Abstract
Total hip arthroplasty has evolved from the first total hip arthroplasty in 1938, through the revolutionization of hip arthroplasty by principles of low friction arthroplasty introduced by Sir John Charnley in 1960s to the present state of the art implants and techniques. The main concern regarding failure of total hip arthroplasty has been the biological response to particulate polyethylene debris generated by conventional metal on polyethylene bearing surfaces leading to osteolysis and aseptic loosening of the prosthesis. Therefore, recent research has been focussing on alternative bearing surfaces to reduce the particulate debris generated. These bearing surfaces include ceramic-polyethylene, metal–metal as well as ceramic–ceramic articulations and have demonstrated lesser friction rates as well as significantly lower wear rates as compared to widely used metal on polyethylene surfaces. Clinical experience until now has shown that metal on metal articulations have significant safety concerns whereas metal-on-highly crosslinked polyethylene, ceramic on ceramic and ceramic on highly crosslinked polyethylene articulations have shown encouraging results to hold promise for wider use in younger and more active patients. This review article discusses positives and drawbacks of various bearing surfaces in current clinical use in total hip arthroplasty as well as briefly explores the newer technologies on the horizon which may even further decrease wear and improve total hip arthroplasty survivorship.
Keywords: Bearing surfaces, Total hip arthroplasty, Evolution
Introduction
Total hip replacement has been widely acclaimed as the “Operation of the century”.1,2 Although multiple treatment modalities have been tried for treatment of hip arthritis, surgical treatment has been tried only in last 150 years. Themistocles Gluck probably performed the first hip arthroplasty (a hemiarthroplasty) in 1891 using an ivory femoral head. A wide range of tissues were tried in early twentieth century as an interposition material e.g. fascia lata, skin, pig's bladder etc. Vitallium mould design of Smith-Peterson was the first one to use artificial materials as a bearing surface in hip arthroplasty (Again, a hemiarthroplasty).3
In total hip replacement surgery, both the acetabular and femoral bearing surfaces are replaced with artificial material like metal, ceramic and/or polymeric components. Wiles performed first total hip replacement in 1938 in United Kingdom using a metal on metal combination.4 This was further developed by surgeons like Ring & McKee during the 1950s & 1960s. During the same period, Dr Ban Saw of erstwhile Burma replaced femoral heads of patients with femoral neck fractures with hand made ivory components achieving excellent results.5
The most significant development in evolution of THR bearing surfaces was the introduction of concept of low friction arthroplasty by Sir John Charnley in 1958, using metal on high-density polyethylene as bearing surface.6 The principles proposed by him remain relatively unchallenged till today despite rapid evolution of multiple facets of hip replacement surgery. In 1970, Boutin introduced the ceramic on ceramic articulation in THR for the first time.7
Currently, the bearing surface which has proved to produce most consistent results in THR is the combination of femoral head made of cobalt chrome alloy articulating on an acetabular component made from ultra high molecular weight polyethylene (UHMWPE).8
The longevity of a total hip prosthesis is the area of highest concern for arthroplasty practitioners as well as their clientele. Hip replacements are being subjected to higher levels of activity in view of more and more hip replacements being done in relatively younger patients and increasing life expectancy of older population. Wear rates of 75–250 μm/year in polyethylene surfaces lead to periprosthetic osteolysis which is a major concern affecting prosthesis survival, especially in the young.9,10 Bearing surfaces in THR have undergone a significant evolution from the introduction of low friction arthroplasty by Charnley to currently popular ceramic on ceramic and ceramic on crosslinked polyethylene. This review critically analyses the development of all currently available options and their strengths as well as weaknesses.
Tribology
Although the long-term survival of THR prosthesis is affected by multiple factors, tribology (Friction, lubrication and wear) of the bearing surface is the most important. The aim is to achieve a bearing surface close enough to articular cartilage which has low coefficient of friction, is capable of significant deformation without failure and exhibits no wear in absence of any pathology. In the natural hip joint, the low coefficient of friction is achieved by three lubrication mechanisms – elastohydrodynamic (EHD) lubrication, μEHD, and squeeze-film lubrication. During the stance phase of walking, EHD and μEHD predominate when pressure is generated in the synovial fluid by an entraining motion between the joint surfaces. During the heel strike phase, squeeze-film action predominates as the synovial fluid gets squeezed out with two cartilage surfaces moving toward each other. Synovial fluid film is retained partly due to deformation of the articular cartilage.11
Ideal bearing surface
Ideal bearing surface in THR prosthesis would have the following features12:
-
1.
