Abstract
We summarized and appraised evidence regarding HIV prevention interventions for adults with criminal justice involvement.
We included randomized and quasi-randomized controlled trials that evaluated an HIV prevention intervention, enrolled participants with histories of criminal justice involvement, and reported biological or behavioral outcomes. We used Cochrane methods to screen 32 271 citations from 16 databases and gray literature. We included 37 trials enrolling n = 12 629 participants. Interventions were 27 psychosocial, 7 opioid substitution therapy, and 3 HIV-testing programs. Eleven programs significantly reduced sexual risk taking, 4 reduced injection drug risks, and 4 increased testing.
Numerous interventions may reduce HIV-related risks among adults with criminal justice involvement. Future research should consider process evaluations, programs involving partners or families, and interventions integrating biomedical, psychosocial, and structural approaches.
Since the inception of the HIV epidemic, populations with criminal justice involvement have experienced an urgent need for HIV prevention and care services. Much of the research in this area to date has focused on HIV risk and prevention in incarceration settings, including both prisons and short-term jails. Incarcerated individuals face overlapping risks for HIV infection: infections are primarily attributed to pre- and postincarceration risk behaviors,1,2 but risks may also include behaviors in prison (e.g., injection drug use [IDU], sexual activity, tattooing, violence),3 elevated prevalence of other sexually transmitted infections (STIs), and sociodemographic risk factors such as poverty, racial discrimination, and living in underserved or socially marginalized communities.3,4 In the United States, approximately 1 in 7 HIV-infected individuals is released from an incarceration facility each year.5 A recent systematic review of HIV prevalence among prisoners in 152 low- and middle-income countries found prevalence estimates greater than 10% in 20 countries,6 and a survey of global evidence found elevated HIV prevalence among prisoners worldwide.3 The population of incarcerated individuals is a large target for intervention; according to the United Nations Office on Drugs and Crime, approximately 10 million people worldwide are held in prison at any one time, and 30 million are incarcerated each year.7
Nonincarcerated adults with a history of criminal justice involvement are also at elevated risk of HIV infection because of these same risk factors, and studies have documented high rates of HIV, sexual risk taking, and substance use among probationers and parolees.8,9 Individuals returning from incarceration to community settings tend to report high rates of condomless sexual activity and drug use,9–11 compounded by relationship disruptions12 and difficulty accessing medical services and fulfilling other basic needs.13,14 The postrelease period is especially characterized by elevated risk taking,13,15,16 return to preincarceration behaviors,17 and high HIV incidence.18 The population of nonincarcerated adults involved with the criminal justice system is also sizeable; in the United States, for example, approximately 4.8 million individuals in the community were under supervision by adult correctional authorities in 2011 (approximately 2% of the population).19
Published research supports the need for HIV risk-reduction efforts for individuals with criminal justice involvement in both incarceration and community settings. Combining evidence from both settings in a single systematic review is valuable given the overlap between incarcerated and nonincarcerated individuals, the return of incarcerated individuals to the community, high rates of recidivism and reincarceration, and the design of HIV prevention interventions that include both incarceration-based and postrelease services (e.g., case management, booster sessions). Although previous reviews have examined intervention effectiveness in this population, an up-to-date and rigorous review is needed. Limitations of previous reviews include the lack of systematic search methods,20,21 the inclusion of a wide range of study designs, or focus on only a subset of studies, such as opioid substitution therapies (OSTs),22–25 treatment of alcohol use disorders,26 needle-exchange programs,27 interventions for women in prison,28 or interventions in incarceration but not community settings.3,29,30 We aimed to summarize and appraise the most methodologically rigorous evidence for the effectiveness of HIV prevention efforts among adults with criminal justice involvement, including both incarceration and community settings.
METHODS
This systematic review followed Cochrane Collaboration procedures, which require at least 2 authors and specify guidelines for defining the review question, searching for studies, selecting studies, extracting data, appraising the risk of bias in included trials, and analyzing data.31 A subset of 26 studies in this review is the subject of a registered Cochrane review of HIV prevention for criminal justice–involved individuals in community (nonincarceration) settings.32
Eligibility Criteria
We limited our review to randomized and quasi-randomized controlled trials, as these designs are most appropriate for identifying causal effects. We included trials regardless of the unit of randomization (individuals or clusters). Quasi-randomized trials were those that did not use strictly random assignment, but approximated randomization in a method unlikely to create consistent bias (e.g., alternation, assignment by birthdate).
Participants were adults (aged 18 years or older) with criminal justice involvement, defined as a lifetime history of arrest or conviction of a criminal act. We made no exclusions by geographic location, probation or parole status, type or level of offense, or recency of criminal justice involvement. Some individuals who are arrested may not be convicted of an offense, but we included arrestees in this review regardless of subsequent conviction or plea: arrestees sustain HIV-related risk behaviors such as drug use, and initial contact with the criminal justice system during arrest and processing may provide opportunities for intervention.33 We also acknowledge that some incarcerated or convicted individuals are innocent of any crime, but we were unable to make exclusions on this basis. Because our focus was the primary prevention of HIV, we excluded studies that only enrolled participants known to be HIV-infected. We also excluded studies of participants who engaged in criminal activity but who lacked involvement with a formal criminal justice system; for example, we excluded studies of individuals who use illicit drugs or engage in sex work unless all participants also reported lifetime history of arrest. We excluded trials that enrolled adults both with and without a history of criminal justice involvement if they did not disaggregate results.
We included trials of any behavioral, social, biomedical, structural, or HIV-testing intervention that was designed to reduce HIV-related risk. We excluded trials of interventions that did not list HIV prevention as a program goal. We made no exclusions by type of intervention staff or setting, including programs that take place in correctional facilities, communities, or both. We included trials with any type of control group (e.g., usual care, no intervention, information about HIV, attention-matched controls, or other HIV prevention services).
We included only studies that reported at least 1 biological or behavioral outcome related to HIV transmission (e.g., STIs, condomless sexual intercourse) or HIV testing uptake. Primary outcomes were HIV and STI incidence. Secondary outcomes were HIV testing and sexual and IDU-related behaviors that convey a risk of HIV infection. We acknowledge that, unlike sexual behavior, IDU-related behavior, or STI or HIV incidence, HIV testing uptake is not indicative of HIV risk, and HIV testing alone may not influence risk behaviors.34,35
We decided to include trials of HIV testing interventions in the review for several reasons. First, the choice to undergo HIV testing presents an opportunity for providers to deliver other interventions, such as single-session interventions that may present comparatively less burden for providers.36 Second, given the large numbers of HIV-infected individuals who are in contact with the criminal justice system each year,5 HIV testing in this population presents important opportunities for secondary prevention and linkage to care, even if treatment as prevention is not a key focus of this review. Third, new biomedical strategies for HIV prevention such as preexposure prophylaxis (PrEP)37–39 cannot be introduced without proof of an HIV-negative test result40; this makes consent to HIV testing an important prerequisite for access to these new technologies. We determined that maximizing HIV testing uptake would likely be of sufficient interest to practitioners and researchers in this field for inclusion as an outcome in the review. When studies met all other eligibility criteria, we also extracted data on substance use, recidivism, reincarceration, intervention acceptability, and intervention costs as ancillary outcomes.
Information Sources
We searched 16 electronic databases without date, country, or language restrictions through January 6, 2014: PubMed, PsycINFO, EMBASE, CENTRAL, the National Criminal Justice Reference Service, Criminal Justice Abstracts, Global Health, the Cumulative Index to Nursing and Allied Health Literature, the Education Resources Information Center, Applied Social Sciences Index and Abstracts, the Allied and Complementary Medicine Database, Sociological Abstracts, Political Science Abstracts, Social Services Abstracts, Social Sciences Citation Index, and Dissertation Abstracts. Searches included truncated terms specific to criminal justice and HIV or AIDS (Box A, available as a supplement to this article at http://www.ajph.org, shows our PubMed search strategy). We did not include terms specific to “adults” in the search; we reserved any trials that met all eligibility criteria except participant age (i.e., studies among juveniles) for a separate review article.
We searched for gray literature by using the Dissertation Abstracts database, conference abstracts from 2000 onward (including the International AIDS Conference, Conference on Retroviruses and Opportunistic Infections, and meetings of the International Society for Sexually Transmitted Diseases Research, American Psychological Association, American Society of Criminology, Academy of Criminal Justice Sciences, International Society of Criminology), Web sites of international and national agencies (e.g., Joint United Nations Programme on HIV/AIDS, World Health Organization, United Nations Office on Drugs and Crime, United Nations Population Fund, World Bank, Centers for Disease Control and Prevention), cross-referencing included articles and relevant reviews, searching clinical trials.gov to locate ongoing studies, and contacting 68 experts working in this field.
We merged results of the search in Endnote X5 reference management software (Thomson Reuters, Philadelphia, PA) and removed duplicate citations. Two reviewers (K. U. and D. D.) assessed abstracts and full articles for inclusion. K. U. and D. D. independently assessed a subset of 3831 citations for potential eligibility and discussed any disagreements, which established consistent application of the inclusion criteria. We then divided the remaining citations for preliminary assessment, marking potentially relevant references and obtaining all full-text versions. After obtaining the full text of potentially eligible citations, K. U. and D. D. independently reviewed all full-text articles to decide on study eligibility, resolving any disagreements by discussion and referral to a third reviewer (D. O.). Reviewers were not blind to any aspect of the studies, and reviewers contacted trialists to obtain any information needed to make eligibility determinations.
Data Collection and Assessing Risk of Bias
Two reviewers (K. U. and D. D.) independently extracted descriptive, methodological, and outcome data from included articles into spreadsheets, again resolving disagreements by discussion and referral to a third reviewer (D. O.). We extracted data on all study characteristics specified in the Cochrane Handbook31 (citation, eligibility, methods, participants, interventions, outcomes, results, and miscellaneous details), as well as information on participation incentives, sample size calculation, intervention acceptability, and cost effectiveness. K. U. and D. D. assessed trials for methodological quality according to the Cochrane Risk of Bias assessment tool.31 Where multiple reports referred to the same study, we extracted data from all available sources.
We summarized outcome data as fully as possible in Review Manager 5.2 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark), but many of the data needed for a meta-analysis were missing or incompletely reported across primary trials (e.g., group numbers, number of events for dichotomous outcomes, means and standard deviations for continuous outcomes). These data limitations prevented meta-analysis. Included studies also presented large variation in study designs, control groups, intervention designs, and definition of outcome measures. As a result, although we had prepared a protocol for conducting a quantitative synthesis, we present a narrative synthesis of findings in the text and tables. We did not conduct statistical tests for publication bias, mediators, or moderators of effects because of the same data limitations.
RESULTS
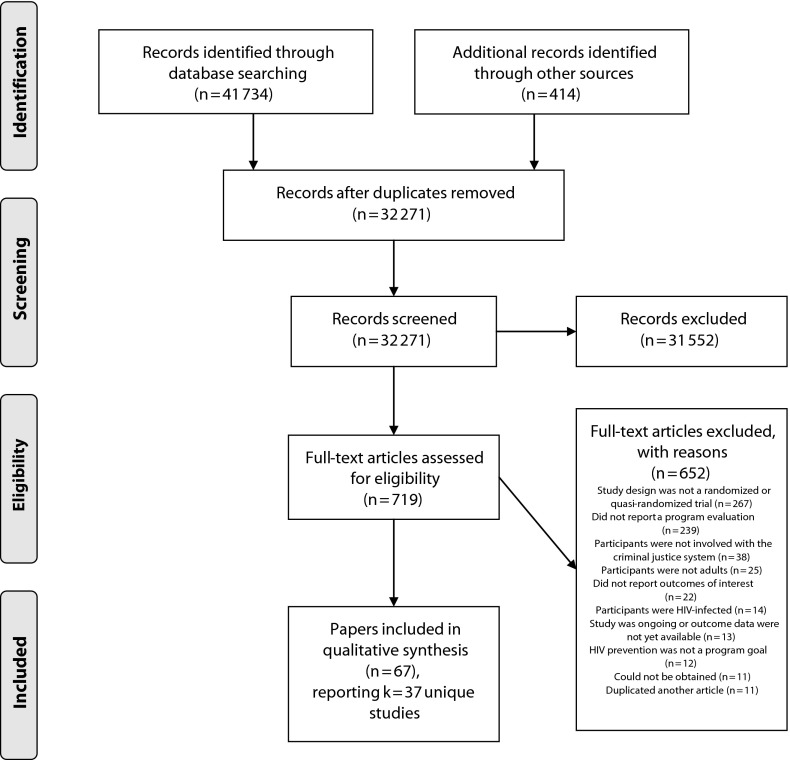
The results of the search are reported in Figure 1. Overall, the search identified 32 271 unique citations, of which 719 appeared to meet eligibility criteria; we were able to obtain full reports for 708. Of these, 67 articles met inclusion criteria; these articles reported k = 37 unique studies, and we designated 1 article for each study as a primary reference.8,33,42–73 Three primary articles reported multiple studies,33,47,60 and we designated 33 articles as supplemental reports.74–106 Of the 267 studies excluded because of study design criteria, the most common study designs were 1-group evaluations (either program descriptions or pre–post designs), followed by contemporaneous nonrandom assignment of participants to groups (e.g., participants self-selected into conditions; different treatments were delivered in different facilities on the basis of logistical constraints), then cohort studies, cross-sectional studies, studies with historical controls, qualitative studies that explored perceived program impacts, and literature reviews.
