. [Google Scholar]; Glaxo Smith Kline (SAS40006) A randomised, double-blind, double-dummy, parallel group comparison of Seretide Diskus/Accuhaler (50/250μg strength) b.i.d. with budesonide 800μg b.i.d. in adolescents and adults with reversible airways obstruction. 2005 http://www.clinicalstudyresults.org.; Jenkins C, Woolcock AJ, Saarelainen P, Lundbaack B, James MH. Salmeterol/fluticasone propionate combination therapy 50/250mcgs twice daily is more effective than budesonide 800 twice daily in treating moderate to severe asthma. Respiratory Medicine. 2000;94(7):715–23. doi: 10.1053/rmed.2000.0875. [DOI] [PubMed] [Google Scholar]; Jenkins C, Woolcock A, James M. Superior overall control of moderate to severe asthma with salmeterol/fluticasone propionate (FP) combination (50/250 mcg bd) compared with three-fold-higher dose of budesonide (800mcg bd) European Respiratory Journal. 2000;Vol. 16(issue Suppl 31):456s. [Google Scholar]; Lundback B, Jenkins C, Price MJ, Thwaites RM. Cost-effectiveness of salmeterol/fluticasone propionate combination product 50/250 microg twice daily and budesonide 800 microg twice daily in the treatment of adults and adolescents with asthma. Respiratory Medicine. 2000;94(7):724–32. doi: 10.1053/rmed.2000.0876. [DOI] [PubMed] [Google Scholar]; Lundback B, Ronmark E, Jonsson AC. Treatment effectiveness and exacerbations during one year with Seretide compared to fluticasone propionate and salmeterol in mild to moderate asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):176s. [Google Scholar]; *; Parnaby A, Lloyd A, Browning D, McCarthy TP. A comparison of the cost-effectiveness of salmeterol/ fluticasone combination inhaler and budesonide in the management of asthma. Thorax. 55(Suppl 3, issue):A64. Vol. [Google Scholar]
- Johansson 2001 {published and unpublished data} .Glaxo Smith Kline (SAS40007) A randomised, double-blind, double-dummy, parallel-group comparison of Seretide Diskus/Accuhaler (50/100μg strength) twice daily (bid) with budesonide 400μg bid in adolescents and adults with reversible airways obstruction. 2005 http://www.clinicalstudyresults.org.; *; Johansson G, McIvor RA, D’Ambrosio FP, Gratziou C, James MH. Comparison of salmeterol/fluticasone propionate combination with budesonide in patients with mild-to-moderate asthma. Clinical Drug Investigation. 2001;21(9):633–42. [Google Scholar]
- Joshi 2005 {published data only} .Joshi J, Jagannath K, Chabbra S, Rajan S, Gogtay J, Po CJ, et al. Salmeterol/fluticasone combination product (SFC) provides better asthma control compared to highdose fluticasone (FP) in symptomatic patients with asthma. European Respiratory Journal. 2005;26(Suppl 49) Abstract No. 2771. [Google Scholar]
- Kelsen 1999 {published and unpublished data} .Glaxo Smith Kline (SLGA5017) A comparison of adding Serevent versus doubling the dose of Beclovent in asthmatic subjects symptomatic on their existing inhaled corticosteroids. 2006 http//:ctr.gsk.co.uk.; *; Kelsen SG, Church NL, Gillman SA, Lanier BQ, Emmett AH, Rickard KA, et al. Salmeterol added to inhaled corticosteroids therapy is superior to doubling the dose of inhaled corticosteroids: a randomized clinical trial. Journal of Asthma. 1999;36(8):703–15. doi: 10.3109/02770909909055422. [DOI] [PubMed] [Google Scholar]
- Kips 2000 {published data only} .Kips JC, O’Connor BJ, Inman MD, Svenson K, Pauwels RA, O’Byrne PM. A long-term study of the antiinflammatory effect of low-dose budesonide plus formoterol versus high-dose budesonide in asthma. American Journal of Respiratory and Critical Care Medicine. 2000;161:996–1001. doi: 10.1164/ajrccm.161.3.9812056. [DOI] [PubMed] [Google Scholar]
- Lalloo 2003 {published and unpublished data} .Lalloo UG, Bantje TA, Kozma D, Krofta K, Ankerst J, Johansen B, et al. Low-dose Symbicort (budesonide/ formoterol) is more effective than double-dose inhaled corticosteroid in mild asthma. Allergy Clinical Immunology International. 2000;(Suppl 2, issue):122. Vol. [Google Scholar]; Lalloo UG, Malolepsky J, Kozma D, Krofta K, Ankerst J, Johansen B, et al. Budesonide and formoterol in a single inhaler controls exacerbations more effectively than a higher dose of inhaled corticosteroids alone, in mild-moderate persistent asthma. European Respiratory Journal. 2001;18(Suppl 33):43s. [Google Scholar]; Lalloo UG, Malolepszy D, Kozma K, Krofta J, Ankerst B, Johanasen NC, et al. Budesonide and formoterol in a single inhaler improves asthma control compared with increasing the dose of corticosteroid in adults with mild to moderate asthma. Chest. 2003;123(5):1480–7. doi: 10.1378/chest.123.5.1480. [DOI] [PubMed] [Google Scholar]; Lalloo UG, Malolepszy J, Kozma D, Krofta K, Ankerst J, Johansen B, et al. Budesonide and formoterol in a single inhaler is more effective than a higher dose of inhaled corticosteroid in mild-moderate persistent asthma. European Respiratory Journal. 2001;18(Suppl 33):159s. [Google Scholar]; Lalloo UG, Malolepszy J, Kozma D, Krofta K, Ankerst J, Johansen B, Thomson NC. Symbicort® (budesonide and formoterol in a single inhaler) is more effective than increasing the dose of inhaled corticosteroids in mild asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; *; SD-039-0348 Efficacy and safety of budesonide/formoterol Turbuhaler® (80/4.5 mcg b.i.d.) in steroid-using asthmatic adults. 2006 www.astrazeneca.com.
- Li 1999 {published data only} .Li X, Ward C, Thien F, Bish R, Bamford T, Bao X, Bailey M, Wilson JW, et al. An antiinflammatory effect of salmeterol, a long-acting B2-agonist, assessed in airway biopsies and bronchoalveolar lavage in asthma. American Journal of Respiratory and Critical Care Medicine. 1999;160(5):1493–9. doi: 10.1164/ajrccm.160.5.9811052. [DOI] [PubMed] [Google Scholar]; *; Reid DW, Ward C, Wang N, Zheng L, Bish R, Orsida B, Walters EH. Possible anti-inflammatory effect of salmeterol against interleukin-8 and neutrophil activation in asthma in vivo. European Respiratory Journal. 2003;21(6):994–9. doi: 10.1183/09031936.03.00109702. [DOI] [PubMed] [Google Scholar]
- LOCCS {published data only} .American Lung Association Asthma Clinical Research Randomized comparison of strategies for reducing treatment in mild persistent asthma. New England Journal of Medicine. 2007;356(20):2027–39. doi: 10.1056/NEJMoa070013. [DOI] [PubMed] [Google Scholar]
- Mitchell 2003 {published data only} .Mitchell C, Jenkins C, Scicchitano R, Rubinfeld A, Kottakis J. Formoterol (Foradil) and medium-high doses of inhaled corticosteroids are more effective than high doses of corticosteroids in moderate-to-severe asthma. Pulmonary Pharmacology & Therapeutics. 2003;16(5):299–306. doi: 10.1016/s1094-5539(03)00071-3. [DOI] [PubMed] [Google Scholar]; *; Mitchell C, Jenkins C, Scicchitano R, Rubinfield A. Adding formoterol is more effective and safer than doubling the dose of inhaled steroids in moderately severe asthmatics. Respiratory and Critical Care Medicine. 2000;161(3):A197. [Google Scholar]
- Murray 1999 {published and unpublished data} .Glaxo Smith Kline (SLGA5018) A comparison of adding Serevent® versus doubling the dose of Beclovent® in asthmatic subjects symptomatic on their existing inhaled corticosteroids. 2006 http:www.ctr.gsk.co.uk.; *; Murray JJ, Church NL, Anderson WH, Bernstein DI, Wenzel SE, Emmett A, et al. Concurrent use of salmeterol with inhaled corticosteroids is more effective than inhaled corticosteroid dose increases. Allergy and Asthma Proceedings. 1999;20(3):173–80. doi: 10.2500/108854199778553028. [DOI] [PubMed] [Google Scholar]
- O’Byrne 2001 {published data only} .AstraZeneca Unpublished data. 2008. (personal communication); Barnes PJ, O’Byrne PM, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Oxis and Pulmicort turbuhaler in the management of asthma OPTIMA international study group. Treatment of mild persistent asthma with low doses of inhaled budesonide alone or in combination with formoterol. Thorax. 2000;55(Suppl 3):A4. [Google Scholar]; Barnes PJ, O’Byrne PM, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Treatment of mild persistent asthma with low doses of inhaled budesonide alone or in combination with formoterol. For the Oxis and Pulmicort Turbuhaler in the Management of Asthma (OPTIMA) international study group. Thorax. 2000;Vol. 55(issue Suppl 3):s5. [Google Scholar]; Grosser D, Smith B. Low-dose budesonide improved asthma control in mild asthma; adding formoterol improved control in corticosteroid-treated patients. ACP Journal Club. 2002;137(1):19. [PubMed] [Google Scholar]; Jönsson BG, Berggren FE, Svensson K, O’Byrne PM. Budesonide and formoterol in mild persistent asthma compared with doubling the dose of budesonide - a cost-effectiveness analysis. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):517s. [Google Scholar]; Jönsson BG, Berggren FE, Svensson K, O’Byrne PM. Economic results of adding formoterol to budesonide in mild persistent asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):331s. [Google Scholar]; O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, Runnerstrom E, Sandstrom T, Svensson K, et al. Low dose inhaled budesonide and formoterol in mild persistent asthma: the OPTIMA randomized trial. American Journal of Respiratory and Critical Care Medicine. 2001;164(8):1392–7. doi: 10.1164/ajrccm.164.8.2104102. [DOI] [PubMed] [Google Scholar]; *; O’Byrne PM, Barnes PJ, Rodriguez-Roisin R, Sandtröm T, Tattersfield AE, Runnerström EM, et al. Addition of formoterol Turbuhaler® to budesonide Tubuhaler® is safe and well tolerated in the long-term treatment of mild asthma: results from the OPTIMA trial. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):330s. [Google Scholar]
- O’Byrne 2005 {published and unpublished data} .Bruce SA, Scherer YK. Maintenance and symptom relief with budesonide plus formoterol reduced severe asthma exacerbations. Evidence-Based Nursing. 2005;8(3):78. doi: 10.1136/ebn.8.3.78. [DOI] [PubMed] [Google Scholar]; Jönsson BG, Berggren FE, Svensson K, O’Byrne PM. Budesonide and formoterol in mild persistent asthma compared with doubling the dose of budesonide - a cost-effectiveness analysis. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):517s. [Google Scholar]; Jönsson BG, Berggren FE, Svensson K, O’Byrne PM. Economic results of adding formoterol to budesonide in mild persistent asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):331s. [Google Scholar]; O’Byrne PM, Bisgaard H, Godard PP, Pistolesi M, Palmqvist M, Zhu Y, et al. Budesonide/formoterol combination therapy as both maintenance and reliever medication in asthma. American Journal of Respiratory & Critical Care Medicine. 2005;171(2):129–36. doi: 10.1164/rccm.200407-884OC. [DOI] [PubMed] [Google Scholar]; *; SD-039-673 Efficacy and safety of budesonide/formoterol (Symbicort) Turbuhaler® as single therapy in patients with mild-moderate asthma. Comparison with Symbicort Turbuhaler and Pulmicort® Turbuhaler as maintenance therapy, both complemented with Bricanyl® Turbuhaler (STAY) 2006 http://www.astrazenecaclinicaltrials.com.
- Ortega-Cisneros 1998 {published data only} .Ortega-Cisnero M, Maldonado-Alaniz ML, Rosas Vargas MA, Sierra-Monge JJL. Salmeterol and inhaled beclomethasone versus high dose inhaled beclomethasone in the control of pediatric patients with moderate asthma. Annals of Allergy, Asthma, and Immunology. 1998;Vol. 80:131. [Google Scholar]
- Pauwels 1997 {published data only} .AstraZeneca Unpublished data. 2008. (personal communication); Pauwels R. Additive effects of inhaled formoterol and budesonide in reducing asthma exacerbations. Allergy. 1998;53:20–3. doi: 10.1111/j.1398-9995.1998.tb04889.x. [DOI] [PubMed] [Google Scholar]; Pauwels RA, Lofdahl CG, Postma DA, Tattersfield AE, O’Byrne P, Barnes PJ, et al. Effect of inhaled formoterol and budesonide on exacerbations of asthma. New England Journal of Medicine. 1997;337(20):1405–11. doi: 10.1056/NEJM199711133372001. [DOI] [PubMed] [Google Scholar]
- Pearlman 1999 {published data only} .FLTA3015 [accessed 9 June 2008];A randomized, double-blind, placebo-controlled, parallel-group pilot trial evaluating safety and efficacy of salmeterol xinafoate and fluticasone propionate individually and in combination in subjects with asthma. 2005 www.ctr.gsk.co.uk.; *; Pearlman DS, Stricker W, Weistein S, Gross G, Chervinsky P, Woodring A, et al. Inhaled salmeterol and fluticasone: a study comparing monotherapy and combination therapy in asthma. Annals of Allergy, Asthma, and Immunology. 1999;82:257–65. doi: 10.1016/S1081-1206(10)62606-3. [DOI] [PubMed] [Google Scholar]
- SAM104926 {published data only} .Glaxo Smith Kline (SAM104926) [accessed 14 January 2008];A multicentre, randomised, double-blind, double dummy, parallel group study to compare the salmeterol/fluticasone propionate combination (SERETIDE) at a dose of 50/100mcg twice daily and fluticasone propionate (FLIXOTIDE) at a dose of 200mcg twice daily, both delivered via a dry powder inhaler (DISKUS) for 12 weeks in asthma in children aged 4-11 years not controlled by inhaled corticosteroids alone at medium dose. 2007 http://ctr.gsk.co.uk.
- SAM30013 {unpublished data only} .Boulet LP, Chapman K, Roberts J, Watson EG. Efficacy of salmeterol/fluticasone propionate HFA MDI versus high dose fluticasone propionate HFA MDI in adolescent and adult asthma. Poster European Respiratory Society Meeting.2003. [Google Scholar]; *; Glaxo Smith Kline (SAM30013) A 12 week, randomized, double-blind, parallel group study to compare the efficacy and safety of salmeterol/fluticasone propionate/ GR106642X (25/50 μg x 2 inhalations) bid with fluticasone propionate (125 μg x 2 inhalations) bid in adolescent and adult patients with mild to moderate asthma. 2005 http://www.ctr.gsk.co.uk.
- SAM30022 {unpublished data only} .Glaxo Smith Kline (SAM30022) A phase IV, multi-centre, double-blind, double-dummy, parallel group, randomised study comparing Seretide (25/50 2 puffs bd) via the Evohaler (MDI-HFA) with Beclometasone dipropionate (200mcg 2 puffs bd) via the MDI-CFC in adolescents and adults experiencing moderate symptoms of reversible airways obstruction. 2005 http://www.ctr.gsk.co.uk.
- SAM40012 {unpublished data only} .Dorinsky P, Emmett A, Sutton L. Reduced risk for asthma exacerbations in pediatric patients receiving salmeterol plus inhaled corticosteroids (ICS) vs ICS alone [Abstract] European Respiratory Journal. 2004;24(Suppl 48):308s. [Google Scholar]; *; Glasxo Smith Kline (SAM40012) [accessed 30 April 2008];A multicentre, randomised, double-blind, double-dummy, parallel group comparison of three treatments: 1) salmeterol/fluticasone propionate (SFC) (50/100mcg strength) bd via DISKUS/ ACCUHALER inhaler, 2) fluticasone propionate 200mcg bd via DISKUS/ACCUHALER inhaler, 3) fluticasone propionate 100mcg bd via DISKUS/ACCUHALER inhaler in children aged 4-11 years with asthma. 2005 http://www.ctr.gsk.co.uk.
- SAM40090 {unpublished data only} .*; Glaxo Smith Kline (SAM40090) A twelve week multi-centre, randomised, double-blind, parallel group, comparative trial of Advair 50/100 mcg Diskus inhalation device BID versus Flovent 250 mcg Diskus inhalation device BID in adolescents and adults with persistent asthma (Program of Advair Control and Effectiveness - Advair Low Dose [PACE-ALD]) 2005 http://www.ctr.gsk.co.uk.
- SAM40100 {unpublished data only} .Glaxo Smith Kline (SAM40100) [accessed 4 January 2008];Randomised, double-blind, comparator study to demonstrate the superiority of salmeterol/fluticasone propionate combination DISKUS™ 50/100mcg bd over fluticasone propionate DISKUS™/ ACCUHALER™ 200mcg bd with respect to airway physiology in asthmatic children treated for 6 weeks. 2006 http://ctr.gsk.co.uk.
- SAM40120 {unpublished data only} .Glaxo Smith Kline (SAM40120) A phase IV, multi-centre, double-blind, parallel group, randomised study comparing Seretide (50/100mcg bd) via the Evohaler (MDI-HFA) with Flixotide (250mcg bd) via the Evohaler (MDI-HFA) in asthmatics with significant smoking history. 2005 http://www.ctr.gsk.co.uk.
- SAS40013 {unpublished data only} .Galxo Smith Kline (SAS40013) Can the serum level of eosinophil cationic protein (ECP) give directions for the choice between increasing the dose of fluticasone propionate or the addition of salmeterol in patients with symptomatic asthma? 2005 http://www.ctr.gsk.co.uk.
- SAS40026 {published and unpublished data} .Bloom J, Calhoun W, König S, Yancey S, Reilly D, Edwards L, et al. Fluticasone propionate/salmeterol 100/50mcg is inhaled steroid sparing in patients who required fluticasone propionate 250mcg for asthma stability. American Thoracic Society 99th International Conference; Poster C33; 2003. [Google Scholar]; Dorinsky P, Yancey S, Reilly D, Stauffer J, Edwards L, Sutton L. Control of airway inflammation is maintained in asthma patients following a reduction in ICS dose with fluticasone propionate/salmeterol (FSC) compared with higher dose fluticasone propionate (FP) alone. European Respiratory Journal. 2004;24(Suppl 48):308s. [Google Scholar]; Glaxo Smith Kline (SAS40026) A randomized, double-blind, parallel group, comparative trial of fluticasone propionate/salmeterol combination product 100/50mcg DISKUS† inhaler BID versus fluticasone propionate 250mcg DISKUS inhaler BID in adolescents and adults with moderate persistent asthma. 2006 http://ctr.gsk.co.uk.; Jarjour NN, Wilson SJ, Koenig SM, Laviolette M, Moore WC, Davis WB, et al. Control of airway inflammation maintained at a lower steroid dose with 100/50 microg of fluticasone propionate/salmeterol. Journal of Allergy and Clinical Immunology. 2006;118(1):44–52. doi: 10.1016/j.jaci.2006.03.043. [DOI] [PubMed] [Google Scholar]; Stauffer J, Yancey S, Waitkus-Edwards K, Edwards L, Dorinsky P. Clinical markers of worsening asthma with the fluticasone/salmeterol 100/50mcg Diskus FSC vs fluticasone propionate (FP) 250mcg alone in patients requiring FP 250mcg BID for asthma stability. Annals of Allergy, Asthma and Immunology. 2004;92(1):144. [Google Scholar]; *; Wilson SJ, Rigden HM, Jarjour N, Laviolette M, Moore WC, Dorinsky PM, et al. Effect of switching from high dose fluticasone propionate (FP) to FP/salmeterol (FSC) on airway inflammation in asthma. European Respiratory Journal. 2004;24(Suppl 48):44s. [Google Scholar]
- SD 039 0726 {unpublished data only} .AstraZeneca (SD 039 0726) [accessed 30 April 2008];A twelve-week, randomized, double-blind, double-dummy, placebo- and active-controlled study of SYMBICORT® pMDI administered once daily in adults and adolescents with asthma. 2005 www.astrazenecaclinicaltrials.com.; *; Berger WE, Bleecker ER, O’Dowd L, Miller CJ, Mezzanotte WS. [accessed 30 April 2008];Asthma control with once-daily budesonide/formoterol (BUD/FM) pressurized metered-dose inhaler. 2007 http://www.abstracts2view.com/ats07.
- SD 039 0728 {unpublished data only} .AstraZeneca (SD 039 0728) [accessed 30 April 2008];A 52-week, randomized, double-blind, single-dummy, parallel-group,multicenter Phase III study comparing the long-term safety of SYMBICORT® pMDI 160/4.5 μg x 4 actuations twice daily to SYMBICORT® pMDI 160/4.5 μg x 2 actuations twice daily and budesonide HFA pMDI 160 μg x 4 actuations twice daily in adult and adolescent subjects with asthma. 2006 www.astrazenecaclinicaltrials.com.; O’Brien CD, Peters SP, Prenner BM, Martin P. [accessed 30 April 2008];Resource use with budesonide/formoterol pressurized metered-dose inhaler (BUD/FM pMDI) versus BUD pMDI in asthma patients. 2007 http://www.abstracts2view.com/ats07.; Peters SP, Prenner BM, Martin P, O’Brien CD. [accessed 30 April 2008];Long-term effects on lung function of budesonide (BUD) and formoterol (FM) in one pressurized metered-dose inhaler (BUD/FM pMDI) and BUD pMDI in patients with asthma. 2007 http://www.abstracts2view.com/ats07.; Prenner BM, Peters SP, Martin P, O’Brien CD. [accessed 30 April 2008];Long-term control of asthma symptoms with budesonide/formoterol pressurized metered-dose inhaler (BUD/FM pMDI) versus BUD pMDI. 2007 http://www.abstracts2view.com/ats07.; Prenner BM, Peters SP, Martin P, O’Brien CD. [accessed 30 April 2008];Safety pharmacodynamics (PD) of budesonide/formoterol (BUD/FM) pMDI in asthma patients. 2007 http://www.abstracts2view.com/ats07.
- SFCF4026 {unpublished data only} .Glaxo Smith Kline (SFCF4026) Maintenance of asthma control in adults: comparison of three therapeutic strategies in patients whose asthma is controlled by a medium dose of inhaled corticosteroid and a long-acting inhaled beta2-agonist. 2005 http://www.ctr.gsk.co.uk.
