Abstract
Objective
Medical school curricula intended to promote empathy varies widely. Even the most effective curricula leave a significant group of students untouched. Pre-existing student factors influence their response to learning experiences. We examined the individual predictors of first semester medical students’ attitudes toward the value of physician empathy in clinical encounters.
Methods
First year students (n = 4732) attending a stratified random sample of 49 US medical schools completed an online questionnaire that included measures of dispositional characteristics, attitudes and beliefs, self-concept and well-being.
Results
Discomfort with uncertainty, close-mindedness, dispositional empathy, elitism, medical authoritarianism, egalitarianism, self-concept and well-being all independently predicted first year medical students’ attitudes toward the benefit of physician empathy in clinical encounters.
Conclusion
Students vary on their attitude toward the value of physician empathy when they start medical school. The individual factors that predict their attitudes toward empathy may also influence their response to curricula promoting empathic care.
Practice implications
Curricula in medical school promoting empathic care may be more universally effective if students’ preexisting attitudes are taken into account. Messages about the importance of physician empathy may need to be framed in ways that are consistent with the beliefs and prior world-views of medical students.
Keywords: Medical education, Empathy, Patient-centered care, Medical students
1. Introduction
There is a substantial body of empirical evidence that physician empathy improves interpersonal and technical quality of care, clinical outcomes and patient satisfaction [1–13]. In addition, interpersonal empathy can reduce racial bias and thus may protect against disparities in care [14–16]. These findings provide support for teaching medical student empathy as a valid part of medical school curricula. However, there is no consensus and little evidence regarding the most effective method of teaching empathy. Two systematic reviews of curricula aimed at promoting empathy in medical students found a wide range of approaches to both defining and teaching empathy [17,18]. While both reviews concluded that it is possible to maintain and/or increase empathy during medical school, examination of the studies reviewed revealed that within each sample of students, despite an increase in average combined scores, there was considerable variation in the degree to which empathy levels changed [17,18]. These studies suggest that even interventions with statistically significant main effects leave significant numbers of medical students untouched. Similarly, an intervention with resident physicians that was enthusiastically endorsed by the New York Times as an example of effective empathy training [19] influenced female participants but had no effect on the primary outcome among male participants [20].
The fact that even the most successful interventions are not benefitting some subgroups suggests that a one-size-fits-all approach to increasing medical student empathy may not be sufficient. There has been little investigation into why some students benefit from empathy promoting curricula while others do not. Educational research shows that prior attitudes and knowledge have a strong effect on current learning [21]. Thus, it is possible that pre-existing student characteristics affect the way they responded to curricula. There is evidence that learners may be alienated from the curricula or distort presented material if their prior knowledge or attitudes are at odds with curricula [21–24]. Individual dispositions may also influence responses to new information and perspectives [21,25–29]. Thus, improving our understanding of the incoming medical student characteristics that predict attitudes toward the value of physician empathy in clinical encounters may be a first step in understanding differences in students’ response to curricula during medical school. It may also provide insight into ways to design curricula that take individual differences into account and thus have a broader impact on medical students’ attitudes toward, and skills at, providing empathic care.
The purpose of this study was to examine whether student dispositional factors, sociopolitical attitudes, self-concept, and well-being predicted incoming first semester medical students’ (n = 4732), attitudes toward physician empathy, independent of socio-demographic factors. Predictors were chosen because they have been shown to be associated with physician and trainees attitudes toward and provision of empathy and patient-centered care in prior studies [25,30–41].
2. Methods
2.1. Sample
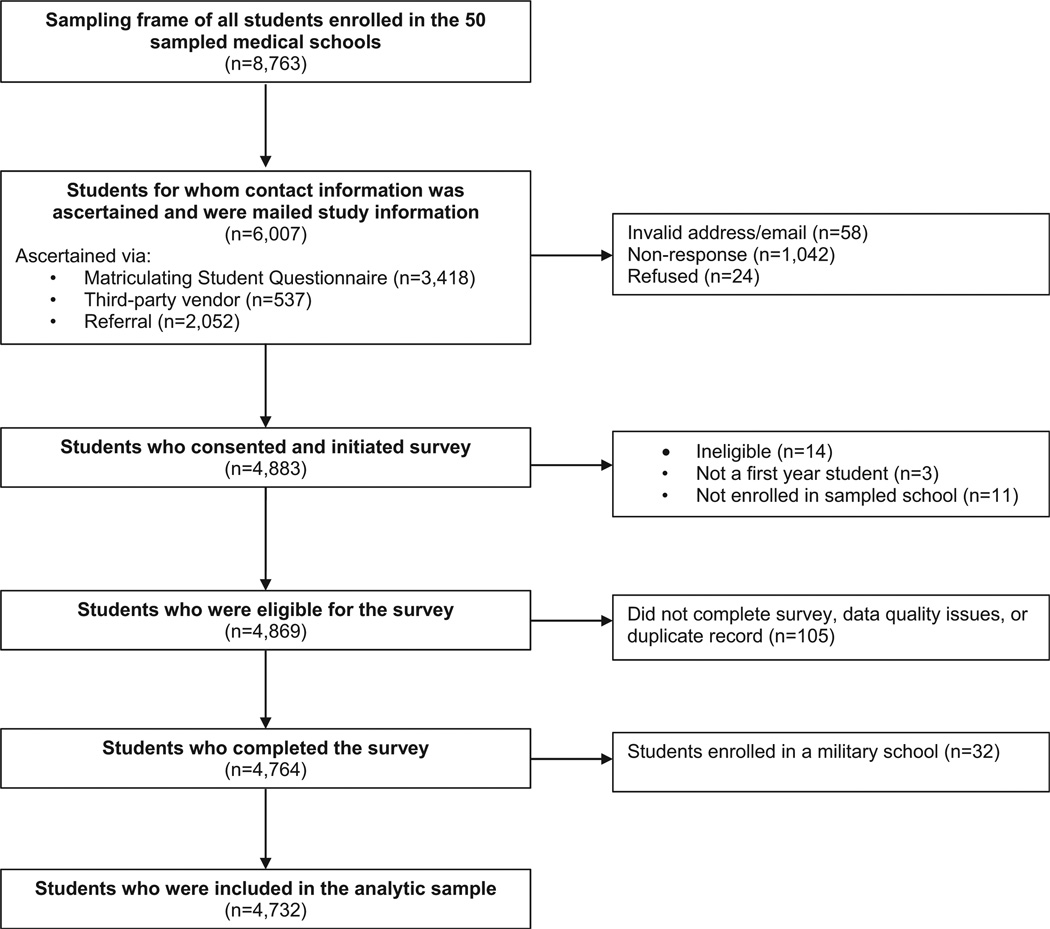
This study uses baseline data collected as part of Medical Student Cognitive Habits and Growth Evaluation Study (CHANGES), a national longitudinal study of medical students who matriculated in US medical schools in the fall of 2010. CHANGES was designed to examine changes in medical students’ well-being, experiences and attitudes between their first year of medical school (baseline) and the end of their last year of medical school. This research study was approved by the Institutional Review Boards of Mayo Clinic, the University of Minnesota, and Yale University. We randomly selected 50 medical schools from strata of public/private schools and 12 regions of the country using a sample proportional to strata size methodology. One sampled school had highly unique characteristics (military school) that would have limited the generalizability of our study findings and was excluded, leaving a sample of 49 schools. Since there are no accurate and comprehensive lists of first-year medical students (MS1) available early-mid fall of their first year, we used several methods to ascertain as many of the 8594 MS1 attending the 49 schools as possible (see Fig. 1).