FIGURE 1—
Flow diagram of included studies in a systematic review of HIV risk-reduction interventions in incarceration and community settings.
Note. Format from Moher et al.41 For more information, visit http://www.prisma-statement.org. PRISMA 2009 Checklist available as a supplement to this article at http://www.ajph.org.
Description of Trials
Participants.
Descriptive information about included trials is reported in Tables 1, 2, and 3. The 37 included studies enrolled n = 12 629 participants at baseline. Participants were primarily from the United States (k = 34; n = 12 047), with additional trials taking place in Australia,50 China,55 and Iran.44 Two trials did not report participant ages, but across the remaining trials, mean participant ages ranged from 25 to 41 years, with a median of 34.5 years. Trials often enrolled single-gender samples: there were 9 trials among men, 12 among women, and 16 among mixed samples (median = 72% male). Across the 32 US trials reporting ethnicity, participant samples were primarily White (≥ 67%) in 6 trials, primarily of non-White race/ethnicity (≤ 33% White) in 14 trials, and mixed in the remaining 12 trials. Trials enrolled participants with a range of criminal justice involvement; at the time the intervention began, participants were incarcerated in residential correctional facilities (k = 19; n = 6329); staying in court-ordered inpatient drug treatment facilities (k = 2; n = 217); in a jail diversion program (k = 1; n = 15); on probation, parole, or work-release (k = 8; n = 3336); or in the community with a mix of supervisory arrangements ranging from parole to no supervision (k = 7; n = 2732). Nine studies provided information about the types of crimes leading to participants’ criminal justice involvement: these typically included arrests because of drug crimes, property crimes, and prostitution.
TABLE 1—
Participants, Intervention Characteristics, and Retention of Included Studies Evaluating Psychosocial Interventions in a Systematic Review of HIV Risk-Reduction Interventions in Incarceration and Community Settings
| Study | Location | Participant Criminal Justice Involvement | Participants (No.; Mean Ages; Race/Ethnicity; Gender) | Intervention; Total Approximate Time | Intervention Setting (Incarceration, Community, or Both) | Control Group | Last Follow-Up; Retention |
| Alemagno et al.42 | Ohio | Probation or community supervision | 212; 36 y; Primarily minority; Mixed | Computer-based brief negotiation and interviewing intervention; 1 session; 0.33 h | Community | Information: written educational materials about HIV | 2 mo; 77% |
| Baxter43 | Arizona | Incarcerated | 134; About 30 y; Primarily White; Mixed | HIV education and risk assessment; 8 h | Incarceration | Not stated—most likely no treatment | 6 mo; not stated |
| Braithwaite et al.45 | Georgia | Incarcerated | 116; 25.3 y; Primarily minority; Men | 1. Active learning peer education, facilitator is HIV-negative former inmate, activities based on social cognitive theory; 12 h | Incarceration | Usual care, videos on health promotion and disease | 3 mo; 41% |
| 2. Active learning peer education, facilitator is HIV-positive former inmate; 12 h | |||||||
| 3. Didactic curriculum with videos; 12 h | |||||||
| Callahan47 | Missouri | Community, some on probation, some with lifetime history of arrest | 204; 39.5 y; Primarily minority; Women | 1. Testing and counseling, well-woman checkup, 4 peer intervention sessions by a health professional paired with a peer leader; 9 h | Community | NE: testing and counseling only (NIDA standard intervention) | 12 mo; 91% |
| 2. Testing and counseling, well-woman checkup; 1 h | |||||||
| Callahan47 | Missouri | Community, some on probation, some with lifetime history of arrest, recruited from drug court | 94; 36.5 y; Primarily minority; Women | 1. Testing and counseling, well-woman checkup, 4 peer intervention sessions by a health professional paired with a peer leader; 9 h | Community | NE: testing and counseling only (NIDA standard intervention) | 12 mo; 90% |
| 2. Testing and counseling, well-woman checkup; 1 h | |||||||
| Clarke et al.48 | Rhode Island | Incarcerated, primarily short-term facility that also serves as a prison | 245; 34.57 y; Primarily White; Women | Motivational interviewing—set goals for changing alcohol use behavior, explored barriers to change, made change plan; 1.5 h | Both (1 session while incarcerated, 1 in community) | None: no treatment, received a list of resources | 6 mo; 79% |
| el-Bassel et al.51 | New York | Incarcerated | 159; 32.8 y; Primarily minority; Women | Group sessions on HIV/AIDS prevention, skills building, and social support; 32 h | Both (16 sessions in incarceration, 6 booster sessions in community) | Information: three 2-h group sessions on HIV | 1 mo; 64% |
| Eldridge et al.52 | Mississippi | Drug offender, court-ordered to drug treatment | 117; 34.2 y; Mixed; Women | 2 sessions on HIV/STD education, then 4 sessions on behavior skills training, including condom skills, sexual refusal, negotiation, and needle-cleaning; 9 h | Community | Usual care: 2 sessions on HIV and STD education | 2 mo; 57% |
| Fish et al.53 | New York | Incarcerated | 240; Age not reported; Ethnicity not reported; Men | Video, comic book, and risk assessment; 0.5 h | Incarceration | NE: risk assessment only | 3 mo; 100% |
| Grinstead et al.54 | California | Incarcerated | 414; 35.7 y; Mixed; Men | Peer educator intervention by HIV-positive inmates; 0.5 h | Incarceration | Usual care | 0.5 mo; 43% |
| Hser et al.55 | Shanghai, China | Drug offender, compulsory residential drug treatment | 100; 38.7 y; Chinese; Mixed | Strengths assessment based on transitional case management before community reentry, weekly contact with social worker, weekly urine testing, employment assistance, referral to MMT in the event of relapse; 3 mo | Both (began in compulsory residential drug treatment, then continued in the community) | Usual care: strengths assessment before reentry, monthly contact with a social worker, random urine testing approximately monthly | 3 mo; 94% |
| Leukefeld et al.59 | Connecticut, Delaware, Kentucky, Rhode Island | Incarcerated | 444; 34.6 y; Primarily White; Women | 5 group sessions in prison focusing on HIV and bloodborne infections, risky relationships, myths about drugs, sexual, relationships, abuse or control, self-protection, safer-sex negotiation, and support. 1 booster in the community 30 d later to boost recall and consider thinking myths; 8.5 h | Both (began in incarceration, then booster sessions in the community) | Information: AIDS awareness video | 3 mo; 77% |
| Longshore et al.60 | Ohio | Community supervision | 192; 31.2 y; Mixed; Mixed | TASC case management including links with local service providers, drug testing, and schedules for reporting to criminal justice agents; 6 mo | Community | Other: alternative case management offering services like counseling and drug testing, but outside TASC protocol | 6 mo; 69% |
| Longshore et al.60 | Oregon | Community supervision | 393; 31.6 y; Mixed; Mixed | TASC case management including links with local service providers, drug testing, and schedules for reporting to criminal justice agents; 6 mo | Community | Other: alternative case management offering services like counseling and drug testing, but outside TASC protocol | 6 mo; 84% |
| Lurigio et al.61 | Illinois | Probation | 99; 30 y; Primarily minority; Mixed | 1. HIV education delivered in one-on-one format including visual displays, included info about lubricants, condoms, dental dams, cleaning needles; 1 h | Community | 1. Attention: matched time, format and activities to No. 1, but subject matter was about heart disease, led by a physician | 1 mo; 51% |
| 2. Same as No. 1, but delivered in a small group format; 1 h. Intervention groups were combined for analysis | 2. Attention: matched time, format and activities to No. 2, but subject matter was about heart disease, led by a physician. Control groups were combined for analysis | ||||||
| Martin and Scarpitti65 | Delaware | Parolees | 456; 29.4 y; Primarily minority; Mixed | Assertive community treatment, drug treatment and case management including AIDS education; 6 mo | Community | Usual care parole | 6 mo; 57% |
| Martin et al.63 | Delaware | Probation | 706; 34.5 y; Primarily minority; Mixed | 2 sessions of a probationer-focused intervention with thought mapping and voluntary HIV testing, booster at 3-month follow-up; 2 h | Community | NE: NIDA enhanced standard intervention with testing; same as intervention group but without the thought mapping | 6 mo; 60% |
| Martin et al.64 | Delaware, Kentucky, Virginia | Incarcerated but scheduled for work release (DE), prison (KY), jail (VA) | 534; 33.9 y; Mixed; Mixed | 1. Peer-designed DVD intervention matched to participant race and gender, focusing on needle cleaning and condom negotiation, delivered with HIV testing and an educational video; 1 h | Incarceration | Information: testing plus educational video shown to all participants | 3 mo; 64% |
| 2. Health practitioner-administered NIDA standard intervention with HIV testing and educational video; 1 h | |||||||
| Marxhausen66 | Delaware | Parole, work release (reentering the community with a supervised status) | 600; Not reported; Mixed; Mixed | One-on-one peer-led intervention focusing on HIV and HCV; 1 h | Community | Other: group-format peer-led intervention | 1 mo (3-mo not available); 74% |
| The full design of the trial included other arms, but a full report was not available | |||||||
| Needels et al.68 | New York | Incarcerated, then community | 704; 34.7 y; Not reported; Women | Empowerment group meetings open to all inmates, individual counseling in jail, case management in the community after release designed to regularize lifestyles and lower risk of risk behavior; 12 mo | Both (group sessions in incarceration, then case management in the community) | NE: empowerment groups (with intervention group), but then usual discharge planning with other case management available in the community; Number of hours unclear | 15 mo; 73% |
| Prendergast et al.69 | 4 sites, unidentified states | Incarcerated, then community (parolees, some probation) | 812; 33.6 y; Mixed; Mixed | Transitional case management—strength assessment 2 mo prerelease, conference call 1 mo prerelease to review discharge plan and mobilize support. Weekly case manager in community for 3 mo, then 3 additional monthly follow-ups for clients needing more help. All participants got substance abuse treatment in jail, referral to publicly funded community treatment (mandated in all study states), and motivational video; 5 mo | Both (strengths-based assessment and conference call in incarceration, then case management in the community) | Usual care: referral to community-based treatment, which included standard supervision and referrals. All participants got substance abuse treatment in jail, referral to publicly funded community treatment (mandated in all study states), and motivational video | 9 mo; 84% |
| Rhodes and Gross33 | Oregon | Arrestees released after arrest or arraignment; some in community, others escorted from lockup to study site | 696; About 33 y; Mixed; Mixed | 1. Case management - video, referral guide, and case management program after release. Focused on drug use, HIV prevention, and linkages to other services. Not focused on controlling illegal behaviors; 6 mo | Community | Info: video and referral guide about HIV | 6 mo; 85% |
| 2. Referral—video, referral guide, plus 1 counseling and referral session with a referral specialist; 1 h | |||||||
| Rhodes and Gross33 | Washington, DC | Arrestees released after arrest or arraignment; some in community, others escorted from lockup to study site | 673; About 35 y; Primarily minority; Mixed | 1. Case management—video, referral guide, and case management program after release. Focused on drug use, HIV prevention, and linkages to other services. Not focused on controlling illegal behaviors; 6 mo | Community | Info: video and referral guide about HIV | 6 mo; 85% |
| 2. Referral—video, referral guide, plus 1 counseling and referral session with a referral specialist; 1 h | |||||||
| Sacks et al.70 | Colorado | Incarcerated | 468; 35.1 y; Mixed; Women | Therapeutic community, including meetings, seminars, groups, and peer education. Also worked 20 h per week in the prison. Everyone at the facility got mental health services, education, health care, vocational training, and community reintegration training; 6 mo | Incarceration | Other: intensive outpatient program, educational 90-h course focusing on drug use and criminal behavior. Everyone at the facility got mental health services, education, health care, vocational training, and community reintegration training; 90 h | 12 mo; 82% |
| Scott and Dennis71 | Illinois | Community—reentering from jail treatment program | 480; 36.7 y; Primarily minority; Women | Motivational interviews at release and monthly postrelease for 3 mo, with later interviews as needed (quarterly). Focused on feedback for drug use, HIV risk, and illegal activity; barriers that prevent stopping; motivation for change. Referral to treatment of women reporting substance use; 3 h or more | Community | Usual care | 3 mo; 96% |
| Weir et al.72 | Oregon | Probation, parole, and recently incarcerated | 530; 35.7 y; Mixed; Women | 1. HIV and IPV intervention. Up to 12 one-on-one counseling intervention sessions over 3 mo. All groups got counseling and testing for HIV, HCV, and STDs, and handbook of community services; 13 h | Community | NE: counseling and testing for HIV, HCV, and STDs, and handbook of community services; 1 h | 9 mo; 84% |
| 2. Same as No. 1 but without discussing IPV; 13 h | |||||||
| Wolitski73 | California, Mississippi, Rhode Island, Wisconsin | Incarcerated, then released | 522; About 23 y; Primarily minority; Men | Project START, 2 individual sessions before release focusing on HIV, hepatitis, and STI knowledge, personal risk-reduction plan, skills training, community reentry; 4 postrelease sessions review and update the plan and discuss barriers, additional sessions as needed; 5.5 h | Both (sessions before and after release) | NE: nonenhanced, 1 session, HIV, STD, and hepatitis risk assessments with risk reduction planning | 5.5 mo; 77% |
Note. IPV = intimate partner violence; MMT = methadone maintenance treatment; NE = a lesser or nonenhanced version of the experimental intervention; NIDA = National Institute on Drug Abuse; STD = sexually transmitted disease; TASC = Treatment Alternatives to Street Crime.
