Abstract
Background
HIV-1 infected macrophages play a key role in HIV-1 infection. Even during anti-retroviral treatment, macrophages keep producing virus due to suboptimal tissue penetration and reduced efficacy of antiretrovirals. It is therefore of major importance to understand which host factors are involved in HIV-1 replication in macrophages. Previously, we have shown that genetic polymorphisms in phosphodiesterase 8a (PDE8A) are strongly associated with HIV-1 replication in these cells. Here we analyzed the mechanism and regulation of PDE8A in HIV-1 replication in macrophages.
Results
PDE8A mRNA expression strongly increases upon differentiation of monocytes into macrophages, which corresponds to the increased susceptibility of mature macrophages to HIV-1. In parallel, expression of microRNA miR-145-5p, predicted to target PDE8A mRNA, strongly decreased. The interaction of miR-145-5p with the 3′ UTR of PDE8A mRNA could be experimentally validated, suggesting that indeed miR-145-5p can regulate PDE8A expression levels. Knockdown of PDE8A in macrophages resulted in a decrease in total HIV-1 replication and proviral DNA levels. These observations confirm that PDE8A regulates HIV-1 replication in macrophages and that this effect is mediated through early steps in the viral replication cycle.
Conclusions
PDE8A is highly expressed in macrophages, and its expression is regulated by miR-145-5p. Our findings strongly suggest that PDE8A supports HIV-1 replication in macrophages and that this effect is mediated at the level of reverse transcription.
Introduction
Macrophages play a key role in HIV-1 infection. They are among the first cells that encounter HIV-1 upon transmission and once infected they facilitate spread of the virus to CD4+ T-cells [1]–[7]. Infected macrophages are relatively resistant to HIV-1 induced apoptosis and can efficiently evade host immunity [8], [9]. Due to the ability of these cells to migrate into the tissue, the virus is disseminated throughout the body [10]–[14]. The introduction of combined antiretroviral therapy (cART) has reversed the fatal outcome of HIV-1 infection. Nonetheless, infected macrophages remain a source of residual virus production during treatment due to the low efficacy of cART, combined with the suboptimal tissue penetration of the drugs [10]–[15]. In addition to their contribution to the viral reservoir, HIV-1 infected macrophages play a crucial role in several AIDS related pathologies such as HIV-1 associated dementia, AIDS-related non-Hodgkin lymphoma and cardiovascular diseases [16]–[19]. It is therefore of major importance to specifically target HIV-1 replication in macrophages. In vitro, freshly isolated monocytes are almost refractory to HIV-1 infection and become permissive during differentiation into macrophages [20]–[23]. The differential susceptibility of monocytes and macrophages to HIV-1 is at least in part regulated by host factors [24]–[29]. Previously, we identified several host-genetic factors that were strongly associated with in vitro HIV-1 replication in macrophages [30], [31]. We observed that four SNPs in the phosphodiesterase 8A (PDE8A) gene were highly associated with HIV-1 replication [31]. This suggests that PDE8A plays an important role in HIV-1 replication in macrophages. Indeed, a recent RNAi screen identified PDE8A as a HIV-1 dependency factor [32]. PDE8A is a phosphodiesterase that hydrolyzes cyclic adenosine monophosphate (cAMP) to AMP [33]. Several studies indeed have shown a role for cAMP in HIV-1 infection and it was demonstrated that cAMP can affect several steps of the viral replication cycle ranging from entry to proviral transcription [34].
Here we analyzed the regulation of PDE8A expression during monocyte differentiation and cytokine polarization. Furthermore, we investigated the effect of PDE8A knockdown on HIV-1 replication.
Results
PDE8A expression during differentiation and polarization of macrophages
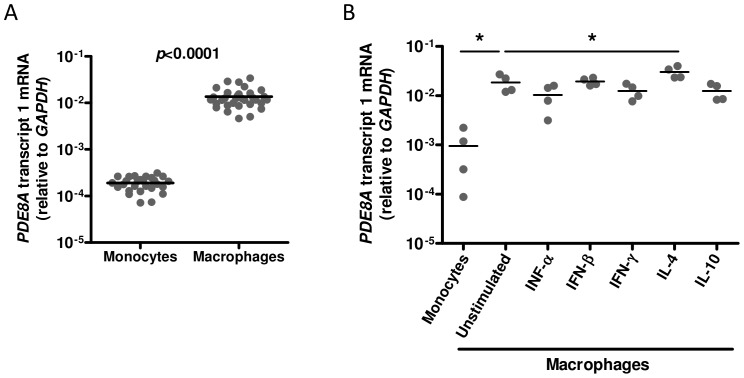
Previously, we showed that genetic polymorphisms in the PDE8A gene are strongly associated with HIV-1 replication in macrophages [30], [31]. In vitro, monocytes become highly susceptible to HIV-1 after differentiation into macrophages [20]–[23]. To determine whether PDE8A plays a role in the differential susceptibility of macrophages during differentiation, PDE8A mRNA expression was analyzed in freshly isolated monocytes and macrophages derived from 31 healthy blood donors. We observed on average a 70-fold increase in PDE8A expression upon differentiation of monocytes into macrophages, which suggests that PDE8A may be one of the factors that support the increased HIV-1 susceptibility of macrophages during differentiation (Figure 1A).
Figure 1. PDE8A expression during macrophage differentiation and polarisation.
(A) PDE8A mRNA expression in freshly isolated monocytes and macrophages cultured for 7 days from 32 donors. (B) PDE8A mRNA expression in freshly isolated monocytes and macrophages from 4 donors cultured in the absence or presence of IFN-α (250 U/ml), IFN-β (250 U/ml), IFN-γ (2501U/ml), IL-4 (10 ng/ml), or IL-10 (100 U/ml) for 7 days. Statistical differences were analyzed using a paired T test: *p<0.05, **p<0.01, ***p<0.001.
HIV-1 replication is strongly inhibited in macrophages stimulated with IFN-α, IFN-β, IFN-γ, IL-4, and IL-10 [22], [24], [35]–[41]. We analyzed whether differential expression of PDE8A during cytokine activation of macrophages may contribute to the decreased susceptibility of these cells to HIV-1 infection. Again, PDE8A mRNA expression increased during differentiation of monocytes into 5-day old macrophages (Figure 1B). Differentiation of monocytes in the presence of IFN-α, IFN-β, IFN-γ, or IL-10 did not change PDE8A expression, whereas the addition of IL-4 increased PDE8A expression (Figure 1B). This indicates that the restriction of HIV-1 replication observed in cytokine stimulated macrophages is not mediated by differential regulation of PDE8A expression.
