Abstract
This article provides an overview of current trends in health expenditures in 29 OECD countries and recent revisions of OECD health accounts. U.S. health expenditures are compared with those of other OECD countries. The interactions of cost-containment measures with changes in the public-private mix of financing and in the composition of health care spending are discussed.
Introduction
The provision of health care services now constitutes one of the largest industries in OECD countries. The impact of this sector is evidenced by the widespread public interest in the constant flow of new innovations reported in the media.
Near-universal coverage of the population under public and private health plans has been achieved in most OECD countries, and there have been impressive gains in the health status of populations in all of these countries.
There remain, however, recurrent concerns regarding the adequacy of resources; the way they are used; and how best to increase the equity, efficiency, and effectiveness of health care. After a decade or more of health care reform, the question of how best to organize health care and its financing remains high on the political agenda in many OECD countries.
To assist health care policymakers and researchers with international comparisons, the OECD Secretariat publishes an annual information system on CD-ROM, OECD Health Data (Organization for Economic Cooperation and Development, 1999a). This covers data on key aspects of health care systems in the 29 OECD member countries and their general demographic, economic, and social contexts (Organization for Economic Cooperation and Development, 1999a; Anderson and Poullier, 1999).
In this article, I provide an overview and basic analysis of the health accounts collected annually by the OECD Secretariat. This updates and complements some of the earlier synthesis and research on this subject (Organization for Economic Cooperation and Development, 1995, 1993; Schieber, Poullier, and Greenwald, 1994) and previous presentations in this journal (Schieber, Poullier, and Greenwald, 1992). Levels of and trends in health expenditures are compared in absolute terms and relative to overall economic growth. The determinants of health care spending growth are revisited.
Progress in the international comparability of health expenditure estimates depends heavily on the quality and detail of national health accounts in OECD member countries.
Although decisive progress in health accounting has been made in several countries over the last 5 years, much research and statistical work remains to be done to make health accounts more comprehensive and comparable across countries. Serious gaps remain in the scope of the data, and problems remain in the comparability of the data across countries. A short overview of recent progress in the methodology of the OECD health accounts and reports on revisions to the expenditure estimates appears later in this article.
1990-1997 Trends Relative to GDP
After many years in which health expenditures grew faster than the economy, in 1997, the United States spent about the same proportion of its gross domestic product (GDP) on health care as in 1992. The trend in this expenditure ratio in the United States is thus for the first time parallel to the average across 25 OECD countries, for which long time series are available (Figure 1 and Table 1) (Organization for Economic Cooperation and Development, 1999d).
Figure 1. Total Health Expenditures as a Percent of Gross Domestic Product: 1970-1997.
Table 1. Total Health Care Expenditures as a Percent of Gross Domestic Product: 1970-1997.
| Country | 1970 | 1980 | 1990 | 1995 | 1997 |
|---|---|---|---|---|---|
|
| |||||
| Percent | |||||
| United States | 7.3 | 9.1 | 12.6 | 14.1 | 13.9 |
| Japan | 4.6 | 6.5 | 6.1 | 7.2 | 7.2 |
| Germany | 6.3 | 8.8 | 8.7 | 10.4 | 10.7 |
| France | 5.8 | 7.6 | 8.9 | 9.8 | 9.6 |
| Italy | 5.2 | 7.0 | 8.1 | 7.7 | 7.6 |
| United Kingdom | 4.5 | 5.6 | 6.0 | 6.9 | 6.8 |
| Canada | 7.0 | 7.2 | 9.2 | 9.4 | 9.2 |
| Average of the 7 Countries | 5.8 | 7.4 | 8.5 | 9.4 | 9.3 |
| Australia | 5.7 | 7.3 | 8.2 | 8.4 | 8.4 |
| Austria | 5.3 | 7.7 | 7.2 | 8.0 | 8.3 |
| Belgium | 4.1 | 6.5 | 7.5 | 7.9 | 7.6 |
| Czech Republic | — | 3.8 | 5.4 | 7.5 | 7.2 |
| Denmark | 5.9 | 9.3 | 8.3 | 8.1 | 8.0 |
| Finland | 5.7 | 6.5 | 8.0 | 7.7 | 7.4 |
| Greece | 5.7 | 6.6 | 7.6 | 8.4 | 8.6 |
| Hungary | — | — | 6.1 | 7.0 | 6.5 |
| Iceland | 5.0 | 6.2 | 7.9 | 8.2 | 7.9 |
| Ireland | 5.3 | 8.7 | 6.7 | 7.0 | 6.3 |
| Korea | 2.3 | 3.7 | 5.2 | 5.4 | 6.0 |
| Luxembourg | 3.7 | 6.2 | 6.6 | 6.7 | 7.0 |
| Mexico | — | — | 3.6 | 4.9 | 4.7 |
| Netherlands | 5.9 | 7.9 | 8.3 | 8.8 | 8.5 |
| New Zealand | 5.2 | 6.0 | 7.0 | 7.3 | 7.6 |
| Norway | 4.5 | 7.0 | 7.8 | 8.0 | 7.5 |
| Poland | — | — | 4.4 | 4.5 | 5.2 |
| Portugal | 2.8 | 5.8 | 6.4 | 7.8 | 7.9 |
| Spain | 3.7 | 5.6 | 6.9 | 7.3 | 7.4 |
| Sweden | 7.1 | 9.4 | 8.8 | 8.5 | 8.6 |
| Switzerland | 4.9 | 6.9 | 8.3 | 9.6 | 10.0 |
| Turkey | 2.4 | 3.3 | 3.6 | 3.3 | 4.0 |
| European Union | 5.1 | 7.3 | 7.6 | 8.1 | 8.0 |
| OECD Europe1 | 4.9 | 7.0 | 7.5 | 7.9 | 7.9 |
| Total OECD1 | 5.0 | 6.9 | 7.6 | 8.1 | 8.1 |
Unweighted arithmetic average. Figures exclude Czech Republic, Hungary, Mexico, and Poland.
NOTE:OECD is Organization for Economic Cooperation and Development.
In 1997, the United States spent approximately 90 percent more on health care as a share of GDP than in 1970. Health expenditures thus increased at a faster pace in the United States than in other OECD countries, which on average are now spending a 60-percent greater share of their GDP on health care than in 1970. In several OECD countries, modest declines during the 1990s were related both to economic upswings in countries and to reforms that have limited the rate of increase in health spending in relation to the rate of growth in GDP (Organization for Economic Cooperation and Development, 1999b).
The United States is now among a group of countries in which the percentage of GDP devoted to health care has stabilized or declined slightly since the early-to-mid-1990s. This gives rise to the question of whether such stabilization can be sustained or is a transitory phenomenon.
A full listing of the factors that account for growth in health expenditures—both in absolute terms and relative to overall economic development—would require a detailed analysis per country, which is not the subject of this article. Here, I concentrate on international comparisons, which draw mainly on lessons learned from the latest version of the comparative data sets of OECD Health Data 99 (Organization for Economic Cooperation and Development, 1999a).
