Abstract
Background:
Despite concerns as to whether nurses can perform reliably and effectively when working longer shifts, a pattern of two 12- to 13-hour shifts per day is becoming common in many hospitals to reduce shift to shift handovers, staffing overlap, and hence costs.
Objectives:
To describe shift patterns of European nurses and investigate whether shift length and working beyond contracted hours (overtime) is associated with nurse-reported care quality, safety, and care left undone.
Methods:
Cross-sectional survey of 31,627 registered nurses in general medical/surgical units within 488 hospitals across 12 European countries.
Results:
A total of 50% of nurses worked shifts of ≤8 hours, but 15% worked ≥12 hours. Typical shift length varied between countries and within some countries. Nurses working for ≥12 hours were more likely to report poor or failing patient safety [odds ratio (OR)=1.41; 95% confidence interval (CI), 1.13–1.76], poor/fair quality of care (OR=1.30; 95% CI, 1.10–1.53), and more care activities left undone (RR=1.13; 95% CI, 1.09–1.16). Working overtime was also associated with reports of poor or failing patient safety (OR=1.67; 95% CI, 1.51–1.86), poor/fair quality of care (OR=1.32; 95% CI, 1.23–1.42), and more care left undone (RR=1.29; 95% CI, 1.27–1.31).
Conclusions:
European registered nurses working shifts of ≥12 hours and those working overtime report lower quality and safety and more care left undone. Policies to adopt a 12-hour nursing shift pattern should proceed with caution. Use of overtime working to mitigate staffing shortages or increase flexibility may also incur additional risk to quality.
Key Words: shift work, quality, safety, nurses, workforce, efficiency, Europe
BACKGROUND
Traditionally, shift work was organized by dividing the day into three 8-hour shifts. This pattern was the norm in nursing for many years. In common with other industries, there is now a trend for some health care employers to adopt longer shifts, typically 2 shifts per day each lasting 12–13 hours. Employees work fewer shifts each week.1 Changes are driven by perceived efficiencies for the employer, and improved work life balance for employees because they work fewer days per week.1–3 However, persistent concerns have been raised about negative impacts on the quality of care associated with working longer hours.
From an employer’s perspective, a move from 3 to 2 shifts per day reduces periods of shift overlap and the number of handovers, thus reducing costs by reducing total workforce requirements.4 Because handovers and overlaps between shifts are regarded as unproductive, the aim is to improve efficiency with no detrimental effect on quality. Indeed a reduced number of handovers might have beneficial effects as handovers are associated with discontinuity and errors.5,6 From an employee perspective, there are reports that many nurses prefer the compressed working week that results from working fewer shifts.7–10
Nonetheless, the introduction of 12-hour shifts has raised concerns. Long working hours are correlated with fatigue and decreased levels of alertness, potentially resulting in more adverse events.11,12 However, the point at which longer shifts adversely affect performance is likely to be industry, context, and task specific,1 and studies in health care have given mixed results.13 A recent study based on a survey of 22,275 registered nurses (RN) in 4 US states found that nurses who worked shifts of ≥12 hours were significantly more likely to report poor quality of care and poor patient safety when compared with nurses working 8- to 9-hour shifts.14 Patients in hospitals where a higher proportion of nurses worked longer shifts also reported lower satisfaction.10 However, the odds of adverse reports of quality and safety were greater for nurses working 10–11 hours than for those working ≥12, which is inconsistent with a simple effect from longer hours worked on the shift. Analysis of a subsample of 3710 pediatric nurses found that reports of poor quality and safety were substantially elevated only among nurses working >13 hours.15
Several issues remain to be clarified. Hospitals in many countries worldwide are implementing 12-hour shifts,7–10 but the extent to which employers are adopting this shift pattern is unclear. Surveys of US RNs indicated that 65% worked shifts of 12–13 hours.14 A survey in 11 European countries indicated variation in shift patterns between countries but did not report specifically on shift length.16 Studies from outside the United States have generally focused on nurse job satisfaction and have not quantified associations with care quality (eg, Richardson and colleagues8,17). It is unclear whether findings relating to quality of care from the United States will be replicated in a European context, where typical weekly working hours are shorter and annual leave allowances more generous18 with the EU working time directive setting limits to both the total working week and continuous hours worked for many countries.
In the past, research in this area has lacked a clear theoretical framework.19 Recently, a simple model has been proposed, whereby increased fatigue during the shift mediates the effect of shift length on performance leading to errors, omissions, and lower efficiency.20 However, previous research has tended to conflate overtime working (working beyond contracted hours) with long shifts. Overtime working has also been associated with adverse quality because of cumulative fatigue, lack of rest, and adverse working environments.21,22 To more fully understand the issue of shift length and make research more useful to guide hospitals in developing their staffing policy it is therefore important to also consider both overtime working and total hours worked.
In this study, we describe the shift patterns worked by nurses on medical and surgical wards in European hospitals and explore associations between hours worked, working beyond contracted hours on a shift, and reports of quality and safety of care while controlling for total hours of work.
