Abstract
Background/Objectives
The role of chronic pain in the occurrence of falls and as a target for falls prevention has received limited attention. We sought to determine the prevalence of clinically relevant falls-related outcomes according to pain status in the older population of the United States.
Design
Cross-sectional analysis of the 2011 National Health and Aging Trends Study, a sample of Medicare enrollees aged ≥65 years (response rate= 71.0%).
Setting
In-person assessments were conducted in the home or residential care facility of the sampled study participant.
Participants
7,601 participants representing 35.3 million Medicare beneficiaries.
Measurements
Participants were asked whether they had been “bothered by pain” and the location of pain as well as questions about balance/coordination, fear of falls, and falls.
Results
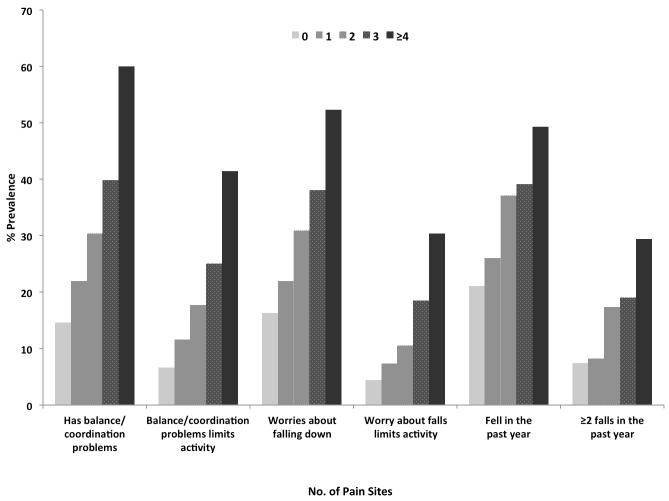
Bothersome pain was reported by 52.9% of the population. Comparing participants with pain to those without pain, the prevalence of recurrent falls (≥2 falls) in the past year was 19.5% and 7.4%, respectively [age- and sex-adjusted prevalence ratio (PR)=2.63; 95% confidence interval (CI):2.28-3.05]. For fear of falls that limits activity, prevalence was 18.0% and 4.4% in those with and without pain, respectively (adjusted PR=3.98; 95% CI:3.24-4.87). Prevalence of balance and falls outcomes increased with number of pain sites. For example, prevalence of problems with balance/coordination that limited activity among participants with 0, 1, 2, 3, and ≥4 sites of pain was 6.6%, 11.6%, 17.7%, 25.0%, and 41.4%, respectively (P<0.001 for trend). Associations were robust to adjustment for several potential confounders, including cognitive and physical performance.
Conclusion
Falls-related outcomes were substantially more common among older adults with pain than in those without pain. Accordingly, pain management strategies should be developed and evaluated for falls prevention.
Keywords: pain; aging; falls, fear of falls; balance; epidemiology
INTRODUCTION
Fall-related injury is a major public health problem that is associated with substantial health care costs and increased risk of disability, hospitalization, nursing home admission, and mortality among older adults.1-4 Several risk factors for falling have been established, including a history of falls, balance impairment, decreased muscle strength, and gait impairment.5 The American Geriatrics Society/British Geriatrics Society (AGS/BGS) practice guidelines for preventing falls recommend interventions for risk factors identified through screening and clinical assessment.6 Interventions that address multiple risk factors have demonstrated significant reduction in the rate of falls among community-dwelling older adults.7 However, the role of chronic pain in the occurrence of falls and as a target for falls prevention has received only limited attention.
Pain is a common symptom among community-dwelling older adults and is the most often cited cause of disability.8-12 A recent analysis of a national sample of Medicare beneficiaries (the National Health and Aging Trends Study) indicated that bothersome pain afflicted over half of the population, three-fourths of whom had pain in multiple anatomic locations, and was significantly associated with decreased grip strength, gait speed, and lower extremity function as measured by the Short Physical Performance Battery, as well as decreased self-reported physical capacity.9 Chronic pain might predispose older persons to falling through multiple pathways, including fear of movement,13 decreased physical activity,14 postural instability,15 muscle weakness and inhibition of neuromuscular response,16, 17 and altered gait and attention.18, 19 Indeed, studies of older adults have shown that chronic pain is associated with falls.20-26 However, the extent of falls-related outcomes in the community-dwelling older adult population has not been characterized according to pain status in a nationally-representative study. Further, most previous studies have not examined the total number of pain sites or specific sites of pain with falls, adjusted for multiple measures of physical capacity, or assessed the association of pain with falls among those without depressive symptoms, a common comorbidity of pain that is associated with increased risk of falling.5, 27 In addition, few studies have investigated the association of pain with fear of falling, a well-established risk factor for falls and activity avoidance among older adults.28 A systematic review published in 2014 identified 12 studies of older adults that examined pain in relation to fear of falling,29 but only 2 of the studies included a non-pain control group, sample sizes were relatively small, and generalizablility was limited. Finally, relatively few studies have investigated the relationship of pain with self-perceived and objective measures of balance, another widely recognized factor associated with falls risk.5 Therefore, using data from a national survey of Medicare beneficiaries, the aims of the current study were to (1) determine the prevalence of falls, fear of falling, and balance impairment according to pain status in the community-dwelling older population of the United States (US); and (2) investigate the association of overall pain status, multisite pain, and site-specific pain with falls, fear of falling, and balance performance.
METHODS
Study Population
Data from the 2011 National Health and Aging Trends Study (NHATS) were analyzed. The NHATS is funded by the US National Institute on Aging, National Institutes of Health to investigate multiple aspects of functioning among older adults.30 Detailed descriptions of the methods and measures used in the NHATS have previously been published.9,30 A stratified, multistage sampling design was used to enroll 8,245 adults ages 65 and older from the Medicare enrollment file [response rate = 71% (8,245/11,637)]. This sample is representative of Medicare beneficiaries living in the contiguous US. There were no exclusion criteria related to health status, cognitive function, or physical function. The study protocol was approved by the Johns Hopkins University Institutional Review Board; all study participants or their proxy-respondents provided written informed consent.
