Abstract
Previous research investigating the roles of effector (Teff) and regulatory (Treg) T cells after injury to the central nervous system (CNS) has yielded contradictory conclusions, with both protective and destructive functions being ascribed to each of these T-cell subpopulations. Here we study this dichotomy by examining how regulation of the immune system affects the response to CNS trauma. We show that in response to CNS injury, Teff and Treg subsets in the CNS-draining deep cervical lymph nodes are activated, and surgical resection of these lymph nodes results in impaired neuronal survival. Depletion of Treg, not surprisingly, induces a robust Teff response in the draining lymph nodes and is associated with impaired neuronal survival. Interestingly, however, injection of exogenous Treg cells, which limits the spontaneous beneficial immune response after CNS injury, also impairs neuronal survival. We found that no Treg accumulate at the site of CNS injury, and that changes in Treg numbers do not alter the amount of infiltration by other immune cells into the site of injury. The phenotype of macrophages at the site, however, is affected: both addition and removal of Treg negatively impact the numbers of macrophages with alternatively activated (tissue-building) phenotype. Our data demonstrate that neuronal survival after CNS injury is impaired when Treg cells are either removed or added. With this exacerbation of neurodegeneration seen with both addition or depletion of Treg, we recommend exercising extreme caution when considering the therapeutic targeting Treg cells after CNS injury, and possibly in chronic neurodegenerative conditions.
Introduction
Acute injury to the central nervous system (CNS) evokes cellular and molecular responses that lead to secondary neurodegeneration, a process of sustained neuronal degeneration (1). Accompanying this period of secondary degeneration is a coordinated immune response to the trauma, including chemotaxis of microglia to ATP released from the damaged cells (2) and directed migration of both the innate and adaptive immune cells to the injury site due to chemokine signals (3). The dogma that this infiltration of immune cells into the injury site was a detrimental response has been challenged by the finding that neuronal survival could be improved by boosting T cell activity rather than by its suppression (4-6), though the phenotype of protective T cells after CNS injury, and particularly the role of regulatory T (Treg) cells in this process, is still a matter of debate (7-10).
Naturally occurring Treg cells, which express the transcription factor Foxp3 (11-13), have been intensively studied for their ability to suppress adaptive immune responses (14-17). This subset of T cells, which develops with high avidity to self-antigens, is especially important in controlling autoimmunity (18). Therefore, it has been proposed that Treg cells mediate their actions by attenuating both protective and inflammatory post-injury immune responses, and thus either exacerbating (19) or ameliorating (20) neuronal degeneration. Despite these studies, the exact mechanism of their action in the injured CNS remains unclear.
Recently, the heterogeneity of macrophages have come to light, with two general classes being described as classically or alternatively activated (21). While classically activated macrophages express high levels of pro-inflammatory cytokines such as TNF and IL-1β, and exhibit a robust respiratory burst (22), alternatively activated (tissue-building) macrophages express high levels of arginase-1 and several factors that play a role in promoting tissue homeostasis and recovery from insults (23). Several studies have shown the neuroprotective ability of alternatively activated macrophages in CNS injury (24-26) but what leads to, and sustains, this phenotype is unclear in the context of CNS trauma.
Here we show that the regulation of the T cell response to CNS injury is taking place in the draining deep cervical lymph nodes rather than at the site of injury. In line with this, surgical resection of the deep cervical lymph nodes results in impaired neuronal survival. We show that removal of Treg cells that leads to exaggerated response of Teff cells is associated with reduction in alternatively activated macrophages at the site of injury and leads to impaired neuronal survival. Exogenous supply of activated Treg cells, however, results in suppression of a neuroprotective IL-4 producing T cells, and consequently also results in suppression of alternatively activated macrophages at the site of injury. Thus, both depletion or addition of Treg cells are detrimental for neuronal survival after injury through regulation of macrophage phenotype.
Materials and Methods
Animals
Female C57Bl/6 (Stock #000664) and UBC-GFP (Stock #004353) mice were purchased from Jackson Laboratories (Bar Harbor, ME); DEREG mice were a gift from Dr. T. Sparwasser (Institute of Infection Immunology, Twincore, Germany); (16) KN2 mice were a gift from Dr. M. Mohrs (Trudeau Institute, Sarnac Lake, NY) (27). All animals were housed in temperature and humidity controlled rooms, maintained on a 12 h/12 h light/dark cycle (lights on 7:00 A.M.), and age-matched in each experiment. All strains were kept in identical housing conditions. All procedures complied with regulations of the Institutional Animal Care and Use Committee (ACUC) at The University of Virginia.
In vivo drug treatment
200 μg all-trans retinoic acid (Fisher) was dissolved in corn oil and injected i.p. every other day starting 3 days before injury. Diphtheria toxin was dissolved at 40 μg/kg in PBS and was injected into C57Bl/6 or DEREG mice two days before optic nerve injury and on the day of optic nerve injury. 250 μg anti-CD25 (clone PC-61) was injected into mice 8 days before optic nerve injury.
Retrograde labeling of retinal ganglion cells
Mice were anesthetized, and the skull was exposed and immobilized in a stereotactic device. Holes were drilled in the skull above the superior colliculus (bilaterally 2.9 mm caudal to bregma and 0.5 mm lateral to midline). One μL 4% Fluoro-gold was injected 2 mm below the meningeal surface at a rate of 0.5 μL/min using a Hamilton syringe and an automatic injector. The dye was allowed to diffuse into the tissue for 1 minute before the syringe was removed. The scalp was then sutured closed, and the mice allowed to recover on warming pads at 37° C before returning them to their cage.
Optic nerve injury
Mice were subjected to an optic nerve injury three days after stereotactic surgery. Briefly, mice were anesthetized with a 1:1:8 mixture of ketamine:xylazine:saline. An incision was made in the connective tissue above the sclera. The venous sinus around the optic nerve was retracted to expose the optic nerve, and the nerve was crushed using an N5 self-closing forceps 2 mm behind the globe for three seconds. The mice were then allowed to recover at 37° C on a warming pad before returning to their cages.
Retina excision
Mice were enucleated, and the cornea removed at the corenal limbus. The lens and the underlying vitreous were removed with forceps. The retina was separated from the sclera and pigment epithelium. Four cuts were made toward the optic disc, and the retina mounted on nitrocellulose paper and fixed in 4% PFA overnight. Pictures of all four quadrants of the retina were taken at equal distances form the optic disc of the retinas using an Olympus IX-71 microscope. The pictures were then counted by a blinded observer to determine the number of RGCs.
Deep cervical lymph node removal
Mice were anesthetized with a 1:1:8 mixture of ketamine:xylazine:saline. A 10 mm incision was made midline above the trachea. Salivary glands and sternocleidomastoid muscles were retracted bilaterally to expose the deep cervical lymph nodes. Deep cervical lymph nodes were removed using Dumont forceps, and the skin was sutured closed. Mice that received sham surgery had their deep cervical lymph nodes exposed, and then the skin was sutured. The mice were allowed to recover on a 37° C warming pad before returning to their cages. Mice were allowed to recover from surgery for at least two weeks before optic nerve injury.
Production of bone marrow chimeras
C57Bl/6 mice underwent split-dose lethal irradiation (350 rad, then 950 rad 48 hours later). Bone marrow cells were isolated by flushing out the femur and tibia of UBC-GFP mice. 1×107 bone marrow cells were injected into the irradiated mice 3 hours after the last irradiation. Mice were allowed to reconstitute for 6 weeks before being used in experiments.
