Abstract
Background
There is increasing interest in the role of brain-derived neurotrophic factor (BDNF) in the onset and course of schizophrenia, but there are conflicting reports about serum levels of BDNF in patients with schizophrenia.
Aim
Conduct a meta-analysis combining studies from China and other countries that have evaluated the relationship of serum BDNF levels to schizophrenia.
Method
We used Cochrane methodology and RevMan 5.1 software to identify and pool the results of studies. Electronic searches of western and Chinese registries and follow-up assessment of references located 268 potential articles. Twenty-five articles (20 in English and 5 in Chinese) published before December 2011 that used case-control methods, included patients with schizophrenia who had no concurrent disorders, and used ELISA technology to assess serum BDNF were included in the analysis. The main outcome was the pooled standardized mean difference (SMD) between cases and controls. The quality of the studies was independently assessed by two raters using the GRADE system. The heterogeneity, sensitivity and potential publication bias of the studies was evaluated using RevMan.
Results
The pooled sample included 1663 patients with schizophrenia and 1355 controls. Fifteen of the included studies were rated as ‘poor quality’ and 10 were rated as ‘very poor quality’. The results of the studies were quite heterogenous (I2=95%) but subgroup analyses found that the heterogeneity was not related to country of origin, sample size, age, gender, prior use of antipsychotic medication, or study quality. The pooled SMD (computed using a random-effect model because of study heterogeneity) was -0.74 (95% CI, -0.99∼-0.50; Z=5.99, p<0.001). Sensitivity analysis found that the result was stable and there was no evidence of publication bias.
Conclusion
Despite the robust statistical findings of lower serum BDNF in patients with schizophrenia than in controls, given the low quality of the available studies and the substantial heterogeneity between studies, the evidence of lower serum BDNF in patients with schizophrenia must be considered ‘weak’. The potential use of serum BDNF as a biomarker for schizophrenia must wait until higher-quality prospective studies that follow patients over time and that use uniform selection and monitoring procedures confirm these preliminary results.
Abstract
背景
脑源性神经营养因子(brain-derived neurotrophic factor, BDNF)在精神分裂症的发生和病程演变过程中所起的作用受到了越来越广泛的关注,但有关精神分裂症与外周血清BDNF水平关系的研究结果不尽一致。
目的
综合国内外研究,系统评价精神分裂症患者外周血清BDNF水平的特点。
方法
我们采用Cochrane系统综述方法和RevMan 5.1软件筛选研究并提取数据。通过国内外电子检索系统的检索并对获得文献的参考文献进行追溯评估,共检出268篇相关文献。其中25篇(20篇英文,5篇中文)被纳入分析,它们为2011年12月底以前公开发表的病例对照研究,研究对象为不伴有其他疾病的精神分裂症患者,采用酶联免疫吸附法检测BDNF的血清水平。系统综述的主要结局指标是病例组与对照组间合并的标准化均数差值(standardized mean difference, SMD)。由两位评价者根据GRADE系统的方法独立评估纳入研究的质量。采用RevMan 5.1软件对研究的异质性、敏感性和可能的发表性偏倚进行检验。
结果
累计1663例精神分裂症患者, 1355名对照纳入Meta分析。15项被评估为低质量研究,10项为极低质量研究。研究结果存在高度的异质性(I2=89%),但亚组分析结果表明,异质性与人种、样本量 、年龄、性别、入组前是否服用抗精神病药物以及研究质量等因素不存在相关性。由于研究间异质性,采用随机效应模型计算合并SMD,结果为-0.74(95% CI, -0.99~-0.50; Z=5.99,p<0.001)。敏感性分析表明结果稳定性较好。无发表偏倚的证据。
结论
尽管统计结果强有力地表明精神分裂症患者外周血BDNF水平低于对照人群,但由于现有研究的质量较低以及各研究之间的结果存在明显的异质性,精神分裂症患者外周血BDNF浓度低的证据应属较“弱”。今后需要开展高质量的前瞻性研究,对患者进行长期随访,并使用统一的入组标准和监测程序,如最终能证实这些初步结果,血清BDNF才有可能用作精神分裂症的生物学指标。
1. Introduction
Schizophrenia is a common form of severe mental illness with a lifetime prevalence of 1% in the general population.[1] The cause of this disabling disorder remains unclear, but a growing body of evidence has focused on the role of neurodevelopmental processes.[2] One marker of neurodevelopmental processes is the activity of the brain-derived neurotrophic factor (BDNF), a key member of the family of neurotrophic factors that play important roles in the growth, survival, differentiation and repair of neurons.[3] Many studies find that patients with schizophrenia have lower levels of BDNF and of BDNF mRNA in their brains compared with normal controls.[4]–[6] Studies using animal models of schizophrenia have also found lower levels of BDNF mRNA in the brains of mice that have been treated to mimic schizophrenia than in the brains of control mice.[7]
BDNF in peripheral blood is produced in the central nervous system (CNS), so changes in BDNF levels in the peripheral blood are considered a reasonable proxy measure of BDNF changes in the CNS.[8] This indirect measure of BDNF activity in the CNS is much easier to perform than direct assessment of BDNF in the CNS so it is a potential biomarker that could be used in the diagnosis and monitoring of treatment for schizophrenia. However, studies about BDNF levels in the peripheral blood of patients with schizophrenia have been inconsistent: most report lower serum BDNF levels compared with controls, [9]–[27] but some find no difference between patients and controls[28]–[32] and a few studies report higher levels of serum BDNF in patients than in controls.[33]
The current paper reports on a systematic review of quantitative studies from China and elsewhere about the relationship of serum BDNF levels to schizophrenia.
