Abstract
Background
Childhood mortality, particularly in the first 5 years of life, is a major global concern and the target of Millennium Development Goal 4. Although the majority of childhood deaths occur in Africa and Asia, these are also the regions where such deaths are least likely to be registered. The INDEPTH Network works to alleviate this problem by collating detailed individual data from defined Health and Demographic Surveillance sites. By registering deaths and carrying out verbal autopsies to determine cause of death across many such sites, using standardised methods, the Network seeks to generate population-based mortality statistics that are not otherwise available.
Objective
To present a description of cause-specific mortality rates and fractions over the first 15 years of life as documented by INDEPTH Network sites in sub-Saharan Africa and south-east Asia.
Design
All childhood deaths at INDEPTH sites are routinely registered and followed up with verbal autopsy (VA) interviews. For this study, VA archives were transformed into the WHO 2012 VA standard format and processed using the InterVA-4 model to assign cause of death. Routine surveillance data also provided person-time denominators for mortality rates. Cause-specific mortality rates and cause-specific mortality fractions are presented according to WHO 2012 VA cause groups for neonatal, infant, 1–4 year and 5–14 year age groups.
Results
A total of 28,751 childhood deaths were documented during 4,387,824 person-years over 18 sites. Infant mortality ranged from 11 to 78 per 1,000 live births, with under-5 mortality from 15 to 152 per 1,000 live births. Sites in Vietnam and Kenya accounted for the lowest and highest mortality rates reported.
Conclusions
Many children continue to die from relatively preventable causes, particularly in areas with high rates of malaria and HIV/AIDS. Neonatal mortality persists at relatively high, and perhaps sometimes under-documented, rates. External causes of death are a significant childhood problem in some settings.
Keywords: Childhood, Africa, Asia, mortality, INDEPTH Network, verbal autopsy, InterVA
Mortality in childhood, particularly in the first 5 years of life, has been a major global concern in recent years. Additional attention has been given to rates of all-cause mortality reduction within the framework of Millennium Development Goal 4 (1) and considerable successes are being achieved in various countries. At the same time, some components of child mortality, for example, deaths in the early days of life, are proving less transigent. Overall burdens of childhood mortality can only be clearly understood when causes of death are reliably attributed, and it has to be recognised that some causes may be more susceptible to reduction than others. At the same time, the mix of causes varies considerably between different settings, as well as between age groups.
Cause-specific childhood mortality in low- and middle-income countries is estimated from a range of sources, including the Child Epidemiology Reference Group (CHERG) (2), and the Global Burden of Disease study (3). However, the data underlying these estimates are often sparse and inconsistent, particularly when it comes to understanding mortality patterns on a population basis (4).
The INDEPTH Network Health and Demographic Surveillance Sites (HDSS) follow vital events within defined populations continuously, and so they provide a means for documenting mortality on a population-related basis (5). Furthermore, by undertaking standardised verbal autopsy (VA) enquiries to follow-up deaths, cause-specific mortality can be assessed within specific childhood age groups to see which cause groups account for substantial components of overall mortality (6).
Our aim in this paper is to describe childhood cause-specific mortality patterns on the basis of a dataset collected at 22 INDEPTH Network HDSSs across Africa and Asia (7). We have chosen here to take as ‘childhood’ the overall age range from birth to 15 years, to give a complete picture of mortality patterns up to adulthood, at the same time providing results separately for the neonatal period, infancy and the under-5 year age group. Although these INDEPTH sites are not constituted as a representative sample, they provide point estimates over a wide range of settings and time periods.
Methods
The overall INDEPTH dataset (8) from which these childhood mortality analyses are drawn is described in detail elsewhere (7). The Karonga, Malawi, site did not contribute VAs for childhood deaths, and the Purworejo, Indonesia; Farafenni, The Gambia; and Vadu, India, sites carried out verbal autopsies for less than half of the childhood deaths that occurred and/or did not report for the period 2006–2012. Therefore these sites are not considered further here. This leaves documentation on 28,751 deaths in 4,387,824 person-years of observation across 18 sites. VA interviews were successfully completed on 25,357 (88.2%) of the deaths that occurred. A summary of the detailed methods used in common for this series of multisite papers is shown in Box 1.
Age–sex–time standardisation
To avoid effects of differences and changes in age–sex structures of populations, mortality fractions and rates have been adjusted using the INDEPTH 2013 population standard (9). A weighting factor was calculated for each site, age group, sex and year category in relation to the standard for the corresponding age group and sex, and incorporated into the overall dataset. This is referred to in this paper as age–sex–time standardisation in the contexts where it is used.
Cause of death assignment
The InterVA-4 (version 4.02) probabilistic model was used for all the cause of death assignments in the overall dataset (10). InterVA-4 is fully compliant with the WHO 2012 Verbal Autopsy standard and generates causes of death categorised by ICD-10 groups (11). The data reported here were collected before the WHO 2012 VA standard was available, but were transformed into the WHO 2012 and InterVA-4 format to optimise cross-site standardisation in cause of death attribution. For a small proportion of deaths, VA interviews were not successfully completed; a few others contained inadequate information to arrive at a cause of death. InterVA-4 assigns causes of death (maximum 3) with associated likelihoods; thus cases for which likely causes did not total 100% were also assigned a residual indeterminate component. This served as a means of encapsulating uncertainty in cause of death at the individual level within the overall dataset, as well as accounting for 100% of every death.
Overall dataset
The overall public-domain dataset (8) thus contains between one and four records for each death, with the sum of likelihoods for each individual being unity. Each record includes a specific cause of death, its likelihood and its age–sex–time weighting.
Box 1. Summary of methodology based on the detailed description in the introductory paper (7).
In this context, all of these data are secondary datasets derived from primary data collected separately by each participating site. In all cases the primary data collection was covered by site-level ethical approvals relating to on-going health and demographic surveillance in those specific locations. No individual identity or household location data were included in the secondary data and no specific ethical approvals were required for these pooled analyses.
