Abstract
Background:
Constitutional type of an individual or prakriti is the basic clinical denominator in Ayurveda, which defines physical, physiological, and psychological traits of an individual and is the template for individualized diet, lifestyle counseling, and treatment. The large number of phenotype description by prakriti determination is based on the knowledge and experience of the assessor, and hence subject to inherent variations and interpretations.
Objective:
In this study we have attempted to relate dominant prakriti attribute to body mass index (BMI) of individuals by assessing an acceptable tool to provide the quantitative measure to the currently qualitative ayurvedic prakriti determination.
Materials and Methods:
The study is cross sectional, multicentered, and prakriti assessment of a total of 3416 subjects was undertaken. Healthy male, nonsmoking, nonalcoholic volunteers between the age group of 20-30 were screened for their prakriti after obtaining written consent to participate in the study. The prakriti was determined on the phenotype description of ayurvedic texts and simultaneously by the use of a computer-aided prakriti assessment tool. Kappa statistical analysis was employed to validate the prakriti assessment and Chi-square, Cramer's V test to determine the relatedness in the dominant prakriti to various attributes.
Results:
We found 80% concordance between ayurvedic physician and software in predicting the prakriti of an individual. The kappa value of 0.77 showed moderate agreement in prakriti assessment. We observed a significant correlations of dominant prakriti to place of birth and BMI with Chi-square, P < 0.01 (Cramer's V-value of 0.156 and 0.368, respectively).
Conclusion:
The present study attempts to integrate knowledge of traditional ayurvedic concepts with the contemporary science. We have demonstrated analysis of prakriti classification and its association with BMI and place of birth with the implications to one of the ways for human classification.
Keywords: Ayusoft, body mass index, place of birth, Prakriti
INTRODUCTION
The interplay and architecture of genetic, epigenetic, and environment-induced changes in the DNA sequences contribute to large phenotypic variations.[1] The post-human genome era, embarked on several major international projects and subsequently their databases such as Human Genome Project, Genome Wide Association Studies, human ENCODE consortium, dbSNPs, dbCNVs, HapMap have all contributed significantly to the understanding of the position, degree, nature, and structure of DNA and its contributions to number of phenotypes as well as diseases. The variation in anatomical, physiological, immunological, psychological, disease susceptibility, disease prognosis, and response to treatment, forms the basic principles of personalized medicine. These variations are diverse and efforts are being made to classify humans based on geographical origin, ethnicity, race, and other factors.[2,3,4]
Ayurveda, Unani (Graeco-Arabic medicinal system), Sasang constitution (Korean medicinal system), and Chinese medicinal system are well known branches of traditional knowledge, which intend to classify individuals based on body temperament by deciphering specific phenotypic characters for health management.[5,6,7] Ayurveda, an Indian traditional system of medicine considers every individual as unique and the treatment is based on the defined constitution types. A basic feature of the theory and practice of Ayurveda is the classification of human beings into three doshas (vata, pitta, and kapha) and their mixed constitutional types called prakriti. The prakriti or the Ayurvedic constitutional type of an individual is fixed at conception and is articulated through physical, psychological, immunological, and behavioral traits as described elaborately in original ayurvedic texts written by Charaka and Susruta.[8,9,10] Further, prakriti also influences the manifestation and course of diseases in an individual and importantly, an individual's response to treatment.[11,12,13] Therefore the determination of constitution type or prakriti of a subject or patient is very important in the practice of Ayurveda.
Several biochemical, genetic, and molecular studies have been performed to relate various features of an individual to prakriti. Initial study by Patwardhan et al. demonstrated a correlation between HLA-DRB1 types with the specific prakriti.[14] Subsequently, Prasher et al. reported biochemical profiles, hematological parameters, and gene expression patterns among vata, pitta, and kapha subjects relating them to inflammatory or cardiovascular diseases.[15] Frequency of association among CYP2C19 genotypes in a prakriti specific fashion was also reported.[16] Similarly expression of EGLN1 gene and the association of rs479200 (C/T) and rs480902 (T/C) in high-altitude adaptation in relation to prakriti was reported.[17] Prakriti determination is traditionally a qualitative, subjective exercise carried out by vaidya. Since it is experience and skill based, inter-observer variations will be inherent. A quantitative tool, such as software, could eliminate much of the subjectivity such that it could be reiteratively tested, modified, and adopted to provide similar prakriti determination. Therefore, considering the immense potential, an interdisciplinary approach to interrogate Ayurvedic principles in the context of contemporary medicine is essential.[12,18]
Traditionally, the prakriti assessment is carried out by the ayurvedic physician on the basis of his knowledge and experience and is therefore subject to inter-observer variations. The quantitative approach to the qualitative assessment of prakriti for the practice of personalized medicine both by ayurvedic physician and contemporary science is essential and attempts are made based on the use of psychometric scaling; however, these lack the physiological and anatomical features in scaling different prakriti types.[19] In order to define traditional prakriti features and clinical phenotypes on the basis of current knowledge and to develop a uniformly acceptable tool, which will provide a quantitative element to the qualitative determination of prakriti, we have evaluated 3416 normal healthy volunteers using prakriti traits as per traditional texts as well as computer-aided prakriti description tool. We have described our attempt to correlate distribution of prakriti among population and also show a dominant prakriti association with body mass index (BMI).
