Abstract
Objective:
To examine the associations between eating behavior traits and weight loss according to sleep quality and duration in adults enrolled in common weight-loss interventions.
Methods:
Participants included overweight and obese men and women (n=150) (mean±s.d. age, 38.8±8.6 years; mean±s.d. body mass index (BMI), 33.3±3.5 kg m−2) who were subjected to a dietary intervention over a period of 12–16 weeks. Anthropometric measurements, eating behavior traits (Three-Factor Eating Questionnaire), sleep quality (total Pittsburgh Sleep Quality Index (PSQI) score) and sleep duration (hours per night, self-reported from the PSQI) were assessed at both baseline and post intervention. Linear regression analysis was used to quantify the relationships between eating behavior traits and changes in anthropometric markers for all subjects and by sleep categories (short sleep: <7 h per night vs recommended sleep: ⩾7 h per night; poor sleep quality: ⩾5 PSQI score vs good sleep quality: <5 PSQI score). We adjusted for age, sex and baseline BMI in analyses.
Results:
Baseline eating behavior traits were modest predictors of weight-loss success, but they were all significantly associated with their changes over the weight-loss intervention (P<0.01). The diet intervention induced significant changes in eating behavior traits and even more for those having a non-favorable eating behavior profile at baseline. We observed that changes in flexible control and strategic dieting behavior were constantly negatively associated with changes in body weight and fat mass (P<0.05) for recommended duration sleepers. The change in situational susceptibility to disinhibition was positively associated with the change in fat mass and body weight for those having healthy sleeping habits (P<0.05). For poor quality sleepers, the change in avoidance of fattening foods was negatively associated with changes in adiposity (P<0.05).
Conclusion:
Eating behavior traits and sleep may act together to influence the outcome of weight-loss programs.
Introduction
A large body of evidence shows that sleeping habits have an influence on body weight regulation.1 More specifically, studies report that short sleep duration and poor sleep quality are both associated with weight gain and obesity.2 Results of recent studies also suggest that lack of sufficient sleep can impact the success of weight-loss interventions. For example, Nedeltcheva et al.3 conducted a crossover study in overweight adults randomly assigned to either 5.5 or 8.5 h per night for 2 weeks in addition to moderate caloric restriction in a laboratory setting. They observed that sleep restriction led to less body fat loss and greater hunger compared with the experimental condition with adequate sleep.
We recently replicated these findings in a real-life setting and showed that both sleep duration (hours per night) and sleep quality (total Pittsburgh Sleep Quality Index (PSQI) score) predicted fat mass loss during common dietary interventions in overweight and obese adults.4 In particular, we observed that a 1-h change in sleep duration was associated with a 0.7 kg change in fat mass after adjustment for covariates. Although the latter study also suggests that poor sleeping habits can undermine dietary efforts to reduce adiposity, the interaction between sleep and eating behaviors with regard to the magnitude of body weight, fat mass and waist circumference (WC) loss is unknown. A better understanding of the connections between sleep and eating behaviors is needed if we want to better tailor weight-loss programs, avoid patients' disappointment and maximize success.
The objective of the present study was therefore to examine the relationship between eating behaviors, sleep quality/quantity and loss of body weight, fat mass and WC in adults involved in diet-based weight-reducing programs. We hypothesized that having good sleeping habits together with adequate eating behavior traits would promote greater weight and fat loss in adults undergoing dietary interventions.
Subjects and methods
Subjects
Four weight-reducing interventions performed at Laval University (Quebec City, Canada) were pooled together to maximize power. Details about these studies have been previously published.5, 6, 7, 8 Briefly, all the studies included in the present article had included a standardized diet aimed at promoting a negative energy balance while subjects were either taking a placebo or a supplement of an active agent. In the present study, only data from participants enrolled in the control (placebo) group of these studies were considered for statistical analyses to avoid the influence of the active supplements on the primary outcome measures (i.e., weight, fat mass and WC losses). Overall, 150 healthy overweight and obese men and women aged between 20 and 55 years were subjected to a diet intervention supervised by a dietician. In most of these interventions,5, 6, 7 each individual received a personalized diet plan targeting 2085–2919 kJd−1 (500–700 kcald−1) decrease in energy intake. In the last study,8 participants were assigned a control diet based on the Canada's Food Guide to promote a negative energy balance.9 Depending on the study, the length of the intervention varied between 12 and 16 weeks. The following inclusion criteria were also considered: absence of pregnancy, breast-feeding or menopause (determined by the cessation of menstruation), stable body weight, body mass index (BMI) between 27 and 42 kg m−2, <3 periods of 20 min of physical activity per week, no use of medication and/or all kinds of supplements that could interfere with the study's objective, without comorbidities, consumption of ⩽10 alcoholic beverages per week or no more than 2 drinks per day depending on the study, and consumption of ⩽5 cups of coffee per day. Every 2 weeks (from the beginning until the completion of the study), participants met their assigned dietician. Compliance was verified by comparing the diet prescribed (total daily energy intake and macronutrient composition) to the actual diet composition of the participants which was checked at every visit using 24 h food recalls. Study protocols were approved by the Laval University Ethics Committee. Written informed consent was obtained from all participants.
Anthropometric and body composition measurements
Height was measured to the nearest 0.1 cm (without shoes and light clothes) using a standard stadiometer and body weight was measured to the nearest 0.1 kg using either a standard beam scale or a digital panel indicator scale. BMI was calculated as body weight divided by height squared (kgm−2). WC was measured with an anthropometric tape at midpoint between the lower border of the last rib and the upper border of the iliac crest. Body fat mass was either measured by dual-energy X-ray absorptiometry6, 7, 8 (GE Medical Systems Lunar, Diegem, Belgium) or by the underwater weighing technique5 with the use of the Siri formula10 to estimate the percentage of body fat from body density. All measurements were performed in the same way and in accordance with standardized procedures at both baseline and at the end of the dietary interventions.