METHODS
We undertook a cross-sectional survey of RNs in medical and surgical wards of acute hospitals as part of the RN4CAST study.23 Data were collected in 12 European countries: Belgium, England, Germany, Finland, Greece, Ireland, The Netherlands, Norway, Poland, Spain, Sweden, and Switzerland. Depending on national legislation, the study was approved by either central (eg, national, regional) or local (eg, hospitals) ethical committees.
Sample
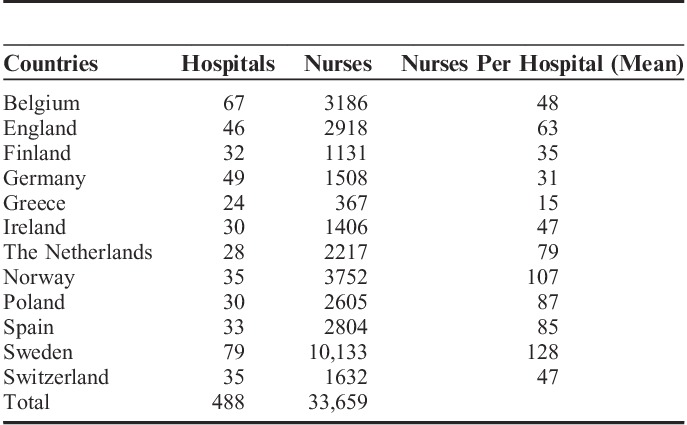
The survey was mailed or directly distributed to RNs in acute general hospitals between June 2009 and June 2010. The target sample was 30 hospitals in each country. In Ireland, Norway and Sweden all eligible hospitals were included. In Belgium, England, Germany, The Netherlands, Switzerland, and Spain, hospital selection was random with stratification for geographical location, type, and size. In Finland, Poland, and Greece, hospitals were sampled purposively to be geographically representative. A minimum of 2 (mean, 5.1) adult medical/surgical wards were randomly selected from each hospital. In Sweden, nurses were approached by the professional association which organizes over 70% of nurses and so all wards were potentially sampled. Specialized nursing units (eg, intensive care, high dependency, long-term care) were excluded because staffing and shift patterns in these can differ substantially. In each ward, all RNs delivering direct care to patients were asked to complete and return a written questionnaire. In total 54,140 questionnaires were distributed. Responses were obtained from 33,659 (62%) RNs in 488 hospitals (Table 1). Fuller details have been published elsewhere.23,24
TABLE 1.
Hospital/Nurse Sample by Country
Measurements
The survey was based on the validated International Hospital Outcomes Study questionnaire.25 The English survey was translated into Dutch, German, Greek, French, Italian, Finnish, Norwegian, Polish, Swedish, and Spanish using the translation-back translation method. Content validity and translation quality indices for all items used in this study were classified as “good” or better (content validity index>0.6).26
Nurses were asked to report the number of hours worked, the period of the day, and whether they had worked beyond their contracted hours on the last shift they worked. Shifts were dichotomized into day (including afternoon/evening shifts) and night shifts. Shift length was grouped into 5 categories: ≤8, 8.1–10, 10.1–11.9, 12–13, >13 hours. Where nurses had identified a shift length that was ≥18 hours, we treated data as missing. Absolute numbers of these were very low (<1%). In most cases it appeared that these nurses had given the number of hours worked weekly. Nurses also reported on the number of patients on the ward and the numbers of nursing staff working on that shift. From this we calculated patient to nurse ratios.
Nurses were asked to evaluate the quality of nursing care on their ward as fair or poor as opposed to good or excellent. This measure has been validated by associations with hospital-level mortality, patient satisfaction, and care processes.27 For analysis, “poor” and “fair” responses were grouped to reflect negative evaluations of quality. Patient safety was rated as poor, failing, acceptable, very good, or excellent with “poor” and “failing” ratings combined to reflect negative evaluations. Nurses were asked to identify whether any necessary activities from a list of 13 core nursing duties were left undone on their last shift worked because of lack of time. Items were derived from the BERNCA instrument, which has validated associations between care left undone, patient experience, and outcomes.28 A rate of care left undone was derived by summing the number of activities ticked per person, resulting in a score indicating the number of areas of care left undone (range from 0 to 13) (see Fig. 1 for details of specific questions used).
FIGURE 1.
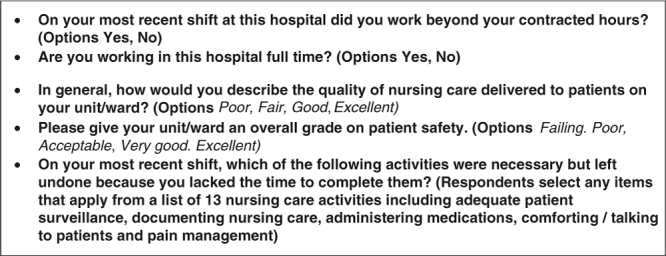
Survey items about shift work and quality.
