Abstract
In low- and middle-income countries (LMIC), determinants of women’s and children’s health are complex and differential vulnerability may exist to risk factors of perinatal distress and preterm birth. We examined the contribution of maternal perinatal distress on preterm birth and infant health in terms of infant survival and mother–infant interaction. A critical narrative and interpretive literature review was conducted. Peer-reviewed electronic databases (MEDLINE, Embase, Global Health, CINHAL), grey literature, and reference lists were searched, followed by a consultation exercise. The literature was predominantly from high-income countries. We identify determinants of perinatal distress and explicate changes in the hypothalamic–pituitary–adrenal axis, sympathetic, immune and cardiovascular systems, and behavioral responses resulting in pathophysiological effects. We suggest cultural–neutral composite measures of allostatic mediators (i.e., several biomarkers) of maternal perinatal distress as objective indicators of dysregulation in body systems in pregnant women in LMIC. Understanding causal links of maternal perinatal distress to preterm birth in women in LMIC should be a priority. The roles of allostasis and allostatic load are considered within the context of the health of pregnant women and fetuses/newborns in LMIC with emphasis on identifying objective indicators of the level of perinatal distress and protective factors or processes contributing to resilience while facing toxic stress. We propose a prospective study design with multiple measures across pregnancy and postpartum requiring complex statistical modeling. Building research capacity through partnering researchers in high-income countries and LMIC and reflecting on unique ethical challenges will be important to generating new knowledge in LMIC.
Keywords: Maternal stress; Pregnancy outcome; Infant, preterm; Allostatic load; Developing countries
Introduction
Both perinatal distress and preterm birth are world-wide problems that are especially burdensome in low- and middle- income countries (LMIC). Maternal prenatal and postnatal distress (i.e., stress, anxiety, or depression at any time in pregnancy and during the first year following birth of the infant), collectively referred to as “perinatal distress,” may be significantly higher in LMIC than high income countries [1]. The prevalence of perinatal mental disorders reported for LMIC is comparable to certain high-risk groups of women living in high-income countries [1–3]. In LMIC the determinants of women’s and children’s health are complex. Moreover, inequities in determinants of health and the social, cultural, and political contexts of women in LMIC negatively influence women’s mental health. Consequently, differential vulnerability may exist not only to risk factors of perinatal distress, but also to predictors of pregnancy outcome [4].
Stress, anxiety, or depression during pregnancy may contribute to preterm birth [5, 6]. Every year, 15 million babies are born prematurely, and 1.1 million will die due to prematurity-related health issues globally [7, 8]. Twelve of the 15 countries which contribute more than 60 % to the global burden of preterm birth are low or low-middle income countries [9]. Preterm birth is one of the major contributors to infant mortality and morbidity [7, 10], accounting for 80 % of the world’s 1.1 million deaths [9]. Africa and South Asia, with the exception of Pakistan, have made some progress in improving neonatal survival; however, death resulting from preterm birth is now the second leading cause of newborn deaths [7, 9]. Up to 50 % of pediatric neurodevelopment problems (e.g., cerebral palsy, lower intelligence quotient) are estimated to be the result of preterm birth [11–14].
Perinatal distress may also adversely influence infant survival, behavior, and development through poor quality of maternal–infant interactions [15–21]. A Taiwanese population-based study, that linked birth and death certificate registry, found the adjusted risk of mortality among preschool children up to age 5 years was 1.47 fold (95 % Confidence Interval, CI 1.16–1.87) when mothers experienced depression in the first year following birth [22]. Infants born in LMIC are already exposed to poverty, poor health, and poor nutrition, which reduces their developmental potential [23]. Beyond these issues, infants of depressed mothers are less likely to be breastfed, have incomplete immunizations, have poorer weight gain, and are more likely to experience illnesses, such as diarrhea, which in turn, may increase the number of hospital admissions and contribute to higher mortality in children under 5 years of age [24–31].
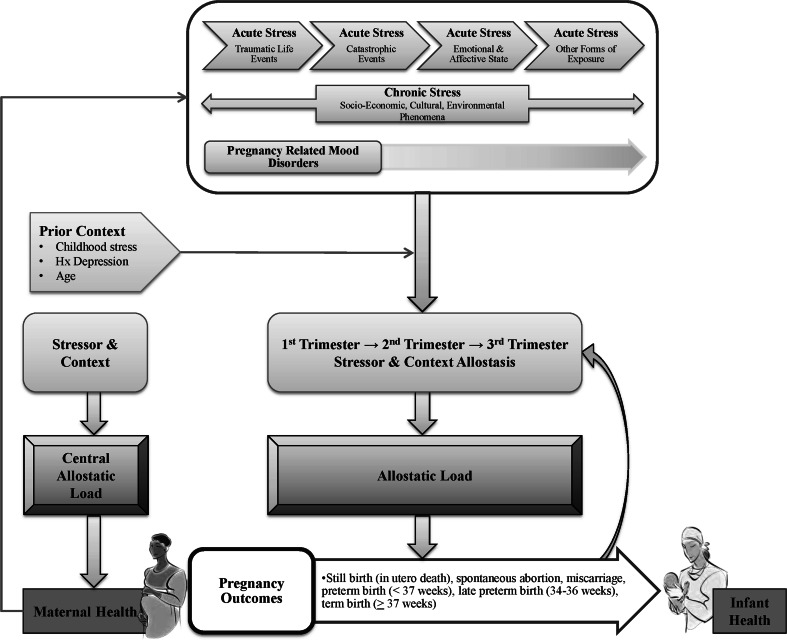
Clinicians typically rely on self-report questionnaires to assess perinatal distress. While very useful, self-report is prone to bias or error [32]. An alternative is to use biomarkers that may offer a more objective and quantifiable indicator of the level of perinatal distress [33]. The conceptual framework of allostatic load [20] links perinatal distress and its physiological responses to multisystem dysregulation, which promotes a cascade of events ultimately impacting pregnancy outcome (i.e., preterm birth) and infant health (i.e., survival and development) [16, 18–20, 34]. In this context, biomarkers that detect physiological compromise may be useful predictors of perinatal distress and its negative consequences. Specifically, perinatal distress may activate aspects of the hypothalamic–pituitary–adrenal (HPA) axis, sympathetic, immune and cardiovascular systems, and promote behavior changes (e.g., smoking, drinking) in the effort to restore allostasis [13, 20]. Over time, given “wear and tear” on the brain and body, biological responses may be compromised, or fail outright. Allostasis refers to the continual changes in set points (i.e., lower or higher ranges) of physiologic systems to maintain constancy [20, 34] with repeated and ongoing (i.e., chronic) exposure to determinants of perinatal distress over the course of pregnancy [16, 35, 36]. The resulting dysregulation of interrelated systems may, over time, reach a “tipping-point” [16] referred to as allostatic load or overload, that ultimately results in pathophysiological effects. In the case of perinatal distress, effects can include preterm birth [20, 34] and altered maternal and infant behaviors that adversely influence infant survival and development [15, 16, 18–21, 37].
A critical narrative and interpretive review [38] was undertaken to: (a) determine the etiologic contribution of perinatal distress on preterm birth in pregnant women in LMIC; and (b) develop a conceptual framework that would explicate the potential casual links of perinatal distress to preterm birth and infant health (i.e., infant survival, and mother–infant interaction). The goal of the review was to inform future research in LMIC by providing a conceptual framework to examine psychosocial and environmental factors as both risk factors and targets of intervention to prevent preterm birth (i.e., improve maternal health outcomes) and improve infant survival and development.