Trained survey research staff conducted in-person interviews and assessments in the homes of study participants living in the community or in residential care facilities (e.g., retirement or assistive living communities). There were 468 (5.7%) participants who were not interviewed because they were living in a nursing home and were not expected to return to their original home residence (instead, a questionnaire was completed by facility staff). Nursing home participants were excluded from the data analysis. The study sample is representative of persons living in all other residential care settings (there were 168 participants in residential care who were not interviewed, but the weights for those in residential care with sample person interviews, n=353, were adjusted to represent those who were missing interviews).30 An additional 5 individuals were excluded because of missing data on the pain questions. Accordingly, the final analytic sample size of the current study was 7,601, which is representative of 35.3 million Medicare beneficiaries living in the US.
Measures
Pain was assessed by asking, “In the last month, have you been bothered by pain?” If the participant answered “yes”, then they were asked to identify the location of pain from a card listing the following anatomic sites: back, hips, knees, legs, feet, hands, wrists, arms, shoulders, stomach, head, and neck. The side of the body where pain occurred was not recorded. The total number of pain sites and selected musculoskeletal sites were analyzed. Participants were also asked how often they took medications for pain: everyday (7 days/week), most days (5-6 days/week), some days (2-4 days/week), rarely (once a week or less), or never.
Several questions about falling were included in the interviews with “yes/no” response options. These questions were prefaced by the following definition: “By falling down we mean any fall, slip, or trip in which you lose your balance and land on the floor or ground or at a lower level.” Participants were asked if they had fallen down in the last 12 months and, if so, had they fallen more than one time in the last 12 months (i.e., recurrent falls). Fear of falling was assessed with the question, “In the last month, did you worry about falling down.” If the participant answered “yes”, then they were asked if this worry ever limited their activities.
Balance was assessed through self-report and performance-based testing. Study participants were asked if they had problems with balance or coordination in the last month and, if so, whether these problems ever limited their activities. Both questions had “yes/no” response options. Standing balance was objectively measured using the protocol of the Short Physical Performance Battery (SPPB)31 and the single legged stand test with eyes open. The SPPB balance protocol instructs participants to stand and maintain their feet in the side-by-side, semi-tandem, and tandem positions for 10 seconds each. If a participant was unable to hold a balance position for a full 10 seconds, then the next more challenging test was not administered. Participants who were able to hold the tandem stand position were then instructed to balance on one leg for 30 seconds with their eyes open. A single timed-trial holding this position was recorded. Participants selected the leg that they preferred to stand on, but there were no practice trials. The following values were assigned for an overall balance score that combines performance on all 4 tests: 0 if participants were unable to hold the side-by-side position for 10 seconds, 1 if participants could only hold the side-by-side standing position for 10 seconds; 2 if they could hold a semi-tandem position for 10 seconds, but were unable to hold a full-tandem position for more than 2 seconds; 3 if they could stand in a full-tandem position for 3 to 9 seconds; 4 if they could stand in a full-tandem position for 10 seconds but did not complete the single-legged balance test; 5, 6, 7, and 8 were assigned to correspond with quartiles of time holding the single-legged stand position; and 9 if they were able to balance on one leg for 30 seconds. Accordingly, balance scores ranged 0-9 with higher scores indicating better performance.
Several other measures of physical capacity were assessed during the home visit. Maximum grip strength was measured in kilograms using a dynamometer (the highest value of 2 trials was analyzed). Usual gait speed was measured in meters per second over a 3 meter course from a standing start (the fastest of 2 timed trials was analyzed). Chair rising performance was assessed and scored according to the SPPB protocol.31 Participants were instructed to rise from a chair and return to the seated position 5 times as quickly as possible while keeping their arms folded over their chest. The time to complete the 5 chair rises was recorded. Scores ranged 0-4, with 0 indicating the inability to complete the test and 4 indicating the highest level of performance.
Tests of verbal recall and orientation were used to assess cognitive function.30 Ten words (common nouns) were read out loud to participants, who were then immediately asked to recall as many words as possible. After an approximately 5-minute delay during which participants answered other survey questions, they were asked again to recall as many of the 10 words as possible. Also assessed was orientation to the day, date, month, and year. The numbers of correct answers to the 3 tests were summed into a composite cognitive performance score, ranging from 0 to 24 possible points.
Demographic and health status variables were also collected during the interview. Participants were asked to report their race/ethnicity and their highest grade of education completed. Smoking status (i.e., never, former, or current smoker) was determined through a standard set of questions. Physical activity was assessed with 2 questions that asked participants whether they walked for exercise or spent time doing vigorous activities that increased their heart rate and breathing in the last month. Participants were assigned to 1 of 3 groups: “sedentary” if they responded ‘no’ to both questions; “walkers” if they answered ‘yes’ to only the question about walking for exercise; or “physically active” if they answered ‘yes’ to the question about vigorous activity. Body mass index (BMI) was calculated by dividing measured weight in kilograms (kg) by measured height in meters squared (m2). Obesity was defined by BMI >30.0 kg/m2. Participants were also asked if a doctor has ever told them that they had any of the following medical conditions: a heart attack or myocardial infarction; high blood pressure or hypertension; arthritis (including osteoarthritis or rheumatoid arthritis); osteoporosis or thinning of the bones; diabetes; lung diseases, such as emphysema, asthma, or chronic bronchitis; a stroke; dementia or Alzheimer’s disease; cancer; a broken or fractured hip (since age 50). The Patient Health Questionnaire-2 (PHQ-2) was used to assess depressive symptoms; a PHQ-2 score >3 was used to define high depressive symptoms.32
Data Analysis
All analyses were weighted to account for unequal probabilities of selection into the NHATS sample. The analytic sample weights account for differential selection of subgroups (e.g., oversampling of black individuals and oldest-old adults) and adjust for non-response. Variance estimates were calculated using a Taylor series linearization that incorporated the complex sample design of the survey. Data management and statistical analysis were performed with Stata/SE version 12.1 (Stata Corp., College Station, Texas).