Results
Over the total of 28,751 deaths during 4,387,824 person-years of observation, 5,213 occurred in the neonatal period (first 28 days of life); 8,967 during the remainder of infancy (from one month up to the first birthday); 10,764 in the 1–4 year age group and 3,807 in the 5–14 year age group. All 18 sites reported mortality during at least part of the period 2006–2012, which comprised 68.8% of overall person-time observed; the period 2000–2005 accounted for a further 25.7%. The most natural way to analyse these longitudinal population data across sites is to calculate site-specific mortality rates per 1,000 person-years, shown in Table 1 by age group, period and site. In the sites that have longer-term data, there are some trends reflecting falling childhood mortality. There are also exceptions, however; at the Agincourt, South Africa site, there are clear indications of mortality rising in the middle period, when the HIV/AIDS epidemic was at its height. For the period 2006–12, the highest rates of neonatal mortality were observed in Asian sites, even though they recorded generally lower mortality rates than many African sites in subsequent age groups.
Table 1.
Childhood all-cause mortality rates per 1,000 person-years by age group and period for 18 INDEPTH HDSS sites
| Age group | 0–28 days | 1–11 months | 1–4 years | 5–14 years | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| Period | <2000 | 2000–05 | 2006–12 | <2000 | 2000–05 | 2006–12 | <2000 | 2000–05 | 2006–12 | <2000 | 2000–05 | 2006–12 |
| Bangladesh: Matlab | 389.8 | 357.6 | 11.8 | 10.6 | 3.2 | 2.3 | 0.8 | 0.6 | ||||
| Bangladesh: Bandarban | 171.0 | 28.6 | 1.9 | 1.0 | ||||||||
| Bangladesh: Chakaria | 458.0 | 16.6 | 4.0 | 1.0 | ||||||||
| Bangladesh: AMK | 444.7 | 326.8 | 11.9 | 8.0 | 3.4 | 2.7 | 0.8 | 0.6 | ||||
| Burkina Faso: Nouna | 101.2 | 142.2 | 92.9 | 39.3 | 42.5 | 24.4 | 29.8 | 19.2 | 12.7 | 6.0 | 2.6 | 1.6 |
| Burkina Faso: Ouagadougou | 136.4 | 20.8 | 7.8 | 1.4 | ||||||||
| Côte d'Ivoire: Taabo | 200.9 | 32.0 | 15.2 | 1.8 | ||||||||
| Ethiopia: Kilite-Awlaelo | 188.0 | 12.6 | 2.8 | 1.1 | ||||||||
| Ghana: Navrongo | 305.5 | 209.7 | 43.5 | 22.0 | 11.4 | 8.2 | 2.2 | 1.7 | ||||
| Ghana: Dodowa | 90.4 | 8.7 | 4.7 | 1.4 | ||||||||
| India: Ballabgarh | 280.0 | 24.4 | 4.0 | 0.8 | ||||||||
| Kenya: Kilifi | 160.0 | 9.6 | 2.5 | 0.8 | ||||||||
| Kenya: Kisumu | 302.6 | 243.0 | 111.7 | 74.2 | 31.7 | 22.8 | 2.7 | 2.4 | ||||
| Kenya: Nairobi | 373.3 | 319.8 | 58.0 | 49.8 | 8.4 | 6.4 | 2.1 | 1.1 | ||||
| Senegal: Niakhar | 210.6 | 126.9 | 31.2 | 16.8 | 20.5 | 9.9 | 3.2 | 1.5 | ||||
| South Africa: Agincourt | 81.0 | 119.7 | 154.7 | 13.5 | 30.3 | 30.9 | 4.4 | 7.0 | 5.3 | 0.7 | 1.0 | 1.3 |
| South Africa: Africa Centre | 151.1 | 53.0 | 49.5 | 27.6 | 8.9 | 4.7 | 1.7 | 1.2 | ||||
| Vietnam: FilaBavi | 123.3 | 3.0 | 1.0 | 0.4 | ||||||||
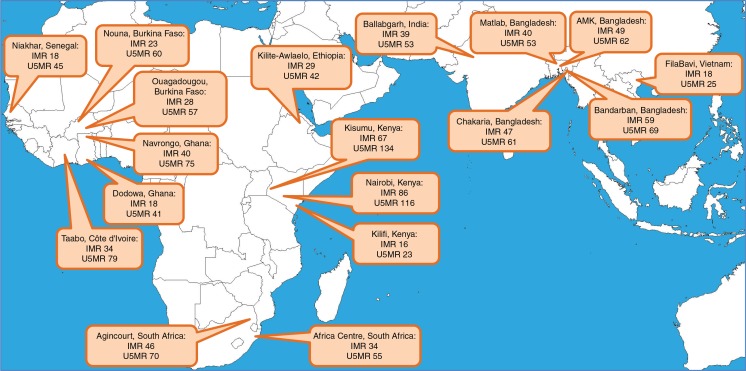
The terms ‘infant mortality rate’ and ‘under-5 mortality rate’ are frequently used, arguably incorrectly, to refer to numbers of deaths per 1,000 live births, rather than to person-time based rates. However, for the sake of comparability with other sources, Fig. 1 shows these widely used measures of infant and under-5 mortality rates per 1,000 live births for the period 2006–2012, during which all 18 sites reported. The FilaBavi site in Vietnam recorded infant mortality of 11 and under-5 mortality of 15 per 1,000 live births, while the Kisumu site on the northern shores of Lake Victoria recorded infant mortality of 78 and under-5 mortality of 152 per 1,000 live births.
Fig. 1.
Location of the 18 contributing INDEPTH HDSSs, showing infant mortality rates (deaths in first year of life per 1,000 live births, IMR) and under-5 mortality rates (deaths in first 5 years of life per 1,000 live births, U5MR) for the period 2006–2012.
Table 2 shows a detailed breakdown of cause-specific mortality rates per 1,000 person-years by site for major causes and cause groups of childhood mortality. More specific considerations of mortality due to malaria, HIV and external causes are given in accompanying papers (12–14) ; these causes are included here for the sake of completeness rather than for detailed discussion.
Table 2.