PDE8A expression is regulated by miR-145-5p during differentiation of macrophages
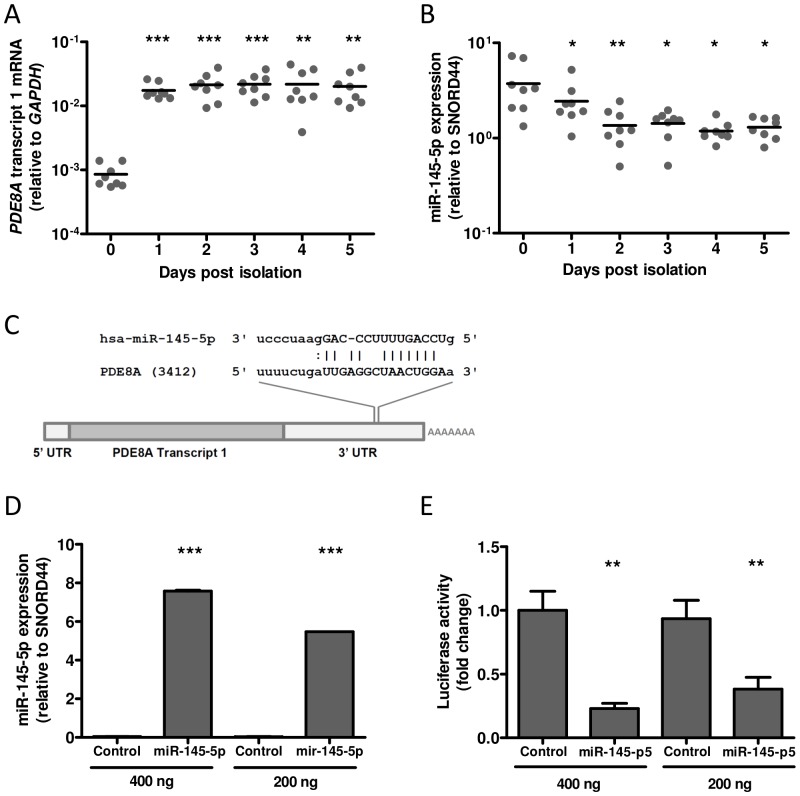
miRNAs are known to play a key role in post-transcriptional regulation of gene expression and recently it was observed that miRNAs are differentially expressed during maturation of monocytes and polarization of macrophages by cytokines [42], [43]. Therefore, we studied whether PDE8A expression is regulated by miRNAs during macrophage differentiation. miRNAs that target PDE8A mRNA were selected from miRNA-mRNA interactions that have been predicted and reported in the Ingenuity Knowledge Base, TarBase and miRecords and TargetScan [44]–[46]. Potential miRNAs regulating PDE8A expression were identified by pairing gene and miRNA expression data from monocytes and macrophages cultured for 5 days [43], [47]. Of the 190 miRNAs that potentially could target PDE8A, we found that miR-145-5p, miR-577 and miR-1280 were significantly downregulated in 5-day cultured macrophages as compared to monocytes, while PDE8A expression was upregulated (Table 1). To confirm these results, we determined PDE8A and miRNA expression during differentiation of monocytes into macrophages in 8 additional donors. PDE8A expression increased significantly during the first day of differentiation and this effect was maintained during differentiation (Figure 2A). In contrast, expression of miR-145-5p decreased significantly during the first day of differentiation and miR-145-5p remained low during subsequent differentiation (Figure 2B). Expression of miR-577 could not be confirmed by qPCR, whereas down-regulation of expression of miR-1280 was not observed (data not shown). miR-145-5p is predicted to target the 3′UTR of the PDE8A mRNA transcript (Figure 2C). To confirm whether miR-145-5p can regulate PDE8A expression, we constructed a miR-145-5p overexpression vector and a luciferase reporter vector in which the 3′UTR of the PDE8A mRNA transcript was cloned into the 3′UTR of the luciferase gene. First, HEK293T cells were transfected with different concentrations of the miR-145-5p vector and miR-145-5p expression levels were analyzed 2 days after transfection by qPCR. We observed a dose dependent increase of miR-145-5p expression as compared to the empty vector control (Figure 2D). Next, we performed co-transfections of the miR-145-5p overexpression vector and the luciferase reporter vector containing the predicted miR-145-5p target sequence. We observed that miR-145-5p is able to down regulate luciferase activity in a dose dependent manner (Figure 2E). This suggests that miR-145-5p is indeed able to target the 3′UTR of PDE8A mRNA thereby regulating protein expression levels.
Table 1. Potential miRNAs targeting PDE8A.
| miRNA ID | Fold Change miRNA Day 5 vs Day 0 # | Source | Confidence | Gene Symbol | Fold Change mRNA Day 5 vs Day 0 # |
| hsa-miR-145-5p | 0.102 | TargetScan Human | High (predicted) | PDE8A | 2.794 |
| hsa-miR-1280 | 0.098 | TargetScan Human | High (predicted) | PDE8A | 2.794 |
| hsa-miR-577 | 0.128 | TargetScan Human | High (predicted) | PDE8A | 2.794 |
Fold change in expression in which day 5 is compared to day 0; >1 is an increase and <1 is a decrease in expression.
Figure 2. Regulation of PDE8A expression by miR-145-5p during differentiation of monocytes into macrophages.
Confirmation of PDE8A mRNA (A) and miR-145-5p (B) expression during differentiation of monocytes into macrophages obtained from 8 donors. PDE8A mRNA or miR-145-5p expression during differentiation was compared with the expression at day 0 by using a paired T test: *p<0.05, **p<0.01, ***p<0.001. (C) Schematic overview of the PDE8A mRNA transcript 1 including the miR-145-5p binding site between base pair 3412 and 3435. (D) Expression levels of miR-145-5p determined by qPCR in HEK293T cells 2 days after transfection with an empty vector control or a vector containing a miR-145-5p expression cassette (n = 2, mean and SD). (E) Direct interaction between miR-145-5p and its target sequence in the PDE8A mRNA transcript was tested by co-transfection of p-hEF1a-miR-145-5p or an empty vector control and p-hEF1a-Luc-3′UTR PDE8A. Luciferase activity was measured 2 days post-transfection (n = 3, mean and SD). Statistical differences were analyzed using an un-paired T test: *p<0.05, **p<0.01, ***p<0.001.