- SLGA5021 {unpublished data only} .Glaxo Smith Kline (SLGA5021) A randomized, double-blind clinical trial comparing the efficacy and safety of salmeterol xinafoate 42mcg b.i.d.* plus fluticasone propionate 88mcg b.i.d.* versus fluticasone propionate 220mcg b.i.d.* alone in subjects with asthma not well controlled on fluticasone propionate 88mcg b.i.d.* (*Doses quoted are ex-actuator: equivalent ex-valve doses are 50mcg, 100mcg and 250mcg, respectively) 2005 http://www.ctr.gsk.co.uk.; Kalberg CJ, Nelson H, Yancey S, Petrocella V, Emmett AH, Rickard KA, et al. A comparison of added salmeterol versus increased-dose fluticasone in patients symptomatic on low-dose fluticasone [abstract] Journal of Allergy and Clinical Immunology. 1998;101(Suppl):6s. [Google Scholar]; Knobil K, Kalberg C, Emmett A, Rickard K. Adding salmeterol is more effective than increasing the dose of fluticasone for patients with asthma who are symptomatic on low dose fluticasone. European Respiratory Journal. 1998;12(supp 29):19s, P160. [Google Scholar]; *; Matz J, Emmett A, Rickard K, Kalberg C. Addition of salmeterol to low-dose fluticasone versus higher-dose fluticasone: an analysis of asthma exacerbations. Journal of Allergy and Clinical Immunology. 2001;107(5):783–9. doi: 10.1067/mai.2001.114709. [DOI] [PubMed] [Google Scholar]
- Van Noord 1999 {published data only} .Schreurs AJ, van Noord JA, Mulder PG. Fluticasone propionate and salmeterol xinafoate in patients with mild to moderate asthma. European Respiratory Journal. 1998;Vol. 12((Suppl 29), issue 19s):P159. [Google Scholar]; *; Van Noord JA, Schreurs AJM, Mol SJM, Mulder PGH. Addition of salmeterol versus doubling the dose of fluticasone propionate in patients with mild to moderate asthma. Thorax. 1999;54:207–12. doi: 10.1136/thx.54.3.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verberne 1998 {published and unpublished data} .Glaxo Smith Kline (SLGB4014 (SLPT15)) Placebo controlled study during one year comparing the addition of salmeterol with an increase of the dose of the inhaled corticosteroid in asthmatic children already on treatment with inhaled corticosteroids. 2006 http://ctr.gsk.co.uk.; *; Verberne AAPH, Frost C, Duiverman EJ, Grol MH, Kerribijn KF. Addition of salmeterol versus doubling the dose of beclomethasone in children with asthma. American Journal of Respiratory and Critical Care Medicine. 1998;158:213–19. doi: 10.1164/ajrccm.158.1.9706048. [DOI] [PubMed] [Google Scholar]
- Vermetten 1999 {published data only} .Glaxo Smith Kline (SMS40180/SLM9021B) A 12 week study to compare the efficacy and safety of salmeterol xinafoate plus beclomethasone dipropionate with a double dose of beclomethasone dipropionate in patients with mild to moderate reversible airways obstruction treated by a general practitioner. 2006 http://www.ctr.gsk.co.uk.; *; Vermetten AM, Boermans JM, Luiten WDVF, Mulder PGH, Vermue NA. Comparison of salmeterol with beclomethasone in adult patients with mild persistent asthma who are already on low-dose inhaled steroids. Journal of Asthma. 1999;36(1):97–106. doi: 10.3109/02770909909065153. [DOI] [PubMed] [Google Scholar]
- Wallin 2003 {published data only} .Glaxo Smith Kline (SLGQ98) A 12 week randomized, double-blind, parallel group study evaluating effect of fluticasone propionate 500mcgBID, fluticasone propionate 200mcg plus salmeterol 50mcg BID or fluticasone propionate 200mcg BID for control of airway inflammation in subjects with asthma, not controlled on inhaled corticosteroids. 2006 http://www.ctr.gsk.co.uk.; Sue-Chu M, Wallin A, Wilson S, Ward J, Sandstrom T, Djukanovic R, et al. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Bronchial biopsy study in asthmatics treated with low and high dose fluticasone propionate (FP) compared to low dose FP combined with salmeterol. 1999. [Google Scholar]; Wallin A, Sandstrom T, Cioppa GD, Holgate S, Wilson S. The effects of regular inhaled formoterol and budesonide on preformed Th-2 cytokines in mild asthmatics. Respiratory Medicine. 2002;96(12):121–5. doi: 10.1053/rmed.2002.1388. [DOI] [PubMed] [Google Scholar]; *; Wallin A, Sue-Chu M, Bjermer L, Ward J, Sanstrom T, Lindberg A, et al. Effect of inhaled fluticasone with and without salmeterol on airway inflammation in asthma. Journal of Allergy and Clinical Immunology. 2003;112(1):72–8. doi: 10.1067/mai.2003.1518. [DOI] [PubMed] [Google Scholar]
- Woolcock 1996a {published and unpublished data} .Glaxo Smith Kline (SMS30045) A multicentre, double-blind, parallel group, randomised study comparing the efficacy and safety of inhaled salmeterol xinafoate 50 mg bd and beclomethasone dipropionate 500 mg bd with that of salmeterol xinafoate 100 mg bd and beclomethasone dipropionate 500 mg or beclomethasone dipropionate 1000 mg bd in patients with reversible airways obstruction. 2006 www.ctr.gsk.co.uk.; *; Woolcock A, Lunback B, Ringdal N, Jacques LA. Comparison of addition of salmeterol to inhaled steroids with doubling the dose of inhaled steroids. Amercian Journal of Respiratory and Critical Care Medicine. 1996;153:1481–8. doi: 10.1164/ajrccm.153.5.8630590. [DOI] [PubMed] [Google Scholar]
- Woolcock 1996b {published and unpublished data} .Glaxo Smith Kline (SMS30045) A multicentre, double-blind, parallel group, randomised study comparing the efficacy and safety of inhaled salmeterol xinafoate 50 mg bd and beclomethasone dipropionate 500 mg bd with that of salmeterol xinafoate 100 mg bd and beclomethasone dipropionate 500 mg or beclomethasone dipropionate 1000 mg bd in patients with reversible airways obstruction. 2006 www.ctr.gsk.co.uk.; *; Woolcock A, Lundback B, Ringdal N, Jacques LA. Comparison of addition of salmeterol to inhaled steroids with doubling the dose of inhaled steroids. American Journal for Respiratory and Critical Care Medicine. 1996;153:1481–8. doi: 10.1164/ajrccm.153.5.8630590. [DOI] [PubMed] [Google Scholar]
- Zhong 2005 {published and unpublished data} .Glaxo Smith Kline (SAM40067) A multicentre, randomized, open-label, parallel-group, six-week treatment study to evaluate the efficacy and safety of Seretide (salmeterol/fluticasone propionate combination product) 50/100 mg strength bd via Accuhaler™ inhaler vs Pulmicort Turbuhaler™ 400 mg bd in Chinese adults with asthma. 2006 http://ctr.gsk.co.uk.; *; Zhong NS, Zheng JP, Cai BQ, Xie CM, Sun TY, Wang DQ, et al. Evaluation of the clinical efficacy and the safety of salmeterol/fluticasone propionate accuhaler compared to budesonide turbuhaler in the control of adult asthma. Zhonghua Jie He He Hu Xi Za Zhi. 2005;28(4):233–7. [PubMed] [Google Scholar]
References to studies excluded from this review
- Aalbers 2004 {published data only} .Aalbers R, Backer V, Kava TTK, Omenaas ER, Sandstrom T, Jorup C, et al. Adjustable maintenance dosing with budesonide/formoterol compared with fixed-dose salmeterol/fluticasone in moderate to severe asthma. Current Medical Research & Opinion. 2004;20(2):225–40. doi: 10.1185/030079903125002928. [DOI] [PubMed] [Google Scholar]; Aalbers R, Backer V, Kava TTK, Welte T, Omenaas ER, Bergqvist PBF, et al. Adjustable dosing with budesonide/ formoterol reduces the rate of asthma exacerbations compared with fixed dosing salmeterol/fluticasone. European Respiratory Society. 2003:2–20. [Google Scholar]; Aalbers R, Backer V, Kava TTK, Welte T, Omenaas ER, Bergqvist PBF, et al. Improvements in FEV1 are greater with budesonide/formoterol than with salmeterol/fluticasone. European Respiratory Society. 2003:P2–19. [Google Scholar]; Aalbers R, Backer V, Kava TTK, Welte T, Omenaas ER, Bergqvist PBF, et al. Is well-controlled asthma weeks a useful measure? Fewer exacerbations in patients treated with budesonide/formoterol than salmeterol/fluticasone. European Respiratory Society. 2003:P2–18. [Google Scholar]; Welte T, Aalbers R, Naya I. Budesonide/formoterol adjustable maintenance dosing (B/F AMD) reduces the burden of asthma more effectively than fixed-dosing (FD) with B/F or salmeterol/fluticasone (S/FL) European Respiratory Journal. 2004;24(Suppl 48):508s. [Google Scholar]
- Adinoff 1998 {published data only} .Adinoff AD, Schwartz HJ, Rickard KA, Yancey SW, Swearingen BE. Salmeterol compared with current therapies in chronic asthma. Journal of Family Practice. 1998;47(4):278–84. [PubMed] [Google Scholar]
- Akpinarli 1999 {published data only} .Akpinarli A, Tuncer A, Saraclar Y, Sekerel BE, Kalayci O. Effect of formoterol on clinical parameters and lung functions in patients with bronchial asthma: a randomised controlled trial. Archives of Disease in Childhood. 1999;81:45–8. doi: 10.1136/adc.81.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ankerst 2003 {published data only} .Ankerst J, Persson G, Weibull E. Cardiovascular effects of a high dose of the budesonide/formoterol single inhaler in asthmatic patients. European Respiratory Journal. 2001;18(Suppl 33):53s. [Google Scholar]; Ankerst J, Persson G, Weibull E. Tolerability of a high dose of budesonide/formoterol in a single inhaler in patients with asthma. Pulmonary Pharmacology & Therapeutics. 2003;16:147–51. doi: 10.1016/S1094-5539(03)00004-X. [DOI] [PubMed] [Google Scholar]
- Anonymous 1999 {published data only} .Anonymous Levalbuterol for asthma. Drugs & Therapeutics. 1999;Vol. 41(issue 1054):51–3. [PubMed] [Google Scholar]
- Anonymous a 2003 {published data only} .Anonymous Flexible dosing of combination inhaler cuts asthma exacerbations. Pharmaceutical Journal. 2003;271(7271):535. [Google Scholar]
- Anonymous b 2003 {published data only} .Anonymous Asthma control with combination therapy. Fortschritte der Medizin. 2003;145(46):46–7. [PubMed] [Google Scholar]
- Anonymous c 2003 {published data only} .Anonymous Excess mortality with salmeterol as single-agent therapy. Prescrire International. 2003;12(66):142. [PubMed] [Google Scholar]
- Arvidsson 1991 {published data only} .Arvidsson P, Larsson S, Lofdahl CG, Melander B, Svedmyr N, Wahlander L. Inhaled formoterol during one year in asthma: a comparison with salbutamol. [ENGLISH] European Respiratory Journal. 1991;4(10):1168–73. [PubMed] [Google Scholar]
- Aubier 1999 {published data only} .Aubier M, Pieters WR, Schlosser NJJ, Steinmetz KO. Salmeterol/fluticasone propionate (50/500 mug) in combination in a Diskus(TM) inhaler (Seretide(TM)) is effective and safe in the treatment of steroid-dependent asthma. Respiratory Medicine. 1999;93(12):876–84. doi: 10.1016/s0954-6111(99)90053-7. [DOI] [PubMed] [Google Scholar]; Pieters WR, Lundback B, Sondhi S, Price MJ. Cost effectiveness analysis of salmeterol/fluticasone propionate 50/500mcg vs fluticasone propionate 500mcg in patients with corticosteroid -dependent asthma. Pharmacoeconomics. 1999;16(Suppl 2):29–34. [Google Scholar]; Pieters WR, Sondhi S, Price MJ, Thwaites RM, Nyth A. European Respiratory Society. Madrid, Spain: Oct-13. 1999. The cost effectiveness of salmeterol/fluticasone propionate 50/500 microgram combination inhaler versus fluticasone propionate 500 microgram in patients with chronic asthma; p. 2458. 1999. [Google Scholar]; Pieters WR, Steinmetz KO, Aubier M, Johnson L, Gomez E, Bogolubov M. Effectiveness of a new salmeterol/ fluticasone propionate (50/500μg) combination inhaler in patients with reversible airways obstruction. European Respiratory Journal. 1998;Vol. 12(issue Suppl 28):35s. [Google Scholar]; Pieters WR, Wilson KK, Smith HCE, Tamminga JJ. Cost-effectiveness of fluticasone propionate/salmeterol combination product and fluticasone propionate/ montelukast in asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; *; Schlosser NJJ, Steinmetz KO, Aubier M, Gomez E, Wixon C. Evaluation of long-term safety of salmeterol/fluticasone propionate (50/500μg) combination inhaler in patients with reversible airways obstruction. European Respiratory Journal. 1998;Vol. 12(issue 28):35s. [Google Scholar]
- Aziz 1998 {published data only} .Aziz I, Hall IP, McFarlane LC, Lipworth BJ. Beta2-adrenoceptor regulation and bronchodilator sensitivity after regular treatment with formoterol in subjects with stable asthma. Journal of Allergy & Clinical Immunology. 1998;101(3):337–41. doi: 10.1016/S0091-6749(98)70245-3. [DOI] [PubMed] [Google Scholar]
- Aziz 1999a {published data only} .Aziz I, Lipworth BJ. A bolus of inhaled budesonide rapidly reverses airway subsensitivity and beta2-adrenoceptor down-regulation after regular inhaled formoterol. Chest. 1999;115(3):623–8. doi: 10.1378/chest.115.3.623. [DOI] [PubMed] [Google Scholar]
- Aziz 1999b {published data only} .Aziz I, Lipworth BJ. In vivo effect of albuterol on methacholine-contracted bronchi in conjunction with salmeterol and formoterol. Journal of Allergy & Clinical Immunology. 1999;103(5 part 1):816–22. doi: 10.1016/s0091-6749(99)70425-2. [DOI] [PubMed] [Google Scholar]
- Aziz 2000 {published data only} .Aziz I, Wilson AM, Lipworth BJ. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Effects of formoterol (FM) and budesonide (BUD) alone or in combination (FM+BUD) on inflammatory markers in asthmatic patients; p. 2854. 1999. [Google Scholar]; *; Aziz I, Wilson AM, Lipworth BJ. Effects of once-daily formoterol and budesonide given alone or in combination on surrogate inflammatory markers in asthmatic adults. Chest. 2000;118(4):1049–58. doi: 10.1378/chest.118.4.1049. [DOI] [PubMed] [Google Scholar]
- Bacci 2002 {published data only} .Bacci E, Di Franco A, Bartoli ML, Carnevali S, Cianchetti S, Dente FL, et al. Comparison of anti-inflammatory and clinical effects of beclomethasone dipropionate and salmeterol in moderate asthma. European Respiratory Journal. 2002;20(1):66–72. doi: 10.1183/09031936.02.00094202. [DOI] [PubMed] [Google Scholar]
- Baki 1998 {published data only} .Baki A, Karaguzel G. Short-term effects of budesonide, nedocromil sodium and salmeterol on bronchial hyperresponsiveness in childhood asthma. Acta Paediatrica Japonica. 1998;40(3):247–51. doi: 10.1111/j.1442-200x.1998.tb01921.x. [DOI] [PubMed] [Google Scholar]
- Balachandran 2001 {published data only} .Balachandran A, Shivbalan S, Subramanyam L. Drug therapy of childhood asthma. Indian Journal of Pediatrics. 2001;68(Suppl 4):S12–16. [PubMed] [Google Scholar]
- Balzano 2002 {published data only} .Balzano G, Fuschillo S, Gaudiosi C. Leukotriene receptor antagonists in the treatment of asthma: an update. Allergy. 2002;57(Suppl 72):16–9. doi: 10.1034/j.1398-9995.57.s72.2.x. [DOI] [PubMed] [Google Scholar]
- Bateman 1998 {published data only} .Bateman ED, Britton M, Carrillo J, Almeida J, Wixon C. Salmeterol/fluticasone combination inhaler. A new, effective and well tolerated treatment for asthma. Clinical Drug Investigation. 1998;16(3):193–201. doi: 10.2165/00044011-199816030-00003. [DOI] [PubMed] [Google Scholar]
- Bateman 2001 {published data only} .Bateman ED, Bantje TA, Gomes M, Toumbis M, Huber R, Eliraz A, et al. Symbicort (budesonide and formoterol in a single inhaler) is a more effective treatment than fluticasone in asthma patients. American Thoracic Society Abstracts. 2001 [Google Scholar]; Bateman ED, Beasley R, Silins V, Bogolubov M. Comparison of salmeterol/fluticasone propionate combination 50/100 bid delivered via metered dose inhaler or diskus in patients with reversible airways obstruction. American Thoracic Society 2000 International Conference; Toronto, Canada. May 5-10.2000. p. A197. [Google Scholar]; Bateman ED, Silins V, Bogolubov M. Clinical equivalence of salmeterol/fluticasone propionate in combination (50/100 mcg twice daily) when administered via a chlorofluorocarbon-free metered dose inhaler or dry powder inhaler to patients with mild-to-moderate asthma. Respiratory Medicine. 2001;95(2):136–46. doi: 10.1053/rmed.2000.1008. [DOI] [PubMed] [Google Scholar]; SFCB3022 [accessed 4 June 2008];A multicentre, randomised, double-blind, double-dummy, parallel-group, three-month comparison of the salmeterol/fluticasone propionate combination product (2×25/50mcg strength) bd via the pressurised metered dose inhaler with salmeterol/fluticasone propionate combination product (1×50/100mcg strength) bd via the Diskus/ Accuhaler™ inhaler and with fluticasone propionate (2×50mcg strength) alone bd via the pressurised metered dose inhaler in adolescents and adults with reversible airways obstruction. 2004 http://ctr.gsk.co.uk.
