Abstract
Background
To reduce the cardiovascular disease burden, Healthy People 2020 established U.S. hypertension goals for adults to: (1) decrease prevalence to 26.9%. (2) raise treatment to 69.5% and control to 61.2%, which requires controlling 88.1% on treatment.
Methods and Results
To assess current status and progress toward these Healthy People 2020 goals, time trends in National Health and Nutrition Examination Surveys 1999–2012 data in twoyear blocks were assessed in adults ≥18 years old age-adjusted to U.S. 2010. From 1999–2000 to 2011–2012, prevalent hypertension was unchanged (30.1% vs. 30.8%, p=0.32). Hypertension treatment (59.8% vs. 74.7%, p<0.001) and proportion of treated adults controlled (53.3% to 68.9%, p=0.0015) increased. Hypertension control to <140/<90 mmHg rose every two years from 1999–2000 to 2009–2010 (32.2% vs. 53.8%, p<0.001) before declining to 51.2% in 2011–2012. Modifiable factor(s) significant in multivariable logistic regression modeling include: (a) increasing body mass index with prevalent hypertension (odds ratio [OR] 1.44). (b) lack of health insurance (OR 1.68) and <2 healthcare visits/year (OR 4.24) with untreated hypertension. (c) healthcare insurance (OR 1.69), ≥2 healthcare visits/year (OR 3.23) and cholesterol treatment (OR 1.90) with controlled hypertension.
Conclusions
The NHANES 1999–2012 analysis suggests that Healthy People 2020 goals for hypertension: (1) prevalence show no progress (2) treatment was exceeded (3) control has flattened below target. Findings are consistent with evidence that: (a) obesity prevention and treatment could reduce prevalent hypertension (b) healthcare insurance, ≥2 healthcare visits/year, and guideline-based cholesterol treatment could improve hypertension control.
Keywords: hypertension, Healthy People 2020, NHANES, population health
Introduction
Hypertension is a major contributor to death and disability from heart and vascular diseases. The estimated number of years of life lost to hypertension-related diseases in 2010 included: ischemic heart disease 7.2 million; stroke 1.9 million; chronic kidney disease, other cardiovascular and circulatory, and hypertensive heart disease 2.2 million combined.1 Treatment and control of hypertension reduce fatal and non-fatal cardiovascular events, especially when combined with effective hypercholesterolemia management.2 Million Hearts estimated that 1,000,000 cardiovascular events could be prevented in the U.S. in a five-year period from 2013–2017, with hypertension control a featured component of the success plan.3
U.S. Healthy People provides evidence-based, 10-year national objectives for pursuing its vision of a society in which all people live long, healthy lives.4 Healthy People 2010 aimed to reduce prevalent hypertension in adults to 16% and raise control to 50%.4 The 2010 control goal was met in 2007–2008 with an estimated 50.1% of all adults with hypertension attaining blood pressure <140/<90.5 However, the goal of reducing prevalent hypertension to 16% was not attained as 29.5% of adults in 2009–2010 either reported taking medication to lower blood pressure or had blood pressure ≥140/≥90 mm Hg.6
Healthy People 2020 established goals for: (1) decreasing prevalent hypertension to 26.9%, based on a 10% relative decrease from 29.9% in 2005–2008 (2) treating 69.5% of all adults with hypertension, which reflects a 10% improvement from 63.2% in 2005–2008 (3) controlling 61.2% of all adults with hypertension based on projected trends.7 The goals of treating 69.5% and controlling 61.2% of all adults with hypertension will require that 88% of treated adults attain control. While Kaiser Permanente in Northern California, a large managed healthcare system, controlled 87.1% of treated adults with hypertension in 2011,8 attaining this level of success in all adults could prove challenging. Many clinical settings, e.g., federally qualified health centers and rural clinics, have fewer resources and supports for quality improvement and provide care for a larger proportions of adults, including the uninsured, who typically have less favorable outcomes than Kaiser.9,10
This analysis of National Health and Nutrition Examination Survey 1999–2012 data was conducted to better understand trends and key variables impacting Healthy People 2020 goals for hypertension prevalence, treatment and control. More specifically, current status and trends in hypertension awareness, treatment, and control were assessed and modifiable factors that could facilitate progress toward Healthy People 2020 goals were identified.
Methods
The National Health and Nutrition Examination Surveys (NHANES) assess health and nutritional status of the U.S. civilian non-institutionalized population. Participants are selected using a multistage, probability sampling design. All adults provided written consent approved by the National Center for Health Statistics.
Participants included adults ≥18 years old in NHANES 1999–2012 with at least one recorded blood pressure (BP).
Race/Ethnicity was determined by self-report and separated into non-Hispanic white (white), non-Hispanic black (black), Hispanic ethnicity, and other.
Blood pressure (BP) was measured by trained professionals using sphygmomanometry and appropriately sized arm cuffs in volunteers after five minutes seated rest. The first BP was excluded in estimating mean systolic and diastolic values for individuals with more than one value as recommended in NHANES physician examination procedures manuals.11-17
Hypertension was defined by: systolic BP ≥140 and/or diastolic BP ≥90 mmHg and/or positive response to “Are you currently taking prescribed medication to lower your BP?”
Awareness of hypertension was defined by the percentage of adults with prevalent hypertension reporting a physician told them they had hypertension.
Treatment of hypertension was defined by the percentage of adults with prevalent hypertension reporting that they were taking prescription medication to lower BP.
Percentage of treated hypertension controlled was calculated as the number of adults on BP medications with values <140/<90 mmHg divided by the number of treated adults.
Hypertension control was defined as BP <140/<90 mmHg in all adults with hypertension including those with diabetes mellitus and chronic kidney disease.18
Diabetes included:19 (a) Diagnosed diabetes defined by positive response(s) to one or more questions, “Have you ever been told by a doctor that you have diabetes?”, “Are you now taking insulin?”, or “Are you now taking diabetic pills to lower your blood sugar?” (b) Undiagnosed diabetes defined by fasting glucose ≥126 mg/dL and/or glycosylated hemoglobin (HbA1c) ≥6.5%.
