Abstract
Objective
To estimate the lifetime risk of stress incontinence, pelvic organ prolapse surgery, or both using current, population-based surgical rates from 2007–2011.
Methods
We used a 2007–2011 a U.S. claims and encounters database. We included women aged 18–89 years and estimated age-specific incidence rates and cumulative incidence (lifetime risk) of stress incontinence surgery, pelvic organ prolapse surgery, and either incontinence or prolapse surgery, with 95% confidence intervals. We estimated lifetime risk until the age of 80 to be consistent with prior studies.
Results
From 2007–2011, we evaluated 10,177,480 adult women who were followed for 24,979,447 person-years. Among these women, we identified 65,397 incident, or first, stress incontinence, and 57,755 incident prolapse surgeries. Overall, we found that the lifetime risk of any primary surgery for stress incontinence or pelvic organ prolapse was 20.0% (95%CI 19.9, 20.2) by the age of 80 years. Separately, the cumulative risk for stress incontinence surgery was 13.6% (95%CI 13.5, 13.7) and that for pelvic organ prolapse surgery was 12.6% (95%CI 12.4, 12.7). For age-specific annual risk, stress incontinence demonstrated a bimodal peak at age 46 and then again at age 70–71 with annual risks of 3.8 and 3.9 per 1,000 women, respectively. For pelvic organ prolapse, the risk increased progressively until ages 71 and 73 when the annual risk was 4.3 per 1,000 women.
Conclusion
Based on a U.S. claims and encounters database, the estimated lifetime risk of surgery for either stress incontinence or pelvic organ prolapse in women is 20.0% by the age of 80.
INTRODUCTION
Stress incontinence and pelvic organ prolapse are highly prevalent conditions(1) which are often managed surgically. Since the introduction of the tension-free mesh slings in the late 1990’s for incontinence(2) and the subsequent development of vaginal mesh procedures for pelvic organ prolapse(3), the surgical management of both conditions has increased substantially.(4, 5)
With these recent changes in surgical practice, an assessment of the lifetime risk of surgery for stress incontinence and pelvic organ prolapse is necessary to understand the overall public health impact and burden of pelvic floor disorders. Furthermore, lifetime surgical risk has critical implications regarding the morbidity associated with surgery (6, 7), the need for skilled surgeons, and the importance of training future providers. Given that urinary incontinence and pelvic organ prolapse are more common in the elderly population(1) and that the U.S. population is aging,(8) a contemporary assessment of lifetime surgical risk is necessary for accurate projections regarding health care utilization in the coming decades.(9, 10)
A commonly referenced statistic is that a woman has an 11.1% lifetime risk of surgery for either incontinence or pelvic organ prolapse by the age of 80 years.(11, 12) This estimate was based on 384 patients who underwent surgery in the Northwest region of the U.S in 1995. The small number of study patients, limited geographic region, and results from two decades ago potentially limit the applicability of the findings to current surgical practice.
Given the limitations of prior data regarding the lifetime risk of urogynecologic surgery in the U.S., we sought to use a large, population-based cohort to evaluate the age-specific incidence of surgery for stress incontinence, pelvic organ prolapse surgery, and either stress incontinence or prolapse surgery, and to estimate the cumulative risk of surgery over a woman’s lifetime.
MATERIALS AND METHODS
For this analysis, we utilized 10 years of data (2002–2011) from the MarketScan Commercial Claims and Encounters database and Medicare Supplemental and Coordination of Benefits database (copyright © 2012 Truven Health Analytics. All rights reserved).(13, 14) These population-based data included de-identified, adjudicated, healthcare claims from approximately 150 payers in the U.S. Individuals included in these databases were those with commercial, employment-based insurance such as employees, their spouses, dependents, as well as retirees. Claims and enrollment data were validated by Truven Health Analytics to ensure completeness, accuracy, and reliability. Unique individuals can be followed over time using encrypted identification numbers, and detailed enrollment data ensured that only those individuals who could generate a claim were included in the population at risk at any given time. This database included approximately 53 million individuals in 2011. Of note, in 2011, 55.1% of the U.S. population, or 170.1 million individuals, had employment-based insurance; thus, this database includes a significant proportion of those with employer-based insurance.(15) This study was determined to be exempt from further review by the Institutional Review Board at the University of North Carolina at Chapel Hill as only database contained only de-identified data.