TABLE 2—
Participants, Intervention Characteristics, and Retention of Included Studies Evaluating Opioid Substitution Therapy Interventions in a Systematic Review of HIV Risk-Reduction Interventions in Incarceration and Community Settings
| Study | Location | Participant Criminal Justice Involvement | Participants (No.; Mean Age; Race/Ethnicity; Gender) | Intervention; Total Approximate Time (Hours or Months) | Intervention Setting (Incarceration, Community, or Both) | Control Group | Last Follow-Up; Retention |
| Bayanzadeh and Afshar44 | Tehran, Iran | Incarcerated | 100; 35.7 y; Iranian; Men | MMT plus CBT group therapy focusing on drug use; 1 daily intervention of CBT and skills, plus 1 weekly harm-reduction class and 1 weekly family education visit; 6 mo | Incarceration | Other: nonmethadone treatment of addictions plus psychotherapeutic medications | 6 mo; 58% |
| Brown et al.46 | Wisconsin | Jail diversion—drug court or treatment | 15; 27.5 y; Primarily White; Mixed | 1. Treatment in a specialist treatment facility (for opioid-dependent offenders) with buprenorphine and naloxone (Suboxone); 12 mo | Community | Other: treatment in a primary care facility with buprenorphine and naloxone (Suboxone); 12 mo | 13.5 mo; Not known |
| 2. Treatment in the specialist treatment facility with MMT; 12 mo | |||||||
| Cropsey et al.49 | Alabama | Probation or parole, community supervision | 36; 31.8 y; Primarily White; Women | Buprenorphine and weekly study visit to discuss adherence, side effects, and medication management, dosage ranged from 8 to 12 mg/day and was based on weekly assessment; 12 wk | Community | Placebo with similar counseling | 5.5 mo; 100% |
| Dolan et al.50 | New South Wales, Australia | Incarcerated | 382; 27 y; Primarily White; Men | MMT, started on 30 mg and increased by 5 mg every 3 d until 60 mg achieved; 4 mo | Incarceration | None: waitlist for MMT | 48 mo; 65% |
| Kinlock et al.58 | Maryland | Incarcerated, then community | 211; 40.3 y; Primarily minority; Men | 1. 12 weekly sessions of drug abuse education, a meeting with the study counselor, and MMT while in prison (beginning at 5 mg and increasing 5 mg every 8 d up to 60 mg) then referred to the program’s community-based facility within 10 d of release; 12 wk | Both (began in incarceration, then continued after release) | Other: group education sessions and individual counseling only, advised to seek drug abuse treatment in the community at a publicly funded program according to standard procedures | 14.5 mo (12 mo after release); 97% |
| 2. Same as No. 1, but MMT not provided during incarceration (provided through postrelease referral instead); 12 wk | |||||||
| Magura et al.62 | New York City | Incarcerated, short term | 133; 39 y; Primarily minority; Men | MMT: 30 mg/day stepped up to 70 mg per day where indicated, referral upon release; 10–90 d | Incarceration | Other: buprenorphine, 4 mg stepped up to 32 mg where indicated; 10–90 d | 6 mo; 61% |
| McKenzie et al.67 | Rhode Island | Incarcerated | 90; 40.7 y; Primarily White; Mixed | 1. Prerelease MMT starting at 5 mg then increasing by 2 mg daily until target dose or release (average MMT lasted 15 d prerelease); 1 HIV risk-reduction and overdose prevention counseling session; referral and funding for a postrelease drug treatment program in community for 12 wk full-time and 12 wk part-time; 26 wk total | Both (began during incarceration, then continued after release) | NE: 1 HIV risk-reduction and overdose prevention counseling session, referral to community MMT program without $ assistance) | 6 mo (12 mo not available); 69% |
| 2. Same as No. 1, but without prerelease MMT; 24 wk total |
Note. CBT = cognitive–behavioral therapy; MMT = methadone maintenance treatment; NE = a lesser or nonenhanced version of the experimental intervention.
TABLE 3—
Participants, Intervention Characteristics, and Retention of Included Studies Evaluating HIV Testing Interventions in a Systematic Review of HIV Risk-Reduction Interventions in Incarceration and Community Settings
| Study | Location | Participant Criminal Justice Involvement | Participants (No.; Mean Age; Race/Ethnicity; Gender) | Intervention; Total Approximate Time | Intervention Setting (Incarceration, Community, or Both) | Control Group | Last Follow-Up; Retention |
| Gordon et al.8 | Maryland, Rhode Island | Probation or parole | 697; 38.7 y; Primarily minority; Mixed | Offered HIV testing directly at the correctional facility in a private office; 5 min | Community | Other: given a card with clinic information and detailed directions for testing at a community testing site (off-site from the corrections office) | Unclear how long they waited for testing to occur; 100% |
| Kavasery et al.57 | Connecticut | Incarcerated | 298; 35 y; Mixed; Men | 1. Offered testing the same day as entry; 5 min | Incarceration | Other: offered testing 1 week after entry | 0 mo; 76% |
| 2. Offered testing the next day after entry; 5 min | |||||||
| Kavasery et al.56 | Connecticut | Incarcerated | 323; 33.6 y; Mixed; Women | 1. Offered testing the same day as entry; 5 min | Incarceration | Other: Offered testing 1 week after entry | 0 mo; 83% |
| 2. Offered testing the next day after entry; 5 min |
Where reported, the median percentage of participants across studies with a high-school diploma or general equivalency diploma was 54% (k = 20); when studies reported average number of years of education, the median across studies was 11.2 (k = 12). Same-sex sexual orientation or behavior was discussed in only 2 studies,72,73 which reported small percentages of participants disclosing same-sex sexual behavior or a same-gender primary partner; another study limited enrollment to individuals reporting heterosexual intercourse,48 and 34 studies did not discuss sexual orientation. Inclusion criteria for enrollment in 23 of the 37 studies required recent substance use or a measure of drug or alcohol dependence (n = 7355). Twenty studies compensated participants for completing assessments or study activities, typically around $10 to $20 for baseline assessments and $25 to $50 for follow-up assessments. Typical recruitment procedures in incarceration facilities included mailings and in-person outreach to incarcerated individuals at the time of intake or a preset time before release; recruitment in community settings included mailings and in-person outreach at times of arrest, release from incarceration, probation visits, or drug court visits.
Interventions.
Interventions varied widely across trials. Seven studies assessed OST for drug treatment (n = 967),44,46,49,50,58,62,67 sometimes paired with psychosocial intervention, with the dual goals of reducing both substance use and associated HIV risk behaviors. These trials included 4 studies of methadone maintenance treatment (MMT), 1 study of buprenorphine maintenance, 1 comparing MMT to buprenorphine maintenance, and 1 comparing MMT to buprenorphine and naloxone (Suboxone) maintenance.
Twenty-seven studies assessed psychosocial strategies for preventing HIV (n = 10 344),33,42,43,44,47,48,51–55,59–61,63–66,68–73 of which 18 also aimed to reduce drug or alcohol use along with HIV risk. Fifteen of the 27 psychosocial intervention studies declared a theoretical basis for the intervention, which most frequently included motivational interviewing, the health belief model, social cognitive theory, and the transtheoretical model. The psychosocial strategies used a group format (k = 5), an individual format (k = 16), or both group and individual activities (k = 3); 2 trials compared group interventions against individual modalities, and 1 did not state a format. Seven interventions included at least 1 peer-led component, and 4 trials included an active treatment arm that was primarily media-based (computer or video intervention); 6 trials evaluated a form of case management. Dosage of psychosocial interventions ranged from a single 20-minute session to 6 full months of a therapeutic community environment; across trials, the median intervention length was 9 hours.
Finally, 3 trials tested the effect of varying the time or place of offering participants an HIV test, with the goal of optimizing HIV testing behavior.8,56,57
Twenty-two of the 37 trials reported at least 1 method for assessing or increasing fidelity of intervention implementation, such as facilitator training and supervision, standardized intervention materials or manuals, attendance logs, fidelity checklists, or review of taped sessions.
Control groups also varied across studies and included no treatment (k = 3), usual care (which could include a range of services varying by local conditions; k = 7), basic information about HIV (k = 6), a diluted or less-intense (“nonenhanced”) version of the active treatment (k = 8), an attention-matched control (i.e., identical in dosage and format to the intervention, but focusing on another topic instead of HIV; k = 1), a placebo for 1 OST trial (k = 1), and another active intervention intended to prevent HIV (k = 11).
Study designs and methodological quality.
Information about methodological quality was underreported (Tables 4, 5, and 6). Thirty-one studies were randomized controlled trials, of which 11 reported the method of randomization (usually a computer-generated randomized sequence). The 6 quasi-randomized controlled trials “randomized” participants by alternation, assignment by month, or coin flip. Nine studies reported strategies for concealing the allocation sequence from staff responsible for recruitment and enrollment. Analyses were generally conducted on a complete case basis, in which participants are analyzed in original assignment groups but without imputing missing data for dropouts (k = 28).107 Four studies conducted per-protocol analyses that excluded or reassigned participants who deviated from the intended interventions, and 4 studies employed full intention-to-treat analyses that accounted for dropouts (or had no attrition).107 The unit of randomization was almost always the individual; in the 3 trials that randomized clusters of participants (by time block or facility), analytic methods for controlling for clustering were not described. Of the 32 studies that commented on baseline equivalence, 13 found group differences at baseline, and 6 of these explicitly described controlling for baseline differences in analyses. With the exception of 1 placebo-controlled trial, no study described methods for blinding participants or personnel to condition. Twenty-eight studies did not describe (or did not use) methods for blinding outcome assessors to reduce risk of detection bias. The longest follow-up ranged from immediate to 14.5 months after baseline, with a median longest follow-up time of 6 months across studies. Median retention across studies was 77% at longest follow-up; 23 studies commented on sources or effects of attrition. Only 5 studies presented a power calculation justifying sample size.
TABLE 4—
Methodological Characteristics of Included Studies Evaluating Psychosocial Interventions in a Systematic Review of HIV Risk-Reduction Interventions in Incarceration and Community Settings
| Study | Study Design | Method of Randomization | Unit of Randomization; Unit of Analysis | Baseline Differences | Power Calculation | Type of Analysis | Results of Any Attrition Analyses |
| Alemagno et al.42 | RCT | Not reported | Individual; Individual | Yes | Not reported | Complete case | Injection drug users in experimental group were more likely to drop out |
| Baxter43 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | Not reported |
| Braithwaite et al.45 | RCT | Not reported | Facility; Individual | Not reported | Not reported | Complete case | Not reported |
| Callahan47 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | Not reported |
| Callahan47 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | Not reported |
| Clarke et al.48 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | No differential attrition by condition |
| el-Bassel et al.51 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | No differences between dropouts and returnees, follow-up rates for experimental and controls were similar |
| Eldridge et al.52 | RCT | Not reported | 3-wk admission blocks; Individual | No differences | Not reported | Complete case | No difference between completers and noncompleters by race, income, relationship, or crack cocaine use; no difference between intervention conditions |
| Fish et al.53 | Quasi-RCT | Coin flip | Individual; Individual | Not reported | Not reported | Complete case | Not reported |
| Grinstead et al.54 | Quasi-RCT | Alternation | Week of participants’ release from prison; Individual | No differences | Not reported | Per protocol | Returnees were more likely to be married or in committed relationship than dropouts |
| Hser et al.55 | RCT | Computer-generated randomization sequence | Individual; Individual | No differences | Not reported | Complete case | Attrition similar across study arms |
| Leukefeld et al.59 | RCT | Computer-generated with Research Randomizer | Individual; Individual | Yesa | Not reported | Complete case | Dropout did not vary by site |
| Longshore et al.60 | RCT | Not reported | Individual; Individual | Yesa | Not reported | Complete case | No differences between dropouts and returnees |
| Longshore et al.60 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | No differences between dropouts and returnees |
| Lurigio et al.61 | RCT | Not reported | Individual; Individual | Not reported | Not reported | Complete case | Returnees did not differ from entire original sample |
| Martin and Scarpitti65 | RCT | Not reported | Individual; Individual | Yes | Not reported | Complete case | Not reported |
| Martin et al.63 | RCT | Not reported | Individual; Individual | Not reported | Not reported | Complete case | Not reported |
| Martin et al.64 | RCT | Computer-generated urn randomization | Individual; Individual | No differences | Not reported | Complete case | Not reported |
| Marxhausen66 | RCT | Not reported | Individual; Individual | Not reported | Yes, 99% power to detect an effect size of 0.25, at α = 0.05 | Complete case | Attrition analyses not reported, but noncompletion of questions occurred at a similar rate between groups among the participants who were retained at follow-up |
| Needels et al.68 | RCT | Not reported | Individual; Individual | Yesa | Not reported | Complete case | Not reported |
| Prendergast et al.69 | RCT | Computer-generated sequence, urn randomization | Individual; Individual | Yes | Not reported | Per protocol | Completers did not differ from noncompleters at 3 mo, but at 9 mo completers were more likely than noncompleters to have history of prostitution or pimping and crack use. At 3 mo, the balance between groups shifted and treatment group was more likely to have lifetime GHB use than controls; at 9 mo the treatment group was more likely to have lifetime suicidal ideation. |
| Rhodes and Gross33 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | No differences between groups; no differences between completers and baseline sample |
| Rhodes and Gross33 | RCT | Not reported | Individual; Individual | No differences | Not reported | Complete case | No differences between groups; no differences between completers and baseline sample |
| Sacks et al.70 | RCT | Not reported | Individual; Individual | Yesa | Not reported | Complete case | No differences between groups at 6 mo or 12 mo |
| Scott and Dennis71 | RCT | Computer-generated sequence using grand urn | Individual; Individual | No differences | Target sample size was 425 for 80% power (2-tail), assuming 90% retention | Complete case | Not reported |
| Weir et al.72 | RCT | Computer-generated | Individual, numbers balanced within each block of 30; Individual | Yesa | Not reported | Complete case | No differences in attrition by group, no differences between completers and dropouts |
| Wolitski73 | Quasi-RCT | Assignment based on month of recruitment in 2 states and month of anticipated release in 2 states | Individual; Individual | Yes | Not reported | Complete case | No differences between dropouts and completers |
Note. GHB = gamma-hydroxybutyrate; RCT = randomized controlled trial.
