Abstract
Background & Objectives
Little is known about how parents think about neonatal intensive care unit (NICU) safety. Due to their physiologic immaturity and small size, infants in NICUs are especially vulnerable to injury from their medical care. Campaigns are underway to integrate patients and family members into patient safety. This study aimed to describe how parents of infants in the NICU conceptualize patient safety and what kinds of concerns they have about safety.
Methods
This mixed-methods study employed questionnaires, interviews, and observation with parents of infant patients in an academic medical centre NICU. Measures included parent stress, family-centredness, and types of safety concerns.
Results
46 parents completed questionnaires and 14 of these parents also participated in 10 interviews (including 4 couple interviews). Infants had a range of medical and surgical problems, including prematurity, congenital diaphragmatic hernia, and congenital cardiac disease. Parents were positive about their infants’ care and had low levels of concern about the safety of procedures. Parents reporting more stress had more concerns. We identified three overlapping domains in parent’s conceptualizations of safety in the NICU, including physical, developmental, and emotional safety. Parents demonstrated sophisticated understanding of how environmental, treatment, and personnel factors could potentially influence their infants’ developmental and emotional health.
Conclusions
Parents have safety concerns that cannot be addressed solely by reducing errors in the NICU. Parent engagement strategies that respect parents as partners in safety and address how clinical treatment articulates with physical, developmental, and emotional safety domains may result in safety improvements.
Keywords: patient safety, neonatal intensive care, parenting
INTRODUCTION
Available data suggest parents are concerned about safety [1, 2] and their role in decisions about their child’s care in the NICU.[3] Yet despite growing calls for patient and parent engagement [4, 5] relatively little is known about how NICU parents conceptualize patient safety. Identifying and preventing potential harm to patients is especially vital in neonatal intensive care units (NICUs) where fragile patients frequently suffer long-term consequences from potentially preventable adverse events.[6–8] Most NICU safety research has focused on classification of errors, testing different methods for identifying adverse events, and estimating the preventability of these events. Kugelman et al. [6] found 18% of infants experienced iatrogenic events and 83% of these events were deemed preventable, with 27% classified as error-related.
The adult and paediatric literature offer little guidance for incorporating parents into safety promotion efforts in the NICU context. If we are to design appropriate and effective interventions to support parents’ partnership in the safety team for their ill newborns,[2, 3, 9, 10] it is essential to understand their perspectives on what constitutes safety. The purpose of this study was to examine the perspectives of parents regarding patient safety in the NICU. We sought to explore how parents conceptualize safety in the NICU as a foundation for building parent-engaged safety interventions.
METHODS
This parallel convergent mixed-methods study used questionnaires, interviews, and field observations to explore parents’ perspectives on safety in the NICU. We designed the exploration for both breadth (questionnaires for all parents) and depth (interviews and observations with a subset of parents). We recruited English-speaking parents over 18 years of age with infants admitted to a single NICU at least 72 hours prior to approach. There were no other inclusion or exclusion criteria.
The study site was a regional tertiary academic medical centre NICU wherein all research recruitment was conducted by dedicated clinical research nurses to ensure that patients and families were not overburdened with requests for research participation. The research nurses screened all patients for parent eligibility and approached eligible parents who were present during research centre hours. The study site was a children’s hospital NICU with co-located obstetric services. The NICU had over 50 beds, admitted over 500 newborns annually and had approximately 250 staff. Data were collected between March and December 2012.
All enrolled participants were asked to complete a questionnaire containing measures of parent stress, parent assessment of unit family-centredness, and ratings of level of safety concerns about medical procedures. In addition, a subset of enrolled participants were purposively sampled for interviews and observations based on range of infant diagnoses and length of stay. Data were collected until we reached saturation and data redundancy. Participants received a $25.00 gift card for each study activity completed. The local Institutional Review Board approved the study and each participant gave signed informed consent.
Instruments
Parents reported on clinical characteristics of their infants, demographic information about themselves, NICU-related stress, [11, 12] and family-centred care [13] in an 84-item multiple choice and free-text response questionnaire. The questionnaire included an investigator-developed ‘Concerns Scale’ wherein parents reported their level of safety concern (‘not at all concerned’, ‘a little concerned’, ‘neutral’, ‘somewhat to ‘very concerned’ on a 1–5 scale) for 12 common NICU procedures or activities. Parents could elaborate on these or describe other concerns with free text. Internal consistency reliability for this scale was 0.90. Parents also responded with free text to the question “When you think about keeping your baby safe here in the hospital, what do you think about?”
