Abstract
Objectives
We aimed to assess women's contraceptive preferences and use in the first 6 months after delivery. The postpartum period represents a key opportunity for women to learn about and obtain effective contraception, especially since 50% of unintended pregnancies to parous women occur within 2 years of a previous birth.
Methods
We conducted a prospective cohort study of 800 postpartum women recruited from three hospitals in Austin and El Paso, TX. Women aged 18–44 who wanted to delay childbearing for at least 24 months were eligible for the study and completed interviews following delivery and at 3 and 6 months postpartum. Participants were asked about the contraceptive method they were currently using and the method they would prefer to use at 6 months after delivery.
Results
At 6 months postpartum, 13% of women were using an IUD or implant, and 17% were sterilized or had a partner who had had a vasectomy. Twenty-four percent were using hormonal methods, and 45% relied on less effective methods, mainly condoms and withdrawal. Yet 44% reported that they would prefer to be using sterilization, and 34% would prefer to be using LARC.
Conclusions
This study shows a considerable preference for LARC and permanent methods at six months postpartum. However, there is a marked discordance between women's method preference and actual use, indicating substantial unmet demand for highly effective methods of contraception.
Keywords: LARC, female sterilization, postpartum contraception, Hispanic, Texas
1. Introduction
Although much is known about the mix of contraceptive methods in use in the United States (U.S.), it is unclear whether the current distribution actually reflects women's preferences. Many women who intend to limit their fertility or delay childbearing continue to rely on methods with relatively high typical-use failure rates such as oral contraceptives, condoms, and withdrawal. While use of long-acting reversible contraception (LARC) has increased over the last decade[1,2], it has been argued persuasively that unintended pregnancy rates could be reduced if more women relied on highly effective methods [3,4].
Yet low utilization of LARC may not reflect the true underlying demand for the IUD and implant. Several demonstration projects, particularly the Contraceptive CHOICE Project in St. Louis, have shown a dramatic uptake of LARC when there is supportive counseling and the methods are provided at no cost [5,6]. Demand for male and female sterilization may not be fully met either due to a variety of access barriers [7-13].
According to the most recent cycle of the National Survey of Family Growth (NSFG), approximately half of all pregnancies in the U.S. are unwanted or mistimed, and 61% of all unintended pregnancies and 75% of unwanted births occur to women who have already had at least one live birth [14,15]. Furthermore, despite the improved access to healthcare and insurance coverage in the immediate postpartum period, and the increased motivation to prevent pregnancy, over half of unintended pregnancies occur within two years following delivery [16]. In this paper, our objectives are to describe contraceptive method preferences in the postpartum period among women in two cities in Texas, and to determine whether women are able to access their preferred methods.
2. Materials and Methods
This study was conducted shortly after the Texas state legislature drastically reduced funding for family planning, and many providers of subsidized family planning services had experienced substantial cuts in their budgets [17]. Participants were recruited after delivery at one hospital in Austin, and two in El Paso chosen to obtain a mix of publicly and privately insured participants and socioeconomic groups. We aimed to enroll four hundred women in each city: 300 who were publicly insured and 100 who were privately insured at the time of delivery. Eligible participants were aged between 18 and 44 years, did not want more children for at least two years at the time of recruitment, delivered a healthy singleton infant whom they expected would go home with them upon discharge, spoke English or Spanish, and lived in the U.S. within 50 miles of the hospital of recruitment. After obtaining signed informed consent from participants, we administered a 20-minute face-to-face baseline interview. Recruitment took place between April and July 2012 in Austin, and between July and November 2012 in El Paso. Follow-up interviews were conducted by telephone at 3 months, 6 months, and 9 months postpartum. We offered a $30 incentive for completing the initial interview, and $15 for completing each of the telephone interviews.
The initial baseline questionnaire collected information on demographic and socioeconomic variables including age, parity, relationship status, ethnicity, education, insurance status, and income. Insurance status, future childbearing intentions, and contraceptive use were assessed at baseline and in each of the three succeeding interviews. Intentions were assessed using the question “Do you plan to have more children in the future?” Those who did want more children were asked a follow-up question to assess the desired timing. In the baseline interview, participants were asked if they had had a tubal ligation, or if an IUD or subdermal implant had been inserted while they were in the hospital. At each successive interview, the contraceptive use questions referred to the full range of methods with a prompt for use of methods that might not be thought of as birth control such as abstinence, or a method that a spouse or partner was using. The very small number of women who stated that they were using two methods together were classified as using the more effective of the two methods [18].