Study reported explicit methods for handling baseline differences in outcome analyses.
TABLE 5—
Methodological Characteristics of Included Studies Evaluating Opioid Substitution Therapy Interventions in a Systematic Review of HIV Risk-Reduction Interventions in Incarceration and Community Settings
| Study | Study Design | Method of Randomization | Unit of Randomization; Unit of Analysis | Baseline Differences | Power Calculation | Type of Analysis | Results of Any Attrition Analyses |
| Bayanzadeh and Afshar44 | Quasi-RCT | Alternated row numbers in a list of participants, stratified by type of drug use | Individual; Individual | Yes | Not reported | Complete case | Not reported |
| Brown et al.46 | RCT | Not reported | Individual; Individual | No differences | Not reported | Could not be determined | Not reported |
| Cropsey et al.49 | RCT | Random numbers table | Individual; Individual | Yes | Not reported | ITT, no attrition | No attrition |
| Dolan et al.50 | RCT | Drew cards from an envelope | Individual, balanced within blocks of 10; Individual | No differences | Yes, powered to detect change in heroin use, not HIV or HCV; 90% power to detect a 23% difference in heroin use at P = .01 | Complete case | No, but attrition did not appear to differ between groups |
| Kinlock et al.58 | RCT | Not reported | Individual, balanced within each block of 9; Individual | No differences | Yes, 90% power to detect a small-to-medium effect size | Complete case | At 6 mo, dropouts had higher rates of self-reported heroin use 30 d before incarceration |
| Magura et al.62 | RCT | Prenumbered envelopes inside sealed envelopes | Individual; Individual | Yesa | Not reported | Per protocol | No differences between the 2 conditions in attrition |
| McKenzie et al.67 | RCT | Computer-generated urn randomization stratified by race and gender | Individual; Individual | No differences | Not reported | Per protocol | Not reported |
Note. ITT = intention to treat; RCT = randomized controlled trial.
Study reported explicit methods for handling baseline differences in outcome analyses.
TABLE 6—
Methodological Characteristics of Included Studies Evaluating HIV Testing Interventions in a Systematic Review of HIV Risk-Reduction Interventions in Incarceration and Community Settings
| Study | Study Design | Method of Randomization | Unit of Randomization; Unit of Analysis | Baseline Differences | Power Calculation | Type of Analysis | Results of Any Attrition Analyses |
| Gordon et al.8 | RCT | Computer-generated sequence | Individual; Individual | Yes | Not reported | ITT, no attrition | No attrition |
| Kavasery et al.57 | Quasi-RCT | Alternation | Individual; Individual | No differences | Not reported | ITT, dropouts were considered like test refusals | Dropouts were attributable to early release, and were more likely to have been incarcerated before |
| Kavasery56 | Quasi-RCT | Alternation | Individual; Individual | No differences | Yes, 80% power to detect 22% difference between arms given baseline uptake of 60% | ITT, dropouts were considered like test refusals | Dropouts were attributable to early release, and they had less opiate-positive results and were less likely to be jailed for drug or sexual offenses |
Note. ITT = intention to treat; RCT = randomized controlled trial.
Twenty-two of the 37 studies reported using a biological measure at baseline or any follow-up, most commonly urine testing for drug use (k = 12), hair testing for drug use (n = 2), unspecified testing for morphine (k = 1), a cervical swab for STIs (k = 1), oral testing for HIV (k = 1), and blood testing for HIV, hepatitis C, and other STIs (k = 5). Despite the fact that at least 6 studies conducted STI testing, however, only 4 studies reported HIV or STI incidence outcomes. Thirty-two studies assessed sexual or IDU behaviors; of those reporting methods of assessment, 2 studies used audio computer-assisted self-interviewing (ACASI), 5 used written questionnaires, and 23 used interviewer-administered questionnaires. Four studies did not report a sexual or IDU behavior, but assessed the proportion of participants who accepted HIV testing according to direct observation or medical records. Self-report measures of sexual behavior, IDU behavior, drug use, and recidivism varied and often appeared to be developed for individual studies, although several used assessments such as the Texas Christian University HIV/AIDS Risk Assessment, the HIV Risk-Taking Behavior Scale, the Criminal Justice Drug Abuse Treatment Studies intake form, the Timeline Followback approach for assessing substance use, and the National Institute on Drug Abuse Risk Behavior Assessment questionnaire; look-back periods for behavioral outcomes ranged from 14 days to 12 months, but typically were 1 to 3 months.
Outcomes
We report the results from primary trials in Table 7. Outcomes are defined here as short-term for assessments occurring less than 6 months from baseline, medium-term at 6 to 12 months from baseline, and long-term at 12 months or longer from baseline. Where a study reported multiple assessments in the same time category (e.g., 6 and 9 months), results from the longer follow-up are reported. For each outcome, we describe the number of trials reporting the outcome of interest, the maximum number of participants across trials retained at the follow-up assessments, statistically significant findings (P < .05) favoring intervention or control groups, and the number of participants represented in comparisons that reached statistical significance. We approximated the number of participants at follow-up for some studies with incomplete reporting; where these studies contribute to totals in this analysis, the total is expressed with a less-than-or-equal-to symbol (“≤”). Where a behavioral outcome was reported by 3 or fewer trials (e.g., sharing tattoo needles), it is not included here.
TABLE 7—
Study Outcomes and Number of Participants at Follow-Up Assessments for Sexual Behavior, Injection Drug Use Behavior, and HIV Testing in a Systematic Review of HIV Risk-Reduction Interventions in Incarceration and Community Settings
| Sexual Behavior |
Injection Drug Use Behavior |
HIV Testing |
||||||||||
| Study | No.a | Settingb | Controlc | Shortd | Medium | Long | Short | Medium | Long | Short | Medium | Long |
| Psychosocial interventions | ||||||||||||
| Alemagno et al.42 | 212 | Comm | Info | 163 | 109e | 163* | ||||||
| Baxter43 | 134 | Incarc | None | 94 | 134* | |||||||
| Braithwaite et al.45 | 116 | Incarc | UC | 116* | ||||||||
| Callahan47 | 204 | Comm | NE | 204 | ||||||||
| Callahan47 | 94 | Comm | NE | 94* | ||||||||
| Clarke et al.48,f | 245 | Both | None | |||||||||
| el-Bassel et al.51 | 159 | Both | Info | 100 | ||||||||
| Eldridge et al.52 | 117 | Comm | UC | 57* | ||||||||
| Fish et al.53 | 240 | Incarc | NE | 239 | ||||||||
| Grinstead et al.54 | 414 | Incarc | UC | ≤ 121* | ≤ 74 | |||||||
| Hser et al.55 | 100 | Both | UC | 94 | 94 | |||||||
| Leukefeld et al.59 | 444 | Both | Info | 344 | ||||||||
| Longshore et al.60 | 192 | Comm | Other | 134 | ||||||||
| Longshore et al.60 | 393 | Comm | Other | 329*,g | ||||||||
| Lurigio et al.61 | 99 | Comm | Attention | 50* | 50 | 50 | ||||||
| Martin and Scarpitti65 | 456 | Comm | UC | 119 | 119 | |||||||
| Martin et al.63 | 706 | Comm | NE | 420 | 420 | |||||||
| Martin et al.64 | 534 | Incarc | Info | 343* | ||||||||
| Marxhausen66 | 600 | Comm | Other | 294 | 229 | |||||||
| Needels et al.68 | 704 | Both | NE | Iatrogenic, 511 | ||||||||
| Prendergast et al.69 | 812 | Both | UC | 692 | 681 | |||||||
| Rhodes and Gross33 | 696 | Comm | Info | 513 | 561 | 513* | 561 | |||||
| Rhodes and Gross33 | 673 | Comm | Info | 571 | 568 | 574 | 568 | |||||
| Sacks et al.70 | 468 | Incarc | Other | 314* | 370 | 388 | 370 | |||||
| Scott and Dennis71 | 480 | Comm | UC | 462 | 462 | |||||||
| Weir et al.72 | 530 | Comm | NE | 391* | 446* | 391 | 446 | |||||
| Wolitski73 | 522 | Both | NE | 397 | 372* | 401e | 376e | |||||
| OST interventions | ||||||||||||
| Bayanzadeh and Afshar44 | 100 | Incarc | Other | 69 | 69* | |||||||
| Brown et al.46 | 15 | Comm | Other | 15* | ||||||||
| Cropsey et al.49 | 36 | Comm | Placebo | 36 | ||||||||
| Dolan et al.50 | 382 | Incarc | None | 253 | 253* | |||||||
| Kinlock et al.58 | 211 | Both | Other | 206 | 203 | 194 | 206 | 203 | 194 | |||
| Magura et al.62 | 133 | Incarc | Other | 81 | 81 | |||||||
| McKenzie et al.67 | 90 | Both | NE | 62 | ||||||||
| Testing interventions | ||||||||||||
| Gordon et al.8 | 697 | Comm | Other | 697* | ||||||||
| Kavasery et al.57 | 298 | Incarc | Other | 298* | ||||||||
| Kavasery et al.56 | 323 | Incarc | Other | 323* | ||||||||
Number of participants randomized at baseline.
Setting: Incarc = the intervention took place wholly in an incarceration setting; Comm = the intervention took place wholly in a community setting; Both = the intervention began in an incarceration setting and continued in the community.
Control groups: Attention = like the experimental group in time and format, but not focused on HIV; Info = information about HIV; NE = a lesser or nonenhanced version of the experimental intervention; None = no intervention; Other = another HIV prevention intervention; Placebo = a placebo; UC = usual care.
Short-term follow-up was defined as < 6 mo from baseline; medium-term was from 6 to < 12 mo, and long-term was 12 mo or longer.
Too few events occurred for meaningful analysis.
This study did not report group comparisons for behavioral outcomes; the outcome of relevance for this review was sexually transmitted infection incidence.
This effect was significant only among participants who reported high levels of baseline risk.
*Statistically significant effect at P < .05, in a direction favoring any intervention group over controls; iatrogenic = statistically significant effect at P < .05, in a direction favoring controls over the intervention group; results without an asterisk or “iatrogenic” next to the number of participants at follow-up did not reach statistical significance, given a significance level of P < .05.
Biological outcomes.
Three studies reported HIV infection outcomes, all at short-term follow-up (n = 456).41,50,55 All findings were nonsignificant with control groups including usual care,55 no treatment or waitlist,50 and information only.42 Two studies reported a measure of STI (n = 285),48,50 including hepatitis C virus incidence50 and time until a positive STI test,48 and both used no-treatment or waitlist controls. Group differences in STI measures were nonsignificant in both studies at short-, medium-, and long-term follow-up.
Sexual behavior.
Seventeen studies reported a measure of condomless sexual intercourse at any follow-up (n = 5219).42,47,55,58–60,63–65,68–73 Three studies (n = 1161) reported significant group differences favoring a peer-designed DVD intervention over a standard video at short- and medium-term follow-up,64 favoring motivational interventions focusing on HIV or HIV plus intimate partner violence over standard counseling and testing at short- and medium-term follow-up,72 and favoring a multisession individualized intervention over a single-session control.73 One study identified a significant difference in the opposite direction at long-term follow-up (n = 511),68 showing that women released from jail who received case management services after jail-based empowerment groups reported a significantly higher frequency of recent condomless sexual intercourse compared with participants who attended the empowerment groups without case management.
Eleven studies reported a measure of number of sexual partners (n = 3211).33,42,43,47,52,58,59,63,68 Only 1 study found a significant group difference (n = 94) at long-term follow-up, favoring the addition of a “well-woman” checkup and peer-led intervention to a testing and counseling intervention for women recruited from drug courts.47
Nine studies reported a measure of condom use (n ≤ 1220).33,42–44,52,54,55,61 Three studies reported evidence of a significant intervention benefit, all at short-term follow-up (n = 228). These results favored the addition of behavior skills training to a standard educational intervention for women court-ordered to drug treatment,52 favored a peer-led intervention over usual care for incarcerated men,54 and favored individual and small-group HIV education over an attention-matched control for adult probationers.61
Eight studies reported results by using a composite index of sexual risk behavior (n = 1185).43,45,46,51,52,62,66,70 Of these, 2 found a significant intervention benefit at any follow-up (n = 131). One trial among incarcerated men found that an educational intervention led by an HIV-negative peer was significantly more beneficial than usual care at short-term follow-up.45 The other trial was a pilot study enrolling n = 15 individuals from a jail diversion program: participants who received MMT or combination buprenorphine and naloxone at a specialist treatment facility for opioid-dependent individuals reported significantly safer behaviors at medium-term follow-up than participants who received buprenorphine and naloxone in a primary care setting.46
Six studies reported a measure of all sexual activity (compared with sexual abstinence; n ≤ 961).42,44,50,54,55,58 No study found a significant difference between experimental conditions at any time point, using a range of control groups that included information, usual care, no treatment, or an alternative HIV prevention intervention.
