Abstract
Introduction:
This study provides a prospective fine-grain description of the incidence and pattern of intentions to quit, quit attempts, abstinence, and reduction in order to address several clinical questions about self-quitting.
Methods:
A total of 152 smokers who planned to quit in the next 3 months called nightly for 12 weeks to an Interactive Voice Response system to report cigarettes/day, quit attempts, intentions to smoke or not in the next day, and so forth. No treatment was provided.
Results:
Most smokers (60%) made multiple transitions among smoking, reduction, and abstinence. Intention to not smoke or quit often did not result in a quit attempt but were still strong predictors of a quit attempt and eventual abstinence. Most quit attempts (79%) lasted less than 1 day; about one fifth (18%) of the participants were abstinent at 12 weeks. The majority of quit attempts (72%) were not preceded by an intention to quit. Such quit attempts were shorter than quit attempts preceded by an intention to quit (<1 day vs. 25 days). Most smokers (67%) used a treatment, and use of a treatment was nonsignificantly associated with greater abstinence (14 days vs. 3 days). Making a quit attempt and failing early predicted an increased probability of a later quit attempt compared to not making a quit attempt early (86% vs. 67%). Smokers often (17%) failed to report brief quit attempts on an end-of-study survey.
Conclusions:
Cessation is a more chronic, complex, and dynamic process than many theories or treatments assume.
INTRODUCTION
Despite the implementation of many public health and tobacco control interventions, the incidence of quit attempts in the United States has not reliably increased in the last 20 years (Malarcher, Dube, Shaw, Babb, & Kaufmann, 2011). Clearly, we need new interventions. One factor impeding the development of new interventions is a paucity of understanding of the natural history of quit attempts (Klingemann et al., 2001). Some models of quit attempts assume that smokers make a clear decision to quit and set a future quit date (Prochaska, DiClemente, & Norcross, 1992). Other descriptions suggest quit attempts are sudden and spontaneous, largely devoid of anticipatory planning (Larabie, 2005).
Although there are descriptions of the postquit attempt process (Hughes, Keely, & Naud, 2004), these typically use abstinence initiation and lapse/or relapse as the outcomes and do not examine the processes leading to a quit attempt or occurring after a lapse/relapse. Most also measure smoking, intentions, and so forth only weekly or monthly and typically examine treatment seekers. To our knowledge, the only prospective, day-by-day descriptions of quit attempts in a real-world setting are two small, brief studies we conducted (Hughes et al., 2013; Peters & Hughes, 2009). These two studies found intentions to quit smoking often change on a daily basis, and many smokers repeatedly and rapidly transitioned among smoking as usual, abstinence, and reduction states, even within a month. This study adds to these studies by using a larger sample size, a longer duration of monitoring and including new measures. This analysis focuses on several specific questions about self-quitting, which are outlined in Table 1.
Table 1.
Clinical Questions About Self-Quitting Tested in this Study
| 1. What is the overall pattern of changes in smoking? |
| 2. How often do smokers intend to stop smoking and do such intentions quit predict a quit attempt or abstinence? |
| 3. How often do smokers actually change (i.e., reduce or stop smoking)? |
| 4. How long do quit attempts last? |
| 5. What percent of quit attempts are “planned” and do planned quit attempts last longer? |
| 6. What methods or treatments were used and does such use predict greater abstinence? |
| 7. Does failing to quit decrease motivation to quit? |
| 8. How accurate is recall of a quit attempt? |
METHODS
Overview
We conducted a prospective cohort study of adult daily smokers who planned to quit smoking at some point in the next three months. Participants called an Interactive Voice Response (IVR) system nightly for 12 weeks to report intentions to not smoke the next day, quit attempts, abstinence, and cigarettes/day. Participants also completed questionnaires monthly. We provided no treatment. This analysis focuses on quit attempts. Future papers will describe variability in cigarettes/day, smoking reduction, and whether environmental cues prompt quit attempts. The University of Vermont Committees on the Use of Human Participants approved the study, and we registered the study at www.clinicaltrials.com (NCT00995644).
Participants
Recruitment
During 2010 and 2011, we recruited smokers via Internet messages. When smokers entered terms such as “quit smoking” into search engines (Google, Yahoo, and Bing), small advertisements appeared that led to our study Web site. We also posted messages on research study web sites (e.g., www.clinicaltrials.gov and www.clinical.connection.com) and on www.craigslist.com in various large cities. A typical message was “Daily cigarette smokers who intend to quit wanted for University of Vermont research study. Reimbursement for completing phone questions and mailed surveys. No need to leave home. This study does not offer treatment.”
Inclusion Criteria
To obtain smokers likely to change their smoking in the next few months, we “enriched” the sample by enrolling only smokers who stated they probably or definitely intended to quit within the next three months. We did this because only 52% of U.S. smokers make a quit attempt each year (Malarcher et al., 2011); that is, on average, 4% of smokers try to quit each month (52%/12 months); thus, we expected that, if we used a representative sample of current smokers, we would observe a quit attempt in only about 12% of those monitored during the three-month study period. Our enriched sample probably represents about a third of cigarette smokers (Wewers, Stillman, Hartmann, & Shopland, 2003).