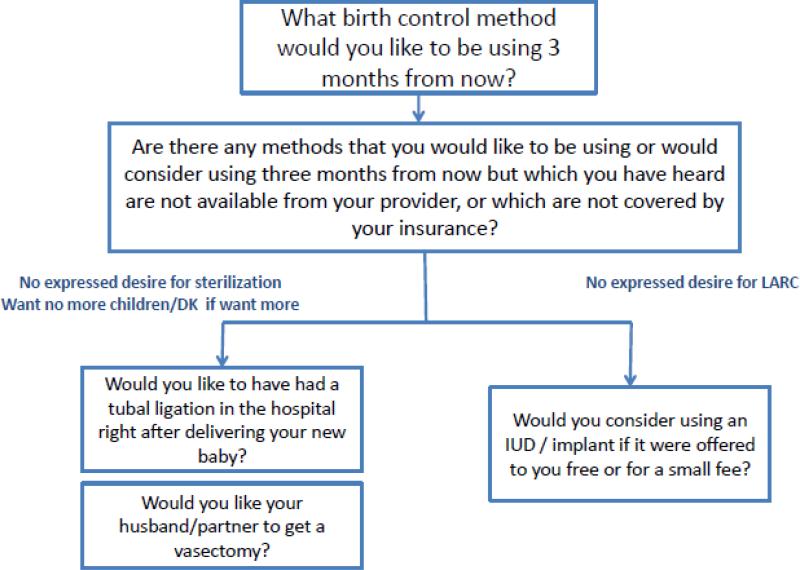
To track participants’ contraceptive preferences, we designed a panel of questions asked over the course of the first three interviews (Figure 1). At the three-month postpartum interview, we asked about the birth control method participants wanted to be using at six months postpartum. We chose six months since by that time most women have resumed sexual relations, and will no longer be relying on exclusive breastfeeding as a contraceptive. This interview also included a prompt asking for any method that the participant might have left out because it was too expensive or not covered by her insurance. At the six-month interview, women who had not mentioned LARC in response to any previous question were also asked “Would you consider using an IUD if it was offered free or for a small fee?” The same question was also asked about the implant. To ensure demand for sterilization was fully captured, women who had not previously expressed a desire for tubal ligation or vasectomy, and who did not want any more children or who did not know if they wanted more children in the future were also asked “Would you like to have had a tubal ligation in the hospital right after you had your new baby?” Finally, these same participants were asked, “Would you like your husband/partner to get a vasectomy?”
Figure 1.
Questions used to measure contraceptive preferences six months postpartum
We distinguished between a participant's preferred contraceptive method given in response to the direct method preference question, and any method that was mentioned as a response to any of the method preference prompts, terming the latter a “latent preference”. We then classified the unprompted preference and the latent preference into a tiered hierarchy constructed according to method efficacy, based upon that detailed in Contraceptive Technology [19]. The lowest tier, which we term “less effective methods” (LEM), includes condoms, withdrawal, spermicides, sponges, fertility-based awareness methods (including the rhythm method), and abstinence. The second tier, which we term “hormonal methods” includes combined and progestin-only contraceptive pills, injectables, the vaginal ring, and the patch. The third tier, LARC, includes the implant, Copper-T IUD, and the levenorgestrel releasing intrauterine system. We also distinguished a fourth tier for permanent methods: female sterilization and vasectomy. If a participant expressed a latent preference for more than one method, her preference was categorized based on the most effective method mentioned. Women who had obtained a tubal ligation, or whose partners or spouses had obtained a vasectomy were classified as having a preference for a permanent method.
Using the same four-tier categorization used for method preferences, we examine actual use of contraception by method at three-month intervals up to nine months postpartum. Then, at six months postpartum, we compare the proportions of respondents using each category of method with (1) the proportions stating an unprompted preference for each category of method, and (2) the proportions stating a latent preference for each category of method, based on the applicable method preference prompts.
The remainder of the analysis is focused on exploring what factors were associated with an expressed preference for highly effective methods, as well as the factors associated with actually obtaining and using such methods among women who expressed a preference for them. First, we examined the how the latent preference for a highly effective method at six months postpartum varied according to the following sociodemographic characteristics: city, age group, parity, educational attainment, insurance status, relationship status, Hispanic ethnicity, annual family income, and childbearing intentions. We then examined the proportion of women who preferred a highly effective method who were actually using one at six months postpartum. We use Chi-squared tests of the homogeneity of proportions to test for the significance of differences in each instance.