Methods
Search and Selection Strategy
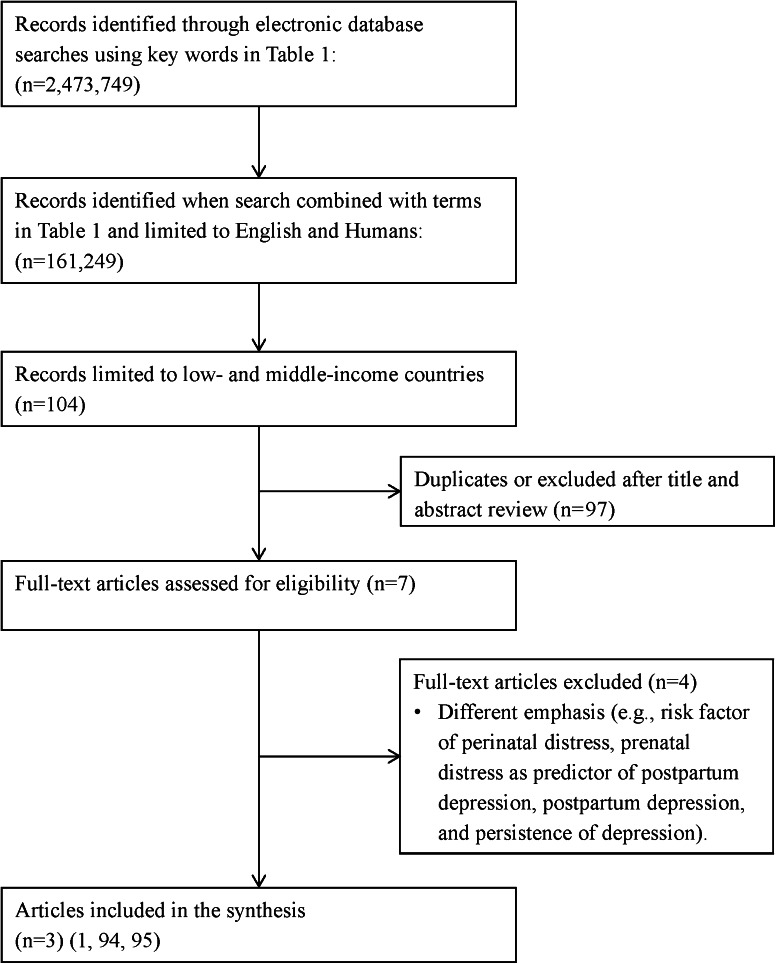
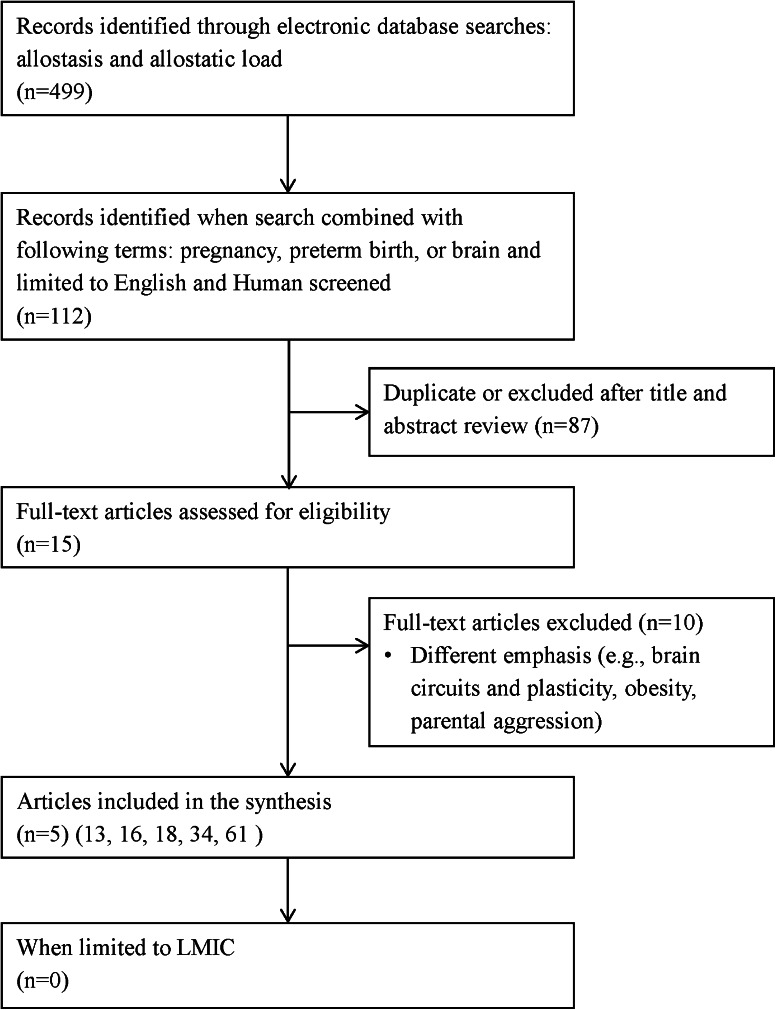
We searched peer-reviewed electronic databases including MEDLINE (1946–January 2013), Embase (1974–January 2013), Global Health (1910–January 2013), and Cumulative Index to Nursing and Allied Health Literature (CINHAL) (1990–January 2013). Grey literature (e.g., unpublished theses, organizational websites), reference lists, and an existing network of experts in the area (including research team members from Pakistan, Kenya, and Tanzania) were also used in identifying relevant publications. A conventional review technique using the search strategy and selection strategy detailed in Table 1 proved to be limiting given the dearth of literature in LMIC (see Figs. 1, 2). In contrast, a search of the existing literature using all key words, combined terms, and exclusion criteria (i.e., etiology and conceptual framework) without limiting the country of origin generated 6,908 records.
Table 1.
Key words, combined terms, and selection criteria
| Key words | Combined terms | Selection criteria | |
|---|---|---|---|
| Etiologic contribution of perinatal distress on preterm birth | Stress; anxiety; depression; stress, maternal; stress, psychological; chronic stress; postpartum depression; perinatal distress; or perinatal depression | Pregnancy; women; pregnant, women; perinatal outcomes; infant health; infant survival; mother–infant interaction; maternal health; or preterm birth | Pregnant or postpartum women; recruitment in low- and middle-income countries; assessed psychosocial health/factors; examined any determinant of health that would impact maternal psychosocial well-being and maternal or infant health; any study design; human; English |
| Conceptual framework | Allostasis or allostatic load | Pregnancy; preterm birth; or brain | Pregnant or postpartum women; recruitment in low- and middle-income countries; maternal health; infant health; any study design; human; English |
Fig. 1.
Overview of trial flow through the search and selection process: Contribution of perinatal distress on preterm birth
Fig. 2.
Overview of trial flow through the search and selection process: Allostasis and allostatic load
Applying a precise review question or narrowing the search by assembling certain levels of evidence is restrictive when the intent of the literature review is also to generate a theory [38]. Consequently, we used a critical narrative and interpretive synthesis approach [38], based in dialectic process including both inductive and deductive reasoning, to guide our sampling of the extant literature, regardless of study type and location of study, while maintaining a focus on the aims of the review. As a starting point we used our earlier review [39] on the relationship between prenatal stress, depression, cortisol and preterm birth, and the literature reviewed here. We then purposefully sampled the existing literature to elaborate on the phenomena of interest and our analysis of the literature. The approach we used to develop the conceptual framework was iterative and the emphasis of the review changed and was informed by our emerging understanding and analysis of the literature (i.e., recursive and reflexive). We continued to sample the literature until there was saturation, that is, similar ideas emerged repeatedly [38]. A total of 73 articles identified through this iterative process complemented the eight articles identified in the initial search (see Figs. 1, 2).
Quality Assessment and Data Extraction
All types of studies were valued for their contribution, as they provided new ways of understanding our emergent conceptual framework and causal links between perinatal distress and preterm birth. Criteria for assessment included: (1) whether the study design was appropriate given the aim and objectives of the study; (2) appraisal of study reporting (e.g., data collection process described, appropriate method of analysis, enough data shared to support interpretation and conclusions); or (3) judgment about whether the study clarified what is known and what is not known, and informed the interpretation of concepts or the review in general [38]. No papers were removed because of poor methodological standards.
Consultation Exercise
Towards the end of the review, a group of stakeholders (researchers, clinicians, academics, and policy decision-makers) from Pakistan, Kenya, Tanzania, and Canada were brought together to add additional insights and refine the conceptual framework. Terminology, such as perinatal distress, was clarified and a common understanding was developed of concepts. Essential elements of the framework were identified and revisions were made to better illustrate relationships between components. Through an iterative and consensus building process with feedback received from peer-reviewers of this manuscript, we present the final conceptual framework (see Fig. 3).
Fig. 3.
Perinatal distress and pathways to pregnancy outcome: Allostatic load as a conceptual framework
Findings
Perinatal mental health of women living in LMIC, particularly mental health during pregnancy, received little attention until 2002. LMIC were represented in only 8 and 15 % of the pregnant- and post-partum related studies, respectively compared to 90 % of high income countries [1, 40]. A systematic review [1] and a report of the World Health Organization-United Nations Population Fund [40] concluded that available literature from LMIC (41 studies) suggests a wide range in prevalence rates of perinatal mental disorders as a consequence of place of recruitment (e.g., tertiary hospital, provincial or district health services, and community facilities), and methodology (e.g., time of data collection, and screening instruments). An average prevalence of 15.9 % (95 % CI 15.0–16.8 %) during pregnancy and 19.8 % (95 % CI 19.2–20.6 %) postpartum were reported [1], with depression and anxiety disorders being the most frequent diagnoses in both periods [1, 40]. The conceptual framework to examine risk factors for perinatal distress varied among the 31 studies and therefore data could not be pooled [1]. Findings related to risk and protective factors of perinatal distress were mixed and the majority did not address all the domains of the social determinants of health used to synthesize the literature, namely, socioeconomic factors, quality of relationship with intimate partner, family and social relationships, reproductive and general health, history of mental health problems, and infant characteristics [1]. Social factors, particularly those beyond the women’s control, seem to influence perinatal mental health of women in LMIC [1]. Moreover, prevention of preterm birth has received little attention in these countries. Although we were able to identify nine studies focusing on preterm birth in LMIC, none examined the relationship between perinatal distress and preterm birth. Five studies [7–10] reviewed epidemiology including global trends, causes, and interventions thus informed this review. However, four studies were excluded as they focused on the use of antenatal steroids in LMIC (two studies), or long-term neurodevelopmental outcomes of preterm infants born in LMIC (two studies). Thus, in LMIC there are missed opportunities to address mental health needs of women along the perinatal continuum and contribute to scientific knowledge and evidence-informed practices and policies to reduce preterm birth and improve infant health outcomes.
