Abstract
Here, we constructed a Yersinia pseudotuberculosis mutant strain with arabinose-dependent regulated and delayed shutoff of crp expression (araC PBAD crp) and replacement of the msbB gene with the Escherichia coli msbB gene to attenuate it. Then, we inserted the asd mutation into this construction to form χ10057 [Δasd-206 ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp] for use with a balanced-lethal Asd-positive (Asd+) plasmid to facilitate antigen synthesis. A hybrid protein composed of YopE (amino acids [aa]1 to 138) fused with full-length LcrV (YopENt138-LcrV) was synthesized in χ10057 harboring an Asd+ plasmid (pYA5199, yopENt138-lcrV) and could be secreted through a type III secretion system (T3SS) in vitro and in vivo. Animal studies indicated that mice orally immunized with χ10057(pYA5199) developed titers of IgG response to whole-cell lysates of Y. pestis (YpL) and subunit LcrV similar to those seen with χ10057(pYA3332) (χ10057 plus an empty plasmid). However, only immunization of mice with χ10057(pYA5199) resulted in a significant secretory IgA response to LcrV. χ10057(pYA5199) induced a higher level of protection (80% survival) against intranasal (i.n.) challenge with ∼240 median lethal doses (LD50) (2.4 × 104 CFU) of Y. pestis KIM6+(pCD1Ap) than χ10057(pYA3332) (40% survival). Splenocytes from mice vaccinated with χ10057(pYA5199) produced significant levels of gamma interferon (IFN-γ), tumor necrosis factor alpha (TNF-α), and interleukin-17 (IL-17) after restimulation with LcrV and YpL antigens. Our results suggest that it is possible to use an attenuated Y. pseudotuberculosis strain delivering the LcrV antigen via the T3SS as a potential vaccine candidate against pneumonic plague.
INTRODUCTION
Yersinia pestis, the etiologic agent causing plague, has been responsible for high mortality in several epidemics throughout human history and remains a current threat as a potential biological-warfare agent (1, 2). Currently, about 2,000 global cases of plague are reported to the World Health Organization each year (3). Most of these cases are of the bubonic form, usually a consequence of the transmission of bacteria to humans via bites from fleas that had previously fed on infected rodents, while contact with domestic cats that had been exposed to Y. pestis is another important transmission mode because of the higher-than-average incidence of pneumonic plague that occurs in these cases (1). Additionally, there has been an emergence of a Y. pestis strain resistant to eight antibiotics, which is a great public health concern (4–6). Therefore, prophylactic vaccination against this disease holds the brightest prospect for its control in the long term, but no safe and efficient vaccines against plague are currently available.
The live EV76 vaccine is an apparent pgm mutant that has been used in some countries in the past (7). However, a concern is that the EV76 vaccine strain can cause disease in primates, thus raising questions about its suitability as a human vaccine (8). Wang et al. summarized the latest progress in live attenuated Y. pestis vaccine development (9). In addition, live bacteria, such as Salmonella species, Escherichia coli, or Lactococcus lactis, or live viruses, such as replication-deficient adenovirus, vesicular stomatitis virus, vaccinia virus, or raccoon poxvirus, have been used as vectors for the effective delivery of F1 and/or V antigen to induce protective immunity to plague (10, 11). Recently, the main focus of plague vaccine research has been to develop subunit vaccines, in particular, those targeting LcrV and F1 antigens, which were found to efficiently protect rodent and cynomolgus macaque against bubonic and pneumonic plague and are well tolerated in humans (12–20). However, the subunit vaccine had insufficient and highly variable protection against plague in African green monkeys (20, 21). Additionally, the usefulness of F1 as a protective antigen is not clear, since F1− strains can cause plague (22). Therefore, vaccines composed of a limited number of antigens (F1 and/or LcrV) may not be able to protect against F1-negative strains (22) or strains harboring LcrV variants (23). Live Yersinia vaccines offer several advantages over recombinant vaccines. Their high antigenic complexity guarantees a response to a broad range of antigenic targets. Additionally, they are often less expensive to manufacture than subunit vaccines (10). Thus, plague vaccines based on live attenuated Yersinia spp. provide the theoretical advantage of simultaneously priming immunity responses to many antigens, thereby reducing the likelihood of antigen circumvention by clever terrorists (24).
Y. pseudotuberculosis is thought to be the direct evolutionary ancestor of Y. pestis (25–27). The two species diverged from one another 2,600 to 28,000 years ago (27–29). But Y. pseudotuberculosis is much less virulent and typically causes enteric disease in humans and animals. Its infections are self-limiting with a low case fatality rate, and its lifestyle as an enteric pathogen will facilitate its use as an oral vaccine. With the exception of two additional plasmids (pPCP1 and pMT1) carried by Y. pestis, the two species share >95% genetic identity and a common virulence plasmid with a conserved colinear backbone (30). BLAST analysis of several major Y. pestis antigens showed that LcrV shares 96% amino acid identity between the two species and that Psn and YadC, two additional antigens shown to be protective against Y. pestis challenge (31–33), share 100% homology (34) and >97% homology (35), respectively. Furthermore, Y. pseudotuberculosis has a much lower number of insertion sequence (IS) copies than Y. pestis and so is genetically much more stable than the latter (30).
Oral immunization with attenuated Y. pseudotuberculosis strains provides partial protection against pulmonary challenge with Y. pestis (36–38). Recently, Derbise et al. reported that a single oral immunization of the encapsulated Y. pseudotuberculosis V674pF1 strain offered great protection against a lethal pneumonic plague challenge (39). Therefore, these data demonstrated the feasibility of using modified Y. pseudotuberculosis strains to control plague transmission and induction of mortality.
Previous studies suggest that Y. pseudotuberculosis is a promising candidate for an oral live carrier vaccine, capable of stimulating antigen specific CD8+ T-cell responses (40, 41). Additionally, delivery of heterologous antigens by the type III secretion system (T3SS) in Y. pseudotuberculosis and Salmonella stimulated antigen-specific cytotoxic T-cell responses, antigen-specific CD8+ memory T cells, and protection against challenge with different pathogens (40, 42, 43). Studies have indicated that both humoral immunity and cellular immunity contribute to vaccine efficacy against plague (21, 24, 44–47). CD8+ T-cell immune responses primed to LcrV appear to confer protection against Y. pestis in mice (48, 49). Studies demonstrated that Chinese-origin rhesus macaques immunized with EV76 or mice immunized with the Y. pestis ΔsmpB-ssrA mutant primed a higher anti-F1 IgG titer but an almost undetectable titer with respect to LcrV antigen (38, 50), results that are consistent with other studies of animals immunized with the EV76 or KWC vaccine (51–57). Mice vaccinated with Y. pestis KIM5 (lacking pgm) generated the CD4 and CD8 T cells that synergistically conferred protection against plague, but T cells from those vaccinated mice could not recognize LcrV (47). Patients who had recovered from plague also barely produced memory T-cell responses to LcrV antigens (58). Pettersson et al. analyzed the localization of LcrV during infection of HeLa cells and were unable to detect any LcrV in the cytosol of the cells (59), but Nilles et al. showed that small amounts of LcrV entered HeLa cells and suggested that this translocation appears to not result from injection via the T3SS (60). So, on the basis of these findings, we hypothesize that a live attenuated Y. pseudotuberculosis strain used as a vector to inject the LcrV antigen via the T3SS might prime both antibody responses and specific T-cell responses to LcrV, resulting in enhanced protective immunity to pneumonic plague. In this study, we demonstrated that oral immunization with χ10057(pYA5199) delivering LcrV via the T3SS primed an IgA response to LcrV and specific cellular responses to both LcrV and YpL and provided significant protection against pneumonic plague.
MATERIALS AND METHODS
Media and reagents.
Tryptone, yeast extract, tryptose blood agar (TBA), and heart infusion broth (HIB) were from Difco. 2,6-Diaminopimelic acid (DAP) and l-arabinose were from Sigma (St. Louis, MO). Oligonucleotides were from IDT (Coralville, IA). Restriction endonucleases were from New England BioLabs (Ipswich, MA). Taq DNA polymerase (New England BioLabs) was used in all PCR tests. Vent DNA polymerase (New England BioLabs) was used to amplify fragments for cloning. T4 ligase was from Promega (San Luis Obispo, CA). Qiagen products (Hilden, Germany) were used to isolate plasmid DNA, gel-purify fragments, and purify PCR products.
Bacterial strains, plasmids, and culture conditions.
All bacterial strains and plasmids used in this study are listed in Table 1. All strains were stored at −70°C in peptone-glycerol. Escherichia coli χ6212 was used as an intermediate host for cloning procedures and grown routinely at 37°C in LB broth (67) or on LB solidified with 1.2% Bacto agar (Difco). The Y. pseudotuberculosis PB1+ strain provided by Robert Perry (University of Kentucky) and used in this study was grown in LB medium at 27°C. When required, chloramphenicol (Cm; 50 μg/ml), arabinose (0.1%), or 2,6-diaminopimelic acid (DAP; 15 μg/ml) was added. TBA containing 5% sucrose was used for sacB gene-based counterselection in allelic-exchange experiments. Y. pestis KIM6+(pCD1Ap) was used for challenge studies as previously reported (68). Y. pestis cells were grown routinely on Congo red agar from peptone-glycerol stocks and in HIB at 28°C (69). HIB Congo red agar plates were used to confirm the pigmentation (Pgm) phenotype of Y. pestis strains (63).
TABLE 1.
Strains and plasmids used in this study
| Strain or plasmid | Description or relevant characteristics | Source, derivation, or reference |
|---|---|---|
| Strains | ||
| E. coli χ6212 | F− λ− ϕ80 Δ(lacZYA-argF) endA1 recA1 hsdR17 deoR thi-1 glnV44 gyrA96 relA1 ΔasdA4 | 61 |
| E. coli χ7213 | thi-1 thr-1 leuB6 fhuA21 lacY1 glnV44 ΔasdA4 recA1 RP4 2-Tc::Mu [λpir]; Kmr | 62 |
| Y. pestis KIM6+ | Pgm+, pMT1, pPCP1, pCD1 | Robert Perry |
| Y. pestis KIM6+(pCD1Ap) | Pgm+, pMT1, pPCP1, pCD1Ap | 63 |
| Y. pestis KIM6 (pCD1Ap) | Pgm−, pMT1, pPCP1, pCD1Ap | Robert Perry |
| Y. pestis χ10006 | Δasd Y. pestis KIM6+ | This study |
| Y. pseudotuberculosis PB1+ | Serotype O:1B | Robert Perry |
| Y. pseudotuberculosis χ10052 | ΔmsbB868 | Y. pseudotuberculosis PB1+ |
| Y. pseudotuberculosis χ10053 | ΔmsbB868::PmsbB msbB (EC) | Y. pseudotuberculosis χ10052 |
| Y. pseudotuberculosis χ10054 | ΔPcrp21::TT araC PBAD crp | Y. pseudotuberculosis PB1+ |
| Y. pseudotuberculosis χ10055 | ΔmsbB868::PmsbB msbB (EC) ΔPcrp21::TT araC PBAD crp | Y. pseudotuberculosis χ10053 |
| Y. pseudotuberculosis χ10056 | Δasd206 ΔPcrp21::TT araC PBAD crp | Y. pseudotuberculosis χ10055 |
| Y. pseudotuberculosis χ10057 | Δasd206 ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp | This study |
| Plasmids | ||
| pRE112 | Suicide vector, Cmr, mob− (RP4)R6K ori, sacB | 64 |
| pYA3332 | Asd+; p15A ori | 65 |
| pYA4581 | SD-crp and y3957′ fragments cloned into XhoI/EcoRI sites and PstI/HindIII sites of pYA3700 | 66 |
| pYA5151 | The flanking regions of ΔmsbB of Y. pseudotuberculosis cloned into PstI sites of pRE112 | This study |
| pYA5152 | The fragment of ΔmsbB::PmsbB(EC) msbB(EC) cloned into PstI sites of pRE112 | This study |
| pYA5153 | The fragment of ΔPcrp::TT araC PBAD crp from pYA4581 cloned into XmaI and KpnI sites of pRE112 | This study |
| pYA5154 | The flanking regions of Δasd of Y. pseudotuberculosis cloned into XmaI and KpnI sites of pRE112 | This study |
| pYA5199 | The sycE-yopE′ (aa 1–138)-lcrV fragment was cloned into pYA3332 | This study |
| pYA5203 | The sycE-yopE′ (aa 1–138)-lcrV fragment and caf operon were cloned into pYA3332 | This study |
Cm, chloramphenicol; Km, kanamycin.