2. Methods
2.1. Study ascertainment
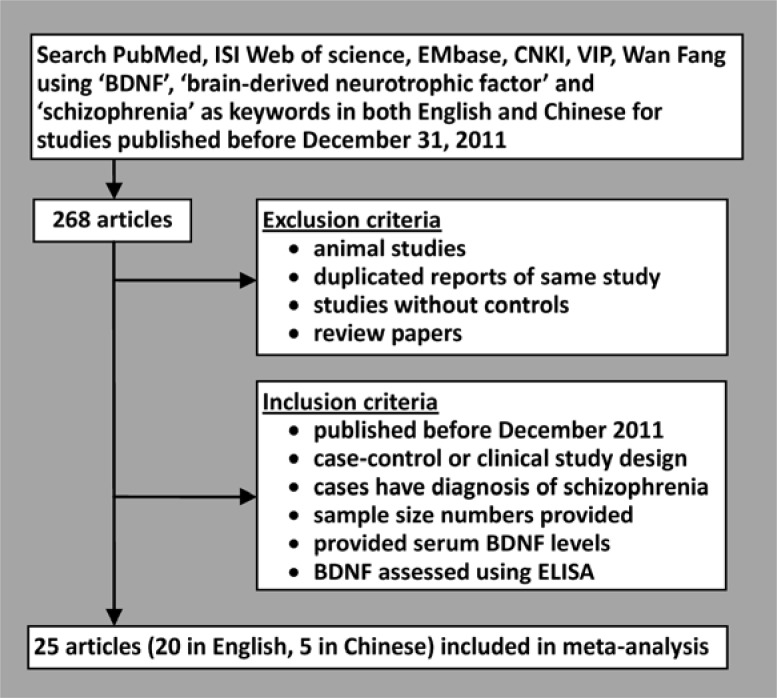
The results of the search strategy are shown in Figure 1. The following databases were used to identify potential studies for the meta-analysis: PubMed, ISI Web of science, EMbase, Chinese National Knowledge Infrastructure (CNKI), Chinese Science and Technology Full-text Database (VIP) and WanFang Data. The search strategies combined free-text searching and keyword searching. The keywords used in the search included English and Chinese versions of ‘schizophrenia,’ ‘brain-derived neurotrophic factor’ and ‘BDNF’. All references of identified articles were also reviewed.
Figure 1. Identification of articles for inclusion.
2.2. Assessment of included studies
All identified articles were independently reviewed by two evaluators (the first two authors) using the following inclusion criteria: a) the article was published in a publicly available journal prior to 31 December, 2011; b) the article provides original data on the sample size and on serum BDNF levels; c) the patient group in the study met diagnostic criteria for schizophrenia (specified by any diagnostic system) and excluded those with concurrent neurological illnesses, substance abuse, or psychotic symptoms secondary to a general medical condition; d) the study used Enzyme-linked Immunosorbent Assay (ELISA) to test the serum BDNF levels; and e) the study used a case-control or clinical trial study design.
The following types of articles were excluded: a) papers about animal studies; b) duplicate reports of previously published data sets; c) papers on studies without a control group; d) papers about genetic polymorphism of BNDF; and e) reviews.
2.3. Quality assessment
The quality of the included studies was independently assessed and cross-checked by the two evaluators using the criteria for evaluating observational studies recommended in the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) [34], [35] statement, as well as the Grading of Recommendations Assessment, Development and Evaluation (GRADE).[36] The quality of evidence was classified A to D as follows.
High quality: Both reviewers were very confident that the actual effect size is close to the estimated effect size.
Medium quality: Reviewers' confidence in the estimated effect size is fair; the actual effect size is probably close to the estimated effect size, but it might be quite different.
Low quality: Reviewers have limited confidence in the estimated effect size; the actual value may be very different from the estimated one.
Very low quality: Reviewers have no confidence in the estimated value of the effect size; it is probable that the actual value is very different from the estimated one.
2.4. Data Retrieval
The articles were managed using EndNote X4 and the data retrieval table was developed using Microsoft Excel. In order to ensure the accuracy of the data retrieval, two evaluators collected, organized and checked the materials independently. In the few cases where the two evaluators' opinions conflicted, they discussed their differences in an attempt to arrive at a consensus opinion; if they remained in disagreement a third evaluator (the corresponding author) made a final decision. The information collected included demographic and clinical characteristics of participants (sample size, age, sex, medication, ethnicity, country, duration of illness) and the mean and standard deviation of the serum BDNF levels in each group.
2.5. Statistical analysis
Meta-analysis was conducted using RevMan 5.1[37] developed by the Cochrane Collaboration. The effect size of continuous variables was summarized using standardized mean difference (SMD). The results of the pooled analyses are shown in the Forest Plots.
2.5.1. Test of heterogeneity
The heterogeneity of the studies was assessed using the chi-squared test and I2 in the RevMan software program. The I2 value assesses the proportion of variance in the SMD that is due to cross-study heterogeneity. When the significance level (i.e., p-value) of the chi-square test is >0.1 and I2<50%, the possibility that the studies are heterogeneous is small, so the fixed-effect model is used to assess pooled results. But when the significance of the chi-square test is <0.1 and I2>50%, the studies are considered heterogeneous so the random-effect model is used to assess pooled results[38] and the sources of the heterogeneity need to be considered. In this study, we assess heterogeneity using sub-group analysis and the Meta regression model in the Stata software package.[39]
2.5.2. Sensitivity analysis
The stability of the results was assessed using sensitivity analysis. To assess the potential effect of each study on the overall conclusion, each included study is sequentially removed and the pooled standardized mean difference (SMD) of the remaining studies is compared to the pooled SMD for all studies.
2.5.3. Publication bias
The potential publication bias was assessed using a fail-safe number (Nfs) and a funnel plot. Nfs indicates how many studies with negative results are needed to reverse the previous conclusion.[40] With 0.05 as the α-level, the formula is Nfs(0.05)=(∑ Z/1.645)2-K where K is the number of studies tested and the Z-value for each study is calculated using the NORMSINV function in Excel based on the p-value of the study calculated using Stata.[41],[42]
3. Results
3.1. Characteristics of included studies
Among the 268 articles identified, 25 (20 in English and 5 in Chinese) were included in the meta-analysis (Figure 1). There were two articles for which the evaluators disagreed about whether or not to include in the analysis, but they were able to resolve their differences after discussion about the articles.
Included studies are listed in table 1. Five studies used drug-naïve patients who had never used antipsychotic medications, 18 studies used patients who had used antipsychotic medication (in one of the studies[20] the patients were drug-free at the time of the BDNF assessment), and two studies included both drug-naïve and drug-exposed patients. Only three of the studies included follow-up assessments of BDNF over the course of treatment;[21],[24],[26] all the other studies were cross-sectional assessments. (In these three studies the post-treatment results were used in the analysis.[10]) Among the 25 studies, 15 received a quality rating of ‘C’ (low) and 10 received a quality rating of ‘D’ (very low). The main reasons for the low quality ratings were that the articles did not provide sufficient details about the methods or did not assess the potential biases in the results.