An immediate question to ask is whether the stabilization of expenditure trends over the last couple of years is due mainly to an upswing in the business cycle in many countries. To analyze this question, an alternative expenditure ratio was calculated, which divides health expenditures by trended GDP instead of current GDP and is somewhat smoother than and more independent of the business cycle.
Table 2 shows that there are clear signs of a real stabilization of the growth of health spending in relation to trend GDP. An expenditure ratio, measured in this way, remained constant on average in 25 OECD countries, from 1995 to 1997, showing less than -0.1 to +0.1 percent of change for 10 countries (including the United States), declining expenditure ratios for 7 countries, and increasing ratios for another 8.
Table 2. Percentage Point Change in Health Care Expenditures as a Percent of Gross Domestic Product: 1975-1997.
| Country | 1975 to 1985 | 1985 to 1995 | 1995 to 1997 |
|---|---|---|---|
|
| |||
| Percentage Point Change | |||
| United States | 2.6 | 3.3 | 0.0 |
| Japan | 1.2 | 0.3 | 0.3 |
| Germany | 0.6 | 1.2 | 0.2 |
| France | 1.4 | 1.4 | -0.2 |
| Italy | 1.0 | 0.7 | -0.3 |
| United Kingdom | 0.4 | 1.0 | -0.1 |
| Canada | 1.3 | 0.8 | -0.3 |
| Average of the 7 Countries | 1.2 | 1.2 | -0.1 |
| Australia | 0.2 | 0.6 | -0.1 |
| Austria | -0.6 | 1.4 | 0.3 |
| Belgium | 1.3 | 0.6 | -0.2 |
| Czech Republic1 | — | 3.0 | -0.3 |
| Denmark | 2.7 | -0.9 | 0.1 |
| Finland | 0.6 | 0.0 | 0.1 |
| Iceland1 | 1.5 | 0.9 | -0.3 |
| Ireland | 0.0 | -0.6 | -0.6 |
| Korea1 | 2.0 | 1.1 | 0.6 |
| Luxembourg1 | 1.0 | 0.6 | 0.3 |
| Netherlands | 0.5 | 0.8 | -0.1 |
| New Zealand | -2.0 | 2.0 | 0.3 |
| Norway | 1.8 | 0.9 | -0.1 |
| Portugal | 0.7 | 1.8 | 0.0 |
| Spain | 0.7 | 1.6 | 0.1 |
| Sweden | 1.0 | -0.9 | 0.1 |
| Switzerland | — | 1.5 | 0.4 |
| Turkey1 | -0.5 | 1.1 | 0.7 |
| European Union2 | 0.8 | 0.6 | 0.0 |
| OECD Europe2 | 0.8 | 0.8 | 0.0 |
| Total OECD2 | 0.8 | 1.0 | 0.0 |
Changes in health share of nominal gross domestic product. Series for trend gross domestic product were unavailable.
Unweighted arithmetic average. Figures exclude Greece, Hungary, Mexico, and Poland.
NOTE:OECD is Organization for Economic Cooperation and Development.
Per Capita Expenditure on Health Care
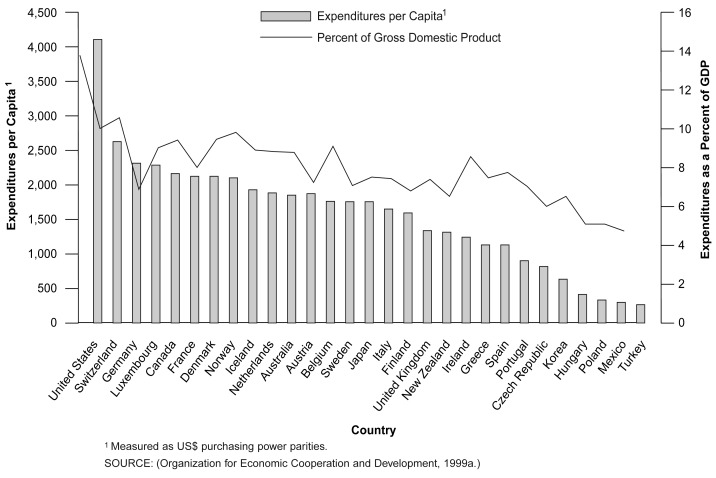
Figure 2 and Table 3 show that countries differ less in terms of expenditure ratios than per capita expenditures. The United States still spends far more per capita on health care than any other OECD country, outspending Canada on an average per capita basis by 2 to 1, Japan by 2.3 to 1, and all other OECD countries by 2.5 to 1.
Figure 2. Health Care Expenditures per Capita and as a Percent of Gross Domestic Product: 1997.
Table 3. Per Capita Expenditures1 on Health Care: 1970-1998.
| Country | 1970 | 1980 | 1990 | 1995 | 1997 | 19982 |
|---|---|---|---|---|---|---|
| United States | 357 | 1,086 | 2,798 | 3,776 | 4,095 | 4,270 |
| Japan | 131 | 524 | 1,082 | 1,637 | 1,760 | 1,780 |
| Germany | 224 | 824 | 1,602 | 2,178 | 2,364 | 2,400 |
| France | 206 | 701 | 1,539 | 1,984 | 2,047 | 2,120 |
| Italy | 154 | 579 | 1,321 | 1,534 | 1,613 | — |
| United Kingdom | 144 | 444 | 955 | 1,253 | 1,391 | 1,450 |
| Canada | 262 | 716 | 1,695 | 2,106 | 2,175 | 2,250 |
| Average of 7 Countries | 211 | 696 | 1,570 | 2,067 | 2,206 | — |
| Australia | 207 | 663 | 1,320 | 1,778 | 1,909 | — |
| Austria | 159 | 663 | 1,205 | 1,675 | 1,905 | — |
| Belgium | 130 | 578 | 1,247 | 1,698 | 1,768 | — |
| Czech Republic | — | — | 575 | 898 | 943 | 950 |
| Denmark | 216 | 832 | 1,424 | 1,855 | 2,042 | 2,100 |
| Finland | 163 | 510 | 1,292 | 1,414 | 1,525 | — |
| Greece | 100 | 345 | 702 | 1,054 | 1,196 | — |
| Hungary | — | — | 510 | 625 | 642 | — |
| Iceland | 137 | 577 | 1,374 | 1,826 | 1,981 | 2,190 |
| Ireland | 98 | 455 | 759 | 1,246 | 1,293 | 1,390 |
| Korea | 15 | 87 | 401 | 688 | 870 | — |
| Luxembourg | 147 | 605 | 1,495 | 2,120 | 2,303 | — |
| Mexico | — | — | 210 | 335 | 363 | — |
| Netherlands | 202 | 679 | 1,326 | 1,777 | 1,933 | — |
| New Zealand | 174 | 458 | 937 | 1,244 | 1,357 | 1,440 |
| Norway | 131 | 632 | 1,365 | 1,860 | 2,017 | — |
| Poland | — | — | 216 | 296 | 386 | — |
| Portugal | 43 | 260 | 614 | 1,046 | 1,148 | — |
| Spain | 82 | 325 | 815 | 1,063 | 1,183 | — |
| Sweden | 270 | 850 | 1,492 | 1,623 | 1,762 | — |
| Switzerland | 252 | 801 | 1,760 | 2,464 | 2,611 | — |
| Turkey | 23 | 75 | 171 | 188 | 259 | — |
| European Union | 156 | 577 | 1,186 | 1,568 | 1,698 | — |
| OECD Europe | 152 | 565 | 1,182 | 1,571 | 1,702 | — |
| Total OECD | 161 | 571 | 1,110 | 1,491 | 1,615 | — |
Measured as US$ purchasing power parities.