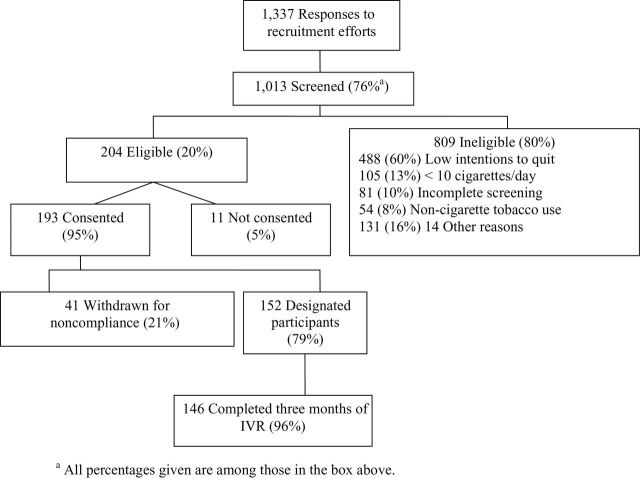
Other inclusion criteria were as follows: ≥18 years of age, smoked ≥10 cigarettes/day for at least one year, did not use other forms of tobacco in the last two weeks and had no plans to do so, had access to a touch-tone phone, able to read and write English, did not work a night shift, typically went to bed between 21:00 and 02:00, and were not pregnant. Potential participants were verbally consented. If participants did not complete at least five of the first seven daily IVR calls or did not provide data for ≥28 days, their data were excluded. The most common reason for ineligibility was low intention to quit in the next three months (Figure 1). One fifth (21%) of those eligible were excluded due to poor initial compliance (i.e., not completing five of the first seven calls), leaving 152 designated participants.
Figure 1.
Participant flow. Note. IVR = Interactive Voice Response. aAll percentages given are among those in the box.
Participant Characteristics
The sample characteristics were similar to those in our two prior pilot studies (Hughes et al., 2013; Peters & Hughes, 2009). They were also comparable to the average U.S. daily smoker who had recently tried to quit in terms of age and race, but the participants were more likely to have graduated high school and be a woman (Table 2; Hughes & Callas, 2010a). Participants also smoked more cigarettes/day and were more dependent smokers than U.S. self-quitters, but appeared to be lighter and less dependent smokers than treatment seekers (Foulds et al., 2006; Sheffer et al., 2009).
Table 2.
Participant Characteristics
| Characteristics | Current study | U.S. smokers |
|---|---|---|
| Age (years) | 45 (13) | 40a |
| Women (%) | 67 | 46a |
| High school grad (%) | 94 | 72a |
| Non-Hispanic Whites (%) | 77 | 74 a |
| Married (%) | 34 | |
| Employed (%) | 45 | |
| Cigarettes/day | 19 (10) | 15b |
| Fagerström Test for Nicotine Dependence | 5.3 (2.2) | 4.7c |
| Plan to quit in next month (%) | 36 | 8d |
| 5+ alcohol drinks in one day in last year (%) | 38 | 22e |
| Used marijuana last month | 10 | 27f |
| Mental Health Inventory > 21(%) | 16 |
aU.S. smokers who made a quit attempt in 2007 (Hughes & Callas, 2010a).
bU.S. smokers in 2010 (King et al., 2011).
cSmokers in Detroit and St Louis in 2003 (Mooney, Leventhal, & Hatsukami, 2006).
dU.S. smokers in 1995–1999 (Wewers et al., 2003).
eU.S. adults (not just smokers) in 2011 (Malarcher et al., 2011).
fBaltimore smokers in 1994 (Ford, Vu, & Anthony, 2002).
Measures
Baseline Questionnaire
Participants completed baseline and monthly questionnaires either via return of mailed questionnaires (19%) or via a password-protected Internet site (81%). The baseline questionnaire collected demographic and smoking information.
Interactive Voice Response
Participants completed the IVR questions nightly for three months. The IVR is an automated phone system in which participants call a number that directs them to enter data using their touch-tone keypad. The IVR has many of the assets of computer-assisted telephone interviewing, plus the increased confidentiality results in more valid substance use reports (Corkrey & Parkinson, 2002). We reimbursed participants $2/day for IVR completions plus $10 bonuses for high compliance. Each evening, the IVR asked if the participant smoked that day and, if so, the number of cigarettes smoked. If the participant did not smoke that day, the IVR asked whether this was an “attempt to stop smoking”; a yes answer was our definition of a quit attempt. If the participant did smoke that day, the IVR asked the smoker “Do you think you will smoke cigarettes tomorrow?” In a prior study, we asked smokers each night whether “they were going to quit the next day every day of the study.” We thought this repeated questioning may have prompted quit attempts and hypothesized that asking about “continuing to smoke” would be a less reactive proxy for quit intentions. However, as discussed in the Discussion, an intention to not smoke the next day may not be isomorphic with a “serious attempt to stop smoking for good.”
At the end of each week, the IVR asked whether participants had made “an attempt to stop smoking that lasted less than a day in the past week.” Thus, we obtained information on two types of quit attempts: (a) those associated with one or more full days of abstinence detected by the daily IVR (“extended quit attempts”) and (b) those not associated with a day of abstinence detected by the weekly IVR (“brief quit attempts”). To prevent counting attempts to re-establish abstinence after a lapse as new quit attempts, we required a new quit attempt be preceded by seven consecutive days of smoking (Hughes et al., 2003). We defined a day of reduction as a nonabstinent day in which the smoker reduced cigarettes/day by ≥50% compared to the mean cigarettes/day when not trying to quit or reduce.
The weekly IVR asked participants to rate their intention to stop smoking in the next week from definitely not, probably not, possibly, probably, and definitely. We defined probably and definitely as a weekly intention to quit (we did not ask whether they had set a quit day).
Monthly Questionnaires
At the end of the first, second, and third months, smokers were asked if they had smoked in the last seven days, whether they intended to quit in the next month (yes/no), and, if so, whether they had set a quit date.
Data Analysis
Some smokers tried to change or did change their smoking status on multiple occasions (see Results) and others did not; thus, some smokers contributed more data on intentions and quit attempts than other smokers. To ensure that each participant contributed equally to the analyses, when reporting averages, we first averaged responses within participants and only then across participants. We used medians to indicate central tendency because many distributions appeared non-normal. Also, when appropriate, we used multilevel regression to account for differences in between- and within-participant variability.
RESULTS
Preliminary Analyses
Among the 12,768 potential days of IVR compliance (152 smokers × 84 days), 5% of days had missing IVR data, 5% of monthly questionnaires were missing, and 5% of participants dropped out of the study (defined as not having any IVR data in the last week of the study).
What Is the Overall Pattern of Change in Smoking?