Six studies reported a measure of engagement in transactional sexual intercourse (n = 1637).47,55,63,68,70 Of these, only one found a significant benefit,70 showing that incarcerated women randomized to take part in a therapeutic community intervention for 6 months were less likely than participants in outpatient treatment to report having sexual intercourse in exchange for money or drugs at medium-term follow-up (n = 314). By contrast, 1 intervention found a significant iatrogenic effect at long-term follow-up (n = 511),68 finding that female jail releasees who received case management services and attended jail-based empowerment groups were more likely to report having sexual intercourse in exchange for money or drugs compared with controls who did not receive case management.
Five studies reported any measure of sexual intercourse under the influence of drugs or alcohol (n = 1289).42,58,60,68 One reported a significant intervention benefit at medium-term follow-up (n = 329),60 favoring case management using the Treatment Alternative to Street Crime model over alternative case management for drug-using probationers and parolees who reported a high baseline frequency of recent sexual intercourse under the influence. One trial reported a significant iatrogenic effect at long-term follow-up (n = 511),68 finding a higher frequency of recent sexual intercourse under the influence among female jail releasees who attended empowerment groups along with receiving case management, compared with controls who solely attended the empowerment groups.
Injection drug use behavior.
Seventeen studies reported a measure of self-reported incidence or frequency of IDU at any follow-up (n ≤ 4173).33,42–44,49,50,54,55,58,63,65–67,70,71,73 Of these, 3 studies found evidence of significant intervention benefit (n = 835); 2 of these were trials of MMT for incarcerated men. In one trial, men who received MMT reported a lower incidence and frequency of heroin and other drug injection at short-term follow-up compared with waitlist controls50; in the other trial, men receiving MMT also reported a lower incidence of IDU at medium-term follow-up compared with controls who received alternatives to MMT.44 The third trial found that participants who received 6 months of case management after arrest were less likely to report IDU compared with controls who viewed an educational video, as well as participants who viewed the video and received a single counseling session, but effects were not sustained at medium-term follow-up.33 Too few events occurred for meaningful analyses in 2 studies.42,73
Twelve studies reported a measure of self-reported needle sharing or use of sterile injection equipment (n ≤ 2605).33,42–44,50,54,55,58,61,62,72 Of these, 4 found a significant group difference at any time point (n = 1005). Three of these also reported significant benefits for incidence and frequency of IDU, described previously.33,44,50 The 2 trials of MMT for incarcerated men found that MMT recipients were less likely to report sharing IDU equipment at short-term follow-up compared with waitlist controls,50 and were less likely to report sharing IDU equipment at medium-term follow-up compared with controls who received other forms of drug treatment.44 The trial of case management found that participants who received case management were less likely than educational video recipients to share needles, even when the video viewers also received a single counseling session; also, among those who did share needles, case management recipients were more likely to clean needles before use than those who received the video without counseling.33 Similar to the results for the frequency of IDU, these effects were not sustained beyond short-term follow-up. The fourth study found that incarcerated participants who received HIV education and risk assessment reported sharing fewer types of drug use equipment than no-treatment controls.43 Too few events occurred for meaningful analysis in 1 study.42
HIV testing behavior.
Six studies (n = 1770) assessed interventions aiming to increase HIV testing behavior.8,42,53,56,57,61 Four found significant differences at short-term follow-up (n = 1481), favoring a computer-based intervention over written information,42 on-site testing at probation offices over off-site referrals,8 offering immediate or next-day testing over 1-week postponed testing for men entering jail,57 and offering next-day testing over immediate or 1-week postponed testing for women entering jail.56
Ancillary Outcomes
Drug use behavior.
Twenty-four studies reported an assessment of drug use at any follow-up (n ≤ 5874),33,44–47,49,50,52,54,55,58,60,62,63,65–71 including all 7 trials that tested OST strategies. Drug use data were derived from biological testing alone in 3 studies44,49,55 self-report alone in 17 studies,33,45–47,52,54,60,62,63,66,67,69–71 and both types of measures in 4 studies.50,58,65,68 Ten studies found a significantly favorable intervention effect at any time point (n = 1975), including 3 studies with a favorable intervention effect for a biological outcome assessment (n = 249).44,49,58 Programs showing benefit included 5 OST interventions, demonstrating evidence for MMT compared with waitlist controls at short-term follow-up,50 MMT compared with non-MMT treatment alternatives at medium-term follow-up44,58 and long-term follow-up,58 prerelease MMT compared with a postrelease MMT referral at medium- and long-term follow-up,58 postrelease MMT referral compared with controls receiving no referral at medium-term follow-up,58 buprenorphine compared with placebo at short-term follow-up,49 and prerelease MMT compared with postrelease referrals to funded community treatment.67
The other 5 trials with significant evidence of treatment benefit tested psychosocial interventions. One trial found significant benefit for an educational intervention led by HIV-positive peers compared with usual care at short-term follow-up.45 The results of another trial favored peer education and “well woman” checkups compared with HIV testing alone at long-term follow-up.47 Findings of a third trial favored case management using the Treatment Alternatives to Street Crime model compared with other case management services at medium-term follow-up, but only among probationers and parolees who reported using a larger number of drugs at baseline.60 A fourth trial found significant benefit for participation in a 6-month prerelease therapeutic community compared with outpatient treatment at medium- and long-term follow-up.70 The final trial found a benefit of case management services at short-term follow-up compared with a single-session counseling session with a video, and compared with viewing the video alone.33 In contrast to these studies, 1 study found a significant iatrogenic effect (n = 90): among participants who agreed to urine testing for drug use, parolees in Assertive Community Treatment case management were more likely to test positive than usual care controls.65
Recidivism.
Eleven studies measured reincarceration at any follow-up (n = 3687),33,50,58,62,65,67,68,70,71,73 of which 6 reported using a data source other than self-report (e.g., state records, study records of whether follow-up interviews took place in correctional facilities).33,62,67,70,73 Of the 11 studies, 3 found a significant group difference at any time point (n = 878). One found that participants who received prerelease MMT and counseling were less likely to report reincarceration at short-term but not medium-term follow-up, compared with participants who received postrelease MMT referral and counseling, and compared with participants who received counseling only.58 Another study found that participants who received case management were less likely to report reincarceration at short-term but not medium-term follow-up, compared with participants who watched an educational video with or without a single counseling session.33 Among participants in a third study who had been reincarcerated, those who had participated in a therapeutic community reported a longer time period before reincarceration occurred, compared with participants who received outpatient treatment.70 One study reported an iatrogenic effect (n = 414), finding that participants who received multiple pre- and postrelease counseling sessions on HIV and reentry were more likely than participants who received a single HIV risk-reduction session to self-report reincarceration at short-term follow-up; this effect disappeared at medium-term follow-up and may be explained by participant tracking strategies at 1 trial site.73
Ten studies measured recidivism by arrest at any follow-up (n = 3477),33,55,60,62,67–71 of which 5 reported using a data source other than self-report (e.g., state records).33,60,70,71 Of the 10 studies, 2 found significantly protective intervention effects at any follow-up (n = 899). One found that the addition of case management after HIV-related jail empowerment groups led to a reduced likelihood of arrest with serious charges at long-term follow-up, compared with participants who did not receive case management.68 The other trial evaluated a therapeutic community, and it found that the therapeutic community participants were less likely than outpatient participants to report overall arrest at medium- but not long-term follow-up, and less likely to report arrest for an offense other than parole violation at medium-term follow-up.70 One study found a significant iatrogenic effect (n = 378), suggesting that participants who received case management using the Treatment Alternatives to Street Crime model had more arrests according to probation records at medium-term follow-up, compared with participants who received case management that did not use that model.60
Seven studies reported any measure of recidivism by self-reported criminal activity at any follow-up (n = 2649).33,58,60,70,71 Of these, 3 found a significant difference between groups at any time point (n = 1157). One found that the addition of prerelease MMT to counseling led to significant reductions in frequency of criminal activity at short- and medium-term follow-up58; this study also found a benefit of prerelease MMT compared with a postrelease MMT referral at short-term follow-up. A second study found that participants who received 6 months of case management were less likely to report recent criminal activity at medium- but not short-term follow-up, compared with participants who viewed an educational video or who received both the video and a single counseling session.33 Finally, a third study found that participants who spent 6 months in a therapeutic community before release from incarceration were less likely to engage in criminal activity and drug-related activity at both medium- and long-term follow-up compared with participants in an intensive outpatient program.70
Intervention acceptability.
Ten studies reported information about intervention acceptability or participant satisfaction.42,44,50,51,52,55,58,59,61,62 Four assessed an OST intervention for drug treatment, and all found a low incidence of adverse events,50,58 high ratings for participant satisfaction with treatment,44,50 willingness to recommend the treatment to others,44 and a high proportion of participants who intended to remain on treatment in the future (which was higher among participants receiving buprenorphine compared with those receiving MMT).62 Among the 6 studies of psychosocial interventions that assessed acceptability, acceptability was also high according to satisfaction outcomes,53,59,61 and general descriptions of participant and staff reception.42,51,55
Intervention costs.
Five trials commented on intervention cost.42,54,63,72,73 Two trials noted that staff training and time may be comparatively costly for psychosocial interventions delivered in a one-on-one format,63,72 and 2 trials noted potential cost savings associated with a peer-led intervention for incarcerated men54 and a computer-based intervention for a mixed-gender sample of individuals on probation.42 A formal cost assessment was available for only 1 study, which found that a multisession intervention with services in both correctional facilities and the community cost approximately $1830 per participant (2009 dollars), whereas a single-session prerelease intervention cost approximately $690 per person.73 The authors concluded that the multisession intervention would be cost-effective if it prevented 1 HIV transmission per 753 participants released from prison.
DISCUSSION
Reducing the risk of HIV infection is a critical priority for adult populations with criminal justice involvement, given overlapping risks such as IDU and noninjection drug use, transactional sexual intercourse, condomless sexual intercourse, high rates of STI, and inadequate access to HIV prevention and other medical services. The past few decades have brought intervention efforts in both community and incarceration settings, via modalities such as OST, case management, counseling and HIV testing, media-based interventions, peer-led interventions, and motivational interviewing, but these have not yet been aggregated in a systematic review. In this review, we assessed descriptive information, methodological details, and results of 37 randomized and quasirandomized controlled trials of interventions that aimed to prevent HIV among adults with criminal justice involvement.
Our analysis suggests that although many interventions do not appear to influence behavioral or biological outcomes in this population (when compared with various controls, many of which also included some HIV prevention services), a range of intervention options show promise. We identified 11 trials demonstrating a significant protective effect of an intervention on a measure of sexual risk behavior,45–47,52,54,60,61,64,70,72,73 4 trials demonstrating a significant benefit for HIV risk behaviors related to IDU behavior,33,43,44,50 and 4 trials demonstrating ways to maximize the uptake of HIV testing services in this population.8,42,56,57 No intervention has yet demonstrated a benefit for both a sexual and an IDU behavior, despite the efforts of 18 trials that reported results in both categories.33,42–44,50,54,55,56,61–63,65,66,70–73 Biological outcomes were underreported, and no study reported a significant program effect on HIV or STI at follow-up. Although several studies identified iatrogenic effects on 1 or more outcomes,60,65,68,73 it does not appear that HIV risk-reduction efforts in this population cause systemic harm; these effects were often explained in primary trials as isolated or chance findings.
Because data limitations prevented a meta-analysis, we cannot comment with certainty on mediators, moderators, or the core program components responsible for program effects. Data on individual program effects should also be interpreted with the control group in mind. These trials, however, offer a variety of intervention options for service providers in different settings. Of particular interest are the 15 interventions that demonstrably reduced self-reported sexual or IDU-related risk behavior compared with controls.33,43–47,50,52,54,60,61,64,70,72,73 Eight of these programs were delivered all or in part in incarceration settings before release43–45,50,54,64,70,73; effective programs for all-male samples included prerelease MMT,44,50 peer-led HIV education programs using an individual54 or group45 format, and motivational interviewing with sessions before and after community reentry.73 For incarcerated mixed-gender or all-female samples, protective effects were observed for several psychosocial programs, including a DVD program developed by peers,64 a 6-month therapeutic community for drug-using incarcerated women,70 and an educational program delivered by health educators.43 Among programs delivered solely outside incarceration settings, 7 trials showed evidence of benefit for mixed-gender and all-female samples after arrest, under community supervision, and in court-ordered residential drug treatment.33,46,47,52,60,61,72 Effective interventions included several types of case management33,60; one-on-one or group-based HIV education delivered by peer leaders47 or health educators52,61,72; services integrating HIV prevention with medical checkups47 or intimate partner violence intervention72; and a pilot study comparing specialized drug treatment to treatment in primary care.46
We concur with previous systematic reviews suggesting that OST in prison may reduce drug-related22 and HIV-related risks.23,29 We also agree with reviews suggesting the effectiveness of certain behavioral interventions in this group.20,21 Our results overlap with a large review of randomized and nonrandomized studies of HIV prevention efforts in prison settings, including voluntary testing, condom provision, needle-exchange programs, bleach programs, safe tattooing initiatives, OST, drug-free units, and drug supply reduction.3 Because correctional policies may be unsupportive of structural interventions in incarceration settings, such as condom provision, needle-exchange initiatives, and bleach programs, we note that this review did not identify any trials of these approaches. This does not mean that such programs are ineffective; to the contrary, previous empirical research suggests that these initiatives are feasible, do not threaten security, and lead to greater use of condoms and sterile injection equipment in prison settings.3 Our review of this literature would support policy modifications to enable a wider variety of HIV prevention efforts, integrating structural interventions alongside psychosocial programs, drug treatment, and larger societal efforts to reduce the impact of incarceration and criminal justice involvement on individuals and communities at risk for HIV.