Perinatal Distress Predicts Preterm Birth
The term “perinatal distress” encompasses a spectrum of psychological conditions in response to experiences of episodic and chronic stress associated with adverse socio-economic, cultural, and environmental phenomena [41]. The North American literature suggests that pregnancy-related anxiety, which relates to the women’s fears about the infant’s health, delivery, her own health and survival during the birthing experience, and the impending responsibility of providing for the child [42], is a stronger determinant of preterm birth than general anxiety [5, 6, 42–44]. Though many North American and European studies have shown an association between general anxiety and preterm birth (e.g., [45, 46]), the findings have been mixed (e.g., [47, 48]). In one study, changes in anxiety level over time rather than the anxiety level at one time point predicted preterm birth [49]. North American and European studies examining the relationship between depression and preterm birth have also shown inconsistent findings, with a minority of the studies finding a statistically significant association between depression and preterm birth (e.g., [44, 46, 50]).
Many distinguishable forms of stress can be grouped into chronic stressors and episodic (i.e., acute) stressors. Chronic stress differs from acute stress, in that the threat or demand is long-lived, and often without resolution [13]. The chronic stress of homelessness or household strain has been associated with preterm birth [41]. A study of 739 low-income African-American pregnant women in the United States found that inadequacy of time and money for non-essentials (e.g., time to look nice, time with friends and family) were mediating factors for preterm birth, whereas multidimensional stress (money worries, family problems, and neighborhood crime) and locus of control were independent predictors of preterm birth [51]. Neighborhood-level stressors, such as poverty, crime, and racial composition have also shown an independent impact on preterm birth [41]. Episodic stressors include catastrophic events, such as natural disasters (e.g., hurricane, earthquake, and drought), and manmade calamities (e.g., political strife, and war), have shown varied impacts on pregnancy outcomes from no detected effect (e.g., [52]), to lower [53] and higher [54] rates of preterm birth. The inconsistent findings may be explained by differences in levels of support, medical care, and changes in behavior following the event [41].
Based on the current literature, a multidimensional approach for examining perinatal distress is evident. None of the studies located examined all of the above dimensions of perinatal distress in relation to preterm birth in the same sample. Whether perinatal distress predicts preterm birth in LMIC remains to be established, as none of the studies considered women in LMIC despite nine of the 11 countries with the highest rate of preterm birth being LMIC [9]. In our pilot study [55] the odds of preterm birth were 1.44 times higher in the depressed Pakistani women than in the non-depressed Pakistani women. The social, cultural, and environmental context of LMIC provide the potential for an in-depth investigation of the multidimensional nature of perinatal distress, which could not be achieved in high-income countries, as all dimensions of perinatal distress co-exist in one setting. Furthermore, the void of empirical literature stemming from LMIC on perinatal distress makes it imperative to examine the etiologic contribution of perinatal distress on preterm birth in LMIC.
Explaining Causal Links of Perinatal Distress to Preterm Birth
In an attempt to adapt or maintain stability (i.e., allostasis), the body responds to perinatal distress (i.e., stress, anxiety, or depression) by producing multisystem physiologic responses through the production of hormonal and neurotransmitter mediators [20, 56, 57]. In addition to being protective or adaptive, these mediators can have damaging effects [58]. Over time, repeated fluctuations and elevated levels of physiologic activity can lead to inefficiency in allostasis where accumulation and overexposure to these mediators (i.e., allostatic load) may results in organ system failure [56, 58]. According to the conceptual framework of allostatic load, composite measures of biomarkers (i.e., hormonal and neurotransmitter mediators) versus individual biomarkers may be a stronger predictor of negative consequences of perinatal distress [56, 59]. The original set of ten parameters of allostatic load continues to expand [60]. Empirically supported allostatic load biomarkers implicated in the pathophysiological process linking perinatal distress to preterm birth include:
Cortisol
The brain coordinates the interconnected set of neuroendocrine and behavioral responses to perinatal distress [58, 61]. Cortisol, regulated via the HPA axis, is a primary hormone reported to be elevated in response to stress induced by physical, cognitive and psychosocial challenges [58, 61]. Cortisol is also proposed to be a primary mediator contributing to allostatic load [59, 61]. Although chronically high levels of cortisol have been the focus in the interplay between stress and allostatic load, low cortisol has also been implicated in adverse health outcomes [61]. Consequently, response and recovery promoting optimal functioning of pathophysiologic processes following stress is important when considering allostatis [61]. Thus, low values and high values may be predictive of preterm birth. Cortisol, measured in blood, has been reported in the majority of studies to have a positive association with preterm birth [62].
Corticotropin-Releasing Hormone
Pathologic levels of cortisol can increase the production of placental corticotropin-releasing hormone (CRH) in a dose response relationship [63]. Placental CRH levels beyond a certain threshold can have a paradoxical effect of preparing for labor and initiating contractions [63]. In the pregnant state, the diurnal variations in hormones, such as cortisol, are to a certain extent diminished [34]. In an attempt to compensate for the dysregulation of cortisol, systemic responses of the metabolic, inflammatory, and cardiovascular systems may also experience dysregulation [36, 64].
Triglyceride, Total Cholesterol, Low-Density Lipoprotein, and High-Density Lipoprotein
Total cholesterol, and high-density lipoprotein (HDL), represent the primary effects in response to dysregulation of cortisol [59]. Hypercholesterolemia (a secondary mediator) may result in response to high levels of cortisol which mobilizes lipids from adipose tissues [65]. Although high levels of cholesterol decreases uterine contractility [65], in combination with the natural lipid profile of pregnancy [66], an allostatic load effect may alter the vulnerability of the uterine smooth muscle thereby changing its propensity to remain quiescent during pregnancy. During pregnancy, the lipid profile of women changes (i.e., increase in triglyceride, total cholesterol, and low-density lipoprotein) in response to hormonal changes occurring with increasing gestational age [66]. Alternation in lipid metabolism, specifically delayed clearance of triglycerides, has been implicated in pregnancy complications (e.g., hypertension and development of preeclampsia) that may lead to medically indicated preterm birth [66], as well as adverse pregnancy and infant outcomes [67].
White Blood Cell Count, C-Reactive Protein, and Cytokines
Primary effects, such as changes in inflammatory biomarkers in response to primary neuromediators (i.e., cortisol) of stress, have been implicated in the pathway to preterm birth. A systematic review examining the association between inflammatory cytokines and risk of spontaneous preterm birth in asymptomatic women concluded that the maternal–fetal interface, rather than systemic inflammation, plays a major role [68]. Pregnancy-related anxiety has been associated with preterm birth [6, 69], but among these two studies, only one found that inflammatory markers mediated this influence [69]. Various scales were used to measure pregnancy-related anxiety and samples were drawn from high-income countries with low rates of preterm birth.
Immunosuppression of cellular and humoral immune activity resulting from dysregulation of neuroendocrine mediators, is either site specific (e.g., bacterial vaginosis) [70] or systemic, and may increase risk of infections which may be monitored by examining changes in white blood cells counts. In a meta-analysis, bacterial vaginosis was identified as a strong risk factor for preterm birth, with individual studies repeatedly and consistently demonstrating an association [70]. A connection has also been demonstrated between prenatal stress and C-reactive protein (CRP) [69]. Increased inflammatory cytokines produced both in response to stress (primary mediators) and in response to the infection stimulates production of CRP and triggers prostaglandin production which is a mediator of labor [71]. Typically increased cortisol levels serve as a negative feedback loop to decrease production of cytokines and hormones [71]; however, the dysregulation of neuromediators most likely impairs this negative feedback loop.
Immunoglobulin G
Immunoglobulin G, an antibody that crosses the placenta, is critical in protecting the infant from infection in the neonatal period. Lower transplacental ratios of immunoglobulin G have been reported in preterm infants [72]. High levels of immunoglobulin G, in response to dysregulation of cortisol, is proposed to saturate binding sites, thereby limiting the placenta’s efficiency in transfer of immunoglobulin G [73]. Since the infant’s humoral response is inefficient, the impaired transfer of immunoglobulin G may further compromise the infant’s ability to fight infection in early life [73] and increase risk of mortality.
Blood Pressure and Heart Rate
Increased blood pressure and heart rate represent a disease state or disorders resulting from allostatic load, as a consequence of secondary outcomes and primary mediator of stress [59]. Cardiovascular reactivity is normally reduced in pregnancy [74]. However, increased levels of cortisol may increase maternal cardiovascular reactivity (e.g., increase blood pressure and heart rate—secondary mediators) [34] by altering maternal, placental or fetal hemodynamics [75]. A relationship has been demonstrated between high diastolic blood pressure responses to stress during pregnancy and decreased gestational age at birth [75–78]. A dose–response pattern has been observed between the rise in blood pressure and spontaneous preterm birth [79].
There is empirical support (approximately 60 studies) for an association between increased allostatic load and negative health consequences of stress (e.g., cardiovascular disease) [80]. Notably, none of the documented studies (e.g., [6, 55, 81–85]) examining the relationship between perinatal distress, biomarkers of stress, and preterm birth have made use of allostatic load in their conceptual framework. Moreover, the scales used to measure perinatal distress, biomarkers of stress examined, time periods of measurements and findings have varied between studies (see Table 2). Individual mediators of stress examined in these studies included cytokines (interleukin-10, interleukin-6 and tumor necrosis factor-alpha), CRP [69], cortisol [6], and CRH [6]. Interrelated physiological (i.e., biochemical) response patterns [86, 87] and composite measures involving several biochemical measures offer a more objective and quantifiable indicator of the level of perinatal distress in pregnant women in LMIC who are in difficult cultures, than self-report psychological measures of perinatal distress [56, 59]. The risk of preterm birth will be higher when there is an inadequate response to prenatal distress (i.e., high perinatal distress and low allostatic load) or prolonged response to a previous stress (i.e., low perinatal distress and high allostatic load) [20, 57]. Identifying high risk pregnant women in LMIC and understanding the pathophysiological process of poor pregnancy and health outcomes will guide the development and evaluation of therapeutic interventions to avert preterm birth.