PDE8A affects HIV-1 replication at the level of reverse transcription
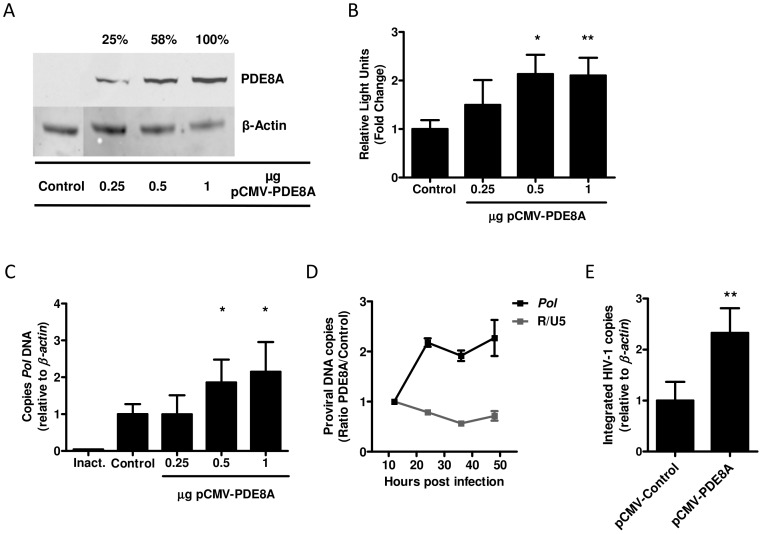
To determine which step of the replication cycle is affected by PDE8A we overexpressed a myc-tagged PDE8A in HEK293T cells and infected these cells with a VSV-G/NL4-3.Luc reporter virus. Overexpression of PDE8A resulted in a dose-dependent increase in luciferase activity (Figure 3A and 3B). This finding confirms our previous results and indicates that PDE8A supports HIV-1 replication. Next, we analyzed the effect of PDE8A overexpression on early steps of the viral replication cycle by analysis of proviral DNA levels during 48-hours post infection. HEK293T cells overexpressing PDE8A showed a dose dependent increase in Pol proviral DNA at 48-hours post infection (Figure 3C). The effect of PDE8A on Pol proviral DNA levels was already mediated within the first 24-hours post infection, whereas levels of strong stop proviral DNA as determined by R/U5 qPCR were not affected (Figure 3D). Furthermore, PDE8A overexpression resulted in increased levels of integrated HIV-1 provirus as determined by Alu-PCR (Figure 3E). This indicates that PDE8A supports HIV-1 replication at the level of reverse transcription.
Figure 3. PDE8A supports HIV-1 replication at the level of reverse transcription.
(A) HEK293T cells were transfected with different concentrations of pCMV6-PDE8A or an empty vector control. PDE8A expression was analyzed forty-eight hours after transfection by western blot. (B) HEK293T cells were transfected with different concentrations of pCMV6-PDE8A or an empty vector control and infected with VSV-G/NL4-3.Luc 48 hours after transfection. Luciferase activity was measured 2 days after infection (n = 3, mean and SD). (C) HEK293T cells were transfected with different concentrations of pCMV6-PDE8A or an empty vector control and infected with VSV-G/NL4-3-Ba-L 48 hours after transfection. Proviral DNA levels were analyzed forty-eight hours after infection by qPCR. Proviral DNA levels are expressed relative to the control after correction for β-actin levels in the same sample (n = 3, mean and SD). (D) HEK293T cells were transfected with 1 µg of pCMV6-PDE8A or 1 µg of empty vector control and infected with VSV-G/NL4-3-Ba-L 48 hours after transfection. R/U5 and Pol proviral DNA levels were analyzed by qPCR during 48 hours post-infection. R/U5 and Pol levels are expressed as the ratio of the expression in cells transfected with pCMV-PDE8A divided by the expression in cells that were transfected with the empty vector control and corrected for β-actin levels (n = 2, mean and SD). (E) HEK293T cells were transfected with 1 µg of pCMV6-PDE8A or 1 µg of the empty vector control and infected with VSV-G/NL4-3-Ba-L 48 hours after transfection. Integrated HIV-1 copies were determined 48 hours post infection by Alu-PCR and expressed relative to the control after correction for β-actin levels in the same sample (n = 2, mean and SD). Statistical differences were analyzed using an un-paired T test: *p<0.05, **p<0.01, ***p<0.001.
PDE8A supports HIV-1 replication in monocyte-derived macrophages
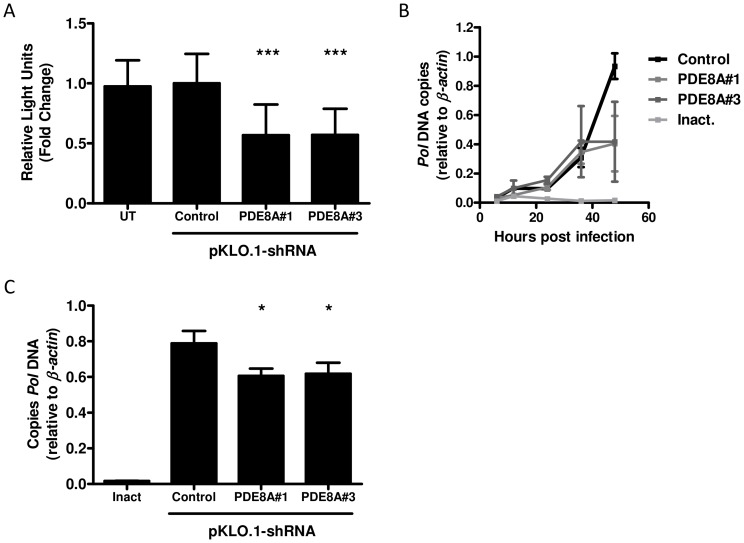
To determine the role of PDE8A in HIV-1 replication in macrophages, we analyzed the effect of PDE8A knockdown by shRNAs on the HIV-1 replication cycle in these cells. We selected two lentiviral vectors that were able to knockdown PDE8A expression (Figure S1A). Macrophages were transduced with the lentiviral vectors expressing either the shRNAs targeting PDE8A or a control shRNA which reduced PDE8A mRNA in most donors (Figure S1B). Subsequent infection with a VSV-G/NL-4-3.Luc reporter virus, resulted in a significant decrease in luciferase activity in the PDE8A knockdown cells (Figure 4A), demonstrating that HIV-1 replication in macrophages is supported by PDE8A. Next, the effect of PDE8A on proviral DNA synthesis was analyzed in macrophages. Knockdown of PDE8A expression resulted in a decrease in Pol proviral DNA levels at 48-hours post-infection (Figure 4B and 4C). This further confirms that PDE8A supports HIV-1 replication in macrophages and that this effect is mediated at the level of reverse transcription.
Figure 4. The effect of PDE8A knockdown on HIV-1 replication in macrophages.
(A) To analyze the effect of PDE8A knockdown on HIV-1 replication in macrophages, monocytes from 4 donors were cultured for 5 days and transduced with lentiviral vectors expressing shRNA control or two shRNA's targeting PDE8A. Forty-eight hours after the lentiviral transduction, macrophages were infected with VSV-G/NL4-3.Luc and luciferase activity was measured at day 2 after infection. The results are given as the mean fold luciferase expression from 4 donors, relative to the medium control. UT: Untransduced control. Statistical differences were analyzed by mixed linear model, repeated covariance: diagonal (IBM SPSS Statistics 20). (B) To determine the effect of PDE8A knockdown on Pol proviral DNA levels, monocytes in which PDE8A was downregulated by lentiviral transduction were infected with VSV-G/NL4-3-Ba-L. Pol proviral DNA levels were analyzed by qPCR during 48 hours post-infection and expressed relative to β-actin. Results are given as mean and sd from 2 donors. (C) Monocytes in which PDE8A was downregulated by lentiviral transduction were infected with VSV-G/NL4-3-Ba-L. Two days post-infection, proviral DNA levels were analyzed by qPCR for Pol. Proviral DNA levels are expressed relative to the control after correction to β-actin for input. Results shown are representative for 3 donors. Inact.: Inactivated virus. Statistical differences were analyzed using a paired T test: *p<0.05, **p<0.01, ***p<0.001.
