Abstract
Short-run subsidies for health products are common in poor countries. How do they affect long-run adoption? A common fear among development practitioners is that one-off subsidies may negatively affect long-run adoption through reference-dependence: People might anchor around the subsidized price and be unwilling to pay more for the product later. But for experience goods, one-off subsidies could also boost long-run adoption through learning. This paper uses data from a two-stage randomized pricing experiment in Kenya to estimate the relative importance of these effects for a new, improved antimalarial bed net. Reduced form estimates show that a one-time subsidy has a positive impact on willingness to pay a year later inherit. To separately identify the learning and anchoring effects, we estimate a parsimonious experience-good model. Estimation results show a large, positive learning effect but no anchoring. We black then discuss the types of products and the contexts inherit for which these results may apply.
Keywords: Technology adoption, experimentation, social learning, anchoring, malaria, prevention
1. INTRODUCTION
In 2010, an estimated 7.6 million children died before the age of five (Liu et al. (2012)). It is estimated that nearly two thirds of these deaths could be averted using existing preventative technologies, such as vaccines, insecticide-treated materials, vitamin supplementation, or point-of-use chlorination of drinking water (Liu et al. (2012), Jones et al. (2003)). An important question yet to be answered is how to increase adoption of these technologies.
A commonly proposed way to increase adoption in the short run is to distribute those essential health products for free or at highly subsidized prices (WHO (2007), Sachs (2005)). There are two main economic rationales to do so. First, given the infectious nature of the diseases they prevent, most of these products generate positive health externalities, and without a subsidy private investment in them is socially suboptimal. Second, when the majority of the population is poor and credit-constrained, subsidies may be needed to ensure widespread access (Cohen and Dupas (2010), Tarozzi, Mahajan, Blackburn, Kopf, Krishnan, and Yoong (2013)).
For some products, such as vaccines, one-time adoption is sufficient to generate important health impacts. One-time subsidies are well-suited for these technologies. But for other products, such as antimalarial bed nets, water treatment kits, or condoms, repeat purchases and consistent use are required to generate the hoped-for health impacts. A key question and ongoing debate is whether one-time subsidies for such technologies increase or dampen private investments in them in the long run.
A short-run subsidy may increase demand in the long run if the product is an experience good. Beneficiaries of a free or highly subsidized sample will be more willing to pay for a replacement after experiencing the benefits and learning the true value of the product if they previously had underestimated these benefits. This learning might spread to others in the community (those ineligible for the subsidy) and increase the overall willingness to pay in the population.
These positive effects hinge upon people using a product or technology that they receive for free or at a highly subsidized price. This might not be the case, however. Households that are not willing to pay a high monetary price for a product might also be unwilling to pay the non-monetary costs associated with using the product on a daily basis. In other words, subsidies may undermine the “screening effect” of prices (Ashraf, Berry, and Shapiro (2010), Chassang, Padro i Miquel, and Snowberg (2012)). Subsidies could also reduce the potential for psychological effects associated with paying for a product, such as the “sunk cost” effect, whereby people who have paid more for a product feel more compelled to put it to good use.2
Even if people use products they receive as free trials, they might be unwilling to pay a higher price for the product once the subsidy ends or is reduced. This could happen if people take previously encountered prices as reference points, or anchors, that affect their subsequent reservation price (Köszegi and Rabin (2006)). Such effects, known in psychology as “background contrast effects” and first identified experimentally by Simonson and Tversky (1992), have recently been observed outside the lab by Simonsohn and Loewenstein (2006). Under such reference-dependent preferences, one-time subsidies for health products could generate a sort of entitlement effect that would dampen long-run adoption.
The view that these negative effects might dominate the standard positive learning and health effects is quite prevalent among development practitioners. There is, however, no rigorous evidence to date as to what short-run subsidies do to long-run adoption of new technologies.
To inform this debate and gauge the relative importance of these effects, we conducted a field experiment in Kenya with a new health product, the Olyset long-lasting insecticide-treated bed net (LLIN), a recent innovation in malaria control. The Olyset LLIN is significantly more comfortable to sleep under than traditional bed nets, it is sturdier and more durable, and it stays effective for much longer. Given these characteristics, its long-run adoption should be boosted by the learning effects of a one-time subsidy, unless anchoring around the subsidized price is important. The experiment included two phases. In Phase 1, subsidy levels for Olyset LLINs were randomly assigned across households within six villages. Households had three months to acquire the product at the subsidized price to which they had been assigned. Prices varied from $0 to $3.80, which is about twice the average daily wage for casual agricultural work in the study area. In Phase 2, a year later, all households in four villages were given a second opportunity to acquire an Olyset LLIN, but this time everyone faced the same price ($2.30). The Olyset was not available outside of the experiment, but traditional nets were available on the market for $1.50.3
This experimental design allows us to estimate the effects of one-off subsidies on demand, both over time and across individuals. We first test whether subsidies increase the short-run level of adoption. We find very large effects: adoption in Phase 1 increases from 7% to over 60% when the price decreases from $3.80 to $0.75, and reaches 98% when the price drops to zero. Moreover, information about the product appears to diffuse through spatial networks—households are more likely to purchase the Olyset in Phase 1 when the density of households around them who receive the high subsidy is (randomly) higher. The timing of voucher redemptions as well as survey evidence further suggest the presence of informational spillovers on the product characteristics within the three months during which vouchers could be redeemed.
We then estimate how the Phase 1 subsidy level affects willingness to pay for an Olyset net in Phase 2. We find that gaining access to a highly subsidized Olyset net in the first year increases households’ observed willingness to pay for an Olyset net a year later: households who had to pay $0.75 or less in Phase 1 were 7.2 percentage points more likely to invest in a $2.30-Olyset in Phase 2 than those who faced a higher Phase 1 price (corresponding to a 49 percent increase). Ultimately, those who benefited from a high subsidy in Phase 1 were three times more likely to own two Olysets by the end of the study period than those who did not. This suggests the presence of a positive learning effect which dominates any potential anchoring or entitlement effect. Suggestive follow-up survey evidence is consistent with the presence of a learning effect. On the other hand, higher exposure through spatial networks in Phase 1 appears to dampen adoption in Phase 2, suggesting a positive health spillover effect that reduces the need for private investment in prevention.
While these reduced form results suggest that the total effect of short-run subsidies on long-run adoption of a new, improved antimalarial bed net is positive, they do not allow us to separate out and quantify the learning effect from the anchoring and health spillover effects. For this, we estimate an experience-good model that allows for reference-dependent preferences, learning from experimentation, informational spillovers, and health spillovers, but assumes agents are myopic (they do not engage in strategic experimentation nor anticipate health spillovers).We estimate the model using both Phase 1 and Phase 2 adoption decisions and find evidence of an economically large and statistically significant learning effect, but no evidence that Phase 1 prices are taken as reference points in Phase 2.
Overall, our results suggest that short-run subsidies for new health products impact long-run adoption through their effect on knowledge about the products, not through anchoring effects. The sign of the learning effect, while positive in our context, will obviously depend on the product and circumstances, however—in particular, on people’s priors on the product as well as on how easily observable the health effectiveness of the product is. In the penultimate section of the paper, we discuss the contexts and products for which learning may go the other way, and make a few conjectures regarding four commonly subsidized products: water filters, chlorine, cookstoves, and deworming. We then relate our results to those of related field studies. The most closely related study is Kremer and Miguel (2007), also in Kenya, which found that introducing a small fee to keep a school-based deworming treatment program going reduced coverage from 75% to 19%. Their experimental setup did not provide the counterfactual, however—what share of households would have paid the fee had they not been exposed to a free trial for a few years? We argue it may have been more than 19%, not because the free trial created a sense of entitlement, but rather, because the free trial enabled households to learn that the private costs of deworming outweigh the private gains.
Besides contributing to the literature on pricing and user fees for health products, and to the lively policy debate on free distribution versus cost-sharing, our paper contributes to a growing literature on the role of learning-by-doing and social learning in technology adoption in poor countries (see Foster and Rosenzweig (2010) for a review; and Munshi and Myaux (2006), Adhvaryu (2012), and Oster and Thornton (2012) for learning about health technologies in particular). Our paper also contributes to the empirical psychology and economics literature, testing behavioral economics in the field (see DellaVigna (2009) for a review), and complements earlier papers that have estimated, in rich countries, how the willingness to pay for a product can be affected by anchors (Ariely, Loewenstein, and Prelec (2003)), previously encountered prices (Simonsohn and Loewenstein (2006), Mazar, Koszegi, and Ariely (2009)), or the range of options available (McFadden (1999), Heffetz and Shayo (2009)). Finally, our paper makes a contribution to the literature on experience-goods pricing (Bergemann and Valimaki (2000, 2006)).
2. BACKGROUND AND EXPERIMENTAL DESIGN
2.1. Background on Insecticide-Treated Bed Nets
Over the past two decades, the use of insecticide-treated bed nets (ITNs) has been established through multiple randomized trials as an effective and cost-effective malaria control strategy for sub-Saharan Africa (Lengeler (2004)). But coverage rates with ITNs remain low. Until recently, one of the key challenges to widespread coverage with ITNs was the need for regular re-treatment with insecticide every 6 months, a requirement few households complied with (D’Alessandro (2001)). This problem was solved recently through a scientific breakthrough: long-lasting insecticidal nets (LLINs), whose insecticidal properties last at least as long as the average life of a net (4–5 years), even when the net is used and washed regularly. The first prototype LLIN, the Olyset Net, was approved by WHO in 2001, but did not get mass produced until 2006. At the time this study started in Kenya in 2007, the Olyset net was not available for sale, and its quality—relative to that of regular ITNs available for sale—was unknown.