Table 2.
Summary of studies examining the relationship between prenatal stress, biomarkers of stress, and preterm birth
| Study and country (region) | Design | Participants (n) | Measures | Results | ||
|---|---|---|---|---|---|---|
| Scales | Specimen | Time, gestation (weeks) | ||||
|
Hobel et al. [81] USA (Los Angeles) |
Prospective case–control studya |
Subsample of 524 Cases: 18 (spontaneous onset of preterm labor) Control: 18 (delivered at term) Inclusion/exclusion criteria: not specified |
PSS-8; STAIT-10 | Plasma CRH, ACTH, cortisol |
18–20 28–30 35– |
Higher plasma CRH levels and ACTH levels were reported at all three time periods and elevated cortisol levels at 18–20 weeks’ gestation and 28–30 weeks’ gestation in women who delivered preterm when compared to those who delivered at term. Stress levels did not differ between 18–20 weeks’ gestation and 28–30 weeks’ gestation. Variance in CRH at 28–30 weeks’ gestation was explained by maternal stress level at 18–20 weeks’ gestation and maternal age. |
|
Erickson et al. [82] Denmark (Odense) |
Prospective case–control cohort designa |
Subsample of 2,927 Cases: 84 (delivered preterm [idiopathic etiology] without complications) Control: 224 (delivered at term and matched, at time of enrollment, to within 10 days of due date of cases) Inclusion criteria: age >18 years, ability to understand Danish. Exclusion criteria: insufficient responses to the questionnaires, placental previa (diagnosed after 30 full gestational weeks), history of severe fetal congenital malformations in previous pregnancy, uterine cervix insufficiency treated with cervical circlage |
Three questionnaires: (1) just before inclusion (past medical history); (2) 30 weeks’ gestation (social and demographic information); (3) birth; (urogenital and obstetric problems) If delivered preterm, completed second and third questionnaire at same time |
Plasma CRH, CRH-binding protein, cortisol Venous blood sample taken during labor (delivered preterm), and 37–43 weeks’ gestation (delivered at term) |
7–23 27–37 |
7–23 weeks: CRH and CRH-binding protein levels were higher in women who delivered preterm when compared to women who delivered at term. 27–37 weeks’ gestation: CRH and cortisol levels were higher but CRH-binding protein levels were lower in women who delivered preterm when compared to women who delivered at term. Previous preterm delivery and engagement in some risk-taking behaviors were associated with preterm birth |
|
Ruiz et al. [83] USA (central Texas) |
Prospective, longitudinal, observational study |
Cases: 78 Inclusion: English speaking, <28 weeks’ gestational age, 18–40 years of age, singleton pregnancy. Exclusion criteria: Rh isoimmunization, cervical cerclage, use of tocolytic agents during current pregnancy, diabetes mellitus requiring insulin, thyroid disorders, chronic renal or heart disease, misses more than 1 monthly prenatal check for data collection |
PSS-10 (23–26, and 31–35 weeks’ gestation) | Blood cortisol (all time points); vaginal swabs for fetal fibronectin, chlamydia, and bacterial vaginosis screen (23–26 and 27–30 weeks’ gestation) |
15–19 20–22 23–26 27–30 31–35 |
Cortisol was a poor predictor of both preterm labor and preterm birth; however an increase in cortisol level was noted in women with genitourinary infection. Change is PSS score, that is decrease in perceived stress during the 2nd trimester, was significantly associated with increase in length of gestation |
|
Mancuso et al. [84] USA (Los Angeles) |
Case–control study nested in a prospective cohorta |
Subsample of 688 Cases: 282 Inclusion criteria: singleton intrauterine pregnancy, gave birth to liveborn infant, received prenatal care in prenatal clinics and private practices in Los Angeles, California. Exclusion criteria: age <18 years, stillborn births, multiple gestation births, lack of birth outcome data, and incomplete psychosocial data |
PSA | Plasma CRH |
18–20 28–30 |
Women with high CRH levels and high maternal prenatal anxiety at 28–30 weeks gestation delivered earlier. CRH levels were significantly higher at both times points in women delivered preterm than women who delivered at term. Mediation effect of CRH |
|
Kramer et al. [6] Canada (Montreal) |
Prospective cohort and nested case–control design |
Subsample of a larger study Cases: 207 Control: 444 Inclusion criteria: age ≥18 years, singleton gestation, and able to speak English or French. Exclusion criteria: severe chronic illness with ongoing treatment (note: other than hypertension, asthma, or diabetes), placenta previa, diagnosis of incompetent cervix in previous pregnancy, impending delivery, or fetus with congenital anomaly |
DHS (lacked basic or essential needs subscale), MSS (chronic stress), AAS (conjugal violence), 5-item scale (injury, job related stress), MIS (intention of pregnancy), ASSIS (perceived social support), PLES (acute stressors), PSS, Dunkel-Schetter 4-item scale (pregnancy related anxiety), RSES, LOT (optimism and pessimism), CES-D, single item (woman’s perception of her risk of birth complications), 8-item scale (commitment to pregnancy) | Hair cortisol, histo-pathologic examination of vaginal swabs, placenta, and cord | 24–26 | Only pregnancy related anxiety was consistently and independently associated with spontaneous preterm birth and a dose–response was reported across quartiles. Hair cortisol was positively associated with gestational age but not CRH. Maternal plasma CRH, hair cortisol, placental histopathology (i.e., features of infection/inflammation, infarction, or maternal vasculopathy) were not associated with stress, anxiety, or distress measures |
|
Pearce et al. [85] Denmark (Odense) |
Case–control study nested in a prospective cohort |
Subsample of 2,927 Cases: 60 [delivering preterm (<37 weeks) without a cause, as determined from clinical findings or laboratory investigations during pregnancy or at delivery] Control: 123 (delivering at term) Inclusion criteria: age >18 years, ability to understand Danish. Exclusion criteria: insufficient responses to the questionnaires, placental previa (diagnosed after 30 full gestational weeks), history of severe fetal congenital malformations in previous pregnancy, uterine cervix insufficiency treated with cervical circlage |
Questionnaire (stressful life events, risk-taking behavior indicated by lack of seat-belt usage) | Serum measures of cortisol, MIF, CRP, CRH, interleukin-1 ß, interleukin-6, interleukin-10, tumor necrosis factor-alpha | <24 | Individual biomarkers: MIF (strongest association), interleukin-10, CRP and tumor necrosis factor-alpha predicted preterm birth at various cutoff levels (e.g., 75th, 85th, and 90th percentile). Logistic regression models: MIF, CRP, risk-taking behavior, and low education consistently predicted preterm birth at various cutoffs; however, the 75th percentile cutoff was the best predictive model. MIF may be a psychobiological mediator |
|
Shaikh et al. [55] Pakistan (Kirachi) |
Prospective cohort study design |
Cases: 132 (125 with complete data) Inclusion criteria: age 18–40 years, 28–30 weeks’ gestation. Exclusion criteria: diabetes mellitus, thyroid disorder, chronic renal or heart disease, or uterine and cervical abnormality, or on antidepressants or other psychotropic drugs, and did not deliver in setting where the study was based |
A–Z Stress Scale, CES-D | Serum cortisol | 28 | A significant positive relationship was reported between maternal depression and stress. No relationship was noted between cortisol value and stress scale or depression scale. Preterm birth was associated with higher parity, past delivery of a male infant, and higher levels of paternal education |
Adopted from Shaikh et al. [39]
AAS Abuse Assessment Screen (adapted), ACTH adrenocorticotropic hormone, ASSIS Arizona Social Support Interview Schedule, CES-D Centre for Epidemiology Studies Depression Scale, CRH corticotropin-releasing hormone, CRP C-reactive protein, DHS Daily Hassles Scale, LOT Life Orientation Test, MIF macrophage migration inhibitory factor, MIS Miller Intendedness Scale, MSS Marital Strain Scale of Pearlin and Schooler, PLES Prenatal Life Events Scale, PSA Pregnancy-Specific Anxiety Scale, PSS-8 Perceived Stress Scale 8-item version, PSS-10 Perceived Stress Scale 10-item version, RSES Rosenberg Self-Esteem Scale, STAIT Spielberger’s State Anxiety Inventory 10-item version
aNot labelled
Explaining Causal Links of Perinatal Distress to Infant Health
Allostatic load or overload exerts its influence on biological indices or mediators of the HPA axis and sympathetic–adrenal–medullary systems involving a complex interplay between the mother and fetus [13, 59]. The dysregulation of cortisol influences the permeability of the placenta to cortisol, thereby altering the placental and fetal environment [64] and potentially increasing permeability of other mediators which typically do not cross the placenta (e.g., epinephrine). The health of the fetus and newborn “mirror” the health of the mother whereby the fetus or newborn mimics the biochemical profile of the mother. Allostatic load in the fetal brain may also alter behavioral systems which involve attachment/approach and avoidance behaviors that are integral to survival [16, 18, 58]. Allostatic load may also alter the function (e.g., affective, cognitive, and social) and structure of the brain, and pathological levels may impact developmental outcomes [19]. Perinatal distress may directly (e.g., alter structure and function of brain) or indirectly (i.e., through mother–infant interaction) influence infant health and well-being.