MATERIALS AND METHODS
Study design
The study was carried out over a period of 2 years at three different centers, Bangalore (Centre1), Pune (Centre2), and Udupi (Centre3) in India. The study protocol was approved by concerned institutional ethical committee and samples were screened after obtaining written informed consent, from all the participants. Healthy male nonsmoking, nonalcoholic subjects of age group between 20 and 30 years were screened for their prakriti. Healthy status of individual, according to the Ayurveda, is based on proper functioning of sensory organs, digestion, excretion process, and comfortable sleep. We excluded participants with diabetes, hypertension, and chronic systemic diseases and also with recent history of acute ailments such as fever. Female subjects were not included in this preliminary study to minimize confounding variations. Each subject was analyzed in a two-step prakriti determination process. First, the subject was interviewed with AyuSoft prakriti software by trained ayurvedic physician lasting about 45 min. Next, the same subject was interviewed and examined by senior ayurvedic physician (vaidya) who was blinded to the AyuSoft result. The senior vaidya with more than 25 years of experience assessed the prakriti of individuals by interview and physical examination. Ayurvedic physician used and filled questionnaires for each individual and prakriti assessment of each individual by vaidya was determined over a period of about 45 min.
Assessment of prakriti by ayurvedic physician
Ayurvedic physician's assessment was based on parameters listed in three primary ayurvedic texts, Charaka Samhita, Susruta Samhita, and Ashtanga Sangraha. All the parameters are expressions of one or the other prakriti as shown in the form of table in supplementary file 1 (110KB, pdf) [Supplementary File1 (110KB, pdf) ].[20,21,22,23] Traditional ayurvedic method of prakriti determination involves a wide range of methods employed by the ayurvedic physician: through physical examination, which involves visual, tactile, olfactory, and auditory assessments; inference based on information collected, by indirect means including asking questions and conclusions drawn based on available data, knowledge, and experience.[22] The parameters include visual assessment of morphological features such as skin color, hair color and consistency, soft tissue to bony tissue proportions; tactile features such as dryness/oiliness of skin, body temperature; analytical features such as radial pulse (naadi); interrogative subjective physical findings such as physical strength, endurance, appetite, sleep and dream patterns, bowel habit, interrogative subjective and intellectual-emotional attributes such as memory, retention, anger response, restlessness/composure [Supplementary File 1 (110KB, pdf) ]. Final conclusion drawn by the ayurvedic physician is based on the assessment of the entire range of these parameters, coupled with direct interaction with the subject. In supplementary file 2 (91.3KB, pdf) , all the parameters considered for the prakriti analysis are mentioned in detail [Supplementary File 2 (91.3KB, pdf) ].
Assessment of prakriti by computer-aided tool – AyuSoft
AyuSoft software was purchased from Centre for Development of Advanced Computing (C-DAC), Pune, Department of Information Technology, Ministry of Communications and Information Technology (MCIT), India. Prakriti assessment by AyuSoft was performed using weightage configuration. There are 85 questions related to the anatomy, physiology, and psychology. Weightage ranging from 1 to 10 is provided for every question to predict the dosha (manifestation of each trait in a given prakriti). Traits related to physical or anatomical features have been assigned higher weightage cut-off as it remains stable throughout the life. In contrast, physiological and psychological factors vary with respect to the habitat and hence lesser weightage was assigned. The prakriti can be determined for all age groups and the weightage configuration can be modulated accordingly within the software by clinicians and thus aids in the assessment of prakriti. All questionnaires define the character of the dosha dominance and report cumulative dominance in percentage within anatomical, physiological, and psychological parameters (www.ayusoft.cdac.in). The Ayurvedic physician who carried out AyuSoft interview was a qualified ayurvedic physician (BAMS graduate) with a minimum of 2 years of experience. Height was measured to the nearest 0.1 cm using wall-mounted stadiometer by asking the subjects to stand straight without footwear. Weight was measured with minimum clothes using a calibrated electronic scale to the nearest 0.1 kg. Height and weight of individuals was measured by the junior ayurvedic physician who was also operating the AyuSoft.
Statistical analysis
The data were collected from all the three centers and prakriti details, BMI and place of birth were tabulated using Microsoft Excel 2007. The BMI was calculated using Quetelet's Index, where BMI is equal to weight in kilograms divided by height in meter squared.[24] Kappa value was determined to see the consistency of the results among the ayurvedic physician and AyuSoft. The graphs generated from various analyses were plotted and the significance of the analysis was computed with the aid of Statistical Package for Social Sciences (SPSS, version 11.5) and GraphPad Prism v5.01. The relatedness parameter in the test was computed with Cramer's test using freely available tool at ‘http://faculty.vassar.edu/lowry/newcs.html’.
RESULTS
Evaluation of AyuSoft
We compared the outcome of two different methods such as outcome of AyuSoft and ayurvedic physician for assessing the prakriti. It was important to validate a consistent tool for prakriti evaluation before any elaborate study to use prakriti as indicator of phenotypes. A total of 3416 subjects were screened for their prakriti. Kappa statistics revealed a substantial agreement with the Kappa value of 0.778 (P <0.001), between ayurvedic physician and AyuSoft [Table 1]. The data suggests fair agreement of 70-80% concordance by combining all the analysis between the two methods [Figure 1A]. A total of 1311 subjects showed a predominant prakriti of equal to or greater than 60%, out of which 971 subjects were analyzed in this study as they have met our inclusion criteria. The inter-observer agreement for the 1311 subjects showed higher kappa value of 0.85 (P < 0.001) [Table 1]. Further, sensitivity and specificity for the AyuSoft's prakriti prediction was evaluated for 1311 subjects. For kapha prakriti, 84.29% sensitivity and high specificity of 98.57% was observed. In the case of pitta prakriti, sensitivity and specificity was found to be higher (95.95% and 92.35%, respectively). The sensitivity and specificity for the prediction of vata prakriti was found to be 97.83% and 98.02%, respectively. The probability of agreeing on pitta prakriti by both vaidya and AyuSoft was found to be low, which could be due to the sample size analyzed of pitta prakriti. In contrast, assessment of “not pitta” prakriti by AyuSoft was highly correlated. The 971 concordant subjects who showed a single dominant prakriti were of the age group between, 20 and 30 years [Figure 2].