Analysis
Intraclass correlation coefficients (ICC 1) were computed from unconditional random intercept models to describe within-country, within-hospital, and within-unit variation for shift length. The ICC 1 measures the degree of similarity between individuals within a cluster.29 It also indicates the proportion of variance in the outcome that can be attributed to variation between groups (wards, hospitals, countries) as opposed to between individuals.30
The association of shift length and overtime with the outcome measures was estimated through a binomial generalized linear mixed model. The association of shift length and overtime with care left undone was estimated by a generalized mixed model with a Poisson distribution. Because of the small sample size of the >13 hours category (n=260, 0.08%), we grouped the >13 hours category with the 12–13 hours into a ≥12 hours category for analysis. The multilevel structure allowed nurses to be nested into units, hospitals, and countries. We controlled for potential confounding variables, including variables chosen because they have been shown elsewhere to have independent relationships with the quality of care in hospitals31,32 or the ability to cope with shift work.33 Control variables were shift type (day/night), ward type, nurse staffing levels (quantified by the ratio of patients per nurse), nurses’ age, full time versus part time working, hospital size (<250, 250–500, >500 beds), high-technology hospitals (those that performed major organ transplant surgery and/or open heart surgery), and teaching status (hospitals that provide training to undergraduate medical students). The variance inflation factor (VIF) was assessed for all model predictors to identify multicollinearity, with VIF<5 indicating no multicollinearity.34 Analysis was conducted using RStudio version 0.96.33035 and lme4 package.36
RESULTS
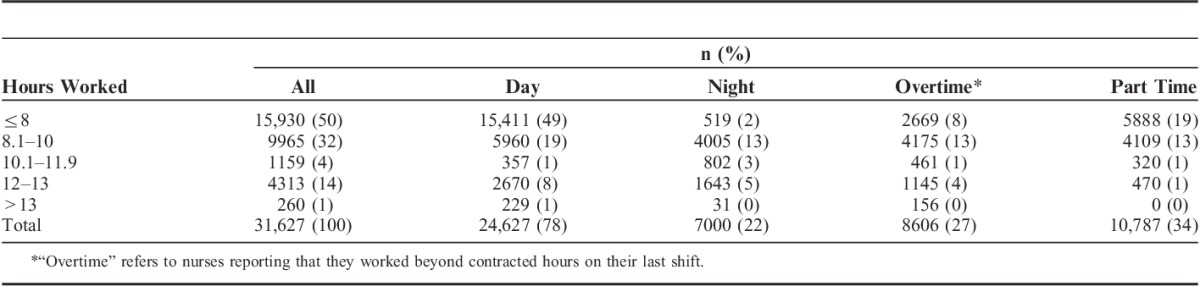
Data from 31,627 respondents working on adult medical/surgical wards was available for analysis. The mean age of respondents was 38. Ninety-two percent were female. Sixty-five percent of nurses worked full time (n=20,513). Sixty-seven percent worked in high-technology hospitals and 68% in teaching hospitals. Fifty-seven percent worked in medical units or mixed medical/surgical units, with the remaining 43% in surgical units. The majority (76%) of nurses reported on day shifts (Table 2).
TABLE 2.
Characteristics of Last Shift Worked and Hours Worked
Shift Length
The most common shift length was≤8 hours (50%, n=15,930). Thirty-two percent worked from 8.1 to 10 hours (n=9963) and 14% (n=4314) worked 12 to 13 hours. Only 260 nurses (1%) worked >13 hours on their last shift.
Countries varied in their typical shift length (Table 3). For Belgium, Germany, Greece, The Netherlands, Norway, and Sweden <5% of nurses reported working shifts of ≥12 hours. In all these countries the majority of day shifts were ≤8 hours. Shifts of ≥12 hours were also rare in Finland, Spain, and Switzerland. For Ireland and Poland, shifts of 12 hours were the norm (≥73% of all shifts). England presented a mixed picture, with 32% of day shifts and 37% of night shifts lasting ≥12 hours. Most variation in shift length was between units, with individuals within units tending to work similar shifts (ICC=0.63). Individuals in the same hospital and country also tended to work similar shifts (ICC=0.58, 0.49) with substantial variation between hospitals and countries.
TABLE 3.