The final step was to conduct multivariable regression analyses of these outcomes. Since women who want to have another child at some point in the future (spacers) would not be expected to want a permanent method of contraception, and might be less interested in a using highly effective method in the postpartum period than women who do not plan to have another child (limiters), we conducted separate analyses for each of these two groups. For spacers, the dependent variable in the first model was a preference for LARC, while for limiters it was a preference for either a long-acting or a permanent method (LAPM). In each case, we counted either an unprompted or a prompted preference as a preference, and included the same covariates considered in the bivariate analyses. The models of actual use at six months postpartum included the same covariates and were restricted to only those participants who had expressed a preference for LARC in the model for spacers, or LAPM in the model for limiters.
All analyses were performed using Stata version 13.0. Human subjects approval for this study was obtained from the appropriate university and hospital Institutional Review Boards.
3. Results
In total, we recruited 803 participants who completed baseline interviews, 403 in Austin and 400 in El Paso. Overall, 672 (84%) participants completed all four interviews, and 709 (89%) completed the six-month interview on which the present analysis is focused. Of the women interviewed at six months postpartum, 12 had become pregnant and were thus excluded. The distribution of the sample by sociodemographic characteristics, insurance status, and desire for additional children are shown in the first column of Table 1.
Table 1.
Preference for and use of long-acting or permanent methods (LAPM) at 6 months postpartum, by socio-demographic characteristics
| Characteristic | n | Proportion with preference for LAPM | χ 2 | Proportion using LAPM among women with preference for LAPM | χ 2 |
|---|---|---|---|---|---|
| City | |||||
| Austin | 377 | 0.77 | 0.41 | ||
| El Paso | 318 | 0.75 | 0.368 | 0.35 | 0.153 |
| Age | |||||
| 18 - 24 | 224 | 0.75 | 0.32 | ||
| 25 - 29 | 197 | 0.75 | 0.29 | ||
| 30+ | 274 | 0.78 | 0.606 | 0.50 | 0.000 |
| Parity | |||||
| 1 | 212 | 0.59 | 0.28 | ||
| 2 | 212 | 0.75 | 0.30 | ||
| 3+ | 271 | 0.91 | 0.000 | 0.49 | 0.000 |
| Education | |||||
| <High School | 224 | 0.84 | 0.36 | ||
| High School | 184 | 0.78 | 0.36 | ||
| >High School | 287 | 0.69 | 0.000 | 0.43 | 0.298 |
| Insurance status at 6 months | |||||
| Retained insurance | 326 | 0.74 | 0.47 | ||
| Lost insurance | 369 | 0.78 | 0.147 | 0.31 | 0.000 |
| Relationship status | |||||
| Married | 350 | 0.74 | 0.41 | ||
| Cohabiting | 208 | 0.78 | 0.36 | ||
| Single | 137 | 0.79 | 0.412 | 0.34 | 0.371 |
| Ethnicity | |||||
| Non-Hispanic | 168 | 0.63 | 0.39 | ||
| Hispanic | 527 | 0.80 | 0.000 | 0.38 | 0.942 |
| Annual household income† | |||||
| < $10,000 | 217 | 0.78 | 0.29 | ||
| $10,000 - 19,999 | 169 | 0.82 | 0.38 | ||
| $20,000 - 34,999 | 110 | 0.82 | 0.49 | ||
| $35,000 - 74,999 | 102 | 0.70 | 0.41 | ||
| $75,000 or more | 85 | 0.64 | 0.005 | 0.46 | 0.016 |
| Childbearing intentions at 6 months* | |||||
| Want more children | 324 | 0.61 | 0.25 | ||
| Want no more children | 205 | 0.89 | 0.23 | ||
| Don't know | 66 | 0.74 | 0.000 | 0.24 | 0.905 |
| Total | 695 | 0.76 | 0.38 |
(n = 683) Does not include 12 women who had missing data on income.
(n = 595) Does not include 100 women who were using sterilization at 6 months.