Construction of plasmids.
All primers used in this study are listed in Table 2. The sycE-yopE (amino acids [aa] 1 to 138) (designated sycE-yopENt138) gene fragment was amplified from Y. pestis using primers 1 and 2. The full-length lcrV gene was amplified from Y. pestis using primers 3 and 4. Then, the sycE-yopENt138 gene fragment was fused with the full-length lcrV through overlapping PCR using primers 1 and 4. The fused fragment, sycE-yopENt138-lcrV, was cloned into BspEI and HindIII sites of pYA3332 (p15A ori) to form plasmid pYA5199 (yopENt138-lcrV), which specifies synthesis of YopENt138-LcrV.
TABLE 2.
Primers used in this work
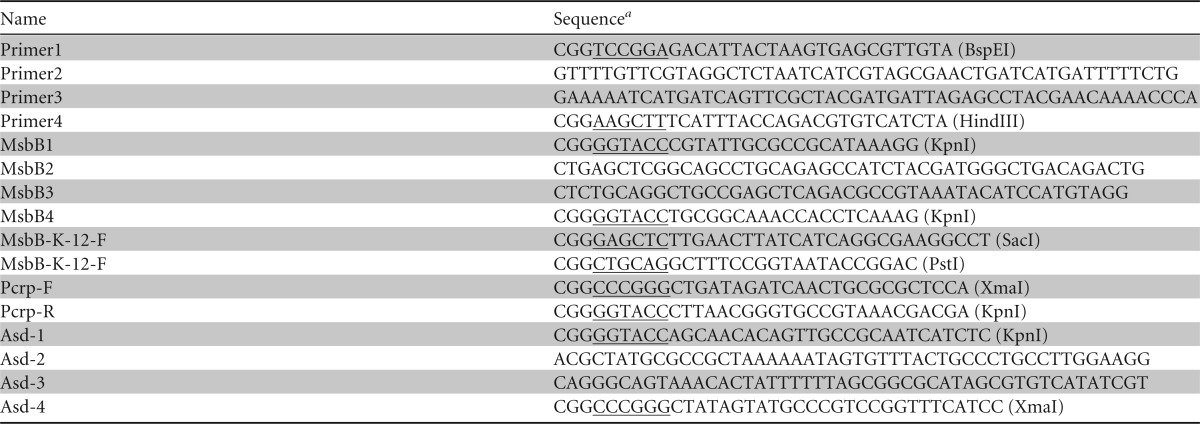
Underlined sequence characters represent the restriction endonuclease sites.
For construction of suicide vectors, primers MsbB1 and MsbB2 and primers MsbB3 and MsbB4 (Table 2) were used for amplifying flanking regions of the msbB gene from Y. pseudotuberculosis PB1/+, respectively. Then, the DNA fragment containing the ΔmsbB was amplified using primers MsbB1 and MsbB4 through overlapping PCR. The fused DNA segment (ΔmsbB) was ligated into the KpnI site of pRE112 to form plasmid pYA5151. In order to replace the msbB gene of Y. pseudotuberculosis PB1/+ by the msbB gene of E. coli K-12, the msbB gene with its native promoter of E. coli K-12 [PmsbB (EC) msbB(EC)] was amplified using primers MsbB-K-12-F and MsbB-K-12-R (Table 2). The segment of PmsbB (EC) msbB(EC) was cloned into the PstI and SacI sites between the flanking regions of ΔmsbB in pYA5151 to form plasmid pYA5152. The segment of ΔPcrp::TT araC PBAD crp was amplified from plasmid pYA4581 (66) using primers Pcrp-F and Pcrp-R (Table 2) and cloned into the KpnI and XmaI sites of pRE112 to form plasmid pYA5153. To delete the asd gene (YPTS_3990) from Y. pseudotuberculosis PB1/+, primers Asd1 and Asd2 and primers Asd3 and Asd4 (Table 2) were used for amplifying flanking regions of the Δasd gene, respectively. Then, the DNA fragment containing the Δasd was amplified using primers Asd1 and Asd4 through overlapping PCR. The fused flanking region (Δasd) was ligated into the KpnI and XmaI sites of pRE112 to form plasmid pYA5154. All the plasmid constructions were verified through sequencing.
Construction of Y. pseudotuberculosis mutants.
To replace the msbB(Ypt) gene with msbB(EC), a Y. pseudotuberculosis ΔmsbB868 mutation, which encompassed a 1,295-bp deletion from the 162 bp before the ATG start codon to 170 bp behind the TAG stop codon of msbB, was constructed. The suicide plasmid pYA5151 (ΔmsbB) was conjugationally transferred from E. coli χ7213 (62) to the Y. pseudotuberculosis PB1/+ wild-type strain. Single-crossover insertion strains were isolated on TBA agar plates containing Cm. Loss of the suicide vector after the second recombination between homologous regions (i.e., allelic exchange) was selected by using the sacB-based sucrose sensitivity counterselection system (70). The colonies were screened for Cms and verified by PCR using primers MsbB1 and MsbB4. The mutant strain was designated χ10052 (ΔmsbB868). Then, χ10052 was conjugated with χ7213 harboring the pYA5152 suicide plasmid [ΔmsbB::PmsbB (EC) msbB(EC)] to transfer ΔmsbB868::PmsbB (EC) msbB(EC) into χ10052. Through same screening procedure, mutant strain χ10053 [ΔmsbB868::PmsbB (EC) msbB(EC)] was confirmed. Then, ΔPcrp21::TT araC PBAD crp was introduced into χ10053 through same procedure to construct mutant strain χ10055 [ΔPcrp21::TT araC PBAD crp ΔmsbB868::PmsbB (EC) msbB(EC)]. Finally, the ΔasdA206-defined deletion was introduced into χ10055 through conjugation of χ7213(pYA5154) (ΔasdA206) with χ10055 to form χ10057. The colonies were confirmed for Cms and for growth only in the presence of DAP and by PCR using primer set Asd1 and Asd4. All the mutant strains were confirmed by DNA sequence analysis.
Analysis of synthesis and secretion of the recombinant proteins.
To analyze the production and secretion of the chimeric proteins through the T3SS, secreted proteins were prepared by using modifications of previously described methods (71). Cultures of Y. pseudotuberculosis χ10057 harboring pYA5199 (yopENt138-lcrV) or pYA3332 (empty plasmid) were grown overnight in LB broth supplemented with 0.05% arabinose at 26°C and subcultured into calcium-chelated medium (1% tryptone, 0.5% yeast extract, 50 mM MOPS [morpholinepropanesulfonic acid; pH 7.0], 16 mM sodium oxalate, 160 mM magnesium chloride). Cultures were incubated for 6 h at 37°C on a roller drum to provide mild aeration. The optical density at 600 nm (OD600) of cultures was measured, and bacterial cell pellets were collected by centrifugation. The pellets were suspended in SDS loading buffer. The volume of sample buffer was adjusted based on the OD600 to normalize the amount loaded on an SDS-PAGE gel. Whole bacterial cells were lysed by heating at 95°C for 5 min. Culture supernatants were concentrated by precipitation with 10% (wt/vol) trichloroacetic acid overnight at 4°C and collected by centrifugation. Pellets were washed with ice-cold acetone and dissolved in 0.05 M Tris-HCl buffer (pH 9.5). Samples were heated at 95°C for 5 min, separated by SDS-PAGE, and blotted onto nitrocellulose membranes. The membranes were probed with rabbit anti-LcrV antibodies as described previously (31).
Translocation of fusion protein YopENt138-LcrV.
The translocation assays were conducted according to procedures described previously (72) with minor modifications. Briefly, HeLa cells (5 × 105) were seeded into 100-mm-diameter tissue culture dishes in Dulbecco modified Eagle medium (DMEM) supplemented with 10% fetal bovine serum and grown to 80% to 90% confluence. Prior to infection, the cells were washed twice with 5 ml of Dulbecco's phosphate-buffered saline (DPBS). Antibiotic-free medium containing 0.5 μg/ml cytochalasin D was added. Overnight bacterial cultures were diluted 1:20 in HIB and incubated for 30 min at 26°C followed by 1 h at 37°C. HeLa cells were infected with the bacteria at a multiplicity of infection (MOI) of 50 for 4 h at 37°C. Subsequently, the culture medium was removed, and the cells were washed three times with 10 ml DPBS. The HeLa cells were treated with 10 μg/ml proteinase K–DPBS for 15 min at 37°C to digest secreted but not translocated bacterial protein. Afterward, 3 ml of chilled HBSS containing 2 mM phenylmethylsulfonyl fluoride (Sigma) was added. Cells detached during the proteinase K treatment and were subsequently collected by low-speed centrifugation (600 × g for 10 min) and lysed in 1 ml of DPBS containing 0.1% Triton X-100, 10 μg/ml DNase, 10 μg/ml RNase, 1 mM phenylmethylsulfonyl fluoride (PMSF), 0.1% (vol/vol) protease inhibitor (P-8340), and 0.01% (vol/vol) phosphatase inhibitor (P-2850) cocktails (Sigma-Aldrich) and then incubated for 15 min at 4°C. Then, the cell lysates were centrifuged at 12,500 × g for 30 min at 4°C, and the pellets (P) obtained, containing the unbroken cells, membranes, and bacteria that had adhered and had been internalized, were resuspended in 200 μl of LDS sample buffer (Pierce ECL, Rockford, IL). The supernatant of the cytoplasmic fraction (C) containing the eukaryotic cytoplasm and the translocated recombinant proteins was filtered through a 0.22-μm-pore-size syringe filter (Millipore), and the proteins were precipitated with 10% trichloroacetic acid and resuspended in 200 μl of LDS sample buffer. Samples were heated at 95°C for 5 min, separated by SDS-PAGE, and blotted onto nitrocellulose membranes. The chimeric proteins were identified using rabbit anti-LcrV antibody followed by peroxidase-conjugated goat anti-rabbit antibody (Sigma, St. Louis, MO). Bound antibodies were detected using an enhanced chemiluminescent detection system (Pierce ECL; Pierce, Rockford, IL).
Animal experiments.
Six-week-old female Swiss Webster mice were purchased from Charles River Laboratories (Wilmington, MA). All animal procedures were approved by the Arizona State University Animal Care and Use Committee. Mice were acclimated for 1 week after arrival and deprived of food and water for 6 h before starting experiments. The median lethal dose (LD50) of the Y. pseudotuberculosis strains in mice was determined according to previous procedures with certain modifications (73–75). Overnight cultures of bacteria were grown at 26°C in LB supplemented with 0.05% arabinose when needed. The next day, 1 ml of this culture was inoculated into 50 ml of the appropriate media and grown with aeration at 26°C to an optical density at 600 nm (OD600) of 1.0. Bacteria were harvested by centrifugation at 24°C and resuspended in 0.5 ml buffered saline solution with gelatin (BSG). Five mice per group were orally inoculated with approximately 107, 108, or 109 CFU of bacteria in 20 μl of BSG by placing a pipette tip behind the incisors of mice. Actual numbers of CFU inoculated were determined by plating serial dilutions onto LB agar. The experiment was repeated one time, and data were combined to calculate the LD50.
To evaluate colonization, 3 mice per group were euthanized on days 3, 6, and 9 after inoculation. Samples of spleen, liver, and Peyer's patches (PPs) were collected and weighed, and BSG buffer (74) was added to reach a final volume of 1 ml. Samples were homogenized and plated onto MacConkey agar supplemented with 1% lactose to determine the number of viable bacteria. The detection limit was 2 CFU. For representation in graphic and statistical analysis, log10 calculations were applied to the values, and recovery of 0 CFU was reported as 1 CFU/g. The experiment was done twice, and data were combined to calculate colonization titers.
To evaluate the immunogenicity of vaccine strains, strain χ10057 harboring plasmid pYA5199 (yopENt138-lcrV) or pYA3332 (empty plasmid) was prepared as described above. Access to food and water was restricted for 6 h, and then 10 mice per group were orally inoculated with 20 μl of BSG containing 1 × 109 CFU of each strain or BSG as a negative control on day 0. Blood was obtained by mandibular vein puncture at biweekly intervals, and serum samples were collected individually after centrifugation. The vaginal tract of each mouse was washed with 100 μl BSG, and the secretory IgA (sIgA) in wash fluids was analyzed individually. The immunogenicity of vaccine strains was evaluated by determining the titers of antibodies in serum or vaginal washes against LcrV (65) and Y. pestis whole-cell lysates (YpL) (76) by enzyme-linked immunosorbent assay (ELISA) as described previously (61).