Low coefficient of friction
-
2.
Small volume of wear particle generation
-
3.
Low tissue reaction to wear particles
-
4.
High resistance to third body wear
-
5.
Enough deformation of articular surfaces to permit adequate fluid film lubrication during the stance phase without increasing wear
The currently used bearing surfaces can be classified into two major classes:
-
1.
Hard-on-soft bearings
-
2.
Hard-on-hard bearings
In this classification, soft bearing is always towards the acetabular side and includes ultra high molecular weight polyethylene (UHMWPE) and highly crosslinked UHMWPE. Hard bearing includes metal alloys (Cobalt chrome) and ceramics (Fig. 1).
Fig. 1.
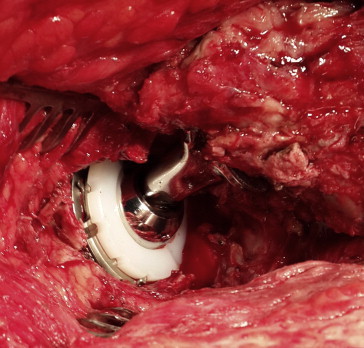
Metal on polyethylene – The gold standard.
Hard-on-soft bearings
Metal-on-highly crosslinked polyethylene
Over the last five decades, the most acceptable bearing surface couple in a prosthetic hip is a cobalt chrome femoral head articulating with a UHMWPE acetabular component in view of the excellent long-term results available. This bearing surface couple remains the standard to which wear testing for other bearing articulations are compared.
Ultra high molecular weight polyethylene (UHMWPE) was first used as a bearing surface on acetabular side in 1958. Several long chains of monomer ethylene constitute UHMWPE. The major problem of UHMWPE combined with metallic heads was early wear which is related to the following factors: Sterilization, material properties, implant geometry and limited shelf life.5 The wear particles generated by metal on UHMWPE articulation cause a chronic inflammatory response to foreign body which is mediated by macrophages with release of lytic enzymes, bone resorbing mediators and pro-inflammatory cytokines. This response ultimately leads to osteolysis in periprosthetic bone which causes fixation failure and aseptic loosening.13–15 Initially, this osteolysis was erroneously believed to be a reaction to bone cement (PMMA) leading to the coinage of term, “Cement disease”.16,17
Periprosthetic osteolysis over the years has been attributed to the polyethylene wear particles. This osteolysis appears to occur more commonly at wear rates of more than 0.1 mm/year and is uncommon when wear rate is less than 0.05 mm/year.18,19 This wear rate has been substantially reduced by cross-linking of polyethylene using gamma radiation and thermal treatment which increased oxidation resistance of UHMWPE as well as decreased abrasive and adhesive wear rates.20,21 In 1998, highly crosslinked polyethylene was used for the first time clinically and marked a significant improvement to UHMWPE bearing surface. Clinical follow-up results as well as simulator studies (10–22 years) have shown minimal wear of the highly crosslinked UHMWPE acetabular components during an expected clinical life span.22–24
Although clinical results of first generation crosslinked polyethylenes have been promising and matching the predicted results, new issues have also cropped up in the form of free radicals and polyethylene oxidation following thermal treatment (annealing) which affects mechanical and crystalline properties of UHMWPE.25,26 In the second generation crosslinked polyethylenes, these issues are being dealt by different methods ranging from sequential annealing to saturate free radicals (X3 – Stryker Orthopaedics, NJ) to use of Vitamin E as a free radical scavenger (EPoly-Biomet, Warsaw, IN).26,27 Although initial results are promising, long-term clinical results of the second generation polyethylenes are not yet available.