Sleep assessment
At both baseline and at the end of the intervention, each participant had to complete the PSQI, a self-rated questionnaire that assesses sleep quality and disturbances over the preceding 1-month time period.11 This questionnaire contains 19 individual items and generates seven component scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication and daytime dysfunction. The sum of the component scores yields one total score with a maximum of 21. A total PSQI score greater than 5 is highly sensitive and specific in distinguishing good from poor sleepers and has been validated in a number of populations.12 In the context of our study, both sleep quality (total PSQI score) and sleep duration (self-reported from the PSQI) were used for statistical analyses. Short sleep duration was defined as <7 h per night and recommended sleep duration as ⩾7 h per night according to the median value in this sample and in agreement with the literature on the topic.1,2 Furthermore, poor sleepers were those having a PSQI score ⩾5 and good sleepers those having a PSQI score <5.
Eating behavior traits assessment
Participants had to complete a French version of the 51-item Three-Factor Eating Questionnaire at baseline and at the end of the intervention.13 This questionnaire measures three dimensions of human eating behavior, that is, cognitive dietary restraint (intent to control food intake), disinhibition (overconsumption of food in response to cognitive or emotional cues) and susceptibility to hunger (food intake in response to feelings and perceptions of hunger). It is also possible to distinguish two types of cognitive dietary restraint behaviors: flexible control and rigid control of eating.14 Other more specific eating behaviors have been identified as subscores in each of the three main dimensions, which offers a more complex picture of eating behavior in humans.15 The Three-Factor Eating Questionnaire is a reproducible and valid tool13,16,17 and the French version has been previously validated.18 We examined each trait (baseline and change), including their respective subscores, as it has been proposed that measuring domain-specific factors are more likely to help in clarifying the complexity of eating behaviors.15
Diet assessment
At both baseline and at the end of the intervention, participants had to fill out a 3-day food record for 2 weekdays and 1 weekend day. A dietician explained to each participant how to accurately complete the dietary record including how to quantify the foods consumed. This method of dietary assessment has been shown to provide a relatively reliable measure of diet in this population.19 Mean daily energy intake was estimated by a dietician using a computerized version of the Canadian Nutrient File.20
Statistical analysis
Using regression analysis, we first quantified the relationships between baseline eating behavior traits and changes in body weight, fat mass and WC. Secondly, we verified the previous relationships by sleep categories (short sleep: <7 h per night vs recommended sleep: ⩾7 h per night; poor sleep quality: ⩾5 PSQI score vs good sleep quality: <5 PSQI score). The same analyses were further examined by using the changes in eating behavior traits. Models were all adjusted for age, sex and baseline BMI. Multiple analysis of variance was used to monitor the effect of the dietary intervention on anthropometric markers, eating behavior traits and sleep. Linear regression analysis was used to quantify the relationships between baseline eating behavior traits and changes in eating behavior traits in response to the diet intervention. The same analysis was carried out for sleep quality and duration. Adiposity changes by tertiles of change in sleep (delta PSQI score (post-pré); Δ+: improvement, 0: no change, Δ−: deterioration) and anthropometric markers were performed using analysis of variance adjusting for age, sex and baseline BMI. A Tukey post hoc test was performed to determine which groups were significantly different. A two-tailed P value of less than 0.05 was considered to indicate statistical significance. Data are presented as means±s.d. All statistical analyses were performed using the JMP version 9 program (SAS Institute, Cary, NC, USA).
Results
Descriptive characteristics of participants are presented in Table 1. Participants lost on average 3.7±3.1 kg of body weight, 2.8±2.8 kg of fat mass and 5.0±3.5 cm of WC over the intervention period. Changes in energy intake were verified with the 3-day food records and were of −522±465 kcal per day on average. Participants complied at 78% with their energy-restricted diet, as assessed by the difference between total energy intake actually consumed and the prescription. The average length of the intervention was 14.0±1.7 weeks. Table 2 shows that body weight, fat mass and WC were all significantly reduced in response to the dietary intervention (P<0.01). Sleep quality was significantly improved in response to the weight-loss program, whereas post-intervention sleep duration was not significantly different from baseline. As shown in Table 2, the diet intervention had significant effects on eating behavior traits for all subjects and on sleep quality (P<0.01).
Table 1. Baseline characteristics of participants.
| Variables |
All subjects |
Poor sleep quality (PSQI score ⩾5) |
Good sleep quality (PSQI score <5) |
Short sleep (<7 h per night) |
Recommended sleep (⩾7 h per night) |
|---|---|---|---|---|---|
| Mean±s.d. | Mean±s.d. | Mean±s.d. | Mean±s.d. | Mean±s.d. | |
| Age (years) | 38.8±8.6 | 40.3±8.8 | 37.8±8.3 | 42.1±8.0 | 37.6±8.6** |
| Sex (n) | |||||
| Men | 83 | 38 | 45 | 34 | 49 |