Fig. 1.
Medical student CHANGES study participant recruitment flowchart.
We ascertained and invited 6007 students (68% of all MS1 attending sampled schools) to participate in the web-based survey. We achieved an 81% response rate (55% of the entire pool of MS1), which is comparable to other published studies of medical students [42]. The sample had similar gender and race distributions to the population of all MS1 in study schools. Sample characteristics and characteristics of medical students in 2010, are shown in Table 1.
Table 1.
Personal characteristics and comparison of respondents of medical student CHANGES survey, matriculating student questionnaire, and AAMC all matriculates.a
| Medical student CHANGES survey (n = 4732) 49 schools N (%) |
Matriculating student questionnaire 2010 (n= 14,638) 131 schools N (%) |
AAMC All matriculants 2010 (n=18,665) 131 schools N (%) |
|
|---|---|---|---|
| Gender | |||
| Male | 2371 (50.1) | 7597 (51.9) | 9911 (53.1) |
| Race | |||
| Black | 303 (6.4) | 995 (6.8) | 1325 (7.1) |
| Alaska Native, American Indian, Pacific Islander | 114 (2.4) | 278 (1.9) | 168 (.9) |
| Asian | 1159 (24.5) | 3513 (24.0) | 4162 (22.3) |
| White | 3237 (68.4) | 10,349 (70.7) | 12,058 (64.6) |
| Unknown/other | 95 (2.0) | 468 (3.2) | 1419 (7.6) |
| Ethnicity | |||
| Hispanic/Latino | 289 (6.1) | 1186 (8.1) | 1531 (8.2) |
Race totals and percentages do not total 100, as students were allowed to choose multiple race categories.
2.2. Data collection and integrity
Students identified as MS1 in any of the sampled schools were sent an email or letter with a link to the informed consent page. Those who consented were linked to an online questionnaire that they advanced through by answering questions placed on consecutive screens (pages). All students completed the survey during the first semester of their first year of medical school. Time spent on each page and total time to completion was recorded. If participants attempted to move to the next page with an unanswered question on the current screen, a warning popped up and they were directed back to the unanswered question. If they chose not to answer that question, they had to click on a button to indicate their desire to skip the question. This protected participants’ right to skip questions while eliminating any timesaving incentives for doing so. All students completed the survey during the first semester of their first year of medical school. After completing the measures, participants were direct to a different secure server where they provided their name and address to receive a $50.00 cash incentive. This allowed us to identify and eliminate duplicates. It also allowed us to confirm that our snowball-sampled respondents were MS1 at the school they identified. Last, responses were examined for indications of systematic response bias (e.g. clicking the same response option to move rapidly through the questionnaire). Invalid or incomplete questionnaires were omitted (n = 32) so that the final analytic sample included 4732 respondents.
2.3. Measures
2.3.1. Dependent variable
Medical students’ attitude toward physician empathy in clinical encounters was assessed using the Jefferson Empathy Scale Student Version [43–45]. While this measure has been simply referred to as “empathy” in some prior studies, it measures attitudes toward the value of physician empathy in clinical encounters. In this measure, medical students were asked to rate their agreement on a 7-point scale from 1 (“strongly disagree”) to 7 (“strongly agree”) to statements such as “A physician who is able to view things from another person’s perspective can render better care” and “Empathy is an important therapeutic factor in medical treatment” (Cronbach’s alpha .88).
2.3.2. Independent variables
2.3.2.1. Socio-demographic factors
Student gender and race and ethnicity were measured using standard socio-demographic questions. Medical student socio-economic status (SES) is difficult to characterize because they have left their family of origin and are adults yet are still in the student role. Their parents’ income may or may not be available to them and their responses on questions about current income are difficult to interpret. Accordingly, we used two measures to assess SES. To obtain an estimate of SES of family of origin, we used student-reported parental highest educational attainment. Examination of the data revealed that there were meaningful differences between students’ whose parents’ highest educational level was high school or less vs. education beyond high school. As our second estimate, we used student self-report on student loan debt accumulated during undergraduate education. We created two categories for this variable – whether they had no student loan debt vs. any student loan debt, again on the basis of empirical observation of meaningful difference. Whether or not students had an undergraduate degree in the field of science, technology, engineering, mathematics (STEM) was assessed by asking students to “Please indicate the major field of study for your undergraduate degree. Select all that apply”. We categorized the following majors as STEM: biological sciences/life sciences; computer and information sciences; engineering; mathematics; physical sciences/technologies. All other majors were put in a single category. The majority of majors in this second category were in the social sciences and humanities.
2.3.2.2. Individual disposition
Dispositional empathy was measured using the Empathic Concern subscale of the Interpersonal Reactivity Index [46]. This scale assesses the tendency to experience feelings of sympathy and compassion for others [46]. Participants responded to statements on a 7-point Likert-type scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”) to statements such as “I often have tender, concerned feelings for people less fortunate than me” (Cronbach’s alpha .82).