- Baumgarten 2002 {published data only} .Baumgarten C, Geldszus R, Behre U, Peslis N, Trautmann M, Viani-Initial Study Group Initial treatment of symptomatic mild to moderate bronchial asthma with the salmeterol/fluticasone propionate (50/250 microg) combination product (SAS40023) European Journal of Medical Research. 2002;7(1):1–7. [PubMed] [Google Scholar]
- Beckett 2003 {published data only} .Beckett P, Hewitt L, Woodcock A, Smith J, Seghal N, Rice L, et al. Improvement in airway hyper-responsiveness (AHR) and lung function with salmeterol/fluticasone propionate combination (SFC) in persistent asthma [abstract]. American Thoracic Society 99th International Conference; Poster C27; 2003. [Google Scholar]
- Beeh 2002 {published data only} .Beeh KM, Beier J, Kornmann O, Wiewrodt R, Buhl R. Efficacy and safety of salmeterol (50 [mu]g) and fluticasone (250 [mu]g) in a single inhaler device (Diskus(R)) in patients with mild to moderate asthma. Pneumologie. 2002;56(2):91–7. doi: 10.1055/s-2002-20089. [DOI] [PubMed] [Google Scholar]
- Behling 1999 {published data only} .Behling B, Matthys H. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Comparison of efficacy and safety of formoterol with terbutaline in children with mild to moderate asthma. 1999. [Google Scholar]
- Bennett 2002 {published data only} .Bennett WD. Effect of beta-adrenergic agonists on mucociliary clearance. Journal of Allergy & Clinical Immunology. 2002;Vol. 110(issue Suppl 6):s291–7. doi: 10.1067/mai.2002.129704. [DOI] [PubMed] [Google Scholar]
- Bensch 2002 {published data only} .Bensch G, Berger WE, Blokhnn M, Socolovshy AL, Thomson MH, Till MD, et al. One year efficacy and safety of inhaled formoterol dry powder in children with persistent asthma. Annals of Allergy Asthma and Immunology. 2002;89:180–90. doi: 10.1016/s1081-1206(10)61935-7. [DOI] [PubMed] [Google Scholar]; Berger W, Bensch G, Blokhin BM, Socolovsky AL, Thompson MH, Till D. Addition of formoterol (Foradil®) improves lung function and symptoms in children with persistent asthma not controlled by inhaled corticosteroids. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Berggren 2001 {published data only} .Berggren F, Ekstrom T. A cost-effectiveness study comparing the as-needed use of formoterol (Oxis) and terbutaline (Bricanyl) in patients with moderate to severe asthma. Respiratory Medicine. 2001;95(9):753–8. doi: 10.1053/rmed.2001.1131. [DOI] [PubMed] [Google Scholar]
- Berlinski 2001 {published data only} .Berlinski A, Waldrep JC. Metering performance of several metered-dose inhalers with different spacers/holding chambers. Journal of Aerosol Medicine. 2001;14(4):427–32. doi: 10.1089/08942680152744631. [DOI] [PubMed] [Google Scholar]
- Bernstein 2002 {published data only} .Bernstein IL. Beta2-agonists: Deja vu all over again: the second-generation controversy. Chest. 2002;122(3):763–5. doi: 10.1378/chest.122.3.763. [DOI] [PubMed] [Google Scholar]
- Bessmertny 2002 {published data only} .Bessmertny O, DiGregorio RV, Cohen H, Becker E, Looney D, Golden J, et al. A randomized clinical trial of nebulized magnesium sulfate in addition to albuterol in the treatment of acute mild-to-moderate asthma exacerbations in adults. Annals of Emergency Medicine. 2002;39(6):585–91. doi: 10.1067/mem.2002.123300. [DOI] [PubMed] [Google Scholar]
- Bijl-Hofland 2001 {published data only} .Bijl-Hofland ID, Cloosterman SG, Folgering HT, van den Elshout FJ, van Weel C, van Schayck CP. Inhaled corticosteroids, combined with long-acting beta(2)-agonists, improve the perception of bronchoconstriction in asthma. American Journal of Respiratory & Critical Care Medicine. 2001;164(5):764–9. doi: 10.1164/ajrccm.164.5.9910103. [DOI] [PubMed] [Google Scholar]
- Bjermer 2000 {published data only} .Bjermer L, Bisgaard H, Bousquet J, Fabbri LM, Greening A, Haahtela T, et al. Montelukast or salmeterol combined with an inhaled steroid in adult asthma: design and rationale of a randomized, double-blind comparative study (the IMPACT Investigation of Montelukast as a Partner Agent for Complementary Therapy-trial) Respiratory Medicine. 2000;94(6):612–21. doi: 10.1053/rmed.2000.0806. [DOI] [PubMed] [Google Scholar]; Bjermer L, Greening A, Haahtela T, Bousquet J, Holgate ST, Picado C, Bisgaard H, et al. Addition of montelukast or salmeterol to fluticasone in patients with uncontrolled asthma: results of the IMPACT trial. Chest (conference); San Diego, CA. 2002. p. 434. [Google Scholar]
- Boonsawat 2003 {published data only} .Boonsawat W, Charoenratanakul S, Pothirat C, Sawanyawisuth K, Seearamroongruang T, Bengtsson T, et al. Formoterol (OXIS) Turbuhaler as a rescue therapy compared with salbutamol pMDI plus spacer in patients with acute severe asthma. Respiratory Medicine. 2003;97(9):1067–74. doi: 10.1016/s0954-6111(03)00139-2. [DOI] [PubMed] [Google Scholar]
- Booth 1993 {published data only} .Booth H, Fishwick K, Harkawat R, Devereux G, Hendrick DJ, Walters EH. Changes in methacholine induced bronchoconstriction with the long acting beta 2 agonist salmeterol in mild to moderate asthmatic patients. Thorax. 1993;48(11):1121–4. doi: 10.1136/thx.48.11.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boulet 1998 {published data only} .Boulet LP, Turcotte H, Cartier A, Milot J, Cote J, Malo JL, et al. Influence of beclomethasone and salmeterol on the perception of methacholine-induced bronchoconstriction. Chest. 1998;114(2):373–9. doi: 10.1378/chest.114.2.373. [DOI] [PubMed] [Google Scholar]
- Boyd 1995 {published data only} .Boyd G. Salmeterol xinafoate in asthmatic patients under consideration for maintenance oral corticosteroid therapy. European Respiratory Journal. 1995;8:1494–8. [PubMed] [Google Scholar]
- Brambilla 1994 {published data only} .Brambilla C, Chastang C, Georges D, Bertin L. Salmeterol compared with slow-release terbutaline in nocturnal asthma. Allergy. 1994;49(6):421–6. doi: 10.1111/j.1398-9995.1994.tb00834.x. [DOI] [PubMed] [Google Scholar]
- Braunstein 2002 {published data only} .Braunstein G. Optimization of asthma control with fluticasone/salmeterol (Seretide) combination: new clinical data. Revue De Pneumologie Clinique. 2002;Vol. 58(issue 3 part 2):s12–5. [PubMed] [Google Scholar]
- Brenner 1988 {published data only} .Brenner M, Berkowitz R, Marshall N, Strunk RC. Need for theophylline in severe steroid-requiring asthmatics. Clinical Allergy. 1988;18(2):143–50. doi: 10.1111/j.1365-2222.1988.tb02853.x. [DOI] [PubMed] [Google Scholar]
- Britton 1992 {published data only} .Britton MG, Earnshaw JS, Palmer JBD. A twelve month comparison of salmeterol with salbutamol in asthmatic patients. European Respiratory Journal. 1992;5(9):1062–7. [PubMed] [Google Scholar]
- Britton 1998 {published data only} .Britton MG, Carrillo T, Almeida J, Wixon C. Combined Serevent™ and fluticasone propionate (50/100μg strength) bd via one Diskus™ (accuhaler™) inhaler compared with salmeterol 50μg and fluticasone propionate 100μg bd via two separate Diskus inhalers. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A415. [Google Scholar]
- Brogden 1991 {published data only} .Brogden RN, Faulds D. Salmeterol xinafoate. A review of its pharmacological properties and therapeutic potential in reversible obstructive airways disease. Drugs. 1991;42(5):895–912. doi: 10.2165/00003495-199142050-00010. [DOI] [PubMed] [Google Scholar]
- Buchvald 2003 {published data only} .Buchvald F, Bisgaard H. Comparisons of the complementary effect on exhaled nitric oxide of salmeterol vs montelukast in asthmatic children taking regular inhaled budesonide. Annals of Allergy, Asthma, and Immunology. 2003;91(3):309–13. doi: 10.1016/S1081-1206(10)63536-3. [DOI] [PubMed] [Google Scholar]; *; Buchvald FF, Bisgaard H. Comparison of add-on of leukotriene receptor antagonist versus long-acting beta2-agonist on FeNO in asthmatic children on regular inhaled budesonide. European Respiratory Society Annual Congress. 2002:P2736. [Google Scholar]
- Buhl 2003a {published data only} .AstraZeneca (SD 039 0666) [accessed 30 April 2008];Symbicort high dose once daily in mild to moderate asthmatic patients. 2000 http://www.astrazenecaclinicaltrials.com.; Buhl R, Creemers JPHM, Vondra V, Martelli NA. Improved and maintained asthma control with once-daily budesonide/ formoterol single inhaler in mild-to-moderate persistent asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):21s. [Google Scholar]; Buhl R, Creemers JPHM, Vondra V, Martelli NA. Once-daily budesonide/formoterol via a single inhaler is effective in mild-to-moderate persistent asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):21s. [Google Scholar]; Buhl R, Creemers JPHM, Vondra V, Martelli NA. Once daily Symbicort (budesonide/eformoterol in a single inhaler) is effective in moderate-persistent asthma. Thorax. 2001;56(Suppl 3):iii 62. [Google Scholar]; Buhl R, Creemers JPHM, Vondra V, Martelli NA. Symbicort® (budesonide and formoterol in a single inhaler) administered once daily is effective in mild to moderate asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; Buhl R, Creemers JPHM, Vondra V, Martelli NA, Naya IP, Eksstrom Once daily budesonide/formoterol in a single inhaler in adults with moderate persistent asthma. Respiratory Medicine. 2003;97:323–30. doi: 10.1053/rmed.2002.1427. [DOI] [PubMed] [Google Scholar]; *; Buhl R, Zetterstrom O, Mellem H, Perpina M, Hedman J, O’Neill S, et al. Improved asthma control with budesonide/ formoterol via a single inhaler compared with budesonide alone, in moderate persistent asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):48s. doi: 10.1183/09031936.01.00065801. [DOI] [PubMed] [Google Scholar]
- Buhl 2003b {published data only} .Boushey H, Bateman E, Bousquet J, Busse W, Clark T, Pauwels R, et al. Achieving total control of asthma with salmeterol/fluticasone propionate versus fluticasone propionate alone: GOAL study results. 4th Triennial World Asthma Meeting.2004. [Google Scholar]; Brambilla C, Le Gros V, Bourdeix I. Formoterol 12 mug BID administered via single-dose dry powder inhaler in adults with asthma suboptimally controlled with salmeterol or on-demand salbutamol: a multicenter, randomized, open-label, parallel-group study. Clinical Therapeutics. 2003;25(7):2022–36. doi: 10.1016/s0149-2918(03)80202-3. [DOI] [PubMed] [Google Scholar]; Buchvald F, Bisgaard H. Comparisons of the complementary effect on exhaled nitric oxide of salmeterol vs montelukast in asthmatic children taking regular inhaled budesonide. Annals of Allergy, Asthma, and Immunology. 2003;91(3):309–13. doi: 10.1016/S1081-1206(10)63536-3. [DOI] [PubMed] [Google Scholar]; Buchvald FF, Bisgaard H. Comparison of add-on of leukotriene receptor antagonist vs. long-acting beta2-agonist on FeNO in asthmatic children on regular inhaled budesonide. European Respiratory Society Annual Congress.2002. p. P2736. [Google Scholar]; Buhl R. Budesonide/formoterol for the treatment of asthma. Expert Opinion in Pharmacotherapy. 2003;4(8):1393–406. doi: 10.1517/14656566.4.8.1393. [DOI] [PubMed] [Google Scholar]; Buhl R. Budesonide/formoterol for the treatment of asthma. Expert Opinion in Pharmacotherapy. 2003;4(8):1393–406. doi: 10.1517/14656566.4.8.1393. [DOI] [PubMed] [Google Scholar]; Busse W, Bateman E, Boushey H, Bousquet J, Clark T, Pauwels R, et al. Aiming to achieve total control with salmeterol/fluticasone propionate and fluticasone propionate alone is well tolerated: Goal 1-year safety data. 4th Triennial World Asthma Meeting.2004. [Google Scholar]; Kotaniemi J, Tilling B, Oien T. A double blind, randomised, parallel group study over 12 weeks comparing Seretide™ (50/100mg bd Diskus™) versus Flixotide™ (250mg bd Diskus™) as first-line regular asthma treatment for steroid-naive adult patients. American Journal of Respiratory & Critical Care Medicine. 2003;167(7):A893. [Google Scholar]; Kraft M, Martin RJ, Lazarus SC, Fahy JV, Boushey HA, Lemanske RF, Jr, et al. Airway tissue mast cells in persistent asthma: predictor of treatment failure when patients discontinue inhaled corticosteroids. Chest. 2003;124(1):42–50. doi: 10.1378/chest.124.1.42. [DOI] [PubMed] [Google Scholar]; Pauwels R, Bateman SE, Boushey H, Bousquet J, Busse W, Clark T, et al. Achievement of guideline-based asthma control with salmeterol/fluticasone propionate compared with fluticasone propionate alone; results of Goal study. Triennial World Asthma Meeting.2004. [Google Scholar]; Pedersen S, Bateman E, Boushey H, Bousquet J, Busse W, Clark T, et al. Aiming for guideline defined total control of asthma improves one-year asthma outcomes: results of the GOAL study. 4th Triennial World Asthma Meeting.2004. [Google Scholar]; *; Strand AM. Initiation of treatment with the salmeterol/ fluticasone propionate (FP) combination product is better than inhaled steroid alone (FP) in asthmatic patients symptomatic on short-acting bronchodilator alone. European Respiratory Journal. 2003;Vol. 22(issue Suppl 45):410s, P2638. [Google Scholar]
- Buhl 2003c {published data only} .Buhl R. Budesonide/formoterol for the treatment of asthma. Expert Opinion in Pharmacotherapy. 2003;4(8):1393–406. doi: 10.1517/14656566.4.8.1393. [DOI] [PubMed] [Google Scholar]
- Busse 1999 {published data only} .Busse W, Nelson H, Wolfe J, Kalberg C, Yancey SW, Rickard KA. Comparison of inhaled salmeterol and oral zafirlukast in patients with asthma. Journal of Allergy & Clinical Immunology. 1999;103(6):1075–80. doi: 10.1016/s0091-6749(99)70182-x. [DOI] [PubMed] [Google Scholar]
- Byrnes 2000 {published data only} .Byrnes C, Shrewsbury S, Barnes PJ, Bush A. Salmeterol in paediatric asthma. Thorax. 2000;55(9):780–4. doi: 10.1136/thorax.55.9.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calhoun 2001 {published data only} .Calhoun WJ, Nelson HS, Nathan RA, Pepsin PJ, Kalberg C, Emmett A, et al. Comparison of fluticasone propionate-salmeterol combination therapy and montelukast in patients who are symptomatic on short-acting 2-agonists alone. American Journal of Respiratory and Critical Care Medicine. 2001;164(5):759–63. doi: 10.1164/ajrccm.164.5.2012124. [DOI] [PubMed] [Google Scholar]
- Calverley 2002 {published data only} .Calverley PMA, Pauwels RA, Vestbo J, Jones PW, Pride NB, Gulsvik A, et al. Salmeterol/fluticasone propionate combination for one year provides greater clinical benefit than its individual components in COPD. American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A226. [Google Scholar]
- Castle 1993 {published data only} .Castle W, Fuller R, Hall J, Palmer J. Serevent nationwide surveillance study: comparison of salmeterol with salbutamol in asthmatic patients who require regular bronchodilator treatment. BMJ. 1993;113(306):1034–7. doi: 10.1136/bmj.306.6884.1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cazzola 2000 {published data only} .Cazzola M, Di Lorenzo G, Di Perna F, Calderaro F, Testi R, Centanni S. Additive effects of salmeterol and fluticasone or theophylline in COPD. Chest. 2000;118(6):1576–81. doi: 10.1378/chest.118.6.1576. [DOI] [PubMed] [Google Scholar]
- Chalmers 1999 {published data only} .Chalmers GW, Macleod KJ, Thomson LJ, Little SA, Patel KR, McSharry C, et al. Sputum cellular and cytokine responses to inhaled endothelin-1 in asthma. Clinical & Experimental Allergy. 1999;29(11):1526–31. doi: 10.1046/j.1365-2222.1999.00496.x. [DOI] [PubMed] [Google Scholar]
- Chan 2001 {published data only} .Chan JS, Cowie RL, Lazarenko GC, Little C, Scott S, Ford GT. Comparison of intramuscular betamethasone and oral prednisone in the prevention of relapse of acute asthma. Canadian Respiratory Journal. 2001;8(3):147–52. doi: 10.1155/2001/613426. [DOI] [PubMed] [Google Scholar]
- Chapman 1999 {published data only} .Chapman KR, Ringdal N, Backer V, Palmqvist M, Saarelainen S, Briggs M. Salmeterol and fluticasone propionate (50/250 mug) administered via combination Diskus inhaler: as effective as when given via separate Diskus inhalers. Canadian Respiratory Journal. 1999;6(1):45–51. doi: 10.1155/1999/894803. [DOI] [PubMed] [Google Scholar]
- Cheer 2003 {published data only} .Cheer SM, Warner GT, Easthope SE. Formoterol delivered by Turnuhaler in paediatric asthma. Paediatric Drugs. 2003;5(1):63–8. doi: 10.2165/00128072-200305010-00008. [DOI] [PubMed] [Google Scholar]
- Chuchalin 2002 {published data only} .Chuchalin AG, Ovcharenko SI, Goriachkina LA, Sidorenko IV, Tsoi AN. Formoterol (Oxis®) Turbuhaler® plus budesonide turbuhaler® is more effective than current non-steroid therapy and budesonide alone in mild to moderate asthma in Russia. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; Chuchalin AG, Ovcharenko SI, Goriachkina LA, SIdorenko IV, Tsoi AN. The safety and efficacy of formoterol (Oxis) turbuhaler plus budesonide (Pulmicort) turbuhaler in mild to moderate asthma: a comparison with budesonide turbuhaler alone and current non-corticosteroid therapy in Russia. International Journal of Clinical Practice. 2002;56(1):15–20. [PubMed] [Google Scholar]; Chuchalin AG, Stahl E, Svensson K, Ovcharenko SI, Goriachkina LA, Sidorenko IV, et al. Formoterol (Oxis®) Turbuhaler® plus budesonide Turbuhaler® and budesonide alone improve health-related quality of life vs non-steroid therapy in mild to moderate asthma in Russia. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; Chuchalin AG, Svensson K, Stahl E, Ovcharenko SI, Goriachkina LA, Sidorenko IV, et al. A health-related quality-of-life comparison of formoterol (Oxis(R)) Turbuhaler (R) plus budesonide (Pulmicort(R)) Turbuhaler(R) with budesonide Turbuhaler(R) alone and noncorticosteroid treatment in asthma: a randomized clinical study in Russia. Respiration. 2002;69(5):427–33. doi: 10.1159/000064022. [DOI] [PubMed] [Google Scholar]; *; Kuna P, Chuchalin A, Ringdal N, De la Padilla EA, Black P, Lindqvist A, et al. Low-dose single-inhaler budesonide/ formoterol administered once daily is effective in mild-persistent asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):158s. [Google Scholar]
- Chuchalin 2008 {unpublished data only} .Chuchalin A, Jacques L, Frith L. Salmeterol/fluticasone propionate via Diskus[TM] once daily versus fluticasone propionate twice daily in patients with mild asthma not previously receiving maintenance corticosteroids. Clinical Drug Investigation. 2008;28(3):169–81. doi: 10.2165/00044011-200828030-00004. [DOI] [PubMed] [Google Scholar]; Glaxo Smith Kline (SAS30024) A 52-week multicentre, randomised, double-blind, double dummy, placebo-controlled parallel group study to compare the efficacy and tolerability of salmeterol/fluticasone propionate combination (SERETIDE/VIANI/ADVAIR) 50/100mcg once daily in the morning with fluticasone propionate (FLIXOTIDE/FLOVENT) 100mcg twice daily and placebo twice daily, all via the DISKUS/ACCUHALER as initial maintenance therapy in mild asthmatic subject. 2005 http://ctr.gsk.co.uk.