The characteristics of study participants were compared according to pain status using adjusted Wald and t-test statistics (Table 1). Prevalence ratios (PR) and 95% confidence intervals (CI) were estimated using Poisson regression to compare prevalence of the falls-related binary outcomes by pain status adjusting for age and sex (Table 2). 33 Poisson regression was also used to model the associations of pain status, total number of pain sites, and site-specific pain with falls-related binary outcomes adjusting for multiple potential confounding factors (Tables 3 and 4). Logistic regression models were not fitted as odds ratios can be overestimated when the study outcomes are common.33 Linear regression was used to model the association of pain with the balance performance score of 0-9 points (Table 3a). An ordinal variable was entered in the models to test for linear trend across the total number of pain sites (Table 3ab). For sensitivity analyses, Poisson regression was used to assess the association of pain with the falls-related outcomes in participants without arthritis, high depressive symptoms, or both conditions.
Table 1.
Percent distribution of demographic and health characteristics according to pain status in adults 65 years and older, United States: National Health and Aging Trends Study, 2011
| Bothersome Pain | |||
|---|---|---|---|
| Characteristic | Yes | No | P-Value |
| Age, n (weighted %) | |||
| 65-69 years | 753 (27.6) | 654 (28.3) | 0.185 |
| 70-74 years | 822 (24.5) | 756 (25.5) | |
| 75-79 years | 832 (19.4) | 679 (18.7) | |
| 80-84 years | 795 (14.4) | 710 (15.0) | |
| 85-89 years | 532 (9.6) | 419 (8.5) | |
| ≥90 years | 369 (4.5) | 280 (4.0) | |
| Sex, n (weighted %) | |||
| Women | 2593 (61.8) | 1840 (50.9) | <0.001 |
| Race/Ethnicity, n (weighted %) | |||
| Non-Hispanic White | 2763 (80.5) | 2418 (80.6) | 0.121 |
| Non-Hispanic Black | 934 (8.5) | 726 (7.6) | |
| Hispanic | 248 (6.8) | 206 (6.7) | |
| Other | 114 (3.3) | 104 (3.7) | |
| Education, n (weighted %) | |||
| <9 years | 576 (11.1) | 411 (9.5) | <0.001 |
| 9-11 years | 614 (12.3) | 444 (10.4) | |
| High school graduate | 1107 (28.0) | 961 (27.2) | |
| Some college/vocational | 1017 (27.4) | 797 (24.9) | |
| College graduate | 413 (11.6) | 450 (14.7) | |
| Masters or professional degree | 331 (9.6) | 385 (13.3) | |
| Smoking history, n (weighted %) | |||
| Never smoked | 1994 (46.2) | 1763 (48.6) | 0.055 |
| Former smoker | 1803 (45.7) | 1442 (42.4) | |
| Current smoker | 301 (8.1) | 286 (9.0) | |
| Body mass index, Mean (SE) | 28.3 (0.1) | 26.9 (0.1) | <0.001 |
| Physical activity, n (% weighted) | <0.001 | ||
| Sedentary | 1635 (35.9) | 985 (24.3) | |
| Walks | 1286 (30.7) | 1121 (30.8) | |
| Physically active | 1182 (33.3) | 1389 (44.9) | |
| Medical conditions, n (weighted %) | |||
| Arthritis | 2960 (70.0) | 1285 (35.5) | <0.001 |
| Osteoporosis | 1060 (26.8) | 497 (14.9) | <0.001 |
| Hip fracture | 253 (5.2) | 126 (2.9) | <0.001 |
| Cancer | 1119 (28.0) | 831 (23.4) | <0.001 |
| Myocardial infarction | 720 (16.3) | 441 (11.5) | <0.001 |
| Diabetes | 1193 (27.7) | 730 (19.5) | <0.001 |
| Stroke | 555 (11.6) | 337 (8.3) | 0.001 |
| Dementia | 288 (5.4) | 166 (3.2) | <0.001 |
| Depressive symptoms | 849 (19.0) | 362 (9.6) | <0.001 |
| Total No. of medical conditions, n (weighted %) | |||
| 0 | 149 (4.4) | 467 (14.7) | <0.001 |
| 1 | 484 (13.6) | 809 (24.9) | |
| 2 | 912 (23.2) | 996 (28.2) | |
| 3 | 1049 (24.9) | 676 (18.4) | |
| ≥4 | 1509 (33.9) | 550 (13.8) | |
| Cognitive performance score, Mean (SE) | 11.3 (0.1) | 11.6 (0.1) | 0.007 |
| Grip strength in kilograms, Mean (SE) | 25.8 (0.2) | 28.6 (0.3) | <0.001 |
| Balance performance score, Mean (SE) | 4.4 (0.1) | 5.5 (0.1) | <0.001 |
| Gait speed in meters/second, Mean (SE) | 0.79 (0.01) | 0.88 (0.01) | <0.001 |
| SPPB chair rise score, Mean (SE) | 2.2 (0.03) | 2.8 (0.03) | <0.001 |
| Frequency of analgesic use, n (weighted %) | <0.001 | ||
| Never | 699 (16.6) | 2120 (59.9) | |
| Rarely (once a week or less) | 807 (20.9) | 811 (24.8) | |
| Some days (2-4 days a week) | 876 (21.2) | 262 (7.4) | |
| Most days (5-6 days a week) | 328 (8.2) | 43 (1.1) | |
| Every day (7 days a week) | 1386 (33.1) | 257 (6.9) | |
SE=standard error
Table 2.
Prevalence of balance/coordination problems, fear of falls, and falls according to pain status in adults 65 years and older, United States: National Health and Aging Trends Study, 2011
| Bothersome Pain | Age- and Sex-adjusted Prevalence Ratio (95% CI) Pain : No Pain |
||
|---|---|---|---|
| Yes (n=4,098) %* |
No (n=3,492) %* |
||
| Balance or Coordination Problems | |||
| Has problems with balance or coordination | 40.2 | 14.6 | 2.67 (2.38-3.00) |
| Balance or coordination problems limits activity | 25.7 | 6.6 | 3.83 (3.27-4.49) |
| Fear of Falls | |||
| Worried about falling down | 37.3 | 16.3 | 2.19 (1.98-2.42) |
| Worry about falling down limits activity | 18.0 | 4.4 | 3.98 (3.24-4.87) |
| Falls | |||
| FallsFell in the past year | 38.9 | 21.0 | 1.82 (1.67-1.98) |
| Falls≥2 falls in the past year | 19.5 | 7.4 | 2.63 (2.28-3.05) |
Weighted percents are shown
Table 3ab.