Table 1. Characteristics of the 25 included studies.
| 1st author year [reference] | country | mean age (years) | male/ female ratio | sample size | mean (sd) duration of illness (years) | mean (sd) serum BDNF of patients (ng/ml) | mean (sd) serum BDNF of controls (ng/ml) | quality evalua- tiona | p | z | |
| 1 | Toyooka 2002 [9] | Japan | 47.0 | 31/38 | MED: 34 CTL: 35 | 25 (12.3) | 6.3 (3.4) | 11.4 (7.7) | C | <0.001 | -3.19 |
| 2 | Shimizu2003 [29] | Japan | 36 | 40/40 | DN: 15 MED:25CTL: 40 | DN: 1.1 (1.4)MED: 14.1 (9.9) | 26.4 (11.0) | 28.5 (9.1) | D | 0.355 | -0.37 |
| 3 | Jockers2004 [28] | Germany | 32.9 | 78/85 | DN: 102CTL: 61 | Incident patients | 13.1 (5.9) | 13.2 (5.2) | D | 0.913 | 1.36 |
| 4 | Pirildar2004 [10] | Turkey | 26.8 | 14/30 | MED: 22CTL: 22 | 1.3 (1.1) | 14.5 (2.9) | 26.8 (9.3) | C | <0.001 | -3.72 |
| 5 | Tan 2004 [11] | China | 46.8 | 72/18 | MED: 46CTL: 44 | 11.8 (6.5) | 7.4 (2.9) | 9.5 (4.4) | D | 0.012 | -2.26 |
| 6 | Tan 2005 [12] | China | 47.2 | 97/29 | MED: 81CTL: 45 | 22.6 (7.7) | 7.3 (2.6) | 9.9 (4.3) | D | <0.001 | -3.72 |
| 7 | Huang 2006 [30] | Taiwan, China | 31.9 | 108/114 | DN: 10MED: 116CTL: 96 | 6.0 (5.0) | 14.2 (6.9) | 14.2 (6.9) | C | 0.974 | 1.95 |
| 8 | Grillo 2007 [13] | Brazil | 35 | 31/38 | MED: 44CTL: 25 | no information | 0.112 (0.048) | 0.169 (0.026) | C | <0.001 | -3.72 |
| 9 | Li 2007 [14] | China | 47.2 | 97/29 | MED: 81CTL: 45 | 9.4 (5.9) | 7.3 (2.6) | 9.9 (4.3) | D | <0.001 | -3.72 |
| 10 | Mackin2007 [31] | England | 42.8 | 30/4 | MED: 20CTL: 14 | noinformation | 13.4 (8.0) | 13.8 (9.17) | C | 0.903 | 1.30 |
| 11 | Zhang 2007 [32] | China | 47.0 | 127/47 | MED: 124CTL: 50 | 22.3 (7.2) | 8.4 (4.2) | 9.3 (4.4) | C | 0.209 | -0.81 |
| 12 | Ikeda 2008 [15] | Japan | 40.8 | 86/75 | MED: 74CTL: 87 | 19.6 (11.2) | 37.1 (20.4) | 52.2 (25.3) | C | <0.001 | -3.72 |
| 13 | Reis 2008 [33] | Brazil | 52.3b | 60/0 | MED: 40CTL: 20 | 32.4 (9.2) | 7.8 (1.8) | 4.4 (2.0) | D | <0.001 | -3.72 |
| 14 | Rizos 2008 [16] | England | 26.0 | 16/13 | DN: 14CTL: 15 | Incident patients | 23.9 (6.0) | 30.0 (8.4) | C | 0.034 | -1.82 |
| 15 | Bai 2009 [20] | China | 32 | 30/28 | MED: 28 CTL: 30 | 1.0c | 0.068 (0.021) | 0.111 (0.039) | D | <0.001 | -3.72 |
| 16 | Chen 2009 [17] | China | 29.5 | 96/82 | DN: 88CTL: 90 | Incident patients | 9.0 (4.2) | 12.1 (2.2) | C | 0.0001 | -3.72 |
| 17 | Vinogradov 2009 [18] | USA | 44.1 | 52/20 | MED: 56CTL: 16 | no information | 25.3 (10.3) | 31.3 (9.0) | C | 0.038 | -1.77 |
| 18 | Xiu 2009 [19] | China | 51.1 | 509/178 | MED: 364CTL: 323 | 27.0 (10.1) | 9.9 (2.0) | 11.9 (2.3) | C | 0.001 | -3.72 |
| 19 | Chend 2010 [26] | China | 28.3 | 86/78 | MED: 80CTL: 84 | 2.0 (1.5) | 10.1 (4.9) | 12.0 (2.5) | D | 0.003 | -2.79 |
| 20 | Fernandesd 2010 [21] | Brazil | 35.4 | 5/2b | MED: 7CTL: 21 | 16.5 (3.7) | 0.16 (0.04) | 0.39 (0.12) | D | <0.001 | -3.72 |
| 21 | Jindal 2010 [22] | USA | 22.3 | 41/23 | DN: 24CTL: 41 | Incident patients | 0.098 (0.031) | 0.117 (0.038) | C | 0.042 | -1.73 |
| 22 | Rizos 2010 [23] | Greece | 26.7 | 29/30 | DN: 37CTL: 22 | Incident patients | 18.9 (8.2) | 29.2 (7.7) | C | 0.001 | -3.72 |
| 23 | Rizosd 2010 [24] | Greece | 45.0 | 61/30 | MED: 47CTL: 44 | 23.8 (7.8) | 19.9 (10.7) | 27.5 (8.2) | C | <0.001 | -3.43 |
| 24 | Carlino2011 [25] | Italy | 46.3 | 40/40 | MED: 40CTL: 40 | 23.1 (11.0) | 25.5 (1.2) | 28.9 (2.5) | C | <0.001 | -3.72 |
| 25 | Zeng 2011 [27] | China | 40.5 | 46/43 | MED: 44CTL: 45 | 2.7 (2.4) | 0.010 (0.004) | 0.020 (0.004) | D | <0.001 | -3.72 |
BDNF, brain-derived neurotrophic factor; ECT, electroconvulsive therapy
MED, medicated patients with schizophrenia; DN, drug-naïve patients with schizophrenia; CTL, control subjects;
a C=low quality (limited confidence in the estimated effect size); D=very low quality (reviewers have no confidence in the estimated effect size)
b no information for controls
c no standard deviation of age provided in paper
d study compared BDNF before versus after treatment with antipsychotic medication (Rizos, 2010 and Chen, 2010) or with ECT (Fernandes, 2010)
Pooling all 25 studies, there were 1663 patients with schizophrenia (the case group) and 1355 individuals without schizophrenia (the control group). Both groups were 66% male; the mean (standard deviation) age was 38.8 (9.8) for cases and 38.0 (9.6) for controls. Outcome measures for all 25 studies were continuous variables. Characteristics of the included studies including sample size, male/female ratio, duration of illness, method of treatment, BDNF level, and the evaluation of the quality of the study are listed in Table 1.