Childhood mortality rates per 1,000 person-years, by cause group and age group, for 18 INDEPTH HDSS sites from 2006 to 2012
| Cause | Birth asphyxia | Neonatal infections | Congenital | Prematurity | Diarrhoea | HIV/AIDS | Malaria | Pneumonia | Other infections | External causes | NCDs | Other causes | Indeterminate | All causes |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 0–28 days | ||||||||||||||
| Bangladesh: Matlab | 30.69 | 116.03 | 4.67 | 71.16 | 0.55 | 35.77 | 67.91 | 326.78 | ||||||
| Bangladesh: Bandarban | 38.20 | 73.43 | 22.58 | 36.83 | 171.04 | |||||||||
| Bangladesh: Chakaria | 104.36 | 42.35 | 1.97 | 105.09 | 1.79 | 73.27 | 129.14 | 457.97 | ||||||
| Bangladesh: AMK | 53.31 | 126.26 | 9.17 | 25.66 | 44.75 | 98.46 | 357.61 | |||||||
| Burkina Faso: Nouna | 18.91 | 44.89 | 0.63 | 5.10 | 2.42 | 20.93 | 92.88 | |||||||
| Burkina Faso: Ouagadougou | 18.42 | 49.15 | 7.80 | 16.90 | 5.83 | 38.33 | 136.43 | |||||||
| Côte d'Ivoire: Taabo | 53.32 | 80.20 | 20.39 | 15.25 | 31.75 | 200.91 | ||||||||
| Ethiopia: Kilite-Awlaelo | 11.56 | 79.00 | 4.00 | 22.12 | 71.32 | 188.00 | ||||||||
| Ghana: Navrongo | 52.57 | 43.80 | 0.95 | 57.14 | 32.36 | 22.91 | 209.73 | |||||||
| Ghana: Dodowa | 11.17 | 15.45 | 5.94 | 16.09 | 41.79 | 90.44 | ||||||||
| India: Ballabgarh | 32.37 | 68.05 | 2.18 | 77.48 | 28.55 | 71.38 | 280.01 | |||||||
| Kenya: Kilifi | 37.98 | 50.88 | 3.04 | 9.92 | 7.00 | 51.20 | 160.02 | |||||||
| Kenya: Kisumu | 52.66 | 65.56 | 2.46 | 9.61 | 0.49 | 27.37 | 84.88 | 243.03 | ||||||
| Kenya: Nairobi | 77.53 | 80.27 | 19.41 | 1.31 | 37.69 | 103.61 | 319.82 | |||||||
| Senegal: Niakhar | 5.83 | 51.38 | 1.10 | 6.48 | 13.01 | 49.11 | 126.91 | |||||||
| South Africa: Agincourt | 26.50 | 73.77 | 10.99 | 1.04 | 13.94 | 28.40 | 154.64 | |||||||
| South Africa: Africa Centre | 10.26 | 20.89 | 4.70 | 1.06 | 2.47 | 0.91 | 12.72 | 53.01 | ||||||
| Vietnam: FilaBavi | 31.56 | 38.58 | 2.36 | 50.74 | 123.24 | |||||||||
| 1–11 months | ||||||||||||||
| Bangladesh: Matlab | 0.03 | 0.30 | 0.04 | 4.85 | 0.92 | 0.19 | 0.19 | 0.86 | 0.62 | 8.00 | ||||
| Bangladesh: Bandarban | 1.61 | 1.03 | 0.85 | 8.15 | 0.42 | 0.77 | 0.36 | 15.40 | 28.59 | |||||
| Bangladesh: Chakaria | 1.39 | 1.55 | 0.07 | 0.08 | 3.46 | 1.86 | 0.76 | 0.59 | 0.38 | 6.44 | 16.58 | |||
| Bangladesh: AMK | 0.05 | 1.11 | 7.24 | 0.48 | 0.35 | 0.21 | 0.43 | 0.69 | 10.56 | |||||
| Burkina Faso: Nouna | 1.17 | 0.09 | 14.14 | 3.32 | 0.43 | 0.59 | 0.17 | 0.08 | 4.40 | 24.39 | ||||
| Burkina Faso: Ouagadougou | 0.64 | 1.72 | 1.80 | 3.03 | 6.66 | 0.92 | 0.15 | 0.68 | 0.62 | 4.64 | 20.86 | |||
| Côte d'Ivoire: Taabo | 0.96 | 1.84 | 2.79 | 5.83 | 8.13 | 2.01 | 0.78 | 0.62 | 9.04 | 32.00 | ||||
| Ethiopia: Kilite-Awlaelo | 0.31 | 0.65 | 0.32 | 6.14 | 0.09 | 0.09 | 5.00 | 12.60 | ||||||