Dispositional perspective taking was measured using the Cognitive Empathy subscale of the Interpersonal Reactivity Index [46]. Participants responded to statements on a 7-point Likert-type scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”) to statements such as “Before criticizing somebody, I try to imagine how I would feel if I were in their place” (Cronbach’s alpha .83).
Discomfort with uncertainty was assessed with the 3-item Discomfort with Ambiguity subscale of the Need for Closure scale [47]. Participants responded to statements on a 7-point Likert-type scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”) to statements such as “I don’t like situations that are uncertain” (Cronbach’s alpha .63).
Close-mindedness was assessed with the 7-item Close-mindedness subscale of the Need for Closure scale [47]. Participants responded on a 7-point Likert-type scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”) to statements such as: “Even after I have made up my mind about something, I am always eager to consider a different option”(reverse scored). (Cronbach’s alpha .65).
2.3.2.3. Sociopolitical attitudes
Egalitarianism and Elitism were both measured using sub-scales of the Social Dominance Orientation scale (SDO) [48] which measures egalitarian and social justice beliefs. The egalitarianism scale includes items such as “We should do what we can to equalize conditions for different groups” and the Elitism scale includes items such as “If certain groups of people stayed in their place, we would have fewer problems” (Cronbach’s alpha = 0.80 and 89, respectively).
Medical authoritarianism was assessed using The Medical Authoritarianism Scale [49]. Participants responded on a 7-point Likert-type scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”) to statements such as: “Conscientious patients deserve better health care than those with self-inflicted problems” and “Those who contribute the most to society should get better health care” (Cronbach’s alpha .88).
2.3.2.4. Self-concept
Locus of Control was measured using the Locus of Control subscale of Pearlin’s Mastery Scale [50]. The locus of control subscale assesses respondents sense of control over events in their life. Students responded to a 7-item self-report measure ranging from 1 (“strongly disagree”) to 7 (“strongly agree”). Sample items included “I have little control over the things that happen to me” and “What happens to me in the future mostly depends on me.”(Cronbach’s alpha .82).
Self-esteem was assessed using the Rosenberg Self Esteem Scale [51]. Participants responded on a 7-point Likert-type scale ranging from 1 (“strongly disagree”) to 7 (“strongly agree”). Sample questions included “I am able to do things as well as most other people” and “I feel I do not have much to be proud of” (Cronbach’s alpha .79).
2.3.2.5. Well-being
Fatigue, anxiety and depression symptoms were assessed using the extensively validated Patient-Reported Outcome Measurement Information System (PROMIS) short form scales [52,53]. The response options for the PROMIS scales ranged from 1 (never) to 5 (Very Often). (Cronbach’s alphas .88, .92 and .94 respectively).
2.4. Analyses
We examined the distribution of all independent and dependent variables. We then examined the bivariate relationship between independent (predictor) variables and the dependent variable, using the SPSS Complex Samples ANOVA for categorical independent variables and linear regression for continuous independent variables. For variables with significant bivariate relationships, we constructed models in which the sets of independent variables were entered into a general linear model in consecutive blocks in the following order: socio-demographic factors, individual disposition, sociopolitical attitudes, self-concept, and well-being. The dependent variable had a modest (.15) but statistically significant association with the 7-item Marlowe–Crowne Social Desirability Scale [54]. Thus, this measure of social desirability bias was included in all multivariable analyses. Variables that were non-significant in each block were dropped when successive blocks were entered into the model. We used the SPSS Complex Samples procedure to take into account the sampling probability, stratification, and clustering in the two-stage design of the CHANGES survey. We obtained 95% confidence intervals and p-values for the model-estimated associations between each outcome and the independent variable. Statistical significance threshold was set a priori at alpha equal to 0.05.
Due to the skewed nature of the dependent variable, we also repeated the analyses using a recoded dependent variable (dichotomized into high and low scores using the median as a cut-point) and repeated the analyses using logistic regression. There were no differences in the patterns of results so the linear regression results are presented here.
3. Results
Table 2 presents the overall distribution of responses on the dependent variables and psychosocial predictors. Table 3 shows the bivariate relationship between the socio-demograph-ic and psychosocial predictor variables and student attitude toward physician empathy in patient encounters. Unadjusted analyses of women and Black students depicted a more positive attitude toward physician empathy than men and white students respectively. We also found that South Asian students had less positive attitudes toward physician empathy than their white counterparts. Lower SES students had more positive attitudes toward physician empathy than their higher SES counterparts. Older age was positively associated with attitudes toward physician empathy. Students who had a STEM undergraduate major had less positive attitudes than those with non-STEM undergraduate majors. Individual disposition, sociopolitical attitudes, self-concept and well-being measures were all associated with attitudes toward physician empathy in clinical encounters at statistically significant levels, with close-mindedness, dispositional empathy and dispositional perspective-taking – having the strongest unadjusted association.
Table 2.
Univariate distribution of dependent variable and psychosocial predictors.
| Mean (s.d.) | Range | N | |
|---|---|---|---|
| Dependent variable | |||
| Attitude toward physician empathy in clinical encounter | 6.32 (0.63) | 1–7 | 4676 |
| Independent variables: psychosocial predictors | |||
| Individual disposition | |||
| Dispositional empathy | 4.81 (0.91) | 1–7 | 4607 |
| Dispositional perspective-taking | 5.27(0.92) | 1–7 | 4608 |
| Discomfort with uncertainty | 4.81 (1.05) | 1–7 | 4622 |
| Close-mindedness | 2.99(0.74) | 1–7 | 4629 |
| Sociopolitical attitudes | |||
| Egalitarianism | 5.12(1.32) | 1–7 | 4631 |
| Elitism | 1.76(1.07) | 1–7 | 4634 |
| Medical authoritarianism | 2.50(1.34) | 1–7 | 4660 |
| Self-concept | |||
| Locus of control | 5.64 (0.93) | 1–7 | 4676 |
| Self-esteem | 5.67(1.06) | 1–7 | 4675 |
| Well-being | |||
| Fatigue | 4.00(0.77) | 1–5 | 4732 |
| Anxiety | 4.00 (0.83) | 1–5 | 4732 |
| Depression | 4.00 (0.83) | 1–5 | 4732 |
Table 3.