3.2. Pooled results
3.2.1. Heterogeneity test
The heterogeneity test found robust cross-study variations in results (χ2=215.55, df=24, p<0.001, I2=89%). Thus, a random-effect model was used to calculate the pooled estimates. Possible causes of heterogeneity include country of origin of the study, methodological quality of the study, differences in sample size, male/female ratio, age of subjects, use of medications, and so forth.
3.2.2. Comparison of BDNF between cases and controls
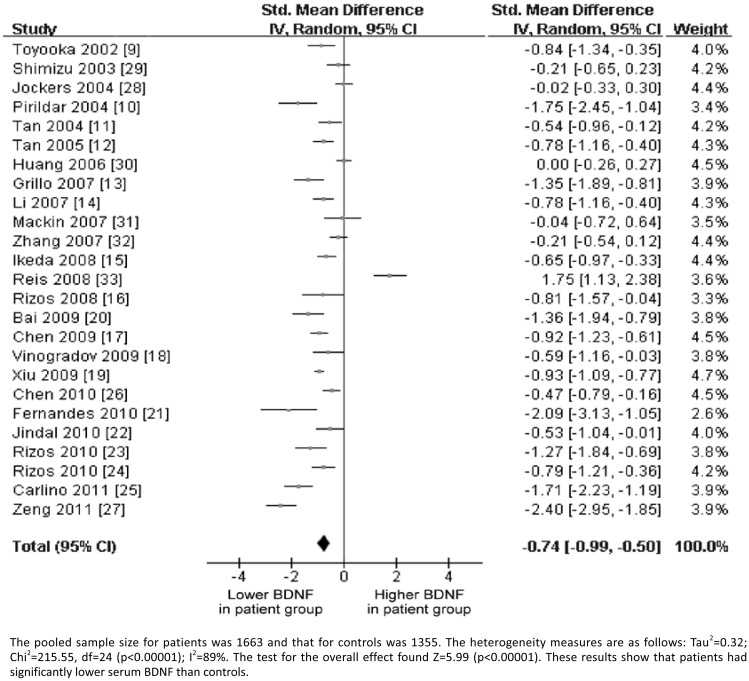
Pooling estimates from 25 studies, a statistically significant lower level of serum BDNF was found in patients with schizophrenia compared to controls (pooled SMD= -0.74; 95%CI=-0.99, -0.50; p<0.001 using a random-effect model, see Figure 2).
Figure 2. Forest plot of differences in BDNF levels between patients with schizophrenia and controls.
3.2.3. Sensitivity analysis
The influence of each study on the overall estimate was assessed by removing studies one by one and comparing the pooled estimate yielded from the remaining 24 studies to the pooled estimate from all 25 studies. Results found a lower level of serum BDNF in patients with schizophrenia compared to controls in all 25 analyses, indicating that removal of any study would not alter the overall results. The overall conclusion also remained unchanged after removing the three studies that evaluated changes in serum BDNF with treatment.[21],[24],[26] These findings suggest that the pooled SMD results are stable.
3.2.4. Publication bias
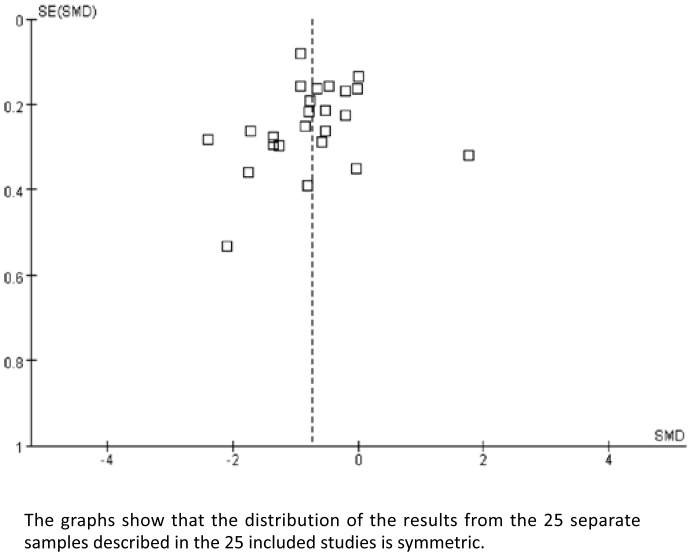
The funnel plot (Figure 3) was symmetric and the computed fail safe N (Nfs) was 1392, which means that 1392 unpublished studies with null results would be needed to make the current results non-significant. Taken together, these findings suggest that there is little publication bias in our results.
Figure 3. Funnel plot of the primary results of the 25 included studies.