| Ghana: Navrongo | 0.69 | 3.14 | 0.99 | 2.59 | 4.93 | 2.09 | 0.44 | 1.11 | 0.25 | 5.76 | 21.99 | |||
| Ghana: Dodowa | 0.51 | 0.39 | 0.36 | 3.47 | 0.23 | 0.15 | 0.16 | 0.35 | 3.12 | 8.74 | ||||
| India: Ballabgarh | 0.63 | 4.16 | 0.71 | 8.88 | 0.99 | 0.53 | 1.20 | 0.39 | 6.94 | 24.43 | ||||
| Kenya: Kilifi | 0.12 | 0.40 | 1.94 | 1.08 | 2.48 | 0.60 | 0.08 | 0.19 | 0.08 | 2.60 | 9.57 | |||
| Kenya: Kisumu | 0.34 | 6.55 | 7.54 | 17.99 | 25.49 | 2.74 | 0.49 | 1.70 | 0.44 | 10.96 | 74.24 | |||
| Kenya: Nairobi | 0.04 | 2.90 | 3.84 | 1.16 | 16.71 | 6.48 | 0.99 | 0.17 | 0.23 | 17.26 | 49.78 | |||
| Senegal: Niakhar | 6.10 | 0.10 | 1.86 | 2.03 | 0.55 | 0.06 | 0.86 | 5.21 | 16.77 | |||||
| South Africa: Agincourt | 0.23 | 3.32 | 4.42 | 0.75 | 12.90 | 2.79 | 0.26 | 0.55 | 0.21 | 5.47 | 30.90 | |||
| South Africa: Africa Centre | 0.29 | 1.87 | 3.97 | 0.26 | 15.96 | 0.59 | 0.22 | 0.24 | 0.49 | 3.65 | 27.54 | |||
| Vietnam: FilaBavi | 0.16 | 1.82 | 0.46 | 0.57 | 3.01 | |||||||||
| 1–4 years | ||||||||||||||
| Bangladesh: Matlab | 0.01 | 0.03 | 0.03 | 0.00 | 0.44 | 0.15 | 1.11 | 0.04 | 0.62 | 0.22 | 2.65 | |||
| Bangladesh: Bandarban | 0.17 | 0.17 | 0.16 | 0.17 | 0.35 | 0.29 | 0.59 | 1.90 | ||||||
| Bangladesh: Chakaria | 0.27 | 0.06 | 0.78 | 0.27 | 1.34 | 0.28 | 0.04 | 0.92 | 3.96 | |||||
| Bangladesh: AMK | 0.27 | 0.03 | 0.49 | 0.05 | 1.37 | 0.01 | 0.03 | 2.25 | ||||||
| Burkina Faso: Nouna | 0.98 | 0.12 | 6.91 | 1.46 | 0.16 | 0.28 | 0.10 | 0.08 | 2.64 | 12.73 | ||||
| Burkina Faso: Ouagadougou | 0.03 | 0.48 | 0.58 | 2.43 | 1.03 | 0.39 | 0.11 | 0.29 | 0.64 | 1.78 | 7.76 | |||
| Côte d'Ivoire: Taabo | 0.07 | 0.70 | 1.55 | 4.88 | 1.50 | 0.54 | 0.23 | 0.58 | 0.24 | 4.92 | 15.21 | |||
| Ethiopia: Kilite-Awlaelo | 0.15 | 0.22 | 0.17 | 0.30 | 0.12 | 0.11 | 0.22 | 0.06 | 1.49 | 2.84 | ||||
| Ghana: Navrongo | 0.05 | 0.74 | 0.76 | 2.08 | 0.53 | 0.46 | 0.44 | 0.83 | 0.24 | 2.04 | 8.17 | |||
| Ghana: Dodowa | 0.13 | 0.19 | 0.85 | 0.98 | 0.18 | 0.17 | 0.21 | 0.14 | 1.87 | 4.72 | ||||
| India: Ballabgarh | 0.03 | 0.72 | 0.05 | 0.59 | 0.61 | 0.07 | 0.42 | 0.12 | 0.06 | 1.30 | 3.97 | |||
| Kenya: Kilifi | 0.01 | 0.09 | 0.48 | 0.61 | 0.33 | 0.07 | 0.09 | 0.08 | 0.06 | 0.70 | 2.52 | |||
| Kenya: Kisumu | 1.26 | 5.18 | 7.61 | 2.46 | 0.60 | 0.41 | 0.75 | 0.71 | 3.82 | 22.80 | ||||
| Kenya: Nairobi | 0.35 | 1.04 | 0.22 | 0.95 | 1.18 | 0.37 | 0.04 | 0.10 | 2.18 | 6.43 | ||||
| Senegal: Niakhar | 2.94 | 0.24 | 3.45 | 0.38 | 0.15 | 0.72 | 0.05 | 1.96 | 9.89 | |||||
| South Africa: Agincourt | 0.02 | 0.34 | 1.88 | 0.28 | 1.07 | 0.43 | 0.17 | 0.23 | 0.15 | 0.78 | 5.35 | |||
| South Africa: Africa Centre | 0.07 | 0.10 | 1.25 | 0.12 | 1.46 | 0.25 | 0.39 | 0.06 | 0.13 | 0.88 | 4.71 | |||
