Abstract
Background:
Knowledge and attitude are significant factors impinging on whether individuals seek healthcare service. This flows on to impact public health knowledge of prevalence of diseases, and in turn, the practice of preventive medicine. As part of the international research collaboration agenda for Prediabetes and Cardiovascular Complications Study, a preliminary survey of one of the Ndokwa communities of Nigeria has been carried out.
Aim:
This study was to understand the baseline knowledge, attitudes and practices of a rural community in regards to cardiovascular diseases, and behavior toward risk management.
Materials and Methods:
Seventy-four volunteer participants were recruited, after public lectures, through secondary school and churches in the community. The survey was done using questionnaire. The knowledge component comprised questions about educational and personal health opinion. The attitude and practice components comprised questions about exercises and visiting healthcare facilities. Occupational backgrounds were also asked.
Results:
It is observed that majority of the community dwellers have (1) completed at least secondary education, (2) never attended a health check-up; and (3) do not engage in physical activity in the context of exercise. Twenty of the participants indicated not being in good health, of which only 35% have attended medical check-up for their ailment. Many of those who are yet to seek healthcare service cite affordability as their reason. With specific regards to diabetes and cardiovascular risk, over 71% of the survey participants are yet to do any blood sugar and/or lipid profile tests.
Conclusion:
This preliminary survey indicates that although the majority of respondents have secondary education and therefore are relatively literate, there is a gap between their knowledge of ill-health versus attitude and practice toward prevention; especially cardiovascular and diabetes diseases.
Keywords: Cardiovascular disease, Diabetes, Low-mid income communities, Public health
Introduction
CVD risk factors, a burden to developing countries
Cardiovascular diseases (CVD) are well established as leading contributors to the burden of diseases in the developing countries,[1,2] as well as the developed world. An estimated 16.7 million, or 29.2% of total global deaths, result from the various forms of CVDs, many of which are preventable by action on the major primary risk factors such as unhealthy diet, physical inactivity and smoking.[3]
Eight risk factors of CVDs account for 61% of cardiovascular deaths and they include alcohol use, tobacco use, high blood pressure, high body mass index/adibosity, high blood cholesterol and glucose, low fruit and vegetable intake, and physical inactivity.[3] However, the burden of these CVD risk factors together with the long prevalence of infectious diseases strangulates the health systems. Convergence of non-communicable and infectious diseases puts new challenges and opportunities to enact responsive changes in policy and research.[4] According to the WHO, despite the fact that these major CVD risk factors are associated with high-income countries, more than 84% of the total global burden of the disease they cause occurs in low- and middle-income countries.[3] Low impact of anti-smoking lobby, lack of facilities for screening at early stages and lack of awareness to CVD risk factors in the developing countries may be contributory factors to high disease burden.
In sub-Saharan Africa, there is significant burden of CVD risks coupled with the burden of infectious diseases. One of the worrisome scenarios is the substantial economic burden in the population at large and in households.[5] Some settings have reported prevalence rates of 86% for diabetes,[6] and 42.5% for hypertension[7] in sub-populations of Nigeria. Diabetes and hypertension have been described as the leading CVD risk factors responsible for the growing CVD burden,[8] but the epidemiology and the burden they inflict on the sub-Saharan nations have not been clearly elucidated, leading to several deaths from CVD unaccounted for.
Knowledge, attitude and practice (KAP) gaps
Data on the knowledge, attitudes and practices (KAP) of the rural communities on the morbidity and mortality of the metabolic syndrome and its associated diabetes and CVD risk is lacking in literature. KAP seeks to identify what people know about their behaviors that predisposes them to the morbidity and mortality of diabetes and CVD, how they feel about such behaviors and what they do, either in response to such behaviors or managements procedures toward the chronic health condition. According to Paul Zimmet and his group,[9] KAP studies can be used for diagnostic purposes since they describe the population's current knowledge, attitude and practice. Secondly they can be implemented to increase insights in a current situation and help design appropriate specific interventions.[10] Thirdly, they can be used as an evaluation tool to evaluate the effectiveness of certain interventions or programmes. In these regards, electronic media is emerging as a useful tool in health interventions,[11,12] including diabetes and other chronic diseases.[13,14]
Objective of the survey
It has been reported that 75% of patients do not know the symptoms of heart diseases, while 91% had never been told about CVD prevention by their doctors.[2] Given the remoteness of Ndokwa communities from the state and federal capital cities; combined with the level of available health campaigns and facilities, it is presumed in this survey that majority of the population may have yet to know about their CVD risk, or attend any CVD risk screening. Therefore, the KAP regarding CVD risk factors is worth identifying in the adult population Ndokwa community. This objective of this preliminary survey is to understand the baseline knowledge, attitudes and practices of the rural community in regards to CVD and diabetes, including their behavior toward risk management. It shall lead into phase one of Prediabetes and Cardiovascular Complications Study (PACCS), to identify the KAP of the people of Ndokwa West local government area of Nigeria.