T cell cultures
For Teff cultures, total lymph nodes were dissected, and a single cell suspension made by mashing through a 70 μm mesh. 3×106 cells/mL were incubated in T cell culture media supplemented with 1 μg/mL anti-CD3 (clone 145-2C11, ATCC stock # CRL-1975, antibody grown and isolated by UVA lymphocyte culture center), and 1 μg/mL anti-CD28 (clone 37.51, Bioxcell, Stock #BE0015-1). For iTreg cultures, the media was supplemented with 10 nM ATRA (Fisher), 5 ng/mL TGFβ (Peprotech), and 250 U/mL IL-2 (R&D). The cultures were maintained for 5 days before CD4+ T cells were isolated using magnetic bead separation (Miltenyi) and injected i.v. into C57Bl/6J mice.
Flow cytometry
Axillary and inguinal lymph nodes or deep cervical lymph nodes were isolated and mashed through a 70 μm strainer in PBS containing 1% BSA and 2 mM EDTA. The following antibodies were used, and are all from eBioscience unless otherwise noted: Foxp3-Alexa 488, CD4-PerCp Cy5.5, TCRβ-APC eFluor780, CD45-APC, CD8-eFluor 450, CD25-PE (BD Bioscience), IL-4-PE, IFN-γ-APC, and CD69-PE Cy7. For intranuclear staining, the cells were fixed overnight in Foxp3 Fix/Perm buffer (eBioscience) before incubating with Foxp3 antibody in FACS buffer containing 0.3% saponin (Fisher). For intracellular staining, mice were injected with 3 μg of BrefeldinA 5 hours before they were sacrificed. The cells were stained for extracellular markers before they were fixed in IC Fixation buffer (eBioscience) for 30 minutes, then permeabilized and stained for intracellular antigens in FACS buffer containing 0.3% saponin.
Macrophage skewing assay
Bone marrow was isolated from WT mice and cultured on untreated petri dishes in DMEM/F12 containing 10 ng/mL MCSF (eBioscience), 10% FCS, L-glutamine, and pen-strep (Invitrogen). The media was changed every 3 days, and macrophages were used after 8 days in vitro. The day before the macrophages were used, they were re-plated on TC-treated 24 well plates. CD4+ T cells from injured or uninjured deep cervical or skin-draining lymph nodes were isolated using magnetic bead separation (Miltenyi) and incubated at 1×106 cells/well in complete macrophage media. 24 hours after addition of T cells, the macrophages were washed 5x with PBS to remove the non-adherent T cells, and RNA was isolated from the macrophages.
Immunohistochemical staining of optic nerve tissue
For arginase-1 staining, mice were perfused transcardially with ice-cold PBS containing 4 U/mL heparin, then with 4% paraformaldehyde. Eyes were enucleated, and frozen on dry ice in OCT. Ten μm sections were cut on a Lyca cryostat and mounted on gelatin coated slides. Sections were then stained for arginase-1 (Santa Cruz Biotechnology, clone V20), CD68 (Biolegend, clone FA11), Iba1 (Biocare Medical, polyclonal) and GFP (Abcam, polyclonal). For CD4 and CD11b staining, mice were perfused transcardially with ice-cold PBS containing 4 U/mL heparin. Eyes were enucleated and frozen on dry ice in OCT. Ten μm sections were cut on a Lyca cryostat and mounted on gelatin coated slides. Slides were post-fixed in 3:1 acetone:ethanol at 4 degrees before staining with the flowing antibodies: CD4-FITC (eBioscience, clone GK-1.5), CD11b (Biolegend, clone M1/70), Foxp3-biotin (eBioscience, clone FKJ-16s). For Foxp3 and CD4 co-staining, CD4 was detected with an anti-fluorescein secondary antibody (Life Technologies) and FoxP3 was detected with Alexfluor 594 conjugated streptavidin (Jackson Immunochemical)
Results
A CD4+ T cell response in the CNS-draining deep cervical lymph nodes after CNS injury
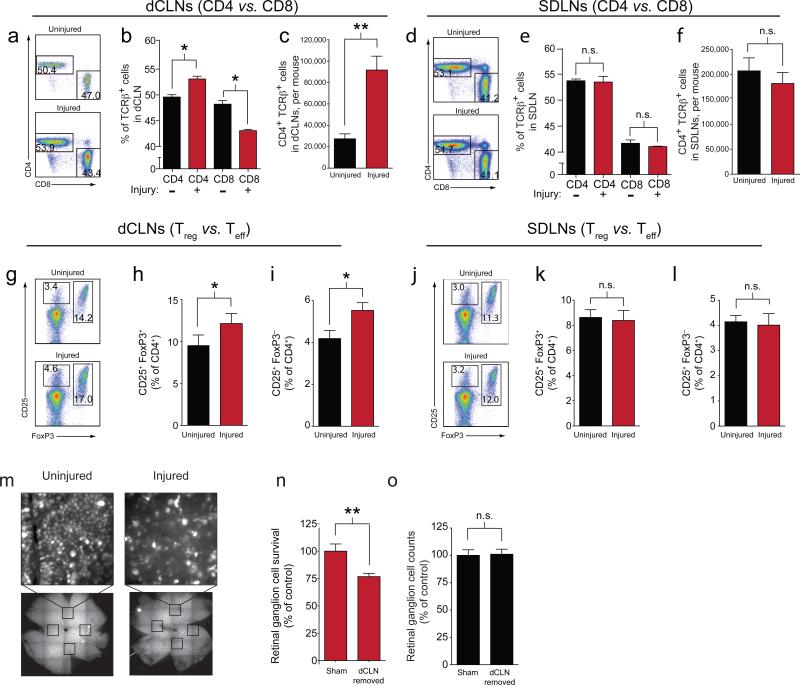
To determine where the immune response to CNS injury was occurring, we first examined CNS draining deep cervical lymph nodes (dCLN) as compared to skin draining lymph nodes (SDLN; axillary and inguinal) for T cell activation and proliferation upon CNS injury. We found an increase in the number and percentage of CD4+ T cells and a concurrent reduction in the percentage of CD8+ T cells in CNS-draining deep cervical lymph nodes (Fig. 1a-c). No change in the number or percentage of CD4+ T cells was observed in the skin-draining lymph nodes (Fig. 1d-f). When the induced CD4+ T cells were examined for sub-population (Treg vs. Teff), both activated Teff (CD4+CD25+Foxp3–) and Treg (CD4+Foxp3+) cells were increased in the dCLNs after the injury (Fig. 1g-i), but not in the skin-draining lymph nodes (Fig. 1j-l). To determine if the immune response in the deep cervical lymph node was playing an important role in the response to CNS injury, we used an optic nerve injury model, where retinal ganglion cells are pre-labeled with the neuronal tracer Fluoro-gold then the optic nerve is injured and the number of surviving retinal ganglion cells (RGCs) in the retina are quantified (Fig. 1m). This injury leads to a decrease in the number of retinal ganglion cells in mice that underwent the deep cervical lymph node removal than those that received a sham surgery (Fig. 1n), while their contralateral uninjured retinas did not display a loss of retinal ganglion cells (Fig. 1o).
Figure 1. The deep cervical lymph nodes display an immune response after CNS injury and their resection exacerbates neuronal survival.