Hypercholesterolemia was defined by non-HDL-cholesterol relative to Framingham 10-year coronary heart disease risk as previously described.2 Non-HDL-cholesterol was used, since LDL-cholesterol values were missing on more than half of subjects and participants with and without values were different.
Hypercholesterolemia Treatment was determined by adults answering affirmatively to “Are you taking prescribed medication to lower your cholesterol?”
Chronic kidney disease (CKD) was defined as estimated glomerular filtration rate (eGFR) <60 mL/1.73 m2/min and/or urine albumin:creatinine ≥300 mg/g, i.e., values previously selected to define a lower blood pressure target than <140/<90 mmHg.20 Serum creatinine values were adjusted to account for methodological differences across surveys.21
Cardiovascular disease included: (i) coronary heart disease (CHD) defined by positive response to three questions listed previously.18 (ii) Stroke was defined by endorsement of “Has a doctor ever told you that you had a stroke?”22 (iii) Congestive heart failure was defined by affirmative response to “Has a doctor ever told you that you had congestive heart failure?”
Medical visits were defined in response to “How many times did 3you receive health care over the last year”? Answers were dichotomized into <2 vs. ≥2 visits annually.2,18
Cigarette smoker was defined if a patient answered “Every day” or “some days” to “Do you now smoke cigarettes?”2
Data analysis. SAS version 9.4 (Cary, NC) survey procedures were used for within survey analyses and appropriate weights accounting for unequal probabilities of selection, oversampling, and nonresponse were used. NHANES reporting guidelines were followed. The clinical epidemiology of hypertension was age-adjusted to the U.S. 2010 Census. In 2010, the proportion of adults aged 18 to 44 years, 45 to 64 years, and ≥65 years was 0.481, 0.348, and 0.171.23 For age-adjusting hypertension awareness, treatment, and control across time, additional weights were calculated, since prevalent hypertension varies by age group. The proportion of adults in each age group that were hypertensive was multiplied by their respective year 2010 weight for all adults. Weights were then calculated by dividing the product for each age group by the sum of products for all three age groups in each survey.5 P-values <0.05 were accepted as statistically significant. . Multiple comparisons with Bonferroni adjustment (pairwise significance level=0.05/3) were applied to assess within and between group differences. PROC SURVEYLOGISTIC was used to assess association between clinical variables and BP control. For within survey between group comparisons at each of the three NHANES time period, Rao-Scott Chi-Square Tests were used to assess differences in distributions of categorical variables and Wald F-tests for differences in continuous variables. Pairwise comparisons between the three NHANES periods were conducted with t-tests of weighted means. Odds ratios and 95% confidence intervals were calculated and statistical significance assumed when 95% confidence intervals do not cross the line of identity (1.0).
Results
The process for identifying 12,262 adults with hypertension in NHANES 1999–2012 is depicted in Figure 1. Across time, adults with hypertension did not differ significantly by age, sex, race, healthcare insurance, or prevalent hypercholesterolemia, CVD, CKD or 10-yr CHD risk <10% (Table 1). The percentage of adults with infrequent healthcare (0–1 visits/year) declined between 1999–2004 and 2009–2012. BMI and prevalent obesity were greater in 2005–2008 and 2009–2012, than 1999–2004. Systolic BP declined with time; diastolic BP was lower in 2005–2008 and 2009–2012 than 1999–2004. Prevalent diabetes and 10-yr CHD risk equivalent status (>20%) were greater in 2009–2012 than 1999–2004.
Figure 1.
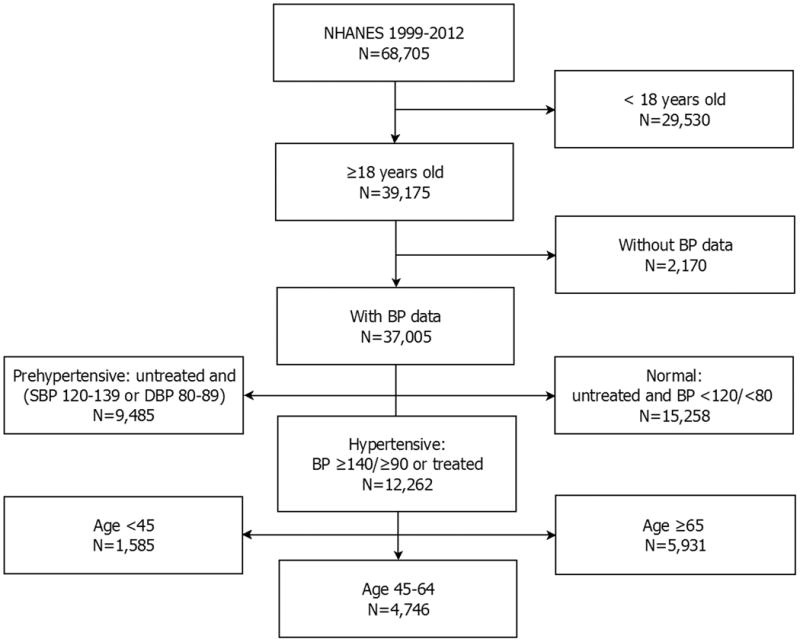
The process is depicted for selecting adults 18–85 years old with hypertension from NHANES. Adults with hypertension were then subdivided by age <45, 45 – 64, and ≥65 years as shown.
Table 1.