Discussion
The HIV-1 genome encodes only 15 proteins and therefore HIV-1 is heavily dependent on host proteins for its replication. Host cell proteins that are required for efficient replication of HIV-1 in macrophages are attractive targets for new therapeutic approaches and therefore it is crucial to better understand the interaction between HIV-1 and these host factors. In our previous work, we have identified polymorphisms in PDE8A that are strongly associated with PDE8A expression and in vitro HIV-1 replication in macrophages [30], [31]. Here, we showed that PDE8A expression is highly upregulated during differentiation of monocytes into macrophages and that miR-145-5p may be involved in the regulation of PDE8A expression during differentiation. We demonstrated that PDE8A supports HIV-1 replication in macrophages and that this effect is mediated at the level of reverse transcription. These data suggest that PDE8A plays an important role in HIV-1 susceptibility of macrophages during differentiation [20]–[23].
PDE8A is a phosphodiesterase that regulates cAMP levels by hydrolyzing cAMP to AMP [33]. In the context of HIV-1 infection cAMP has been described as having opposing effects on the different steps of the viral replication cycle, which seems to be partially cell type dependent (reviewed by [34]). Here we show that increasing PDE8A expression levels are associated with higher concentrations of HIV-1 proviral DNA and subsequent higher levels of integrated HIV-1 provirus. This suggests that PDE8A supports HIV-1 replication at the level of reverse transcription. The increased proviral DNA synthesis in macrophages may be the result of low cAMP levels mediated by high PDE8A expression levels. Indeed, Thivierge et al. and Hayes et al. have shown that high cAMP levels decrease viral replication in macrophages [48], [49]. Thivierge et al. attributed this effect to decreased expression of co-receptor CCR5 in cells with high cAMP levels [48], however they did not determine the effect of cAMP on the different steps in viral replication and only analyzed virus production in the culture supernatant. Here we used a VSV-G pseudotyped reporter virus to circumvent CD4 and CCR5 mediated entry and demonstrated that PDE8A affects HIV-1 replication independent of CCR5 expression levels. Hayes et al. demonstrated that high cAMP levels decreased HIV-1 mRNA expression and viral replication in macrophages, but this may have been the result of decreased proviral DNA synthesis as the effect of high cAMP levels on proviral DNA synthesis was not determined in this study [49].
PDE8 isoforms exhibit an extremely high affinity for cAMP and it is therefore suggested that PDE8 enzymes have an important role in protecting any associated protein from fluctuations in basal cAMP concentrations [50]. Besides the direct effect of PDE8A on total cellular cAMP levels, it is also possible that PDE8A affects the replication cycle via a binding partner like RAF-1. It has been demonstrated that RAF-1 plays a role in HIV-1 infection in dendritic cells, and that it is required for the induction of proviral transcription [51]. PDE8A associates with RAF-1 and prevents its inactivation by phosphorylation by protein kinase A (PKA) [52]. However, we observed that knockdown of RAF-1 did not affect the ability of PDE8A to support HIV-1 replication (data not shown). This indicates that the effect of PDE8A on HIV-1 replication described here is not mediated through RAF-1.
Conclusions
Here we demonstrated that PDE8A supports HIV-1 replication in macrophages at the level of reverse transcription. PDE8A is highly expressed in macrophages and can be regulated by miR-145-5p during differentiation. Macrophages are considered to be a source of residual viral replication even under cART. Since PDE enzymes are considered promising targets for pharmacological intervention [53]–[56], blocking of PDE8A may specifically interfere with HIV-1 replication in primary macrophages.
Methods
Ethics statement
This study has been conducted in accordance with the ethical principles set out in the declaration of Helsinki, and was approved by the Medical Ethics Committee of the Academic Medical Center and the Ethics Advisory Body of the Sanquin Blood Supply Foundation in Amsterdam, The Netherlands. Written informed consent was obtained from all participants.
Cell culture
Peripheral blood mononuclear cells (PBMC) were obtained from buffy coats from healthy blood donors. PBMC were isolated by Ficoll-Isopaque density gradient centrifugation and subsequently monocytes were isolated by magnetic-activated bead technology using CD14+ magnetic microbeads (Miltenyi Biotec, Bergisch Gladbach, Germany). Monocytes were differentiated in Iscove's modified Dulbecco medium (IMDM) supplemented with 10% (v/v) heat-inactivated human pool serum (HPS), penicillin (100 U/ml), streptomycin (100 µg/ml) and cyproxin (5 µg/ml) in the presents or absence of IFN-α (250 U/ml), IFN-β (250 U/ml), IFN-γ (250 U/ml), IL-4 (10 ng/ml), or IL-10 (100 U/ml) and maintained in a humidified 10% CO2 incubator at 37°C. HEK293T cells were cultured in Dulbecco's Modified Eagle Medium without Hepes (DMEM) (Lonza, Basel, Switzerland) supplemented with 10% (v/v) inactivated fetal calf serum (FCS), penicillin (100 U/ml) and streptomycin (100 µg/ml), and maintained in a humidified 10% CO2 incubator at 37°C [57].
Plasmids
For PDE8A overexpression and testing knockdown efficiency of the shRNAs targeting PDE8A, a vector expressing a MYC-tagged PDE8A under the control of the CMV promotor (Origene, Rockville, MD, USA) was used. The vector containing the miR-145-5p overexpression cassette was created by cloning the stem-loop sequence of human miR-145-5p (miRBase accession number MI0000461) including approximately 100 base pairs up- and down-stream of the stem-loop in a HIV-1 based lentiviral expression vector pLV-hEF1a in which expression is driven by the human Elongation Factor 1 alpha promotor (p-LV-hEF1a-miR-145-5p) [58], [59]. The luciferase reporter vector containing the 3′UTR of the PDE8A mRNA transcript, which is targeted by miR-145-5p was constructed as follows: The miR-145-5p target sequence from 3′UTR of the PDE8A mRNA transcript, including flanking regions of 40 base pairs, was cloned into the 3′UTR sequence of a luciferase reporter gene in a pLV-pHEF1a-Luciferase vector in which expression is driven by the human Elongation Factor 1 alpha promotor (p-hEF1a-Luc-3′UTR PDE8A) [58], [59]. Primers used for cloning are listed in Table S1.