Association of pain and number of pain sites with (A) self-reported problems with balance/coordination and performance-based assessment of standing balance, and (B) fear of falling and falls in adults 65 years and older, United States: National Health and Aging Trends Study, 2011
| A. | |||
|---|---|---|---|
|
| |||
| Problems with balance/coordination PR (95% CI) |
Balance/coordination problems limits activity PR (95% CI) |
Standing balance performance β (95% CI) |
|
| Pain status | |||
| No pain | 1.00 | 1.00 | Ref. |
| Pain | 1.80 (1.59-2.02) | 2.15 (1.79-2.59) | −0.18 (−0.33, −0.02) |
|
| |||
| No. of pain sites | |||
| 0 | 1.00* | 1.00* | Ref. * |
| 1 | 1.32 (1.12-1.55) | 1.57 (1.16-2.12) | −0.04 (−0.25, 0.16) |
| 2 | 1.61 (1.38-1.87) | 1.93 (1.56-2.39) | −0.12 (−0.39, 0.15) |
| 3 | 1.94 (1.62-2.31) | 2.08 (1.56-2.78) | −0.33 (−0.57, −0.08) |
| ≥4 | 2.47 (2.13-2.87) | 2.99 (2.42-3.70) | −0.34 (−0.55, −0.13) |
| B. | ||||
|---|---|---|---|---|
|
| ||||
| Fell in the past year PR (95% CI) |
≥2 falls in the past year PR (95% CI) |
Worries about falling down PR (95% CI) |
Worry about falling limits activity PR (95% CI) |
|
| Pain status | ||||
| No pain | 1.00 | 1.00 | 1.00 | 1.00 |
| Pain | 1.48 (1.33-1.66) | 1.76 (1.48-2.09) | 1.55 (1.37-1.75) | 2.06 (1.59-2.67) |
|
| ||||
| No. of pain sites | ||||
| 0 | 1.00* | 1.00* | 1.00* | 1.00* |
| 1 | 1.21 (1.06-1.38) | 1.00 (0.72-1.39) | 1.26 (1.06-1.50) | 1.49 (1.02-2.19) |
| 2 | 1.53 (1.31-1.79) | 1.96 (1.61-2.40) | 1.53 (1.28-1.84) | 1.65 (1.18-2.32) |
| 3 | 1.54 (1.30-1.83) | 1.81 (1.32-2.47) | 1.63 (1.39-1.91) | 2.41 (1.68-3.46) |
| ≥4 | 1.75 (1.51-2.04) | 2.44 (1.96-3.03) | 1.84 (1.59-2.14) | 2.78 (2.04-3.79) |
P-value <0.001 for test of trend
PR=Prevalence Ratio; CI=Confidence Interval; β=unstandardized regression coefficient
All 6 models adjusted for age, sex, race/ethnicity, education, smoking history, body mass index, obesity, depressive symptoms, dementia, arthritis, osteoporosis, hip fracture, cancer, chronic lung disease, myocardial infarction, diabetes, hypertension, stroke, total number of medical conditions, cognitive performance, exercise, and frequency of analgesic medication use as well as for performance in chair rising, usual gait speed, and grip strength.
P-value <0.001 for test of trend
PR=Prevalence Ratio; CI=Confidence Interval
All 8 models adjusted for age, sex, race/ethnicity, education, smoking history, body mass index, obesity, depressive symptoms, dementia, arthritis, osteoporosis, hip fracture, cancer, chronic lung disease, myocardial infarction, diabetes, hypertension, stroke, total number of medical conditions, cognitive performance, exercise, and frequency of analgesic medication use as well as for performance in balance standing, chair rising, usual gait speed, and grip strength.
Table 4.
Association of specific musculoskeletal pain sites with falls in adults 65 years and older, United States: National Health and Aging Trends Study, 2011
| No. (Weighted %) |
Fell in the past year PR (95% CI) |
≥2 falls in the past year PR (95% CI) |
|
|---|---|---|---|
| Back and other pain sites | |||
| No pain | 2,721 (53.7) | 1.00 | 1.00 |
| Pain sites other than back | 1,003 (19.3) | 1.45 (1.27-1.66) | 1.46 (1.15-1.84) |
| Back only | 247 (4.8) | 1.33 (1.06-1.68) | 1.40 (0.91-2.17) |
| Back and other pain sites | 1,152 (22.2) | 1.56 (1.37-1.78) | 2.16 (1.76-2.65) |
|
| |||
| Knee and other pain sites | |||
| No pain | 2,721 (53.7) | 1.00 | 1.00 |
| Pain sites other than knee | 1,294 (25.7) | 1.42 (1.25-1.61) | 1.67 (1.34-2.08) |
| Knee only | 153 (2.9) | 1.12 (0.84-1.49) | 0.59 (0.28-1.26) |
| Knee and other pain sites | 955 (17.8) | 1.67 (1.45-1.92) | 2.11 (1.73-2.57) |
|
| |||
| Hip and other pain sites | |||
| No pain | 2,721 (53.7) | 1.00 | 1.00 |
| Pain sites other than hip | 1,637 (31.5) | 1.46 (1.31-1.64) | 1.65 (1.35-2.02) |
| Hip only | 62 (1.2) | 0.65 (0.35-1.21) | 1.08 (0.47-2.48) |
| Hip and other pain sites | 703 (13.6) | 1.64 (1.41-1.92) | 2.10 (1.69-2.61) |
|
| |||
| Feet and other pain sites | |||
| No pain | 2,721 (53.7) | 1.00 | 1.00 |
| Pain sites other than feet | 1,657 (31.9) | 1.42 (1.25-1.61) | 1.63 (1.34-1.99) |
| Feet only | 87 (1.8) | 1.73 (1.30-2.31) | 1.50 (0.80-2.80) |
| Feet and other pain sites | 658 (12.6) | 1.64 (1.45-1.86) | 2.16 (1.70-2.73) |
|
| |||
| Shoulder/neck and other pain sites | |||
| No pain | 2,721 (53.7) | 1.00 | 1.00 |
| Pain sites other than shoulder/neck | 1,308 (25.0) | 1.46 (1.30-1.64) | 1.63 (1.32-2.01) |
| Shoulder/neck only | 115 (2.4) | 1.14 (0.75-1.74) | 0.96 (0.43-2.14) |
| Shoulder/neck and other pain sites | 979 (19.0) | 1.58 (1.37-1.82) | 2.06 (1.66-2.55) |
|
| |||
| Hand/wrist/arm and other pain sites | |||
| No pain | 2,721 (53.7) | 1.00 | 1.00 |
| Pain sites other than hand/wrist/arm | 1,695 (32.5) | 1.43 (1.28-1.59) | 1.63 (1.35-1.98) |
| Hand/wrist/arm only | 43 (0.9) | 1.54 (1.01-2.34) | 0.97 (0.28-3.37) |
| Hand/wrist/arm and other pain sites | 664 (12.9) | 1.63 (1.39-1.92) | 2.16 (1.71-2.73) |
PR=Prevalence Ratio; CI=Confidence Interval
All 12 models adjusted for age, sex, race/ethnicity, education, smoking history, body mass index, obesity, depressive symptoms, dementia, arthritis, osteoporosis, hip fracture, cancer, chronic lung disease, myocardial infarction, diabetes, hypertension, stroke, total number of medical conditions, cognitive performance, exercise, and frequency of analgesic medication use as well as for performance in balance standing, chair rising, usual gait speed, and grip strength.