Bivariate relationships between predictors and attitudes toward physician empathy in clinical encounters (linear relationships adjusted for complex samples).
| Mean score on DV |
(SE) | Sig | |
|---|---|---|---|
| Gender | .00 | ||
| Men | 6.22 | 0.016 | |
| Women | 6.43 | 0.009 | |
| Race/ethnicity | .00 | ||
| White | 6.33 | 0.012 | ref |
| Black (vs. white) | 6.41 | 0.036 | .05 |
| Hispanic (vs. white) | 6.36 | 0.029 | ns |
| East Asian (vs. white) | 6.31 | 0.019 | ns |
| South Asian (vs. white) | 6.24 | 0.026 | .00 |
| Other race/ethnicity (vs. white) | 6.37 | 0.058 | ns |
| Highest parental degree | .00 | ||
| Parent has post-high school education (vs. high school or less) | 6.32 | 0.01 | |
| High school or less | 6.4 | 0.02 | |
| Undergrad major | .00 | ||
| Did not have undergrad STEM major (vs STEM major) | 6.38 | 0.012 | |
| STEM major | 6.3 | 0.011 | |
| Undergrad student loan debt | .00 | ||
| No Debt | 6.31 | 0.011 | |
| Has Undergrad Student Loan Dept | 6.34 | 0.013 | |
| Bivariate association |
|||
| 95% C.I. | Sig. | ||
| Age | 0.014 | 0.009, 0.019 | .00 |
| Discomfort with uncertainty | −0.021 | −0.006, −0.037 | .00 |
| Close-mindedness | −0.25 | −0.28, −0.23 | .00 |
| Dispositional empathy/empathic concern | 0.28 | 0.26, 0.31 | .00 |
| Dispositional perspective-taking | 0.24 | 0.21, 0.26 | .00 |
| Medical authoritarianism | −0.13 | −0.14, −0.11 | .00 |
| Elitism (SDO) | 0.16 | 0.18, −0.17 | .00 |
| Egalitarianism (SDO) | −0.14 | 0.13, 0.16 | .00 |
| Locus of control | 0.062 | 0.045, 0.08 | .00 |
| Global self-esteem | 0.089 | 0.072, 0.11 | .00 |
| Fatigue | .033 | 0.013, 0.053 | .00 |
| Anxiety | .022 | 0.004, 0.041 | .02 |
| Depression | −.036 | −0.058, −0.015 | .00 |
The results of multivariate analyses are presented in Table 4. There are 5 models presented. Categories of variables were entered in successive blocks to show the impact on each set of predictors when other predictors were entered into the model. Block one examined the impact of socio-demographic factors independent of each other. When all socio-demographic predictors were entered into the model, Black race became non-significant, as did SES (student loan debt). All other socio-demographic factors that were significant in the bivariate analysis remained statistically significant predictors. When individual disposition variables were entered into the model the effects of age and SES (parents’ highest degree) became non-significant. Negative predictors included discomfort with uncertainty (b = −.04; p<.001) and close-mindedness (b = −.11; p < .001) while the tendency to respond to others with empathic concern (b = .20; p < .001) and perspective-taking (b = .09; p < .001) were positive predictors of attitudes toward physician empathy in patient encounters. Model 3 shows that sociopolitical attitudes predicted attitudes toward physician empathy in the encounter independent of other variables. Students higher on medical authoritarianism (b = −.04; p < .001) and SDO elitism (b = −.03; p = .001) had more negative attitudes toward patient empathy and those higher in egalitarianism had (b = .04; p < .001) more positive attitudes toward physician empathy in encounters.
Table 4.
Predictors of attitude toward physician empathy in patient encounters.
| Model 1: Socio-demographic |
Model 2:Added individual disposition |
Model 3: Added socio-political attitudes |
Model 4: Added self-concept |
Model 5: Added well-being |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Predictor | b | 95% confidence interval (lower, upper) |
Sig. | b | 95% confidence interval (lower, upper) |
Sig. | b | 95% confidence interval (lower, upper) |
Sig. | b | 95% confidence interval (lower, upper) |
Sig. | b | 95% confidence interval (lower, upper) |
Sig. |
| Intercept | 6.18 | (6.04, 6.32) | .00 | 4.93 | (4.72, 5.15) | .00 | 5.06 | (4.88, 5.23) | .00 | 4.60 | (4.37, 4.82) | .00 | 4.41 | (4.17, 4.66) | .00 |
| Men | −.21 | (−.25, −.18) | .00 | −.10 | (−.12, −.07) | .00 | −.06 | (−.09, −.03) | .00 | −.07 | (−.10, −.04) | .00 | −.06 | (−.09, −.03) | .00 |
| Black (vs. white) | .03 | (−.03, .08) | NS | ||||||||||||
| Hispanic (vs. white) | .02 | (−.05, .08) | NS | ||||||||||||
| East Asian (vs. white) | −.01 | (−.06, .03) | NS | ||||||||||||
| S. Asian (vs. white) | −.08 | (−.14, −.02) | .01 | −.11 | (−.16, −.05) | .00 | −.11 | (−.16, −.07) | .00 | −.10 | (−.15, −.05) | .00 | −.10 | (−.15, −.05) | .00 |
| Other race/ethnicity (vs. white) | .06 | (−.06, .18) | NS | ||||||||||||
| Age | .01 | (.01, .02) | .00 | .00 | (.00, .01) | NS | |||||||||
| Parent education> high school | −.08 | (−.14, −.02) | .01 | −.04 | (−.10, .02) | NS | |||||||||
| NOT STEM major | .05 | (.02, .07) | .00 | .05 | (.02, .07) | .00 | .04 | (.02, .06) | .00 | .05 | (.02, .07) | .00 | .04 | (.02, .07) | .00 |
| Has loan debt | −.01 | (−.04, .02) | NS | ||||||||||||
| Discomfort with uncertainty | −.04 | (−.02, −.05) | .00 | −.04 | (−.03, −.06) | .00 | −.05 | (−.03, −.06) | .00 | −.04 | (−.03, −.06) | −.00 | |||
| Close-mindedness | −.11 | (−.13, −.08) | .00 | −.09 | (−.12,−.07) | .00 | −.08 | (−.11,−.06) | .00 | −.08 | (−.11, −.06) | .00 | |||
| Dispositional empathy/concern | .20 | (.18, .22) | .00 | .16 | (.14, .18) | .00 | .15 | (.13, .17) | .00 | .15 | (.13, .17) | .00 | |||
| Dispositional perspective-taking | .09 | (.07, .11) | .00 | .08 | (.06, .10) | .00 | .08 | (.06, .10) | .00 | .07 | (.05, .09) | .00 | |||
| Medical authoritarianism | −.04 | (−.05, −.02) | .00 | −.03 | (−.05, −.02) | .00 | −.03 | (−.05, −.02) | .00 | ||||||
| Elitism (SDO) | −.03 | (−.05, −.01) | .00 | −.03 | (−.05,−.01) | .00 | −.03 | (−.05, −.01) | .00 | ||||||
| Egalitarianism (SDO) | .04 | (.03, .06) | .00 | .04 | (.03, .05) | .00 | .04 | (.03, .06) | .00 | ||||||
| Locus of control | .01 | (.00, .03) | .07 | .03 | (.01, .04) | .00 | |||||||||
| Global self-esteem | .07 | (.05, .09) | .00 | .07 | (.05, .09) | .00 | |||||||||
| Fatigue symptoms | .03 | (.00, .05) | .03 | ||||||||||||
| Anxiety symptoms | .04 | (.02, .06) | .00 | ||||||||||||
| Depression symptoms | −.01 | (−.03, .01) | NS | ||||||||||||