Some smokers (18%) had no episodes of change; that is, no abstinence or ≥50% reduction, or a single episode (22%); however, most smokers (60%) had multiple episodes of abstinence or reduction (Figure 2). If the criterion for reduction is lowered to ≥25%, then 3% had no episodes, 8% had one episode, and 89% had multiple episodes of change.
Figure 2.
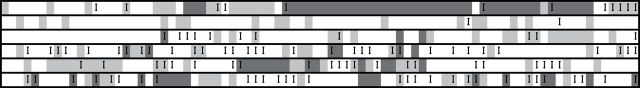
Examples of multiple transitions across intention, smoking, reduction, and abstinence states for six participants. Columns represent days of the study. Rows represent individual participants. Black boxes represent a day of intentional abstinence. Gray boxes represent a day of reduction in cigarettes/day by ≥50%. An I represents a day in which, on the night before, smokers reported they planned not to smoke that day.
How Often Do Smokers Prospectively Intend to Stop Smoking and Do Such Intentions Predict Quit Attempts and Abstinence?
Intention to change was measured in three ways: (a) intention to not smoke the next day, (b) intention to quit in the next week, and (c) intention to quit in the next month. Whether these predicted quitting is outlined in Table 3. During the 12 weeks, 24% of participants never stated they planned to not smoke the next day during the study, 17% reported one such intention, 19% reported from two to three such intentions, and 40% reported four or more such intentions. Across all days of the study, intending to not smoke the next day was rare, intending to quit in the next week was uncommon, but intending to quit in the next month was common (Table 3).
Table 3.
Intentions and Subsequent Quit Attempts and Abstinence
| Intention | Incidence of intention | Incidence of quit attempta | Incidence of abstinence | ||
|---|---|---|---|---|---|
| % | % | OR b (95% CI) | % | OR b (95% CI) | |
| Daily | |||||
| Intend to smoke | 93 | 3 | <1c | ||
| Do not intend to smoke | 7 | 16 | 4.9 (3.8, 6.4) | 8c | 35.0 (21.0, 59.0) |
| Weekly | |||||
| No intention to quit | 81 | 17 | 2d | ||
| Intend to quit | 19 | 62 | 7.2 (4.9, 10.6) | 11d | 7.2 (3.8, 13.7) |
| Monthly | |||||
| No intention to quit | 46 | 36 | 1e | ||
| Intend to quit, no quit date | 42 | 62 | 2.9 (1.8, 4.6) | 6e | 5.7 (1.2, 27.0) |
| Intend and set quit date | 12 | 76 | 5.7 (2.7, 12.2) | 12e | 10.8 (1.9, 58.8) |
Note. OR = odds ratio; CI = confidence interval.
aShort or long quit attempt.
bFrom multilevel regression. These are unadjusted results as none of the baseline variables predicted quitting.
cAbstinent next day.
dAbstinent on last day of week.
eAbstinent for last seven days of month.
An intention to not smoke the next day was rarely followed by a quit attempt, but an intention to quit in the next week or in the next month was often followed by a quit attempt. Stating one would not smoke on the next day on the IVR strongly predicted a greater probability of a quit attempt and the probably of abstinence the next day (Table 3). Similar results occurred with stating one would quit in the next week (and abstinence in next week) or quit in the next month (and abstinence in the next month).
Few smokers set a quit date (24% of those who planned to quit in the next month); those who did had a nonsignificantly greater probability of making a quit attempt (multilevel regression, p = .09) or becoming abstinence (multilevel regression, p = .27) in the next month than those who intended to quit but did not set a quit date (Table 3).
How Often Do Smokers Actually Change (i.e., Stopped or Reduced Smoking)?
Overall, 66 participants (43%) reported 88 extended quit attempts and 111 participants (73%) reported 323 brief quit attempts; that is, 79% of all quit attempts were brief quit attempts. Combining brief and extended quit attempts, 127 participants (84%) reported 411 attempts. Among those who made a quit attempt, the median number of attempts was 2 (1, 4). Overall, 16% of participants never made a quit attempt, 27% made one quit attempt, 16% made two, and 40% made three or more quit attempts; thus, among those who made a quit attempt, 67% made repeated quit attempts. Abstinence that was not due to a quit attempt was rare (<1%). Reduction was also common; 91 participants (79%) reported reducing ≥50%; 21% had one episode, 20% had from two to three episodes, and 38% had four or more episodes. If the criterion is changed to ≥25%, then 97% reported at least one episode and 71% reported four or more episodes.
How Long Do Quit Attempts Last?
On the longest quit attempt of each smoker, 48% of attempts lasted less than a day, 8% lasted only one day, 6% lasted from two to seven days, and 38% lasted more than seven days. Few smokers (18%) were seven-day point prevalent abstinent at the end of the study or were abstinent from their first quit attempt to the end of the study (15%). None of the baseline characteristics (Table 1), including Fagerström Test for Nicotine Dependence, predicted the duration of the longest quit attempt.
We examined lapse to relapse transitions only among extended quit attempts. Of the 88 extended quit attempts, 22% did not lapse. Among the 55 attempts in which a lapse occurred, in 60% the smoker immediately transitioned to daily smoking, in 18% they began daily smoking 2–6 days after the first lapse, in 9% it began 7–13 days after the lapse, and in 7% it was 14 or more days after the lapse. Among those who lapsed, the median time to return to their usual cigarettes/day was 7.5 days (3, 14).
What Percent of Quit Attempts Are Planned, and Do Planned Quit Attempts Last Longer?
Overall, 28% of quit attempts were preceded by an intention to not smoke the next day (our definition of planned). Planned quit attempts lasted longer than unplanned quit attempts (median = 25 days vs. <1 day, log-rank test, χ2 = 33.4, p < .0001).
What Methods or Treatments Were Used, and Did Such Use Predict More Abstinence?