Day and Night Shift Length by Country
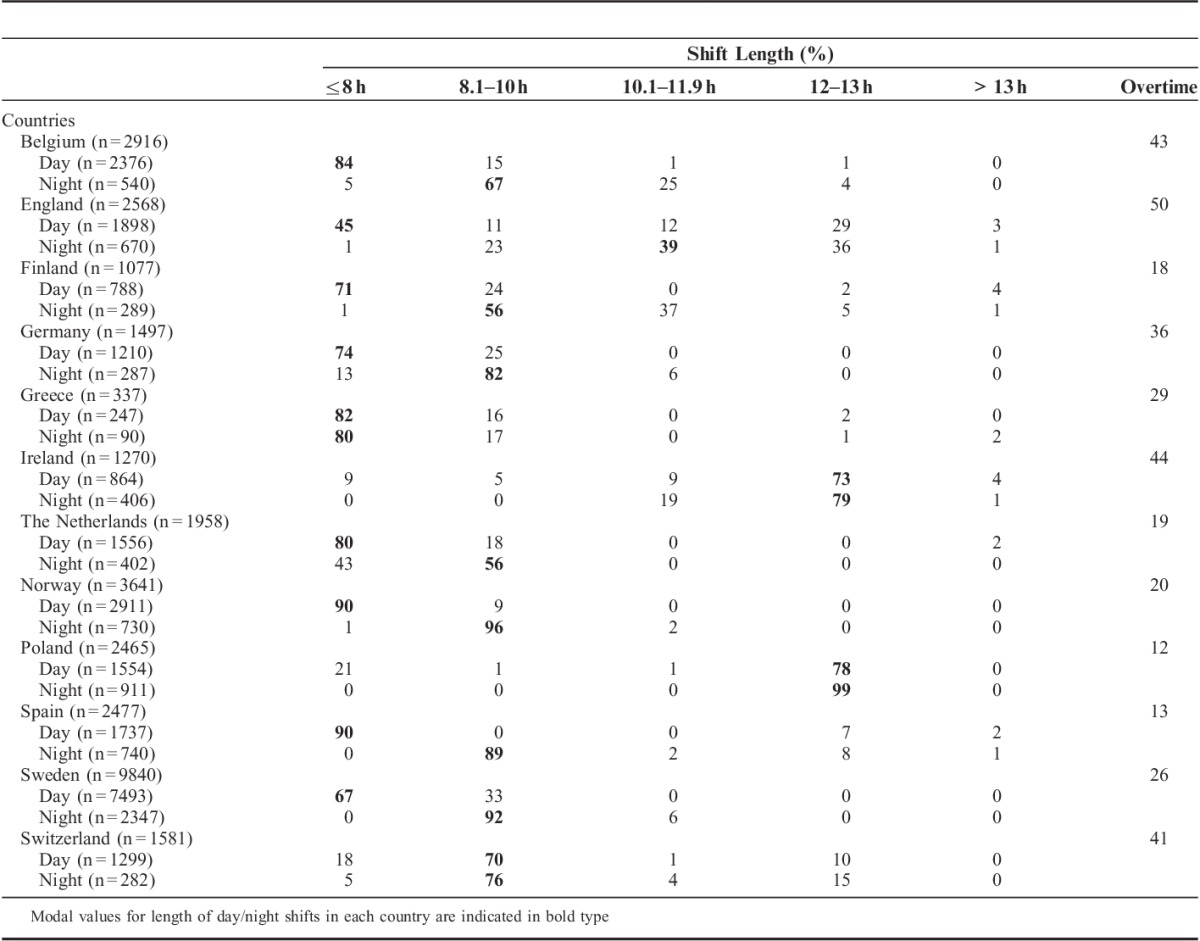
Overall, 8606 nurses (27%) reported that they had worked overtime (beyond their contracted hours) on their last shift (Table 2). Most reports of overtime work were made by nurses who reported working 8.1–10 hours (49%, 4175/8606). A majority of nurses who reported working shifts of >13 hours worked overtime on that shift (60%, 156/260). There was wide variation between hospitals, with a range from 0% to 80% of nurses working overtime. There was also variation between countries ranging from 50% (England) to 12% (Poland) (Table 3).
Associations With Quality, Safety, and Care Left Undone
Twenty-five percent (n=7815) of nurses reported poor/fair quality of care and 7% (2736) reported “poor” or “failing” patient safety. Distributions of quality and safety statements by country are reported elsewhere.24 Nurses reported on average 3 activities left undone on their last shift. Only 3934 nurses (12%) did not report leaving any care undone.
Longer shifts and working overtime were significantly associated with quality of care, patient safety reports, and care left undone (<0.05). Compared with nurses working ≤8 hours, nurses working ≥12 hours on their last shift were more likely to rate the quality of nursing care in their unit as “poor” or “fair” (OR=1.30; 95% CI, 1.10–1.53) and more likely to report “failing” or “poor” patient safety in their units (OR=1.41; 95% CI, 1.13–1.76). Although not statistically significant, odds of adverse quality and safety were raised for all shift lengths >8 hours although only marginally for shifts of 8.1–10 hours. Nurses working ≥12 hours reported higher rates of care left undone than did nurses working ≤8 hours (RR=1.13; 95% CI, 1.09–1.16). All shifts >8 hours were associated with statistically significant increases in the rate of care left undone (P<0.05) (Table 4).
TABLE 4.