| Women | 67 | 24 | 43 | 16 | 51 |
| Body weight (kg) | 94.4±15.4 | 94.2±13.0 | 94.9±16.8 | 94.6±11.1 | 94.2±16.5 |
| BMI (kg m−2) | 33.3±3.5 | 33.2±3.8 | 33.6±3.4 | 33.3±3.3 | 33.4±3.6 |
| Waist circumference (cm) | 106.0±11.1 | 106.3±10.2 | 106.2±11.8 | 106.4±8.8 | 105.8±11.8 |
| Fat mass (kg) | 36.6±8.8 | 36.34±9.5 | 37.3±8.6 | 35.9±8.8 | 37.0±8.8 |
| Delta weight (kg) | −3.7±3.14 | −4.5±2.8 | −3.2±3.3* | −4.0±2.3 | −3.6±3.4 |
| Delta fat mass (kg) | −2.8±2.8 | −3.6±2.2 | −2.4±3.0* | −3.1±2.3 | −2.7±2.9 |
| Delta waist circumference (cm) | −5.0±3.5 | −5.6±3.6 | −4.7±3.4 | −4.8±2.8 | −5.0±3.7 |
| Sleep duration (h) | 7.2±0.9 | 6.7±0.9 | 7.6±0.7** | 6.0±0.5 | 7.6±0.6** |
| PSQI (total score) | 4.6±2.6 | 7.1±2.2 | 2.9±1.0** | 6.8±2.9 | 3.9±2.1** |
| TFEQ | |||||
| Cognitive dietary restraint (0–21) | 7.4±3.8 | 7.0±3.8 | 7.5±3.8 | 6.9±3.7 | 7.5±3.9 |
| Flexible control (0–7) | 2.1±1.6 | 1.7±1.6 | 2.2±1.5 | 1.8±1.5 | 2.2±1.6 |
| Rigid control (0–7) | 2.4±1.7 | 2.6±1.5 | 2.3±1.7 | 2.6±1.7 | 2.4±1.7 |
| Strategic dieting behavior (0–4) | 0.6±1.0 | 0.4±0.9 | 0.7±1.0 | 0.4±0.8 | 0.7±1.0 |
| Attitude to self-regulation (0–5) | 2.5±1.3 | 2.7±1.3 | 2.5±1.3 | 2.6±1.2 | 2.6±1.3 |
| Avoidance of fattening foods (0–4) | 2.0±1.2 | 1.8±1.2 | 2.1±1.2 | 1.8±1.1 | 2.0±1.2 |
| Disinhibition (0–16) | 8.4±3.1 | 8.9±2.9 | 8.1±3.2 | 8.6±2.8 | 8.3±3.1 |
| Habitual susceptibility (0–5) | 1.6±1.4 | 1.6±1.3 | 1.6±1.5 | 1.4±1.2 | 1.6±1.5 |
| Emotional susceptibility (0–3) | 1.7±1.2 | 1.9±1.2 | 1.6±1.3 | 1.9±1.2 | 1.7±1.2 |
| Situational susceptibility (0–5) | 3.4±1.3 | 3.5±1.2 | 3.3±1.3 | 3.4±1.1 | 3.3±1.3 |
| Susceptibility to hunger (0–14) | 6.1±3.4 | 6.7±3.2 | 5.7±3.4 | 5.7±3.1 | 6.2±3.4 |
| Internal locus of hunger (0–6) | 2.2±1.7 | 2.4±1.6 | 2.1±1.8 | 1.9±1.6 | 2.3±1.7 |
| External locus of hunger (0–6) | 2.8±1.6 | 3.1±1.7 | 2.6±1.6 | 2.7±1.6 | 2.8±1.7 |
| Energy intake (kcal per day) | 2524±584 | 2535±536 | 2512±586 | 2631±587 | 2478±564 |
Abbreviations: BMI, body mass index; PSQI, Pittsburgh Sleep Quality Index; TFEQ, Three-Factor Eating Questionnaire.
Mean values were significantly different among sleep categories *P<0.05, **P<0.01.
Analysis of comparison among sleep categories were performed using analysis of variance.
Table 2. Treatment effects on anthropometric markers, eating behavior traits and sleeping habits.
| Variables | Before | After |
|---|---|---|
| Anthropometric markers | ||
| Body weight (kg) | 94.4±15.4 | 89.4±15.3** |
| Fat mass (kg) | 36.7±8.8 | 33.1±9.5** |
| Waist circumference (cm) | 106.0±11.1 | 99.89±11.5** |
| Eating behavior traits | ||
| Cognitive dietary restraint | 7.37±3.86 | 12.27±4.03** |
| Flexible control | 2.07±1.56 | 4.14±1.74** |
| Rigid control | 2.40±1.66 | 3.52±1.74** |
| Strategic dieting behavior | 0.62±0.97 | 1.83±1.34** |
| Attitude to self-regulation | 2.54±1.29 | 3.47±1.32** |
| Avoidance of fattening foods | 1.95±1.21 | 2.84±1.04** |
| Disinhibition | 8.38±3.06 | 6.41±2.79** |
| Habitual susceptibility | 1.57±1.41 | 0.97±1.00** |
| Emotional susceptibility | 1.70±1.23 | 1.19±1.24** |
| Situational susceptibility | 3.37±1.27 | 2.39±1.44** |
| Susceptibility to hunger | 6.13±3.39 | 3.43±2.84** |
| Internal locus of hunger | 2.19±1.73 | 1.03±1.38** |
| External locus of hunger | 2.84±1.64 | 1.45±1.40** |
| Sleeping habits | ||
| Sleep quality | 4.59±2.61 | 3.74±2.13** |
| Sleep duration | 7.23±0.90 | 7.22±1.36 |
Values are means±s.d.
Mean values were significantly different from before treatment *P<0.05, **P<0.01.
Treatment effects were analyzed using multiple analysis of variance.
Baseline eating behavior traits were all significantly associated with their changes over the intervention for all subjects (Table 3). However, as shown in Table 3, when performing the same analysis by sleep categories, no significant relationship was observed between both baseline disinhibition and emotional susceptibility to disinhibition with the changes in these behaviors for the poor sleep quality category. Likewise, no significant association was observed for baseline situational susceptibility to disinhibition with its change during weight loss for those having inadequate sleeping habits (Table 3).
Table 3. Associations between baseline eating behaviour traits and changes of these variables in response to the diet intervention in all subjects and subjects classified according to sleep quality or sleep duration.
| Variables | All subjects r | Poor sleep quality (PSQI score ⩾5) r | Good sleep quality (PSQI score <5) r | Short sleep (<7 h per night) r | Recommended sleep (⩾7 h per night) r |
|---|---|---|---|---|---|
| Cognitive dietary restraint | −0.47** | −0.57** | −0.40** | −0.50* | −0.46** |
| Flexible control | −0.48** | −0.58** | −0.34** | −0.48* | −0.48** |
| Rigid control | −0.47** | −0.49** | −0.46** | −0.24* | −0.47** |
| Strategic dieting behavior | −0.52** | −0.53** | −0.51** | −0.55** | −0.51** |
| Attitude to self-regulation | −0.51** | −0.65** | −0.45** | −0.68** | −0.46** |
| Avoidance of fattening foods | −0.63** | −0.71** | −0.58** | −0.63** | −0.61** |
| Disinhibition | −0.50** | −0.22 | −0.60** | −0.53** | −0.48** |
| Habitual susceptibility | −0.71** | −0.58** | −0.76** | −0.85** | −0.68** |
| Emotional susceptibility | −0.38** | −0.27 | −0.42** | −0.43* | −0.36** |
| Situational susceptibility | −0.34** | −0.06 | −0.52** | −0.35 | −0.35** |
| Susceptibility to hunger | −0.59** | −0.49** | −0.69** | −0.62** | −0.60** |
| Internal locus of hunger | −0.63** | −0.55** | −0.71** | −0.77** | −0.62** |
| External locus of hunger | −0.64** | −0.58** | −0.72** | −0.55** | −0.66** |
Abbreviation: PSQI, Pittsburgh Sleep Quality Index.