Virus production
YU2 and VSV-G pseudotyped NL4-3.Luc.R-E- luciferase reporter virus were produced by transfection of respectively pYU2 or pNL4-3.Luc.R-E- with pCMV-VSV-G in HEK293T cells. Lentiviral vectors were produced by co-transfection of pLV-CMV-GFP [58], [59] or pLKO.1 constructs expressing shRNA candidates from the MISSION TRC-Hs 1.0 library (PDE8A TRCN48874, PDE8A TRCN48876 and control SHC001; Sigma-Aldrich St. Louis, MO, USA) [60] and pCMV-VSV-G, pMDLgp and pRSV-Rev in HEK293T cells [61]. Transfections were performed with the calcium phosphate method. In short, plasmid DNA was diluted in 0.042M HEPES containing 0.15M CaCl2, subsequently mixed with an equal volume of 2× HEPES buffered saline pH 7.2, incubated at room temperature for 15 min and added to the culture medium. After 24 h incubation in a humidified 3% CO2 incubator at 37°C, the culture medium was replaced and cultures were continued at 10% CO2 at 37°C. Virus was harvested at 48 and 72 h after transfection and passed through a 0.22 µm filter. HIV-1 virus titers were quantified by determining the TCID50 on TZMBL, HEK293T or U87 cells [62]. Lentiviral vector supernatant was concentrated by centrifugation at 50,000xg for 2 hours directly after harvesting. Equal amounts of lentiviral vector as determined by p24 ELISA were used to inoculate target cells.
Infection of 293T cells
Cells were transfected as described previously with pCMV6-PDE8A [31]. Twenty-four hours post transfection cells were detached using trypsin (Invitrogen, Carlsbad, CA) and seeded in 24-wells plates to determine proviral DNA levels and in 96-wells plates to determine total HIV-1 replication. To determine proviral DNA levels, cells were inoculated at a multiplicity of infection (MOI) of 0.01 with VSV-G pseudotyped NL4-3-B-aL which was treated with DNAse (200 ng/ml) (RQ1; Promega Corp., Madison WI, USA) for 45 min at 37°C in medium containing 6 mM MgCl2. As a control, a heat-inactivated (30 min; 56 C) inoculum was used. During 48-hours hours post infection, total DNA was isolated using the L6 method [63]. Proviral DNA was measured by qPCR using primers and probes detecting R/U5 or Pol products (Table S1). To determine the effect of PDE8A on total HIV-1 replication, cells were inoculated at an MOI of 0.01 with VSV-G pseudotyped NL4-3.Luc.R-E- luciferase reporter virus. Forty-eight hours post infection, luciferase activity was determined as a measure for HIV-1 replication, by adding 25 µl substrate (0.83 mM ATP, 0.83 mM d-luciferin (Duchefa, Haarlem, The Netherlands), 18.7 mM MgCl2, 0.78 µM Na2H2P2O7, 38.9 mM Tris pH 7.8, 0.39% (v/v) glycerol, 0.03% (v/v) Triton X-100, and 2.6 µM dithiothreitol) directly to the culture medium. Luminescence was measured for 1 s per well using a luminometer (Berthold, Bad Wildbad, Germany).
Lentiviral vector transduction and HIV-1 infection of primary cells
Monocytes were cultured for 5 days and transduced with lentiviral vectors expressing shRNA control or two shRNA's targeting PDE8A. Medium was replaced with IMDM without serum or antibiotics and two hours later, macrophages were inoculated with lentiviral vectors at a MOI of 10. Sixteen hours post transduction, medium was replaced with IMDM supplemented with 10% (v/v) heat-inactivated human pool serum (HPS), penicillin (100 U/ml), streptomycin (100 µg/ml) and cyproxin (5 µg/ml). Forty-eight hours post transduction, macrophages were infected with VSV-G pseudotyped luciferase reporter virus at a MOI of 0.2 to analyze total replication. In addition, macrophages were inoculated at a MOI of 0.012 with DNAse-treated YU2 to analyze the effect on proviral DNA levels. Forty-eight hours post transfection luciferase activity was measured as described above.
Nucleic acid isolation and quantitative PCR
Total RNA was extracted using the High Pure RNA Isolation kit (Roche, Basel, Switzerland) or TriPure Isolation Reagent (Roche). Reverse transcription of mRNA was performed using the Roche Transcriptor First Strand cDNA Synthesis kit (Roche) using a maximum of 1 µg total RNA and oligo(dT) primers. Reverse transcription of miRNAs was performed using the qScript microRNA cDNA synthesis kit (Quanta BioScineces Inc., Gaithersburg, MD). Resulting cDNA was used for quantitative PCR (qPCR) analysis using SYBR Green I Master or Probes Master (Roche) and target specific primers (Table S1). For quantification of miR-145-5p and SNORD44 control, specifically designed primers (Table S1) were used in combination with the PerfeCTa Universal PCR Primer, including the Human positive control (SNORD44) primers (Quanta BioSciences Inc.). Integrated HIV-1 DNA was measured by two-step Alu-PCR as described previously [51]. In short, during the first step Alu-LTR sequences were amplified with an HIV-1-specific primer (LTR R region) and a primer that anneals to the abundant genomic Alu repeats. The HIV-1-specific primer was extended with a marker region at the 5′ end, which was used for specificity in the second-round PCR. The second step consisted out of a nested quantitative real-time PCR in which PCR products from the first step were amplified with primers annealing to the aforementioned marker region and a HIV-1 specific primer (LTR U5 region) (Table S1). To account for the signal contributed by unintegrated HIV-1 DNA, the first-round PCR was also done with the HIV-1-specific primer alone as a control. HIV-1 integration was normalized relative to β-actin DNA. qPCRs were performed on a Lightcycler 480 II (Roche) and gene expression values were obtained using Roche's LightCycler relative quantification software (release 1.5.0).
Western blot analysis
The effect of PDE8A overexpression and subsequent knockdown by shRNAs on protein levels was analyzed by western blot. Two days post transfection, HEK293T cells were lysed in RIPA-buffer (150 mM NaCl, 1% Triton X-100, 0.5% sodium deoxycholate, 0.1% SDS, 50 mM Tris, pH 8.0) containing Complete EDTA free protease inhibitor (Roche). After adding NuPAGE LDS 4× sample buffer (Invitrogen) and 0.1 M DTT, samples were heated at 95°C for 10 min. The Odyssey Protein Weight Marker was used as a size reference (LI-COR, Lincoln, NE, USA). Proteins were separated by SDS-PAGE (NuPAGE 10% Bis-Tris precast gel and MES SDS running buffer (Invitrogen) and transferred to a nitrocellulose membrane (Protran, Schleicher & Schuell, Dassel, Germany) using NuPAGE transfer buffer. After blocking for 2 hours with PBS containing 5% Protifar (Nutricia, Schiphol, The Netherlands) and 0.5% bovine serum albumin, the blot was incubated with OP10L anti-c-Myc antibody to detect MYC-tagged PDE8A (1∶5000; Calbiochem, San Diego, CA, USA), and SC-1616 anti-β-actin antibody (1∶200; Santa Cruz Biotechnology, Santa Cruz, CA, USA) to detect β-actin. IRDye 800CW conjugated Goat anti-Mouse IgG (1∶15000; 926-32210, LI-COR, Lincoln, NE, USA) and IRDye 680LT conjugated Donkey anti-Goat IgG (1∶15000; 926–32224, LI-COR) were used as secondary antibodies to visualize expression using the Odyssey infrared image system (LI-COR). Image J software was used to quantify protein expression.