Estimated.
NOTE:OECD is Organization for Economic Cooperation and Development.
U.S. health care spending per capita was $4,095 in 1997, compared with an average of $1,615 (calculated on a U.S. dollar GDP purchasing power parity [PPP] basis) for the OECD as a whole and $1,698 in the European Union. Switzerland had the second-highest spending per capita, followed by Germany, Luxembourg, and Canada.
There are two main reasons why countries differ less in terms of expenditure ratios than in per capita expenditures. First, there seems to be some correlation between low health expenditure ratios and lower per capita GDP. (However, recent revisions of health expenditure estimates in several OECD countries have shown that this association is partly a statistical artifact: The lower income countries tended to underestimate private spending on health and consequently their overall expenditure ratio.) Second, and perhaps more important, expenditure comparisons depend critically on the monetary conversion factor chosen.
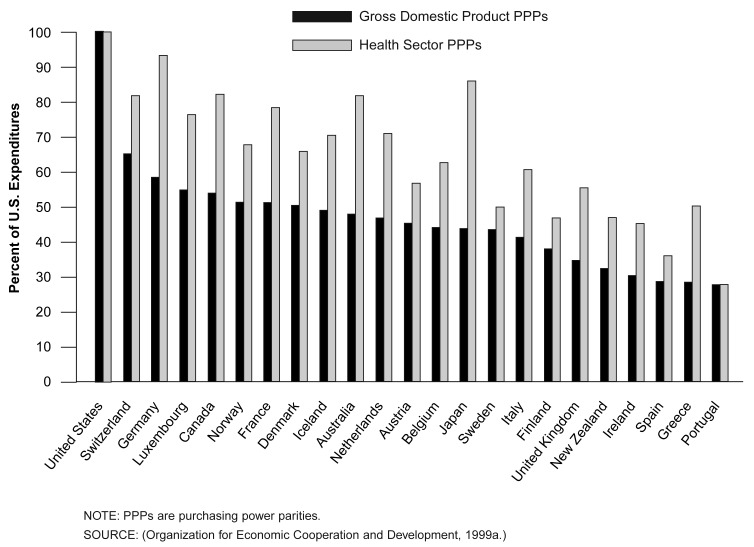
U.S. dollar GDP PPPs are the conversion factor used in Figure 2. However, overall, GDP PPPs differ substantially from health sector PPPs for many countries. Figure 3 shows that per capita expenditures calculated using health sector PPPs vary less across countries. For the United States, this means that the difference in per capita expenditures between the United States and all other OECD countries is largely the result of higher relative prices for health care in the United States (Gerdtham and Jönsson, 1991; Evans, 1998).
Figure 3. Health Care Expenditures per Capita as a Percent of U.S. Expenditures: 1996.
Unfortunately, price comparisons and PPPs for health care goods and services are among the weak points in international health care data sets. Health-specific PPPs and hence the results shown in Figure 3 should therefore be used with caution
Convergence or Divergence of Expenditure Patterns?
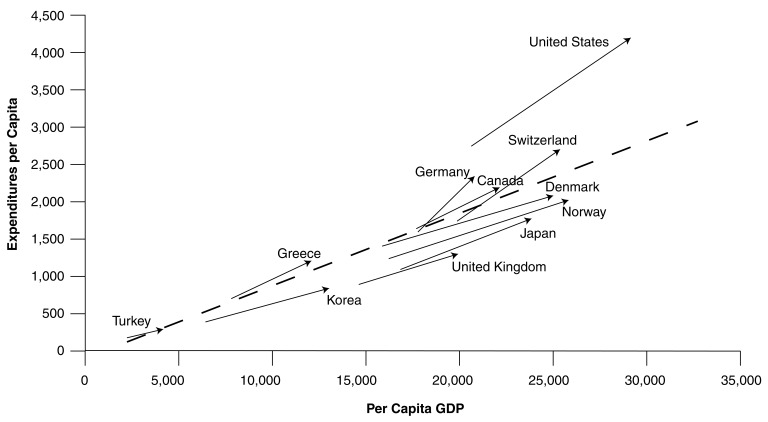
A well-known observation is that growing wealth is associated with higher per capita health spending both over time and across countries. The most frequent illustration of this fact is provided in Figure 4, which compares per capita health spending with per capita GDP figures for the year 1997.
Figure 4. Distribution of per Capita Income and per Capita Health Care Expenditures: 1997.
Figure 4 suggests that OECD countries fall into three broad clusters according to income class: countries with annual per capita incomes of US$20,000 and less; those with average incomes between US$20,000 and US$30,000; and the two countries with the highest incomes, the United States and Luxembourg, which are apparent outliers from the linear relationship.
The association between income and health expenditure seems to be much stronger for the first cluster than for the remaining countries, for which similar income levels are associated with substantially different health expenditure levels. As an illustration: Split into two groups at the US$20,000 level, a regression for the first lower income group shows an R2 measure that is more than twice as high as that of the second group: 0.94 compared with 0.42. (Different functional forms and more sophisticated econometric techniques are necessary for a more refined analysis of the determinants of health expenditures across OECD countries. Compare New Directions in Health Care Policy [Organization for Economic Cooperation and Development, 1995] for an overview of methodology and results of pooled cross-section and time-series analysis.)
Of the second group, all but one of the Scandinavian countries lie below the trend lines, as do Japan, Ireland, and the United Kingdom. Germany, France, and Switzerland are the three countries spending considerably more than what would be expected from the trend line in Figure 4.
Health care spending in Germany is relatively high compared with its per capita GDP mainly because health care spending in the 5 eastern and 11 western States have converged much faster after reunification than did overall economic productivity. Sweden, the Netherlands, and Canada are all close to or on the trend line.
The slope of the trend line and the R2 vary over time with individual countries moving closer to or further away from the trend line (Schieber, Poullier, and Greenwald, 1992). Hints on specific developments in individual countries are provided by Figure 5, which illustrates the way in which some countries have converged with and other countries have diverged from the OECD trend. Arrows show the movement of countries away from and toward the common trend shown by the combined sample of both years.
Figure 5. Change in per Capita Health Care Expenditures Relative to Change in per Capita GDP1 1990-1997.