Strengths
This review has many strengths. To our knowledge, this is the first systematic review to synthesize evidence of effectiveness for all HIV risk-reduction interventions serving adults with criminal justice involvement. We limited this review to the evidence most appropriate for demonstrating causal effects by including only randomized and quasi-randomized controlled trials; we also limited our review to the most relevant outcome data through our exclusive focus on behavioral and biological outcomes, rather than HIV knowledge or attitudinal outcomes. Our search for trial evidence was highly sensitive, without limits for language, date, participant age, geography, or study design terms.
To our knowledge, we are among the first in this area to search not only databases of public health literature, but also databases of criminal justice scholarship (e.g., Criminal Justice Abstracts, National Criminal Justice Reference Service). These databases contributed 4773 unique citations to our search and yielded 1 primary article encompassing 2 studies,60 as well as 2 supplemental reports.103,105 We add to previous literature by including data on intervention acceptability, cost, and outcomes such as drug use and recidivism.
Generalizability and Limitations
Several limitations affect the generalizability of findings. Despite our international search, we found only 3 studies outside the United States. Variation across correctional systems and state or federal laws may limit the generalizability of these results to non-US settings, and even from 1 US state to another. Thus, although some of these effective interventions may be transferable to other locations, it will be important to investigate feasibility and acceptability before doing so. The characteristics of participants in the included trials may also limit generalizability in some scenarios; for example, 6 trials enrolled primarily White participants; 9 and 12 trials were limited to female or male participants, respectively; participants’ criminal justice involvement (where reported) derived from property and drug-related crimes; and average ages across trials had a mean of 34.5 years (which may limit generalizability to younger samples). Data limitations prevented a meta-analysis, which hampered our ability to conduct subgroup analyses by participant and intervention characteristics. Publication bias is an unavoidable limitation of systematic reviewing, and we may have missed unpublished or ongoing trials; we also did not include studies indexed after January 2014. We did not control for the use of multiple statistical tests: this review reports the results of 358 statistical tests, of which 75 reached statistical significance in either direction at a level of P < .05.
This review is also challenged by methodological weaknesses and underreporting across primary trials, particularly missing information about method of randomization, concealment of the allocation sequence from recruitment staff, blinding of outcome assessors, impacts and sources of attrition, sample size calculations, fidelity of program implementation, and intervention acceptability and costs. With the complexity of reporting results in a narrative format, we chose to report methodological details and study outcomes separately, rather than organizing our presentation of results according to methodological quality; a meta-analysis would have facilitated a more integrated approach. Incomplete outcome reporting is a key concern for this review, particularly for biological outcomes such as HIV and STI testing. Self-reported outcome data are an inevitable limitation of sexual behavior results; we also note that, despite several studies that used biological outcomes for the assessment of drug use, biological assessments were underused, and no study used biological outcomes to measure injection behaviors (e.g., inspection for injection stigmata). The limitations of self-reported data are well-known,108,109 but these results may still be useful for the assessment of drug use and sexual behavior.110–112
Future Research
Areas for future research.
Many studies in this review found evidence of reductions in sexual and IDU-related HIV risk behaviors among adults with criminal justice involvement. But we lack an understanding of the program elements that may drive these effects, and there is little guidance to understand how participant characteristics, implementation fidelity, and features of the intervention setting may influence program effectiveness. In light of the promising outcomes of 5 peer-led interventions for reducing sexual risk behavior,45,47,54,64,70 especially in incarceration settings, further research might consider the mechanisms by which peer intervention influences behavior among parolees, probationers, and incarcerated adults. Peer education programs may also reduce disciplinary infractions among peer educators themselves, suggesting multiple types of benefits in incarceration settings.113 Interventions that reduce both sexual risk and risks related to IDU should also be a priority, and the results of this review suggest that combining OST with HIV-related psychosocial interventions may be a promising direction. Moreover, there is little information available to guide service providers seeking to implement evidence-based interventions for this population; ongoing research should incorporate process evaluations and prioritize data on program acceptability, cost, and strategies for adapting or transferring effective interventions.
Several populations appear to be underrepresented in the research base to date. Research in non-US settings using randomized or quasi-randomized methods, particularly in low- and middle-income countries, would be an important addition to the evidence base on HIV prevention for adults with criminal justice involvement. Additional studies are also needed to expand HIV prevention efforts for sexual minority adults in this population; research has documented high STI risk among men who have sex with men in incarceration settings,114,115 but this review identified no trials of HIV prevention efforts in this subpopulation. Comparatively few studies have investigated HIV prevention efforts in drug courts or compulsory residential drug treatment, presenting another avenue for future work. Almost every trial tested an individually focused intervention, but several interventions mobilized family support through family education44 or a prerelease conference call.69 Given the linkages between relationship stability and risk among adults with criminal justice involvement and their partners,2,12,116 there is an opportunity for further efforts to integrate partners and families. We also did not identify any randomized trials testing structural interventions such as needle exchange programs24,27 or segregation of sexual-minority inmates in incarceration settings.114,117
Finally, additional research may seek to integrate lessons from psychosocial HIV prevention, OST, and advances in biomedical HIV prevention (e.g., PrEP, postexposure prophylaxis, male circumcision). No randomized study has yet examined the effectiveness of a biomedical HIV prevention strategy in this population. Given findings in this review showing promise for OST in this population, as well as recent evidence that antiretroviral PrEP can reduce HIV risk among people who inject drugs,38 future research may identify opportunities for clinical interventions combining drug treatment with biomedical HIV prevention technologies such as PrEP or postexposure prophylaxis. Initiating these combinations may be appropriate for incarcerated individuals before or immediately after release, as the time immediately following release from incarceration may be a particularly risky period for HIV exposure.
Methodological recommendations for future research.
Our results identify many ways to improve the design and reporting of future research. Although conducting randomized trials in incarceration settings is challenging, these examples demonstrate that randomization is feasible in some facilities. For trials that use random assignment, we urge more complete reporting of methodological details such as method of randomization, method of concealing allocation sequence from recruitment personnel, and methods of blinding outcome assessors. When randomized trials take place in a single facility, there is a heightened possibility for contamination across trial arms because of information sharing among participants in intervention and control groups. Multisite evaluations are logistically complicated in this context,118 but multisite studies that randomize entire facilities to treatment conditions may minimize contamination issues. Future trials should make every effort to use and report biological endpoints, including testing for HIV, hepatitis C, other STIs, and drug use; although testing is expensive for individual trials, research funders and HIV prevention research networks could make concerted efforts to support the use of these measures. Even if results for an individual study are prone to floor effects, improved reporting of biological endpoints will facilitate efforts to aggregate results across studies—particularly if other sources of underreporting such as methodological details and outcome data are corrected.
Because incomplete outcome reporting was observed, we encourage trialists to report group comparisons for all outcomes at every follow-up, including group sizes, means, standard deviations, and number of dichotomous events. Where possible, analyses of trial data should account for dropouts, cluster randomization, and baseline differences. Relatively few trials used ACASI methods for assessing behavioral outcomes, and we encourage the use of ACASI as a potential strategy for limiting self-report bias,119–123 although we recognize its limitations124–126 and potential logistical barriers to its use in incarceration settings. We also encourage the use of standardized and previously validated measures for sexual behavior, IDU behavior, and drug use activity, both to improve internal validity and to facilitate the aggregation of results in meta-analyses.
Acknowledgments
This review did not receive external funding. The review was conceptualized and begun while K. Underhill was a postdoctoral fellow at Brown University and supported by National Institute on Alcohol Abuse and Alcoholism grant 5T32 AA07459-24 (Ruth L. Kirschstein National Service Research Award). The review was concluded while K. Underhill received salary support from National Institute of Mental Health grant 5K01MH093273. We are grateful for internal support from the Brown/Tufts/Lifespan Center for AIDS Research and the Yale Center for Interdisciplinary Research on AIDS.
We are also grateful to Josiah Rich, MD, MPH, for his advance review and helpful suggestions for revision, and we thank the anonymous peer reviewers for additional feedback.
Human Participant Protection
This is a systematic review of the literature; there were no human participants. No institutional review board review was required.
References
- 1.Braithwaite RL, Arriola KR. Male prisoners and HIV prevention: a call for action ignored. Am J Public Health. 2008;98(suppl 1):S145–S149. doi: 10.2105/ajph.98.supplement_1.s145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blankenship KM, Smoyer AB. Between spaces: understanding movement to and from prison as an HIV risk factor. In: Sanders B, Thomas YF, Deeds BG, editors. Crime, HIV and Health: Intersections of Criminal Justice and Public Health Concerns. New York, NY: Springer; 2013. pp. 207–221. [Google Scholar]
- 3.Effectiveness of Interventions to Address HIV in Prisons. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS, World Health Organization, and United Nations Office on Drugs and Crime; 2007. [Google Scholar]
- 4.Beckwith CG, Zaller ND, Fu JJ, Montague BT, Rich JD. Opportunities to diagnose, treat, and prevent HIV in the criminal justice system. J Acquir Immune Defic Syndr. 2010;55(suppl 1):S49–S55. doi: 10.1097/QAI.0b013e3181f9c0f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Spaulding AC, Seals RM, Page MJ, Brzozowski AK, Rhodes W, Hammett TM. HIV/AIDS among inmates of and releasees from US correctional facilities, 2006: declining share of epidemic but persistent public health opportunity. PLoS ONE. 2009;4(11):e7558. doi: 10.1371/journal.pone.0007558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dolan K, Kite B, Black E, Aceijas C, Stimson GV. HIV in prison in low-income and middle-income countries. Lancet Infect Dis. 2007;7(1):32–41. doi: 10.1016/S1473-3099(06)70685-5. [DOI] [PubMed] [Google Scholar]
- 7.HIV in Prisons: Situation and Needs Assessment Toolkit. Vienna, Austria: United Nations Office on Drugs and Crime; 2010. [Google Scholar]
- 8.Gordon MS, Kinlock TW, McKenzie M, Wilson ME, Rich JD. Rapid HIV testing for individuals on probation/parole: outcomes of an intervention trial. AIDS Behav. 2013;17(6):2022–2030. doi: 10.1007/s10461-013-0456-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Belenko S, Langley S, Crimmins S, Chaple M. HIV risk behaviors, knowledge, and prevention education among offenders under community supervision: a hidden risk group. AIDS Educ Prev. 2004;16(4):367–385. doi: 10.1521/aeap.16.4.367.40394. [DOI] [PubMed] [Google Scholar]
- 10.Green TC, Pouget ER, Harrington M et al. Limiting options: sex ratios, incarceration rates, and sexual risk behavior among people on probation and parole. Sex Transm Dis. 2012;39(6):424–430. doi: 10.1097/OLQ.0b013e318254c81a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adams LM, Kendall S, Smith A, Quigley E, Stuewig JB, Tangney JP. HIV risk behaviors of male and female jail inmates prior to incarceration and one year post-release. AIDS Behav. 2013;17(8):2685–2694. doi: 10.1007/s10461-011-9990-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Khan MR, Behrend L, Adimora AA, Weir SS, Tisdale C, Wohl DA. Dissolution of primary intimate relationships during incarceration and associations with post-release STI/HIV risk behavior in a Southeastern city. Sex Transm Dis. 2011;38(1):43–47. doi: 10.1097/OLQ.0b013e3181e969d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luther JB, Reichert ES, Holloway ED, Roth AM, Aalsma MC. An exploration of community reentry needs and services for prisoners: a focus on care to limit return to high-risk behavior. AIDS Patient Care STDS. 2011;25(8):475–481. doi: 10.1089/apc.2010.0372. [DOI] [PubMed] [Google Scholar]
- 14.Pollack H, Khoshnood K, Altice F. Health care delivery strategies for criminal offenders. J Health Care Finance. 1999;26(1):63–77. [PubMed] [Google Scholar]
- 15.Epperson MW, El-Bassel N, Chang M, Gilbert L. Examining the temporal relationship between criminal justice involvement and sexual risk behaviors among drug-involved men. J Urban Health. 2010;87(2):324–336. doi: 10.1007/s11524-009-9429-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams J, Nowels C, Corsi K, Long J, Steiner JF, Binswanger IA. HIV risk after release from prison: a qualitative study of former inmates. J Acquir Immune Defic Syndr. 2011;57(5):429–434. doi: 10.1097/QAI.0b013e31821e9f41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seal DW, Eldrige GD, Kacanek D, Binson D, Macgowan RJ. A longitudinal, qualitative analysis of the context of substance use and sexual behavior among 18- to 29-year-old men after their release from prison. Soc Sci Med. 2007;65(11):2394–2406. doi: 10.1016/j.socscimed.2007.06.014. [DOI] [PubMed] [Google Scholar]
- 18.Gough E, Kempf MC, Graham L et al. HIV and hepatitis B and C incidence rates in US correctional populations and high risk groups: a systematic review and meta-analysis. BMC Public Health. 2010;10:777. doi: 10.1186/1471-2458-10-777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glaze LE, Parks E. Correctional Populations in the United States, 2011. Washington, DC: US Department of Justice; 2012. [Google Scholar]