On January 1st of each year from 2007–2011, we identified all women aged 18–89 who were continuously enrolled for the prior 3 years (look-back period) and the following 12 months (follow-up period). We excluded women aged older than 89 years because the number of women and procedures in this age category were low; thus, the data were not very precise for this age group. We also excluded women who had any surgery for stress incontinence or pelvic organ prolapse during the 3-year look-back period based on current procedural terminology (CPT) codes. For stress incontinence we included the following CPT codes: 57288; 51840, 51841, 58152, 51715, 57220, 51845, 57289, 51990, 51992, 58267 or 58293. For pelvic organ prolapse, we included the following CPT codes: 57200, 57210, 57230, 57240, 57250, 57260, 57265, 57268, 57270, 56810, 57284, 57285, 57423, 57267, 57282, 57283, 57280, 57425, 57106, 57107, 57109, 57110, 57111, 57112, 57120, or 58400. We also included hysterectomy as a pelvic organ prolapse surgery if there was a primary diagnosis of prolapse associated with the hysterectomy which occurred on the same date as surgery. A diagnosis of pelvic organ prolapse was based on the International Classification of Disease (ICD-9) diagnosis code of 618.x.
Among women who had no stress incontinence or pelvic organ prolapse surgeries during the look-back period, we identified all incident surgical procedures for stress incontinence and pelvic organ prolapse during the 12-month follow-up period. We estimated the number of women who underwent a surgery for stress incontinence, the number with a surgery for pelvic organ prolapse, and the number of women with any surgery for either stress incontinence or prolapse during the 12-month follow-up period. In this open cohort study, a woman could contribute more than one year of age-specific follow-up if she remained eligible on January 1st of subsequent years.
We estimated age-specific, one-year risks of incident surgery by dividing the number of women experiencing a surgery during the 12 months of follow-up by the number of eligible women for each year of age from 18–89. We also estimated the average risk for the following age groups: 18–29, 30–39, 40–49, 50–59, 60–69, 70–79, and 80–89 years to facilitate comparison with previously published estimates.(11, 12) We estimated age-specific surgery rates for stress incontinence only, pelvic organ prolapse only, and either stress incontinence or prolapse, and reported annual risk per 1,000 women with 95% confidence intervals (CIs) based on the binomial distribution.(16)
Our primary outcome was the cumulative risk of undergoing either stress incontinence or pelvic organ prolapse surgery beginning at the age of 18 up to 80 years of age. Because our objective was to estimate lifetime risk of these surgeries, it was important to account for death as a competing risk, as not all women live to the age of 80. Age-specific estimates of all-cause mortality were calculated using national census data and mortality data from the Centers for Disease Control on U.S. females from 2007.(17, 18) We used the DevCan software (National Cancer Institute)(16) to estimate the cumulative risk of surgery for stress incontinence, pelvic organ prolapse, or either with appropriate 95% confidence intervals, adjusted for the competing risk of death using methods developed by Fay et al.(19, 20)
For our primary analysis, the identification of incident surgeries during the follow-up period was based on excluding women who had any history of surgery for either stress incontinence or pelvic organ prolapse during the prior three years. To assess the sensitivity of our findings, we repeated the analysis using a five-year look-back period, limiting the population of eligible women to those who had five years of continuous enrollment and no stress incontinence or pelvic organ prolapse procedures during that period. While the longer look-back period increased the likelihood that the surgeries identified during follow-up were truly incident (rather than repeat) procedures, the trade-off was that fewer women have five years of continuous enrollment, and thus, our age-specific estimates and ultimately the estimates of lifetime risk based on these data were less precise.