Few (17%) quit attempts were preceded by gradual reduction, that is, a ≥50% reduction in smoking. We did not ask about use of treatments with every quit attempt, but at the end of the study, we asked whether participants had used any treatment during the study. Among those who made one or more quit attempts, 49% had used a medication alone, 5% had used counseling alone, and 18% used both at some point during the study. Smokers who used a treatment at some point during the study had a nonsignificantly greater median duration of their longest quit attempt than those who did not use a treatment (multilevel regression 14 vs. 3 days, p = ns). A similar nonsignificant result occurred when we examined only medication treatment, that is, 14 vs. 4 days (multilevel regression p = ns), when we examined individual medications, and when we entered cigarettes/day and dependence scores as covariates to minimize indication bias
Does Failing to Quit Decrease Motivation to Quit?
Those who made a quit attempt and failed in the first two weeks were more likely to make a second attempt than those who did not make a quit attempt during the first two weeks (86% vs. 67%, relative risk [RR] = 1.3, χ2 = 6.8, p = .01). A similar result occurred among those making a failed quit within the first four weeks (73% vs. 52%, RR = 1.4, χ2 = 6.4, p = .01). Among those who made multiple quit attempts, the duration of the first and second quit attempts (n = 86) and the first and third quit attempts (n = 61) was similar; however, the duration of the fourth quit attempt was longer than the first quit attempt (34% vs. 17% lasted ≥1 day, log-rank test χ2 = 9.4, p < .002; n = 47).
How Accurate Is Recall of Quit Attempts?
At the end of the study, we asked smokers whether they “tried to stop smoking while in the study.” Most retrospective reports of quitting (81%) were concordant with the IVR reports; however, 17% of smokers reported a quit attempt on an IVR call, but at the end of the study stated they did not make a quit attempt. Whether the attempt was planned or not did not influence recall; however, among those who only made brief quit attempts, 40% reported no quit attempt, but among those who only made extended quit attempts, only 3% reported no quit attempt.
DISCUSSION
Our major results are summarized in Table 4.
Table 4.
Major Findings
| 1. Most smokers had multiple, and often rapid, attempts to stop or reduce during the 12 weeks. |
| 2. Intentions to not smoke the next day often did not result in a quit attempt (16%), but most intentions to quit in the next week or month did so (60% and 62%). Intentions were strong prospective predictors of quit attempts and abstinence (odds ratios 3.3–35.0). Setting a quit date was rare (21%) and showed a nonsignificant trend to predict greater abstinence. |
| 3. Most smokers (60%) attempted to quit or reduce multiple times during the study. |
| 4. The longest quit attempt lasted less than a day on 48% of quit attempts. Few (18%) were abstinent at the end of the study. |
| 5. Three fourths of quit attempts (72%) were unplanned (i.e., were not preceded by an intention not to smoke the next day). Planned quit attempts lasted longer (25 days vs. 1 day) than unplanned quit attempts. |
| 6. Use of treatments was common, and treatment was nonsignificantly associated with greater abstinence (14 days vs. 3 days). |
| 7. Quitting and failing early on predicted increased, not decreased, quit attempts later (86% vs. 67%). Repeat quit attempts were not less successful than the initial quit attempt. |
| 8. On a retrospective survey, smokers often (17%) failed to report brief quit attempts. |
Limitations and Assets
One limitation is our use of only smokers who planned to quit at some point during the next 12 weeks in order to make sure we observed a sufficient number of quit attempts. Whether our results would occur in less motivated or more motivated smokers is unclear. Another possible limitation of the study is that the intensive monitoring in the study may have increased quitting via experimenter demand. We tried to limit such “reactivity” (Korotitsch & Nelson-Gray, 1999) by having no in-person contact with participants and using a putatively less-intrusive method of asking intentions about quitting smoking. An alternative would have been to use a less-intensive monitoring such as weekly recall, but even this brief recall appears to allow retrospective bias (Shiffman, 2009). Another limitation is that the sample differed from the average U.S. smoker (Hughes & Callas, 2010a) in several respects, in part, because we intentionally chose smokers likely to attempt to change within the 12 weeks of the study. Clearly, further natural history studies using population-based samples, or samples of interest (e.g., adolescents, self-quitters, or nondaily smokers) are needed to examine the replicability and generalizability of our results. Another limitation is that we did not biochemically verify quit attempts. Verification of quit attempts that occur at random times and last only from one to two days is difficult and we know of no report of doing this successfully. Also, self-reports of smoking in nonintervention trials appear to be valid (SRNT Subcommittee on Biochemical Verification, 2002).
The major asset of the study is that it provided a prospective, fine-grained measurement of intention and smoking status on a daily basis. This is important because, as mentioned previously, several lines of evidence indicate retrospective recall of quit attempts is poor (Berg et al., 2010; Borland, Partos, & Cummings, 2012; Borland, Partos, Yong, Cummings, & Hyland, 2012; Gilpin & Pierce, 1994). For example, in our study, 40% of smokers, who reported a brief quit attempt on a daily IVR, at the end of the study reported they did not make a quit attempt during the study. A final asset is the low incidence of missing data.
Repeated Attempts to Change Smoking
This study replicates the results of prior studies that among smokers who plan to quit in the near future, most make multiple, often rapid, transitions among smoking, abstinence, and reduction, and between intentions to smoke and intentions not to smoke, over short periods of time (Etter & Sutton, 2002; Hughes, Keely, Fagerström, & Callas, 2005; Hughes et al., 2005, 2013; Peters & Hughes, 2009). The complex and dynamic patterns in this study and our prior studies suggest that, for many smokers, an attempt to stop or reduce smoking does not end at lapse or relapse. For example, in this prospective study, among those who made a quit attempt in the first two weeks, 67% made repeat quit attempts during the following 10 weeks. This incidence of recycling is much greater than reported in prior retrospective studies, that is, 6% within three months (Curry, Marlatt, Peterson, & Lutton, 1988), 38% within one year (Hughes, Hymowitz, Ockene, Simon, & Vogt, 1981), and 26% within two years (Brandon, Tiffany, Obremski, & Baker, 1990). One possible reason for this discrepancy is that smokers forget (Berg et al., 2010; Borland, Partos, & Cummings, 2012; Borland, Partos, Yong et al., 2012; Cooper et al., 2010) or intentionally under-report (Carpenter, Sterba, Boatright, & West, 2011) quit attempts. In fact, we found this to occur in our data set.