Characteristics of adults with hypertension in three NHANES time periods.
| NHANES | 1999–2004 | 2005–2008 | 2009–2012 | P-Values | ||
|---|---|---|---|---|---|---|
| Sample, N | 4761 | 3561 | 3940 | 1999–2004 vs 2005–2008 | 1999–2004 vs 2009–2012 | 2005–2008 vs 2009–2012 |
| US Population, N | 56,190,763 | 61,719,757 | 66,901,677 | |||
| Prevalent HTN, % | 28.4(0.7) | 29.5(0.7) | 30.5(1.0) | |||
| Age, years | 58.9(0.4) | 59.0(0.6) | 59.7(0.4) | 0.91 | 0.15 | 0.32 |
| Sex | ||||||
| Male, % | 47.0(0.9) | 48.1(0.8) | 48.7(1.0) | 0.34 | 0.21 | 0.69 |
| Female, % | 53.0(0.9) | 51.9(0.8) | 51.3(1.0) | 0.34 | 0.21 | 0.69 |
| Race | ||||||
| White, % | 73.7(1.9) | 74.1(2.5) | 70.6(2.9) | 0.91 | 0.35 | 0.36 |
| Black, % | 13.2(1.5) | 14.3(2.0) | 14.6(1.9) | 0.65 | 0.55 | 0.90 |
| Hispanic, % | 8.9(1.6) | 7.5(1.0) | 9.1(1.6) | 0.47 | 0.94 | 0.41 |
| Other, % | 4.1(0.5) | 4.2(0.6) | 5.7(0.8) | 0.96 | 0.09 | 0.12 |
| Healthcare visits/year | ||||||
| 0-1 | 21.4(0.9) | 20.0(1.1) | 17.9(1.0) | 0.35 | 0.01 | 0.14 |
| ≥2 | 78.6(0.9) | 80.0(1.1) | 82.1(1.0) | 0.35 | 0.01 | 0.14 |
| Insured | 90.4(0.7) | 89.0(0.8) | 88.8(0.8) | 0.17 | 0.12 | 0.88 |
| BMI, kg/m2 | 30.0(0.2) | 30.6(0.2) | 31.0(0.2) | 0.02 | <0.001 | 0.08 |
| BMI ≥30 | 43.3(1.0) | 46.0(1.0) | 49.5(1.2) | 0.06 | <0.001 | 0.03 |
| SBP, mmHg | 141.2(0.5) | 136.4(0.4) | 134.5(0.6) | <0.001 | <0.001 | 0.01 |
| DBP, mmHg | 76.6(0.4) | 74.3(0.4) | 73.1(0.6) | <0.001 | <0.001 | 0.09 |
| non-HDL, mg/dL | 157.8(1.0) | 148.4(0.8) | 144.8(0.9) | <0.001 | <0.001 | 0.004 |
| Hypercholesterolemia,% | 61.4(1.0) | 62.5(1.1) | 63.2(1.2) | 0.47 | 0.26 | 0.70 |
| Cholesterol Treatment,% | 23.2(0.9) | 32.6(1.3) | 37.1(1.2) | <0.001 | <0.001 | 0.01 |
| Diabetes, %, | 20.1(0.7) | 25.0(1.1) | 27.2(0.9) | <0.001 | <0.001 | 0.11 |
| CVD, % | 20.2(0.9) | 21.4(1.2) | 20.3(0.8) | 0.43 | 0.93 | 0.46 |
| CKD, % | 15.4(0.6) | 16.4(1.0) | 15.8(0.9) | 0.36 | 0.70 | 0.65 |
| Smoking, % | 17.3(0.7) | 19.0(1.0) | 15.5(0.9) | 0.17 | 0.11 | 0.01 |
| 10-yr CHD Risk | ||||||
| >20,% | 37.5(0.9) | 41.1(1.4) | 41.7(1.1) | 0.03 | 0.002 | 0.73 |
| <10,% | 20.5(0.9) | 18.6(1.4) | 18.4(1.0) | 0.22 | 0.11 | 0.94 |
Data are presented as mean and Standard Error (SE). Abbreviations: NHANES=National Health and Nutrition Examination Survey; N=number; HTN=hypertension; M=male; F=female; BMI=body mass index; S=systolic; D=diastolic; BP=blood pressure; non-HDL=non-high-density lipoprotein cholesterol; CVD=cardiovascular disease; CKD=chronic kidney disease; 10-yr CHD Risk = Framingham 10-yr coronary heart disease risk.
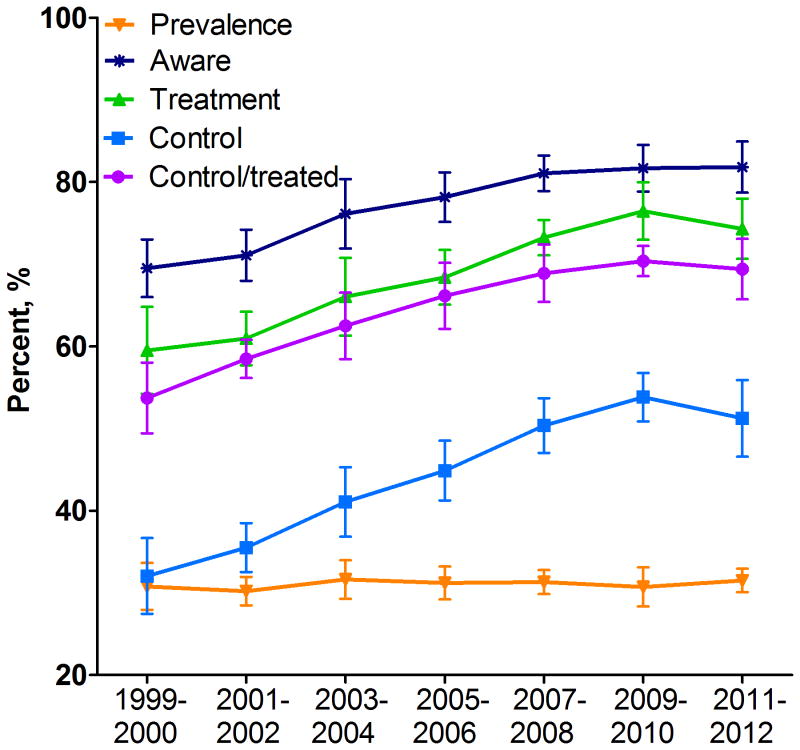
With age-adjusted to U.S. 2010 census, prevalent hypertension (Figure 2) did not change over time (p=0.32), whereas awareness, treatment, and control increased (all p<0.001) as did controlled/treated (p=0.0015). Prevalent hypertension did not change significantly in any of the six groups by age and race/ethnicity, whereas awareness, treatment, proportion of treated adults controlled and control increased over time in all groups except for adults <45 years (Figure 3). The other exception was in Hispanics, where the proportion of treated adults with hypertension controlled did not increase over time (p=0.09). Prevalent hypertension rose with increasing age; awareness and treatment were higher in the two older groups than adults <45 years. The proportion of treated adults controlled was higher at ages <45 and 45–64 than ≥65 years. Hypertension control was greater among adults 45–64 than 18–44 years old.