Results of Multilevel Regression Models: Associations Between the Model Predictors, and Quality of Care, Patient Safety, and Care Left Undone
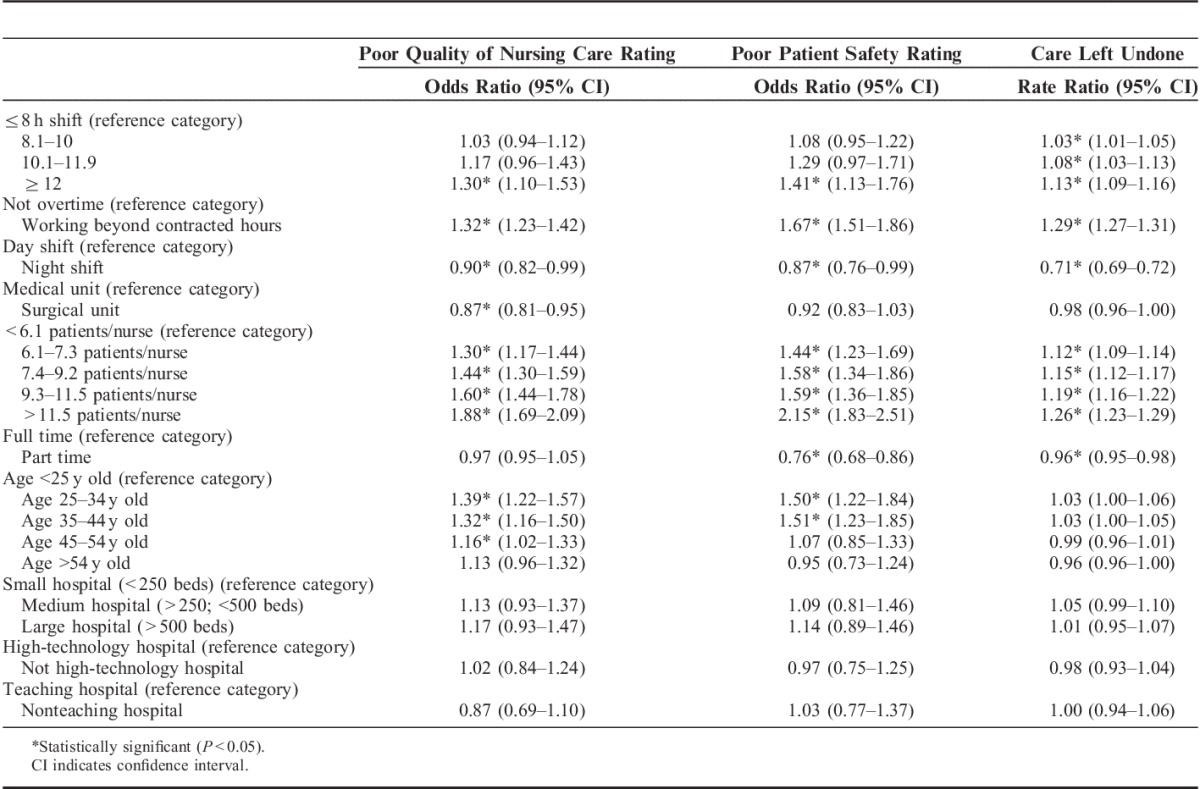
Nurses working overtime on their last shift were more likely to report poor/fair quality of nursing care (OR=1.32; 95% CI, 1.23–1.42), poor/failing patient safety (OR=1.67; 95% CI, 1.51–1.86), and higher rates of care left undone (RR=1.29; 95% CI, 1.27–1.31) (Table 4).
There were significant associations between reports of quality, safety, or missed care for several control variables including night shifts (fewer negative evaluations), patient to nurse ratio (more negative evaluations with more patients per nurse), and part time work (fewer negative evaluations) (Table 4).
We tested for interaction between shift length and overtime (model not shown—available from authors); however, the relationship was not significant. To assess the impact of our decision to collapse the 12–13 hours and >13-hour categories, we analyzed the data with the 12–13 hours and >13-hour categories separately. To ensure conclusions were not biased by post hoc classification of safety ratings, we analyzed the data with “acceptable” safety ratings grouped with “poor” and “failing.” These changes did not alter results significantly.
DISCUSSION
To our knowledge, this is the first study in Europe to demonstrate a relationship between longer shifts worked by hospital nurses and problems in the quality and safety of care. Shifts of ≥12 hours and working overtime (beyond contracted hours) on a shift were independently associated with nurses’ reports of lower quality of care, poorer patient safety, and increasing rates of care left undone. All shifts >8 hours were associated with increasing rates of care left undone. Our results show substantial variation in typical shift patterns between European countries. Although overall only 15% of nurses reported working ≥12 hours on their last shift, long shifts were common in England, Ireland, and Poland. The reason for the variation is unclear. Of countries where 12-hour shifts were common, only England was reported as experiencing nursing shortages at the time of the study,37 although the pattern may have been established in Poland and Ireland during historical periods of shortage. Twenty-seven percent of all nurses reported working overtime on their last shift.
In the USA, shifts of ≥12 hours are prevalent7,38 and have been associated with poorer quality ratings.10,15 However, it was not clear in these studies whether the adverse associations between shift length and quality were the result of the number of hours worked on the shift or working overtime. Associations between overtime and deficits in health care quality have also been reported previously.21,22,39–41 Our study shows working overtime on a shift to be a negative factor independent of the total hours worked on the shift and also clearly indicates that shifts of ≥12 hours are associated with reports of reduced quality, independently of working overtime and the length of the normal working week (full time vs. part time).
These findings raise questions for health care organizations, especially in the current economic climate, where employers in many countries are aiming to use the existing workforce more efficiently, either to reduce expenditure or because of nursing shortages. Previous research indicates that low nurse staffing levels are associated with worse patient outcomes.24,42 This finding is supported by our analysis. Moving from 3 shorter shifts per day to 2 longer ones to maintain current patient to nurse ratios with fewer total staff has been advocated in England and elsewhere, with claimed savings of up to 14% on salary costs for nurses working shifts.5 However, such a strategy may not have the desired effect if nurses perform less effectively and safely.