Relationship was statistically significant *P<0.05, **P<0.01.
r and P values are for the relationship between baseline eating behavior traits and changes of these in response to the diet intervention.
The associations between baseline eating behavior traits and changes of these in response to the diet intervention were tested using linear regression analysis.
After adjusting for covariates, baseline situational susceptibility to disinhibition was negatively associated with changes in body weight and WC for all subjects (r=−0.21; r=−0.18; P<0.05). For good and poor quality sleepers, baseline susceptibility to hunger was associated with fat and weight loss, respectively (r=0.33; r=−0.29; P<0.05) (Table 4a). For good quality sleepers, baseline flexible control and external locus of hunger were significantly associated with the change in fat mass (r=−0.06; r=0.27; P<0.05) (Table 4a). For those within the recommended sleep duration category, baseline situational susceptibility to disinhibition was negatively associated with changes in body weight and WC (P<0.05) (Table 4b).
Table 4. Associations between baseline eating behavior traits and changes in morphological variables in response to the diet intervention in subjects classified according to sleep quality (a) or sleep duration (b).
|
(a) | ||||||
|---|---|---|---|---|---|---|
| Baseline eating behavior traits |
Delta fat mass |
Delta body weight |
Delta WC |
|||
| PSQI⩾5 | PSQI<5 | PSQI⩾5 | PSQI<5 | PSQI⩾5 | PSQI<5 | |
| r | r | r | r | r | r | |
| Cognitive dietary restraint | 0.06 | −0.09 | 0.09 | −0.09 | −0.04 | −0.11 |
| Flexible control | 0.13 | −0.25* | 0.13 | −0.21 | 0.12 | −0.22 |
| Rigid control | −0.12 | 0.01 | 0.001 | 0.03 | −0.16 | 0.03 |
| Strategic dieting behavior | 0.16 | −0.02 | 0.12 | 0.04 | 0.10 | −0.14 |
| Attitude to self-regulation | 0.01 | −0.02 | 0.02 | −0.09 | −0.17 | −0.06 |
| Avoidance of fattening foods | 0.15 | 0.03 | 0.14 | 0.03 | 0.04 | 0.01 |
| Disinhibition | −0.19 | −0.01 | −0.20 | −0.06 | 0.01 | 0.07 |
| Habitual susceptibility | −0.11 | 0.03 | −0.15 | −0.02 | −0.03 | 0.14 |
| Emotional susceptibility | −0.04 | 0.004 | 0.002 | 0.09 | 0.12 | 0.16 |
| Situational susceptibility | −0.20 | −0.15 | −0.25 | −0.19 | −0.01 | −0.21 |
| Susceptibility to hunger | −0.20 | 0.33* | −0.29* | 0.14 | −0.20 | 0.16 |
| Internal locus of hunger | −0.19 | 0.24 | −0.27 | 0.004 | −0.02 | 0.09 |
| External locus of hunger | −0.15 | 0.27* | −0.21 | 0.11 | −0.14 | 0.05 |
|
(b) | ||||||
|---|---|---|---|---|---|---|
| Baseline eating behavior traits |
Delta fat mass |
Delta body weight |
Delta WC |
|||
| <7 h per night | ⩾7 h per night | <7 h per night | ⩾7 h per night | <7 h per night | ⩾7 h per night | |
| r | r | r | r | r | r | |
| Cognitive dietary restraint | 0.21 | −0.11 | 0.28 | −0.01 | 0.02 | −0.04 |
| Flexible control | 0.17 | −0.07 | 0.28 | −0.05 | 0.25 | −0.003 |
| Rigid control | 0.03 | 0.01 | 0.04 | 0.04 | −0.02 | −0.01 |
| Strategic dieting behavior | 0.17 | 0.05 | 0.15 | 0.09 | 0.13 | −0.07 |
| Attitude to self-regulation | 0.31 | −0.03 | 0.28 | −0.05 | −0.18 | −0.05 |
| Avoidance of fattening foods | 0.001 | 0.13 | 0.11 | 0.10 | 0.07 | 0.06 |
| Disinhibition | −0.14 | −0.04 | −0.25 | −0.08 | −0.08 | 0.04 |
| Habitual susceptibility | −0.14 | 0.05 | −0.23 | −0.02 | −0.22 | 0.12 |
| Emotional susceptibility | 0.01 | 0.04 | −0.18 | 0.07 | −0.11 | 0.15 |
| Situational susceptibility | −0.13 | −0.20 | −0.01 | −0.22* | 0.01 | −0.23* |
| Susceptibility to hunger | −0.05 | 0.13 | −0.14 | −0.002 | −0.13 | −0.01 |
| Internal locus of hunger | −0.12 | 0.07 | −0.24 | −0.06 | −0.10 | −0.06 |
| External locus of hunger | −0.02 | 0.13 | −0.21 | 0.01 | −0.18 | 0.07 |
Abbreviations: PSQI, Pittsburgh Sleep Quality Index; WC, waist circumference.
Relationship was statistically significant *P<0.05, **P<0.01.
r and P values are for the relationship between baseline eating behavior traits and anthropometry markers according to sleep quality or duration categories.
The associations between baseline eating behavior traits and anthropometric markers according to sleep categories were tested using linear regression analysis adjusting for age, sex and baseline body mass index. Bold indicates significant results.
For all subjects, we observed that the changes in cognitive dietary restraint, flexible control and strategic dieting behavior were constantly significantly negatively associated with changes in weight and fat mass for all subjects (P<0.05) (Table 5a). The change in situational susceptibility to disinhibition was positively associated with changes in weight and fat mass for all subjects (P<0.05) (Table 5a).