Determination of protective efficacy.
A single colony of Y. pestis KIM6+(pCD1Ap) was inoculated into HIB medium supplemented with 25 μg/ml ampicillin and grown overnight at 26°C. Bacteria were diluted into 10 ml of fresh HIB enriched with 0.2% xylose and 2.5 mM CaCl2 and supplemented with 25 μg/ml ampicillin to obtain an OD620 of 0.1 and incubated at 37°C for intranasal (i.n.) infections (pneumonic plague). Cultures were grown to an OD620 of 0.6. The cells were then harvested, and the pellet was resuspended in 1 ml of isotonic PBS. Groups of Swiss Webster mice (10/group) were orally immunized with 109 CFU of χ10057 strains containing different plasmids. One group of mice (5/group) was orally vaccinated with BSG as a control. On day 35 after initial immunization, animals lightly anesthetized with a 1:5 xylazine-ketamine mixture were challenged intranasally with 1 × 104 CFU Y. pestis KIM6+(pCD1Ap)–20 μl PBS. All infected animals were observed over a 15-day period for the development of signs of plague infection.
Measurement of antibody responses.
An enzyme-linked immunosorbent assay (ELISA) was used to assay antibodies to LcrV (77) or YpL (76) in serum. Polystyrene 96-well flat-bottom microtiter plates (Dynatech Laboratories Inc., Chantilly, VA) were coated with 100 ng/well of purified rLcrV or YpL. Antigens suspended in sodium carbonate bicarbonate coating buffer (pH 9.6) were applied with 100-μl volumes in each well. The coated plates were incubated overnight at 4°C. The procedures for measuring antibody titer were described in our previous report (65). Absorbance readings that were 0.1 higher than PBS control values were considered to represent a positive result.
Analysis of T-cell activation by measuring cytokine production.
Spleens taken aseptically from euthanized animals were dissociated using cell strainers (BD Biosciences). The spleen cell suspensions were depleted of red blood cells (RBC) using RBC lysis buffer (Sigma), and splenocytes were extensively washed with cold PBS. Cells resuspended in RPMI 1640 plus GlutaMAX (Gibco) supplemented with 5% fetal bovine serum and 100 μg/ml penicillin-streptomycin were seeded in 96-well plates (1 × 106/well) and stimulated with YpL antigen (4 μg/ml), the LcrV antigen (4 μg/ml), or concanavalin A (ConA) (Sigma) (1 μg/ml) as a positive control. After 3 days, the supernatant was collected and measured for cytokine content using a multiplex assay with BioPlex (Bio-Rad).
Statistical analysis.
The log-rank test was used for analysis of the survival curves. Data are expressed as means ± standard deviations (SD). Two-way analysis of variance (ANOVA) was used for antibody titer and cytokine analysis. The Student t test was used to compare bacterial loads in challenged mouse groups. A P value of <0.05 was considered significant.
RESULTS
Construction of a live attenuated Y. pseudotuberculosis strain as a carrier for delivering antigen.
Rebeil at al. demonstrated that Y. pseudotuberculosis PB1 produces penta-acylated and C16:1-containing hexa-acylated lipid A species when grown at 21°C, while tetra-acylated lipid A and C16:0-containing penta-acylated lipid A are observed when the same strain is grown at 37°C (78). The temperature-sensitive difference in lipid A acylation results in Y. pseudotuberculosis has not yet been elucidated. Y. pseudotuberculosis contains a biochemically uncharacterized lpxL homolog that may be responsible for formation of penta-acylated lipid A at 21°C and/or 37°C. Additionally, Pérez-Gutiérrez et al. (79) have shown that the Y. enterocolitica MsbB acyltransferase is temperature sensitive and has a high (94%) degree of identity with MsbB (YPTS_2105) of Y. pseudotuberculosis. Therefore, we infer that MsbB in Y. pseudotuberculosis is temperature sensitive.
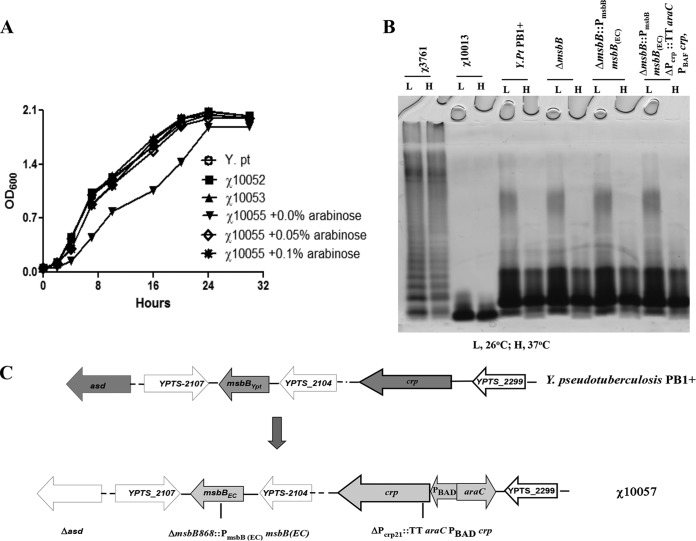
The major tetra-acylated lipid A at 37°C (mammalian host temperature) formed in Y. pestis can suppress early immune responses (80, 81). In order to overcome the immunosuppression, Y. pestis was engineered to produce hexa-acylated lipid A by expressing E. coli LpxL (68, 80). This strain was attenuated and could induce potent protective immunity to plague (68, 80). Our studies showed that combining production of hexa-acylated lipid A and regulation of Crp synthesis under the control of a araC PBAD regulon made the Y. pestis mutant more attenuated than Y. pestis with hexa-acylated lipid A alone while retaining great immunogenicity (68). Here, we used an approach to achieve Y. pseudotuberculosis attenuation similar to that described in our previous paper (68). Unlike Y. pestis, Y. pseudotuberculosis encodes a functional lpxL homolog (82). In addition, MsbB in Y. pseudotuberculosis may be temperature sensitive, resulting in major production of tetra-acylated lipid A observed in Y. pseudotuberculosis grown at 37°C and associated with immunosuppressive properties (78). Therefore, we replaced only the msbB gene and its promoter in Y. pseudotuberculosis with the E. coli msbB gene and its native promoter [ΔmsbB:: PmsbB::msbB(EC)] to drive the mutant strain to synthesize hexa-acylated lipid A at 37°C, which can be recognized by Toll-like receptor 4 (TLR4) to enhance immunostimulatory properties. We thus constructed χ10053 [ΔmsbB::PmsbB msbB(EC)]. Then, the ΔPcrp21::TT araC PBAD crp mutation was introduced into strain χ10053 to construct χ10055 [ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp] to obtain much attenuation. Measurement of bacterial growth indicated that the growth curve of the mutant strain with the ΔmsbB868 or ΔmsbB868::PmsbB msbB(EC) mutation was the same as that of the wild-type strain, while mutant strain χ10055 also containing the ΔPcrp21::TT araC PBAD crp mutation required arabinose for optimal growth (Fig. 1A).
FIG 1.
LPS phenotypes, growth curves of mutant and parent strains, and schematic diagram of strain constructions. (A) The growth curves of Y. pseudotuberculosis PB1+ (Y. pt), χ10052, χ10053, and χ10055 in LB medium supplemented with different amounts (0%, 0.05%, and 0.1%) of arabinose at 26°C. (B) LPS was visualized by the use of silver-staining polyacrylamide gel electrophoresis (PAGE) gels. The strains (from left to right) are as follows: χ3761 (Salmonella enterica serovar Typhimurium UK-1), χ10013 (ΔlpxP32 Y. pestis KIM6+), wild-type Y. pseudotuberculosis PB1+ (Y. pt PB1+), χ10052 (ΔmsbB868), χ10053 [ΔmsbB868::PmsbB msbB(EC)], and χ10055 [ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp]. All strains were cultured at 26°C and 37°C. (C) Schematic diagram depicting the chromosomal structure of χ10057 [Δasd206 ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp].
Lipopolysaccharide (LPS) synthesis of each mutant was analyzed by silver staining (Fig. 1B). The result demonstrated that there was no detectable alteration in the lipid A acylation pattern of wild-type Y. pseudotuberculosis PB1+ that was dependent on growth temperature. Surprisingly, the lipid A portion was not altered even in the msbB (YPTS_2105) mutant strain. In addition, replacing the Y. pseudotuberculosis msbB gene and its promoter with the E. coli msbB gene and its native promoter [ΔmsbB:: PmsbB::msbB(EC)] also did not cause any shifts in the migration of LPS as analyzed by silver staining (Fig. 1B). The lipid A structures of wild-type Y. pseudotuberculosis PB1+, χ10052 (ΔmsbB), χ10053 [ΔmsbB:: PmsbB::msbB(EC)], and χ10055 [ΔmsbB::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp] were further analyzed by matrix-assisted laser desorption ionization–mass spectrometry (MALDI-MS). However, as has been previously reported (78, 83), the data were extremely complex (see Fig. S1 in the supplemental material). Although MALDI-MS indicated the presence of a complex mixture of lipid A structures, we observed that all strains synthesized penta-, hexa-, and hepta-acylated lipid A species at 37°C with minor temperature-dependent variations in the proportions of the major lipid A species. Consistent with the activity of MsbB in Y. pestis, minor peaks corresponding to the proposed lauroyl (C12)-containing lipid A molecules were absent in the ΔmsbB mutant relative to the wild type. No significant changes in the acylation state were observed in the lipid A population obtained from ΔmsbB compared to ΔmsbB::PmsbB::msbB(EC) mutants (see Fig. S1).
Virulence of χ10055 determined by oral administration in Swiss Webster mice demonstrated that the LD50 of χ10055 increased at least by 102-fold (>4 × 109 CFU) compared to that of the wild-type strain (LD50 = 5 × 107 CFU). But we did not observe any changes in the virulence of χ10052 (ΔmsbB868) and χ10053 [ΔmsbB868::PmsbB::msbB(EC)] (data not shown). To facilitate antigen synthesis specified by plasmids in recombinant Y. pseudotuberculosis strains, we adapted the balanced-lethal Asd+ plasmid maintenance system developed for Salmonella (84) in Y. pseudotuberculosis. Based on the attenuated χ10055 mutant, the Δasd mutation was introduced into χ10055 to construct χ10057 [Δasd-206 ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp], which was used as a carrier for delivering antigen (Fig. 1C).
Synthesis, secretion, and translocation of recombinant chimeric YopENt138-LcrV proteins by strain χ10057.
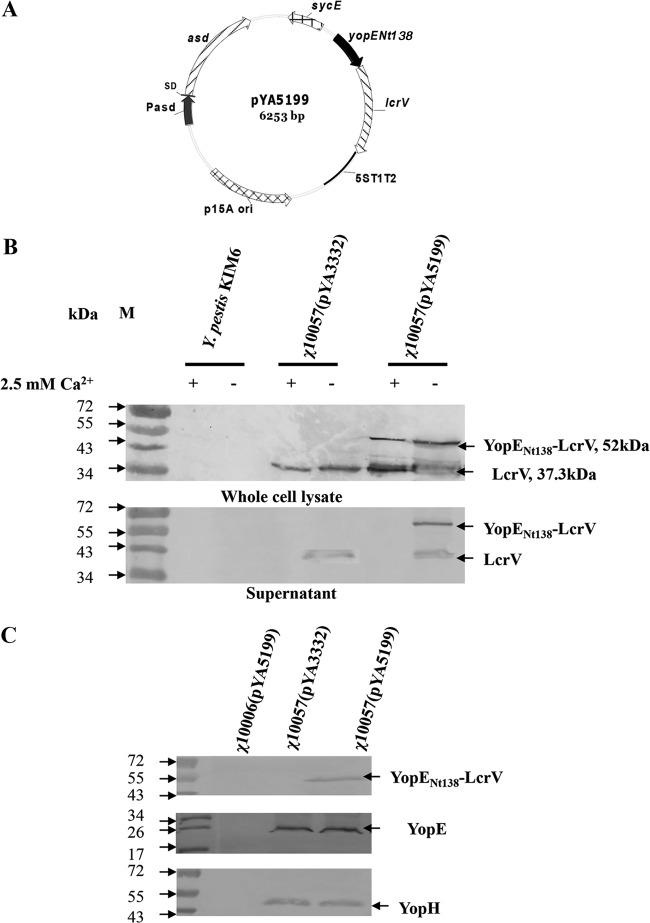
Cellular immunity plays an important role in protection against pneumonic plague (45, 46, 85–88). To stimulate cellular immunity, heterologous antigens fused with YopE (aa 1 to 138) allow the chimeric protein to be specifically transported via the T3SS of live attenuated Y. pseudotuberculosis strains to become accessible to the major histocompatibility complex (MHC) class I-restricted antigen-processing pathways and stimulate an antigen-specific cellular immune response (40, 41). Thus, we constructed plasmid vectors containing the secretion and translocation signals of the Yersinia T3SS YopE effector protein, which are specified by the first 138 amino acids in the amino-terminal region of YopE (designated YopENt138). SycE encoded by sycE is the chaperon protein for YopE and increases the translocation of YopE fusion protein (89) or YopENt138 fusion protein (43, 90). The lcrV of Y. pestis generated by in-frame fusion with sycE-yopENt138 was cloned into pYA3332 to generate pYA5199 (Fig. 2A).