The research overview or protocol of PACCS has been described[15] and the over-reaching study aims is to develop a screening protocol for the risk of future CVD and diabetes mellitus in people with prediabetes and undiagnosed diabetes; as well as to establish a framework for early identification and intervention of prediabetes including strategies for holistic management and monitoring of progression.
Materials and Methods
Ahead of commencement of phase one of the longitudinal study, a preliminary assessment was conducted in June 2013 to identify needs and gaps in the study area, in order to tailor research activities appropriately. Ethics approval was obtained from Human Research Ethics Committee of Novena University and the Local Government Ministry of Health at Kwale, Delta State Nigeria.
Study setting
The study setting is based on PACCS. Abbi community housing a Primary Health Care center within the Local council was selected for the study. The mixed secondary/high (Abbi Grammar School) institution was contacted through the principal for a public lecture and recruitment of participants among the staff and students. Churches in the community were also contacted through their respective pastors. In all cases public lectures were followed by provision of information sheets as well as consent forms and questionnaires. Seventy four volunteers, of equal number (37) of each gender, complied/responded and were included in the pilot screening. Exclusion criteria were age less than 18 years or greater than 60 years, if the subject had previous diagnosis of diabetes, and the inability to provide contacts for future follow-up should screening for MS and prediabetes be positive.
A questionnaire from Stanford Patient Education Research Centre was modified to target the general population and gather vital information. The questionnaire was grouped into seven sections that encompassed:
Knowledge questions’ set 1: Educational and occupational background of participants,
Knowledge questions’ set 2: Opinion on their general health condition,
Attitude and practice questions’ set 3: Monitoring for CVD risk factors they have performed or that have been done on them,
Attitude and practice questions’ set 4: Exercise activities that they do.
Daily activities, dietary habit and existing symptoms of disease were other information collected; which would be analysed later. Data was keyed into excel sheet and analysed using IBM SPSS Statistics 22. Cross-tabulations were generated and evaluated. Also their knowledge of having a disease condition in relation to gender difference was assessed.
KAP was evaluated by determining the percent of those whose health status require healthcare, but failed to seek for such service. This was achieved by stratifying participants’ opinion on their general health condition, and then cross-checking with responses on the questionnaire regarding visiting clinic and/or monitoring for CVD risk factors they have performed or have been done on them.
Results
The study had 74 participants of 120 shared questionnaires, out of which 37 (50%) were males and 37 (50%) were females. The age of participants ranged between 18 and 74 years. The age group 45-54 years has the highest number of respondents [Table 1]. Educational and occupational status is given in Table 2.
Table 1.
Age and sex distribution of respondents
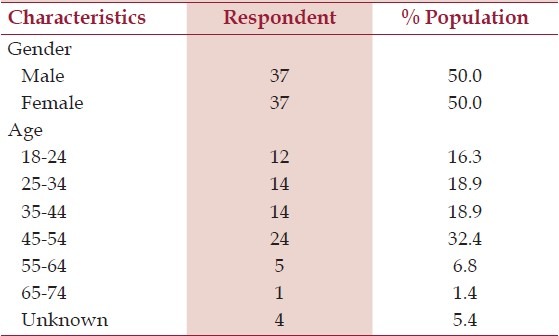
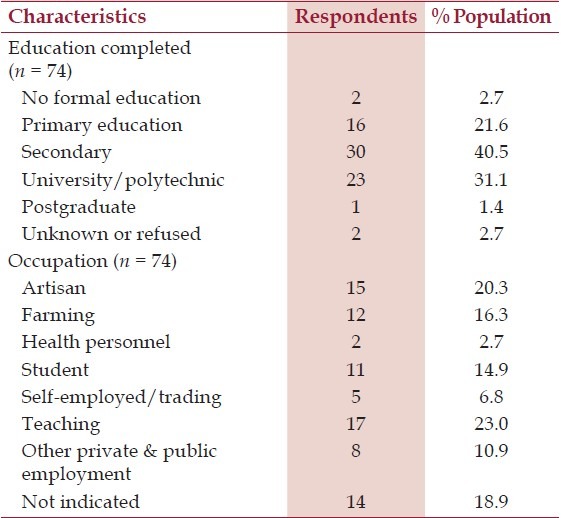
Table 2.