A subset of parents participated in recorded interviews that were conducted in parents’ homes or in meeting rooms on the medical centre campus. Questions followed a guide (Table 1) but were adapted to follow participants’ concerns. Because our aim was to understand how parents conceptualize safety, our questions were designed to elicit their perspective and we did not provide a definition of safety. Interviews lasted 60–90 minutes. Observations lasting approximately two hours each involved sitting with parents in the NICU while they were at the bedside with their infants, focusing on the unit environment, unit activity, and parents’ safety-related actions and communications with health care professionals.[14] Informal observations of the NICU environment were ongoing throughout recruitment. Interviews and observations were conducted by the principal investigator (AL) or the graduate research assistant (CJ), neither of whom are NICU nurses. Staff members interacting with enrolled parent(s) during observations were informed of the study purpose. We took fieldnotes openly and transcribed them as soon as possible thereafter.
Table 1.
Interview Guide
|
Data Analysis
Questionnaires and interview/field data were analysed separately and then compared to determine how they informed, expanded on, or challenged each other to form an integrated understanding of the data [15, 16]. We used descriptive statistics and correlation analysis to characterize demographic and numeric questionnaire responses. We analysed qualitative data using thematic analysis [17] for free text responses and a constructivist grounded theory approach for interview and observation data with the aim of developing a theoretical explanation of parents’ concerns and conceptualizations of NICU safety.
Grounded theory is a systematic method for studying human experience, social interaction, and social process.[18–20] Data analysis occurs iteratively and simultaneously with data collection. Researchers engage in repeated close readings of interview transcripts and field notes, searching for units of meaning or “codes” that describe the underlying social processes and interactions, constantly comparing the data both within and between interviews or observations. Codes are organized into categories that are both highly represented in the data and account for the greatest variation in the data.[18–21] We developed open, focused, and theoretical codes to describe aspects (dimensions) of participants’ experiences, which we further developed and differentiated through theoretical sampling (seeking new data or re-examining existing data to answer questions raised by the analysis).[21, 22]
Rigor was maintained through reflexivity, attention to interview and transcription quality, member reflection, and systematic analysis.[23] Rigor was enhanced by the use of multiple data sources, analysts, and analytic methods. Investigators have clinical backgrounds in obstetric nursing (AL, KW), midwifery (CJ), and NICU and paediatrics (KF & LF), thus we considered our effect as clinician investigators on all aspects of the study. Participants were informed the data collectors (AL & CJ) were academic research nurses. At consent and at interviews we assured participants that we would not discuss their comments with hospital staff. Interview participants almost universally began by emphasizing how positive they felt about their infants’ care and raised any ‘negative’ observations only as we demonstrated non-judgemental interest in their views. We engaged in ongoing validation of interpretations with participants to avoid making assumptions about meaning.[24–26] We used memoing and group discussion to uncover analytic assumptions related to our nursing experience.
RESULTS
Fifty-five parents enrolled in the study: 46 completed questionnaires (83%) and 9 did not return questionnaires or complete any study activities. Fourteen of the 46 parents were interviewed (representing 12 infants) and three were observed (representing 5 infants). Six participants had individual interviews; eight requested to be interviewed as couples. Participant characteristics are displayed in Table 2. Three infants were readmitted before or during the period of participation in the study. Three infants sustained moderate to severe injuries during their hospitalization. One injury was due to a known but potentially preventable risk. It was unclear whether or not the two remaining injuries were iatrogenic.
Table 2.