More specifically, at the time of the experiment, the “status quo” technology that households in Kenya had access to was a regular ITN, subsidized by Population Services International (PSI). Pregnant women and parents of children under 5 years old could purchase an ITN for the subsidized price of Kenyan shillings (Ksh) 50 ($0.75) at health facilities, and the general population could purchase ITNs for the subsidized price of Ksh 100 ($1.50) at local stores.
In our study sample, 80% of households owned at least one bed net (of any kind) at baseline, but given the large average household size, the coverage rate at the individual level was still low, with only 41% of household members regularly sleeping under a net. About 33% of households had an LLIN of the brand PermaNetA® at baseline. The PermaNetA® LLINs were received free from the government during a mass distribution scheme targeting parents of children under 5 and conducted in conjunction with the measles vaccination campaign of July 2006, ten months before the onset of this study. These PermaNets differ substantially from the Olyset LLIN used in our experiment: they are circular and not rectangular, made of polyester and not polyethylene, and have a smaller mesh. They cannot be distinguished from traditional retreatable ITNs with the naked eye, while Olyset nets can. Finally, Olyset nets have been judged to be more comfortable to sleep under than either traditional ITNs or the PermaNetA®, thanks to the wider mesh that enables more air to go through (making the area under the net less hot).
2.2. Experimental Design: Phase 1
The experiment was conducted in Busia District, Western Kenya, where malaria transmission occurs throughout the year. In Phase 1, the study involved 1120 households from six rural enumeration areas. Participating households were sampled as follows. In each area, the school register was used to create a list of households with children.4 Listed households were then randomly assigned to a subsidy level for an Olyset net. The subsidy level varied from 100% to 40%; the corresponding final prices faced by households ranged from 0 to 250 Ksh, or at the prevailing exchange rate of Ksh 65 to US$1 at the time, from 0 to US$3.8.5 Seventeen different prices were offered in total, but each area, depending on its size, was assigned only four or five of these 17 prices. Thus, if an area was assigned the price set {Ksh 50, 100, 150, 200, 250}, all the study households in the area were randomly assigned to one of these five prices according to a computer-generated random number. All price sets included high, intermediate, and low subsidy levels. However, the lowest price offered in a given area was randomly varied across areas, and drawn from the following set: {0, 40, 50, 70}. Only two areas had a price set that included free distribution for some households.
After the random assignment to subsidy levels had been performed in office, trained enumerators visited each sampled household. A baseline survey was administered to the female and/or male head of each consenting household.6 At the end of the interview, the respondent was given a discount voucher for an Olyset net corresponding to the randomly assigned subsidy level. The voucher indicated (1) its expiration date, (2) where it could be redeemed, (3) the final (post-discount) price to be paid to the retailer for the net, and (4) the recommended retail price and the amount discounted from the recommended retail price. Vouchers could be redeemed at participating local retailers (one per area). The six participating retailers were provided with a stock of blue, extra-large, rectangular Olyset nets. At the time of the study, such nets were not available to households through any other distribution channel, which facilitated tracking of the study-supplied nets.
The participating retailers received as many Olyset nets as vouchers issued in their community, and no more. They were not authorized to sell the study nets to households outside the study sample. For each redeemed voucher, the retailers were instructed to note the voucher identification number and the date of redemption in a standardized receipt book designed for the experiment. The list of redeemed vouchers and the voucher stubs themselves were collected from retailers every two weeks.7
The subset of households who had redeemed their Olyset voucher was sampled for a short-run follow-up administered during an unannounced home visit 2 months, on average, after the voucher had been redeemed. During the follow-up visit, enumerators asked to see the net that was purchased with the voucher, so as to ascertain that it was a study-supplied Olyset net. The follow-up survey also checked whether households had been charged the assigned price for the net. Usage was assessed as follows: (1) whether the respondent declared having started using the net, and (2) whether the net was observed hanging above the bedding at the time of the visit.
2.3. Experimental Design: Phase 2
In a subset of areas (four out of six), a long-run follow-up was conducted 12 months after the distribution of the first Olyset voucher.8 All households in those areas were sampled for the long-run follow-up (both those who had redeemed their first voucher, and those who had not). Data on the (presumed) incidence of malaria in the previous month were collected. Households were also asked if they knew people who had redeemed their vouchers and what they had heard about the net acquired with the voucher. In addition, for those who had redeemed the voucher, usage of the Olyset net was recorded as in the first follow-up.
At the end of the visit, households received a second Olyset voucher, redeemable at the same retailer as the voucher received a year earlier. All households faced the same price (Ksh 150, or $2.30) for this second voucher. The setup used with retailers was identical to Phase 1.
By comparing the take-up rate of the second, uniformly priced voucher across Phase 1 price groups, we can test whether being exposed to a high subsidy dampens or enhances willingness to pay for the product a year later. Note, however, that since LLINs have a lifespan of 4 to 5 years, at the time they received the second Olyset voucher, households who had purchased an Olyset with the first voucher in Phase 1 did not yet need to replace their first one. The redemption rate for the second voucher thus measures, for those households, the willingness to pay for an additional Olyset, or the discounted present value of a replacement Olyset (if households wanted to hoard the second Olyset until a replacement was needed).
2.4. Baseline Characteristics and Balance Check
The baseline survey was administered at households’ homes between April and October 2007. It assessed household demographics, socioeconomic status, and bed net ownership and coverage. Table I presents summary statistics on 15 household characteristics, and their correlation with the randomized Phase 1 price assignment. Specifically, we regress each baseline characteristic on a quadratic in the price faced in Phase 1 and a set of area fixed effects. We report the coefficient estimates and standard errors in columns 3 and 4, as well as the p-value for a test that the two coefficients on the price polynomial are jointly significant (column 5). All of the coefficient estimates are small and none can be statistically distinguished from zero, suggesting that the randomization was successful at making the price assignment orthogonal to observable baseline characteristics. Column 6 shows that randomized assignment to a “high subsidy” level (price ≤ Ksh 50) is also, as expected, completely orthogonal to household characteristics.
TABLE I.
Baseline Characteristics of Participating Households
| (1) | (2) | (3) | (4) | (5) | (6) | (7) | |
|---|---|---|---|---|---|---|---|
| Sample Mean |
Std. Dev. |
Phase 1 Price (in US$) |
(Phase 1 Price in US$) Squared |
(Price and Price Squared) |
High Subsidy in Phase 1 |
N | |
| Household (HH) demographics | |||||||
| Household size | 7.1 | 2.7 | −1.207 (0.536) | −0.919 (0.443) | 0.145 | −0.586 (0.393) | 1112 |
| Age of household head | 45.7 | 13.4 | −1.608 (2.608) | −2.311 (2.165) | 0.065 | −1.064 (1.912) | 1079 |
| Number of children (under 18) currently living in household | 5.4 | 2.9 | −0.747 (0.552) | −0.606 (0.456) | 0.490 | −0.299 (0.405) | 1120 |
| Socio-Economic Status | |||||||
| Female head has completed primary school | 0.25 | 0.43 | −0.068 (0.084) | −0.013 (0.07) | 0.765 | −0.020 (0.062) | 1116 |
| Number of household members with an income- generating activity | 1.8 | 1.0 | −0.247 (0.203) | −0.094 (0.168) | 0.071 | −0.2 (0.149) | 1112 |
| Household assets index value (in US$) | 338 | 325 | −30.866 (62.897) | 6.329 (51.957) | 0.800 | −30.097 (46.132) | 1120 |
| Electricity at home | 0.02 | 0.14 | 0.013 (0.027) | 0.019 (0.022) | 0.791 | 0.004 (0.02) | 1108 |
| At least one member of HH has a bank account | 0.12 | 0.33 | −0.071 (0.064) | −0.045 (0.053) | 0.520 | −0.016 (0.047) | 1116 |
| Bednet Ownership at Baseline | |||||||
| Number of bednets owned | 1.7 | 1.5 | −0.226 (0.292) | −0.274 (0.241) | 0.636 | −0.051 (0.214) | 1112 |
| Share of HH members that slept under a net the previous night | 0.41 | 0.37 | −0.038 (0.072) | −0.047 (0.059) | 0.615 | 0.002 (0.052) | 1112 |
| HH owns a circular PermaNet LLINa | 0.33 | 0.47 | −0.169 (0.132) | −0.195 (0.141) | 0.520 | −0.068 (0.076) | 538 |
| HH ever received a free bednet | 0.32 | 0.47 | −0.108 (0.091) | −0.095 (0.075) | 0.533 | −0.027 (0.067) | 1112 |
| Has ever shopped at shop where voucher has to be redeemed | 0.62 | 0.49 | −0.036 (0.085) | 0.029 (0.071) | 0.609 | −0.035 (0.062) | 1110 |
| Declared willingness to pay for a bed net (in US$) | 1.56 | 1.55 | −0.285 (0.306) | −0.003 (0.252) | 0.353 | −0.202 (0.225) | 1100 |
| Distance from shop where voucher has to be redeemed (in km) | 1.86 | 1.58 | −0.677 (0.302) | −0.534 (0.249) | 0.108 | −0.334 (0.222) | 1094 |
Notes: Columns 3 and 4 show coefficient estimates and their standard errors for two independent variables (the Phase 1 price, column 3, and its square, column 4) estimated through a common linear regression (one for each row) with area fixed effects. Column 6 presents coefficient estimates from a separate OLS regression with area fixed effects for each row. Standard errors are presented in parentheses.
The LLINs subsidized during the experiment were family-size rectangular Olysets.