- 20.Oser CB, Harland Harp KL, Staton-Tindall M. Handbook of Evidence-Based Substance Abuse Treatment in Criminal Justice Settings. Vol. 11. New York, NY: Springer; 2011. Drug abuse HIV/AIDS interventions in criminal justice settings; pp. 293–309. [Google Scholar]
- 21.Hammett TM, Gaiter JL, Crawford C. Reaching seriously at-risk populations: health interventions in criminal justice settings. Health Educ Behav. 1998;25(1):99–120. doi: 10.1177/109019819802500108. [DOI] [PubMed] [Google Scholar]
- 22.Hedrich D, Alves P, Farrell M, Stöver H, Møller L, Mayet S. The effectiveness of opioid maintenance treatment in prison settings: a systematic review. Addiction. 2012;107(3):501–517. doi: 10.1111/j.1360-0443.2011.03676.x. [DOI] [PubMed] [Google Scholar]
- 23.Larney S. Does opioid substitution treatment in prisons reduce injecting-related HIV risk behaviours? A systematic review. Addiction. 2010;105(2):216–223. doi: 10.1111/j.1360-0443.2009.02826.x. [DOI] [PubMed] [Google Scholar]
- 24.Dolan K, Rutter S, Wodak AD. Prison-based syringe exchange programmes: a review of international research and development. Addiction. 2003;98(2):153–158. doi: 10.1046/j.1360-0443.2003.00309.x. [DOI] [PubMed] [Google Scholar]
- 25.Stallwitz A, Stover H. The impact of substitution treatment in prisons—a literature review. Int J Drug Policy. 2007;18(6):464–474. doi: 10.1016/j.drugpo.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 26.Springer SA, Azar MM, Altice FL. HIV, alcohol dependence, and the criminal justice system: a review and call for evidence-based treatment for released prisoners. Am J Drug Alcohol Abuse. 2011;37(1):12–21. doi: 10.3109/00952990.2010.540280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lines R, Jurgens R, Betteridge G, Stover H, Laticevschi D, Nelles J. Prison Needle Exchange: Lessons From a Comprehensive Review of International Evidence and Experience. Toronto, Ontario: Canadian HIV/AIDS Legal Network; 2004. [Google Scholar]
- 28.Lichtenstein B, Malow R. A critical review of HIV-related interventions for women prisoners in the United States. J Assoc Nurses AIDS Care. 2010;21(5):380–394. doi: 10.1016/j.jana.2010.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jürgens R, Ball A, Verster A. Interventions to reduce HIV transmission related to injecting drug use in prison. Lancet Infect Dis. 2009;9(1):57–66. doi: 10.1016/S1473-3099(08)70305-0. [DOI] [PubMed] [Google Scholar]
- 30.Jahanfar S, Myers J. Harm reduction interventions to prevent HIV/AIDS transmission in involuntary detainees. Cochrane Database Syst Rev. 2007 (3)(CD006737) [Google Scholar]
- 31.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. Oxford, England: The Cochrane Collaboration; 2011. [Google Scholar]
- 32.Underhill K, Operario D, Dumont D. Interventions for HIV prevention in non-incarcerated criminal justice-involved populations. Cochrane Database Syst Rev. In press. [Google Scholar]
- 33.Rhodes W, Gross M. Case Management Reduces Drug Use and Criminality Among Drug-Involved Arrestees: An Experimental Study of an HIV Prevention Intervention. Rockville, MD: National Institute of Justice and National Institute on Drug Abuse; 1997. [Google Scholar]
- 34.Denison JA, O’Reilly KR, Schmid GP, Kennedy CE, Sweat MD. HIV voluntary counseling and testing and behavioral risk reduction in developing countries: a meta-analysis, 1990–2005. AIDS Behav. 2008;12(3):363–373. doi: 10.1007/s10461-007-9349-x. [DOI] [PubMed] [Google Scholar]
- 35.Weinhardt LS, Carey MP, Johnson BT, Bickham NL. Effects of HIV counseling and testing on sexual risk behavior: a meta-analytic review of published research, 1985–1997. Am J Public Health. 1999;89(9):1397–1405. doi: 10.2105/ajph.89.9.1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Eaton LA, Huedo-Medina TB, Kalichman SC et al. Meta-analysis of single-session behavioral interventions to prevent sexually transmitted infections: implications for bundling prevention packages. Am J Public Health. 2012;102(11):e34–e44. doi: 10.2105/AJPH.2012.300968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Grant RM, Lama JR, Anderson PL et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choopanya K, Martin M, Suntharasamai P et al. Antiretroviral prophylaxis for HIV infection in injecting drug users in Bangkok, Thailand (the Bangkok Tenofovir Study): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2013;381(9883):2083–2090. doi: 10.1016/S0140-6736(13)61127-7. [DOI] [PubMed] [Google Scholar]
- 39.Baeten JM, Donnell D, Ndase P et al. Antiretroviral prophylaxis for HIV prevention in heterosexual men and women. N Engl J Med. 2012;367(5):399–410. doi: 10.1056/NEJMoa1108524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Preexposure Prophylaxis for the Prevention of HIV Infection in the United States 2014: A Clinical Practice Guideline. Atlanta, GA: Centers for Disease Control and Prevention; 2014. [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff J, Altman DG The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(6):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alemagno SA, Stephens RC, Stephens P, Shaffer-King P, White P. Brief motivational intervention to reduce HIV risk and to increase HIV testing among offenders under community supervision. J Correct Health Care. 2009;15(3):210–221. doi: 10.1177/1078345809333398. [DOI] [PubMed] [Google Scholar]
- 43.Baxter S. AIDS education in the jail setting. Crime Delinq. 1991;37(1):48–63. [Google Scholar]
- 44.Bayanzadeh SA, Afshar P. Final Report of Research Project: A Study of the Effectiveness of Psychopharmacological and Psychological Interventions in Reducing Harmful/High Risk Behaviors Among Substance User Prisoners. Tehran, Iran: United Nations Office on Drugs and Crime; 2004. [Google Scholar]
- 45.Braithwaite RL, Stephens TT, Treadwell HM, Braithwaite K, Conerly R. Short-term impact of an HIV risk reduction intervention for soon-to-be released inmates in Georgia. J Health Care Poor Underserved. 2005;16(4, suppl B):130–139. doi: 10.1353/hpu.2005.0111. [DOI] [PubMed] [Google Scholar]
- 46.Brown R, Gassman M, Hetzel S, Berger L. Community-based treatment for opioid dependent offenders: a pilot study. Am J Addict. 2013;22(5):500–502. doi: 10.1111/j.1521-0391.2013.12049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Callahan C. The Association of Criminal Justice System Involvement on Change in High-Risk Behaviors Among Urban, Crack-Cocaine Using Women [doctoral thesis] St Louis, MO: George Warren Brown School of Social Work, Graduate School of Arts and Sciences of Washington University; 2008. [Google Scholar]
- 48.Clarke JG, Anderson BJ, Stein MD. Hazardously drinking women leaving jail: time to first drink. J Correct Health Care. 2011;17(1):61–68. doi: 10.1177/1078345810385915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cropsey KL, Lane PS, Hale GJ et al. Results of a pilot randomized controlled trial of buprenorphine for opioid dependent women in the criminal justice system. Drug Alcohol Depend. 2011;119(3):172–178. doi: 10.1016/j.drugalcdep.2011.06.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dolan KA, Shearer J, White B, Zhou J, Kaldor J, Wodak AD. Four-year follow-up of imprisoned male heroin users and methadone treatment: mortality, re-incarceration and hepatitis C infection. Addiction. 2005;100(6):820–828. doi: 10.1111/j.1360-0443.2005.01050.x. [DOI] [PubMed] [Google Scholar]
- 51.el-Bassel N, Ivanoff A, Schilling RF, Gilbert L, Borne D, Chen DR. Preventing HIV/AIDS in drug-abusing incarcerated women through skills building and social support enhancement: preliminary outcomes. Soc Work Res. 1995;19(3):131–141. [PubMed] [Google Scholar]
- 52.Eldridge GD, St Lawrence JS, Little CE et al. Evaluation of the HIV risk reduction intervention for women entering inpatient substance abuse treatment. AIDS Educ Prev. 1997;9(1, suppl):62–76. [PubMed] [Google Scholar]
- 53.Fish DG, Walker SJ, Singaravelu K et al. Improving knowledge, attitudes, and testing for communicable diseases among New York State inmates. J Correct Health Care. 2008;14(4):290–298. [Google Scholar]
- 54.Grinstead OA, Zack B, Faigeles B, Grossman N, Blea L. Reducing postrelease HIV risk among male prison inmates: a peer-led intervention. Crim Justice Behav. 1999;26(4):453–465. [Google Scholar]
- 55.Hser YI, Fu L, Wu F, Du J, Zhao M. Pilot trial of a recovery management intervention for heroin addicts released from compulsory rehabilitation in China. J Subst Abuse Treat. 2013;44(1):78–83. doi: 10.1016/j.jsat.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kavasery R, Maru DS, Cornman-Homonoff J, Sylla LN, Smith D, Altice FL. Routine opt-out HIV testing strategies in a female jail setting: a prospective controlled trial. PLoS ONE. 2009;4(11):e7648. doi: 10.1371/journal.pone.0007648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kavasery R, Maru DS, Sylla LN, Smith D, Altice FL. A prospective controlled trial of routine opt-out HIV testing in a men’s jail. PLoS ONE. 2009;4(11):e8056. doi: 10.1371/journal.pone.0008056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kinlock TW, Gordon MS, Schwartz RP, O’Grady K, Fitzgerald TT, Wilson M. A randomized clinical trial of methadone maintenance for prisoners: results at 1-month post-release. Drug Alcohol Depend. 2007;91(2-3):220–227. doi: 10.1016/j.drugalcdep.2007.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leukefeld C, Havens J, Tindall MS et al. Risky relationships: targeting HIV prevention for women offenders. AIDS Educ Prev. 2012;24(4):339–349. doi: 10.1521/aeap.2012.24.4.339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Longshore D, Turner S, Anglin MD. Effects of case management on drug users’ risky sex. Prison J. 1998;78(1):6–30. [Google Scholar]
- 61.Lurigio AJ, Petraitis J, Johnson BR. Joining the front line against HIV: an education program for adult probationers. AIDS Educ Prev. 1992;4(3):205–218. [PubMed] [Google Scholar]
- 62.Magura S, Lee JD, Hershberger J et al. Buprenorphine and methadone maintenance in jail and post-release: a randomized clinical trial. Drug Alcohol Depend. 2009;99(1-3):222–230. doi: 10.1016/j.drugalcdep.2008.08.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Martin SS, O’Connell DJ, Inciardi JA, Surratt HL, Beard RA. HIV/AIDS among probationers: an assessment of risk and results from a brief intervention. J Psychoactive Drugs. 2003;35(4):435–443. doi: 10.1080/02791072.2003.10400490. [DOI] [PubMed] [Google Scholar]
- 64.Martin SS, O’Connell DJ, Inciardi JA, Surratt HL, Maiden KM. Integrating an HIV/HCV brief intervention in prisoner reentry: results of a multisite prospective study. J Psychoactive Drugs. 2008;40(4):427–436. doi: 10.1080/02791072.2008.10400649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martin SS, Scarpitti FR. An intensive case management approach for paroled IV drugs users. J Drug Issues. 1993;23(1):43–59. [Google Scholar]
- 66.Marxhausen JL. Effects of a Peer-Driven HIV/HCV Intervention Program With Reentering Drug Offenders. Ann Arbor, MI: Walden University; 2013. [Google Scholar]
- 67.McKenzie M, Zaller N, Dickman SL et al. A randomized trial of methadone initiation prior to release from incarceration. Subst Abus. 2012;33(1):19–29. doi: 10.1080/08897077.2011.609446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Needels K, James-Burdumy S, Burghardt J. Community case management for former jail inmates: its impacts on rearrest, drug use, and HIV risk. J Urban Health. 2005;82(3):420–433. doi: 10.1093/jurban/jti092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Prendergast M, Frisman L, Sacks JY et al. A multi-site, randomized study of strengths-based case management with substance-abusing parolees. J Exp Criminol. 2011;7(3):225–253. doi: 10.1007/s11292-011-9123-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sacks JY, Sacks S, McKendrick K et al. Prison therapeutic community treatment for female offenders: profiles and preliminary findings for mental health and other variables (crime, substance use and HIV risk) J Offender Rehabil. 2008;46(3-4):233–261. [Google Scholar]
- 71.Scott CK, Dennis ML. The first 90 days following release from jail: findings from the Recovery Management Checkups for Women Offenders (RMCWO) experiment. Drug Alcohol Depend. 2012;125(1-2):110–118. doi: 10.1016/j.drugalcdep.2012.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Weir BW, O’Brien K, Bard RS et al. Reducing HIV and partner violence risk among women with criminal justice system involvement: a randomized controlled trial of two motivational interviewing-based interventions. AIDS Behav. 2009;13(3):509–522. doi: 10.1007/s10461-008-9422-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wolitski RJ. Relative efficacy of a multisession sexual risk-reduction intervention for young men released from prisons in 4 states. Am J Public Health. 2006;96(10):1854–1861. doi: 10.2105/AJPH.2004.056044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Daniels J, Crum M, Ramaswamy M, Freudenberg N. Creating REAL MEN: description of an intervention to reduce drug use, HIV risk, and rearrest among young men returning to urban communities from jail. Health Promot Pract. 2011;12(1):44–54. doi: 10.1177/1524839909331910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Dolan KA, Shearer J, MacDonald M, Mattick RP, Hall W, Wodak AD. A randomised controlled trial of methadone maintenance treatment versus wait list control in an Australian prison system. Drug Alcohol Depend. 2003;72(1):59–65. doi: 10.1016/s0376-8716(03)00187-x. [DOI] [PubMed] [Google Scholar]
- 76.Gordon MS, Kinlock TW, Schwartz RP, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: findings at 6 months post-release. Addiction. 2008;103(8):1333–1342. doi: 10.1111/j.1360-0443.2008.002238.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Inciardi JA, Surratt HL, Martin SS, O’Connell DJ, Salandy AD, Beard RA. Developing a multimedia HIV and hepatitis intervention for drug-involved offenders reentering the community. Prison J. 2007;87(1):111–142. [Google Scholar]
- 78.Kinlock TW, Gordon MS, Schwartz RP, Fitzgerald TT, O’Grady KE. A randomized clinical trial of methadone maintenance for prisoners: results at 12 months postrelease. J Subst Abuse Treat. 2009;37(3):277–285. doi: 10.1016/j.jsat.2009.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kinlock TW, Gordon MS, Schwartz RP, O’Grady KE. A study of methadone maintenance for male prisoners: 3-month postrelease outcomes. Crim Justice Behav. 2008;35(1):34–47. doi: 10.1177/0093854807309111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Leukefeld C, Roberto H, Hiller M, Webster M, Logan TK, Staton-Tindall M. HIV prevention among high-risk and hard-to-reach rural residents. J Psychoactive Drugs. 2003;35(4):427–434. doi: 10.1080/02791072.2003.10400489. [DOI] [PubMed] [Google Scholar]
- 81.Sacks JY, McKendrick K, Hamilton Z. A randomized clinical trial of a therapeutic community treatment for female inmates: outcomes at 6 and 12 months after prison release. J Addict Dis. 2012;31(3):258–269. doi: 10.1080/10550887.2012.694601. [DOI] [PubMed] [Google Scholar]
- 82.Sosman J, Macgowan R, Margolis A et al. Sexually transmitted infections and hepatitis in men with a history of incarceration. Sex Transm Dis. 2011;38(7):634–639. doi: 10.1097/OLQ.0b013e31820bc86c. [DOI] [PubMed] [Google Scholar]
- 83. Vemulapalli CF, Callahan C, Ben Abdallah A, Cottler LB. Deconstructing HIV prevention interventions among drug abusing female offenders: preliminary results of long-term follow-up efforts. Poster presentation at: the 68th Annual Scientific Meeting of the College on Problems of Drug Dependence; June 17–22, 2006; Scottsdale, AZ.