RESULTS
From 2007–2011, 10,177,480 women 18 to 89 years of age contributed an average of 2.5 years of follow-up for a total of 24,979,447 person-years of follow-up (Table 1). Among these adult women, there were 65,397 women who had an incident surgery for stress incontinence, 57,755 women who had an incident surgery for pelvic organ prolapse, and 94,518 women who had an incident procedure for either stress incontinence or prolapse.
TABLE 1.
Study Population Who Had One-Year of Continuous Follow-Up and Who Did Not Have a Stress Incontinence or Pelvic Organ Prolapse Procedure During the Prior 3 Years
| Characteristic | Person-Years | % of Total Person-Years |
|---|---|---|
| Age | ||
| 18–29 | 2,987,244 | 12.0 |
| 30–39 | 3,642,368 | 14.6 |
| 40–49 | 5,278,482 | 21.1 |
| 50–59 | 6,306,039 | 25.2 |
| 60–69 | 3,720,152 | 14.9 |
| 70–79 | 1,876,460 | 7.5 |
| 80–89 | 1,168,702 | 4.7 |
| Region | ||
| Northeast | 2,606,670 | 10.4 |
| North Central | 6,837,698 | 27.4 |
| South | 10,776,805 | 43.1 |
| West | 4,695,963 | 18.8 |
| Unknown | 62,311 | 0.3 |
| Year | ||
| 2007 | 3,418,269 | 13.7 |
| 2008 | 4,192,798 | 16.8 |
| 2009 | 5,755,982 | 23.0 |
| 2010 | 5,153,437 | 20.6 |
| 2011 | 6,458,961 | 25.9 |
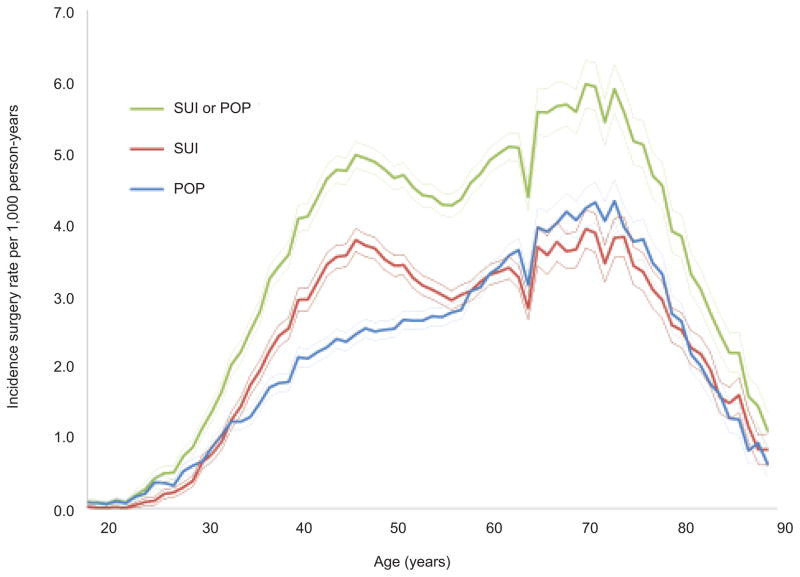
The age-specific estimates of the one-year risk of incident surgery for stress incontinence only, pelvic organ prolapse only, or either incontinence or prolapse for women between the ages of 18 to 89, are shown in Figure 1. For each decade of age, we also estimated the average annual risk (Table 2). Because Figure 1 illustrates the one-year risk of incident surgery for each year of age between 18 and 89, it provides more granularity than the data in Table 2. For stress incontinence, there were two peaks: first at age 46 when the annual risk was 3.8 per 1,000 women and then at age 70–71 when the annual risk was 3.9 per 1,000 women. For pelvic organ prolapse, the annual risk increased with age until a peak of 4.3 per 1,000 women at age 71 and 73. For either incontinence or prolapse surgery, the highest risk was 6.0 per 1,000 women at age 70.