Model 4 estimated the additional impact of self-concept. In that model only global self-esteem was significant (b = .07; p < .001). Other variables remained significant, but the direction of the relationship on discomfort with uncertainty changed. In Model 5, both global self-esteem and locus of control were significant and positive predictors. Higher levels of fatigue and anxiety symptoms were both associated with more positive attitudes toward physician empathy, but the relationship between depression symptoms and attitudes toward physician empathy was not statistically significant in the multivariate model. Given that fatigue, anxiety and depression symptoms were highly correlated in this sample; we also examined the impact of depression symptoms with anxiety and fatigue removed from the model. Depression symptoms remained non-statistically significant. Among significant predictors in Model 5, the strongest positive psychosocial factors were empathetic concern (b = .15; p < .001), perspective-taking (b = .07; p<.001), and global self-esteem (b = .07; p < .001). The strongest negative factors included three socio-demographic factors and one psychosocial factor: South Asian race relative to white race (b = −.10; p < .001), close-mindedness (b = −.08; p < .001), and male gender (b = −.06; p < .001).
4. Discussion and conclusion
4.1. Discussion
Individual disposition, sociopolitical attitudes, self-concept and well-being all independently predicted first year medical students’ attitudes toward the benefit of physician empathy in clinical encounters. The relationship between these individual factors and attitudes toward the benefit of physician empathy among medical students when they start medical school suggests the possibility that these factors will also influence student engagement with and benefit from medical school curricula focused on teaching students to provide empathic care. Understanding and starting from learners existing attitudes and knowledge is a central tenet of adult education and theory [21] and interventions that are tailored to individuals’ existing views on the world are more effective than using a single approach to all learners [55].
Dispositional factors affect the way individuals perceive themselves and interact with new information, people, and activities [25,56]. In this study, students who arrived at medical school high on dispositional empathy (the tendency toward empathic concern) and dispositional perspective taking (tendency to react to other by taking their view) had, as we might expect, a positive attitude toward physician empathy in clinical encounters. These findings are consistent with evidence that dispositional empathic concern and dispositional perspective taking are associated with attitudes toward and provision of empathy among practicing physicians [35]. Students who are high on these dispositional factors will likely find curricula focused on promoting empathic care relatively comfortable and easy because it fits with their current outlook and response tendencies. They may have a similar worldview with the teachers and instructors delivering curricula on empathic care. Oh the other hand, students who are lower on these factors may find the behavioral requirements of providing empathic care much more challenging. They may find the concepts and perspectives covered in such curricula less familiar. The activities will require unfamiliar ways of responding and so may be more difficult for students low on dispositional empathy and/or perspective taking than those higher on these dispositional attributes.
Close-mindedness and difficulty with uncertainty independently predicted more negative attitudes toward physician empathy in clinical encounters. Empathy involves perspective taking – that is, the ability to see things from another’s point of view. Taking on another’s point of view requires willingness to consider new perspectives. By definition, people who are high on close-mindedness have low comfort with, and preference against, entertaining new and different ideas and perspectives [47]. Empathy training activities may be very uncomfortable and perhaps even highly anxiety-producing for students who are high on close-mindedness because they require the student to engage in processes that run counter to their dispositional preferences and response tendencies.
Differences in disposition seemed to partially account for gender differences in attitude toward physician empathy. Consistent with prior studies [57], men had a less positive attitude toward physician empathy in all of the multivariate models. However, the strength of this gender effect decreased (−.21 to −.09) when the individual disposition variables were entered into the model. This suggests that men’s lower value on physician empathy may be partially, but not entirely due to differences in individual disposition.
Students’ pre-existing sociopolitical attitudes also predicted attitude toward physician empathy in clinical encounters, with medical authoritarianism and elitism associated with more negative attitudes and egalitarianism more positive attitudes. This is consistent with studies showing lower empathy and patient-centeredness among people high in authoritarian and elitism sociopolitical attitudes [58–60]. Furthermore, there are studies showing that medical authoritarianism increases over the course of medical education [61,62] while empathy decreases [61,63,64]. The causal relationship is unclear; empathy and authoritarianism may be independently affected by experiences in medical school. However, it is also possible that reduction in empathy is caused by changes in socio-political attitudes toward more authoritarian perspectives and this deserves more investigation.
The finding that global self-esteem and locus of control were associated with more positive attitudes toward physician empathy is consistent with prior studies showing higher empathy among individuals with stronger self-concept [65] and provides support for efforts to provide a more supportive and affirming medical school environment. Last, the finding that worse well-being, as assessed by fatigue and anxiety symptoms, independently predicted more positive attitudes toward physician empathy is of note and inconsistent with some prior studies showing a positive association between well-being and empathy [32,66,65,67,68]. However, it may be consistent with studies showing a relationship between empathy and burnout, suggesting the possibility that the emotional labor or effort involved in responding empathically may cause additional wear and tear on medical students [69,68].