Characteristics of Participants
| Parent Characteristics | 46 |
|---|---|
| Gender | 35 (78% ) Female |
| Age (years); median (range) | 35.0 (19–42) |
| Race | |
| White | 34 (74%) |
| Asian | 2 (4%) |
| Black | 1 (2%) |
| Native Hawaiian/Pacific Islander | 1 (2%) |
| Not reported | 8 (18%) |
| Hispanic Ethnicity | 17(37%) |
| Education | |
| High school | 7 (15%) |
| College | 30 (65%) |
| Graduate school | 9 (20%) |
| Occupation | |
| Service/Technical | 25 (54%) |
| Professional/Manager | 10 (22%) |
| Homemaker | 6 (13%) |
| Not given | 5 (11%) |
| Marital Status | |
| Single | 1 (2%) |
| Partnered | 15 (33%) |
| Married | 30 (65%) |
| First-time parent | 28 (61%) |
| Parent stressor scales scores; mean (SD) (1= not at all stressful; 5= extremely stressful) | 2.6 (± 0.62) |
| Family-Centred Care; mean (SD) (1=strongly disagree; 5=strongly agree) | |
| Environment | 3.7 (± 0.7) |
| Caring for My Child | 3.8 (± 0.8) |
| Discharge readiness | 3.3 (± 1.8) |
| Relationship with Staff | 4.2 (± 0.7) |
|
| |
|
Characteristics of the parents’ hospitalized infants
| |
| Inborn | 34 (74%) |
| Expected Admission | 28 (62%) |
| Diagnosis | |
| Prematurity | 16 (35%) |
| Congenital diaphragmatic hernia | 8 (17%) |
| Cardiac defect | 6 (13%) |
| Gestational age at birth (weeks); median (range) | 36.9 (27–41) |
| Length of stay at enrolment (days); median (range) | 28.0 (6–84) |
Participants demonstrated moderate NICU-related stress scores and generally agreed that the study NICU was family-centred. Mean ratings were highest for ‘relationship with staff’ and lowest for ‘readiness for discharge.’ Participants had low levels of safety concern about procedures (Table 3), and the number and level of concerns was correlated with NICU-related stress (Spearman’s rho=.337; p=.022) but not with family-centred care ratings.
Table 3. Self-reported degree of concern regarding safety of procedures Question.
Below is a list of common procedures, treatments, and equipment in the NICU (ICN). Please rate your level of concern about their safety by filling in the circle in the column that matches your feelings. Response options: Not at all Concerned, A little concerned, Neutral, Moderately concerned, Very concerned
| Procedure | % Moderately or Very Concerned N (%) |
|---|---|
| IVs | 18 (39) |
| Medications | 13 (28) |
| Feeding | 12 (26) |
| Lumbar puncture | 10 (22) |
| Blood samples | 8 (17) |
| Tape or adhesives | 8 (17) |
| Ventilators | 8 (17) |
| Skin care | 7 (15) |
| Tubing | 7 (15) |
| CPAP | 6 (13) |
| Monitoring | 4 (9) |
| Incubator | 2 (4) |
IV; intravenous line
CPAP; continuous positive airway pressure
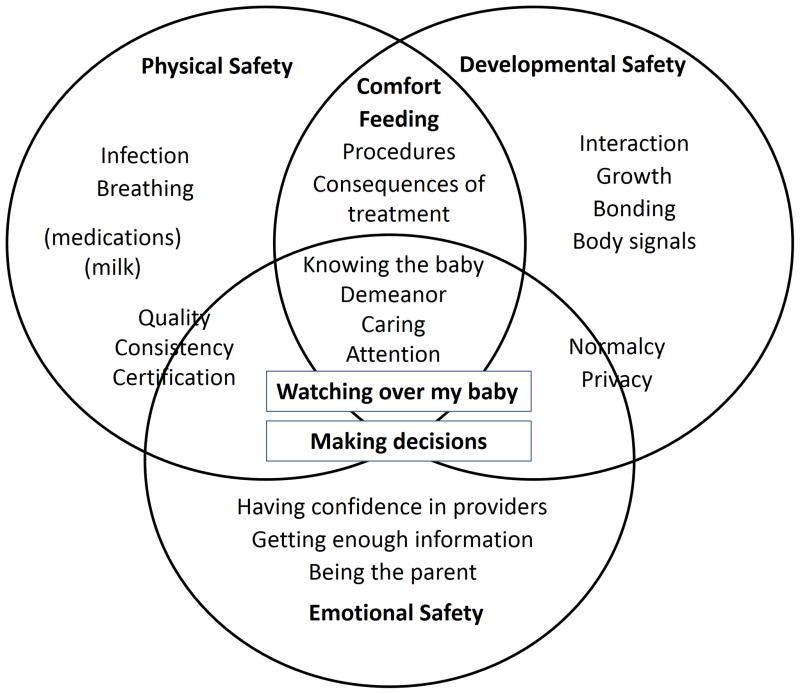
Parents viewed safety as a combination of the clinical teams’ actions and parents’ contributions to monitoring and improving their baby’s condition across three dimensions: physical, developmental, and emotional (Figure 1).
I also think what parents can do for preemies is as important as what the hospital can do, and what the hospital can do is as important as what the parents can do. It needs both, and of course a hospital keeps them alive in ways that parents might not be able to, but I think parents get them to develop in ways that the hospital wouldn’t be able to. [Interview]
Figure 1.