Our results suggest that, consistent with other data (Joseph, Rice, An, Mohiuddin, & Lando, 2004), smokers who fail to quit are often not discouraged and are ready to try again in the near future. This result suggests that interventions that continue to engage the smoker after a failed quit attempt may be helpful. In fact, the three studies with some of the highest quit rates, all continued to intervene with smokers even after they relapsed (Anthonisen et al., 1994; Hall, Humfleet, Reus, Munoz, & Cullen, 2004; Hughes et al., 1981). Although some treatment studies have focused on prompting a new quit attempt (i.e., recycling), with a few exceptions (Smith et al., 2001; Stapleton et al., 1995), these studies prompted a new quit many months after the relapse (Partin et al., 2006). Given our results that often smokers appear ready to try to quit soon after a relapse, further trials of recycling interventions that occur immediately after a relapse should be implemented. In fact, several clinical treatments such as smoking reduction, nicotine medication sampling, and practice quit attempts are being tested as methods to prompt new quit attempts (Carpenter, Alberg, Gray, & Saladin, 2010; Carpenter, Hughes, Solomon, & Callas, 2004; Carpenter et al., 2011).
Intentions to Not Smoke
The large majority of intentions to not smoke the next day (84%) did not result in a quit attempt. This may have been an artifact of how we asked the question. Although intention to quit may appear to be a dichotomous outcome, several studies have shown that commitment to quit can be a continuous outcome (Hall, Havassy, & Wasserman, 1990, 1991). Perhaps answering “no” to “do you think you will smoke cigarettes tomorrow” may represent a relatively small commitment to quitting compared to answering “yes” to “do you plan to quit.” However, even when we asked directly about intention to quit in the next week or month, about 40% of those who said they would attempt to quit, never did so. This is consistent with prior studies (Hughes et al., 2005; Prochaska, Velicer, DiClemente, & Fava, 1988).
In this prospective study, the large majority (72%) of quit attempts were preceded by an intention to smoke the next day. In most prior retrospective studies, the proportion of quit attempts that were not preceded by an intention to quit was smaller (37%–52%) than in our study (Cooper et al., 2010; Larabie, 2005; Sendzik, McDonald, Brown, Hammond, & Ferrence, 2011; West & Sohal, 2006). This discrepancy may be due to recall bias (i.e., smokers forget many quit attempts) and perhaps this is especially true for quit attempts not preceded by planning (Berg et al., 2010; Borland, Partos, & Cummings, 2012; Borland, Partos, Yong et al., 2012; Gilpin & Pierce, 1994). Another possibility is our use of a different intention question. Prior retrospective studies have used either open-ended questions (Larabie, 2005; Murray, McNeill, Lewis, Britton, & Coleman, 2010), asked about “planned” quit attempts (Ferguson, Shiffman, Gitchell, Sembower, & West, 2009; Sendzik et al., 2011; West & Sohal, 2006) or asked how long before the attempt smokers chose a quit day (Cooper et al., 2010).
This prospective study found quit attempts preceded by an intention not to smoke (i.e., similar to planned quit attempts) were much more likely to be successful than those preceded by an intention to smoke (i.e., similar to unplanned quit attempts). In contrast, retrospective studies have found that unplanned quit attempts were as successful, and, in several cases, more successful, than planned quit attempts (Cooper et al., 2010; Ferguson et al., 2009; Larabie, 2005; Sendzik et al., 2011; West & Sohal, 2006). One possible reason for this discrepancy is, again, recall bias in the retrospective studies such that many brief quit attempts were forgotten, or our question wording. Clearly, further “prospective” tests of the outcomes of planned versus unplanned quit attempts are needed (Hughes & Callas, 2011).
Intentions to quit smoking remained high after a failed quit attempt as indicated by the fact that the majority of smokers made multiple attempts to change during the 12 weeks of the study. Consistent with a prior population-based study, a recent quit attempt predicted a future quit attempt (Partos, Borland, Yong, Hyland, & Cummings, 2013); however, inconsistent with that study, we found future quit attempts were not less successful than the initial quit attempt.
Quit and Reduction Attempts
Two thirds of smokers stated they used a cessation treatment during the study. This incidence appears to be much higher than in large, retrospective population-based surveys, where 34% reported using a treatment on their last quit attempt (Shiffman, Brockwell, Pillitteri, & Gitchell, 2008). This is probably because our incidences were based on use of a treatment at any time during the three months of the study, not on use during a given quit attempt. Case–control studies of treatment users versus nonusers differ in whether use of treatment is associated with increased success (Hughes, Peters, & Naud, 2011). Most of these studies used retrospective recall and, thus, are subject to selection biases (Berg et al., 2010; Borland, Partos, & Cummings, 2012; Borland, Partos, Yong et al., 2012). Our prospective cohort study found a nonsignificant trend for treatment to be associated with a longer duration of abstinence.
Consistent with prior prospective studies of self-quitters, most quit attempts were brief. We found most (79%) lasted less than a day, which is similar to that found in prior studies (Hughes et al., 2004). Whether such short quit attempts are “serious” quit attempts is debatable (Carpenter & Hughes, 2004; Hughes & Callas, 2010b). Several surveys use a duration of 24hr to define a serious quit attempt; however, some criticize this because many dependent smokers may seriously attempt to quit but not be able to abstain for 24hr (Carpenter & Hughes, 2004). Another implication of our finding lapses occur soon after the quit date is that it suggests most treatment should be scheduled very soon after the quit date and, in fact, a recent study found better outcomes with such front-loaded treatment (Garvey et al., 2012).
Most smokers who lapsed transitioned immediately to daily smoking (i.e., median lapse to relapse was one day). In contrast, prior reports of lapse to relapse transitions have reported mean lapse to relapse times of 6–40 days (Brandon et al., 1990; Hughes et al., 1981; Shiffman et al., 2006). This discrepancy may be because the prior reports were of treatment-seeking smokers receiving intensive treatment or because they did not include brief quit attempts.