Overtime working is common in nursing. This is reflected by the prevalence seen in the current study and in reports from US43,44 and elsewhere.45 In our survey, reported overtime varied between hospitals from 0% to 80% consistent with surveys from the US which also show substantial variation between hospitals.43 Variation of such magnitude suggests that it is unlikely to be a simple product of variation in workforce supply but may also result from variation in staffing policies. The results of this study suggest that the apparent flexibility for employers, using overtime to meet dynamic staffing requirements, may be counterproductive because of the negative associations with quality and safety.
Although increased fatigue, loss of alertness, and impaired decision making are plausible mechanisms to explain reduced ratings of quality and safety with longer shifts, this does not fully explain an adverse effect from overtime independent of shift length. Overtime has previously been associated with increased nurse turnover10,46 and it may be that use of overtime is associated with less favorable working environments for nurses, which are known to be linked to subjective and objective measures of reduced quality and safety of care.23,47 Overtime can be an individual voluntary strategy of “working late” (unpaid) to complete work or an organizational strategy of asking or requiring workers (unpaid or with additional pay or time off in lieu) to extend working hours to meet demand. Although the distinction between these modes of overtime has been questioned,10 they may be relevant in determining engagement and motivation for those working overtime. For example, overtime that is mandatory may have a negative effect on psychological well-being related to lack of control.48
The degree to which nurses are subsidizing health services through unpaid overtime and the impact of long hours and overtime on burnout have implications for both the costs and the effectiveness of extended shifts, which require further exploration. The paradox whereby longer shifts appear to be preferred by nurses because of the compressed working week,7–10 and yet deliver poorer evaluations of safety and quality of care also merits further investigation.
Our study has some limitations. Our analysis of cross-sectional survey data showed associations between shift patterns and quality and safety, but it is not possible to infer causality. Because we did not test for interaction effects between country and shift work, we can only estimate the average effect across all countries and cannot explore differences between countries related to (for example) cultural differences. The outcome measures used in this study were nurses’ self-report. The clinical importance of the differences noted is unclear. Although nurses’ self-reports of quality and safety have validated associations with objective measures such as rates of mortality and failure to rescue,27 further research should include objective measures and consider patients’ experiences. Although our sampling strategy was designed to obtain a representative sample of hospitals and nurses in each country, we cannot fully judge the extent to which this was successful because of lack of data for comparison for most countries. Furthermore, the primary purpose of the RN4CAST study was not to assess shift work in particular and so the survey did not ask about the nature of overtime and more specific aspects of shift work, including the number of hours overtime, the nurses usual shift pattern, the possibility of taking breaks during shifts and opportunity to rest between shifts, factors that may be relevant in modeling the effects of shift work on performance.1 Although we were able to use full time versus part time status as a proxy for total hours worked, we did not directly measure hours worked.
CONCLUSIONS
European nurses working >12 hours and those working overtime on a shift were more likely to describe the quality of nursing care delivered to patients on their unit as fair or poor, to assess patient safety as poor or fair, and to report more care items left undone on their last shift, when compared with nurses working ≤8 hours and no more than their contracted hours. In some countries, long shifts (12 h) seem to be the norm and it is advocated as a cost-effective strategy for hospitals in England and elsewhere. However, our results suggest that a policy of moving to longer shifts to reduce overall workforce requirements may have unintended consequences and reduce the efficiency and effectiveness of the workforce in delivering high quality, safe care. Similarly, the increased flexibility associated with overtime may not deliver the desired goals for employers.
Footnotes
The RN4CAST Consortium consists of: Walter Sermeus (Director), Koen Van den Heede, Luk Bruyneel, Emmanuel Lesaffre, Luwis Diya (Belgium, Catholic University Leuven); Linda Aiken, Herbert Smith, Douglas Sloane (USA, University of Pennsylvania); Anne-Marie Rafferty, Jane Ball, Simon Jones (UK, King’s College London); Peter Griffiths (UK, University of Southampton); Juha Kinnunen, Anneli Ensio, Virpi Jylhä (Finland, University of Eastern Finland); Reinhard Busse, Britta Zander, Miriam Blümel (Germany, Berlin University of Technology); John Mantas, Dimitrios Zikos, Marianna Diomidous (Greece, University of Athens); Anne Scott, Anne Matthews, Anthony Staines (Ireland, Dublin City University); Inger Margrethe Holter, Ingeborg Strømseng Sjetne (Norway, Norwegian Knowledge Centre for the Health Services); Tomasz Brzostek, Maria Kózka, Piotr Brzyski (Poland, Jagiellonian University Collegium Medicum); Teresa Moreno- Casbas, Carmen Fuentelsaz-Gallego, Esther Gonzalez-María, Teresa Gomez-Garcia (Spain, Institute of Health Carlos III); Carol Tishelman, Rikard Lindqvist, Lisa Smeds Alenius (Sweden, Karolinska Institutet); Sabina De Geest, Maria Schubert, René Schwendimann (Switzerland, Basel University); Maud Heinen, Lisette Schoonhoven, Theo van Achterberg (The Netherlands, Radboud University Medical Centre).