FIG 2.
Synthesis, secretion, and translocation of YopENt138-LcrV in χ10057(pYA5199). (A) Physical map of pYA5199. (B) The synthesis and secretion of YopENt138-LcrV were determined in χ10057(pYA5199) by Western blotting. Y. pestis KIM6+ (no-pCD1 plasmid) was used as the negative control and χ10057(pYA3332) as the vector control. (C) Translocation of YopENt138-LcrV into the cytosol of HeLa cells infected by χ10057(pYA5199) was detected by the use of an enhanced chemiluminescent detection system. χ10006(pYA5199) (Δasd Y. pestis KIM6+) was used as the negative control and χ10057(pYA3332) as the vector control; translocation of YopE and YopH was used as the interior control.
To test secretion of the chimeric YopENt138-LcrV protein, cultures of χ10057 harboring either pYA3332 (plasmid control) or pYA5199 (yopENt138-lcrV) were grown at 26°C to an OD600 of 0.8 in LB medium with 0.05% arabinose and then subcultured into calcium-chelated medium supplemented with 0.05% arabinose for 6 h at 37°C as described in Materials and Methods. Immunoblotting was used to detect synthesis of YopENt138-LcrV fusion protein. The molecular mass of YopENt138-LcrV was 52 kDa as expected (Fig. 2B). These results demonstrated that the YopENt138-LcrV hybrid proteins were synthesized and secreted in vitro.
To analyze translocation of the hybrid proteins, HeLa cells were infected with χ10057 harboring either pYA3332 as a negative control or pYA5199 (yopENt138-lcrV). Our results demonstrated that YopENt138-LcrV was translocated into the cytosol of host cells by the Y. pseudotuberculosis mutant strain (Fig. 2C).
Virulence and persistence of recombinant strains harboring different plasmids in mice.
To investigate whether plasmids introduced into the χ10057 strain [Δasd-206 ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp] affect its virulence, we infected Swiss Webster mice orally with 4.5 × 109 CFU of χ10057(pYA3332) (vector control) or 7.0 × 109 CFU of χ10057(pYA5199) (yopENt138-lcrV). All the mice infected with χ10057 harboring different plasmids did not show any sign of weight loss or any symptoms of disease. Thus, the LD50s of χ10057(pYA3332) and χ10057(pYA5199) were more than 4.5 × 109 CFU. In addition, our results demonstrated survival of 6 of 10 mice infected with 1.5 × 107 CFU of wild-type Y. pseudotuberculosis PB1+, 4 of 10 mice infected with 1.5 × 108 CFU of Y. pseudotuberculosis PB1+, and 1 of 10 mice infected with 1.5 × 109 CFU of Y. pseudotuberculosis PB1+. Therefore, the LD50 of wild-type Y. pseudotuberculosis PB1+ was around 1.5 × 108 CFU. On the basis of these data, we evaluated the ability of the χ10057 strain harboring different plasmids to disseminate into Peyer's patches, spleens, and livers of mice. We orally infected groups of mice with 0.7 × 109 CFU of wild-type Y. pseudotuberculosis PB1+, 1.5 × 109 CFU of χ10057(pYA3332), or 1.3 × 109 CFU of χ10057(pYA5199).
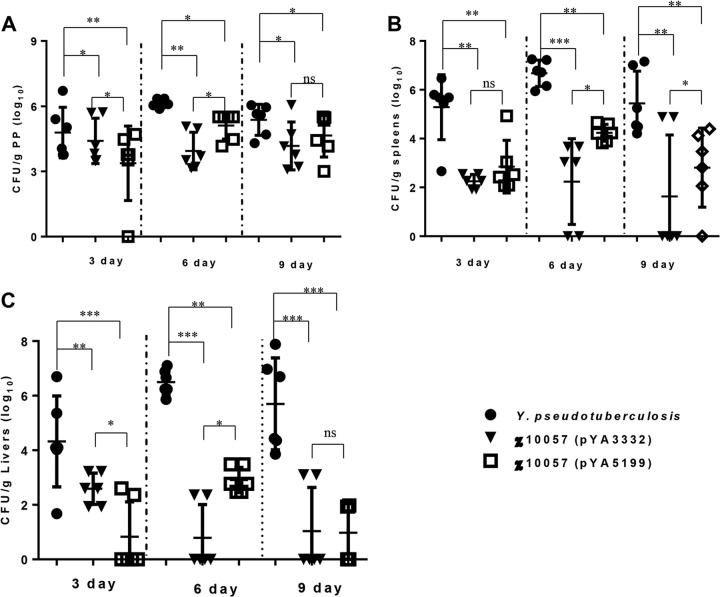
In the Peyer's patches, the titers of wild-type Y. pseudotuberculosis PB1+ strain steadily increased at 3 and 6 days postinfection and slightly declined at 9 days postinfection. The titers of χ10057(pYA3332) and χ10057(pYA5199) strains were significantly lower than that of the wild-type PB1+ strain at different time points postinfection (Fig. 3A). The bacterial titers of χ10057(pYA5199) significantly increased, while the titers of χ10057(pYA3332) decreased around 1 log at 6 days postinfection. At 9 days postinfection, the bacterial titers of the two mutant strains reached similar levels (Fig. 3A). The wild-type strain colonized effectively in the spleen and liver and reached higher titers at 3, 6, and 9 days postinfection, but the mutant strain containing different plasmids was unable to effectively disseminate into spleen and liver at 3 days postinfection (Fig. 3B and C). Although the titers of χ10057(pYA5199) in spleens and livers were significantly lower than those of the wild-type strain, strain χ10057(pYA5199) synthesizing YopENt138-LcrV seemed to be more effective in colonizing the spleen and liver than χ10057(pYA3332) at 6 days postinfection (Fig. 3B and C). At 9 days postinfection, the titers of χ10057(pYA3332) and χ10057(pYA5199) in the spleen and liver were very low (Fig. 3B and C). At 15 days postinfection, no bacteria are detected in the spleens and livers of mice infected with χ10057(pYA3332) and χ10057(pYA5199) (data not shown). The results suggested that χ10057(pYA5199) synthesizing YopENt138-LcrV might increase its ability to invade the spleen and liver at 6 days postinfection.
FIG 3.
Kinetics of bacterial burden in mice infected orally with Y. pseudotuberculosis PB1+, χ10057(pYA3332), or χ10057(pYA5199). Groups of mice were inoculated orally with 0.7 × 109 CFU of wild-type Y. pseudotuberculosis PB1+, 1.5 × 109 CFU of χ10057(pYA3332), or 1.3 × 109 CFU of χ10057(pYA5199). CFU counts per organ in Peyer's patches (A), spleens (B), and livers (C) from 3 mice per group were determined at various times (3, 6, and 9 days). Error bars represent standard deviations. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ns, not significant. The experiment was performed twice with similar results, and the results were pooled for presentation.
Efficacy of protection against pneumonic plague challenge.
The LD50 of Y. pestis KIM6+(pCD1Ap) used as a challenge strain was 100 CFU for i.n. challenge (68). Groups of mice were orally immunized with a single dose (109 CFU) of χ10056(pYA3332), χ10057(pYA3332) (plasmid control), χ10056(pYA5199), or χ10057(pYA5199) (yopENt138-lcrV) or with BSG as a negative control or were subcutaneously immunized with 2.5 × 107 CFU of Y. pestis KIM5 (Pgm−) as a standard attenuated Y. pestis vaccine and were challenged intranasally with ∼240 LD50 (2.4 × 104 CFU) of Y. pestis KIM6+ (pCD1Ap) at 35 days after the initial immunization. Results showed that a single oral dose of χ10057(pYA5199) provided 80% protection against an i.n. KIM6+(pCD1Ap) challenge (Fig. 4). Partial protection was provided by immunization with Y. pestis KIM5 (Pgm−) (60%), χ10056(pYA3332) (42%), χ10056(pYA5199) (40%), or χ10057(pYA3332) (40%). Their protective efficacy was significantly lower than that of χ10057(pYA5199). None of the mice immunized with BSG were protected (Fig. 4).
FIG 4.
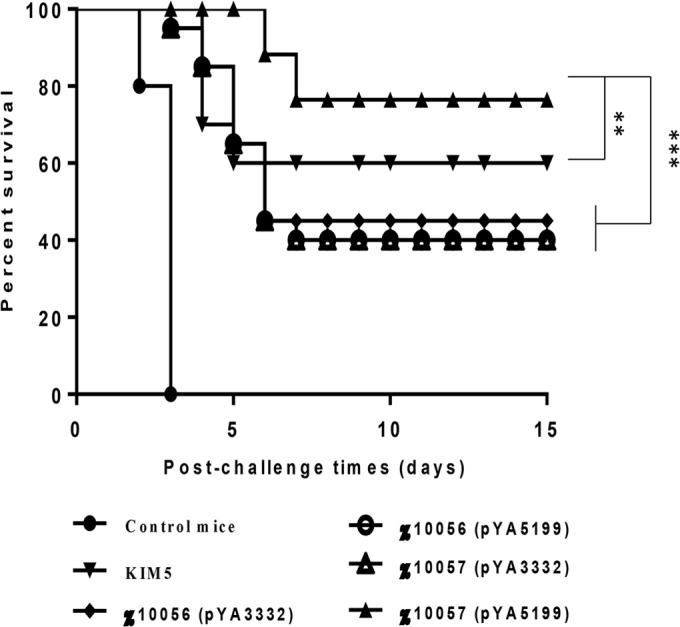
Mouse survival after Y. pestis KIM6+(pCD1Ap) challenge. Swiss Webster mice were orally vaccinated with a dose of 2.0 × 109 CFU of χ10056(pYA3332), 2.5 × 109 CFU of χ10056(pYA5199) as the plasmid control, 2.6 × 109 CFU of χ10057(pYA3332), or 2.2 × 109 CFU of χ10057(pYA5199) or with BSG as the negative control or were subcutaneously immunized with 2.5 × 107 CFU of Y. pestis KIM5 (Pgm−) as a standard attenuated Y. pestis vaccine. Mice were challenged at 35 days after initial vaccination with 2.4 × 104 CFU of Y. pestis KIM6+(pCD1Ap) via the i.n. route. Survival of immunized mice was significantly greater than that of the PBS controls in all experiments (****, P < 0.0001). Survival of mice immunized with χ10057(pYA5199) was significantly greater than that of mice immunized with strains χ10056(pYA3332), χ10056(pYA5199), and χ10057(pYA3332) (***, P < 0.001) and with Y. pestis KIM5 (**, P < 0.01). In each experiment, there were 10 mice in the vaccinated group and 5 mice in the control group. All experiments were performed twice with similar outcomes, and the results were pooled for presentation.
The mice surviving wild-type Y. pseudotuberculosis PB1+ infection were also pooled (10 mice) for intranasal challenge with ∼130 LD50 (1.3 × 104 CFU) of Y. pestis KIM6+ (pCD1Ap). Only 3 mice survived pneumonic challenge during 15 days of observation.
Antibody responses in mice orally immunized with the recombinant Y. pseudotuberculosis strains.