Ceramic on crosslinked polyethylene
Use of ceramic head on crosslinked polyethylene liners is gradually gaining wider acceptance, though it is still not very widely used. Clinical as well as laboratory data have shown that wear rates for ceramic on polyethylene bearings are significantly lesser than metal on polyethylene bearings with studies showing 10%–50% lesser wear.28
Various advantages of ceramic femoral heads over metal femoral heads articulating with crosslinked polyethylene are as follows: 1. The polished surface of ceramics have much lesser coefficient of friction as compared to metal; 2. Better joint lubrication is achieved with ceramics; 3. Metal ions are released from metal femoral heads causing oxidation and surface roughening whereas ceramics are chemically inert with no such issues; 4. Ceramic heads have lower susceptibility to surface scratching.29,30
Hard-on-hard bearings
The main drawback of hard-on-soft bearings is the wear-particle related periprosthetic osteolysis leading to failure of arthroplasty. In view of this, other bearing surface alternatives developed which included metal on metal as well as ceramic on ceramic bearing surfaces. These bearing surfaces generate much lesser wear particles and the size of the wear particles released is much smaller (0.015–0.12 μm) whereas osteolysis is triggered by much larger particles (0.2–7 μm).31
Metal on metal bearings
Metal on metal hip resurfacing (MoM HR)
Resurfacing of the arthritic hip joint seems to be the best arthroplasty choice considering the minimal bone loss involved and excellent stability possible. First attempts to resurface started in 1930s with Smith-Peterson cup arthroplasty and Teflon shells by Sir John Charnley in 1950s. Though these procedures produced good short-term results, they had a high failure rate due to high wear leading to severe osteolysis. The interest in resurfacing waned after success of metal on polyethylene bearing surfaces in 1960s and 1970s and poor results of notable attempts from Wagner from Germany and Tharies from USA.5
A resurgence of the metal on metal hip resurfacing occurred after McMinn D et al designed a new implant in 1990s, Birmingham Hip Resurfacing (BHR) prosthesis, based on some of the earlier successful metal on metal designs like McKee Farrar and Stanmore and newer metallurgy available.32 Though these implants are expected to give better range of motion, higher stability, higher scratch resistance, bone conservation and relative ease of revision, these are not without their own share of problems. There have been recent concerns about higher blood levels of Cobalt and Chromium ions leading to concern about higher cancer risk as well as occurrence of pseudotumours, also called Aseptic Lymphocyte dominated Vasculitis Associated lesions (ALVAL).33 This is an area of intense current controversy with some designs having been withdrawn from market (ASR prosthesis from DePuy) due to high failure rates whereas BHR prosthesis continues to be used, though under much closer follow-up and scrutiny. Though higher failure rates are an accepted fact, the controversy remains about whether the cause of failure was poor component positioning, implant design or a combination of both. In addition, higher failure rates have been reported in obese, females and smaller femoral head components (Fig. 2.).
Fig. 2.
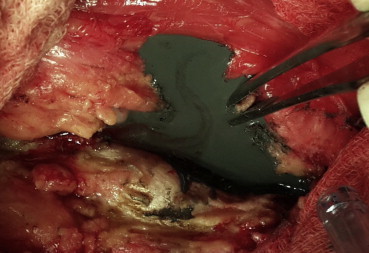
Extensive metallosis – Revision of a metal on metal.
Metal on metal hip arthroplasty
With early success of metal on metal hip resurfacing, the same bearing surface was used for hip replacement with stemmed femoral components as this permitted use of larger femoral heads which increase the head to neck ratio facilitating higher excursion distance and higher stability making it advantageous to be used in revision for unstable/dislocated hip prosthesis.34
However this bearing surface had a higher failure rate for the same reasons as enumerated for hip resurfacing. In addition, there were concerns about the corrosion at the trunnion of stem to femoral head junction leading to coining of a new term called “trunnionosis”.35 In view of these additional concerns and reports of high failure rates, the use of metal on metal bearing surface with stemmed femoral components has been abandoned largely over the last couple of years.