Accuracy of Recall of Quit Attempts
Prior reports have used cross-sectional analyses to suggest most quit attempts are forgotten, especially brief quit attempts (Berg et al., 2010; Borland, Partos, & Cummings, 2012; Gilpin & Pierce, 1994). Our study provided a more direct test and replicated these results, with an especially large difference in failed recall of extended versus brief quit attempts (40% vs. 3%). One prior analysis suggested recall over 3- to 4-month periods might be accurate (Gilpin & Pierce, 1994); our results are concordant with that estimate in that only 3% of those who made one or more extended quit attempts over the three months reported no such quit attempts; however, the generalizability of this finding is limited by the possibility that the daily reporting of smoking status increased the accuracy of recall.
SUMMARY
Our results replicate prior findings that smoking cessation attempts in real-world settings often produces a complex back and forth pattern of quit attempts, initial abstinence, lapse, relapse, and reduction, and that attempts to quit often continue after the first relapse. Thus, our results suggest that treatment efforts that continue for several weeks after a lapse or relapse may be more effective. We believe future descriptions of the cessation process should not stop at the first lapses/relapses, but rather continue to measure smoking change attempts. Our results also suggest many quit attempts are unplanned and of very brief duration, and thus, treatment systems that allow treatments to be applied very quickly (e.g., by mobile phone) need to be developed.
Our results contradicted several results from large, population-based surveys (e.g., success of planned vs. unplanned quit attempts and rapidity of relapse). Because our study used a small sample and had a brief follow-up, prospective replication tests of our results are needed.
Finally, our study illustrates the feasibility of collecting day-by-day data for long periods using IVR technology and the resultant rich database. Such studies can provide prospective, rather than retrospective, predictions and, thus, may produce more valid results.
FUNDING
This study was funded by U.S. National Institute on Drug Abuse (DA-025089).
DECLARATION OF INTERESTS
JH has received grants and consulting fees from many for-profit and nonprofit companies that develop or sell smoking cessation products and services or engage in tobacco control education or advocacy.
ACKNOWLEDGMENTS
We thank Emily Casey, Ginger Cloud, Miki Dash, Tonya Ferraro, Matthew MacKinnon, Sharon Muellers, Adam Rhodes-Rogan, and Beth Walsh for their help in the conduct of the study, and Ron Borland and Saul Shiffman for comments on our report. The study was registered at www.clinicaltrials.gov, NCT # 00995644.
REFERENCES
- Anthonisen N. R., Connett J. E., Kiley J. P., Altose M. D., Bailey W. C., Buist A. S, … Wise A. (1994). Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health Study. Journal of the American Medical Association, 272, 1497–1505. 10.1001/jama.1994.03520190043033 [PubMed] [Google Scholar]
- Berg C. J., An L. C., Kirch M., Guo H., Thomas J. L., Patten C. A, … West R. (2010). Failure to report attempts to quit smoking. Addictive Behaviors, 35, 900–904. 10.1016/j.addbeh.2010.06.009 [DOI] [PubMed] [Google Scholar]
- Borland R., Partos T. R., Cummings K. M. (2012). Systematic biases in cross-sectional community studies may underestimate the effectiveness of stop-smoking medications. Nicotine & Tobacco Research, 14, 1483–1487. 10.1093/ntr/nts002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borland R., Partos T. R., Yong H. H., Cummings K. M., Hyland A. (2012). How much unsuccessful quitting activity is going on among adult smokers? Data from the International Tobacco Control Four Country cohort survey. Addiction, 107, 673–682. 10.1111/j.1360-0443.2011.03685.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon T. H., Tiffany S. T., Obremski K. M., Baker T. B. (1990). Postcessation cigarette use: The process of relapse. Addictive Behaviors, 15, 105–114. 10.1016/0306-4603(90)90013-N [DOI] [PubMed] [Google Scholar]
- Carpenter M. J., Alberg A. J., Gray K. M., Saladin M. E. (2010). Motivating the unmotivated for health behavior change: A randomized trial of cessation induction for smokers. Clinical Trials, 7, 157–166. 10.1177/1740774510361533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter M. J., Hughes J. R. (2004). Defining quit attempts: What difference does a day make? Addiction, 100, 257–259 Retrieved from www.addictionjournal.org/ [DOI] [PubMed] [Google Scholar]
- Carpenter M. J., Hughes J. R., Gray K. M., Wahlquist A. E., Saladin M. E., Alberg A. J. (2011). Nicotine therapy sampling to induce quit attempts among smokers unmotivated to quit: A randomized clinical trial. Archives of Internal Medicine, 171, 1901–1907. 10.1001/archinternmed.2011.492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter M. J., Hughes J. R., Solomon L. J., Callas P. W. (2004). Both smoking reduction with nicotine replacement therapy and motivational advice increase future cessation among smokers unmotivated to quit. Journal of Consulting and Clinical Psychology, 72, 371–381. 10.1037/0022-006X.72.3.371 [DOI] [PubMed] [Google Scholar]