Table 5. Associations between changes in eating behavior traits and changes in morphological variables in response to the diet intervention for all participants (a) and in participants classified according to their sleep quality (b) or sleep duration (c).
|
(a) | |||
|---|---|---|---|
| Delta eating behavior traits | Delta fat mass | Delta body weight | Delta WC |
| r | r | r | |
| Cognitive dietary restraint | −0.24* | −0.23* | −0.18 |
| Flexible control | −0.25* | −0.32** | −0.30** |
| Rigid control | −0.06 | −0.03 | 0.01 |
| Strategic dieting behavior | −0.22* | −0.28** | −0.19* |
| Attitude to self-regulation | −0.06 | −0.02 | 0.02 |
| Avoidance of fattening foods | −0.20* | −0.18 | −0.03 |
| Disinhibition | 0.11 | 0.16 | 0.02 |
| Habitual susceptibility | 0.10 | 0.15 | 0.05 |
| Emotional susceptibility | −0.03 | 0.03 | 0.01 |
| Situational susceptibility | 0.24* | 0.22* | 0.09 |
| Susceptibility to hunger | 0.07 | 0.17 | 0.08 |
| Internal locus of hunger | 0.06 | 0.11 | 0.03 |
| External locus of hunger | 0.11 | 0.21* | 0.05 |
|
(b) | ||||||
|---|---|---|---|---|---|---|
| Delta eating behavior traits |
Delta fat mass |
Delta body weight |
Delta WC |
|||
| PSQI⩾5 | PSQI<5 | PSQI⩾5 | PSQI<5 | PSQI⩾5 | PSQI<5 | |
| r | r | r | r | r | r | |
| Cognitive dietary restraint | −0.21 | −0.18 | −0.21 | −0.15 | −0.13 | −0.11 |
| Flexible control | −0.29 | −0.12 | −0.30 | −0.19 | −0.32* | −0.12 |
| Rigid control | −0.05 | −0.09 | −0.10 | −0.04 | −0.01 | 0.02 |
| Strategic dieting behavior | −0.23 | −0.14 | −0.23 | −0.21 | −0.19 | −0.10 |
| Attitude to self-regulation | −0.09 | −0.07 | −0.07 | −0.01 | 0.15 | −0.04 |
| Avoidance of fattening foods | −0.32* | −0.14 | −0.24 | −0.09 | −0.30* | 0.05 |
| Disinhibition | 0.11 | 0.18 | 0.11 | 0.22 | −0.24 | 0.13 |
| Habitual susceptibility | 0.02 | 0.16 | 0.06 | 0.18 | −0.16 | 0.01 |
| Emotional susceptibility | −0.05 | 0.05 | 0.05 | 0.09 | −0.14 | 0.08 |
| Situational susceptibility | 0.18 | 0.34* | 0.16 | 0.31* | −0.09 | 0.21 |
| Susceptibility to hunger | 0.08 | 0.06 | 0.19 | 0.15 | 0.05 | 0.01 |
| Internal locus of hunger | 0.08 | 0.07 | 0.12 | 0.10 | −0.04 | 0.06 |
| External locus of hunger | 0.11 | 0.11 | 0.23 | 0.18 | 0.01 | −0.07 |
|
(c) | ||||||
|---|---|---|---|---|---|---|
| Delta eating behavior traits |
Delta fat mass |
Delta body weight |
Delta WC |
|||
| <7 h per night | ⩾7 h per night | <7 h per night | ⩾7 h per night | <7 h per night | ⩾7 h per night | |
| r | r | r | r | r | r | |
| Cognitive dietary restraint | −0.30 | −0.21 | −0.39 | −0.18 | −0.31 | −0.02 |
| Flexible control | −0.18 | −0.26* | −0.32 | −0.31* | −0.45* | −0.26* |
| Rigid control | −0.33 | −0.02 | −0.35 | 0.03 | −0.25 | 0.01 |
| Strategic dieting behavior | −0.02 | −0.23* | −0.20 | −0.28* | −0.32 | −0.16 |
| Attitude to self-regulation | −0.42* | −0.002 | −0.32 | 0.03 | 0.16 | 0.02 |
| Avoidance of fattening foods | −0.11 | −0.22* | −0.16 | −0.15 | −0.35 | −0.11 |
| Disinhibition | 0.05 | 0.09 | 0.33 | 0.11 | 0.05 | −0.004 |
| Habitual susceptibility | 0.19 | 0.07 | 0.34 | 0.09 | 0.25 | −0.01 |
| Emotional susceptibility | 0.13 | −0.03 | 0.26 | 0.003 | 0.13 | −0.05 |
| Situational susceptibility | 0.03 | 0.27* | 0.17 | 0.23* | −0.03 | 0.14 |
| Susceptibility to hunger | −0.04 | 0.09 | 0.02 | 0.17 | 0.09 | 0.06 |
| Internal locus of hunger | −0.02 | 0.08 | −0.04 | 0.11 | −0.02 | 0.04 |
| External locus of hunger | 0.14 | 0.12 | 0.20 | 0.19 | 0.07 | 0.02 |
Abbreviations: PSQI, Pittsburgh Sleep Quality Index; WC, waist circumference.
Relationship was statistically significant *P<0.05, **P<0.01.
r and P values are for the relationship between changes in eating behavior traits and anthropometry markers according to sleep quality or duration categories.
The associations between changes in eating behavior traits and anthropometric markers according to sleep categories were tested using linear regression analysis adjusting for age, sex and baseline body mass index. Bold indicates significant results.
By performing the analysis by sleep categories, we observed within the sleep quality category that the change in situational susceptibility to disinhibition was positively associated with changes in body weight and fat mass for good sleepers (P<0.05) (Table 5b). For poor sleepers, the change in avoidance of fattening foods was negatively associated with changes in fat mass and WC (P<0.05) (Table 5b).
Within the recommended sleep duration subcategory, we observed that changes in flexible control and strategic dieting behavior were constantly negatively associated with changes in body weight and fat mass (P<0.05) (Table 5c). Relationships between the change in flexible control with the change in WC was not influenced by sleep duration (P<0.05) (Table 5c). The change in situational susceptibility to disinhibition was positively associated with the change in fat mass and body weight within the recommended sleep duration subcategory (P<0.05) (Table 5c).