| Vietnam: FilaBavi | 0.09 | 0.29 | 0.08 | 0.16 | 0.34 | 0.96 | ||||||||
| 5–14 years | ||||||||||||||
| Bangladesh: Matlab | 0.00 | 0.05 | 0.09 | 0.19 | 0.09 | 0.06 | 0.07 | 0.55 | ||||||
| Bangladesh: Bandarban | 0.07 | 0.18 | 0.07 | 0.07 | 0.15 | 0.10 | 0.06 | 0.33 | 1.03 | |||||
| Bangladesh: Chakaria | 0.03 | 0.04 | 0.15 | 0.34 | 0.17 | 0.02 | 0.25 | 1.00 | ||||||
| Bangladesh: AMK | 0.01 | 0.07 | 0.09 | 0.19 | 0.12 | 0.01 | 0.07 | 0.56 | ||||||
| Burkina Faso: Nouna | 0.02 | 0.60 | 0.14 | 0.07 | 0.11 | 0.20 | 0.49 | 1.63 | ||||||
| Burkina Faso: Ouagadougou | 0.09 | 0.35 | 0.16 | 0.10 | 0.13 | 0.05 | 0.06 | 0.41 | 1.35 | |||||
| Côte d'Ivoire: Taabo | 0.27 | 0.27 | 0.25 | 0.11 | 0.22 | 0.12 | 0.06 | 0.48 | 1.78 | |||||
| Ethiopia: Kilite-Awlaelo | 0.02 | 0.03 | 0.05 | 0.07 | 0.28 | 0.11 | 0.04 | 0.45 | 1.05 | |||||
| Ghana: Navrongo | 0.07 | 0.13 | 0.08 | 0.17 | 0.40 | 0.46 | 0.02 | 0.41 | 1.74 | |||||
| Ghana: Dodowa | 0.07 | 0.21 | 0.20 | 0.13 | 0.14 | 0.11 | 0.01 | 0.46 | 1.33 | |||||
| India: Ballabgarh | 0.01 | 0.05 | 0.01 | 0.09 | 0.22 | 0.10 | 0.01 | 0.35 | 0.84 | |||||
| Kenya: Kilifi | 0.20 | 0.12 | 0.07 | 0.06 | 0.13 | 0.05 | 0.00 | 0.15 | 0.78 | |||||
| Kenya: Kisumu | 0.44 | 0.59 | 0.30 | 0.18 | 0.14 | 0.23 | 0.04 | 0.47 | 2.39 | |||||
| Kenya: Nairobi | 0.11 | 0.05 | 0.05 | 0.24 | 0.15 | 0.16 | 0.00 | 0.31 | 1.07 | |||||
| Senegal: Niakhar | 0.16 | 0.30 | 0.08 | 0.12 | 0.30 | 0.01 | 0.53 | 1.50 | ||||||
| South Africa: Agincourt | 0.28 | 0.05 | 0.23 | 0.24 | 0.11 | 0.10 | 0.01 | 0.32 | 1.34 | |||||
| South Africa: Africa Centre | 0.16 | 0.01 | 0.07 | 0.41 | 0.25 | 0.15 | 0.01 | 0.16 | 1.22 | |||||
| Vietnam: FilaBavi | 0.07 | 0.04 | 0.25 | 0.36 |
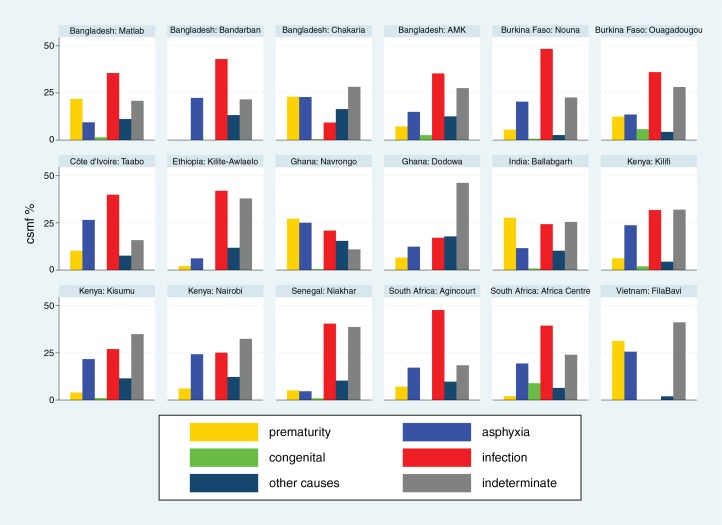
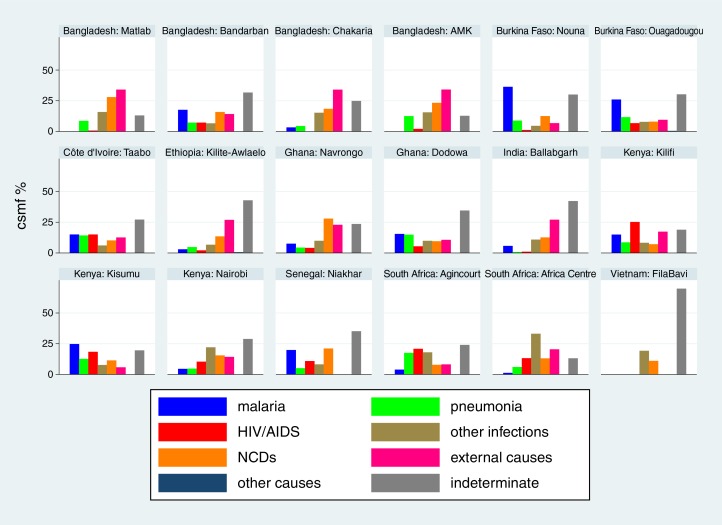
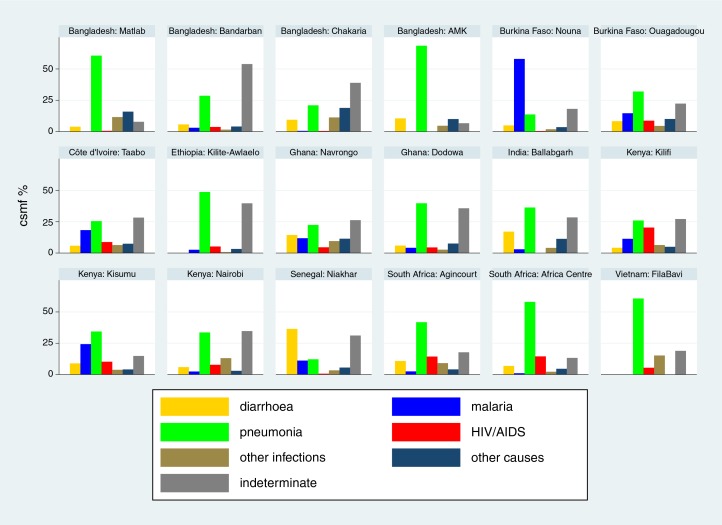
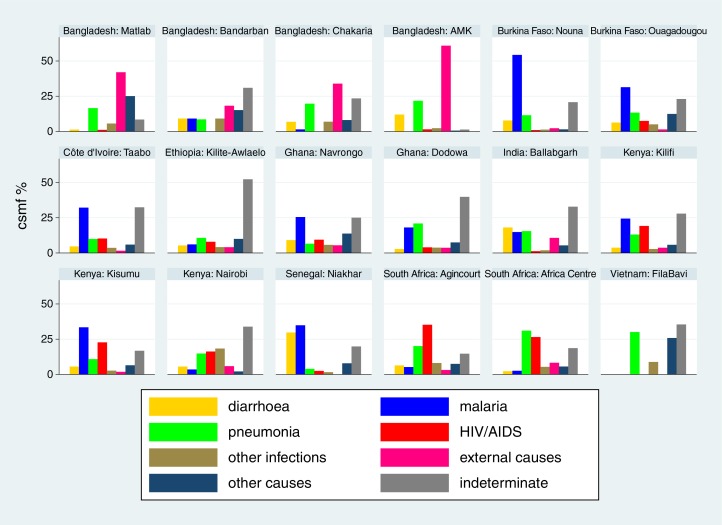
Cause-specific mortality fractions (CSMF) for each of the 18 sites (15–32) are shown separately for each age group (neonates, 1–11 months, 1–4 years and 5–14 years) in Figs. 2–5 respectively, to give a sense of what the dominant causes of mortality are in particular sites and age groups. For most sites, infections accounted for the largest proportion of neonatal deaths, although prematurity was also an important cause in some settings. Pneumonia dominated as the major cause of infant deaths, although malaria was also important in some endemic areas. Local factors dictated major causes in the 1–4 year age group, from external causes in Bangladesh to malaria and HIV/AIDS in highly endemic settings. For the 5–14 year age group, external causes and, in some places, malaria continued as important causes, while there was also an increased proportion of mortality due to non-communicable diseases in some sites.
