Abstract
OBJECTIVE
To estimate rates of non-adherence to telemedicine strategies aimed at treating drug addiction.
METHODS
A systematic review was conducted of randomized controlled trials investigating different telemedicine treatment methods for drug addiction. The following databases were consulted between May 18, 2012 and June 21, 2012: PubMed, PsycINFO, SciELO, Wiley (The Cochrane Library), Embase, Clinical trials and Google Scholar. The Grading of Recommendations Assessment, Development and Evaluation was used to evaluate the quality of the studies. The criteria evaluated were: appropriate sequence of data generation, allocation concealment, blinding, description of losses and exclusions and analysis by intention to treat. There were 274 studies selected, of which 20 were analyzed.
RESULTS
Non-adherence rates varied between 15.0% and 70.0%. The interventions evaluated were of at least three months duration and, although they all used telemedicine as support, treatment methods differed. Regarding the quality of the studies, the values also varied from very poor to high quality. High quality studies showed better adherence rates, as did those using more than one technique of intervention and a limited treatment time. Mono-user studies showed better adherence rates than poly-user studies.
CONCLUSIONS
Rates of non-adherence to treatment involving telemedicine on the part of users of psycho-active substances differed considerably, depending on the country, the intervention method, follow-up time and substances used. Using more than one technique of intervention, short duration of treatment and the type of substance used by patients appear to facilitate adherence.
Keywords: Drug Users, Patient Acceptance of Health Care, Patient Dropouts, Telemedicine, Review
Abstract
OBJETIVO:
Estimar taxas de não adesão em intervenções com estratégias de telemedicina para tratamento de dependência química.
MÉTODOS:
Foi realizada revisão sistemática de ensaios clínicos randomizados com diferentes métodos terapêuticos de dependência química que incluíam telemedicina. Foram consultadas as bases de dados PubMed, PsycINFO, SciELO, Wiley (The Cochrane Library), Embase e Clinical Trials e a plataforma Google Scholar no período de 18/4/2012 a 21/6/2012. Para avaliar a qualidade dos estudos, utilizou-se a escala Grading of Recommendations Assessment, Development and Evaluation. Os critérios avaliados foram: adequada sequência da geração de dados, ocultação da alocação, cegamento, descrição das perdas e exclusões e análises por intenção de tratar. Foram selecionados 274 estudos, dos quais 20 foram analisados.
RESULTADOS:
As taxas de não adesão variaram entre 15,0% e 70,0%. As intervenções avaliadas possuíam no mínimo três meses de intervenção e, embora todos utilizassem a telemedicina como apoio, os métodos de tratamentos foram diferentes. Em relação à qualidade dos estudos, os valores também variaram entre muito baixa qualidade e alta qualidade. Os estudos com qualidade alta demonstraram maiores taxas de adesão, bem como aqueles que utilizaram mais de uma técnica de intervenção e tempo limitado de tratamento. Estudos com monousuários apontaram maiores taxas de adesão que estudos com poliusuários.
CONCLUSÕES:
As taxas de não adesão a tratamentos para usuários de substâncias psicoativas por meio de telemedicina apresentaram consideráveis diferenças, dependendo do país, método da intervenção, tempo de seguimento e substâncias utilizadas. O uso de mais de uma técnica de intervenção, tempo curto de tratamento e o tipo de substância utilizada pelos pacientes parecem facilitar a adesão.
INTRODUCTION
Adherence to treatment for drug addiction is one of the biggest challenges in mental health clinical practice. 42 It is measured by the dropout rate, expressed as a percentage, reflecting the losses in monitored individuals, for whatever reason, over a specific time. Poor adherence to treatment is responsible for many setbacks in treating drug addiction as it leads to reductions in the efficacy of treatment, to socioeconomic costs and to high mortality rates. 2 Adherence is related to attitudes and beliefs regarding both the disease and the treatment, to level of knowledge concerning the disease, to personality and family structure characteristics and to the history and severity of the disease, as well as to factors linked to the type of intervention and to the health care professionals, which may or may not facilitate commitment to the therapy, thus increasing motivation to be treated. 41
Health care professionals monitor these behaviors which include taking medication, attending appointments, accompaniment by the family and keeping in contact with support services, goals to be developed in order for the patient to improve their health. When the patient is more engaged, this is associated with better outcomes, whereas high levels of abandoning the monitoring and control make it difficult to evaluate the results of the interventions. 3 In studies of efficacy, adherence is essential in order to examine issues such as internal and external validity, which are compromised when there are high losses of patients during treatment and monitoring. a
Drug addiction interventions using telemedicine, such as counselling via the telephone, 23 , 26 internet 38 and text messages 14 aim to minimize the impact of abandoning treatment when offered together with fate-to-face interventions and often represent significant treatment alternatives when used in isolation. 18 , 36
Even when it is easy to collect data, there are still few studies on dropout rates for isolated interventions or interventions in combination with face-to-face telemedicine based interventions. 38 In addition, little is known about reasons for non-adherence and the specific components that can improve patient engagement in studies using telemedicine based interventions. 17 Randomized clinical trial with alcohol users showed that 80 of the 136 individuals who participated in an internet intervention completed the six-month monitoring period, representing a dropout rate of approximately 42.0%. 5 In face-to-face interventions for drug addiction, generally, 50.0% of patients abandon treatment before the end of the period. 12 The rates have been studied from different perspectives. In Brazil, there are still few studies on telemedicine based interventions. The rate of adherence to treatment for drug addiction and the cultural, technological and disease-related factors that influence its effectiveness and the patients’ engagement with recommendations made through internet, telephone and text message are unknown.