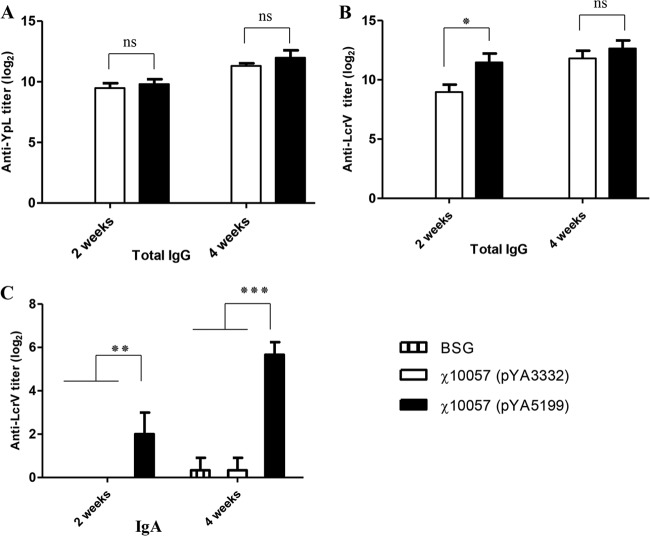
Measurement of total IgG responses to YpL indicated that the levels of anti-YpL titers of χ10057(pYA3332) and χ10057(pYA5199) were similar by week 2 and were boosted by week 4 to levels similar to those of the anti-YpL antibodies (Fig. 5A). The anti-YpL titers from both strains were significantly higher than those from the BSG-immunized group (P < 0.001) (Fig. 5A). The IgG titers of anti-LcrV were slightly higher in mice immunized with χ10057(pYA5199) than in those immunized with χ10057(pYA3332) by week 2 (Fig. 5B). The anti-LcrV titers induced by χ10057(pYA3332) and χ10057(pYA5199) were boosted to similar levels in mice immunized with either strain by week 4.
FIG 5.
Antibody responses in sera and vaginal washes of mice immunized with BSG, χ10057(pYA3332), or χ10057(pYA5199). (A) Total IgG response to Y. pestis KIM5+ whole-cell lysate (YpL). (B) Total IgG response to recombinant LcrV. (C) The secretory IgA response to LcrV. The sera from 12 mice were individually analyzed, and the experiments were performed twice with consistent results. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ns, not significant.
Live attenuated vaccines administered by the oral route can generate mucosal immune responses, in addition to effective development of humoral immune responses (91). Here, we looked at secretory IgA (sIgA) to LcrV in vaginal washes of mice orally immunized with χ10057(pYA5199) and χ10057(pYA3332). The measurement of sIgA indicated that only χ10057(pYA5199)-immunized mice produced significant levels of anti-LcrV IgA at week 2 (P < 0.01) and week 4 (P < 0.001), while the χ10057(pYA3332)- or BSG-immunized mice did not produce any levels of anti-LcrV IgA (Fig. 5C).
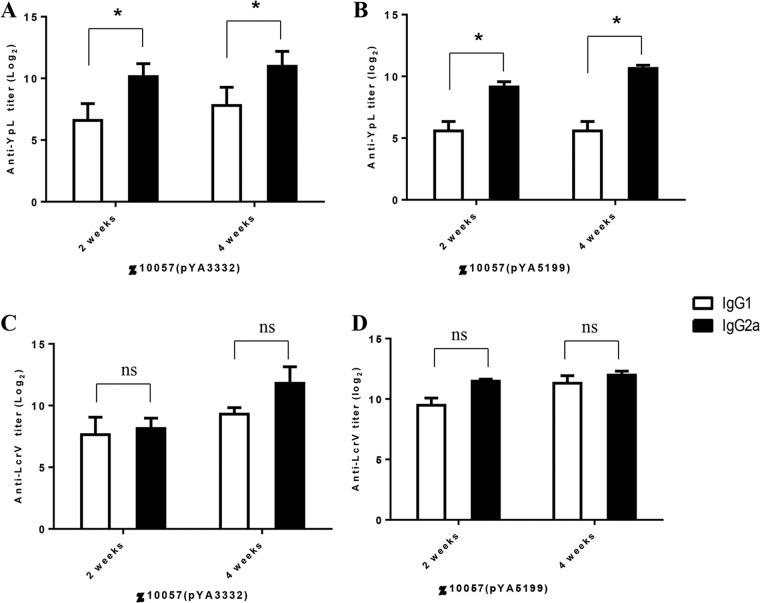
We also measured titers of IgG subtypes (IgG1 and IgG2a) in sera from mice immunized with χ10057(pYA3332) and χ10057(pYA5199). The levels of anti-YpL IgG1 and IgG2a isotype antibodies rapidly increased after vaccination at 2 weeks and gradually increased at 4 weeks. At 2 and 4 weeks postimmunization with χ10057(pYA3332), the ratios of the level of IgG1 to YpL to that of IgG2a to YpL were 0.65:1 and 0.7:1, respectively. Similarly, the ratios of the level of IgG1 to YpL to that of IgG2a to YpL were 0.6:1 and 0.65:1 in mice at 2 and 4 weeks postimmunization with χ10057(pYA5199), respectively (Fig. 6A and B). The results indicated that the Th1-biased response to YpL was primed by both χ10057(pYA3332) and χ10057(pYA5199). The levels of anti-LcrV IgG1 and IgG2a antibodies also rapidly increased after vaccination at 2 weeks and were boosted slightly at 4 weeks postimmunization. But the ratio of IgG1 to IgG2a was very close to 1 in mice immunized with χ10057(pYA3332) or χ10057(pYA5199) (Fig. 6C and D).
FIG 6.
Serum IgG1 and IgG2a responses to YpL and recombinant LcrV. (A) Levels of IgG1 and IgG2a antibody to YpL in sera of mice orally immunized with χ10057(pYA3332). (B) Levels of IgG1 and IgG2a antibody to YpL in sera of mice orally immunized with χ10057(pYA5199). (C) Levels of IgG1 and IgG2a antibody to recombinant LcrV in sera of mice orally immunized with χ10057(pYA3332). (D) Levels of IgG1 and IgG2a antibody to recombinant LcrV in sera of mice orally immunized with χ10057(pYA5199). The sera from 12 mice were individually analyzed, and the experiments were performed twice with consistent results. *, P < 0.05.
Cellular immune response in mice orally immunized with χ10057(pYA5199).
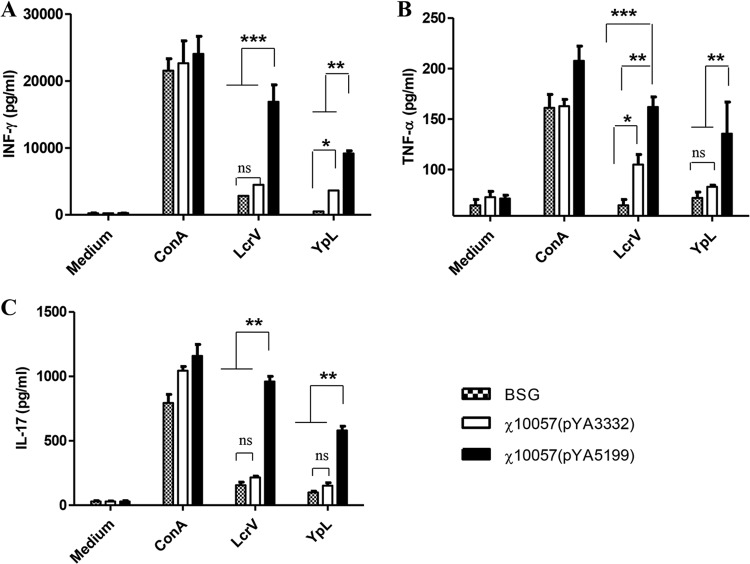
Several reports have demonstrated that protection against pneumonic plague requires cell-mediated immunity induced by IFN-γ and TNF-α (45, 46). IL-17 also contributes to cell-mediated defense against pulmonary Y. pestis infection (92). So, we looked at these three important cytokines. To evaluate cellular immune responses by examining production of IFN-γ, TNF-α, and IL-17 after immunization, we orally vaccinated Swiss Webster mice (4/group) with 109 CFU of χ10057(pYA3332) or χ10057(pYA5199) and with BSG as a negative control. At 21 days after the initial vaccination, splenocytes isolated from mice immunized with BSG, χ10057(pYA3332), or χ10057(pYA5199) were stimulated for 72 h with 4 μg/ml of LcrV, 4 μg/ml of YpL, 1 μg/ml of concanavalin A (ConA) as a positive control, or media (RPMI 1640) as a negative control. The supernatants of the cultures were collected and analyzed using a mouse multiplex assay with BioPlex (Bio-Rad). Results showed that splenic cells from mice vaccinated with χ10057(pYA5199) produced levels of IFN-γ, TNF-α, and IL-17 in response to restimulation with the LcrV antigen that were significantly higher than those observed for χ10057(pYA3332), while cells from the BSG-immunized mice did not produce these cytokines (Fig. 7). These results suggested that immunization with a Y. pseudotuberculosis strain delivering LcrV via the T3SS could elicit an LcrV-specific cellular immune response. Splenic cells from mice vaccinated with χ10057(pYA5199), χ10057(pYA3332), or BSG also produced cytokine profiles similar to those seen with YpL restimulation, but the levels of IFN-γ, TNF-α, and IL-17 produced by YpL stimulation were significantly lower than those produced by LcrV stimulation (Fig. 7). In addition, production of IL-4 in supernatants was measured, but the levels of IL-4 were very low (see Fig. S4A in the supplemental material). We compared the levels of IFN-γ with those of IL-4 in the supernatant of splenic cells stimulated with LcrV in vitro. The ratio of IFN-γ to IL-4 determined for the mouse group subjected to χ10057(pYA5199) immunization was significantly higher than the ratio seen with mice subjected to immunization with BSG and χ10057(pYA3332) (see Fig. S4B). The results suggested that the immune response elicited by immunization of χ10057(pYA5199) had a Th1 bias.
FIG 7.
Cellular immune responses in mice immunized with a live attenuated Y. pseudotuberculosis strain. Splenocytes isolated from Swiss Webster mice vaccinated orally with strain χ10057(pYA3332) (vector control), χ10057(pYA5199) (yopENt138-lcrV), or BSG at 21 days after initial immunization were stimulated in vitro with 4 μg/ml of either purified LcrV or YpL. The mitogen concanavalin A (ConA; 1 μg/ml) served as the positive control, and RPMI 1640 media were used as negative controls. Levels of antigen-specific IFN-γ, TNF-α, and IL-17 cytokines in the culture supernatants produced from splenic cells after 3 days of stimulation were measured by Bioplex assays. (A) Production of IFN-γ. (B) Production of TNF-α. (C) Production of IL-17. Data represent the means ± standard errors (SE) of the results determined for 8 mice for each experiment (the results of two experiments were pooled). *, P < 0.05; **, P < 0.01; ***, P < 0.001; ns, not significant.
DISCUSSION
Our MALDI-MS analysis suggested that the msbB (YPTS_2105) deletion did not significantly alter the major lipid A structures observed in Y. pseudotuberculosis. Protein alignment indicated that YPTS_2105 and MsbB of E. coli K-12 are 65% identical and that YPTS_2105 and MsbB of Y. pestis are 99% identical. D'Hauteville et al. showed that Shigella flexneri had two functional msbB genes, one carried by the chromosome (msbB1) and the other by the virulence plasmid (msbB2), the products of which act in complement to produce full acyl-oxy-acylation of the myristate at the 3′ position of the lipid A glucosamine disaccharide (93). We assumed that Y. pseudotuberculosis PB1+ might have another msbB gene elsewhere, but no extracted gene with high identity to the msbB of E. coli or Y. pestis was identified as a result performing a deep BLAST search among the genomes of Y. pseudotuberculosis PB1+, Y. pestis KIM, and E. coli K-12. Thus, it is possible that lpxP might be responsible for providing hexa-acylation of lipid A in Y. pseudotuberculosis PB1+. Currently, the MS data do not convincingly support the hypothesis that YPTS_2105 encodes a functioning MsbB; however, at least three minor peaks corresponding to lauroyl (C12)-modified lipid A were absent in ΔmsbB lipid A mixtures. Our results showing that hexa-acylated lipid A was predominant in Y. pseudotuberculosis PB1+ at 37°C are inconsistent with previous reports (78). In addition, using a different strain and different growth conditions, Montminy also showed that Y. pseudotuberculosis IP266 contained predominately tetra-, penta-, and hexa-acylated lipid A species when grown at 37°C (94). These contradictions may have been caused by differences in the bacterial strains and/or growth conditions used. A complete examination of the genetic basis for the complex multitude of modified lipid A molecules observed in Y. pseudotuberculosis is beyond the scope of this report and will be performed in a subsequent study.