Figure 1.
Age-specific annual risk (per 1,000 women) of surgery for stress urinary incontinence (SUI), pelvic organ prolapse (POP), or either SUI or POP surgery with 95% confidence intervals (CI).
TABLE 2.
Estimated Average Age-Specific Annual Risk of Stress Incontinence Surgery, Pelvic Organ Prolapse Surgery, or Either Incontinence or Pelvic Organ Prolapse Surgery per 1,000 Women
| Stress Incontinence Surgery | Pelvic Organ Prolapse Surgery | Either Incontinence or Prolapse Surgery | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Age | Annual Risk | (95% CI) | Annual Risk | (95% CI) | Annual Risk | (95% CI) |
| 18–29 | 0.1 | (0.1, 0.1) | 0.2 | (0.2, 0.2) | 0.3 | (0.3, 0.3) |
| 30–39 | 1.7 | (1.6, 1.7) | 1.4 | (1.3, 1.4) | 2.5 | (2.4, 2.5) |
| 40–49 | 3.4 | (3.4, 3.5) | 2.4 | (2.3, 2.4) | 4.6 | (4.6, 4.7) |
| 50–59 | 3.1 | (3.1, 3.2) | 2.8 | (2.7, 2.8) | 4.5 | (4.4, 4.5) |
| 60–69 | 3.3 | (3.3, 3.4) | 3.6 | (3.5, 3.6) | 5.1 | (5.0, 5.2) |
| 70–79 | 3.4 | (3.4, 3.5) | 3.8 | (3.7, 3.9) | 5.3 | (5.2, 5.4) |
| 80–89 | 1.8 | (1.7, 1.9) | 1.7 | (1.6, 1.7) | 2.6 | (2.5, 2.7) |
CI, confidence interval.
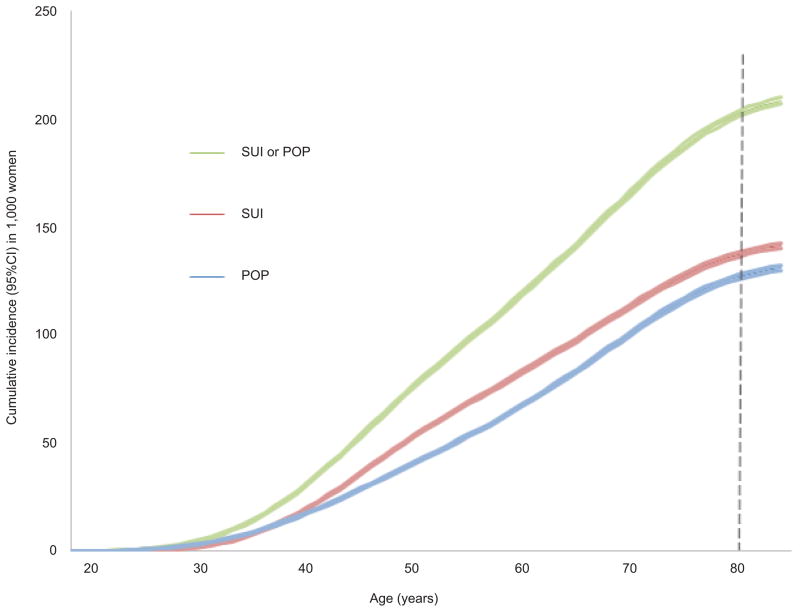
For the primary outcome, we estimated that the lifetime risk for either incontinence or prolapse surgery was 200.1 per 1,000 women or 20.0% (95% CI 19.9, 20.2) from age 18 to 80 (Figure 2). For surgery for stress incontinence or pelvic organ prolapse surgery, the lifetime risks were 13.6% (95%CI 13.5, 13.7) and 12.6% (95%CI 12.4, 12.7), respectively. The previously reported estimate of an 11.1% lifetime risk of either surgery (11) is now reached by the age of 58, based on the annual risk of surgery during 2007–2011.