2.5. Verifying Compliance With Study Protocol
All households that redeemed their vouchers declared, when interviewed at follow-up, that they had been charged the assigned price when they redeemed their voucher at the shop. This suggests that participating retailers respected the study protocol. Moreover, the sales logs kept by participating retailers show that, in total over Phase 1 and Phase 2, 95% of the redeemed vouchers were redeemed by a member of the household that had received the voucher. Only two of the individuals that redeemed a voucher declared having paid to acquire the voucher. This suggests that there was almost no arbitrage between households prior to voucher redemption.
To check whether households sold the Olyset to their neighbor after redeeming the voucher, we conducted unannounced home visits and asked to see the Olyset that had been purchased with the voucher (as mentioned above, the study-supplied nets were easily recognizable). These home visits were conducted after both Phase 1 and Phase 2. Overall, more than 90% of households that had redeemed a voucher could show the corresponding Olyset during the spot check.
3. EXPERIMENTAL RESULTS
The experimental results are shown graphically in Figures 1 and 2, and in Table II. We find three main results: (1) adoption in Phase 1 is very sensitive to own-price; (2) adoption in Phase 1 is positively affected by exposure to neighbors who received a large subsidy; (3) adoption in Phase 2 is not lower among high subsidy recipients in Phase 1; in fact, it is somewhat higher.
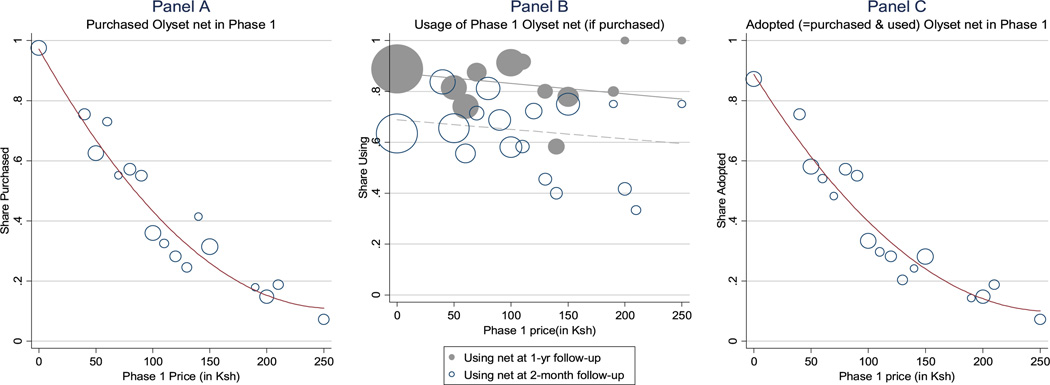
Figure 1.
Effects of phase 1 price subsidy on Phase 1 adoption. Notes: Data from 1120 households (Panels A and C), 479 households (Panel B, hollow circles), 273 households (Panel B, solid circles). The size of the circles reflects the relative size of the sample at each price point. The lines are quadratic fits (Panels A and C) or linear fits (panel B). The 1-yr follow-up was conducted in only four of the six study areas. Usage is self-reported (see Table II for results on observed usage). The exchange rate at the time of the study was around Ksh 65 to US$1.
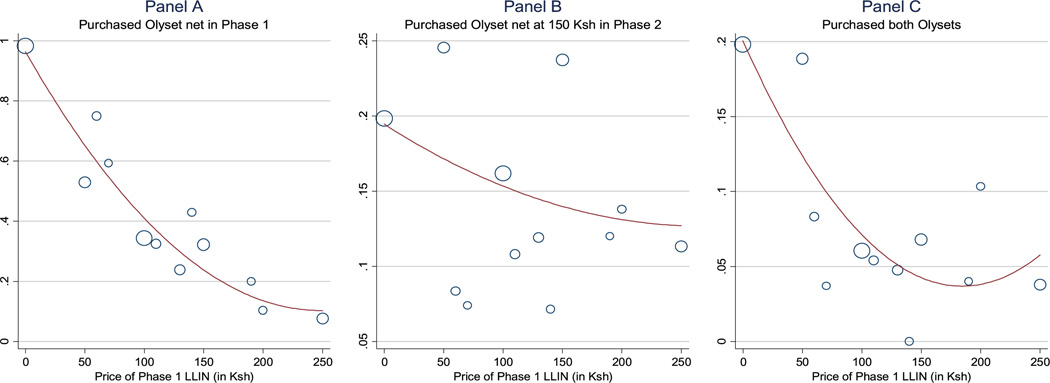
Figure 2.
Effects of Phase 1 price subsidy on Phase 2 adoption. Notes: Data from 599 households in the four areas sampled for Phase 2. Panel A reproduces Panel A of Figure 1 for the subsample included in Phase 2. The size of the circles reflects the relative size of the sample at each price point. The lines are quadratic fits.
TABLE II.
Experimental Results
| (1) | (2) | (3) | (4) | (5) | |
|---|---|---|---|---|---|
| Purchased Olyset Net in Phase 1 |
Purchased and Used Olyset Net in Phase 1a |
Purchased Olyset at 150 Ksh in Phase 2 |
Purchased Both Olysets |
Purchased Waterguardb |
|
| Phase 1 Price ≤ Ksh 50 (high subsidy) | 0.387 (0.034)*** [0.034]*** | 0.281 (0.033)*** [0.033]*** | 0.068 (0.040)* [0.04]* | 0.115 (0.031)*** [0.033]*** | 0.046 (0.065) [0.052] |
| Density of Phase 1 high subsidy recipients within 500-meter radius | 0.223 (0.092)** [0.083]*** | 0.168 (0.090)* [0.088]* | −0.183 (0.099)* [0.119] | −0.102 (0.078) [0.104] | −0.156 (0.144) [0.145] |
| Area fixed effects | Yes | Yes | Yes | Yes | Yes |
| Observations | 1094 | 1094 | 584 | 584 | 256 |
| Mean of dependent variable | 0.458 | 0.321 | 0.158 | 0.094 | 0.434 |
| Mean of dependent variable in non-“high subsidy” group | 0.341 | 0.233 | 0.137 | 0.057 | 0.411 |
Notes: Linear probability model estimates. All regressions include enumeration area fixed effects and control for two cross-cutting randomized treatments (gender of voucher recipient and framing) discussed in Dupas (2009). Twenty-six (15) observations are dropped for Phase 1 (Phase 2) because they do not have valid GIS data to compute the social exposure variables. White standard errors presented in parentheses. Standard errors corrected for spatial dependence are presented in brackets.
indicates significance at 10%;
at 5%;
at 1%.
Results are unaffected if household-level characteristics shown in Table I are controlled for.
Results are also unaffected if a control for population density (total number of study households within 500-meter radius) is controlled for.
“Purchased and Used Olyset in Phase 1” is a dummy equal to 1 if the household redeemed the first Olyset voucher and the net was seen hanging during at least one of the two surprise follow-up visits.
Waterguard is a water purification product. Vouchers for Waterguard subsidized at 50% were offered 5 months after the first Olyset voucher was distributed, to test for the presence of cross-product entitlement effects. This Waterguard voucher sub-experiment was conducted in only the two enumeration areas where the High Subsidy was a full subsidy. See Section 5 of the text for details.
3.1. Short-Run: Phase 1 Adoption
Direct Effects
Figure 1 presents experimental evidence on the impact of price on Phase 1 adoption. Panel A shows that the demand function is quite steep: take-up is quasi-universal for free vouchers (at 97.5%), but drops to 70% and then 55% when the price goes to Ksh 40 ($0.6) and Ksh 90 ($1.4), and further drops to around 30% when the price crosses the Ksh 100 threshold ($1.5).
In contrast, Panel B of Figure 1, which shows usage rates (among those who redeemed their voucher) at both the 2-month and 1-year follow-up, suggests that the likelihood that people used the Olyset net does not increase with the price paid. As a result, the adoption rate (purchase × usage) drops substantially as the price increases (as the subsidy level decreases): after 12 months, adoption is at 90% under the full subsidy regime, just below 60% at the Ksh 50 price point, and lower than 10% when the price is Ksh 250 (see Figure 1, Panel C).9
The result that initial adoption is very sensitive to price is consistent with the result obtained among pregnant women by Cohen and Dupas (2010), in a separate study also in Western Kenya. It is also consistent with the results in Tarozzi et al. (2013), who found that regular bed net coverage in Orissa (India) decreases from 51% to 10% when the price increases from free to full.
Compared to other health products, the adoption function we observe is not as steep as that observed by Kremer and Miguel (2007), who found that increasing the price of deworming from 0 to Ksh 20 decreases adoption from 75% to 19%. Adoption of Olyset nets is also much higher overall than that observed by Ashraf, Berry, and Shapiro (2010) concerning water disinfectant: they found that increasing the price from 300 to 800 Zambian Kwacha (which is equivalent to going from just Ksh 6 to Ksh 17) decreases the purchase rate from 80% to 50%, but leaves the adoption rate (purchase × usage) unaffected, at roughly 30%.
Spillover Effects
Given the large differences in take-up across price groups, the random assignment of households to price groups in Phase 1 generates an exogenous source of geographic variation in exposure to Olyset nets. Appendix Figure A.1 shows that households that received a voucher for a highly subsidized Olyset net typically redeemed it within a few weeks (a few days if they got a free one). In contrast, those who were assigned a high price not only were very unlikely to redeem their voucher, as we have seen above, but also if they did, they took two months to redeem. Thus, across neighborhoods within a given village, the “exposure” to Olyset nets within the first three months the voucher could be redeemed varied with the share of households that received a high subsidy level. Since this share was exogenously determined by the random assignment, we can exploit this variation to estimate social effects without running into the reflection problem (Manski (1993)).