The aim of this study was to estimate non-adherence rates in drug addiction treatment strategies using telemedicine.
METHODS
Randomized clinical trials meeting the following criteria were selected: a) testing different telemedicine treatment methods in drug users and estimating factors associated with non-adherence rates; b) population aged over 18; c) published in English between 2000 and 2012. Telemedicine is a recent field of study and studies were found from 2000 onwards, hence the start date for the search. The authors searched for publications in English as the majority of publications were in this language.
The following search terms were used “randomized controlled trial”, “drug abuse”, “telemedicine” and its “mesh terms” in Google Scholar, and in the PubMed, PsycINFO, SciELO, Wiley (The Cochrane Library), Embase and Clinical trials databases. The search strategy included Boolean operators combining the limits and filters for each term. The studies found were then evaluated to verify the following characteristics: year of publication, demographic region in which the study was carried out, the psychoactive substance included in the studies, a description of the sample allocation (randomization), blinding of outcomes, description of losses and exclusion, analysis by intention to treat, number of drug addicts (sample size), number of groups in the study, division of participants into control or intervention groups, type of intervention used with the groups, type of control used, stratification of groups by sex, age of the individuals being monitored and length of follow-up, the means used to apply the intervention and the frequency with which it was applied, methods of measuring the results, control and intervention group scores before and after the proposed intervention, relationship of adherence for the control and intervention groups.
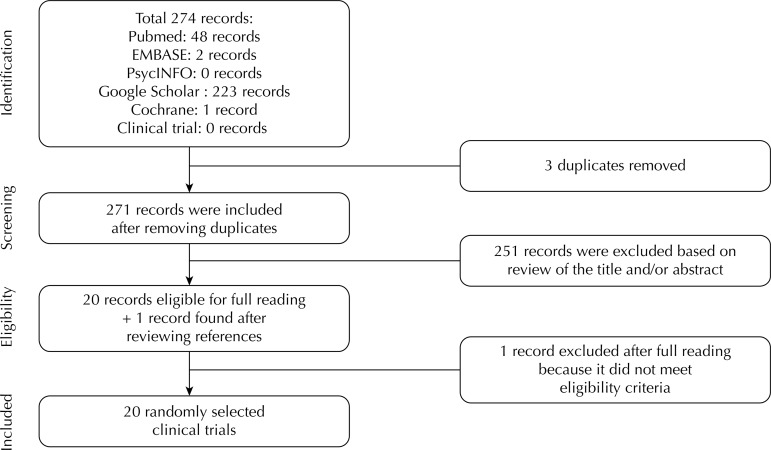
There were 274 records recovered. Of these, 253 were excluded after analysis of the title and the abstract ( Figure ). The remaining 20 articles were analyzed by 2 investigators (LS and LRF) and compared in case of disagreement. Inclusion or exclusion was decided by a third assessor (TM).
Figure. Flowchart of the stages of the systematic review.
In order to analyze the quality of the randomized clinical trials, the GRADE scale was used. 22 To ensure transparency and simplicity, the GRADE system classifies the quality of evidence into one of four levels, high, moderate, low and very low quality. Studies scoring 5/5 were considered high quality, score of 4/5 and 3/5 were of moderate quality and 2/5 and 1/5 were low and very low quality, respectively. Evidence based on randomized clinical trials begins with high quality evidence, but confidence in the evidence can decrease for a variety of reasons including: limitations of the study, inconsistent results, indirect evaluations, inaccuracy and indications of bias. 22 Thus, the definitions of quality can be classified as: 22
High quality research: very unlikely that confidence in the estimate of effect changes;
Moderate quality research: likely to have a significant impact on confidence in the estimate of effect and may change the estimate;
Low quality research: very likely to have a significant impact on confidence in the estimate of effect and the estimate is likely to change;
In very low quality research, the estimate of effect is very uncertain.
The clinical relevance of the studies included was evaluated using the United States Preventive Services Task Force (USPSTF) criteria 24 in accordance with the five questions recommended by the Cochrane Back Review Group. 43 Each question was classified as positive (+) if the relevant item was met; negative (-) if the item was not found and unclear (u) if the data were not available for analysis. Thus, the relevance of the interventions can be classified as:
Good (5/5): consistent results, well designed, well conducted study of a representative population that directly evaluates effects on health results;
Reasonable (4/5 and 3/5): sufficient evidence to determine effects on health results, although the strength of relevancy is limited by the number, quality, size or consistency of the included study, or generalization for routine practice and the results;
Limited or poor (2/5 and 1/5): there is insufficient evidence to evaluate the effects on health results due to the limited number of studies, inexplicable inconsistency, important faults in the design or conduct of the study, problems in the evaluation of lack of information on important results.
RESULTS
Of the 20 randomized clinical trials analyzed, the most commonly studied substance was alcohol (13 articles) and the majority of the research was on users of single psycho-active substances (13 articles). The number of patients involved in each study varied between 20 and 230 in the studies with smaller samples and between 358 and 873 in those with large samples. The participants’ ages varied between 24 and 58 years of age.