1Measured in US$ purchasing power parities.
NOTES: GDP is gross domestic product. The beginning of the arrows indicates health spending and GDP per capita in 1990. The end of the arrow indicates the corresponding values for 1997.
SOURCE: (Organization for Economic Cooperation and Development, 1999a.)
As has been noted in previous analysis for various time periods, the United States moved further away from the common trend of other OECD countries in the years before 1993, the year after which the United States spending ratio stabilized. Other diverging countries are Germany (because of the economic shock of reunification as already mentioned), Switzerland, and Luxembourg. In several countries, such as Greece, Canada, and the United Kingdom, health expenditures grew parallel to the overall trend. Some Scandinavian countries, such as Denmark and Norway, seem to have been more successful with cost-containment measures than other OECD countries.
Continuing Stabilization in 1998
Will the stabilization of health expenditure trends, observed recently in a majority of OECD countries, continue into the near future? The answer to this question is of interest not only to policymakers and health care planners but also to the whole range of suppliers of health care services and goods. And it increasingly interests the broad public, which has a growing awareness that cost-containment measures applied to health care under public budgets may affect access to services, coverage under public programs, and copayment levels.
Table 4 provides a synthesis of some current projections for the year 1998 and/or preliminary health expenditure estimates for a selection of OECD countries together with preliminary GDP figures. Sources and methods for these estimates can be found in OECD Health Data (Organization for Economic Cooperation and Development, 1999b).
Table 4. Estimated Health Care Expenditures as a Percent of Gross Domestic Product (GDP): 1997-1998.
| Country | Health Care Expenditures | Change in GDP | |||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| 1997 | 1998 | 1997-1998 | |||||
|
|
|
|
|||||
| Total | Public | Total | Public | Total | Public | ||
|
| |||||||
| Percent of GDP | Percent Change | ||||||
| United States | 13.9 | 6.5 | 14.0 | 6.5 | 5.3 | 5.8 | 4.9 |
| Japan | 7.2 | 5.7 | 7.4 | 5.8 | 0.8 | -1.0 | -2.5 |
| Germany | 10.7 | 8.3 | 10.6 | 8.1 | 2.3 | 1.5 | 3.7 |
| France | 9.6 | 7.1 | 9.6 | 7.1 | 3.5 | 3.8 | 4.0 |
| United Kingdom | 6.8 | 5.8 | 6.9 | 5.8 | 5.6 | 6.0 | 4.6 |
| Canada | 9.2 | 6.4 | 9.3 | 6.5 | 3.8 | 3.7 | 2.6 |
| Czech Republic | 7.2 | 6.6 | 7.2 | 6.6 | 7.6 | 8.1 | 7.7 |
| Denmark | 8.0 | 6.7 | 8.0 | 6.7 | 3.9 | 3.9 | 4.4 |
| Iceland | 7.9 | 6.7 | 8.3 | 7.0 | 14.8 | 16.0 | 10.5 |
| Ireland | 6.3 | 4.9 | 6.1 | 4.8 | 10.9 | 13.4 | 14.8 |
| New Zealand | 7.6 | 5.9 | 8.0 | 6.2 | 7.0 | 6.6 | 0.9 |
NOTE: Data for 1998 are estimated.
Expenditure ratios tend to remain relatively stable or increase slightly for the countries analyzed in Table 4. For Japan and New Zealand, expenditure ratios are estimated to increase mainly because of low or negative growth of the national economy compared with moderate increases in health expenditure.
Decomposition of Health Expenditure Growth
The decomposition of health expenditure growth into price and volume components is used on a regular basis in many countries for projections of national health expenditures. A similar approach, applied to a cross-section comparison of expenditure growth across countries, helps to identify which growth elements underlie the marked increase of health expenditure ratios relative to GDP in past years. For these decompositions, readers should be aware that price and volume measurement is an extremely difficult task for health care services. International comparisons of trends of expenditure in real terms should consequently be used with caution
This section provides an update of the basic model developed for this purpose. (For more details on the underlying mathematics, refer to Schieber and Poullier, 1989, and Schieber, Poullier, and Greenwald, 1992.) Estimates of the relative magnitude of the growth elements are shown in Table 5 for 16 OECD countries. A comparison of these calculations for 1980-1996 reveals surprisingly similar results to tables published earlier.
Table 5. Percent Change in Health Expenditures and Factors Accounting for That Growth: 1980-1996.
| Country | Annual Compound Rite of Growth,1980-1996
|
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Health Expenditures as a Percent of GDP | Nominal Health Expenditure Growth | Health care Price Inflation
|
Real Health Expenditure Growth
|
Real GDP Growth
|
|||||||||
| Health Expenditures as a Percent of GDP
|
Total | Economywide Inflation | Excess Health Care Inflation | Total | Population Growth | Growth in Real Spending per capita | Total | Real GDP per Capita | Excess per Capita Volume Growth | ||||
| 1980 | 1996 | ||||||||||||
| United States | 9.1 | 14.1 | 2.7 | 9.4 | 6.1 | 3.8 | 2.2 | 3.1 | 1.0 | 2.1 | 2.6 | 1.6 | 0.5 |
| Japan | 6.5 | 7.1 | 0.6 | 5.3 | 1.9 | 1.5 | 0.5 | 3.3 | 0.5 | 2.8 | 3.2 | 2.7 | 0.1 |
| Germany | 8.8 | 10.8 | 1.3 | 6.9 | 3.4 | 3.0 | 0.4 | 3.5 | 1.8 | 1.6 | 2.5 | 0.7 | 0.9 |
| France | 7.6 | 9.8 | 1.6 | 8.4 | 4.0 | 4.8 | -0.7 | 4.2 | 0.5 | 3.7 | 1.8 | 1.3 | 2.4 |
| Italy | 7.0 | 7.8 | 0.7 | 11.2 | 9.4 | 8.4 | 0.9 | 1.6 | 0.1 | 1.5 | 1.8 | 1.7 | -0.1 |
| United Kingdom | 5.6 | 6.9 | 1.3 | 8.9 | 6.6 | 5.2 | 1.3 | 2.2 | 0.3 | 1.9 | 2.2 | 1.9 | 0.0 |
| Canada | 7.2 | 9.3 | 1.6 | 7.9 | 4.8 | 3.8 | 1.0 | 3.0 | 1.2 | 1.7 | 2.3 | 1.0 | 0.7 |
| Average of the 7 Countries | 7.4 | 9.4 | 1.4 | 8.3 | 5.2 | 4.4 | 0.8 | 3.0 | 0.8 | 2.2 | 2.3 | 1.6 | 0.6 |
| Australia | 7.3 | 8.6 | 1.1 | 9.7 | 5.2 | 5.4 | -0.2 | 4.2 | 1.4 | 2.8 | 2.9 | 1.5 | 1.3 |
| Austria | 7.7 | 8.0 | 0.2 | 5.8 | 5.3 | 3.4 | 1.9 | 0.5 | 0.4 | 0.1 | 2.2 | 1.7 | -1.6 |
| Belgium | 6.5 | 7.8 | 1.1 | 6.7 | 4.8 | 3.8 | 1.0 | 1.8 | 0.2 | 1.6 | 1.7 | 1.5 | 0.1 |
| Denmark | 9.3 | 8.1 | -0.9 | 5.7 | 4.1 | 4.3 | -0.2 | 1.5 | 0.2 | 1.4 | 2.2 | 2.0 | -0.7 |
| Finland | 6.5 | 7.8 | 1.2 | 8.3 | 6.8 | 5.0 | 1.7 | 1.5 | 0.4 | 1.0 | 2.0 | 1.5 | -0.5 |
| Netherlands | 7.9 | 8.7 | 0.6 | 4.9 | 2.4 | 2.0 | 0.3 | 2.5 | 0.6 | 1.9 | 2.2 | 1.6 | 0.3 |
| Norway | 7.0 | 7.8 | 0.7 | 8.4 | 5.8 | 4.5 | 1.2 | 2.5 | 0.4 | 2.1 | 3.0 | 2.6 | -0.5 |
| Spain | 5.6 | 7.4 | 1.7 | 12.2 | 7.3 | 7.8 | -0.4 | 4.6 | 0.3 | 4.3 | 2.4 | 2.1 | 2.1 |
| Switzerland | 6.9 | 10.1 | 2.5 | 7.1 | 3.9 | 3.2 | 0.6 | 3.1 | 0.6 | 2.4 | 1.3 | 0.6 | 1.8 |
| Average of All 16 Countries | 7.3 | 8.8 | 1.1 | 7.9 | 5.1 | 4.4 | 0.7 | 2.7 | 0.6 | 2.1 | 2.3 | 1.6 | 0.4 |
NOTE: GDP is gross domestic product.