Using GIS coordinates, we compute, for each household in the sample, the number of sampled households that live within a given radius, and the number and share of them who received a voucher for a high subsidy.10 On average, households have 1.28 neighbors within a 250-m radius (4.01 neighbors within 500 m, 7.77 within 750 m) who received a high subsidy. This represents, at the mean, 22–25% of the study households living within these radii.11
Table II presents estimates of the spillover effects estimated parametrically through OLS, controlling for own subsidy status. We run the following regression:
where Yhj1 is whether household h from area j bought the Phase 1 Olyset; Highhj1 is a dummy equal to 1 if household received a high subsidy (price of Ksh 50 or lower) in Phase 1, and υ j is an area fixed effect. The regressor of interest is ShareHighhj1, the share of neighbors (within a 500-m radius; the results are unchanged when we use alternative radii) who received a high subsidy in Phase 1. (We impute this share to be zero if there are no other study households in this radius.) In the specifications shown, we do not control for the total number of study households within 500 meters, but results are unchanged if we do. Finally, since the density measures may be spatially correlated, we present standard errors corrected for spatial dependence in brackets, in addition to presenting the White standard errors in parentheses. We use the spatial dependence correction proposed by Conley (1999).12
The results in Table II, row 2, suggest positive spillovers—if all of a household’s neighbors sampled for the study received a high subsidy, the probability of redeeming one’s own voucher increases by 22 percentage points. This implies that households are almost 50% more likely to invest in the Olyset net if all of their sampled neighbors received the high subsidy. This is a nontrivial effect since the average price households had to pay for the Olyset net in Phase 1 was Ksh 109 ($1.65), close to the average daily wage and a relatively large sum for rural households.13
3.2. Long-Run: Phase 2 Adoption
Direct Effects
The effect of high subsidies on Phase 1 adoption suggests a large potential for it to affect Phase 2 adoption through learning effects. We now test whether households who benefited from a high subsidy in Phase 1 were more or less willing to pay for an Olyset net in Phase 2.
Recall that the price of the second Olyset offer was uniform across all households (at Ksh 150). Panel B of Figure 2 presents the average purchase rate for the second Olyset net, for each Phase 1 price. Average take-up appears higher among the higher subsidy groups (Phase 1 price of 0 or Ksh 50).14
Based on this, in column 3 of Table II, we present results of an OLS regression in which the dependent variable is a dummy for having purchased the Phase 2 Olyset net, and the main regressor is a dummy for having received a “high subsidy” in Phase 1 (price ≤ Ksh 50). As was clear from the figures, the effect of having received a high subsidy in Phase 1 has a very large effect on purchase and adoption in Phase 1 (columns 1 and 2), but the effect on Phase 2 purchase is much more modest (column 3). The Phase 2 effect is only significant at the 10% level, but is robust to controlling for household-level controls (not shown).15
Overall, the evidence points to a positive effect of a high Phase 1 subsidy on Phase 2 adoption, but the effect is not strong, and only at the margin of significance. Note, however, that the take-up of the second voucher among high subsidy recipients reflects mostly the demand for a second Olyset net, whereas for most households that received a high price for the first voucher, the take-up of the second voucher reflects the demand for a first Olyset net (since take-up of the first voucher was low at high prices). Under the reasonable assumption that the marginal utility of Olyset nets is decreasing in the number owned, holding everything constant, the demand for a second Olyset net would be lower than the demand for a first Olyset net. In other words, the fact that the take-up for the second voucher is not significantly lower in the high subsidy group than in the low subsidy group by itself suggests that the willingness to pay in the high subsidy group may have increased.16
Survey evidence suggests households who acquired an Olyset net had, overall, a very positive experience with it, suggesting positive learning. Households who had purchased the first Olyset net were asked: “In your opinion, how does this Olyset net compare to other nets you may have had in the past?” The great majority (90%) said that the Olyset was better.17 At the 2-month follow-up, the main (non-exclusive) reasons given for why the Olyset was better concerned the heightened comfort level (37%), the sturdiness (40%), and the health effectiveness (26%). At the 1-year follow-up, the same share of respondents mentioned comfort and sturdiness, but the share mentioning health effectiveness had risen to 40%. Finally, among those who purchased the Phase 1 Olyset, the self-reported willingness to pay for a replacement Olyset was $2.7, much higher than their self-reported willingness to pay $1.6 for an ITN at baseline.
Spillover Effects
Does this positive experience trickle to others? The coefficient on social exposure in column 3 of Table II suggests that redemption in Phase 2 was negatively affected by exposure via neighbors. This is somewhat surprising given the static spillover effects—if exposure via neighbors increased experimentation in Phase 1 and there are learning effects, then we should expect a reduced form effect from exposure to subsidized neighbors on Phase 2 adoption. The fact that we do not could be driven by people reacting to the health spillovers over time: people with more neighbors using an Olyset net get convinced to invest in one themselves, but as the malaria transmission rate decreases over the course of the year in areas with higher Olyset coverage, the private returns to investing in prevention decrease in those areas. Consistent with this interpretation, we find that greater exposure to highly subsidized neighbors lowered the probability that a household invested in two Olyset nets (column 4 of Table II). Estimates of the health effects in Table A.I indeed suggest positive health spillovers, though statistical power is very limited.18
4. MECHANISMS: STRUCTURAL MODEL AND ESTIMATION
The results so far strongly suggest that a one-time subsidy for the Olyset net did not reduce future willingness to pay. This means that potential negative anchoring effects of subsidies were, if present, overwhelmed by a positive learning effect, but the reduced form results do not enable us to separately identify the magnitudes of each these effects separately. Moreover, we find some evidence that exposure to highly subsidized neighbors reduces long-term adoption, possibly by reducing the need for prevention, creating a second channel through which the reduced form effect of a short-term subsidy on long-run adoption is providing a lower bound on learning. In this section, we tease out these various countervailing forces and separate out the learning by doing from other effects by imposing some structure and jointly estimating Phase 1 and Phase 2 decisions.
4.1. Model
We consider a very stylized model. There are two periods and one preventative health product. In each period, households invest in the product if the expected utility gain outweighs the utility costs.
Households’ utility is composed of two additive terms: intrinsic utility and gain–loss utility. Intrinsic utility is a function of absolute outcomes, expected private benefits, and private costs. Gain-loss utility captures reference-dependence: households can experience utility losses when they pay more for the product than expected, and utility gains when they pay less than expected.
The expected private benefit from adopting the product depends on the disease burden, own vulnerability, and beliefs about the quality of the product. The quality itself depends on a number of factors, such as sturdiness, comfort, and effectiveness at preventing infection, but for simplicity we assume that individuals aggregate their beliefs about these different factors into this one attribute we call “quality.”
We allow for two forms of spillovers: health spillovers (e.g., if bed net coverage reaches a certain threshold in the community, the disease risk is reduced), and information spillovers (people can get a signal about the product’s quality from their neighbors). We assume that households are myopic—they do not engage in strategic experimentation nor anticipate health spillovers. They do, however, observe accurate information on the disease burden in real time.
When the product is first introduced at the beginning of period 1, the disease burden is high and vulnerability to risk is maximal for everyone. Households do not know the quality of the product, and they do not have a reference point for the price of the new product.
Households who acquire the product in period 1 get information about some of its characteristics (e.g., sturdiness, comfort) and immediately update their beliefs about its quality and thus the private returns to using it. This information about the product’s basic characteristics can diffuse spatially and affect other households’ decision to adopt the product in period 1.
In period 2 (a year later), households face a new price for the product. They now take the price they faced in period 1 as reference price. The disease risk has changed based on the local level of adoption in period 1. Moreover, households who adopted in period 1 are less vulnerable to risk since they own one unit of the product. They also updated their beliefs about the product’s quality based on their health outcome in the previous year. The health outcome is privately observed, however; thus, learning from experimentation does not diffuse spatially.19
4.1.1. Formal Setup and Notations
Household h invests in the product in period t if the expected utility gain outweighs the utility costs:
where E(Rt) denotes the expected health gain (in utility terms) of using the health product in period t. ε ht is a household- and time-specific preference shock, pt is the price at which the product is offered in period t, a is the marginal utility from income, and f(prt − pt) is the gain–loss utility.
We consider the following linear form for the gain–loss utility (dropping the time subscripts): f(pr − p) = r × (p − pr) if pr ≥ p (gains) and f(pr − p) = λ r× (p−pr) if pr <p (losses), where pr is the reference price, r is what we call the reference-dependence parameter (which can be interpreted as the weight attached to gain–loss utility), and λ is the loss aversion parameter.20
Finally, we consider E(Rt) = E(m)γ tυht, where m is the quality of the product, γ t is the disease risk in the area, and υht is the vulnerability of household h to this disease risk at time t. The disease risk γ t depends on the overall rate of adoption of the health technology among neighbors in the previous period, but households are myopic and do not anticipate these health spillover effects. A household’s vulnerability to the disease risk, υht, depends on the household’s ownership of the product: if the household does not own a long-lasting bed net, adopting one has a higher return (υht = 1) than if it already has one (υht < 1).
4.1.2. Period 1 Adoption
When the product is introduced at the beginning of period 1, households have a prior about its quality m, a distribution period 1 as the reference price; therefore, the gain–loss utility term is zero. Given the disease burden γ1 and vulnerability υht = 1, household h buys in period 1 if
Note that households in this model are myopic: they do not consider the motive of adopting in period 1 in order to learn more about the quality of the technology. This assumption is reasonable in our context, since the product we consider in the experiment was not available on the market at the time, and households did not anticipate that we would come back after one year to offer the product again.21
Households who acquire the product in period 1 get information about its characteristics and immediately (and homogeneously) update their beliefs about its quality: their prior on m shifts from the distribution to the distribution .