(a) Flow cytometry of CD4+ and CD8+ lymphocytes in the deep cervical lymph nodes from uninjured mice or from mice 5 days post-injury. Numbers indicate percent CD4+ and CD8+ T cells, as a percentage of TCRβ+ cells. (b, c) Frequency of CD4+ and CD8+ as a percent of TCRβ+ lymphocytes (b) and number of CD4+TCRβ+ T cells (c) in the deep cervical lymph nodes, as quantified by flow cytometry 5 days after injury (n = 3 per group; *, p < 0.05; **, p < 0.01; Student's t-test; representative of > 3 experiments). (d) Flow cytometry of CD4+ and CD8+ lymphocytes in the skin-draining lymph nodes of uninjured mice or from mice 5 days post-injury. Numbers indicate percent CD4+ and CD8+ T cells, as a percentage of TCRβ+ cells. (e, f) Frequency of CD4+ and CD8+ T cells, as a percent of TCRβ+ cells (e) and number of CD4+ T cells (f) in the skin draining lymph nodes 5 days post-injury, as quantified by flow cytometry (n = 3 per group; Student's t-test; representative of > 3 experiments). (g) Flow cytometry of CD4+ lymphocytes in the deep cervical lymph node of uninjured mice or from mice 5 days post-injury. Numbers indicate percent activated Teff and Treg cells, as a percentage of CD4+ cells. (h, i) Frequency of Treg (h) and Teff (i) cells in the dCLNs as a percent of the uninjured dCLN (n = 6 per group; *, p < 0.05, Student's t-test, representative of two experiments). (j) Flow cytometry of CD4+ lymphocytes in the skin-draining lymph nodes of uninjured mice or from mice 5 days post-injury. Numbers indicate percent activated Teff and Treg cells, as a percentage of CD4+ cells. (k, l) Frequency of Treg (k) and Teff (l) cells in the SDLNs as a percent of the uninjured SDLN (n = 6 per group; Student's t-test; representative of two experiments). (m) Representative images of Fluoro-gold stained retinas from uninjured or injured eyes. Boxes represent fields counted for retinal ganglion cell quantification. (n) Neuronal survival of mice receiving sham surgery or undergoing deep cervical lymph node removal 2 weeks prior to injury, as assessed by Fluoro-gold staining. Survival is quantified as a percent of control survival (n = 11 sham and 12 dCLN removed; **, p < 0.01, Student's t-test; representative of two experiments). (o) Retinal ganglion cell counts of the contralateral uninjured retina of mice receiving sham surgery or undergoing deep cervical lymph node removal 2 weeks prior to injury, as assessed by Fluoro-gold staining. RGC counts are quantified as a percent of the control (n = 11 sham and 12 dCLN removed; Student's t-test; representative of two experiments).
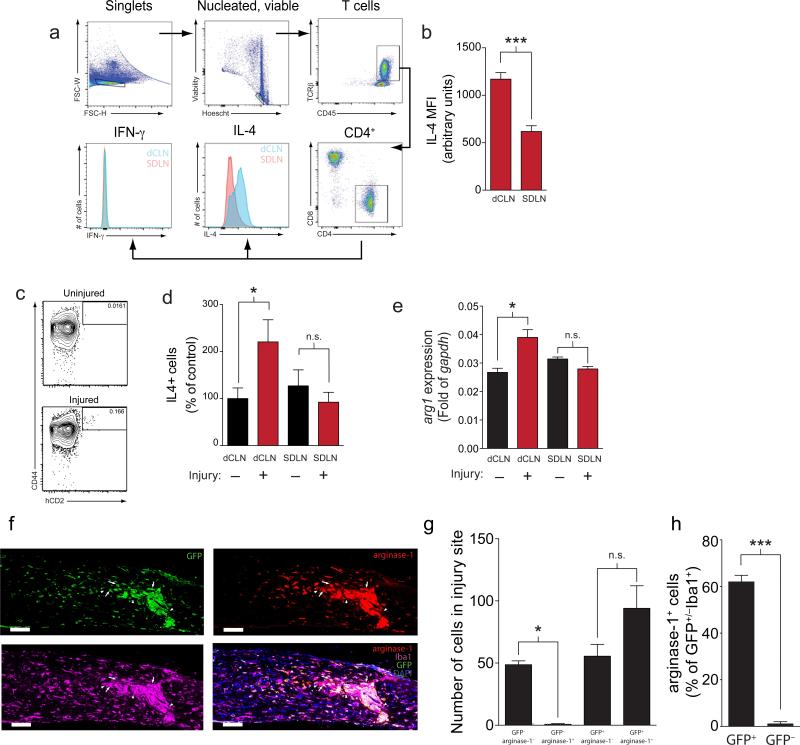
To determine if T cells from the injured dCLN displayed a different phenotype after CNS injury than the SDLN, we used flow cytometry to analyze the intracellular cytokines produced in the lymph nodes after injury. T cells from the dCLN displayed higher levels of IL-4 after optic nerve injury than those from the SDLN (Fig. 2a, b). To examine if this phenotype is induced by the injury, we used KN2 reporter mice that express hCD2 when IL-4 is being translated. In these mice, hCD2 expression is seen in CD44+ memory T cells (Fig. 2c), and this hCD2 expression is induced after injury in the dCLNs after injury, but not in the SDLNs (Fig. 2d). To determine if T cells induced after optic nerve injury in the draining lymph nodes are capable of supporting alternative activation of macrophages, we isolated T cells from injured and uninjured dCLNs and SDLNs and co-cultured them with a pure population of bone-marrow derived macrophages. T cells from the deep cervical lymph nodes of optic nerve-injured mice were able to support an alternative activation phenotype of bone marrow macrophages in vitro, while T cells obtained from SDLNs of injured mice or from dCLNs of uninjured mice were unable to promote this alternatively activated (tissue-building) phenotype of macrophages (Fig. 2e). This suggests that the injury indeed induces Teff cells in the draining dCLN that are capable of promoting a neuroprotective macrophage phenotype.
Figure 2. CNS injury promotes a milieu conducive to alternative activation of macrophages in the deep cervical lymph nodes.
(a) Gating strategy and representative staining of IL-4 production by CD4+ T cells in the draining deep cervical lymph nodes and skin-draining lymph nodes after CNS injury. (b) Quantification of the mean fluorescence intensity of IL-4 staining of CD4+ T cells in the deep cervical lymph node or skin-draining lymph node (n = 4 per group; ***, p < 0.001; Student's t-test; representative of two experiments). (c) Representative staining of hCD2 (IL-4) production by CD4+ T cells in the draining deep cervical lymph nodes in injured and uninjured mice. (d) Quantification of the number of hCD2+ staining of CD4+ T cells in the deep cervical lymph node or skin-draining lymph node in uninjured and injured mice (n = 5 per group; *, p < 0.05; Student's t-test; representative of two experiments). (e) arg1 mRNA expression of bone-marrow derived macrophages that had been co-cultured with CD4+ T cells from the indicated lymph nodes of mice with or without optic nerve injury for 24 hours (n = 3 per group; *, p < 0.05; One-way ANOVA with Bonferroni's post-test; representative of > 3 experiments). (f) Representative images of injured optic nerves of GFP ⇒ C57Bl/6 bone marrow chimeras stained for arginase-1 and Iba1. Arrowheads point to GFP– radio-resistant microglia, while arrows point to infiltrating macrophages (scale bar = 100 μm). (g) Quantification of percent of Iba1+ cells in the injured optic nerve that are GFP+arginase-1+, GFP+arginase-1–, GFP–arginase-1+, and GFP–arginase-1– (n = 3 per group; One-way ANOVA with Bonferroni's post-test; *, p < 0.05). (h) Quantification of the percent of GFP+ and GFP– cells that are arginase-1+ in the injured optic nerve (n = 3 per group; Student's t-test; ***, p < 0.001).