Figure 2.
Cumulative incidence, or lifetime risk, of surgery for stress urinary incontinence (SUI), pelvic organ prolapse (POP), or SUI or POP surgery from age 18 years through age 84 years. The width of the lines represents the 95% confidence interval (CI) of the cumulative incidence at each age. The cumulative incidence (95% CI) by age 80 per 1,000 women was 200.1 (95% CI 198.7–201.5) for SUI or POP, 135.9 (95%CI 134.8–137.1) for SUI only, and 125.6 (95% CI 124.4–126.7) for POP only.
We conducted several sensitivity analyses to determine the robustness of our findings. In the sensitivity analysis using a five-year (rather than three-year) look-back period, the lifetime risks were slightly lower at 19.8% (95%CI 19.6, 20.0) for either surgery, 13.5 (95%CI 13.3, 13.7) for stress incontinence, and 12.4% (95%CI 12.2, 12.6) for pelvic organ prolapse surgery. We also conducted a sensitivity analysis in which we did not consider hysterectomy with a primary diagnosis of pelvic organ prolapse as a qualifying prolapse procedure. The resulting estimates of lifetime risk of surgery for pelvic organ prolapse were slightly lower (11.8%, 95%CI: 11.7, 11.9) as were those for the combined risk of surgery for either pelvic organ prolapse or stress incontinence (19.5%, 95%CI: 19.3, 19.6). We also considered whether regional variation in surgical rates would affect our estimates. Weighting the Marketscan sample to more accurately reflect the geographic distribution of women with employer-based insurance in the U.S. resulted in estimates of lifetime risk of surgery for stress incontinence or pelvic organ prolapse that were slightly lower (19.4%).
DISCUSSION
In this contemporary, population-based analysis, we found that the lifetime risk of surgery for either stress incontinence or pelvic organ prolapse was 20.0%. Thus, in a hypothetical cohort of women who are currently 18 years of age, one out of every five would be expected to undergo surgery for either stress incontinence or pelvic organ prolapse by age 80, highlighting the public health affect of these conditions. For perspective, a woman’s lifetime risk of developing breast cancer is 14.8%, while the lifetime risk of lung cancer is 6.3%.(21) Despite the fact that the lifetime risk of stress incontinence and pelvic organ prolapse surgery is significantly higher than that of breast cancer or lung cancer, women lack awareness and knowledge regarding these gynecologic conditions,(22, 23) which translates into limited healthcare seeking for these conditions which greatly impair quality of life.(22, 24)
Our cumulative incidence of 20.0% is nearly double that of two older U.S studies which reported rates of incontinence and prolapse surgery of 11.1%(11) and 11.8%.(12) We believe that this may be attributable to several different factors. First, the introduction of new surgical techniques, namely mid-urethral synthetic slings and transvaginal mesh procedures for pelvic organ prolapse, have resulted in higher rates of stress incontinence(4) and mesh prolapse surgeries.(5) For example, the rate of sling procedures increased from 209.7 to 266.5 per 100,000 person years from 2000 to 2009,(4) and the rate of vaginal mesh procedures increased from a rate of 36.7 to 60.8 per 100,000 person years from 2005 to 2010.(5) These products potentially allowed more gynecologists to offer pelvic floor repair based on a perception of improved ease and efficiency. In addition, the regional variation in stress incontinence and pelvic organ prolapse surgery in the U.S. may contribute, with higher rates in the South and the Midwest compared to the Northeast and West.(4, 5) Both of the prior studies were based in the Northwest,(11, 12) which may have underestimated the overall lifetime risk of surgery. Finally, previous investigations did not report confidence intervals around the cumulative risk, and with significantly smaller sample sizes, these estimates were likely less precise.