During the course of period 1 (which in the experiment corresponds to the 3-month window during which the voucher for the first Olyset net could be redeemed), households that did not immediately get the product themselves can learn about it from others. We consider the following social diffusion process: a household with n owner households within a 250-m radius, N households total in that radius, and c social contacts among them, has a chance to update its beliefs to .22 If they learn, they update their purchase decision and buy in period 1 if
4.1.3. Period 2 Adoption
In period 2 (a year later), the disease risk has changed based on adoption in period 1. Specifically, we consider that γ2 = αγ1, with α<1 if local take-up of the product in period 1 is above a certain threshold t, and γ2 = γ1 otherwise. This threshold effect reflects the shape of health spillovers identified in the medical literature (e.g., Hawley et al. (2003), Killeen et al. (2007)).
Moreover, households have updated their beliefs about the product’s quality. Those who adopted in period 1 received a private signal r1h = m + ν, with ν ~𝒩(0,k2), and update their belief using Bayes’s law; they adopt in period 2 if
where is how much they updated their belief on the mean quality, and υ2 < 1 indicates that the returns to the second Olyset net are lower than those of the first Olyset net.23
Finally, households that did not adopt the product in period 1 adopt in period 2 if
where l3 = 0 for those who did not learn about the product’s characteristics from a neighbor over the course of the year, and l3 = l1 for those who did (since we assume that adopters discuss the observable characteristics of the product with their neighbors, but not their private health signals).
4.2. Estimation
We estimate the model by maximum likelihood. To compute the likelihood function, we assume that the distribution of the independent and identically distributed (i.i.d.) preference shocks εht is logistic, such that, at any period t, the probability that a household purchases the product is
We allow for area fixed effects and estimate the following five parameters of interest: (1) μ: the prior on quality; (2) l1: how much the mean prior on quality changes upon acquisition—this is the learning from product characteristics, which can be transmitted through social learning; (3) l2: how much the mean prior on quality changes upon experimentation over a year; (4) r: the reference-dependence parameter; and finally, (5) a: the marginal utility of income (the higher â is, the more sensitive to price the demand is). Note that failing to reject the null for r does not necessarily imply individuals do not exhibit reference-dependence, only that there is no loss aversion over the period 1 price (i.e., there is no anchoring around the period 1 price).
Assumptions
We impose the following values in our benchmark estimation (and test for sensitivity of the results to these assumptions in Figure A.2):
Based on the medical literature cited above, the threshold for health spillovers is t = 0.6 over a 500-m radius, and the strength of the spillover effects is α = 0.8. In other words, if Olyset net coverage reaches at least 60households living within 500 m of household h, the disease risk faced by household h after a year is reduced by 20%.24
The return to the second Olyset net is 85% that of the first one: υ2 = 0.85. This could be because the second Olyset net is not put to use immediately and the discount factor is 0.85, or because there are diminishing returns to individual Olyset coverage within a given household (since the insecticide halo generated by one Olyset net can be sufficient to keep mosquitoes at bay from the entire sleeping area).25
The loss aversion parameter is set at λ = 1.6. (A recent review by Booij, van Praag, and van den Kullen (2010) showed the range of estimates for λ in the literature is [1.07; 2.61] (Table I).)
We set the number of social contacts at c = 4. This is based on the evidence from Dupas et al. (2013) discussed in footnote 10.
Identification
Separate identification of the learning from experimentation (l2) and reference-dependence parameter (r) is made possible by the random variation in period 1 price (which creates random variation in both experimentation and reference points) along with the random variation in the share of neighbors within a 500-m radius receiving the high subsidy. This latter variation generates random variation in coverage density and thus in the disease environment (and thereby in the returns to investing in an Olyset net) in Phase 2, holding own Phase 1 price constant. Thus, different rates of take-up among households facing the same price sequence but a different disease environment helps pin down the learning effect.
The random variation in the share of neighbors within a 250-m radius receiving a high subsidy (and therefore the share of neighbors who acquire the product immediately upon receiving the voucher) enables estimation of l1 from the Phase 1 adoption decision. The random variation in subsidy levels across neighbors within a 250-m radius also affects the ownership rate at the onset of Phase 2, but this alone cannot be used to estimate l1 (or to estimate information spillovers about health effectiveness if we allowed them) from the Phase 2 adoption decision of those who did not purchase in Phase 1, since by then it is confounded by the health spillover (the change in the disease burden).26
Results
The results under the benchmark specification are presented in Table III. The estimate of the reference-dependence parameter (r) is small economically—at only 6.6% of the estimated value of the marginal utility of income (a).
TABLE III.
Maximum Likelihood Estimates
| Estimate | Std. Err. | ||
|---|---|---|---|
| Prior on effectiveness | μ | 2.423 | 0.295*** |
| Learning from characteristics | l1 | 0.309 | 0.226 |
| Learning from experimentation | l2 | 0.696 | 0.313* |
| Marginal utility from income | a | 0.0219 | 0.0018*** |
| Reference-dependence parameter | r | 0.0015 | 0.0012 |
| Total learning effect | l =l1 + l2 | 1.005 | 0.323*** |
Notes: Sample includes 584 households with valid GIS data in the 4 areas sampled for Phase 2. Estimates from the benchmark model under the values 1.6, 0.6, 0.8, 0.85, and 4, for, respectively, the following parameters: loss aversion λ, health spillovers threshold t, spillover effect α, relative return of second net υ2, and number of social contacts c. Sensitivity of the estimates to these values is presented in Figure A.2.
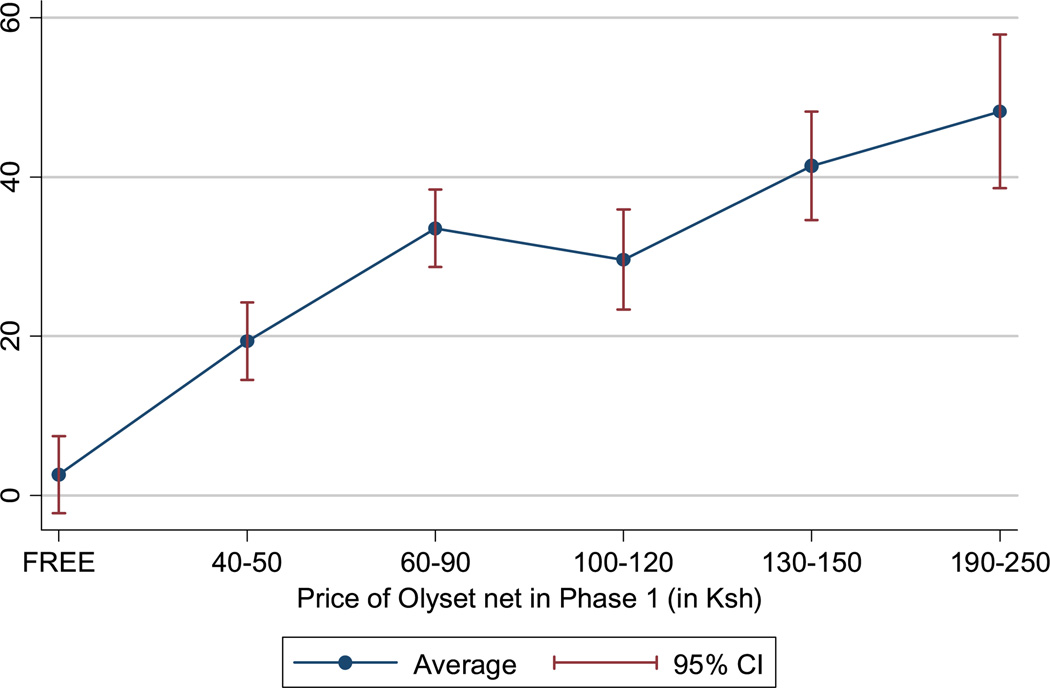
In contrast, the total learning effect after a year’s worth of experimentation (l = l1 + l2) is very large: comparing the value of the estimate to that of μ, it corresponds to an increase in perceived quality of 41%. In monetary terms, this total learning effect increases demand in period 2 as much as decreasing the price from Ksh 150 to Ksh 105 (so it corresponds to the effect of a 30% price drop). Interestingly, the short-term learning from product characteristics (l1), which can be transferred to neighbors, makes up only about 31% of the total learning effect; it is significant at conventional levels (the p-value in the benchmark case is 0.171). The magnitude of l1 means that learning about the product from neighbors increases demand by about as much as a 9 price drop.27
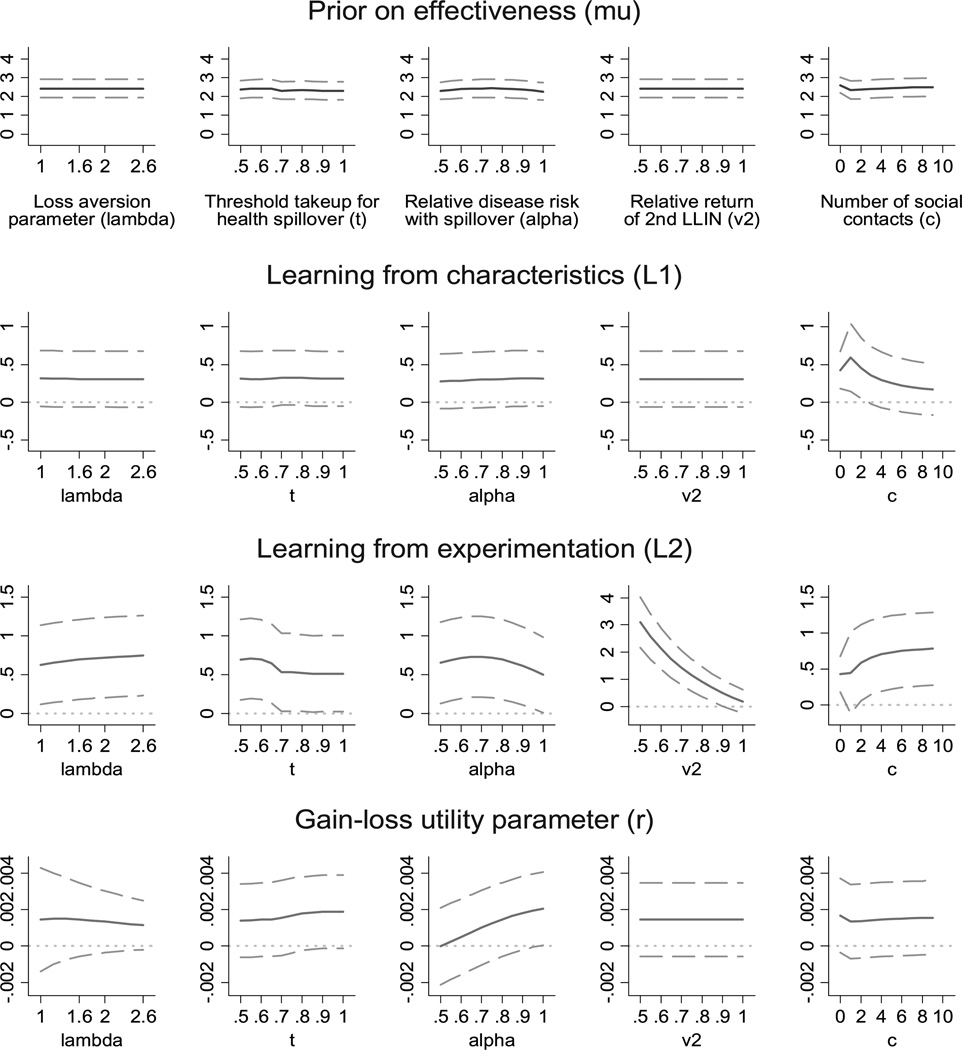
Sensitivity
We test the sensitivity of these results in Figure A.2. We plot the coefficient estimate and the 90% confidence interval over a large range of possible values for the five parameters that are imposed rather than estimated. Overall, the results appear very robust, although looking at the sensitivity analysis helps visualize which assumption matters for the identification of the coefficients of interest. Clearly, the estimate of learning through year-long experimentation (l2) directly depends on the assumption on diminishing returns—if there are no diminishing returns (υ2 = 1), the learning effect is much smaller. The estimate of the reference-dependence parameter is sensitive to assumptions on the shape and magnitude of the health spillovers: as spillovers reduce in strength (α → 1), the reference-dependence parameter increases, but it remains small in economic terms, and if α = 1, we lose separate identification of the reference-dependence parameter and the learning from experimentation. If we knock off the informational spillovers by setting the number of social contacts (c) at zero or very close to zero, the two learning parameters (learning from characteristics and learning from experimentation) cannot be separately identified, though their sum remains unchanged.