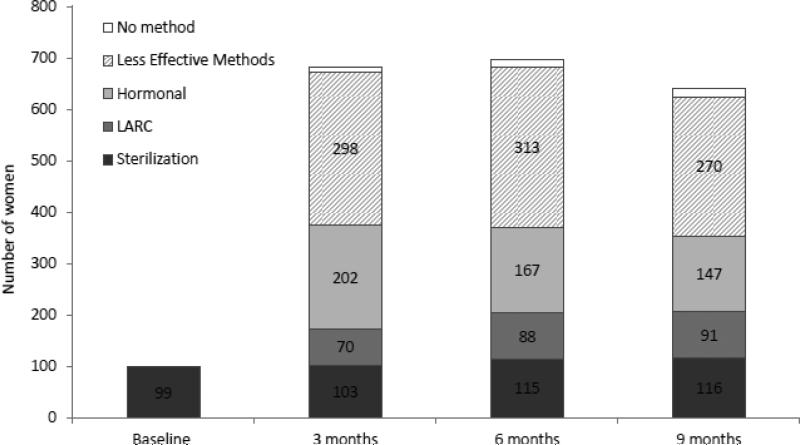
The use of contraception by method category is shown in Figure 2 at each of the four interview time-points. Postpartum female sterilization accounts for all of the contraceptive use in the baseline interview. By three months, almost all participants were using some form of contraception. There was substantial use of LEM and hormonal methods, some uptake of LARC, and only a slightly greater proportion relying on sterilization than at baseline. This pattern changed little over the next six months.
Figure 2.
Contraceptive method use at various durations postpartum
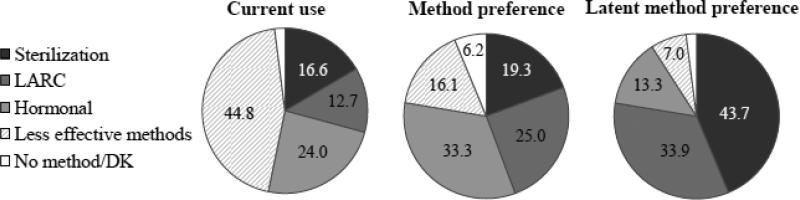
Figure 3 shows both contraceptive method use and method preference at 6 months postpartum. There was a substantial difference between actual method use and the methods participants said they would like to be using by six months when asked at the three month interview. The preference for use of both LARC and sterilization far exceeded its actual use. Using the broader specification of preference incorporating the prompts for interest in LARC and permanent methods (latent preference), the difference between preference and actual use widens considerably (rightmost chart).
Figure 3.
Contraceptive use and method preferences at six months postpartum
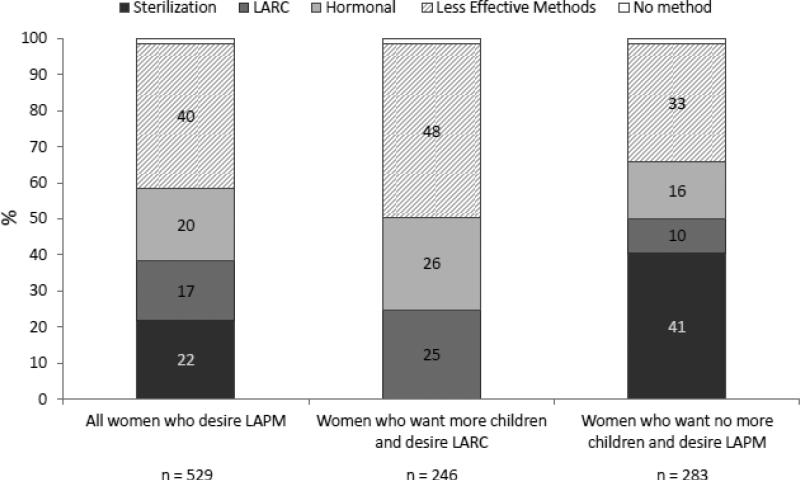
Figure 4 shows the actual method use at six months postpartum for all of the women with a preference for LAPM (first column). Only 39% were using a long-acting or permanent method, and nearly two-thirds of the remainder were using a less effective method. The figure also shows the actual method use among women who both wanted more children and expressed a preference for LARC, and that among women who wanted no more children and expressed a preference for LAPM. Remarkably, nearly half of the spacers with a preference for LARC were using LEM, as were a third of the limiters with a preference for LAPM.
Figure 4.
Methods being used at 6 months postpartum among women desiring long-acting or permanent methods (LAPM)
Women with higher parity, Hispanics, and women who did not want additional children were more likely to have a latent preference for LAPM, while women with higher educational attainment and women with a higher annual household income were less likely to have a latent preference for one of these methods (Table 1). On the other hand, age, parity, having insurance, and higher annual household income were all positively associated the likelihood of using LAPM among women with a latent preference for such a method.