Educational and occupational distribution of respondents
Summarizes responses to questions used to assess knowledge, and attitude about CVD/health risk factors are also presented [Table 3]. Four major physical activities were identified among participants. The percentage of physical activities they engaged during last 4 weeks is shown in Figure 1.
Table 3.
Summary of knowledge and att itude about CVD risk factors
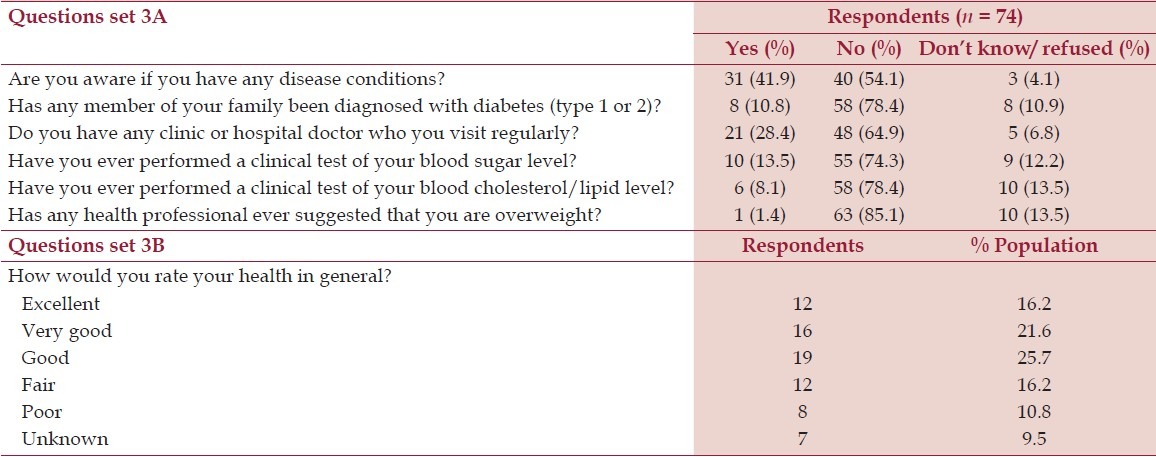
Figure 1.

Percentage of physical activities engaged by participants during last 4 weeks
Twenty participants indicated that their health conditions are not good, but only seven have visited a clinic for check-up. Further, only 39.2% of the population can remember having attended a health facility for check-up; less have performed test for blood glucose level (BGL) or lipid profile [Figure 2]. The participants’ responses to reasons for not seeking medical attention were “There is no reason”, “There is no ill-health”, “I hardly fall sick”, “I am healthy”, “My health is good”, “It's expensive”, “No money to attend regular check-up”, “Due to financial problem”.
Figure 2.
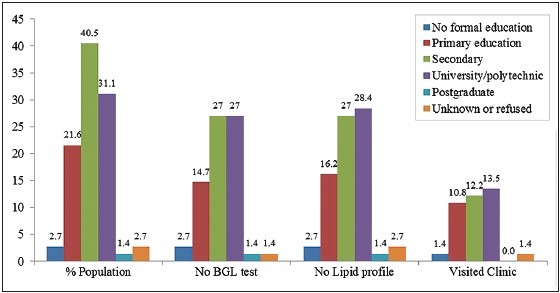
Percentage of population who never visited health facility
The proportion of participants that responded of having knowledge of suffering a disease condition is presented in Figure 3. Among the 41.9% respondents that confirmed having a disease condition, 9.5% have high blood pressure and 1.4% affirmed to be suffering from diabetes [Figure 3].
Figure 3.
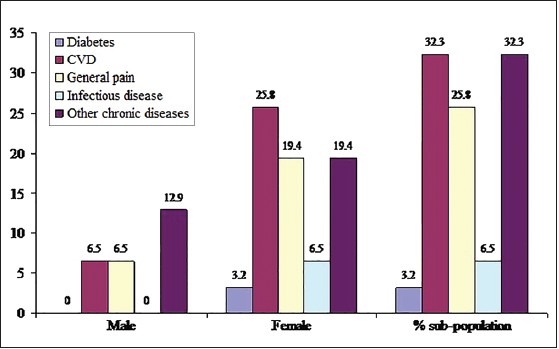
Prevalence of diseases according to participants’ knowledge
Discussion
This survey has included participants considered to be adult age from 18-years old [Table 1]. Reviewing the volunteers as a representation of the study population, it is observed that over 71% have achieved secondary school education or higher. In the context of physical activity, it is observed that only about 16.3% are in a physically demanding occupation [Table 2].