Table 1.
Implementation of kappa statistics for the screened and selected subjects in assessment of prakriti by vaidya and Ayusoft
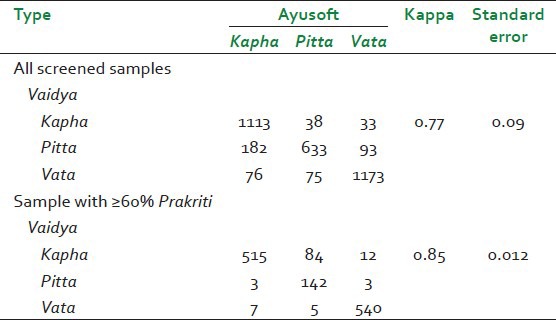
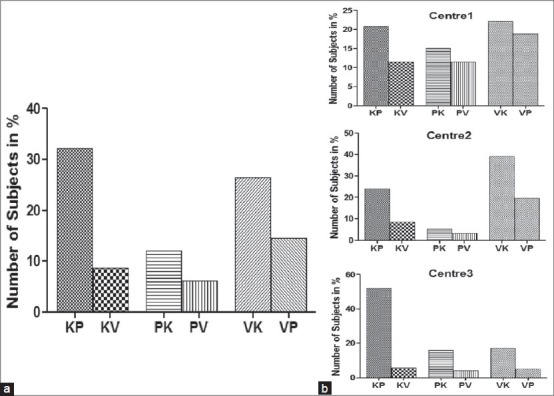
Figure 1.
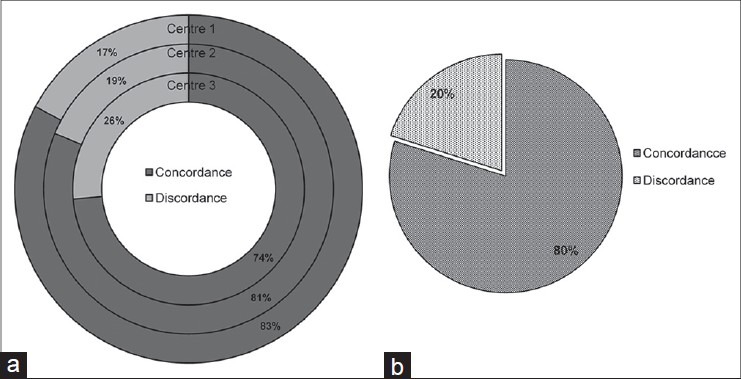
Concordance in the determination of prakriti from three different subject recruitment centers. Prakriti was simultaneously determined by a senior ayurvedic physician and Ayusoft; and analysis of concordance-discordance of the two was plotted. (a) Concordance and discordance in prakriti analysis by a senior ayurvedic physician and Ayusoft in Centers 1, 2, and 3, respectively. (b) Overall concordance and discordance. No significant difference in determination of prakriti among the centers as determined by chi-square test
Figure 2.
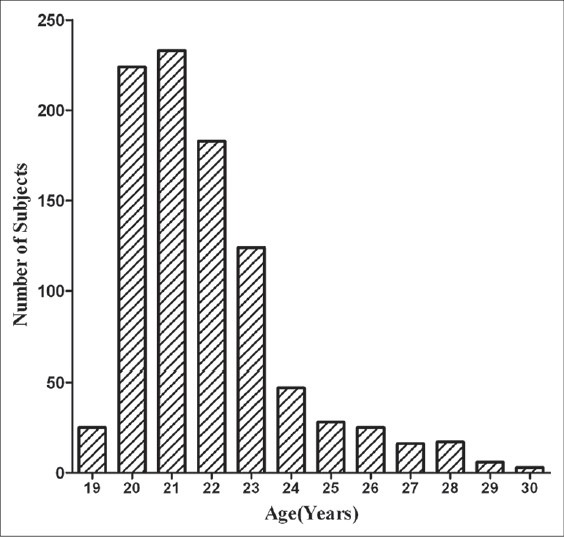
Age distribution in the samples greater than 60% for a single dominant prakriti. Subjects with single dominant prakriti (971) were chosen from 3416 individuals who were enrolled into the study. Age distribution of these individuals is shown, which was also used for computation of BMI
Prakriti distribution
As the subjects included in the study were from three centers of different geographical climatic regions, their distribution of the three constitutional types and regions are shown in Figure 3A. The distribution of selected dominant prakriti samples was higher in proportion for kapha and vata at 41% and lower prevalence of pitta prakriti at 18% [Figure 3B]. In the subjects screened at Centre1, all three constitutions showed variations with vata (41.4%), pitta (26.0%), and kapha (32.4%), respectively. At Centre2, vata subjects represented at higher percentage with 58.8% followed by kapha (32.5%) and pitta (8.5%), respectively. In contrast to Centre2, results from Centre3 showed subjects with kapha prakriti were at 57.6% followed by vata (22.2%) and pitta (20%), respectively [Figure 3C]. The results obtained from screening by ayurvedic physician and AyuSoft also allowed us to identify second dominant prakriti and these are summarized in Figure 4. Of the total subjects included in the study, 32.2% were of kapha-pitta (KP) prakriti while the second highest was observed of vata-kapha (VK) prakriti (26.5%). Pitta-kapha (PK) and vata-pitta (VP) prakriti were 12% and 14.6%, respectively. A lower incidence of the prakriti type was observed in kapha-vata (KV) and pitta-vata (PV) with a distribution of 8.6% and 6.2%, respectively [Figure 4A]. It was interesting to note that, out of 3416 volunteers screened, there were no individuals who scored a nil or beyond 90% for any given prakriti. In addition, four subjects had all the three prakriti in equal proportion (sama prakriti). The minimum percentage of prakriti scored in the screened subjects was of 5% for vata, 8% for pitta, and 5% for kapha. Similarly, maximum percentage of the prakriti observed was 86% for vata, 86% for pitta, and 87% for kapha traits, respectively. The distribution of the second dominant prakriti in the selected subjects across three centre's was also studied [Figure 4]. The KP prakriti was highest in Centre3 (17.1%), while it was 8.4% in Centre2 and 6.7% in Centre1. On the