All of the studies used telemedicine combined with different interventions, such as brief motivational intervention, individual therapy, group therapy, cognitive-behavioral therapy – using strategies for coping, for identifying risky situations and identifying problems associated with use, among others – and preventing relapses. The non-adherence rate varied between 7.4% and 68.8%. The majority of studies followed patients for more than six months and described losses and exclusions; randomization and allocation concealment were adequate in half of the studies, 26.0% blinded the results and 63.0% analyzed according to intention to treat ( Table 1 ).
Table 1. Characteristics and main results of the selected randomized clinical trials, GRADEa score and clinical relevance score. (N = 20).
| Source/Country in which the study was conducted /Substance studied/Sample size | Type of intervention/Method to minimize abandonment/Non-adherence rate | Outcome measured | GRADE totalb – Clinical relevancec |
|---|---|---|---|
| Agyapong et al (2012)1 | SMS/control Not used 7.4% in 3 months | Text messaging support showed improvement in outcomes for patients with depression and comorbidity (alcohol dependence). | 5/5-5/5 |
| Ireland | |||
| Alcohol | |||
| N = 54 | |||
| Blankers M et al (2011)5 | Cognitive behavioral therapy and motivational interviewing online/internet Motivational e-mails, telephone calls to collect data, 15 Euro voucher for every questionnaire completed 41.0% in 6 months | Reducing the number of units of alcohol per week in 6 months. | 4/5-5/5 |
| Holland | |||
| Alcohol | |||
| N = 205 | |||
| Joseph A et al (2011)28 | Prevalence of relapse and telephone /usual care Not used 8.4% in 18 months | The approach increased short tobacco abstinence in the and long term. | 5/5-5/5 |
| United States | |||
| Tobacco | |||
| N = 443 | |||
| McKay J et al (2011)34 | Counselling and telephone monitoring/ telephone monitoring/usual treatment Not used 26.2% in 24 months | Telephone monitoring and counseling decreased % of days of alcohol consumption up to 18 months of intervention. | 5/5-5/5 |
| United States | |||
| Alcohol | |||
| N = 252 | |||
| Postel M et al (2011)38 | Internet/waiting list Not used Non-adherence rate not estimated | Gender, educational level, age, initial intake and motivational level were predictors of | 1/5-2/5 |
| Holland | |||
| Alcohol | |||
| N = 924 | |||
| Whittaker R et al (2011)48 | Video message/control Not used 27.0% in 6 months | Efficacy not shown in the tested intervention. Dropout rates were high in both groups. | 5/5-3/5 |
| New Zealand | |||
| Tobacco | |||
| N = 226 | |||
| Fernandes S et al (2010)18 | Brief, motivational telephone interview/telephone control Not used 68.8% in 6 months | Positive efficacy for stopping marijuana use. | 2/5-3/5 |
| Brazil | |||
| Marijuana | |||
| N = 1.744 | |||
| Girard B et al (2010)20 | Virtual game Not used 60.4% in 6 months | E-cigarettes led to a significant reduction in nicotine dependence, abstinence and dropout rates. | 5/5-4/5 |
| Canada | |||
| Tobacco | |||
| N = 91 | |||
| Zanjani F et al (2010)49 | Brief motivational telephone interview/usual care Participants in the intervention group received a letter to reinforce presence in the continued treatment using motivational components. 22.1% in 6 months | The proposed intervention did not lead to a significant improvement in the results of psychiatric health. | 3/5-5/5 |
| United States | |||
| Tobacco | |||
| N = 113 | |||
| Eberhard S et al (2009)15 | Motivational telephone interview (1 session-15 min.) Intervention group received feedback at the beginning 12.5% in 6 months | Alcohol consumption reduced to safe levels. | 1/5-2/5 |
| Sweden | |||
| Alcohol | |||
| N = 344 | |||
| Kavanagh D & Connolly J (2009)30 | Letter and telephone: immediate treatment/delayed treatment Not used 52.9% in 12 months | High levels of adherence to treatment and substantial reduction of alcohol use. | 5/5-4/5 |
| Australia | |||
| Alcohol | |||
| N = 204 | |||
| Kay-Lambkin F et al (2009)31 | Computerized cognitive behavioral therapy/brief intervention Not used 28.9% in 12 months | Marijuana use and hazardous use of substances reduced with computerized therapy. | 4/5-5/5 |
| Australia | |||
| Alcohol and marijuana | |||
| N = 97 | |||
| Litt M et al (2009)33 | Individual treatment program (cell phone)/package of cognitive-behavioral therapy Not used 15.5% in 16 weeks | Intervention decreased the days of alcohol intake and increased use of coping strategies. | 1/5-2/5 |
| United States | |||
| Alcohol and marijuana | |||
| N = 110 | |||
| Brendryen H et al (2008)6 | Messages via Internet, e-mail and cellular (SMS) (I) X Self-help booklet (C) The proposed intervention already included the method of minimization of abandonment 32.6% in 12 months | Better rates of abstinence from tobacco. | 5/5-5/5 |
| Norway | |||
| Tobacco | |||
| N = 290 | |||
| El-Khorazaty M et al (2007)16 | Educational intervention and multimodal integrative counseling /usual care Telephone contacts, current contact information, financial incentives, training of staff in the recruitment and implementation of the study, salary support for staff, quick resolution to the problems that the team could have, continuous monitoring of the study 20.0% in 9 months | Specific recruitment and retention strategies increased the rate of minority participation in trials. | 2/5-2/5 |
| United States | |||
| Polydrug | |||
| N = 1.070 | |||