- Carpenter M. J., Sterba K. R., Boatright A. S., West R. (2011). ‘Closet’ quit attempts: Prevalence, correlates and association with outcome. Addiction, 106, 2214–2220. 10.1111/j.1360-0443.2011.03538.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper J., Borland R., Yong H. H., McNeill A., Murray R. L., O’Connor R. J., Cummings M. (2010). To what extent do smokers make spontaneous quit attempts and what are the implications for smoking cessation maintenance? Findings from the International Tobacco Control Four country survey. Nicotine & Tobacco Research, 12, S51–S57. 10.1093/ntr/ntq052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corkrey R., Parkinson L. (2002). Interactive voice response: Review of studies 1989-2000. Behavior Research Methods, Instruments, & Computers, 34, 342–353. 10.3758/BF03195462 [DOI] [PubMed] [Google Scholar]
- Curry S., Marlatt G. A., Peterson A. V. J., Lutton J. (1988). Survival analysis and assessment of relapse rates. In Donovan D. M., Marlatt G. A. (Eds.), Assessment of addictive behaviors (pp. 497). New York, NY: The Guilford Press; [Google Scholar]
- Etter J. F., Sutton S. (2002). Assessing ‘stage of change’ in current and former smokers. Addiction, 97, 1171–1182. 10.1046/j.1360-0443.2002.00198.x [DOI] [PubMed] [Google Scholar]
- Ferguson S. G., Shiffman S., Gitchell J. G., Sembower M. A., West R. (2009). Unplanned quit attempts–results from a U.S. sample of smokers and ex-smokers. Nicotine & Tobacco Research, 11, 827–832. 10.1093/ntr/ntp072 [DOI] [PubMed] [Google Scholar]
- Ford D. E., Vu H. T., Anthony J. C. (2002). Marijuana use and cessation of tobacco smoking in adults from a community sample. Drug and Alcohol Dependence, 67, 243–248. 10.1016/S0378-8716(02)00066-2 [DOI] [PubMed] [Google Scholar]
- Foulds J., Gandhi K. K., Steinberg M. B., Richardson D. L., Williams J. M., Burke M. V., Rhoads G. G. (2006). Factors associated with quitting smoking at a tobacco dependence treatment clinic. American Journal of Health Behavior, 30, 400–412. 10.5993/AJHB.30.4.6 [DOI] [PubMed] [Google Scholar]
- Garvey A. J., Kalman D., Hoskinson R. A., Jr, Kinnunen T., Wadler B. M., Thomson C. C., Rosner B. (2012). Front-loaded versus weekly counseling for treatment of tobacco addiction. Nicotine & Tobacco Research,14, 578–585. 10.1093/ntr/ntr256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin E., Pierce J. P. (1994). Measuring smoking cessation: Problems with recall in the 1990 California Tobacco Survey. Cancer Epidemiology, Biomarkers & Prevention, 3, 613–617 Retrieved from http://cebp.aacrjournals.org/ [PubMed] [Google Scholar]
- Hall S. M., Havassy B. E., Wasserman D. A. (1990). Commitment to abstinence and acute stress in relapse to alcohol, opiates, and nicotine. Journal of Consulting and Clinical Psychology, 58, 175–181. 10.1037/0022-006X.58.2.175 [DOI] [PubMed] [Google Scholar]
- Hall S. M., Havassy B. E., Wasserman D. A. (1991). Effects of commitment to abstinence, positive moods, stress, and coping on relapse to cocaine use. Journal of Consulting and Clinical Psychology, 59, 526–532. 10.1037/0022-006X.59.4.526 [DOI] [PubMed] [Google Scholar]
- Hall S. M., Humfleet G. L., Reus V. I., Muñoz R. F., Cullen J. (2004). Extended nortriptyline and psychological treatment for cigarette smoking. American Journal of Psychiatry, 161, 2100–2107. 10.1176/appi.ajp.161.11.2100 [DOI] [PubMed] [Google Scholar]
- Hughes G. H., Hymowitz N., Ockene J. K., Simon N., Vogt T. M. (1981). The multiple risk factor intervention trial (MRFIT). V. Intervention on smoking. Preventive Medicine, 10, 476–500. 10.1016/0091-7435(81)90061-X [DOI] [PubMed] [Google Scholar]
- Hughes J. R., Callas P. W. (2010a). Data to assess the generalizability of samples from studies of adult smokers. Nicotine & Tobacco Research, 12, 73–76. 10.1093/ntr/ntp168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R., Callas P. W. (2010b). Definition of a quit attempt: A replication test. Nicotine & Tobacco Research, 12, 1176–1179. 10.1093/ntr/ntq165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R., Callas P. W. (2011). Is delaying a quit attempt associated with less success? Nicotine & Tobacco Research, 13, 1228–1232. 10.1093/ntr/ntr207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R., Keely J. P., Fagerström K.-O., Callas P. W. (2005). Intentions to quit smoking change over short periods of time. Addictive Behaviors, 30, 653–662. 10.1016/j.addbeh.2004.08.011 [DOI] [PubMed] [Google Scholar]
- Hughes J. R., Keely J. P., Niaura R. S., Ossip-Klein D. J., Richmond R. L., Swan G. E. (2003). Measures of abstinence in clinical trials: Issues and recommendations. Nicotine & Tobacco Research, 5, 13–25. 10.1080/1462220031000070552 [PubMed] [Google Scholar]
- Hughes J. R., Keely J., Naud S. (2004). Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction, 99, 29–38. 10.1111/j.1360-0443.2004.00540.x [DOI] [PubMed] [Google Scholar]
- Hughes J. R., Peters E. N., Naud S. (2011). Effectiveness of over-the-counter nicotine replacement therapy: A qualitative review of nonrandomized trials. Nicotine & Tobacco Research, 13, 512–522. 10.1093/ntr/ntr055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes J. R., Solomon L. J., Fingar J. R., Naud S., Helzer J. E., Callas P. W. (2013). The natural history of efforts to stop smoking: A prospective cohort study. Drug and Alcohol Dependence, 128, 171–174. 10.1016/j.drugalcdep.2012.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph A. M., Rice K., An L. C., Mohiuddin A., Lando H. (2004). Recent quitters’ interest in recycling and harm reduction. Nicotine & Tobacco Research, 6, 1075–1077. 10.1080/14622200412331324893 [DOI] [PubMed] [Google Scholar]