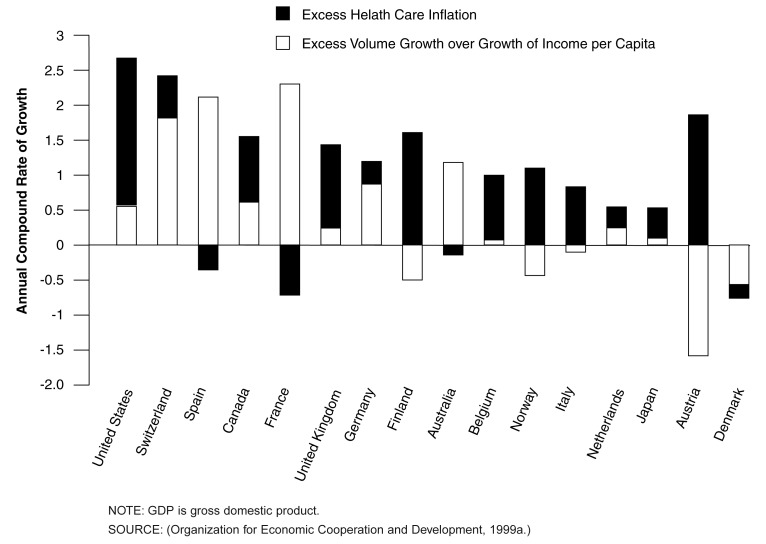
From 1980 to 1996, increases in the health care price deflator were higher than those of the GDP deflator in 12 of the 16 countries under study. The growth of the volume of real health care services per capita surpassed overall income growth in only 11 countries during the same period.
In times when health expenditures grow faster than the overall economy, one of the following conditions must hold true:
Health care prices grow faster than general GDP inflation.
The volume of health care services per capita increases faster than overall economic growth per capita (measured as real GDP per capita).
Table 5 shows the excess of health care inflation over GDP inflation and the excess growth in the volume of health care over growth in the volume of GDP per capita. These calculations show that the excess of health care inflation over the GDP deflator was the dominating factor accounting for rising health expenditure ratios in the past.
The United States not only spends a higher share of GDP on health care than all other countries under study but has also experienced the fastest divergence between the growth paths of health expenditures and GDP.
The excess volume growth of real health expenditures per capita over real GDP per capita accounts for less than 20 percent of the growth of nominal health expenditures relative to nominal GDP. In the United States, the difference between the growth rates of nominal health expenditures and nominal GDP was on average 2.7 percent per year for the period 1980-1996. Roughly 2.2 percent of this difference was due to excess health care inflation. Excess per capita volume growth was only 0.6 percent on average during this time period.
Countries are ranked in Figure 6 according to their divergence between the growth path in health expenditures and GDP. The divergence is broken down into excess health care inflation and excess health care volume growth over real income growth.
Figure 6. Decomposition of Excess Health Care Expenditure Growth Relative to GDP Growth: 1980-1996.
Trends in Health Care Financing
There are large differences in the way health care services are funded in OECD countries. Figure 7 provides a breakdown of total health spending into main sources of funding; this information was collected as part of the current revisions and amendments to OECD health accounts. The 20 countries for which comparable data are available are ranked in Figure 7 by the s ha re of public funding in total health expenditures.
Figure 7. Health Care Expenditures by Source of Funds: 1996.
Public funding is either by central (Federal), State (provincial/regional) and local government, or by social security plans. Countries with primarily government-funded (tax-based) systems are the Scandinavian countries, Ireland, New Zealand, and the United Kingdom. Public funding through social security plans is dominant in Austria, France, Germany, Japan, and Switzerland. Examples of mixed systems with predominant public funding are Belgium, Spain, Italy, and Portugal. These systems are somewhere between the prototypes of social insurance and tax-based national health services.
There were only 5 of the sample of 20 OECD countries in 1997 with a public share of health care funding of less than two-thirds of total spending: Greece, Korea, Mexico, Portugal, and the United States. Korea has the lowest public share of all OECD countries, followed closely by the United States (Table 6). A further analysis of the structure of private financing in these countries, however, reveals important differences: Private funding in the United States is mostly by private health insurance, whereas out-of-pocket payments are the most important source of private funding in Greece, Korea, and Portugal
Table 6. Public Share of Total Health Care Spending: 1970-1997.