In addition to activating the HPA axis, and sympathetic, immune and cardiovascular systems, psychosocial health during pregnancy has been linked to negative maternal health behavior (e.g., consuming non-nutritive substances like soil, consumption of alcohol, and cigarette smoking) [88]. Maternal prenatal distress and postnatal distress may result in the same disorders simply manifested along the perinatal continuum [89]. Altered parenting patterns (i.e., lack of responsivity to infants’ needs [90, 91], inability to coordinate age-appropriate activities [92], and harsh parenting style [93] ) observed in mothers with PPD may contribute to infant stress, with cumulative stress influencing vulnerability to death, disease, or poor developmental outcomes through the effects of infant allostatic load [15–21]. Although in LMIC there is limited evidence examining the contribution of prenatal distress to infant health outcomes (e.g., [94]), there is extensive scientific evidence linking PPD and infant health [95] that may be explained by the conceptual framework of allostatic load.
Our pilot data suggests that the odds of depression are 2.7 times greater (95 % CI 1.16–6.17, p = 0.015) in Pakistani mothers of preterm infants than Pakistani mothers of full-term infants [96]. Thus, for infants born in LMIC, the interactive effects of biological vulnerability associated with being born premature, social vulnerability inherent in women’s responses to their environment during the postpartum period and inequities in determinants of health (i.e., poverty, poor nutrition) places them at triple jeopardy to experience poorer health outcomes. In LMIC, premature infants’ chance of survival, well-being and lifetime developmental and behavioral success may depend on reducing or managing risk factors associated with perinatal distress. For example, implementing early interventions to reduce the risk of stress, anxiety or depression during pregnancy or improve maternal behavior (i.e., increase responsiveness to infant) in the months following the birth of the infant may be warranted.
Discussion
The conceptual framework of allostatic load relates preterm birth to the social, environmental, and biological antecedent of perinatal distress, thereby enabling researchers to examine the interrelationships between various determinants of health. It provides an integrated model that is essential to examine the nature of risk (i.e., cumulative risk) across many systems at the same time and the temporal effects of the risk(s). The use of the conceptual framework of allostatic load to examine the etiologic contributions of perinatal distress on pregnancy and infant outcomes will necessitate longitudinal study designs with multiple time points (e.g., first trimester, early and late second trimester, and third trimester), and multiple measures of data collection (i.e., all dimensions of perinatal distress).
Although for our purpose we have focused on the negative pregnancy outcome of preterm birth, the conceptual model can be used to investigate pathways for positive pregnancy outcomes. A positive health focus may facilitate population level interventions directed at promoting mental health during pregnancy or “salutogenesis” within the context of their social, cultural, and political environment [97]. In LMIC, focusing on what makes women resilient in the face of toxic stress (i.e., pervasive, uncontrollable stress)—that is, improving their sense of coherence or “way of being in the world” [98]—may reduce the burden of health care service delivery. Furthermore, this type of research will facilitate identification of culture-sensitive strategies [98] to promote the mental health of women along the perinatal continuum. However, it will be important to debate and discuss social and cultural norms and policies that undermine, both at an individual level and society level, women’s mental health during pregnancy and postpartum and access to mental health services.
Building research capacity will be essential to addressing the under-representation of pregnancy and post-partum related studies in LMIC. Facilitating partnerships between researchers in high-income countries and LMIC to identify and resolve unique challenges related to ethical conduct of research will be important to generating new knowledge in LMIC. Key among these challenges is the communication and understanding of informed consent [99]. Since women in LMIC are underprivileged (e.g., poor, with limited access to health care), they may be particularly vulnerable to coercion. Moreover, in keeping with the World Medical Association Declaration of Helsinki, the research should “be responsive to the health needs and priorities of this population or community” [100]. Since mental health care services may be non-existent or limited and predominantly hospital based [101] consideration should be given to developing or strengthening local mental health care referral services that will continue to serve the women after completion of the study. Strategies (e.g., referrals) will need to be developed to minimize risk and prevent harm to women participating in the study over the course of their pregnancy and following birth of their baby.
Aside from these ethical issues, studies involving blood sampling for allostatic load parameters need to critically consider the available laboratory infrastructure. Study procedures including procurement of laboratory samples, storage, transportation and processing may create technical and logistical difficulties. Establishing standard procedures, training and supervision of local researchers to develop research capacity, and assisting with knowledge transfer may mitigate logistical issues and ensure adherence to study protocols [102, 103]. Furthermore, quality assurance measures may need to be established to ensure quality data [104]. Recruitment and retention of subjects may present significant challenges [105] as infrastructure, including communication to arrange follow-up visits and clinical facilities for care may be lacking [102].
Conclusion
Pregnant women in LMIC have been a neglected population in studies on perinatal distress and pregnancy and infant outcomes. Given inequities in determinants of health and the social, cultural, and political contexts of childbearing women in LMIC, these women may experience differential vulnerability to risk factors for perinatal distress and poor pregnancy outcomes. Prospective studies with multiple biological and psychosocial measures of stress, depression or depressive symptoms and its antecedents (e.g., childhood stress, major life events, etc.), state and trait anxiety, and pregnancy-related anxiety may add new knowledge and enhance our understanding about the etiologic contributions of psychosocial processes to preterm birth. A theoretical framework of allostatic load will enable researchers to concurrently examine social, environmental, and genetic antecedents of stress-related vulnerability and physiological (e.g., immune system, placenta) and behavioral responses that influence not only pregnancy outcomes of women in LMIC but also the life trajectories of health and wellness of the fetuses/infants (i.e., mortality and morbidity over time) [64]. Interrelated physiological (i.e., biochemical) response patterns [86, 87] and composite measures involving several biochemical measures offer a more objective and quantifiable indicator of the level of perinatal distress in pregnant women in LMIC. We propose that researcher maintain a positive health focus by identifying protective factors or processes that contribute to resilience in the face of toxic stress. When planning research studies using an integrative approach with both biological and psychosocial measures in LMIC, of critical importance is the adherence to principles of ethical conduct of research, engaging local researchers and other stakeholders to anticipate operational challenges to conducting research, and ensuring that the research is responsive to the needs of women during the perinatal period.
Acknowledgments
We would like to thank the Canadian Institute for Health Research for supporting the planning meeting (reference number 264531), which supported the conceptualization of the framework to guide our research project entitled “Biomarkers of allostatic load in LMIC pregnant women: perinatal distress, preterm birth, and infant health”. We would like to thank the Aga Khan University, School of Nursing and Midwifery, Karachi for hosting this planning meeting and Ms. Rozina Shazad, Dr. Saleem Iqbal and Ms. Rose Swai for participating in the planning meeting. A special thanks to Jill Norris for providing technical assistance in the preparation of the manuscript.
Footnotes
On behalf of MiGHT—Maternal Infant Global Health Team (Global collaborators in Research) [alphabetical order] Ms. Dorcas Akoya Amunga; Ms. Dorcus Asami Satia; Dr. Susan Dahinten; Dr. Farooq Ghani; Dr. Imtiaz Jehan; Dr. Zeenatkhanu Kanji; Mr. Adam King; Dr. Nicole Letourneau; Dr. Aliyah Mawji; Dr. Alliya Mohamed; Dr. Joseph Wangira Musana; Mrs. Mwasha Loveluck; Dr. Haider Ali Naqvi; Dr. Christopher T. Naugler; Ms. Christine Omukani Okoko; Dr. M. Sarah Rose; Dr. Pauline Samia; Ms. Kiran Shaikh; Ms. Salima Gulamani; Mr. Josephat Wambua; Ms. Saba Wasim; Dr. Ilona S. Yim.
References
- 1.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bulletin of the World Health Organization. 2012;90(2):139G–149G. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Price SK, Proctor EK. A rural perspective on perinatal depression: Prevalence, correlates, and implications for help-seeking among low-income women. The Journal of Rural Health. 2009;25(2):158–166. doi: 10.1111/j.1748-0361.2009.00212.x. [DOI] [PubMed] [Google Scholar]
- 3.Gress-Smith JL, Luecken LJ, Lemery-Chalfant K, Howe R. Postpartum depression prevalence and impact on infant health, weight, and sleep in low-income and ethnic minority women and infants. Maternal and Child Health Journal. 2012;16(4):887–893. doi: 10.1007/s10995-011-0812-y. [DOI] [PubMed] [Google Scholar]
- 4.Denton M, Prus S, Walters V. Gender differences in health: A Canadian study of the psychosocial, structural and behavioural determinants of health. Social Science and Medicine. 2004;58(12):2585–2600. doi: 10.1016/j.socscimed.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Dunkel Schetter C, Tanner L. Anxiety, depression and stress in pregnancy: Implications for mothers, children, research, and practice. Current Opinion in Psychiatry. 2012;25(2):141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kramer MS, Lydon J, Séguin L, Goutlet L, Kahn SR, McNamara H, et al. Stress pathways to spontaneous preterm birth: The role of stressors, psychological distress, and stress hormones. American Journal of Epidemiology. 2009;169(11):1319–1326. doi: 10.1093/aje/kwp061. [DOI] [PubMed] [Google Scholar]
- 7.Lawn JE, Gravett MG, Nunes TM, Rubens CE, Stanton C, GAPPS Review Group Global report on preterm birth and stillbirth (1 of 7): Definitions, description of the burden and opportunities to improve data. BMC Pregnancy Childbirth. 2010;10(Suppl 1):S1. doi: 10.1186/1471-2393-10-S1-S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gann, C. (2012). Premature birth endangers 15 M babies worldwide. ABC News. May 3. http://abcnews.go.com/blogs/health/2012/05/03/premature-birth-endangers-15m-babies-worldwide/.