Supported by the European Union’s Seventh Framework Programme (FP7/2007-2013, grant agreement no. 223468), the Norwegian Nurses Organisation and the Norwegian Knowledge Centre for the Health Services, Swedish Association of Health Professionals, the regional agreement on medical training and clinical research (ALF) between Stockholm County Council and Karolinska Institutet, Committee for Health and Caring Sciences (CfV) and Strategic Research Program in Care Sciences (SFO-V) at Karolinska Institutet.
The authors declare no conflict of interest.
REFERENCES
- 1.Ferguson SA, Dawson D. 12-h or 8-h shifts? It depends. Sleep Med Rev. 2012;16:519–528 [DOI] [PubMed] [Google Scholar]
- 2.Caruso CC, Waters TR. A review of work schedule issues and musculoskeletal disorders with an emphasis on the healthcare sector. Ind Health. 2008;46:523–534 [DOI] [PubMed] [Google Scholar]
- 3.Lorenz SG. 12-hour shifts: an ethical dilemma for the nurse executive. J Nurs Adm. 2008;38:297–301 [DOI] [PubMed] [Google Scholar]
- 4.Sullivan C, Reading S. Nursing shortages: let’s be flexible. Collegian. 2002;9:24–28 [DOI] [PubMed] [Google Scholar]
- 5.NHS Evidence. Moving to 12-hour shift patterns: to increase continuity and reduce costs. Basingstoke and North Hampshire NHS Foundation Trust; 2010
- 6.Committee on Quality of Health Care in America. Crossing the Quality Chasm, A New Health System for the 21st Century. 2001Washington, DC: Institute of Medicine, National Academy Press [Google Scholar]
- 7.Stone PW, Du Y, Cowell R, et al. Comparison of nurse, system and quality patient care outcomes in 8-hour and 12-hour shifts. Med Care. 2006;44:1099–1106 [DOI] [PubMed] [Google Scholar]
- 8.Richardson A, Turnock C, Harris L, et al. A study examining the impact of 12-hour shifts on critical care staff. J Nurs Manag. 2007;15:838–846 [DOI] [PubMed] [Google Scholar]
- 9.Nelson R. Long work hours for nurses. AJN Am J Nurs. 2012;112:19. [DOI] [PubMed] [Google Scholar]
- 10.Stimpfel AW, Sloane DM, Aiken LH. The longer the shifts for hospital nurses, the higher the levels of burnout and patient dissatisfaction. Health Aff (Millwood). 2012;31:2501–2509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trinkoff AM, Johantgen M, Storr CL, et al. Nurses’ work schedule characteristics, nurse staffing, and patient mortality. Nurs Res. 2011;60:1–8 [DOI] [PubMed] [Google Scholar]
- 12.Geiger-Brown J, Rogers A, Trinkoff AM, et al. Sleep, sleepiness, fatigue, and performance of 12-hour-shift nurses. Chronobiol Int. 2012;29:211–219 [DOI] [PubMed] [Google Scholar]
- 13.Estabrooks CA, Cummings GG, Olivo SA, et al. Effects of shift length on quality of patient care and health provider outcomes: systematic review. Qual Saf Health Care. 2009;18:181–188 [DOI] [PubMed] [Google Scholar]
- 14.Stimpfel AW, Aiken LH. Hospital staff nurses’ shift length associated with safety and quality of care. J Nurs Care Qual. 2013;28:122–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stimpfel AW, Lake ET, Barton S, et al. How differing shift lengths relate to quality outcomes in pediatrics. J Nurs Adm. 2013;43:95–100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ogińska HCD, Estryn-Behar M, Pokorski J. NEXT-Study Group. Hasselnhorn HMTB, Müller H. Work schedules of nurses in Europe. Working Conditions and Intent to Leave the Profession Among Nursing Staff in Europe. 2003Stockholm, Sweden: National Institute for Working Life;82–87 [Google Scholar]
- 17.Todd C, Robinson G, Reid N. 12-hour shifts: job satisfaction of nurses. J Nurs Manag. 1993;1:215–220 [DOI] [PubMed] [Google Scholar]
- 18.Lee S, McCann D, Messenger JC. Working Time Around the World Trends in Working Hours, Laws and Policies in a Global Comparative Perspective Sangheon. 2007Abbingdon: Routledge [Google Scholar]
- 19.Bernreuter M, Sullivan M. Survey and critique of studies related to shift length variations in nursing from 1970 to 1993. Int J Nurs Stud. 1995;32:188–197 [DOI] [PubMed] [Google Scholar]
- 20.Patterson PD, Weaver MD, Hostler D, et al. The shift length, fatigue, and safety conundrum in EMS. Prehosp Emerg Care. 2012;16:572–576 [DOI] [PubMed] [Google Scholar]
- 21.Bae SH. Presence of nurse mandatory overtime regulations and nurse and patient outcomes. Nurs Econ. 2013;31:59–6889; quiz 69 [PubMed] [Google Scholar]