| Country | 1970 | 1975 | 1980 | 1985 | 1990 | 1995 | 1997 |
|---|---|---|---|---|---|---|---|
| United States | 37.8 | 42.1 | 42.4 | 40.6 | 40.5 | 45.8 | 46.4 |
| Japan | 69.8 | 72.0 | 71.3 | 70.7 | 77.6 | 78.5 | 79.9 |
| Germany | 72.8 | 79.0 | 78.7 | 77.4 | 76.2 | 78.1 | 77.1 |
| France | 74.7 | 77.2 | 78.8 | 76.9 | 74.5 | 74.3 | 74.2 |
| Italy | 86.9 | 84.5 | 80.5 | 77.2 | 78.1 | 69.3 | 69.9 |
| United Kingdom | 87.0 | 91.1 | 89.4 | 85.8 | 84.1 | 84.4 | 84.6 |
| Canada | 70.2 | 76.4 | 75.6 | 75.6 | 74.6 | 71.1 | 69.8 |
| Australia | 56.7 | 72.8 | 62.9 | 71.5 | 67.3 | 67.1 | 66.7 |
| Austria | 63.0 | 69.6 | 68.8 | 76.1 | 73.5 | 73.9 | 73.0 |
| Belgium | 87.0 | 79.6 | 83.4 | 81.8 | 88.9 | 87.8 | 87.6 |
| Czech Republic | 96.6 | 96.9 | 96.8 | 92.2 | 96.2 | 92.7 | 91.7 |
| Denmark | 86.3 | 91.9 | 86.5 | 85.9 | 83.7 | 83.7 | 83.8 |
| Finland | 73.8 | 78.6 | 79.0 | 78.6 | 80.9 | 75.5 | 76.0 |
| Greece | 42.6 | — | 55.6 | — | 62.7 | 58.7 | 57.7 |
| Iceland | 81.7 | 87.2 | 88.2 | 87.0 | 86.6 | 84.1 | 83.8 |
| Ireland | 81.7 | 79.0 | 81.6 | 75.7 | 72.9 | 74.2 | 76.7 |
| Korea | 8.2 | 13.2 | 26.5 | 34.7 | 40.3 | 42.1 | 45.5 |
| Luxembourg | 88.9 | 91.8 | 92.8 | 89.2 | 93.1 | 92.4 | 91.8 |
| Mexico | — | — | — | — | 58.8 | 57.2 | 60.0 |
| Netherlands | 84.3 | 73.4 | 74.7 | 75.1 | 72.7 | 76.9 | 72.6 |
| New Zealand | 80.3 | 73.7 | 88.0 | 82.4 | 77.2 | 77.3 | |
| Norway | 91.6 | 96.2 | 85.1 | 85.8 | 83.3 | 83.3 | 82.2 |
| Portugal | 59.0 | 58.9 | 64.3 | 54.6 | 65.5 | 60.5 | 60.0 |
| Spain | 65.4 | 77.4 | 79.9 | 81.1 | 78.7 | 78.3 | 76.1 |
| Sweden | 86.0 | 90.2 | 92.5 | 90.4 | 89.9 | 83.4 | 83.3 |
| Switzerland | 63.9 | 68.9 | 67.5 | 66.1 | 68.4 | 72.3 | 69.9 |
| Turkey | 37.3 | 49.0 | 27.3 | 50.2 | 61.0 | 70.8 | 72.8 |
| European Union | 76.0 | 80.2 | 79.1 | 79.0 | 78.4 | 76.8 | 76.3 |
| OECD Europe | 75.5 | 80.0 | 77.6 | 78.3 | 78.5 | 77.7 | 77.2 |
| Total OECD | 70.5 | 74.8 | 73.8 | 74.2 | 74.5 | 73.8 | 73.7 |
NOTE:OECD is Organization for Economic Cooperation and Development.
This has important implications for health policy analysis of these countries. First, another warning on data quality is appropriate: The collection of the data in Table 6 has only recently been undertaken by the OECD Secretariat. Good estimates of out-of-pocket payments, in particular, are difficult to obtain. Greece and Korea, for example, revised their estimates substantially upward in OECD Health Data 99 (Organization for Economic Cooperation and Development, 1999b), which also lead to a marked change in their estimates of total spending. Second, the notion of the public-private mix used in the analysis presented in this article is based on the concept of direct sources of payment, attempting to ascertain who actually pays (the consumer or a third party).
It should be noted that this analysis in terms of gross financing leads to a potentially distorted picture for countries such as the United States, which has an elaborate system of tax incentives for private insurance. An alternative concept of “net social expenditure” has therefore been developed by the OECD Secretariat, which takes the redistributive effects of tax deductions into account. Empirical results show that the difference between the United States and other OECD countries in terms of net social spending is smaller than in terms of gross social spending (Adema 1999).
Shifting Public-Private Mix
Health expenditures are among the most dynamic components of private consumption in a majority of OECD countries. With growing wealth, households tend to put more health care goods into their “shopping basket,” such as new (and traditional) drugs, alternative medicine, and first class accommodations when they are inpatients (often financed by complementary insurance). Relatively wealthy pensioners add to this private health care expenditure with their out-of-pocket payments (Figure 8).
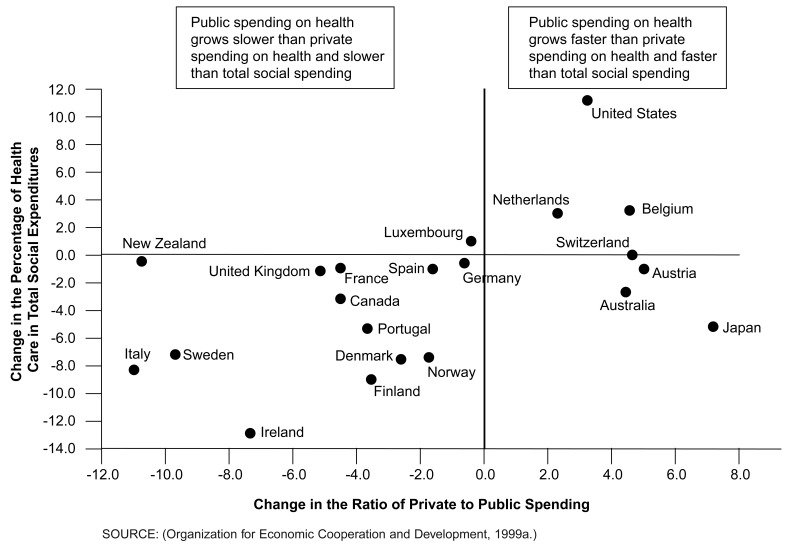
Figure 8. Public-Private Mix of Health Expenditures and the Share of Health Care in Total Social Expenditures: 1980-1995.
At the same time, public insurance plans have increased their rates of copayment and cost sharing in general. As a result, out-of-pocket payments as a share of total health care funding have increased in a majority of OECD countries for which comparable data are available (Table 7). Countries differ substantially, however, with respect to the fundamental role of and trend in out-of-pocket payments: In some countries, copayments tend to decrease relative to overall spending as countries increase the coverage of the population by public plans and other third-party-payment arrangements. Other countries with universal coverage seem to put an increasing burden of copayment on their patients, partly in an attempt to contain costs under public plans.