3.2.5. Sub-group analyses
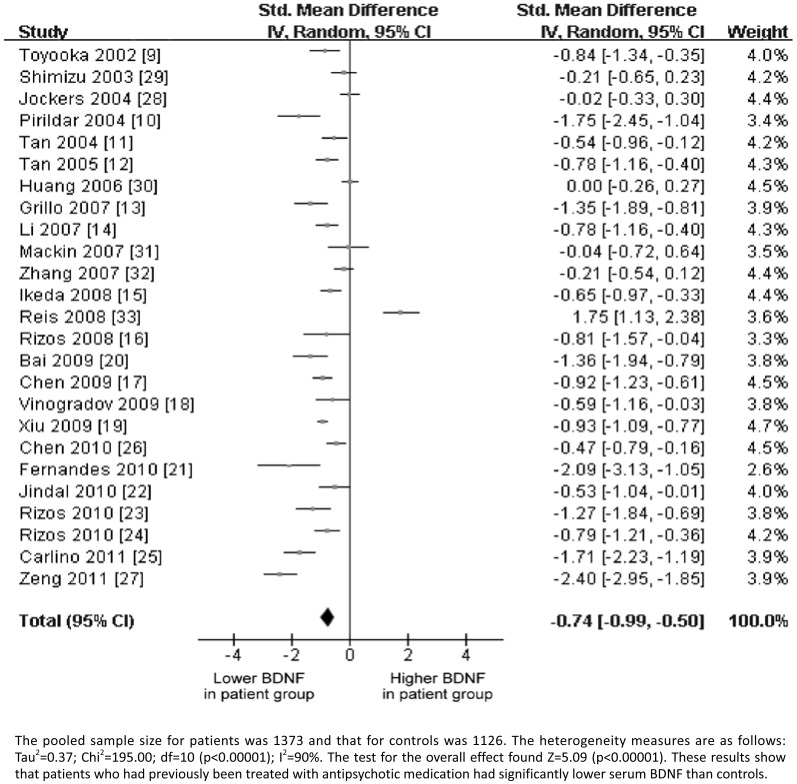
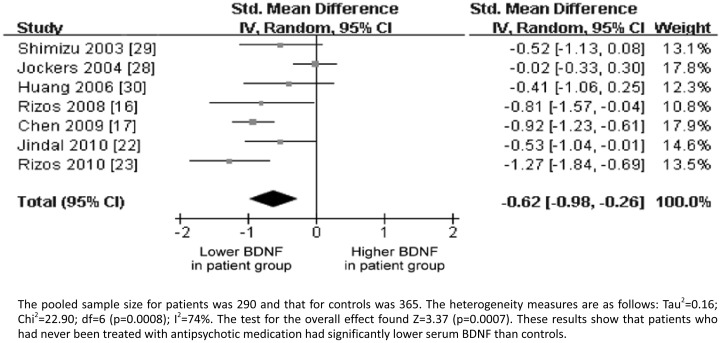
Of the 25 studies included in this meta-analysis, 20 included patients who had been treated with antipsychotic medication and 7 included drug-naïve patients (2 studies included both types of patients). Separate meta-analyses were conducted for these two sub-groups of studies. The heterogeneity tests found statistically significant variation in the study results (I2=90% and 74%, respectively, p<0.001) so the random-effect model was used to provide the overall estimates. Results found a lower level of serum BDNF in patients with schizophrenia compared to controls in both subgroups of studies. The pooled SMD was -0.75 (95% CI=-1.04, -0.46; Z=5.09; p<0.001) for the antipsychotic medication-exposed patients and -0.62 (95% CI=-0.98, -0.26; Z=3.37; p<0.001) for drug-naïve patients (Figures 4 and 5).
Figure 4. Forest plot of differences in BDNF levels between patients with schizophrenia who had been treated with antipsychotic medication and controls.
Figure 5. Forest plot of differences in BDNF levels between antipsychotic medication-naïve patients with schizophrenia and controls.
We also conducted separate meta-analyses for the 10 studies from China and the 15 studies from other countries. Since heterogeneity tests found statistically significant variation in study results (I2=89% and p<0.001 for both groups of studies), the random-effect model was used to provide the overall estimate. Lower levels of serum BDNF in patients with schizophrenia (compared to controls) were found from studies in China as well as from studies conducted in other countries. The pooled SMD was -0.80 (95% CI=-1.13, -0.48; Z=4.89; p<0.001) for studies in China and -0.70 (95% CI=-1.09, -0.31, Z=3.50, p<0.001) for studies from other countries.
Comparison of the results of the 15 studies rated as ‘low quality’ and the 10 studies rated as ‘very low quality’ also found that the patient group in both subgroups of studies had lower serum BDNF than the control group. The 15 low-quality studies were heterogenous (I2=83%, p<0.001) so a random-effect model was used; the SMD was -0.80 (95% CI=-1.05, -0.55; Z=6.30; p<0.001). The 10 very low-quality studies were also heterogeneous (I2=93%, p<0.001); the SMD was -0.66 (95% CI=-1.18, -0.13; Z=2.46; p<0.001).
3.2.6. Meta regression analysis
Table 2 shows the results for the meta regression (using Stata 11.2 software) which used the study SMD as the dependent variable and patient mean age, patient gender ratio, sample size, study location (China vs. non-China), medication status (medication-naïve vs. medication-exposed) and study quality (low vs. very low) as the dependent variables. No significant associations were found between these covariates and the results of the studies.
Table 2. Meta-regression of relationship of study factors to heterogeneity of study resultsa.
| Variables | Regression coefficient (β) | Standard error of β | Standardized Beta | t-value | p-value | 95% CI of β |
| mean age of patients | 0.067 | 0.085 | 0.175 | 0.80 | 0.435 | -0.108, 0.242 |
| M/F gender ratio | -2.93 | 5.19 | 10.74 | -0.56 | 0.578 | -13.67, 7.80 |
| Sample size | 0.005 | 0.006 | 0.019 | 0.84 | 0.409 | -0.001, 0.018 |
| Location (China vs. other) | 1.24 | 1.71 | 2.38 | 0.49 | 0.292 | -1.14, 3.62 |
| Drug-naïve vs. drug-exposed | -1.32 | 2.54 | 5.28 | -0.52 | 0.609 | -6.60, 3.96 |
| Low study quality vs ‘very low’ study quality | 1.07 | 1.16 | 2.41 | 0.92 | 0.365 | -1.33, 3.48 |
95% CI, 95% confidence interval
a Study result is the standardized mean difference (SMD) of serum BDNF between patients and controls; R2for model=0.028
3.2.7. Comparison of serum BDNF before and after treatment
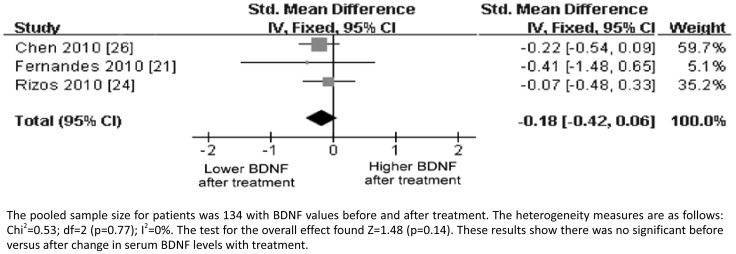
Of the 25 studies included in this meta-analysis, three were comparisons of before and after treatment (medication [24], [26] or ECT[21]). Heterogeneity tests found no statistically significant variation in the results for the three studies (I2<1%, p=0.77), so a fixed-effect model was used to compute the overall estimate. The results indicated no difference in the level of serum BDNF in patients before versus after treatment (pooled SMD= -0.18; 95% CI=-0.42, 0.06; Z=1.48; p=0.14; Figure 6).
Figure 6. Forest plot of BDNF levels among patients with schizophrenia before and after treatment.