- 9.March of Dimes, PMNCH, Save the Children, WHO. (2012). Born too soon: The global action report on preterm birth. In C. P. Howson, M. V. Kinney, J. E. Lawn, (Eds.), Written report. World Health Organization: Geneva. http://whqlibdoc.who.int/publications/2012/9789241503433_eng.pdf.
- 10.Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000. International Journal of Epidemiology. 2006;35(3):706–718. doi: 10.1093/ije/dyl043. [DOI] [PubMed] [Google Scholar]
- 11.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371(9606):75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Green NS, Damus K, Simpson JL, Iams J, Reece EA, Hobel CJ, et al. Research agenda for preterm birth: Recommendations from the March of Dimes. American Journal of Obstetrics and Gynecology. 2005;193(3 Pt 1):626–635. doi: 10.1016/j.ajog.2005.02.106. [DOI] [PubMed] [Google Scholar]
- 13.Latendresse G. The interaction between chronic stress and pregnancy: Preterm birth from a biobehavioral perspective. Journal of Midwifery & Women’s Health. 2009;54(1):8–17. doi: 10.1016/j.jmwh.2008.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rafati S, Borna H, Akhavirad M-B, Fallah N. Maternal determinants of giving birth to low-birth-weight neonates. Archives of Iranian Medicine. 2005;8(4):277–281. [Google Scholar]
- 15.Beck CT. The effects of postpartum depression on child development: A meta-analysis. Archives of Psychiatric Nursing. 1998;12(1):12–20. doi: 10.1016/S0883-9417(98)80004-6. [DOI] [PubMed] [Google Scholar]
- 16.Ganzel BL, Morris PA, Wethington E. Allostasis and the human brain: Integrating models of stress from the social and life sciences. Psychological Review. 2010;117(1):134–174. doi: 10.1037/a0017773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Archives of Women’s Mental Health. 2003;6(4):263–274. doi: 10.1007/s00737-003-0024-6. [DOI] [PubMed] [Google Scholar]
- 18.Howell BR, Sanchez MM. Understanding behavioral effects of early life stress using the reactive scope and allostatic load models. Development and Psychopathology. 2011;23(4):1001–1016. doi: 10.1017/S0954579411000460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huizink AC, Robles de Medina PG, Mulder EJ, Visser GH, Buitelaar JK. Stress during pregnancy is associated with developmental outcome in infancy. Journal of Child Psychology and Psychiatry. 2003;44(6):810–818. doi: 10.1111/1469-7610.00166. [DOI] [PubMed] [Google Scholar]
- 20.McEwen BS, Wingfield JC. The concept of allostasis in biology and biomedicine. Hormones and Behavior. 2003;43(1):2–15. doi: 10.1016/S0018-506X(02)00024-7. [DOI] [PubMed] [Google Scholar]
- 21.Monk C, Spicer J, Champagne F. Linking prenatal maternal adversity to developmental outcomes in infants: The role of epigenetic pathways. Development and Psychopathology. 2012;24(4):1361–1376. doi: 10.1017/S0954579412000764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen YH, Tsai SY, Lin HC. Increased mortality risk among offspring of mothers with postnatal depression: A nationwide population-based study in Taiwan. Psychological Medicine. 2011;41(11):2287–2296. doi: 10.1017/S0033291711000584. [DOI] [PubMed] [Google Scholar]
- 23.Grantham-McGregor S, Cheung YB, Cueto S, Glewwe P, Richter L, Strupp B, International Child Development Steering Group Developmental potential in the first 5 years for children in developing countries. Lancet. 2007;369(9555):60–70. doi: 10.1016/S0140-6736(07)60032-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rahman A, Lovel H, Bunn J, Iqbal Z, Harrington R. Mothers’ mental health and infant growth: A case–control study from Rawalpindi, Pakistan. Child: Care, Health and Development. 2004;30(1):21–27. doi: 10.1111/j.1365-2214.2004.00382.x. [DOI] [PubMed] [Google Scholar]
- 25.Adewuya AO, Fatoye FO, Ola BA, Ijaodola OR, Ibigbami SM. Sociodemographic and obstetric risk factors for postpartum depressive symptoms in Nigerian women. Journal of Psychiatric Practice. 2005;11(5):353–358. doi: 10.1097/00131746-200509000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Adewuya AO, Ola BO, Aloba OO, Mapayi BM, Okeniyi JA. Impact of postnatal depression on infants’ growth in Nigeria. Journal of Affective Disorders. 2008;108(1–2):191–193. doi: 10.1016/j.jad.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization. (2009). Maternal mental health and child health and development in resource-constrained settings. Report of a UNFPA/WHO international expert meeting: The interface between reproductive health and mental health, Hanoi, June 21–23, 2007. World Health Organization Document Production Services: Geneva. WHO/RHR/09.24. http://whqlibdoc.who.int/hq/2009/WHO_RHR_09.24_eng.pdf.
- 28.Black MM, Baqui AH, Zaman K, El Arifeen S, Black RE. Maternal depressive symptoms and infant growth in rural Bangladesh. American Journal of Clinical Nutrition. 2009;89(3):951S–957S. doi: 10.3945/ajcn.2008.26692E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R. Impact of maternal depression on infant nutritional status and illness: A cohort study. Archives of General Psychiatry. 2004;61(9):946–952. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- 30.Rahman A, Patel V, Maselko J, Kirkwood B. The neglected ‘m’ in MCH programmes—Why mental health of mothers is important for child nutrition. Tropical Medicine & International Health. 2008;13(4):579–583. doi: 10.1111/j.1365-3156.2008.02036.x. [DOI] [PubMed] [Google Scholar]
- 31.Rahman A, Bunn J, Lovel H, Creed F. Maternal depression increases infant risk of diarrhoeal illness: A cohort study. Archives of Disease in Childhood. 2007;92(1):24–28. doi: 10.1136/adc.2005.086579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cohen S in collaboration with the Psychosocial Working Group. (2013). Measures of psychological stress [Internet]. The Regents of the University of California: San Franscisco, CA [revised February 2000; cited 2013 June 2]. http://www.macses.ucsf.edu/research/psychosocial/stress.php.
- 33.Mayeux R. Biomarkers: Potential uses and limitations. NeuroRx. 2004;1(2):182–188. doi: 10.1602/neurorx.1.2.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shannon M, King TL, Kennedy HP. Allostasis: A theoretical framework for understanding and evaluating perinatal health outcomes. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2007;36(2):125–134. doi: 10.1111/j.1552-6909.2007.00126.x. [DOI] [PubMed] [Google Scholar]
- 35.Cicchetti D. Allostatic load. Development and Psychopathology. 2011;23(3):723–724. doi: 10.1017/S0954579411000277. [DOI] [PubMed] [Google Scholar]
- 36.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience and Biobehavioral Reviews. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 37.Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Archives of Women’s Mental Health. 2003;6(4):263–274. doi: 10.1007/s00737-003-0024-6. [DOI] [PubMed] [Google Scholar]
- 38.Dixon-Woods M, Cavers D, Agarwal S, Annandale E, Arthur A, Harvey J, et al. Conducting a critical interpretive synthesis of the literature on access to healthcare by vulnerable groups. BMC Medical Research Methodology. 2006;6:35. doi: 10.1186/1471-2288-6-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shaikh J, Premji S, Khowaja K, Tough S, Kazi A, Khowaja S. The relationship between prenatal stress, depression, cortisol and preterm birth: A review. Open Journal of Depression. 2013;2(3):24–31. doi: 10.4236/ojd.2013.23006. [DOI] [Google Scholar]
- 40.UNFPA and World Health Organization, Department of Mental Health and Substance Abuse. (2008). Maternal mental health and child health and development in low and middle income countries: Report of the meeting held in Geneva, Switzerland, 30 January–1 February, 2008. World Health Organization: Geneva. NLM classification: WS 105.5.F2. http://www.who.int/mental_health/prevention/suicide/mmh_jan08_meeting_report.pdf.