Table 7. Out-of-Pocket Payments as a Percent of Total Health Care Expenditures: 1980-1997.
| Country | 1980 | 1990 | 19971 |
|---|---|---|---|
|
| |||
| Percent | |||
| Austria | 16.3 | 22.4 | 25.1 |
| Canada | — | 14.2 | 16.5 |
| Denmark | 9.7 | 12.0 | 12.6 |
| Finland | 18.4 | 15.5 | 19.9 |
| Germany | 10.3 | 11.1 | 10.8 |
| Iceland | 11.8 | 13.4 | 16.2 |
| Ireland | — | 15.1 | 12.9 |
| Korea | — | 53.0 | 52.0 |
| Luxembourg | 7.2 | 5.5 | 7.0 |
| New Zealand | 12.0 | 17.6 | 23.5 |
| Portugal | — | 46.3 | 44.6 |
| Switzerland | — | 29.1 | 29.8 |
| Turkey | — | — | 31.7 |
| United Kingdom2 | 6.0 | 9.0 | 11.5 |
| United States | 24.4 | 20.7 | 17.2 |
1997 or latest year available (1995 or 1996).
Estimated.
With the available data, however, it is difficult to separate this induced private spending from other structural changes, such as increased “luxury” spending on health care. Some evidence about a possible link between cost-containment measures under public plans and the relative growth of private health care spending is provided in Figure 8. Total social spending is mainly the sum of: health care, sickness cash benefits, old age cash benefits, survivors', family, disability, housing and unemployment assistance, and active labor market policy Organization for Economic Cooperation and Development, 1999b. Figure 8 shows that there is some association between growth of private spending as part of total spending on health and the growth of public spending within total social spending. In the majority of the countries studied in Figure 8, public expenditure on health decreased as part of total social spending, while at the same time, a growing part of health care was paid for by private sources (mainly out-of-pocket payment and private insurance).
Trends in Service Delivery and Spending
Health care reforms in many OECD countries over a decade or more have resulted in shifts both in the public-private mix of financing and in the division of labor among levels of care (primary, secondary, tertiary). Table 8 provides an overview of transformation in health sectors in OECD countries.
Table 8. Percent of Health Care Spending by Sector: 1980-1997.
| Country | Inpatient Care | Outpatient Care | Pharmaceuticals | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| 1980 | 1997 | 1980 | 1997 | 1980 | 1997 | |
|
| ||||||
| Percent | ||||||
| United States | 48.7 | 41.5 | 27.2 | 33.2 | 8.7 | 10.0 |
| Japan | 30.9 | 30.4 | 44.6 | 42.1 | 21.2 | 21.2 |
| Germany | 33.2 | 34.1 | 34.3 | 33.8 | 13.4 | 12.3 |
| France | 48.2 | 44.9 | 25.2 | 27.6 | 15.9 | 17.2 |
| Italy | 46.7 | 49.4 | 27.5 | 30.6 | 13.7 | 19.4 |
| United Kingdom | 53.5 | 42.2 | — | — | 12.8 | 15.9 |
| Canada | 53.4 | 43.6 | 24.8 | 26.4 | 8.4 | 13.7 |
| Australia | 52.9 | 43.9 | 22.3 | 27.2 | 7.9 | 11.6 |
| Austria | 18.8 | 20.7 | 19.3 | 25.6 | 10.9 | 14.0 |
| Belgium | 33.1 | 39.4 | 39.2 | 38.7 | 17.4 | 18.4 |
| Czech Republic | — | 35.6 | — | 29.8 | — | 25.3 |
| Denmark | 60.5 | 67.6 | 21.0 | 18.6 | 6.4 | 8.7 |
| Finland | 48.4 | 41.2 | 39.9 | 48.7 | 10.7 | 14.9 |
| Greece | 26.5 | 26.7 | 24.6 | — | 18.8 | 21.4 |
| Iceland | 59.1 | 55.0 | 16.9 | 23.0 | 15.9 | 16.0 |
| Ireland | 58.8 | — | — | — | 10.9 | 10.6 |
| Korea | — | 24.4 | — | 42.2 | — | — |
| Luxembourg | 31.3 | 32.9 | 49.5 | 50.8 | 14.5 | 11.7 |
| Netherlands | 57.3 | 52.6 | 27.7 | 28.1 | 7.9 | 10.9 |
| New Zealand | 72.2 | 56.5 | 8.4 | 7.1 | 13.0 | 15.4 |
| Norway | 63.9 | 61.6 | 18.4 | 20.8 | 8.7 | 7.2 |
| Portugal | 28.7 | 36.2 | — | — | 19.9 | 25.2 |
| Spain | 54.1 | 46.9 | 12.6 | 11.9 | 21.0 | 18.6 |
| Sweden | — | — | — | — | 6.5 | 12.7 |
| Switzerland | 42.6 | 50.7 | 45.5 | 39.1 | 15.2 | 7.7 |
| European Union Average | 42.8 | 41.8 | 30.5 | 32.1 | 14.0 | 15.1 |
| OECD Average | 46.5 | 42.5 | 27.8 | 30.3 | 13.0 | 15.0 |
NOTES:OECD is Organization for Economic Cooperation and Development. Data not available for Hungary, Mexico, Poland, and Turkey. The 1997 data represent the latest year available (Norway, 1990;New Zealand, 1992;Spain, 1993;Greece, 1994; Portugal, Switzerland, and United Kingdom, 1995; Australia, Austria, Germany, Ireland, Japan, and Luxembourg, 1996). Total expenditure on health includes public and private spending. Only major sectors are shown, thus percentages do not add to 100.OECD and European Union averages include countries where data are available for selected years.
Since 1980, there has been a shift toward primary care and away from specialist care in Australia, Austria, Finland, France, Iceland, the Netherlands, and the United States. This reflects, in part, cost-containment efforts: There is evidence that overall health care spending is lower when the ratio of primary care spending to total spending is higher (Organization for Economic Cooperation and Development, 1995).
In the United States, the proportion of total health care spending devoted to inpatient car e declined by 7.2 percentage points between 1980 and 1997, while the proportion of resources channeled to outpatient care increased by 5 percentage points. This is likely to have been, in part, a result of the shift toward managed care. The proportion of total spending devoted to pharmaceuticals has increased in most OECD countries over the same period. However, although the United States has high absolute pharmaceutical spending per capita, it continues to allocate one of the smallest proportions of total health care spending to pharmaceuticals (10 percent in 1997).
It is difficult to assess from the available international data sets to what degree the emerging consensus of the public health movement has resulted in a shift of resources toward a relative increase in spending on preventive services. This is certainly an area of international health statistics where more work is needed.
Other questions that are difficult to answer include: Do costs of public health administration and private health insurance increase faster than personal health care services and medical goods? Are administrative costs in the United States higher relative to other countries? Is there a tendency toward ever-increasing shares of administrative costs? The evidence from the available data in OECD Health Data 99 (Organization for Economic Cooperation and Development, 1999b) is inconclusive at the moment.
There seems to be, however, some evidence that expenditures on health research and development grow faster than personal services, in particular research and development of the pharmaceutical industry. There remain at the same time open questions about the statistics and health-policy reasons for a smaller reported share of investment into health care facilities in many OECD countries in the 1990s compared with the 1970s.
Revisions of Health Expenditure Estimates
Those working on international comparisons of health expenditure estimates continue to wrestle with four main obstacles to international comparability:
Differences in the way the boundaries are drawn in countries between health care and other social care, in particular regarding care for the disabled and for frail elderly persons.