4. Discussion
4.1. Main findings
Pooling from the 25 studies, 1663 individuals with schizophrenia and 1355 without schizophrenia were included in this meta-analysis. There was significant between-study heterogeneity (I2=89%) so a random-effect model was used to compute the pooled estimates. The pooled standardized mean difference (SMD) indicated that there was a significantly lower serum BDNF level in the schizophrenia group when compared to the control group. Sensitivity analysis found that the pooled results were robust. A symmetrical funnel plot of the studies and the large estimated fail safe number indicated that there was little evidence for publication bias. The methodological quality of the studies identified was poor, largely due to insufficient description of the methods and lack of adjustment for potential biases.
With a few exceptions, our findings are similar to those of a recently reported meta-analysis of Green and colleagues[43] that pooled the results of 16 studies and found reduced serum BDNF in both drug-naïve and drug-exposed patients with schizophrenia. Our review identified more studies because we searched more databases and included studies published in Chinese. Unlike our study, their meta-regression analysis found that reduced serum BDNF was associated with increasing age. Most importantly, they reported that the evidence was of ‘moderate quality’ while our more rigorous assessment of data quality found that the studies were all either of ‘low quality’ or of ‘very low quality’.
4.2. Limitations
Our search strategy did not identify unpublished articles or those published in languages other than English or Chinese and it may have missed articles published in supplemental journals or as conference abstracts. However, the lack of publication bias in the results suggests that failure to identify such studies probably had little effect on the overall outcome.
The more disturbing problem is the heterogeneity of the study results. Despite strictly enforcing inclusion and exclusion criteria that limited included papers to controlled studies of patients with schizophrenia who did not have other concurrent diagnoses and that used the same method to assess serum BDNF levels, we still found substantial heterogeneity between the studies. Our subgroup analyses and meta-regression analysis indicated that this heterogeneity could not be explained by cross-study differences in medication status (drug-naïve vs. drug-exposed), country of origin, study quality, patient age, patient gender, or sample size. One factor we were unable to assess that has been shown to be related to BDNF levels – differences in BDNF Val66Met polymorphism[44] – may have influenced in study heterogeneity, but we doubt that this could explain the large cross-study differences we found.
We expect the main reason for the heterogeneity of results between studies was the low scientific quality of the included studies (10 graded as ‘very low quality’ and 15 graded as ‘low quality’). There were methodological, clinical and analytic components of these studies that were obscured in the reports that may have substantially influenced the results. For example, several of the studies did not provide detailed information about the type or dose of medication used or details about the ELISA kit employed, [11], [15], [26], [29]–[31] so it was not possible to include these variables in our analysis.
4.3. Significance
In 2005, Angelucci and colleagues [45] hypothesized that brain functioning in patients with schizophrenia is related to levels of BDNF and/or the expression of the BDNF receptor TrkB. Specifically, they suggested that the BDNF Val66Met single nucleotide polymorphism (GUG substitution of AUG) results in lower expression of BDNF in the central nervous system, and, thus, plays an important role in the onset and course of schizophrenia. Studies in Han Chinese have provided supplementary confirmation for this hypothesis: BDNF levels have been associated with the development of schizophrenia and with the short term memory of patients with schizophrenia;[46] and the BDNF Val66Met polymorphism has been associated with the age of onset of schizophrenia[47] and with the severity of cognitive decline in schizophrenia.[48]
BDNF can pass through the blood-brain-barrier and undergoes the same maturation and aging process in peripheral blood as in the brain.[8] Thus, if subsequent research confirms the importance of BDNF in the onset and course of schizophrenia, serum BDNF could be a valuable potential biomarker for the disorder.
This meta-analysis pooled 25 rigorously selected studies and found a statistically significant lower level of serum BDNF in individuals with schizophrenia than in control subjects, supporting the hypothesis that BDNF plays a role in the illness. However, the validity of results was undermined by the low quality of the included studies and by the heterogeneity of results. Thus, despite the strong statistical findings, we consider the evidence of lower serum BDNF in patients with schizophrenia – which is almost exclusively dependent on cross-sectional studies – as ‘weak.’ Prospective studies with larger samples that follow patients over the course of illness and that use uniform selection and monitoring procedures are needed to confirm the relevance of these preliminary results. It is too early to decide whether or not serum BDNF can be used as a biomarker for schizophrenia.
Biography

Dr. Huiru Cui graduated from Jining Medical College in Shandong Province in 2006 and received a Masters in Medical Science from Fudan University in Shanghai in 2009. She is currently working as a researcher in the Department of Biochemistry and Pharmacology of the Shanghai Mental Health Center at the Shanghai Jiao Tong University School of Medicine. Her current research interests are evidence-based medical studies and fMRI studies of brain functioning.
Footnotes
Conflict of interest: The authors report no conflict of interest related to this manuscript
Funding: This meta-analysis was supported by the National Key Basic Research Program (No. 2007CB512306), the National Science and Technology High-Level Research Program (No. 2008AA02Z412), the National Natural Science Fund (No. 30770773), and the Shanghai Program for Fostering Scientific Leaders in Health (No. XBR2011005).