Ceramic on ceramic
In the late 60s, ceramic on ceramic bearings were first introduced in hip arthroplasty by Boutin.36 They have undergone many generations of changes since then during which the susceptibility to fracture (a problem in early generation ceramics) has been overcome. Since ceramics are harder than metals, are biologically inert and have better lubrication properties leading to low wear rates, ceramic on ceramic bearings make an attractive choice for ensuring long-term survival of hip prosthesis. The minimal wear particles released from ceramic on ceramic bearings are also biologically relatively inert and at nanometric size, significantly reducing the osteolysis produced due to polyethylene wear particles. In addition, ceramic on ceramic bearing combination also has lesser coefficient of friction, higher wettability with biologically inert wear particles. Clinical results have confirmed higher survivorship, lesser wear and low osteolysis making these bearings an excellent choice for young and active individuals.37
There are two types of ceramic bearings – Zirconia and Alumina. Though alumina has been preferred over zirconia in the past, the newest generation of ceramics are much better performing composites which incorporate tetragonal, nanosized, yttria-stabilized zirconia particles (close to 25%) into an alumina matrix (close to 75%) improving the composite's mechanical properties by preventing initiation and propagation of cracks (marketed as Biolox Delta by Ceramtec, Plochigen, Germany). A small amount (<1%) of chromium oxide further strengthens the composite ceramic. The wear rates of the new composite ceramic bearings are significantly less than older alumina bearings38,39 (Fig. 3).
Fig. 3.

Fractured ceramic liner of acetabular component.
Though the ceramics are the new preferred bearing surface, especially in the young, they are not without their share of complications which include squeaking noises, stripe wear, a rare bearing surface fracture or chipping during insertion. Complications have been more commonly associated with acetabular component malposition (more vertical cups), smaller femoral heads and non-adherence to meticulous surgical technique.40,41
A fractured ceramic component required revision by careful removal of ceramic fragments and revision with a ceramic bearing only. A softer bearing surface is likely to have an accelerated wear due to third body wear. There are variable reports about the cause of squeaking noise ranging from component malposition, edge loading as well as lax hips. There has been an association of stripe wear with squeaking but not all bearings with wear stripes squeak, and not all pristine bearings are silent27,42 (Fig. 4).
Fig. 4.

Revised fractured ceramic bearing surfaces.
Future directions
-
1
Ceramic femoral head articulating with metal acetabular component: First described by Firkins et al, the likely advantage of this bearing combination is likely to be lower wear and generations of much lesser metal particles. It also allows use of larger ceramic heads reducing the risk of ceramic fracture & increasing the number of femoral head options. Clinical studies are evaluating performance of this bearing coupling at select centres.38,43
-
2
Oxinium: Oxidized zirconium (Oxinium, Smith & Nephew) has been developed and is in clinical usage for femoral heads for less than a decade. It is expected to provide wear resistance of ceramic without its fracture risk. However, long-term clinical results are yet to prove its advantages.
-
3
Silicon nitride bearings: Ceramic (Alumina/Zirconium) fractures have remained a concern in ceramic bearings. An alternative bearing surface is being explored manufactured from powder of Silicon nitride (Si3N4). This alternative ceramic has been used successfully in aerospace bearings as well as diesel engines. The Si3N4–Si3N4 pairings have a friction coefficient of 0.001 compared to 0.08for Al2O3–Al2O3. Mechanical testing has shown higher fracture toughness, higher flexural strength, higher resistance to hydrothermal degradation. Biocompatibility tests have shown that Si3N4 does not produce any adverse reactions behaving similar to alumina.44 Clinical trials are currently underway and results of same would decide clinical applicability and availability of this new alternative ceramic in the future.
-
4
Compliant bearings: Cartilage is an example of a compliant bearing that has a low modulus but is capable of large deformation without failure. Polyurethanes are synthetic polymers having properties comparable to those of articular cartilage. Extensive laboratory and mechanical studies have been underway over the last decade to determine suitability of polyurethanes as a bearing surface aimed at obtaining a bearing surface couple in which the surfaces are separated by pressure developed in joint fluid as well as by deformation of articular surfaces.11 This is significantly different approach from the currently used bearing surfaces which operate under mixed lubrication conditions resulting in higher wear.
-
5
Prevention of retroacetabular stress shielding: Stiff hemispherical acetabular shells lead to retroacetabular bone loss due to stress shielding.45 This stress shielding is not related to thickness of the shell. Cambridge Cup (Howmedica, Staines, UK), a horseshoe-shaped all polymer acetabular construct (polyethylene bearing surface, carbon fibre reinforced polybutyleneterphthalate shell with hydroxyapatite coating), showed an early reduction in bone loss with this flexible design and the recovery in bone density in the weight bearing region of the acetabulum at 2 years follow-up.46 MITCH™ PCR Cup (Stryker SA, Montreux, Switzerland), a second generation horseshoe-shaped design, has both a structure and bearing surface of carbon fiber/polyetheretherketone (PEEK) composite and is fixed to bone with a hydroxylapatite coating. The femoral head is alumina ceramic.