Information gaps in and underestimation of private expenditure on health.
Lack of international standards for the functional and industrial classification of health expenditures in health accounts.
Lack of standardization in health accounting methodology with national accounting methodology, which provides the universally accepted toolbox for classifying other economic statistics.
These obstacles are generally recognized by those working on international comparisons. However, progress in raising standards has been rather slow over the years because of the limited resources invested in this difficult area both in many countries and by international initiatives.
The evolution of the OECD health accounts has resulted in improved and better harmonized data over the last 3 years. A list of examples follows:
OECD estimates for Denmark and Sweden have been revised at the boundary between health and social care.
Greece and Korea have revised their estimates of private health expenditures;
Canada has recently revisited the public-private mix in health care (Canadian Institute for Health Information, 1999).
Germany and France are currently adding more detail to the functional breakdown in health accounts.
Other countries have strengthened the links between their national health accounts (NHA) and other economic and social statistics (e.g., Austria and the United States) or have projects underway for doing so (e.g., Australia and the United Kingdom).
Many more countries are currently revisiting their NHA, considering health accounts, or starting to design a NHA project (notably the Czech Republic, Hungary, and Poland).
Revisions to OECD Health Accounts Methodology
The OECD (1993) health accounts have gradually become an informal quasi-standard for uniform reporting on health care systems. Over the years, gradual harmonization of concepts and definitions has gone hand in hand with the annual data collection by the OECD Secretariat of health and health care statistics.
At the request of its member countries, the OECD Secretariat drafted a report entitled, A System of Health Accounts for International Data Collection (to be published) to assist researchers and statisticians with more detailed guidelines on health accounting. The primary aim of this manual is to provide a common framework for enhancing the comparability of health care data across countries.
The manual establishes a conceptual basis of statistical reporting rules and proposes a newly developed International Classification for Health Accounts, which covers three basic dimensions: the functions of health care, the providers of health care services, and the sources of funding. Selected definitions are presented for integrating non-monetary resource statistics into the manual, such as data on health care personnel.
The manual is currently being tested with OECD member countries. Many non-member countries and several international organizations have also welcomed it. The synergy from numerous health accounting initiatives currently underway in many regions of the world should lead to a better understanding of the economics of health care delivery and its financing. In addition, it is hoped that this process will receive the commitment of policymakers and health planners to make the necessary statistical resources available on a continuing basis.
Conclusions
Two sets of conclusions may be drawn from this article. First, some interesting and important trends in health spending are revealed by the latest OECD health data. For example, the recent stabilization of the U.S. health expenditure share of GDP is paralleled by a similar stabilization in the average share for 25 OECD countries. Nevertheless, per capita health spending in the United States has remained at least twice that of the nearest OECD country. A breakdown of health expenditure growth into price and volume effects suggests that, in the United States, excess inflation from 1980 to 1996 was about four times the rate of volume growth, whereas in the OECD as a whole it was five times the excess volume growth. That may raise fresh questions about the efficiency of health care spending across OECD.
Second, more comparable information on the detailed structure of private funding, especially estimates of the net cost-sharing and of the net financial burden of private funding for health, is needed to take into account the complex structure of copayment regulations and tax deductions in force in many countries.
Despite steady improvements in the health data available across OECD countries, major improvements in coverage and comparability of the key indicators are still needed. For example, greater harmonization of the boundaries of total heath expenditures would be required. This means that more investment in health accounting by individual countries as well as by regional and international organizations is required.
Acknowledgments
The assistance of Jeremy Hurst in drafting this article is gratefully acknowledged.
Footnotes
Manfred Huber is with the Health Policy Unit, Organization for Economic Cooperation and Development (OECD). The research presented in this article was performed at OECD and was supported by the Health Care Financing Administration (HCFA) under Contract Number 500-95-0001. The views expressed in this article reflect those of the author and do not necessarily reflect the views of OECD or HCFA.
Reprint Requests: Manfred Huber, OECD Health Policy Unit, 2 rue André Pascal, 75775 Paris Cedex 16. E-mail: manfred.huber@oecd.org
References
- Adema W. Labour Market and Social Policy Occasional Papers No 39. Paris: Organization for Economic Cooperation and Development; 1999. Net Social Public Expenditure. [Google Scholar]
- Anderson G, Poullier JP. Health Spending, Access, and Outcomes: Trends in Industrialized Countries. Health Affairs. 1999;18(3):178–192. doi: 10.1377/hlthaff.18.3.178. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information. The Evolution of Public and Private Health Care Spending in Canada, 1960-1997. Ontario: 1999. [Google Scholar]
- Evans RG. Going for Gold: The Redistributive Agenda Behind Market-Based Health Care Reform. In: Chinitz D, Cohen J, editors. Governments and Health Systems: Implications of Difering Involvement. John Wiley & Sons; Chichester: 1998. [Google Scholar]
- Gerdtham UG, Jönsson B. Price and Quantity in International Comparisons of Health Care Expenditure. Applied Economics. 1991;23:1519–1528. doi: 10.1016/0167-6296(91)90005-8. [DOI] [PubMed] [Google Scholar]
- Organization for Economic Cooperation and Development. OECD Health Systems, Facts and Trends, 1960-1991. No.3. I and II. Paris: 1993. Health Policy Studies. [Google Scholar]
- Organization for Economic Cooperation and Development. New Directions in Health Care Policy. No.7. Paris: 1995. Health Policy Studies. [Google Scholar]
- Organization for Economic Cooperation and Development. CD-ROM and User's Guide. Paris: 1999a. OECD Health Data 99. [Google Scholar]
- Organization for Economic Cooperation and Development. OECD Statistics Show Improving Health Trends, Stable Health Expenditure Shares of GDP. OECD Press Release; Paris: Jul 26, 1999b. [Google Scholar]
- Organization for Economic Cooperation and Development. Social Expenditure Database, 1980-1996. Paris: 1999c. [Google Scholar]
- Organization for Economic Cooperation and Development. OECD Health Data 99. 1999d Dec 10; Internet address: http://www.oecd.org/els/health/sources/oecd0062.htm.
- Organization for Economic Cooperation and Development. A System of Health Accounts for International Data Collection. No.9. OECD Health Policy Studies; Paris: To be published. [Google Scholar]
- Schieber G, Poullier JP. Over view of International Comparisons of Health Care Expenditures. Health Care Financing Review. 1989;(1989 Annual Supplement):1–7. [PMC free article] [PubMed] [Google Scholar]
- Schieber G, Poullier JP, Greenwald L. U.S. Health Expenditure Performance: An International Comparison and Data Update. Health Care Financing Review. 1992;13(4):1–87. [PMC free article] [PubMed] [Google Scholar]
- Schieber G, Poullier JP, Greenwald L. Health System Performance in OECD Countries, 1980-1992. Health Affairs. 1994;13(3):100–112. doi: 10.1377/hlthaff.13.4.100. [DOI] [PubMed] [Google Scholar]