- Cloosterman 2001 {published data only} .Cloosterman SG, Bijl-Hofland ID, van Herwaarden CL, Akkermans RP, van Den Elshout FJ, Folgering HT, et al. A placebo-controlled clinical trial of regular monotherapy with short-acting and long-acting beta(2)-agonists in allergic asthmatic patients. Chest. 2001;119(5):1306–15. doi: 10.1378/chest.119.5.1306. [DOI] [PubMed] [Google Scholar]
- Condemi 2001 {published data only} .Condemi JJ. Comparison of the efficacy of formoterol and salmeterol in patients with reversible obstructive airway disease: a multicenter, randomized, open-label trial. Clinical Therapeutics. 2001;23(9):1529–41. doi: 10.1016/s0149-2918(01)80125-9. [DOI] [PubMed] [Google Scholar]
- Creticos 1999 {published data only} .Creticos PS, Freidhoff LR, Bernstein DI, Chu T, Khattignavong AP, Pasatiempo AM. Comparison of an inhaled corticosteroid (triamcinolone acetonide) to a long-acting bronchodilator (salmeterol), the combination, and placebo in mild-moderate adult asthmatic patients. International Archives of Allergy and Immunology. 1999;118:345–6. doi: 10.1159/000024129. [DOI] [PubMed] [Google Scholar]
- Crompton 1999 {published data only} .Crompton GK, Ayres JG, Basran G, Schiraldi G, Brusasco V, Eivindson A, et al. Comparison of oral bambuterol and inhaled salmeterol. American Journal of Respiratory & Critical Care Medicine. 1999;159(3):824–8. doi: 10.1164/ajrccm.159.3.9806117. [DOI] [PubMed] [Google Scholar]
- Currie 2003a {published data only} .Currie GP, Lee DKC, Haggart K, Bates CE, Lipworth BJ. Effects of montelukast on surrogate inflammatory markers in corticosteroid-treated patients with asthma. American Journal of Respiratory and Critical Care Medicine. 2003;167(9):1232–8. doi: 10.1164/rccm.200209-1116OC. [DOI] [PubMed] [Google Scholar]
- Currie 2003b {published data only} .Currie GP, Bates CE, Lee DKC, Jackson CM, Lipworth BJ. Effects of fluticasone plus salmeterol versus twice the dose of fluticasone in asthmatic patients. European Journal of Clinical Pharmacology. 2003;59(1):11–5. doi: 10.1007/s00228-003-0571-9. [DOI] [PubMed] [Google Scholar]
- Currie 2003c {published data only} .Currie GP, Lee DK, Dempsey OJ, Fowler SJ, Cowan LM, Lipworth BJ. A proof of concept study to evaluate putative benefits of montelukast in moderate persistent asthmatics. British Journal of Clinical Pharmacology. 2003;55(6):609–15. doi: 10.1046/j.1365-2125.2003.01813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Alonzo 1994 {published data only} .D’Alonzo GE, Nathan RA, Henochowicz, Morris RJ, Ratner P, Rennard SI. Salmetrol xinafoate as maintenance therapy compared with albuterol in patients with asthma. JAMA. 1994;271:1412–16. [PubMed] [Google Scholar]
- D’Urzo 2001 {published data only} .D’Urzo AD, Chapman KR, Cartier A, Hargreave FE, Fitzgerald M, Tesarowski D. Effectiveness and safety of salmeterol in non-specialist practice settings. Chest. 2001;119:714–19. doi: 10.1378/chest.119.3.714. [DOI] [PubMed] [Google Scholar]
- Dahl 1989 {published data only} .Dahl R, Pedersen B, Hagglof B. Nocturnal asthma: effect of treatment with oral sustained-release terbutaline, inhaled budesonide, and the two in combination. Journal of Allergy & Clinical Immunology. 1989;83(4):811–5. doi: 10.1016/0091-6749(89)90019-5. [DOI] [PubMed] [Google Scholar]
- Dahl 1991 {published data only} .Dahl R, Earnshaw JS, Palmer JBD. Salmeterol: a four week study of a long-acting beta-adrenoceptor agonist for the treatment of reversible airways disease. European Respiratory Journal. 1991;4(10):1178–84. [PubMed] [Google Scholar]
- Dal Negro 2001a {published data only} .Dal Negro R, Micheletto C, Tognella S, Trevisan F, Pomari C. Short-term bronchodilation following salmeterol 50mcg and combined salmeterol + fluticasone p (50/250mcg) via Diskus: a randomized, double blind cross-over study in reversible airway obstruction. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Dal Negro 2001b {published data only} .Dal Negro RW, Micheletto C, Pomari C, Trevisan F, Tognella S. The combination salmeterol (S) + fluticasone propionate (F) in mild-to-moderate asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):426s. [Google Scholar]
- Dal Negro 2002 {published data only} .Dal Negro R, Micheletto C, Trevison F, Tognells S, Pomari C, Spencer S. Salmeterol & fluticasone 50μg/250μg bid versus salmeterol 50μg bid and vs placebo in the long-term treatment of COPD. American Journal of Respiratory and Critical Care Medicine. 2002;(issue Suppl 8):A228. [Google Scholar]
- Davis 2001 {published data only} .Davis ES, Bowers B, Pepsin P, Kalberg C, Dorinsky P. The impact of fluticasone propionate/salmeterol combination product compared to oral montelukast on asthma related quality of life. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Dekhuijzen 2002 {published data only} .Dekhuijzen PNR, Diamant Z. The role of montelukast, a leukotriene receptor antagonist, in the treatment of asthma. Pharmaceutisch Weekblad. 2002;137(1):38–9. [Google Scholar]
- Del Rio Navarro 2001a {published data only} .Del Rio Navarro BE, Sienra-Monge JJL, Alvarez-Amador M, Reyes-Ruiz N, Arevalo-Salas A, Berber A. Serum potassium levels, CPK-MB and ECG in children suffering asthma treated with beclomethasone or beclomethasone-salmeterol. Allergologia et Immunopathologia. 2001;29(1):16–21. doi: 10.1016/s0301-0546(01)79010-6. [DOI] [PubMed] [Google Scholar]
- Del Rio Navarro 2001b {published data only} .Del Rio BE, Corona L, Fregosa R, Berber A, Magana J, Sienra-Monge JL. Effect of salmeterol and salmeterol plus beclomethasone on the saliva flow and saliva IgA levels on patients with chronic moderate persistent asthma (CMPA) Journal of Allergy and Clinical Immunology. 2001;Vol. 107(issue 2):s11. doi: 10.1016/s1081-1206(10)62925-0. [DOI] [PubMed] [Google Scholar]; Del Rio Navarro BE, Coron-Hernandez L, Fragoso-Rios R, Berber A, Torres-Alcantara S, Cuairan-Ruidiaz V, et al. Effect of salmeterol and salmeterol plus beclomethasone on saliva flow and IgA in patients with moderate-persistent chronic asthma. Annals of Allergy, Asthma, and Immunology. 2001;87(5):420–3. doi: 10.1016/s1081-1206(10)62925-0. [DOI] [PubMed] [Google Scholar]
- Dente 2001 {published data only} .Dente FL, Scuotri L, Bacci E, DeSanctis M, Di Franco A, Giannini D, et al. Combined treatment with fluticasone plus salmeterol protects against allergen-induced asthmatic responses better than each drug alone. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):349s. [Google Scholar]; Dente FL, Scuotri L, Bacci E, Di Franco A, Giannini D, Taccola M, et al. Effects of combined treatment - fluticasone plus salmeterol - on allergen-induced asthmatic responses. American Journal of Respiratory and Critical Care Medicine Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. p. A419. [Google Scholar]
- Di Franco 1999 {published data only} .Di Franco A, Giannini D, Bacci E, Dente FL, Vagaggini B, Paggiaro PL. Comparison of different long-term asthma treatments in subjects with mild-to-moderate asthma. Monaldi Archives for Chest Disease. 1999;54(5):390–3. [PubMed] [Google Scholar]
- Dicpinigaitis 2002 {published data only} .Dicpinigaitis PV, Dobkin JB, Reichel J. Antitussive effect of the leukotriene receptor antagonist zafirlukast in subjects with cough-variant asthma. Journal of Asthma. 2002;39(4):291–7. doi: 10.1081/jas-120002285. [DOI] [PubMed] [Google Scholar]
- Didier 1997 {published data only} .Didier A, Campos Oriola R. A two-month comparison of salmeterol/beclomethasone and slow-release terbutaline/budesonide in moderate asthma management. Clinical Drug Investigation. 1997;14(1):1–11. [Google Scholar]
- Dorinsky 2001 {published data only} .Dorinsky P, Kalberg C, Pepsin P, Emmett A, Bowers B, Rickard K. The fluticasone/salmeterol combination product is superior to montelukast as first-line asthma control. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):263s. [Google Scholar]; Dorinsky PM, Kalberg C, Pepsin P, Emmett A, Rickard K. Greater onset of improvement in clinical efficacy measures with first line use of the fluticasone/salmeterol combination product compared to montelukast. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23; 2001. 2001. [Google Scholar]
- Dorinsky 2002 {published data only} .Dorinsky P, Jones S, Kalberg C, Emmett A, Rickard K. Sustained protection against activity-induced bronchospasm (AIB) during chronic treatment with the fluticasone propionate/salmeterol combination (FSC) American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A568. [Google Scholar]
- Durham 1999 {published data only} .Durham S. Long acting inhaled beta2-agonists: anti-inflammatory effects not evident during treatment of day to day asthma. European Respiratory Journal. 1999;14(2):249–50. doi: 10.1034/j.1399-3003.1999.14b02.x. [DOI] [PubMed] [Google Scholar]
- Ek 2000 {published data only} .Ek A, Palmberg L, Larsson K. Influence of fluticasone and salmeterol on airway effects of inhaled organic dust;an in vivo and ex vivo study. Clinical & Experimental Immunology. 2000;121(1):11–6. doi: 10.1046/j.1365-2249.2000.01245.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eliraz 2001a {published data only} .Eliraz A, Fritscher CC, Perez CMR, Boonsawat W, Nang AN, Bardin P, et al. Budesonide and formoterol in a single inhaler quickly gains asthma control compared with fluticasone propionate in mild asthma. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):48s. [Google Scholar]
- Eliraz 2001b {published data only} .Eliraz A, Ramirez-Rivera A, Ferranti P, Holzer R, Garcia JM, Turcotte C, et al. Similar efficacy following four weeks treatment of asthmatics with formoterol 12 mcg BD delivered by two different dry powder inhalers; differences in inhaler handling. International Journal of Clinical Practice. 2001;55(3):164–70. [PubMed] [Google Scholar]
- Eliraz 2002 {published data only} .Eliraz A, Fritscher CC, Perez CMR, Boonsawat W, Nang AN, Bardin P, et al. Symbicort® (budesonide/formoterol) achieves more rapid control of asthma that fluticasone in patients with mild asthma. American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A567. [Google Scholar]
- Ericsson 2001 {published data only} .Ericsson K, Bantje TA, Huber R, Borg S, Andersson F. Symbicort Turbohaler is more effective than fluticasone Diskus in the treatment of asthma. Thorax. 2001;Vol. 56(issue Suppl 3):iii 63. [Google Scholar]
- Everden 2002 {published data only} .Everden P, Lloyd A, Hutchinson J, Plumb J. Cost-effectiveness of eformoterol Turbohaler(R) versus salmeterol Accuhaler(R) in children with symptomatic asthma. Respiratory Medicine. 2002;96(4):250–8. doi: 10.1053/rmed.2001.1258. [DOI] [PubMed] [Google Scholar]
- Faurschou 1994 {published data only} .Faurschou P, Engel AM, Haanaes OC. Salmeterol in two different doses in the treatment of nocturnal bronchial asthma poorly controlled by other therapies. Allergy. 1994;49(40):827–32. doi: 10.1111/j.1398-9995.1994.tb00782.x. [DOI] [PubMed] [Google Scholar]
- Faurschou 1996 {published data only} .Faurschou P, Steffensen I, Jacques L. Effect of addition of inhaled salmeterol to the treatment of moderate-to-severe asthmatics uncontrolled on high-dose inhaled steroids. European Respiratory Journal. 1996;9(9):1885–90. doi: 10.1183/09031936.96.09091885. [DOI] [PubMed] [Google Scholar]
- Fish 2001 {published data only} .Fish J, Boone R, Emmett A, Yancey S, Knobil K, Rickard K. Salmeterol added to inhaled corticosteroids (ICS) provides greater asthma control compared to montelukast. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue Suppl 3):A203. [Google Scholar]; Fish JE, Israel E, Murray JJ, Emmett A, Boone R, Yancey SW, et al. Salmeterol powder provides significantly better benefit than montelukast in asthmatic patients receiving concomitant inhaled corticosteroid therapy. Chest. 2001;120(2):423–30. doi: 10.1378/chest.120.2.423. [DOI] [PubMed] [Google Scholar]
- Fitzgerald 1999 {published data only} .Fitzgearld JM, Chapman KR, Della Cioppa G, Stubbing D, Fairbarn MS, Till MD, et al. The Canadian FO/OD1 Study Group Sustained bronchoprotection, bronchodilatation and symptom control during regular formoterol use in asthma of moderate or greater severity. Journal of Allergy and Clinical Immunology. 1999;103(3 Pt 1):427–35. doi: 10.1016/s0091-6749(99)70467-7. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick 1990 {published data only} .Fitzpatrick MF, Mackay T, Driver H, Douglas NJ. Salmeterol in nocturnal asthma: a double-blind, placebo controlled trial of long-acting inhaled beta2 agonist. BMJ. 1990;301:1365–8. doi: 10.1136/bmj.301.6765.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuglsang 1995 {published data only} .Fuglsang G, Agertoft L, Vikre Jorgensen J, Pedersen S. Influence of budesonide on the response to inhaled terbutaline in children with mild asthma. Pediatric Allergy and Immunology. 1995;6(2):103–8. doi: 10.1111/j.1399-3038.1995.tb00268.x. [DOI] [PubMed] [Google Scholar]
- Garcia-Marcos 2003 {published data only} .Garcia-Marcos L, Schuster A, Cobos Barroso N. Inhaled corticosteroids plus long-acting beta(2)-agonists as a combined therapy in asthma. Expert Opinion on Pharmacotherapy. 2003;4(1):23–39. doi: 10.1517/14656566.4.1.23. [DOI] [PubMed] [Google Scholar]
- Gardiner 1994 {published data only} .Gardiner PV, Ward C, Booth H, Allison A, Hendrick EH, Walters DJ. Bronchoalveolar lavage inflammatory indices in asthmatics. American Journal of Respiratory and Critical Care Medicine. 1994;150:1006–11. doi: 10.1164/ajrccm.150.4.7921429. [DOI] [PubMed] [Google Scholar]
- Gessner 2003 {published data only} .Gessner C, Stenglein S, Brautigam M, Muller A, Schauer J. Miflonide/Foradil via Aerolizer compared with other anti-inflammatory and anti-obstructive therapeutic regimens. Pneumologie. 2003;57(3):137–43. doi: 10.1055/s-2003-37738. [DOI] [PubMed] [Google Scholar]
- Giannini 1996 {published data only} .Giannini D, Carletti A, Dente FL, Testi R, Bacci D, Bancalari L, et al. Effect of inhaled beclomethasone dipropionate (BDP) on tolerance to salmeterol (S) in allergen induced bronchoconstriction. European Respiratory Journal. 1996;Vol. 9(issue 23):272s. [Google Scholar]
- Giannini 1998 {published data only} .Giannini D, di Franco A, Bacci E, Conti I, Dente FL, Kotopulos C, et al. One-week regular treatment with salmeterol induces tolerance to the protective effect of salmeterol on allergen challenge only in subjects not regularly treated with salmeterol and inhaled corticosteroid. European Respiratory Journal. 1998;12(Suppl 28):156s. [Google Scholar]; Giannini D, Di Franco A, Bacci E, Conti I, Dente FL, Kotopulos C, et al. Long-term treatment with salmeterol and inhaled corticosteroids does not induce tolerance to the protective effect of salmeterol on allergen challenge. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A414. [Google Scholar]
- Giannini 1999 {published data only} .Giannini D, Bacci E, Dente FL, Di Franco A, Vagaggini B, Testi R, et al. Inhaled beclomethasone dipropionate reverts tolerance to the protective effect of salmeterol on allergen challenge. Chest. 1999;115(3):629–34. doi: 10.1378/chest.115.3.629. [DOI] [PubMed] [Google Scholar]
- Giannini 2000 {published data only} .Giannini D, Di Franco A, Bacci E, Dente FL, Taccola M, Vagaggini B, et al. The protective effect of salbutamol inhaled using different devices on methacholine bronchoconstriction. Chest. 2000;117(5):1319–23. doi: 10.1378/chest.117.5.1319. [DOI] [PubMed] [Google Scholar]
- Giannini 2001 {published data only} .Giannini D, Tonelli M, Di Franco A, Bacci E, Conti I, Dente FL, et al. Tolerance to the protective effect of salmeterol on allergen challenge in mild untreated asthmatics and in moderate asthmatics on inhaled corticosteroid treatment. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):103s. [Google Scholar]
- Giannini 2002 {published data only} .Giannini D, Tonelli M, Di Franco A, Bacci E, Conti I, Dente FL, et al. Tolerance to the protective effect of salmeterol + fluticasone combination (50/250 μg) on allergen challenge in mild untreated asthmatics. American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A566. [Google Scholar]
- Gizycki 2000 {published data only} .Gizycki MJ, Venge P, Dahl R, Jeffery PK. Comparison of the effects of six weeks treatment with fluticasone or salmeterol on the late phase response (LPR) in mild asthma - a bronchial biopsy study. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue Suppl 3):A203. [Google Scholar]
- GOAL {published data only} .Bateman ED, Boushey HA, Bousquet J, Busse WW, Clark TJ, Pauwels RA, Pedersen SE, GOAL Investigators Group Can guideline-defined asthma control be achieved? The Gaining Optimal Asthma ControL study. American Journal of Respiratory & Critical Care Medicine. 2004;170(8):836–44. doi: 10.1164/rccm.200401-033OC. [DOI] [PubMed] [Google Scholar]
- Gold 2001 {published data only} .Gold M, Jõgi R, Mulder PGH, Akveld MLM. Salmeterol/ fluticasone propionate combination 50/100μg bid is more effective than fluticasone propionate 100μg bid plus montelukast 10 mg once daily in reducing exacerbations. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):262s. [Google Scholar]
- Grootendorst 2001 {published data only} .Grootendorst DC, Dahlen SE, Van Den Bos JW, Duiverman EJ, Veselic-Charvat M, Vrijlandt EJ, et al. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clinical and Experimental Allergy. 2001;31(3):400–8. doi: 10.1046/j.1365-2222.2001.01022.x. [DOI] [PubMed] [Google Scholar]
- Grutters 1999 {published data only} .Grutters J, Brinkman L, Koenderman L, Van den Bosch J, Lammers JW. The effect of treatment of allergic asthmatics with salmeterol (SLM), beclomethasone (BDP) or the combination on lung function and bronchial hyper-responsiveness (BHR) after allergen challenge. European Respiratory Journal. 1997;Vol. 10(issue Suppl 25):474s. [Google Scholar]; *; Grutters JC, Brinkman L, Aslander MM, van der Bosch JMM, Koenderman L, Lammers JMJ. Asthma modulates priming - associated blood eosinophil responsiveness in allergic asthmatics. European Respiratory Journal. 1999;14:915–22. doi: 10.1034/j.1399-3003.1999.14d31.x. [DOI] [PubMed] [Google Scholar]
- Gustafsson 1994 {published data only} .Gustafsson PM, Von BA, Jenkins MM. Salmeterol 50 mug twice daily in the treatment of mild-to-moderate asthma in childhood - a comparison of two inhalation devices. European Journal of Clinical Research. 1994;5:63–73. [Google Scholar]
- Hacki 2001 {published data only} .Hacki M, Knoblauch A, Leuppi J. Asthma treatment. Pharma-Kritik. 2001;23(16):61–4. [Google Scholar]
- Hasani 2003 {published data only} .Hasani A, Toms N, O’Connor J, Dilworth JP, Agnew JE. Effect of salmeterol xinafoate on lung mucociliary clearance in patients with asthma. Respiratory Medicine. 2003;97(6):667–71. doi: 10.1053/rmed.2003.1498. [DOI] [PubMed] [Google Scholar]
- Heyneman 2002 {published data only} .Heyneman CA, Crafts R, Holland J, Arnold AD. Fluticasone versus salmeterol/low-dose fluticasone for long-term asthma control. Annals of Pharmacotherapy. 2002;36(12):1944–9. doi: 10.1345/aph.1A311. [DOI] [PubMed] [Google Scholar]
- Hultquist 2000 {unpublished data only} .Hultquist C. Personal communication. 2000. Unpublished data.
- Ind 2002 {published data only} .Ind PW, Villasante C, Shiner RJ, Pietinalho A, Boszormenyi NG, Soliman S, et al. Safety of formoterol by Turbuhaler as reliever medication compared with terbutaline in moderate asthma. European Respiratory Journal. 2002;20(4):859–66. doi: 10.1183/09031936.02.00278302. [DOI] [PubMed] [Google Scholar]
- Isabelle 2001 {published data only} .Isabelle P, Bjamer D, Neuparth N, Desfougeres JL. Efficacy and safety of salmeterol/fluticasone combination 50/ 100mug bd via two different powder devices in children. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Jarvis 1999 {published data only} .Jarvis B, Faulds D. Inhaled fluticasone propionate. A review of its therapeutic efficacy at dosages <= 500 mug/day in adults and adolescents with mild to moderate asthma. Drugs. 1999;57(5):769–803. doi: 10.2165/00003495-199957050-00016. [DOI] [PubMed] [Google Scholar]
- Jeffery 2002 {published data only} .Jeffery PK, Venge P, Gizycki MJ, Egerod I, Dahl R, Faurschou P. Effects of salmeterol on mucosal inflammation in asthma: a placebo-controlled study. European Respiratory Journal. 2002;20(6):1378–85. doi: 10.1183/09031936.02.00542001. [DOI] [PubMed] [Google Scholar]
- Jenkins 2002a {published data only} .Jenkins C, Wilson J, Rutherford C, Perry AS, Whitehead PJ. Asthma management costs are lower with combination fluticasone/salmeterol (25/50 mcg BD) in a single inhaler than with budesonide (800 mcg BD) plus eformoterol (12 mcg BD) via separate inhalers. 2002. Respirology. 2002;Vol. 7(issue Suppl):A20. [: P23] [Google Scholar]
- Jenkins 2002b {published data only} .Jenkins C. Combination therapy with fluticasone and salmeterol for symptomatic asthma produces similar benefits when given by accuhaler in a single or two separate devices over 24 weeks. Respirology. 2002;Vol. 7(issue Suppl):A20. [Google Scholar]
- Johansson 1999 {published data only} .Johansson G, Price MJ, Sondhi S. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/100mug versus fluticasone propionate 100mug in adults and adolescents with asthma III. Pharmacoeconomics. 1999;16(Suppl 2):15–21. [Google Scholar]
- Jones 1994 {published data only} .Jones KP. Salmeterol xinafoate in the treatment of mild to moderate asthma in primary care. Thorax. 1994;49:971–5. doi: 10.1136/thx.49.10.971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juniper 1995 {published data only} .Juniper EF, Johnston PR, Borkhoff CM, Guyatt GH, Boulet LP, Haukioja A. Quality of life in asthma clinical trials: comparison of salmeterol and salbutamol. American Journal of Respiratory & Critical Care Medicine. 1995;151(1):66–70. doi: 10.1164/ajrccm.151.1.7812574. [DOI] [PubMed] [Google Scholar]
- Juniper 1999 {published data only} .Juniper EF, Svenson K, O’Byrne PM, Barnes PJ, Bauer CA, Lofdahl C-GA, et al. Asthma quality of life during 1 year of treatment with budesonide with or without formoterol. European Respiratory Journal. 1999;14:1038–43. doi: 10.1183/09031936.99.14510389. [DOI] [PubMed] [Google Scholar]
- Kalra 1996 {published data only} .Kalra S, Swystun VA, Bhagat R, Cockcroft DW. Inhaled corticosteroids do not prevent the development of tolerance to the bronchoprotective effect of salmeterol. Chest. 1996;109(4):953–6. doi: 10.1378/chest.109.4.953. [DOI] [PubMed] [Google Scholar]
- Kardos 2001 {published data only} .Kardos P, Bruggenjurgen B, Martin A, Meyer-Sabellek W, Richter K, Vogelmeier C, et al. Treatment of bronchial asthma using a new adjustable combination treatment plan: Asthma Control Plan (ATACO) [German] Pneumologie. 2001;55(5):253–7. doi: 10.1055/s-2001-13947. [DOI] [PubMed] [Google Scholar]