The interplay of physical, developmental, and emotional safety from the parents’ perspective
Physical Safety
Parents’ concerns about physical safety included safe practices for medication and breast milk administration, infection control, apnoeic episodes or other breathing issues, the infant’s physical comfort, and the potential consequences of treatments. Regarding medication and breast milk, parents identified the importance of avoiding administration mistakes. Regarding infection control, parents observed that visitors and staff did not always follow good infection control practices. Parents were keenly aware of the need to shield their babies from infection.
I know other siblings do come and I think that’s great, but the screening mechanism doesn’t seem like it’s up to the level of scrutiny that you would expect because a lot of kids that we saw in there both times, you know, just green dripping through their nose and sneezing and coughing…that would make me a little uncomfortable. [Interview]
Parents’ concerns about their infants’ respiratory status were threaded throughout many of the interviews, especially in premature infants and infants with congenital diaphragmatic hernia (CDH).
Parents expected clinicians to have a high level of technical competence and generally found this to be true. Parents identified the quality and consistency of nursing care as central to physical safety, as they were quite aware that the nurses were providing the moment-to-moment surveillance their infants required.
[W]hen Baby S got her staph infection, they caught it before she was even running a temp for it because she started having more Bradys [bradycardias] and so they immediately took blood and found out that she had an infection starting… so that I think is a huge part with keeping them safe in the NICU is that watching for those little signs and the nurses are really good. [Interview]
Parents also expressed concern for pain, pain management, and gentle handling of their infants in their discussions of safety.
Developmental Safety
Infants’ developmental needs were a central focus of parents’ discussions about safety. Parents worried about how specific treatments or consequences of treatments might affect their infants’ development. Parents identified interaction, growth, bonding, understanding the babies’ signals, and providing consistency as important factors in what we are calling “developmental safety.”
You know, he’s a baby. He needs to learn to suck, swallow, and breathe all at the same time. So if everyone is doing it differently, then how is he supposed to learn how to do that? [Interview]
[T]here’s a lot of noise in the NICU … The monitors make noise; he was near a laundry basket one day and people kept banging that laundry basket down … So I just moved it. I moved it near where there weren’t any babies because I don’t want any baby’s development to be compromised. [Interview]
Parents found that the lack of privacy in the open wards and the lack of normalcy of their situations interfered with their ability to establish and maintain the level and kind of interactions they wished to have with their infants. Parents spoke about the impact of the NICU environment on the bonding process between themselves and their infants.
[W]hen he was a newborn, of course we were worried and we were worried about the bonding and all of that….But now he’s a little person and he’s engaged and he needs attention in a different way too. And when- after his surgery, he had a lot of pain episodes and sometimes he just needed - aside from morphine or whatever - he just needed someone to hold him until he calmed down. [Interview]
Several parents had infants who were “growing up” in the NICU, having been hospitalized for several months, or readmitted at several months of age. These parents were conscious of their infants’ increasing need for meaningful interaction with them and with staff.
Emotional Safety
Emotional safety was relational, and had both parental and infant components. For parents, emotional safety comprised having confidence in their infants’ medical and nursing providers, getting enough information, and having opportunities to “be the parent” for their infants. If relationships with providers were difficult, access to information limited, or parents felt cut off from parenting opportunities, their sense of equilibrium was challenged and they became worried about their infants’ care. Parents were reassured by observing providers making a human connection with their infants, and observing these relationships increased their confidence in the safety of their baby’s care:
[T]he safety of your child, that’s obviously one of the first things you think about and, you know, their care.…with some of the nurses, you can just tell that he’s being taken care of. Like just by the expressions on [Baby]. So that’s definitely one of my biggest things. It’s just so reassuring going home at night and knowing that my child’s in safe hands. [Interview]
Furthermore, parents expressed certainty that the infants were aware of and responsive to the emotion tone of those around them, and that part of safety was that their infants felt loved and did not feel stress transmitted from others.