Because we observed that T cells in the draining lymph node were able to promote an alternative activation of macrophages, we addressed a possibility that T cells are controlling the phenotype of the infiltrating monocytes/macrophages. Arginase-1 expressing macrophages (M2-type) have been previously described to support neuronal survival after CNS injury (24-26, 28). Indeed, using immunohistochemistry of injured optic nerves we demonstrate that arginase-1 expression is induced in the injury site (Fig. 2f), whereas there is no detectable arginase-1 staining in the uninjured optic nerves (Fig. S1a). We established GFP ⇒ C57Bl/6 bone marrow chimeric mice (29), whose peripheral immune system is replaced by the GFP+ bone marrow, but which have a significant number of GFP– microglia in the optic nerve (Fig. S1b). Therefore, despite the issues inherent with bone marrow transplantation following irradiation (30), the large majority of the engrafted Iba1 positive cells in the uninjured CNS of chimeric mice are of non-GFP origin. It is, therefore, conceivable to assume that an increase of GFP+ cells after injury results primarily from their peripheral recruitment of monocyte-derived macrophages, although, as stated above, the procedure has its limitation. In the chimeric mice, most of the GFP+Iba1+ cells in the site of the injury were arginase-1 positive, suggesting that at least the majority of the infiltrating cells were highly skewed after injury. However, significantly fewer of the radio-resistant GFP–Iba1+ microglia were arginase-1 positive, suggesting that macrophages infiltrating from the periphery are the primary source of alternatively activated myeloid cells (Fig. 2g, h). This preferential skew of infiltrating myeloid cells suggests that their phenotype switch took place in the periphery prior to infiltration rather than in the CNS parenchyma. These results in line with previous findings, suggesting that monocytes with an alternatively activated phenotype are arriving from a periphery through a unique path into the injured CNS (25).
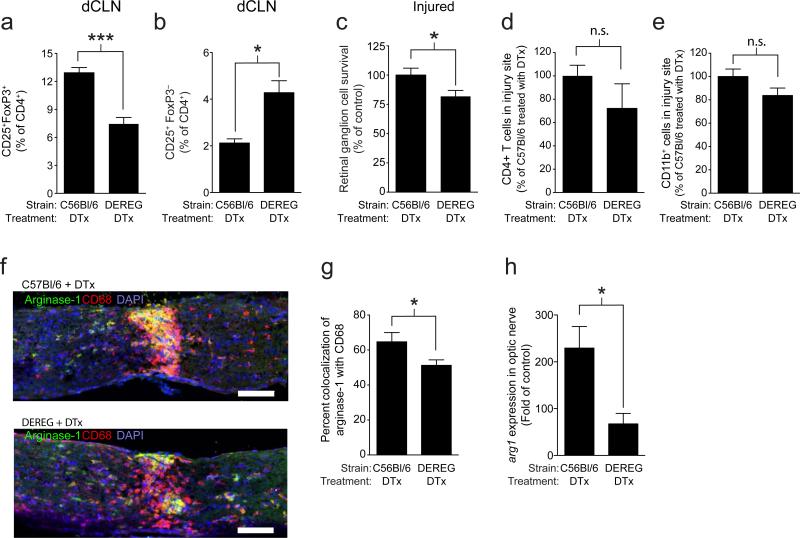
Depletion of Treg exacerbates neurodegeneration after CNS injury
The contribution of different subsets of T cells to neuronal survival after CNS injury has been intensively studied (4, 5, 19, 31, 32), yet their role in this post-injury neuronal survival remains controversial (8, 10, 33). Because Treg cells are known to exert asymmetric control of T cell responses in non-pathological situations (34), we tested the hypothesis that Treg cells were responding to injury in the draining lymph nodes, where they controlled the phenotype of Teff cells. We used DEREG mice (16), which express the diphtheria toxin receptor under the Foxp3 promoter to assess the effect of Treg depletion on neuronal survival. Treatment of these mice with 40 μg/kg of diphtheria toxin (DTx) 2 days before injury completely eliminates Treg cells in the bloodstream (Fig. S2a). Seven days after injury, the DEREG mice treated with DTx still displayed decreased numbers of Treg cells in their CNS-draining deep cervical lymph nodes (Fig. 3a), and an increase in the number of activated Teff cells in the deep cervical and skin-draining lymph nodes (Fig 3b, S2b).
Figure 3. Alleviation of Treg suppression after CNS injury leads to a reduced neuronal survival after optic nerve injury.
(a, b) Bar graphs represent quantification of flow cytometry analysis of the deep cervical lymph nodes of DEREG or wild type littermates treated with DTx two days before injury and on the day of injury, showing percent of CD25+Foxp3+ Treg cells (a) and of CD25+Foxp3– Teff cells (b), graphed as a percentage of TCRβ+CD4+ cells (n = 12 wild type and 9 DEREG treated mice; ***, p < 0.001; *, p < 0.05; Student's t-test; representative of three experiments). (c) Neuronal survival after optic nerve injury in DEREG and wild type mice injected with 40 μg/kg DTx two days before injury and on the day of injury. Survival is quantified as a percent of control survival. (n = 19 wild type and 25 DEREG; *, p < 0.05, Student's t-test, representative of three experiments). (d) Quantification of the number of CD4+ T cells found in the injury site of DEREG mice treated with DTx normalized to the number of CD4+ T cells found in the injury site of C57Bl/6 mice treated with DTx. (n = 3 per group; Student's t-test; representative of 2 experiments) (e) Quantification of the number of CD11b+ cells found in the injury site, normalized to the number of CD11b+ T cells found in the injury site of C57Bl/6 mice treated with DTx. (n = 3 C57Bl/6 treated with DTx and 9 DEREG treated with DTx, Student's t-test; representative of 2 experiments) (f) Representative images of CD68 and arginase-1 in injured optic nerve of DEREG and WT mice treated with two doses of 40 μg/kg DTx. (g) Arginase-1+ area graphed as a percent of CD68+ area in C57Bl/6 or DEREG mice treated with DTx (n = 3 C57Bl/6 treated with DTx and 8 DEREG treated with DTx; *, p < 0.05; Student's t-test). (h) Quantitative PCR for arg1 of optic nerves of C57Bl/6 or DEREG mice treated with 40 μg/kg DTx 2 days before injury and on the day of injury normalized to arg1 expression in the contralateral uninjured nerve (n = 7 C57Bl/6 treated with DTx and 4 DEREG treated with DTx; *, p < 0.05; Student's t-test; representative of 2 experiments).
To test the effect of Treg cell depletion on CNS injury, we again used the optic nerve crush injury model. As expected from previous studies (35), DEREG mice treated with DTx, and thus depleted of Treg cells, showed a decrease in the number of surviving RGCs seven days after injury, as compared to wild type mice treated with DTx (Fig. 3c). We examined the contralateral retina of injured mice (Fig. S2c) and histological sections of uninjured mice treated with DTx (Fig. S2d), which did not display any loss of RGCs or immune cell infiltrate, suggesting DTx by itself did not have destructive effects on uninjured CNS tissue. Furthermore, there was no difference in neuronal survival in C57Bl/6 mice treated with saline or DTx (Fig. S2e), confirming that DTx treatment was not causing non-specific effects at the dose we are using. To further establish the role of depletion of Treg cells, we used an anti-CD25 antibody, which depletes regulatory T cells (that express high levels of CD25 (36)). In mice that were Treg-depleted, there was a decrease in the number of CD25+Foxp3+ Treg cell in the deep cervical lymph node even 7 days after optic nerve injury, and a corresponding decrease in neuronal survival (Fig. S2f, g), consistent with the results seen in DEREG mice.
Although no change in overall numbers of CD4+ T cells (Fig. 3d) or CD11b+ myeloid cells (Fig. 3e) at the site of injury was found, the phenotype of accumulated macrophages was altered in DEREG mice treated with DTx. A significant decrease in arginase-1 expressing CD68 (a marker of activated macrophages) cells was evident (Fig. 3f, g), suggesting a decrease in alternatively activated macrophages (M2-type) after injury in Treg-depleted mice. No difference in the total amount of CD68+ area was detected (Fig. S3a). To confirm the histological observations, we also examined the injured tissue by PCR. The mRNA expression of arg1, the gene for arginase-1, was reduced in DEREG mice, confirming the decrease in alternatively activated macrophages after Treg depletion (Fig. 3h).