Conclusion
Needless to say that, despite all the modern advances in materials and designs, meticulous surgical technique still remains the most important determinant of the success and longevity of total hip arthroplasty. Component malpositioning and joint laxity (Sequelae of poor technique) lead to instability, edge loading and accelerated wear leading to bearing surface damage adversely affecting the longevity of the hip prosthesis.
To conclude, total hip replacement surgery remains a highly successful procedure providing good pain relief and improvement of activity levels in arthritic hip joints. Despite its success, the expectations continue to increase with more and more young patients undergoing hip replacement and most of them seeking higher activity level (higher range of motion and stability in those ranges) as well as longevity of the prosthesis. Besides the fixation method for the prosthesis, bearing surfaces remain the most important determinant of longevity of the hip prosthesis. Newer bearing surfaces in current clinical practice (Ceramic on ceramic, ceramic on crosslinked polyethylene, ceramic on crosslinked polyethylene) have shown promise in decreasing the wear rates. With success of these wear reducing bearing surfaces, the scientific community will need to focus on not only further reducing abrasive wear but on reducing stress shielding of acetabulum as well by newer materials as well as designs. The final frontier in hip replacement bearing surfaces would be biological resurfacing of the arthritic hip joint, which, unfortunately, remains in theoretical realm only at present.
Conflicts of interest
All authors have none to declare.
References
- 1.Learmonth I.D., Young C., Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007 Oct 27;370(9597):1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 2.Coventry M.B. Foreword. In: Amutz H.C., editor. Hip Arthroplasty. Churchill Livingstone; New York: 1991. [Google Scholar]
- 3.Smith Peterson M.N. The classic: evolution of mould arthroplasty of the hip joint. J Bone Joint Surg Br. 1948;30B:L59. [PubMed] [Google Scholar]
- 4.Wiles P. The surgery of the osteoarthritic hip. Br J Surg. 1958;45:88–97. doi: 10.1002/bjs.18004519315. [DOI] [PubMed] [Google Scholar]
- 5.Sandiford N.A., Alao U., Skinner J.A., Samsani S.R. Hip arthroplasty, recent advances in hip and knee arthroplasty. In: Fokter Samo., editor. 2012. InTech, Available from: http://www.intechopen.com/books/recent-advances-in-hip-and-knee-arthroplasty/hip-arthroplasty. [Google Scholar]
- 6.Charnley J. Arthroplasty of the hip: a new operation. Lancet. 1961;1:1129–1132. doi: 10.1016/s0140-6736(61)92063-3. [DOI] [PubMed] [Google Scholar]
- 7.Dorlot J.M. Long-term effects of alumina components in total hip prostheses. Clin Orthop. 1992;282:47–52. [PubMed] [Google Scholar]
- 8.Black J. Prospects for alternate bearing surfaces in total replacement arthroplasty of the hip. In: Puhl W., editor. Performance of the Wear Couple BIOLOX Forte in Hip Arthroplasty: Proceedings of the 2nd Symposium on Ceramic Wear Couple. Germany: Ferdinand Enke Verlag; Stuttgart: 1997. pp. 2–10. [Google Scholar]
- 9.Harris W.H. The problem is osteolysis. Clin Orthop. 1995;311:46–53. [PubMed] [Google Scholar]
- 10.Ranawat C.S., Peters L.E., Umlas M.E. Fixation of the acetabular component: the case for cement. Clin Orthop. 1997;344:207–215. [PubMed] [Google Scholar]
- 11.Scholes S.C. Compliant layer acetabular cups: friction testing of a range of materials and designs for a new generation of prosthesis that mimics the natural joint. Proc Inst Mech Eng H. 2006;220:583–596. doi: 10.1243/09544119H06404. [DOI] [PubMed] [Google Scholar]