| Hubbard R et al (2007)26 | Telephone group/standard care group Both groups were reminded to enroll in outpatient and continuing care following; reminded of the dates of the calls (I) Not used 29.2% in 13 weeks | Well-developed telephone approaches facilitate the approaches between professional and patient. | 4/5-5/5 |
| United States | |||
| Polydrug | |||
| N = 339 | |||
| Parker D et al (2007)37 | Motivational interview (telephone), incentives, self-help material/incentives and self-help material/self-help material Joining a monetary incentive program (30 days of abstinence confirmed by screening) 30.7% in 6 months (postpartum) | Telephone counseling was well received by pregnant low-income women. The cessation rate was higher among those who received the intervention. | 2/5-4/5 |
| United States | |||
| Tobacco | |||
| N = 1.065 | |||
| Vidrine D et al (2006)47 | Telephone/standard care Not used 18.9% in 3 months | Intervention by phone showed greater reduction in anxiety and depression, and increased self-efficacy. | 1/5-2/5 |
| United States | |||
| Tobacco | |||
| N = 95 | |||
| Currie S et al (2004)11 | Individual face-to-face treatment (I) X self-help/telephone support (C) Not used 36.0% X 50.0% in 6 months | Better sleep parameters for both groups and equal levels of lapse and relapse to alcohol. | 1/5-2/5 |
| Canada | |||
| Alcohol | |||
| N = 57 | |||
| Hall J & Hubert D (2000)23 | Case management/interactive voice response system/control Not used Non-adherence rate not estimated | The use of telemedicine facilitated interaction with customers and decreased costs. | 0/5-1/5 |
| United States | |||
| Polydrug | |||
| N = 230 |
I: Intervention Group; C: Control Group
a GRADE study quality scale, Guyatt GH et al (2008).
b The complete data for the scale are described in Table 3.
c The complete data for the scale are described in Table 4.
Regarding the quality of the results analyzed, 50.0% were of moderate to high quality ( Table 2 ). As for clinical relevance, 13 studies had a reasonable level of relevance ( Table 3 ).
Table 2. Quality of the studies according to GRADE criteriaa: randomized clinical trials.
| First author/Year of publication | Proper sequence of data generation | Allocation concealment | Blinding | Description of losses and exclusions | Analysis by intention to treat | Score |
|---|---|---|---|---|---|---|
| Agyapong et al (2012)1 | Yes | Yes | Yes | Yes | Yes | 5/5 |
| Blankers et al (2011)5 | Yes | Yes | No | Yes | Yes | 4/5 |
| Joseph et al (2011)28 | Yes | Yes | Yes | Yes | Yes | 5/5 |
| McKay et al (2011)34 | Yes | Yes | Yes | Yes | Yes | 5/5 |
| Postel et al (2011)38 | No | No | No | Yes | No | 1/5 |
| Whittaker et al (2011)48 | Yes | Yes | Yes | Yes | Yes | 5/5 |
| Fernandes et al (2010)18 | Yes | No | No | Yes | No | 2/5 |
| Girard et al (2010)20 | No | No | No | Yes | Yes | 2/5 |
| Zanjani et al (2010)49 | Yes | Yes | No | Yes | Unclear | 3/5 |
| Eberhard et al (2009)15 | No | No | No | No | Yes | 1/5 |
| Kavanagh & Connolly (2009)30 | Yes | Yes | Yes | Yes | Yes | 5/5 |
| Kay-Lambkin et al (2009)31 | Yes | Yes | No | Yes | Yes | 4/5 |
| Litt et al (2009)33 | No | No | No | Yes | Unclear | 1/5 |
| Brendryen et al (2008)6 | Yes | Yes | Yes | Yes | Yes | 5/5 |
| El-Khorazaty et al (2007)16 | No | No | No | Yes | Yes | 2/5 |
| Hubbardi et al (2007)26 | Yes | Yes | No | Yes | Yes | 4/5 |
| Parker et al (2007)37 | No | No | No | Yes | Yes | 2/5 |
| Vidrine et al (2006)47 | No | No | No | Yes | No | 1/5 |
| Currie et al (2004)11 | No | No | No | Yes | No | 1/5 |
| Hall & Hubert (2000)23 | No | No | No | No | No | 0/5 |
a GRADE study quality questionnaire, Guyatt GH et al (2008).
Tabela 3. Relevância clínica dos estudos selecionados.
| Source | Description of patients | Description of interventions and definition of treatment | Results with clinical relevance | Clinical importance | Benefits x Potential harm | Total |
|---|---|---|---|---|---|---|
| Agyapong et al (2012)1 | + | + | + | + | + | 5/5 |
| Blankers et al (2011)5 | + | + | + | + | + | 5/5 |
| Joseph et al (2011)28 | + | + | + | + | + | 5/5 |
| McKay et al (2011)34 | + | + | + | + | + | 5/5 |
| Postel et al (2011)38 | + | + | - | - | - | 2/5 |
| Whittaker et al (2011)48 | + | + | + | - | - | 3/5 |
| Fernandes et al (2010)18 | + | + | - | + | - | 3/5 |
| Girard et al (2010)20 | + | + | - | + | + | 4/5 |
| Zanjani et al (2010)49 | + | + | + | + | + | 5/5 |
| Eberhard et al (2009)15 | + | + | - | - | - | 2/5 |
| Kavanagh & Connolly (2009)30 | + | + | + | + | - | 4/5 |
| Kay-Lambkin et al (2009)31 | + | + | + | + | + | 5/5 |
| Litt et al (2009)33 | + | + | - | - | - | 2/5 |
| Brendryen et al (2008)6 | + | + | + | + | + | 5/5 |
| El-Khorazaty et al (2007)16 | + | + | - | - | - | 2/5 |
| Hubbardi et al (2007)26 | + | + | + | + | + | 5/5 |
| Parker et al (2007)37 | + | + | - | + | + | 4/5 |
| Vidrine et al (2006)47 | + | + | - | - | - | 2/5 |
| Currie et al (2004)11 | + | + | - | - | - | 2/5 |
| Hall & Hubert (2000)23 | - | + | - | - | - | 1/5 |
DISCUSSION
Lower rates of non-adherence are related to high quality studies evaluated using GRADE. Studies with single users, limited intervention time and which used different techniques to stop drug use appeared to increase rates of adherence. The interventions in the randomized clinical trials evaluated in this systematic review were of at least three months duration and, although all of them used telemedicine as primary or secondary support, the treatment methods differed, which may have affected adherence.