- Kavuru 2000 {published data only} .Edin HM, Payne E, Herrle MR, Schoaf L, Mather DB, Scott CA, et al. Salmeterol/fluticasone propionate combination via HFA MDI improves quality of life in asthma patients. Journal of Allergy and Clinical Immunology. 2001;Vol. 107(issue 2):s246. [Google Scholar]; Edin HM, Prillaman B, Baitinger LA, House K, Shah TP. Improved ability to perform strenuous activities after treatment with fluticasone propionate-salmeterol combination. American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A112. [Google Scholar]; Edwards T, Gross G, Mitchell D, Chervinsky P, Woodring A, Baitinger L, et al. The salmeterol xinafoate/fluticasone propionate dry powder combination product via Diskus® inhaler improves asthma control compared to salmeterol xinafoate or fluticasone propionate dry powder alone. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A414. [Google Scholar]; Johansson G, Price MJ, Sondhi S. Cost-effectiveness analysis of salmeterol/fluticasone propionate 50/100mug vs fluticasone propionate 100mug in adults and adolescents with asthma III: results. Pharmacoeconomics. 1999;16(Suppl 2):15–21. [Google Scholar]; Kavuru M, Melamed J, Gross G, Laforce C, House K, Prilaman B. Salmeterol and fluticasone propionate combined in a new powder inhalation device for the treatment of asthma: a randomised, double blind,placebo controlled trial. Journal of Allergy and Clinical Immunology. 2000;105(6):1108–16. doi: 10.1067/mai.2000.105711. [DOI] [PubMed] [Google Scholar]; Nathan R, Woodring A, Baitinger L, Prillaman B, Faris M, House K, et al. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. The salmeterol/fluticasone propionate diskus combination decreases the incidence of exacerbations compared to treatment with salmeterol or fluticasone propionate alone; p. 848. 1999. [Google Scholar]; *; Nathan RA, Dorinsky P, Carranza Rosenzweig JRC, Shah T, Edin H, Prillaman B. Improved ability to perform strenuous activities after treatment with fluticasone propionate/ salmeterol combination in patients with persistent asthma. Journal of Asthma. 2003;40(7):815–22. doi: 10.1081/jas-120023573. [DOI] [PubMed] [Google Scholar]
- Keating 2002 {published data only} .Keating GM, Faulds D. A multi-dose dry powder inhaler. Drugs. 2002;62(13):1887–95. doi: 10.2165/00003495-200262130-00005. [DOI] [PubMed] [Google Scholar]
- Keith 2001 {published data only} .Cowie R, Boulet LP, Stepner N, Simms L, Johnson D, Scott C, et al. Fluticasone propionate/salmeterol (FSC) HfaMDI therapy provides effective control in the long-term (1 year) management of patients with persistent asthma (PA) American Journal of Respiratory and Critical Care Medicine. 2001;163(Suppl 5):A862. [Google Scholar]; Keith P, D Urzo A, Stepner N. Fluticasone/salmeterol combination (FSC) is safe and provides effective long-term (52 week) control in the management of patients with persistent asthma (PA) European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):176s. [Google Scholar]
- Kemp 1984 {published data only} .Kemp JP, Chervinsky P, Orgel HA, Meltzer EO, Noyes JH, Mingo TS. Concomitant bitolterol mesylate aerosol and theophylline for asthma therapy, with 24 hr electrocardiographic monitoring. Journal of Allergy & Clinical Immunology. 1984;73(1 part 1):32–43. doi: 10.1016/0091-6749(84)90481-0. [DOI] [PubMed] [Google Scholar]
- Kemp 1998 {published data only} .Kemp JP, Cook DA, Incaudo GA, Corren J, Kalberg C, Emmett A, et al. Salmeterol improves quality of life in patients with asthma requiring inhaled corticosteroids. Journal of Allergy and Clinical Immunology. 1998;101:188–95. doi: 10.1016/s0091-6749(98)70383-5. [DOI] [PubMed] [Google Scholar]
- Ketchell 2002 {published data only} .Ketchell RI, Jensen MW, Spina D, O’Connor BJ. Dose-related effects of formoterol on airway responsiveness to adenosine 5′-monophosphate and histamine. European Respiratory Journal. 2002;19(4):611–16. doi: 10.1183/09031936.02.00332001. [DOI] [PubMed] [Google Scholar]
- Kidney 1995 {published data only} .Kidney J, Pizzichini MMM, Wong B, Morris MM, Efthimadis A, Dolovich J, et al. Salmeterol compared with beclomethasone and placebo on allergen induced asthmatic and inflammatory responses. European Respiratory Journal. 1995;(Suppl 8):19336s. doi: 10.1183/09031936.96.09030449. Vol. [DOI] [PubMed] [Google Scholar]
- Kirby 2000 {published data only} .Kirby S, Falcoz C, Daniel MJ, Milleri S, Squassante L, Ziviani L, et al. Salmeterol and fluticasone propionate given as a combination: lack of systemic pharmacodynamic and pharmacokinetic interactions. European Journal of Clinical Pharmacology. 2000;56(11):781–91. doi: 10.1007/s002280000233. [DOI] [PubMed] [Google Scholar]
- Knobil 2000 {published data only} .Knobil K, Dorinsky P, Yancey S, Emmett A, Rickard K. Salmeterol is superior to montelukast as add-on therapy to inhaled corticosteroids. European Respiratory Journal. 2000;Vol. 16(issue Suppl 31):457s. [Google Scholar]
- Knorr 2001 {published data only} .Knorr B, Franchi LM, Bisgaard H, Vermeulen JH, LeSouef P, Santanello N, et al. Montelukast, a leukotriene receptor antagonist, for the treatment of persistent asthma in children aged 2 to 5 years. Pediatrics. 2001;108(3):E48. doi: 10.1542/peds.108.3.e48. [DOI] [PubMed] [Google Scholar]
- Kopp 2002 {published data only} .Kopp M. Antiinflammatory therapy in different age groups. Arztliche Praxis Padiatrie. 2002;(issue 2):28–9. [Google Scholar]
- Kraft 2003 {published data only} .Kraft M, Martin RJ, Lazarus SC, Fahy JV, Boushey HA, Lemanske RF, Jr, et al. Airway tissue mast cells in persistent asthma: predictor of treatment failure when patients discontinue inhaled corticosteroids. Chest. 2003;124(1):42–50. doi: 10.1378/chest.124.1.42. [DOI] [PubMed] [Google Scholar]
- Kuna 2002 {published data only} .Kuna P, Kuprys I. Symbicort Turbuhaler: a new concept in asthma management. International Journal of Clinical Practice. 2002;56(10):797–803. [PubMed] [Google Scholar]
- LaForce 1994 {published data only} .LaForce C, Liddle RF, Yancey SW. Salmeterol response in asthmatic patients using inhaled corticosteroids and in those not using inhaled corticosteroids. Annals of Allergy. 1994 [Google Scholar]
- Lai 1995 {published data only} .Lai CKW, Chan CHS, Ho SS, Hui ACF, Lai KN. Inhaled salmeterol and albuterol in asthmatic patients receiving high-dose inhaled corticosteroids. Chest. 1995;108:36–40. doi: 10.1378/chest.108.1.36. [DOI] [PubMed] [Google Scholar]
- Lange 2001 {published data only} .Lange ML, House KW, Scott CA, Shah TP, Akveld MLM. The salmeterol/fluticasone propionate combination 50/ 100μg bid is effective as initial maintenance therapy in mild and moderate asthmatics. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):176s. [Google Scholar]
- Langton Hewer 1995 {published data only} .Langton Hewer S, Hobbs J, French D, Lenney W. Pilgrims progress: the effect of salmeterol in older children with chronic severe asthma. Respiratory Medicine. 1995;89:435–40. doi: 10.1016/0954-6111(95)90213-9. [DOI] [PubMed] [Google Scholar]
- Lazarus 2001 {published data only} .Lazarus SC, Boushey HA, Fahy JV, Chinchilli VM, Lemanske RF, Jr, Sorkness CA, et al. Long-acting beta2 agonist monotherapy vs continued therapy with inhaled corticosteroids in patients with persistent asthma: a randomized controlled trial. JAMA. 2001;285(20):2583–93. doi: 10.1001/jama.285.20.2583. [DOI] [PubMed] [Google Scholar]
- Leblanc 1996 {published data only} .Leblanc P, Knight A, Kreisman H, Borkhoff CM, Johnston PR. A placebo-controlled, crossover comparison of salmeterol and salbutamol in patients with asthma. American Journal of Respiratory and Critical Care Medicine. 1996;154:324–8. doi: 10.1164/ajrccm.154.2.8756801. [DOI] [PubMed] [Google Scholar]
- Lemanske 2001 {published data only} .*; Lemanske RF, Sorkness C, Mauger E, Lazarus S, Boushey H, Fahy J, et al. Inhaled corticosteroid reduction and elimination in patients with persistent asthma receiving salmeterol: a randomized controlled trial. JAMA. 2001;285(20):2594–603. doi: 10.1001/jama.285.20.2594. [DOI] [PubMed] [Google Scholar]
- Lenney 1995 {published data only} .Lenney W, Pedersen S, Boner AL, Ebbutt A, Jenkins MM, on behalf of an International Study Group Efficacy and safety of salmeterol in childhood asthma. European Journal of Pediatrics. 1995;154:983–90. doi: 10.1007/BF01958642. [DOI] [PubMed] [Google Scholar]
- LHSRG 2000 {published data only} .The Lung Health Study Research Group Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary disease. New England Journal of Medicine. 2000;343(26):1902–9. doi: 10.1056/NEJM200012283432601. [DOI] [PubMed] [Google Scholar]
- Lindqvist 2001 {published data only} .Lindqvist AE, Karjalainen EM, Laitinen LA, Kava T, Altraja A, Pulkkinen M, et al. Salmeterol (sim), fluticasone propionate (fp) or disodium cromoglycate (dscg) in the treatment of newly diagnosed asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Lipworth 1998 {published data only} .Lipworth B, Tan S, Devlin M, Aiken T, Baker R, Hendrick D. Effects of treatment with formoterol on broncho-protection against methacholine. American Journal of Medicine. 1998;104(5):431–8. doi: 10.1016/s0002-9343(98)00086-2. [DOI] [PubMed] [Google Scholar]
- Lipworth 1999a {published data only} .Lipworth BJ, Hall IP, Aziz I, Tan KS, Wheatley A. Beta2-adrenoceptor polymorphism and broncho-protective sensitivity with regular short- and long-acting beta2-agonist therapy. Clinical Science. 1999;96(3):253–9. [PubMed] [Google Scholar]
- Lipworth 1999b {published data only} .Lipworth BJ, Aziz I. A high dose of albuterol does not overcome broncho-protective sub-sensitivity in asthmatic subjects receiving regular salmeterol or formoterol. Journal of Allergy & Clinical Immunology. 1999;103(1 part 1):88–92. doi: 10.1016/s0091-6749(99)70530-0. [DOI] [PubMed] [Google Scholar]
- Lipworth 2000 a {published data only} .Lipworth BJ, Dempsey OJ, Aziz I. Functional antagonism with formoterol and salmeterol in asthmatic patients expressing the homozygous glycine-16 beta(2)-adrenoceptor polymorphism. Chest. 2000;118(2):321–8. doi: 10.1378/chest.118.2.321. [DOI] [PubMed] [Google Scholar]
- Lipworth 2000 b {published data only} .Lipworth BJ, Dempsey OJ, Aziz I, Wilson AM. Effects of adding a leukotriene antagonist or a long-acting beta(2)-agonist in asthmatic patients with the glycine-16 beta(2)-adrenoceptor genotype. American Journal of Medicine. 2000;109(2):114–21. doi: 10.1016/s0002-9343(00)00454-x. [DOI] [PubMed] [Google Scholar]
- Lipworth 2002 {published data only} .Lipworth BJ, Jackson CM. Marginal benefits of adding formoterol. Thorax. 2002;Vol. 57(issue 12):1089. doi: 10.1136/thorax.57.12.1089-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lockey 1999 {published data only} .Lockey RF, DuBuske LM, Friedman B, Petrocella V, Cox F, Rickard K. Nocturnal asthma: effect of salmeterol on quality of life and clinical outcomes. Chest. 1999;115(3):666–73. doi: 10.1378/chest.115.3.666. [DOI] [PubMed] [Google Scholar]
- Lowhagen 2002 {published data only} .Lowhagen O, Wever AMJ, Lusuardi M, Moscato G, De Backer WA, Gandola L, et al. The inflammatory marker serum eosinophil cationic protein (ECP) compared with PEF as a tool to decide inhaled corticosteroid dose in asthmatic patients. Respiratory Medicine. 2002;96(2):95–101. doi: 10.1053/rmed.2001.1218. [DOI] [PubMed] [Google Scholar]
- Lucioni 2002 {published data only} .Lucioni C, Mangrella M, Mazzi S, Negrini C, Vaghi A. Treatment of patients with asthma with a fixed combination of budesonide and formoterol: A pharmacoeconomic evaluation versus some therapeutic alternatives. Pharmacoeconomics - Italian Research Articles. 2002;4(1):15–23. [Google Scholar]
- Lötvall 2002 {published data only} .Lötvall J, van der Woude HJ, Palmqvist M, Arvidsson P, Beckman O, Boorsma M, et al. More rapid onset of action of budesonide/formoterol (Symbicort®) than salmeterol/ fluticasone (Seretide™) American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A567. [Google Scholar]
- Magadle 2001 {published data only} .Magadle R, Berar-Yanay N, Weiner P. Long-acting bronchodilators in premenstrual exacerbation of asthma. Respiratory Medicine. 2001;95(9):740–3. doi: 10.1053/rmed.2001.1132. [DOI] [PubMed] [Google Scholar]
- Malmqvist-Granlund 2000 {published data only} .Malmqvist-Granlund K, Asking L, Lindbald T, Rollwage U, Steckel H. An in vitro comparison of budesonide/ formoterol and fluticasone/salmeterol in dry powder inhalers. European Respiratory Journal. 2000;Vol. 16(issue Suppl 31):455s. [Google Scholar]
- Malolepszy 2002 {published data only} .Malolepszy J. Efficacy and tolerability of oral theophylline slow-release versus inhalative formoterol in moderate asthma poorly controlled on low-dose steroids. Atemwegsund Lungenkrankheiten. 2002;28(2):78–87. [Google Scholar]
- McCarthy 2000 {published data only} .McCarthy TP, Boone R, Yancey S, Rickard K. Salmeterol compared to montelukast as adjunctive therapy to inhaled corticosteroids. Thorax. 2000;Vol. 55(issue Suppl 3):A63. [Google Scholar]
- McCarthy 2002 {published data only} .McCarthy TP, Grening AP, Holgate SK, Whitehead C, Rice L. Salmeterol/fluticasone propionate combination (SFC) is more effective that beclometasone dipropionate (BDP) in patients not well controlled on bronchodilators alone. American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A566. [Google Scholar]
- Mcivor 1998 {published data only} .Mcivor RA, Pizzichini E, Turner MO, Hussack P, Hargreave FE, Sears MR. Potential masking effects of salmeterol on airway inflammation in asthma. American Journal of Respiratory & Critical Care Medicine. 1998;158(3):924–30. doi: 10.1164/ajrccm.158.3.9802069. [DOI] [PubMed] [Google Scholar]
- Meier 1997 {published data only} .Meier CR, Jick H. Drug use and pulmonary death rates in increasingly symptomatic asthma patients in the UK. Thorax. 1997;52(7):612–7. doi: 10.1136/thx.52.7.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meijer 1995 {published data only} .Meijer Ferda G, Postma Dirkje S, Mulder Paul GH, Van Aalderen Wim MC. Long-term circadian effects of salmeterol in asthmatic children treated with inhaled corticosteroids. American Journal of Respiratory and Critical Care Medicine. 1995;152:1887–92. doi: 10.1164/ajrccm.152.6.8520751. [DOI] [PubMed] [Google Scholar]
- Michel 2000 {published data only} .Michel O, Olbrecht J, Moulard D, Sergysels R. Effect of anti-asthmatic drugs on the response to inhaled endotoxin. Annals of Allergy, Asthma, and Immunology. 2000;85(4):305–10. doi: 10.1016/S1081-1206(10)62534-3. [DOI] [PubMed] [Google Scholar]
- Midgren 1992 {published data only} .Midgren B, Melander B, Persson G. Formoterol, a new long-acting beta 2 agonist, inhaled twice daily, in stable asthmatic subjects. Chest. 1992;101(4):1019–22. doi: 10.1378/chest.101.4.1019. [DOI] [PubMed] [Google Scholar]
- Miraglia del Giudice {published data only} .Miraglia del Giudice M, Capristo M, Amelio R, Rocco A, Fusco N, Brunese FP. Combined fluticasone propionate/ salmeterol (Diskus) vs fluticasone propionate (Diskus) in the control of persistent asthma in children. American Thoracic Society 99th International Conference; Poster D78; 2003. p. A117. [Google Scholar]
- Molimard 2001 {published data only} .Molimard M, Bourcereau J, Le Gros V, Bourdeix I, Leynadier F, Duroux P. Comparison between formoterol 12 ug bid and on-demand salbutamol in moderate persistent asthma. Respiratory Medicine. 2001;95(1):64–70. doi: 10.1053/rmed.2000.0972. [DOI] [PubMed] [Google Scholar]
- Murray 1998 {published data only} .Murray JJ, Hagaman DD, Dworski R, Keane B, Sheller JR. Inhibition by salmeterol and beclomethasone of late phase response to segmental antigen challenge in asthmatics. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A872. [Google Scholar]
- Nagel 2002 {published data only} .Nagel MW, Wiersema KJ, Bates SL, Mitchell JP. Performance of large- and small-volume valved holding chambers with a new combination long-term bronchodilator/anti-inflammatory formulation delivered by pressurized metered dose inhaler. Journal of Aerosol Medicine. 2002;15(4):427–33. doi: 10.1089/08942680260473506. [DOI] [PubMed] [Google Scholar]
- Nathan 1998 {published data only} .Nathan RA, Pinnas JL, Schwartz HJ, Grossman J, Yancey SW, Emmett AH, et al. A six-month, placebo-controlled comparison of the safety and efficacy of salmeterol or beclomethasone for persistent asthma. Annals of Allergy, Asthma, and Immunology. 1999;82:521–9. doi: 10.1016/S1081-1206(10)63159-6. [DOI] [PubMed] [Google Scholar]
- Nathan 2001 {published data only} .Nathan RA, Mitchell D, Condemi J, Heller A, Schoaf L, Herrle M, et al. Cardiovascular and hypothalamic-pituitary-adrenal axis safety of fluticasone propionate/salmeterol HFA MDI in adolescent and adult patients with asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; Rooklin A, Elkayam D, Weiler J, Windom H, Schoaf L, Scott C, et al. The fluticasone propionate/salmeterol HFA MDI is significantly more efficacious in treating asthma than placebo HFA MDI, fluticasone propionate CFC MDI or salmeterol CFC MDI. Journal of Allergy and Clinical Immunology. 2001;Vol. 107(issue 2):s100. [Google Scholar]
- Nelson 1999 {published data only} .Nelson HS, Berkowitz RB, Tinkelman DA, Emmett AH, Rickard KA, Yancey SW. Lack of subsensitivity to albuterol after treatment with salmeterol in patients with asthma. American Journal of Respiratory and Critical Care Medicine. 1999;159(5 part 1):1556–61. doi: 10.1164/ajrccm.159.5.9807128. [DOI] [PubMed] [Google Scholar]
- Nelson 2000 {published data only} .Nelson H, Chervinsky P, Greos L, Pelskow W, Baitinger L, Scott C, et al. The salmeterol/fluticasone propionate combination product improves asthma control compared with the individual products in asthmatics treated with prn short-acting beta2-agonists alone. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue Suppl 3):A196. [Google Scholar]; Nelson HS, Baitinger L, Scott C, House K, Payne E, Shah T. Salmeterol/fluticasone propionate (50/100μg dose) non-CFC metered dose inhaler is safe and effective in in patients with asthma using short-acting ß2-agonists alone. European Respiratory Journal. 2000;Vol. 16(issue 31):53s. [Google Scholar]; Nelson HS, Busse WW, Kerwin E, Church N, Emmett A, Rickard K, et al. Fluticasone propionate/salmeterol combination provides more effective asthma control than low-dose inhaled corticosteroid plus montelukast. Journal of Allergy and Clinical Immunology. 2000;106(6):1088–95. doi: 10.1067/mai.2000.110920. [DOI] [PubMed] [Google Scholar]; Nelson HS, Chervinsky P, Greos L, Pleskow W, Baitinger L, Scott C, et al. The salmeterol/fluticasone propionate combination product improves asthma control compared with the individual products in asthmatics treated with PRN short-acting beta2-agonists alone. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue 3 part 2 (Suppl 1)):A196. [Google Scholar]
- Nelson 2001 {published data only} .Nelson HS, Nathan RA, Kalberg C, Yancey SW, Rickard KA. Comparison of inhaled salmeterol and oral zafirlukast in asthmatic patients using concomitant inhaled corticosteroids. Medscape General Medicine. 2001;Vol. 3(issue 4):3. [PubMed] [Google Scholar]
- Nelson 2003 {published data only} .Nelson HS, Wolfe JD, Gross D, Geos LS, Baitinger L, Scott C, et al. Efficacy and safety of fluticasone propionate 44mcg/salmeterol 21mcg administered in a hydrofluoroalkane metered-dose inhaler as an initial asthma maintenance treatment. Annals of Allergy, Asthma, and Immunology. 2003;91:263–9. doi: 10.1016/s1081-1206(10)63528-4. [DOI] [PubMed] [Google Scholar]; *; Pyke SD, Frith L, Pritchard J, Johnson M, Theophilus A, Shah T. Synergy with salmeterol and fluticasone propionate after administration from a single inhaler (Seretide™) European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):176s. [Google Scholar]
- Newnham 1995 {published data only} .Newnham DM, Grove A, McDevitt DG, Lipworth BJ. Subsensitivity of bronchodilator and systemic beta 2 adrenoceptor responses after regular twice daily treatment with eformoterol dry powder in asthmatic patients. Thorax. 1995;50(5):497–504. doi: 10.1136/thx.50.5.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen 1999 {published data only} .Nielsen LP, Pedersen B, Faurschou P, Madsen F, Wilcke JTR, Dahl R. Salmeterol reduces the need for inhaled corticosteroids in steroid-dependent asthmatics. Respiratory Medicine. 1999;93:863–68. doi: 10.1016/s0954-6111(99)90051-3. [DOI] [PubMed] [Google Scholar]
- Nightingale 2002 {published data only} .Nightingale JA, Rogers DF, Barnes PJ. Comparison of the effects of salmeterol and formoterol in patients with severeasthma. Chest. 2002;121(5):1401–6. doi: 10.1378/chest.121.5.1401. [DOI] [PubMed] [Google Scholar]
- Norhaya 1999 {published data only} .Norhaya MR, Yap TM, Zainudin BMZ. Addition of inhaled salmeterol to inhaled corticosteroids in patients with poorly controlled nocturnal asthma. Respirology. 1999;4:77–81. doi: 10.1046/j.1440-1843.1999.00153.x. [DOI] [PubMed] [Google Scholar]
- Nsouli 2001 {published data only} .Nsouli SM, McNutt WJ. The additive effects of montelukast and salmeterol in moderate asthmatics who are uncontrolled on a low dose on inhaled corticosteroids. Annals of Allergy, Asthma and Immunology. 2001;86:81. [Google Scholar]
- O’Brian 2001 {published data only} .O’Brian J, Carlos-Palma A, Bogolubov M, Davies P, Payne E. Benefits of fluticasone propionate/salmeterol [fp/s] hfa mdi are apparent on the first day of dosing. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- O’Connor 2002 {published data only} .O’Connor RD, O’Donnell JC, Pinto LA, Wiener DJ, Legorreta AP. Two-year retrospective economic evaluation of three dual-controller therapies used in the treatment of asthma. Chest. 2002;121(4):1028–35. doi: 10.1378/chest.121.4.1028. [DOI] [PubMed] [Google Scholar]
- Orsida 2001 {published data only} .Orsida BE, Ward C, Li X, Bish R, Wilson JW, Thien F, et al. Effect of a long-acting beta(2)-agonist over three months on airway wall vascular remodelling in asthma. American Journal of Respiratory and Critical Care Medicine. 2001;164(1):117–21. doi: 10.1164/ajrccm.164.1.2006003. [DOI] [PubMed] [Google Scholar]
- Palmer 1992 {published data only} .Palmer JBD, Stuart AM, Shepherd GL, Viskum K. Inhaled salmeterol in the treatment of patients with moderate to severe reversible obstructive airways disease - a 3 month comparison of the efficacy and safety of twice-daily salmeterol (100 mcg) with salmeterol (50 mcg) Respiratory Medicine. 1992;86:409–17. doi: 10.1016/s0954-6111(06)80008-9. [DOI] [PubMed] [Google Scholar]
- Palmqvist 2001 {published data only} .Palmqvist M, Arvidsson P, Beckman O, Peterson S, Lotvall J. Onset of bronchodilation of budesonide/formoterol vs salmeterol/fluticasone in single inhalers. Pulmonary Pharmacology & Therapeutics. 2001;14(1):29–34. doi: 10.1006/pupt.2000.0260. [DOI] [PubMed] [Google Scholar]
- Paterson 1999 {published data only} .Paterson MC, Wilson AM, Dempsey OJ, Sims EJ, Lipworth BJ. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. The effect of combination therapy with salmeterol and montelukast in asthmatic patients receiving inhaled corticosteroids; p. 3490. 1999. [Google Scholar]
- Pauwels 1998 {published data only} .Pauwel RA, Yernault JC, Demedts MG, Geusens P. Safety and efficacy of fluticasone and beclomethasone in moderate to severe asthma. American Journal of Respiratory & Critical Care Medicine. 1998;157(3 part 1):827–32. doi: 10.1164/ajrccm.157.3.9610009. [DOI] [PubMed] [Google Scholar]