Mucosal exposure to infectious agents and other foreign antigens often results in the development of mucosal and serum antibodies and cell-mediated immune responses. Delivering specific vaccine antigens through mucosal immunization remains an attractive approach for immunization against infections, especially those acquired at mucosal surfaces. Induction of IgA responses provides specific protection against many respiratory, enteric, and genital infections (91). As we know, recombinant attenuated Salmonella vaccines (RASVs) have been used mostly to induce mucosal and systemic immunity either to Salmonella itself or to heterologous antigens delivered by RASVs (95–97). Live attenuated Y. pseudotuberculosis strains as oral vaccines against different pathogens, including those causing plague, have been explored (36–40).
The stimulation of mucosal immunity and adaptive immunity was expected to result in protection against infection starting at other mucosal surfaces (98) and thus to potentially protect against pneumonic plague. Our results indicated that χ10057 harboring different plasmids was highly attenuated but still could temporarily colonize in the gut and internal organs of mice for more than a week. However, the protective efficacy of χ10057(pYA5199) was significantly better than that of χ10057(pYA3332). Antibody responses indicated that the titers of total IgG to YpL and LcrV primed in mice immunized with χ10057(pYA3332) and χ10057(pYA5199) did not show any significant difference (Fig. 5A and B) but that the titers of IgA to LcrV primed from χ10057(pYA5199) immunization were significantly higher than that induced by χ10057(pYA3332) (Fig. 5C). Thus, the anti-LcrV IgA production observed in mice vaccinated with χ10057(pYA5199) (yopENt138-lcrV) may contribute higher protection against pneumonic plague and can be associated with yopENt138-lcrV expression in χ10057(pYA5199). Tjärnlund et al. have indicated that actively secreted IgA plays a role in protection against mycobacterial infections in the respiratory tract and modulates the proinflammatory response induced by mycobacteria (99). Furuya et al. also suggested that IgA indirectly affects adaptive T-cell immunity through modulating the homeostasis of the mucosal surface (100). Currently, it is unclear whether the IgA produced by immunization with χ10057(pYA5199) might be associated with elicitation of a proinflammatory response and might influence T-cell immunity. We are planning to conduct investigations to test this hypothesis.
Additionally, compared to those from mice orally vaccinated with χ10057(pYA3332), splenocytes from mice orally vaccinated with χ10057(pYA5199) produced high levels of cytokines such as IFN-γ, TNF-α, and IL-17 upon restimulation with both LcrV antigen and YpL (Y. pestis whole-cell lysate) in vitro (Fig. 7), which indicated the development of LcrV-specific and Y. pestis-specific cellular immune responses in mice vaccinated with χ10057(pYA5199) (yopENt138-lcrV). As indicated in Fig. 7, we also observed that splenic cells from vaccinated mice produced significantly lower levels of IFN-γ, TNF-α, and IL-17 upon YpL restimulation than were seen upon LcrV stimulation (Fig. 7). This could have been due to the method of preparation of YpL, since YpL was made from a lysate of Y. pestis KIM+(pCD1Ap) cultured overnight in the calcium-chelated HIB medium at 37°C (76). As we know, tetra-acylated lipid A of Y. pestis KIM6+(pCD1Ap) predominated at 37°C (68, 78, 101–103). Thus, predominant tetra-acylated lipid A in Y. pestis whole-cell lysate prepared under this condition inhibited the induction of proinflammatory cytokines and type I interferons (80), which might result in lower levels of IFN-γ, TNF-α, and IL-17 production.
Derbise et al. indicated that introduction of the pGEN-caf plasmid (low-copy-number plasmid) expressing F1 antigen into an attenuated Y. pseudotuberculosis strain V674 to form V674 pF1 greatly enhanced protective efficacy (39). There are significant differences between our study and that by Derbise et al., such as the use of different Y. pseudotuberculosis strains (PB1+ versus IP32953), different mouse species (Swiss Webster versus OF1), different challenge strains [KIM6+(pCD1Ap) versus CO92], and different mutations [ΔmsbB868::PmsbB msbB(EC) ΔPcrp21::TT araC PBAD crp versus ΔHPI ΔyopK ΔpsaA] and the harboring of different recombinant plasmids (pYA5199 versus pGEN-caf). However, the encapsulated Y. pseudotuberculosis V674 pF1 strain, which provided complete protection against intranasal challenge with 105 CFU of Y. pestis CO92 (39), was more efficacious than χ10057(pYA5199) (yopENt138-lcrV), which provided 80% protection against intranasal challenge with 2.4 × 104 CFU of Y. pestis KIM6+(pCD1Ap). In our study, we also cloned the caf operon into pYA5199 to form pYA5203. χ10057 harboring pYA5203 produced and secreted levels of YopENt138-LcrV similar to those seen with the strain containing pYA5199 and also synthesized high levels of F1 antigen under conditions of culture temperatures of 37°C and 26°C, which affected the bacterial growth rate (data not shown). Animal experiments demonstrated that no colonization and no protection were observed in the spleens and livers of mice immunized with χ10057(pYA5203) delivering YopENt138-LcrV/F1 (data not shown). Our observations indicated that overexpressing caf1 in live attenuated Y. pseudotuberculosis strains affected the growth rate of bacteria, weakened the bacterial resistance in mice, and decreased immunogenicity. Cao et al. also demonstrated that overexpressing caf1 in wild-type Salmonella enterica serovar Typhimurium greatly attenuated the virulence of the Salmonella in vivo (104). Thus, we are trying to reduce caf1 expression to optimal levels in the same host strain, χ10057, in which synthesizing optimal levels of F1 antigen and LcrV simultaneously may improve their immunogenicity to confer protective immunity against pneumonic plague.
Supplementary Material
ACKNOWLEDGMENTS
We thank Jacquelyn Kilbourne for assistance with mouse bleeding.
This research was supported by National Institutes of Health grant AI095872 to W.S.
We declare that we have no conflicts of interest.
Footnotes
Published ahead of print 11 August 2014
Supplemental material for this article may be found at http://dx.doi.org/10.1128/IAI.02173-14.
REFERENCES
- 1. Perry RD, Fetherston JD. 1997. Yersinia pestis–etiologic agent of plague. Clin. Microbiol. Rev. 10:35–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Prentice MB, Rahalison L. 2007. Plague. Lancet 369:1196–1207. 10.1016/S0140-6736(07)60566-2 [DOI] [PubMed] [Google Scholar]
- 3. Rollins SE, Rollins SM, Ryan ET. 2003. Yersinia pestis and the plague. Am. J. Clin. Pathol. 119(Suppl):S78–S85. 10.1309/DQM93R8QNQWBFYU8 [DOI] [PubMed] [Google Scholar]
- 4. Guiyoule A, Rasoamanana B, Buchrieser C, Michel P, Chanteau S, Carniel E. 1997. Recent emergence of new variants of Yersinia pestis in Madagascar. J. Clin. Microbiol. 35:2826–2833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Guiyoule A, Gerbaud G, Buchrieser C, Galimand M, Rahalison L, Chanteau S, Courvalin P, Carniel E. 2001. Transferable plasmid-mediated resistance to streptomycin in a clinical isolate of Yersinia pestis. Emerg. Infect. Dis. 7:43–48. 10.3201/eid0701.010106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Galimand M, Guiyoule A, Gerbaud G, Rasoamanana B, Chanteau S, Carniel E, Courvalin P. 1997. Multidrug resistance in Yersinia pestis mediated by a transferable plasmid. N. Engl. J. Med. 337:677–680. 10.1056/NEJM199709043371004 [DOI] [PubMed] [Google Scholar]
- 7. Titball RW, Williamson ED. 2004. Yersinia pestis (plague) vaccines. Expert Opin. Biol. Ther. 4:965–973. 10.1517/14712598.4.6.965 [DOI] [PubMed] [Google Scholar]
- 8. Meyer KF, Smith G, Foster L, Brookman M, Sung M. 1974. Live, attenuated Yersinia pestis vaccine: virulent in nonhuman primates, harmless to guinea pigs. J. Infect. Dis. 129(Suppl):S85–S120. 10.1093/infdis/129.Supplement_1.S85 [DOI] [PubMed] [Google Scholar]
- 9. Wang X, Zhang X, Zhou D, Yang R. 2013. Live-attenuated Yersinia pestis vaccines. Expert Rev. Vaccines 12:677–686. 10.1586/erv.13.42 [DOI] [PubMed] [Google Scholar]
- 10. Sun W, Roland KL, Curtiss R., III 2011. Developing live vaccines against plague. J. Infect. Dev. Ctries. 5:614–627. 10.3855/jidc.2030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Feodorova VA, Corbel MJ. 2009. Prospects for new plague vaccines. Expert Rev. Vaccines 8:1721–1738. 10.1586/erv.09.129 [DOI] [PubMed] [Google Scholar]
- 12. Anderson GW, Jr, Heath DG, Bolt CR, Welkos SL, Friedlander AM. 1998. Short- and long-term efficacy of single-dose subunit vaccines against Yersinia pestis in mice. Am. J. Trop. Med. Hyg. 58:793–799 [DOI] [PubMed] [Google Scholar]
- 13. Andrews GP, Heath DG, Anderson GW, Jr, Welkos SL, Friedlander AM. 1996. Fraction 1 capsular antigen (F1) purification from Yersinia pestis CO92 and from an Escherichia coli recombinant strain and efficacy against lethal plague challenge. Infect. Immun. 64:2180–2187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Heath DG, Anderson GW, Jr, Mauro JM, Welkos SL, Andrews GP, Adamovicz J, Friedlander AM. 1998. Protection against experimental bubonic and pneumonic plague by a recombinant capsular F1-V antigen fusion protein vaccine. Vaccine 16:1131–1137. 10.1016/S0264-410X(98)80110-2 [DOI] [PubMed] [Google Scholar]
- 15. Leary SE, Williamson ED, Griffin KF, Russell P, Eley SM, Titball RW. 1995. Active immunization with recombinant V antigen from Yersinia pestis protects mice against plague. Infect. Immun. 63:2854–2858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Simpson WJ, Thomas RE, Schwan TG. 1990. Recombinant capsular antigen (fraction 1) from Yersinia pestis induces a protective antibody response in BALB/c mice. Am. J. Trop. Med. Hyg. 43:389–396 [DOI] [PubMed] [Google Scholar]
- 17. Une T, Brubaker RR. 1984. Roles of V antigen in promoting virulence and immunity in yersiniae. J. Immunol. 133:2226–2230 [PubMed] [Google Scholar]
- 18. Williamson ED, Eley SM, Griffin KF, Green M, Russell P, Leary SE, Oyston PC, Easterbrook T, Reddin KM, Robinson A, Titball RW. 1995. A new improved sub-unit vaccine for plague: the basis of protection. FEMS Immunol. Med. Microbiol. 12:223–230. 10.1111/j.1574-695X.1995.tb00196.x [DOI] [PubMed] [Google Scholar]
- 19. Williamson ED, Flick-Smith HC, Lebutt C, Rowland CA, Jones SM, Waters EL, Gwyther RJ, Miller J, Packer PJ, Irving M. 2005. Human immune response to a plague vaccine comprising recombinant F1 and V antigens. Infect. Immun. 73:3598–3608. 10.1128/IAI.73.6.3598-3608.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Quenee LE, Ciletti NA, Elli D, Hermanas TM, Schneewind O. 2011. Prevention of pneumonic plague in mice, rats, guinea pigs and non-human primates with clinical grade rV10, rV10–2 or F1-V vaccines. Vaccine 29:6572–6583. 10.1016/j.vaccine.2011.06.119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Smiley ST. 2008. Current challenges in the development of vaccines for pneumonic plague. Expert Rev. Vaccines 7:209–221. 10.1586/14760584.7.2.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Winter CC, Cherry WB, Moody MD. 1960. An unusual strain of Pasteurella pestis isolated from a fatal human case of plague. Bull. World Health Organ. 23:408–409 [PMC free article] [PubMed] [Google Scholar]