Figure 2.
The percentages are shown (mean and 95% confidence intervals) for hypertension prevalence, awareness, treatment, control and proportion of treated patients controlled (control/treated) among adults ≥18 years old in NHANES 1999–2012 at two-year increments. All trend lines showed a significant increase over time (p≤0.0015) except for prevalent hypertension (p=0.32).
Figure 3.
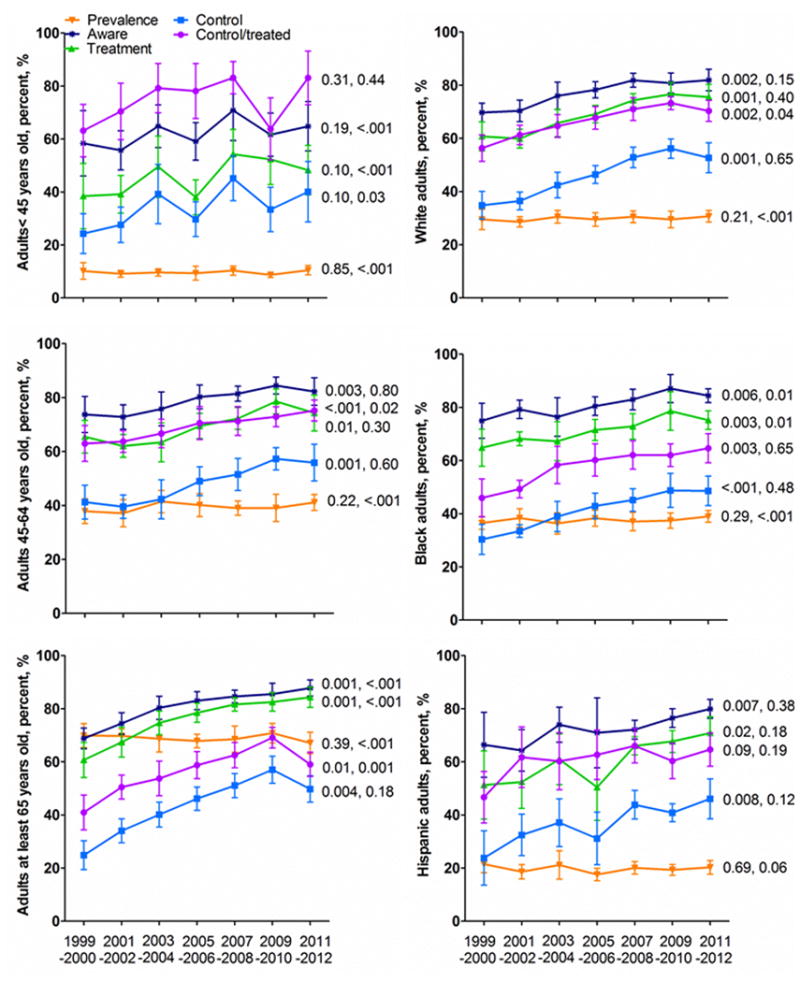
The percentages are shown (mean and 95% confidence intervals) for hypertension prevalence, awareness, treatment, control and proportion of treated patients controlled (control/treated) among adults subdivided by age group (left: <45, 45 – 64, ≥65 years) and race/ethnicity (right: white, black, Hispanic) in NHANES 1999–2012 at two-year increments. Note p-values on the left are for over time trend and p-values on the right are for between group comparisons with p-values on the top panel for comparison between top and middle panel, on the middle panel for comparison between middle and bottom panel, on the bottom panel for comparison between top and bottom panel.
Prevalent hypertension was higher in black than white and Hispanic adults (Figure 3). Hypertension awareness and treatment were higher in black than Hispanics adults. The proportion of treated adults controlled was higher in whites than blacks. Hypertension control did not differ significantly between the three race/ethnicity groups, although 95% confidence intervals were relatively wide, especially in Hispanic adults.
Data for the clinical epidemiology of hypertension in Figure 2 are provided in Supplemental Table 1. Descriptive data for the three age groups shown in Figure 3 are provided in Supplemental Table 2. P-values for between group within time period and within group between time periods are provided in Supplemental tables 2a and 2b, respectively. Descriptive data for the white, black, and Hispanic groups in Figure 3 are provided in Supplemental Table 3. Pvalues for within and between group comparisons are provided in Supplemental Tables 3a and 3b. Of note, in 2004–2008 and 2009–2012, blacks were less likely to be treated for hypercholesterolemia than whites (p<0.001), despite higher 10-year CHD risk (p<0.001).
Results of the multivariable logistic regression analysis to identify variables associated with hypertension awareness, treatment and control are shown in Table 2. Among modifiable variables, prevalent hypertension was greater with increasing body mass index, more frequent healthcare and in adults reporting treatment for cholesterol. Adults unaware of hypertension were less likely to have more frequent healthcare, higher body mass indices, and to affirm treatment for hypercholesterolemia. Adults with untreated hypertension were less likely to have more frequent healthcare, to be obese, insured, and to affirm treatment for hypercholesterolemia. The ratio of treated patients controlled was higher in adults with more frequent healthcare, with healthcare insurance, and who reported treatment for hypercholesterolemia in the prior month. Hypertension control was greater in subjects with more frequent care, higher body mass indices, healthcare insurance, and those reporting hypercholesterolemia treatment in the prior month.