RESULTS
The characteristics of study participants are shown in Table 1 by pain status. Pain did not vary significantly by age or race/ethnicity, but was more common in women than in men and in those with lower levels of education. Older adults with pain were more sedentary and had higher BMI values, greater disease burden, and lower cognitive and physical performance than those without pain. As expected, daily analgesic use was more common among older adults with pain than in those who did not report pain.
The prevalence of balance/coordination problems, fear of falls, and falls in the past year are shown in Table 2 according to pain status. All 6 balance/falls outcomes were approximately 2 to 4 times more common among older adults with bothersome pain than in those without pain adjusting for age and sex (P<0.001 for all comparisons). In terms of absolute numbers in the Medicare population, there were 3.6 million older adults with pain who reported recurrent falls (≥2 falls) in the past year compared with 1.2 million older adults without pain (P<0.0001). For fear of falls that limits activity, the absolute numbers were 3.4 million and 0.7 million in those with pain and without pain, respectively (P<0.0001). Accordingly, the subpopulation of older adults with pain comprises the majority of fallers in the total older adult population.
In addition to pain status, Figure 1 illustrates that the prevalence of falls-related outcomes increased with the total of number of pain sites. When adjusting for potential confounding factors, including cognitive performance, chair rising ability, gait speed, and grip strength, the association of total number of pain sites with self-reported problems with balance/coordination remained significant and graded in a stepwise fashion (Table 3a; P for trend<0.001). Further, objectively measured standing balance performance decreased with greater number of pain sites (Table 3a; P for trend<0.001). Similar associations of pain status and number of pain sites were observed with falls in the past year and fear of falls adjusting for potential confounders, including balance performance (Table 3b). Excluding head and stomach pain did not meaningfully change any of the associations of total number of pain sites with the falls-related outcomes (P for trend<0.001 for each fall-related outcome; results not shown).
Figure 1.
Prevalence of balance/coordination problems, fear of falling, and falls according to the number of pain sites in adults 65 years and older, United States: National Health and Aging Trends Study, 2011
The associations of specific musculoskeletal pain sites with falls outcomes are shown in Table 4. Although back pain alone and foot pain alone were each individually associated with increased prevalence of a fall in the past year, relatively few older adults had pain only in these locations or in any other single location. Importantly, each of the musculoskeletal pain sites was associated with falls when it co-occurred with pain in other locations.
To assess the pain-falls relationship further, sensitivity analyses were performed by excluding participants with arthritis and/or high depressive symptoms, 2 common conditions that are established risk factors for falls and that are often comorbid with pain. Adjusting for the same covariates listed in Table 3b, pain was associated with increased likelihood of recurrent falls in the past year even when excluding participants with arthritis (adjusted PR=1.49; 95% CI: 1.11-2.00), high depressive symptoms (adjusted PR=1.84; 95% CI: 1.48-2.29), or both conditions (adjusted PR=1.60; 95% CI: 1.18-2.16). Pain also remained significantly associated with balance problems that limited activity (adjusted PR=2.15; 95% CI: 1.52-3.04) and fear of falls that limited activity (adjusted PR=1.92; 95% CI: 1.26-2.93) when excluding participants with arthritis and depressive symptoms. Notably, the associations of pain with activity limiting balance problems (adjusted PR=3.89; 95% CI: 2.34-6.48) and activity limiting fear of falls (adjusted PR=2.21; 95% CI: 1.07-4.56) remained after further exclusion of participants who reported a fall in the previous year.
DISCUSSION
In this nationally representative sample of Medicare beneficiaries in 2011, problems with balance or coordination, fear of falls, and a history of falls were substantially more common among older adults with bothersome pain than in those without pain. Indeed, approximately three-fourths of older adults who reported recurrent falls had bothersome pain (Table 2). Similar distributions of pain were observed in older adults who limited their activity because of problems with balance or coordination and in those who reported a fear of falling that limited their activity. Importantly, the prevalence of falls-related outcomes increased with the total number of pain sites, particularly for recurrent falls—an outcome strongly associated with a high risk of serious injury. Given that 40% of community-dwelling older adults have pain in 2 or more locations,9 the findings of the current study indicate that older adults with multisite pain should be targeted for falls prevention services.