- 23. Anisimov AP, Dentovskaya SV, Panfertsev EA, Svetoch TE, Kopylov PK, Segelke BW, Zemla A, Telepnev MV, Motin VL. 2010. Amino acid and structural variability of Yersinia pestis LcrV protein. Infect. Genet. Evol. 10:137–145. 10.1016/j.meegid.2009.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Smiley ST. 2008. Immune defense against pneumonic plague. Immunol. Rev. 225:256–271. 10.1111/j.1600-065X.2008.00674.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wren BW. 2003. The yersiniae–a model genus to study the rapid evolution of bacterial pathogens. Nat. Rev. Microbiol. 1:55–64. 10.1038/nrmicro730 [DOI] [PubMed] [Google Scholar]
- 26. Skurnik M, Peippo A, Ervela E. 2000. Characterization of the O-antigen gene clusters of Yersinia pseudotuberculosis and the cryptic O-antigen gene cluster of Yersinia pestis shows that the plague bacillus is most closely related to and has evolved from Y. pseudotuberculosis serotype O:1b. Mol. Microbiol. 37:316–330. 10.1046/j.1365-2958.2000.01993.x [DOI] [PubMed] [Google Scholar]
- 27. Achtman M, Zurth K, Morelli G, Torrea G, Guiyoule A, Carniel E. 1999. Yersinia pestis, the cause of plague, is a recently emerged clone of Yersinia pseudotuberculosis. Proc. Natl. Acad. Sci. U. S. A. 96:14043–14048. 10.1073/pnas.96.24.14043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Morelli G, Song Y, Mazzoni CJ, Eppinger M, Roumagnac P, Wagner DM, Feldkamp M, Kusecek B, Vogler AJ, Li Y, Cui Y, Thomson NR, Jombart T, Leblois R, Lichtner P, Rahalison L, Petersen JM, Balloux F, Keim P, Wirth T, Ravel J, Yang R, Carniel E, Achtman M. 2010. Yersinia pestis genome sequencing identifies patterns of global phylogenetic diversity. Nat. Genet. 42:1140–1143. 10.1038/ng.705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Achtman M, Morelli G, Zhu P, Wirth T, Diehl I, Kusecek B, Vogler AJ, Wagner DM, Allender CJ, Easterday WR, Chenal-Francisque V, Worsham P, Thomson NR, Parkhill J, Lindler LE, Carniel E, Keim P. 2004. Microevolution and history of the plague bacillus, Yersinia pestis. Proc. Natl. Acad. Sci. U. S. A. 101:17837–17842. 10.1073/pnas.0408026101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chain PS, Carniel E, Larimer FW, Lamerdin J, Stoutland PO, Regala WM, Georgescu AM, Vergez LM, Land ML, Motin VL, Brubaker RR, Fowler J, Hinnebusch J, Marceau M, Medigue C, Simonet M, Chenal-Francisque V, Souza B, Dacheux D, Elliott JM, Derbise A, Hauser LJ, Garcia E. 2004. Insights into the evolution of Yersinia pestis through whole-genome comparison with Yersinia pseudotuberculosis. Proc. Natl. Acad. Sci. U. S. A. 101:13826–13831. 10.1073/pnas.0404012101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Branger CG, Fetherston JD, Perry RD, Curtiss R., III 2007. Oral vaccination with different antigens from Yersinia pestis KIM delivered by live attenuated Salmonella typhimurium elicits a protective immune response against plague. Adv. Exp. Med. Biol. 603:387–399. 10.1007/978-0-387-72124-8_36 [DOI] [PubMed] [Google Scholar]
- 32. Murphy BS, Wulff CR, Garvy BA, Straley SC. 2007. Yersinia pestis YadC: a novel vaccine candidate against plague. Adv. Exp. Med. Biol. 603:400–414. 10.1007/978-0-387-72124-8_37 [DOI] [PubMed] [Google Scholar]
- 33. Sun W, Olinzock J, Wang S, Sanapala S, Curtiss R., III 2014. Evaluation of YadC protein delivered by live attenuated Salmonella as a vaccine against plague. Pathog. Dis. 70:119–131. 10.1111/2049-632X.12076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Buchrieser C, Rusniok C, Frangeul L, Couve E, Billault A, Kunst F, Carniel E, Glaser P. 1999. The 102-kilobase pgm locus of Yersinia pestis: sequence analysis and comparison of selected regions among different Yersinia pestis and Yersinia pseudotuberculosis strains. Infect. Immun. 67:4851–4861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Forman S, Wulff CR, Myers-Morales T, Cowan C, Perry RD, Straley SC. 2008. yadBC of Yersinia pestis, a new virulence determinant for bubonic plague. Infect. Immun. 76:578–587. 10.1128/IAI.00219-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Taylor VL, Titball RW, Oyston PC. 2005. Oral immunization with a dam mutant of Yersinia pseudotuberculosis protects against plague. Microbiology 151:1919–1926. 10.1099/mic.0.27959-0 [DOI] [PubMed] [Google Scholar]
- 37. Blisnick T, Ave P, Huerre M, Carniel E, Demeure CE. 2008. Oral vaccination against bubonic plague using a live avirulent Yersinia pseudotuberculosis strain. Infect. Immun. 76:3808–3816. 10.1128/IAI.00034-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Okan NA, Mena P, Benach JL, Bliska JB, Karzai AW. 2010. The smpB-ssrA mutant of Yersinia pestis functions as a live attenuated vaccine to protect mice against pulmonary plague infection. Infect. Immun. 78:1284–1293. 10.1128/IAI.00976-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Derbise A, Cerda Marin A, Ave P, Blisnick T, Huerre M, Carniel E, Demeure CE. 2012. An encapsulated Yersinia pseudotuberculosis is a highly efficient vaccine against pneumonic plague. PLoS Negl. Trop. Dis. 6:e1528. 10.1371/journal.pntd.0001528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rüssmann H, Gerdemann U, Igwe EI, Panthel K, Heesemann J, Garbom S, Wolf-Watz H, Geginat G. 2003. Attenuated Yersinia pseudotuberculosis carrier vaccine for simultaneous antigen-specific CD4 and CD8 T-cell induction. Infect. Immun. 71:3463–3472. 10.1128/IAI.71.6.3463-3472.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wiedig CA, Kramer U, Garbom S, Wolf-Watz H, Autenrieth IB. 2005. Induction of CD8+ T cell responses by Yersinia vaccine carrier strains. Vaccine 23:4984–4998. 10.1016/j.vaccine.2005.05.027 [DOI] [PubMed] [Google Scholar]
- 42. Lotter H, Russmann H, Heesemann J, Tannich E. 2004. Oral vaccination with recombinant Yersinia enterocolitica expressing hybrid type III proteins protects gerbils from amebic liver abscess. Infect. Immun. 72:7318–7321. 10.1128/IAI.72.12.7318-7321.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rüssmann H, Igwe EI, Sauer J, Hardt WD, Bubert A, Geginat G. 2001. Protection against murine listeriosis by oral vaccination with recombinant Salmonella expressing hybrid Yersinia type III proteins. J. Immunol. 167:357–365. 10.4049/jimmunol.167.1.357 [DOI] [PubMed] [Google Scholar]
- 44. Williamson ED. 2009. Plague. Vaccine 27:D56–D60. 10.1016/j.vaccine.2009.07.068 [DOI] [PubMed] [Google Scholar]
- 45. Parent MA, Berggren KN, Kummer LW, Wilhelm LB, Szaba FM, Mullarky IK, Smiley ST. 2005. Cell-mediated protection against pulmonary Yersinia pestis infection. Infect. Immun. 73:7304–7310. 10.1128/IAI.73.11.7304-7310.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Parent MA, Wilhelm LB, Kummer LW, Szaba FM, Mullarky IK, Smiley ST. 2006. Gamma interferon, tumor necrosis factor alpha, and nitric oxide synthase 2, key elements of cellular immunity, perform critical protective functions during humoral defense against lethal pulmonary Yersinia pestis infection. Infect. Immun. 74:3381–3386. 10.1128/IAI.00185-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Philipovskiy AV, Smiley ST. 2007. Vaccination with live Yersinia pestis primes CD4 and CD8 T cells that synergistically protect against lethal pulmonary Y. pestis infection. Infect. Immun. 75:878–885. 10.1128/IAI.01529-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang S, Goguen JD, Li F, Lu S. 2011. Involvement of CD8+ T cell-mediated immune responses in LcrV DNA vaccine induced protection against lethal Yersinia pestis challenge. Vaccine 29:6802–6809. 10.1016/j.vaccine.2010.12.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Shreewastav RK, Ali R, Uppada JB, Rao DN. 2012. Cell-mediated immune response to epitopic MAP (multiple antigen peptide) construct of LcrV antigen of Yersinia pestis in murine model. Cell. Immunol. 278:55–62. 10.1016/j.cellimm.2012.07.002 [DOI] [PubMed] [Google Scholar]
- 50. Qiu Y, Liu Y, Qi Z, Wang W, Kou Z, Zhang Q, Liu G, Liu T, Yang Y, Yang X, Xin Y, Li C, Cui B, Huang S, Liu H, Zeng L, Wang Z, Yang R, Wang H, Wang X. 2010. Comparison of immunological responses of plague vaccines F1+rV270 and EV76 in Chinese-origin rhesus macaque, Macaca mulatta. Scand. J. Immunol. 72:425–433. 10.1111/j.1365-3083.2010.02456.x [DOI] [PubMed] [Google Scholar]
- 51. Williamson ED, Eley SM, Griffin KF, Green M, Russell P, Leary SEC, Oyston PCF, Easterbrook T, Reddin KM, Robinson A, Titball RW. 1995. A new improved subunit vaccine for plague - the basis of protection. FEMS Immunol. Med. Microbiol. 12:223–230. 10.1111/j.1574-695X.1995.tb00196.x [DOI] [PubMed] [Google Scholar]
- 52. Qi Z, Zhou L, Zhang Q, Ren L, Dai R, Wu B, Wang T, Zhu Z, Yang Y, Cui B, Wang Z, Wang H, Qiu Y, Guo Z, Yang R, Wang X. 2010. Comparison of mouse, guinea pig and rabbit models for evaluation of plague subunit vaccine F1+rV270. Vaccine 28:1655–1660. 10.1016/j.vaccine.2009.02.078 [DOI] [PubMed] [Google Scholar]
- 53. Williamson ED, Eley SM, Stagg AJ, Green M, Russell P, Titball RW. 2000. A single dose sub-unit vaccine protects against pneumonic plague. Vaccine 19:566–571. 10.1016/S0264-410X(00)00159-6 [DOI] [PubMed] [Google Scholar]
- 54. Williamson ED, Eley SM, Stagg AJ, Green M, Russell P, Titball RW. 1997. A sub-unit vaccine elicits IgG in serum, spleen cell cultures and bronchial washings and protects immunized animals against pneumonic plague. Vaccine 15:1079–1084. 10.1016/S0264-410X(96)00303-9 [DOI] [PubMed] [Google Scholar]
- 55. Williamson ED, Vesey PM, Gillhespy KJ, Eley SM, Green M, Titball RW. 1999. An IgG1 titre to the F1 and V antigens correlates with protection against plague in the mouse model. Clin. Exp. Immunol. 116:107–114. 10.1046/j.1365-2249.1999.00859.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Quenee LE, Cornelius CA, Ciletti NA, Elli D, Schneewind O. 2008. Yersinia pestis caf1 variants and the limits of plague vaccine protection. Infect. Immun. 76:2025–2036. 10.1128/IAI.00105-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Braciale VL, Nash M, Sinha N, Zudina IV, Motin VL. 2008. Correlates of immunity elicited by live Yersinia pestis vaccine. Infect. Dis. 23:473–480. 10.1007/978-1-59745-569-5_50 [DOI] [Google Scholar]
- 58. Li B, Du C, Zhou L, Bi Y, Wang X, Wen L, Guo Z, Song Z, Yang R. 2012. Humoral and cellular immune responses to Yersinia pestis infection in long-term recovered plague patients. Clin. Vaccine Immunol. 19:228–234. 10.1128/CVI.05559-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Pettersson J, Holmstrom A, Hill J, Leary S, Frithz-Lindsten E, von Euler-Matell A, Carlsson E, Titball R, Forsberg A, Wolf-Watz H. 1999. The V-antigen of Yersinia is surface exposed before target cell contact and involved in virulence protein translocation. Mol. Microbiol. 32:961–976. 10.1046/j.1365-2958.1999.01408.x [DOI] [PubMed] [Google Scholar]