Treating drug addiction is a complex process. In addition to the factors related to treatment methods, coping abilities, 9 , 33 motivation, self-efficacy, 33 the users’ emotional state 4 and social support 13 influence the process of changing behavior, affecting adherence to treatment for substance abuse. 8 For Brazilian alcoholics, rates of non-adherence to drug addiction treatment depend on the type of intervention, on the result related to abstinence, as they had to avoid consuming alcohol for six months after the intervention. 45
Of the studies evaluated, six 1 , 6 , 28 , 30 , 34 , 48 were of high quality and the clinical relevance of four of these was good. 1 , 6 , 28 , 34 Considering the impact of non-adherence rates in each of the six best studies, a difference in non-adherence rates can be identified, even in well-designed studies. Agyapong et al 1 used SMS (an effective technique often used on studies of adherence, a as, with the development of new technology, individuals are increasingly more interconnected, due to growing use of this technology), and had the lowest non-adherence rate of the randomized clinical trials. Thus, reminders or messages received during the treatment period contributed to better adherence. 25 On the other hand, the study by Agyapong et al, 1 when compared to the other good quality ones, had the shortest follow-up time.
Lower rates of non-adherence are also found in shorter treatments, or those with a limited time, irrespective of the use of telemedicine. According to a meta-analysis of data on face-to-face therapy, 44 a short follow-up time is more effective than treatments that have no time limit or even those in which there is a limited, albeit extensive, period. Another important factor in the study by Agyapong et al 1 is that the treatment was only for alcohol users, and the literature describes how it is easier for users of a single substance to follow treatment and stop taking it than for users of more than one drug. 39 The study using pharmacological treatment 28 for tobacco had a low non-adherence rate, which may be explained by the use of medication that, by increasing rates of quitting, 21 , 27 may motivate the patient to adhere more to treatment. 46 Moreover, research conducted with smokers shows that pharmacological treatment is widely studied, 35 with positive results for treating nicotine dependence. 21 , 27 It is probable that the use of strategies to prevent relapse with longer follow-up than in the other studies (one year) and the patients’ financial incentive ($25 per follow up conducted) may also have positively influenced adherence results.
The study of users of alcohol alone 34 had a higher non-adherence rate compared with other good quality studies. Alcohol dependence is also associated with high rates of non-adherence in face-to-face treatment. 45 Even with more follow-up, the patients in this study 34 were monitored for longer than in other studies, probably due to the use of a combination of different techniques. 34 Making use of more than one technique, including using telemedicine, is a good alternative for treating drug users, 36 as, when the intervention contains different tools and approaches, 7 there is a greater possibility of the individual being engaged, 2 and the results of the treatment may also be better. 29 The study by Brendryen et al 6 highlights using the telemedicine Happy Ending technique, consisting of an intense stop smoking program with the help of contact via e-mail, text messages, a helpline for dealing with cravings and a system to prevent relapse. Moreover, it emphasizes how psychological support can be efficaciously provided through modern communication technology with excellent results. 6 The study by Brendryen et al 6 was of high quality and had better results for stopping smoking when technological interventions were used, confirming that well-designed studies have more reliable results.
As the quality of the studies included in this systematic review decreased, there was an increase in non-adherence rates. This shows that in research that is more reliable in estimating effect – represents the effect present in the population and not only in the sample studied – there are better adherence rates. 10 In moderate quality studies, 5 , 26 , 31 , 49 only that of Blankers et al 5 had high rates of non-adherence (41.0% in six months) and the others showed little variation (between 22.0% and 29.0%). Regarding clinical relevance of the moderate quality studies, only that of Blankers et al 5 had reasonable relevance, whereas the others met the criteria evaluated with good clinical relevance. Although the study by Blankers et al 5 was conducted solely with alcohol users, the only intervention technique used was that of online therapy, in which there was no contact with a therapist and the individuals was self-guided by the programs used. The authors themselves highlight the technique as being effective but limited to reduced alcohol consumption. Kay-Lambkin et al 31 and Zanjani et al 49 used brief intervention techniques associated with other interventions. The former presented an intervention for alcohol and marijuana and had a higher non-adherence rate. 31 This may be related to use of two substances and to the follow-up time, as well as to the characteristics of the profile of those who use marijuana 19 who often have difficulty viewing their marijuana consumption as problematic. 40 The treatment in the study by Zanjani et al 49 was conducted solely with smokers, with a six-month follow-up to facilitate adherence. 44 Hubbard et al 26 only used groups via telephone with tele-counselors and indicated that in-person clinical monitoring is necessary to keep abstinence.