Assessment of the participants’ responses to questions regarding physical activity indicates that most people do not engage in exercise. For instance, it is observed that 64.9% do not do swimming exercise, while only 1.4% does it for >3 hrs/week. The exercise activity most frequently done is bicycling and walking with 16.2% engaging in either of the two for over 3 hrs/week [Figure 1].
In evaluation of KAP, 20 participants indicated that their health conditions are poor or below good, of which only seven have visited a clinic for check-up. The other 13 translates to 65% of those who have knowledge of ill-health, but with KAP gap. This study shows that only 39.2% of the population can ever remember having attended a health facility for check-up [Figure 2], though only 28.4% do so regularly [Table 3]. With such KAP deficiency the people may not have relevant information that can inform their health condition and enhance the attitude of health seeking behavior. Among those who have never visited a clinic, 10.4% of the sub-population does not have any reason for not visiting clinic or doctor [Table 3]. This can be viewed as nonchalant attitude to health. Eight (16.7%) of our respondents believed that not falling ill or being apparently healthy is good enough reason not to seek health checks. This is the context where CVD risk assessment tools are important especially for prediabetes and pre-hypertension. Health literacy impacts on the effectiveness of chronic disease management of which patient self-management is a central pillar.[16,17] Self-management, which is a pillar of chronic disease management is unachievable if patients are unaware of their condition.[18] Poor health literacy is also associated with socio-demographic factors such as age, socioeconomic status, and education levels.[17,19] This could be seen in 10 (13.5%) respondents in our study who claimed that their poor financial status is a reason for not seeking health checks with a doctor or clinic. Further observation from the survey revealed that about three quarter of the population have never done blood glucose check or lipid profile [Figure 2]. While there is no formal country (Nigeria) specific guideline for CVD prevention and management, this high proportion of the population represents the KAP gap regarding CVD risk within the community. In other words, if any existing risk in this population progresses to overt CVD, there could be an epidemic that the public healthcare department may be unprepared for.
We assessed the population in regard to their knowledge of disease condition. It seems that females have greater number of diseases. For instance, seven women indicated having suffered hypertension, whereas only one male participant indicated so. Among the top six diseases prevalent in the community, females show to have 25.8% of CVD conditions, while males show relatively low knowledge of these disease conditions [Figure 3]. According to Uchenna and his group,[2] 83.5% had not checked their blood cholesterol in the last 18 months. While their result corroborates with our finding, they differ in setting being that they sampled patients attending a specialist clinic. KAP gap on CVD risk factors is not relative only to patients but also to clinicians. Despite the relevance of this topic, clinical awareness is still unsatisfactory.[20] A report in the UK investigated 34 general practitioners’ knowledge and attitudes to impaired glucose tolerance and the results indicate that awareness of the existence of impaired glucose tolerance was satisfactory but that consciousness of the prevalence and clinical significance of impaired glucose tolerance was poor: 16 (47%) participants were unaware of the risk of impaired glucose tolerance progressing to type 2 diabetes mellitus, and 21 (62%) were unaware of the increased risk of CVD.[21] There is therefore, the need for concerted effort for health education about CVD risk factors in these communities and such health education should be informed using lay perceptions in order to maximize the appropriateness of the message and their effect on knowledge, attitude and behavior.[22]
Conclusions
This preliminary survey indicates a high proportion of the population not seeking medical attention for various reasons. The scenario was borne out of perceived knowledge, attitude and practice of the people toward CVD risk factors; and appropriate health education, measures to improve affordability and accessibility to health interventions would be an important tenet to increase KAP gaps and CVD prevention and management.
Acknowledgment
This work was made possible by support provided by Charles Darwin University to Dr Uba Nwose. The work is been supported by the Director of Friends Laboratory Obiaruku; the Principal of Abbi Grammar School Abbi; and Ndokwa West local government of Nigeria.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: Systematic analysis of population health data. Lancet. 2006;367:1747–57. doi: 10.1016/S0140-6736(06)68770-9. [DOI] [PubMed] [Google Scholar]
- 2.Uchenna D, Ambakederemo T, Jesuorobo D. Awareness of heart disease prevention among patients attending a specialist clinic in Southern Nigeria. Int J Prev Treat. 2012;1:40–3. [Google Scholar]
- 3.WHO. Global atlas on cardiovascular disease prevention and control. 2011. [July 9, 2014]. at http://www.who.int/cardiovascular_diseases/publications/atlas_cvd/en/# .