Prior studies have also demonstrated an association between pain and falls among older adults.20, 22-24, 34 For example, in a cohort of 749 older adults living in Boston, Leveille and colleagues prospectively showed that greater pain intensity, increased pain interference with function, and polyarticular (multisite) pain were associated with increased risk of falls over an 18-month period.24 Additionally, prospective studies of hip pain and knee pain have reported associations with falls.21, 34 Interestingly, the association of osteoarthritis with fractures is mixed with some studies indicating increased risk,21, 35, 36 no significant risk21, 37, or even decreased risk.38-40 The current study extends this previous work by estimating the prevalence of falls according to pain status in a large sample of community-dwelling older adults that is representative of 35.3 million Medicare beneficiaries in the US. We also extend previous findings from the NHATS showing that not only is pain strongly associated with decreased muscle strength, gait speed, and overall lower extremity function,9 but also associated with impaired balance and activity-limiting fear of falling—2 common, well-established risk factors for falls. Pain was associated with self-reported problems with balance or coordination and with performance-based assessment of balance, indicating that both self-appraisal of balance ability and actual balance capacity are reduced among older adults with pain. Further, the pain-falls relationship was robust even when excluding older adults with comorbid arthritis and/or high depressive symptoms, a finding not previously reported.
Several potential and not necessarily independent mechanisms might underlie the association of pain with falls. Considering, for example, that chronic musculoskeletal pain is associated with decreased physical activity, it is conceivable that pain predisposes older persons to cycles of disuse or bouts of disability that contribute to muscle weakening, reduced endurance, and gait slowing over time. Pain, particularly in the lower body (i.e., back, hips, knees, and feet), can also alter gait biomechanics and postural stability,15, 18, 19, 41-44 which over time possibly increase feelings of unsteadiness and a fear of falling that in turn can reduce the pattern, volume, and intensity of physical activity. Pain-associated inhibition of muscle function and knee buckling may contribute to falls as well.16, 17, 45 An increased risk for falls might also result from changes in brain structure and function that are associated with chronic pain, such as decreased gray matter volume in regions involved with pain processing and motor control as well as decreased attention and executive function.46-48 Finally, certain pharmacological treatments of chronic pain (e.g., opioids) are associated with increased risk for falls and fractures,49, 50 although the proportion of older adults on long-term prescription analgesics and adherence to these treatment regimens are relatively low when considering the high prevalence of falls observed among those with pain.51, 52 It is likely that any causal effect of pain on falls evolves from a combination of maladaptive behavior and physiologic impairments.
There are several strengths and limitations that should be considered when interpreting the study findings. The primary aim of the current study was to determine the scope of clinically relevant falls-related outcomes according to pain in the community-dwelling older adult population. Although the cross-sectional design is appropriate for this study purpose, a recognized limitation is that causal relationships cannot be inferred and that falls were assessed by self-reported recall over the past year. It is certainly possible that some proportion of pain cases among older adults results from falls-related injuries and that participants with pain might be more likely to report a fall (i.e., recall bias); however, as previously noted, several prospective studies have demonstrated an increased risk for falls associated with chronic pain. Indeed, using monthly assessments, Leveille et al. showed that greater pain severity significantly increased the risk of falls in the subsequent month.24
Another limitation of the current study was that detailed information about pain characteristics, such as quality, severity, duration, or frequency, were not collected. Nonetheless, asking older adults whether they are bothered by pain has good face-validity, and this questionnaire item was previously shown to be strongly associated with depressive symptoms, chronic musculoskeletal conditions, and several self-reported and performance-based measures of physical capacity.9 Specific treatment information for pain also was not available, but the frequency of analgesic medication use was assessed and accounted for in the statistical models. A strength of the study was that the location of pain was assessed, which enabled examination of the associations of site-specific pain as well as the number of pain sites with the falls outcomes. In addition, several measures of health and function were assessed that allowed us to adjust for many potential factors that may confound the pain-falls relationship, including cognitive function, physical performance, and exercise. The large sample size permitted a series of sensitivity analyses that demonstrated the robust association of pain with falls, fear of falls and balance problems after excluding participants with arthritis and high depressive symptoms. Finally, a clear strength is the generalizability of the study sample to the older, community-dwelling Medicare population.
In summary, pain is a common condition that is strongly associated with falls-related outcomes that are known to increase risk for serious injury among older adults. In fact, the NHATS falls-related questions are similar to the screening questions recommended in the AGS/BGS clinical practice guidelines for falls prevention6 and recommended by the Centers for Disease Control and Prevention53 as well as ones mandated by the Center for Medicare and Medicaid Services.54 Although pain is increasingly recognized as a risk factor for falls,5, 55 few intervention studies, if any, have targeted pain to prevent falls in community settings. In view of the findings of the current study and others, effective pain management strategies should be developed and integrated into multifactorial falls prevention programs.
ACKNOWLEDGEMENTS
Funding: The National Health and Aging Trends Study is sponsored by the National Institute on Aging (grant number NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health.
Sponsor’s Role: The National Institute on Aging had no role in the design and conduct of the current study; management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Author Contributions: Kushang V. Patel conceived the study, analyzed the data, and wrote the initial draft of the manuscript and revised it; Elizabeth A. Phelan, Suzanne G. Leveille, Sarah E. Lamb, Celestin Missikpode, Robert B. Wallace, Jack M. Guralnik, and Dennis C. Turk interpreted the data, provided critical feedback, and revised the manuscript.