Among women who wanted more children or were not sure about it, logistic multivariable regression analysis revealed that only two variables had a significant association with a latent preference for LARC: Women over 30 were less likely to prefer LARC and Hispanic women were more likely to prefer LARC. The second model in Table 2 addressed the factors associated with actual use of LARC among women in this group who had expressed a preference for or interest in LARC. Having more than a High School education, having retained insurance coverage, and Hispanic ethnicity were positively associated with actual use of LARC, while women age 30 or more had lower odds of using LARC. However, the most striking predictor in this model was annual family income: the estimated odds of a woman in this group with an annual household income exceeding $75,000 using LARC were nearly eleven times those of a woman an annual income of less than $10,000.
Table 2.
Logistic regression models predicting preference for, and use of LARC, among women who want more children or who don't know if they want more children
| Preference (n= 382) | Use given preference (n=220) | |||
|---|---|---|---|---|
| Odds ratio | 95% C.I. | Odds ratio | 95% C.I. | |
| City | ||||
| Austin | ref | ref | ref | ref |
| El Paso | 0.70 | 0.42-1.16 | 1.12 | 0.52-2.43 |
| Age | ||||
| 18 - 24 | ref | ref | ref | ref |
| 25 - 29 | 0.77 | 0.44-1.33 | 0.45† | 0.20-1.02 |
| 30+ | 0.34** | 0.18-0.64 | 0.28* | 0.09-0.87 |
| Parity | ||||
| 1 | ref | ref | ref | ref |
| 2 | 1.03 | 0.63-1.70 | 0.80 | 0.37-1.70 |
| 3+ | 1.33 | 0.71-2.53 | 1.94 | 0.77-4.88 |
| Education | ||||
| <High school | ref | ref | ref | ref |
| High school | 0.91 | 0.48-1.73 | 1.68 | 0.63-4.45 |
| >High school | 0.78 | 0.40-1.57 | 2.94† | 1.00-8.66 |
| Insurance status at 6 months | ||||
| Retained insurance | ref | ref | ref | ref |
| Lost insurance | 0.77 | 0.46-1.29 | 0.35** | 0.17-0.75 |
| Relationship Status | ||||
| Married | ref | ref | ref | ref |
| Cohabiting | 1.37 | 0.79-2.36 | 1.43 | 0.64-3.21 |
| Single | 1.26 | 0.65-2.44 | 1.66 | 0.61-4.52 |
| Ethnicity | ||||
| Non-Hispanic | ref | ref | ref | ref |
| Hispanic | 1.91* | 1.04-3.50 | 3.07* | 1.06-8.88 |
| Annual Family Income | ||||
| <$10,000 | ref | ref | ref | ref |
| $10,000-19,999 | 1.62 | 0.87-3.02 | 1.38 | 0.56-3.40 |
| $20,000-34,999 | 1.01 | 0.46-2.18 | 3.09† | 0.96-9.97 |
| $35,000-74,999 | 1.32 | 0.60-2.93 | 1.61 | 0.49-5.30 |
| $75,000 or more | 1.37 | 0.51-3.67 | 8.23** | 1.69-40.02 |
p < 0.01
p < 0.05
p < 0.10
Similar models for the participants who wanted no more children are shown in Table 3 for having a latent preference for, and then actually using either a long-acting or a permanent method. In this group, having three or more children was positively associated with a latent preference for LAPM, while having an annual family income exceeding $35,000 was negatively associated with a latent preference for LAPM. In the model for actual use of LAPM among women with a latent interest in LAPM and no desire for further childbearing, higher parity and having insurance were both significant covariates.
Table 3.