contrary, Centre1 showed highest KV constituent subjects (3.7%) followed by Centre2 with 3% and Centre3 with 1.9%. The PK subjects were also found to be higher in Centre3 with 5.3% followed by Centre2 with 4.8% and Centre1 with 1.9%, respectively. On the contrary, the PV constituent subjects were higher in Centre1 with 3.7% followed by Centre3 with 1.3% and Centre2 with 1.1%. VK combination was found to be highest with 13.6% in Centre2 followed by 7.2% in Centre1 and 5.7% in Centre3. In addition to VK, the VP constituent subjects were found in higher percentage in Centre2 with 6.9% followed by Centre1 with 6.1% and Centre3 with 1.6% [Figure 4B]. These results suggest importance of geographical locations in prakriti distribution of population is a common occurrence with distinct phenotypes.
Figure 3.
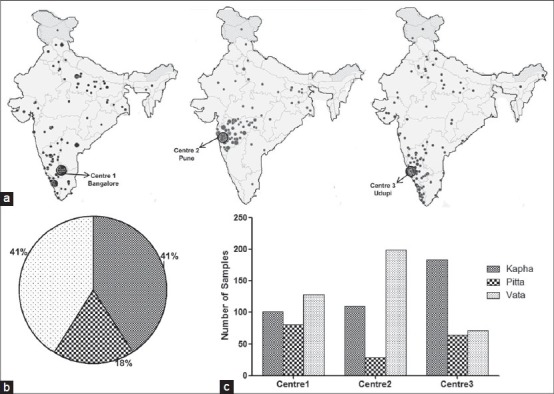
Distribution of three constitutional type of prakriti across three centers. The subjects with prakriti greater than 60% for kapha, pitta, and vata were analyzed for each center and shown. (a) Place of birth of selected subjects is represented as small dots and centre with large dots on the Indian map. (b) Overall distribution of predominance equal to or greater than 60% kapha, pitta, and vata prakriti. (c) Prakriti distribution across three different centers is shown
Figure 4.
Distribution of second dominant dosha within the selected subjects. Letters K, P, and V denotes kapha, pitta, and vata, respectively. Combinations of the constitutional types indicate the second dominant prakriti in the subject. The dominant prakriti is always indicated first in each group. For example, in group KP, kapha is dominant prakriti. (a) Distribution of KP, KV, PK, PV, VK, and VP in all centers. (b) Distribution of KP, KV, PK, PV, VK, and VP across three centers
Association of geographical climatic region and prakriti
All selected individual's place of birth was categorized into three geographical climatic regions namely, arid and semiarid, tropical wet and dry, and last tropical wet, based on the topography-climate-vegetation profile of a given geographical area. According to Ayurveda, place of birth (desha), human body and substances interact continuously and share many properties as they are ultimately derived from the same five classical elements.[25] The concept of place of birth and body types are explained in supplementary files 3 (70.1KB, pdf) and 4 (162.3KB, pdf) [Supplementary Files 3 (70.1KB, pdf) and 4 (162.3KB, pdf) ]. In Tropical wet climate (coastal regions), 49.6% of the subjects possess kapha prakriti as opposed to 21.6% with pitta and 28.8% with vata prakriti. In addition, subjects representing regions with moderate climate (Tropical wet and dry) showed dominant prakriti type of kapha with 43.3% as against to pitta (23.1%) and vata (33.5%), respectively. In contrast, the regions with arid and semi arid climate (dry climatic region) showed vata as the dominant prakriti in individuals with 52.3% compared with pitta (15.3%) and kapha (32.3%) prakriti, respectively [Figure 5]. A statistical test to measure the relatedness was performed that yielded the Cramer's V-value of 0.156, which signifies relatedness with lower significance.
Figure 5.