Studies considered to be of 16 , 18 , 20 , 37 have high non-adherence rates, which may be explained by difficulty maintaining the effect estimate. 10 The evaluation of the results for the discussion of adherence to telemedicine were based on the relevance of the studies that, in this case, may be considered of poor reliability. Using a greater number of techniques contributed to higher adherence rates 16 , 37 and adherence to interventions may increase in drug users who have made various attempts to stay clean, 32 irrespective of whether a face-to-face or telemedicine intervention was used.
Among the limitations of this study is the fact that the therapies used in the studies used different telemedicine strategies and had different periods of follow-up, which makes it difficult to compare them. Another limitation is that the studies were on treatments for different types of substances and included users of single substances or poly drug users.
Despite the limitations found, it was possible to observe that certain factors favor non-adherence to treatment for drug addiction using telemedicine. Adherence is better when more than one intervention technique is used and when the treatment time is shorter.
In some countries, the use of telemedicine is of recent date. Treatments that use this tool are still unknown to many patients and professionals, which leads us to believe that this decreases confidence in the possibility of a positive result and leads to non-adherence.
As rates of non-adherence are high, more research is necessary on personal and socioeducational characteristics of patients which affect non-adherence to interventions using telemedicine technology.
Footnotes
This study was supported by the Secretaria Nacional de Políticas sobre Drogas, Associação Mário Tannhauser de Ensino, Pesquisa e Assistência (SENAD/AMTEPA – 00187.000520/2010-61 Term 04/2010), by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) through a research productivity grant 1C (HMTB – Process 303742/2010-0, in 2011-2014) and by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) through doctoral grants (TCM: 95414720010, in 2010 and LRF: 00331585090, in 2012).
World Health Organization. Adherence to long-term therapies: evidence for action. Geneva; 2003 [cited 2010 Nov 23]. Available from: http://www.who.int/chp/knowledge/publications/adherence_report/en/
Article based on the Doctoral thesis of Moreira TC, entitled: “Qualidade de Vida e Voz em usuários de substâncias psicoativas”, presented to the Programa de Pós-Graduação em Ciências da Saúde of the Universidade Federal de Ciências da Saúde de Porto Alegre , in 2013.
REFERENCES
- 1.Agyapong VIO, Ahern S, McLoughlin DM, Farren CK. Supportive text messaging for depression and comorbid alcohol use disorder: single-blind randomised trial. J Affect Disord. 2012;141(2-3):168–176. doi: 10.1016/j.jad.2012.02.040. [DOI] [PubMed] [Google Scholar]
- 2.Amato L, Minozzi S, Davoli M, Vecchi S, Ferri MM, Mayet S. Psychosocial and pharmacological treatments versus pharmacological treatment for opioid detoxification. CD005031Cochrane Database Syst Rev. 2008;(3) doi: 10.1002/14651858. [DOI] [PubMed] [Google Scholar]
- 3.Ball SA, Carroll KM, Canning-Ball M, Rounsaville BJ. Reasons for dropout from drug abuse treatment: Symptoms, personality, and motivation. 10.1016/j.addbeh.2005.05.013Addict Behav. 2006;31(2):320–330. doi: 10.1016/j.addbeh.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 4.Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111(1):33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- 5.Blankers M, Koeter MW, Schippers GM. Internet therapy versus internet self-help versus no treatment for problematic alcohol use: A randomized controlled trial. J Consult Clin Psychol. 2011;79(3):330–341. doi: 10.1037/a0023498. [DOI] [PubMed] [Google Scholar]
- 6.Brendryen H, Drozd F, Kraft P. A digital smoking cessation program delivered through internet and cell phone without nicotine replacement (happy ending): randomized controlled trial. e51J Med Internet Res. 2008;10(5) doi: 10.2196/jmir.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bock BC, Graham AL, Whiteley JA, Stoddard JL. A review of web-assisted tobacco interventions (WATIs) e39J Med Internet Res. 2008;10(5) doi: 10.2196/jmir.9890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, et al. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: A multisite effectiveness study. Drug Alcohol Depend. 2006;81(3):301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung T, Langenbucher J, Labouvie E, Pandina RJ, Moos RH. Changes in alcoholic patients’ coping responses predict 12-month treatment outcomes. 10.1037//0022-006X.69.1.92J Consult Clin Psychol. 2001;69(1):92–100. doi: 10.1037//0022-006x.69.1.92. [DOI] [PubMed] [Google Scholar]
- 10.Coutinho ESF, Cunha GM. Conceitos básicos de epidemiologia e estatística para a leitura de ensaios clínicos controlados. Rev Bras Psiquiatr. 2005;27(2):146–151. doi: 10.1590/S1516-44462005000200015. [DOI] [PubMed] [Google Scholar]