- 12.Minakawa H., Stone M.H., Wroblewski B.M. Quantification of third-body damage and its effect on UHMWPE wear with different types of femoral head. J Bone Joint Surg Br. 1998;80-B:894–899. doi: 10.1302/0301-620x.80b5.8675. [DOI] [PubMed] [Google Scholar]
- 13.Maloney W.J., Jasty M., Harris W.H., Galante J.O., Callaghan J.J. Endosteal erosion in association with stable uncemented femoral components. J Bone Joint Surg Am. 1990;72:1025–1034. [PubMed] [Google Scholar]
- 14.Vernon-Roberts B., Freeman M.A.R. The tissue response to total joint replacement prosthesis. In: Swanson S.A.V., Freeman M.A.R., editors. The Scientific Basis of Joint Replacement. Pitman Medical Publishing; Tunbridge Wells: 1977. pp. 86–129. [Google Scholar]
- 15.Willert H.G. Reactions of the articular capsule to wear products of artificial joint prosthesis. J Biomed Mater Res. 1977;11:157–164. doi: 10.1002/jbm.820110202. [DOI] [PubMed] [Google Scholar]
- 16.Archibeck M.J., Jacobs J.J., Roebuck K.A., Glant T.T. The basic science of periprosthetic osteolysis. Instr Course Lect. 2001;50:185–195. [PubMed] [Google Scholar]
- 17.Amstutz H.C., Campbell P., Kossrovsky N., Clarke I.C. Mechanism and clinical significance of wear debris induced osteolysis. Clin Orthop Relat Res. 1992;276:7–18. [PubMed] [Google Scholar]
- 18.Green T.R., Fisher J., Stone M., Wroblewski B.M., Ingham E. Polyethylene particles of a ‘critical size’ are necessary for the induction of cytokines by macrophages in vitro. Biomaterials. 1998;19:2297–2302. doi: 10.1016/s0142-9612(98)00140-9. [DOI] [PubMed] [Google Scholar]
- 19.Dumbleton J.H., Manley M.T., Edidin A.A. A literature review of the association between wear rate and osteolysis in total hip arthroplasty. J Arthroplasty. 2002;17:649. doi: 10.1054/arth.2002.33664. [DOI] [PubMed] [Google Scholar]
- 20.Kurtz S.M. Elsevier; San Diego: 2004. The UHMWPE Handbook. [Google Scholar]
- 21.Dorr L.D., Wan Z., Shahrdar C. Clinical performance of a Durasul highly cross-linked polyethylene acetabular liner for total hip arthroplasty at five years. J Bone Joint Surg Am. 2005;87:1816. doi: 10.2106/JBJS.D.01915. [DOI] [PubMed] [Google Scholar]
- 22.D'Antonio J.A., Manley M.T., Capello W.N. Five year experience with crossfire highly cross-linked polyethylene. Clin Orthop Relat Res. 2005;441:143–150. doi: 10.1097/00003086-200512000-00024. [DOI] [PubMed] [Google Scholar]
- 23.Atienza C., Jr., Maloney W.J. Highly cross-linked polyethylene bearing surfaces in total hip arthroplasty. J Surg Orthop Adv. 2008;17:27–33. [PubMed] [Google Scholar]
- 24.Digas G. 5-year experience of highly cross-linked polyethylene in cemented and uncemented sockets. Two randomized studies using radiostereometric analysis. Acta Orthop. 2007;78(6):746–754. doi: 10.1080/17453670710014518. [DOI] [PubMed] [Google Scholar]
- 25.Kurtz S.M., Manley M.T., Wang A. Comparison of the properties of annealed crosslinked (crossfire) and conventional polyethylene as hip bearing materials. Bull Hosp Jt Dis. 2003;61:17. [PubMed] [Google Scholar]
- 26.Dumbleton J.H., D'Antonio J.A., Manley M.T. The basis for a second generation highly crosslinked UHMWPE. Clin Orthop Relat Res. 2006;453:265. doi: 10.1097/01.blo.0000238856.61862.7d. [DOI] [PubMed] [Google Scholar]
- 27.Manley M.T., Sutton K. Bearings of the future for total hip arthroplasty. J Arthroplasty. 2008;23(suppl 7):47–51. doi: 10.1016/j.arth.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 28.Simon J.A., Dayan A.J., Ergas E., Stuchin S.A., DiCesare P.E. Catastrophic failure of the acetabular component in a ceramic-polyethylene bearing total hip arthroplasty. J Arthroplasty. 1998;13:108–113. doi: 10.1016/s0883-5403(98)90085-7. [DOI] [PubMed] [Google Scholar]