Estimated lifetime incidence rates of pelvic floor surgeries in other countries vary. In the Netherlands, de Boer et al.(25) reported a 20.3% risk of prior surgery in women aged 76–85 years. Among parous women in United Kingdom, Abdel-Fattah et al. found a 12.2% lifetime risk of incontinence and pelvic organ prolapse surgery.(26) A cross-sectional study from Australia reported a rate of 19% for pelvic organ prolapse surgery, which is significantly higher than our rate of 12.6%.(27) This international variance could be explained by true global differences in disease prevalence or differences in surgical practice patterns. For accurate public health planning, it is helpful to have current estimates of surgical rates that are reflective of national practice.
Regarding age-specific incidence, our study showed similar trends to prior studies with the highest rates of surgery in women aged 70–79.(11, 12) Our annual risk of surgery for either incontinence or pelvic organ prolapse surgery in this age group was 5.3 per 1,000 women (95% CI 5.2, 5.4) compared to 3.70 per 1,000 person-years from Fialkow et al.(12) and 6.62 per 1,000 person-years from Olsen et al.(11) By evaluating incident surgery rates by age in decades, some of the details regarding the impact of age may not be evident. In our study, we were able to provide insight into how stress incontinence surgery rates change with yearly increases in age, and we found two peaks in incidence around age 46 and 70–71 years. For pelvic organ prolapse, we found that our highest annual risk of incident surgery was 4.3 per 1,000 women at 71 and 73 years, and Smith et al. also noted the highest rate among 65–69 year olds from 2001–2005 with a rate of 5.0 per 1,000 person-years (95% CI 4.7, 5.4).(27)
The strengths of this study include the large, population-based cohort of over 10 million women that reflects practice patterns across the entire country during recent years. This is in contrast to prior U.S. studies which utilized data from almost two decades ago, focused on a single region, evaluated substantially smaller cohorts, and did not estimate confidence intervals. Our estimates of lifetime risk are based on the surgery rates between 2007 and 2011, which reflect practice since the introduction of mesh procedures for incontinence and pelvic organ prolapse.(4, 5) The magnitude of data allowed for calculation of incidence rates at every year of age, permitting a more accurate estimation of cumulative incidence. We also estimated confidence intervals to provide a sense of the precision of our age-specific and cumulative incidence estimates. Lastly, a novel aspect of our study is that we accounted for competing risks of mortality, and we utilized rigorous, state-of-the-art methodology developed and utilized by the National Cancer Institute to estimate lifetime risk of different types of cancer.(16, 19, 20)
Our study also had several limitations. While healthcare claims data provide an enormous number of subjects and procedures to evaluate, they do not permit a review of past medical records, and we are limited to the data included in healthcare claims. For example, we were unable to evaluate race, body mass index and comorbidities, such as obesity, diabetes or smoking with accuracy. Furthermore, we were limited our ability to definitively exclude women with prior surgeries; however, our estimates did not change significantly when we conducted a sensitivity analysis with a longer look-back period. For pelvic organ prolapse surgeries, we included hysterectomies with a primary diagnosis of prolapse. It is possible that uterine prolapse may be used as a billable diagnosis to perform a hysterectomy for a non-billable reason, such as contraception, and thus, might result in an over-estimation of the use of hysterectomy for symptomatic prolapse. These procedures represented 6.4% of incident procedures for pelvic organ prolapse and excluding them from the analysis had a modest effect on the estimates of lifetime risk. Our rationale for including hysterectomies was that women with uterovaginal prolapse are commonly undertreated by a hysterectomy alone as they do not undergo any concomitant prolapse surgeries. A study of California discharge data found that only 35% of women who underwent a hysterectomy for a primary diagnosis of uterovaginal prolapse had a concomitant apical support procedure.(28) Our study population was comprised of individuals with employer-based insurance or those with supplemental insurance from their employer or retirement benefit once they transition into Medicare. We were not able to evaluate the uninsured or those on Medicaid, a population who may have different surgery rates. That said, the majority of Americans (55%) have employment-based insurance so these estimates represent a substantial portion of the US population.(15)
Based on surgery rates from 2007–2011, the lifetime risk of undergoing a stress incontinence or pelvic organ prolapse surgery by the age of 80 is 20.0%. These surgeries will place a growing demand on health care resources and will require a commensurate increase in the number of trained pelvic floor surgeons. The high rates of surgery for both stress incontinence and pelvic organ prolapse continue to expose the need for improved prevention strategies.