- 84.Wilson ME, Kinlock TW, Gordon MS, O’Grady KE, Schwartz RP. Postprison release HIV-risk behaviors in a randomized trial of methadone treatment for prisoners. Am J Addict. 2012;21(5):476–487. doi: 10.1111/j.1521-0391.2012.00250.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Wolitski RJ, Project START Study Group. Project START reduces HIV risk among prisoners after release. Oral presentation at: XV International AIDS Conference; July 14, 2004; Bangkok, Thailand.
- 86.Rhodes AG, Taxman FS, Friedmann PD, Cropsey KL. HCV in incarcerated populations: an analysis of gender and criminality on risk. J Psychoactive Drugs. 2008;40(4):493–501. doi: 10.1080/02791072.2008.10400655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hebert MR, Clarke JG, Caviness CM, Ray MK, Friedmann PD, Stein MD. Feasibility of gaining access to women in jail for health interventions. Women Health. 2008;47(3):79–93. doi: 10.1080/03630240802134159. [DOI] [PubMed] [Google Scholar]
- 88.Stein MD, Caviness CM, Anderson BJ. Incidence of sexually transmitted infections among hazardously drinking women after incarceration. Womens Health Issues. 2012;22(1):e1–e7. doi: 10.1016/j.whi.2011.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stein MD, Caviness CM, Anderson BJ, Hebert M, Clarke JG. A brief alcohol intervention for hazardously drinking incarcerated women. Addiction. 2010;105(3):466–475. doi: 10.1111/j.1360-0443.2009.02813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Strong DR, Caviness C, Anderson B, Brown RA, Stein M. Assessing the severity of hazardous drinking and related consequences among incarcerated women. Alcohol Clin Exp Res. 2010;34(5):907–914. doi: 10.1111/j.1530-0277.2010.01163.x. [DOI] [PubMed] [Google Scholar]
- 91.Wu F. Linking Heroin Users in China to Drug Treatment and Other Resources in the Community: Effect of a Recovery Management Intervention Model [doctoral dissertation] Los Angeles, CA: University of California, Los Angeles; 2013. [Google Scholar]
- 92.Keough AB. Association Between Social and Financial Support and Recidivism Amongst Incarcerated Females [master’s dissertation] San Diego, CA: San Diego State University; 2013. [Google Scholar]
- 93.Havens JR, Leukefeld CG, Oser CB et al. Examination of an interventionist-led HIV intervention among criminal justice-involved female prisoners. J Exp Criminol. 2009;5(3):245–272. doi: 10.1007/s11292-009-9081-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Leukefeld C, Oser CB, Havens J et al. Drug abuse treatment beyond prison walls. Addict Sci Clin Pract. 2009;5(1):24–30. doi: 10.1151/ascp095124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Anglin MD, Longshore D, Turner S. Treatment alternatives to street crime: an evaluation of five programs. Crim Justice Behav. 1999;26(2):168–195. [Google Scholar]
- 96.O’Connell DJ, Swan H, Martin SS, Surratt HL, Visher CA. A continuum of care model for HIV in correctional settings. In: Sanders W, Thomas YF, Deeds B, editors. Crime, HIV and Health: Intersections of Criminal Justice and Public Health Concerns. New York, NY: Springer; 2013. [Google Scholar]
- 97.Inciardi JA. Criminal Justice Drug Abuse Treatment Studies (CJ-DATS): HIV/hepatitis prevention for re-entering drug offenders (ICPSR 29061) 2011. Available at: http://www.icpsr.umich.edu/icpsrweb/NAHDAP/series/244/studies/29061?sortBy=7&archive=NAHDAP&keyword[0]=HIV&paging.startRow=1. Accessed August 10, 2014.
- 98.Lopez C-RR. Assessing the Association Between Risky Sexual Behaviors and Hepatitis C Among Drug Users Recently Released from Incarceration. San Diego, CA: San Diego State University; 2013. [Google Scholar]
- 99.Medical Letter on the CDC and FDA. Atlanta, GA: NewsRX; 2004. Prevention program lowers unprotected sex among recently released prisoners; p. 39. [Google Scholar]
- 100.Johnson AP, Macgowan RJ, Eldridge GD et al. Cost and threshold analysis of an HIV/STI/hepatitis prevention intervention for young men leaving prison: Project START. AIDS Behav. 2013;17(8):2676–2684. doi: 10.1007/s10461-011-0096-7. [DOI] [PubMed] [Google Scholar]
- 101.Medical Letter on the CDC and FDA. Atlanta, GA: NewsRX; 2004. With more intensive counseling, prisoners take fewer sexual risks after release; pp. 104–105. [Google Scholar]
- 102.Grinstead O, Eldridge G, MacGowan R et al. An HIV, STD, and hepatitis prevention program for young men leaving prison: Project START. J Correct Health Care. 2008;14(3):183–196. [Google Scholar]
- 103.Martin SS, Inciardi JA. Case management treatment program for drug-involved prison releasees. Prison J. 1993;73(3):319–331. [PubMed] [Google Scholar]
- 104.Anglin MD, Longshore D, Turner S, McBride D, Inciardi J, Prendergast M. Los Angeles, CA: The UCLA Drug Abuse Research Center; 1996. Studies of the functioning and effectiveness of Treatment Alternatives to Street Crime (TASC) programs, final report. [Google Scholar]
- 105.Dolan K, Shearer J, White B. A Randomised Controlled Trial of Methadone Maintenance Treatment in NSW Prisons. Sydney, Australia: National Drug and Alcohol Research Centre, University of New South Wales; 2002. [Google Scholar]
- 106.Stephens T, Braithwaite R, Conerly R. Self-reported injection drug use and needle sharing behavior among soon-to-be-released adult male inmates. Am J Health Stud. 2005;20(1/2):66–71. [Google Scholar]
- 107.Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999;319(7211):670–674. doi: 10.1136/bmj.319.7211.670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Weinhardt LS, Forsyth AD, Carey MP, Jaworski BC, Durant LE. Reliability and validity of self-report measures of HIV-related sexual behavior: progress since 1990 and recommendations for research and practice. Arch Sex Behav. 1998;27(2):155–180. doi: 10.1023/a:1018682530519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Harrison LD. The validity of self-reported data on drug use. J Drug Issues. 1995;25(1):91–111. [Google Scholar]
- 110.Darke S. Self-report among injecting drug users: a review. Drug Alcohol Depend. 1998;51(3):253–263. doi: 10.1016/s0376-8716(98)00028-3. discussion 267–268. [DOI] [PubMed] [Google Scholar]
- 111.Del Boca FK, Noll JA. Truth or consequences: the validity of self-report data in health services research on addictions. Addiction. 2000;95(suppl 3):S347–S360. doi: 10.1080/09652140020004278. [DOI] [PubMed] [Google Scholar]
- 112.Fishbein M, Pequegnat W. Evaluating AIDS prevention interventions using behavioral and biological outcome measures. Sex Transm Dis. 2000;27(2):101–110. doi: 10.1097/00007435-200002000-00008. [DOI] [PubMed] [Google Scholar]
- 113.Collica-Cox K. Counting down: HIV prison-based peer education programs and their connection to reduced disciplinary infractions. Int J Offender Ther Comp Criminol. 2013;58(8):931–952. doi: 10.1177/0306624X13490660. [DOI] [PubMed] [Google Scholar]
- 114.Chen JL, Callahan DB, Kerndt PR. Syphilis control among incarcerated men who have sex with men: public health response to an outbreak. Am J Public Health. 2002;92(9):1473–1474. doi: 10.2105/ajph.92.9.1473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tuli K, Kerndt PR. Preventing sexually transmitted infections among incarcerated men who have sex with men: a cost-effectiveness analysis. Sex Transm Dis. 2009;36(2 suppl):S41–S48. doi: 10.1097/OLQ.0b013e3181574daa. [DOI] [PubMed] [Google Scholar]
- 116.Grinstead OA, Faigeles B, Comfort M et al. HIV, STD, and hepatitis risk to primary female partners of men being released from prison. Women Health. 2005;41(2):63–80. doi: 10.1300/J013v41n02_05. [DOI] [PubMed] [Google Scholar]
- 117.Harawa NT, Sweat J, George S, Sylla M. Sex and condom use in a large jail unit for men who have sex with men (MSM) and male-to-female transgenders. J Health Care Poor Underserved. 2010;21(3):1071–1087. doi: 10.1353/hpu.0.0349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Robillard AG, Gallito-Zaparaniuk P, Arriola KJ, Kennedy S, Hammett T, Braithwaite RL. Partners and processes in HIV services for inmates and ex-offenders. Facilitating collaboration and service delivery. Eval Rev. 2003;27(5):535–562. doi: 10.1177/0193841X03255631. [DOI] [PubMed] [Google Scholar]
- 119.Des Jarlais DC, Paone D, Milliken J et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet. 1999;353(9165):1657–1661. doi: 10.1016/s0140-6736(98)07026-3. [DOI] [PubMed] [Google Scholar]
- 120.Langhaug LF, Sherr L, Cowan FM. How to improve the validity of sexual behaviour reporting: systematic review of questionnaire delivery modes in developing countries. Trop Med Int Health. 2010;15(3):362–381. doi: 10.1111/j.1365-3156.2009.02464.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Macalino GE, Celentano DD, Latkin C, Strathdee SA, Vlahov D. Risk behaviors by audio computer-assisted self-interviews among HIV-seropositive and HIV-seronegative injection drug users. AIDS Educ Prev. 2002;14(5):367–378. doi: 10.1521/aeap.14.6.367.24075. [DOI] [PubMed] [Google Scholar]
- 122.Perlis TE, Des Jarlais DC, Friedman SR, Arasteh K, Turner CF. Audio-computerized self-interviewing versus face-to-face interviewing for research data collection at drug abuse treatment programs. Addiction. 2004;99(7):885–896. doi: 10.1111/j.1360-0443.2004.00740.x. [DOI] [PubMed] [Google Scholar]
- 123.Islam MM, Topp L, Conigrave KM et al. The reliability of sensitive information provided by injecting drug users in a clinical setting: clinician-administered versus audio computer-assisted self-interviewing (ACASI) AIDS Care. 2012;24(12):1496–1503. doi: 10.1080/09540121.2012.663886. [DOI] [PubMed] [Google Scholar]
- 124.Brown JL, Swartzendruber A, DiClemente RJ. Application of audio computer-assisted self-interviews to collect self-reported health data: an overview. Caries Res. 2013;47(suppl 1):40–45. doi: 10.1159/000351827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Brown JL, Vanable PA, Eriksen MD. Computer-assisted self-interviews: a cost effectiveness analysis. Behav Res Methods. 2008;40(1):1–7. doi: 10.3758/brm.40.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Phillips AE, Gomez GB, Boily MC, Garnett GP. A systematic review and meta-analysis of quantitative interviewing tools to investigate self-reported HIV and STI associated behaviours in low- and middle-income countries. Int J Epidemiol. 2010;39(6):1541–1555. doi: 10.1093/ije/dyq114. [DOI] [PubMed] [Google Scholar]