5. DISCUSSION: EXTERNAL VALIDITY
Our results suggest that a one-time, introductory subsidy for long-lasting insecticide-treated nets enabled learning, and this learning boosted willingness to pay for them a year later, holding the disease risk constant. In this section, we discuss how generalizable this finding is. We ask three questions: (1) Did the experimental design limit the scope for anchoring around subsidized prices? (2) Are there cross-product entitlement effects of subsidies? (3) For what types of health products and contexts would we expect the same results to obtain?
Did the Experimental Design Limit the Scope for Anchoring?
We find no meaningful evidence that people anchor around subsidized prices. Is that a true result or is it an artifact of the experimental design? Two experimental features could have limited the scope for anchoring effects in our setting. First, subsidies were randomized across households within a village. Since households may have noticed that their neighbors received a different subsidy level than theirs, this could have limited the salience of one given price around which to anchor. It is worth noting that most subsidy programs have some form of targeting rules, however, also yielding heterogeneous pricing across households within a village. For example, subsidies are often targeted based on demographics (presence of a pregnant woman in the household or number of children) or means-tested, and how much people anchor under such programs might be similar to what we observe in our experimental setting.
Second, recall from Section 2.3 that the recommended retail price and the amount discounted from the recommended retail price were indicated on the Phase 1 vouchers. This may have reduced the potential for anchoring. From a policy standpoint, indicating the non-subsidized price on a voucher or product is relatively costless and quite common (this was the case in the Ashraf, Berry, and Shapiro (2010) experiment with chlorine); therefore, estimating the overall effect of subsidies in the presence of full information about the non-subsidized price is of direct policy interest. That said, it would be useful for future research to test the extent to which anchoring effects are at play in the absence of such information. For products such as bed nets, whose retail value tends to be known, it may not have mattered, but for less known products anchoring effects might be larger.
Cross-Product Entitlement Effects?
Another potential worry is that subsidies for one product may lead to entitlement effects vis-a-vis other products. In particular, households might expect that the government or NGO that subsidized product A will also soon start to subsidize product B (if product B belongs to the same class of product, say health products), and thus adopt a “wait and see” stance. To test whether this is the case in the Kenyan context, in the two areas where the high subsidy was a full subsidy, we distributed vouchers for partially subsidized WaterGuard, around 5 months after the first Olyset voucher was distributed. The results are shown in Column 5 of Table II. Take-up of WaterGuard was not lower among recipients of free Olysets (in fact, it was slightly higher, though insignificantly so), suggesting no cross-pro duct entitlement effects. In other words, households who get a chance to receive a free Olyset net do not expect that other health technologies should be given to them for free in order for them to experiment with them.
Which Health Products Do These Results Apply to?
Would the results obtained for bed nets apply for other preventative health products? Besides vaccines, which are already universally subsidized, the other key products for which subsidies are commonly discussed are water purification products (chlorine solutions and filters), cookstoves, and deworming medicines.
The first potential difference between these products and bed nets concerns the level and accuracy of priors on the returns to using the product. As mentioned earlier, the Olyset, the bed net considered in the study, is much more comfortable than earlier generations of bed nets. To the extent that people assume all nets are equally comfortable, people’s priors on the private returns to using Olysets were therefore likely to be underestimates. In contrast, both water disinfectants and deworming pills have important negative side effects (water disinfectant makes the water taste like chlorine, while deworming treatment makes children nauseated for a few days). It is unlikely that households without prior exposure to these products would anticipate such side effects, and therefore their priors on the returns are likely overestimates. With regard to cookstoves, evidence suggests that households tend to overestimate how difficult it is to adapt one’s cooking to the new stove; thus, they may underestimate the returns to switching.
The second difference is in the durability of the product, and hence the potential for a one-off subsidy to enable learning about the health effectiveness of a product. A bottle of water disinfectant lasts only about 1 month for a standard household, whereas deworming treatment needs to be repeated only every 6 months, and bed nets, cookstoves, and water filters have a lifespan of multiple years. A mother who got a free sample of water disinfectant is unlikely to have learned much about the effectiveness of the product when she needs to make a repurchase decision a month later. In contrast, by the time a bed net, filter, or cookstove needs to be replaced a few years later, households will have had ample time to observe their impact on health.
A third dimension concerns the magnitude of the health externality. The health externality is low for water disinfectants, water filters, and cookstoves, high for deworming, and high for bed nets but only above a certain threshold (Hawley et al. (2003), Killeen et al. (2007)).
Putting all this together, we make the following conjectures:
One-time subsidies for cookstoves and water filters have the potential to boost subsequent adoption through learning effects. This boosting effect will be higher than for the Olyset net, given that health externalities are lower for these products; thus, private returns remain large even when coverage rates are high.
A one-time subsidy for water disinfectant is unlikely to have a meaningful impact on subsequent adoption: it will have a possibly negative learning effect (people learn that chlorine tastes bad, but within one month they do not learn that it reduces diarrhea). This is in line with the empirical evidence to date: Ashraf, Berry, and Shapiro (2010) found that Zambian households who are enticed to buy one bottle of disinfectant when it is subsidized end up not using it to purify their water, suggesting a potentially negative learning effect (they were put off by the chlorinated taste) or no learning at all (they did not even try it). Dupas et al. (2013) looked at the long-run impact of giving just one free bottle of water disinfectant to mothers of young children in Kenya, and, while they saw an increase in short-run adoption among subsidy recipients, they found no effect whatsoever on the probability that households use water disinfectant two years later. A longer subsidy (repeated free trials), on the other hand, appears to boost long-run adoption.
A one-time subsidy for deworming is likely to reduce subsequent adoption: it will have a negative learning effect. This is also in line with the evidence to date: Kremer and Miguel (2007) observed lower adoption rates of deworming treatment among households who have more social contacts who received a deworming subsidy, and argued that this is driven mostly by households learning that the private returns to deworming are outweighed by private costs.
6. CONCLUSION
It is often argued that subsidies for high-return technologies or products in the short run might be detrimental for their adoption in the long run. There are two main arguments: (1) subsidies may not foster learning about the technology nor improve health if subsidy recipients do not use it; and (2) previously encountered prices may act as “anchors” that affect people’s valuation of a product independently of its intrinsic qualities.