Logistic regression models predicting preference for, and use of long-acting or permanent methods (LAPM), among women who want no more children or are sterilized
| Preference (n= 301) | Use given preference (n=280) | |||
|---|---|---|---|---|
| Odds Ratio | 95% C.I. | Odds ratio | 95% C.I. | |
| City | ||||
| Austin | ref | ref | ref | ref |
| El Paso | 0.46 | 0.16-1.35 | 0.60† | 0.34-1.05 |
| Age | ||||
| 18 - 24 | ref | ref | ref | ref |
| 25 - 29 | 1.71 | 0.45-6.50 | 0.67 | 0.27-1.63 |
| 30+ | 2.87 | 0.75-10.94 | 1.39 | 0.61-3.20 |
| Parity | ||||
| 1 | ref | ref | ref | ref |
| 2 | 2.87 | 0.66-12.47 | 1.65 | 0.42-6.42 |
| 3+ | 3.96† | 0.90-17.43 | 4.49* | 1.17-17.28 |
| Education | ||||
| <High School | ref | ref | ref | ref |
| High School | 1.60 | 0.38-6.71 | 0.98 | 0.50-1.93 |
| >High School | 2.05 | 0.45-9.30 | 1.63 | 0.74-3.59 |
| Insurance Status | ||||
| Retained Insurance | ref | ref | ref | ref |
| Lost Insurance | 1.07 | 0.33-3.44 | 0.35** | 0.19-0.66 |
| Relationship Status | ||||
| Married | ref | ref | ref | ref |
| Cohabiting | 1.07 | 0.29-3.88 | 1.09 | 0.57-2.10 |
| Single | 0.77 | 0.16-3.80 | 1.02 | 0.46-2.28 |
| Ethnicity | ||||
| Non-Hispanic | ref | ref | ref | ref |
| Hispanic | 2.05 | 0.60-6.97 | 0.66 | 0.30-1.50 |
| Annual Family Income | ||||
| <$10,000 | ref | ref | ref | ref |
| $10,000-19,999 | 0.39 | 0.08-2.85 | 1.64 | 0.78-3.48 |
| $20,000-34,999 | 0.43 | 0.07-2.67 | 1.22 | 0.56-2.68 |
| $35,000-74,999 | 0.12* | 0.02-0.82 | 1.26 | 0.47-3.40 |
| $75,000 or more | 0.20 | 0.02-2.12 | 0.34 | 0.10-1.13 |
p < 0.01
p < 0.05
p < 0.10
4. Discussion
Our findings demonstrate substantial differences between the contraceptive methods being used and the methods women would prefer to be using in the postpartum period in two communities in Texas. Many more women had a preference for both LARC and permanent methods than were actually using these methods six months after delivery. The bivariate and multivariable analyses of differences in preferences for long-acting and permanent methods revealed that preference for these methods was not confined to particular segments of the population. The one exception is that Hispanics had a higher interest in, and use of LARC than other ethnic/racial groups among participants who wanted to or might have an additional child, which is consistent with nationally representative data [2].
In contrast, our analyses of the likelihood of actually using LARC or LAPM by women with a preference for a highly effective method indicated that advantaged groups were more likely than others to have realized their preference. The inability of low-income, uninsured women and couples to obtain or use LARC and permanent methods in this time frame is consistent with the reports we have collected from family planning clinic leaders in Texas regarding the impact of the 2011 funding cuts on their ability to provide these methods to this population [17]. However, the lack of access we observed is likely also related to other barriers limiting the provision of LARC and male and female sterilization including lack of provider training, misperceptions regarding eligibility, safety and effectiveness, insufficient counseling, and structural barriers related to the postpartum provision of both LARC and female sterilization [20-23]. Recent studies in California have shown that even in a state with a well-funded family planning program less than half of Medicaid recipients had a contraceptive claim within 90 days of delivery[24], and only 7% initiated use of LARC [25].
Immediate postpartum placement of IUDs and implants has been shown to reduce rapid repeat pregnancy, and yield high contraceptive use rates in the postpartum period [26-29]. Implementing postpartum LARC provision could do much to alleviate the large differences between preferences and use that we observed in these two Texas communities. Certainly one of the most promising policy improvements is to facilitate the provision of postpartum LARC through a specific funding mechanism for women with public insurance that would enable separate reimbursement such as now exists in several states [30]. In Texas, the Department of State Health Services and the Health and Human Services Commission (which manages the state's Medicaid program) are now considering a set of reimbursement mechanisms that would pay for postpartum LARC by drawing on the different possible funding streams for contraceptives for low-income women. Additionally, there is a need to reduce funding constraints, simplify consent forms, and alleviate logistical issues so as to increase access to postpartum tubal ligation, which varies widely across hospitals in Texas[31].
For women who have not decided on a contraceptive method at the time of delivery, access to LARC in the months following delivery needs to be assured by way of the various public and private insurances and primary health care programs now operating in the state. In 2013, the legislature took a critical step forward, restoring much of the public funding for family planning that was cut so deeply in the 2011. However, much of this funding is only now beginning to replenish or start programs, and it remains to be seen whether these efforts will substantially increase access to long-acting and permanent methods. Some of the funded organizations lack experience providing LARC and sterilization, and it will be important to ensure that they have the training as well as the timely supply of methods to meet the demand identified here. Interval sterilization procedures, both male and female, are rare among public patients in this study, likely due to women losing insurance coverage, their male partners not having insurance, and providers’ reluctance to accept state funding due to low reimbursement levels.