The fact that we, the parents cannot directly care for the baby in the NICU, it is important that the baby feels no stress and the nurse/doctors being aware of his mannerism/behaviour [questionnaire]
I think [love has to do with safety] - It’s not just to feel loved but it’s also something that a baby needs, I think so. But it’s not that a doctor can prescribe like 10 minutes of love, no? Or like 15 minutes to be held. It’s not measurable. [Interview]
Safety at Intersecting Domains
Parents’ concerns often lay at the intersections of physical, developmental, and emotional safety. Comfort care, procedures, and treatments were described as having implications that were both physical and developmental. For example, many of the parents’ developmental safety concerns about feeding practice in the NICU were also related to physical safety. Parents were particularly troubled by inconsistencies in feeding practices among nurses, and by instances where the nurses seemed too busy to either feed their infants at the designated time, or give their infants the pacing needed to complete nipple feeds. Some parents of younger infants or infants with CDH observed their infants tolerated feedings better when given by pump rather than gravity, preferred this, and saw it as a safety concern related to the infant’s physiologic status:
Mother: Don’t drop feed his food….So whenever he has the drop feed, like when they hang the syringe and it just kind of goes in, he acts like it goes way too fast and he gets sick off it. … And it put him back, literally because he was so upset from that. Like his stomach- it was just way too fast. I mean, so for that night, the night and the day after he was- Father: He was down for like a day. [Interview]
Also, this whole feeding thing - again, from monitoring the situation, obviously we’re not the experts here. But we feel that when they increase the feeding to the level they did recently and the reactions they’re having with all these desats [oxygen desaturations] and everything else, and the concentration of the formula with the- whatever shake they are making nowadays. It’s causing issues and- between us we talk about it and between us and other couples, we talk about it. [Interview]
Other parents saw oral feeding as a clear developmental need and felt that pump feeding was not desirable. These parents worried about staff not being able to give the infant the chance to take the feeding orally with resulting over-reliance on pump feeding. Some parents were also concerned about timed versus on-demand feeding. On-demand feeding might not happen frequently enough if the nurses were busy; in contrast a strict feeding schedule was viewed as somewhat physiologically unnatural, leaving the infant “full all the time.”
And that milk is just yucky for him, let’s say the feed is the 9:00 feed, so feeding around 9:30 to burping, wait for it, wait for him to settle a little bit and then feed him some more so he could take, you know, it’s not just feeding the whole bottle at once or if he doesn’t eat it well, we’d put it in the pump. We’d tell them, “Hey, just you’ve got to give him time.” He takes his time, give him the bottle…whatever he doesn’t take just wait a couple of minutes, and then feed him again. And I understand sometimes they’re busy and you know they can’t do that. [Interview]
[T]hey would tell me that I can like feed him with the pump, like all night. But to me it doesn’t look very physiological and I’m worried that maybe his brain and all that is going to…I mean I tried to find out articles, but they just say that they compared the weight gain, but they don’t compare if they develop or like for the brain. So I think that area needs like a little research. [Interview]
All three domains of safety intersected in the central processes of watching over my baby and making decisions. For the most part, parents were confident that the staff, and in particular nurses, were watching over their babies effectively. This was demonstrated to parents by the staff’s knowledge of their infants, expressions of caring, attention, and demeanour, and observations of consistency in practices and skills. However, parents identified mistakes in care including incorrect documentation of birth weight, failure to recognize a respiratory emergency due to alarms being turned down, missed medical orders, and orders for blood work entered in the wrong infant’s medical record.
The mother is telling the physician about a problem that occurred last night: another child’s lab orders were entered on her baby’s record. Apparently these labs were not drawn, because the mother questioned the nurse about them, but she is a little distressed about the mistake. The physician agrees with her, yes, we need to really look at this and make sure we address the problem. [Observation]
Parents also had concerns about the skill level of some nursing staff, as well as frequent rotation of nurses and physicians and inconsistencies in nursing practice that might lead to diminished capacity for knowing their infant as an individual. Parents indicated that not “knowing the baby” could interfere with clinicians’ ability to detect subtle changes in condition or provide developmentally appropriate comfort for their child. In these situations, parents tried to compensate for perceived staff deficiencies by increasing their own vigilance at the bedside when possible.
The first thing or the thing that makes the biggest impact [on safety] is the nurse, which nurse is taking care of them. I have seen the majority are very good nurses, but there are some that are not. And when you’re here during that day and that particular nurse that you believe, is not very good is here during the day, you can sort of control a little bit more because you’re watching over your baby. But when it’s the night shift and you have to go home you’re not at peace, you know. It’s very difficult. [Interview]
Some parents were distressed by decision-making processes in the NICU, and felt that they often were not consulted about or informed of procedures performed on their infants. Most of these concerns had to do with physical wellbeing and safety, such as type of medication, fortification of feeding, changes is respiratory support, or whether to do surgery.