- 11.Currie SR, Clark S, Hodgins DC, El-Guebaly N. Randomized controlled trial of brief cognitive-behavioural interventions for insomnia in recovering alcoholics. 10.1111/j.1360-0443.2004.00835.xAddiction. 2004;99(9):1121–1132. doi: 10.1111/j.1360-0443.2004.00835.x. [DOI] [PubMed] [Google Scholar]
- 12.Weert-van Oene GH, Burger H, Grobbee DE, Schrijvers AJ. Identification of patients at high risk of noncompliance in substance dependence treatment. Eur Addict Res. 2007;13(2):74–80. doi: 10.1159/000097936. [DOI] [PubMed] [Google Scholar]
- 13.Dobkin PL, Civita M, Paraherakis A, Gill K. The role of functional social support in treatment retention and outcomes among outpatient adult substance abusers. Addiction. 2002;97(3):347–356. doi: 10.1046/j.1360-0443.2002.00083.x. [DOI] [PubMed] [Google Scholar]
- 14.Downer SR, Meara JG, Costa AC. Use of SMS text messaging to improve outpatient attendance. Med J Aust. 2005;183(7):366–368. doi: 10.5694/j.1326-5377.2005.tb07085.x. [DOI] [PubMed] [Google Scholar]
- 15.Eberhard S, Nordström G, Höglund P, Öjehagen A. Secondary prevention of hazardous alcohol consumption in psychiatric out-patients: a randomised controlled study. Soc Psychiatry Psychiatr Epidemiol. 2009;44(12):1013–1021. doi: 10.1007/s00127-009-0023-7. [DOI] [PubMed] [Google Scholar]
- 16.El-Khorazaty MN, Johnson AA, Kiely M, El-Mohandes AAE, Subramanian S, Laryea HA, et al. Recruitment and retention of low-income minority women in a behavioral intervention to reduce smoking, depression, and intimate partner violence during pregnancy. 233BMC Public Health. 2007;7 doi: 10.1186/1471-2458-7-233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Eysenbach G. The law of attrition. e11J Med Internet Res. 2005;7(1) doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fernandes S, Ferigolo M, Benchaya MC, Moreira TC, Pierozan PS, Mazoni CG, et al. Brief Motivational Intervention and telemedicine: A new perspective of treatment to marijuana users. Addict Behav. 2010;35(8):750–755. doi: 10.1016/j.addbeh.2010.03.001. [DOI] [PubMed] [Google Scholar]
- 19.Fernandes S, Ferigolo M, Benchaya MC, Pierozan PS, Moreira TC, Santos V, et al. Abuso e dependência de maconha: comparação entre sexos e preparação para mudanças comportamentais entre usuários que iniciam a busca por tratamento. 10.1590/S0101-81082010005000004Rev Psiquiatr Rio Gd Sul. 2010;32(3):80–85. [Google Scholar]
- 20.Girard B, Turcotte V, Bouchard S, Girard B. Crushing virtual cigarettes reduces tobacco addiction and treatment discontinuation. Cyberpsychol Behav. 2009;12(5):477–483. doi: 10.1089/cpb.2009.0118. [DOI] [PubMed] [Google Scholar]
- 21.Gourlay SG, Stead LF, Benowitz NL. Clonidine for smoking cessation. CD000058Cochrane Database Syst Rev. 2004;(3) doi: 10.1002/14651858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guyatt GH, Oxman AD, Vist G, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–926. doi: 10.1136/bmj.39489.470347.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hall JA, Huber DL. Telephone management in substance abuse treatment. Telemed J E Health. 2000;6(4):401–407. doi: 10.1089/15305620050503870. [DOI] [PubMed] [Google Scholar]
- 24.Harris RP, Helfand M, Woolf SH, Lohr KN, Mulrow CD, Teutsch SM, et al. Methods Work Group, Third US Preventive Services Task Force. Current methods of the US Preventive Services Task Force. Am J Prevent Med. 2001;20(3Suppl):21–35. doi: 10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 25.Hasvold PE, Wootton R. Use of telephone and SMS reminders to improve attendance at hospital appointments: a systematic review. J Telemed Telecare. 2011;17(7):358–364. doi: 10.1258/jtt.2011.110707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hubbard RL, Leimberger JD, Haynes L, Patkar AA, Holter J, Liepman MR, et al. Telephone enhancement of long-term engagement (TELE) in continuing care for substance abuse treatment: a NIDA clinical trials network (CTN) study. Am J Addict. 2007;16(6):495–502. doi: 10.1080/10550490701641678. [DOI] [PubMed] [Google Scholar]
- 27.Hughes JR. Motivating and helping smokers to stop smoking. J Gen Intern Med. 2003;18(12):1053–1057. doi: 10.1111/j.1525-1497.2003.20640.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Joseph AM, Fu SS, Lindgren B, Rothman AJ, Kodl M, Lando H, et al. Chronic Disease Management for Tobacco Dependence: a randomized, controlled trial. Arch Intern Med. 2011;171(21):1894–1900. doi: 10.1001/archinternmed.2011.500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jungerman FS. Boas Práticas nas abordagens psicossociais da dependência de substâncias. In: Boas práticas no tratamento do uso e dependência de substâncias. São Paulo: Roca; 2007. pp. 174–175. [Google Scholar]
- 30.Kavanagh D, Connolly JM. Mailed treatment to augment primary care for alcohol disorders: a randomised controlled trial. Drug Alcohol Rev. 2009;28(1):73–80. doi: 10.1111/j.1465-3362.2008.00011.x. [DOI] [PubMed] [Google Scholar]