Acknowledgments
Dr. Wu is supported by K23HD068404, Eunice Kennedy Shriver National Institute of Child Health & Human Development. Dr. Jonsson Funk is supported by grant number K02HS017950 from the Agency for Healthcare Research and Quality (AHRQ).
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Presented at the 34th Annual Meeting of the American Urogynecologic Society, Las Vegas, NV, Oct 18, 2013.
Financial Disclosure: Catherine A. Matthews has received grant funding from Pelvalon and has been a consultant to American Medical Systems. The other authors did not report any potential conflicts of interest.
References
- 1.Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008 Sep 17;300(11):1311–6. doi: 10.1001/jama.300.11.1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.FDA. 510(K) Number K974098. 1998 Jan 28; Available at: http://www.accessdata.fda.gov/cdrh_docs/pdf/K974098.pdf. Retrieved on December 10, 2013.
- 3.FDA Safety Communication. Update on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse. Issued on July 13, 2011. Available at: http://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm262435.htm. Retrieved on December 10, 2013.
- 4.Jonsson Funk M, Levin PJ, Wu JM. Trends in the surgical management of stress urinary incontinence. Obstet Gynecol. 2012 Apr;119(4):845–51. doi: 10.1097/AOG.0b013e31824b2e3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jonsson Funk M, Edenfield AL, Pate V, Visco AG, Weidner AC, Wu JM. Trends in use of surgical mesh for pelvic organ prolapse. Am J Obstet Gynecol. 2013 Jan;208(1):79.e1–7. doi: 10.1016/j.ajog.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sung VW, Weitzen S, Sokol ER, Rardin CR, Myers DL. Effect of patient age on increasing morbidity and mortality following urogynecologic surgery. Am J Obstet Gynecol. 2006 May;194(5):1411–7. doi: 10.1016/j.ajog.2006.01.050. [DOI] [PubMed] [Google Scholar]
- 7.Erekson EA, Yip SO, Ciarleglio MM, Fried TR. Postoperative complications after gynecologic surgery. Obstet Gynecol. 2011 Oct;118(4):785–93. doi: 10.1097/AOG.0b013e31822dac5d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vincent GK, Velkoff VA. THE NEXT FOUR DECADES, The Older Population in the United States: 2010 to 2050. Washington, D.C: U.S. Census Bureau; 2010. [Google Scholar]
- 9.Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstet Gynecol. 2009 Dec;114(6):1278–83. doi: 10.1097/AOG.0b013e3181c2ce96. [DOI] [PubMed] [Google Scholar]
- 10.Wu JM, Kawasaki A, Hundley AF, Dieter AA, Myers ER, Sung VW. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol. 2011 Sep;205(3):230.e1–5. doi: 10.1016/j.ajog.2011.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997 Apr;89(4):501–6. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 12.Fialkow MF, Newton KM, Lentz GM, Weiss NS. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008 Mar;19(3):437–40. doi: 10.1007/s00192-007-0459-9. [DOI] [PubMed] [Google Scholar]
- 13.Source: MarketScan® is a registered trademarks of Truven Health Analytics formerly. Thomson Reuters (Healthcare) Inc; Truven Health Analytics MarketScan® Commercial Claims and Encounters Database, 2000–2009. Available at: http://www.truvenhealth.com/your_healthcare_focus/pharmaceutical_and_medical_device/data_databases_and_online_tools.aspx. Retrieved on July 17, 2013. [Google Scholar]
- 14.Hansen LG, Chang S. Health Research Data for the Real World: The MarketScan Databases. White paper. 2011 Available at: http://www.truvenhealth.com/assets/2012_Truven_MarketScan_white_paper.pdf. Retrieved on July 17, 2013.