- Pearlman 1992 {published data only} .Pearlman DA, Chervinsky P, LaForce C, Seltzer JM, Southern DL, Kemp JP, et al. A comparison of salmeterol with albuterol in the treatment of mild to moderate asthma. NEJM. 1992;327:1420–5. doi: 10.1056/NEJM199211123272004. [DOI] [PubMed] [Google Scholar]
- Pearlman 1994 {published data only} .Pearlman DS, Liddle R. Controlling asthma symptoms: salmeterol compared with salbutamol in large-scale multicentre studies. European Respiratory Review. 1994;4(21):301–5. [Google Scholar]
- Pearlman 2001 {published data only} .Pearlman DS, Kent E, Lanz MJ, Peden D, Baitinger L, Herrle M, et al. Fluticasone propionate/salmeterol HFA MDI has a rapid onset of effect in asthmatics treated with short or long-acting beta2-agonists (ba) or inhaled corticosteroids. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Pearlman 2002 {published data only} .*; Pearlman DS, White MV, Lieberman AK, Pepsin PJ, Kalberg C, Emmett A, et al. Fluticasone propionate/ salmeterol combination compared with montelukast for the treatment of persistent asthma. Annals of Allergy, Asthma, and Immunology. 2002;88(2):227–35. doi: 10.1016/S1081-1206(10)62001-7. [DOI] [PubMed] [Google Scholar]
- Perez 2000 {published data only} .Perez O. Montelukast treatment in children with asthma. Revista Alergia Mexico. 2000;47(1):30–2. [PubMed] [Google Scholar]
- Peters 2000 {published data only} .Peters JI, Shelledy DC, Jones AP, Jr, Lawson RW, Davis CP, LeGrand TS. A randomized, placebo-controlled study to evaluate the role of salmeterol in the in-hospital management of asthma. Chest. 2000;118(2):313–20. doi: 10.1378/chest.118.2.313. [DOI] [PubMed] [Google Scholar]
- Pifferi 2002 {published data only} .Pifferi M, Caramella D, Ragazzo V, Pietrobelli A, Boner AL. Low-density areas on high-resolution computed tomograms in chronic pediatric asthma. Journal of Pediatics. 2002;141(1):104–8. doi: 10.1067/mpd.2002.125006. [DOI] [PubMed] [Google Scholar]
- Pinnas 1998 {published data only} .Pinnas JL, Schwartz H, Yancey SW, Rickard K. Six month comparison of beclomethasone vs. salmeterol or placebo in adults with asthma. American Journal of Respiratory and Critical Care Medicine. 1998;Vol. 157(issue Suppl 3):A417. [Google Scholar]
- Pizzichini 1996 {published data only} .Pizzichini MM, Kidney JC, Wong BJ, Morris MM, Efthimiadis A, Dolovich J, et al. Effect of salmeterol compared with beclomethasone on allergen-induced asthmatic and inflammatory responses. European Respiratory Journal. 1996;9(3):449–55. doi: 10.1183/09031936.96.09030449. [DOI] [PubMed] [Google Scholar]
- Pljaskic-Kamenov 2000 {published data only} .Pljaskic-Kamenov SS, Filipovic MD, Kamenov BA. Comparison of addition of salmeterol xinafoate to budesonide with budesonide alone on symptoms and quality of life in asthmatic children. European Respiratory Journal. 2000;Vol. 16(issue Suppl 31):518s. [Google Scholar]
- Pohl 2006 {published data only} .Pohl W, Vetter N, Zwick H, Hrubbs W. Budesonide/ formoterol adjustable maintenance dosing (AMD) improves health related quality of life (HRQL) compared with highdose budesonide (AMD) [Abstract] European Respiratory Journal. 2004;24(Suppl 48):311s. [Google Scholar]; *; Pohl WR, Vetter N, Zwick H, Hrubos W. Adjustable maintenance dosing with budesonide/formoterol or budesonide: double-blind study. Respiratory Medicine. 2006;100(3):551–60. doi: 10.1016/j.rmed.2005.05.019. [DOI] [PubMed] [Google Scholar]
- Pohunek 2006 {published data only} .Pohunek P, Kuna P, De Boeck K. Budesonide/formoterol improves lung function compared with budesonide alone in children with asthma [Abstract] European Respiratory Journal. 2004;24(Suppl 48):379s. doi: 10.1111/j.1399-3038.2006.00425.x. [DOI] [PubMed] [Google Scholar]; Pohunek P, Kuna P, Jorup C, De Boeck K. Budesonide/ formoterol improves lung function compared with budesonide alone in children with asthma. Pediatric Allergy and Immunology. 2006;17(6):458–65. doi: 10.1111/j.1399-3038.2006.00425.x. [DOI] [PubMed] [Google Scholar]; *; Pohunek P, Matulka M, Rybnicek O, Kopriva F, Honomichlova H, Svobodova T. Dose-related efficacy and safety of formoterol (Oxis) Turbuhaler compared with salmeterol Diskhaler in children with asthma. Pediatric Allergy and Immunology. 2004;15(1):32–9. doi: 10.1046/j.0905-6157.2003.00096.x. [DOI] [PubMed] [Google Scholar]
- Price 2002 {published data only} .Price D, Dutchman D, Mawson A, Bodalia B, Duggan S, Todd P. FLOW (Eformoterol in the management of mild asthma-formoterol Turbohaler with budesonide turbohaler) Research group. Thorax. 2002;57:791–8. doi: 10.1136/thorax.57.9.791. [DOI] [PMC free article] [PubMed] [Google Scholar]; Price MJ, Briggs AH. Development of an economic model to assess the cost effectiveness of asthma management strategies. Pharmacoeconomics. 2002;Vol. 20(issue 3):183–94. doi: 10.2165/00019053-200220030-00004. [DOI] [PubMed] [Google Scholar]; Price MJ, Sondhi S, Yan S, Nyth A, House K. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Salmeterol/ fluticasone propionate combination inhaler is more cost effective than fluticasone propionate in patients with asthma. 1999. [Google Scholar]
- Pujet 1995 {published data only} .Pujet JC, Evano CI. A randomized double-blind study comparing inhaled beclomethasone with long-acting theophylline for the first-line treatment of moderate asthma. Semaine Des Hopitaux. 1995;71(27-28):865–72. [Google Scholar]
- Pyke 2001 {published data only} .Pyke SD, Frith L, Pritchard J, Johnson M, Theophilus A, Shah T. Synergy with salmeterol and fluticasone propionate after administration from a single inhaler (Seretide™) European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):176s. [Google Scholar]
- Rance 2002 {published data only} .Rance L, Musin L. Asthma management costs in Canada are lower with combination fluticasone propionate/salmeterol (250/50mcg BID) in as single inhaler than with budesonide 800mcg BID plus eformoterol 12 mcg BID via separate inhalers. Chest (conference); San Diego, CA. 2002. p. s6. [Google Scholar]
- Remington 2002 {published data only} .Remington TL, Heaberlin A, DiGiovine B. Combined budesonide/formoterol turbuhaler treatment of asthma. Annals of Pharmacotherapy. 2002;36(12):1918–28. doi: 10.1345/aph.1C124. [DOI] [PubMed] [Google Scholar]
- Rickard 1999 {published data only} .Rickard KA, Yancey S, Emmett AH, Kalberg CJ. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Salmeterol compared to zafirlukast when added to inhaled corticosteroid therapy in patients with persistent asthma; p. 839. 1999. [Google Scholar]
- Rickard 2001 {published data only} .Rickard K, Dorinsky PM, Knobil K, Pepsin P, Akveld MLM. The salmeterol/fluticasone propionate combination 50/100μg bid is more effective than oral montelukast 10mg of as a first line therapy in mild and moderate asthmatics. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):262s. [Google Scholar]
- Rijssenbeek-Nouwens {published data only} .Rijssenbeek-Nouwens LHM, Oosting AJ, De Monchy JGR, Bregman I, Postma DS, De Bruin-Weller MS. The effect of anti-allergic mattress encasings on house dust mite-induced early- and late-airway reactions in asthmatic patients. A double-blind, placebo-controlled study. Clinical & Experimental Allergy. 2002;32(1):117–25. doi: 10.1046/j.0022-0477.2001.01256.x. [DOI] [PubMed] [Google Scholar]
- Ringbaek 1996 {published data only} .Ringbaek TJ, Soes-Petersen U, Christensen M, Iversen ET, Rasmussen FV. Salmeterol improves the control of disease in patients with moderate asthma. A comparative study of inhaled salmeterol 50 mg and salbutamol depot tablets 8 mg, both administered twice daily. Ugeskrift for Laeger. 1996;158(27):3940–43. [PubMed] [Google Scholar]
- Ringdal 1997 {published data only} .Ringdal N, Eliraz A, Pruzinec R, Weber HH, Mulder PG, Akveld M, et al. The salmeterol/fluticasone combination is more effective than fluticasone plus oral montelukast in asthma. Respiratory Medicine. 2003;97(3):234–4. doi: 10.1053/rmed.2003.1436. [DOI] [PubMed] [Google Scholar]
- Ringdal 2002 {published data only} .Alonso JF, Badiola C, Kielhorn A. Economic evaluation of salmeterol/fluticasone combination versus budesonide plus formoterol in Spain. European Respiratory Journal. 2001;18(Suppl 33):49s. [Google Scholar]; Ringdal N, Chuchalin A, Chovan L, Tudoric N, Maggi E, Whitehead PJ. Evaluation of different inhaled combination therapies (EDICT): a randomised, double-blind comparison of Seretide (50/250 microg bd Diskus vs. formoterol (12 microg bd) and budesonide (800 microg bd) given concurrently (both via Turbuhaler) in patients with moderate-to-severe asthma. Respiratory Medicine. 2002;96(11):851–61. doi: 10.1053/rmed.2002.1416. [DOI] [PubMed] [Google Scholar]; Ringdal N, Chuchalin AG, Chovan L, Whitehead PJ. A comparison of Advair™/Seretide™ (salmeterol 50 mcg/ fluticasone propionate 250 mcg bid) with formoterol 12 mcg + budesonide 800 mcg bid in moderate-severe asthma. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue 3 part 2 (Supp1)):A196. [Google Scholar]; Ringdal NR, Chovan L, Chuchalin AG, Whitehead PJ. Advair™/Seretide™ (250/50mu-g bid) shows exacerbation benefit over budesonide plus formoterol bid in moderate-severe asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Robert 2002 {published data only} .Robert J, Desfougeres JL. Contribution of salmeterol in ambulatory practice to the improvement of asthma and quality of life in childhood. Allergie et Immunologie. 2002;34(8):287–92. [PubMed] [Google Scholar]
- Rocca-Serra 2002 {published data only} .Rocca-Serra JP, Vicaut E, Lefrancois G, Umile A. Efficacy and tolerability of a new non-extrafine formulation of beclomethasone HFA-134a in patients with asthma: comparison with beclomethasone CFC. Clinical Drug Investigation. 2002;22(10):653–65. [Google Scholar]
- Rosenhall 2002 {published data only} .Rosenhall L, Heinig JH, Lindqvist A, Leegaard J, Stahl E, Bergqvist PB. Budesonide/formoterol (Symbicort) is well tolerated and effective in patients with moderate persistent asthma. International Journal of Clinical Practice. 2002;56(6):427–33. [PubMed] [Google Scholar]; Rosenhall L, Heinig JH, Lindqvist A, Leegard J, Bergqvist PBF. Symbicort (budesonide/eformoterol in a single inhaler) is safe and effective in the treatment of asthma. Thorax. 56(Suppl 3):iii 63. Vol. [Google Scholar]
- Rosenhall 2003 {published data only} .Rosenhall L, Elvstrand A, Tilling B, Vinge I, Jemsby P, Stahl E, et al. One-year safety and efficacy of budesonide/ formoterol in a single inhaler (Symbicort Turbuhaler ) for the treatment of asthma. Respiratory Medicine. 2003;97(6):702–8. doi: 10.1053/rmed.2003.1504. [DOI] [PubMed] [Google Scholar]; Rosenhall L, Heinig JH, Lindqvist A, Leegard J, Bergqvist PBF. Budesonide and formoterol in a single inhaler is safe and effective in the treatment of asthma. European Respiratory Journal. 2001;18(Suppl 33):159s. [Google Scholar]; Rosenhall L, Stahl E, Heinig JH, Lindquist A, Leegard J, Bergqvist PBF. Health-related quality of life and asthma control in patients using Symbicort® (budesonide and formoterol in a single inhaler). Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; *; Rosenhall L, Stahl E, Heinig JH, Lindqvist A, Leegard J, Bergqvist PBF. Health-related quality of life and asthma control in patients treated with budesonide and formoterol in a single inhaler. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):46s. [Google Scholar]
- Rosenthal 1999 {published data only} .Rosenthal RR, Busse WW, Kemp JP, Baker JW, Kalberg C, Emmett A, et al. Effect of long-term salmeterol therapy compared with as-needed albuterol use on airway hyper-responsiveness. Chest. 1999;116(3):595–602. doi: 10.1378/chest.116.3.595. [DOI] [PubMed] [Google Scholar]
- Roth 2002 {published data only} .Roth M, Johnson PR, Rudiger JJ, King GG, Ge Q, Burgess JK, et al. Interaction between glucocorticoids and beta2 agonists on bronchial airway smooth muscle cells through synchronised cellular signalling. Lancet. 2002;360(9342):1293–9. doi: 10.1016/S0140-6736(02)11319-5. [DOI] [PubMed] [Google Scholar]
- Russell 1995 {published data only} .Russell G, Williams DAJ, Weller P, Price JF. Salmeterol xinafoate on children on high dose inhaled steroids. Annals of Allergy, Asthma and Immunology. 1995;75:423–8. [PubMed] [Google Scholar]
- Saari 2002 {published data only} .Saari SM, Vidgren MT, Herrala J, Turjanmaa VMH, Koskinen MO, Nieminen MM. Possibilities of formoterol to enhanced the peripheral lung deposition of the inhaled liposome corticosteroids. Respiratory Medicine. 2002;96(12):999–1005. doi: 10.1053/rmed.2002.1393. [DOI] [PubMed] [Google Scholar]
- SAM40034 {unpublished data only} .Glaxo Smith Kline (SAM40034) A double-blind, randomised, parallel group, 12-week comparison of fluticasone propionate/salmeterol combination Diskus 100/ 50mcg BID with fluticasone propionate (FP) 250mcg BID as initial maintenance treatment in persistent asthma (Seretide Nordic Jump-Up Study) 2004 http://www.ctr.gsk.co.uk.; Kotaniemi J, Tiling B, Oien T. A double-blind randomised, parallel group study over 12 weeks comparing Seretide (50/100mcg bd Diskus) versus Flixotide ( 250 mcg bd Diskus) as first line regular treatment for steroid-naive adult patients. American Journal of Respiratory and Critical Care Medicine. 2003;Vol. 167(issue 7):A893. [Google Scholar]; Oien T, Tilling B, Kontaniemi J. 12 weeks comparing salmeterol/fluticasone propionate (SFC, 50/100mcg bd diskus) versus fluticasone propionate (FP, 250mcg bd diskus) as first-line regular asthma treatment. European Respiratory Journal. 2003;22(Suppl 22):236s. [Google Scholar]
- SAM40036 {unpublished data only} .Glaxo Smith Kline (SAM40036) A 12-week multicentre, randomised, double-blind, double-dummy, parallel group study to compare the efficacy and tolerability of once daily (QD) salmeterol/fluticasone propionate combination (salm/ FP) 50/100mcg at night via the DISKUS/ACCUHALER with QD budesonide (BUD) 400mcg at night via a breath-actuated dry powder inhaler (BADPI) as initial maintenance therapy in mild-to-moderate asthmatic subjects. 2004 http://www.ctr.gsk.co.uk.; Pauwels R, Smiltena I, Bagdonas A, Eliraz E, Firth R. Seretide once daily is more effective than budesonide 400mcg once daily in mild asthma. American Journal of Respiratory and Critical Care Medicine. 2004;169(7):A86. [Google Scholar]
- SAS30015 {published data only} .McCarthy TP, Greening AP, Holgate SK, Whitehead C, Rice L. The efficacy of salmeterol/fluticasone propionate combination (SFC) metered dose inhaler compared with beclomethasone dipropionate (BDP) in patients not well controlled at step 1 of the British guidelines on asthma management (BGAM) Thorax. 2001;Vol. 56(issue Suppl 3):iii 62. [Google Scholar]; McCarthy TP, Russell D, Baxter LE. A comparison of the efficacy of salmeterol/fluticasone propionate combination (SF) with beclometasone dipropionate (BDP) delivered via metered dose inhaler (MDI) in patients not well controlled on bronchodilators alone. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):53–4s. [Google Scholar]; SAS30015 A randomised, double-blind, double-dummy, cross-over, repeat dose study to compare the effects of SERETIDE DISKUS (salmeterol/fluticasone propionate combination; 50/250mcg) with co-administered salmeterol (50mcg) and fluticasone propionate (250mcg) DISKUS on lung function in Japanese and Caucasian asthmatic subjects. 2005 http://ctr.gsk.co.uk.; *; Tolley K, Martin A, Rice L, McCarthy TP. Salmeterol/ fluticasone propionate combination (SFC) demonstrates improved health outcomes and good cost effectiveness compared with beclometasone dipropionate. American Journal of Respiratory and Critical Care Medicine. 2002;165(Suppl 8):A112. [Google Scholar]
- Schreurs 1996 {published data only} .Schreurs AJM, Sinninghe Damste HEJ, de Graaff CS, Greefhorst APM. A dose-response study with formoterol Turbuhaler as maintenance therapy in asthmatic patients. European Respiratory Journal. 1996;9:1678–83. doi: 10.1183/09031936.96.09081678. [DOI] [PubMed] [Google Scholar]
- Seares 2003 {published data only} .Seares MR, McIvor A, Becker A, Fitzgearld JM, Boulet LP, Ernsy P, et al. Budesonide/formoterol adjustable maintenance dosing effectively improves asthma symptom severity: a multicentre Canadian study. European Respiratory Society. 2003 [Google Scholar]
- Serrier 2003 {published data only} .Serrier P, Roche N, Pello JY, Larguier JS, Mezzi K. Asthma control achieved with inhaled corticosteroids and long-acting beta2-agonists in a free or fixed combination: Results of the ALISE survey. Fre. Presse Medicale. 2003;32(11):493–7. [PubMed] [Google Scholar]
- Shapiro 2000 {published data only} .Cook CK, Prillaman BA, House KW, Rickard KA, Shah TP. Concurrent use of salmeterol/fluticasone propionate Diskus powder combination product and fluticasone propionate aqueous nasal spray does not adversely affect HPA-axis function. Annals of Allergy, Asthma and Immunology. 2001;86(1):98. [Google Scholar]; Edin HM, Payne E, Herrle MR, Schoaf L, Mather DB, Scott CA, et al. Salmeterol/fluticasone propionate combination via HFA MDI improves quality of life in asthma patients. Journal of Allergy and Clinical Immunology. 2001;Vol. 107(issue 2):s246. [Google Scholar]; Edin HM, Prillaman B, Baitinger LA, House K, Shah TP. Improved ability to perform strenuous activities after treatment with fluticasone propionate-salmeterol combination. American Journal of Respiratory and Critical Care Medicine. 2002;Vol. 165(issue Suppl 8):A112. [Google Scholar]; McCarthy TP, Edin HM, House K, Vandermeer AK. Quality of life and asthma control assessment in patients previously on inhaled corticosteroids (ICS) treated with salmeterol/fluticasone combination (SFC) metered dose inhaler (MDI) Thorax. 2001;Vol. 56(issue Suppl 3):iii63. [Google Scholar]; McCarthy TP, Edin HM, House K, Yan SK, Vandermeer AK. The effects of salmeterol/fluticasone combination (SFC) dry powder inhaler (DPI) on asthma control and quality of life in patients previously treated with inhaled corticosteroids (ICS) Thorax. 2001;Vol. 56(issue Suppl 3):iii 63. [Google Scholar]; Nathan R, Woodring A, Baitinger L, Prillaman B, Faris M, House K, et al. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. The salmeterol/fluticasone propionate Diskus combination decreases the incidence of exacerbations compared to treatment with salmeterol or fluticasone propionate alone; p. 848. 1999. [Google Scholar]; Nathan RA, Dorinsky P, Carranza Rosenzweig JRC, Shah T, Edin H, Prillaman B. Improved ability to perform strenuous activities after treatment with fluticasone propionate/ salmeterol combination in patients with persistent asthma. Journal of Asthma. 2003;40(7):815–22. doi: 10.1081/jas-120023573. [DOI] [PubMed] [Google Scholar]; *; Shapiro G, Lumry W, Wolfe J, Given J, White MV, Woodring L, et al. Combined salmeterol 50mcg and fluticasone propionate 350mcg in the Diskus device for the treatment of asthma. American Journal of Respiratory and Critical Care Medicine. 2000;161(2 Pt 1):527–34. doi: 10.1164/ajrccm.161.2.9905091. [DOI] [PubMed] [Google Scholar]
- Shapiro 2001 {published data only} .Shapiro GG, Mendelson LM, Pearlman DS. Once-daily budesonide inhalation powder (Pulmicort Turbuhaler) maintains pulmonary function and symptoms of asthmatic children previously receiving inhaled corticosteroids. Annals of Allergy, Asthma, and Immunology. 2001;86(6):633–40. doi: 10.1016/S1081-1206(10)62291-0. [DOI] [PubMed] [Google Scholar]
- Sheth 2002 {published data only} .Sheth K, Borker R, Emmett A, Rickard K, Dorinsky P. Cost-effectiveness comparison of salmeterol/fluticasone propionate versus montelukast in the treatment of adults with persistent asthma. Pharmacoeconomics. 2002;20(13):909–18. doi: 10.2165/00019053-200220130-00004. [DOI] [PubMed] [Google Scholar]
- Sienra-Monge 2001 {published data only} .Sienra-Monge JJL, Del Rio BE, Alvarez ME, Magana AJ. Comparison of quality of life and pulmonary function on moderate asthmatic children treated with beclomethasone and beclomethasone plus salmeterol. Journal of Allergy and Clinical Immunology. 2001;Vol. 107(issue 2):s263. [Google Scholar]
- Simons 1997 a {published data only} .Simons FE, Gerstner TV, Cheang MS. Tolerance to the broncho-protective effect of salmeterol in adolescents with exercise-induced asthma using concurrent inhaled glucocorticoid treatment. Pediatrics. 1997;99(5):655–9. doi: 10.1542/peds.99.5.655. [DOI] [PubMed] [Google Scholar]
- Simons 1997 b {published data only} .Simons FER. A comparison of beclomethasone, salmeterol and placebo in children with asthma. New England Journal of Medicine. 1997;337:1659–65. doi: 10.1056/NEJM199712043372304. [DOI] [PubMed] [Google Scholar]
- Sorkness 2007 {published data only} .Sorkness CA, Lemanske RF, Jr, Mauger DT, Boehmer SJ, Chinchilli VM, Martinez FD, et al. Long-term comparison of 3 controller regimens for mild-moderate persistent childhood asthma: The Pediatric Asthma Controller Trial. Journal of Allergy & Clinical Immunology. 2007;119(1):64–72. doi: 10.1016/j.jaci.2006.09.042. [DOI] [PubMed] [Google Scholar]
- Sovani 2008 {published data only} .Sovani MP, Whale CI, Oborne J, Cooper S, Mortimer K, Ekström T, et al. Poor adherence with inhaled corticosteroidsfor asthma: can using a single inhaler containing budesonide and formoterol help? The British Journal of General Practice. 2008;Vol. 58(issue 546):37–43. doi: 10.3399/bjgp08X263802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Staehr 1995 {published data only} .Staehr P, Vestbo I. Salmeterol improves control in asthmatic patients treated in general practice. A comparative study of salmeterol (Serevent) and salbutamol. Ugeskr-Laeger. 1995;157(1):36–40. [PubMed] [Google Scholar]
- Stanford 2002 {published data only} .Stanford RH, Borker R, Dorinsky P, Pepsin P, Kalberg C, Emmett A, et al. The costs and efficacy of fluticasone propionate/salmeterol combination versus montelukast in the treatment of adults with persistent asthma. Chest (conference); San Diego, CA. 2002. p. 422. [Google Scholar]
- Stelmach 2002a {published data only} .Stelmach I, Grzelewski T, Majak P, Majak J, Bobrowska M, Jerzynska J, et al. The effect of triamcinolone, montelukast and formoterol on serum levels of il-4, IgE and clinical parameters in children with asthma. Polski Merkuriusz Lekarski. 2001;11(63):247–51. [PubMed] [Google Scholar]; Stelmach I, Jerzynska J, Majak P, Grzelewski T, Gorski P, Stelmach W, et al. Effect of triamcinolone acetonide, montelukast, nedocromil sodium, formoterol on serum levels of sICAM-1, sIL-2R and clinical parameters of asthma in children. Polski Merkuriusz Lekarsk. 2002;12(68):99–103. [PubMed] [Google Scholar]
- Stelmach 2002b {published data only} .Stelmach I, Jerzynska J, Kuna P. A randomized, double-blind trial of the effect of glucocorticoid, anti-leukotriene and [beta]-agonist treatment on IL-10 serum levels in children with asthma. Clinical & Experimental Allergy. 2002;32(2):264–9. doi: 10.1046/j.1365-2222.2002.01286.x. [DOI] [PubMed] [Google Scholar]
- Stempel 2002 {published data only} .Stempel DA, O’Donnell JC, Meyer JW. Inhaled corticosteroids plus salmeterol or montelukast: effects on resource utilization and costs. Journal of Allergy & Clinical Immunology. 2002;109(3):433–9. doi: 10.1067/mai.2002.121953. [DOI] [PubMed] [Google Scholar]