This paper used a randomized field experiment to estimate the effect of a one-time, targeted subsidy on the long-run adoption of a new health product (the long-lasting antimalarial bed net Olyset), which is both more comfortable and more effective than its predecessor. We find that temporary subsidies for a subset of households increase short-run adoption rates among both subsidy recipients and their neighbors, and subsequently increase willingness to pay for bed nets through learning effects that appear to trump any potential anchoring effect. Structural estimation of an experience-good model that allows for both information and health spillovers generates results consistent with an important learning from own experimentation effect, no anchoring around subsidized prices, and positive social diffusion effects of product characteristics.
The extent to which the adoption of new products is affected through “free trial” periods and how it diffuses through neighbors or friends is a central question, especially for less developed economies where modern diffusion channels, such as TV commercials, do not reach the great majority of the population. The empirical evidence provided in this paper suggests that, at least for some class of preventative health products, learning by doing and social learning are important channels through which short-term, targeted subsidies can affect long-run adoption. The extent to which these results would apply to curative health products may vary depending on the availability of information on the true underlying cause of illness (Adhvaryu (2012), Cohen, Dupas, and Schaner (2013)) and the counterfeit prevalence (Björkman, Svensson, and Yanagizawa-Drott (2012)).
APPENDIX
Figure A.1—Number of days needed to redeem Phase 1 Olyset voucher, by Phase 1 price group. Notes: Data from 479 households that redeemed their Phase 1 voucher.
TABLE A.I.
Health Effects
| (1) | (2) | |
|---|---|---|
|
Dep. Var Had Malaria in the Month Preceding the 1-Yr Follow-up Survey |
||
| Phase 1 Price ≤ Ksh 50 (high subsidy) | −0.027 (0.023) | −0.025 (0.023) |
| Share of study households with high subsidy within 500-m radius | −0.079 (0.057) | −0.083 (0.058) |
| Total # of study households within 500-m radius | −0.002 (0.001)* | −0.002 (0.001)* |
| Observations | 937 | 906 |
| Household-level controls | No | Yes |
| Mean of dep. variable in non-“high subsidy” group | 0.098 | 0.098 |
Notes: Sample restricted to the four areas where the first year follow-up was conducted for both redeemers and non-redeemers of the Phase 1 voucher. Coefficient estimates obtained using linear regression with area fixed effects and gender fixed effects. Sample includes up to two observations per household (male and female head). Standard errors are clustered at the household level. Price varies from 0 to US$3.8. Household level controls in column 2 include all variables presented in Table I.
Significant at 10%;
significant at 5%;
significant at 1%.
Sensitivity of maximum likelihood estimates. Notes: This graph shows how the ML estimates vary as the imputed values for the scalars λ, t, α, υ2, and c change. For each of these, we re-estimated the ML estimates for μ, l1, l2, r, and a under 11 possible values over the range shown on the x-axis, holding the other four scalars at their benchmark values. Benchmark values are: λ = 1.6, t = 0.6, α = 0.8, υ2 = 0.85, and c = 4.
Footnotes
I am grateful to Jean-Marc Robin, four anonymous referees, Arun Chandrasekhar, Christian Hellwig, Adriana Lleras-Muney, and Aprajit Mahajan for detailed suggestions, and to Sandra Black, Sylvain Chassang, Jessica Cohen, Esther Duflo, Giacomo De Giorgi, Liran Einav, Frederico Finan, Seema Jayachandran, Robert Jensen, Rohini Pande, Jonathan Robinson, Justin Sydnor, and numerous seminar participants for helpful comments and discussions. I thank Moses Baraza, Katie Conn, and their field team for their outstanding project implementation and data collection. The study was funded by the Acumen Fund, the Adessium Foundation, the ExxonMobil Foundation, and a Dartmouth Faculty Burke Award. The Olyset nets used in the study were donated by Sumitomo Chemical. The data and analysis code are available online (see Dupas (2014)). All errors are my own.
Recent experiments conducted in urban Zambia and rural Kenya find no evidence for the psychological sunk cost effect, however (Ashraf, Berry, and Shapiro (2010), Cohen and Dupas (2010)).
When 23 local retail shops around the study areas were offered the opportunity to stock Olyset nets, they were unwilling to purchase Olyset nets at wholesale prices above $1.50, fearing lack of demand. This is not specific to the study context. Products considered for public subsidies are typically not available at local markets precisely because of low demand at unsubsidized prices.
Around 90% of households in the study areas have children. Since Kenya introduced Free Primary Education in 2003, school participation is high. In 2007, the year this study started, the net primary enrollment rate was estimated at 86% and the gross primary enrollment rate was 113%. We estimate that our sample represents around 80% of all households in the study areas.
A few years prior to this study, the Kenya Central Bureau of Statistics and the World Bank estimated that 68% of individuals in Busia district (the area of study) live below the poverty line, estimated at $0.63 per person per day in rural areas (the level of expenditures required to purchase a food basket that allows minimum nutritional requirements to be met) (Central Bureau of Statistics (2003)).
Whether the female head, male head, or both were interviewed and given the voucher was randomized across households. It had little effect on take-up (see Dupas (2009)). All regressions below include controls for the randomized gender assignment.
Participating retailers were not allowed to keep the proceeds of the study Olyset sales. However, as an incentive to follow the protocol, participating retailers were promised a fixed sum of $75 to be paid upon completion of the study, irrespective of the number of nets sold but conditional on the study rules being strictly respected.
Unfortunately, two areas (randomly selected among the four areas without free distribution) had to be left out at the time of the long-run follow-up for budgetary reasons.
Attrition at follow-up was not correlated with price, and therefore the estimates of the effect of price on adoption are unbiased.
We use neighbors as proxies for social contacts, as we did not map out social networks in the areas of studies. To the extent that our measure of social networks is noisy, this will bias our results downward. Note, however, that neighbors are a very important part of social networks in rural Western Kenya. Data collected by Dupas, Hoffmann, Kremer, and Zwane (2013) in the same area of study show that 68% of women in rural households speak to at least four neighbors daily, and 91% speak to at least four neighbors a few times a week.
Regression estimates confirm that, within village/area, these exposure measures are not significantly correlated with the voucher price (results not shown).
Spatial correlation is a concern because two households who live near each other will have overlapping radii. The greater the distance between two households, the smaller the overlap will be. In fact, once the distance between two households reaches 2r meters, their r-meters radii will not overlap at all. The Conley covariance matrix allows general correlation pattern for distances shorter than 2r. Specifically, it uses weights that are the products of two kernels, one for each geographic coordinate (longitude and latitude). The kernels go from 1 to zero, decreasing linearly with the distance between the two observations and reaching zero when the distance is 2r.
We tested for heterogeneity in the strength of the spillover by own-subsidy status by running a specification interacting Highhj1 and ShareHighhj1. The coefficient on the interaction term was positive but small and insignificant.
Recall that Phase 2 was conducted in only four of the six areas. Panel A of Figure 2 reproduces Panel A of Figure 1, showing the purchase rate in Phase 1, for the subset of households included in Phase 2.
In a specification estimating separately the effects of getting the full subsidy and the high-but-not-full subsidy on Phase 2 purchases, the point estimates for both subsidy groups appear virtually identical to each other, but given the relative small sample size, the standard errors increase and we cannot reject the null for either of them (though the 95% confidence intervals are [−0.026;+0.162] and [−0.044;+0.180] and we can reject any negative impact of more than a few percentage points).
Follow-up data on the usage of the Olyset net obtained with the second voucher suggests that the second Olyset had indeed lower immediate returns for households: the Olyset acquired with the second voucher was 23% more likely to still be in its package at the time of the follow-up visit two to four months later (potentially suggesting that part of the demand for the second Olyset was driven by hoarding, since that type of net was not available on the market at the time of the study). Respondents who had their Olyset in its package reported storing it for the future. As long as the discount factor is less than 1, this implies lower returns (everything else constant) to the second Olyset.
The rate was 96% among those who had started using the Olyset, and 70% among those who had purchased it but not yet started using it.
Table A.I presents regression results where the unit of observation is an adult, the dependent variable is whether the person is reported as having had a malaria episode in the month preceding the 1-year follow-up survey, and the regressors of interest are own and peers’ Phase 1 subsidy status. There are up to two observations per household (the husband and the wife). Standard errors are clustered at the household level.
This is a strong assumption. We make it because it would not be possible to estimate separately the health effectiveness information spillover from the health spillover, since the same variation in neighborhood coverage drives both. Since empirically it seems the effect of the health spillover dominates, we ignore spillovers in learning about health effectiveness, but we acknowledge this as a limitation.
This linear form for gain–loss utility means no diminishing sensitivity. We have estimated the model using a power gain–loss function (Tversky and Kahneman (1991)) and various levels for the degree of diminishing sensitivity, and the results are unchanged. We show the results with the linear assumption for simplicity.
For products that are available on the market, forward-looking households could invest in a product even if the myopic gains are outweighed by the costs, for the option value of learning. The magnitude of this option value will depend on beliefs with respect to the long-run price, but nonlinearly: if people expect the price in the long run to be outside their budget set, then the option value of learning is zero. If they expect the long-run price to be free, the option value is also zero. But at intermediate price beliefs, the option value of learning will be positive. To the extent households are forward-looking this way, the scope for subsidies to affect short- and long-run adoption will be reduced.
The probability to learn l1 from a social contact who owns the product is 1. The probability that a given social contact owns the product is The chance that the household does not learn l1 from a given social contact is thus , and the chance of learning from at least one contact is .
The model assumes that all those who acquire the product in the first period experiment with it and get both signals (l1 and l2) on quality. We make the simplification of equating acquisition to usage, since it is what we observe empirically (remember Figure 2, panel B). For products that are more costly to use than anticipated (e.g., people only discover how badly chlorinated water tastes once they have tried it once), it is possible that the initial learning l1 is negative—that is, the mean prior decreases right after acquisition, and some households may, after that, not find it worthwhile to use the product (as found in Ashraf, Berry, and Shapiro (2010)). In that case, they would not receive the private signal r1h and their period 2 decision would depend on their downward-revised prior on quality, the distribution . This would reduce the scope for subsidies to boost adoption in the long run.