This study had several limitations and its results should be interpreted with caution. First, it is cross-sectional, and so causal direction is uncertain. In this case, the dependent variable is unlikely to be a cause of the independent variables. Nevertheless, an observed relationship between two variables, such as medical authoritarianism and attitudes toward physician empathy, does not necessarily mean that intervening to influence one variable will cause changes in the other. A second limitation involved our inability to ascertain and invite all MS1 in the school sample, creating potential sample bias. While that is generally more of a concern when estimating population characteristics than it is in estimating relationships between variable, it is possible that the results presented here do not generalize to those students who did not participate. However, we do have evidence regarding predictors of attitudes toward physician empathy in 55% of first year students in the 49 schools included in the sample. Last, the predictors of attitude toward empathy in doctor–patient encounters were limited to those included in the questionnaire; there may be many other important predictors that were not measured in this study.
4.2. Conclusion
Students vary on their attitude toward the value of physician empathy when they start medical school. The individual factors that predict their attitudes toward empathy may also influence their response to curricula promoting empathic care.
4.3. Practice implications
Students with a STEM background, lower dispositional empathy and perspective taking, higher close-mindedness and discomfort with uncertainty may find the content, activities, and practices involved in curricula promoting empathy more challenging than their counterparts. Those who are low on dispositional empathy may need a longer exposure to the concepts and more time practicing empathic responding than those high on this characteristic. Students who are high on close-mindedness and/or difficulty with uncertainty may find the curricula more threatening and may need more support for change. Students’ who are high on medical authoritarianism and elitism and low on egalitarianism sociopolitical attitudes may be more resistant to curricula promoting empathic care. Messages about the benefits and value of physician empathy may need to be framed in ways that are consistent with their beliefs and prior world-view [70]. Further research is needed to identify intervention strategies which either create general programming that is broad enough to appeal across a disparate set of student dispositions, or utilizes practical approaches to tailoring that individualizes the framing and appeal for particular students. For example, effective instructors might describe empathy conceptually without introducing subjective-sounding language at first, and attempt to ground its value in terms that might be more familiar to people with more authoritarian or non-egalitarian world-views.
In an article entitled The Role of Empathy in Medicine: A Medical Student’s Perspective [71], Elliot Hirsh writes: “Initially, it was somewhat difficult for me to understand the importance of these sessions. I appreciated our instructor’s intentions but often felt that the material could have been more effectively presented. In retrospect, I was probably one of the milder critics of the course; a large number of students did not take the curriculum seriously, seeing it as a waste of time that could have been better spent studying. The challenge for medical educators is to present the information in a format that makes it relevant and actively engages the students” (p 435–426). Understanding the factors that affect medical students’ attitudes toward physician empathy is a starting point for accomplishing this goal.
Acknowledgements
We thank Deborah Finstad for her assistance for her editorial contribution to this manuscript as well as her contribution to the study overall.
Footnotes
Funding: This study was funded by a grant from the National Heart, Lung, and Blood Institute, National Institutes of Health, Grant R01 HL085631.
All learners construct knowledge from an inner scaffolding of their individual and social experiences, emotions, will, aptitudes, beliefs, values, self-awareness, purpose, and more … if you are learning in a classroom, what you understand is determined by how you understand things, who you are, and what you already know.
Peter Senge, Director of the Center for Organizational Learning at MIT
Conflict of interest
None of the authors have any actual or potential conflict of interest including any financial, personal or other relationships with other people or organizations within three years of beginning the submitted work that could inappropriately influence, or be perceived to influence, their work.
References
- 1.Derksen F, Bensing J, Lagro-Janssen A. Effectiveness of empathy in general practice: a systematic review. Br J Gen Pract. 2013;63:e76–e84. doi: 10.3399/bjgp13X660814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–364. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan JE, Keeley RD, Engel M, Emsermann C, Brody D. Aspects of patient and clinician language predict adherence to antidepressant medication. J Am Board Fam Med. 2013;26:409–420. doi: 10.3122/jabfm.2013.04.120201. [DOI] [PubMed] [Google Scholar]
- 4.Steinhausen S, Ommen O, Thum S, Lefering R, Koehler T, Neugebauer E, et al. Physician empathy and subjective evaluation of medical treatment outcome in trauma surgery patients. Patient Educ Couns. 2013;95:53–60. doi: 10.1016/j.pec.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Lelorain S, Bredart A, Dolbeault S, Sultan S. A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psychooncology. 2012;21:1255–1264. doi: 10.1002/pon.2115. [DOI] [PubMed] [Google Scholar]
- 6.Rakel D, Barrett B, Zhang Z, Hoeft T, Chewning B, Marchand L, et al. Perception of empathy in the therapeutic encounter: effects on the common cold. Patient Educ Couns. 2011;85:390–397. doi: 10.1016/j.pec.2011.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rakel DP, Hoeft TJ, Barrett BP, Chewning BA, Craig BM, Niu M. Practitioner empathy and the duration of the common cold. Fam Med. 2009;41:494–501. [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mikesell L. Medicinal relationships: caring conversation. Med Educ. 2013;47:443–452. doi: 10.1111/medu.12104. [DOI] [PubMed] [Google Scholar]