- Stoloff 2002 {published data only} .Stoloff S, Poinsett-Holmes K, Dorinsky PM. Combination therapy with inhaled long-acting beta(2)-agonists and inhaled corticosteroids: a paradigm shift in asthma management. Pharmacotherapy. 2002;22(2):212–26. doi: 10.1592/phco.22.3.212.33550. [DOI] [PubMed] [Google Scholar]
- Strand 2003 {published data only} .Strand AM. Initiation of treatment with the salmeterol/ fluticasone propionate (FP) combination product is better than inhaled steroid alone (FP) in asthmatic patients symptomatic on short-acting bronchodilator alone. European Respiratory Journal. 2003;(Suppl 45):410s, P2638. Vol. [Google Scholar]
- Tal 2003 {published data only} .Tal A, Simon G, Vermeulen JH. Symbicort® (budesonide and formoterol in a single inhaler) is effective and well tolerated in children with asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard MI, et al. Budesonide/formoterol in a single inhaler versus inhaled corticosteroids alone in the treatment of asthma. Pediatric Pulmonology. 2002;34:342–50. doi: 10.1002/ppul.10173. [DOI] [PubMed] [Google Scholar]; Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. Rapid and sustained improvements in lung function and symptom control with budesonide/ formoterol in adolescent asthma. European Respiratory Journal. 2001;Vol. 18(issue 33):494s. [Google Scholar]; Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. International Paediatric Respiratory and Allergy Congress. Prague: Apr 1-4, 2001. Symbicort (budesonide and formoterol in a single inhaler) improves lung function in children with asthma. [Google Scholar]; Tal A, Simon G, Vermeulen JH, Petru V, Cobos N, Everard ML, et al. International Paediatric Respiratory and Allergy Congress. Prague: Apr 1-4, 2001. Symbicort (budesonide and formoterol in a single inhaler) is more effective that budesonide alone in children with asthma; pp. 84–5. [Google Scholar]; *; Vermeulen JH, Simon G, Tal A. Symbicort® (budesonide and formoterol in a single inhaler) improves lung function in asthmatic children aged 4-17 years. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]
- Tan 1997 {published data only} .Tan S, Hall IP, Dewar J, Dow E, Lipworth B. Association between beta 2-adrenoceptor polymorphism and susceptibility to bronchodilator desensitisation in moderately severe stable asthmatics. Lancet. 1997;350(9083):995–9. doi: 10.1016/S0140-6736(97)03211-X. [DOI] [PubMed] [Google Scholar]
- Tattersfield 2001 {published data only} .Tattersfield AE, Lofdahl CG, Postma DS, Eivindson A, Schreurs AG, Rasidakis A, et al. Comparisons of formoterol and terbutaline for as-needed treatment of asthma: a randomised trial. Lancet. 2001;357(9252):257–61. doi: 10.1016/S0140-6736(00)03611-4. [DOI] [PubMed] [Google Scholar]; *; Tattersfield AE, Postma DS, Barnes PJ, Svensson K, Bauer CA, O’Byrne PM, et al. Exacerbations of asthma: a descriptive study of 425 severe exacerbations. The FACET International Study Group. American Journal of Respiratory & Critical Care Medicine. 1999;160(2):594–9. doi: 10.1164/ajrccm.160.2.9811100. [DOI] [PubMed] [Google Scholar]
- Thomson 2003 {published data only} .Thomson NC, Shepherd M. Leukotriene receptor antagonists as add-on therapy for adults with asthma. Thorax. 2003;58(3):190–2. doi: 10.1136/thorax.58.3.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonelli 2001 {published data only} .Tonelli M, Giannini D, Di Franco A, Carnevali S, Bartoli ML, Cianchetti S, et al. Symptoms, induced sputum eosinophil percentages and treatment with salmeterol or fluticasone in mild asthmatics. European Respiratory Journal. 2001;(Suppl 33):336s. Vol. [Google Scholar]
- Trautmann 2001 {published data only} .Trautmann M. Treatment with salmeterol/fluticasone propionate (50/250g) inhaler improves lung function, asthma symptoms and quality of life in a large group of patients with mild to moderate asthma. American Journal of Respiratory and Critical Care Medicine. 2001;Vol. 163(issue 5):A864. [Google Scholar]
- Turner 1998 {published data only} .Turner MO, Johnston PR, Pizzichini E, Pizzichini MM, Hussack PA, Hargreave FE. Anti-inflammatory effects of salmeterol compared with beclomethasone in eosinophilic mild exacerbations of asthma: a randomized, placebo controlled trial. Canadian Respiratory Journal. 1998;5(4):261–8. doi: 10.1155/1998/868379. [DOI] [PubMed] [Google Scholar]
- Ullman 1990 {published data only} .Ullman A, Hedner J, Svedmyr N. Inhaled salmeterol and salbutamol in asthmatic patients. An evaluation of asthma symptoms and the possible development of tachyphylaxis. American Review of Respiratory Disease. 1990;142(3):571–5. doi: 10.1164/ajrccm/142.3.571. [DOI] [PubMed] [Google Scholar]
- Vagaggini 1999 {published data only} .Vagaggini B, Carnevali S, Macchioni P, Taccola M, Fornai E, Bacci E, et al. Airway inflammatory response to ozone in subjects with different asthma severity. European Respiratory Journal. 1999;13(2):274–80. doi: 10.1034/j.1399-3003.1999.13b09.x. [DOI] [PubMed] [Google Scholar]
- Van Asperen 2002 {published data only} .van Asperen P, Mellis CM, Sly PD. The role of corticosteroids in the management of childhood asthma. Medical Journal of Australia. 2002;176(4):168–73. doi: 10.5694/j.1326-5377.2002.tb04347.x. [DOI] [PubMed] [Google Scholar]
- Van den Berg 2000 {published data only} .Van den Berg NJ, Ossip MS, Hederos CA, Anttila H, Ribeiro BL, Davies PI. Salmeterol/fluticasone propionate (50/100 ug) in combination in Diskus inhaler (Seretide) is effective and safe in children with asthma. Pediatric Pulmonology. 2000;30:97–105. doi: 10.1002/1099-0496(200008)30:2<97::aid-ppul4>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Van der Molen 1997a {published data only} .van de Molen T, Postma DS, Kraan J, Chapman K, Grossman R, Turner MO, et al. No influence of six months treatment with formoterol on airway hyper-responsiveness in asthma subjects using inhaled corticosteroids. American Journal of Respiratory and Critical Care Medicine American Thoracic Society 1998 International Conference Chicago Illinois.1998. [Google Scholar]; van der Molen T, Postma DS, Schreurs AJ, Bosveld HE, Sears MR, Meyboom de Jong B. Discriminative aspects of two generic and two asthma-specific instruments: relation with symptoms, bronchodilator use and lung function in patients with mild asthma. Quality of Life Research. 1997;6(4):353–61. doi: 10.1023/a:1018483310277. [DOI] [PubMed] [Google Scholar]; van der Molen T, Postma DS, Turner MO, Meyboomde Jong B, Malo JL, Chapman K, et al. Effects of the long acting beta agonist formoterol on asthma control in asthmatic patients using inhaled corticosteroids. Thorax. 1997;52:535–9. doi: 10.1136/thx.52.6.535. [DOI] [PMC free article] [PubMed] [Google Scholar]; *; van der Molen T, Sears MR, de Graaff CS, Postma DS, Meyboom-de Jong B. Quality of life during formoterol treatment: comparison between asthma-specific and generic questionnaires. European Respiratory Journal. 1998;12(1):30–4. doi: 10.1183/09031936.98.12010030. [DOI] [PubMed] [Google Scholar]
- Van der Woude 2001 {published data only} .van der Woude HJ, Winter TH, Boorsma M, Bergqvist PBF, Aalbers A. Symbicort® (budesonide and formoterol in a singe inhaler) provides rapid relief on methacholine-induced bronchoconstriction. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23; 2001. 2001. [Google Scholar]; van der Woude HJ, Winter TH, Boorsma M, Bergqvist PBF, Aalbers R. More rapid relief of methacholine-induced bronchoconstriction with budesonide/formoterol than with salmeterol/fluticasone. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):53s. [Google Scholar]
- Van Noord 2001 {published data only} .van Noord JA, Lill H, Carrillo Diaz T, Greefhorst AP, Davies P. Clinical equivalence of a salmeterol/ fluticasone propionate combination product delivered via a chlorofluorocarbon-free metered-dose inhaler with the Diskus in patients with moderate to severe asthma. Clinical Drug Investigation. 2001;21(4):243–55. [Google Scholar]; *; van Noord JA, Lill H, Carrillo T, Davies P. Clinical equivalence of salmeterol/fluticasone propionate combination 50/500 bid delivered via metered dose inhaler (MDI) or Diskus™ in patients with reversible airways obstruction. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue Suppl 3):A197. [Google Scholar]
- Verberne 1997 {published data only} .Verberne AAPH, Frost C, Roorda RJ, van der Laag H, Kerrebijn KF. One year treatment with salmeterol compared with beclomethasone in children with asthma. American Journal of Respiratory and Critical Care Medicine. 1997;156:688–95. doi: 10.1164/ajrccm.156.3.9611067. [DOI] [PubMed] [Google Scholar]
- Vestbo 2000 {published data only} .Vestbo J, Sorensen T, Lange P, Brix A, Torre P, Viskum K. Long-term effect of inhaled budesonide in patients with mild to moderate chronic obstructive lung disease. Ugeskrift for Laeger. 2000;162(4):493–7. [PubMed] [Google Scholar]
- Vickers 2000 {unpublished data only} .Vickers M. Assessment of long-term efficacy of early introduction of inhaled steroids in asthma. National Health Technology Assessment (NCCHTA) [Google Scholar]
- Vilsvik 2001 {published data only} .Vilsvik J, Ankerst J, Palmqvist M, Persson G, Schaanning J, Schwabe G, et al. Protection against cold air and exercise-induced bronchoconstriction while on regular treatment with Oxis. Respiratory Medicine. 2001;95(6):484–90. doi: 10.1053/rmed.2001.1074. [DOI] [PubMed] [Google Scholar]
- Von Berg 1989 {published data only} .von-Berg A, Berdel D. Formoterol and salbutamol metered aerosols: comparison of a new and an established beta-2-agonist for their bronchodilating efficacy in the treatment of childhood bronchial asthma. Pediatric Pulmonology. 1989;7(2):89–93. doi: 10.1002/ppul.1950070207. [DOI] [PubMed] [Google Scholar]
- Wallaert 1999 {published data only} .Wallaert B, Brun P, Ostinelli J, Murciano D, Champel F, Blaive B, et al. A comparison of two long-acting beta-agonists, oral bambuterol and inhaled salmeterol, in the treatment of moderate to severe asthmatic patients with nocturnal symptoms. The French Bambuterol Study Group. Respiratory Medicine. 1999;93(1):33–8. doi: 10.1016/s0954-6111(99)90074-4. [DOI] [PubMed] [Google Scholar]
- Wallin 1990 {published data only} .Wallin A, Melander B, Rosenhall L, Sandstrom T, Wahlander L. Formoterol, a new long acting beta 2 agonistfor inhalation twice daily, compared with salbutamol in the treatment of asthma. Thorax. 1990;45(4):259–61. doi: 10.1136/thx.45.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallin 2002 {published data only} .Wallin A, Sandstrom T, Cioppa GD, Holgate S, Wilson S. The effects of regular inhaled formoterol and budesonide on preformed Th-2 cytokines in mild asthmatics. Respiratory Medicine. 2002;96(12):1021–5. doi: 10.1053/rmed.2002.1388. [DOI] [PubMed] [Google Scholar]; Wallin A, Sandstrom T, Soderberg M, Howarth P, Djukanovic R, Wilson S, et al. Effects of formoterol, budesonide and placebo treatment on asthmatic airway inflammation. Annals of Allergy, Asthma, and Immunology. 1998:8088. [Google Scholar]; Wallin A, Sandstrom T, Soderberg M, Howarth P, Lundback B, Della-Cioppa G, et al. The effects of regular inhaled formoterol, budesonide, and placebo on mucosal inflammation and clinical indices in mild asthma. American Journal of Respiratory & Critical Care Medicine. 1999;159(1):79–86. doi: 10.1164/ajrccm.159.1.9801007. [DOI] [PubMed] [Google Scholar]
- Warner 2001 {published data only} .Warner JO. The role of leukotriene receptor antagonists in the treatment of chronic asthma in childhood. Allergy. 2001;56:22–9. doi: 10.1034/j.1398-9995.2001.00005.x. [DOI] [PubMed] [Google Scholar]
- Weersink 1997 {published data only} .Weersink EJ, van Zomeren EH, Koeter GH, Postma DS. Treatment of nocturnal airway obstruction improves daytime cognitive performance in asthmatics. American Journal of Respiratory & Critical Care Medicine. 1997;156(4 part 1):1144–50. doi: 10.1164/ajrccm.156.4.9701001. [DOI] [PubMed] [Google Scholar]; Weersink EJM, Doouma RR, Postma DS, Koeter GH. Fluticasone propionate, salmeterol xinafoate and their combination in the treatment of nocturnal asthma. American Journal of Respiratory and Critical Care Medicine. 1997;155:1241–6. doi: 10.1164/ajrccm.155.4.9105061. [DOI] [PubMed] [Google Scholar]
- Weinstein 1998 {published data only} .Weinstein SF, Pearlman DS, Bronsky EA, Byrne A, Arledge T, Liddle R, et al. Efficacy of salmeterol xinafoate powder in children with chronic persistent asthma. Annals of Allergy, Asthma, and Immunology. 1998;81:51–8. doi: 10.1016/S1081-1206(10)63109-2. [DOI] [PubMed] [Google Scholar]
- Weinstein 2001 {published data only} .Weinstein SF, Pearlman DS, Condemi JJ, Herrle MR, Scott CA, Payne JE, et al. Superior efficacy of the fluticasone propionate/salmeterol (88/42mcg) HFA-MDI combination product versus the individual components in asthmatics previously treated with either short- or long-acting beta2-agonists or inhaled corticosteroids. Journal of Allergy and Clinical Immunology. 2001;107(2):S102. [Google Scholar]
- Wempe 1992 {published data only} .Wempe JB, Tammeling EP, Koeter GH, Hakansson L, Venge P, Postma DS. Blood eosinophil numbers and activity during 24 hours: effects of treatment with budesonide and bambuterol. Journal of Allergy and Clinical Immunology. 1992;90(5):757–65. doi: 10.1016/0091-6749(92)90099-n. [DOI] [PubMed] [Google Scholar]
- Wilcke 1998 {published data only} .Wilcke JT, Iversen ET, Kok-Jensen A. Effect of salmeterol is independent of previously inhaled salbutamol: a clinical controlled study. Lung. 1998;176(2):133–9. doi: 10.1007/pl00007595. [DOI] [PubMed] [Google Scholar]
- Wilding 1997 {published data only} .Wilding P, Clark M, Thompson Coon J, Lewis S, Rushton L, Bennett J, et al. Effect of long term treatment with salmeterol on asthma control: a double-blind, randomised crossover study. BMJ. 1997;314:1441–6. doi: 10.1136/bmj.314.7092.1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson 2001a {published data only} .Dempsey OJ, Wilson AM, Sims EJ, Lipworth BJ. Additive anti-inflammatory effects of montelukast but not salmeterol in asthmatics suboptimally controlled on inhaled steroids. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue Suppl 3):A198. [Google Scholar]; Wilson AM, Dempsey OJ, Sims EJ, Lipworth BJ. A comparison of salmeterol and montelukast as second-line therapy in asthmatic patients not controlled on inhaled corticosteroids. Thorax. 1999;Vol. 54(issue Suppl 3 A66):189. [Google Scholar]; Wilson AM, Dempsey OJ, Sims EJ, Lipworth BJ. Evaluation of salmeterol or montelukast as second-line therapy for asthma not controlled with inhaled corticosteroids. Chest. 2001;119(4):1021–6. doi: 10.1378/chest.119.4.1021. [DOI] [PubMed] [Google Scholar]
- Wilson 2001b {published data only} .Wilson SJ, Wallin A, Della-Cioppa G, Sandstrom T, Holgate ST. Effects of budesonide and formoterol on NF-kappaB, adhesion molecules, and cytokines in asthma. American Journal of Respiratory & Critical Care Medicine. 2001;164(6):1047–52. doi: 10.1164/ajrccm.164.6.2010045. [DOI] [PubMed] [Google Scholar]; Wilson SJ, Ward JA, Djukanovic R, Wallin A, Sue-Chu M, Sandstrom T, et al. Effects of high and low dose inhaled fluticasone propionate (FP) compared to low dose FP combined with salmeterol (SAL) on airway inflammation in asthma. American Journal of Respiratory and Critical Care Medicine. 2000;Vol. 161(issue Suppl 3):A196. [Google Scholar]
- Wong 1992 {published data only} .Wong BJ, Dolovich J, Ramsdale EH, O’Byrne P, Gontovnick L, Denburg JA, et al. Formoterol compared with beclomethasone and placebo on allergen-induced asthmatic responses. American Review of Respiratory Disease. 1992;146(5 part 1):1156–60. doi: 10.1164/ajrccm/146.5_Pt_1.1156. [DOI] [PubMed] [Google Scholar]
- Woolcock 1995 {published data only} .Woolcock A. Continuing patient care with metered-dose inhalers. Journal of Aerosol Medicine: Deposition, Clearance, and Effects in the Lung. 1995;8(Suppl 2):s5–s10. doi: 10.1089/jam.1995.8.suppl_2.s-5. [DOI] [PubMed] [Google Scholar]
- Wooltorton 2003 {published data only} .Wooltorton E. Salmeterol (Serevent) asthma trial halted early. Canadian Medical Association Journal. 2003;168(6):738. [PMC free article] [PubMed] [Google Scholar]
- Yancey 1997 {published data only} .Yancey SW, Rickard KA, Emmett A, Cox F. The response to salmeterol or theophylline in asthmatics either receiving or not-receiving inhaled corticosteroids. Annals of Allergy, Asthma and Immunology. 1997;78:110. [Google Scholar]
- Yates 1995 {published data only} .Yates DH, Sussman HS, Shaw MJ, Barnes PJ, Chung KF. Regular formoterol treatment in mild asthma: effect on bronchial responsiveness during and after treatment. American Journal of Respiratory and Critical Care Medicine. 1995;152(41):1170–4. doi: 10.1164/ajrccm.152.4.7551366. [DOI] [PubMed] [Google Scholar]
- Yates 1996 {published data only} .Yates DH, Kharitonov SA, Barnes PJ. An inhaled glucocorticoid does not prevent tolerance to the bronchoprotective effect of a long-acting inhaled beta 2-agonist. American Journal of Respiratory & Critical Care Medicine. 1996;154(6 part 1):1603–7. doi: 10.1164/ajrccm.154.6.8970342. [DOI] [PubMed] [Google Scholar]
- Youngchaiyud 1995 {published data only} .Youngchaiyud P, Permpikul C, Suthamsmai T, Wong E. A double-blind comparison of inhaled budesonide, long-acting theophylline, and their combination in treatment of nocturnal asthma. Allergy. 1995;50:28–33. doi: 10.1111/j.1398-9995.1995.tb02480.x. [DOI] [PubMed] [Google Scholar]
- Yurdakul 2002 {published data only} .Yurdakul AS, Calisir HC, Tunctan B, Ogretensoy M. Comparison of second controller medications in addition to inhaled corticosteroid in patients with moderate asthma. Respiratory Medicine. 2002;96(5):322–9. doi: 10.1053/rmed.2002.1282. [DOI] [PubMed] [Google Scholar]
- Zarkovic 1998 {published data only} .Zarkovic J, Gotz MH, Holgate ST, Taak NK. Effect of long-term regular salmeterol treatment in children with moderate asthma. Clinical Drug Investigation. 1998;15(3):169–75. [Google Scholar]
- Zetterstrom 2001 {published data only} .Zetterstrom O, Buhl R, Mellem H. Efficacy and safety of Symbicort® (budesonide and formoterol in a single inhaler) in adults with asthma. Annual Thoracic Society 97th International Conference; San Francisco CA. May 18-23.2001. [Google Scholar]; Zetterstrom O, Buhl R, Mellem H, Perpina M, Hedman J, O’Neill S, et al. The new single inhaler product containing both budesonide/formoterol improves asthma control in adults. European Respiratory Journal. 2000;Vol. 16(issue Suppl 31):455s. doi: 10.1183/09031936.01.00065801. [DOI] [PubMed] [Google Scholar]; Zetterström O, Buhl R, Mellem H, Perpiñá M, Hedman J, O’Neill S, et al. Efficacy and safety of a new single inhaler product containing both budesonide and formoterol in adult asthma. European Respiratory Journal. 2000;Vol. 16(issue 31):455s. [Google Scholar]; Zetterstrom O, Buhl R, Perpina M, Hedman J, O’Neill S, Ekstrom T. Improved asthma control with budesonide/ formoterol in a single inhaler, compared with budesonide alone. European Respiratory Journal. 2001;18:262–8. doi: 10.1183/09031936.01.00065801. [DOI] [PubMed] [Google Scholar]
- Zhong 2002 {published and unpublished data} .SAM30008 A multi-centre, randomized, open-label, parallel-group, comparison study of the salmeterol/ fluticasone propionate combination product via one Diskus/Accuhaler inhaler with salmeterol via one Diskus/ Accuhaler inhaler and fluticasone propionate via another Diskus/Accuhaler inhaler in adults with asthma. 2005 http://ctr.gsk.co.uk.; *; Zhong N. Comparison of the effectiveness and safety in use of salmeterol/fluticasone delivered together in a Seretide Acuhaler or salmeterol and fluticasone delivered separately for patients with moderate or severe asthma. Chinese Journal of Tuberculosis and Respiratory Disease. 2002;25(6):371. [Google Scholar]
- Zimmerman 2004 {published data only} .Zimmerman B, D’Urzo A, Berube D. Efficacy and safety of formoterol turbuhaler(R) when added to inhaled corticosteroid treatment in children with asthma. Pediatric Pulmonology. 2004;37(2):122–7. doi: 10.1002/ppul.10404. [DOI] [PubMed] [Google Scholar]; Zimmerman B, D’Urzo A, Berube D. Efficacy and tolerability of formoterol turbuhaler(r) compared with placebo, in children (6-11 yr) with asthma poorly controlled with inhaled corticosteroids. American Journal of Respiratory and Critical Care Medicine. 2002;165(8 suppl):A746. [Google Scholar]; *; Zimmerman B, D’Urzo A, Berube D. Efficacy and tolerability of formoterol Turbuhaler in 6-11 year old children with asthma, not adequately controlled with inhaled corticosteroids. European Respiratory Society Annual Congress. 2002;2002:P2734. [Google Scholar]
References to studies awaiting assessment
- Boskovska 2001 {published data only} .Boskovska MI, Dokic D, Busletic-Bozinovska K, Arbutina S, Goseva Z. Concomitant use of low-dose inhaled corticosteroids and a long-acting bronchodilator vis a vis doubling the dose of inhaled corticosteroid in asthma patients. European Respiratory Journal. 2001;(issue Suppl 33):98s. [Google Scholar]
- Currie 2002 {published data only} .Currie GP, Stenback S, Lipworth BJ. Dissociation in effects of fluticasone but not fluticasone/salmeterol on lung function and airway hyperresponsiveness in mild persistent asthma. European Respiratory Society Annual Congress. 2002:385s. [Google Scholar]
- Djordjevic 1999 {published data only} .Djordjevic D, Zickovic D, Stankovic I, Pejcic T, Ducic J, Rancic M, et al. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Comparative study of three months treatment in combination of salmeterol and beclomethasone dipropionate (bdp) with doubling the dose of bdp in mild asthma; p. 849. 1999. [Google Scholar]
- Ozkaya 1999 {published data only} .Ozkaya O, Turktas I, Cengizlier R. European Respiratory Society. Madrid, Spain: Oct 9-13, 1999. Low dose budesonide plus formoterol versus high dose budesonide in children with bronchial asthma; p. P365. 1999. [Google Scholar]
- Stankovic 2000 {published data only} .Stankovic IJ, Djordjevic DV, Pejcic TA, Zivkovic DS, Rancic MR, Ristic LM, et al. Formoterol and beclomethasone dipropionate versus higher dose beclomethasone dipropionate in asthma patients. European Respiratory Journal. 2000;16(Suppl 31):455s. [Google Scholar]
- Stojkovic-Andjelkovi 2001 {published data only} .Stojkovic-Andjelkovic AK, Pajovic DM, Protrka OJ, Ugrinovic BS, Obradovic SM, Pavicevic MD. Effect of combination fluticasone propionate and salmeterol diskhaler in treatment of moderate to severe asthma: comparison of initial high dose, constant medium dose and placebo. European Respiratory Journal. 2001;Vol. 18(issue Suppl 33):123s. [Google Scholar]
- VIAPAED 102318 {unpublished data only} .GlaxoSmithKline (VIAPAED 102318) [accessed 29 October 2008];Steroid-sparing with the salmeterol/fluticasone propionate 50/100 mcg b.i.d. combination compared to fluticasone propionate 200mcg b.i.d. alone in the management of children and adolescents with moderate persistent asthma. 2008 http://www.gsk-clinicalstudyregister.com.