- 31.Kay-Lambkin FJ, Baker AL, Lewin TJ, Carr VJ. Computer-based psychological treatment for comorbid depression and problematic alcohol and/or cannabis use: a randomized controlled trial of clinical efficacy. Addiction. 2009;104(3):378–388. doi: 10.1111/j.1360-0443.2008.02444.x. [DOI] [PubMed] [Google Scholar]
- 32.Koob GF, Le Moal M. Neurobiological mechanisms for opponent motivational processes in addiction. Philos Trans R Soc Lond B Biol Sci. 2008;363(1507):3113–3123. doi: 10.1098/rstb.2008.0094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Litt MD, Kadden RM, Cooney NL, Kabela E. Coping skills and treatment outcomes in cognitive-behavioral and interactional group therapy for alcoholism. J Consult Clin Psychol. 2003;71(1):118–128. doi: 10.1037/0022-006X.71.1.118. [DOI] [PubMed] [Google Scholar]
- 34.McKay JR, Van Horn D, Oslin DW, Ivey M, Drapkin ML, Coviello DM, et al. Extended telephone-based continuing care for alcohol dependence: 24-month outcomes and subgroup analyses. Addiction. 2011;106(10):1760–1769. doi: 10.1111/j.1360-0443.2011.03483.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mitrouska I, Bouloukaki I, Siafakas NM. Pharmacological approaches to smoking cessation. Pulm Pharmacol Ther. 2007;20(3):220–232. doi: 10.1016/j.pupt.2005.10.012. [DOI] [PubMed] [Google Scholar]
- 36.Obermayer JL, Riley WT, Asif O, Jean-Mary J. College smoking-cessation using cell phone text messaging. J Am Coll Health. 2004;53(2):71–78. doi: 10.3200/JACH.53.2.71-78. [DOI] [PubMed] [Google Scholar]
- 37.Parker DR, Windsor RA, Roberts MB, Hecht J, Hardy NV, Strolla LO, et al. Feasibility, cost, and cost-effectiveness of a telephone-based motivational intervention for underserved pregnant smokers. Nicotine Tob Res. 2007;9(10):1043–1051. doi: 10.1080/14622200701591617. [DOI] [PubMed] [Google Scholar]
- 38.Postel MG, Haan HA, ter Huurne ED, van der Palen J, Becker ES, Jong CAJ. Attrition in web-based treatment for problem drinkers. e117J Med Internet Res. 2011;13(4) doi: 10.2196/jmir.1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ray AL, Hutchison R, Bryan A. Psychosocial predictors of treatment outcome, dropout and change processes in a pharmacological clinical trial for alcohol dependence. Addict Disord Their Treat. 2006;5(4):179–190. doi: 10.1097/01.adt.0000210701.63165.5a. [DOI] [Google Scholar]
- 40.Reniscow K, Smith M, Harrison L, Drucker E. Correlates of occasional cigarette and marijuana use: are teens harm reducing? Addict Behav. 1999;24(2):251–266. doi: 10.1016/S0306-4603(98)00059-8. [DOI] [PubMed] [Google Scholar]
- 41.Rosa AR, Kapczinski F, Oliva R, Stein A, Barros HMT. Monitoramento da adesão ao tratamento com lítio. Rev Psiquiatr Clin. 2006;33(5):249–261. doi: 10.1590/S0101-60832006000500005. [DOI] [Google Scholar]
- 42.Rutkowski BA, Gallon S, Rawson RA, Freese TE, Bruehl A, Crèvecoeur-Macphail D, et al. Improving client engagement and retention in treatment: The Los Angeles County experience. J Subst Abuse Treat. 2010;39(1):78–86. doi: 10.1016/j.jsat.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 43.Staal JB, Bie R, Vet HC, Hildebrandt J, Nelemans P. Injection therapy for subacute and chronic low-back pain. CD001824Cochrane Database Syst Rev. 2008;16(3) doi: 10.1002/14651858.CD001824.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Swift JK, Greenberg RP. Premature discontinuation in adult psychotherapy: a meta-analysis. J Consult Clin Psychol. 2012;80(4):547–559. doi: 10.1037/a0028226. [DOI] [PubMed] [Google Scholar]
- 45.Terra MB, Barros HMT, Stein AT, Figueira I, Palermo LH, Athayde LD, et al. Do Alcoholics Anonymous Groups Really Work? Factors of Adherence in a Brazilian Sample of Hospitalized Alcohol Dependents. Am J Addict. 2008;17(1):48–53. doi: 10.1080/10550490701756393. [DOI] [PubMed] [Google Scholar]
- 46.Velicer WF, Prochaska JO, Fava JL, Norman GJ, Redding CA. Smoking cessation and stress management: Applications of the Transtheoretical Model of behavior change. Homeostasis Hlth Dis. 1998;38(5-6):216–233. [Google Scholar]
- 47.Vidrine DJ, Arduino RC, Gritz ER. Impact of a cell phone intervention on mediating mechanisms of smoking cessation in individuals living with HIV/AIDS. Nicotine Tob Res. 2006;8(Suppl 1):S103–S108. doi: 10.1080/14622200601039451. [DOI] [PubMed] [Google Scholar]
- 48.Whittaker R, Dorey E, Bramley D, Bullen C, Denny S, Elley CR, et al. A theory-based video messaging mobile phone intervention for smoking cessation: randomized controlled trial. e10J Med Internet Res. 2011;13(1) doi: 10.2196/jmir.1553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zanjani F, Bush H, Oslin D. Telephone-based psychiatric referral-care management intervention health outcomes. Telemed J E Health. 2010;16(5):543–550. doi: 10.1089/tmj.2009.0139. [DOI] [PMC free article] [PubMed] [Google Scholar]