- 15.DeNavas-Walt C, Proctor BD, Smith JC. US Census Bureau, Current Population Reports, P60–243, Income, Poverty, and Health Insurance Coverage in the United States: 2011. U.S. Government Printing Office; Washington, D.C: 2012. Available at: http://www.census.gov/prod/2012pubs/p60-243.pdf. Retrieved on July 17, 2013. [Google Scholar]
- 16.Wilson EB. Probable Inference, the Law of Succession, and Statistical Inference Journal of the American Statistical Association. Journal of the American Statistical Association. 1927;22:209–12. [Google Scholar]
- 17.Population Projections, United States, 2004 – 2030, by state, age and sex, on CDC WONDER On-line Database. 2005 Sep; Available at: http://wonder.cdc.gov/population-projections.html. Retrieved on July 30, 2013.
- 18.Worktable 310. Deaths by single years of age, race, and sex, United States, 2007. CDC/NCHS, National Vital Statistics System. 2010 Apr; Available at: http://www.cdc.gov/nchs/data/dvs/MortFinal2007_Worktable310.pdf. Retrieved on July 30, 2013.
- 19.Fay MP. Estimating age conditional probability of developing disease from surveillance data. Popul Health Metr. 2004 Jul 27;2(1):6. doi: 10.1186/1478-7954-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fay MP, Pfeiffer R, Cronin KA, Le C, Feuer EJ. Age-conditional probabilities of developing cancer. Stat Med. 2003 Jun 15;22(11):1837–48. doi: 10.1002/sim.1428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.National Cancer Institute. Surveillance Research. Lifetime Risk Tables. Avaliable at: http://seer.cancer.gov/csr/1975_2010/results_merged/topic_lifetime_risk.pdf. Retrieved on December 10, 2013.
- 22.Doshi AM, Van Den Eeden SK, Morrill MY, Schembri M, Thom DH, Brown JS, et al. Women with diabetes: understanding urinary incontinence and help seeking behavior. J Urol. 2010 Oct;184(4):1402–7. doi: 10.1016/j.juro.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kiyosaki K, Ackerman AL, Histed S, Sevilla C, Eilber K, Maliski S, et al. Patients’ understanding of pelvic floor disorders: what women want to know. Female Pelvic Med Reconstr Surg. 2012 May-Jun;18(3):137–42. doi: 10.1097/SPV.0b013e318254f09c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Berger MB, Patel DA, Miller JM, Delancey JO, Fenner DE. Racial differences in self-reported healthcare seeking and treatment for urinary incontinence in community-dwelling women from the EPI Study. Neurourol Urodyn. 2011 Nov;30(8):1442–7. doi: 10.1002/nau.21145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.de Boer TA, Slieker-Ten Hove MC, Burger CW, Kluivers KB, Vierhout ME. The prevalence and factors associated with previous surgery for pelvic organ prolapse and/or urinary incontinence in a cross-sectional study in The Netherlands. Eur J Obstet Gynecol Reprod Biol. 2011 Oct;158(2):343–9. doi: 10.1016/j.ejogrb.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 26.Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S. Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open. 2011;1(2):e000206. doi: 10.1136/bmjopen-2011-000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010 Nov;116(5):1096–100. doi: 10.1097/AOG.0b013e3181f73729. [DOI] [PubMed] [Google Scholar]
- 28.Elliott CS, Rhoads KF, Comiter CV, Chen B, Sokol ER. Improving the accuracy of prolapse and incontinence procedure epidemiology by utilizing both inpatient and outpatient data. Int Urogynecol J. 2013 Nov;24(11):1939–46. doi: 10.1007/s00192-013-2113-z. [DOI] [PubMed] [Google Scholar]