The thresholds identified in the literature are 50% (Hawley et al. (2003)) and 35–65% (Killeen et al. (2007)). Here we take a slightly higher threshold of 60%, since our sample includes only around 80% of the total population in the areas of study.
We picked 0.85 because it is an upper bound for discount factors elicited experimentally (see, e.g., Schaner (2013) for a mean estimated weekly discount factor as low as 0.70 in rural Kenya, and Harrison, Lau, and Melonie (2002) for an average discount rate of 28% (equivalent to a discount factor of 0.78) in Denmark). Sensitivity of the results to the value of this parameter is presented in Figure A.2 and discussed below.
We use the 250-m radius for the information spillover versus the 500-m radius for the health spillover to help with the identification. The neighborhood variables are obviously highly correlated between the 250- and 500-m radii, but not identical, and the variation between the two (which is random) is useful for identification.
The model does not allow for an income (via health) effect. The one-year follow-up survey data, however, suggest that the incidence of malaria among household heads (either the male or the female) may have been lower among households who received a high subsidy in Phase 1, though we do not have enough statistical power to reject the null of no health effect (see Appendix Table A.I). A health effect among household heads could potentially have generated an income effect. We do not have data on income to directly test for an income effect, which means that, in the estimation, any potential income effect is picked up by the learning from experimentation. parameter (l2). Our estimate of learning may therefore be an overestimate.
REFERENCES
- Adhvaryu A. Working Paper. University of Michigan; 2012. Learning, Misallocation, and Technology Adoption: Evidence From New Malaria Therapy in Tanzania. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ariely D, Loewenstein G, Prelec D. Coherent Arbitrariness: Stable Demand Curves Without Stable Preferencesa. Quarterly Journal of Economics. 2003;118(1):73–106. [Google Scholar]
- Ashraf N, Berry J, Shapiro J. Can Higher Prices Stimulate Product Use? Evidence From a Field Experiment in Zambia. American Economic Review. 2010;100(5):2383–2413. [Google Scholar]
- Bergemann D, Välimäki J. Experimentation in Markets. The Review of Economic Studies. 2000;67(2):213–234. [Google Scholar]
- Bergemann D, Välimäki J. Dynamic Pricing of New Experience Goods. The Journal of Political Economy. 2006;114(4):713–743. [Google Scholar]
- Björkman M, Svensson J, Yanagizawa-Drott D. Working Paper. Harvard University; 2012. Can Good Products Drive Out Bad? Experimental Evidence From Local Markets for Antimalarial Medicine in Uganda. [Google Scholar]
- Booij AS, Van Praag BMS, Van den Kullen G. A Parametric Analysis of Prospect Theory Is Functionals for the General Population. Theory and Decision. 2010;68:115–148. [Google Scholar]
- Central Bureau of Statistics. From Districts to Locations. Vol. I. Nairobi: The Regal Press Kenya Ltd; 2003. Geographic Dimensions of Well-Being in Kenya: Where Are the Poor? Online at http://www.worldbank.org/research/povertymaps/kenya/volume_index.htm. [Google Scholar]
- Chassang S, Padro i Miquel G, Snowberg E. Selective Trials: A Principal-Agent Approach to Randomized Controlled Experiments. American Economic Review. 2012;102(4):1279–1309. [Google Scholar]
- Cohen J, Dupas P. Free Distribution or Cost-Sharing? Evidence From a Randomized Malaria Experiment. Quarterly Journal of Economics. 2010;125(1):1–45. [Google Scholar]
- Cohen J, Dupas P, Schaner S. Price Subsidies, Diagnostic Tests, and Targeting of Malaria Treatment. Working Paper 17943, NBER. 2013 [Google Scholar]
- Conley T. GMM Estimation With Cross Sectional Dependence. Journal of Econometrics. 1999;92:1–45. [Google Scholar]
- D’Alessandro U. Insecticide-Treated Bed Nets to Prevent Malaria. The Challenge Lies in Implementation. British Medical Journal. 2001;322:249–250. doi: 10.1136/bmj.322.7281.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DellaVigna S. Psychology and Economics: Evidence From the Field. Journal of Economic Literature. 2009;47(2):315–372. [Google Scholar]
- Dupas P. What Matters (and What Does not) in Households’ Decision to Invest in Malaria Prevention? American Economic Review. 2009;99(2):224–230. doi: 10.1257/aer.99.2.224. [DOI] [PubMed] [Google Scholar]
- Dupas P. Supplement to ‘Short-Run Subsidies and Long-Run Adoption of New Health Products: Evidence From a Field Experiment’. Econometrica Supplemental Material. 2014;82 doi: 10.3982/ECTA9508. http://www.econometricsociety.org/ecta/supmat/9508_data_and_programs.zip. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupas P, Hoffmann V, Kremer M, Zwane A. Unpublished Manuscript. Harvard University; 2013. Micro-Ordeals, Targeting and Habit Formation. [Google Scholar]
- Foster A, Rosenzweig M. Microeconomics of Technology Adoption. Annual Review of Economics. 2010;2:395–424. doi: 10.1146/annurev.economics.102308.124433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison GW, Lau MI, Melonie BW. Estimating Individual Discount Rates in Denmark: A Field Experiment. American Economic Review. 2002;92(5):1606–1617. [Google Scholar]
- Hawley WA, Phillips-Howard PA, ter Kuile FO, et al. Community-Wide Effects of Permethrin-Treated Bed Nets on Child Mortality and Malaria Morbidity in Western Kenya. American Journal of Tropical Medicine and Hygiene. 2003;68(4 Suppl):121–127. [PubMed] [Google Scholar]
- Heffetz O, Shayo M. How Large Are Non-Budget-Constraint Effects of Prices on Demand? American Economic Journal: Applied Economics. 2009;1(4):170–199. [Google Scholar]
- Jones G, Steketee R, Black RE the Bellagio Child Survival Study Group. How Many Child Deaths Can We Prevent This Year? Lancet. 2003;362:65–71. doi: 10.1016/S0140-6736(03)13811-1. [DOI] [PubMed] [Google Scholar]
- Killeen GF, Smith TA, Ferguson HM, et al. Preventing Childhood Malaria in Africa by Protecting Adults From Mosquitoes With Insecticide-Treated Nets. PLoS Medicine. 2007;4(7) doi: 10.1371/journal.pmed.0040229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Köszegi B, Rabin M. A Model of Reference-Dependent Preferences. Quarterly Journal of Economics. 2006;121(4):1133–1165. [Google Scholar]
- Kremer M, Miguel E. The Illusion of Sustainability. Quarterly Journal of Economics. 2007;122(3):1007–1065. [Google Scholar]
- Lengeler C. Insecticide-Treated Bed Nets and Curtains for Preventing Malaria. Cochrane Dabatase Syst Rev. 2004;2:CF000363. doi: 10.1002/14651858.CD000363.pub2. [DOI] [PubMed] [Google Scholar]
- Liu L, Johnson HL, Cousens S, et al. for the Child Health Epidemiology Reference Group WHO and UNICEF. Global, Regional, and National Causes of Child Mortality: An Updated Systematic Analysis for 2010 With Time Trends Since 2000. Lancet. 2012;379:2151–2161. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- Manski C. Identification of Endogenous Social Effects: The Reflection Problem. Review of Economic Studies. 1993;60(3):531–542. [Google Scholar]
- Mazar N, Koszegi B, Ariely D. Working Paper. UC Berkeley; 2009. Price-Sensitive Preferences. [Google Scholar]
- Mcfadden D. Rationality for Economists? Journal of Risk and Uncertainty. 1999;19:73–105. [Google Scholar]
- Munshi K, Myaux J. Social Norms and the Fertility Transition. Journal of Development Economics. 2006;80(1):1–38. [Google Scholar]
- Oster E, Thornton R. Determinants of Technology Adoption: Private Value and Peer Effects in Menstrual Cup Take-Up. Journal of the European Economic Association. 2012;10(6):1263–1293. [Google Scholar]
- Sachs J. The End of Poverty: Economic Possibilities for Our Time. New York: Penguin Press; 2005. [DOI] [PubMed] [Google Scholar]
- Schaner S. Working Paper. Dartmouth College; 2013. Do Opposites Detract? Intrahousehold Preference Heterogeneity and Inefficient Strategic Savings. [Google Scholar]
- Simonsohn U, Loewenstein G. Mistake #37: The Effect of Previously Encountered Prices on Current Housing Demand. Economic Journal. 2006;116(508):175–199. [Google Scholar]
- Simonson I, Tversky A. Choice in Context—Tradeoff Contrast and Extremeness Aversion. Journal of Marketing Research. 1992;29(3):281–295. [Google Scholar]
- Tarozzi A, Mahajan A, Blackburn B, Kopf D, Krishnan L, Yoong J. Micro-Loans, Insecticide-Treated Bednets and Malaria: Evidence From a Randomized Controlled Trial in Orissa (India) Unpublished Manuscript. 2013 doi: 10.1257/aer.104.7.1909. [DOI] [PubMed] [Google Scholar]
- Tversky A, Kahneman D. Loss Aversion in Riskless Choice: A Reference-Dependent Model. Quarterly Journal of Economics. 1991;106(4):1039–1061. [Google Scholar]
- WHO. WHO Global Malaria Programme: Position Statement on ITNs. 2007 Available at http://www.who.int/malaria/publications/atoz/itnspospaperfinal.pdf.