- Zharov 2004 {published data only} .Zaharov T, Kamenov SS, Kamenov BA. Improvements in FEV and PEF were greater with salmeterol/fluticasone (S/F) than with beclomethasone dipropionate (BDP) European Respiratory Journal. 2004;24(Suppl 48):380s. [Google Scholar]; Zhaharov TV, Kamenov SS, Kamenov BA. Improvements in FEV and PEF were greater with salmeterol/fluticasone (S/F) than with beclomethasone dipropionate (BDP) European Respiratory Journal. 2004;24(Suppl 48):379s. [Google Scholar]
References to ongoing studies
- Aziz {published data only} .Aziz I. Comparison of anti inflammatory effect of once daily inhaled formoterol and once daily inhaled budesonide on inflammatory markers in asthmatic patients. Clinical Pharmacology, Ninewells Hospital and Medical School, University of Dundee, DUNDEE, DD1 9SY; Scotland UK: [Google Scholar]
- Barnes a {published data only} .Barnes NC. Respiratory Medicine, London Chest Hospital. Bonner Road, London, E2 9JX, United Kingdom: A randomized parallel 3 arm study to assess asthma control, lung function, costs and quality of life in patients with asthma treated with formoterol twice daily and either budesonide once or twice daily from a novel multidisc dry powder inhaler. [Google Scholar]
- Barnes b {published data only} .Barnes PJ. Effect of low dose formoterol and budesonide on exhaled breath in asthma. Royal Brompton and Harefield NHS Trust; [Google Scholar]
- Bush {published data only} .Bush A. Department of Paediatrics, Imperial College School of Medicine. Royal Brompton and Harefield NHS Trust; Brompton Campus, Dovehouse Street, London, SW3 6LY, United Kingdom: Efficacy and safety of budesonide/formoterol Turbuhaler , compared to budesonide turbuhaler metered dose, in steroid using asthmatic adolescent patients, double blind, double dummy parallel group, Phase III, multicentre study. [Google Scholar]
- Currie {published data only} .Currie GP. Are there additional anti-inflammatory effects of leukotriene receptor antagonists in persistent asthmatics receiving inhaled steroid alone and combined inhaled steroid/long acting B2-agonists? Academic Publications; [Google Scholar]
- Goves {published data only} .Goves JR. Department of Paediatrics, Level 4 John Radcliffe Hospital. Headington, Oxford, OX3 9DU; Headley Way: Eformoterol in the management of mild asthma -eformoterol Turbohaler R with budesonide Turbohaler R. [Google Scholar]
- Hill {published data only} .Hill J. The ASSURE Study - the effectiveness and safety of an individualised Symbicort Turbohaler maintenance dosing regimen (Symbicort Asthma Control Plan) versus Symbicort Turbohaler given as standard regular twice daily therapy.
- Kharitonov {published data only} .Kharitonov SA. Effect of inhaled corticosteroids (budesonide 100 micrograms/400 micrograms vs placebo) and formoterol on localisation of glucocorticoid receptor and exhaled markers in asthma. Royal Brompton and Harefield NHS Trust; [Google Scholar]
- Lipworth 2001 {unpublished data only} .Lipworth BJ. Relative lung bioavailability with fluticasone via dry powder inhaler versus: (a) fluticasone/salmeterol combination vis dry powder inhaler; (b) fluticasone/ salmeterol combination via HFA-pMDI plus spacer, in patients with moderate persistent asthma. Academic publications; 2001. Vol. June. [Google Scholar]
- Millar {published data only} .Millar AB. South West Regional Office, North Bristol NHS Trust. Lung Research Unit, Southmead Hospital; Southmead Road, Westbury-on-Trym, Bristol, BS10 5NB, UK: A randomised double-blind multi-centre study to evaluate the effect of adding alternative agents to inhaled steroids in adult asthmatics. (Telephone: 0117 9595348) [Google Scholar]
- Ruggins {published data only} .Ruggins N. Pragmatic trial of add-on therapy in paediatric asthma. Southern Derbyshire Acute Hospitals NHS Trust; [Google Scholar]
- Thomson {published data only} .Thomson NC. Respiratory Medicine, Gartnavel General Hospital. Great Western Road, Glasgow, G12 0YN, Scotland: Budesonide/formoterol fixed combination in adults with asthma. [Google Scholar]
- Young {published data only} .Young KM. St Mary’s Surgery. 37 St Mary’s Street, Ely, Cambs, CB7 4HF: [Google Scholar]
Additional references
- Adams 2008 .Adams NP, Bestall JC, Lasserson TJ, Jones P, Cates CJ. Fluticasone versus placebo for chronic asthma in adults and children. Cochrane Database of Systematic Reviews. 2008;(Issue 4) [DOI: 10.1002/14651858.CD003135.Pub4] [Google Scholar]
- Adkins 1997 .Adkins JC, McTavish D. Salmeterol: a review of its pharmacological properties and clinical efficacy in the management of children with asthma. Drugs. 1997;54(2):331–54. doi: 10.2165/00003495-199754020-00011. [DOI] [PubMed] [Google Scholar]
- Australia 2006 .Anonymous . Asthma Management Handbook. 6th Edition. National Asthma Campaign; Melbourne: 2006. http://www.nationalasthma.org.au/publications/amh/amhcont.htm. [Google Scholar]
- Bartow 1998 .Bartow RA, Brogden RN. Formoterol: an update of its pharmacological properties and therapeutic efficacy in the management of asthma. Drugs. 1998;55(2):302–22. doi: 10.2165/00003495-199855020-00016. [DOI] [PubMed] [Google Scholar]
- BTS 2008 (updated June 09) .British Thoracic Society/Scottish Intercollegiate Guidelines Network [accessed 9 August 2009]; [updated June 2009];British Guidelines on Asthma Management. 2008 http://www.brit-thoracic.org.uk.
- Cates 2002 .Cates CJ. Simpson’s paradox and calculation of number needed to treat from meta-analysis. Bio Med Central. BMC Medical Research Methodology. 2002;2:1. doi: 10.1186/1471-2288-2-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates 2009a .Cates CJ, Lasserson TJ, Jaeschke R. Regular treatment with salmeterol and inhaled steroids for chronic asthma: serious adverse events. Cochrane Database of Systematic Reviews. 2009;(Issue 3) doi: 10.1002/14651858.CD006922.pub2. [DOI: 10.1002/14651858.CD006922.pub2] [DOI] [PubMed] [Google Scholar]
- Cates 2009b .Cates CJ, Lasserson TJ, Jaeschke R. Regular treatment with formoterol and inhaled steroids for chronic asthma: serious adverse events. Cochrane Database of Systematic Reviews. 2009;(Issue 2) doi: 10.1002/14651858.CD006924.pub2. [DOI: 10.1002/14651858.CD006924] [DOI] [PubMed] [Google Scholar]
- Chalmers 2002 .Chalmers GW, Macleod KJ, Little SA, Thomson LJ, McSharry CP, Thomson NC. Influence of cigarette smoking on inhaled corticosteroids treatment in mild asthma. Thorax. 2002;57:226–30. doi: 10.1136/thorax.57.3.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaudhuri 2003 .Chaudhuri R, Livingston E, McMahon AD, Thomson L, Borland W, Thomson NC. Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthma. American Journal of Respiratory & Critical Care Medicine. 2003;168(11):1308–11. doi: 10.1164/rccm.200304-503OC. [DOI] [PubMed] [Google Scholar]
- D’Alonzo 1997 .D’Alonzo GE, Tolep KA. Salmeterol in the treatment of chronic asthma. American Family Physician. 1997;56(2):558–62. [PubMed] [Google Scholar]
- Deeks 2001 .Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD, Altman DG, editors. Systematic reviews in health care: meta-analysis in context. BMJ Publishing; London: 2001. pp. 285–312. [Google Scholar]
- DerSimonian 1986 .DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials. 1986;7:177–88. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- Ducharme 2006 .Ducharme FM, Lasserson TJ, Cates CJ. Long-acting beta2-agonists versus anti-leukotrienes as add-on therapy to inhaled corticosteroids for chronic asthma. Cochrane Database of Systematic Reviews. 2006;(Issue 4) doi: 10.1002/14651858.CD003137.pub3. [DOI: 10.1002/14651858.CD003137.pub3] [DOI] [PubMed] [Google Scholar]
- Egger 1997 .Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ernst 2006 .Ernst P, McIvor A, Ducharme FM, Boulet LP, Fitzgerald M, Chapman KR, et al. Safety and effectiveness of long-acting inhaled beta-agonist bronchodilators when taken with inhaled corticosteroids. Annals of Internal Medicine. 2006;146(9):692–4. doi: 10.7326/0003-4819-145-9-200611070-00012. [DOI] [PubMed] [Google Scholar]
- Fireman 1995 .Fireman P. Beta2-agonists and their safety in the treatment of asthma. Allergy Proceedings. 1995;16:235–9. doi: 10.2500/108854195778702693. [DOI] [PubMed] [Google Scholar]
- Georgitis 1999 .Georgitis JW. The 1997 asthma management guidelines and therapeutic issues relating to the treatment of asthma. Chest. 1999;115(1):210–17. doi: 10.1378/chest.115.1.210. [DOI] [PubMed] [Google Scholar]
- Gibson 2005 .Gibson PG, Powell H, Ducharme F. Long-acting beta2-agonists as an inhaled corticosteroid-sparing agent for chronic asthma in adults and children. Cochrane Database of Systematic Reviews. 2005;(Issue 4) doi: 10.1002/14651858.CD005076.pub2. [DOI: 10.1002/14651858.CD005076.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- GINA 2008 .Global Initiative for Asthma Global Strategy for Asthma Management and Prevention. 2008 NIH Publication 02-3659. http://www.ginasthma.com.
- Gleser 1996 .Gleser LJ, Olkin I. Models for estimating the number of unpublished studies. Statistics in Medicine. 1996;15:2493–507. doi: 10.1002/(SICI)1097-0258(19961215)15:23<2493::AID-SIM381>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- Greenland 1985 .Greenland S, Robins JM. Estimation of a common effect parameter from sparse follow-up data. Biometrics. 1985;41:55–68. [PubMed] [Google Scholar]
- Higgins 2003 .Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(557):560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jadad 1996 .Jadad AR, Moore A, Carroll D, Jenkinson C, Reynolds DJM, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Controlled Clinical Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- Lemiere 2004 .Lemiere C, Bai T, Bayliff C, Becker A, et al. Adult Asthma guidelines - update 2003. Canadian Respiratory Journal. 2004;11(Suppl A):9A–18A. doi: 10.1155/2004/271362. [DOI] [PubMed] [Google Scholar]
- Manning 2008 .Manning P, Gibson PG, Lasserson TJ. Ciclesonide versus placebo for chronic asthma in adults and children. Cochrane Database of Systematic Reviews. 2008;(Issue 2) doi: 10.1002/14651858.CD006217.pub2. [DOI: 10.1002/14651858.CD006217.Pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore 1998 .Moore RH, Khan A, Dickey BF. Long-acting inhaled beta2-agonists in asthma therapy. Chest. 1998;113:1095–108. doi: 10.1378/chest.113.4.1095. [DOI] [PubMed] [Google Scholar]
- Nelson 1995 .Nelson HS. Beta-adrenergic bronchodilators. New England Journal of Medicine. 1995;333(8):499–506. doi: 10.1056/NEJM199508243330807. [DOI] [PubMed] [Google Scholar]
- Ni Chroinin 2005 .Ni Chroinin M, Greenstone IR, Danish A, Magdolinos H, Masse V, Zhang X, et al. Long-acting beta2-agonists versus placebo in addition to inhaled corticosteroids in children and adults with chronic asthma. Cochrane Database of Systematic Reviews. 2005;(Issue 4) doi: 10.1002/14651858.CD005535. [DOI: 10.1002/14651858.CD005535] [DOI] [PubMed] [Google Scholar]
- Ni Chroinin 2009a .Ni Chroinin M, Greenstone I, Lasserson TJ, Ducharme FM. Addition of inhaled long-acting beta2-agonists to inhaled steroids as first line therapy for persistent asthma in steroid-naive adults. Cochrane Database of Systematic Reviews. 2009;(Issue 4) doi: 10.1002/14651858.CD005307.pub2. [DOI: 10.1002/14651858.CD005307.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ni Chroinin 2009b .Ni Chroinin M, Lasserson TJ, Greenstone I, Ducharme FM. Addition of long-acting beta-agonists to inhaled corticosteroids for chronic asthma in children. Cochrane Database of Systematic Reviews. 2009;(Issue 3) doi: 10.1002/14651858.CD007949. [DOI: 10.1002/14651858.CD007949] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NIH Publication 2007 .National Asthma Education and Prevention Program . NIH Publication. National Heart, Lung and Blood Institute; Bethesda, MD: 2007. Expert Panel Report 3 (EPR 3) Guidelines for the Diagnosis and Management of Asthma. http://www.nhlbi.nih.gov/guidelines/asthma/index.htm. [Google Scholar]
- Reddel 2000 .Reddel HK, Jenkins CR, Marks GB, Ware SI, Xuan W, Salome CM, et al. Optimal asthma control, starting with high doses of inhaled budesonide. European Respiratory Journal. 2000;16:226–35. doi: 10.1034/j.1399-3003.2000.16b08.x. [DOI] [PubMed] [Google Scholar]
- RevMan 2008 .The Nordic Cochrane Centre. The Cochrane Collaboration . Review Manager (RevMan). 5.0. The Nordic Cochrane Centre, The Cochrane Collaboration; Copenhagen: 2008. [Google Scholar]
- Salpeter 2006 .Salpeter SR, Buckley NS, Ormiston TM, Salpeter EE. Meta-analysis: effect of long-acting {beta}-agonists on severe asthma exacerbations and asthma-related deaths. Annals of Internal Medicine. 2006;144:904–12. doi: 10.7326/0003-4819-144-12-200606200-00126. [DOI] [PubMed] [Google Scholar]
- Sears 1998 .Sears MR. Asthma treatment: Inhaled beta-agonists. Canadian Respiratory Journal. 1998;5(Suppl A):54A–59A. [PubMed] [Google Scholar]
- Sharek 1999 .Sharek PJ, Bergman D, Ducharme F. Beclomethasone for asthma in children: effects on linear growth. Cochrane Database of Systematic Reviews. 1999;(Issue 3) doi: 10.1002/14651858.CD001282. [DOI: 10.1002/14651858.CD001282] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrewsbury 2000 .Shrewsbury S, Pyke S, Britton M. Meta-analysis of increased dose of inhaled steroid or addition of salmeterol in symptomatic patients (MIASMA) BMJ. 2000;320:1368–73. doi: 10.1136/bmj.320.7246.1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storms 2003 .Storms W. Clinical trials: Are these your patients? Journal of Allergy & Clinical Immunology. 2003;5(Suppl):S107–S111. doi: 10.1016/j.jaci.2003.09.019. [DOI] [PubMed] [Google Scholar]
- Suissa 2001 .Suissa S, Ernst P. Inhaled corticosteroids: impact on asthma morbidity and mortality. Curr Rev Allergy Clin Immunol. 2001;107(937):944. doi: 10.1067/mai.2001.115653. [DOI] [PubMed] [Google Scholar]
- Warner 1998 .Warner JO, Naspitz CK, editors. Third international pediatric consensus statement on the management of childhood asthma. Pediatric Pulmonology. 1998;25:1–17. doi: 10.1002/(sici)1099-0496(199801)25:1<1::aid-ppul1>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Greenstone 2005 .Greenstone IR, Ni Chroinin M, Masse V, Danish A, Magdalinos H, Zhang X, et al. Combination of inhaled long-acting beta2-agonists and inhaled steroids versus higher dose of inhaled steroids in children and adults with persistent asthma. Cochrane Database of Systematic Reviews. 2005;(Issue 4) doi: 10.1002/14651858.CD005533. [DOI: 10.1002/14651858.CD005533] [DOI] [PubMed] [Google Scholar]
- * Indicates the major publication for the study