- 10.Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the nature and specific effectiveness of clinical empathy: a theoretical overview and contribution towards a theory-based research agenda. Patient Educ Couns. 2009;74:339–346. doi: 10.1016/j.pec.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 11.Weng HC, Steed JF, Yu SW, Liu YT, Hsu CC, Yu TJ, et al. The effect of surgeon empathy and emotional intelligence on patient satisfaction. Adv Health Sci Educ Theory Pract. 2011;16:591–600. doi: 10.1007/s10459-011-9278-3. [DOI] [PubMed] [Google Scholar]
- 12.Bland P. Patients of empathetic GPs have better outcomes. Practitioner. 2013;257:255. [PubMed] [Google Scholar]
- 13.Pedersen R. Empirical research on empathy in medicine - a critical review. Patient Educ Couns. 2009;76:307–322. doi: 10.1016/j.pec.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 14.van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93:248–255. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 16.Penner LA, Gaertner S, Dovidio JF, Hagiwara N, Porcerelli J, Markova T, et al. A social psychological approach to improving the outcomes of racially discordant medical interactions. J Gen Intern Med. 2013;28:1143–1149. doi: 10.1007/s11606-013-2339-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stepien KA, Baernstein A. Educating for empathy. A review. J Gen Intern Med. 2006;21:524–530. doi: 10.1111/j.1525-1497.2006.00443.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Batt-Rawden SA, Chisolm MS, Anton B, Flickinger TE. Teaching empathy to medical students: an updated, systematic review. Acad Med. 2013;88:1171–1177. doi: 10.1097/ACM.0b013e318299f3e3. [DOI] [PubMed] [Google Scholar]
- 19.Chen PW. Can doctors learn empathy? New York City: New York Times; 2012. [Google Scholar]
- 20.Riess H, Kelley JM, Bailey RW, Dunn EJ, Phillips M. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27:1280–1286. doi: 10.1007/s11606-012-2063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bransford JD, Brown AL, Cocking RR. How people learn: brain, mind, experience, and school, expanded edition. Washington, DC: National Academic Press; 2000. Committee on Developments in the Science of Learning NRC, editor. [Google Scholar]
- 22.Resnick LB. Mathematics and science learning: a new conception. Science. 1983;220:477–478. doi: 10.1126/science.220.4596.477. [DOI] [PubMed] [Google Scholar]
- 23.Svin M. Teaching & learning resources. Teaching guides Minneapolis, MN: University of Minnesota Center for Teaching and Learning; 2007. What they don’t know can hurt them: the role of prior knowledge in learning. [Google Scholar]
- 24.Robertson WC. Detection of cognitive structure with protocol data: predicting performance on physics transfer problems. Cogn Sci. 1990;14:253–280. [Google Scholar]
- 25.Hojat M, Erdmann JB, Gonnella JS. Personality assessments and outcomes in medical education and the practice of medicine: AMEE Guide No 79. Med Teach. 2013;35:e1267–e1301. doi: 10.3109/0142159X.2013.785654. [DOI] [PubMed] [Google Scholar]
- 26.Johns MW, Dudley HA, Masterton JP. The sleep habits, personality and academic performance of medical students. Med Educ. 1976;10:158–162. doi: 10.1111/j.1365-2923.1976.tb00432.x. [DOI] [PubMed] [Google Scholar]
- 27.Flook AJ, Robinson PJ. Academic performance with and without knowledge of scores on tests of intelligence, aptitude, and personality: a further study. J Educ Psychol. 1972;63:123–129. doi: 10.1037/h0032640. [DOI] [PubMed] [Google Scholar]
- 28.Cowell MD, Entwistle NJ. The relationships between personality, study attitudes and academic performance in a technical college. Br J Educ Psychol. 1971;41:85–90. doi: 10.1111/j.2044-8279.1971.tb00661.x. [DOI] [PubMed] [Google Scholar]
- 29.Kelvin RP, Lucas CJ, Ojha AB. The relation between personality, mental health and academic performance in university students. Br J Soc Clin Psychol. 1965;4:244–253. doi: 10.1111/j.2044-8260.1965.tb00471.x. [DOI] [PubMed] [Google Scholar]
- 30.Austin EJ, Evans P, Magnus B, O’Hanlon K. A preliminary study of empathy, emotional intelligence and examination performance in MBChB students. Med Educ. 2007;41:684–689. doi: 10.1111/j.1365-2923.2007.02795.x. [DOI] [PubMed] [Google Scholar]
- 31.Dehning S, Gasperi S, Krause D, Meyer S, Reiss E, Burger M, et al. Emotional and cognitive empathy in first-year medical students. ISRN Psychiatry. 2013;2013:801530. doi: 10.1155/2013/801530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lamothe M, Boujut E, Zenasni F, Sultan S. To be or not to be empathic: the combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Fam Pract. 2014;15:15. doi: 10.1186/1471-2296-15-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dehning S, Girma E, Gasperi S, Meyer S, Tesfaye M, Siebeck M. Comparative cross-sectional study of empathy among first year and final year medical students in Jimma University, Ethiopia: steady state of the heart and opening of the eyes. BMC Med Educ. 2012;12:34. doi: 10.1186/1472-6920-12-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glaser KM, Markham FW, Adler HM, McManus PR, Hojat M. Relationships between scores on the Jefferson Scale of physician empathy, patient perceptions of physician empathy, and humanistic approaches to patient care: a validity study. Med Sci Monit. 2007;13:CR291–CR294. [PubMed] [Google Scholar]
- 35.Gleichgerrcht E, Decety J. Empathy in clinical practice: how individual dispositions, gender, and experience moderate empathic concern, burnout, and emotional distress in physicians. PLOS ONE. 2013;8:e61526. doi: 10.1371/journal.pone.0061526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lourinho I, Severo M. Are personality traits really weak/moderate predictors of empathy? Med Teach. 2013;35:611. doi: 10.3109/0142159X.2013.786169. [DOI] [PubMed] [Google Scholar]
- 37.Haight SJ, Chibnall JT, Schindler DL, Slavin SJ. Associations of medical student personality and health/wellness characteristics with their medical school performance across the curriculum. Acad Med. 2012;87:476–485. doi: 10.1097/ACM.0b013e318248e9d0. [DOI] [PubMed] [Google Scholar]
- 38.Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–527. doi: 10.1046/j.1365-2923.2002.01234.x. [DOI] [PubMed] [Google Scholar]
- 39.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–1569. doi: 10.1176/appi.ajp.159.9.1563. [DOI] [PubMed] [Google Scholar]