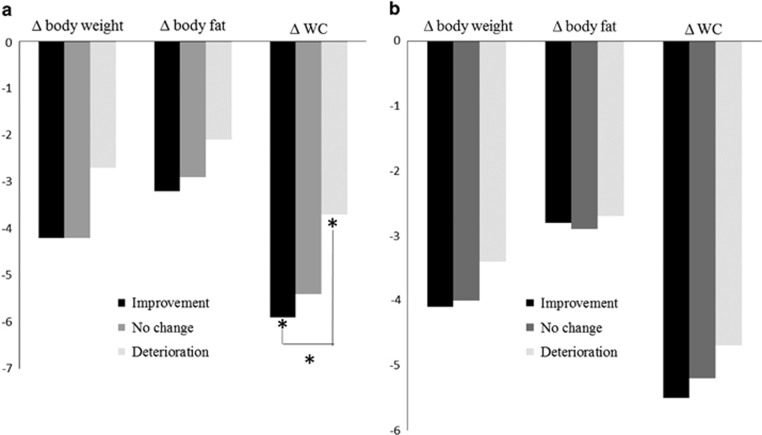
Finally, we compared the changes in anthropometric markers by tertiles of change in sleeping habits (three groups were formed; improvement, no change and deterioration). There was a significant relationship in those who improved and deteriorated their sleep quality (P<0.05) with the change in WC. Adjusted WC means were −5.9 cm versus −3.7 cm in those who improved and deteriorated their sleep quality, respectively (Figure 1a).
Figure 1.
Associations between changes in sleep quality (a) and sleep duration (b) with changes in morphological variables in response to the diet intervention. The relationship was statistically significant at *P<0.05 and **P<0.01. P values are for the relationship between tertiles of change in sleeping habits and anthropometric markers. Values are expressed as least squares means. The associations between tertiles of change in sleeping habits and anthropometric markers were performed using analysis of variance adjusting for age, sex and baseline body mass index. A Tukey post hoc test was performed to determine which groups were significantly different.
Discussion
Results from the present study show that eating behavior traits are related with weight-loss outcome and that sleep quality and duration seem to influence these relationships. Cognitive dietary restraint and its related subscores all increased in response to the diet intervention. Disinhibition and its related subscores all decreased in response to the weight-loss program. Those variations in eating behavior traits are associated with weight-loss success and maintenance.21 Susceptibility to hunger and its related subcores all diminished as a treatment effect. Those changes benefit weight losers because higher levels of susceptibility to hunger cause a problem for subsequent overconsumption of energy and are positively associated with the level of obesity.22,23
Our results are in agreement with those of Teixeira et al.24 because baseline eating behavior traits were modest predictors of weight-loss success. This emphasizes the need to consider the effect of the dietary intervention on eating behavior traits to develop strategies for long-term treatment of obesity. Indeed, baseline situational susceptibility to disinhibition was negatively associated with weight-loss outcomes and the change in the latter revealed an opposite trend. One possible explanation might be that individualized dietary advice proposed by the dietician to highly disinhibited individuals at baseline favored higher control over food intake resulting in better compliance to the diet plan. Indeed, the diet intervention induced significant changes in eating behavior traits in the expected direction with weight loss for all participants. There were significant improvements in disinhibition traits for all participants and even more for those having a non-favorable eating behavior profile at baseline. As for cognitive dietary restraint, even though this eating behavior trait increased in response to the intervention, only flexible control predicted adiposity changes.
By looking at changes in eating behavior traits by sleep categories, results of the present study show that improvement in flexible control of eating was associated with greater body weight, fat mass and WC losses in individuals having good sleep duration. In particular, we observed that a positive increment of one unit in the level of flexible control was associated with a reduction of 0.57 kg in body weight after adjustment for covariates. More flexible control was also associated with WC reduction for short duration and poor quality sleepers. Increased level of flexible control over eating is associated with lower body weight and is predictive of long-term weight-loss outcomes.22 Although speculative, one explanation could be that eating behavior trait dominated the influence of sleeping habits on their effect on visceral adiposity.
An increase in strategic dieting behavior (a subscore of cognitive dietary restraint) was associated with body weight and fat loss solely within the recommended sleep duration subcategory. In a longitudinal study quantifying the associations between the change in eating behaviors and body weight changes over 6 years, women relied more on strategic dieting behavior and avoided more fattening foods as a way to diminish food intake.25 Although the present study was not sufficiently powered to detect differences between men and women, future studies should investigate whether the associations between eating/sleeping behaviors and body weight, fat and WC loss are gender specific.
An increase in avoidance of fattening foods (a subscore of cognitive dietary restraint) was associated with more body fat mass and WC loss. The later relationship was only observed in the poor quality sleepers subcategory. Moreover, positive associations between the changes in situational susceptibility to disinhibition and body weight and fat loss were solely seen in those having healthy sleeping habits. Among eating behavior traits that were regularly significantly associated with body weight and adiposity loss, situational susceptibility to disinhibition seems to have the most pronounced impact on body weight in our cohort. Indeed, a positive increment of one unit in the level of this variable was associated with an increase of 0.67 kg of body weight after adjustment for covariates among the recommended sleep duration subcategory. On the other hand, a positive increment of one unit in the levels of strategic dieting behavior and flexible control was associated with a decrease of 0.63 kg and 0.57 kg of body weight, respectively, after adjustment for covariates also among the recommended sleep duration subcategory. This is in agreement with other research that has identified the disinhibition subscale to be the trait most persistently associated with obesity and higher energy consumption.26
The mechanisms that can explain why insufficient sleep may impede the success of dietary interventions are largely unknown. Proposed explanations are that higher ghrelin concentrations generally observed in short sleepers may facilitate the retention of fat.27,28 Additionally, the increased drive to eat that accompanies lack of sleep can certainly compromise adherence to caloric restriction because of the fact that dieting also increases hunger. Killgore et al.29 showed that short sleep duration might make people more vulnerable to hedonic food consumption. There was a significant positive relation between the change in situational susceptibility to disinhibition and the change in total energy intake within all sleep categories in the present study. Greater scores in situational susceptibility to disinhibition were related to more energy consumed. Interestingly, the change in this particular trait resulted in food intake modifications and thus weight and fat mass change uniquely among those having healthy sleeping habits.
A recent study by Dweck et al.30 examined the role of stress and emotional eating (as assessed by the Dutch Eating Behavior Questionnaire)31 in short and normal sleepers. They observed that poor sleep quality was associated with high scores of emotional and external eating but not of dietary restraint. Short sleep duration was also associated with higher food consumption among stressed emotional eaters versus normal sleepers. The authors proposed the same conclusion as Chaput et al.32 in that the effects of sleep deprivation on food consumption are dependent on individual characteristics. Another study indicated that poor sleep quality was associated with an increase in hunger, disinhibition, dietary restraint and emotional susceptibility to disinhibition whereas sleep duration was not.33 Thus, poor sleep quality could be an indicator or marker of problematic eating behaviors.