I worry about not being involved in my child’s care at all. Our son had a bladder infection and was 5 days into taking antibiotics before we even knew about the infection. [He] was on his second day of blood transfusions before we knew. He developed an arrhythmia and no one talked to us about it until the next day.…. We are in contact at least once a day - for us to go days without knowing about a change in his condition is just poor communication. [Questionnaire]
Distress also arose for some parents when staff made seemingly minor decisions parents viewed as rightfully their own. This was particularly painful for a couple who felt they were thereby denied an important developmental interaction with their infant.
Well, a nurse decided to bottle feed him in the middle of the night. And, we were still working on breastfeeding. That’s kind of a big decision to make…. if you had your baby at home, you wouldn’t even have to think about it. But when someone else is caring for your baby when you’re not there, it’s like you don’t really know what they’re deciding to do. So, when we found out that he had been bottle fed before we ever got to bottle feed him, it was really upsetting. Because, you know, that’s - it shouldn’t happen like that. [Interview]
However, parent perspectives varied with regard to making decisions about their infants’ care. While one couple felt they were never consulted unless required to sign a formal consent, other parents felt very included as team members. Some parents wanted as much control as possible, while others felt ill-equipped to participate in decision-making and were usually happy to defer to physician and nurse expertise.
DISCUSSION
This is the first study to our knowledge specifically exploring patient safety from the perspective of NICU parents. Parents in our study thought about safety in ways that extend beyond traditional definitions of freedom from medical harm and physical injury. Parents demonstrated sophisticated understanding of some of their infants’ developmental needs and the potential for a range of environmental, treatment, and personnel factors to influence their child’s developmental and emotional health. This breadth of NICU parents’ concerns is consistent with Fagerhaugh et al.’s descriptions of the breadth of “all of the work” or trajectory of being a patient, including the importance of composure, trust, and identity work to adult patients’ perceptions of safety. [27] Our findings suggest parents have concerns that cannot be addressed by focusing primarily on errors in the NICU. Rather, parent engagement strategies that address the articulation of clinical treatment with physical, developmental, and emotional safety domains in a manner that respects parents as partners in safety may be more likely to be successful and satisfying to parents and clinicians alike.
Similar to adult oncology patients, [28] parents had a high degree of confidence in their infants’ providers and a low level of procedural concern. Parent stress levels were similar to other studies with NICU parents,[12, 29] and parents had a generally positive assessment of the NICU’s family-centredness. The modest correlation between parents’ stress and procedural concern but not with perceptions of family-centredness requires further study, as does the range of perspectives on what constitutes desirable involvement in decision-making. Parents’ concerns about continuity of nursing care, nursing practices, communication with physicians, and the need to ‘watch over’ their infants are also consistent with studies describing experiences of parenting in the NICU and some of the challenges to involving parents in care.[30, 31] This study generates novel insight about developmental and emotional aspects of parents’ understandings of what it means for their infant to be safe in the NICU.
Limitations of the study include a small sample of English-speaking parents drawn from a single NICU. Parents with constraints limiting their time in the unit were less accessible for recruitment and may have been less likely to participate. Non-participants may have different perspectives on NICU patient safety. However, the consistency of our findings with other studies of parent experience suggests some transferability. The recruitment of parents in the NICU while their infants are hospitalized heightens concern for social desirability bias, as parents may fear offering criticism could negatively influence their infants’ care. Although some interview participants seemed to view us as ‘part of’ the hospital, those who did so most openly were also the most open with criticisms of care. We also frequently received both positive comments about care and suggestions for improvement on the same questionnaires.
While the number of parents interviewed was relatively small, we shared our developing conceptual model with several parents near the end of recruitment and they confirmed the model reflected their experience. Many parents indicated willingness to be observed, yet we found it unexpectedly difficult to schedule observation sessions due to the unpredictability of parents’ schedules and infant condition on a given day. Observations that we were able to conduct yielded rich information about the environment, real-time capture of discussion of medical errors, and nurse-parent and physician-parent communication. For future studies more traditional embedded ethnographic observation would be an important complement to focused observations with specific parents.
Greater understanding of parents’ safety concerns may lead to new opportunities to improve safety for vulnerable NICU infants. Further research is needed to explore the views of parents, in particular parents who are not able to visit frequently and non-English speaking parents. Likewise, future studies should concurrently explore the views of clinicians and parents and examine areas of concordance, dissonance, and priority. Parents could then be engaged in meaningful partnerships to design safety interventions that promote early problem recognition, error trapping, and successful rescue processes in neonatal care, without unduly adding to the burden families already experience.