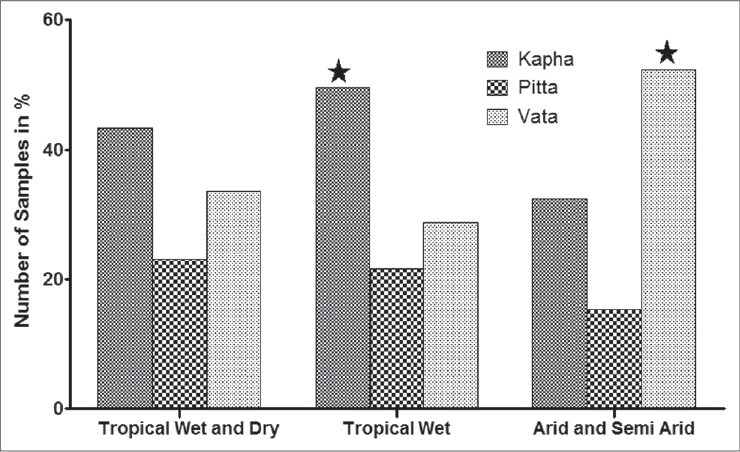
Association between place of birth and prakriti determination. Number of individual observed in each region categorized as tropical wet (Coastal), tropical dry and wet (Moderate), and arid and semi-arid (Dry) Arid and Semi-arid region constitute 52.3% of vata dominant prakriti and tropical wet (Coastal) region is with 49.6% of kapha prakriti and shows slight relatedness Cramer's V-value nearer to 0 (V=0.156) in distribution and marked with “*”
Prakriti and body mass index
In the present study, an attempt was made to establish the association between the prakriti and BMI. BMI was broadly classified into three categories. The subjects with BMI less than 20, between 20 and 25, and greater than 25 were denoted as low, moderate, and high BMI, respectively. In the selected 971 subjects for a predominant prakriti, BMI of less than 20 was found in vata prakriti (71% of the subjects; Chi-square P < 0.0001) followed by pitta (19%) and kapha (10%) prakriti, respectively. The moderate BMI (20-25) was dominant in kapha prakriti (47%) followed by vata (32%) and pitta (21%), respectively. BMI greater than 25 was predominantly found in kapha constituent individuals with 79% incidence as opposed to vata (11%) and pitta (44%) prakriti, respectively [Figure 6]. The impact of the second dosha was also analyzed in relation to BMI; with subjects belonging to kapha constituents and vata prakriti as their second dosha showed lower BMI as opposed to subjects with pitta as their second dosha. A similar trend was also observed in vata constituent subjects who showed higher BMI with kapha as their second prakriti. A statistical test to measure the relatedness using the Cramer's test yielded a value of 0.368 indicating significant relatedness in our observations.
Figure 6.
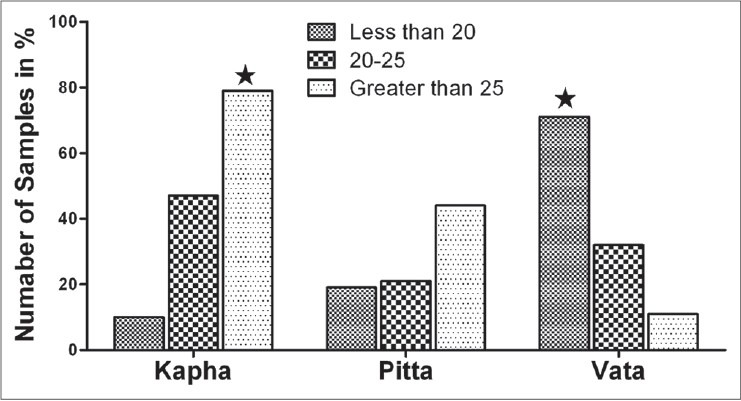
Influence of prakriti on the Body Mass Index (BMI) in selected subjects. BMI was measured for 971 subjects who have shown greater than 60% for a single dominant prakriti. Significant correlation (Cramer's V-value = 0.368) of vata and kapha prakriti in low and high BMI, respectively, is represented with an “*”
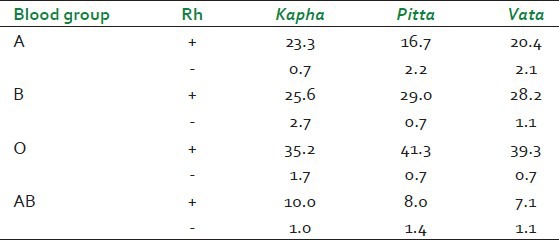
Incidence of different blood group with prakriti
The incidences of each of the blood groups in the three extreme constitutional types were computed and are shown in Table 2. The distribution of A+ blood group was highest among the kapha prakriti subjects (23.3%) followed by vata (20.4%) and pitta prakriti (16.7%), respectively. The scenario with B+ was different with the higher prevalence in pitta (29%) followed by vata (28.2%) and kapha prakriti respectively (25.6%). The same trend was observed in O+ blood group with the higher incidence in pitta (41.3%) followed by vata (39.3%) and kapha (35.2%) prakriti. In the case of AB+ blood group, the higher prevalence was seen in kapha individuals (10%) followed by pitta (8.0%) and vata (7.1%), respectively. The distribution of blood groups was O (37.6%), followed by B (30.7%), A (22.5%), and AB (9.2%). The analysis based on the Rh factor showed higher proportion of Rh+ than the Rh- and there was no significant distribution of Rh factor among prakriti. Our results are in agreement with national average distribution of blood groups.[26,27] None of these showed statistically significant variations among the various prakriti tested.
Table 2.