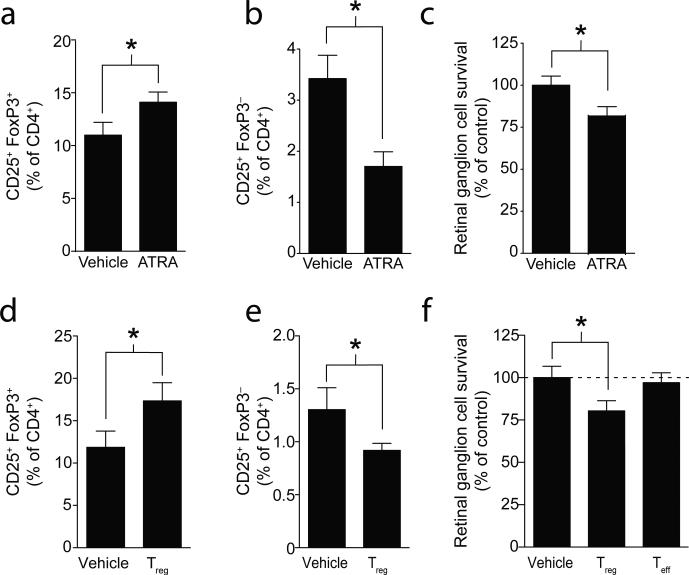
Exogenous Treg cells inhibit a beneficial response to CNS injury
A complete depletion of Treg cells using DEREG mice resulting in impaired outcome of CNS injury in our optic nerve crush injury model (Fig. 3c). However, the question still remains whether increased activity of Treg cells would conversely offer a benefit after CNS injury. First, we tested the physiological outcome of Treg manipulation via potentiation of Treg suppressive function by treating mice with all-trans retinoic acid (ATRA), which induces differentiation of Treg cells (37), stabilizes the Treg phenotype (38), and makes Treg cells more suppressive (38). As expected, treatment of mice with ATRA increased the Treg population in the deep cervical lymph nodes after injury (Fig. 4a) but surprisingly not in the SDLN (Fig. S4a) and resulted in a decrease of activated effector T cells in the deep cervical and skin-draining lymph nodes (Fig. 4b, S4b). Interestingly, and in line with some reports (19) but contrary to other previous findings (7), mice treated with ATRA exhibited decreased neuronal survival compared to vehicle treated mice (Fig. 4c), suggesting that induction of highly suppressive Treg cells limits the protective Teff responses. To rule out a possible in vivo effect of ATRA on cells other than T cells, we differentiated Treg cells in vitro (iTreg) using ATRA and TGFβ (Fig. S4c). Injection of iTreg cells into CNS-injured mice also resulted in an increase in Treg cells (Fig. 4d) and attenuation of their activated Teff response to injury in the deep cervical lymph nodes (Fig. 4e), but no change in the number of Treg cells and Teff cells in the skin-draining lymph nodes (data not shown) and a reduction in neuronal survival (Fig. 4f). Mice treated with Teff cells (that were activated without TGFβ and ATRA, and that contained only ~3% Foxp3+ Treg compared to ~85% in Treg designated culture conditions) did not show any change in neuronal survival (Fig. 4f), possibly due to the large number of Teff cells already present in wild type mice.
Figure 4. Potentiation of Treg function impairs neuronal survival after optic nerve injury.
(a, b) Bar graphs represent quantification of flow cytometry analysis of the deep cervical lymph nodes of wild type mice treated with vehicle or ATRA showing percent of CD25+Foxp3+ Treg cells (a) and of CD25+Foxp3– Teff cells (b), graphed as a percentage of TCRβ+CD4+ cells (n = 7 vehicle treated and n = 9 ATRA treated; *, p < 0.05, Student's t-test; representative of two experiments (c) Retinal ganglion cell survival in wild type mice treated with vehicle or ATRA. Survival is quantified as a percent of control survival. (n = 7, vehicle and n = 9, ATRA; *, p < 0.05, Student's t-test, representative of two experiments). (d, e) Bar graphs represent quantification of flow cytometry analysis of deep cervical lymph nodes of wild type mice treated with vehicle or 1×106 exogenous Treg cells one day before injury and one day after injury, showing percent of CD25+Foxp3+ Treg cells (d) and of CD25+Foxp3– Teff cells (e), graphed as a percentage of TCRβ+CD4+ cells (n = 12 Treg cells injected and n = 13 vehicle injected; *, p < 0.05, Student's t-test). (f) Neuronal survival in wild type mice injected with vehicle, 1×106 Treg or 1×106 Teff cells two days before injury and on the day of injury. Survival is quantified as a percent of control survival (n = 13 vehicle injected, 12 Treg cell injected, and 7 Teff cell injected; *, p < 0.05, One-way ANOVA with Bonferroni's post-test; representative of two experiments).
Interestingly, 7 days after Treg injection, only very few of the injected cells were found in the dCLN, despite of a substantial increase in overall Treg numbers (Fig. S4d). These results suggest that the injected Treg cells induce endogenous T cell differentiation, possibly through their high levels of secreted and membrane bound TGFβ [(39, 40).
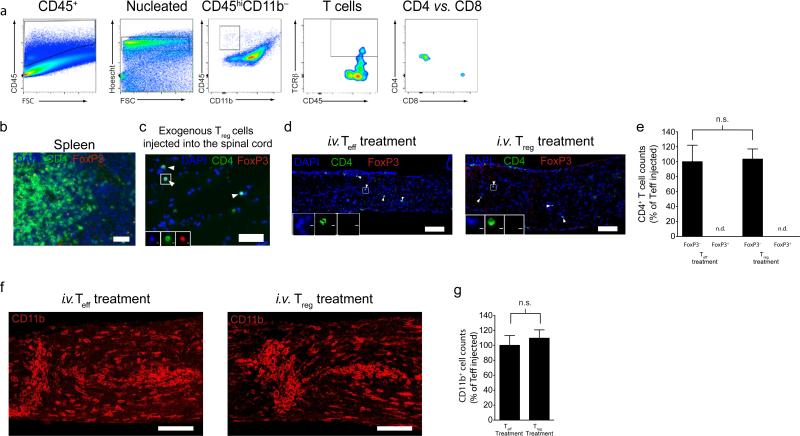
Treg cells do not infiltrate the injured CNS after injury
Because Treg cells are exerting a negative effect on the outcome to CNS injury, we sought to determine if Treg cells were also gaining access to the site of injury. Upon injury, there is the influx of Teff cells to the CNS parenchyma (Fig. 5a). Despite being able to visualize Treg cells using Foxp3 immunolabeling in the spleen (Fig. 5b) and in spinal cords that had been injected directly with Treg cells (Fig. 5c), we did not see Treg cells in the parenchyma of the injured optic nerve in animals after exogenous i.v. injection of Treg cells (Fig. 5d) or in injured wild-type mice, wild-type mice injected with Teff cells, DEREG mice treated with DTx, and wild-type mice treated with DTx (data not shown). Furthermore, there was no difference in the number of CD4+ Teff cells at the injury site of Treg-treated mice (Fig. 5e). Therefore, it seems unlikely that acute manipulation of Treg cells in our experimental paradigms is affecting neuronal survival through the migration of effector T cells in to the site of the injury. Next, to determine if addition of Treg cells could affect monocyte migration to the injured CNS, we quantified the number of CD11b+ cells accumulating at the site of injury. As with CD4+ T cells, there was no change in the number of CD11b+ cells that migrated to the site of injury in Treg-treated mice (Fig. 5f, g), further suggesting that Treg cells are not controlling immune cell migration in this injury model.
Figure 5. Boost with exogenous Treg cells does not alter immune cell infiltration into the injury site.