Our findings agree with results obtained in previous studies showing that poor sleeping habits could attenuate dietary efforts to reduce adiposity.3,4,34 Indeed, we observed that having healthy sleeping habits favored eating behavior traits that were significantly associated with body weight and adiposity loss. Additionally, we observed that improvement and deterioration in sleeping habits were constantly associated with more and less body weight and fat loss, respectively. Interestingly, there was a significant decrease in WC in those who improved their sleep quality. Poor sleep quality ends up in overall sleep loss and our finding is concordant with recent epidemiological and laboratory evidence that confirm the association between sleep loss and obesity.35 A longitudinal study by Chaput et al.36 demonstrated that switching from a short to a recommended sleep duration was associated with less visceral fat mass gain over time. Additionnally, Chaput et al.37 showed that short sleep duration favors abdominal obesity in children. More research is needed to verify the effects of sleeping habits improvement in the treatment of obesity.
This study is the first one to simultaneously examine the relationships between eating behaviors, sleep and adiposity loss. Although replication studies are clearly needed to confirm the observed findings, our results suggest that eating and sleeping may interact together to predict the outcome of weight-loss programs. One must nevertheless keep in mind that most significant associations reported in the present study had coefficients of correlation ranging between 0.2 and 0.3, suggesting that they explain a small part of the variability in the related variables. However, this is generally the case in the fields of obesity and nutrition because many factors are at play. Despite small effect sizes, we believe that more attention should be paid to eating behaviors and sleep hygiene during weight loss to maximize success.
Our results need to be interpreted in light of the following limitations. First, the small sample size and exploratory nature of this investigation preclude any definitive conclusion about the interconnections between eating behaviors, sleeping habits and fat loss. Second, the results come from a pool of four different weight-loss interventions with slightly different aims and interventions; the idea explored in the present study was thus a retrospective analysis. For example, the pre-post study design does not include a control group (i.e., individuals reviewed on a regular basis but with no instructions provided). Third, we have to keep in mind the limitations of self-reported measures as well as the possibility of residual confounding by unmeasured variables. Fourth, the present study only allows for the identification of associations and does not permit causal inferences. Fifth, other dimensions of sleep (e.g., timing, architecture, consistency and continuity) have not been assessed and could be related to eating behaviors and adiposity loss. Likewise, obstructive sleep apnea diagnosis or daytime sleepiness were not available and could have provided relevant information. Sixth, the PSQI covers sleep quality over the month prior to administration, suggesting that the PSQI performed at the end of the weight-loss program covers sleep during part of the intervention. Seventh, we did not control for stress, personality traits and depression, which might be pertinent targets for health-care professionals as they seem to be important determinants of weight-loss success.30,34,38,39 Finally, the external generalizability is limited to the sample studied.
In conclusion, sleep may modulate eating behavior in adults involved in different dietary interventions and may act together to influence the outcome of weight-loss programs. Although replication studies are needed to confirm our preliminary findings, one must remember that multiple factors can impact the success of weight-loss programs. In particular, dietary practitioners should explore sleep hygiene and eating behavior traits as part of their overall assessment before prescribing any dietary plan if they want to improve the effectiveness of their intervention.
Acknowledgments
We express our gratitude to the subjects for their participation and the staff of the Physical Activity Sciences Laboratory at Laval University for their contribution to this study. None of the authors had a personal interest or potential conflict of interest with the organizations sponsoring the projects. JPC holds a Junior Research Chair in Healthy Active Living and Obesity Research. AT is partly funded by the Canada Research Chair in Environment and Energy Balance.
The authors declare no conflict of interest.
References
- Chaput JP, Tremblay A. Insufficient sleep as a contributor to weight gain: an update. Curr Obes Rep. 2012;1:245–256. [Google Scholar]
- Chaput JP. Sleep patterns, diet quality and energy balance. Physiol Behav. 2014;134:86–91. doi: 10.1016/j.physbeh.2013.09.006. [DOI] [PubMed] [Google Scholar]
- Nedeltcheva AV, Kilkus JM, Imperial J, Schoeller DA, Penev PD. Insufficient sleep undermines dietary efforts to reduce adiposity. Ann Intern Med. 2010;153:435–441. doi: 10.1059/0003-4819-153-7-201010050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Tremblay A. Sleeping habits predict the magnitude of fat loss in adults exposed to moderate caloric restriction. Obesity Facts. 2012;5:561–566. doi: 10.1159/000342054. [DOI] [PubMed] [Google Scholar]
- Major GC, Doucet E, Jacqmain M, St-Onge M, Bouchard C, Tremblay A. Multivitamin and dietary supplements, body weight and appetite: results from a cross-sectional and a randomised double-blind placebo-controlled study. Br J Nutr. 2008;99:1157–1167. doi: 10.1017/S0007114507853335. [DOI] [PubMed] [Google Scholar]
- Major GC, Alarie F, Dore J, Phouttama S, Tremblay A. Supplementation with calcium+vitamin D enhances the beneficial effect of weight loss on plasma lipid and lipoprotein concentrations. Am J Clin Nutr. 2007;85:54–59. doi: 10.1093/ajcn/85.1.54. [DOI] [PubMed] [Google Scholar]
- Sanchez M, Darimont C, Drapeau V, Emady-Azar S, Lepage M, Rezzonico E, et al. Effect of Lactobacillus rhamnosus CGMCC1.3724 supplementation on weight loss and maintenance in obese men and women. Br J Nutr. 2013;3:1–13. doi: 10.1017/S0007114513003875. [DOI] [PubMed] [Google Scholar]
- Drapeau V, Arguin H, Tremblay A.Impact of satiating diet on satiety quotient and body weight in obese men Appl Physiol Nutr Metab 20103537320795291 [Google Scholar]
- Eating Well with Canada's Food Guide Ottawa, Canada, 2007. Available from http://www.hc-sc.gc.ca/fn-an/food-guide-aliment/index-eng.php (accessed 17 August 2014).