Distribution of blood groups (in percentage) was represented among dominant prakriti
DISCUSSION
Prakriti assessment is critical to the practice of Ayurveda, which prompted several researchers and ayurvedic practitioners to develop various methodologies. These include pulse detection, psychometric scaling, development of questionnaires and software such as AyuSoft. Prakriti assessment through pulse detection is widely practiced by ayurvedic physicians, which requires experience and knowledge of prakriti prediction. Study on the prakriti assessment using pulse detection by Kurande et al.[28] showed a moderate qualitative agreement among senior ayurvedic physicians. Recently, Shilpa et al.[19] developed systematic questionnaire for the manifestation of prakriti and reported it as satisfactory validity tool in predicting prakriti. However, this approach was limited to the psychological traits alone. Several published reports on the prakriti scaling were based on the systematic questionnaires followed by inter-rater variability analysis and lacked quantitative approach. In this manuscript, we have quantitatively analyzed prakriti by using software together with traditional ayurvedic concepts and have shown a moderate level of reliability. The prakriti determination in Ayurveda is very important in the context of practice of traditional medicine and for its application in diagnostics, disease management, and prognostication of a disease or a condition. Recent works on prakriti phenotype-genotype correlation based on HLA gene polymorphism, CYP2CP polymorphism and EGLN1 polymorphism provided a scientific evidence for the human variations based on the prakriti concept.[14,16,17] In these studies, the assessment of prakriti was qualitative and based on questionnaires developed by ayurvedic physicians, which were further validated by two or more ayurvedic physicians. This kind of approach results in significant inter-rater variability in quantitative estimation of doshas, ultimately in the assessment of prakriti.[29] Prasher et al.[15] screened a total of 850 unrelated normal individuals based on subjective assessment through definitive questionnaires and found 80% of concordance in the inter-rater prakriti determination. Bhalerao et al.[34] developed a set of questionnaires with multiple choice options and have shown concordance of 90% between two clinicians for the assessment of prakriti in a very small population (n = 30).
In the present study, we have compared qualitative and quantitative assessment of prakriti by employing ancient knowledge of Ayurveda and a logical tool, AyuSoft. AyuSoft is a software designed by C-DAC, Pune and is being used for prakriti assessment by several researchers.[30] Here we have screened a total of 3416 subjects in three centers in south India (Bangalore, Pune, and Udupi). The prakriti was first determined by AyuSoft followed by a senior ayurvedic physician for each individual. Comparison between the AyuSoft and ayurvedic physician revealed a fair agreement of 80% concordance [Figure 1B]. Further, sensitivity and specificity of AyuSoft's prediction of prakriti was found to correlate with >60% dominant of a given prakriti.
The prakriti determined at the time of conception depend on various factors involving metaphysical (aatma, purvajanma-krita karma), psychological (sattvaja), protophysical (five classical elements), hereditary (matraja, pitraja), maternal diet, lifestyle, doshik dominance in the maternal reproductive tract, place of birth, time of birth, age of parents, socio-economic condition, and idiosyncrasy.[9,31,32] In the present study, we observed higher proportion of the population screened showed kapha and vata prakriti at 41% and lower prevalence of pitta prakriti at 18% [Figure 3B]. Several research groups have attributed human genetic differences to geographical location and also showed its implications to the modern medicine.[2,32] To understand this difference in the prakriti distribution, we examined the impact of geographical location (desha) of the birth place of dominant prakriti individuals. Research work carried out by Aggarval et al. has shown the link between the EGLN1 gene polymorphism specific prakriti and high altitude adaptation, thus providing an evidence for genomic association of prakriti with geographical location. In the Ayurvedic texts, it is indicated that five classical elements (air, earth, ether, fire, and water) combine in different proportions to form the entire range of naturally formed substances including lands, flora, and human doshas-dhatus-malas.[25] Each desha will have one or the other element dominating in it, and as such each desha has a natural affinity to the corresponding dosha and consequently, to the corresponding prakriti. For example, water (Jala Mahabhuta) is dominant in wet lands (anoopa desha) and kapha dosha, suggesting that wet lands will show a high incidence of kapha prakriti. Supplementary file 5 (65.8KB, pdf) contains table showing impact of geographical location and prakriti [Supplementary File 5 (65.8KB, pdf) ]. The above trend is also evident in our present study wherein the topical wet coastal region shows a higher prevalence of individuals with kapha prakriti (43.3%); while in the dry regions, vata prakriti was more dominant (52.3%). Hence, our results in general, conform to the ayurvedic texts.
We analyzed distribution of BMI across three types of prakriti in selected individuals (N = 971). It has been reported in the traditional texts that kapha prakriti subjects have slower metabolic rates with plump (upachita) or well built (paripurna sarvanga) features. Vata prakriti individuals show features of weight loss (apachita), small structure (alpa shareera), poor eating habits (laghu ahara), and erratic food intake (chapal ahara). Accordingly, when we compared the BMI with specific prakriti types, we found that majority of the individuals with BMI greater than 25 segregated to kapha prakriti (79%). Similarly, 71% of vata prakriti subjects with low and inconsistent food intake were from low BMI group. A previous study has mapped differences in lipid profile among specific prakriti and our study appears to support the findings.[15] Similar trend was observed by Bhalerao et al., where VP prakriti has lesser BMI as compared with KP prakriti.[34] In case of Sasang constitution, Jang et al.[35] reported that Tae-eumin (TE) type were significantly associated with abdominal obesity and considered it as a risk factor for these phenotypes. In this study, BMI was calculated and higher BMI (25.8 ± 2.8) in case of TE were found, which are similar to our results. Using a similar approach, we have observed immune variation in dominant prakriti individuals, selected, based on the same methodology. We have reported a higher level of expression of CD14 markers in pitta and CD25 and CD56 in kapha prakriti, the later correlates with higher immune response observed in individuals with kapha prakriti.[36] These observations are consistent with what is described in ayurvedic texts.