Our analysis is subject to a number of limitations. The findings may not be widely generalizable to the entire state since they come from a sample of women delivering in only 3 hospitals in 2 cities. It is also possible that the sequence of prompts used in our six-month interview to ascertain latent preference may have led to response bias by suggesting that we were not satisfied with the answer already given to the direct question. However, previous experience in El Paso with the question about whether the respondent would have liked to have been sterilized at the time of her last delivery, and found that responses had a very high correspondence with answers given in a more detailed interview conducted a year or two later [10]. Finally, the results reported here only refer to the time period after the cuts in family planning funding enacted in 2011, and do not demonstrate any change in the availability of long-acting and permanent methods that they may have precipitated.
While this study was conducted in the particular context of two Texas cities, the question it addresses is a general one: Are women obtaining the contraceptive method they would like to be using in a timely manner in the postpartum period? We are not able to discern the answer through the current set of questions in national (NSFG) or state (PRAMS/BRFSS) surveys, but this information is vital to determining where the system fails and how to improve it. Perhaps the most important lesson of this study is how much can be learned by asking women about their method preference directly and repeatedly as they pass through the postpartum period.
Implications.
In two Texas cities, many more women preferred long-acting and permanent contraceptive methods (LAPM) than were able to access these methods at six months postpartum. Women's contraceptive needs could be better met by counseling about all methods, reducing cost barriers and by making LAPM available at more sites.
Acknowledgements
We thank Chloe Dillaway, Natasha Mevs-Korff, Jon Amastae, PhD, and Ted Held, MD for their contributions to this research. Earlier versions of this paper were presented at the North American Forum on Family Planning, October 7, 2014, Seattle WA, and at the Annual Meeting of the Population Association of America, May 2, 2014, Boston MA.
Funding acknowledgement: This project was supported by a grant from an Anonymous Foundation, and an NICHD center grant (5 R24 HD042849) awarded to the Population Research Center at the University of Texas at Austin. ARAA is supported by an NICHD Individual Predoctoral Fellowship (F31 HD079182-01).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosure: The authors have no conflicts of interest or competing financial interests to declare.
References
- 1.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the U.S., 2007-2009. Fertil Steril. 2012;98:893–97. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kavanaugh ML, Jerman J, Hubacher D, et al. Characteristics of women in the united states who use long-acting reversible contraceptive methods. Obstet Gynecol. 2011;117:1349–57. doi: 10.1097/AOG.0b013e31821c47c9. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal PD, Voedisch A, Gemzell-Danielsson K. Strategies to prevent unintended pregnancy: Increasing use of long-acting reversible contraception. Human Reprod Update. 2011;17:121–37. doi: 10.1093/humupd/dmq026. [DOI] [PubMed] [Google Scholar]
- 4.Trussell J, Wynn LL. Reducing unintended pregnancy in the united states. Contraception. 2008;77:1–5. doi: 10.1016/j.contraception.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 5.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120:1291–97. doi: 10.1097/aog.0b013e318273eb56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366:1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 7.Gilliam M, Davis SD, Berlin A, Zite NB. A qualitative study of barriers to postpartum sterilization and women's attitudes toward unfulfilled sterilization requests. Contraception. 2008;77:44–9. doi: 10.1016/j.contraception.2007.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Zite N, Wuellner S, Gilliam M. Failure to obtain desired postpartum sterilization: Risk and predictors. Obstet Gynecol. 2005;105:794–99. doi: 10.1097/01.AOG.0000157208.37923.17. [DOI] [PubMed] [Google Scholar]
- 9.Zite N, Wuellner S, Gilliam M. Barriers to obtaining a desired postpartum tubal sterilization. Contraception. 2006;73:404–07. doi: 10.1016/j.contraception.2005.10.014. [DOI] [PubMed] [Google Scholar]
- 10.Potter JE, White K, Hopkins K, et al. Frustrated demand for sterilization among low-income latinas in el paso, texas. Perspect Sexual Reprod Health. 2012;44:228–35. doi: 10.1363/4422812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thurman AR, Harvey D, Shain RN. Unfulfilled postpartum sterilization requests. J Reprod Med. 2009;54:467–72. [PubMed] [Google Scholar]
- 12.Borrero S, Zite N, Potter JE, Trussell J. Medicaid policy on sterilization--anachronistic or still relevant? N Engl J Med. 2014;370:102–4. doi: 10.1056/NEJMp1313325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thurman AR, Janecek T. One-year follow-up of women with unfulfilled postpartum sterlization requests. Obstet Gynecol. 2010;116:1071–77. doi: 10.1097/AOG.0b013e3181f73eaa. [DOI] [PubMed] [Google Scholar]
- 14.Finer LB, Zolna MR. Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception. 2011;84:478–85. [Google Scholar]
- 15.Finer LB, Zolna MR. Am J Public Health. Suppl 1. Vol. 104. S43-8: 2014. Shifts in intended and unintended pregnancies in the united states, 2001-2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Finer LB. 2011. Personal communication. In.