Clinically, our findings reinforce the idea that consistency in providers and practices can contribute to safety, and suggest that parents make careful observations and have opinions about NICU safety. Parents should be invited and encouraged to share observations and concerns with their baby’s healthcare team. The new insights into parents’ perspectives on NICU patient safety suggest parents are an untapped resource and are potentially ready, willing, and able to be active partners in improving NICU patient safety.
Acknowledgments
We are grateful to participating parents for their willingness to share their time with the research team. We also thank the research nurses in the host NICU for helping us with recruiting.
FUNDING
This project was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through UCSF-CTSI Grant Number KL2TR000143 and by the Association of Women’s Health, Obstetric, and Neonatal Nurses/March of Dimes Foundation Margaret Comerford Freda Research Grant. The study was also supported in part by a training grant (#T32 NR07088) from the National Institutes of Health, National Institute of Nursing Research.
Footnotes
COMPETING INTERESTS
None to report.
The contents of the publication are solely the responsibility of the authors and do not necessarily represent the official views of the NIH, AWHONN, or the March of Dimes.
References
- 1.Rathert C, Brandt J, Williams ES. Putting the ‘patient’ in patient safety: a qualitative study of consumer experiences. Health Expect. 2011 doi: 10.1111/j.1369-7625.2011.00685.x. Epub 2011/06/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suresh GK, Edwards WH. Central Line-Associated Bloodstream Infections in Neonatal Intesive Care: Changing the Mental Model from Inevitability to Preventability. Am J Perinatol. 2011 doi: 10.1055/s-0031-1286182. Epub 2011/09/01. [DOI] [PubMed] [Google Scholar]
- 3.Conway JB, Celenza J, Abraham MR. Advancing Patient- and Family-Centered Newborn Intensive Care. In: Horbar JD, Leahy K, Handyside J, editors. NICQ 2007: Improvement in Action. Burlington, VT: Vermont Oxford Network; 2010. [Google Scholar]
- 4.The Joint Commission. Facts about Speak Up Intitiatives 2011. 2011 Jul; Available from: http://www.jointcommission.org/assets/1/18/Speak_Up.pdf.
- 5.Maurer M, Dardess P, Carman K, et al. Prepared by American Institutes for Research under contract HHSA 290-200-600019. Vol. 2012. Rockville, MD: Agency for Health Care Research and Quality; May, 2012. Guide to Patient and Family Engagement: Environmental Scan Report. Report No.: Contract No.: AHRQ Publication No. 12-0042-EF. [Google Scholar]
- 6.Kugelman A, Inbar-Sanado E, Shinwell ES, et al. Iatrogenesis in neonatal intensive care units: observational and interventional, prospective, multicenter study. Pediatrics. 2008;122(3):550–5. doi: 10.1542/peds.2007-2729. Epub 2008/09/03. [DOI] [PubMed] [Google Scholar]
- 7.Sharek PJ, Horbar JD, Mason W, et al. Adverse events in the neonatal intensive care unit: development, testing, and findings of an NICU-focused trigger tool to identify harm in North American NICUs. Pediatrics. 2006;118(4):1332–40. doi: 10.1542/peds.2006-0565. Epub 2006/10/04. [DOI] [PubMed] [Google Scholar]
- 8.Raju TN, Suresh G, Higgins RD. Patient safety in the context of neonatal intensive care: research and educational opportunities. Pediatr Res. 2011;70(1):109–15. doi: 10.1038/pr.2011.334. Epub 2011/03/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edwards WH. Patient safety in the neonatal intensive care unit. Clin Perinatol. 2005;32(1):97–106. vi. doi: 10.1016/j.clp.2004.11.009. Epub 2005/03/22. [DOI] [PubMed] [Google Scholar]
- 10.Schwappach DL. Review: engaging patients as vigilant partners in safety: a systematic review. Med Care Res Rev. 2010;67(2):119–48. doi: 10.1177/1077558709342254. Epub 2009/08/13. [DOI] [PubMed] [Google Scholar]