miRNA target selection
Selected microRNAs that were predicted to target PDE8A mRNA were identified with the microRNA Target Filter tool from IPA (Ingenuity Systems Inc., Redwood City, CA, USA). Expression of miRNAs in monocytes and macrophages was characterized by next-generation sequencing with the SOLiD system and qPCR, EMBL-EBI ArrayExpress public database (http://www.ebi.ac.uk/arrayexpress/) accession number: EMTAB-1969 [43]. miRNA expression from 1 donor was paired with the mean expression of PDE8A from 2 donors obtained from gene expression data in similar samples (GSE35495), SubSeries GSE49240 (samples GSM1195728–39), part of the SuperSeries GSE35495 [47]; miRNAs were selected if expression levels were lower in macrophages, compared to monocytes.
Statistical analysis
For statistical analysis the paired and unpaired T-test or the mixed linear model, repeated covariance: diagonal were used (IBM SPSS Statistics 20).
Supporting Information
(A) Western Blot analysis of HEK293T cells in which the efficiency of the lentiviral vectors containing shRNAs against an MYC-tagged PDE8A or a control shRNA was determined. (B) Efficiency of PDE8A mRNA downregulation was analyzed by transduction of macrophages with lentiviral vectors expressing shRNAs against PDE8A or a control shRNA. PDE8A mRNA expression was determined 2 days post-transduction by qPCR. Statistical differences were analyzed using a paired T test.
(TIF)
Primers used for qPCRs and cloning.
(DOCX)
Acknowledgments
We are grateful to all blood donors from Sanquin Blood Bank for their participation in this study. Finally, we would like to thank Theo Geijtenbeek for critical reading of the manuscript.
Data Availability
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported by the Academic Medical Center of the University of Amsterdam and the Landsteiner Foundation of Blood Research (registration number 0526). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Carr JM, Hocking H, Li P, Burrell CJ (1999) Rapid and efficient cell-to-cell transmission of human immunodeficiency virus infection from monocyte-derived macrophages to peripheral blood lymphocytes. Virology 265: 319–329. [DOI] [PubMed] [Google Scholar]
- 2. Gendelman HE, Orenstein JM, Martin MA, Ferrua C, Mitra R, et al. (1988) Efficient isolation and propagation of human immunodeficiency virus on recombinant colony-stimulating factor 1-treated monocytes. J Exp Med 167: 1428–1441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Groot F, Welsch S, Sattentau QJ (2008) Efficient HIV-1 transmission from macrophages to T cells across transient virological synapses. Blood 111: 4660–4663. [DOI] [PubMed] [Google Scholar]
- 4. Gupta P, Collins KB, Ratner D, Watkins S, Naus GJ, et al. (2002) Memory CD4(+) T cells are the earliest detectable human immunodeficiency virus type 1 (HIV-1)-infected cells in the female genital mucosal tissue during HIV-1 transmission in an organ culture system. J Virol 76: 9868–9876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ho DD, Rota TR (1985) Schooley RT, Kaplan JC, Allan JD, et al (1985) Isolation of HTLV-III from cerebrospinal fluid and neural tissues of patients with neurologic syndromes related to the acquired immunodeficiency syndrome. N Engl J Med 313: 1493–1497. [DOI] [PubMed] [Google Scholar]
- 6. Mann DL, Gartner S, Le SF, Buchow H, Popovic M (1990) HIV-1 transmission and function of virus-infected monocytes/macrophages. J Immunol 144: 2152–2158. [PubMed] [Google Scholar]
- 7. Nicholson JKA, Cross GD, Callaway CS, McDougal JS (1986) In vitro infection of human monocytes with human T lymphotropic virus type III/lymphadenopathy-associated virus (HTLV-III/LAV). J Immunol 137: 323–329. [PubMed] [Google Scholar]
- 8. Olivetta E, Federico M (2006) HIV-1 Nef protects human-monocyte-derived macrophages from HIV-1-induced apoptosis. Exp Cell Res 312: 890–900. [DOI] [PubMed] [Google Scholar]
- 9. Swingler S, Mann AM, Zhou J, Swingler C, Stevenson M (2007) Apoptotic killing of HIV-1-infected macrophages is subverted by the viral envelope glycoprotein. PLoS Pathog 3: 1281–1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang H, Dornadula G, Beumont M, Livornese L Jr, Van UB, et al. (1998) Human immunodeficiency virus type 1 in the semen of men receiving highly active antiretroviral therapy. N Engl J Med 339: 1803–1809. [DOI] [PubMed] [Google Scholar]
- 11. Poles MA, Boscardin WJ, Elliott J, Taing P, Fuerst MM, et al. (2006) Lack of decay of HIV-1 in gut-associated lymphoid tissue reservoirs in maximally suppressed individuals. J Acquir Immune Defic Syndr 43: 65–68. [DOI] [PubMed] [Google Scholar]
- 12. Lambotte O, Chaix ML, Gasnault J, Goujard C, Lebras P, et al. (2005) Persistence of replication-competent HIV in the central nervous system despite long-term effective highly active antiretroviral therapy. AIDS 19: 217–218. [DOI] [PubMed] [Google Scholar]
- 13. Guadalupe M, Sankaran S, George MD, Reay E, Verhoeven D, et al. (2006) Viral suppression and immune restoration in the gastrointestinal mucosa of human immunodeficiency virus type 1-infected patients initiating therapy during primary or chronic infection. J Virol 80: 8236–8247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Chun TW, Nickle DC, Justement JS, Meyers JH, Roby G, et al. (2008) Persistence of HIV in gut-associated lymphoid tissue despite long-term antiretroviral therapy. J Infect Dis 197: 714–720. [DOI] [PubMed] [Google Scholar]
- 15. Mayer KH, Boswell S, Goldstein R, Lo W, Xu C, et al. (1999) Persistence of human immunodeficiency virus in semen after adding indinavir to combination antiretroviral therapy. Clin Infect Dis 28: 1252–1259. [DOI] [PubMed] [Google Scholar]
- 16. Crowe SM, Westhorpe CL, Mukhamedova N, Jaworowski A, Sviridov D, et al. (2010) The macrophage: the intersection between HIV infection and atherosclerosis. J Leukoc Biol 87: 589–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gonzalez-Scarano F, Martin-Garcia J (2005) The neuropathogenesis of AIDS. Nat Rev Immunol 5: 69–81. [DOI] [PubMed] [Google Scholar]