References
- 1.Jiang KD. Psychiatry. 2nd ed. Beijing: People's Health Publishing House; 2010. pp. 116–117. [Google Scholar]
- 2.Ashe PC, Berry MD, Boulton AA. Schizophrenia, a neurodegenerative disorder with neurodevelopmental antecedents. Prog Neuropsychopharmacol Biol Psychiatry. 2001;25(4):691–707. doi: 10.1016/s0278-5846(01)00159-2. [DOI] [PubMed] [Google Scholar]
- 3.Lewin GR, Barde YA. Physiology of the neurotrophins. Annu Rev Neurosci. 1996;19:289–317. doi: 10.1146/annurev.ne.19.030196.001445. [DOI] [PubMed] [Google Scholar]
- 4.Weickert CS, Hyde TM, Lipska BK, Herman MM, Weinberger DR, Kleinman JE. Reduced brain-derived neurotrophic factor in prefrontal cortex of patients with schizophrenia. Mol Psychiatry. 2003;8(6):592–610. doi: 10.1038/sj.mp.4001308. [DOI] [PubMed] [Google Scholar]
- 5.Mellios N, Huang HS, Baker SP, Galdzicka M, Ginns E, Akbarian S. Molecular determinants of dysregulated GABAergic gene expression in the prefrontal cortex of subjects with schizophrenia. Biol Psychiatry. 2009;65(12):1006–1014. doi: 10.1016/j.biopsych.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 6.Wong J, Hyde TM, Cassano HL, Deep-Soboslay A, Kleinman JE, Weickert CS. Promoter specific alterations of brain-derived neurotrophic factor mRNA in schizophrenia. Neuroscience. 2010;169(3):1071–1084. doi: 10.1016/j.neuroscience.2010.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ashe PC, Chlan-Fourney J, Juorio AV, Li XM. Brain-derived neurotrophic factor (BDNF) mRNA in rats with neonatal ibotenic acid lesions of the ventral hippocampus. Brain Res. 2002;956(1):126–135. doi: 10.1016/s0006-8993(02)03176-1. [DOI] [PubMed] [Google Scholar]
- 8.Karege F, Schwald M, Cisse M. Postnatal developmental profile of brain-derived neurotrophic factor in rat brain and platelets. Neurosci Lett. 2002;328(3):261–264. doi: 10.1016/s0304-3940(02)00529-3. [DOI] [PubMed] [Google Scholar]
- 9.Toyooka K, Asama K, Watanabe Y, Muratake T, Takahashi M, Someya T, et al. Decreased levels of brain-derived neurotrophic factor in serum of chronic schizophrenic patients. Psychiatry Res. 2002;110(3):249–257. doi: 10.1016/s0165-1781(02)00127-0. [DOI] [PubMed] [Google Scholar]
- 10.Pirildar S, Gonul AS, Taneli F, Akdeniz F. Low serum levels of brain-derived neurotrophic factor in patients with schizophrenia do not elevate after antipsychotic treatment. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28(4):709–713. doi: 10.1016/j.pnpbp.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Tan YL, Zhou DF, Zou YZ, Cao LY, Su JM, Yao FX. The level of brain-derived neurotrophic factor in serum in schizophrenia patients with tardive dyskinesia. Chin J Ment Dis. 2004;30(5):332–334. (in Chinese) [Google Scholar]
- 12.Tan YL, Dong FZ, Lian YC, Yi ZZ, Xiang YZ. Decreased BDNF in serum of patients with chronic schizophrenia on long-term treatment with antipsychotics. Neurosci Lett. 2005;382(1-2):27–32. doi: 10.1016/j.neulet.2005.02.054. [DOI] [PubMed] [Google Scholar]
- 13.Grillo RW, Ottoni GL, Leke R, Souza DO, Portela LV, Lara DR. Reduced serum BDNF levels in schizophrenic patients on clozapine or typical antipsychotics. J Psychiatr Res. 2007;41(1-2):35–35. doi: 10.1016/j.jpsychires.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Li YG, Tan YL, Zhou DF, Cao LY, Yang FD, Zhang XY, et al. Serum level of brain-derived neurotrophic factor in Long-term treatment of chronic schizophrenic patients. Chin J Ment Dis. 2007;8(33):482–483. (in Chinese) [Google Scholar]
- 15.Ikeda Y, Yahata N, Ito I, Nagano M, Toyota T, Yoshikawa T, et al. Low serum levels of brain-derived neurotrophic factor and epidermal growth factor in patients with chronic schizophrenia. Schizophr Res. 2008;101(1-3):58–66. doi: 10.1016/j.schres.2008.01.017. [DOI] [PubMed] [Google Scholar]
- 16.Rizos EN, Rontos I, Laskos E, Arsenis G, Michalopoulou PG, Vasilopoulos D, et al. Investigation of serum BDNF levels in drug-naive patients with schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2008;32(5):1308–1311. doi: 10.1016/j.pnpbp.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 17.Chen da C, Wang J, Wang B, Yang SC, Zhang CX, Zheng YL, et al. Decreased levels of serum brain-derived neurotrophic factor in drug-naive first-episode schizophrenia: relationship to clinical phenotypes. Psychopharmacology (Berl) 2009;207(3):375–380. doi: 10.1007/s00213-009-1665-6. [DOI] [PubMed] [Google Scholar]
- 18.Vinogradov S, Fisher M, Holland C, Shelly W, Wolkowitz O, Mellon SH. Is serum brain-derived neurotrophic factor a biomarker for cognitive enhancement in schizophrenia? Biol Psychiatry. 2009;66(6):549–553. doi: 10.1016/j.biopsych.2009.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xiu MH, Hui L, Dang YF, Hou TD, Zhang CX, Zheng YL, et al. Decreased serum BDNF levels in chronic institutionalized schizophrenia on long-term treatment with typical and atypical antipsychotics. Prog Neuropsychopharmacol Biol Psychiatry. 2009;33(8):1508–1512. doi: 10.1016/j.pnpbp.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 20.Bai ZS, Zhao HQ, Gao ZQ, Zhong AF. Serum level of brain-derived neurotrophic factor in schizophrenic patients with unsuccessful suicide attempt. J Chin Psychiatry. 2009;19(01):22–24. (in Chinese) [Google Scholar]
- 21.Fernandes BS, Massuda R, Torres M, Camargo D, Fries GR, Gama CS, et al. Improvement of schizophrenia with electroconvulsive therapy and serum brain-derived neurotrophic factor levels: Lack of association in a pilot study. Psychiatry Clin Neurosci. 2010;64(6):663–665. doi: 10.1111/j.1440-1819.2010.02153.x. [DOI] [PubMed] [Google Scholar]
- 22.Jindal RD, Pillai AK, Mahadik SP, Eklund K, Montrose DM, Keshavan MS. Decreased BDNF in patients with antipsychotic naive first episode schizophrenia. Schizophr Res. 2010;119(1-3):47–51. doi: 10.1016/j.schres.2009.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rizos EN, Michalopoulou PG, Siafakas N, Stefanis N, Douzenis A, Rontos I, et al. Association of serum brain-derived neurotrophic factor and duration of untreated psychosis in first-episode patients with schizophrenia. Neuropsychobiology. 2010;62(2):87–90. doi: 10.1159/000315438. [DOI] [PubMed] [Google Scholar]