We found AyuSoft being useful in quantitatively expressing the dosha dominance and this is one of the outcomes of the study. The major implications based on the design is that how such a large dipartite human variations can be cohesively partitioned regardless of region (within sampled areas in India), place of birth, and then taking one phenotype (i.e. BMI) for a prakriti for example. In this preliminary study, we show examples of advantages that can be derived from traditional knowledge for the practice of personalized medicine. We also show what features cannot be used (e.g. blood groups). Larger implications of this study can only be extrapolated after a concerted study. This large study was an attempt to find correlations between some of the features described in traditional texts and to draw an analogy to contemporary knowledge by using acceptable methodologies. This was also an attempt to understand how the personalized medicine was traditionally practiced. We believe that our systematic interrogation and findings may bring awareness to the researchers and the validity of science behind the traditional medicine. Some of the aspects that we have studied such as desha, prakriti and BMI relates to what is already mentioned in Ayurvedic literature, which may create a strong base for the practical use of Ayurveda literature. Our study may provide a foundation for undertaking further research, implementation of various aspects of Ayurveda, and gain new perspective about human variations.
CONCLUSION
The present study exemplifies the association of BMI and place of birth of individuals with their constitution type or prakriti, which is in conformity with textual references in Ayurveda. For example, individuals with kapha prakriti show higher BMI as opposed to vata prakriti. In addition, we have also shown that prakriti assessment performed intuitively by the ayurvedic physician has a good correlation with Ayusoft measurements, thereby providing an effective and quantitative instrument to assess the prakriti of individuals. This study suggests the importance of interrogating the ancient concepts and procedures of Ayurveda by the tools of contemporary science, which may yield new knowledge of value in the practice of medicine.
ACKNOWLEDGMENT
The authors gratefully acknowledge the financial support from Office of the Principal Scientific Adviser to the Government of India (PSA to GOI) under the program “A Science Initiative in Ayurveda”. The authors thank Innovation in Science Pursuit for Inspired Research (INSPIRE), Department of Science and Technology, Government of India for providing INSPIRE fellowship to HR. The authors thank Dr. S.M Sathye and Dr. Vilas Nanal, senior ayurvedic physicians for their cooperation and support. The authors gratefully acknowledge cooperation of all the volunteers who have participated in this study.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared.
REFERENCES
- 1.Storey JD, Madeoy J, Strout JL, Wurfel M, Ronald J, Akey JM. Gene-expression variation within and among human populations. Am J Hum Genet. 2007;80:502–9. doi: 10.1086/512017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manica A, Prugnolle F, Balloux F. Geography is a better determinant of human genetic differentiation than ethnicity. Hum Genet. 2005;118:366–71. doi: 10.1007/s00439-005-0039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Race E. The use of racial, ethnic, and ancestral categories in human genetics research. Am J Hum Genet. 2005;77:519–32. doi: 10.1086/491747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rotimi CN. Are medical and nonmedical uses of large-scale genomic markers conflating genetics and ‘race’? Nat Genet. 2004;36:S43–7. doi: 10.1038/ng1439. [DOI] [PubMed] [Google Scholar]
- 5.Hankey A. A test of the systems analysis underlying the scientific theory of Ayurveda's Tridosha. J Altern Complement Med. 2005;11:385–90. doi: 10.1089/acm.2005.11.385. [DOI] [PubMed] [Google Scholar]
- 6.Kim JY, Pham DD, Koh BH. Comparison of Sasang constitutional medicine, traditional chinese medicine and Ayurveda. Evid Based Complement Alternat Med. 2011;2011:239659. doi: 10.1093/ecam/neq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patwardhan B, Warude D, Pushpangadan P, Bhatt N. Ayurveda and traditional Chinese medicine: a comparative overview. Evid Based Complement Alternat Med. 2005;2:465–74. doi: 10.1093/ecam/neh140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jayasundar R. Ayurveda: A distinctive approach to health and disease. Curr Sci India. 2010;98:908–14. [Google Scholar]
- 9.Valiathan MS. 1st ed. Chennai: Orient Longman; 2003. The legacy of Caraka; pp. 1vii–viii. [Google Scholar]
- 10.Valiathan MS. 1st ed. Hyderabad: Hyderabad Universities Press (India) Private Limited; 2009. The legacy of Vagbhata; pp. 2–3. [Google Scholar]
- 11.Mukerji M, Prasher B. Ayurgenomics: A new approach in personalized and preventive medicine. Sci Cult. 2011;77:10–7. [Google Scholar]
- 12.Sethi TP, Prasher B, Mukerji M. Ayurgenomics: A new way of threading molecular variability for stratified medicine. ACS Chem Biol. 2011;6:875–88. doi: 10.1021/cb2003016. [DOI] [PubMed] [Google Scholar]