- 11.Franck LS, Cox S, Allen A, et al. Measuring neonatal intensive care unit-related parental stress. J Adv Nurs. 2005;49(6):608–15. doi: 10.1111/j.1365-2648.2004.03336.x. Epub 2005/03/02. [DOI] [PubMed] [Google Scholar]
- 12.Franck LS, McQuillan A, Wray J, et al. Parent stress levels during children’s hospital recovery after congenital heart surgery. Pediatr Cardiol. 2010;31(7):961–8. doi: 10.1007/s00246-010-9726-5. Epub 2010/05/25. [DOI] [PubMed] [Google Scholar]
- 13.Bruns DA, Klein S. An evaluation of family-centered care in a Level III NICU. Infants Young Child. 2005;18(3):222–33. [Google Scholar]
- 14.Schatzman L, Strauss A. Field Research: Strategies for a Natural Sociology. Prentice Hall; 1972. [Google Scholar]
- 15.Bazeley P. Analysing Mixed Methods Data. In: Andrew S, Halcomb EJ, editors. Mixed Methods Research for Nursing and the Health Sciences. Ames, Iowa: Wiley-Blackwell; 2009. pp. 84–118. [Google Scholar]
- 16.Creswell JW, Plano Clark VL. Designing and Conducting Mixed Methods Research. Thousand Oaks, CA: Sage; 2011. [Google Scholar]
- 17.Braun VB, Clark V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. [Google Scholar]
- 18.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Hawthorne, NY: Aldine De Gruyter; 1967. [Google Scholar]
- 19.Strauss AL. Qualitative Analysis for Social Scientists. Cambridge: Cambridge University Press; 1987. [Google Scholar]
- 20.Schatzman L. Dimensional analysis: notes on an alternative approach to the grounding of theory in qualitative research. In: Maines DR, editor. Social Organization and Social Process: Essays in Honor of Anselm Strauss. New York: Aldine de Gruyter; 1991. pp. 303–14. [Google Scholar]
- 21.Kools S, McCarthy M, Durham R, et al. Dimensional Analysis: Broadening the Conception of Grounded Theory. Qual Health Res. 1996;6:312–30. [Google Scholar]
- 22.Coyne IT. Sampling in qualitative research. Purposeful and theoretical sampling; merging or clear boundaries? J Adv Nurs. 1997;26(3):623–30. doi: 10.1046/j.1365-2648.1997.t01-25-00999.x. Epub 1997/09/26. [DOI] [PubMed] [Google Scholar]
- 23.Tracy SJ. Qualitative Quality: Eight “Big-Tent” Criteria for Excellent Qualitative Research. Qual Inq. 2010;16(10):837–51. [Google Scholar]
- 24.Lyndon A. Social and environmental conditions creating fluctuating agency for safety in two urban academic birth centers. J Obstet Gynecol Neonatal Nurs. 2008;37(1):13–23. doi: 10.1111/j.1552-6909.2007.00204.x. Epub 2008/01/30. [DOI] [PubMed] [Google Scholar]
- 25.Angen MJ. Evaluating interpretive inquiry: Reviewing the validity debate and opening the dialogue. Qual Health Res. 2002;10:378–93. doi: 10.1177/104973230001000308. [DOI] [PubMed] [Google Scholar]
- 26.Giddings LS, Grant BM. From Rigour to Trustworthiness: Validating Mixed Methods. In: Andrew S, Halcomb EJ, editors. Mixed Methods Research for Nursing and the Health Sciences. Ames, Iowa: Wiley-Blackwell; 2009. pp. 119–34. [Google Scholar]
- 27.Fagerhaugh SY, Strauss A, Suczeck B, et al. Hazards in Hospital Care: Ensuring Patient Safety. San Francisco: Jossey-Bass; 1987. [Google Scholar]
- 28.Schwappach DL, Wernli M. Am I (un)safe here? Chemotherapy patients’ perspectives towards engaging in their safety. Qual Saf Health Care. 2010;19(5):e9. doi: 10.1136/qshc.2009.033118. Epub 2010/04/30. [DOI] [PubMed] [Google Scholar]
- 29.Franck LS, Cox S, Allen A, et al. Parental concern and distress about infant pain. Arch Dis Child Fetal Neonatal Ed. 2004;89(1):F71–5. doi: 10.1136/fn.89.1.F71. Epub 2004/01/09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hurst I. Vigilant watching over: mothers’ actions to safeguard their premature babies in the newborn intensive care nursery. J Perinat Neonatal Nurs. 2001;15(3):39–57. doi: 10.1097/00005237-200112000-00005. Epub 2002/01/12. [DOI] [PubMed] [Google Scholar]
- 31.Skene C, Franck L, Curtis P, et al. Parental involvement in neonatal comfort care. J Obstet Gynecol Neonatal Nurs. 2012;41(6):786–97. doi: 10.1111/j.1552-6909.2012.01393.x. Epub 2012/07/14. [DOI] [PubMed] [Google Scholar]