- 17.White K, Grossman D, Hopkins K, Potter J. Cutting family planning in texas. N Engl J Med. 2012;367:1179–81. doi: 10.1056/NEJMp1207920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trussell J. Contraceptive failure in the United States. Contraception. 2011;83:397–404. doi: 10.1016/j.contraception.2011.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trussell J, Guthrie KA. Choosing a contraceptive: Efficacy, safety, and personal considerations. In: Hatcher RA, Trussell J, Nelson AL, Cates W, Kowal D, Policar M, editors. Contraceptive technology: Twentieth revised edition. Ardent Media; New York, NY: 2011. [Google Scholar]
- 20.Biggs MA, Harper CC, Malvin J, Brindis CD. Factors influencing the provision of long-acting reversible contraception in California. Obstet Gynecol. 2014;123:593–602. doi: 10.1097/AOG.0000000000000137. [DOI] [PubMed] [Google Scholar]
- 21.Harper C, Blum M, Thiel de Bocanegra H, et al. Challenges in translating evidence to practice: The provision of intrauterine contraception. Obstet Gynecol. 2008;111:1359–69. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 22.Aiken AR, Hopkins K, Grossman D, et al. Contraceptive counseling during prenatal and postpartum care in two cities in Texas. Contraception. 2013;88:465. [Google Scholar]
- 23.Dehlendorf C, Levy K, Ruskin R, Steinauer J. Health care providers' knowledge about contraceptive evidence: A barrier to quality family planning care? Contraception. 2010;81:292–8. doi: 10.1016/j.contraception.2009.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thiel de Bocanegra H, Chang R, Menz M, et al. Postpartum contraception in publicly-funded programs and interpregnancy intervals. Obstet Gynecol. 2013;122:296–303. doi: 10.1097/AOG.0b013e3182991db6. [DOI] [PubMed] [Google Scholar]
- 25.Thiel de Bocanegra H, Chang R, Howell M, Darney P. Interpregnancy intervals: Impact of postpartum contraceptive effectiveness and coverage. Am J Obstet Gynecol. 2014;210:311, e1–8. doi: 10.1016/j.ajog.2013.12.020. [DOI] [PubMed] [Google Scholar]
- 26.Celen S, Moroy P, Sucak A, et al. Clinical outcomes of early postplacental insertion of intrauterine contraceptive devices. Contraception. 2004;69:279–82. doi: 10.1016/j.contraception.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 27.Chen BA, Reeves MF, Creinin MD, Schwarz EB. Postplacental or delayed levonorgestrel intrauterine device insertion and breast-feeding duration. Contraception. 2011;84:499–504. [Google Scholar]
- 28.Chen BA, Reeves MF, Hayes JL, et al. Postplacental or delayed insertion of the levonorgestrel intrauterine device after vaginal delivery: A randomized controlled trial. Obstet Gynecol. 2010;116:1079–87. doi: 10.1097/AOG.0b013e3181f73fac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tocce KM, Sheeder JL, Teal SB. Rapid repeat pregnancy in adolescents: Do immediate postpartum contraceptive implants make a difference? Am J Obstet Gynecol. 2012;206:481, e1–7. doi: 10.1016/j.ajog.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 30.Teal SB. Postpartum contraception: Optimizing interpregnancy intervals. Contraception. 2014;89:487–88. doi: 10.1016/j.contraception.2014.04.013. [DOI] [PubMed] [Google Scholar]
- 31.Potter JE, Stevenson AJ, White K, et al. Hospital variation in postpartum tubal sterilization rates in California and Texas. Obstet Gynecol. 2013;121:152–58. doi: 10.1097/aog.0b013e318278f241. [DOI] [PMC free article] [PubMed] [Google Scholar]