- 13.Patwardhan B, Mashelkar RA. Traditional medicine-inspired approaches to drug discovery: Can Ayurveda show the way forward? Drug Discov Today. 2009;14:804–11. doi: 10.1016/j.drudis.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 14.Bhushan P, Kalpana J, Arvind C. Classification of human population based on HLA gene polymorphism and the concept of Prakriti in Ayurveda. J Altern Complement Med. 2005;11:349–53. doi: 10.1089/acm.2005.11.349. [DOI] [PubMed] [Google Scholar]
- 15.Prasher B, Negi S, Aggarwal S, Mandal AK, Sethi TP, Deshmukh SR, et al. Whole genome expression and biochemical correlates of extreme constitutional types defined in Ayurveda. J Transl Med. 2008;6:48. doi: 10.1186/1479-5876-6-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ghodke Y, Joshi K, Patwardhan B. Traditional medicine to modern pharmacogenomics: Ayurveda Prakriti type and CYP2C19 gene polymorphism associated with the metabolic variability. Evid Based Complement Alternat Med 2011. 2011:1–5. doi: 10.1093/ecam/nep206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aggarwal S, Negi S, Jha P, Singh PK, Stobdan T, Pasha MA, et al. EGLN1 involvement in high-altitude adaptation revealed through genetic analysis of extreme constitution types defined in Ayurveda. Proc Natl Acad Sci U S A. 2010;107:18961–6. doi: 10.1073/pnas.1006108107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patwardhan B, Bodeker G. Ayurvedic genomics: Establishing a genetic basis for mind-body typologies. J Altern Complement Med. 2008;14:571–6. doi: 10.1089/acm.2007.0515. [DOI] [PubMed] [Google Scholar]
- 19.Shilpa S, Murthy CG. Development and standardization of Mysore Tridosha scale. Ayu. 2011;32:308–14. doi: 10.4103/0974-8520.93905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Acharya YT, editor. Vimanasthana 8/95, Varanasi: Chaukhambha Orientalia; 1997. Charak samhitha; pp. 277–78. [Google Scholar]
- 21.Acharya YT, editor. Sharirasthana 4/65-76, Varanasi: Chaukhambha Sanskrit Sansthan; 2007. Sushrutha samhita; pp. 361–62. [Google Scholar]
- 22.Caldecott T. Ayurveda: The divine science of life. Elsevier Health Sciences. 2006:27–34. [Google Scholar]
- 23.Nambodiri N, editor. Varanasi: Chaukhambha Krishndas Academy; 2010. Ashtang Hrudaya, 3/84-102; pp. 193–95. [Google Scholar]
- 24.Garrow JS, Webster J. Quetelet's index (W/H2) as a measure of fatness. Int J Obes. 1985;9:147–53. [PubMed] [Google Scholar]
- 25.Acharya YT, editor. Varanasi: Chaukhambha Sanskrit Sansthan; 1997. Sushrutha samhita, Sootrasthana 35/42; pp. 157–58. [Google Scholar]
- 26.Das PK, Nair SC, Harris VK, Rose D, Mammen JJ, Bose YN, et al. Distribution of ABO and Rh-D blood groups among blood donors in a tertiary care centre in South India. Trop Doct. 2001;31:47–8. doi: 10.1177/004947550103100121. [DOI] [PubMed] [Google Scholar]
- 27.Periyavan S, Sangeetha SK, Marimuthu P, Manjunath BK, Seema DM. Distribution of ABO and Rhesus-D blood groups in and around Bangalore. Asian J Transfus Sci. 2010;4:41. doi: 10.4103/0973-6247.59391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kurande V, Waagepetersen R, Toft E, Prasad R, Raturi L. Repeatability of pulse diagnosis and body Constitution diagnosis in traditional Indian ayurveda medicine. Global Advances in Health and Medicine. 2012;1:36–42. doi: 10.7453/gahmj.2012.1.5.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rastogi, Sanjeev . In Evidence-Based Practice in Complementary and Alternative Medicine. Berlin Germany, Springer: 2012. Prakriti Analysis in Ayurveda: Envisaging the Need of Better Diagnostic Tools; pp. 99–111. [Google Scholar]
- 30.Mahalle NP, Kulkarni MV, Pendse NM, Naik SS. Association of constitutional type of Ayurveda with cardiovascular risk factors, inflammatory markers and insulin resistance. J Ayurveda Integr Med. 2013;3:150–57. doi: 10.4103/0975-9476.100186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kamini D, Ks D. Factors Influencing Prakriti (Constitution) and Influenced by Prakriti (Constitution) Int J Ayu Herb Med. 2012;2:477–87. [Google Scholar]
- 32.Tripathi NS. Concept of formation of “Prakriti” in ayurveda. Indian J Res. 2011;5:1–5. [Google Scholar]
- 33.Tishkoff SA, Kidd KK. Implications of biogeography of human populations for ‘race’ and medicine. Nat Genet. 2004;36:S21–7. doi: 10.1038/ng1438. [DOI] [PubMed] [Google Scholar]
- 34.Bhalerao S, Deshpande T, Thatte U. Prakriti (Ayurvedic concept of constitution) and variations in platelet aggregation. BMC Complement Altern Med. 2012;12:248–53. doi: 10.1186/1472-6882-12-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eunsu J, Baek Y, Park K, Lee S. Could the Sasang constitution itself be a risk factor of abdominal obesity? BMC Complement Altern Med. 2013;13:72–8. doi: 10.1186/1472-6882-13-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rotti H, Guruprasad KP, Nayak J, Kabbekkodu SP, Kukreja H, Mallya S, et al. Immunophentyping of normal individuals classified on the basis of human dosha prakriti. J Ayurveda Integr Med. 2014;5:43–49. doi: 10.4103/0975-9476.128857. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