Fig. 2.
Cause-specific mortality fractions (CSMF) for major cause of death groups for neonates at 18 INDEPTH sites during 2006–2012.
Fig. 5.
Cause-specific mortality fractions (CSMF) for major cause of death groups for children aged 5–14 years at 18 INDEPTH sites during 2006–2012.
Fig. 3.
Cause-specific mortality fractions (CSMF) for major cause of death groups for infants (1–11 months) at 18 INDEPTH sites during 2006–2012.
Discussion
This large-scale description of childhood mortality, all based on individually documented deaths within defined populations in Africa and Asia, provides important insights into the continuing causes of deaths that would be regarded as largely preventable in other parts of the world. Despite encouraging progress in reducing childhood mortality in many places, the data presented here reflect an overall situation from these sites in recent years where around 1 out of every 12 children born does not survive into adulthood.
The causes behind these individual tragedies are multifactorial, including poverty, living conditions and health services, and cannot be explored in full detail from the data presented here. What we do know from these cause of death data is that there are substantial differences in patterns of childhood mortality between countries, and in some cases, such as Kenya, also widespread within-country variation. Certain infectious diseases, particularly malaria and HIV/AIDS, contribute major components of childhood mortality in settings where they occur commonly, and hence account for a substantial part of variation in overall mortality. For example, at the Kisumu, Kenya, site malaria and HIV/AIDS together accounted for 56% of deaths in the 1–4 year age group; but other causes did not occur at rates that were markedly different from those in a number of other sites. Conversely, at the FilaBavi, Vietnam site, where overall mortality in the 1–4 year age group was less than 10% of the level observed in Kisumu, pneumonia accounted for 29% of the relatively few deaths that did occur. Similarly, it is very obvious from Fig. 4 that external causes of death are a major problem in Bangladesh. This illustrates the importance of considering both population-based cause-specific mortality rates and CSMF when coming to any understanding of significant causes of mortality burdens within particular populations. Both parameters are essential information to have when considering interventions, either for specific diseases or for health promotion in general.
Fig. 4.
Cause-specific mortality fractions (CSMF) for major cause of death groups for children aged 1–4 years at 18 INDEPTH sites during 2006–2012.
One of the strengths of maintaining surveillance of all deaths within particular populations, as the INDEPTH HDSS sites do, is that by definition the results for each particular cause constitute a clear component of 100% total mortality. By contrast, when deaths due to particular causes are documented at health facilities, or in vertical disease-oriented programmes, denominators are always unclear. In addition, the InterVA-4 methodology that was used in this dataset captures the uncertainty around cause of death assignment at the individual level, which is presented here as part of the ‘indeterminate’ category. Although some studies have sought to reclassify so-called ‘garbage’ cause of death codes into more specific groupings (33), in reality the assignment of cause of death at the individual level is not something that can proceed with total certainty for every case, irrespective of the methods used, and this may be particularly true for some childhood deaths. We contend therefore that maintaining an ‘indeterminate’ category that encompasses uncertainty in individual cause of death assignments, as well as accounting for a minority of deaths for which a VA interview was for some reason not possible, is an important and realistic concept in these population-based analyses (34). Whether or not the ‘indeterminate’ group actually constitutes a similar mix of causes of death as those that are successfully assigned has to remain a matter for conjecture.
Because childhood mortality globally is reported as falling, we have concentrated our analyses here on data from the 2006 to 2012 period to reflect a relatively contemporary scenario. A detailed comparative study by country, age group and cause of death between these results and other findings on cause-specific child mortality is beyond the scope of this paper. However, some selected comparisons can be made. The GBD2010 global estimates of child mortality (35) are approximately contemporaneous with the 2006–12 time period presented here, as are the 2010 mortality estimates presented by UNICEF in the State of the World's Children 2012 (36). The basic rates of all-cause childhood mortality are reasonably congruent between these sources and the findings from the INDEPTH sites, although this is by no means a precise comparison (specific population site measurements versus national estimates). The perennial concern that some early neonatal deaths may have been considered as stillbirths (37), and therefore not registered as deaths, may have been an issue at some of the INDEPTH sites in Africa that registered fairly low neonatal mortality rates in comparison to infant mortality. More systematic application of the WHO 2012 VA tool (11) in the future may help to resolve this, since it contains a number of questions specifically aimed at making this distinction. Operationally, it is probably important to consider undertaking a VA interview for all third trimester pregnancies that do not result in a live baby, rather than making a priori distinctions between stillbirths and early neonatal deaths, in order to capture all available information. Local cultural and spiritual beliefs around the deaths of babies may also be an important consideration.
Conclusions
Individual deaths in childhood are always causes for great sadness; all the more so if the circumstances and the eventual cause of death mean that survival could have been reasonably possible. These analyses of individual deaths show that large numbers of children in Africa and Asia continue to die of avoidable causes, starting from suboptimal delivery care, through treatable infections and preventable accidents. Despite some countries achieving MDG4 targets, there is still room for further improvement. Documenting the magnitude of the various leading causes of childhood death, across relevant age groups, is a pre-requisite for planning effective survival interventions.