Table 2.
Relationship of clinical variables to the clinical epidemiology of hypertension.
| Prevalent Hypertension | Unaware of Hypertension | Untreated Hypertension | Control / Treated Htn | Hypertension Control | |
|---|---|---|---|---|---|
| Age group <45 vs ≥65 | 0.08 0.07-0.10 |
1.12 0.84-1.49 |
1.51 1.17-1.95 |
2.71 2.08-3.53 |
1.37 1.09-1.71 |
| Age group <45 - 64 vs ≥65 | 0.35 0.32-0.39 |
0.74 0.627-0.89 |
0.83 0.71-0.98 |
1.81 1.58-2.06 |
1.67 1.45-1.91 |
| Black vs. White | 1.86 1.64-2.12 |
0.78 0.65-0.93 |
0.75 0.65-0.86 |
0.63 0.56-0.72 |
0.83 0.73-0.94 |
| Hispanic vs. White | 0.87 0.74-1.03 |
1.22 0.95-1.58 |
1.27 1.00-1.61 |
0.76 0.62-0.94 |
0.73 0.62-0.87 |
| Male vs. Female | 1.10 1.01-1.22 |
1.20 1.02-1.43 |
1.25 1.10-1.43 |
1.26 1.09-1.45 |
1.03 0.90-1.17 |
| DM vs. no DM | 1.58 1.38-1.79 |
0.647 0.519-0.808 |
0.59 0.49-0.72 |
0.94 0.78-1.20 |
1.16 0.99-1.35 |
| CVD vs. no CVD | 1.43 1.23-1.65 |
0.42 0.33-0.52 |
0.54 0.44-0.66 |
0.96 0.80-1.15 |
1.24 1.04-1.48 |
| CKD vs. no CKD | 2.12 1.82-2.47 |
0.64 0.50-0.82 |
0.56 0.44-0.72 |
0.85 0.71-1.01 |
1.09 0.93-1.3 |
| ≥2 vs 0 – 1 visits / yr | 1.55 1.40-1.70 |
0.30 0.25-0.35 |
0.24 0.19-0.29 |
1.30 1.01-1.68 |
3.23 2.63-3.99 |
| Insured vs. Uninsured | 1.03 0.90-1.18 |
0.83 0.66-1.06 |
0.60 0.47-0.76 |
1.44 1.07-1.90 |
1.69 1.35-2.11 |
| BMI / 5kg/ m2 | 1.44 1.38-1.49 |
0.76 0.71-0.816 |
0.80 0.75-0.86 |
1.00 0.94-1.06 |
1.11 1.06-1.16 |
| Smoker vs. non-Smoker | 0.96 0.85-1.08 |
0.98 0.80-1.22 |
1.04 0.86-1.25 |
1.19 0.99-1.43 |
1.09 0.93-1.28 |
| Treated vs. Untreated for Cholesterol | 2.29 2.00-2.63 |
0.46 0.37-0.57 |
0.39 0.26-0.42 |
1.25 1.06-1.46 |
1.90 1.62-2.21 |
The joint relationships derived from multivariable logistic regression modeling (multivariable odds ratios and 95% confidence intervals) are shown for the relationship of modifiable and nonmodifiable clinical variables (first vertical column on the left) to dependent variables listed in the first horizontal row (prevalent hypertension, lack of hypertension awareness [unaware hypertension], untreated hypertension, proportion of treated patients controlled, and hypertension control). BMI/5 kg/m2 indicates the estimated effect of a 5 kg/m2 increase in BMI.
Abbreviations: DM=diabetes mellitus, CVD=cardiovascular disease; CKD=chronic kidney disease; body mass index=body mass index.
Discussion
The main objective of this NHANES 1999 to 2012 analysis was to assess current status and trends in the clinical epidemiology of hypertension relative to Healthy People 2020 goals.7 Prevalent hypertension varied within a narrow range of 30.1%–30.8% between 1999–2000 and 2011–2012 (Figure 2). Given that prevalent hypertension stabilized at absolute levels 3–4% above the 2020 goal of 26.9%, new strategies or novel approaches are required.
A secondary goal of this NHANES 1999–2012 analysis was to identify modifiable factors that could facilitate progress toward Healthy People 2020 goals for hypertension prevalence, treatment, and control. Reducing prevalent hypertension is definition dependent. Healthy People 2020 defined prevalent hypertension as treatment for hypertension and/or BP ≥140/≥90 mmHg.7 Thus, in addition to decreasing incident hypertension, prevalent hypertension can be reduced by lifestyle changes that (1) decrease BP to <140/<90 in untreated adults (2) control BP to <140/<90 without medications in previously treated adults.