(a) Representative gates of flow cytometry of CD4+ and CD8+ lymphocytes in the injured optic nerve seven days post-injury. Optic nerves were pooled from eight mice, and cells were stained for analysis by flow cytometry. (b) Representative image from splenic tissue stained for CD4 (green) and Foxp3 (red) (scale bar = 100 μm). (c) Representative image from spinal cord tissue directly injected (ex vivo) with in vitro induced regulatory T cells stained for CD4 (green) and Foxp3 (red) (scale bar = 50 μm). (d) Representative images of CD4+Foxp3– and CD4+Foxp3+ T cells in the optic nerve parenchyma of Teff- and Treg-treated mice (scale bar = 100 μm). (e) Quantification of the number of CD4+Foxp3– and CD4+Foxp3+ T cells in the optic nerve parenchyma of Teff and Treg treated mice (n = 4 mice per group; One-way ANOVA with Bonferroni's post-test; scale bar = 100 μm). (f) Representative images of CD11b+ cells in injury site of the optic nerve of Teff- and Treg-treated mice (scale bar = 100 μm). (g) Quantification of the number of CD11b+ cells in injury site of the optic nerve of Teff and Treg treated mice (n = 9 mice per group; Student's t-test; representative of two experiments).
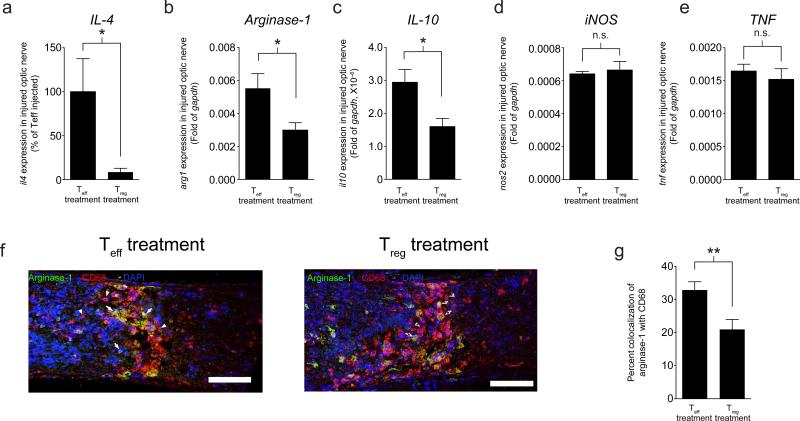
To determine if T cell-derived cytokines are affected by Treg manipulation after CNS injury, we examined the mRNA expression of genes from the optic nerve of injured mice treated with either Teff or Treg cells. Mice treated with Treg cells display a dramatic decrease in the amount of IL-4 mRNA compared to mice treated with Teff cells (Fig. 6a), suggesting a change in the Th2 response to damage at the injury site with Treg treatment. To determine if these changes are having effects downstream on myeloid cells after CNS injury, we examined markers of myeloid skewing in the injured optic nerves of mice treated with Treg cells. Indeed, Treg treated mice displayed a decrease in the mRNA expression of alternatively activated macrophage markers arg1 and il10, while there was no change in the classical activation markers nos2 and tnf (Fig. 6b-e). To further demonstrate that there was a loss of alternative activation of macrophages in Treg injected mice, we examined colocalization between CD68, a marker of activated myeloid cells, and argniase1 by immunofluorescence. While Teff injected mice displayed marked expression of arginase-1 in the CD68+ fraction 7 days after injury, injection of Treg cells led to a decrease in arginase-1 expression by myeloid cells (Fig. 6f, g), further demonstrating that both addition and deletion of Treg cells is detrimental in CNS trauma through their effects on the innate immune response at the site of injury.
Figure 6. Treg cell injection leads to a loss of an alternative activation phenotype of myeloid cells at the site of injury.
Optic nerves of Teff- and Treg- cell injected mice were collected 7 days post injury and examined for expression of the following genes relative to expression of gapdh (a) il4 (n = 11 per group *, p < 0.05; Student's t-test; representative of two experiments); (b) arg1; (c) il10; (d) nos2; (e) tnf; (b-e; n = 6 per group; *, p < 0.05; Student's t-test); (f) Representative images of Teff- and Treg- cell injected mice 7 days after injury stained for arginase-1 (green) and CD68 (red) (scale bar = 100 μm). (g) Arginase-1+ area graphed as a percent of CD68+ area in Teff- and Treg- cell injected mice 7 days post-injury (n = 9 Teff cell injected and 6 Treg cell injected; **, p < 0.01; Student's t-test; representative of two experiments).
Discussion
There has been an ongoing debate about the role of Treg cells in CNS injury and in neurodegenerative conditions. We show here that complete depletion of Treg cells using DEREG mice, a manipulation which has been shown to lead to development of numerous organ-specific autoimmune diseases (16), leads to increased neurodegeneration after CNS trauma. However, the same deleterious effect on neuronal survival can be seen when Treg numbers are increased either by pharmacological compounds or by exogenous supply of Treg cells. Changes in Treg numbers correlate with the phenotype of macrophages populating the injury site, with alternatively activated macrophages being spontaneously induced by the injury, yet inhibited by Treg cell addition or overruled by an exaggerated immune response as a result of Treg cell depletion.
Early work in models of stroke and Parkinson's disease showed that depletion of Treg cells led to increased neurodegeneration, while increases in Treg cell numbers and function improved disease outcome (10, 41). More recent work, using the same manipulations, has shown that Treg cells play a detrimental role after CNS injuries (7), supporting the hypothesis that they are suppressing a beneficial autoimmune response (19). There are several factors that may have contributed to these disparate findings. There are technical challenges with the current Treg depletion strategies that have hindered interpretation of depletion studies, such as targeting of activated effector cells with anti-CD25 treatment (42, 43). Furthermore, several studies have shown that Treg cells have the potential to downregulate Foxp3 and become effector cells, especially when placed in lymphopenic or inflammatory conditions (38, 44, 45), probably due to heterogeneity in the fate commitment of the Treg cell population (46), complicating transfer experiments into mice with abnormal adaptive immune systems. However, the conditions that drive this switch from Treg to Teff, and relevance of these models in vivo, is still a matter of debate (47). Although DTx treatment may have indirect effects, overall the DEREG mouse offers a unique model for Treg deletion in vivo by both avoiding targeting CD25, indirectly affecting activated Teff, and avoiding cell transfer, which inevitably changes the cell phenotype. Therefore, although imperfect, DEREG model presents the best currently available model for Treg depletion.
Our work further addresses the question of how Treg cells are affecting the outcome from CNS injury. While we show that Treg cells have profound effects on neuronal survival from injury, they are not found at the site of the injury, but are rather enriched in the draining lymph node. Treg cells are known to exert asymmetric control of T cell responses in non-pathological situations (34), raising the possibility that these Treg cells are exerting their action on the phenotype of Teff cells in the draining lymph node. The Teff cells, in turn, direct the phenotype of the infiltrating innate immune cells. Previous works demonstrated that precursors for alternatively activated macrophages arrive the injured CNS through a unique path of the choroid plexus (25) and are coming “pre-determined” to differentiate into alternatively activated macrophages.
Several studies have shown that alternative activation of macrophages is a beneficial response to CNS injury (25, 28) Tissue-building macrophages produce growth factors such as IGF1, VEGF, TGFβ, and factors that remodel the extracellular matrix such as MMPs and RELMα, and promote a tissue building phenotype in injured tissue (21). T cells, and specifically Th2 effector cells, produce several cytokines, such as IL-4 for example, that can induce alternatively activated macrophages (48). Our results suggest that T cells induced in the CNS-draining deep cervical lymph nodes control the phenotype of the infiltrating monocytes, and future studies need to concentrate on a better understanding the molecular interaction between T cells and myeloid cells that results in myeloid cells of a particular phenotype to migrate to the site of injury. There potentially could be additional mediators between T cell response and the phenotype of macrophages recruited to the site of injury. It is also unknown whether T cells recirculate between the injured CNS site and the draining deep cervical lymph nodes. If such a recirculation occurs, T cell-macrophage interaction could potentially take place in three different sites – the site of injury, the lymph nodes and blood. Although we show here that removal of deep cervical lymph nodes is detrimental for neuronal survival, we have not addressed if their removal after the injury has been inflicted could affect the phenotype of macrophages and, subsequently, neuronal survival.