- 40.Hojat M, Mangione S, Kane GC, Gonnella JS. Relationships between scores of the Jefferson Scale of Physician Empathy (JSPE) and the Interpersonal Reactivity Index (IRI) Med Teach. 2005;27:625–628. doi: 10.1080/01421590500069744. [DOI] [PubMed] [Google Scholar]
- 41.Hojat M, Mangione S, Nasca TJ, Gonnella JS, Magee M. Empathy scores in medical school and ratings of empathic behavior in residency training 3 years later. J Soc Psychol. 2005;145:663–672. doi: 10.3200/SOCP.145.6.663-672. [DOI] [PubMed] [Google Scholar]
- 42.Dyrbye LN, Thomas MR, Harper W, Massie FS, Jr, Power DV, Eacker A, et al. The learning environment and medical student burnout: a multicentre study. Med Educ. 2009;43:274–282. doi: 10.1111/j.1365-2923.2008.03282.x. [DOI] [PubMed] [Google Scholar]
- 43.Tavakol S, Dennick R, Tavakol M. Psychometric properties and confirmatory factor analysis of the Jefferson Scale of Physician Empathy. BMC Med Educ. 2011;11:54. doi: 10.1186/1472-6920-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fields SK, Mahan P, Tillman P, Harris J, Maxwell K, Hojat M. Measuring empathy in healthcare profession students using the Jefferson Scale of Physician Empathy: health provider - student version. J Interprof Care. 2011;25:287–293. doi: 10.3109/13561820.2011.566648. [DOI] [PubMed] [Google Scholar]
- 45.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson Scale of Physician Empathy: further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77:S58–S60. doi: 10.1097/00001888-200210001-00019. [DOI] [PubMed] [Google Scholar]
- 46.Davis M. Measuring individual differences in empathy: evidence for a multidimensional approach. J Pers Soc Psychol. 1983;44:113–126. [Google Scholar]
- 47.Webster DM, Kruglanski AW. Individual-differences in need for cognitive closure. J Pers Soc Psychol. 1994;67:1049–1062. doi: 10.1037//0022-3514.67.6.1049. [DOI] [PubMed] [Google Scholar]
- 48.Sidanius J, Pratto F. Social dominance: an intergroup theory of social hierarchy and oppression. New York, NY: Cambridge University Press; 1999. [Google Scholar]
- 49.Merrill JM, Laux LF, Lorimor R, Thornby JI, Vallbona C. Authoritarianism’s role in medicine. Am J Med Sci. 1995;310:87–90. doi: 10.1097/00000441-199531030-00001. [DOI] [PubMed] [Google Scholar]
- 50.Pearlin L, Schooler C. The structure of coping. J Health Soc Behav. 1978;19:2–21. [PubMed] [Google Scholar]
- 51.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 52.Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Liu H, Cella D, Gershon R, Shen J, Morales LS, Riley W, et al. Representativeness of the Patient-Reported Outcomes Measurement Information System Internet panel. J Clin Epidemiol. 2010;63:1169–1178. doi: 10.1016/j.jclinepi.2009.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;24:349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- 55.Haidt J. The righteous mind: why good people are divided by politics and religion pantheon. 2012 [Google Scholar]
- 56.Entwistle N, McCune V. The disposition to understand for oneself at university: integrating learning processes with motivation and metacognition. Br J Educ Psychol. 2013;83:267–279. doi: 10.1111/bjep.12010. [DOI] [PubMed] [Google Scholar]
- 57.Hegazi I, Wilson I. Maintaining empathy in medical school: it is possible. Med Teach. 2013;35:1002–1008. doi: 10.3109/0142159X.2013.802296. [DOI] [PubMed] [Google Scholar]
- 58.Sidanius J, Kteily N, Sheehy-Skeffington J, Ho AK, Sibley C, Duriez B. You’re inferior and not worth our concern: the interface between empathy and social dominance orientation. J Pers. 2013;81:313–323. doi: 10.1111/jopy.12008. [DOI] [PubMed] [Google Scholar]
- 59.Frosch DL, May SG, Rendle KA, Tietbohl C, Elwyn G. Authoritarian physicians and patients’ fear of being labeled ‘difficult’ among key obstacles to shared decision making. Health Aff (Millwood) 2012;31:1030–1038. doi: 10.1377/hlthaff.2011.0576. [DOI] [PubMed] [Google Scholar]
- 60.Merrill JM, Lorimor RJ, Thornby JI, Vallbona C. Reliance on high technology among senior medical students. Am J Med Sci. 1998;315:35–39. doi: 10.1097/00000441-199801000-00007. [DOI] [PubMed] [Google Scholar]
- 61.Tsimtsiou Z, Kerasidou O, Efstathiou N, Papaharitou S, Hatzimouratidis K, Hatzichristou D. Medical students’ attitudes toward patient-centred care: a longitudinal survey. Med Educ. 2007;41:146–153. doi: 10.1111/j.1365-2929.2006.02668.x. [DOI] [PubMed] [Google Scholar]
- 62.Lavin B, Haug M, Belgrave LL, Breslau N. Change in student physicians’ views on authority relationships with patients. J Health Soc Behav. 1987;28:258–272. [PubMed] [Google Scholar]
- 63.Hojat M, Vergare MJ, Maxwell K, Brainard G, Herrine SK, Isenberg GA, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–1191. doi: 10.1097/ACM.0b013e3181b17e55. [DOI] [PubMed] [Google Scholar]
- 64.Hojat M, Mangione S, Nasca TJ, Rattner S, Erdmann JB, Gonnella JS, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38:934–941. doi: 10.1111/j.1365-2929.2004.01911.x. [DOI] [PubMed] [Google Scholar]
- 65.Novack DH, Epstein RM, Paulsen RH. Toward creating physician-healers: fostering medical students’ self-awareness, personal growth, and well-being. Acad Med. 1999;74:516–520. doi: 10.1097/00001888-199905000-00017. [DOI] [PubMed] [Google Scholar]
- 66.Epstein RM. Mindful practice. J Amer Med Assoc. 1999;282:833–839. doi: 10.1001/jama.282.9.833. [DOI] [PubMed] [Google Scholar]
- 67.Novack DH, Suchman AL, Clark W, Epstein RM, Najberg E, Kaplan C. Calibrating the physician, personal awareness effective patient care. Working group on promoting physician personal awareness, American academy on physician and patient. J Amer Med Assoc. 1997;278:502–509. doi: 10.1001/jama.278.6.502. [DOI] [PubMed] [Google Scholar]
- 68.Thomas MR, Dyrbye LN, Huntington JL, Lawson KL, Novotny PJ, Sloan JA, et al. How do distress and well-being relate to medical student empathy? A multi-center study. J Gen Intern Med. 2007;22:177–183. doi: 10.1007/s11606-006-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carmel S, Glick SM. Compassionate-empathic physicians: personality traits and social-organizational factors that enhance or inhibit this behavior pattern. Social Sci Med. 1996;43:1253–1261. doi: 10.1016/0277-9536(95)00445-9. [DOI] [PubMed] [Google Scholar]
- 70.Haidt J, Graham J, Joseph C. Above and below left-right: ideological narratives and moral foundations. Psychol Inq. 2009;20:110–119. [Google Scholar]
- 71.Hirsch EM. The role of empathy in medicine: a medical student’s perspective. Virtual Mentor. 2007;9:423–427. doi: 10.1001/virtualmentor.2007.9.6.medu1-0706. [DOI] [PubMed] [Google Scholar]