Prospective observational and interventional studies document that body mass index and changes in body mass index are strongly related to incident and prevalent hypertension across the adult age span;24–27 and, this was the only modifiable, lifestyle-related factor included in our analysis. Higher levels of physical activity, lower levels of sodium intake, a Dietary Approaches to Stop Hypertension concordant diet, and less analgesic use are other modifiable factors associated with reduced likelihood of incident hypertension.25 While efficacious, the percentage of the U.S. population is small whose lifestyle patterns are consistent with a low risk for prevalent and incident hypertension.25,26,28 New strategies to improve lifestyle patterns in the population are required to reduce prevalent hypertension to the Healthy People 2020 goal of 26.9%. A complementary strategy includes antihypertensive medication, which reduces incident hypertension in adults with pre-hypertension.29
The Healthy People 2020 goal of controlling hypertension in 61.2% of all adults is challenging given control at 51.2% in NHANES 2011–2012 (Figure 2). Hypertension control begins with awareness. Age-adjusted awareness of hypertension rose from 69.6% (66.0%–73.2%) in 1999–2000 to 81.2 [79.1%–83.3%] in 2007–2008 but remained flat in 2009–2012 (Figure 2). Hypertension awareness is lower in adults who are male and infrequently use healthcare (Table 2). While health insurance was not independently related to awareness, insurance increases healthcare utilization and risk factor awareness.30,31 Growth of accountable care organizations should also raise hypertension screening and awareness.32
Healthy People 2020 aim to treat 69.5% of all adults with hypertension, which was exceeded in 2007–2012. Modifiable variables strongly associated with untreated hypertension are frequency of healthcare and insurance. Efforts to provide healthcare insurance to more adults and growth of organizations accountable for care outcomes including hypertension control should further increase the proportion of adults with hypertension on treatment.31–34
The Healthy People 2020 goal of controlling 88.1% of treated patients is likely the most challenging as levels have stabilized since 2007–2008 at <70%. By increasing the percentage of patients who are aware and treated, the proportion of treated adults who must be controlled to attain the BP control goal of 61.2% declines and becomes more feasible. While 87.1% of adults with hypertension were controlled during 2011 in a large insured, managed-care organization,8 this substantially exceeds levels observed among treated patients in the U.S. (Figure 2). Less evident is that higher control rates require BP control on a greater percent of visits, which necessitates mean systolic and diastolic blood pressure and/or inter-visit BP variability below current levels.35
The main analysis for this report centered on hypertension control at <140/<90 mmHg for all adults irrespective of age and comorbid health conditions.2,8 The evidence-based treatment goal for adults ≥60 years was recently established as <150/<90 mmHg by the Committee appointed to JNC 8,35 which would increase the percentage of treated patients controlled and overall control.18 However this recommendation is at variance with other guidelines and expert opinion,36 which continue to recommend a BP goal of <140/<90 except for adults ≥80 years old for whom the BP goal of <150/<90 is recommended.
The Healthy People 2020 goal of controlling hypertension in 61.2% of all adults requires the product of proportion of adults with hypertension treated and proportion of treated adults controlled reach the stated level. If 78% of adults are treated, moderately above levels in 2007–2012, then the proportion of treated adults with hypertension controlled to attain 61.2% control in the U.S. adult population declines from 88.1% to 78.5%, which is in the range obtained by a growing number of practice settings.37 In multivariable analysis, modifiable factors independently associated with hypertension control in treated adults included health insurance, ≥2 annual healthcare visits, and hypercholesterolemia treatment.
Previous reports document that health insurance is associated with hypertension control among adults treated for hypertension.30-32 The link between hypercholesterolemia treatment, mainly statins, and hypertension control is largely indirect. In a meta-analysis of 40 randomized placebo-controlled studies, patients randomized to statins had a 2.6 mm Hg reduction in systolic BP compared to the placebo group.38 In the Anglo-Scandinavian Cardiac Outcomes Trials (ASCOT), hypertensive patients randomized to atorvastatin had a significantly lower risk of treatment resistant hypertension than patients randomized to placebo.39 These studies were not designed to assess statin effects on BP or treatment resistance and do not constitute compelling evidence to recommend statins for BP reduction. However, if statins lower BP and reduce treatment resistant hypertension as suggested by randomized, placebo-controlled trials,38,39 then implementing the 2013 Cholesterol Guidelines, which increase the number of hypertensive adults eligible for statin therapy by a net of ∼7 million,40 could improve hypertension control.
Race/ethnicity disparities in hypertension control persist when controlling for confounding factors (Table 2). Hypertension control was lower in black than white adults with hypertension, although blacks were more likely to be aware of and treated for hypertension than whites. Thus, the primary factor contributing to less hypertension control in black than white adults is the lower proportion of treated individuals attaining target blood pressure (Table 2). Greater attention in black adults to modifiable factors independently associated with the proportion of treated adults controlled including ≥2 healthcare visits/year and health insurance could improve equity in hypertension control. Moreover, in 1999–2012, blacks were less likely to report cholesterol treatment than whites, despite greater 10-year CHD risk (Supplemental Tables 3, 3a). Thus, implementing current guideline-based statin therapy may improve equity in hypertension control.
Hypertension control was also lower in Hispanic than white adults when accounting for potential confounders (Table 2). Hispanic adults were less likely than white adults to receive treatment for hypertension and less likely to be controlled when treated. Variables independently associated with both untreated hypertension and proportion of treated adults controlled included infrequent healthcare and lack of health insurance. With regard to the importance of health insurance, in a previous NHANES report of adults with multiple risk factors, Hispanics <65 years old were roughly three times more likely to be uninsured than whites in the age group (41% vs. 13%).41 In particular, Hispanics <65 years were less likely to be treated for hypertension and less likely to be controlled when treated, which is consistent with the current report. Disparities in multiple risk factor control between whites and Hispanics <65 years old were not evident at ages ≥65 years. While this analysis did not focus on age by race/ethnicity subgroups, greater attention to these modifiable variables, especially in Hispanic adults <65 years old, could improve equity in hypertension control.
In this report, adults <45 years were less likely to be aware of and treated for hypertension than older adults, but more likely to be controlled when treated. Our previous NHANES analyses indicate that infrequent healthcare, especially among men <45 years old, is a major contributor to undiagnosed and untreated hypertension in this age group.42
Limitations include relatively small cross-sectional samples of the U.S. population. Confidence intervals are often wide, which limits power for detecting clinically significant differences in the epidemiology of hypertension. Blood pressure was measured by trained professionals using a standardized protocol. Yet, hypertension status among untreated adults and control among treated adults were based on a single evaluation. Moreover, significant associations between independent and dependent variables in multivariable logistic regression analyses do not establish causal relationships.