- 4.Remais JV, Zeng G, Li G, Tian L, Engelgau MM. Convergence of non-communicable and infectious diseases in low- and middle-income countries. Int J Epidemiol. 2013;42:221–7. doi: 10.1093/ije/dys135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fuster V, Kelly BB, Vedanthan R. Promoting global cardiovascular health: Moving forward. Circulation. 2011;123:1671–8. doi: 10.1161/CIRCULATIONAHA.110.009522. [DOI] [PubMed] [Google Scholar]
- 6.Udenze IC, Azinge EC, Arikawe AP, Egbuagha EU, Onyenekwu C, Ayodele O, et al. The prevalence of metabolic syndrome in persons with type 2 diabetes at the lagos university teaching hospital, Lagos, Nigeria. West Afr J Med. 2013;32:126–32. [PubMed] [Google Scholar]
- 7.Akintunde AA, Ayodele OE, Akinwusi PO, Opadijo GO. Metabolic syndrome: Comparison of occurrence using three definitions in hypertensive patients. Clin Med Res. 2011;9:26–31. doi: 10.3121/cmr.2010.902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choukem SP, Kengne AP, Dehayem YM, Simo NL, Mbanya JC. Hypertension in people with diabetes in sub-Saharan Africa: Revealing the hidden face of the iceberg. Diabetes Res Clin Pract. 2007;77:293–9. doi: 10.1016/j.diabres.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Zimmet P, de Courten M, Hodge AM, Tuomilehto J. The Epidemiology of Diabetes Mellitus. USA: John Wiley & Sons, Ltd; 2002. Epidemiology, Evidence for Prevention: Type 2 Diabetes; pp. 41–9. [Google Scholar]
- 10.Harris J, Felix L, Miners A, Murray E, Michie S, Ferguson E, et al. Adaptive e-learning to improve dietary behaviour: A systematic review and cost-effectiveness analysis. Health Technol Assess. 2011;15:1–160. doi: 10.3310/hta15370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hieftje K, Edelman EJ, Camenga DR, Fiellin LE. Electronic media-based health interventions promoting behavior change in youth: A systematic review. JAMA Pediatr. 2013;167:574–80. doi: 10.1001/jamapediatrics.2013.1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jham BC, Duraes GV, Strassler HE, Sensi LG. Joining the podcast revolution. J Dent Educ. 2008;72:278–81. [PubMed] [Google Scholar]
- 13.Stellefson M, Chaney B, Barry AE, Chavarria E, Tennant B, Walsh-Childers K, et al. Web 2.0 chronic disease self-management for older adults: A systematic review. J Med Internet Res. 2013;15:e35. doi: 10.2196/jmir.2439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gruber D. Consumer engagement for diabetes technology: Easier said than done. J Diabetes Sci Technol. 2010;4:754–8. doi: 10.1177/193229681000400333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nwose EU, Richards RS, Digban K, Bwititi PT, Ennis G, Yee KC, et al. Cardiovascular risk assessment in prediabetes and undiagnosed diabetes mellitus study: International collaboration research overview. N Am J Med Sci. 2013;5:625–30. doi: 10.4103/1947-2714.122303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barber MN, Staples M, Osborne RH, Clerehan R, Elder C, Buchbinder R. Up to a quarter of the Australian population may have suboptimal health literacy depending upon the measurement tool: Results from a population-based survey. Health Promot Int. 2009;24:252–61. doi: 10.1093/heapro/dap022. [DOI] [PubMed] [Google Scholar]
- 17.Adams RJ, Stocks NP, Wislon DH, Hill CL, Gravier S, Kickbusch I, et al. Health literacy - A new concept for general practice? Aust Fam Physician. 2009;38:144–7. [PubMed] [Google Scholar]
- 18.Hocking A, Laurence C, Lorimer M. Patients’ knowledge of their chronic disease: The influence of socio-demographic characteristics. Aust Fam Physician. 2013;42:411–6. [PubMed] [Google Scholar]
- 19.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: Translating evidence into action. Health Aff (Millwood) 2001;20:64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 20.Anselmino M, Sillano D. Impact of pre-diabetes and diabetes on cardiovascular outcomes. Curr Vasc Pharmacol. 2012;10:680–3. doi: 10.2174/157016112803520882. [DOI] [PubMed] [Google Scholar]
- 21.Wylie G, Hungin AP, Neely J. Impaired glucose tolerance: Qualitative and quantitative study of general practitioners’ knowledge and perceptions. BMJ. 2002;324:1190. doi: 10.1136/bmj.324.7347.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kiawi E, Edwards R, Shu J, Unwin N, Kamadjeu R, Mbanya JC. Knowledge, attitudes, and behavior relating to diabetes and its main risk factors among urban residents in Cameroon: A qualitative survey. Ethn Dis. 2006;6:503–9. [PubMed] [Google Scholar]