REFERENCES
- [1].Rubenstein LZ. Falls in older people: Epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35(Suppl 2):ii37–ii41. doi: 10.1093/ageing/afl084. [DOI] [PubMed] [Google Scholar]
- [2].Shumway-Cook A, Ciol MA, Hoffman J, et al. Falls in the Medicare population: incidence, associated factors, and impact on health care. Phys Ther. 2009;89:324–332. doi: 10.2522/ptj.20070107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bohl AA, Phelan EA, Fishman PA, et al. How are the costs of care for medical falls distributed? The costs of medical falls by component of cost, timing, and injury severity. Gerontologist. 2012;52:664–675. doi: 10.1093/geront/gnr151. [DOI] [PubMed] [Google Scholar]
- [4].Gill TM, Murphy TE, Gahbauer EA, et al. Association of injurious falls with disability outcomes and nursing home admissions in community-living older persons. Am J Epidemiol. 2013;178:418–425. doi: 10.1093/aje/kws554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Tinetti ME, Kumar C. The patient who falls: “It’s always a trade-off”. JAMA. 2010;303:258–266. doi: 10.1001/jama.2009.2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Panel on Prevention of Falls in Older Persons AGS, British Geriatrics S Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- [7].Gillespie LD, Robertson MC, Gillespie WJ, et al. Interventions for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2012;9 doi: 10.1002/14651858.CD007146.pub3. CD007146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Covinsky KE, Lindquist K, Dunlop DD, et al. Pain, functional limitations, and aging. J Am Geriatr Soc. 2009;57:1556–1561. doi: 10.1111/j.1532-5415.2009.02388.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Patel KV, Guralnik JM, Dansie EJ, et al. Prevalence and impact of pain among older adults in the United States: Findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154:2649–2657. doi: 10.1016/j.pain.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ettinger WH, Jr, Fried LP, Harris T, et al. Self-reported causes of physical disability in older people: The Cardiovascular Health Study. CHS Collaborative Research Group. J Am Geriatr Soc. 1994;42:1035–1044. doi: 10.1111/j.1532-5415.1994.tb06206.x. [DOI] [PubMed] [Google Scholar]
- [11].Leveille SG, Fried L, Guralnik JM. Disabling symptoms: What do older women report? J Gen Intern Med. 2002;17:766–773. doi: 10.1046/j.1525-1497.2002.20229.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Melzer D, Gardener E, Guralnik JM. Mobility disability in the middle-aged: cross-sectional associations in the English Longitudinal Study of Ageing. Age Ageing. 2005;34:594–602. doi: 10.1093/ageing/afi188. [DOI] [PubMed] [Google Scholar]
- [13].Vlaeyen JW, Kole-Snijders AM, Boeren RG, van Eek H. Fear of movement/(re)injury in chronic low back pain and its relation to behavioral performance. Pain. 1995;62:363–372. doi: 10.1016/0304-3959(94)00279-N. [DOI] [PubMed] [Google Scholar]
- [14].Patel KV, Dansie EJ, Turk DC. Impact of chronic musculoskeletal pain on objectively measured daily physical activity: A review of current findings. Pain Manag. 2013;3:467–474. doi: 10.2217/pmt.13.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lihavainen K, Sipila S, Rantanen T, et al. Contribution of musculoskeletal pain to postural balance in community-dwelling people aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2010;65A:990–996. doi: 10.1093/gerona/glq052. [DOI] [PubMed] [Google Scholar]
- [16].Graven-Nielsen T, Lund H, Arendt-Nielsen L, et al. Inhibition of maximal voluntary contraction force by experimental muscle pain: A centrally mediated mechanism. Muscle Nerve. 2002;26:708–712. doi: 10.1002/mus.10225. [DOI] [PubMed] [Google Scholar]
- [17].Henriksen M, Alkjaer T, Simonsen EB, et al. Experimental muscle pain during a forward lunge--the effects on knee joint dynamics and electromyographic activity. Br J Sports Med. 2009;43:503–507. doi: 10.1136/bjsm.2008.050393. [DOI] [PubMed] [Google Scholar]
- [18].Lamoth CJ, Meijer OG, Daffertshofer A, et al. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: Changes in motor control. Eur Spine J. 2006;15:23–40. doi: 10.1007/s00586-004-0825-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Lamoth CJ, Stins JF, Pont M, et al. Effects of attention on the control of locomotion in individuals with chronic low back pain. J Neuroeng Rehabil. 2008;5:13. doi: 10.1186/1743-0003-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Arden NK, Crozier S, Smith H, et al. Knee pain, knee osteoarthritis, and the risk of fracture. Arthritis Rheum. 2006;55:610–615. doi: 10.1002/art.22088. [DOI] [PubMed] [Google Scholar]
- [21].Arden NK, Nevitt MC, Lane NE, et al. Osteoarthritis and risk of falls, rates of bone loss, and osteoporotic fractures. Study of Osteoporotic Fractures Research Group. Arthritis Rheum. 1999;42:1378–1385. doi: 10.1002/1529-0131(199907)42:7<1378::AID-ANR11>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- [22].Blyth FM, Cumming R, Mitchell P, et al. Pain and falls in older people. Eur J Pain. 2007;11:564–571. doi: 10.1016/j.ejpain.2006.08.001. [DOI] [PubMed] [Google Scholar]
- [23].Leveille SG, Bean J, Bandeen-Roche K, et al. Musculoskeletal pain and risk for falls in older disabled women living in the community. J Am Geriatr Soc. 2002;50:671–678. doi: 10.1046/j.1532-5415.2002.50161.x. [DOI] [PubMed] [Google Scholar]
- [24].Leveille SG, Jones RN, Kiely DK, et al. Chronic musculoskeletal pain and the occurrence of falls in an older population. JAMA. 2009;302:2214–2221. doi: 10.1001/jama.2009.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Mickle KJ, Munro BJ, Lord SR, et al. Foot pain, plantar pressures, and falls in older people: A prospective study. J Am Geriatr Soc. 2010;58:1936–1940. doi: 10.1111/j.1532-5415.2010.03061.x. [DOI] [PubMed] [Google Scholar]
- [26].Stubbs B, Binnekade T, Eggermont L, et al. Pain and the risk for falls in community-dwelling older adults: Systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95:175–187. e179. doi: 10.1016/j.apmr.2013.08.241. [DOI] [PubMed] [Google Scholar]