In summary, our analysis shows that age-adjusted prevalent hypertension has remained at roughly 30% of adults from 1999–2012, which is above the Healthy People 2020 goal of 26.9%. Awareness, treatment, proportion of treated adults controlled, and control of hypertension improved from 1999–2000 to 2011–2012. Yet, these key variables did not change significantly between 2007–2008 and 2011–2012. Specifically, the proportion of treated adults with controlled hypertension has flattened at levels substantially below values required to attain the Healthy People 2020 control goal of 61.2%. To foster progress, our analysis is consistent with previous data that obesity prevention and treatment could reduce incident and prevalent hypertension. Also in agreement with earlier reports, increasing the proportion of adults with health insurance and increasing healthcare utilization are two modifiable variables independently linked with hypertension treatment and control. The new cholesterol guideline, which if implemented would lead to a greater proportion of adults with hypertension on statins,40 may also raise hypertension control. Ongoing efforts to reduce the proportion of uninsured adults, growth of accountable care organizations, and dissemination and implementation of best practices emerge as potentially useful solutions to reducing these critical gaps and attaining the Healthy People 2020 hypertension control goal.
Supplementary Material
Acknowledgments
Funding Sources: This work was supported in part by NIH HL105880; United States Army, W81XWH-10-2-0057, Centers for Disease Control, Atlanta, GA (Community Transformation Grant thru the South Carolina Department of Health and Environmental Control [SC DHEC]), and the State of South Carolina, Columbia, SC.
Footnotes
Conflict of Interest Disclosures: Dr. Egan has received income as a consultant to Blue Cross Blue Shield South Carolina, Daiichi-Sankyo, Medtronic, Novartis and research support from Daiichi-Sankyo, Medtronic, Novartis, and Takeda. None of the other authors has any disclosures to report.
References
- 1.US Burden of Disease Collaborators. The State of US Health, 1990–2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Egan BM, Li J, Qanungo S, Wolfman TE. Blood pressure and cholesterol control in hypertensive hypercholesterolemic patients. A report from NHANES 1988–2010. Circulation. 2013;128:29–41. doi: 10.1161/CIRCULATIONAHA.112.000500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frieden TR, Berwick DM. The “Million Hearts” initiative—preventing heart attacks and strokes. N Engl J Med. 2011;365:e27. doi: 10.1056/NEJMp1110421. [DOI] [PubMed] [Google Scholar]
- 4.Healthy People 2010. [accessed 19 March 2014];12: Heart disease and stroke. http://www.cdc.gov/dhdsp/docs/hp2010.pdf.
- 5.Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. doi: 10.1001/jama.2010.650. [DOI] [PubMed] [Google Scholar]
- 6.Guo F, He D, Zhang W, Walton RG. Trends in prevalence, awareness, management, and control of hypertension among United States adults, 1999 to 2010. JACC. 2012;60:599–606. doi: 10.1016/j.jacc.2012.04.026. [DOI] [PubMed] [Google Scholar]
- 7. [accessed 28 May 2014];Healthy People 2020 hypertension control goal (HDS-12) http://www.healthypeople.gov/2020/topicsobjectives2020/DataDetails.aspx?hp2020id=HDS-5.1.
- 8.Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013;310:699–705. doi: 10.1001/jama.2013.108769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Medicaid and Community Health Centers: the Relationship between Coverage for Adults and Primary Care Capacity in Medically Underserved Communities. [accessed 28 May 2014];Kaiser Commission on Medicaid and the Uninsured. http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8293.pdf.
- 10.Radford AD, Kirk DA, Howard HA, Holmes M. Review of 2009 Medicare Outpatient Claims Data. NC Rural Health Research & Policy Analysis Center; [Accessed 28 May 2014]. Profile of rural health clinics: Clinic & Medicare patient characteristics. Findings Brief #108, March 2013. http://www.shepscenter.unc.edu/rural/pubs/finding_brief/FB108.pdf. [Google Scholar]
- 11.National Health and Nutrition Examination Survey III, Cycle 2. [Accessed April 5, 2010]; http://www.cdc.gov/nchs/data/nhanes/nhanes3/cdrom/nchs/manuals/phys.pdf.
- 12.National Health and Nutrition Examination Survey. [Accessed April 5, 2010];Physician examination procedures manual. (original 1999, revised 2000). http://www.cdc.gov/nchs/nhanes/nhanes_01_02/physician_year_3.pdf.
- 13.National Health and Nutrition Examination Survey. [Accessed April 5, 2010];Physician examination procedures manual. 2003 Jan; http://www.cdc.gov/nchs/nhanes/nhanes_03_04/PE.pdf.
- 14.National Health and Nutrition Examination Survey. [Accessed April 5, 2010];Physician examination procedures manual. (revised January 2004). http://www.cdc.gov/nchs/data/nhanes/nahnes_05_06/PE.pdf.
- 15.National Health and Nutrition Examination Survey. [Accessed April 5, 2010];Physician examination procedures manual. 2007 Jan; http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_pe.pdf.
- 16.National Health and Nutrition Examination Surveys (NHANES) [Accessed 17 July 2014];Physician examination procedures manual. 2009 Aug; http://www.cdc.gov/nchs/data/nhanes/nhanes_09_10/physician.pdf.
- 17.National Health and Nutrition Examination Surveys (NHANES) [Accessed 17 July 2014];Physician examination procedures manual. 2011 Sep; http://www.cdc.gov/nchs/data/nhanes/nhanes_11_12/Physician_Exam_Manual.pdf.
- 18.Egan BM, Li J, Shatat IF, Fuller JM, Sinopoli A. Closing the gap in hypertension control between younger and older adults: NHANES 1988 to 2010. Circulation. 2014;129:2052–2061. doi: 10.1161/CIRCULATIONAHA.113.007699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muntner P, DeSalvo KB, Wildman RP, Raggi P, He J, Whelton PK. Trends in the prevalence, awareness, treatment, and control of cardiovascular disease risk factors among noninstitutionalized patients with a history of myocardial infarction and stroke. Am J Epidemiol. 2006;163:913–920. doi: 10.1093/aje/kwj124. [DOI] [PubMed] [Google Scholar]
- 20.U.S. Census Bureau. Population by sex and selected age groups:2000 and 2010. [accessed 21 March 2014]; http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf.