Our results support the notion that a spontaneous immune response after CNS trauma is beneficial and is tightly regulated by Treg cells (19). Elimination of Treg leads to an excessive immune response, which is detrimental for injured tissue. However, injection of Treg cells or potentiation of their suppressive function inhibits a spontaneous immune response to injury and also results in impaired neuronal survival. Further works should be aimed at understanding the divergent properties of Treg cells that lead to this dichotomous response to injury and finding the compounds that could alleviate Treg function yet preserve the beneficial nature/phenotype of Teff cells. Without better understanding of Teff/Treg interactions after CNS injury, therapies for CNS injuries that primarily target the Treg compartment should be taken with extreme caution as alteration of Treg may result in impaired outcome of CNS trauma.
Supplementary Material
Acknowledgments
We thank Shirley Smith for editing the manuscript. We thank the members of the Kipnis lab for their valuable comments during multiple discussions of this work.
This work was supported by a grant from the National Institute of Neurological Disorders and Stroke, NIH (NS061973 award to J. K).
References
- 1.Yoles E, Schwartz M. Degeneration of spared axons following partial white matter lesion: implications for optic nerve neuropathies. Experimental Neuroloy. 1998;153:1–7. doi: 10.1006/exnr.1998.6811. [DOI] [PubMed] [Google Scholar]
- 2.Davalos D, Grutzendler J, Yang G, Kim JV, Zuo Y, Jung S, Littman DR, Dustin ML, Gan WB. ATP mediates rapid microglial response to local brain injury in vivo. Nat Neurosci. 2005;8:752–758. doi: 10.1038/nn1472. [DOI] [PubMed] [Google Scholar]
- 3.Ransohoff RM. Chemokines and chemokine receptors: standing at the crossroads of immunobiology and neurobiology. Immunity. 2009;31:711–721. doi: 10.1016/j.immuni.2009.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moalem G, Leibowitz-Amit R, Yoles E, Mor F, Cohen IR, Schwartz M. Autoimmune T cells protect neurons from secondary degeneration after central nervous system axotomy. Nat Med. 1999;5:49–55. doi: 10.1038/4734. [DOI] [PubMed] [Google Scholar]
- 5.Serpe CJ, Kohm AP, Huppenbauer CB, Sanders VM, Jones KJ. Exacerbation of facial motoneuron loss after facial nerve transection in severe combined immunodeficient (scid) mice. J Neurosci. 1999;19:Rc7. doi: 10.1523/JNEUROSCI.19-11-j0004.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kipnis J, Avidan H, Markovich Y, Mizrahi T, Hauben E, Prigozhina TB, Slavin S, Schwartz M. Low-dose gamma-irradiation promotes survival of injured neurons in the central nervous system via homeostasis438 driven proliferation of T cells. European Journal of Neuroscience. 2004;19:1191–1198. doi: 10.1111/j.1460-9568.2004.03207.x. [DOI] [PubMed] [Google Scholar]
- 7.Kleinschnitz C, Kraft P, Dreykluft A, Hagedorn I, Gobel K, Schuhmann MK, Langhauser F, Helluy X, Schwarz T, Bittner S, Mayer CT, Brede M, Varallyay C, Pham M, Bendszus M, Jakob P, Magnus T, Meuth SG, Iwakura Y, Zernecke A, Sparwasser T, Nieswandt B, Stoll G, Wiendl H. Regulatory T cells are strong promoters of acute ischemic stroke in mice by inducing dysfunction of the cerebral microvasculature. Blood. 2013;121:679–691. doi: 10.1182/blood-2012-04-426734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhao W, Beers DR, Liao B, Henkel JS, Appel SH. Regulatory T lymphocytes from ALS mice suppress microglia and effector T lymphocytes through different cytokine-mediated mechanisms. Neurobiol Dis. 2012;48:418–428. doi: 10.1016/j.nbd.2012.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ren X, Akiyoshi K, Vandenbark AA, Hurn PD, Offner H. CD4(+)FoxP3(+) regulatory T-cells in cerebral ischemic stroke. Metab Brain Dis. 2010 doi: 10.1007/s11011-010-9226-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reynolds AD, Banerjee R, Liu JN, Gendelman HE, Mosley RL. Neuroprotective activities of CD4+CD25+ regulatory T cells in an animal model of Parkinson's disease. Journal of Leukocyte Biology. 2007;82:1083–1094. doi: 10.1189/jlb.0507296. [DOI] [PubMed] [Google Scholar]
- 11.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 2003;4:330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 12.Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science. 2003;299:1057–1061. [PubMed] [Google Scholar]
- 13.Khattri R, Cox T, Yasayko SA, Ramsdell F. An essential role for Scurfin in CD4+CD25+ T regulatory cells. Nat Immunol. 2003;4:337–342. doi: 10.1038/ni909. [DOI] [PubMed] [Google Scholar]
- 14.Zhou R, Horai R, Silver PB, Mattapallil MJ, Zarate-Blades CR, Chong WP, Chen J, Rigden RC, Villasmil R, Caspi RR. The living eye “disarms” uncommitted autoreactive T cells by converting them to Foxp3(+) 24 regulatory cells following local antigen recognition. J Immunol. 2012;188:1742–1750. doi: 10.4049/jimmunol.1102415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thornton AM, Shevach EM. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med. 1998;188:287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lahl K, Loddenkemper C, Drouin C, Freyer J, Arnason J, Eberl G, Hamann A, Wagner H, Huehn J, Sparwasser T. Selective depletion of Foxp3(+) regulatory T cells induces a scurfy-like disease. Journal of Experimental Medicine. 2007;204:57–63. doi: 10.1084/jem.20061852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fontenot JD, Rasmussen JP, Williams LM, Dooley JL, Farr AG, Rudensky AY. Regulatory T cell lineage specification by the forkhead transcription factor foxp3. Immunity. 2005;22:329–341. doi: 10.1016/j.immuni.2005.01.016. [DOI] [PubMed] [Google Scholar]
- 18.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self480 tolerance causes various autoimmune diseases. J Immunol. 1995;155:1151–1164. [PubMed] [Google Scholar]
- 19.Kipnis J, Mizrahi T, Hauben E, Shaked I, Shevach E, Schwartz M. Neuroprotective autoimmunity: Naturally occurring CD4(+)CD25(+) regulatory T cells suppress the ability to withstand injury to the central nervous system. Proceedings of the National Academy of Sciences of the United States of America. 2002;99:15620–15625. doi: 10.1073/pnas.232565399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reddy J, Illes Z, Zhang X, Encinas J, Pyrdol J, Nicholson L, Sobel RA, Wucherpfennig KW, Kuchroo VK. Myelin proteolipid protein-specific CD4+CD25+ regulatory cells mediate genetic resistance to experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A. 2004;101:15434–15439. doi: 10.1073/pnas.0404444101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gordon S, Martinez FO. Alternative activation of macrophages: mechanism and functions. Immunity. 2010;32:593–604. doi: 10.1016/j.immuni.2010.05.007. [DOI] [PubMed] [Google Scholar]