- 29.Semlitsch M., Willert H.G. Clinical wear behaviour of ultra-high molecular weight polyethylene cups paired with metal and ceramic ball heads in comparison to metal-on-metal pairings of hip joint replacements. Proc Inst Mech Eng H. 1997:73–88. doi: 10.1243/0954411971534700. [DOI] [PubMed] [Google Scholar]
- 30.Jazrawi M.L., Frederick J.K., DiCesare P.E. Alternative bearing surfaces for total joint arthroplasty. J Am Acad Orthop Surg. 1998;6:198–203. doi: 10.5435/00124635-199807000-00001. [DOI] [PubMed] [Google Scholar]
- 31.Schmalzried T.P., Peters P.C., Maurer B.T., Bragdon C.R., Harris W.H. Long-duration metal-on-metal total hip arthroplasties with low wear of the articulating surfaces. J Arthroplasty. 1996;11:322–331. doi: 10.1016/s0883-5403(96)80085-4. [DOI] [PubMed] [Google Scholar]
- 32.McMinn D., Daniel J. History and modern concepts in surface replacement. Proc Inst Mech Eng J Eng Med H. 2006;220:239–251. doi: 10.1243/095441105X68944. [DOI] [PubMed] [Google Scholar]
- 33.Willert H.G., Buchhorn G.H., Fayyazi A. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87:28–36. doi: 10.2106/JBJS.A.02039pp. [DOI] [PubMed] [Google Scholar]
- 34.Dumbleton J.H., Manley M.T. Metal-on-metal total hip replacement: what does the literature say? J Arthroplasty. 2005;20:174. doi: 10.1016/j.arth.2004.08.011. [DOI] [PubMed] [Google Scholar]
- 35.Pastides P.S., Dodd M., Sarraf K.M., Charles A.W.O. Trunnionosis – a pain in the neck. World J Orthop. 2013 October 18;4(4):161–166. doi: 10.5312/wjo.v4.i4.161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Boutin P. Arthroplastie totale de la hanche par prosthese en alumina fritee. Rev Chir Orthop. 1972;58:229–246. [PubMed] [Google Scholar]
- 37.Jonathan P.G. Ceramic hip replacement history. Semin Arthroplasty. 2011;22(4):214–217. [Google Scholar]
- 38.D'Antonio J. Ceramic materials as bearing surfaces for THA. J Am Acad Orthop Surg. 2009;17:63–68. [PubMed] [Google Scholar]
- 39.Tateiwa T. Ceramic total hip arthroplasty in the United States: safety and risk issues revisited. Am J Orthop. 2008;37:26–31. [PubMed] [Google Scholar]
- 40.Dennis D.A. The squeaking hip: a cause for concern-disagrees. Orthopedics. 2007;30:739. doi: 10.3928/01477447-20070901-33. [DOI] [PubMed] [Google Scholar]
- 41.Ranawat A.S., Ranawat C.S. The squeaking hip: a cause for concern-agrees. Orthopedics. 2007;30:738. doi: 10.3928/01477447-20070901-32. [DOI] [PubMed] [Google Scholar]
- 42.Restrepo C. The noisy ceramic hip: is component malpositioning the cause? J Arthroplasty. 2008;23:643–649. doi: 10.1016/j.arth.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 43.Firkins P.J. A novel low wearing differential hardness, ceramic-on metal hip joint prosthesis. J Biomech. 2001;34:1291–1298. doi: 10.1016/s0021-9290(01)00096-3. [DOI] [PubMed] [Google Scholar]
- 44.Bal B.S. Fabrication and testing of silicon nitride bearings in total hip arthroplasty. J Arthroplasty. 2009;24(1):110–116. doi: 10.1016/j.arth.2008.01.300. [DOI] [PubMed] [Google Scholar]
- 45.Manley M.T., Ong K.L., Kurtz S.M. The potential for bone loss in acetabular structures following THA. Clin Orthop Relat Res. 2006;453:246. doi: 10.1097/01.blo.0000238855.54239.fd. [DOI] [PubMed] [Google Scholar]
- 46.Field R.E., Cronin M.D., Singh P.J. Bone remodelling around the Cambridge cup: a DEXA study of 50 hips over 2 years. Acta Orthop. 2006;77:726. doi: 10.1080/17453670610012908. [DOI] [PubMed] [Google Scholar]