Acknowledgements
We are grateful to all the residents of INDEPTH HDSS sites who have contributed personal information to this mortality dataset, and to the field staff who undertook so many verbal autopsy interviews and data management staff who handled the data at every participating site. INDEPTH acknowledges all the site scientists who have participated in bringing this work together, and who variously participated in analysis workshops in Ghana, Belgium, Thailand and the United Kingdom. The INDEPTH Network is grateful for core funding from Sida, the Wellcome Trust, and the William & Flora Hewlett Foundation. The Umeå Centre for Global Health Research is core funded by Forte, the Swedish Research Council for Health, Working Life and Welfare (grant 2006-1512). PB's residency at the University of the Witwatersrand Rural Knowledge Hub to analyse and draft these results was supported by the European Community Marie Curie Actions IPHTRE project (no. 295168). icddr,b is thankful to the Governments of Australia, Bangladesh, Canada, Sweden and the UK for providing core/unrestricted support. The Ouagadougou site acknowledges the Wellcome Trust for its financial support to the Ouagadougou HDSS (grant number WT081993MA). The Kilite Awlaelo HDSS is supported by the US Centers for Disease Control and Prevention (CDC) and the Ethiopian Public Health Association (EPHA), in accordance with the EPHA-CDC Cooperative Agreement No.5U22/PS022179_10 and Mekelle University, though these findings do not necessarily represent the funders' official views. The Kilifi site is supported through core support to the KEMRI-Wellcome Trust Major Overseas Programme from the Wellcome Trust. TNW is supported by a Senior Fellowship (091758) and CN through a Strategic Award (084538) from the Wellcome Trust. This paper is published with permission from the Director of KEMRI. The Kisumu site wishes to acknowledge the contribution of the late Dr. Kubaje Adazu to the development of KEMRI/CDC HDSS, which was implemented and continues to be supported through a cooperative agreement between KEMRI and CDC. The Nairobi Urban Health and Demographic Surveillance System (NUHDSS), Kenya, since its inception has received support from the Rockefeller Foundation (USA), the Wellcome Trust (UK), the William and Flora Hewlett Foundation (USA), Comic Relief (UK), the Swedish International Development Cooperation Agency (SIDA) and the Bill and Melinda Gates Foundation (USA). The Agincourt site acknowledges that the School of Public Health and Faculty of Health Sciences, University of the Witwatersrand, and the Medical Research Council, South Africa, have provided vital support since inception of the Agincourt HDSS. Core funding has been provided by the Wellcome Trust, UK (Grants 058893/Z/99/A; 069683/Z/02/Z; 085477/Z/08/Z) with contributions from the National Institute on Aging (NIA) of the NIH, William and Flora Hewlett Foundation, and Andrew W Mellon Foundation, USA.
This paper is part of the Special Issue: INDEPTH Network Cause-Specific Mortality. More papers from this issue can be found at http://www.globalhealthaction.net
Footnotes
Authors are listed arbitrarily in order of their site code, and alphabetically within each site.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Wang H, Liddell CA, Coates MM, Mooney MD, Levitz CE, Schumacher AE, et al. Global, regional and national levels of neonatal, infant, and under-5 mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:957–79. doi: 10.1016/S0140-6736(14)60497-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, et al. Global, regional and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet. 2012;379:2151–61. doi: 10.1016/S0140-6736(12)60560-1. [DOI] [PubMed] [Google Scholar]
- 3.Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2095–128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Byass P, de Courten M, Graham WJ, Laflamme L, McCaw-Binns A, Sankoh OA, et al. Reflections on the Global Burden of Disease 2010 Estimates. PLoS Med. 2013;10:e1001477. doi: 10.1371/journal.pmed.1001477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sankoh O, Byass P. The INDEPTH Network: filling vital gaps in global epidemiology. Int J Epidemiol. 2012;41:579–88. doi: 10.1093/ije/dys081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Leitao J, Chandramohan D, Byass P, Jakob R, Bundhamcharoen K, Choprapawon C, et al. Revising the WHO verbal autopsy instrument to facilitate routine cause-of-death monitoring. Glob Health Action. 2013;6 doi: 10.3402/gha.v6i0.21518. 21518, http://dx.doi.org/10.3402/gha.v6i0.21518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Streatfield PK, Khan WA, Bhuiya A, Alam N, Sié A, Soura AB, et al. Cause-specific mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.25362. 25362, http://dx.doi.org/10.3402/gha.v7.25362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.INDEPTH Network INDEPTH Network Cause-Specific Mortality – Release 2014. Oct 2014. Provided by the INDEPTH Network Data Repository. www.indepth-network.org.
- 9.Sankoh O, Sharrow D, Herbst K, Kabudula CW, Alam N, Kant S, et al. The INDEPTH standard population for low- and middle-income countries, 2013. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.23286. 23286, http://dx.doi.org/10.3402/gha.v7.23286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byass P, Chandramohan D, Clark SJ, D'Ambruoso L, Fottrell E, Graham WJ, et al. Strengthening standardised interpretation of verbal autopsy data: the new InterVA-4 tool. Glob Health Action. 2012;5 doi: 10.3402/gha.v5i0.19281. 19281, http://dx.doi.org/10.3402/gha.v5i0.19281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Verbal autopsy standards: the 2012 WHO verbal autopsy instrument. Geneva: WHO; 2012. [Google Scholar]
- 12.Streatfield PK, Khan WA, Bhuiya A, Hanifi SMA, Alam N, Diboulo E, et al. Malaria mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.25369. 25369, http://dx.doi.org/10.3402/gha.v7.25369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Streatfield PK, Khan WA, Bhuiya A, Hanifi SMA, Alam N, Millogo O, et al. HIV/AIDS-related mortality in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.25370. 25370, http://dx.doi.org/10.3402/gha.v7.25370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Streatfield PK, Khan WA, Bhuiya A, Hanifi SMA, Alam N, Diboulo E, et al. Mortality from external causes in Africa and Asia: evidence from INDEPTH Health and Demographic Surveillance System sites. Glob Health Action. 2014;7 doi: 10.3402/gha.v7.25366. 25366, http://dx.doi.org/10.3402/gha.v7.25366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Razzaque A, Nahar L, Akter Khanam M, Streatfield PK. Socio-demographic differentials of adult health indicators in Matlab, Bangladesh: self-rated health, health state, quality of life and disability level. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.4618. 4618, http://dx.doi.org/10.3402/gha.v3i0.4618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.INDEPTH Network. Bandarban HDSS. Available from: http://www.indepth-network.org/Profiles/Bandarban HDSS.pdf.