- Siri WE. The gross composition of the body. Adv Biol Med Phys. 1956;4:239–280. doi: 10.1016/b978-1-4832-3110-5.50011-x. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. J Psychosom Res. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- Stunkard A, Messick S. The three factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res. 1985;29:13. doi: 10.1016/0022-3999(85)90010-8. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J, Stunkard AJ, Pudel V. Validation of the flexible and rigid control dimensions of dietary restraint. Int J Eat Disord. 1999;26:53–64. doi: 10.1002/(sici)1098-108x(199907)26:1<53::aid-eat7>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Bond MJ, McDowell AJ, Wilkinson JY. The measurement of dietary restraint, disinhibition and hunger: an examination of the factor structure of the Three Factor Eating Questionnaire (TFEQ) Int J Obes Relat Metab Disord. 2001;256:900–906. doi: 10.1038/sj.ijo.0801611. [DOI] [PubMed] [Google Scholar]
- Laessle RG, Tuschl RJ, Kotthaus BC, Pirke KM. A comparison of the validity of three scales for the assessment of dietary restraint. J Abnorm Psychol. 1989;98:504–507. doi: 10.1037//0021-843x.98.4.504. [DOI] [PubMed] [Google Scholar]
- Allison DB, Kalinsky LB, Gorman BS. A comparison of the psychometric properties of three dimensions of dietary restrait. Psychol Assessment. 1992;4:8. [Google Scholar]
- Lluch A. University of Nancy: France; 1995. Identification des conduites alimentaires par approches nutritionnelles et psychométriques: implications thérapeutiques et préventives dans l'obésité humaine (Identification of food intake behaviours by nutritional and psychometrics means: implications for prevention and treatment of human obesity). PhD thesis. [Google Scholar]
- Yang YJ, Kim MK, Hwang SH, Ahn Y, Shim JE, Kim DH. Relative validities of 3-day food records and the food frequency questionnaire. Nutr Res Pract. 2010;42:142–148. doi: 10.4162/nrp.2010.4.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Government of Canada . The Canadian Nutrient File. Health and Welfare Canada: Ottawa, Canada; 2010. [Google Scholar]
- Keranen AM, Savolainen MJ, Reponen AH, Kujari ML, Lindeman SM, Bloigu RS, et al. The effect of eating behavior on weight loss and maintenance during a lifestyle intervention. Prev Med. 2009;49:32–38. doi: 10.1016/j.ypmed.2009.04.011. [DOI] [PubMed] [Google Scholar]
- Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005;6:67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- Provencher V, Drapeau V, Tremblay A, Despres JP, Lemieux S. Eating behaviors and indexes of body composition in men and women from the Quebec family study. Obes Res. 2003;11:783–792. doi: 10.1038/oby.2003.109. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Going SB, Sardinha LB, Lohman TG. A review of psychosocial pre-treatment predictors of weight control. Obes Rev. 2005;6:43–65. doi: 10.1111/j.1467-789X.2005.00166.x. [DOI] [PubMed] [Google Scholar]
- Drapeau V, Provencher V, Lemieux S, Després JP, Bouchard C, Tremblay A. Do 6-y changes in eating behaviors predict changes in body weight? Results from the Quebec Family Study. Int J Obes Relat Metab Disord. 2003;27:808–814. doi: 10.1038/sj.ijo.0802303. [DOI] [PubMed] [Google Scholar]
- Bryant EJ, King NA, Blundell JE. Disinhibition: its effects on appetite and weight regulation. Obes Rev. 2008;9:409–419. doi: 10.1111/j.1467-789X.2007.00426.x. [DOI] [PubMed] [Google Scholar]
- Rodriguez A, Gomez-Ambrosi J, Catalan V, Gil MJ, Becerril S, Sainz N, et al. Acylated and desacyl ghrelin stimulate lipid accumulation in human visceral adipocytes. Int J Obes (Lond) 2009;33:541–552. doi: 10.1038/ijo.2009.40. [DOI] [PubMed] [Google Scholar]
- Tschop M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000;407:908–913. doi: 10.1038/35038090. [DOI] [PubMed] [Google Scholar]
- Killgore WD, Kahn-Greene ET, Lipizzi EL, Newman RA, Kamimori GH, Balkin TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. 2008;9:517–526. doi: 10.1016/j.sleep.2007.07.003. [DOI] [PubMed] [Google Scholar]
- Dweck JS, Jenkins SM, Nolan LJ. The role of emotional eating and stress in the influence of short sleep on food consumption. Appetite. 2014;72:106–113. doi: 10.1016/j.appet.2013.10.001. [DOI] [PubMed] [Google Scholar]
- van Strien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. Int J Eat Disorder. 1986;5:295–315. [Google Scholar]
- Chaput JP, Després JP, Bouchard C, Tremblay A. The association between short sleep duration and weight gain is dependent on disinhibited eating behavior in adults. Sleep. 2011;34:1291–1297. doi: 10.5665/SLEEP.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilkus JM, Booth JN, Bromley LE, Darukhanavala AP, Imperial JG, Penev PD. Sleep and eating behavior in adults at risk for type 2 diabetes. Obesity (Silver Spring) 2012;20:112–117. doi: 10.1038/oby.2011.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder CR, Gullion CM, Funk KL, Debar LL, Lindberg NM, Stevens VJ. Impact of sleep, screen time, depression and stress on weight change in the intensive weight loss phase of the LIFE study. Int J Obes (Lond) 2012;36:86–92. doi: 10.1038/ijo.2011.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beccuti G, Pannain S. Sleep and obesity. Curr Opin Clin Nutr Metab Care. 2011;14:402–412. doi: 10.1097/MCO.0b013e3283479109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaput JP, Bouchard C, Tremblay A. Change in sleep duration and visceral fat accumulation over 6 years in adults. Obesity (Silver Spring) 2014;22:E9–E12. doi: 10.1002/oby.20701. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Tremblay A. Does short sleep duration favor abdominal adiposity in children. Int J Pediatr Obes. 2007;2:188–191. doi: 10.1080/17477160701306144. [DOI] [PubMed] [Google Scholar]
- French SA, Epstein LH, Jeffery RW, Blundell JE, Wardle J. Eating behavior dimensions. Associations with energy intake and body weight. A review. Appetite. 2012;59:541–549. doi: 10.1016/j.appet.2012.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekker MH, van de Meerendonk C, Mollerus J. Effects of negative mood induction and impulsivity on self-perceived emotional eating. Int J Eat Disorder. 2004;36:461–469. doi: 10.1002/eat.20041. [DOI] [PubMed] [Google Scholar]