- 18. Hsue PY, Hunt PW, Schnell A, Kalapus SC, Hoh R, et al. (2009) Role of viral replication, antiretroviral therapy, and immunodeficiency in HIV-associated atherosclerosis. AIDS 23: 1059–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Huysentruyt LC, McGrath MS (2010) The role of macrophages in the development and progression of AIDS-related non-Hodgkin lymphoma. J Leukoc Biol 87: 627–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Rich EA, Chen IS, Zack JA, Leonard ML, O'Brien WA (1992) Increased susceptibility of differentiated mononuclear phagocytes to productive infection with human immunodeficiency virus-1 (HIV-1). J Clin Invest 89: 176–183 10.1172/JCI115559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Naif HM, Shan L, Alali M, Sloane A, Wu L, et al. (1998) CCR5 expression correlates with susceptibility of maturing monocytes to human immunodeficiency virus type 1 infection. J Virol 72: 830–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schuitemaker H, Kootstra NA, Koppelman MH, Bruisten SM, Huisman HG, et al. (1992) Proliferation-dependent HIV-1 infection of monocytes occurs during differentiation into macrophages. J Clin Invest 89: 1154–1160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sonza S, Maerz A, Deacon N, Meanger J, Mills J, et al. (1996) Human immunodeficiency virus type 1 replication is blocked prior to reverse transcription and integration in freshly isolated peripheral blood monocytes. J Virol 70: 3863–3869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cobos Jiménez V, Booiman T, de Taeye SW, van Dort KA, Rits MA, et al. (2012) Differential expression of HIV-1 interfering factors in monocyte-derived macrophages stimulated with polarizing cytokines or interferons. Sci Rep 2: 763 10.1038/srep00763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hrecka K, Hao C, Gierszewska M, Swanson SK, Kesik-Brodacka M, et al. (2011) Vpx relieves inhibition of HIV-1 infection of macrophages mediated by the SAMHD1 protein. Nature 474: 658–661 10.1038/nature10195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lahouassa H, Daddacha W, Hofmann H, Ayinde D, Logue EC, et al. (2012) SAMHD1 restricts the replication of human immunodeficiency virus type 1 by depleting the intracellular pool of deoxynucleoside triphosphates. Nat Immunol 13: 223–228 10.1038/ni.2236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goldstone DC, Ennis-Adeniran V, Hedden JJ, Groom HC, Rice GI, et al.. (2011) HIV-1 restriction factor SAMHD1 is a deoxynucleoside triphosphate triphosphohydrolase. Nature. doi: 10.1038/nature10623. [DOI] [PubMed]
- 28. White TE, Brandariz-Nunez A, Valle-Casuso JC, Amie S, Nguyen LA, et al. (2013) The retroviral restriction ability of SAMHD1, but not its deoxynucleotide triphosphohydrolase activity, is regulated by phosphorylation. Cell Host Microbe 13: 441–451 10.1016/j.chom.2013.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Allouch A, David A, Amie SM, Lahouassa H, Chartier L, et al. (2013) p21-mediated RNR2 repression restricts HIV-1 replication in macrophages by inhibiting dNTP biosynthesis pathway. Proc Natl Acad Sci U S A 110: E3997–E4006 10.1073/pnas.1306719110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bol SM, Moerland PD, Limou S, van RY, Coulonges C, et al. (2011) Genome-Wide Association Study Identifies Single Nucleotide Polymorphism in DYRK1A Associated with Replication of HIV-1 in Monocyte-Derived Macrophages. PLoS One 6: e17190 10.1371/journal.pone.0017190 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bol SM, Booiman T, Bunnik EM, Moerland PD, van DK, et al. (2011) Polymorphism in HIV-1 dependency factor PDE8A affects mRNA level and HIV-1 replication in primary macrophages. Virology 420: 32–42 S0042-6822(11)00376-X [pii]; 10.1016/j.virol.2011.08.013 [doi] [DOI] [PubMed] [Google Scholar]
- 32. Zhou H, Xu M, Huang Q, Gates AT, Zhang XD, et al. (2008) Genome-scale RNAi screen for host factors required for HIV replication. Cell Host Microbe 4: 495–504 S1931-3128(08)00330-2 [pii]; 10.1016/j.chom.2008.10.004 [doi] [DOI] [PubMed] [Google Scholar]
- 33. Fisher DA, Smith JF, Pillar JS, St Denis SH, Cheng JB (1998) Isolation and characterization of PDE8A, a novel human cAMP-specific phosphodiesterase. Biochem Biophys Res Commun 246: 570–577 S0006-291X(98)98684-3 [pii]; 10.1006/bbrc.1998.8684 [doi] [DOI] [PubMed] [Google Scholar]
- 34. Moreno-Fernandez ME, Rueda CM, Velilla PA, Rugeles MT, Chougnet CA (2012) cAMP during HIV infection: friend or foe? AIDS Res Hum Retroviruses 28: 49–53 10.1089/AID.2011.0265 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Naif H, Ho-Shon M, Chang J, Cunningham AL (1994) Molecular mechanisms of IL-4 effect on HIV expression in promonocytic cell lines and primary human monocytes. J Leukoc Biol 56: 335–339. [DOI] [PubMed] [Google Scholar]
- 36. Montaner LJ, Griffin P, Gordon S (1994) Interleukin 10 inhibits initial reverse transcription of human immunodeficiency virus type 1 and mediates a virostatic latent state in primary blood-derived human macrophages in vitro. J Gen Virol 75: 3393–3400. [DOI] [PubMed] [Google Scholar]
- 37. Montaner LJ, Bailer RT, Gordon S (1997) IL-13 acts on macrophages to block the completion of reverse transcription, inhibit virus production, and reduce virus infectivity. J Leukoc Biol 62: 126–132. [DOI] [PubMed] [Google Scholar]
- 38. Montaner LJ, da Silva RP, Sun J, Sutterwala S, Hollinshead M, et al. (1999) Type 1 and type 2 cytokine regulation of macrophage endocytosis: differential activation by IL-4/IL-13 as opposed to IFN-gamma or IL-10. J Immunol 162: 4606–4613. [PubMed] [Google Scholar]
- 39. Kootstra NA, van 't Wout A, Huisman HG, Miedema F, Schuitemaker H (1994) Interference of interleukin-10 with human immunodeficiency virus type 1 replication in primary monocyte-derived macrophages. J Virol 68: 6967–6975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Cassol E, Cassetta L, Rizzi C, Alfano M, Poli G (2009) M1 and M2a polarization of human monocyte-derived macrophages inhibits HIV-1 replication by distinct mechanisms. J Immunol 182: 6237–6246 182/10/6237 [pii]; 10.4049/jimmunol.0803447 [doi] [DOI] [PubMed] [Google Scholar]
- 41. Cassol E, Cassetta L, Alfano M, Poli G (2010) Macrophage polarization and HIV-1 infection. J Leukoc Biol 87: 599–608 jlb.1009673 [pii]; 10.1189/jlb.1009673 [doi] [DOI] [PubMed] [Google Scholar]