- 41.Dunkel Schetter C, Glynn LM. Stress in pregnancy: Empirical evidence and theoretical issues to guide interdisciplinary researchers. In: Contrada R, Baum A, editors. Handbook of stress. New York: Springer; 2011. pp. 321–343. [Google Scholar]
- 42.Dunkel Schetter C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Review of Psychology. 2011;62:531–558. doi: 10.1146/annurev.psych.031809.130727. [DOI] [PubMed] [Google Scholar]
- 43.Dole N, Savitz DA, Hertz-Picciotto I, Siega-Riz AM, McMahon MJ, Buekens P. Maternal stress and preterm birth. American Journal of Epidemiology. 2003;157(1):14–24. doi: 10.1093/aje/kwf176. [DOI] [PubMed] [Google Scholar]
- 44.Orr ST, James SA, Blackmore Prince C. Maternal prenatal depressive symptoms and spontaneous preterm births among African-American women in Baltimore, Maryland. American Journal of Epidemiology. 2002;156(9):797–802. doi: 10.1093/aje/kwf131. [DOI] [PubMed] [Google Scholar]
- 45.Goldenberg RL, Cliver SP, Mulvihill FX, Hickey CA, Hoffman HJ, Klerman LV, et al. Medical, psychosocial, and behavioral risk factors do not explain the increased risk for low birth weight among black women. American Journal of Obstetrics and Gynecology. 1996;175(5):1317–1324. doi: 10.1016/S0002-9378(96)70048-0. [DOI] [PubMed] [Google Scholar]
- 46.Dayan J, Creveuil C, Herlicoviez M, Herbel C, Baranger E, Savoye C, Thouin A. Role of anxiety and depression in the onset of spontaneous preterm labor. American Journal of Epidemiology. 2002;155(4):293–301. doi: 10.1093/aje/155.4.293. [DOI] [PubMed] [Google Scholar]
- 47.Andersson L, Sundstrom-Poromaa I, Wulff M, Astrom M, Bixo M. Neonatal outcome following maternal antenatal depression and anxiety: A population-based study. American Journal of Epidemiology. 2004;159(9):872–881. doi: 10.1093/aje/kwh122. [DOI] [PubMed] [Google Scholar]
- 48.Dominguez TP, Schetter CD, Mancuso R, Rini CM, Hobel C. Stress in African American pregnancies: Testing the roles of various stress concepts in prediction of birth outcomes. Annals of Behavioral Medicine. 2005;29(1):12–21. doi: 10.1207/s15324796abm2901_3. [DOI] [PubMed] [Google Scholar]
- 49.Glynn LM, Schetter CD, Hobel CJ, Sandman CA. Pattern of perceived stress and anxiety in pregnancy predicts preterm birth. Health Psychology. 2008;27(1):43–51. doi: 10.1037/0278-6133.27.1.43. [DOI] [PubMed] [Google Scholar]
- 50.Jesse DE, Seaver W, Wallace DC. Maternal psychosocial risks predict preterm birth in a group of women from Appalachia. Midwifery. 2003;19(3):191–202. doi: 10.1016/S0266-6138(03)00031-7. [DOI] [PubMed] [Google Scholar]
- 51.Misra DP, O’Campo P, Strobino D. Testing a sociomedical model for preterm delivery. Paediatric and Perinatal Epidemiology. 2001;5(2):110–122. doi: 10.1046/j.1365-3016.2001.00333.x. [DOI] [PubMed] [Google Scholar]
- 52.Engel SM, Berkowitz GS, Wolff MS, Yehuda R. Psychological trauma associated with the World Trade Center attacks and its effect on pregnancy outcome. Paediatric and Perinatal Epidemiology. 2005;19(5):334–341. doi: 10.1111/j.1365-3016.2005.00676.x. [DOI] [PubMed] [Google Scholar]
- 53.Rich-Edwards JW, Kleinman KP, Strong EF, Oken E, Gillman MW. Preterm delivery in Boston before and after September 11th, 2001. Epidemiology. 2005;16(3):323–327. doi: 10.1097/01.ede.0000158801.04494.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Xiong X, Harville EW, Mattison DR, Elkind-Hirsch K, Pridjian G, Buekens P. Exposure to Hurricane Katrina, post-traumatic stress disorder and birth outcomes. The American Journal of the Medical Sciences. 2008;336(2):111–115. doi: 10.1097/MAJ.0b013e318180f21c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shaikh K, Premji SS, Rose MS, Kazi A, Khowaja S, Tough S. The association between parity, infant gender, higher level of paternal education and preterm birth in Pakistan: A cohort study. BMC Pregnancy Childbirth. 2011;11:88. doi: 10.1186/1471-2393-11-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation–allostatic load and its health consequences. Archives of Internal Medicine. 1999;157(19):2259–2268. doi: 10.1001/archinte.1997.00440400111013. [DOI] [PubMed] [Google Scholar]
- 57.McEwen B, Nasveld P, Palmer M, Anderson R, (Centre for Military, Veterans’ Health) Allostatic Load: A review of the literature. Canberra: Department of Veterans’ Affairs; 2012. [Google Scholar]
- 58.McEwen BS. Protective and damaging effects of stress mediators: Central role of the brain. Dialogues in Clinical Neuroscience. 2006;8(4):367–381. doi: 10.31887/DCNS.2006.8.4/bmcewen. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Seeman TE, McEwen BS, Rowe JW, Singer BH. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proceedings of the National Academy of Sciences. 2001;98(8):4770–4775. doi: 10.1073/pnas.081072698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bellingrath S, Weigl T, Kudielka BM. Chronic work stress and exhaustion is associated with higher allostastic load in female school teachers. Stress. 2009;12(1):37–48. doi: 10.1080/10253890802042041. [DOI] [PubMed] [Google Scholar]
- 61.Badanes LS, Watamura SE, Hankin BL. Hypocortisolism as a potential marker of allostatic load in children: Associations with family risk and internalizing disorders. Development and Psychopathology. 2011;23(3):881–896. doi: 10.1017/S095457941100037X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Giurgescu C. Are maternal cortisol levels related to preterm birth? Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2009;38(4):377–390. doi: 10.1111/j.1552-6909.2009.01034.x. [DOI] [PubMed] [Google Scholar]
- 63.Wadhwa PD, Garite TJ, Porto M, Glynn L, Chicz-DeMet A, Dunkel-Schetter C, et al. Placental corticotropin-releasing hormone (CRH), spontaneous preterm birth, and fetal growth restriction: A prospective investigation. American Journal of Obstetrics and Gynecology. 2004;191(4):1063–1069. doi: 10.1016/j.ajog.2004.06.070. [DOI] [PubMed] [Google Scholar]
- 64.Beckie TM. A systematic review of allostatic load, health, and health disparities. Biological Research for Nursing. 2012;14(4):311–346. doi: 10.1177/1099800412455688. [DOI] [PubMed] [Google Scholar]
- 65.Lowe NK, Corwin EJ. Proposed biological linkages between obesity, stress, and inefficient uterine contractility during labor in humans. Medical Hypotheses. 2011;76(5):755–760. doi: 10.1016/j.mehy.2011.02.018. [DOI] [PubMed] [Google Scholar]
- 66.Ekhator CN, Ebomoyi MI. Blood glucose and serum lipid profiles during pregnancy. African Journal of Diabetes Medicine. 2012;20(1):16–19. [Google Scholar]
- 67.Vrijkotte TG, Krukziener N, Hutten BA, Vollebregt KC, van Eijsden M, Twickler MB. Maternal lipid profile during early pregnancy and pregnancy complications and outcomes: The ABCD study. Journal of Clinical Endocrinology and Metabolism. 2012;97(11):3917–3925. doi: 10.1210/jc.2012-1295. [DOI] [PubMed] [Google Scholar]
- 68.Wei SQ, Fraser W, Luo ZC. Inflammatory cytokines and spontaneous preterm birth in asymptomatic women: A systematic review. Obstetrics and Gynecology. 2010;116(2 Pt 1):393–401. doi: 10.1097/AOG.0b013e3181e6dbc0. [DOI] [PubMed] [Google Scholar]
- 69.Coussons-Read ME, Lobel M, Carey JC, Kreither MO, D’Anna K, Argys L, et al. The occurrence of preterm delivery is linked to pregnancy-specific distress and elevated inflammatory markers across gestation. Brain, Behavior, and Immunity. 2012;26(4):650–659. doi: 10.1016/j.bbi.2012.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Leitich H, Bodner-Adler B, Brunbauer M, Kaider A, Egarter C, Husslein P. Bacterial vaginosis as a risk factor for preterm delivery: A meta-analysis. American Journal of Obstetrics and Gynecology. 2003;189(1):139–147. doi: 10.1067/mob.2003.339. [DOI] [PubMed] [Google Scholar]
- 71.Gennaro S, Hennessy MD. Psychological and physiological stress: Impact on preterm birth. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2003;32(5):668–675. doi: 10.1177/0884217503257484. [DOI] [PubMed] [Google Scholar]
- 72.van den Berg JP, Westerbeek EA, Berbers GA, van Gageldonk PG, van der Klis FR, van Elburg RM. Transplacental transport of IgG antibodies specific for pertussis, diphtheria, tetanus, haemophilus influenzae type b, and Neisseria meningitidis serogroup C is lower in preterm compared with term infants. The Pediatric Infectious Disease Journal. 2010;29(9):801–805. doi: 10.1097/INF.0b013e3181dc4f77. [DOI] [PubMed] [Google Scholar]