- 22.Olds DM, Clarke SP. The effect of work hours on adverse events and errors in health care. J Saf Res. 2010;41:153–162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sermeus W, Aiken LH, Van den Heede K, et al. Nurse forecasting in Europe (RN4CAST): rationale, design and methodology. BMC Nurs. 2011;10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aiken LH, Sermeus W, Van den Heede K, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012;344:e1717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bruyneel L, Heede KVd, Diya L, et al. Predictive validity of the International Hospital Outcomes Study Questionnaire: an RN4CAST Pilot Study. J Nurs Sch. 2009;41:202–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Squires A, Aiken LH, van den Heede K, et al. A systematic survey instrument translation process for multi-country, comparative health workforce studies. Int J Nurs Stud. 2013;50:264–273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McHugh MD, Stimpfel AW. Nurse reported quality of care: a measure of hospital quality. Res Nurs Health. 2012;35:566–575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schubert M, Glass TR, Clarke SP, et al. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care. 2008;20:227–237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McGraw KO, Wong S. Forming inferences about some intraclass correlation coefficients. Psychol Methods. 1996;1:30–46 [Google Scholar]
- 30.Nakagawa S, Schielzeth H. Repeatability for Gaussian and non-Gaussian data: a practical guide for biologists. Biol Rev Camb Philos Soc. 2010;85:935–956 [DOI] [PubMed] [Google Scholar]
- 31.Silber JH, Romano PS, Rosen AK, et al. Failure-to-rescue: comparing definitions to measure quality of care. Med Care. 2007;45:918–925 [DOI] [PubMed] [Google Scholar]
- 32.Ball JE, Murrells T, Rafferty AM, et al. ‘Care left undone’ during nursing shifts: associations with workload and perceived quality of care. BMJ Qual Saf. 2014;23:116–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saksvik IB, Bjorvatn B, Hetland H, et al. Individual differences in tolerance to shift work—a systematic review. Sleep Med Rev. 2011;15:221–235 [DOI] [PubMed] [Google Scholar]
- 34.Kock N.Kock N. Using WarpPLS in E-Collaboration Studies: Descriptive Statistics, Settings. Interdisciplinary Applications of Electronic Collaboration Approaches and Technologies. 2013Hershey PA: IGI Global;62–78 [Google Scholar]
- 35.R Development Core Team. R: A language and environment for statistical computing (Version 0.96.330). Vienna, Austria, R Foundation for Statistical Computing. 2013. Available at: http://www.R-project.org/
- 36.Bates D, Maechler M, Bolker B, et al. lme4: Linear mixed-effects models using S4 classes. R package version 0.999999-22013. 2011. http://CRAN.R-project.org/package=lme4.
- 37.Büscher A, SiVertsen B, White J. Nurses and midwives: a force for health. Survey on the situation of nursing and midwifery in the Member States of the European Region of the World Health Organization. WHO Regional Office for Europe, Copenhagen, Denmark. 2009 [Google Scholar]
- 38.The National Institute for Occupational Safety and Health. Work schedules: shift work and long work hours. 2013. Available at: http://www.cdc.gov/niosh/topics/workschedules/. Accessed May 07, 2013
- 39.Dean GE, Scott LD, Rogers AE. Infants at risk: when nurse fatigue jeopardizes quality care. Adv Neonatal Care. 2006;6:120–126 [DOI] [PubMed] [Google Scholar]
- 40.Surani S, Murphy J, Shah A. Sleepy nurses: are we willing to accept the challenge today? Nurs Admin Q. 2007;31:146–151 [DOI] [PubMed] [Google Scholar]
- 41.Rogers AE, Hwang W-T, Scott LD, et al. The working hours of hospital staff nurses and patient safety. Health Aff (Millwood). 2004;23:202–212 [DOI] [PubMed] [Google Scholar]
- 42.Kane RL, Shamliyan TA, Mueller C, et al. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007;45:1195–1204 [DOI] [PubMed] [Google Scholar]
- 43.Berney B, Needleman J, Kovner C. Factors influencing the use of registered nurse overtime in hospitals, 1995–2000. J Nurs Sch. 2005;37:165–172 [DOI] [PubMed] [Google Scholar]
- 44.Bae S-H, Brewer C. Mandatory overtime regulations and nurse overtime. Pol Polit Nurs Pract. 2010;11:99–107 [DOI] [PubMed] [Google Scholar]
- 45.Yu S, Kim TG. Evaluation of nurse staffing levels and outcomes under the government—recommended staffing levels in Korea. J Nurs Manag. 2013doi 10.1111/jonm.12155 [DOI] [PubMed] [Google Scholar]
- 46.Hayes LJ, O’Brien-Pallas L, Duffield C, et al. Nurse turnover: a literature review—an update. Int J Nurs Stud. 2012;49:887–905 [DOI] [PubMed] [Google Scholar]
- 47.Aiken L, Clarke S, Sloane D, et al. Effects of hospital care environment on patient mortality and nurse outcomes. J Nurs Admin. 2008;38:223–229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lobo VM, Fisher A, Ploeg J, et al. A concept analysis of nursing overtime. J Adv Nurs. 2013;69:2401–2412 [DOI] [PubMed] [Google Scholar]