- 42. Graff JW, Dickson AM, Clay G, McCaffrey AP, Wilson ME (2012) Identifying functional microRNAs in macrophages with polarized phenotypes. J Biol Chem 287: 21816–21825 M111.327031 [pii]; 10.1074/jbc.M111.327031 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Cobos Jiménez V, Bradley EJ, Willemsen AM, van Kampen AH, Baas F, et al. (2014) Next-generation sequencing of microRNAs uncovers expression signatures in polarized macrophages. Physiol Genomics 46: 91–103 physiolgenomics.00140.2013 [pii]; 10.1152/physiolgenomics.00140.2013 [doi] [DOI] [PubMed] [Google Scholar]
- 44. Vergoulis T, Vlachos IS, Alexiou P, Georgakilas G, Maragkakis M, et al. (2012) TarBase 6.0: capturing the exponential growth of miRNA targets with experimental support. Nucleic Acids Res 40: D222–D229 gkr1161 [pii]; 10.1093/nar/gkr1161 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Xiao F, Zuo Z, Cai G, Kang S, Gao X, et al. (2009) miRecords: an integrated resource for microRNA-target interactions. Nucleic Acids Res 37: D105–D110 gkn851 [pii]; 10.1093/nar/gkn851 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Garcia DM, Baek D, Shin C, Bell GW, Grimson A, et al. (2011) Weak seed-pairing stability and high target-site abundance decrease the proficiency of lsy-6 and other microRNAs. Nat Struct Mol Biol 18: 1139–1146 nsmb.2115 [pii]; 10.1038/nsmb.2115 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Martinez FO, Helming L, Milde R, Varin A, Melgert BN, et al. (2013) Genetic programs expressed in resting and IL-4 alternatively activated mouse and human macrophages: similarities and differences. Blood 121: e57–e69 blood-2012-06-436212 [pii]; 10.1182/blood-2012-06-436212 [doi] [DOI] [PubMed] [Google Scholar]
- 48. Thivierge M, Le Gouill C, Tremblay MJ, Stankova J, Rola-Pleszczynski M (1998) Prostaglandin E2 induces resistance to human immunodeficiency virus-1 infection in monocyte-derived macrophages: downregulation of CCR5 expression by cyclic adenosine monophosphate. Blood 92: 40–45. [PubMed] [Google Scholar]
- 49.Hayes MM, Lane BR, King SR, Markovitz DM, Coffey MJ (2002) Prostaglandin E(2) inhibits replication of HIV-1 in macrophages through activation of protein kinase A. Cell Immunol 215: : 61–71. S0008874902000175 [pii]. [DOI] [PubMed] [Google Scholar]
- 50. Soderling SH, Bayuga SJ, Beavo JA (1998) Cloning and characterization of a cAMP-specific cyclic nucleotide phosphodiesterase. Proc Natl Acad Sci U S A 95: 8991–8996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Gringhuis SI, van der Vlist V, van den Berg LM, den DJ, Litjens M, et al. (2010) HIV-1 exploits innate signaling by TLR8 and DC-SIGN for productive infection of dendritic cells. Nat Immunol 11: 419–426 ni.1858 [pii]; 10.1038/ni.1858 [doi] [DOI] [PubMed] [Google Scholar]
- 52. Brown KM, Day JP, Huston E, Zimmermann B, Hampel K, et al. (2013) Phosphodiesterase-8A binds to and regulates Raf-1 kinase. Proc Natl Acad Sci U S A 110: E1533–E1542 1303004110 [pii]; 10.1073/pnas.1303004110 [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Francis SH, Houslay MD, Conti M (2011) Phosphodiesterase inhibitors: factors that influence potency, selectivity, and action. Handb Exp Pharmacol 47–84. 10.1007/978-3-642-17969-3_2 [doi]. [DOI] [PubMed]
- 54. Schwartz BG, Kloner RA (2010) Drug interactions with phosphodiesterase-5 inhibitors used for the treatment of erectile dysfunction or pulmonary hypertension. Circulation 122: 88–95 122/1/88 [pii]; 10.1161/CIRCULATIONAHA.110.944603 [doi] [DOI] [PubMed] [Google Scholar]
- 55. Giembycz MA, Field SK (2010) Roflumilast: first phosphodiesterase 4 inhibitor approved for treatment of COPD. Drug Des Devel Ther 4: 147–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Zhang HT (2009) Cyclic AMP-specific phosphodiesterase-4 as a target for the development of antidepressant drugs. Curr Pharm Des 15: 1688–1698. [DOI] [PubMed] [Google Scholar]
- 57. Pear WS, Nolan GP, Scott ML, Baltimore D (1993) Production of high-titer helper-free retroviruses by transient transfection. Proc Natl Acad Sci U S A 90: 8392–8396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Follenzi A, Ailles LE, Bakovic S, Geuna M, Naldini L (2000) Gene transfer by lentiviral vectors is limited by nuclear translocation and rescued by HIV-1 pol sequences. Nat Genet 25: 217–222 10.1038/76095 [doi] [DOI] [PubMed] [Google Scholar]
- 59. Kootstra NA, Munk C, Tonnu N, Landau NR, Verma IM (2003) Abrogation of postentry restriction of HIV-1-based lentiviral vector transduction in simian cells. Proc Natl Acad Sci U S A 100: 1298–1303 10.1073/pnas.0337541100 [doi];0337541100 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Root DE, Hacohen N, Hahn WC, Lander ES, Sabatini DM (2006) Genome-scale loss-of-function screening with a lentiviral RNAi library. Nat Methods 3: 715–719 nmeth924 [pii]; 10.1038/nmeth924 [doi] [DOI] [PubMed] [Google Scholar]
- 61. Dull T, Zufferey R, Kelly M, Mandel RJ, Nguyen M, et al. (1998) A third-generation lentivirus vector with a conditional packaging system. J Virol 72: 8463–8471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. van 't Wout AB, Schuitemaker H, Kootstra NA (2008) Isolation and propagation of HIV-1 on peripheral blood mononuclear cells. Nat Protoc 3: 363–370. [DOI] [PubMed] [Google Scholar]
- 63. Kootstra NA, Schuitemaker H (1999) Phenotype of HIV-1 lacking a functional nuclear localization signal in matrix protein of gag and Vpr is comparable to wild-type HIV-1 in primary macrophages. Virology 253: 170–180. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(A) Western Blot analysis of HEK293T cells in which the efficiency of the lentiviral vectors containing shRNAs against an MYC-tagged PDE8A or a control shRNA was determined. (B) Efficiency of PDE8A mRNA downregulation was analyzed by transduction of macrophages with lentiviral vectors expressing shRNAs against PDE8A or a control shRNA. PDE8A mRNA expression was determined 2 days post-transduction by qPCR. Statistical differences were analyzed using a paired T test.
(TIF)
Primers used for qPCRs and cloning.
(DOCX)
Data Availability Statement
The authors confirm that all data underlying the findings are fully available without restriction. All relevant data are within the paper and its Supporting Information files.