- 73.Palmeira P, Quinello C, Silveira-Lessa AL, Zago CA, Carneiro-Sampaio M. IgG placental transfer in healthy and pathological pregnancies. Clinical and Developmental Immunology. 2012;2012:985646. doi: 10.1155/2012/985646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.de Weerth C, Buitelaar JK. Physiological stress reactivity in human pregnancy—A review. Neuroscience and Biobehavioral Reviews. 2005;29(2):295–312. doi: 10.1016/j.neubiorev.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 75.McCubbin JA, Lawson EJ, Cox S, Sherman JJ, Norton JA, Read JA. Prenatal maternal blood pressure response to stress predicts birth weight and gestational age: A preliminary study. American Journal of Obstetrics and Gynecology. 1996;175(3 Pt 1):706–712. doi: 10.1053/ob.1996.v175.a74286. [DOI] [PubMed] [Google Scholar]
- 76.Gomez de Ponce R, Gomez Ponce de Leon L, Coviello A, De Vito E. Vascular maternal reactivity and neonatal size in normal pregnancy. Hypertens Pregnancy. 2001;20(3):243–256. doi: 10.1081/PRG-100107827. [DOI] [PubMed] [Google Scholar]
- 77.Hatch M, Berkowitz G, Janevic T, Sloan R, Lapinski R, James T, et al. Race, cardiovascular reactivity, and preterm delivery among active-duty military women. Epidemiology. 2006;17(2):178–182. doi: 10.1097/01.ede.0000199528.28234.73. [DOI] [PubMed] [Google Scholar]
- 78.Hilmert, C. J., Dominquez, T. P., Schetter, C. D., Srinivas, S. K., Glynn, L. M., Hobel, C. J., et al. (2014). Lifetime racism and blood pressure changes during pregnancy: Implications for fetal growth. Health Psychology, 33(1), 43–51. [DOI] [PMC free article] [PubMed]
- 79.Zhang J, Villar J, Sun W, Merialdi M, Abdel-Aleem H, Mathai M, et al. Blood pressure dynamics during pregnancy and spontaneous preterm birth. Am J Obstet Gynecol. 2007;197(2):162.e1–162.e6. doi: 10.1016/j.ajog.2007.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Juster RP, Lupien S. A sex- and gender-based analysis of allostatic load and physical complaints. Gender Medicine. 2012;9(6):511–523. doi: 10.1016/j.genm.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 81.Hobel CJ, Dunkel-Schetter C, Roesch SC, Castro LC, Arora CP. Maternal plasma corticotropin-releasing hormone associated with stress at 20 weeks’ gestation in pregnancies ending in preterm delivery. American Journal of Obstetrics and Gynecology. 1999;180(1 Pt 3):S257–S263. doi: 10.1016/S0002-9378(99)70712-X. [DOI] [PubMed] [Google Scholar]
- 82.Erickson K, Thorsen P, Chrousos G, Grigoriadis DE, Khongsaly O, McGregor J, et al. Preterm birth: Associated neuroendocrine, medical, and behavioral risk factors. Journal of Clinical Endocrinology and Metabolism. 2001;86(6):2544–2552. doi: 10.1210/jcem.86.6.7607. [DOI] [PubMed] [Google Scholar]
- 83.Ruiz RJ, Fullerton J, Brown CE, Schoolfield J. Relationships of cortisol, perceived stress, genitourinary infections, and fetal fibronectin to gestational age at birth. Biological Research for Nursing. 2001;3(1):39–48. doi: 10.1177/109980040100300106. [DOI] [PubMed] [Google Scholar]
- 84.Mancuso RA, Schetter CD, Rini CM, Roesch SC, Hobel CJ. Maternal prenatal anxiety and corticotropin-releasing hormone associated with timing of delivery. Psychosomatic Medicine. 2004;66(5):762–769. doi: 10.1097/01.psy.0000138284.70670.d5. [DOI] [PubMed] [Google Scholar]
- 85.Pearce BD, Grove J, Bonney EA, Bliwise N, Dudley DJ, Schendel DE, et al. Interrelationship of cytokines, hypothalamic–pituitary–adrenal axis hormones, and psychosocial variables in the prediction of preterm birth. Gynecologic and Obstetric Investigation. 2010;70(1):40–46. doi: 10.1159/000284949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Shapiro GD, Fraser WD, Frasch MG, Séguin JR. Psychosocial stress in pregnancy and preterm birth: Associations and mechanisms. Journal of Perinatal Medicine. 2013;41(6):631–645. doi: 10.1515/jpm-2012-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Halbreich U. The association between pregnancy processes, preterm delivery, low birth weight, and postpartum depressions—The need for interdisciplinary integration. American Journal of Obstetrics and Gynecology. 2005;193(4):1312–1322. doi: 10.1016/j.ajog.2005.02.103. [DOI] [PubMed] [Google Scholar]
- 88.Young SL. Pica in pregnancy: New ideas about an old condition. Annual Review of Nutrition. 2010;30:403–422. doi: 10.1146/annurev.nutr.012809.104713. [DOI] [PubMed] [Google Scholar]
- 89.Hayes BA. From ‘postnatal depression’ to ‘perinatal anxiety and depression’: Key points of the National Perinatal Depression Plan for nurses and midwives in Australian primary health care settings. Contemporary Nurse. 2010;35(1):58–67. doi: 10.5172/conu.2010.35.1.058. [DOI] [PubMed] [Google Scholar]
- 90.Beck CT. Predictors of postpartum depression: An update. Nursing Research. 2001;50(5):275–285. doi: 10.1097/00006199-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 91.Feldman R, Eidelman AI. Neonatal state organization, neuromaturation, mother–infant interaction, and cognitive development in small-for-gestational-age premature infants. Pediatrics. 2006;118(3):e869–e878. doi: 10.1542/peds.2005-2040. [DOI] [PubMed] [Google Scholar]
- 92.Oehler JM, Hannan T, Catlett A. Maternal views of preterm infants’ responsiveness to social interaction. Neonatal network: NN. 1993;12(6):67–74. [PubMed] [Google Scholar]
- 93.Bugental DB, Happaney K. Predicting infant maltreatment in low-income families: The interactive effects of maternal attributions and child status at birth. Developmental Psychology. 2004;40(2):234–243. doi: 10.1037/0012-1649.40.2.234. [DOI] [PubMed] [Google Scholar]
- 94.Ross J, Hanlon C, Medhin G, Alem A, Tesfaye F, Worku B, et al. Perinatal mental distress and infant morbidity in Ethiopia: A cohort study. Archives of Disease in Childhood-Fetal and Neonatal Edition. 2011;96(1):F59–F64. doi: 10.1136/adc.2010.183327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Parsons CE, Young KS, Rochat TJ, Kringelbach ML, Stein A. Postnatal depression and its effects on child development: A review of evidence from low- and middle-income countries. British Medical Bulletin. 2012;101(1):57–79. doi: 10.1093/bmb/ldr047. [DOI] [PubMed] [Google Scholar]
- 96.Gulamani SS, Premji SS, Kanji Z, Azam SI. Preterm birth a risk factor for postpartum depression in Pakistani women. Open Journal of Depression. 2013;2(4):72–81. doi: 10.4236/ojd.2013.24013. [DOI] [Google Scholar]
- 97.Lindstrom B, Eriksson M. Salutogenesis. Journal of Epidemiology and Community Health. 2005;59(6):440–442. doi: 10.1136/jech.2005.034777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Benyamin M, Hadar S, Asher S. Culture-sensitive therapy and salutogenesis: Treating Israeli Bedouin of the Negev. International Review of Psychiatry. 2011;23(6):550–554. doi: 10.3109/09540261.2011.637904. [DOI] [PubMed] [Google Scholar]
- 99.Gikonyo C, Bejon P, Marsh V, Molyneux S. Taking social relationships seriously: Lessons learned from the informed consent practices of a vaccine trial on the Kenyan Coast. Social Science and Medicine. 2008;67(5):708–720. doi: 10.1016/j.socscimed.2008.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.World Medical Association. (2008). World Medical Association declaration of Helsinki: Ethical principles for medical research involving human subjects [Internet]. 59th WMA General Assembly Seoul, October 2008, pp. 1–5. http://www.wma.net/en/30publications/10policies/b3/index.html.
- 101.Saxena S, Lora A, Morris J, Berrino A, Esparza P, Barrett T, et al. Mental health services in 42 low- and middle-income countries: A WHO-AIMS cross national analysis. Psychiatric Services. 2011;62(2):123–125. doi: 10.1176/appi.ps.62.2.123. [DOI] [PubMed] [Google Scholar]
- 102.Marchetti E, Mazarin-Diop V, Chaumont J, Martellet L, Makadi MF, Viviani S, et al. Conducting vaccine clinical trials in sub-Saharan Africa: Operational challenges and lessons learned from the Meningitis Vaccine Project. Vaccine. 2012;30(48):6859–6863. doi: 10.1016/j.vaccine.2012.09.008. [DOI] [PubMed] [Google Scholar]
- 103.Lang TA, White NJ, Tran HT, Farrar JJ, Day NP, Fitzpatrick R, et al. Clinical research in resource-limited settings: Enhancing research capacity and working together to make trials less complicated. PLoS Neglected Tropical Diseases. 2010;4(6):e619. doi: 10.1371/journal.pntd.0000619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Mbuagbaw L, Thabane L, Ongolo-Zogo P, Lang T. The challenges and opportunities of conducting a clinical trial in a low resource setting: The case of the Cameroon mobile phone SMS (CAMPS) trial, an investigator initiated trial. Trials. 2011;12:145. doi: 10.1186/1745-6215-12-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Padayatchi N, Mac Kenzie WR, Hirsch-Moverman Y, Feng PJ, Villarino E, Saukkonen J, et al. Lessons from a randomised clinical trial for multidrug-resistant tuberculosis. The International Journal of Tuberculosis and Lung Disease. 2012;16(12):1582–1587. doi: 10.5588/ijtld.12.0315. [DOI] [PubMed] [Google Scholar]