- 22.Chawla A, Nguyen KD, Goh YP. Macrophage-mediated inflammation in metabolic disease. Nat Rev Immunol. 2011;11:738–749. doi: 10.1038/nri3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brancato SK, Albina JE. Wound macrophages as key regulators of repair: origin, phenotype, and function. Am J Pathol. 2011;178:19–25. doi: 10.1016/j.ajpath.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kigerl KA, Gensel JC, Ankeny DP, Alexander JK, Donnelly DJ, Popovich PG. Identification of two distinct macrophage subsets with divergent effects causing either neurotoxicity or regeneration in the injured mouse spinal cord. J Neurosci. 2009;29:13435–13444. doi: 10.1523/JNEUROSCI.3257-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shechter R, Miller O, Yovel G, Rosenzweig N, London A, Ruckh J, Kim KW, Klein E, Kalchenko V, Bendel P, Lira SA, Jung S, Schwartz M. Recruitment of beneficial M2 macrophages to injured spinal cord is orchestrated by remote brain choroid plexus. Immunity. 2013;38:555–569. doi: 10.1016/j.immuni.2013.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.David S, Kroner A. Repertoire of microglial and macrophage responses after spinal cord injury. Nat Rev Neurosci. 2011;12:388–399. doi: 10.1038/nrn3053. [DOI] [PubMed] [Google Scholar]
- 27.Mohrs K, Wakil AE, Killeen N, Locksley RM, Mohrs M. A Two-Step Process for Cytokine Production Revealed by IL-4 Dual-Reporter Mice. Immunity. 2005;23:419–429. doi: 10.1016/j.immuni.2005.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fenn AM, Hall JC, Gensel JC, Popovich PG, Godbout JP. IL-4 Signaling Drives a Unique Arginase+/IL-1β+ Microglia Phenotype and Recruits Macrophages to the Inflammatory CNS: Consequences of Age-Related Deficits in IL-4Rα after Traumatic Spinal Cord Injury. J Neurosci. 2014;34:8904–8917. doi: 10.1523/JNEUROSCI.1146-14.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shechter R, London A, Varol C, Raposo C, Cusimano M, Yovel G, Rolls A, Mack M, Pluchino S, Martino G, Jung S, Schwartz M. Infiltrating blood-derived macrophages are vital cells playing an anti-inflammatory role in recovery from spinal cord injury in mice. PLoS Med. 2009;6:e1000113. doi: 10.1371/journal.pmed.1000113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Derecki NC, Cronk JC, Lu Z, Xu E, Abbott SB, Guyenet PG, Kipnis J. Wild-type microglia arrest pathology in a mouse model of Rett syndrome. Nature. 2012;484:105–109. doi: 10.1038/nature10907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lu HZ, Xu L, Zou J, Wang YX, Ma ZW, Xu XM, Lu PH. Effects of autoimmunity on recovery of function in adult rats following spinal cord injury. Brain Behavior and Immunity. 2008;22:1217–1230. doi: 10.1016/j.bbi.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 32.Ling C, Sandor M, Suresh M, Fabry Z. Traumatic injury and the presence of antigen differentially contribute to T-cell recruitment in the CNS. J Neurosci. 2006;26:731–741. doi: 10.1523/JNEUROSCI.3502-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jones TB, Ankeny DP, Guan Z, McGaughy V, Fisher LC, Basso DM, Popovich PG. Passive or active immunization with myelin basic protein impairs neurological function and exacerbates neuropathology after spinal cord injury in rats. J Neurosci. 2004;24:3752–3761. doi: 10.1523/JNEUROSCI.0406-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tian L, Altin JA, Makaroff LE, Franckaert D, Cook MC, Goodnow CC, Dooley J, Liston A. Foxp3+ regulatory T cells exert asymmetric control over murine helper responses by inducing Th2 cell apoptosis. Blood. 2011;118:1845–1853. doi: 10.1182/blood-2011-04-346056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bettelli E, Baeten D, Jäger A, Sobel RA, Kuchroo VK. Myelin oligodendrocyte glycoprotein-specific T and B cells cooperate to induce a Devic-like disease in mice. J Clin Invest. 2006;116:2393–2402. doi: 10.1172/JCI28334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Setiady YY, Coccia JA, Park PU. In vivo depletion of CD4+FOXP3+ Treg cells by the PC61 anti-CD25 monoclonal antibody is mediated by FcgammaRIII+ phagocytes. Eur J Immunol. 2010;40:780–786. doi: 10.1002/eji.200939613. [DOI] [PubMed] [Google Scholar]
- 37.Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, Cheroutre H. Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science. 2007;317:256–260. doi: 10.1126/science.1145697. [DOI] [PubMed] [Google Scholar]
- 38.Zhou X, Kong N, Wang J, Fan H, Zou H, Horwitz D, Brand D, Liu Z, Zheng SG. Cutting edge: all-trans retinoic acid sustains the stability and function of natural regulatory T cells in an inflammatory milieu. J Immunol. 2010;185:2675–2679. doi: 10.4049/jimmunol.1000598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tran DQ, Andersson J, Wang R, Ramsey H, Unutmaz D, Shevach EM. GARP (LRRC32) is essential for the surface expression of latent TGF550 beta on platelets and activated FOXP3+ regulatory T cells. Proc Natl Acad Sci U S A, United States. 2009:13445–13450. doi: 10.1073/pnas.0901944106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sakaguchi S, Yamaguchi T, Nomura T, Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133:775–787. doi: 10.1016/j.cell.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 41.Liesz A, Suri-Payer E, Veltkamp C, Doerr H, Sommer C, Rivest S, Giese T, Veltkamp R. Regulatory T cells are key cerebroprotective immunomodulators in acute experimental stroke. Nat Med. 2009;15:192–199. doi: 10.1038/nm.1927. [DOI] [PubMed] [Google Scholar]
- 42.Johnson BD, Jing W, Orentas RJ. CD25+ regulatory T cell inhibition enhances vaccine-induced immunity to neuroblastoma. J Immunother. 2007;30:203–214. doi: 10.1097/01.cji.0000211336.91513.dd. [DOI] [PubMed] [Google Scholar]
- 43.Walsh JT, Kipnis J. Regulatory T cells in CNS injury: the simple, the complex and the confused. Trends Mol Med. 2011 doi: 10.1016/j.molmed.2011.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhou X, Bailey-Bucktrout SL, Jeker LT, Penaranda C, Martinez-Llordella M, Ashby M, Nakayama M, Rosenthal W, Bluestone JA. Instability of the transcription factor Foxp3 leads to the generation of pathogenic memory T cells in vivo. Nat Immunol. 2009;10:1000–1007. doi: 10.1038/ni.1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Komatsu N, Mariotti-Ferrandiz ME, Wang Y, Malissen B, Waldmann H, Hori S. Heterogeneity of natural Foxp3+ T cells: a committed regulatory T-cell lineage and an uncommitted minor population retaining plasticity. Proc Natl Acad Sci U S A. 2009;106:1903–1908. doi: 10.1073/pnas.0811556106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.d'Hennezel E, Yurchenko E, Sgouroudis E, Hay V, Piccirillo CA. Single-cell analysis of the human T regulatory population uncovers functional heterogeneity and instability within FOXP3+ cells. J Immunol. 2011;186:6788–6797. doi: 10.4049/jimmunol.1100269. [DOI] [PubMed] [Google Scholar]
- 47.Rubtsov YP, Niec RE, Josefowicz S, Li L, Darce J, Mathis D, Benoist C, Rudensky AY. Stability of the regulatory T cell lineage in vivo. Science. 2010;329:1667–1671. doi: 10.1126/science.1191996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Van Dyken SJ, Locksley RM. Interleukin-4- and interleukin-13-mediated alternatively activated macrophages: roles in homeostasis and disease. Annu Rev Immunol. 2013;31:317–343. doi: 10.1146/annurev-immunol-032712-095906. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.