- 60. Nilles ML, Fields KA, Straley SC. 1998. The V antigen of Yersinia pestis regulates Yop vectorial targeting as well as Yop secretion through effects on YopB and LcrG. J. Bacteriol. 180:3410–3420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kang HY, Srinivasan J, Curtiss R., III 2002. Immune responses to recombinant pneumococcal PspA antigen delivered by live attenuated Salmonella enterica serovar Typhimurium vaccine. Infect. Immun. 70:1739–1749. 10.1128/IAI.70.4.1739-1749.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Wang S, Li Y, Scarpellini G, Kong W, Shi H, Baek CH, Gunn B, Wanda SY, Roland KL, Zhang X, Senechal-Willis P, Curtiss R., III 2010. Salmonella vaccine vectors displaying delayed antigen synthesis in vivo to enhance immunogenicity. Infect. Immun. 78:3969–3980. 10.1128/IAI.00444-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Gong S, Bearden SW, Geoffroy VA, Fetherston JD, Perry RD. 2001. Characterization of the Yersinia pestis Yfu ABC inorganic iron transport system. Infect. Immun. 69:2829–2837. 10.1128/IAI.67.5.2829-2837.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Kang HY, Dozois CM, Tinge SA, Lee TH, Curtiss R., III 2002. Transduction-mediated transfer of unmarked deletion and point mutations through use of counterselectable suicide vectors. J. Bacteriol. 184:307–312. 10.1128/JB.184.1.307-312.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Branger CG, Sun W, Torres-Escobar A, Perry R, Roland KL, Fetherston J, Curtiss R., III 2010. Evaluation of Psn, HmuR and a modified LcrV protein delivered to mice by live attenuated Salmonella as a vaccine against bubonic and pneumonic Yersinia pestis challenge. Vaccine 29:274–282. 10.1016/j.vaccine.2010.10.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Sun W, Roland KL, Kuang X, Branger CG, Curtiss R., III 2010. Yersinia pestis with regulated delayed attenuation as a vaccine candidate to induce protective immunity against plague. Infect. Immun. 78:1304–1313. 10.1128/IAI.01122-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Bertani G. 1951. Studies on lysogenesis. I. The mode of phage liberation by lysogenic Escherichia coli. J. Bacteriol. 62:293–300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Sun W, Six D, Kuang XY, Roland KL, Raetz CRH, Curtiss R., III 2011. A live attenuated strain of Yersinia pestis KIM as a vaccine against plague. Vaccine 29:2986–2998. 10.1016/j.vaccine.2011.01.099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Straley SC, Bowmer WS. 1986. Virulence genes regulated at the transcriptional level by Ca2+ in Yersinia pestis include structural genes for outer membrane proteins. Infect. Immun. 51:445–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Sun W, Wang S, Curtiss R., III 2008. Highly efficient method for introducing successive multiple scarless gene deletions and markerless gene insertions into the Yersinia pestis chromosome. Appl. Environ. Microbiol. 74:4241–4245. 10.1128/AEM.00940-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Kim TJ, Chauhan S, Motin VL, Goh EB, Igo MM, Young GM. 2007. Direct transcriptional control of the plasminogen activator gene of Yersinia pestis by the cyclic AMP receptor protein. J. Bacteriol. 189:8890–8900. 10.1128/JB.00972-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Collazo CM, Galan JE. 1997. The invasion-associated type III system of Salmonella typhimurium directs the translocation of Sip proteins into the host cell. Mol. Microbiol. 24:747–756. 10.1046/j.1365-2958.1997.3781740.x [DOI] [PubMed] [Google Scholar]
- 73. Kong Q, Six DA, Roland KL, Liu Q, Gu L, Reynolds CM, Wang X, Raetz CR, Curtiss R., III 2011. Salmonella synthesizing 1-dephosphorylated lipopolysaccharide exhibits low endotoxic activity while retaining its immunogenicity. J. Immunol. 187:412–423. 10.4049/jimmunol.1100339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Wang S, Li Y, Shi H, Sun W, Roland KL, Curtiss R., III 2011. Comparison of a regulated delayed antigen synthesis system with in vivo-inducible promoters for antigen delivery by live attenuated Salmonella vaccines. Infect. Immun. 79:937–949. 10.1128/IAI.00445-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Zhang Y, Bliska JB. 2010. YopJ-promoted cytotoxicity and systemic colonization are associated with high levels of murine interleukin-18, gamma interferon, and neutrophils in a live vaccine model of Yersinia pseudotuberculosis infection. Infect. Immun. 78:2329–2341. 10.1128/IAI.00094-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Sun W, Roland KL, Branger CG, Kuang X, Curtiss R., III 2009. The role of relA and spoT in Yersinia pestis KIM5+ pathogenicity. PLoS One 4:e6720. 10.1371/journal.pone.0006720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Sun W, Curtiss R., III 2012. Amino acid substitutions in LcrV at putative sites of interaction with toll-like receptor 2 do not affect the virulence of Yersinia pestis. Microb. Pathog. 53:198–206. 10.1016/j.micpath.2012.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Rebeil R, Ernst RK, Gowen BB, Miller SI, Hinnebusch BJ. 2004. Variation in lipid A structure in the pathogenic yersiniae. Mol. Microbiol. 52:1363–1373. 10.1111/j.1365-2958.2004.04059.x [DOI] [PubMed] [Google Scholar]
- 79. Pérez-Gutiérrez C, Llobet E, Llompart CM, Reinés M, Bengoechea JA. 2010. Role of lipid A acylation in Yersinia enterocolitica virulence. Infect. Immun. 78:2768–2781. 10.1128/IAI.01417-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Montminy SW, Khan N, McGrath S, Walkowicz MJ, Sharp F, Conlon JE, Fukase K, Kusumoto S, Sweet C, Miyake K, Akira S, Cotter RJ, Goguen JD, Lien E. 2006. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat. Immunol. 7:1066–1073. 10.1038/ni1386 [DOI] [PubMed] [Google Scholar]
- 81. Telepnev MV, Klimpel GR, Haithcoat J, Knirel YA, Anisimov AP, Motin VL. 2009. Tetraacylated lipopolysaccharide of Yersinia pestis can inhibit multiple Toll-like receptor-mediated signaling pathways in human dendritic cells. J. Infect. Dis. 200:1694–1702. 10.1086/647986 [DOI] [PubMed] [Google Scholar]
- 82. Zhou D, Yang R. 2009. Molecular Darwinian evolution of virulence in Yersinia pestis. Infect. Immun. 77:2242–2250. 10.1128/IAI.01477-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Krasikova IN, Gorbach VI, Solov'eva TF, Ovodov YS. 1978. Studies on lipid A from Yersinia pseudotuberculosis lipopolysaccharide. Isolation and general characterization. Eur. J. Biochem. 89:287–289. 10.1111/j.1432-1033.1978.tb20925.x [DOI] [PubMed] [Google Scholar]
- 84. Nakayama K, Kelly SM, Curtiss R., III 1988. Construction of an Asd+ expression vector: stable maintenance and high expression of cloned genes in a Salmonella vaccine strain. Biotechnology (NY) 6:693–697. 10.1038/nbt0688-693 [DOI] [Google Scholar]
- 85. Janssen WA, Surgalla MJ. 1969. Plague bacillus: survival within host phagocytes. Science 163:950–952. 10.1126/science.163.3870.950 [DOI] [PubMed] [Google Scholar]
- 86. Pujol C, Grabenstein JP, Perry RD, Bliska JB. 2005. Replication of Yersinia pestis in interferon gamma-activated macrophages requires ripA, a gene encoded in the pigmentation locus. Proc. Natl. Acad. Sci. U. S. A. 102:12909–12914. 10.1073/pnas.0502849102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Lukaszewski RA, Kenny DJ, Taylor R, Rees DG, Hartley MG, Oyston PC. 2005. Pathogenesis of Yersinia pestis infection in BALB/c mice: effects on host macrophages and neutrophils. Infect. Immun. 73:7142–7150. 10.1128/IAI.73.11.7142-7150.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Elvin SJ, Williamson ED. 2004. Stat 4 but not Stat 6 mediated immune mechanisms are essential in protection against plague. Microb. Pathog. 37:177–184. 10.1016/j.micpath.2004.06.009 [DOI] [PubMed] [Google Scholar]
- 89. Feldman MF, Müller S, Wüest E, Cornelis GR. 2002. SycE allows secretion of YopE-DHFR hybrids by the Yersinia enterocolitica type III Ysc system. Mol. Microbiol. 46:1183–1197. 10.1046/j.1365-2958.2002.03241.x [DOI] [PubMed] [Google Scholar]
- 90. Rüssmann H, Weissmüller A, Geginat G, Igwe EI, Roggenkamp A, Bubert A, Goebel W, Hof H, Heesemann J. 2000. Yersinia enterocolitica-mediated translocation of defined fusion proteins to the cytosol of mammalian cells results in peptide-specific MHC class I-restricted antigen presentation. Eur. J. Immunol. 30:1375–1384. [DOI] [PubMed] [Google Scholar]
- 91. Ogra PL, Faden H, Welliver RC. 2001. Vaccination strategies for mucosal immune responses. Clin. Microbiol. Rev. 14:430–445. 10.1128/CMR.14.2.430-445.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Lin JS, Kummer LW, Szaba FM, Smiley ST. 2011. IL-17 contributes to cell-mediated defense against pulmonary Yersinia pestis infection. J. Immunol. 186:1675–1684. 10.4049/jimmunol.1003303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. D'Hauteville H, Khan S, Maskell DJ, Kussak A, Weintraub A, Mathison J, Ulevitch RJ, Wuscher N, Parsot C, Sansonetti PJ. 2002. Two msbB genes encoding maximal acylation of lipid A are required for invasive Shigella flexneri to mediate inflammatory rupture and destruction of the intestinal epithelium. J. Immunol. 168:5240–5251. 10.4049/jimmunol.168.10.5240 [DOI] [PubMed] [Google Scholar]
- 94. Montminy SW. 2009. Evasion of LPS-TLR4 signaling as a virulence determinate for Yersinia pestis. University of Massachusetts Medical School Worcester, Worcester, MA [Google Scholar]
- 95. McSorley SJ, Asch S, Costalonga M, Reinhardt RL, Jenkins MK. 2002. Tracking salmonella-specific CD4 T cells in vivo reveals a local mucosal response to a disseminated infection. Immunity 16:365–377. 10.1016/S1074-7613(02)00289-3 [DOI] [PubMed] [Google Scholar]
- 96. Mittrücker HW, Raupach B, Köhler A, Kaufmann SH. 2000. Cutting edge: role of B lymphocytes in protective immunity against Salmonella typhimurium infection. J. Immunol. 164:1648–1652. 10.4049/jimmunol.164.4.1648 [DOI] [PubMed] [Google Scholar]
- 97. Li Y, Wang S, Xin W, Scarpellini G, Shi Z, Gunn B, Roland KL, Curtiss R., III 2008. A sopB deletion mutation enhances the immunogenicity and protective efficacy of a heterologous antigen delivered by live attenuated Salmonella enterica vaccines. Infect. Immun. 76:5238–5246. 10.1128/IAI.00720-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Holmgren J, Czerkinsky C. 2005. Mucosal immunity and vaccines. Nat. Med. 11:S45–S53. 10.1038/nm1213 [DOI] [PubMed] [Google Scholar]
- 99. Tjärnlund A, Rodríguez A, Cardona PJ, Guirado E, Ivanyi J, Singh M, Troye-Blomberg M, Fernández C. 2006. Polymeric IgR knockout mice are more susceptible to mycobacterial infections in the respiratory tract than wild-type mice. Int. Immunol. 18:807–816. 10.1093/intimm/dxl017 [DOI] [PubMed] [Google Scholar]
- 100. Furuya Y, Kirimanjeswara GS, Roberts S, Metzger DW. 2013. Increased susceptibility of IgA-deficient mice to pulmonary Francisella tularensis live vaccine strain infection. Infect. Immun. 81:3434–3441. 10.1128/IAI.00408-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Kawahara K, Tsukano H, Watanabe H, Lindner B, Matsuura M. 2002. Modification of the structure and activity of lipid A in Yersinia pestis lipopolysaccharide by growth temperature. Infect. Immun. 70:4092–4098. 10.1128/IAI.70.8.4092-4098.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Knirel YA, Lindner B, Vinogradov EV, Kocharova NA, Senchenkova SN, Shaikhutdinova RZ, Dentovskaya SV, Fursova NK, Bakhteeva IV, Titareva GM, Balakhonov SV, Holst O, Gremyakova TA, Pier GB, Anisimov AP. 2005. Temperature-dependent variations and intraspecies diversity of the structure of the lipopolysaccharide of Yersinia pestis. Biochemistry 44:1731–1743. 10.1021/bi048430f [DOI] [PubMed] [Google Scholar]
- 103. Sun W, Six DA, Reynolds CM, Chung HS, Raetz CR, Curtiss R., III 2013. Pathogenicity of Yersinia pestis synthesis of 1-dephosphorylated lipid A. Infect. Immun. 81:1172–1185. 10.1128/IAI.01403-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Cao L, Lim T, Jun S, Thornburg T, Avci R, Yang X. 2012. Vulnerabilities in Yersinia pestis caf operon are unveiled by a Salmonella vector. PLoS One 7:e36283. 10.1371/journal.pone.0036283 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.