- King B., Dube S., Kaufmann R., Shaw L., Pechacek T. (2011). Vital signs: Current cigarette smoking among adults aged >18 years - United States, 2005–2010. Morbidity and Mortality Weekly Report, 60, 1207–1211 Retrieved from www.cdc.gov/mmwr/ [PubMed] [Google Scholar]
- Klingemann H., Sobell L., Barker J., Blomqvist J., Cloud W., Ellinstad T, … Tucker J. (2001). Promoting self-change from problem substance use: Practical implications for policy, prevention and treatment. Dordrecht, the Netherlands: Kluwer Academic Publications [Google Scholar]
- Korotitsch W. J., Nelson-Gray R. O. (1999). An overview of self-monitoring research in assessment and treatment. Psychological Assessment, 11, 415–425. 10.1037/1040-3590.11.4.415 [Google Scholar]
- Larabie L. C. (2005). To what extent do smokers plan quit attempts? Tobacco Control, 14, 425–428. 10.1136/tc.2005.013615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malarcher A., Dube S., Shaw L., Babb S., Kaufmann R. (2011). Quitting smoking among adults—United States, 2001–2010. Morbidity and Mortality Weekly Report, 60, 1513–1519 Retrieved from www.cdc.gov/mmwr/ [PubMed] [Google Scholar]
- Mooney M. E., Leventhal A. M., Hatsukami D. K. (2006). Attitudes and knowledge about nicotine and nicotine replacement therapy. Nicotine & Tobacco Research, 8, 435–446. 10.1080/14622200600670397 [DOI] [PubMed] [Google Scholar]
- Murray R. L., McNeill A., Lewis S., Britton J., Coleman T. (2010). Unplanned attempts to quit smoking: A qualitative exploration. Addiction, 105, 1299–1302. 10.1111/j.1360-0443.2010.02980.x [DOI] [PubMed] [Google Scholar]
- Partin M. R., An L. C., Nelson D. B., Nugent S., Snyder A., Fu S. S, … Joseph A. M. (2006). Randomized trial of an intervention to facilitate recycling for relapsed smokers. American Journal of Preventive Medicine, 31, 293–299. 10.1016/j.amepre.2006.06.021 [DOI] [PubMed] [Google Scholar]
- Partos T. R., Borland R., Yong H. H., Hyland A., Cummings K. M. (2013). The quitting rollercoaster: How recent quitting history affects future cessation outcomes (data from the International Tobacco Control 4-country cohort study). Nicotine & Tobacco Research, 15, 1578–1587. 10.1093/ntr/ntt025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters E. N., Hughes J. R. (2009). The day-to-day process of stopping or reducing smoking: A prospective study of self-changers. Nicotine & Tobacco Research, 11, 1083–1092. 10.1093/ntr/ntp105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska J. O., DiClemente C. C., Norcross J. C. (1992). In search of how people change. Applications to addictive behaviors. The American Psychologist, 47, 1102–1114. 10.1037/0003-066X.47.9.1102 [DOI] [PubMed] [Google Scholar]
- Prochaska J. O., Velicer W. F., DiClemente C. C., Fava J. (1988). Measuring processes of change: Applications to the cessation of smoking. Journal of Consulting and Clinical Psychology, 56, 520–528. 10.1037/0022-006X.56.4.520 [DOI] [PubMed] [Google Scholar]
- Sendzik T., McDonald P. W., Brown K. S., Hammond D., Ferrence R. (2011). Planned quit attempts among Ontario smokers: Impact on abstinence. Addiction, 106, 2005–2013. 10.111/j.1360-0443.2011.03498.x [DOI] [PubMed] [Google Scholar]
- Sheffer C. E., Stitzer M., Payne T. J., Applegate B. W., Bourne D., Wheeler J. G. (2009). Treatment for tobacco dependence for rural, lower-income smokers: Outcomes, predictors, and measurement considerations. American Journal of Health Promotion, 23, 328–338. 10.4278/ajhp.06031933 [DOI] [PubMed] [Google Scholar]
- Shiffman S. (2009). How many cigarettes did you smoke? Assessing cigarette consumption by global report, Time-Line Follow-Back, and ecological momentary assessment. Health Psychology, 28, 519–526. 10.1037/a0005197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Brockwell S. E., Pillitteri J. L., Gitchell J. G. (2008). Use of smoking-cessation treatments in the United States. American Journal of Preventive Medicine, 34, 102–111. 10.1016/j.amepre.2007.09.033 [DOI] [PubMed] [Google Scholar]
- Shiffman S., Scharf D. M., Shadel W. G., Gwaltney C. J., Dang Q., Paton S. M, … Clark D. B. (2006). Analyzing milestones in smoking cessation: Illustration in a nicotine patch trial in adult smokers. Journal of Consulting and Clinical Psychology, 74, 276–285. 10.1037/0022-006X.74.2.276 [DOI] [PubMed] [Google Scholar]
- Smith S. S., Jorenby D. E., Fiore M. C., Anderson J. E., Mielke M. M., Beach K. E, … Baker T. B. (2001). Strike while the iron is hot: Can stepped-care treatments resurrect relapsing smokers? Journal of Consulting and Clinical Psychology, 69, 429–439. 10.1037//0022-006X.69.3.429 [DOI] [PubMed] [Google Scholar]
- SRNT Subcommittee on Biochemical Verification. (2002). Biochemical verification of tobacco use and cessation. Nicotine & Tobacco Research, 4, 149–159. 10.1080/14622200210123581 [DOI] [PubMed] [Google Scholar]
- Stapleton J. A., Russell M. A., Feyerabend C., Wiseman S. M., Gustavsson G., Sawe U, … Wiseman D.(1995). Dose effects and predictors of outcome in a randomized trial of transdermal nicotine patches in general practice. Addiction, 90, 31–42. 10.1111/j.1360-0443.1995.tb01007.x [DOI] [PubMed] [Google Scholar]
- West R., Sohal T. (2006). “Catastrophic” pathways to smoking cessation: Findings from national survey. British Medical Journal, 332, 458–460. 10.1136/bmj.38723.573866.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wewers M. E., Stillman F. A., Hartman A. M., Shopland D. R. (2003). Distribution of daily smokers by stage of change: Current Population Survey results. Preventive Medicine, 36, 710–720. 10.1016/S0091-7435(03)00044-6 [DOI] [PubMed] [Google Scholar]