- 17.Hanifi MA, Mamun AA, Paul A, Hasan SA, Hoque S, Sharmin S, et al. Profile: the Chakaria Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:667–75. doi: 10.1093/ije/dys089. [DOI] [PubMed] [Google Scholar]
- 18.Lindeboom W, Das SC, Ashraf A. Dhaka, Bangladesh: ICDDR,B; 2011. Health and Demographic Surveillance Report 2009 – Abhoynagar and Mirsarai. [Google Scholar]
- 19.Sié A, Louis VR, Gbangou A, Müller O, Niamba L, Stieglbauer G. The Health and Demographic Surveillance System (HDSS) in Nouna, Burkina Faso, 1993–2007. Glob Health Action. 2010;3 doi: 10.3402/gha.v3i0.5284. 5284, http://dx.doi.org/10.3402/gha.v3i0.5284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rossier C, Soura A, Baya B, Compaoré G, Dabiré B, Dos Santos S, et al. Profile: the Ouagadougou Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:658–66. doi: 10.1093/ije/dys090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kouadio MK, Righetti AA, Abé NN, Wegmüller R, Weiss MG, N'goran EK, et al. Local concepts of anemia-related illnesses and public health implications in the Taabo health demographic surveillance system, Côte d'Ivoire. BMC Hematol. 2013;13:5. doi: 10.1186/2052-1839-13-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Weldearegawi B, Ashebir Y, Gebeye E, Gebregziabiher T, Yohannes M, Mussa S, et al. Emerging chronic non-communicable diseases in rural communities of Northern Ethiopia: evidence using population-based verbal autopsy method in Kilite Awlaelo surveillance site. Health Policy Plan. 2013;28:891–8. doi: 10.1093/heapol/czs135. [DOI] [PubMed] [Google Scholar]
- 23.Oduro AR, Wak G, Azongo D, Debpuur C, Wontuo P, Kondayire F, et al. Profile: the Navrongo Health and Demographic Surveillance System. Int J Epidemiol. 2012;41:968–76. doi: 10.1093/ije/dys111. [DOI] [PubMed] [Google Scholar]
- 24.Gyapong M, Sarpong D, Awini E, Manyeh AK, Tei D, Odonkor G, et al. Profile: the Dodowa Health and Demographic Surveillance System. Int J Epidemiol. 2013;42:1686–96. doi: 10.1093/ije/dyt197. [DOI] [PubMed] [Google Scholar]
- 25.Kant S, Misra P, Gupta S, Goswami K, Krishnan A, Nongkynrih B, et al. Profile: the Ballabgarh Health and Demographic Surveillance System (CRHSP-AIIMS) Int J Epidemiol. 2013;42:37–644. doi: 10.1093/ije/dyt055. [DOI] [PubMed] [Google Scholar]
- 26.Scott JA, Bauni E, Moisi JC, Ojal J, Gatakaa H, Nyundo C, et al. Profile: The Kilifi Health and Demographic Surveillance System (KHDSS) Int J Epidemiol. 2012;41:650–7. doi: 10.1093/ije/dys062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Odhiambo FO, Laserson KF, Sewe M, Hamel MJ, Feikin DR, Adazu K, et al. Profile: the KEMRI/CDC Health and Demographic Surveillance System – Western Kenya. Int J Epidemiol. 2012;41:977–87. doi: 10.1093/ije/dys108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oti SO, Mutua M, Mgomella GS, Egondi T, Ezeh A, Kyobutungi C. HIV mortality in urban slums of Nairobi, Kenya 2003–2010: a period effect analysis. BMC Public Health. 2013;13:588. doi: 10.1186/1471-2458-13-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Delaunay V, Douillot L, Diallo A, Dione D, Trape JF, Medianikov O, et al. Profile: the Niakhar Health and Demographic Surveillance System. Int J Epidemiol. 2013;42:1002–11. doi: 10.1093/ije/dyt100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kahn K, Collinson MA, Gómez-Olivé FX, Mokoena O, Twine R, Mee P, et al. Profile: Agincourt health and socio-demographic surveillance system. Int J Epidemiol. 2012;41:988–1001. doi: 10.1093/ije/dys115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herbst AJ, Mafojane T, Newell ML. Verbal autopsy-based cause-specific mortality trends in rural KwaZulu-Natal, South Africa, 2000–2009. Popul Health Metr. 2011;9:47. doi: 10.1186/1478-7954-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huong DL, Minh HV, Vos T, Janlert U, Van DD, Byass P. Burden of premature mortality in rural Vietnam from 1999–2003: analyses from a Demographic Surveillance Site. Popul Health Metr. 2006;4:9. doi: 10.1186/1478-7954-4-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Naghavi M, Makela S, Foreman K, O'Brien J, Pourmalek F, Lozano R. Algorithms for enhancing public health utility of national causes-of-death data. Popul Health Metr. 2010;8:9. doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Byass P. The democratic fallacy in matters of clinical opinion: implications for analysing cause-of-death data. Emerg Themes Epidemiol. 2011;8:1. doi: 10.1186/1742-7622-8-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Global Burden of Disease Study. Data downloads: GBD 2010 mortality results 1970–2010. 2010. Available from: http://ghdx.healthdata.org/global-burden-disease-study-2010-gbd-2010-data-downloads [cited 16 June 2014].
- 36.UNICEF. State of the World's Children 2012: children in an urban world. New York: UNICEF; 2012. [Google Scholar]
- 37.Lawn J, Shibuya K, Stein C. No cry at birth: global estimates of intrapartum stillbirths and intrapartum-related neonatal deaths. Bull World Health Organ. 2005;83:409–17. [PMC free article] [PubMed] [Google Scholar]