- 21.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Jr, Narva AS, Ortiz E. 2014 Evidence-based guideline for the management of high blood pressure in adults. Report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311:507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 22.American Diabetes Association. Standards of medical care in diabetes 2010. Diab Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–2446. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 24.Selvin E, Manzi J, Stevens LA, Van Lente F, Lacher DA, Levey AS, Coresh J. Calibration of serum creatinine in the National Health and Nutrition Examination Surveys (NHANES) 1988–1994, 1999–2004. Am J Kidney Dis. 2007;50:918–926. doi: 10.1053/j.ajkd.2007.08.020. [DOI] [PubMed] [Google Scholar]
- 25.Jones DW, Kim JS, Andrew ME, Kim SJ, Hong YP. Body mass index and blood pressures in Korean men and women: The Korean National Blood Pressure Survey. J Hypertension. 1994;12:1433–1437. doi: 10.1097/00004872-199412000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Forman JP, Stampfer MJ, Curhan GC. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA. 2009;302:404–401. doi: 10.1001/jama.2009.1060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Geiber RP, Gaziano JM, Manson JE, Buring JE, Sesso HD. A prospective study of body mass index and the risk of developing hypertension in men. Am J Hypertens. 2007;20:370–377. doi: 10.1016/j.amjhyper.2006.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stevens VJ, Obarzanek E, Cook NR, Lee IM Appel LJ, Smith West D, Milas NC, Mattfeldt-Beman M, Belden L, Bragg C, Millstone M, Raczynski J, Brewer A, Singh B, Cohen J. Trials for the Hypertension Prevention Research Group. Long-term weight loss and changes in blood pressure: Results of the Trials of Hypertension Prevention, Phase II. Ann Intern Med. 2001;134:1–11. doi: 10.7326/0003-4819-134-1-200101020-00007. [DOI] [PubMed] [Google Scholar]
- 29.Julius S, Nesbitt S, Egan BM, Weber MA, Michelson EL. Kaciroti N for TROPHY Investigators. A therapeutic intervention to change the natural history of prehypertension: The TROPHY Study main results. N Engl J Med. 2006;354:1685–1697. doi: 10.1056/NEJMoa060838. [DOI] [PubMed] [Google Scholar]
- 30.Duru OK, Vargas RB, Kermah D, Pan D, Norris KC. Health insurance status and hypertension monitoring and control in the United States. Am J Hypertens. 2007;20:348–353. doi: 10.1016/j.amjhyper.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 31.Brooks EL, Preis SR, Hwang SJ, Murabito JM, Benjamin EJ, Kelly-Hayes, Sorlie P, Levy D. Health insurance and cardiovascular disease risk factors. Am J Med. 2010;123:741–747. doi: 10.1016/j.amjmed.2010.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Accountable Care Organizations 2013: Program analysis (ACO21) Preventive screening: Screening for high blood pressure. [accessed March 14, 2014];2012 Dec 21; http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/ACONarrativeMeasures-Specs.pdf.
- 33.Ostchega Y, Hugher JP, Wright JD, McDowell MA, Louis T. Are demographic characteristics and health care access and utilization, and comorbid conditions associated with hypertension among US adults? Am J Hypertens. 2008;21:159–65. doi: 10.1038/ajh.2007.32. [DOI] [PubMed] [Google Scholar]
- 34.Decker SL, Kostova D, Kenney GM, Long SK. Health status, risk factors, and medical conditions among persons enrolled in Medicaid vs. uninsured low-income adults potentially eligible for Medicaid under the Affordable Care Act. JAMA. 2013;309:2579–2586. doi: 10.1001/jama.2013.7106. [DOI] [PubMed] [Google Scholar]
- 35.Parati G, Omboni S, Bilo G. Why is out-of-office blood pressure measurement needed? Home blood pressure measurements will increasingly replace ambulatory blood pressure monitoring in the diagnosis and management of hypertension. Hypertension. 2009;54:181–187. doi: 10.1161/HYPERTENSIONAHA.108.122853. [DOI] [PubMed] [Google Scholar]
- 36.Wright JT, Jr, Fine LJ, Lackland DT, Ogedegbe G, Dennison Himmelfarb CR. Evidence supporting a systolic blood pressure goal of <150 mm Hg in patients ≥60 years: The minority view. Ann Intern Med. 2014 doi: 10.7326/M13-2981. [DOI] [PubMed] [Google Scholar]
- 37. [accessed 19 March 2014];Million Hearts® 2013 hypertension control challenge champions announced. http://millionhearts.hhs.gov/newsevents/hypertension_control_champions.html.
- 38.Briasoulis A, Agarwal V, Valachis A, Messerli FH. Antihypertensive effects of statins: A meta-analysis of prospective controlled studies. J Clin Hypertens. 2013;15:310–320. doi: 10.1111/jch.12081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gupta AK, Nasothimiou EG, Chang CL, Sever PS, Dahlöf B, Poulter NR. Baseline predictors of resistant hypertension in the Anglo-Scandinavian Cardiac Outcome Trial (ASCOT): a risk score to identify those at high-risk. J Hypertension. 2011;29:2014–2013. doi: 10.1097/HJH.0b013e32834a8a42. [DOI] [PubMed] [Google Scholar]
- 40.Pencina MJ, Mavar-Boggan AM, D'Agostino RB, Williams K, Neely B, Sniderman AD, Peterson ED. Application of new cholesterol guidelines to a population-based sample. N Engl J Med. 2014;370:1422–1431. doi: 10.1056/NEJMoa1315665. [DOI] [PubMed] [Google Scholar]
- 41.Egan BM, Li Jiexiang, Wolfman TE, Sinopoli A. Demographic differences in concurrent vascular risk factor control in patients with diabetes: NHANES 1988–2010. J Am Soc Hypertens. 2014;8:394–404. doi: 10.1016/j.jash.2014.03.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Egan BM, Zhao Y, Axon RN, Brzezinski WA, Ferdinand KD. Uncontrolled and apparent treatment resistant hypertension in the U.S. 1988–2008. Circulation. 2011;124:1046–1058. doi: 10.1161/CIRCULATIONAHA.111.030189. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.