- [27].Eggermont LH, Penninx BW, Jones RN, et al. Depressive symptoms, chronic pain, and falls in older community-dwelling adults: The MOBILIZE Boston Study. J Am Geriatr Soc. 2012;60:230–237. doi: 10.1111/j.1532-5415.2011.03829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Scheffer AC, Schuurmans MJ, van Dijk N, et al. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Ageing. 2008;37:19–24. doi: 10.1093/ageing/afm169. [DOI] [PubMed] [Google Scholar]
- [29].Stubbs B, West E, Patchay S, et al. Is there a relationship between pain and psychological concerns related to falling in community dwelling older adults? A systematic review. Disabil Rehabil. 2014 Jan 28; doi: 10.3109/09638288.2014.882419. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- [30].Kasper JD, Freedman VA. National Health and Aging Trends Study Round 1 Users Guide. Johns Hopkins University School of Public Health; Baltimore: 2012. [Google Scholar]
- [31].Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- [32].Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: Validity of a two-item depression screener. Med Care. 2003;41:1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- [33].Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences. Am J Epidemiol. 2005;162:199–200. doi: 10.1093/aje/kwi188. [DOI] [PubMed] [Google Scholar]
- [34].Nevitt MC, Cummings SR, Kidd S, et al. Risk factors for recurrent nonsyncopal falls. A prospective study. JAMA. 1989;261:2663–2668. [PubMed] [Google Scholar]
- [35].Bergink AP, van der Klift M, Hofman A, et al. Osteoarthritis of the knee is associated with vertebral and nonvertebral fractures in the elderly: The Rotterdam Study. Arthritis Rheum. 2003;49:648–657. doi: 10.1002/art.11380. [DOI] [PubMed] [Google Scholar]
- [36].Wright NC, Lisse JR, Walitt BT, et al. Women’s Health Initiative I. Arthritis increases the risk for fractures--results from the Women’s Health Initiative. J Rheumatol. 2011;38:1680–1688. doi: 10.3899/jrheum.101196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Jones G, Nguyen T, Sambrook PN, et al. Osteoarthritis, bone density, postural stability, and osteoporotic fractures: A population based study. J Rheumatol. 1995;22:921–925. [PubMed] [Google Scholar]
- [38].Cumming RG, Klineberg RJ. Epidemiological study of the relation between arthritis of the hip and hip fractures. Ann Rheum Dis. 1993;52:707–710. doi: 10.1136/ard.52.10.707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Dequeker J, Johnell O. Osteoarthritis protects against femoral neck fracture: The MEDOS study experience. Bone. 1993;14(Suppl 1):S51–56. doi: 10.1016/8756-3282(93)90350-j. [DOI] [PubMed] [Google Scholar]
- [40].Kanis J, Johnell O, Gullberg B, et al. Risk factors for hip fracture in men from southern Europe: The MEDOS study. Mediterranean Osteoporosis Study. Osteoporos Int. 1999;9:45–54. doi: 10.1007/s001980050115. [DOI] [PubMed] [Google Scholar]
- [41].Thorp LE, Sumner DR, Wimmer MA, et al. Relationship between pain and medial knee joint loading in mild radiographic knee osteoarthritis. Arthritis Rheum. 2007;57:1254–1260. doi: 10.1002/art.22991. [DOI] [PubMed] [Google Scholar]
- [42].Hurwitz DE, Ryals AR, Block JA, et al. Knee pain and joint loading in subjects with osteoarthritis of the knee. J Orthop Res. 2000;18:572–579. doi: 10.1002/jor.1100180409. [DOI] [PubMed] [Google Scholar]
- [43].Maly MR, Costigan PA, Olney SJ. Mechanical factors relate to pain in knee osteoarthritis. Clin Biomech (Bristol, Avon) 2008;23:796–805. doi: 10.1016/j.clinbiomech.2008.01.014. [DOI] [PubMed] [Google Scholar]
- [44].Eggermont LH, Bean JF, Guralnik JM, et al. Comparing pain severity versus pain location in the MOBILIZE Boston study: Chronic pain and lower extremity function. J Gerontol A Biol Sci Med Sci. 2009;64:763–770. doi: 10.1093/gerona/glp016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Felson DT, Niu J, McClennan C, et al. Knee buckling: prevalence, risk factors, and associated limitations in function. Ann Intern Med. 2007;147:534–540. doi: 10.7326/0003-4819-147-8-200710160-00005. [DOI] [PubMed] [Google Scholar]
- [46].Weiner DK, Rudy TE, Morrow L, et al. The relationship between pain, neuropsychological performance, and physical function in community-dwelling older adults with chronic low back pain. Pain Med. 2006;7:60–70. doi: 10.1111/j.1526-4637.2006.00091.x. [DOI] [PubMed] [Google Scholar]
- [47].Buckalew N, Haut MW, Morrow L, et al. Chronic pain is associated with brain volume loss in older adults: Preliminary evidence. Pain Med. 2008;9:240–248. doi: 10.1111/j.1526-4637.2008.00412.x. [DOI] [PubMed] [Google Scholar]
- [48].Smallwood RF, Laird AR, Ramage AE, et al. Structural brain anomalies and chronic pain: a quantitative meta-analysis of gray matter volume. J Pain. 2013;14:663–675. doi: 10.1016/j.jpain.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169:1952–1960. doi: 10.1001/archinternmed.2009.357. [DOI] [PubMed] [Google Scholar]
- [50].Rolita L, Spegman A, Tang X, et al. Greater number of narcotic analgesic prescriptions for osteoarthritis is associated with falls and fractures in elderly adults. J Am Geriatr Soc. 2013;61:335–340. doi: 10.1111/jgs.12148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Pahor M, Guralnik JM, Wan JY, et al. Lower body osteoarticular pain and dose of analgesic medications in older disabled women: The Women’s Health and Aging Study. Am J Public Health. 1999;89:930–934. doi: 10.2105/ajph.89.6.930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Stewart C, Leveille SG, Shmerling RH, et al. Management of persistent pain in older adults: The MOBILIZE Boston Study. J Am Geriatr Soc. 2012;60:2081–2086. doi: 10.1111/j.1532-5415.2012.04197.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Stevens JA, Phelan EA. Development of STEADI: A fall prevention resource for health care providers. Health Promot Pract. 2013;14:706–714. doi: 10.1177/1524839912463576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Shubert TE, Smith ML, Prizer LP, et al. Complexities of fall prevention in clinical settings: A commentary. Gerontologist. 2013 Jul 25; doi: 10.1093/geront/gnt079. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- [55].Deandrea S, Lucenteforte E, Bravi F, et al. Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology. 2010;21:658–668. doi: 10.1097/EDE.0b013e3181e89905. [DOI] [PubMed] [Google Scholar]