- 24.Rizos EN, Papadopoulou A, Laskos E, Michalopoulou PG, Kastania A, Vasilopoulos D, et al. Reduced serum BDNF levels in patients with chronic schizophrenic disorder in relapse, who were treated with typical or atypical antipsychotics. World J Biol Psychiatry. 2010;11(2):251–255. doi: 10.3109/15622970802182733. [DOI] [PubMed] [Google Scholar]
- 25.Carlino D, Leone E, Di Cola F, Baj G, Marin R, Dinelli G, et al. Low serum truncated-BDNF isoform correlates with higher cognitive impairment in schizophrenia. J Psychiatr Res. 2011;45(2):273–279. doi: 10.1016/j.jpsychires.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 26.Chen DC, Li YL, Xiu MH, Wang N, Yang KB, Nie Y, et al. Effect of risperidone treatment on serum levels of BDNF and the correlation of between serum BDNF levels and clinical efficiency and cognition improvement in first-episode schizophrenic patient. Chin J Ment Dis. 2010;36(9):529–532. (in Chinese) [Google Scholar]
- 27.Zeng Y, Kuang L, Gan Y, Chen JM, Ai M, Wang W, et al. Expression and significance of serum BDNF in patients with schizophrenia. Journal of Chongqing Medical University. 2011;36(4):476–478. (in Chinese) [Google Scholar]
- 28.Jockers-Scherubl MC, Danker-Hopfe H, Mahlberg R, Selig F, Rentzsch J, Schurer F, et al. Brain-derived neurotrophic factor serum concentrations are increased in drug-naive schizophrenic patients with chronic cannabis abuse and multiple substance abuse. Neurosci Lett. 2004;371(1):79–83. doi: 10.1016/j.neulet.2004.08.045. [DOI] [PubMed] [Google Scholar]
- 29.Shimizu E, Hashimoto K, Watanabe H, Komatsu N, Okamura N, Koike K, et al. Serum brain-derived neurotrophic factor (BDNF) levels in schizophrenia are indistinguishable from controls. Neurosci Lett. 2003;351(2):111–114. doi: 10.1016/j.neulet.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Huang TL, Lee CT. Associations between serum brain-derived neurotrophic factor levels and clinical phenotypes in schizophrenia patients. J Psychiatr Res. 2006;40(7):664–668. doi: 10.1016/j.jpsychires.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 31.Mackin P, Gallagher P, Watson S, Young AH, Ferrier IN. Changes in brain-derived neurotrophic factor following treatment with mifepristone in bipolar disorder and schizophrenia. Aust N Z J Psychiatry. 2007;41(4):321–326. doi: 10.1080/00048670701213211. [DOI] [PubMed] [Google Scholar]
- 32.Zhang XY, Tan YL, Zhou DF, Cao LY, Wu GY, Xu Q, et al. Serum BDNF levels and weight gain in schizophrenic patients on long-term treatment with antipsychotics. J Psychiatr Res. 2007;41(12):997–1004. doi: 10.1016/j.jpsychires.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 33.Reis JH. Increased serum levels of brain-derived neurotrophic factor in chronic institutionalized patients with schizophrenia. Neurosci Lett. 2008;439(2):157–159. doi: 10.1016/j.neulet.2008.05.022. [DOI] [PubMed] [Google Scholar]
- 34.Ebrahim S, Clarke M. STROBE: new standards for reporting observational epidemiology, a chance to improve. Int J Epidemiol. 2007;36(5):946–948. doi: 10.1093/ije/dym185. [DOI] [PubMed] [Google Scholar]
- 35.Egger M, Altman DG, Vandenbroucke JP. Commentary: strengthening the reporting of observational epidemiology the STROBE statement. Int J Epidemiol. 2007;36(5):948–950. doi: 10.1093/ije/dym199. [DOI] [PubMed] [Google Scholar]
- 36.Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.RevMan 5.1, released on 22 March 2011. Available from http://ims.cochrane.org/revmn. [Accessed 7 October 2012]
- 38.Egger M, Smith GD, Schneider M, Minder C, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sterne JAC, Bradburn MJ, Egger M. Meta-analysis in Stata. In: Egger M, Smith GD, Altman D, editors. Systematic Reviews in Health Care: Meta-Analysis in Context. London: BMJ Books; 2001. pp. 347–369. [Google Scholar]
- 40.Rosenberg MS. The file-drawer problem revisited: a general weighted method for calculating fail-safe numbers in meta-analysis. Evolution. 2005;59(2):464–468. [PubMed] [Google Scholar]
- 41.Yang HX, Wu YL, Ling L, Han L. Effectiveness of extent of lymphadenectomy for survival in patients with resectable non-small cell lung cancer. J Evid Based Med. 2002;2(3):132–139. [Google Scholar]
- 42.Su L, Hu H, Chen J, Wang JJ, Wang LW, Shi SX. P50 sensory gating studies in schizophrenics: a systematic review. Natl Med J China. 2010;90(29):2020–2024. (in Chinese) [PubMed] [Google Scholar]
- 43.Green MJ, Matheson SL, Shepherd A, Weickert CS, Carr VJ. Brain-derived neurotrophic factor levels in schizophrenia: a systematic review with meta-analysis. Mol Psychiatry. 2011;16(9):960–972. doi: 10.1038/mp.2010.88. [DOI] [PubMed] [Google Scholar]
- 44.Bus BA, Arias-Vasquez A, Franke B, Prickaerts J, de Graaf J, Voshaar RC. Increase in serum brain-derived neurotrophic factor in met allele carriers BDNF Val66Met polymorphism is specific to males. Neuropsychobiology. 2012;65(4):183–187. doi: 10.1159/000336997. [DOI] [PubMed] [Google Scholar]
- 45.Angelucci F, Brene S, Mathe AA. BDNF in schizophrenia, depression and corresponding animal models. Mol Psychiatry. 2005;10(4):345–352. doi: 10.1038/sj.mp.4001637. [DOI] [PubMed] [Google Scholar]
- 46.Zhang XY, Liang J, Chen DC, Xiu MH, De Yang F, Kosten TA, et al. Low BDNF is associated with cognitive impairment in chronic patients with schizophrenia. Psychopharmacology (Berl) 2012;222(2):277–284. doi: 10.1007/s00213-012-2643-y. [DOI] [PubMed] [Google Scholar]
- 47.Yi ZH, Zhang C, Wu Z, Hong W, Li ZZ, Fang YR, et al. Lack of effect of brain derived neurotrophic factor (BDNF) Val66Met polymorphism on early onset schizophrenia in Chinese Han population. Brain Res. 2011;1417(12):146–150. doi: 10.1016/j.brainres.2011.08.037. [DOI] [PubMed] [Google Scholar]
- 48.Zhang XY, Chen DC, Xiu MH, Haile CN, Luo X, Xu K, et al. Cognitive and serum BDNF correlates of BDNF Val66Met gene polymorphism in patients with schizophrenia and normal controls. Hum Genet. 2012;131(7):1187–1195. doi: 10.1007/s00439-012-1150-x. [DOI] [PMC free article] [PubMed] [Google Scholar]